Sternoclavicular and Acromioclavicular Joint Injuries
-
General information
-
Anatomy and mechanism.
The sternoclavicular joint is a diarthroidal joint between the medial
clavicle and the clavicular notch of the sternum. Though there is
little intrinsic osseous stability, the sternoclavicular ligaments are
reinforced by the costoclavicular ligaments, disc ligament,
interclavicular ligament, and joint capsule; thus explaining the rarity
of this injury.The sternoclavicular joint is the major articulation
between the axial and appendicular skeleton. The majority of
scapulothoracic motion occurs through the sternoclavicular joint, which
allows approximately 45 degrees of rotation around its long axis.
Injuries to the sternoclavicular joint represent only 3% of shoulder
girdle injuries (1).A sternoclavicular injury is always a high-energy event,
and, therefore, other injuries should be expected. Due to the posterior
proximity of critical structures such as the great vessels, phrenic
nerve, trachea, and esophagus, associated injuries should be diagnosed
promptly.The mechanism of injury can either be from a direct blow
to the anterior clavicle causing a posterior dislocation or an indirect
medial force vector to the shoulder. If the medial force drives the
scapula posteriorly (retracted) along the thorax, the sternoclavicular
joint dislocates anteriorly, and if driven anteriorly (protracted), the
sternoclavicular joint dislocates posteriorly. -
Classification. The joint may sustain a simple strain (Type I) which is not dislocated but painful, have subluxation (Type II), or frank dislocation (Type III), depending on the degree of ligament disruption (2). More importantly, sternoclavicular dislocations are described according to the direction of dislocation, anterior or posterior dislocation.An important point to distinguish is the possibility of
a medial clavicular physeal fracture which can displace anteriorly or
posteriorly as well, thus mimicking a dislocation. This physis does not
close until the early 20s and should be suspected under the age of 25.As an aside, there is an atraumatic type of dislocation
due to ligamentous laxity, but emphasis in this chapter will remain on
the traumatic variety.
-
-
Diagnosis
-
History and physical exam.
The history always is significant for a high-energy mechanism, usually
a motor vehicle collision. The patient should be asked about the
presence of shortness of breath and difficulty breathing or swallowing.
Hoarseness and stridor should be documented. Pain is well localized and
associated with swelling and ecchymosis. There is usually a palpable
and mobile prominence just anterior and lateral to the sternal notch in
the case of the more common anterior dislocation, or perhaps a
puckering of the skin with a sense of fluctuance due to a posterior
dislocation. Chest auscultation and a thorough neurovascular exam to
the ipsilateral extremity is important to document early. -
Radiographs. A serendipity x-ray view of the shoulder is a 40-degree cephalic tilt view centered on the manubrium (3). In this view, an anterior dislocation will be manifested with a superior appearing clavicular head.Once suspected, a computed tomography (CT) examination
with 2-mm cut intervals should also be obtained to visualize the
location and extent of
P.218
dislocation,
evaluate the retrosternal region for soft tissue injury, differentiate
between medial clavicle fractures, or possibly elucidate a physis (when
it appears above the age of 18) injury.
-
-
Treatment
-
Nonoperative.
The majority of sternoclavicular injuries are anterior dislocations,
and these should be treated nonoperativley with the expectation of good
functional results and usually with complete resolution of pain (3).
Cosmetic asymmetry will remain, closed reduction will not remain
reduced, and no brace has been proven to be efficacious in this regard.
This expectant result also holds true for the growth plate injuries
which are displaced anteriorly. -
Operative. An
acute posterior dislocation should undergo a manipulative reduction to
unlock the retrosternal clavicular head. The rationale for the need for
closed reduction relates to the concern that impingement on critical
structures may yield late sequelae from erosion or irritation (4).A pointed bone tenaculum may be useful to grab the head
of the clavicle and pull it back to its proper relation to the
manubrium. A roll between the shoulder blades while the patient is
supine, in combination with lateral traction of the abducted arm, is a
helpful adjunctive maneuver. Due to possible violation of critical
structures in the mediastinum, anesthesia should always be on hand to
manage the airway, and a thoracic surgeon should always be on standby
during the procedure. Performing the reduction maneuver under general
anesthesia with optimum airway control should be considered.Many authors have described techniques for stabilization
of the unstable sternoclavicular joint using various tendon
reconstructions and/or Kirschner wires with mixed results (5). A warning against the use of smooth wires is restated throughout the literature due to the problem of migration. -
Follow-up. A
sling may be used for 1 month to support the extremity during the acute
phase of pain during a period of relative immobility. Motion and
function should be allowed to advance as discomfort allows. Shorter or
longer periods with relative rest are required according to which type
(I, II, or III) dislocation is present. The patient may need
reassurance for months during a period of gradually resolving symptoms. -
Complications.
Retrosternal dislocations are frequently missed, likely due to the lack
of physical exam findings in the context of a multiply injured patient (6).
Missed or late diagnosis of associated injuries of the mediastinum and
brachial plexus are well documented. Failure of fixation, hardware
migration, and redislocation have also been reported after operative
stabilization and are likely due to the high forces acting on this main
articulation between the upper extremity and the axial skeleton (7).
Lastly, arthritic symptoms of the sternoclavicular joint are not
uncommon, and many authors have described resection of the clavicular
head to address refractory pain (8).
-
-
General information
-
Anatomy and mechanism.
The acromioclavicular joint is a synovial, diarthroidal joint that
contains a small, round meniscus composed of fibrocartilage much like
the knee. The static linkage of the lateral clavicle to the upper
extremity is via the coracoclavicular and acromioclavicular ligaments
as well as the joint capsule. The acromioclavicular AC joint capsule is
strongest at its superior and posterior margin (9).
The scapula is suspended from the clavicle via the coracoclavicular
ligaments, which run from the base of the coracoid to the undersurface
of the clavicle (Fig. 14-1).The acromioclavicular dislocation, commonly referred to
as a shoulder separation, is a much more common injury, likely due to
its more vulnerable position on the lateral aspect of the shoulder. The
joint absorbs direct force with any blow to the shoulder such as the
most common mechanism of a fall on the shoulder. -
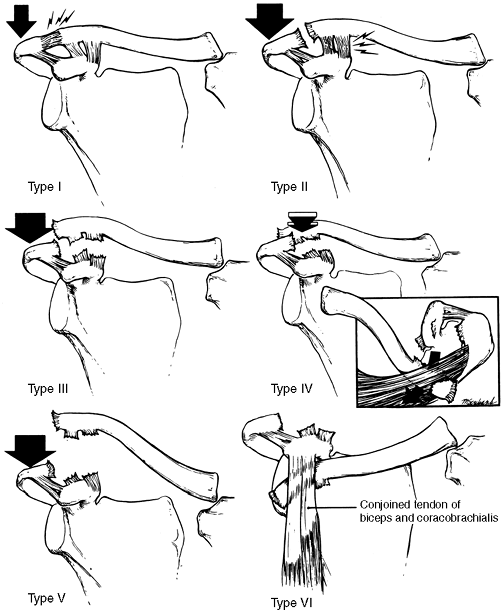
Classification (Fig. 14-2).
The Tossy classification was the first to grade acromioclavicular
dislocations (Types I–III). Rockwood modified this classification by
P.219
adding three more types (IV, V, and VI), based on directions of displacement (10). The joint may sustain a simple strain with minimal displacement referred to as a Type I. The Type II
injury is described as being displaced superiorly less than one half
the diameter of the clavicle and is thought to be associated with
complete tearing of the acromioclavicular ligaments but relative
sparing of the coracoclavicular ligaments. The Type III
dislocation represents complete disruption of the coracoclavicular and
acromioclavicular ligaments with superior displacement. A Type IV acromioclavicular dislocation is complete and displaced posteriorly; whereas a Type V
is an extreme variation of Type III, where the clavicle buttonholes
through the trapezius into the subcutaneous tissue and thus is
associated with much more stripping of trapezius and deltoid. The Type VI dislocation is an inferior dislocation under the coracoid process.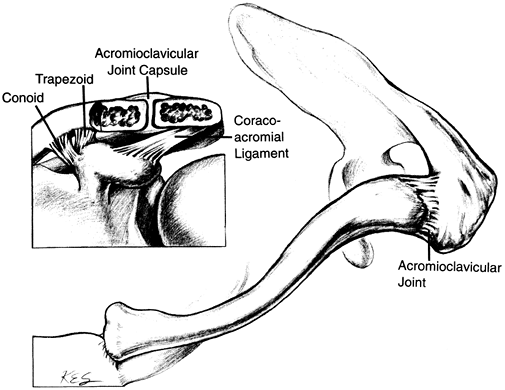 Figure 14-1.
Figure 14-1.
This illustration highlights the anatomy of the acromioclavicular
joint. The joint capsule as well as the conoid and trapezoid portions
of the coracoclavicular ligament are the static stabilizers of the the
acromioclavicular joint. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven Press, 1993:80, with permission.)
-
-
Diagnosis
-
History and physical exam.
The history usually details a fall to the shoulder, and it is
associated with well-localized pain. The acromioclavicular joint is
typically swollen and point tender. If a visual or palpable stepoff
exists, or the distal clavicle feels reducible, then there is at least
a Type II injury. In Types III to VI, the physical findings are
dramatic. -
Radiographs.
Typically, an anteroposterior x-ray of the shoulder reveals the injury,
though imaging of the joint can be enhanced with a 10-degree cephalic
tilt view. Visualization of both acromioclavicular joints on the same
large x-ray casette helps to understand relative displacement. Such a
radiograph taken with the patient hanging weights in each hand was a
popular study but has fallen into disfavor because it is painful and
does not change management. The examiner looks for increased distance
between the coracoid and the clavicle.![]() Figure 14-2. Schematic drawings of the classification of ligamentous injuries that can occur to the acromioclavicular ligament. Type I:
Figure 14-2. Schematic drawings of the classification of ligamentous injuries that can occur to the acromioclavicular ligament. Type I:
A mild force applied to the point of the shoulder does not disrupt
either the acromioclavicular or the coracoclavicular ligaments. Type II:
A moderate to heavy force applied to the point of the shoulder will
disrupt the acromioclavicular ligaments, but the coracoclavicular
ligaments remain intact. Type III: When a
severe force is applied to the point of the shoulder, both the
acromioclavicular and coracoclavicular ligaments are disrupted. Type IV:
In this major injury, not only are the acromioclavicular and
coracoclavicular ligaments disrupted but also the distal end of the
clavicle is displaced posteriorly into or through the trapezius muscle.
Type V: A violent force has been applied to
the point of the shoulder, not only rupturing the acromioclavicular and
coracoclavicular ligaments but also disrupting the deltoid and
trapezius muscle attachments and creating a major separation between
the clavicle and the acromion. Type VI:
Another major injury is an inferior dislocation of the distal end of
the clavicle to the subcoraciod position. The acromioclavicular and
coracoclavicular ligaments are disrupted. (From Rockwood CA, Williams
GR, Young DC. Injuries to the acromioclavicular joint. In: Rockwood CR,
Green DP, Bucholz RW, et al., eds. Fractures in adults, 4th ed. Philadelphia, PA: Lippincott-Raven, 1996:1354, with permission.)
-
-
Treatment
-
Nonoperative.
Type I and II acromioclavicular injuries should be treated
nonoperativley with the expectation of good functional results and
usually with complete resolution of pain (11).
Ice should be provided in the acute setting to relieve swelling, as
welll as to support the arm against gravity. As is the case for the
sternoclavicular dislocation, a closed reduction will not remain
reduced, and no brace has been proven to be efficacious in this regard.As for Type III dislocations, clinical studies comparing
operative versus nonoperative treatment seem to indicate that there is
no benefit from surgical treatment (11,12,13,14), though some experts believe that the overhead throwing athlete and manual laborer should undergo reconstruction (10). -
Operative.
Many surgical procedures have been described to repair an
acromioclavicular dislocation with the goal of preventing superior
migration. The strategy is either to fix the distal clavicle directly
to the acromion or to augment the coracoclavicular ligaments to
maintain a reduced joint. Some surgeons advocate a combination of these
two strategies to maintain the reduction against the great forces
acting to displace the clavicle. Though each strategy can be employed
in the acute or delayed setting, if a reconstruction is done late, it
is usually combined with a distal clavicle resection.The most widely known procedure is the Weaver-Dunn (15),
and most surgeons augment some variation of this repair with fixation
across the acromioclavicular joint, into the coracoid, or around the
base of the coracoid and clavicle like a sling. The Weaver-Dunn itself
involves bringing up the coracoclavicular ligament through the end of a
resected distal clavicle.A new device called the hook plate is gaining
popularity. The plate is fixed to the cephalad border of the distal
clavicle, and a terminal hook sweeps under the acromion so the clavicle
is restrained from springing superiorly. -
Follow-up. As
is the case with the sternoclavicular dislocation, a sling may be used
for a few weeks to support the extremity during the acute phase of
pain. A period of relative immobility is instituted, but motion is
advanced as discomfort allows. Shorter or longer periods with relative
rest are required according to which Type (I–III) of injury is present.
Often the Type I and II injuries hurt for a longer period of time than
the Type III injuries due to partial communication of the joint
surfaces and tethering of partially torn ligamentous structures. The
patient may need reassurance for months during a period of gradually
resolving symptoms. -
Complications.
Occasionaly, symptomatic posttraumatic osteolysis or arthritis of the
acromioclavicular joint develops. An arthroscopic or open resection of
the distal clavicle can be done to resect the distal 1.5 to 2.0 cm of
bone, and results have generally been favorable (16).Most of the complications related to surgery relate to
failure of fixation causing chronic symptomatic instability. Hardware
failure such as slippage of Kirschner wires or cutout of
coracoclavicular screws, as well as graft or suture cutting through the
distal clavicle, are not uncommon events and underscore the technically
demanding nature of the reconstruction.
-
-
Diagnosis: Anteroposterior shoulder radiograph, 15-degree cephalad oblique radiograph, clinical examination
-
Treatment: Grades I–III, sling for comfort for 7–10 days, then range-of-motion exercises
-
Indications for surgery: Grade IV, V, or VI injuries
-
Recommended technique: Subcoracoid suture loop with coracoclavicular (CC) ligament and deltotrapezial fascial repair
GC, Wallace WA, Stablforth PG, et al. The management of acute
acromioclavicular dislocation: a randomized prospective controlled
trial. J Bone Joint Surg (Br) 1989;71:848–850.
RD, Hawkins RJ, Grainger RW. A comparative analysis of operative versus
non-operative treatment of grade III acromioclavicular separations. Clin Orthop 1985;193:150–155.
SD, Baumgarten TE, Andrews JR. Arthroscopic resection of the distal
aspect of the clavicle with concomitant subacromial decompression. J Bone Joint Surg (Am) 2001;83:328.
MR. Complete dislocation of the acromioclavicular joint: the nature of
the traumatic lesion and effective methods of treatment with an
analysis of 41 cases. J Bone Joint Surg (Am) 1946;28:813–837.