TENDON DISORDERS OF THE FOOT AND ANKLE
Clinical Instructor of Orthopaedics, the University of Texas Health
Sciences Center in San Antonio; and Orthopaedic Surgeon, Orthopaedic
Surgery Associates of San Antonio 9150 Huebner Road, San Antonio,
Texas, 78240.
in the posterior compartment of the leg to produce a common tendon, the
Achilles tendon, which inserts into the posterior tuberosity of the
calcaneus. The tendon does not
have
an accompanying synovial sheath, but it is surrounded by a peritenon or
fibrous covering that is derived from the crural fascia. During
steady-state walking, the primary function of the gastrocsoleus muscle
group is to decelerate the tibia as it passes over the foot. This is
accomplished with eccentric muscle contraction. Toe-off is a passive
event during steady-state walking and an active event during
steady-state running or acceleration (20).
Achilles tendon dysfunction is best divided into paratenonitis,
tendinosis, and partial or complete rupture. Paratenonitis is defined
by inflammation of the tissues surrounding, but not including, the
Achilles tendon. Paratenonitis is commonly attributed to athletic
training errors, such as ineffective stretching or warm-up and overuse.
Mechanical factors, such as excessive foot pronation or a tight
Achilles tendon, have also been implicated. Tendinosis is defined by
degenerative changes within the substance of a tendon; these changes
are probably age related and may represent a precursor to partial
tears. Histologic examination of chronic Achilles tendinosis reveals
abnormal fibrous structure, focal hypercellularity, and vascular
proliferation. Curiously, inflammatory cells are not found (2).
Angiographic and microangiographic examinations reveal a paucity of
vasculature in the segment of tendon between 2 and 6 cm proximal to the
insertion (18). Clinical findings suggest that this same area is susceptible to tendinosis and rupture.
pain, prevent further degeneration, and preserve function. The goal of
treating Achilles tendon ruptures is to restore the functional
integrity to the gastrosoleus complex. For both conditions, surgical
and nonsurgical methods are used in an effort to maximize outcome.
over the Achilles tendon that is aggravated by activity. Physical
examination begins with gait analysis; moderate to severe tendinosis
produces an antalgic pattern. Examine the patient in the standing
position to evaluate swelling or fullness related to the Achilles
tendon. Assess calf atrophy by comparison with the contralateral
extremity. Have the patient perform a repeated single-heel rise test.
This is accomplished by having the patient stand at a nearby wall using
hands for balance. The patient lifts the unaffected extremity while
performing repeated single-heel rises on the affected extremity. The
test is positive if the patient is unable to perform the maneuver owing
to pain or if the maneuver causes pain at the Achilles tendon. Then
seat the patient and palpate the posterior leg to assess swelling and
tenderness. Nodular or fusiform swelling typically accompanies
tendinosis.
tendinosis begins with a lateral radiographic view of the distal leg
and hind foot. Look for intratendinous calcification associated with
tendinosis and check the topography of the posterior superior
calcaneus. The presence of a hyperconvex superior tuberosity of the
calcaneus may be associated with distal tendinosis. Although it is not
required for evaluation of Achilles tendinosis or rupture, magnetic
resonance imaging (MRI) is probably the most useful imagining modality.
On a T2-image sequence, tendinosis shows increased signal activity
within the tendon as well as localized thickening, cystic changes, and
even partial tears.
antecedent symptoms or may follow a period of pain associated with
Achilles tendinosis. Rupture is associated with the acute onset of pain
over the Achilles tendon and the loss of plantar flexion power, either
subtle or overt. Occasionally, the patient recalls sensing or hearing a
“pop” at the time of rupture. Examination of the standing patient may
reveal subtle to massive swelling along the posterior leg. With the
patient in a prone position, perform a Thompson’s test by squeezing the
calf at midsubstance and looking for the absence of foot
plantarflexion. When foot plantarflexion is not observed, the test is
considered positive and the diagnosis of ruptured Achilles tendon is
established (41). Palpation of the Achilles
tendon itself may reveal a defect. Failure to find this defect,
however, does not rule out tendon disruption.
identified on MRI, but the diagnosis is usually obvious on clinical
examination as well. MRI is not required for the routine evaluation of
Achilles tendon ruptures.
ranging from small focal areas of degeneration associated with mild
pain and minimal dysfunction through significant areas of degeneration
and partial tearing associated with significant discomfort and loss of
function. Furthermore, tendinosis can be classified with an anatomic
system based on the location of the degeneration relative to the
insertion. Noninsertional tendinosis includes degenerative changes of
the Achilles tendon between the musculotendinous junction to a point
proximal to the insertion. Insertional tendinosis is limited to
degeneration at the Achilles tendon insertion. This entity tends to be
more focal, but similar treatment principles apply.
application of ice, and nonsteroidal anti-inflammatory medication.
Patients with moderate to severe symptoms require immobilization with a
weight-bearing cast or removable cast boot. Once the pain, swelling,
and tenderness have resolved, institute a rehabilitation program. Place
emphasis on stretching the gastrosoleus motor complex. Also correct
training errors related to intensity or frequency of activity.
may be treated by surgical or nonsurgical methods. The ideal treatment
of the acute, complete Achilles tendon rupture remains controversial.
Nonsurgical methods have the advantage of avoiding wound complications,
but they appear to have a higher rerupture rate (14,29).
Patients treated with surgical primary repair have a significantly
lower rerupture rate and a higher degree of satisfaction;
unfortunately, they are also prone to surgical complications such as
deep infection, fistula, and skin or tendon necrosis (14,29)
tendon ruptures, use a non-weight-bearing equinus cast for 6 weeks,
followed by a weight-bearing cast boot for a second 6-week period, then
place a silicone heel wedge in the cast boot and subsequent shoewear.
On the resolution of local warmth and swelling, begin a motion and
strengthening program. Surgical treatment consists of primary repair of
the Achilles tendon. Achilles tendinosis that is recalcitrant to a
prolonged course of immobilization and conservative management requires
surgical debridement and possible reconstruction. Although it is not
required, an MRI may be obtained in order to better delineate the
extent of tendon degeneration.
-
Using general or regional anesthesia and
a proximal thigh tourniquet, make a longitudinal incision parallel to
and 1.5 cm anterior to the medial border of the Achilles tendon.
Because the wound is prone to marginal necrosis and breakdown, exercise
caution when handling soft tissues. By sharp dissection, expose the
Achilles paratenon and incise it longitudinally, allowing complete
inspection of the tendon. -
Degenerative changes are suggested by
changes in local color, swelling, localized tissue edema, cystic
changes, and partial tears. Sharply excise all degenerative sections.
If the functional integrity of the tendon is compromised, perform a
reconstructive procedure. If, however, the remaining tendon remains
functionally competent, carefully repair the subcutaneous tissue with
interrupted absorbable sutures and close the skin with nylon or skin
clips. -
Apply a large, bulky, compression dressing with the foot in a neutral position.
-
Postoperative management:
Ten days after surgery, remove the sutures, place the leg in a
removable cast, and begin a range-of-motion and strengthening program.
After local swelling and warmth have resolved, gradually resume
athletic activity.
in the loss of functional integrity, it must be reconstructed. The
flexor hallucis longus (FHL) tendon transfer provides not only
additional collagen but also an additional motor unit.
-
Make an incision on the medial aspect of
the forefoot from the navicular to the metatarsal head. Identify the
abductor hallucis muscle and release its fascia longitudinally from the
first metatarsal. Retract the muscle to visualize the plantar nerves as
well as the FHL and flexor disitorum longus (FDL) tendons. -
Carefully release the flexor knot of
Henry as well as all fascial connections between the FHL and FDL
tendons. Tenodese the distal FHL tendon with a #2 nonabsorbable suture.
Then divide it just proximal to the tenodesis. -
Then make an incision along the medial
aspect of the Achilles tendon from the calcaneus for as proximal as
necessary. Identify the FHL muscle and its tendon. Pull it into the
proximal wound. Using a quarter-inch drill, make a tunnel through the
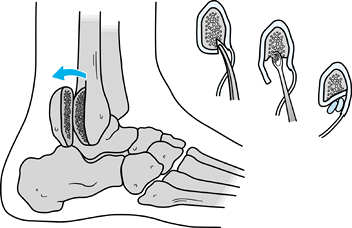
superior tuberosity of the calcaneus, smoothing its edges (Fig. 118.1). Then pass the FHL tendon through the tunnel. With the foot in a
P.3126
plantarflexed position, carefully adjust the tension in an effort to
approximate that of the contralateral Achilles tendon. Then suture the
FHL tendon to itself and to the adjacent Achilles tendon with
nonabsorbable suture. Typically, the remaining section of FHL tendon is
woven across the Achilles tendon defect.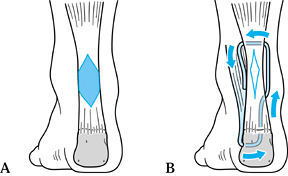 Figure 118.1. Debridement and reconstruction of the Achilles tendon with the FHL tendon. A: The shaded area represents the area of tendinosis and debridement. B: Reconstruction with the FHL tendon. See text for details.
Figure 118.1. Debridement and reconstruction of the Achilles tendon with the FHL tendon. A: The shaded area represents the area of tendinosis and debridement. B: Reconstruction with the FHL tendon. See text for details. -
If further reinforcement is required,
perform a plantaris tendon weave, a turn-down of the central one third
of the Achilles tendon, or a V–Y advancement of the musculotendinous junction. -
Close the subcutaneous tissue with interrupted absorbable sutures and close the skin with nylon or skin clips.
-
Apply a large bulky compression dressing with the foot in a plantarflexed position.
-
Postoperative management:
Ten days after surgery, remove the sutures and apply another
plantarflexed cast. Between 2 and 4 weeks after surgery, gradually
bring the foot up to a plantigrade position and continue in a cast. At
5 weeks after surgery, use a removable cast boot so that
range-of-motion and strengthening exercises can be instituted. At 12
weeks, discontinue immobilization. After local swelling and warmth have
resolved, gradually resume athletic activity.
 |
|
Figure 118.2. Reconstruction of Achilles tendon with turn-down flap. A: Abnormal segment of Achilles tendon has been excised, leaving normal ends proximal and distal. B: A segment of proximal tendon is harvested. The lateral edge of the tendon has been left intact proximally. C: The proximal end is tubularized and then pivoted downward. D: The graft has been passed through the calcaneal tunnel and sutured back to itself.
|
-
With the patient in the prone position,
make a longitudinal incision from the midportion of the calf in the
midline, extending distally to the posteromedial heel. Expose the
posterior calcaneus and Achilles tendon, and excise the scar in the
defect. -
Using a 4.5 mm drill, make a transverse tunnel in the calcaneal tuberosity, and enlarge it as needed using curets.
-
Divide the lateral half of the Achilles
tendon tranversely at the proximal musculotendinous junction, just up
to the lateral edge. Leave the lateral edge intact as a cuff. Split the
proximal tendon longitudinally both laterally and in the midline. In
the midline, turn the tendon down, stopping 1 inch proximal to the site
of rupture. Separate this segment from the underlying muscle with a
pair of scissors. -
Insert several stay stitches of 0 absorbable suture at the pivot point to prevent distal tearing.
-
Form a tube of the now-distal end by
sewing its medial and lateral sides together with a running 0
absorbable suture. Weave a #1 nonabsorbable suture through the end of
the graft, and pass the suture through the calcaneal tunnel. Place the
ankle in 20° of plantarflexion and tension the graft. Sew it back to
itself with the nonabsorbable suture. Use multiple stitches of 0
absorbable suture to augment this repair and to secure the graft to the
calcaneal periosteum at the medial and lateral ends of the tunnel. -
Divide the plantaris tendon proximally,
leaving its calcaneal insertion intact, and fan it out as a covering
for the reconstruction. -
Proximally repair the remaining medial half of the tendon to the remaining lateral cuff with interrupted 0 absorbable sutures.
-
Close the subcutaneous tissue and skin of
both wounds in layers. Apply a short-leg posterior splint with the
ankle in 20° of plantarflexion. -
Postoperative management:
Remove the skin sutures at one week and apply a short-leg
non-weight-bearing cast, with the ankle in 20° plantarflexion, which is
worn for 5 weeks. Then apply a removable orthosis with the ankle at
neutral for 4 to 6 more weeks. Allow active ankle exercises for motion
without resistance during this time. Begin passive motion and
soft-tissue mobilization between 8 and 10 weeks after surgery. Swimming
and cycling can begin 4 months after surgery, followed by
plantarflexion-resistive exercises. A permanent loss of power must be
expected, but running and jumping are possible. Return to sports
requires a minimum of 12 months recovery.
-
Using general or regional anesthesia and
a proximal thigh tourniquet, make a longitudinal incision parallel to
and 1.5 cm anterior to the medial border of the Achilles tendon.
Because these wounds are prone to marginal necrosis and breakdown,
exercise caution when handling soft tissues. -
Sharply dissect directly to the Achilles
paratenon. Incise the paratenon longitudinally, allowing complete
inspection of the tendon rupture. Debride the rupture site of hematoma. -
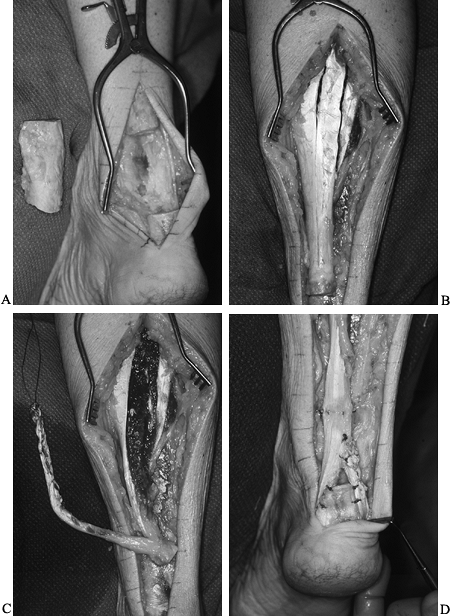
Approximate the tendon ends and do a primary repair with a core suture of #3 nonabsorbable braided suture (Fig. 118.3).
Follow with a circumferential peripheral tendon repair with braided
nonabsorbable suture. Weave the plantaris across the repair site and
secure it with 2-0 braided nonabsorbable sutures.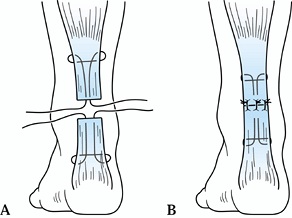 Figure 118.3. Primary repair of an acute Achilles tendon rupture with a core suture. A: Insertion of sutures. B: Completed repair.
Figure 118.3. Primary repair of an acute Achilles tendon rupture with a core suture. A: Insertion of sutures. B: Completed repair. -
Carefully repair the subcutaneous tissue with multiple absorbable sutures and close the skin with fine nylon or skin clips.
-
Apply a large, bulky compression dressing with the foot in a plantarflexed position.
-
Postoperative management:
Remove the sutures 10 days after surgery and apply a non-weight-bearing
cast, with the foot in a plantarflexed position. Over the next 4 weeks,
gradually bring the position of the foot to a plantigrade position. At
the 4-week postoperative visit, apply a removable cast boot and begin
range-of-motion and low-resistance exercises. At the 8-week
postoperative
P.3127P.3128
visit,
begin weight bearing. At 12 weeks after surgery, immobilization can be
discontinued. Gradually resume athletic activity once local warmth and
swelling have resolved. -
Delay postsurgical stretching of the
Achilles tendon until local swelling, warmth, and tenderness have
resolved. Early and aggressive stretching may result in lengthening of
the gastrosoleus complex with concomitant loss of power. Once local
conditions permit, warm-up and stretching of the entire lower extremity
remain important tools in the enhancement of performance and reduction
of repeat injury.
treated with either surgical or nonsurgical intervention. The rerupture
rate appears to be higher in those patients treated with cast
immobilization alone (14,29), particularly in those treated with less than 8 weeks of immobilization (19).
complications because of the subcutaneous position of the tendon.
Surgical technique requires preservation of full-thickness skin flaps,
gentle soft-tissue handling, and tension-free closure. Before
immobilization of the foot at surgery, verify the viability of the skin
overlying the Achilles tendon, with the foot in the proposed position
of immobilization.
complete Achilles tendon ruptures, we prefer early, primary repair for
healthy, active individuals. We believe that this treatment modality
allows a faster and more complete recovery.
posterior tibial muscle forms a tendon that courses behind the medial
malleolus, turns anteriorly, and inserts directly into the navicular
tuberosity. The tendon is surrounded by a synovial sheath. The position
of the tendon relative to the ankle and subtalar joint axes of rotation
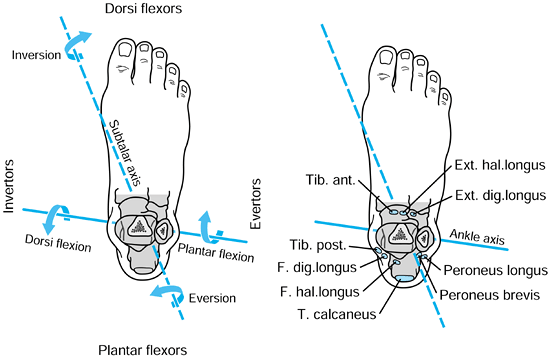
defines its function as an invertor and plantarflexor of the foot (Fig. 118.4) (22).
Insufficiency of the posterior tibial tendon (PTT) results in the
production of an asymmetric flatfoot identified by heel valgus, midfoot
collapse and abduction, and forefoot pronation. Insufficiency may be
related to acute or chronic tenosynovitis or partial or complete
rupture. It is unknown why the PTT is predisposed to injury, but it may
be related to a zone of relative hypovascularity within the tendon
located behind and distal to the medial malleolus (11).
PTT dysfunction occurs more frequently in patients with diabetes,
hypertension, and obesity compared with the general population (13).
 |
|
Figure 118.4.
Relationship of the tendons crossing the ankle relative to the axes of rotation for the ankle and subtalar joints. (Redrawn from Mann RA. Biomechanics of the Foot. In: American Academy of Orthopaedic Surgeons: Atlas of Orthotics. St Louis: Mosby–Year Book, 1985, with permission.) |
impairment to the lower extremity. The primary goal of treatment is to
re-establish the function of the PTT, when possible. For patients with
advanced disease, the substitution or addition of the FDL tendon may be
required. The most advanced stages of dysfunction are not amenable to
soft-tissue reconstruction and require identification and treatment of
fixed deformities.
viewed from behind, the patient with PTT dysfunction may have decreased
heel inversion between flatfoot and toe-off, and in advanced cases, an
antalgic gait may be noted. Examination of the standing patient may
reveal varying degrees of swelling over the course of the PTT, as well
as heel valgus, midfoot collapse, and abduction. Ask the patient to
perform a repeated single-heel rise test. This is accomplished by
having the patient stand at a nearby wall, using the hands for balance.
The patient lifts the unaffected extremity while performing repeated
single-heel rises on the affected extremity. Patients with
tenosynovitis or mild degenerative changes are able to perform the
maneuver repeatedly with evidence of good heel height and heel
inversion, but this is typically a painful maneuver. In advanced
stages, heel height and heel inversion decrease. Finally, patients with
complete dysfunction of the PTT are unable to perform the maneuver.
Then seat the
patient
and palpate the posterior leg to assess swelling over the PTT and
associated tenderness. Tenderness at the sinus tarsi may indicate
lateral impingement in advanced cases. Early findings include supple
motion at the ankle, hindfoot, midfoot, and forefoot. With progression
of the disorder, subtalar motion becomes limited and the heel
eventually becomes fixed in a valgus position, midfoot abduction
increases with a concomitant decrease in midfoot adduction, and
forefoot pronation becomes fixed, which paradoxically produces fixed
forefoot varus when the heel is held in a neutral position. In the most
advanced cases, Achilles contracture produces equinus deformity, which
is most easily appreciated when ankle motion is evaluated with the heel
held in a neutral position. Manual motor testing reveals loss of
function varying from slight weakness associated with tenosynovitis to
complete loss of function associated with chronic tendinosis or
complete rupture.
views of the foot and ankle. Valgus tilt of the ankle mortise increases
the amount of chronic stress across the posterior tibial tendon. Loss
of ankle joint height, especially at the lateral joint line, is a risk
factor for rapidly progressive arthrosis after hindfoot fusion. An
enlarged or accessory tarsal navicular is a predisposition to PTT
dysfunction. Assess foot alignment, with particular attention to
midfoot collapse on the lateral view and midfoot abduction on the
anteroposterior view. Advanced imaging of the PTT is best accomplished
with MRI (4). The tendon is normally round to
oval in shape with a low, homogenous signal. Tenosynovitis is easily
identified by increased fluid surrounding the tendon. Degeneration and
partial and complete tears are identified on the T2 sequence by
thickening, increased signal activity, and cystic changes.
synovitis; tendinosis manifested by partial or complete tears, leading
to loss of the functional integrity; tendinosis with supple hind foot
valgus; and tendinosis associated with fixed deformity of the subtalar
and transverse tarsal joints.
reduction or modification in activity. For advanced or recalcitrant
symptoms, immobilize the leg in a short-leg walking cast or removable
cast boot. For risk factors such as excessive pronation, use orthotic
devices.
that discussed earlier. Immobilization for 6 to 8 weeks may be
required. Occasionally, symptoms recur immediately on discontinuation
of treatment. For patients unwilling to pursue surgical treatment, a
custom ankle-foot orthosis is indicated.
nonoperative treatment is predicated on the presence of hindfoot and
forefoot deformity. Patients with mild to moderate deformity may be
treated in a custom ankle-foot orthosis. Patients with severe deformity
require more extensive bracing with a double upright brace and medial T-strap.
tendinosis with MRI to evaluate the extent of tendon degeneration.
Patients with advanced tendinosis with loss of PTT function do not
require evaluation by MRI. The presence of hindfoot valgus, supple or
fixed, along with the presence of any fixed deformity including
Achilles tendon
contracture, must be appreciated before surgical intervention.
adequate course of conservative management require debridement of the
PTT sheath (40).
-
Using general or regional anesthetic and
a proximal tourniquet, make a linear incision over the course of the
PTT from the tip of the medial malleolus to the navicular. Sharply
dissect down to the tendon sheath, which is longitudinally divided
throughout the length of the surgical wound. -
Synovitis is manifested by the presence
of an effusion, synovial proliferation, and increased vascular
activity. Systematically excise the synovium. -
Occasionally, proximal exposure of the
PTT is required. Extend the skin incision proximally over the course of
the PTT. Leave a 1 cm section of PTT sheath and flexor retinaculum
intact at the medial malleolus. Once the tendon is completely exposed,
carefully inspect it. The treatment of tendon tears is discussed later. -
On completion of the procedure, loosely
close the tendon sheath, followed by subcutaneous tissue closure with
interrupted absorbable suture and skin closure with nylon or skin
clips. Immobilize the foot and ankle in a neutral position. -
Postoperative management:
Remove sutures or skin clips 10 days after surgery and apply a
removable cast. Begin range-of-motion exercises and allow weight
bearing as tolerated. At 4 weeks after surgery, begin a strengthening
program. Permit a gradual return to activities once local swelling and
warmth resolve.
conservative management require surgical intervention in a timely
manner in order to reduce the risk of permanent structural changes.
-
Expose the PTT sheath and debride as
previously described. Using sharp resection, completely remove the
degenerative portions of the tendon, which are indicated by color
changes, thickening, loss of tendon consistency, cystic changes, and
partial tears. If necessary, debride the entire tendon from the
navicular to a point proximal to the degenerative changes. -
On completion of tendon debridement,
inspect the deltoid and spring ligaments. Reconstruct excessive laxity
in the spring ligament by excision and imbrication of redundant tissue. -
Harvest the FDL tendon by extending the
incision to the medial forefoot. Identify the abductor hallucis muscle
and release its fascia longitudinally from the first metatarsal.
Plantar retraction of the muscle allows visualization of the plantar
nerves as well as the FHL and FDL tendons. Carefully release the flexor
knot of Henry as well as all fascial connections between the FHL and
FDL tendons. Perform a distal tenodesis with a #2 nonabsorbable suture.
Divide the FDL tendon just proximal to the tenodesis. -
Now turn attention to the proximal aspect
of the surgical exposure. Identify the FDL tendon posterior to the PTT
sheath, where it is secured and retracted proximally. -
Make a quarter-inch drill hole through
the medial portion of the navicular. Take care not to violate the
adjacent articular surfaces. Pass the free end of the FDL tendon from
the plantar to dorsal side of the navicular. No attempt is made to
place the tendon transfer within the posterior tibial tendon sheath.
Plantarflex and invert the foot and increase tension across the tendon
transfer. Secure the transfer with multiple interrupted nonabsorbable
sutures. Occasionally, the free end of the tendon can be sutured to a
more proximal portion of the FDL tendon. -
Repair the abductor hallucis muscle to
the first metatarsal. Close the subcutaneous tissue and close the skin
with nylon suture or skin clips. Immobilize the foot and ankle in a
plantarflexed and inverted position. -
Postoperative management:
After 10 days, remove the sutures or skin clips. Apply a
non-weight-bearing short-leg cast, with the foot maintained in a
plantarflexed and inverted position. At 4 weeks, place the foot in the
neutral position and fit a removable cast boot. At 6 weeks after
surgery, start range-of-motion exercises for the foot and ankle, and
allow weight bearing to tolerance with the cast boot. Institute a
strengthening program with an elastic band after 8 weeks. Activities
are gradually resumed once local warmth and swelling are resolved.
a valgus position. Patients with posterior tibial tendinosis and
flexible hindfoot valgus require debridement and reconstruction of the
posterior tibial tendon, along with correction of the propensity for
hindfoot valgus. This is accomplished with medial displacement
calcaneal osteotomy as well as FDL tendon transfer (16,28,31).
The osteotomy reduces the lateral displacement of the heel and
decreases the valgus forces produced by weight bearing and the pull of
the gastrosoleus complex.
-
Approach the calcaneus through a lateral incision in
P.3131
line with the posterior border of the fibula with blunt dissection to
localize the sural nerve. Expose the lateral border of the calcaneus
from the posterior aspect of the posterior facet of the subtalar joint
to the inferior border of the calcaneus. -
Use a sagittal saw to osteotomize the
calcaneus just posterior to the posterior facet. Carefully approach and
divide the medial cortex of the calcaneus. On completion of the
osteotomy, use a broad osteotome to elevate the medial soft tissues
carefully. At this point, translate the posterior tuberosity of the
calcaneus medially approximately 1 cm. -
Temporarily fix the osteotomy with
K-wires. Verify by examination that heel valgus has been corrected.
Accomplish permanent fixation with a single partially threaded 7.0 mm
screw advanced from the posterior tuberosity into the anterior process
of the calcaneus. -
Then debride and reconstruct the
posterior tibial tendon as previously described. Apply a bulky dressing
and splint the foot and ankle in a plantarflexed and inverted position. -
Postoperative management:
After 10 days, remove the sutures or skin clips. Apply a
non-weight-bearing short-leg cast with the foot in a plantarflexed and
inverted position. At 4 weeks, place the foot in the neutral position
and apply a removable cast boot. At 6 weeks, repeat radiographs; if
union appears eminent, allow weight bearing to tolerance with a cast
boot. Institute a strengthening program with an elastic band after 8
weeks. Gradually resume activities once local warmth and swelling are
resolved.
is not amenable to soft-tissue reconstruction. When the deformity is
limited to the subtalar joint, and the remainder of the foot remains
supple (i.e., the absence of fixed forefoot varus), then treatment with
an isolated subtalar arthrodesis is possible. The surgical technique
for hindfoot arthrodesis is described in Chapter 115. Take care to produce a neutral heel and plantigrade foot before the placement of internal fixation.
will eventually produce fixed forefoot deformities, namely, forefoot
varus. The correction of the subtalar deformity alone will not produce
a plantigrade foot. Fixed forefoot deformity is best addressed with a
double or triple arthrodesis. The triple arthrodesis increases the
likelihood of talonavicular fusion and is used in patients at risk for
nonunion (e.g., those who smoke or who have diabetes, rheumatoid
arthritis, or excessive bone loss). On completion of the arthrodesis,
final assessment of foot position allows a true evaluation of Achilles
tendon contracture. Occasionally, a triple hemisection, gastrocnemius
recession, or an open Achilles tendon lengthening is necessary. Failure
to identify Achilles tendon contracture results in inordinate stress
across the transverse tarsal arthrodesis and increases the likelihood
of talonavicular malunion and nonunion.
nonsurgical methods as well as those managed with soft-tissue
reconstruction are placed on programs designed to maintain motion of
the foot and ankle, and to increase strength of the posterior tibial
muscle or the transferred FDL muscle. Orthotics designed to resist
excessive pronation and hindfoot valgus are also prescribed as needed.
posterior tibial tendon dysfunction, synovitis, or mild tendinosis to
progress to a more advanced stage requiring more invasive and more
morbid intervention.
the lateral compartment of the leg. Distally, they form individual
tendons, which pass behind the lateral malleolus to turn anteriorly
toward their respective insertions at the base of the fifth metatarsal
and the base of the first metatarsal. At the lateral malleolus, the
peroneus brevis tendon remains anterior to the peroneus longus tendon.
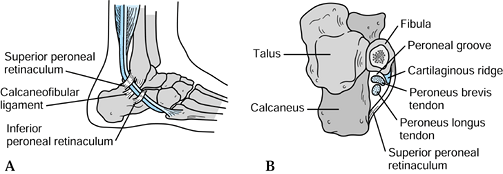
The tendons are retained behind the lateral malleolus by the superior
peroneal retinaculum (14), a structure that originates from the periosteum on the posterolateral ridge of the fibula (5). The peroneal groove or retromalleolar sulcus is a shallow bony groove (9) that is deepened by a fibrocartilaginous ridge (Fig. 118.5).
The position of the tendons relative to the axis of rotation of the
ankle and subtalar joints determine their function as plantar flexors
and evertors of the foot (Fig. 118.4).
 |
|
Figure 118.5.
Anatomic relationships at the lateral aspect of the ankle. Note on the cross section that the peroneal groove is supplemented by a fibrocartilaginous ridge. |
groove to a position anterior to the lateral malleolus. The injury
occurs as a result of sudden, forceful, passive dorsiflexion of the
inverted foot with reflex contraction of the PTs (8,27,39); an association with chronic lateral ankle instability has also been reported (12).
Dislocation of the peroneal tendons out of the peroneal groove is
associated with a variety of underlying pathoanatomic findings,
including a tear of the superior peroneal retinaculum, elevation of the
superior retinaculum off the lateral border of the fibula with
concomitant dissection of the tendon beneath the lateral fibular
periosteum, and fracture of the posterolateral margin of the fibula.
the posterolateral border of the fibula may occur as a clinical or
subclinic entity. This condition has been implicated as a major
causative factor in the development of longitudinal tears of the
peroneus brevis tendon (17,36).
Anatomic factors associated with longitudinal tears of the peroneus
brevis tendon include laxity of the superior peroneal retinaculum,
compression of the peroneus brevis tendon by the overlying peroneus
longus tendon (17,32,36),
the presence of peroneal musculature at the peroneal groove, and
finally, the presence of an anomalous peroneal muscle such as the
peroneus quartus muscle (38). A longitudinal tear of the peroneal tendons has also been described after acute and chronic lateral ankle inversion injury (3,33).
maintained in a reduced position by a cast. Recurrent or chronic
dislocation requires surgical stabilization by soft-tissue or bony
reconstruction, or both. Longitudinal ruptures associated with chronic
subluxation of the peroneal tendons may respond to a period of
immobilization. Surgical treatment requires the identification and
correction of all pathoanatomic features in addition to the debridement
and repair of the longitudinal tendon rupture.
especially in the acute setting. Clinical findings are very similar to
that of a lateral ankle ligament sprain. Furthermore, peroneal tendon
injury can occur concomitantly with lateral ankle ligament injury.
over the course of the PTs as well as the lateral border of the fibula.
The patient may offer a history of forceful, passive, dorsiflexion of
the foot and the detection of a “pop” at the time of injury. Many
patients are able to describe accurately the translation of the tendon
out of the peroneal groove. The tendon typically reduces spontaneously.
Often, the patient presents after the condition becomes recurrent or
chronic. Examination of the acute injury reveals swelling and
tenderness behind the lateral malleolus (1,8,10,24,27).
This is in contrast to the inversion lateral ankle sprain, which is
associated with tenderness anterior to the lateral malleolus.
Observation of the contralateral extremity may reveal asymptomatic
physiologic subluxation. With the foot held in a plantarflexed and
everted position, active dorsiflexion may result in apprehension,
subluxation, and even dislocation. Dislocation is typically quite
painful and is not elicited as a routine part of our examination.
Gentle palpation of the PTs at the peroneal groove while the foot is
taken through active circumduction may reveal the presence of nodule
formation or snapping. Complete the examination with evaluation of
lateral ankle ligament stability.
brevis tendon associated with chronic subluxation present with acute or
chronic lateral ankle pain localized to the retrofibular region. This
pain may be associated with intermittent or persistent swelling, a
recurrent “popping” sensation, or lateral ankle instability.
Examination of the lateral ankle reveals mild to moderate swelling over
the course of the peroneal tendons at the peroneal groove.
Palpation
of the region while the ankle is actively circumducted reveals nodule
formation and possibly a “popping” phenomenon. Resisted ankle
dorsiflexion may confirm the presence of physiologic subluxation of the
peroneal tendons. Resisted manual motor testing may reproduce pain as
well as weakness of the respective muscles. Once again, lateral ankle
instability must be ruled out.
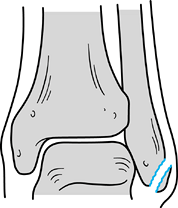
dislocation rarely demonstrates an avulsion fracture off the rim of the
lateral malleolus (Fig. 118.6) (21).
Obtain stress views if lateral ankle instability is an associated
finding. For cases that present a diagnostic dilemma, use MRI to detect
tenosynovitis, partial or complete ruptures, subluxation, dislocation,
competency of the superior peroneal retinaculum, the presence of a
large distal peroneus brevis muscle insertion, the competency of
lateral ankle ligaments, and internal derangement of the ankle and
subtalar joints.
 |
|
Figure 118.6. Oden type III peroneal tendon dislocation with the characteristic rim fracture.
|
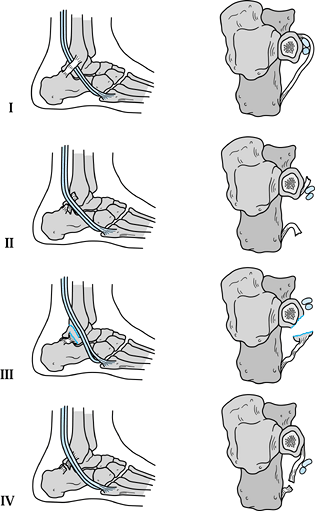
In a type I injury, the superior peroneal retinaculum remains in
continuity with the periosteum overlying the lateral border of the
fibula; the tendons translate out of the peroneal groove and dissect
beneath the periosteum, forming a false pouch. In the type II injury,
the superior peroneal retinaculum is disrupted by an anterior tear. The
type III injury is marked by an avulsion fracture off the posterior
fibular margin. Finally, the type IV injury is defined by a posterior
tear of the superior peroneal retinaculum.
 |
|
Figure 118.7.
Oden classification of peroneal tendon dislocation. (Redrawn from Oden RF. Tendon Injuries about the Ankle Resulting from Skiing. Clin Orthop 1987;216:63, with permission.) |
tendons with a well-fitted, non-weight-bearing, short-leg cast applied
with the foot in slight plantarflexion. Window the cast over the
peroneal tendons at the peroneal groove. Place one-quarter to one-half
inch of felt padding over the tendons and reduce the window. Instruct
the patient to adjust the thickness of the felt pad for comfort.
Immobilize the foot for 6 weeks, at which time, the stability of the
peroneal tendons should be checked. An additional 4 weeks of casting
may be necessary. Rehabilitation focuses on motion, strength, and
proprioception. Occasionally, the patient is able to detect recurrent
dislocation within the cast. These patients, as well as all patients
with recurrent or chronic dislocation, will not respond to nonsurgical
treatment methods (1,15,23,24,25,26 and 27,34,42).
peroneal tendon is initially symptomatic. Treatment includes decreased
activity, application of ice, and oral nonsteroidal anti-inflammatory
agents. Patients that fail to respond
require enforced rest with a weight-bearing cast. A taping program may allow continued athletic activity.
findings associated with peroneal tendon dislocation is very difficult.
Therefore, it is impossible to anticipate the exact nature of the
surgical repair and reconstruction. The patient must be prepared for
debridement of the peroneal tenosynovium; excision of excessive distal
peroneus brevis muscle insertion; resection of an anomalous peroneal
tendon such as the peroneus quartus; deepening of the peroneal groove;
imbrication and reconstruction of the superior peroneal retinaculum;
and finally, debridement, repair, or tenodesis of the peroneal tendons.
Failure to address contributing pathology or concomitant injury, may
result in the persistence of symptoms. An MRI and a computed tomography
(CT) scan can be used to delineate pathologic findings further, but
these are not used for routine evaluation of peroneal dislocation or
partial longitudinal tears.
-
Utilizing a general or regional anesthetic and a proximal thigh tourniquet, make an L-shaped
incision over the course of the peroneal tendons. Limit the initial
exposure to 6 cm, with the majority of the incision proximal to the tip
of the lateral malleolus. If dissection is carried distal to the
lateral malleolus, take care to avoid the sural nerve and its
communicating branch, which occasionally is found crossing the course
of the peroneal tendons. -
Expose the superior peroneal retinaculum
and verify its integrity by manipulation of the foot and ankle with
significant digital pressure posterior and medial to the peroneal
tendons. Sharply divide the retinaculum and synovial sheath in line
with the posterior border on the lateral malleolus. Complete the
exposure by systematic synovectomy and tenolysis of the peroneal
tendons. If the dissection is carried distal to the tip of the lateral
malleolus, leave a 1 cm cuff of superior peroneal retinaculum and
underlying synovial sheath intact. -
Resect peroneus brevis muscle that lies
within the peroneal groove off the tendon. At this point, dislocate the
peroneal tendons. Debride and repair partial longitudinal tears as
described below. If the bony peroneal groove appears shallow or convex,
a deepening procedure is indicated (Fig. 118.8).![]() Figure 118.8.
Figure 118.8.
Treatment of peroneal tendon dislocation with a groove-deepening
procedure. (Redrawn from Arrowsmith SR, Fleming LL, Allman FL.
Traumatic Dislocation of the Peroneal Tendons. Am J Sports Med 1983;11:142, with permission.) -
Make a longitudinal incision through the
overlying periosteum and expose the underlying cancellous bone by
elevating an osteoperiosteal flap. Deepen the bony groove by removing
the cancellous bone, replacing the osteo-periosteal flap, and smoothing
the remaining cancellous surfaces with bone wax. Reduce the tendons and
their excursion and stability by passive motion of the foot and ankle. -
At this point, repair and imbricate tears
of the superior peroneal retinaculum. In the more common situation in
which the superior peroneal retinaculum and the lateral fibular
periosteum are elevated off the lateral border of the fibula, several
pathoanatomic features must be addressed. First, obliterate the false
pouch created by elevation of the lateral fibular periosteum.
Accomplish this by curettage of the overlying lateral fibula. Next,
advance the superior peroneal retinaculum into multiple drill holes
placed through the posterolateral border of the fibula. Use multiple
nonabsorbable sutures to complete a tight reconstruction. Finally,
advance the remaining superior peroneal retinaculum and lateral fibular
periosteum posteriorly, and repair them over the underlying
reconstruction. This procedure obliterates the false pouch, and
advances and reconstructs the superior peroneal retinaculum. -
Once the repair is complete and its
integrity verified, reapproximate the subcutaneous tissue with
absorbable suture and close the skin with nylon or skin clips.
Immobilize with the foot and ankle with a compression dressing in
neutral position. -
Postoperative management:
At 10 days after surgery, apply a removable cast boot for
non-weight-bearing ambulation. Teach range-of-motion exercises. At 6
weeks after surgery, begin weight bearing, as well as proprioception
and strengthening exercises. Gradually resume activities once local
swelling and warmth have resolved.
-
Next, incise the superior retinaculum
posterior to the posterolateral border of the fibula. Leave a cuff of
tissue attached to the fibula for subsequent repair and imbrication.
Initially, complete the exposure to the tip of the fibula and perform a
complete synovectomy and tenolysis. When present, resect a distal
insertion of the peroneus brevis muscle. Carefully retracted and
inspect each tendon. -
If the initial exploration is negative,
extend the exposure distally over the course of the peroneal tendons.
Leave a 1 cm cuff of superior peroneal retinaculum and synovium intact
inferior to the tip of the fibula to act as a pulley. -
Debride partial longitudinal tears with
associated fibrillation to normal tendon. After debridement, if the
remaining tendon appears functional, repair the longitudinal tear with
running Polydioxanone (PDS; Ethicon, Inc., Wayne, NJ) or nylon suture.
If the tendon appears flattened, it may be tubularized with a running
suture. If after debridement the remaining tendon does not appear to be
functional, perform a tenodesis between the peroneus brevis and longus
tendons proximal and distal to the peroneal groove, and sharply excise
the pathologic section of tendon. At this point, take care to establish
that the tendons demonstrate full excursion and stability within the
peroneal groove. Instability must be addressed with the techniques
described in the previous section. -
Close the peroneal sheath with a running
nylon suture. Repair the subcutaneous tissue and close the skin with
nylon suture or skin clips. Apply a compression dressing with the foot
and ankle immobilized in a neutral position. -
Postoperative management:
Ten days after surgery, apply a removable cast boot, and begin
non-weight-bearing ambulation and range-of-motion exercises. At 6 weeks
after surgery, progress to weight bearing to tolerance with the cast
boot and institute a proprioception and strengthening program.
Gradually resume activities when local warmth and swelling resolve.
treatment program, focus rehabilitation on ankle and subtalar
range-of-motion, ankle and subtalar stability, peroneal motor
strengthening, and finally, lower extremity proprioception. Resume full
athletic activity only when local warmth and swelling have resolved and
the patient demonstrates full pain-free range of motion without
evidence of tendon or joint instability.
tendons fails to reveal significant pathologic findings. At this point,
do not hesitate to extend the exposure distally beyond the tip of the
fibula. Again, take care to maintain a cuff of peroneal retinaculum and
synovial sheath to function as a distal pulley.
soft-tissue techniques fail to provide adequate stability, do not
hesitate to perform a sliding osteotomy of the fibula (6) or a reconstruction using a lateral slip of the Achilles tendon (15).
degree of suspicion. When it is detected, concomitant injury must be
identified and treated in order to maximize the functional outcome.
Individualize surgical treatment and address each identifiable
pathologic condition.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
S, Michelson, J, Jahss, M. Clinical Significance of Magnetic Resonance
Imaging in Preoperative Planning for Reconstruction of Posterior Tibial
Tendon Ruptures. Foot Ankle 1992;13:208.
MJ, Sobel M, Bohne WHO. Lateral Ankle Instability as a Cause of
Superior Peroneal Retinacular Laxity: An Anatomic and Biomechanical
Study of Cadaveric Feet. Foot Ankle 1993;14:330.
AE, Scott WN, Sculco TP, Patterson AH. Rupture of the Tendo Achillis.
An Objective Assessment of the Surgical and Non-surgical Treatment. J Bone Joint Surg 1976;58-A:990.
MA, Noyez JF, Mulier JC. Recurrent Dislocation of the Peroneal Tendons:
Results of Rerouting the Tendons under the Calcaneofibular Ligament. Am J Sports Med 1986;14:148.
MS, Corrigan J, Thompso F, Schon L. Tendon Transfer Combined with
Calcaneal Osteotomy for Treatment of Posterior Tibial Tendon
Insufficiency: A Radiologic Investigation. Foot Ankle 1995;16:712.
GC, Manoli A. A New Operative Approach for Flatfoot Secondary to
Posterior Tibial Tendon Insufficiency: A Preliminary Report. Foot Ankle 1997;18:206.
A, Wolf M. Subluxation of the Peroneal Tendons: A Case Treated by
Rerouting the Tendons under the Calcaneofibular Ligament. J Bone Joint Surg 1975;57-A:115.
M, Geppert MJ, Olson EJ, Bohne WHO. The Dynamics of Peroneus Brevis
Tendon Splits: A Proposed Mechanism, Technique of Diagnosis, and
Classification of Injury. Foot Ankle 1992;13:413.