Revision Total Hip Arthroplasty
performed in North America per year. Longer life expectancy,
implantation of prosthetic hips in younger and active patients, and the
increase in the number of patients with hip arthroplasty in place for
decades are some of the reasons for the rise in the incidence of
revision THA. Hip arthroplasty may fail and necessitate revision for
many reasons (Table 15-1). The goal of revision
THA, as for primary surgery, is to relieve the patients’ symptoms and
restore function. The main challenge of revision surgery, however, is
to accomplish these objectives in the setting of compromised bone
stock, poor soft tissue, and the possible presence of infection. Hence,
both planning and execution of revision hip arthroplasty can be very
different and in many occasions much more difficult than primary
arthroplasty. Extensile surgical approaches, more sophisticated
prosthetic devices, and more restricted postoperative protocols are
common in revision arthroplasty. Because of the above noted challenges,
the outcome of revision arthroplasty in terms of improvement in
function (as measured by validated instruments), complication rate, and
longevity of the prosthesis are inferior compared with primary THA.
with failed hip arthroplasty. Other modes of presentation can include
mechanical symptoms (such as subluxation) and dysfunction owing to hip
stiffness or limp. Wear and osteolysis may be asymptomatic. Regardless
of the mode of presentation, all patients with presumed failure of hip
arthroplasty need a detailed clinical and radiographic evaluation.
patient disability imparted by the symptoms may be elicited from
detailed history. The cause of pain that has been present since primary
THA is likely to be different from symptoms that commenced many years
after the initial arthroplasty. Evaluation of patient comorbidities
such as diabetes predisposing to infection, history of spinal disease
that can masquerade as hip pain, medications that may cause muscular
pain, and previous surgical history in the affected hip as well as
other joints is also critical. Detailed examination to confirm
suspected cause, measurement of limb length, assessment of abductor
strength and gait, and detection of neurovascular insufficiency are
also necessary.
very informative and are likely to demonstrate the cause of failure in
most cases. Gross component malpositioning, severe osteolysis, wear,
radiolucent lines indicative of loosening, fractures, limb-length
discrepancy, and occasionally signs of infection can be discerned from
the initial radiographs. A full-length femur radiograph is valuable if
long-stem femoral fixation is anticipated. On occasion other imaging
modalities such as long-leg standing radiographs to assess limb length,
computerized tomography (CT) to better assess component positioning or
the degree of osteolysis, or MRI to evaluate coexistence of spinal
conditions may need to be performed. Furthermore, nuclear imaging and
aspiration of the joint to confirm or rule out periprosthetic infection
may also need to be considered. On very rare occasions specialized
tests such as intravenous pyelography or angiography may be performed
in patients with intrapelvic components or intrapelvic cement that may
need to be removed.
(such as the change of acetabular liner) to a very complex surgery
(such as revision of well-fixed acetabular and femoral components).
Preoperative planning is paramount to ensure appropriate provisions are
in place during revision surgery. Although the decision to
perform
revision of one or both components can be made in most cases prior to
surgery, sometimes unrecognized loosening, malpositioning, or damage to
the bearing surface of a nonmodular femoral stem necessitates revision
of a component that was not anticipated preoperatively. Furthermore,
removal of well-fixed and well-positioned monolithic femoral
components, to allow better visualization of the acetabulum, may be
necessary during revision surgery. Hence, it is essential for the
reconstructive surgeon to have studied the previous operative records
of the patient to ensure that appropriate components, instruments, and
support teams will be available during revision THA.
|
TABLE 15-1 Indications for Revision HIP Arthroplasty
|
|
|---|---|
|
 |
|
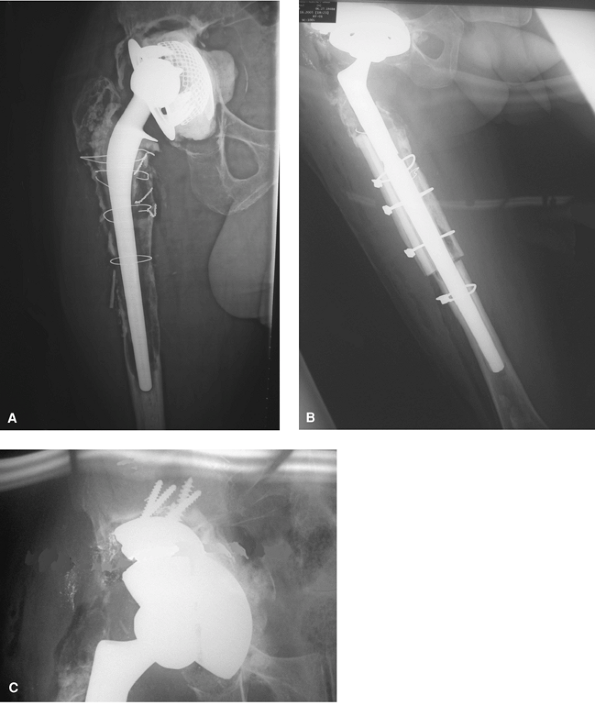
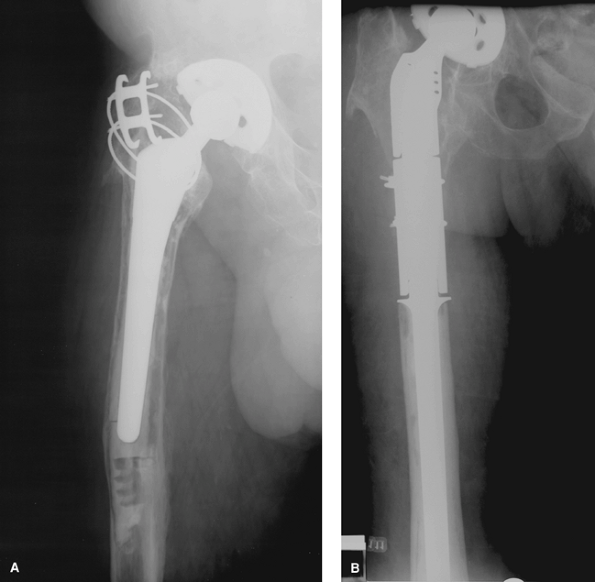
Figure 15-1 Anteroposterior radiograph (A)
of a proximally coated stem in a patient with severe thigh pain. Aseptic loosening of the femoral stem was suspected but obscure to confirm based on the radiographs. Note the reactive lines around the proximally coated region of the stem and the lack of osteointegration. Anteroposterior radiograph of the hip in a patient with gross loosening and subsidence of the femoral stem (B). Revision in which modular femoral stem was used (C). |
indications for revision THA. Aseptic loosening can present with
radiolucent lines at the prosthesis/bone, cement/bone, or
cement/prosthesis (debonding) interfaces. Radiolucent lines indicative
of definite loosening are usually progressive (i.e., developed over
time) or circumferential (covering the entire prosthesis surface) and
usually >2 mm wide. Diagnosis of aseptic loosening of an uncemented
femoral stem can be challenging (Fig. 15-1A).
Engh et al. have described major and minor radiographic signs of stem
loosening: The presence of reactive lines (white lines around the
stem), stem subsidence (Fig. 15-1B), and distal
pedestal not in contact with the tip of the stem are some of those
radiographic signs. Component subsidence or change in position, if
subtle, can be ascertained only by evaluation of serial radiographs.
Further imaging studies such as oblique radiographs may be required to
confirm aseptic loosening that is suspected clinically but cannot be
confirmed on conventional radiographs. A clinical history of start-up
pain usually is present with a loose femoral stem. Revision of loose
femoral components often can be done without the need for extensile
approaches (Fig. 15-1C) unless the component
subsides under the greater trochanter, making extraction without a
fracture difficult. Revision of a loose acetabular component can also
be performed with minimal bone loss if careful exposure of the
acetabulum is performed. Exposure of the
acetabulum in the presence of a well-fixed femoral stem can be challenging.
Around hip implants, the process is usually the result of activation of
macrophages and osteoclasts that can occur with generation of wear
particles or with infection. Osteolysis without component loosening can
be asymptomatic and forms the main rationale for periodic evaluation of
patients with joint arthroplasty, particularly those at specific risk
for this problem. Active patients with high demand on their prosthetic
hip are in this category. Conventional radiography underestimates the
degree of osteolysis. In recent years the use of CT scans to assess the
extent and location of osteolysis has been described.
 |
|
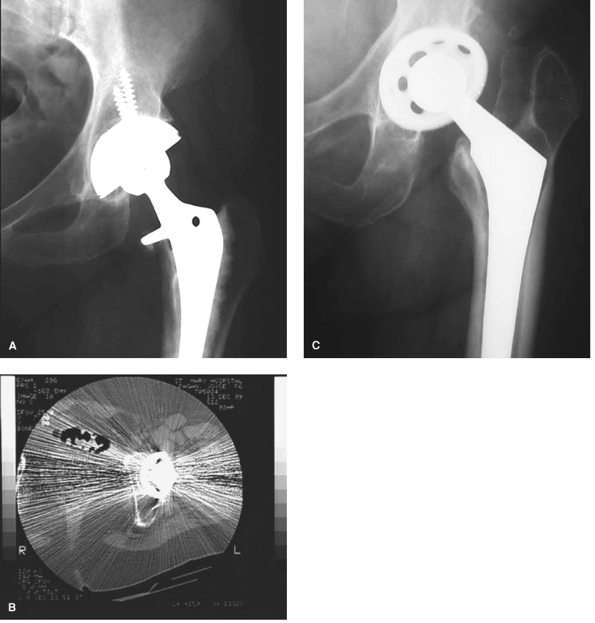
Figure 15-2 Anteroposterior radiograph of the hip in a 69-year-old patient with polyethylene wear and extensive osteolysis (A). The revision of both the acetabular and femoral component was performed (B). Trabecular metal augments were used to fill the defect in the acetabulum (C).
|
of surgical procedure for patients with asymptomatic osteolysis is
currently in evolution and not universally agreed on. There is,
however, no dispute in that surgical intervention should be considered
for patients with extensive osteolysis and impending periprosthetic
fracture, particularly in younger patients in whom bone mass is
critical, and for symptomatic patients. Options available for treatment
of osteolysis around well-fixed acetabular components include isolated
periacetabular bone grafting through a trapdoor or through access
points around the cups or through screw holes, replacement of the
bearing surface with or without bone grafting of the lesion (done
through screw holes), or revision of the acetabular component.
Osteolysis associated with loose acetabular or femoral components is
addressed by revision arthroplasty. Frequently particulate or bulk
allograft bone is used in an effort to restore the bone mass and allow
mechanical fixation of the components.
complication. The incidence of dislocation following THA varies between
0.3% and 10% after primary and up to 28% after revision arthroplasty.
It is well accepted that dislocation is more common after THA in
patients with impaired cognition, soft tissue laxity or deficiency,
underlying diagnosis of hip fracture, and female gender. Furthermore,
technical factors such as the use of a small-diameter femoral head and
performing the surgery through a posterolateral approach without
capsular repair seem to adversely influence the risk of instability.
Other technical factors such as the use of elevated acetabular liners,
femoral component neck geometry, and femoral component offset may also
influence the risk of instability. As our understanding of the causes
of dislocation has evolved over the last decade, refinements in
surgical techniques have been introduced that probably will result in a
decline in this complication.
However, most reported dislocations occur within the first few months
after the index surgery. About two thirds of dislocations can be
treated by closed reduction without a need for further intervention.
Recurrent instability, which often necessitates reoperation, can occur
owing to many reasons. The most common include component malpositioning
and soft tissue laxity. However, two important points need to be
mentioned. First is that the cause of recurrent instability in many
cases may be multifactorial. Second, the exact cause for recurrent
instability in some cases cannot be discerned with certainty. The
surgical treatment options available to address recurrent instability
consist of revision of malpositioned components, use of a
larger-diameter femoral head, bipolar arthroplasty, greater
trochanteric advancement, soft tissue re-enforcement, and the use of
constrained liners.
recurrent instability depends on the cause. Revision arthroplasty for
recurrent instability in general is much more likely to be successful
when a discernible cause for instability can be identified.
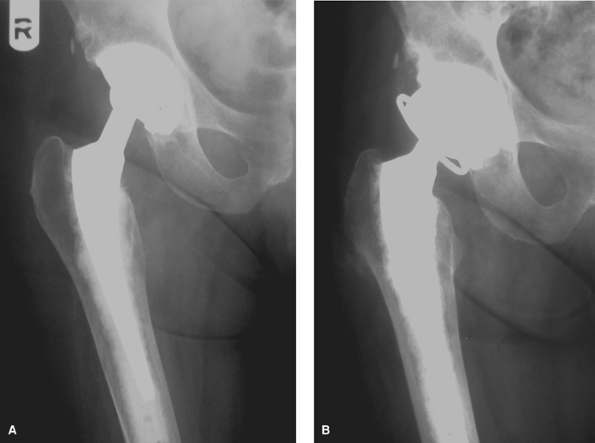
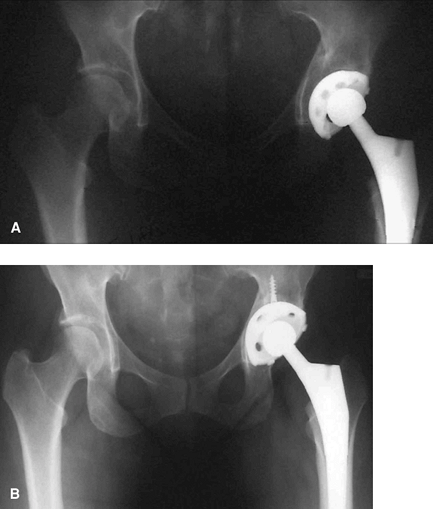
Although definitions of malpositioning vary, the optimal positioning
for acetabular component is thought to be 10 to 30 degrees of
anteversion and 35 to 50 degrees of inclination or abduction. When
components are positioned outside this zone, instability is more likely
to result. The position of the acetabular component in relation to the
anatomic landmarks (the teardrop on the radiographs) is also important.
Cross-sectional studies such as CT may be needed to accurately assess
component position (Fig. 15-3B).
main cause of instability, then the use of a larger femoral head,
bipolar arthroplasty, or more commonly a constrained liner is advocated
(Fig. 15-4). One of the main attractions of
constrained liners is that they may be used without the need to revise
a well-fixed and well-positioned acetabular components.
infection (PPI) continues to occur following THA. The incidence of PPI
is reported to be between 0.5% and 3%. Several factors adversely
influence the incidence of PPI, including revision surgery and
compromised immune status of the patient.
are thought to result from infecting organisms that gained access to
the joint during surgery or soon after from overlying skin or a
draining wound. Infections of this type generally become symptomatic
within a few days or weeks of the arthroplasty. Late chronic infections
may result from proliferation of organisms inoculated during surgery,
either from the air, surgical instruments, or the implant itself. The
lag period is the time taken for the organisms to proliferate and
declare deep infection. Hematogenous infections
represent seeding of an arthroplasty site by organisms carried by the
blood stream from a different site (e.g., urinary tract infection,
cutaneous or mucosal ulcer, and so on). The distinction between these
types may be difficult and is somewhat arbitrary.
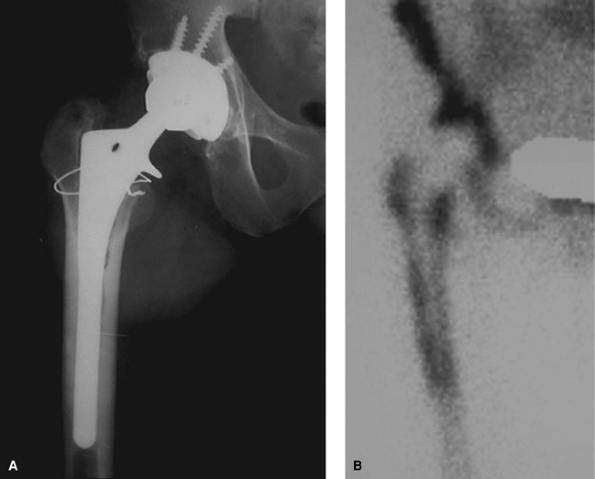
much difficulty, the detection of occult infection using the current
methods for diagnosis can be challenging. A high degree of suspicion
for PPI should be entertained in patients with early loosening of
components. Serologic tests such as C-reactive protein, erythrocyte
sedimentation rate, and white cell count may be used to screen for
infection. Aspiration of the joint is the most definitive test for
ongoing PPI. A few nonspecific changes suggestive of infection may be
apparent on plain radiographs (Fig. 15-5A).
These include periosteal reaction, scattered foci of osteolysis, and
generalized bone resorption in the absence of wear. However, most
patients with PPI, especially those presenting acutely, do not have
obvious radiographic findings suggestive of infection, or have
radiographic features indistinguishable from those seen in aseptic
loosening. The use of additional imaging such as the bone scan
(particularly labeled white blood cell scans), and recently, positron
emission tomography (PET) may occasionally be useful (Fig. 15-5B).
debridement of the hip with retention of the components, one-stage
exchange arthroplasty, or resection arthroplasty with delayed
reimplantation. PPI occurring early (within 4 weeks) after index
arthroplasty or hematogenous infection presenting acutely may be
treated with irrigation and debridement without resection of the
components as long as the components are well positioned and fixed. The
reported success rate of this method varies but probably is about 50%.
Two-stage exchange is the most common method of treating prosthetic
infection in North America. An antibiotic-impregnated bone cement
spacer frequently is placed in the hip after the initial resection, and
the patient usually is treated with 4 to 8 weeks of intravenous
antibiotics. On rare occasions one-stage exchange arthroplasty may be
considered for patients infected with a low-virulence organism that is
sensitive to most antibiotics. Resection arthroplasty may be the
treatment of choice for a select group of patients
with inadequate bone stock or soft tissues precluding reimplantation or recalcitrant infection.
 |
|
Figure 15-3 Anteroposterior radiograph of a patient with component malpositioning and instability (A). The computed tomography clearly showed malposition of the acetabular component as retroversion (B). The retroverted cup was repositioned during revision surgery (C).
|
factor limiting the longevity of the hip arthroplasty. Age and activity
level are among the most important predictors of bearing wear rate.
Polyethylene wear per se is usually not an indication for revision THA
unless it results in polythene fracture, wear-through, osteolysis, or
pain (owing to synovitis from wear debris). In recent years great
strides in the design of articulation materials have been made with
promising prospects. The introduction of highly cross-linked
polyethylene is one such improvement that has resulted in reduction of
wear both in vitro and in vivo.
Other alternative bearing surfaces that are currently in use include
alumina ceramic-on-ceramic and metal-on-metal articulations.
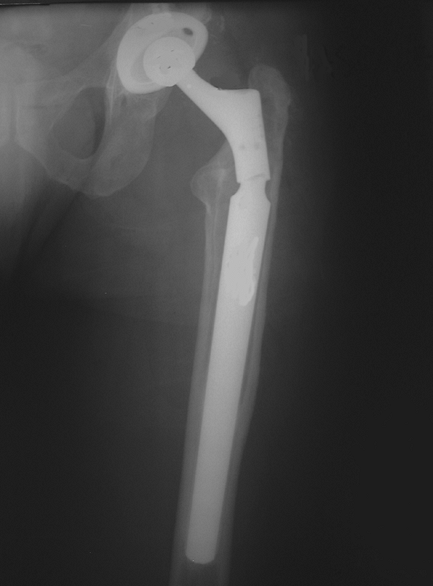
around the hip have been proposed. The Vancouver periprosthetic
fracture classification system is widely used and lends itself to
devising a treatment strategy. This classification system takes into
account the site of fracture, the status of the femoral component, and
the proximal femoral bone quality. Type A fractures are around the
proximal femur involving the greater trochanter or the lesser
trochanter. The stability of the stem is not usually compromised. These
fractures often are associated with osteolysis of the proximal femur.
Treatment is directed toward management of underlying osteolysis. The
fracture itself does not usually require fixation
unless
the greater trochanter is displaced to compromise abductor function.
Type B fractures are those occurring around the femoral stem. In type
B1 fractures the femoral stem is stable. Most can be treated with
internal fixation of the fracture using plates, screws, cerclage
cables, and strut grafts while retaining the well-fixed stem. Fractures
associated with loosening of the femoral stem (types B2 and B3) are
treated with revision of the femoral component and simultaneous
fracture fixation (Fig. 15-6).
 |
|
Figure 15-4
Anteroposterior radiograph of a patient with recurrent instability that was deemed secondary to inadequate soft tissue (abductor) envelope (A). The acetabular component, although slightly vertical, was found to be well fixed during surgery. A constrained liner with a larger femoral head was used to address the problem in this patient (B). |
 |
|
Figure 15-5 Plain radiograph showing area of focal osteolysis (scalloping) around the midportion of a well-fixed uncemented stem (A).
This appearance is highly suggestive of periprosthetic infection. Increased uptake in the corresponding area of infection in the right femur was noted on the PET scan (B). |
 |
|
Figure 15-6 Anteroposterior radiograph of a patient with Vancouver type B3 periprosthetic fracture (A). Proximal femoral replacement was used for reconstruction of this fracture (B).
|
replacement is not uncommon and can be bothersome to the patient.
Patients frequently complain of LLD in the early postoperative period,
and in most instances the LLD is functional and the symptoms resolve
with time. However, there remains a small subset of patients who
continue to be symptomatic. Most can be treated with shoe lifts to
compensate for the problem; further surgery is performed only in rare
instances (Fig. 15-7).
early prostheses made of stainless steel or cast cobalt chromium that
were susceptible to fatigue fracture. Improvements in engineering and
metallurgy have enabled manufacturers to produce arthroplasty
components that are extremely strong and resilient. Fractures of modern
monolithic femoral stems are exceedingly rare. Fracture of the femoral
stem, in the rare occasions that may occur, usually involves modular
components (Fig. 15-8). Poor proximal bone
support in a stem that is well fixed distally can lead to cantilever
loading of the stem and subsequent fatigue fracture.
dissociation or dislodging of the acetabular liner has also been
reported. This problem was more common particularly with some designs
of acetabular components that did not have sophisticated locking
mechanisms.
management of bone loss. Depending on the extent and location of bone
loss, different surgical strategies are used.
classification systems. The American Academy of Orthopaedic Surgeons
(AAOS) system can be used in both primary and revision arthroplasty. It
categorizes bone loss as segmental or cavitary defects along with
pelvic discontinuity and arthrodesis. Segmental defect describes full-thickness
loss of bone in the supporting rim of acetabulum or the medial wall. Cavitary defect
describes volumetric loss of bone within the acetabular cavity.
Complete transverse disruption of the supporting anterior and posterior
columns of acetabulum constitutes pelvic discontinuity.
Another classification system proposed by Paprosky is based on the
severity of bone loss and helps predict the surgeon’s ability to
achieve implant stability with a hemispheric cup. The system describes
four radiographic landmarks to evaluate the extent of bone loss, which
are the following: proximal migration of acetabular component
(migration of joint center), integrity of the teardrop, ischial bone
loss, and violation of the Köhler line by prosthetic migration.
 |
|
Figure 15-7 The anteroposterior radiograph (A)
of the hip in a 54-year-old patient in whom the acetabular component has been placed inferior to the anatomic position (teardrop), with the revised hip radiograph (B) demonstrating proper positioning of the cup that addressed the limb lengthening. |
femoral bone loss have been proposed. Most define the severity of
proximal bone loss by the amount of cancellous bone loss, the amount of
cortical bone loss, and the distal extent of this bone loss. These
classification methods can be used to choose necessary revision
implants.
is obtaining adequate exposure of the hip. If possible, the old
incision should be used or incorporated into the new incision. In many
revisions a conventional anterolateral or posterolateral approach may
be used. The advantages of anterolateral or direct lateral approaches
include excellent acetabular exposure, decreased rate of sciatic nerve
palsy, and reduced incidence of postoperative dislocations.
Disadvantages of the anterolateral approach include difficulty of
accessing the posterior column for cage implantation or bone grafting,
increased risk of heterotopic ossification, reduced visualization of
the proximal femur, and the higher incidence of postoperative limp.
Advantages of the posterolateral approach are good visualization of the
posterior column and entire acetabulum, preservation of the abductor
mechanisms, and lower incidence of heterotopic ossification.
Disadvantages include difficult acetabular exposure when the femoral
component is in situ, and a higher dislocation rate compared with
anterior or lateral approaches.
 |
|
Figure 15-8 Anteroposterior radiograph of the pelvis demonstrating fatigue fracture of the modular conical femoral stem.
|
revision arthroplasty. One of the most common extensile exposures is
the extended trochanteric osteotomy (ETO). ETO is considered the
exposure of choice for removal of well-fixed stems. It is also
particularly useful for removal of a well-fixed cement mantle,
particularly in infected cases. Another extensile exposure is the
Wagner osteotomy in which the proximal femur is split in the coronal
plane. Finally, conventional trochanteric osteotomy, or so-called
trochanteric
slide
(in which the abductors, greater trochanter, and vastus lateralis are
kept in continuity), also are useful in selected complex revisions.
Extensile exposures allow better visualization of both the femur and
the acetabulum while minimizing soft tissue damage. Fixation of
extended osteotomies can be performed with the use of cables or wires.
The osteotomy fragment can sometimes be advanced to modulate soft
tissue tension and enhance hip stability.
the acetabular component while avoiding bone loss. Removal of a loose
acetabular component usually can be performed with relative ease. In
recent years acetabular extraction systems have been introduced; these
consist of thin curved osteotomes that can be inserted behind the cup
and rotated around a ball placed inside the liner. It is crucial that
the osteotome be placed at the interface between the cup and the cement
mantle or the bone as opposed to being inserted into the substance of
retroacetabular bone.
be performed after obtaining good exposure of the femur. Extended
exposures may be needed for removal of a well-fixed femoral stem or
cement mantle. In cases where a portion of cement mantle remains,
particularly in the distal femur, the use of an anterolateral window in
the cortex may be most appropriate for complete removal of the
remaining cement. It is important to remember that any such defect in
the cortex will need to be bypassed by a stem spanning at least two
cortical diameters distal to the defect. In most cases the cement
mantle can be removed with the use of a combination of ultrasonic or
mechanical extraction systems.
infection, malposition, or wear. The objective of the procedure should
be restoration of the hip center of rotation, remedy of deficient bone,
and secure component fixation in optimal orientation.
revisions. Several large series report excellent mid- to long-term
survivorship of their techniques. The outcome is good even with limited
acetabular bone grafting including morselized grafting of cavitary
defects. The prerequisite for a successful outcome is obtaining
appropriate press fit and adequate surface area of contact between the
cementless cup and the host bone. The use of newer high-friction,
highly porous metals such as tantulum may allow successful
reconstruction using this method even when the bone loss is severe. It
is important to note that the location of the contact area is a
critical factor. Deficiencies of the superior weight bearing dome at
the socket may be filled with structural allograft or metallic
component augments. Many defects may be obliterated by reaming of the
cavity to allow insertion of a jumbo acetabular cup. The advantage of
using a jumbo cup is that it allows restoration of the hip center of
rotation and improved cup contact against the host bone.
acetabular rim can be treated using a cementless hemispheric cup. The
defect is usually reamed away prior to insertion of the uncemented cup.
Defects remaining after reaming can be treated with particulate bone
grafting. The bone graft is packed into the defect using the reamer in
a reverse direction. For larger defects with intact columns, structural
graft or metal augments may be used.
cementless hemispheric components. In most cases the rim area is intact
allowing press-fit insertion of the cementless component. Larger
defects can be filled with particulate bone grafting. For larger
defects, especially in the medial wall region, impaction bone grafting
with wire mesh can be considered.
defects. Cementless jumbo cups, with bone grafting, can be used in most
cases as long as adequate surface area of contact between the porous
acetabular cup and the host bone can be achieved. For cases with a
small surface area of contact and a large defect, proper fixation of an
uncemented component may not be possible. For these cases cemented cups
with impaction grafting or reconstruction cages may be more appropriate.
acetabular reconstruction for pelvic discontinuity with complete
separation of inferior and superior regions as a result of transverse
defects and/or fractures. In spite of all preoperative radiographic
assessments, pelvic discontinuity may be recognized or detected only
during surgery. Hence, it is crucial for reconstruction surgeons to
ensure that appropriate acetabular components are in place to deal with
this problem during complex revisions. Pelvic discontinuity should be
suspected in patients with massive bone loss. Any defects leading to
disruption of the posterior column should also lead the surgeon to
suspect pelvic discontinuity. When detected, appropriate reduction and
fixation of the “fracture,” usually by plating of the posterior column,
typically is performed prior to insertion of an acetabular component.
length and hip stability, and when possible to restore bone stock.
commonly during primary THA, the results of revision THA using this
stem design are disappointing. The main reason is that after removal of
a previous femoral stem, little to no bone may exist to allow proper
fixation of this stem design and subsequent biologic integration in the
metaphyseal region of the proximal femur. Hence, proximally coated
femoral stems are not commonly used during revision surgery.
revision hip arthroplasty. The extensively coated stems bypass the
sclerotic and often weakened proximal femur to achieve secure fixation
in the relatively healthy femoral diaphysis. The implant’s initial
rotational stability and subsequent biologic fixation are excellent in
most cases. To optimize the outcome, these stems should be implanted in
femoral canals with adequate (>5 cm) diaphyseal length for scratch
fit. The stem should bypass any defects in the cortex by at least two
canal diameters. An onlay cortical allograft may be used for larger
defects (more than one third of the canal diameter) of the cortex. All
cement in the femoral canal should be removed before reaming the canal.
A curved stem, conforming to the anatomy of the canal, should be used
when longer components are being implanted. Depending on the design,
reaming of the femoral canal to an appropriate diameter to allow good
press fit without causing fracture should be carried out. In cases with
high likelihood for fracture of the femur or in cases in which
longitudinal fracture of the femur occurs, cerclage cables or wires may
be used. Although extensively coated stems are reported to have
excellent outcomes in revision surgery, some problems are associated
with this femoral component design, one of which is stress shielding.
can be used to gain diaphyseal fixation. Modular femoral stems provide
intraoperative versatility to allow adjustment of limb length, offset,
and version.
patients with neoplastic conditions, the indications for this type of
reconstructive procedure were expanded to include patients presenting
with failed THA and massive proximal femoral bone loss. With
refinements in design, namely introduction of modular prostheses,
megaprostheses have been used in cases of proximal femoral bone
deficiency.
elderly or sedentary patients with massive proximal bone loss. In
younger patients in whom bone loss of high magnitude is encountered
that cannot be reconstructed by conventional means, an
allograft-prosthetic composite would be preferred over femoral
prosthetic replacement.
placed against defects in the femoral cortex or an allograft-prosthetic
composite (APC). The type and length of allograft used depend on
various factors, particularly the extent of bone loss and the status of
the soft tissues. An important prerequisite for the use of APC is the
availability of sufficient distal femoral length for secure fixation of
the femoral stem. The advantages of using an APC (besides its ability
to restore bone mass) are that it allows transmission of normal load to
the distal host bone and prevents further distal bone loss. The soft
tissue in the proximal region of the femur also can be attached to the
allograft bone with some potential for healing and integration. The
major disadvantages of using an APC are the higher incidence of
infection, graft fracture, nonunion of the allograft with the host
bone, technical difficulty of fashioning the composite, and the
relatively long operation time.
used revision femoral components, cemented stems also may be used in
selected cases. Cemented femoral revision generally is indicated in
patients with good bone stock and available cancellous bone for
interdigitation. Following removal of a previous femoral component,
usually little if any cancellous bone remains; thus the mechanical bond
of cement to bone in revision typically is reduced, particularly if the
previous component was cemented. Hence, the use of cemented femoral
components during revision surgery is limited. Femoral impaction
allografting and revision with allograft-prosthesis composite are two
scenarios in which cemented femoral stems need to be used. Another
occasion is when a well-fixed prior cement mantle is left in place and
another femoral component is either impacted into the mantle or
cemented into the previous cement mantle, the so-called
cement-within-cement technique. If this strategy is to be used, some
important steps needs to be taken. The mantle is dried, then multiply
scratched and roughened to increase the contact surface area and
improve interdigitation for the new cement mantle. The cement is
injected during a relatively liquid stage.
femora with cavitary metaphyseal or diaphyseal deficiencies and an
intact cortical envelope. Small segmental deficiencies also can be
treated with the use of a wire mesh or cortical strut graft. The
technique involves compression of particulate cancellous bone allograft
into the cavitary defects to reconstruct the osseous architecture of
the femur and concomitant use of a polished cemented femoral stem.
Before insertion of the grafts, the inner surface of the femur should
be cleaned thoroughly. A cement plug is inserted to restrict the bone
graft. The recommended graft size is generally as small as 4 to 6 mm3. Special instruments are used to obtain optimal graft impaction. The stem
is cemented into the graft mantle. The major advantage of using femoral
impaction allograft is the restoration of bone stock. This technique,
however, is challenging. Subsidence of the stem, either with or without
the graft mantle, have been reported in a few series, emphasizing that
the results are dependent on technique and patient selection. A high
incidence of periprosthetic fracture also has been reported at the tip
of the femoral stem when short-stemmed implants were used routinely.
which stem design or type should be used during revision surgery, some
general rules apply. The first goal should be a good long-term clinical
outcome, and a secondary goal should be restoration or maintenance of
bone mass. The first objective usually precludes the use of
conventional monoblock proximally coated uncemented stems in almost all
cases and also the use of cemented stems in most cases. The use of both
aforementioned stem designs necessitate good quality and volume of bone
in the metaphysis and the canal, which is rarely the case during
revision surgery. Hence, uncemented distally fixed stems are used more
commonly. When extensively coated stems are being used, it is crucial
to ensure that adequate diaphyseal fixation is achieved. This minimizes
the possibility of stem subsidence, pain, instability, and limb
shortening. For patients with extensive bone loss, proximal femoral
replacement in older and less active patients and allograft-prosthesis
composite in younger patients are preferred. Regardless of which stem
design and type are used, revision surgery can be a challenging
experience and should be undertaken only by those familiar with all the
intricacies. Attention to detail and delivery of optimal surgical care
are essential for a predictable and good outcome of any surgical
procedure, particularly revision arthroplasty.
JA, Capello WN, Borden LS, et al. Classification and management of
acetabular abnormalities in total hip arthroplasty. Clin Orthop. 1989;243:126–137.
R, Gonzalez C, Cabanela ME, et al. Extended femoral osteotomy for
revision of hip arthroplasty: results and complications. J Arthroplasty. 2005;20:79–83.
BW, Bolder SB, Gardeniers JW, et al. Acetabular revision with impacted
morselized cancellous bone grafting and a cemented cup. A 15- to 20-
year follow-up. J Bone Joint Surg Br. 2004;86: 492–497.
