Radius and Ulna Shaft
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > III – Upper Extremity Fractures and Dislocations > 21 – Radius and Ulna Shaft
21
Radius and Ulna Shaft
EPIDEMIOLOGY
-
Forearm fractures are more common in men
than women; secondary to the higher incidence in men of motor vehicle
accidents, contact athletic participation, altercations, and falls from
a height. -
The ratio of open fractures to closed fractures is higher for the forearm than for any other bone except the tibia.
ANATOMY
-
The forearm acts as a ring; a fracture
that shortens either the radius or the ulna results either in a
fracture or a dislocation of the other forearm bone at the proximal or
distal radioulnar joint. Nightstick injuries are an exception. -
The ulna, which is relatively straight,
acts as an axis around which the laterally bowed radius rotates in
supination and pronation. A loss of supination and pronation may result
from radial shaft fractures in which the lateral curvature has not been
restored. -
The interosseous membrane occupies the
space between the radius and ulna. The central band is approximately
3.5 cm wide running obliquely from its proximal origin on the radius to
its distal insertion on the ulna. Sectioning of the central band alone
reduces stability by 71% (Fig. 21.1). -
Fracture location dictates deforming forces:
-
Radial fractures distal to the supinator
muscle insertion but proximal to the pronator teres insertion tend to
result in supination of the proximal fragment owing to unopposed pull
of the supinator and biceps brachii muscles. -
Radial fractures distal to the supinator
and pronator teres muscles tend to result in neutral rotational
alignment of the proximal fragment.
-
FRACTURES OF BOTH THE RADIUS AND ULNA SHAFTS
Mechanism of Injury
-
These are most commonly associated with
motor vehicle accidents, although they are also commonly caused by
direct trauma (while protecting one’s head), gunshot wounds, and falls
either from a height or during athletic competition. -
Pathologic fractures are uncommon.
Clinical Evaluation
-
Patients typically present with gross deformity of the involved forearm, pain, swelling, and loss of hand and forearm function.
-
A careful neurovascular examination is
essential, with assessment of radial and ulnar pulses, as well as
median, radial, and ulnar nerve function. -
One must carefully assess open wounds because the ulna border is subcutaneous, and even superficial wounds can expose the bone.
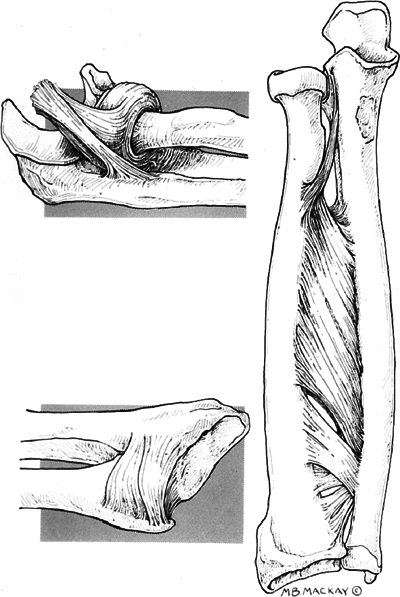 Figure
Figure
21.1. Line diagram showing the soft tissue connections of the radius
and the ulna to each other. The proximal radioulnar joint is stabilized
by the annular ligament. The distal radioulnar joint is stabilized by
the dorsal and volar radioulnar ligaments and the triangular
fibrocartilage complex.(From Richards RR. Chronic disorders of the forearm. J Bone Joint Surg 1996;78A:916–930.) -
Excruciating, unremitting pain, tense
forearm compartments, or pain on passive stretch of the fingers should
raise suspicions of impending or present compartment syndrome.
Compartment pressure monitoring should be performed, with emergency
fasciotomy indicated for diagnosed compartment syndrome.
P.217
Radiographic Evaluation
-
Anteroposterior (AP) and lateral views of
the forearm should be obtained, with oblique views obtained as
necessary for further fracture definition. -
Radiographic evaluation should include
the ipsilateral wrist and elbow to rule out the presence of associated
fracture or dislocation. -
The radial head must be aligned with the capitellum on all views.
P.218
Classification
Descriptive
-
Closed versus open
-
Location
-
Comminuted, segmental, multifragmented
-
Displacement
-
Angulation
-
Rotational alignment
OTA Classification of Fractures of the Radial and Ulna Shaft
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
Treatment
Nonoperative
-
The rare, nondisplaced fracture of both
the radius and the ulna may be treated with a well-molded, long arm
cast in neutral rotation with the elbow flexed to 90 degrees. -
The patient should have frequent follow-up to evaluate for possible loss of fracture reduction.
Operative
-
Open reduction and internal fixation is
the procedure of choice for displaced forearm fractures involving the
radius and ulna in adults. -
Internal fixation involves use of compression plating (3.5-mm dynamic compression plate) with or without bone grafting.
-
Principles of plate fixation:
-
Restore ulnar and radial length (prevents subluxation of either the proximal or distal radioulnar joint).
-
Restore rotational alignment.
-
Restore radial bow (essential for rotational function of the forearm).
-
-
A volar Henry approach may be used for
fixation of the distal one-third of the radius with plate placement on
the flat volar surface. Midshaft fractures may be approached and
stabilized via a dorsal or volar approach. -
The ulna may be plated on either the
volar or dorsal aspect, depending on the location of the fragments and
contour of the ulna surrounding the fracture site. Using two separate
incisions decreases the incidence of radioulnar synostosis. -
One should consider bone grafting if substantial comminution or bone loss exists.
-
Open fractures may receive primary open
reduction and internal fixation after debridement, except in severe
open injuries. This approach restores stability, limits dead space, and
improves wound care. The timing of bone grafting of open
P.219
fractures is controversial; it can be performed at the time of delayed primary closure or at 6 weeks after injury. -
External fixation may be used in cases
with severe bone or soft tissue loss, gross contamination, infected
nonunion, or in cases of open elbow fracture-dislocations with soft
tissue loss. -
Good results have been reported with
locked intramedullary nail fixation. However, the indications for
intramedullary nailing over plate and screws have not been clearly
defined. Some of the reported indications are segmental fractures, open
fractures with bone or soft tissue loss, pathologic fractures, and
failed plate fixation.
Complications
-
Nonunion and malunion: These are
uncommon, most often related to infection and errors of surgical
technique. Patients may require removal of hardware, bone grafting, and
repeat internal fixation. -
Infection: The incidence is only 3% with
open reduction and internal fixation. It necessitates surgical
drainage, debridement, copious irrigation, wound cultures, and
antibiotics. If internal fixation is found to be stable, it does not
necessarily need to be removed because most fractures will unite
despite infection. Massive infections with severe soft tissue and
osseous compromise may necessitate external fixation with wounds left
open and serial debridements. -
Neurovascular injury: This is uncommon,
associated with gunshot injury or iatrogenic causes. Nerve palsies can
generally be observed for 3 months, with surgical exploration indicated
for failure of return of nerve function. Injuries to the radial or
ulnar arteries may be addressed with simple ligation if the other
vessel is patent. -
Volkmann ischemia: This devastating
complication follows compartment syndrome. Clinical suspicion should be
followed by compartment pressure monitoring with emergency fasciotomy
if a compartment syndrome is diagnosed. -
Posttraumatic radioulnar synostosis: This
is uncommon (3% to 9% incidence); the risk increases with massive crush
injuries or closed head injury. It may necessitate surgical excision if
functional limitations of supination and pronation result, although a
nonarticular synostosis excision is rarely successful in the proximal
forearm. Postoperative low-dose radiation may decrease the incidence of
recurrence.
FRACTURES OF THE ULNA SHAFT
-
These include nightstick and Monteggia fractures, as well as stress fractures in athletes.
-
A Monteggia lesion denotes a fracture of the proximal ulna accompanied by radial head dislocation.
Mechanism of Injury
-
Ulna nightstick
fractures result from direct trauma to the ulna along its subcutaneous
border, classically as a victim attempts to protect the head from
assault. -
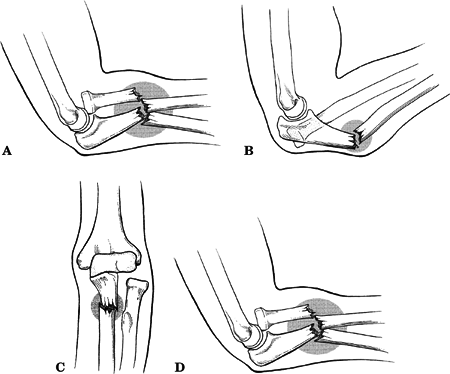
Monteggia fractures are produced by various mechanisms (by Bado classification) (Fig. 21.2):
P.220
| Type I: | Forced pronation of the forearm |
| Type II: | Axial loading of the forearm with a flexed elbow |
| Type III: | Forced abduction of the elbow |
| Type IV: | Type I mechanism in which the radial shaft additionally fails |
 |
|
Figure
21.2. The Bado classification of Monteggia fractures. (A) Type I. An anterior dislocation of the radial head with associated anteriorly angulated fracture of the ulna shaft. (B) Type II. Posterior dislocation of the radial head with a posteriorly angulated fracture of the ulna. (C) Type III. A lateral or anterolateral dislocation of the radial head with a fracture of the ulnar metaphysic. (D) Type IV. Anterior dislocation of the radial head with a fracture of the radius and ulna. (From Bado JL. The Monteggia lesion. Clin Orthop 1967;50:70–86..)
|
Clinical Evaluation
-
Patients with a nightstick fracture
typically present with focal swelling, pain, tenderness, and variable
abrasions at the site of trauma. -
Patients with Monteggia fractures present
with elbow swelling, deformity, crepitus, and painful range of elbow
motion, especially supination and pronation. -
A careful neurovascular examination is
essential, because nerve injury, especially to the radial or posterior
interosseous nerve, is common. Most nerve injuries have been described
with Type II Bado fractures.
Radiographic Evaluation
-
AP and lateral views of the elbow and forearm (to include the wrist) should be obtained.
-
Oblique views may aid in fracture definition.
-
Normal radiographic findings:
-
A line drawn through the radial head and shaft should always line up with the capitellum.
-
Supinated lateral: Lines drawn tangential to the radial head anteriorly and posteriorly should enclose the capitellum.
-
P.221
Bado Classification of Monteggia Fractures (Fig. 21.2)
| Type I: | Anterior dislocation of the radial head with fracture of ulnar diaphysis at any level with anterior angulation |
| Type II: | Posterior/posterolateral dislocation of the radial head with fracture of ulnar diaphysis with posterior angulation |
| Type III: | Lateral/anterolateral dislocation of the radial head with fracture of ulnar metaphysis |
| Type IV: | Anterior dislocation of the radial head with fractures of both radius and ulna within proximal third at the same level |
Classification
OTA Classification of Fractures of the Ulna Shaft
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
Treatment
Nightstick Fractures
-
Nondisplaced or minimally displaced ulna
fractures may be treated with plaster immobilization in a sugar-tong
splint for 7 to 10 days. Depending on the patient’s symptoms, this may
be followed by functional bracing for 8 weeks with active
range-of-motion exercises for the elbow, wrist, and hand, or simple
immobilization in a sling with a compression wrap. -
Displaced fractures (>10-degree
angulation in any plane or >50% displacement of the shaft) should be
treated with open reduction and internal fixation using a 3.5-mm
dynamic compression plate.
Monteggia Fractures
-
Closed reduction and casting of Monteggia fractures should be reserved only for the pediatric population.
-
Monteggia fractures require operative
treatment, with closed reduction of the radial head with the patient
under anesthesia, and open reduction and internal fixation of the ulna
shaft with a 3.5-mm dynamic compression plate or reconstruction plate. -
After fixation of the ulna, the radial head is usually stable (>90%).
-
Failure of the radial head to reduce with
ulna reduction and stabilization is usually the result of an interposed
annular ligament or rarely the radial nerve. -
If open reduction is required for the radial head, the annular ligament should be repaired.
-
Associated radial head fractures may require fixation.
-
Postoperatively, the patient is placed in
a posterior elbow splint for 5 to 7 days. With stable fixation,
physical therapy can be started with active flexion-extension and
supination-pronation exercises. If fixation or radial head stability is
questionable, the patient may be placed in a long arm cast with serial
radiographic evaluation to determine healing, followed by a supervised
physical therapy regimen.
P.222
Complications
-
Nerve injury: most commonly associated
with Bado Type II and III injuries involving the radial and/or median
nerves, as well as their respective terminal branches, the posterior
and anterior interosseous nerves. These may also complicate open
reduction owing to overzealous traction or reduction maneuvers.
Surgical exploration is indicated for failure of nerve palsy recovery
after a 3-month period of observation. -
Radial head instability: uncommon
following anatomic reduction of the ulna. If redislocation occurs <6
weeks postoperatively with a nonanatomic reduction of the ulnar, repeat
reduction and fixation of the ulna with an open reduction of the radial
head may be considered. Dislocation of the radial head >6 weeks
postoperatively is best managed by radial head excision.
FRACTURES OF THE RADIAL SHAFT
-
Fractures of the proximal two-thirds of
the radius without associated injuries may be considered to be truly
isolated. However, radial fractures involving the distal third involve
the distal radioulnar joint until proven otherwise. -
A Galeazzi or Piedmont fracture
refers to a fracture of the radial diaphysis at the junction of the
middle and distal thirds with associated disruption of the distal
radioulnar joint. It has also been referred to as the “fracture of
necessity,” because it requires open reduction and internal fixation to
achieve a good result. This lesion is approximately three times as
common as Monteggia fractures.-
Variants: Fracture can occur anywhere
along the radius or associated with fractures of both radius and ulna
with distal radioulnar joint disruption.
-
-
Four major deforming forces contribute to a loss of reduction if the fracture is treated by nonoperative means:
-
Weight of the hand: This results in dorsal angulation of the fracture and subluxation of the distal radioulnar joint.
-
Pronator quadratus insertion: This tends to pronate the distal fragment with proximal and volar displacement.
-
Brachioradialis: This tends to cause proximal displacement and shortening.
-
Thumb extensors and abductors: They
result in shortening and relaxation of the radial collateral ligament,
allowing displacement of the fracture despite immobilization of the
wrist in ulnar deviation.
-
-
A reverse Galeazzi fracture denotes a fracture of the distal ulna with associated disruption of the distal radioulnar joint.
P.223
Mechanism of Injury
-
Radial diaphyseal fractures may be caused by direct trauma or indirect trauma, such as a fall onto an outstretched hand.
-
The radial shaft in the proximal two
thirds is well padded by the extensor musculature; therefore, most
injuries severe enough to result in proximal radial shaft fractures
typically result in ulna fracture as well. In addition, the anatomic
position of the radius in most functional activities renders it less
vulnerable to direct trauma than the ulna. -
Galeazzi fractures may result from direct
trauma to the wrist, typically on the dorsolateral aspect, or a fall
onto an outstretched hand with forearm pronation. -
Reverse Galeazzi fractures may result from a fall onto an outstretched hand with forearm supination.
Clinical Evaluation
-
Patient presentation is variable and is
related to the severity of the injury and the degree of fracture
displacement. Pain, swelling, and point tenderness over the fracture
site are typically present. -
Elbow range of motion, including
supination and pronation, should be assessed; rarely, limited forearm
rotation may suggest a radial head dislocation in addition to the
diaphyseal fracture. -
Galeazzi fractures typically present with
wrist pain or midline forearm pain that is exacerbated by stressing of
the distal radioulnar joint in addition to the radial shaft fracture. -
Neurovascular injury is rare.
Radiographic Evaluation
-
AP and lateral radiographs of the forearm, elbow, and wrist should be obtained.
-
Radiographic signs of distal radioulnar joint injury are:
-
Fracture at base of the ulnar styloid.
-
Widened distal radioulnar joint on AP x-ray.
-
Subluxed ulna on lateral x-ray.
-
>5 mm radial shortening.
-
Classification
OTA Classification of Fractures of the Radial Shaft
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
Treatment
Proximal Radius Fracture
-
Nondisplaced fractures may be managed in
a long arm cast. Any evidence of loss of radial bow is an indication
for open reduction and internal fixation. The cast is continued until
radiographic evidence of healing occurs. -
Displaced fractures are best managed by open reduction and plate fixation using a 3.5-mm dynamic compression plate.
P.224
Galeazzi Fractures
-
Open reduction and internal fixation
comprise the treatment of choice, because closed treatment is
associated with a high failure rate. -
Plate and screw fixation is the treatment of choice.
-
An anterior Henry approach (interval
between the flexor carpi radialis and the brachioradialis) typically
provides adequate exposure of the radius fracture, with plate fixation
on the flat, volar surface of the radius. -
The distal radioulnar joint injury
typically results in dorsal instability; therefore, a dorsal
capsulotomy may be utilized to gain access to the distal radioulnar
joint if it remains dislocated after fixation of the radius. Kirschner
wire fixation may be necessary to maintain reduction of the distal
radioulnar joint if unstable. If the distal radioulnar joint is
believed to be stable, however, postoperative plaster immobilization
may suffice. -
Postoperative management:
-
If the distal radioulnar joint is stable: Early motion is recommended.
-
If the distal radioulnar joint is unstable: Immobilize the forearm in supination for 4 to 6 weeks in a long arm splint or cast.
-
Distal radioulnar joint pins, if needed, are removed at 6 to 8 weeks.
-
Complications
-
Malunion: Nonanatomic reduction of the
radius fracture with a failure to restore rotational alignment or
lateral bow may result in a loss of supination and pronation, as well
as painful range of motion. This may require osteotomy or distal ulnar
shortening for cases in which symptomatic shortening of the radius
results in ulnocarpal impaction. -
Nonunion: This is uncommon with stable fixation, but it may require bone grafting.
-
Compartment syndrome: Clinical suspicion
should be followed by compartment pressure monitoring with emergency
fasciotomy if a compartment syndrome is diagnosed.-
One should assess all three forearm compartments and the carpal tunnel.
-
-
Neurovascular injury:
-
This is usually iatrogenic.
-
Superficial radial nerve injury (beneath the brachioradialis) is at risk with anterior radius approaches.
-
Posterior interosseous nerve injury (in the supinator) is at risk with proximal radius approaches.
-
If no recovery occurs, explore the nerve at 3 months.
-
-
Radioulnar synostosis: This is uncommon (3% to 9.4% incidence).
-
Risk factors include:
-
Fracture of both bones at the same level (11% incidence).
-
Closed head injury.
-
Surgical delay >2 weeks.
-
Single incision for fixation of both bone forearm fractures.
-
Penetration of the interosseous membrane by bone graft or screws, bone fragments, or surgical instruments.
-
Crush injury.
-
Infection.
P.225 -
-
The worst prognosis is with distal synostosis, and the best is with diaphyseal synostosis.
-
-
Recurrent dislocation: This may arise as
a result of radial malreduction. It emphasizes the need for anatomic
restoration of the radial fracture to ensure adequate healing and
biomechanical function of the distal radioulnar joint.
