RADIAL NERVE PALSY
penetrating injuries to the lower arm and the upper forearm and from
fractures of the middle to distal third of the humerus. The major
functional impairment is an alteration in the ability to grasp and
release.
-
Phase 1 constitutes opening the hand
widely and requires the long extensors of the fingers and the thumb,
abduction of the first metacarpal, and intrinsic muscle action. -
Phase 2 involves surrounding the object and requires combined long flexors and intrinsic action.
-
Phase 3 is gripping the object between
the fingers and the palm or between the fingers and the thumb and
requires strong action of the long flexors. Phase 3 also requires
stabilization of the wrist by the wrist extensors to prevent the strong
finger flexors from pulling the wrist into flexion, causing a loss in
power grip strength. Opening the hand for release requires the long
extensors and the intrinsic muscles to perform as in phase 1 of grasp.
In high radial nerve palsy, grasp phases 1 and 3 and the ability to
release are severely impaired. In posterior interosseous nerve palsy,
at least one of the radial wrist extensors is intact for wrist
stability during phase 3 of grasp, and only grasp phase 1 and release
are affected. Reconstruction for radial nerve palsy is directed at
rebalancing the grasp-release mechanism necessary for normal hand
function.
originates from the posterior cord of the brachial plexus. Contributing
nerve fibers can be traced from the fifth through the eighth cervical
roots, with the largest contribution usually from the seventh. The
nerve enters the upper arm posteriorly, accompanying the deep brachial
artery between the long and medial heads of the triceps. The radial
nerve does not travel in the spiral groove of the humerus but lies
instead on the upper part of the medial triceps, separated from the
underlying bone by a layer of muscle approximately 3.4 mm thick (40). The nerve is in direct contact with the humerus only in the distal arm, where it pierces the lateral intermuscular septum.
 |
|
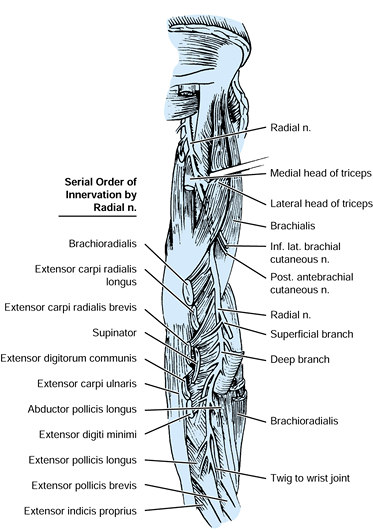
Figure 55.1. The radial nerve is shown as it courses through the arm and forearm. (Modified from Hollinshead WH. Anatomy for Surgeons, Vol 3. The Back and Limbs, 3rd ed. New York; Harper & Row, 1982, with permission)
|
branches to the triceps: a branch to the long head arising about 7.1 cm
below the tip of the acromion, a branch to the medial head arising
about 9.5 cm below the acromial tip, the nerve to the lateral head
arising about 10.1 cm, and another larger branch to the medial head
about 11.2 cm below the acromial tip (19). Sunderland reported more variability, with 5 to 10 branches typically found (36).
Because the branches to the triceps arise high in the arm, paralysis of
the triceps from a fracture of the humerus is unlikely.
septum about 10 cm proximal to the lateral epicondyle and enters the
anterior arm between the brachialis and the brachioradialis. The motor
branches to the brachioradialis and the extensor carpi radialis longus
are given off in this area above the elbow. A branch is often extended
to the brachialis, but the predominant innervation of this muscle is
the musculocutaneous nerve (29).
branch at about the level of the lateral epicondyle. The level of
bifurcation varies from 4.5 cm above the lateral epicondyle to 4 cm
below, with division at or below the epicondyle more common (19).
At about this same level, the radial nerve gives a branch to the
extensor carpi radialis brevis. Salsbury found this branch to arise
from the superficial branch of the radial nerve in 56% of specimens,
from the deep branch in 36%, and from the angle formed by the two in 8%
(29). With the exception of the frequent branch
to the extensor carpi radialis brevis, the superficial branch of the
radial nerve is purely sensory.
branches, the superficial branch continues distally and dorsally under
the cover of the brachioradialis. It emerges from under this muscle at
the junction of the middle and distal thirds of the forearm to continue
subcutaneously along the dorsoradial aspect of the forearm to supply
skin on the lateral part of the dorsum of the wrist and hand.
as the posterior interosseous nerve. Its function is purely motor,
except for several branches to the wrist joint at its most terminal
extent, which are sensory. The posterior interosseous nerve passes from
the proximal anterior forearm to the posterior forearm through the
supinator muscle, which it innervates. The proximal margin of the
supinator forms a fibrous arch, referred to as the arcade of Frohse,
through which the nerve passes (12).
approximately 8 cm below the elbow joint, and it immediately divides
into multiple branches. Spinner observed that the branches seem to be
arranged into two major groups (34). The first
group supplies the superficial layer of extensor muscles (the extensor
digitorum communis, extensor digiti minimi, and extensor carpi
ulnaris), and the second group supplies the deep layer (the abductor
pollicis longus, extensor pollicis longus and brevis, and extensor
indicis proprius). The serial order of innervation varies, but it
usually follows a proximal to distal pattern (Fig. 55.1).
considered relatively predictable and reproducible. Some surgeons have
advocated early definitive tendon transfers to the exclusion of
neurolysis or neurorrhaphy for a high radial nerve lesion or a
segmental nerve defect (2,7). We think this approach denies the patient a potentially superior result.
If recovery is delayed, neurolysis becomes extremely valuable.
Functional return after neurolysis in neurapraxia or axonotmesis can be
excellent. The myelin sheaths are still intact or at least properly
aligned, allowing selective reinnervation of the
muscles
by the same regenerating axons as before injury. This reinnervation
restores independent control of the individual muscles, a
characteristic that is never achieved with primary nerve repair, nerve
graft, or tendon transfers.
function after primary radial nerve repair or nerve grafting can be
expected in 77% of patients (21). Even if the
return in muscle function is limited, the result is often superior to
that achieved by tendon transfers alone when combined with definitive
tendon transfers. Therefore, initial emphasis should be placed on the
nerve injury.
nature and severity of the inciting injury. Closed injuries, such as
crush injuries, low-velocity gunshot wounds, and closed fractures,
result in neurapraxia or axonotmesis, and they should simply be
observed initially. In open injuries, such as open fractures and
lacerations, the nerve should be explored during the initial irrigation
and debridement of the wound.
Several factors influence prognosis for patients with such fractures.
Partial paralysis indicates continuity of the nerve and is a good
prognostic sign. Functional recovery can be expected. Kaiser et al.
believe that a comminuted, middle-third fracture of the humerus with
immediate onset radial nerve palsy offers the poorest prognosis for
nerve recovery (17). This poor prognosis is
related to the high energy involved in this fracture. They suggest
early exploration of nerves with this fracture pattern.
fracture of the distal humerus places the radial nerve at particular
risk for entrapment in the fracture site (14).
They think early exploration is indicated if this fracture pattern is
associated with a radial nerve palsy. In contrast, Pollock and
colleagues, who noted a 92% spontaneous recovery rate irrespective of
the fracture pattern, recommend initial observation in all closed
humerus fractures with associated radial nerve palsy (25).
If nerve function shows no signs of improvement in 3 to 4 months,
explore the nerve with neurolysis or neurorrhaphy. In a more recent
study, Foster et al. examined a series of 14 patients with radial nerve
palsy caused by open humeral shaft fractures. The nerve was either
lacerated or interposed in the fracture in 64% of patients (11).
fractures. For all closed fractures of the humerus associated with a
radial nerve palsy, we treat the nerve injury expectantly if the
fracture can be reduced closed. Most patients can be expected to
recover in 1 to 4 months. In 3 to 4 weeks, if recovery has not begun,
assess the extent of the nerve damage by electromyography. If no
neurologic recovery is observed in 3 to 4 months, we explore the nerve
with neurolysis or neurorrhaphy. If reduction is blocked by any
soft-tissue interposition, especially if the fracture is of the distal
spiral oblique type, we explore the nerve and reduce and internally fix
the fracture.
of immediate onset, early exploration should be considered. Radial
nerve palsies that are delayed in onset, even after manipulation, may
be observed. In open fractures, the nerve should be explored during
irrigation and debridement of the fracture. Repair nerves and fix rigid
fractures. Repair segmental defects with interfascicular grafts.
Functional nerve return can be expected in as many as 77% of patients (21).
grafting defects as large as 15 cm. As a general rule, nerve
regeneration progresses at a rate of 1 mm per day (32).
Lesions above the elbow may progress at a slower rate. After giving up
on a nerve repair, we have occasionally been surprised to find some
muscle function return several months after that predicted by the
1-mm-per-day formula.
deformity cannot be overemphasized. Use splints and physical therapy
while awaiting nerve recovery and before considering tendon transfers.
Splinting must be individualized. A simple palmar cock-up splint may
increase the grip strength 3 to 5 times (9).
Most patients are well served by such a splint. A patient requiring
greater excursion of the fingers may prefer a dynamic splint with
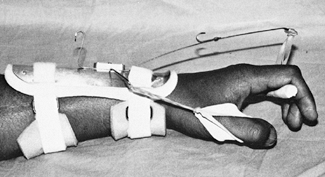
extension assists for the wrist and metacarpophalangeal joints (Fig. 55.2) (24,37,38).
 |
|
Figure 55.2.
A dynamic splint with an extension assist for the wrist metacarpophalangeal joints of the fingers and abduction or extension assist for the thumb are shown. |
fundamental principles of tendon transfers and biomechanics (see Chapter 54).
In selecting radial nerve transfers, approach each patient
individually, with attention to age, occupation, and recreational
goals. Become familiar with the limitations and uses of the different
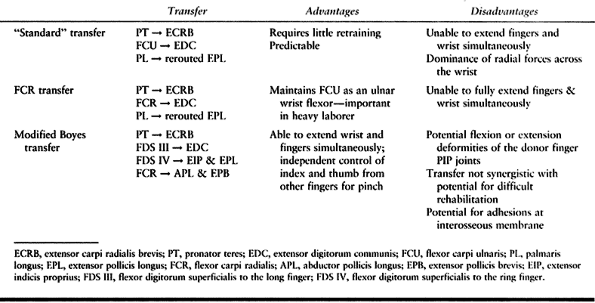
available transfers (Table 55.1). The transfers discussed here assume an isolated radial nerve palsy.
 |
|
Table 55.1. Transfers for Radial Nerve Palsy
|
resulting effects on tendon gliding from the adhesions that inevitably
form. Avoid longitudinal incisions along the path of the transfer,
which tend to form adhesions through their entire length between the
transferred tendon and the overlying fascia and skin. Incisions passing
directly over tendon junctures are especially troublesome and may
inhibit the transferred tendon from gliding. Make small transverse
incisions to mobilize muscle-tendon units if the unit is freely
dissectible from its surrounding structures. If the muscle to be
transferred requires significant dissection, avoid incisions that run
in a direct line with the proposed path of the transfer. The skin is
fairly mobile in the forearm, and adequate exposure can often be
obtained by simple retraction without extensive skin incisions.
motor tendons to restore wrist extension. Transfer the insertion of the
pronator teres to the extensor carpi radialis brevis at its
musculotendinous junction. Avoid the dual insertion of the pronator
teres to the extensor carpi radialis brevis and extensor carpi radialis
longus (3,4,9). Brand described the biomechanical reasons for avoiding dual insertion (6).
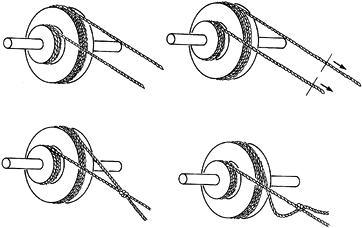
If each rope is wrapped around its respective pulley and pulled
separately, more rope unwraps from the larger pulley, which has a
larger moment arm. If the two ropes are tied together and tension is
placed on the knot, the rope around the larger pulley (larger moment
arm) becomes loose because a longer length of rope is pulled off the
larger pulley than the smaller one. The rope to the smaller pulley
remains tight and is therefore the only one effective in turning the
shaft. The extensor carpi radialis longus has a smaller moment arm for
wrist extension than does the extensor carpi radialis brevis. With
insertion of the pronator teres into both radial wrist extensors, as
the pronator teres begins to contract, the extensor carpi radialis
brevis with its larger moment arm for wrist extension becomes slack,
and the extensor carpi radialis longus provides the only effective
wrist extensor.
 |
|
Figure 55.3. A: Two ropes are attached to two different-sized pulleys on the same shaft. B: If each rope is pulled separately, more rope unwraps from the larger pulley. If the two ropes are tied together (C) and tension is placed on the knot (D),
the rope around the larger pulley will become loose because a longer length of rope is pulled off the larger pulley than the smaller one. The rope to the smaller pulley remains tight and is the only one effective in turning the shaft. (From Brand PW: Clinical Mechanics of the Hand. St. Louis: C.V. Mosby, 1985, with permission.) |
teres had only been transferred to the extensor carpi radialis brevis.
The extensor carpi radialis longus has a larger moment arm for radial
deviation of the wrist than for wrist extension, and with a dual
insertion of the pronator teres, attempted wrist extension results in
significant radial deviation.
rehabilitate or have less need for independent digital control, use
what is known as the standard or flexor carpi ulnaris (FCU) transfer (15,16,28,30).
Transfer the pronator teres to the extensor carpi radialis brevis for
restoration of wrist extension; the flexor carpi ulnaris around the
ulnar side of the forearm to the extensor digitorum communis for finger
extension; and the palmaris longus to the rerouted extensor pollicis
longus for thumb extension and abduction. One disadvantage of this set
of transfers is the inadequate excursion of the flexor carpi ulnaris to
accommodate wrist and finger extension. The patient is unable to extend
the wrist fully and the fingers at the same time. Brand also pointed
out the dominance of radial forces after this transfer (6).
We have not found this a significant problem among carefully selected
patients. The flexor carpi ulnaris transfer for finger extension has
been the most reproducible of such transfers. A recent report from
Roslein and Wilgis demonstrated that six patients were doing well at an
average of 8 years after an FCU transfer (27).
If the palmaris longus is not available, use the flexor digitorum
superficialis to the ring finger, which is divided between the A1 and A2 pulleys.
-
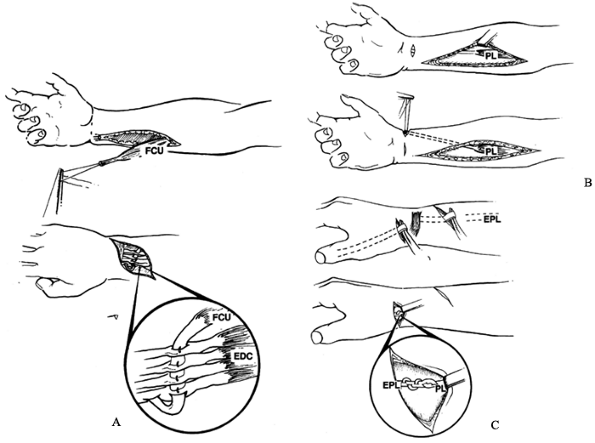
The incisions for the flexor carpi ulnaris transfer are shown in Figure 55.4.
Under tourniquet control, expose the pronator teres insertion through a
7 cm longitudinal midaxial incision (incision 1) over the middle third
of the radius while the forearm is held in neutral rotation.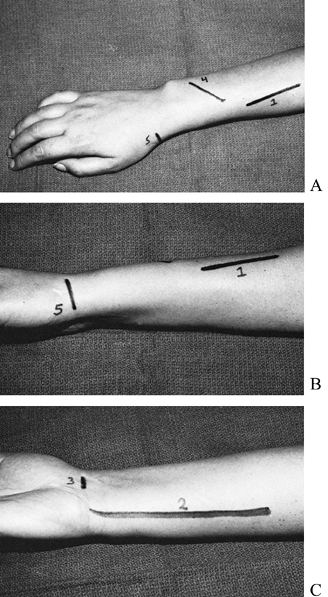 Figure 55.4. Incisions for the flexor carpi ulnaris (standard) transfer are shown. A: Dorsal incision. B: View of ulnar side. C: Palmar view.
Figure 55.4. Incisions for the flexor carpi ulnaris (standard) transfer are shown. A: Dorsal incision. B: View of ulnar side. C: Palmar view. -
Identify the insertion of the pronator
teres by developing the interval between the brachioradialis and the
extensor carpi radialis longus, carefully protecting the sensory branch
of the radial nerve. Even in radial nerve palsy, trauma to the sensory
branch may produce a painful neuroma. The insertion of the pronator
teres
P.1638
is predominantly muscular, with very little tendinous component. -
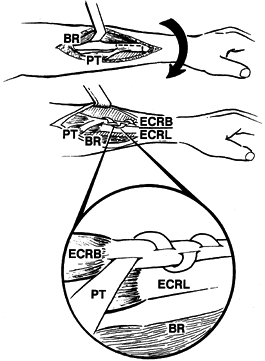
To gain sufficient tendon length, elevate the pronator teres off the radius with a 3 cm strip of periosteum (Fig. 55.5). The periosteum in adults is thin, and this strip is usually small; handle it with care (Fig. 55.6).
![]() Figure 55.5.
Figure 55.5.
Pronator teres (PT) to extensor carpi radialis brevis (ECRB) transfer
is illustrated. The pronator teres is elevated off its radius insertion
with a 3 cm strip of periosteum and then passed superficial to the
brachioradialis (BR) and the extensor carpi radialis longus (ECRL).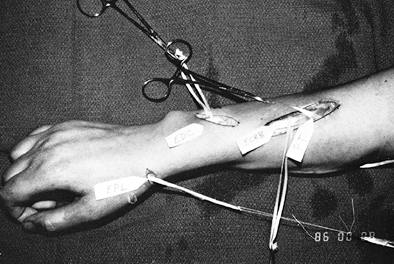 Figure 55.6.
Figure 55.6.
In adults, the strip of periosteum elevated off of the radius with the
pronator teres (PT) is thin and should be handled with care. -
Bring the pronator teres out proximally
from underneath the rachioradialis, and pass it superficially over the
brachioradialis and extensor carpi radialis longus to the extensor
carpi radialis brevis. Simply pronate the forearm to expose the
extensor carpi radialis brevis. The periosteal strip of the pronator
teres will later be woven through the extensor carpi radialis brevis
tendon just distal to the musculotendinous junction. Mobilize all the
muscle-tendon units, however, before completing any junctures. -
To expose the flexor carpi ulnaris (Fig. 55.7A),
make a longitudinal incision (incision 2) along the palmar ulnar
forearm directly overlying the flexor carpi ulnaris muscle belly.
Distally, start the incision at the proximal wrist crease just proximal
to the pisiform. Continue the incision proximally to the junction of
the middle and proximal thirds of the forearm.![]() Figure 55.7. The flexor carpi ulnaris transfer is shown. A:
Figure 55.7. The flexor carpi ulnaris transfer is shown. A:
The flexor carpi ulnaris (FCU) is mobilized and tunneled subcutaneously
around the ulnar border of the forearm. The flexor carpi ulnaris tendon
is passed through a slit in each of the extensor digitorum communis
(EDC) tendons in a proximal-ulnar to distal-radial direction at a 45°
angle proximal to the dorsal retinaculum. The palmaris longus (PL) is
mobilized (B) and tunneled subcutaneously to meet the rerouted extensor pollicis longus (EPL)(C),
providing simultaneous extension and radial abduction to the thumb. The
pronator teres is transferred to the extensor carpi radialis brevis for
wrist extension. -
Place a tag suture in the flexor carpi
ulnaris tendon, and detach it from its insertion on the pisiform. Use
the tag suture to provide traction on the tendon and to mobilize the
flexor carpi ulnaris from its underlying extensive origin from the ulna
and its overlying origin from the fascia. Stop this mobilization 5 cm
distal to the flexor carpi ulnaris origin to avoid damaging its
innervation from the ulnar nerve. -
Expose the extensor digitorum communis
tendons through a 3 cm oblique incision (incision 4) in the distal
forearm, cutting in a proximal–radial to distal–ulnar direction. Tunnel
a tendon passer subcutaneously from the ulnar margin of incision 4 to
the proximal extent of incision 2. With this tendon passer, bring the
flexor carpi ulnaris subcutaneously around the ulnar side of the
forearm to lie along the ulnar aspect of the extensor digitorum
communis. If the bulk of the distal muscle belly of the flexor carpi
ulnaris in its new position seems excessive, bring it out of its tunnel
and trim it from its tendon. -
If a palmaris longus exists, transfer it to the rerouted extensor pollicis longus (see Fig. 55.7B).
Reroute the extensor pollicis longus tendon subcutaneously along the
radial border of the wrist, enabling the transfer to extend and
radially abduct the thumb. -
Expose the palmaris longus distal
insertion into the palmar fascia through a 1 cm transverse incision
(incision 3) at the proximal wrist crease. Expose the proximal tendon
and muscle belly of the palmaris longus through the proximal portion of
incision 2. Divide the palmaris longus tendon distally, and deliver it
into the proximal portion of incision 2. -
Make a 2 cm transverse incision (incision
5) over the radial aspect of the wrist just distal to the radial
styloid, and expose the extensor pollicis longus tendon in the dorsal
extent of this incision. -
Identify and divide the extensor pollicis
longus tendon proximal to the dorsal retinaculum (incision 4), and
deliver this tendon from its dorsal compartment into incision 5. -
Tunnel a tendon passer subcutaneously
from incision 5 to the proximal extent of incision 2, and deliver the
palmaris longus tendon across the palmar aspect of the forearm into
incision 5 to meet the rerouted extensor pollicis longus. Deflate the
tourniquet, achieve hemostasis, and close incisions 2 and 3. -
Make the junction between the pronator
teres and the extensor carpi radialis brevis last, because the
tenodesis effect caused by flexing and extending the wrist is used to
make sure the tension of the finger and thumb transfers are appropriate
and produce synchronous motion. The juncture of the periosteal strip of
the pronator teres to the extensor carpi radialis brevis may be tenuous
and intolerant of the repeated wrist manipulations involved with
setting the tension of the finger and thumb transfers. -
For the flexor carpi ulnaris to extensor
digitorum communis transfer, we prefer an end-to-side juncture rather
than an end-to-end juncture. Some patients have demonstrated improved
motor function return even a few years after injury. Dividing the
extensor digitorum communis tendons for an end-to-end juncture deprives
the patient of a potentially superior result if any motor function
returns after the transfers have been completed. -
Pass the flexor carpi ulnaris tendon
through a slit in each of the extensor digitorum communis tendons in a
proximal–ulnar to distal–radial direction at a 45° angle (Fig. 55.7A).
Determine the site where the flexor carpi ulnaris is passed through the
extensor digitorum communis tendons by fully flexing the wrist and
fingers to make sure the juncture is proximal enough to remain
unrestricted by the dorsal retinaculum. Suture each extensor digitorum
communis tendon individually to the flexor carpi ulnaris with 4-0
nonabsorbable braided Dacron. -
The tension under which the transfers are
sutured is critical. Set the tension by placing the metacarpophalangeal
joints and the wrist joint in full extension, and suture the flexor
carpi ulnaris tendon under slight tension. -
For the palmaris longus to extensor
pollicis longus transfer, place the thumb, interphalangeal, and
metacarpophalangeal joints in full extension and the carpometacarpal
joint in full radial abduction. Weave the palmaris longus tendon three
times through the extensor pollicis longus tendon and suture it with
4-0 nonabsorbable braided Dacron, as described by Pulvertaft (Fig. 55.7C) (26).
Pull the palmaris longus tendon distally under mild tension while
completing this juncture. Move the wrist, fingers, and thumb through a
full range of motion to ensure that motion is synchronous and no
restrictions are caused by the junctures. -
Set the tension for the wrist transfer by
placing the wrist joint in maximal extension. Pull the pronator teres
under slight tension to the extensor carpi radialis brevis tendon just
distal to the musculocutaneous junction. Weave the pronator teres
through the extensor carpi radialis brevis tendon, and suture it in
place (Fig. 55.5). -
Assess the tension of all the transfers
again by rotating the wrist through a range of motion. With the fingers
fully extended with flexion of the wrist and with the fingers flexed
into the palm with extension of the wrist, a synchronous tenodesis
effect should be observed. -
In older patients or in patients who may
be difficult to reeducate, suture the musculotendinous units under
moderate tension to provide an extra component of sensory feedback
through the stretch reflex. -
Close the remainder of the wounds while
maintaining the wrist and fingers in maximal extension and the thumb in
maximal extension and radial abduction. Apply dressings and splints as
described under “Postoperative Care.” -
If the palmaris longus is not available,
use the flexor digitorum superficialis tendon to the ring finger to the
rerouted extensor pollicis longus for thumb extension and abduction.
Make a 1 cm transverse incision in the distal palm over the fourth
metacarpophalangeal joint, and divide the flexor digitorum
superficialis tendon between the A1 and A2
pulleys. Deliver the tendon into the middle forearm through incision 2,
and tunnel it subcutaneously into incision 5 to meet the rerouted
extensor pollicis longus. The juncture and tension are identical to
those described for the palmaris longus transfer.
difficulty if the flexor carpi ulnaris is sacrificed for transfer. The
flexor carpi ulnaris is a strong ulnar deviator and an important wrist
stabilizer, and it is necessary for activities like hammering. In these
patients, select the flexor carpi radialis to provide finger extension (5,35,39). The flexor carpi radialis also has a greater excursion than the flexor carpi ulnaris (6). This allows more extension of the fingers with wrist extension.
-
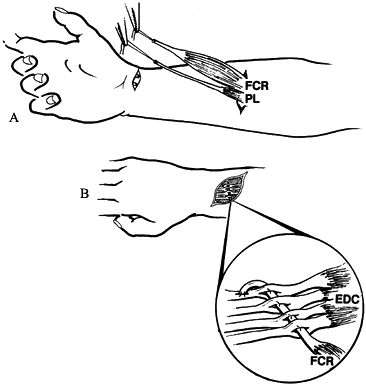
For wrist extension, use the pronator
teres to extensor carpi radialis brevis, which is exposed through a 7
cm longitudinal midaxial incision (incision 1) (Fig. 55.8) along the middle third of the forearm, as previously described.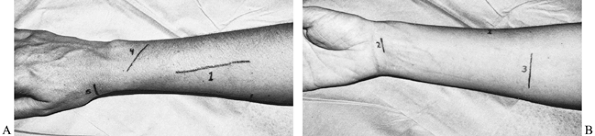 Figure 55.8. A, B: Incisions for the flexor carpi radialis transfer.
Figure 55.8. A, B: Incisions for the flexor carpi radialis transfer. -
Expose the insertion of the flexor carpi
radialis and palmaris longus through a 1 cm transverse incision
(incision 2) at the proximal wrist crease, extending from the radial
side of the flexor carpi radialis tendon to the radial side of the
palmaris longus. Avoid damaging the palmar cutaneous branch of the
median nerve with this incision. -
Expose the proximal muscle bellies of the
flexor carpi radialis and palmaris longus through a 3 cm transverse
palmar incision (incision 3) at the level of the junction of the
proximal and middle thirds of the forearm. Divide the tendons of the
flexor carpi radialis and palmaris
P.1641
longus
distally, free both of these muscle–tendon units of their fascial
attachments by blunt dissection, and deliver both into incision 3 (Fig. 55.9A).![]() Figure 55.9. The flexor carpi radialis transfer. A: The flexor carpi radialis (FCR) and the palmaris longus (PL) are mobilized through the same forearm incision. B:
Figure 55.9. The flexor carpi radialis transfer. A: The flexor carpi radialis (FCR) and the palmaris longus (PL) are mobilized through the same forearm incision. B:
The flexor carpi radialis is tunneled around the radial border of the
forearm and passed through a slit in each of the extensor digitorum
communis (EDC) tendons to provide finger extension. The palmaris longus
is transferred to the rerouted extensor pollicis longus for thumb
abduction and extension, and the pronator teres is transferred to the
extensor carpi radialis brevis for wrist extension. -
Expose the extensor digitorum communis
tendons through a 3 cm oblique incision (incision 4) in the distal
forearm, moving in a proximal–ulnar to distal–radial direction. Into
this incision, tunnel the flexor carpi radialis subcutaneously around
the radial side of the forearm superficial to the brachioradialis,
extensor carpi radialis longus, and extensor carpi radialis brevis.
Make a 2 cm transverse incision (incision 5) over the radial aspect of
the wrist just distal to the radial styloid, and expose the extensor
pollicis longus tendon in the dorsal extent of this incision. -
Return to incision 4, and identify and divide the extensor pollicis longus tendon at its musculotendinous junction.
-
Deliver the extensor pollicis longus from
its dorsal compartment into incision 5. Tunnel the palmaris longus
subcutaneously from incision 3 to meet the rerouted extensor pollicis
longus tendon in incision 5. -
Deflate the tourniquet, achieve
hemostasis, and close incisions 2 and 3. Make the junction between the
pronator teres and the extensor carpi radialis brevis last (see earlier
section on standard transfer). -
Pass the flexor carpi radialis tendon
through a slit in each of the extensor digitorum communis tendons in a
proximal–radial to distal–ulnar direction at a 45° angle (Fig. 55.9B).
Determine the site at which the flexor carpi radialis is passed through
the extensor digitorum communis tendons by fully flexing the wrist and
fingers to confirm that the juncture is proximal enough to be
unrestricted by the dorsal retinaculum. Suture each extensor digitorum
communis tendon individually to the flexor carpi radialis with 4-0
nonabsorbable braided Dacron. Set the tension in the flexor carpi
radialis to extensor digitorum communis transfer by placing the
metacarpophalangeal joints and the wrist joint in full extension.
Suture the flexor carpi radialis tendon under slight tension. -
For transfers of the palmaris longus to
the extensor pollicis longus and of the pronator teres to the extensor
carpi radialis brevis, do exactly as described earlier under standard
transfer. -
Close the remaining wounds while
maintaining the wrist and fingers in maximal extension and the thumb in
maximal extension and radial abduction. -
Apply dressings and splints as described
under “Postoperative Care”. If the palmaris longus is not available,
use the flexor digitorum superficialis tendon to the ring finger to the
rerouted extensor pollicis longus for thumb extension and abduction
(see description under “Standard or Flexor Carpi Ulnaris Transfer”).
motion in the fingers independent of wrist motion and who are
cooperative rehabilitation candidates, use a modification of the
transfer described by Boyes (4,10).
The flexor digitorum superficialis of the middle and ring fingers are
passed through windows in the interosseous membrane to act as finger
extensors. The flexor digitorum superficialis tendon of the middle
finger is sutured to the extensor digitorum communis of all four
fingers, and the flexor digitorum superficialis tendon of the ring
finger is sutured to the extensor indicis proprius and the extensor
pollicis longus.
finger and thumb from the other fingers for the pinch function. The
flexor carpi radialis is brought around the radial side of the forearm
to the abductor pollicis longus to provide thumb abduction. Boyes
describes insertion of the pronator teres into the extensor carpi
radialis longus and extensor carpi radialis brevis for wrist extension.
We insert the pronator teres only into the extensor carpi radialis
brevis for the reasons described earlier. In young patients, retraining
the out-of-phase flexor digitorum superficialis to act as a finger
extensor has not been a major problem.
-
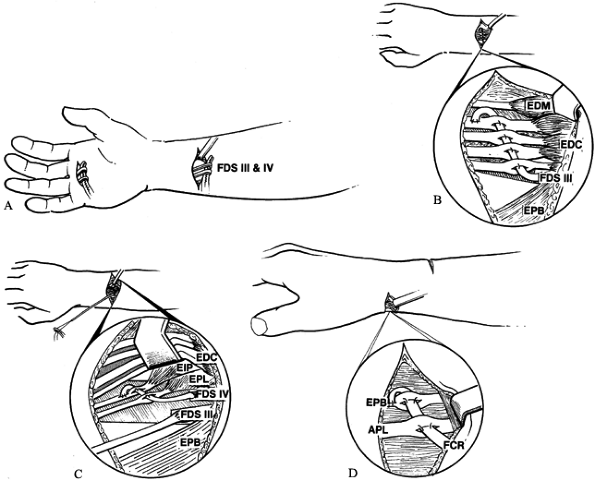
Under tourniquet control, expose the pronator teres insertion through a 7 cm longitudinal midaxial incision (incision 1) (Fig. 55.10) over the middle third of the radius while the forearm is held in neutral rotation.
 Figure 55.10. Incisions for the flexor digitorum superficialis (modified Boyes) transfer are shown. A: Dorsal incisions. B: Palmar incisions.
Figure 55.10. Incisions for the flexor digitorum superficialis (modified Boyes) transfer are shown. A: Dorsal incisions. B: Palmar incisions. -
Isolate and mobilize the pronator teres with a 3 cm strip of periosteum, as previously described.
-
Make a 2 cm transverse incision (incision
2) in the distal palm over the third and fourth metacarpophalangeal
joints, and identify the flexor digitorum superficialis tendons of the
middle and ring fingers between the A1 and A2 pulleys (Fig. 55.11A).![]() Figure 55.11. The flexor digitorum superficialis (modified Boyes) transfer is shown. A: The flexor digitorum superficialis tendons to the long and ring fingers (FDS III and IV) are divided distally between the A1 and A2 pulley and delivered into the midforearm. B:
Figure 55.11. The flexor digitorum superficialis (modified Boyes) transfer is shown. A: The flexor digitorum superficialis tendons to the long and ring fingers (FDS III and IV) are divided distally between the A1 and A2 pulley and delivered into the midforearm. B:
The two flexor digitorum superficialis tendons are passed through
windows in the interosseous membrane to the dorsal forearm. The flexor
digitorum superficialis to the ring finger is transferred to the
extensor pollicis longus (EPL) and extensor indicis proprius (EIP) to
provide index and thumb extension independent of finger extension. C:
The flexor digitorum superficialis to the long finger is passed through
a slit in each of the extensor digitorum communis (EDC) tendons in a
radial to ulnar direction to provide finger extension. The extensor
digiti minimi (EDM) is not included in this transfer if the extensor
digitorum communis tendon to the little finger is present. D:
The flexor carpi radialis (FCR) is transferred to the abductor pollicis
longus (APL) and extensor pollicis breves (EPB) to provide thumb
abduction. The juncture is made distal to the dorsal retinaculum. The
pronator teres to extensor carpi radialis brevis transfer provides
wrist extension. -
Identify the proximal flexor digitorum
superficialis muscle–tendon units through a 3 cm transverse palmar
incision (incision 3) at the junction between the middle and distal
forearm. Divide the flexor digitorum superficialis tendons between the A1 and A2 pulleys, and deliver the tendons into incision 3. -
At a level just proximal to the pronator
quadratus through incision 3, excise two 1 × 2 cm openings from the
interosseous membrane, one on each side of the anterior interosseous
artery, taking care to protect it and the posterior interosseous artery
on the dorsal side of the membrane. -
Expose the extensor digitorum communis,
extensor indicis proprius, and extensor pollicis longus tendons through
a 3 cm transverse incision (incision 4) just proximal to the wrist. -
Pass the divided flexor digitorum
superficialis tendons through the interosseous membrane, with the
superficialis tendon of the long finger passing radially between the
profundus tendons and the flexor pollicis longus tendon and the
superficialis tendon of the ring finger passing to the ulnar side of
the profundus tendons. -
Through a 2 cm transverse incision
(incision 5) at the base of the thumb, divide the flexor carpi radialis
tendon just proximal to the flexor retinaculum. Through this same
incision, expose the abductor pollicis longus and the extensor pollicis
brevis in the first compartment. -
Deflate the tourniquet, achieve hemostasis, and close incisions 2 and 3.
-
Retract the extensor digitorum communis
tendons ulnarly, and weave the ring finger superficialis tendon first
through the extensor pollicis longus and then through the extensor
indicis proprius tendon while
P.1643
maintaining
the index metacarpophalangeal, thumb, and wrist in extension and
pulling the superficialis tendon distally under moderate tension (Fig. 55.11B).
Make the juncture near enough to the extensor retinaculum to avoid
impingement when the wrist and fingers are flexed simultaneously. -
In bringing the superficialis through the
interosseous membrane, pull the tendon distal enough to present the
muscle belly into the interosseous window to prevent adhesions. Pass
the superficialis of the long finger through a slit in each of the
extensor digitorum communis tendons in a proximal–radial to
distal–ulnar direction at a 45° angle (Fig. 55.11C). -
Suture each extensor digitorum communis
tendon individually while you bring the superficialis tendon under
moderate tension distally and hold the finger metacarpophalangeal
joints and wrist joint in extension. -
Weave the flexor carpi radialis through the abductor
P.1644
pollicis longus and extensor pollicis brevis with the thumb in full
radial abduction and the flexor carpi radialis under mild tension (Fig. 55.11D).
Rotate the thumb through a range of motion to ensure that there is no
impingement of this latter juncture with the first dorsal compartment
tunnel. -
Complete the pronator teres to extensor
carpi radialis brevis juncture, as previously described. Close the
remainder of the incisions, and apply dressings and splints as
described under “Postoperative Care.”
brachioradialis, extensor carpi radialis longus, and in most cases, the
extensor carpi radialis brevis innervations are intact. A wrist
extensor need not be replaced in these patients. Because all of the
radial wrist extensors are intact, a significant amount of radial
deviation may occur with wrist extension. In this group of patients,
use the flexor carpi radialis for finger extension.
the ring finger may be transferred to the rerouted extensor pollicis
longus to restore thumb extension and abduction. For patients requiring
a greater range of finger motion, pass the flexor digitorum
superficialis of the middle and ring fingers through windows in the
interosseous membrane, to act as finger and thumb extensors. Use the
flexor carpi radialis to provide thumb abduction. Sacrificing the ulnar
deviating force of the flexor carpi ulnaris exaggerates radial
deviation caused by the radial wrist extensors. Therefore, we do not
use the flexor carpi ulnaris to obtain finger extension in posterior
interosseous nerve palsy.
the extensor carpi radialis brevis as an “internal splint” while
awaiting nerve recovery (9). This transfer
allows the patient to remain brace free. If neurologic return does not
occur, nothing has been lost and the remainder of the definitive
transfers can be completed. This transfer is useful in selected cases.
Patients with a poor prognosis for relatively early nerve recovery
because of a high radial nerve laceration, a large defect requiring a
long graft, or a nerve graft or nerve repair performed in a less than
optimal tissue bed are all considered candidates.
noncompliance or job-related conditions. We also consider early
pronator teres to extensor carpi radialis brevis transfer in these
patients. As with any tendon transfer, early transfers cannot be
considered until a full or near-full passive range of motion has been
achieved and tissue equilibrium exists (3).
-
Immediate postoperative care is similar
in each of the transfers. After the incisions have been closed, apply a
bulky plaster-reinforced compression dressing that maintains the elbow
at 90° of flexion, forearm in neutral, the wrist at 45° of
dorsiflexion, the metacarpophalangeal, the proximal interphalangeal,
and distal interphalangeal joints of the fingers at 0°, and the thumb
at maximal extension and abduction. No immobilization of the fingers or
thumb is required for the early transfer of the isolated pronator teres
to extensor carpi radialis brevis. -
Remove the dressing 10 days
postoperatively for suture removal. Apply a long arm cast, maintaining
forearm, wrist, and fingers in the same position. The patient wears
this cast for approximately 3 more weeks. Then change to a removable
short arm splint, maintaining the wrist in 45° of dorsiflexion and
metacarpophalangeal joints in 20° of flexion, and leaving the proximal
and distal interphalangeal joints free. Supervised physical therapy is
started at this time. -
Discontinue use of the splint 2 to 3
weeks later, unless an extensor lag at the metacarpophalangeal joints
or the wrist occurs, for which nighttime splinting is continued until
it resolves.
flexion contracture or hyperextension deformity at the proximal
interphalangeal joint. Littler suggested that these deformities can be
eliminated, at least to the point where no functional impairment
occurs, by dividing the flexor digitorum superficialis tendon
proximally between the A1 and A2 pulleys instead of at its insertion (22).
when the flexor digitorum superficialis (a finger flexor) is
transferred to the extensor digitorum communis or the extensor pollicis
longus (finger extensors). Many surgeons believe that the flexor
digitorum superficialis is an easy muscle to retrain, and in young
patients, this seems to be true (6,10). We avoid this transfer in older patients who may have difficulty with reeducation.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
JH. Tendon Transfers in the Hand. Proceedings of the 15th General
Assembly of the Japan Medical Congress. Medicine in Japan in 1959.
1959;5:958.
RG, Boyes JH, Stark HH, Ashworth CR. Tendon Transfers for Radial Nerve
Palsy: Use of Superficialis Tendons for Digital Extension. J Hand Surg 1978;3:560.
ER, Littler JW. Transferring the Flexor Superficialis Tendon: Technical
Considerations in the Prevention of Proximal Interphalangeal Joint
Disability. J Hand Surg 1980;5:498.