Proximal Humerus, Scapula, and Clavicle
Through its sternoclavicular and the acromioclavicular (AC) joints, the
clavicle contributes to the overall motion of the upper extremity. The
clavicle can protract and retract.394 It also rotates and elevates to contribute to shoulder abduction.2,263,394
In addition, the clavicle provides the attachment site for the two
predominant mobilizers of the upper extremity: the pectoralis major and
the deltoid muscles. The integrity of the clavicle, therefore, is
crucial to the optimal functioning of the entire upper extremity.
most frequently fractured bones in the body. First, the clavicle is
subcutaneous throughout most of its span, being situated on the
anterosuperior aspect of the thorax. Second, nearly all of the forces
imparted onto the upper extremity are transmitted through the clavicle
to the trunk. The clavicle is the bone most commonly injured during
labor and delivery, occurring in 0.5% of all deliveries and accounting
for nearly 90% of all obstetrical fractures.40,106,160,474
Congenital pseudarthrosis of the clavicle, usually right-sided, needs
to be distinguished from birth-related fractures. In older children,
clavicular fractures occur frequently, with the reported rates ranging
between 8% and 15% of all pediatric fractures.314,336,412
The incidence of obstetrical clavicle fractures is increased for larger-birth weight infants.40,106,272,332
In addition, deliveries requiring the use of instruments or specialized
obstetric maneuvers are more likely to result in clavicular fractures.106,194,272,332
Based on these findings, it has been postulated that fractures in these
difficult deliveries result from lateral-to-medial pressure on the
shoulders during passage through the narrow birth canal. However,
despite the above trends, the majority of birth-related clavicular
fractures occur in deliveries of average-birth weight infants who
receive routine and otherwise uneventful obstetrical care. Thus, on the
whole, obstetrical clavicle fractures are sometimes unavoidable
consequences of vaginal deliveries for anatomic or physiologic reasons
that may not be evident before or even after delivery.
 |
|
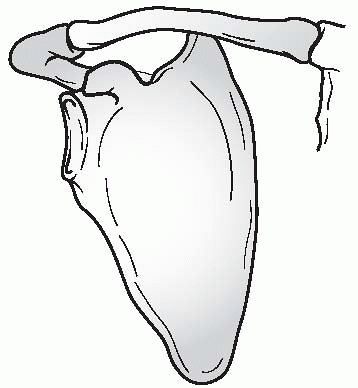
FIGURE 17-1 Relationship between the scapula, clavicle, and sternum.
|
Indirect applications of force, typically falling onto an outstretched
hand, are much less likely to result in clavicular fractures.525
Clavicular fractures may also occur in children victimized by child
abuse, but no pathognomonic pattern for isolated clavicular fractures
resulting from child abuse has been described.238,293
to the clavicle during athletic activities such as football or
indirectly through athletic activities such as gymnastics. Most
commonly, the direct mechanism is responsible for clavicle fractures,
AC joint injuries, or sternoclavicular joint injuries.314,412 A large proportion of these sports injuries may be preventable with the use of protective equipment and adequate padding.512 Although rare, stress fractures of the clavicle have been reported.2,593
identify. The presence of generalized edema may prevent the palpation
of normal clavicular margins.196 To
minimize pain, newborns with clavicular fractures demonstrate
pseudoparalysis of the affected arm, characterized by voluntary
splinting or immobilization of the ipsilateral arm.125,374
This pseudoparalysis is similar in presentation to a brachial plexus
birth injury. To reduce the pull of the sternocleidomastoid muscle
across the fracture site, affected infants turn their head toward the
side of the fracture. In addition, infants with acute clavicular
fractures typically exhibit an asymmetric Moro reflex.443,485
In the absence of radiographic confirmation, the diagnosis of clavicle
fracture may be suspected and later confirmed after a mass is noticed
in the affected clavicle. This mass represents a healing fracture
callus that forms 7 to 10 days after the initial trauma. Often by this
point, the fracture is sufficiently stabilized by fracture callus that
it causes little discomfort to the infant. At this stage of healing,
the pseudoparalysis will resolve. If there is an associated, unresolved
birth palsy, neurologic limitations would persist.
usually straightforward. Children have moderate to severe pain around
the area of the fracture and voluntarily immobilize and stop using the
affected arm. Tenderness, ecchymosis, and edema are invariably present;
in fractures with large displacement, a bony prominence or deformity
may be noted. Most children with clavicular fractures keep their heads
turned to the side of the fracture to relax the sternocleidomastoid
muscle.196
over the affected joints in children with either AC or sternoclavicular
joint injuries. The children usually self-protect against painful
motion of the limb. True dislocations of the AC joint or the
sternoclavicular joint are rare. Injuries to the medial and lateral end
of the clavicle in children are more commonly physeal fractures.
and clavicular fracture occur together on rare occasions. Attributing
acute torticollis entirely to the clavicular fracture may delay the
diagnosis of atlantoaxial displacement, and delayed diagnosis of
atlantoaxial displacement increases the risk of permanent atlantoaxial
rotatory fixation.3,57
When present, the child’s head will be laterally bent toward and
rotated away from the fractured clavicle. The diagnosis of C1-C2
subluxation is best confirmed by dynamic computed tomography (CT).
are particularly worrisome for associated injury or compression of the
great vessels, the esophagus, or the trachea.184,591
Suspicion of these injuries is further increased in children who have
difficulty speaking, breathing, or swallowing. Pulses in the
ipsilateral upper extremity may be diminished or absent, and the neck
veins may be distended if there is vascular compromise from the
displaced medial clavicle. Any of these injuries associated with
posterior sternoclavicular joint dislocations can be life-threatening,
and precautionary diagnostic and treatment steps should be taken at the
onset of treatment. If available, a thoracic or vascular surgeon should
be consulted or notified prior to reduction attempts.
the clavicle is the standard study for a clavicular fracture. In
addition, ultrasonography has been a valuable supplement in
establishing the diagnosis of clavicular fractures in neonates.230,285,287 Ultrasonography can be used to detect occult clavicular fractures.203,442 Bone healing may be detected on ultrasound 1 week before on radiographs.
necessary to supplement the AP radiograph in evaluating the clavicular
fracture. For fractures in the middle third of the clavicle, several
views may be beneficial: cephalad-directed views, the apical oblique
view, and the apical lordotic view. The cephalad-directed views are
helpful in illustrating the degree of fracture displacement. These
views are taken with the x-ray beam 20 to
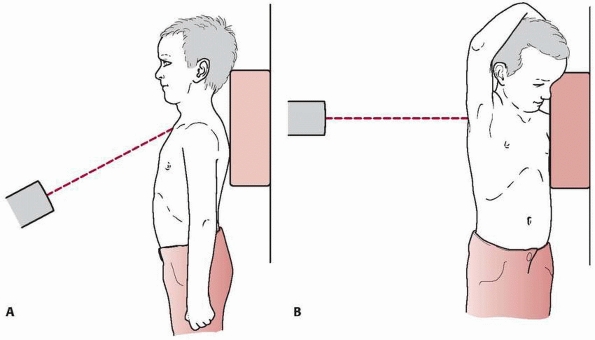
40 degrees cephalad to the clavicle (Fig. 17-2A).
The apical oblique view is taken with the x-ray beam 45 degrees lateral
to the axial axis of the body and 20 degrees cephalad to the clavicle.
This view is better suited to identify fractures in the middle third of
the clavicle, where significant curvature is present in the bone.574
The apical lordotic view is a perpendicular view of the AP radiograph.
It is taken laterally with the shoulder abducted more than 130 degrees (Fig.17-2B).
This degree of shoulder abduction, however, can cause significant
discomfort in children with acute clavicular fractures. Therefore, this
radiographic view may be better suited for evaluating the healing of
the clavicular fracture rather than for the initial assessment of the
fracture.456
 |
|
FIGURE 17-2 A. Cephalad-directed views. B. Apical lordotic view.
|
require additional radiographic views for full assessment. In addition
to the views mentioned above, an axillary lateral view is helpful in
evaluating the fracture and its displacement. If the injury to the
lateral clavicle or the AC joint is not obvious on the radiographs, a
radiographic stress view with the child holding 5 to 10 pounds of
weight with his or her hand or having an assistant gently pull on the
arm downward is helpful. The stress view may show subtle injuries to
the distal clavicle or the degree of instability with ligamentous
injuries to AC joint. If enhanced evaluation of the AC joint is
desired, a CT scan should be performed.
 |
|
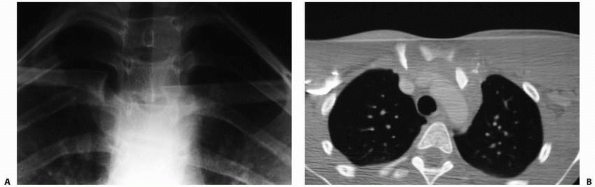
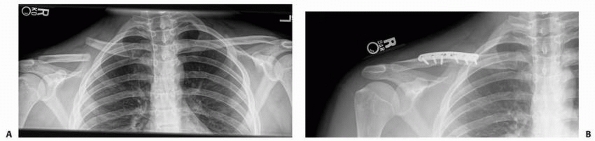
FIGURE 17-3 A. Serendipity view of the medial clavicle. Note inferior displacement of medial end of left clavicle. B. CT confirmed left sternoclavicular posterior dislocation.
|
characterize fractures of the medial third of the clavicle and
sternoclavicular injuries. The “serendipity” view, where a broad x-ray
beam with 40 degrees of cephalic tilt projects both clavicles on the
same film, is helpful for evaluating fractures in this portion of the
clavicle (Fig. 17-3).459
By comparing with the uninjured contralateral side, the location of
injury and the degree of displacement often can be determined. However,
this view can be difficult to interpret, especially for mild injuries.
Currently, CT is the best method for evaluating injuries in the medial
third of the clavicle. Thin slice CT provides detailed information
about the morphology of the medial clavicle, the medial physis, the
degree of displacement, and possible injury to the underlying
intrathoracic structures (Fig. 17-4). Virtually
every acute injury of the medial end of the clavicle should be
evaluated with CT, and it also is useful for follow-up of chronic
injuries.
and rate of injury, prognosis, and treatment options, clavicular
fractures
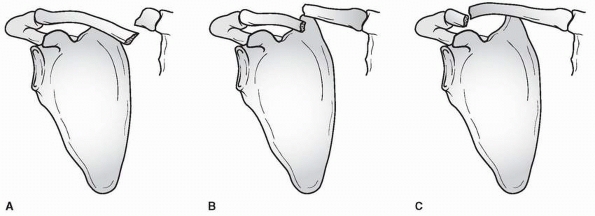
are broadly categorized by their anatomic location: medial third, middle third, and distal third (Fig. 17-5). Most clavicular fractures occur at the middle third, with the reported rates ranging from 76% to 85%.386,412 The second most common site of clavicular injury is the distal third, with the reported rates between 10% and 21%.386,412,451,469 Fractures in the medial third of the clavicle are relatively uncommon and represent only 3% to 5% of all clavicular fractures.412,469
 |
|
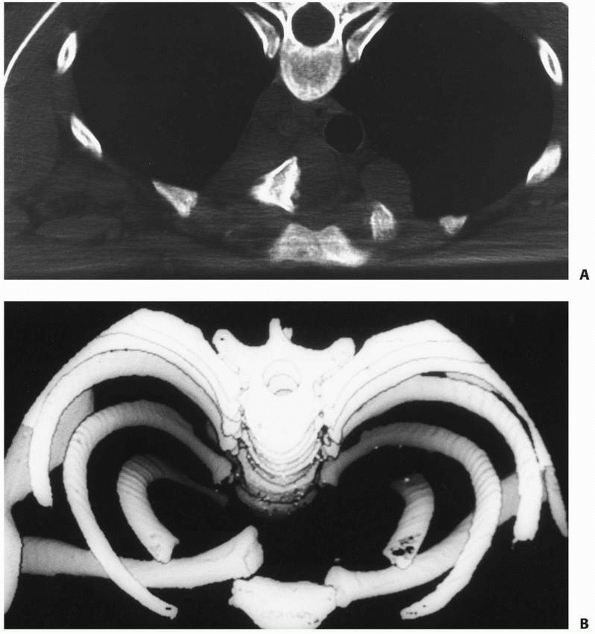
FIGURE 17-4 A. CT image of the clavicle showing posterior retrosternal dislocation of the medial end of the clavicle. B. Three-dimensional reconstruction of image shown in A.
|
Type I fractures occur in the middle third of the clavicle and
generally include all fractures lateral to the sternocleidomastoid
muscle and medial to the coracoclavicular ligament. Type II fractures
are in the distal clavicle, including all injuries lateral to the
coracoclavicular ligament. Type III fractures are medial to the
sternocleidomastoid muscle. Within this general framework, further
classifications exist for injuries to the distal and medial ends of the
clavicle.
 |
|
FIGURE 17-5 A. Fracture of the medial third of the clavicle. B. Fracture of the middle third of the clavicle. C. Fracture of the lateral third of the clavicle.
|
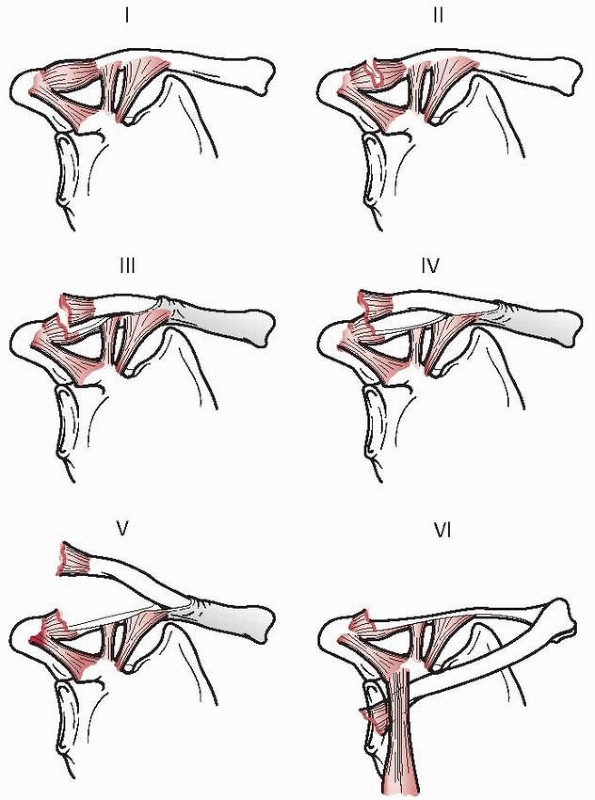
Distal clavicular fractures lateral to the coracoclavicular ligament
and injuries to the AC joint are categorized by a system proposed by
Dameron and Rockwood
(Fig. 17-6).125
Although derived from the system for adult distal clavicular injuries,
this classification system incorporates the observation that the distal
clavicle displaces through a disruption in its periosteal sleeve rather
than by true disruption of the coracoclavicular ligaments. Also, true
AC dislocations rarely occur in children. Most injuries in this region
are either metaphyseal or physeal fractures.159,420
However, because distal clavicular epiphyseal ossification does not
occur until age 18 or 19, these injuries may have the radiographic
appearance of an AC dislocation rather than a fracture
(pseudodislocation).159,420,543
 |
|
FIGURE 17-6 Dameron and Rockwood125 classification of distal/lateral fractures.
|
are characterized by mild strains of the ligaments or periosteal tears.
No gross changes are seen on radiographs. Type II injury includes
complete disruption of the AC ligaments or lateral periosteal
attachment, with mild damage to the superolateral aspect of the
periosteal sleeve. Mild instability of the distal clavicle results from
this type of injury, and minimal widening of the AC joint may be seen
on a radiograph. In type III injury, complete disruption of the AC
ligaments or periosteal attachment occurs in addition to a large
disruption in the superolateral periosteal sleeve. Noticeable superior
displacement of the distal clavicle is seen on an AP radiograph, and
the coracoid-clavicle interval is 25% to 100% greater than on the
contralateral uninjured side.73,126
Similar soft tissue disruptions are seen in type IV injuries. The
distal clavicle, however, is displaced posteriorly and is often
embedded in the trapezius muscle.31
Minimal changes may be noted on an AP radiograph, and an axillary
lateral radiograph may be required to identify the posterior clavicular
displacement. Type V injuries are similar to type III injuries; the
difference lies in the fact that the superior aspect of the periosteal
sleeve is completely disrupted in type V injuries. This allows
displacement of the distal clavicle into the subcutaneous tissues,
occasionally splitting the deltoid and the trapezius muscles. On an AP
radiograph, the coracoid-clavicle interval is more than 100% greater
than on the contralateral uninjured side. In type VI injuries, the
distal clavicle is displaced inferiorly, with its distal end located
inferior to the coracoid process.188
The medial physis of the clavicle is the last physis in the body to
close, and the fusion of this epiphysis to the shaft occurs as late as
23 to 25 years of age.274,572 The sternoclavicular ligaments attach primarily to the epiphysis, leaving the physis unprotected outside the capsule.296
Because of its unique anatomy, traumatic insults to the medial end of
the clavicle in children usually result in fractures through the physis
rather than dislocations through the sternoclavicular joint. Therefore,
these injuries are categorized most appropriately in the Salter-Harris
classification system.481 Most
fractures at the medial end of the clavicle are Salter-Harris type I or
II fractures. These injuries are further subdivided by the direction of
the clavicular displacement, either anterior or posterior. Although
anterior displacement of the clavicle occurs more frequently, more
attention is given to fractures with posterior displacement due to the
possibility of concomitant mediastinal injuries requiring emergent
intervention. Many anterior instability patients have ligamentous
laxity and no significant traumatic history. Posterior
fracture-dislocations are usually secondary to an adduction force, such
as a soccer goalie fall on the ground.
connected to the axial skeleton through the sternoclavicular joint. The
medial two thirds of the bone are tubular, whereas the lateral end is
flatter and is stabilized in its position by the two coracoclavicular
ligaments. The clavicle appears early during embryonic development. By
the fifth or sixth week of gestation, it begins ossification at two
separate centers: medial and lateral.183,394,418 By the seventh or eighth week of gestation, its overall contour and shape are already formed.183 During childhood, approximately 80% of clavicular growth and longitudinal growth occur at the medial physis.423
Despite this early ossification and growth, complete growth of the
clavicle does not occur until early adulthood. The lateral physis
continues to proliferate until 18 to 19 years of age, and the medial
physis does not close until 23 to 25 years of age.274,543,572
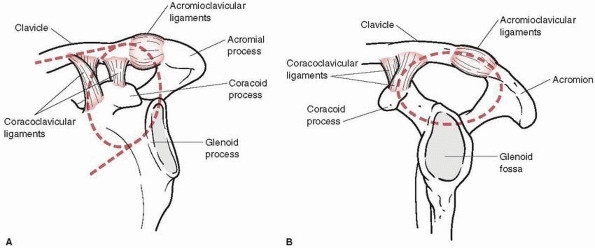
the AC joint, a joint that lacks inherent structural stability. It is
held together in part by the AC ligaments, which are relatively weak
secondary stabilizers. The primary stabilizers of the joint are the two
coracoclavicular ligaments, the conoid and the trapezoid, which
stabilize the lateral end of the clavicle next to the acromion.
Although the distal clavicle and the coracoid process usually do not
articulate, a coracoclavicular joint has been reported in adults.286 In children, the distal clavicle and the acromion are surrounded by thick periosteum that forms a protective tube
around the bony structures. The coracoclavicular ligaments are attached
to the periosteum on the inferior surface of the distal clavicle.
Because these ligament attachments are stronger than the periosteum,
displacement of the distal clavicle occurs through a disruption in the
periosteum rather than by detachment of the ligaments. In fact,
displacement of the distal clavicle through this periosteum in children
has been likened to having “a banana being peeled out of its skin.” As
mentioned above, the distal clavicular physis does not completely
ossify until late adolescence.543 Therefore, fractures through the distal clavicular physis or metaphysis may be mistakenly identified as AC joint dislocations.
 |
|
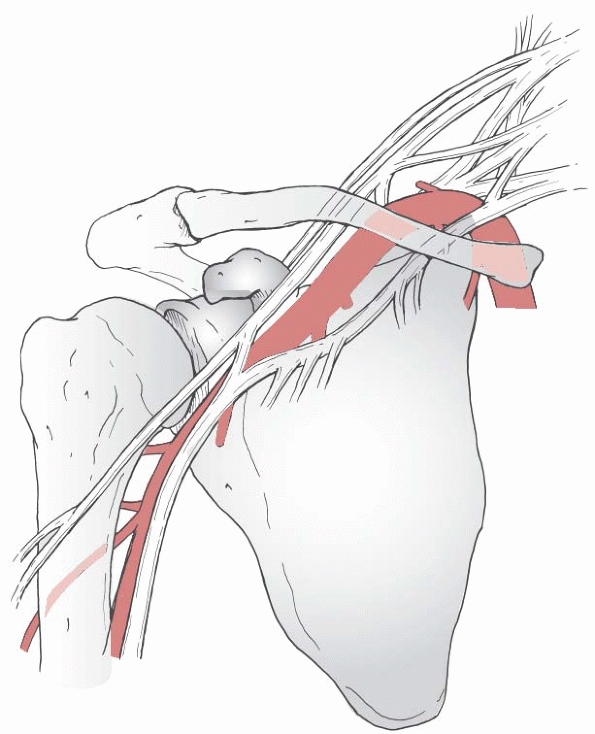
FIGURE 17-7 Relationship of the brachial plexus and artery to the proximal humerus and the scapula.
|
the first rib through the sternoclavicular joint. Similar to the AC
joint, this joint also lacks inherent structural stability. It is held
together by a series of strong ligaments, including the intra-articular
disc ligament, the anterior and posterior capsular ligaments, the
interclavicular ligament, and the costoclavicular ligament.41 In children, the medial physis of the clavicle is still open, and the capsular ligaments attach primarily to the epiphysis.41,274,572 Therefore, injuries to the medial clavicle typically result in physeal fractures with the epiphysis attached to the sternum.
|
TABLE 17-1 Interventions for Clavicle Fractures
|
|||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
number of different muscles. On its superior surface, the clavicular
head of the sternocleidomastoid muscle is attached. On the posterior
surface, the trapezius muscle is attached, whereas the pectoralis major
and the deltoid muscles are attached on the anterior surface.
Inferiorly, the clavicle provides attachment sites for the subclavius
muscle as well as the clavipectoral fascia.
vessels and the brachial plexus. These vital structures are located
posterior to the clavicle, crossing the clavicle at the junction
between the medial two thirds and lateral one third of the bone (Fig. 17-7).
Due to this close proximity, the neurovascular status of the
ipsilateral upper extremity may be jeopardized in children with
displaced clavicular shaft fractures. In addition, as discussed above,
posterior dislocation of the sternoclavicular joint can lead to
compression or injuries of the great vessels within the mediastinum.
Therefore, the neurovascular status of the ipsilateral upper extremity
must be documented before the initiation of treatment for any
clavicular injury.
motion and optimal function of the upper extremity. In the anterior to
posterior direction, the clavicle can protract and retract
approximately 35 degrees.394 Laterally, it can rotate and elevate to contribute approximately 30 degrees to shoulder abduction.263,394
The clavicle provides the attachment sites for the major mobilizers of
the upper arm, the pectoralis major, and the deltoid muscles. Finally,
together with the scapula, the distal clavicle forms the superior
shoulder suspensory complex (SSSC, described in the scapula section).
As proposed by Goss,202 the SSSC provides a scaffold from which the upper extremity suspends and articulates in order to function.
nonoperative. If the infant appears to be in significant discomfort,
the affected arm can be immobilized to the body for a short period of
time, typically less than 2 weeks. Immobilization of the affected arm
can be easily and effectively accomplished by using a safety pin
to attach the long shirt sleeve to the shirt or simple stockinette sling.279,361,484
The parents should be warned not to disturb the upper extremity by
unnecessary movements in the acute period. In addition, they should be
informed that the infant will develop a noticeable mass over the
fracture site that will typically resolve within 6 months.443
|
TABLE 17-2 Treatment Pros and Cons: Clavicle Fractures
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|
|
expected from nonoperative treatment with a sling or figure-of-eight
splint. This is particularly true in younger children. Furthermore,
reduction of clavicle fracture is seldom necessary because of the great
potential for remodeling these fractures.422
treatment in most cases of diaphyseal clavicle fractures. Use of a
sling is typically well tolerated by children and is not associated
with any of the difficulties of the figure-of-eight splint. Treatment
of both nondisplaced and displaced clavicular fractures with a sling
has shown remarkably good results. In fact, in comparison with a
figure-of-eight splint, treatment of clavicular fractures with a sling
resulted in similar final outcomes.13,273,524
One review found that complications such as nonunion, malunion, and
neurovascular problems were so rare in pediatric clavicle fractures
that follow-up beyond the initial visit was not necessary.81
Although reduction of the fracture is not required for a successful
outcome, correct application of the figure-of-eight splint retracts the
shoulders and may achieve improved alignment of the fracture.422
However, the figure-of-eight splint can be difficult to keep in proper
alignment and sometimes is poorly tolerated because of discomfort.
Caution must be exercised when using the figure-of-eight splint in
order to avoid known complications, such as edema, compression of the
axillary vessels, and brachial plexopathy.171,324,398
 |
|
FIGURE 17-8 A. Radiograph of displaced midshaft clavicle fracture of the dominant upper extremity of a throwing athlete. B. Surgical fixation was performed with a contoured plate and screws.
|
middle third clavicular fractures include severely displaced and
irreducible fractures that threaten skin integrity, concomitant
vascular injury requiring repair, irreducible compression of the
subclavian vessels, compromise of the brachial plexus, and open
fractures.252,267,396,439,598
In addition, as discussed separately in this chapter, concomitant
displaced fractures in various regions of the scapula, including the
acromion, the coracoid, and the scapular neck, may compromise the SSSC
and require operative repair.202
However, a prospective, randomized study reported that operatively
treated adult clavicle fractures had improved functional outcomes,
decreased time to union, and fewer symptomatic malunions and nonunions
than those treated nonoperatively with a sling.84
While the patients treated operatively also had more hardware-related
complications, the study supported primary plate fixation of midshaft
clavicle fractures in adults. Therefore, internal fixation can be
offered to active, skeletally mature adolescents and young adults with
displaced diaphyseal clavicle fractures (Fig. 17-8).
can be performed. Various precontoured clavicle plates are available.
Intramedullary stabilization with elastic nails or screws is a less
invasive procedure.280,304
Because of the subcutaneous location of the clavicle, implant
prominence can be expected and may lead to soft tissue irritation.84
population typically are pseudodislocations of the AC joint, with
fractures through the metaphysis or the physis and fracture
displacement through the torn periosteum.152,420
The AC joint and the coracoclavicular ligaments usually are undamaged.
Therefore, exceptional potential remodeling exists for these fractures,
allowing successful nonoperative treatment for most injuries to the
distal clavicle.
displaced injuries of the distal clavicle (types I, II, and III) are
treated without surgery.50,125,223,420,460
These injuries are managed with a sling immobilization followed by
early rehabilitation with range-of-motion exercises. Most children
treated with nonoperative management have no significant long-term
functional or cosmetic deficits.
clavicle fractures remains controversial. Some investigators report
that most children experience no functional deficits regardless of the
method of treatment.50,223
Others report that distal clavicular injuries with either fixed or
gross displacement should be treated with open reduction. In the young,
this involves periosteal repair and internal fixation in the older
patient to prevent permanent deformity.28,73,125,127,159,223,420,466
One report suggested that although displaced distal clavicular injuries
in children under 13 years of age may be amenable to nonoperative
treatment, those in children over 13 years of age should be treated
with open reduction and internal fixation.152 Any intra-articular fracture fragment displacement, similar to an adult injury, requires anatomic reduction and fixation.
grossly displaced distal clavicular fractures in children, as long as
the integrity of the SSSC is maintained, it appears that neither
nonoperative nor operative management results in long-term deficit in
the normal function of the shoulder. Treatment options, therefore,
should be individualized for each child and his or her family based on
compliance as well as acceptance of the possible cosmetic deformity.
fractures through the physis. Similar to distal clavicular injuries,
there is debate regarding the remodeling potential of these fractures.
Acute posteriorly displaced injuries are more commonly treated with
operative reduction and repair now.198,569
require active intervention. Symptomatic treatment is all that is
required for these stable fractures. In fact, nondisplaced fractures
often are missed during initial examination and are only discovered
after a mass or bump is noted over the medial clavicle and periosteal
healing is seen on the radiograph. The patient and parents should be
informed that the mass is a healing callus surrounding the fracture and
that it should remodel and disappear in 4 to 8 months.
are associated with atraumatic, generalized ligamentous laxity, similar
to multidirectional instability of the shoulder. These will
spontaneously reduce with shoulder motion and do not require emergency
room or acute operative care. Appropriate physical therapy and patience
is recommended. Late reconstruction for chronic, symptomatic
instability has variable results.27
There are rare acute, anterior traumatic dislocations. In adults, this
has been seen in power weightlifters with disruption of the anterior
ligaments. Closed reduction can be performed by longitudinal traction
to the affected upper extremity while the shoulder is abducted to 90
degrees.484 Gentle posterior
pressure also should be applied over the fracture for reduction. After
the reduction is accomplished, the clavicle should be immobilized with
a figure-of-eight splint.484
However, anteriorly displaced sternoclavicular dislocations do not pose
a risk to the underlying mediastinal structures, and once achieved,
maintenance of reduction can be difficult to maintain. Moreover, while
a cosmetic deformity exists, there is no evidence that there is a
decrease in shoulder function.48
Therefore, management without reduction and with a sling or
figure-of-eight sling is acceptable. With the rare, anteriorly
displaced physeal fracture, remodeling may occur in the young.
sternoclavicular dislocations require immediate evaluation for the
presence of concomitant injuries of the airway and/or great vessels. CT
scans are mandatory to assess the degree of displacement. Nondisplaced
and minimally displaced fractures can be treated without reduction.
These mild injuries can be expected to remodel without significant
residual deformity or pain. For fractures and dislocations with
significant posterior displacement or those associated with compromise
of the airway or great vessels, reduction should be performed. The
timing of this is based on whether the underlying structures are
compressed and whether the compression is causing respiratory or
hemodynamic compromise. Under general anesthesia, closed reduction has
been recommended, followed by open reduction if necessary. It is
advisable to notify thoracic surgery before beginning reduction in the
operating room in case of a mediastinal emergency and surgical
instruments should be prepared for a possible open reduction. Excellent
results have been reported with open reduction and stabilization with
either nonabsorbable or wire suture, and many centers now utilize this
as primary, definitive treatment for posterior fracture-dislocations of
the medial clavicle.198,569
general anesthesia, a bolster is placed in the midline between the
scapulae with the patient in the supine position. This positioning
alone may cause reduction. Gentle longitudinal traction through the
ipsilateral arm is then applied if necessary. If these reduction
maneuvers are unsuccessful, direct reduction using a sterile towel clip
is then attempted. After sterile preparation of the skin, the surgeon
pierces the skin with the towel clip and grasps the medial end of the
clavicle while an assistant applies longitudinal traction to the
ipsilateral upper arm. The clavicle is then manipulated into a reduced
position.484 If the above reduction
techniques are unsuccessful or the reduction is unstable, then open
reduction is performed. In many centers, closed reduction is no longer
attempted and open repair is primary treatment due to loss of reduction
by closed treatment.
chest, clavicle, and mediastinum to opposite anterior chest is prepped
in case of a surgical mediastinal emergency with reduction. An anterior
incision is utilized from the midportion of the clavicle to the
sternum. Dissection is carried through the platysma and fascia to the
periosteum while protecting the sensory nerves. Anterior periosteal
incision is started laterally to safely identify the bone. Care is
taken in dissection medially as the clavicle is displaced into the
mediastinum. Anterior dissection is completed to the sternum while
protecting the intact soft tissue attachments medially from the sternum
to the epiphysis in the posteriorly displaced, physeal fractures. A
bone-holding clamp is applied to the clavicle, and the anesthesiologist
is notified that reduction is to be performed. Reduction to anatomic
location is achieved. Careful hemodynamic monitoring is observed. If
all is well, then repair is performed. In the situation of a fracture,
nonabsorbable sutures are passed from the anterior medial metaphysis to
the epiphysis through drill holes. In the less common posterior
dislocation, the sutures are passed from the anterior sternum to the
epiphysis. Periosteal repair is then performed and this provides
anatomic reduction and stability. Internal fixation with metal implants
is contraindicated because of the possibility of implant migration with
resulting potential serious or fatal consequences.103
for postoperative immobilization for 4 to 6 weeks, followed by
range-of-motion and strengthening rehabilitation. Return to sports is
delayed until 3 months.
diagnosis and reassurance and education of the parents. The family is
told that a bump will develop over the fracture site and that the
fracture will heal uneventfully. If the infant initially demonstrates
discomfort with the fracture, the long arm sleeve of the infant’s shirt
can be pinned to the shirt for 7 to 10 days to provide adequate
immobilization.
generally have a significant level of pain and discomfort. We usually
prefer a sling for relief of pain through immobilization. Occasionally,
we use a figure-of-eight harness to provide retraction of the shoulder
to gain length at the level of the fracture and to reduce pain. With
the use of the figure-of-eight harness, it is important to inspect the
skin on weekly follow-ups for 3 weeks to ensure that no unusual sharp
bone fragments create any skin problems at the site of passage of the
figure-of-eight harness over the fracture. Despite this intervention,
the parents are still informed that the fracture will take a couple of
months to remodel and that there may be a bump for up to a year after
the fracture.
skeletally immature children is rarely indicated. The indications for
surgery are fractures that have the potential to develop full-thickness
skin loss over the apex of a fracture and fractures that cause
clavicular impingement on either the brachial plexus or the subclavian
vessels. Even with these fractures, gentle manipulation and closed
reduction should be attempted. Open fractures require open surgery. If
open repair is done, the fractured clavicle generally can be placed
into the periosteal sleeve and the periosteal sleeve can be repaired
over the fractured clavicle without the need for additional internal
fixation in the young. In the active, skeletally mature patient,
operative management and stabilization with a plate, intramedullary
screw, or flexible nail can be considered (see Fig 17-8).
The possible earlier union time by surgical stabilization and improved
function should be balanced against the potential for implant-related
complication, such as implant prominence.
treated nonoperatively by our team. A CT study is performed acutely on
every posterior displaced fracture or dislocation and on the majority
of injuries with anterior displacement as well. Anterior displacements
of the medial end of the clavicle generally are associated with
ligamentous laxity and usually treated nonoperatively. If a decision is
made to treat an anterior displaced physeal fracture with closed
reduction, longitudinal traction is applied to the upper extremity with
moderate abduction of the humerus, and general pressure is applied over
the sternoclavicular joint. Persistent instability with anterior
displacement of the sternoclavicular joint from laxity is acceptable.
With anterior physeal fractures, there may be remodeling. With or
without a reduction, after 2 to 4 weeks of immobilization, a program of
progressive rehabilitation can begin.
of the sternoclavicular joint may be either joint dislocations or a
physeal disruption. This injury may be acute and life-threatening. If
posterior displacement causes impingement of posterior vital
structures, closed reduction is performed under general anesthesia in
the operating room followed by open reduction if closed techniques are
unsuccessful. Some of these injuries can be treated successfully with
closed reduction with general anesthesia and stand-by support of the
cardiovascular service. Our current preference is to perform open
reduction in most cases.
and involves the placement of a bolster in the midline along the level
of the spine and spinous processes. Both humeri are adducted to the
level of the chest, and anterior pressure is placed over the deltoid
and humeral head toward the table with a downward pressure over both
proximal humeri. This is generally sufficient to provide adequate
retraction of the shoulder and restore the length of the clavicle at
the level of the sternoclavicular joint. Further downward pressure to
the level of the table provides a fulcrum force to reduce the medial
end of the clavicle anteriorly into the sternoclavicular joint. A towel
clip may be required to assist the reduction in difficult cases. When
performed, the towel clip is placed subcutaneously and grasps the
medial third of the clavicle to aid in the reduction process. It is
usually difficult to confirm reduction given the overlying soft tissue
swelling and technical difficulty in obtaining adequate confirmatory
radiographs, so a small incision is helpful in confirming reduction.
Furthermore, open reduction of the medial end of the sternoclavicular
joint is indicated when closed reduction fails or results in an
unstable retrosternal displacement. If the dislocation is unstable,
generally repair of the capsule with a nonabsorbable suture through the
capsule of the joint at the level of the sternum through holes drilled
into the medial
end
of the clavicle is sufficient to provide anterior stability of the
dislocation. Internal fixation is not recommended in this location.
Postoperatively, we place the patient in a figure-of-eight harness for
3 to 6 weeks after a closed reduction or a sling after an open
reduction and suture stabilization.
children and adolescents are treated nonoperatively. These fractures
heal rapidly because of the early deposition of periosteal new bone and
remodeling. Generally, patients can be treated with a sling and pain
management with appropriate oral analgesics and ice to control
swelling. Early range-of-motion therapy is recommended at approximately
10 days to 2 weeks. Clinical union is generally seen by 4 to 6 weeks.
clavicular injury, an open approach can be useful in replacing the
distal clavicle in its periosteal sleeve, and repair of the periosteal
sleeve may be sufficient to provide adequate fixation.
-
Every newborn with a delivery-related clavicle fracture should be evaluated for concurrent brachial plexus palsy.
-
Obtain a CT scan for posterior displaced medial clavicle fractures and posterior displaced sternoclavicular dislocations.
-
When performing reduction of posterior
displaced clavicles with a towel clip, grasp the clavicle in the
central portion of the middle third. This enables better mobilization
than grasping near the medial end. If adequate closed reduction is
uncertain or unstable, an open reduction and suture stabilization is a
safe and effective procedure.
association with clavicular fractures, including subclavian and
axillary artery disruption, subclavian vessel compression, and the
development of a arteriovenous fistula.37,252,276,387,547
In addition, displaced fractures of the medial clavicle may result in
compression or injury of the great vessels within the mediastinum.184,591
Occasionally, these compressions can be relieved nonoperatively by
reducing the fracture and eliminating the excessive pressure on the
vessels.252,387
However, if nonoperative treatment does not alleviate the vascular
compromise, operative reduction of the fracture and possible vascular
repair may be required. Certainly, if the structural integrity of the
vessels is compromised, operative repair by an experienced vascular or
thoracic surgeon is necessary.
displaced medial clavicular fractures can result in compression of the
trachea and esophagus, causing difficulty with speech, the airway, or
with swallowing (dysphonia or dysphagia).184,591 Clavicular fractures resulting from severe trauma can be associated with pneumothorax.146,382 Rarely, a pneumothorax results from obstetrical clavicular fractures.350
reported in association with both birth-related and traumatic
clavicular fractures. Brachial plexus palsy may present early or late
after the traumatic insult and occasionally requires operative
reduction of the fracture.37,131,132,252,268 Rarely, nerve deficits can result from inappropriate use of the figure-of-eight splints.324,398 Although permanent nerve deficits have been reported, most brachial plexus injuries resolve spontaneously.268,277
clavicular fractures have been associated with numerous complications,
including hardware irritation, migration, infection, and nonunion.103,170,373,374,408,493,494
Although most of these complications can be adequately treated, there
have been serious, even fatal, results from hardware migration.103
Therefore, whenever possible, fixation of pediatric clavicular
fractures should use nonmigratory, low-profile hardware. If plate
fixation is utilized, implant removal may be necessary and carries with
it the risk of refracture.
most children experience no long-term deformities because of their
tremendous potential for remodeling. Older patients with segmental or
marked fracture displacement may have symptomatic malunions.
Exostectomy or osteotomy have been performed in these circumstances.
Refracture does occur in less than 3% of clavicle fractures. Return to
contact sports should take this risk into consideration. Rare cases of
clavicular reduplication and cleidoscapular synostosis have been
reported.420,452 These unusual complications may require additional intervention.
should be distinguished from congenital pseudarthrosis and
pseudarthrosis secondary to other pathologic processes.72,77,408,429,451,566,584 Operative indications for posttraumatic clavicle fracture pseudarthroses are unacceptable cosmetic deformity and pain.55,77,364,584
However, operative repair with grafting and internal fixation of the
pseudarthroses have been associated with additional iatrogenic
complications, such as pneumothorax, subclavian vessel damage, air
embolism, and brachial plexus deficit.157
titanium elastic nails will take hold for severely displaced fractures
remains to be seen. There may be greater use of open reduction and
plate or intramedullary screw fixation of midshaft clavicle fracture in
the active, skeletally mature patient. Operative indications for
midshaft clavicular fractures without skin or neurovascular compromise
in adolescents remains debatable at this time.
protected by multiple layers of muscle and other soft tissue. Only 1%
of all fractures involve the scapula.202,221
However, when scapular injuries occur, they are almost certainly a
result of high-energy trauma and may be associated with significant
injuries to other major organ systems.377,540,583
Therefore, all children with apparently isolated scapular fractures
should be meticulously evaluated on the secondary trauma survey for the
presence of potentially life-threatening visceral injuries that require
further intervention.
into the glenoid fossa, which in turn results in the fracture.
Depending on the direction of the force, the fracture may injure the
rim of the glenoid or the entire glenoid fossa. Less commonly,
fractures may result from direct trauma to the glenoid.
occur via direct impact or avulsion mechanisms. The direct impact
mechanism is typically of high-energy and rarely is an isolated injury.
As with all other high-energy injuries, child abuse must be excluded as
a cause for scapular injury when no clear traumatic cause is evident.296 The avulsion-type fractures may occur at any of the several muscle attachments on the scapula.
and tenderness around the shoulder girdle and resist movement of the
affected arm. Localized edema may obscure the overall shoulder contour,
which may be more evident by comparison with the contralateral
shoulder. The diagnosis of scapular fractures is frequently missed
because of the attention required by more significant injuries.
many of which are life-threatening. In one reported series, the rate of
death among patients with scapular fractures exceeded 14%.540
artery and the brachial plexus, fractures of the scapula often are
associated with neurovascular injury.540
The ipsilateral arm must be carefully examined to document arterial or
neurologic deficits before the initiation of treatment. When injury to
axillary or distal vasculature is suspected, an angiogram may be
performed to examine the integrity of the vessels.
life-threatening injuries, such as hemothorax, pneumothorax, cardiac
contusions, as well as fractures of the spine, clavicle, rib, and
humerus.377,540
evaluation of the multiply injured patient. In the rare case where the
scapular fracture is the initially identified fracture, a complete
trauma evaluation should be undertaken for head, chest, abdominal, and
retroperitoneal injuries. If suspicion is high, a general trauma
evaluation may be requested. Conversely, scrutiny for fractures of the
scapula should be included in the evaluation of the multiply
traumatized child.
initially on the AP chest radiograph from a trauma series. However, AP
and lateral radiographs of the scapula will facilitate detection of
fractures not evident on the AP chest view, as well as allowing better
description of the fracture pattern. In addition to these, other
special radiographic views can aid in fracture characterization. The
Stryker notch view, for example, better reveals coracoid fractures,
whereas the axillary lateral view is better suited to identify glenoid
fractures. The axillary lateral view also is helpful in confirming the
location of the humeral head with the glenoid. When available, CT with
three-dimensional reconstruction provides the most detailed
representation of scapular anatomy. In addition, CT is essential in
characterizing intra-articular injuries of the glenoid.
also be scrutinized for evidence of scapulothoracic dissociation.
Scapulothoracic dissociation typically occurs in patients with massive,
direct trauma to the chest or proximal upper extremity and is highly
associated with ipsilateral neurovascular injury.150,471
This devastating injury should be suspected if the medial border of the
scapula is displaced laterally, if there is a clavicular fracture with
a large displacement, or if there is a complete AC joint separation
with large displacement.11,428
radiographic interpretation. For example, os acromiale is commonly
mistaken for an acute fracture. This variation occurs when the centers
of ossification in the acromion fail to unite.99
Os acromiale is considered a normal variant, is present in 10% of
normal shoulders, and is bilateral in 60% of affected individuals.11,335
Typically, os acromiale is located in the anterior and inferior aspect
of the distal acromion and has a smooth and uniform appearance on
radiographs. Occasionally os acromiale is symptomatic. If radiographic
studies and clinical examination cannot distinguish between a fracture
and a developmental variation, further evaluation with a bone scan may
clarify the diagnosis.150 Other
variants in scapular anatomy include Sprengel’s anomaly, absent
acromion, bipartite or tripartite acromion, bipartite coracoid, and
coracoid duplication.99,290,375,430,483
scapular fractures have been reported. Many are descriptive and based
primarily on the anatomic location of fracture. Ada and Miller4
divided scapular fractures into categories of acromion, spine,
coracoid, neck, glenoid, and body. In their series of children and
adults, fractures occurred most often in the body (35%), followed by
the neck (27%); fractures of the coracoid were least common (7%).4 Thompson et al.540
classified scapular fractures into three broad anatomic locations:
fractures of the glenoid and the glenoid neck, fractures of the
acromion and the coracoid, and fractures of the body (Fig 17-9). Other anatomic location-based scapular classifications have been reported by Imatani261 and by Wilbur and Evans.583
anatomic location of the fracture, with additional subclassifications
based on multiple reported studies (see Fig. 17-9 and Table 17-3).
However, most of these studies are not specific for pediatric scapular
fractures, so application of this classification system and its
supportive studies to pediatric scapular fractures should be
individualized to each child. The fracture should be adequately
evaluated for its anatomic location, displacement, comminution, and
articular involvement. In addition, ipsilateral neurovascular status,
the overall status of the patient, and other concomitant injuries
should be fully characterized.
which make up nearly 50% of all scapular fractures, are broadly
categorized into those with and without displacement. Although an
isolated fracture of the scapular neck is believed to be a stable bony
construct, ipsilateral fractures to both the scapular neck and the
clavicle may lead to disruption of the suspensory mechanism of the
shoulder.202,330 Therefore, fractures of the scapular neck are categorized into those with and without concomitant
injury to the clavicle. For similar considerations, fractures of the
coracoid process are categorized into those with and without
concomitant injury to the AC joint.
 |
|
FIGURE 17-9 General classification of scapular/glenoid fractures.
|
|
TABLE 17-3 Interventions for Scapular Fractures
|
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
with and without displacement. Displaced fractures are further
subclassified based on the presence or absence of subacromial
narrowing. Subacromial space narrowing may occur after inferior
displacement of the acromion or after superior displacement of an
ipsilateral glenoid fracture. When treated conservatively, these
fracture patterns often lead to subacromial impingement in adults and
result in decreased range of shoulder motion and increased shoulder
pain.305 Although its applicability
to acromial fractures in younger children is still debated, this
finding significantly affects the treatment options for acromial
fractures in older children.
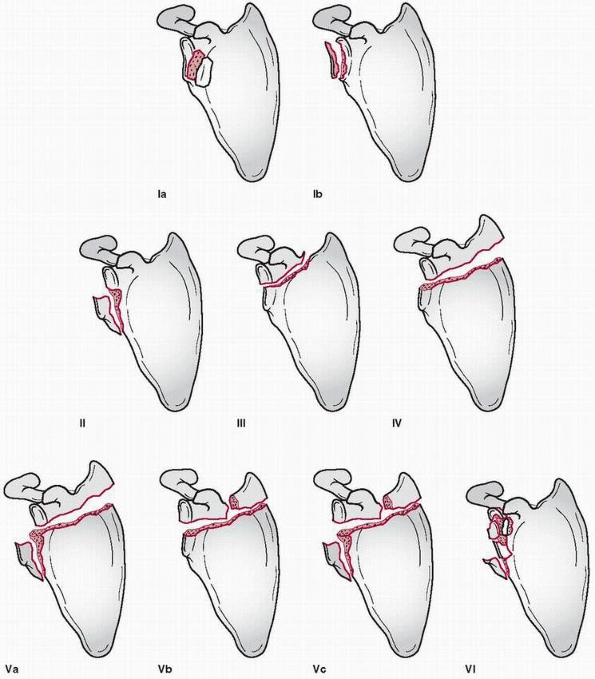
humeral head is driven onto the glenoid fossa. Depending on the
direction of the force applied to the humeral head, the fracture may
involve the entire fossa or just the rim. If the entire fossa is
involved, the fracture line may then exit in multiple locations about
the scapula. Hence, fractures of the glenoid are classified into five
distinct groups based on their anatomic location and course of the
fracture. This system was initially proposed by Ideberg257,258 and later expanded by Goss.201
Type I fractures are isolated glenoid rim fractures, with Ia involving
the anterior rim and Ib involving the posterior rim. Type II, III, and
IV fractures are glenoid fractures with fracture lines exiting through
lateral, superior, and medial aspects of the scapula, respectively.
Type V fractures are various combinations of type II, III, and IV
fractures. Type Va, for example, is a combination of types II and IV.
Type Vb is a combination of types III and IV, whereas type Vc is a
combination of types II, III, and IV. Type VI fractures are comminuted
fractures of the glenoid fossa. These various types of glenoid
fractures are associated with distinct patterns of morbidity and
treatment options.
or articulations between the thorax and the scapula are completely
severed. When there is an ipsilateral neurovascular injury, it is
sometimes referred to as a forequarter amputation. This is in contrast
to scapulothoracic dislocation, where only the inferior scapulothoracic
articulation is displaced.150 Although intrathoracic dissociations have been reported,406
scapulothoracic dissociations are typically laterally displaced. These
injuries are categorized as open or closed with intact or compromised
neurovascular status.
trimester of gestation. It first appears near the level of lower
cervical spine, C4-C7, and then descends to its final position on the
lateral aspect of the upper thorax during development. Most of the
scapula is formed by intramembranous ossification. Numerous centers of
ossification exist for the scapula: three for the body, two for the
coracoid process, two to five for the acromion,99
and one for the glenoid. These ossification centers during childhood
are often mistakenly identified as fractures. In some developmental
anomalies, distinct ossification centers fail to fuse and persist into
adulthood.375 These conditions are
also frequently characterized as fractures. With few exceptions,
however, a developmental variation and a fracture can be distinguished
by clinical history, physical examination, and radiographic appearance.
three-dimensional structure. It is responsible for linking the upper
extremity to the axial skeleton and contains attachments to 17 distinct
muscles. The anterior aspect of the scapular body is a relatively flat
surface, most of which is covered by the subscapularis muscle. The
posterior aspect of the scapula is divided into two fossae by the
scapular spine. These superior and inferior scapula fossae are mostly
covered by the supraspinatus and the infraspinatus muscles,
respectively. The anteromedial border of the scapular body provides
attachment to the serratus anterior muscle. The posteromedial border
contains the attachment sites of the levator scapulae, rhomboideus
major and minor, and latissimus dorsi muscles. The omohyoid muscle
attaches to the superior aspect of the scapular body, whereas the teres
minor and major muscles and the triceps muscle attach to the lateral
border. The scapular spine provides attachments to the trapezius and
deltoid muscles, and the long head of the biceps muscle originates from
the superior rim of the glenoid. Finally, the pectoralis minor muscle,
as well as the conjoined tendon of the coracobrachialis and short head
of the biceps muscles, attach to the coracoid process.
participates in the formation of both glenohumeral and AC joints. The
glenohumeral joint is stabilized by multiple dynamic and static forces
about the joint, which are discussed separately. The AC joint is
stabilized in part by the presence of two coracoclavicular ligaments
that position the distal clavicle immediately medial to the acromion.
The two ligaments are the conoid and the trapezoid ligaments, with the
conoid being the more medial of the two.
neurovascular structures that can be injured during a scapular
fracture. Most notable are the brachial plexus and the axillary artery,
which course across the anterosuperior aspect of the scapula. They are
immediately posterior and inferior to the tip of the coracoid process.
Medial to the base of the coracoid process is the scapular notch with
the overlying transverse scapular ligament. The suprascapular nerve and
artery pass under and over the ligament, respectively, in the scapular
notch and are susceptible to injury with nearby fractures. The axillary
nerve travels within an intermuscular interval immediately inferior to
the glenoid and is also susceptible to injury with displaced fractures
of the glenoid neck.376
locations about the scapula, with one fracture influencing the
stability of another. Goss202
proposed this and subsequently introduced the concept of a SSSC. The
SSSC is a set of bony struts attached to a circular complex of
structures at the lateral end of the scapula (Fig. 17-10).
The superior and inferior bony struts are the middle clavicle and the
lateral scapula body/spine, respectively. The circular complex is
composed of the AC ligament, acromion, glenoid process, coracoid
process, coracoclavicular ligament, and distal clavicle. As a whole,
the SSSC is responsible for linking the upper extremity to the axial
skeleton. Traumatic injury to any single component of the SSSC may
result in a minimally displaced fracture because the inherent stability
of the circular complex is still intact. However, when multiple
structures of the circular complex are injured, a double disruption to
the circle occurs. This, in turn, results in significant
instability.
Similarly, injury to one of the structures of the ring complex with a
concomitant injury to a bony strut also may create an unstable
construct. Goss202 proposed that the treatment decisions for scapular injuries should be based on the maintenance of SSSC integrity.
 |
|
FIGURE 17-10 Superior shoulder suspensory complex. A. AP view of the bone-soft tissue ring and superior and inferior bone struts. B. Lateral view of the bone-soft tissue ring.
|
evidence-based recommendations regarding current treatment options for
scapular fractures in children. Therefore, most of the following
comments are inferred from studies of adult populations.
the integrity of the SSSC. In addition, because of the numerous muscle
attachments, fractures of the scapular body are quite stable and can be
treated conservatively in most cases (see Table 17-3).
Several studies have shown that conservative treatment of nondisplaced
or minimally displaced scapular body fractures in adults is generally
associated with excellent results. Based on these studies, similar
treatment is recommended for equivalent fractures in the pediatric
population.261,410,471,488
In adults, conservative treatment of scapular body fractures with
significant displacement of more than 10 mm, however, resulted in
unfavorable outcomes.410 Since a
comparable study of pediatric scapular body fractures has not yet been
reported, we can only assume that widely displaced fractures in
children would have a similarly poor long-term outcome. The threshold
for acceptable displacement has not been described. A closed reduction
of an angulated, greenstick fracture or the scapula mimicking scapular
winging has been reported which yielded satisfactory results.58
without concomitant injury to the clavicle can be treated
conservatively.341 However, if there
is also ipsilateral clavicular injury, surgical intervention generally
is recommended to re-establish the SSSC.4,240,330,401 Whether open reduction and fixation of the clavicle is sufficient to stabilize the fracture240 or whether the neck fracture also must be reduced in addition to the clavicle330
is debatable. For patients in whom surgical intervention is not
possible, external fixation or traction may be an acceptable option.134
base. Isolated fractures of the coracoid process usually are
nondisplaced and can be treated conservatively with a sling and
mobilization as tolerated. Displaced coracoid fractures occur with
ipsilateral injury to the distal clavicle or the AC joint. Most
investigators favor open reduction and internal fixation of these
fractures to restore the integrity of the SSSC.390,471,583
Displaced coracoid fractures near the suprascapular notch with injury
to the suprascapular nerve also have been described, with some
investigators advocating early exploration.402
typically nondisplaced. In adults, acromial fractures with subacromial
narrowing are associated with subsequent development of subacromial
impingement when treated nonsurgically.305
Therefore, most investigators recommend open reduction and internal
fixation for displaced acromial fractures where the subacromial space
has been compromised,305 or with another disruption in the SSSC.202
unless other elements of the SSSC are disrupted. These fractures
generally have excellent outcomes with nonsurgical treatment.
Significant displacement or angulation, however, may limit glenohumeral
motion.134,410
In adults, glenoid neck fractures with more than 10 mm of displacement
or 40 degrees of angulation result in poor outcomes when treated
without surgical reduction.4
Therefore, it is reasonable to infer that pediatric glenoid neck
fractures with significant displacement or angulation also require
surgical intervention.
based on the presence or absence of shoulder instability.
Immobilization treatment of asymptomatic glenoid rim fractures rarely
results in long-term morbidity.601
For glenoid rim fractures with resulting shoulder subluxation or
instability, however, operative reduction and fixation are recommended
to prevent permanent or recurrent dislocations.134,214,221 In adults, shoulder instability occurs when the fracture was displaced more than 10 mm or
when the fracture involved more than either 25% of the anterior or 33% of the posterior aspects of the glenoid.134
Anterior and posterior approaches to the glenoid generally are
recommended for open reduction and internal fixation of anterior and
posterior rim fractures, respectively.202
Displaced fractures, on the other hand, are associated with significant
morbidity (pain, stiffness, and limited range of motion) when treated
without surgical reduction. Patients with intra-articular displacement
greater than 5 mm should be considered for surgical reduction and
fixation.134,323,519
In type IV glenoid fractures, where significant comminution is present,
acceptable operative reduction and fixation may be difficult to
achieve, and these fractures may be better treated with nonsurgical
options.202,258
For open reduction and internal fixation of these fractures, a
posterior approach generally provides the most acceptable exposure.202
generally focuses on stabilization and repair of the neurovascular
injury. If the axillary artery and the brachial plexus are not
salvageable, an early amputation should be considered.428
Limb salvage is usually attempted if limb viability cannot be
determined. Immediate exploration of the brachial plexus is warranted
when a concomitant vascular injury requires an operative repair. If a
vascular injury is not present, the brachial plexus need not be
explored acutely. After a period of 4 to 6 weeks, the extent of the
brachial plexus injury should be documented (physical examination,
electromyography/nerve conduction velocity, magnetic resonance imaging
[MRI]) prior to surgical reconstruction, such as nerve repair or
musculotendinous transfer.202,428
Immediate operative stabilization of an ipsilateral clavicular fracture
generally is necessary only if the bony instability compromises the
integrity of the neurovascular structures.
scapula or glenoid fractures can be undertaken more thoroughly. With
rare exception, scapula fractures are treated without surgery.
Fractures of the glenoid generally are treated with observation and
follow-up, including physical therapy and rehabilitation. For the rare
displaced glenoid intra-articular and highly displaced fractures, open
reduction with internal fixation is recommended.108
This is generally performed via an anterior deltopectoral approach, but
posterior approaches to the scapula and glenoid may be necessary
depending on the fracture type.
by closed manipulative methods. In those associated with residual
scapular deformity, an open approach may be required. With
scapulothoracic disassociation, it is important to attend to the
priorities of trauma care, including an appropriate and detailed
neurovascular examination. Vascular consultation or evaluation may be
required, given the potential for massive injury to the brachial artery
or plexus. In these instances, early or late amputation should be
considered.
-
Suspect scapula fractures in patients with multiple trauma and scrutinize the radiographs.
-
Maintain a high index of suspicion for visceral injuries when a scapula body fracture presents as an isolated injury.
-
Be aware of normal variants in scapular
anatomy, such as os acromiale. Review radiographs of the contralateral
scapula if necessary. -
Look for radiographic evidence of scapulothoracic dissociation.
-
Most scapula fractures are managed without surgery.
-
Highly displaced scapula body fractures and glenoid fossa fractures require open reduction and internal fixation.
concomitant injuries frequently associated with scapular fractures were
discussed throughout this section.11,261,471,540
Due to their proximity, the axillary and the suprascapular nerves may
be injured in association with glenoid and coracoid fractures,
respectively.376,402
In addition, the energy required to create scapular fractures likely
results in other injuries, such as rib fractures, pneumothorax, and
vascular avulsions. All or portions of the lower brachial plexus are
susceptible to injury with scapulothoracic dissociations.150,428,483 This devastating injury also has been associated with the development of compartment syndrome in the upper arm.588
The presence of a complete brachial plexus avulsion is predictive of a
poor functional outcome with a scapulothoracic dissociation.597
generally involve improper functioning of the upper extremity.
Displaced fractures of the scapular body and spine, for example,
infrequently result in upper extremity weakness and pain with movement.4
Similarly, fractures of the acromion can result in pain and decreased
range of upper extremity motion secondary to subacromial impingement.305
Displaced intra-articular fractures of the glenoid are associated with
glenohumeral subluxation or dislocation, as well as early progression
of degenerative arthritis.134,214,202,221
Most problems related to injuries of the scapula are not necessarily
related to treatment but are more often related to failure to
accurately evaluate associated major systems injuries.
skeletally immature children is rare. None of the ancient writings of
Hippocrates (460-375 B.C.), Galen (A.D. 131-201), and Paul of Aegena
(A.D. 625-690) made specific mention of this injury in children.460
Most textbooks that address children’s shoulder problems do not even
discuss dislocations of the glenohumeral joint, and others merely touch
on the subject.54,440,453,504,537,573
glenohumeral dislocations in children less than 12 years of age are
rare. Although several case reports have been presented, no
large series of this entity are available.227,237,337,565 In Rowe’s472
review of 500 dislocated shoulders, only 8 patients were under 10 years
of age. In this same series, 99 patients were 10 to 20 years of age,
but no details on skeletal maturity were given.470,472 Rockwood460
reported a series of 44 patients with shoulder dislocations,
predominantly adolescents. Many articles have been published on
adolescent patients without discussing their skeletal maturity.197,371,389,416
As the child reaches adolescence, the incidence of shoulder instability
increases, but in the skeletally immature patient, this injury can
still be considered rare. However, Marans et al.,365
in 1992, presented a series of 21 patients with open physes from two
major trauma centers. The recent trend in highly competitive, organized
youth sports may be a reason for the change. In addition, generalized
ligamentous laxity is clearly an associative causative factor for
glenohumeral instability in the young.
should be present to assign patients to this group, whereas patients
who dislocate with relatively minor trauma should be assigned to the
atraumatic group. The vast majority of traumatic dislocations are
anterior. The mechanism of injury is similar to that observed in the
adult. Typically, a force applied to the outstretched hand forces the
arm and shoulder into a maximally abducted, externally rotated
position. At this point, the humeral head is levered out of the glenoid
process anteriorly, with the head lodging against the anterior neck of
the glenoid. This occurs commonly in contact sports, falls, fights, and
motor vehicle accidents.51,247,392
A labral tear (Bankart lesion) and/or capsular stretch injury occurs,
potentially with a compression injury to the humeral head (Hill-Sachs
lesion).
all age groups, posterior dislocations represent only 2% to 4% of all
traumatic dislocations. The history for posterior dislocations is one
of violent trauma with the arm in a position of flexion, internal
rotation, and adduction. This can occur in falls and in motor vehicle
accidents as the arm braces the body against impact. Other common
mechanisms that produce posterior dislocations include convulsions and
electroshock. In these cases, the shoulder is dislocated posteriorly by
the violent contraction of the shoulder internal rotators, which
normally are stronger than the shoulder external rotators. The history
of the mechanism of injury and a high index of suspicion are necessary
to avoid missing a posterior dislocation.138,142,225,414,557
This problem represents traumatic epiphyseal separation of the proximal
humerus, which is certainly much more common than a true traumatic
dislocation of the shoulder in this age group. Most true traumatic
dislocations of the shoulder in the neonatal period occur in babies
with underlying birth trauma to the brachial plexus or central nervous
system.
reported on a 3-month-old infant with Erb-Duchenne palsy who sustained
a traumatic luxatio erecta of the shoulder during a planned shoulder
manipulation. Posterior dislocation of the shoulder also can occur as a
secondary traumatic phenomenon in unrecognized brachial plexus injuries
of the upper trunk at delivery.23,339,581,582 Green and Wheelhouse205
reported a dislocation in a 7.5-month-old infant that was secondary to
a septic brain injury. Progressive posterior dislocation and
glenohumeral deformity is extremely common in infants and children with
chronic birth brachial plexopathy.
is common in children and adolescents. The child who presents with
shoulder dislocation without a clear history of trauma should arouse
suspicion that atraumatic instability may be present. These patients
have inherent joint laxity that allows the shoulder to be dislocated
either voluntarily or involuntarily as the result of a minimal
traumatic event (Fig. 17-11).87
For example, throwing, hitting an overhead tennis shot, or pushing the
body up when in bed would not constitute significant trauma. These
patients have multidirectional instability. In the individual who
dislocates voluntarily, conscious selective firing of muscles while
antagonists are inhibited, combined with arm positioning, allows the
shoulder to dislocate. A key to the diagnosis is that atraumatic
instability, whether voluntary or involuntary, is not associated with
much pain. Even if reduction is necessary, the pain usually disappears
rapidly. In most instances, spontaneous reduction occurs without
manipulation.460 In these cases, the use of conscious sedation or general anesthesia will often lead to reduction without manipulation.
addition to multidirectional joint laxity, include Ehlers-Danlos and
Marfan’s syndrome, congenital glenoid and/or humeral deformities, and
emotional and psychiatric instability. True congenital dislocations of
the shoulder are most commonly associated with developmental defects
and multiple congenital abnormalities.99,114,187,208,436
Arthrogryposis, neglected septic arthritis, and neurologic defects also
have been implicated in atraumatic dislocations in the young child.23,197,205,232,528,581
anterior dislocation presents with a painful, swollen shoulder. Obvious
deformity is present with a prominent acromion and flattening of the
contour of the lateral upper arm. The arm is often supported by the
contralateral hand and held in a slightly abducted and externally
rotated position. Despite swelling, the humeral head can usually be
palpated in a position anterior to the glenoid.
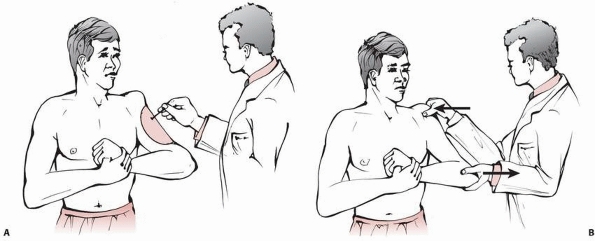
status should be performed. The axillary nerve is the most commonly
injured with anterior dislocation, and special attention to its
function should be included in the physical examination.53
The sensory distribution of the axillary nerve is along the upper
lateral arm, and motor innervation is to the deltoid and teres minor
muscles. Light touch is adequate for sensory testing in the upper arm
region. A convenient way to test deltoid function is to support the
involved elbow in one of the examiner’s hands while using the
examiner’s opposite hand to palpate the muscle belly of the deltoid.
The patient is asked to abduct the arm against resistance for about 1
inch so that deltoid firing is initiated. This examination confirms the
motor function of the axillary nerve (Fig. 17-12).
has spontaneously reduced, the arm is well located with an overall
normal appearance of the shoulder. The shoulder demonstrates a full
range of motion, although the patient avoids the cocking position in
abduction, external rotation. The apprehension test
with
the arm abducted above 90 degrees is positive. A positive apprehension
test, along with a suggestive history, is a very diagnostic physical
sign for recurrent anterior instability.
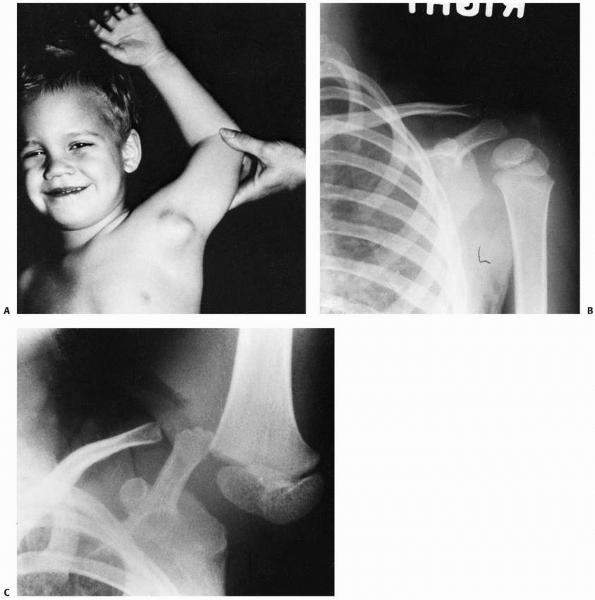 |
|
FIGURE 17-11
Congenital laxity of the left shoulder in a 4-year-old boy who is totally asymptomatic and has full range of motion of the left shoulder. A. With abduction and extension, the head subluxates anteriorly and inferiorly. B. An AP radiograph shows some lateral displacement of the humeral head. C. With overhead elevation, the humeral head is noted to displace anteriorly, laterally, and inferiorly. (Courtesy of Don Jones, MD.) |
dislocation, an affected patient presents with flattening of the
anterior aspect of the shoulder and posterior fullness. The arm is held
at the side with the forearm internally rotated across the chest. A
Putti sign with superior scapular winging is present. The patient
resists any attempt at motion. Although difficult to elicit in the
acute situation because of pain, hallmark findings of posterior
dislocation are lack of shoulder external rotation and inability to
supinate the forearm. It is advantageous to examine the shoulder with
the patient seated so that the examiner can visualize the shoulders
from above. From this perspective, posterior fullness and anterior
flattening can be better visualized. As for anterior dislocations, the
neurovascular status should be evaluated meticulously. A history of
convulsion or electrical shock should raise the index of suspicion for
posterior dislocation.
physis, the so-called pseudodislocation of the shoulder, can mimic an
anterior dislocation. As is the case for true dislocations, the child
is irritable and holds the affected arm abducted and externally
rotated. There is resistance to any type of motion.
patients with atraumatic shoulder instability is the relative lack of
pain associated with the subluxation or dislocation.15,128,288,321,362,473,511
Even in cases of involuntary atraumatic dislocation, the minor pain
associated with the dislocation itself subsides rapidly after
reduction. Episodes of atraumatic subluxation and dislocation
occur much more frequently than traumatic dislocations, and in almost all cases spontaneous reduction is the rule.
 |
|
FIGURE 17-12 A. Sensory distribution for the axillary nerve important in anterior dislocation. B.
Deltoid muscle can be tested in acute anterior dislocation by grabbing the muscle belly with the right hand while supporting the elbow with the left. The patient then can actively contract the deltoid by pushing the elbow against the examiner’s hand while the examiner feels the muscle contraction. |
Characteristics of multiple joint laxity include hyperextension at the
elbows, knees, and metacarpophalangeal joints along with pes planus.
Striae of the skin can be present. Skin hyperelasticity is a noted
characteristic of Ehlers-Danlos syndrome.
by a positive sulcus sign and significant translation on an anterior
and posterior drawer test. The sulcus sign is a dimpling of the skin
below the acromion when manual longitudinal traction is applied to the
arm (Fig. 17-13). This produces an inferior
subluxation of the humeral head away from the acromion that enlarges
the subacromial space and causes dimpling of the skin. The drawer or
shift and load test is performed with the examiner seated behind the
patient. The scapula is stabilized with one hand and forearm while the
humeral head is manually translated anteriorly and posteriorly by the
examiner’s opposite hand (Fig. 17-14). Although
some translation within the glenohumeral joint is expected in all
patients, those with multidirectional laxity demonstrate translation of
greater than 5 mm anteriorly and posteriorly from a neutral position.
anteriorly, posteriorly, or inferiorly. The most common direction of
dislocation in voluntary instability is posterior or inferior. The
patient who can voluntarily dislocate the shoulder can force the
humeral head posteriorly by contracting the anterior deltoid and
internal rotators while inhibiting the antagonistic muscles (Fig. 17-15).
The elbow is positioned in horizontal adduction, and the head is
dislocated. The arm can then be abducted, and the shoulder reduces,
often with an audible clunk.
be injured at the time of a shoulder dislocation, the axillary nerve is
the most common associated nerve injury. Fortunately, most axillary
nerve injuries associated with dislocations are neurapraxic and recover
spontaneously with time and observation. In the event of complete,
unresolved axillary nerve palsy, significant disability can result due
to the lack of deltoid function.35,53,105,116,153,353
reported an axillary artery and a brachial plexus injury in a luxatio
erecta dislocation in an 11-year-old child. The artery was repaired
with a vein graft and the brachial plexus injury fully recovered.
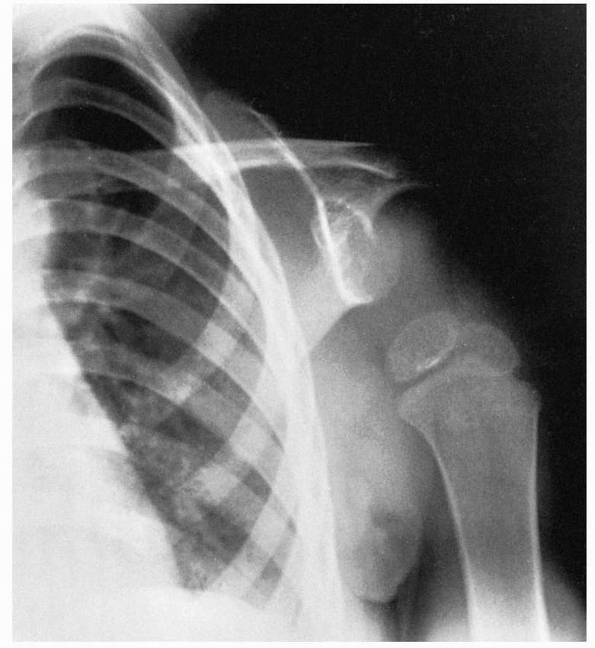 |
|
FIGURE 17-13
Dramatic demonstration of inferior subluxation of the glenohumeral joint in a patient with multidirectional instability. The clinical correlate is the sulcus sign. |
 |
|
FIGURE 17-14
Drawer test. This technique is used to subluxate the shoulder manually both anteriorly and posteriorly to demonstrate multidirectional laxity. |
growth plates have a low incidence of true traumatic dislocation of the
shoulder. Traumatic lesions on plain radiographs are similar to those
found in adults (Fig. 17-16). On the AP or
internally rotated views of the proximal humerus, the Hill-Sachs
compression lesion on the posterolateral aspect of the humeral head is
commonly found. This injury to the proximal humerus occurs as the
humeral head is impacted against the anterior rim of the glenoid during
a dislocation (Fig. 17-17). Bony injury to the
anterior glenoid rim can occur with dislocation as well. Injury to the
glenoid ranges from small avulsion-type fractures to substantial bony
fractures. Anterior glenoid rim injuries are best seen as a double
density on the AP view of the shoulder or as a separate fragment on the
axillary and West Point lateral views. The West Point lateral view
projects the anteroinferior glenoid rim and most clearly shows this
lesion when it is present. In traumatic posterior dislocation, the
reverse Hill-Sachs lesion can be seen on the anterior part of the
humeral head and in some cases will be seen in conjunction with
fracture of the posterior rim of the glenoid.
 |
|
FIGURE 17-15 Voluntary anterior dislocation of the right shoulder in an 8-year-old boy. A. The patient voluntarily has dislocated the right shoulder anteriorly. B.
The shoulder voluntarily reduced. The patient explained that he was taught to do this by an older brother who also had voluntary dislocation of the shoulders. |
which the diagnosis may be unclear clinically, an arthrogram with CT
scan can sometimes better delineate the extent of capsular stripping
from the anterior glenoid rim. More recently, saline arthrograms and
contrast MRI scans have enhanced our ability to define the degree of
injury to the labrum, capsule, and articular surfaces.210,461 CT scanning and MRI are useful for analyzing the significance of fractures of the glenoid rim (Figs. 17-18 and 17-19).
In addition, the size of the reverse Hill-Sachs lesion of the humeral
head in posterior dislocations is best analyzed with a CT scan.309,578
congenital or developmental defects, radiographs are usually normal.
Among patients who do have congenital defects, the most common
abnormality seen on radiographs is hypoplasia or aplasia of the
glenoid. In patients with multidirectional laxity and atraumatic
dislocation, stress radiographs can usually show instability in
anterior, posterior, and inferior directions. The inferior component of
multidirectional instability can be demonstrated by applying weights to
the arm in an AP film. If laxity is present, this stress view will show
the humeral head subluxating inferiorly in its relation to the glenoid.269
In diagnostic dilemmas, contrast-injected MRI scans can define the
presence of labral pathology which will aid in surgical decisions.
-
Traumatic dislocations.
-
Atraumatic dislocations—voluntary or involuntary
-
Congenital abnormalities or deficiencies of bone or soft tissue
-
Hereditary joint laxity problems, such as Ehlers-Danlos syndrome
-
Developmental joint laxity problems
-
Emotional and psychiatric disturbances
-
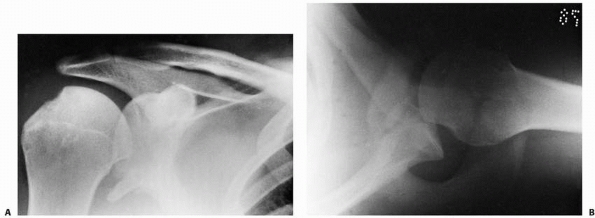 |
|
FIGURE 17-16 Traumatic anterior dislocation of the right shoulder in a 15-year-old boy. A. On the AP view, note the Hill-Sachs lesion as well as the anteroinferior bony fragment off the glenoid rim. B.
Axillary radiograph made with the arm in 90 degrees of abduction demonstrates the anterior subluxation as well as the deficiency of the anterior glenoid rim. |
adults, but no consensus exists as to a classification scheme in
children and adolescents.
degree, and chronicity. Two basic schemes have been used to classify
shoulder dislocations in children and adolescents. The more common of
these is based on the direction or location of the dislocation.
Although this scheme is useful in describing the clinical and
radiographic features of the injury, it does not address the underlying
pathology in children and adolescents.460
Therefore, a second classification scheme describing the etiology of
the dislocation is also useful when considering treatment options for
this injury in children. This second system is similar to that used for
adults but takes into account the rare congenital and developmental
problems unique to children. As discussed later in the section on
treatment of this problem, accurate classification is important in
selecting the appropriate conservative versus surgical options.21,125,421
 |
|
FIGURE 17-17 AP radiograph of anterior shoulder dislocation in a skeletally immature adolescent patient.
|
anterior, posterior, inferior (luxatio erecta), and multidirectional.
As in adults, anterior dislocation in children and adolescents is the
most common, constituting at least 90% of glenohumeral dislocations (Fig. 17-20).
Several isolated reports of posterior dislocation in children and
adolescents have been documented, but traumatic posterior dislocation
is rare in children, as in adults.60,168,237,372 Luxatio erecta or an inferior locked dislocation is uncommon but has been reported in children.174,320,380 Multidirectional luxatio of the shoulder has been well described as a distinct clinical entity by Burkhead and Rockwood,80 O’Driscoll and Evans,416 and Rockwood.460,461
subluxation or a dislocation. A subluxation is an incomplete
dislocation characterized by pain, a feeling of slipping, or a dead
feeling in the arm. A complete dislocation of the humeral head out of
the glenoid fossa is characterized by a displacement and locking of the
head on the rim of the glenoid.
acute, recurrent, or chronic. A single episode of instability can be
described as an acute injury. As in the skeletally mature patient, an
acute injury can lead to a recurrent instability, depending on the
damage to the labral, capsule and ligaments, and bony restraints of the
joint. A chronic instability exists when an acute dislocation
is not reduced, and in children, is usually associated with congenital or neuropathic dislocations.
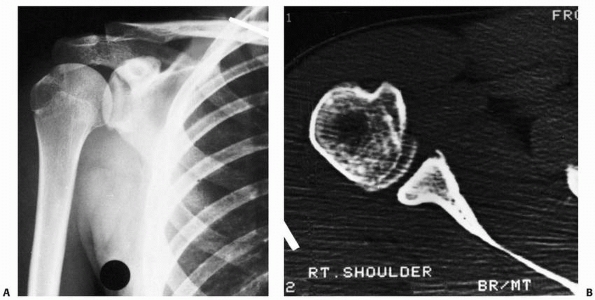 |
|
FIGURE 17-18 A.
AP radiograph of a 14-year-old boy with recurrent anterior subluxation. Notice the presence of a Hill-Sachs compression fracture on the humeral head and a subtle double density at the anteroinferior glenoid rim. B. CT scan shows this to be an avulsion-type bony injury of the anterior glenoid. |
the section on fractures of the proximal humerus. The glenohumeral
joint consists of the articulation between the large convex humeral
head and the relatively flat, concave glenoid fossa. Since there is
very little bony constraint inherent to the glenohumeral joint, this
joint is anatomically suited to accommodate the wide range of motion
necessary to perform upper extremity function. The articular surface
area and radius of curvature of the humeral head are about three times
that of the relatively flat glenoid surface. Although the glenoid fossa
is deepened by the labrum, the mismatch in the surface area and the
radius of curvature explains the relative lack of joint stability.
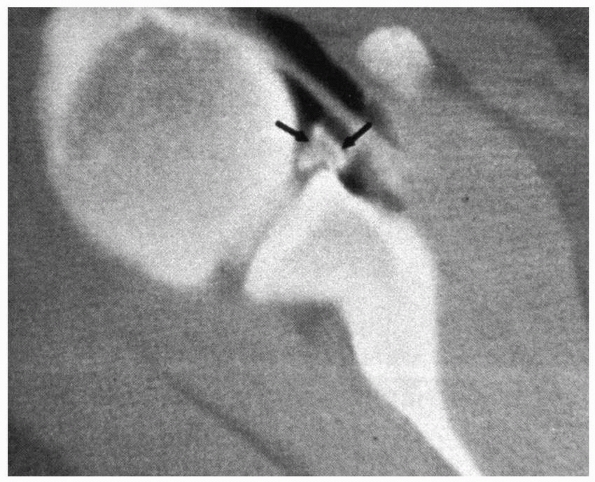 |
|
FIGURE 17-19 MRI in a patient with recurrent anterior instability of the shoulder. The arrows demonstrate a calcified bony Bankart lesion.
|
capsular/ligamentous complex. The capsule on its inner surface is
reinforced by thickened areas known as the anterior glenohumeral
ligaments. This complex capsular/ligamentous structure must provide
stability against abnormal translation while allowing a wide range of
motion. With the arm abducted, the inferior capsule is highly
redundant. The most important ligament is the anteroinferior
glenohumeral ligament, located within the inferior redundant area. It
is mechanically designed to tighten as the arm is abducted and
externally rotated, much like the effect of wringing out a washcloth.
This structure becomes the primary site of pathology in anterior
shoulder instability, either when the anteroinferior glenohumeral
ligament attachment to the glenoid and labrum is stripped from the
anterior neck of the glenoid or as these ligaments are disrupted in
midsubstance (Fig. 17-21). Disruption of the capsular labral attachment is known as a Perthes or Bankart lesion.
glenohumeral joint is along the anatomic neck of the humerus except
medially, where the attachment is more distal along the shaft. The
physis, therefore, lies in an extracapsular position except on the
medial side. As in most pediatric joint injuries, the strong capsular
attachment to the epiphysis makes failure through the physis a much
more common injury than true capsular/ligamentous injury.125,293,551 Therefore, fracture through the physis is more common than a dislocation in the skeletally immature patient.
supraspinatus, infraspinatus, and teres minor. These muscle-tendon
units surround the joint anteriorly, superiorly, and posteriorly. They
serve an important function as dynamic secondary stabilizers of the
joint by forming a force-couple with the large shoulder muscles
(deltoid, pectoralis major, teres major, and latissimus dorsi). As the
glenohumeral joint moves through its range of motion, the cuff provides
a dynamic stabilizing effect, preventing
excessive
translation of the humeral head on the glenoid. In addition, the biceps
and triceps as well as parascapular muscles are important dynamic
stabilizers of the shoulder. This is important when addressing
rehabilitation of acute and recurrent glenohumeral dislocation.
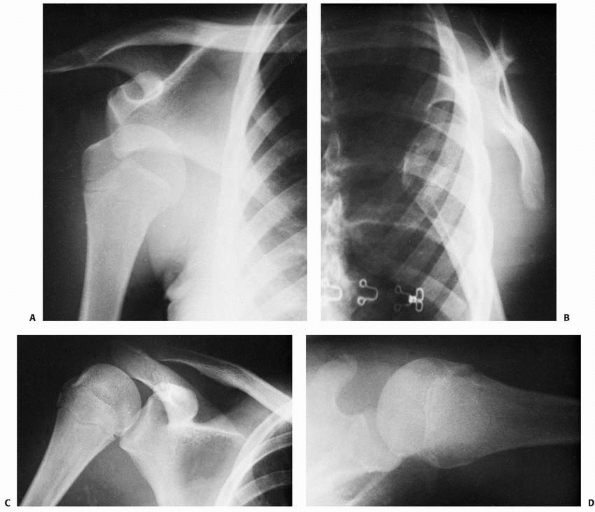 |
|
FIGURE 17-20 Anterior dislocation of the right shoulder in a 15-year-old girl. A. Note the typical subcoracoid position on the AP film. B. On a true scapular lateral film, note the anterior displacement of the humeral head. C. Postreduction film demonstrates a Hill-Sachs compression fracture in the posterolateral aspect of the humeral head. D. On the postreduction axillary film, note the posterolateral compression fracture of the humeral head.
|
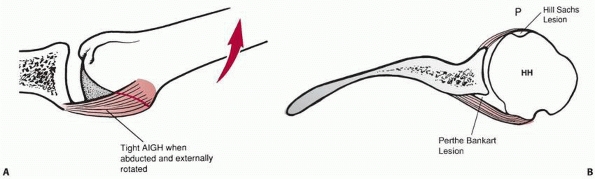 |
|
FIGURE 17-21 A.
The tight anteroinferior glenohumeral ligament complex with the arm abducted and externally rotated. This ligament sling is the primary restraint against anterior instability of the shoulder. B. A cross-section in the transverse plane through the glenohumeral joint demonstrates the common lesions associated with anterior instability of the shoulder: Hill-Sachs lesion, Perthes-Bankart lesion, and redundant anteroinferior glenohumeral ligaments. (HH, humeral head; P, posterior.) |
The majority of treatment recommendations presented in this section are
extrapolated from the adult and adolescent literature, as well as from
the experience of Dameron and Rockwood.125
undergo closed reduction by one of the standard techniques. For
anterior dislocation, many reduction techniques have been described.
Most clinicians prefer light sedation with intravenous or intramuscular
injection. The traction/countertraction method is believed to be the
most gentle. A bed sheet placed in the axilla of the affected shoulder
passes above and below the patient so that countertraction can be
applied to the body while longitudinal traction in line with the
deformity is applied to the arm. Steady, continuous traction fatigues
the muscles that lock the dislocation, and eventually reduction is
accomplished by disimpacting the humerus from the glenoid.
technique, the patient is placed prone on the examination table. A
weight is applied to the affected arm. As the shoulder girdle muscles
relax, reduction is achieved atraumatically (Fig. 17-22).389 Another less-often-practiced technique is scapular manipulation. Kothari and Dronen301 and McNamara379 report that this latter technique is a safe, effective way to reduce glenohumeral dislocations.
debate. The adult literature suggests that the period of immobilization
may not be truly important in predicting recurrent dislocation. A sling
or a sling-and-swathe with the arm internally rotated is the most
common method of immobilization.18,135
However, a recent randomized trial noted that immobilization in
external rotation may decrease the risk of recurrence when compared to
immobilization in internal rotation.265
|
TABLE 17-4 Interventions for Glenohumeral Subluxation and Dislocation
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
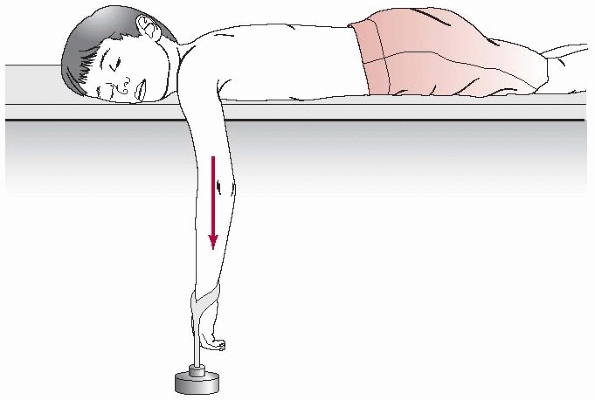 |
|
FIGURE 17-22
The Stimson technique for closed shoulder reduction. With the patient in prone position, weight is hung from the wrist to distract the shoulder joint. Eventually, with sufficient fatigue in the shoulder musculature, the joint can be easily reduced. |
somewhat similar to that for anterior dislocations.
Traction/countertraction is the most effective method. Traction is
applied in line with the deformity, and the humeral head is gently
lifted back into its normal relationship with the glenoid. Most
clinicians agree that immobilization should be with the arm in neutral
rotation or slight external rotation at the shoulder. This may require
the use of a spica cast or modified shoulder spica cast, as described
by Dameron and Rockwood.125
traumatic shoulder dislocation in children is understandably poorly
defined, given the rarity of reports in the pediatric orthopaedic
literature.187,249 In 1963, Rowe470
reported a 100% incidence of recurrence in children 1 to 10 years of
age with anterior dislocation. He also reported a 94% incidence of
recurrence in adolescents and young adults (ages 11 to 20).470 Elbaum et al.153
reported a recurrence rate of 71% in 9 pediatric patients with
traumatic anterior dislocations. The average age was 9 years. After
reduction, they were immobilized for 3 weeks and then were treated with
rehabilitation. However, Rockwood460 reported a recurrence rate of only 50% in a series of adolescents and young adults 13.8 to 15.8 years of age. Hovelius et al.249
reported a 47% recurrence rate in patients less than 20 years of age.
In the 25 years following, it was found that half of the primary
dislocations that had been treated nonoperatively in patients from 12
to 25 years old had not recurred or had surgical stabilization.248,250
Furthermore, recurrent dislocation necessitating operative treatment
had developed in 38% of shoulders in patients who were 12 to 25 years
of age at the time of initial dislocation, compared with 18% in
patients who were 26 to 40 years old. The type and duration of the
initial treatment had no effect on the rate of recurrence. Vermeiren et
al.558 reported a recurrence rate of 68% in patients younger than 20 years of
age. Younger patients involved in contact sports or who require
overhead occupational use of the arm are more likely to have a
redislocation when compared to older less active peers.477 They reported a better prognosis if the dislocation was associated with a fracture of the joint. Heck227 reported a case of traumatic anterior dislocation in a 7-year-old boy who remained stable at a 5-year follow-up. Endo et al.155
reported no recurrence in 2 patients, ages 3 and 9, with traumatic
anterior dislocation. However, the follow-up was only 2 years in the
3-year-old and 1 year in the 9-year-old. Wagner and Lyne565 reported an 80% recurrence rate in 10 patients with clearly open proximal humeral epiphyses. Marans et al.365
reported the fate of traumatic anterior dislocations of the shoulder in
21 children (15 boys, 6 girls) in what may be the largest documented
series to date. All the children had one or more documented anterior
dislocation(s) after the initial injury. Some of the children had been
immobilized in a sling-and-swathe for 6 weeks. The literature reflects
that the natural history of shoulder dislocations in adolescents and
young adults demonstrates recurrence rates for dislocation of 50% to
90% despite the treatment program used after the initial dislocation.
treatment of anterior shoulder instability. Once again, specific
results for procedures such as the Putti-Platt, Bankart, and
Magnuson-Stack have not been documented for children. Barry et al.36
described the effective use of the coracoid transfer for recurrent
anterior instability in adolescents. Capsular procedures that
specifically address the capsular pathology have been described by Neer,403 Jobe,349 and Rockwood et al.,461 but results in specifically in children’s dislocations were not documented. Goldberg et al.197 and Jones et al.278
have reported on the use of arthroscopic techniques for capsular repair
in adolescents. A meta-analysis at that time comparing open and
arthroscopic repairs in the treatment of anterior shoulder instability
found a significantly higher risk of recurrent instability, recurrent
dislocation, and reoperation for arthroscopic repairs. However,
arthroscopic repairs appeared to have a better functional result.326
The keys to any surgical procedure is labral repair and appropriate
capsular tightening. The trend is towards more arthroscopic repairs of
the labrum and capsule.
the shoulder appears more difficult than treatment for true traumatic
dislocations. Emphasis should be placed on careful diagnosis in these
cases. Specific congenital bony or neurologic deficits should be
recognized. The sequelae of Ehlers-Danlos syndrome or other collagen
deficiency syndromes should be noted.
or involuntary dislocations, a significant history of trauma is usually
lacking. These patients have minimal pain associated with the
dislocation and on clinical examination usually have other signs of
multidirectional laxity of the opposite shoulder. Most of these
dislocations reduce spontaneously and are associated with little pain.
Rowe et al.,473 Neer,403 and Burkhead and Rockwood80,460,461
have described the use of a vigorous rehabilitation program involving
strengthening of the rotator cuff as the treatment of choice for these
patients. Most patients who do not have significant emotional and
psychiatric problems are reasonably successful over time in improving
their shoulder stability with a program of scapular stabilization with
dynamic muscle rebalancing and strengthening.
is considered only if a strict 6- to 12-month rehabilitation program
fails. Shoulder reconstructions involving subscapularis shortening,
including the Magnuson-Stack and Putti-Platt procedures, or “bone
blocks” such as the Bristow are not sufficient for preventing future
instability, and are rarely performed. Neer403
described the inferior capsular shift reconstruction specifically for
patients with multidirectional laxity of the shoulder with atraumatic
instability. This procedure attempts to eliminate the overall capsular
laxity and is used only after rehabilitation has failed. Huber and
Gerber254 reported on 25 consecutive
children with 36 involved shoulders with voluntary subluxation of the
shoulder. The children managed by “skillful neglect” had a satisfactory
outcome, but only 50% of those treated with an operative procedure to
prevent later degenerative arthritis had good results. They concluded
that voluntary subluxation of the shoulder has a favorable result and
that there is no indication for surgery with this problem in children.
in children is to establish whether the dislocation is traumatic or
atraumatic in nature. A careful history of the mechanism of injury and
physical examination designed to elicit evidence of multidirectional
instability of the opposite shoulder, generalized joint laxity, or a
congenital or developmental problem will facilitate this distinction.
Care should be taken to identify the voluntary dislocator, who should
be treated nonoperatively in all cases, with rare exceptions.
reduction with analgesia or anesthesia should be performed.
Prereduction and postreduction radiographs are taken, and neurologic
and vascular examinations are performed before and after reduction. We
generally perform the traction/countertraction method under light
sedation. For an anterior traumatic dislocation, we immobilize the
shoulder in internal rotation for 4 weeks. For a posterior dislocation,
we immobilize the shoulder for 4 weeks in a prefabricated commercially
available splint or a modified spica cast with the shoulder in neutral
rotation. After the 4 weeks of immobilization, we institute a
rehabilitation program stressing rotator cuff strengthening.
dislocation is 50% or higher. Although we hesitate to intervene
surgically after the initial dislocation, the patient and parents
should be counseled regarding the high recurrence rate, in some cases
even after compliance to rehabilitation program. With a second
dislocation, the patient should be considered a recurrent dislocator,
and surgical intervention should be considered. If present, a Bankart
lesion is repaired anatomically to the anterior glenoid rim. A stable,
healed labrum in anatomic location is the key to surgical success
either open or arthroscopically. In cases without a Bankart lesion, we
use the capsular shift procedure as described by Rockwood.461 A capsular shift may also be used in conjunction with a Bankart repair to tighten the redundant anteroinferior capsule.
Care must be taken not to overtighten the capsule by either open or arthroscopic technique.
intervention. For the first month, pendulum exercises and gentle
elevation exercises are performed. The shoulder is protected in a
sling, especially at night. The second and third months are used to
regain range of motion, including protected external rotation. This
procedure is designed to address the pathology without limiting motion.
The fourth through sixth months are used for a progressive
strengthening program, which includes strengthening of the rotator cuff
and deltoid. At 6 months, the reconstruction is mature enough to
release the child to a full activity level.
accomplished if necessary after an acute dislocation in a fashion
similar to that described for traumatic dislocations. Again, attention
should be focused on confirming the diagnosis of atraumatic
dislocation. Patients with voluntary dislocation and their families
should be counseled that the dislocations can be harmful to the joint
and should be discouraged.
with a vigorous rehabilitation program. Only in the face of recurrence
after 6 to 12 months of supervised rehabilitation should surgical
intervention be considered. Great care should be taken to exclude the
voluntary dislocator as a surgical candidate. Psychiatric evaluation is
instituted if necessary. A capsular procedure as described by Neer or
the capsular shift technique described by Rockwood can be used to
eliminate laxity of the joint capsule in a circumferential manner.403,460,461
Surgical management of the atraumatic dislocator is difficult and
requires meticulous attention to detail during both the surgical
procedure and the postoperative rehabilitation program. Recurrence rate
is much higher in the atraumatic patient treated surgically.
for instability about the shoulder for both traumatic and atraumatic
problems is emphasized.18,125
Specific exercises are used to strengthen the rotator cuff and deltoid
muscles. The scapular stabilizers are also strengthened. Three-inch
wide strips of rubber (Thera-Bands, The Hygenic Corporation, Akron, OH)
are used to strengthen the cuff and deltoid muscles; Theratubes (The
Hygenic Corporation, Akron, OH) are used later if necessary.
progressive resistive strengthening varies depending on the extent of
the problem as well as the patient’s age, size, and baseline strength.
Exercises are performed four to six times a day. After basic
strengthening has been accomplished, isokinetic exercises using the
flexion/extension plane and the internal and external rotation plane
are effective for maximizing endurance and strength in the shoulder
girdle musculature.
the time of dislocation or during relocation. Although rare, axillary
or brachial plexus neurapraxia that does not spontaneously recover
requires neurodiagnostic evaluation and possibly surgical
reconstruction. Vascular injury should be evaluated immediately for
repair.
the success or failure rates of surgical reconstruction of the shoulder
for recurrent dislocation in children. As discussed, traumatic
dislocation in a child or adolescent can progress to recurrent
dislocation in 50% to 100% of cases. Rockwood et al.80,460,461
have shown that more than 85% of atraumatic dislocators can be managed
with a vigorous rehabilitation program and do not require surgery.
Surgical treatment of these problems in children could be expected to
have a success rate at least equal to that in adults. Greater than 90%
success in stopping traumatic dislocations would be expected with
surgical reconstruction.1,36,284
include recurrent dislocation, recurrent subluxation, painfully
restricted motion, problems with anchor migration or impingement about
the shoulder, and neurologic injury. Perhaps the most common problem
associated with the standard reconstructions about the shoulder that
include subscapularis tendon-shortening procedures (Magnuson-Stack and
Putti-Platt) is loss of external rotation. This loss in adults has been
associated in some patients with a more rapid progression to
glenohumeral arthritis.224,355 It is no longer recommended.
shoulder, including the Bristow and the DuToit stapling procedures,
have been associated with complications of metal impingement on the
humeral head or encroachment on the articular surface. Both problems
can lead to pain and eventual arthritic change.26,54,417,603 More recent osseous suture anchors may extrude into the joint and cause articular damage.
(Bankart repair) for the acute first-time traumatic dislocator remains
to be seen and played out in research of this injury. Initial
indications seem to suggest that the procedure has value for the very
active individual with a high likelihood of recurrent dislocation.
Arthroscopic results continue to improve as these techniques become
more disseminated. In the future, long-term studies will provide for
further comparison with open repair procedures.
uncommon injuries of childhood, with an incidence of 1.2 to 4.4 per
1000 per year,45,313,590 fewer than 5% of all pediatric fractures.242,264,313,314,467
Fractures in this region have enormous potential to heal and remodel,
perhaps more so than anywhere else in the body, mainly due to the thick
periosteum of the proximal humerus, the proximity to the physis, the
near universal motion of the joint, and the fact that 80% of humeral
growth is proximal. Thus, proximal humeral fractures in children with
sufficient growth remaining can be expected to heal without significant
residual functional or cosmetic deficits in most cases.
arm may be stressed such that a separation through the physis of the proximal humerus can occur.124,209,218,222,325,361,509
These fractures are generally believed to result from hyperextension
and/or rotation of the arm during the passage through the birth canal (Fig. 17-23).124,209,218,222,325,361,509
As might be expected, obstetric proximal humeral fractures occur most
frequently during vaginal deliveries of infants with larger size or
breech presentation.83,177,271,509
Prenatal size and presentation, however, have not been accurate
predictive factors for these fractures because proximal humeral
fractures may occur during vaginal deliveries of infants of all sizes
and weights. Hence, other infant and maternal factors play a role.83,177,271
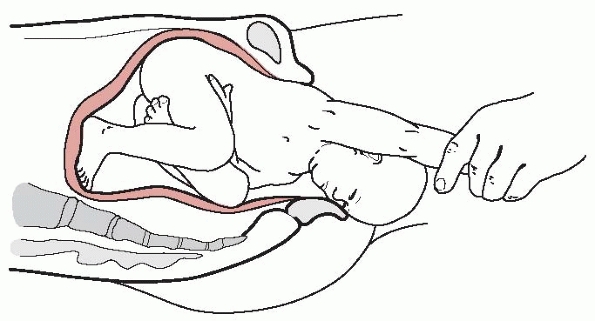 |
|
FIGURE 17-23 Hyperextension or rotation of the ipsilateral arm may result in a proximal humeral or physeal injury during birth.
|
the proximal humerus is trauma, both direct and indirect. In this age
group, these fractures can involve the metaphysis, the physis, or both.
The trauma can be a direct blow to the shoulder area, especially to the
posterior aspect,124,404,515 or indirect, as in a fall onto an outstretched hand that transmits the force through the arm to the proximal humerus.6,67,271
Indirect trauma can result in forced or nonphysiologic positioning of
the upper extremity, which in turn may cause a fracture of the proximal
humerus. Specifically, six potential mechanisms of upper extremity
positioning have been proposed to explain the resulting proximal
humeral fractures: forced extension, forced flexion, forced extension
with lateral or medial rotation, and forced flexion with lateral or
medial rotation.585 Although trauma
has been acknowledged as the most common mechanism of pediatric
proximal humeral fractures, it is still controversial whether a fall or
a direct blow is the more common etiology of the fracture.
higher-energy injuries and are frequently seen in motor vehicle crashes
and sporting activities (Figs. 17-24 and 17-25).30,298 Approximately 50% of shoulder girdle fractures in children have been reported to be associated with sports and play activities.411
Athletic activities associated with proximal humeral fractures include
contact sports (football, hockey), horseback riding (fall from horses),
gymnastics (upper extremity impact and weight bearing), and baseball
(repetitive throwing).121,314,345,548
pathologic and result from other conditions such as malignant or benign
tumors and pituitary gigantism.5,308,458,484 They also can be a complication of radiation therapy to the shoulder region.151
In addition, shoulder joint neuropathy secondary to Arnold-Chiari
malformation, myelomeningocele, or syringomyelia has been implicated as
an etiologic factor in proximal humeral fractures.30,346 An unknown percentage of pediatric proximal humeral fractures are part of the injuries associated with child abuse (Fig. 17-26).175
Because no clear fracture pattern in the proximal humerus is suggestive
of abuse, an index of suspicion must remain high when evaluating
infants or young children with humeral fractures.505
 |
|
FIGURE 17-24 Motor vehicle crashes may result in proximal humeral fracture due to blunt trauma to the shoulder region.
|
newborns may be subtle and not readily identified. For example, the
infant may be irritable when handled by caregivers or when there is
movement of the upper extremity. The infant may refuse to move the arm,
giving the appearance of paralysis, called “pseudoparalysis.” Infants
exhibiting upper extremity paralysis also may be suffering from
posterior humeral head dislocation.544
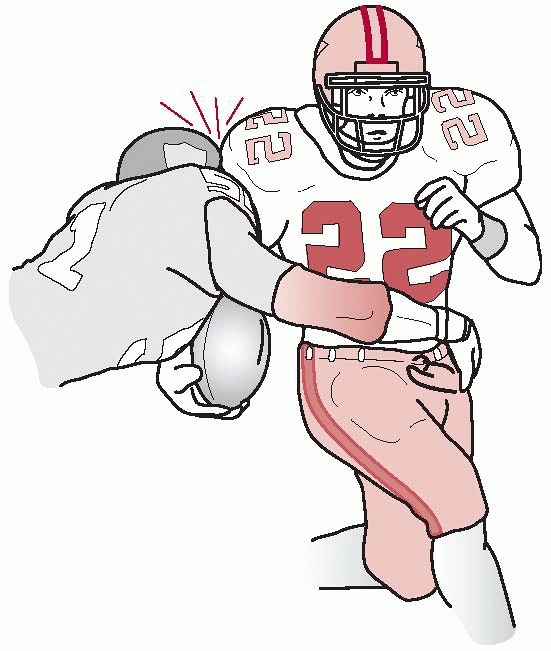 |
|
FIGURE 17-25 Blunt trauma from contact sports may result in fracture of the proximal humerus in children.
|
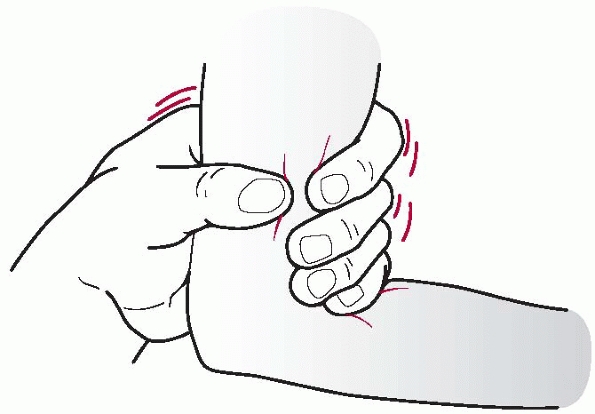 |
|
FIGURE 17-26
Although the exact mechanism of injury may vary in child abuse, fracture of the proximal humerus may result from twisting at the elbow or forearm. |
with a proximal humeral fracture: a traumatic injury with the immediate
development of moderate to severe global shoulder pain exacerbated by
motion of the arm. They often present with an obvious deformity, or
fullness, in the anterior shoulder region, with the overall contour of
the shoulder altered in comparison with the contralateral uninjured
shoulder. The arm is internally rotated against the abdomen and the
patient usually refuses to use the involved arm. Pain, swelling, and
ecchymosis are invariably present to some degree.
is due to the pull of the pectoralis major muscle on the distal
fragment. With posterior fracture dislocations, children demonstrate
limited and extremely painful external rotation. Some children with
fractures of the greater tuberosity have an unusual presentation of
luxatio erecta where the involved shoulder is positioned in extreme
abduction.174 This position reduces
the displacement across the fracture as the greater tuberosity is
pulled superiorly by the supraspinatus muscle. The elbow is typically
flexed in luxatio erecta, allowing the hand to be near or above the
head.174,300
Fractures of the lesser tuberosity affect the function of the inserting
subscapularis muscle; hence, abduction and external rotation of the
shoulder will be limited and painful.292,468,564
may be associated with concomitant dislocations of the glenohumeral
joint. The direction of the dislocation may be anterior, posterior, or
inferior.107,174,175,207,300,416,557 Neurologic injury to the brachial plexus can result from fractures and fracture-dislocations of the proximal humerus.19,144,174,557,561
The fracture can be displaced into the axilla and may have vascular
compromise requiring emergent reduction. Typically, these nerve
deficits are transient, and full function returns in 6 to 12 months.268,306
There may be an associated pain syndrome that lasts for months in these
rare situations of proximal humerus fracture associated with brachial
plexopathy. Fractures of the proximal humerus in children also can be
associated with other injuries, including rib fractures and
pneumothorax.484
and plain radiographs are of limited value in evaluation of proximal
humeral fractures in infants. On an AP radiograph, a change in the
positional relationship between the proximal humeral metaphysis and the
scapula and acromion often is visible. A comparison with the uninjured
contralateral shoulder may reveal this alteration more clearly. A
“vanishing epiphysis” sign also has been reported to describe
posteriorly displaced physeal fractures of the proximal humerus (Fig. 17-27).294,491
On an AP radiograph, the epiphysis appears to vanish when it is
displaced posteriorly. For complete evaluation of proximal humeral
fractures in newborns and infants, ultrasonographic studies can be
diagnostic and informative.71,164,251,553
MRI will reveal the injury pattern clearly but requires conscious
sedation or general anesthesia in infants for accurate analysis. In
addition to proximal humeral fractures, the differential diagnosis for
such “paralysis” in infants includes brachial plexus injury, septic
shoulder, and clavicular fractures.
Ideally, a true AP view of the shoulder and an axillary lateral view
provide the most information about the fracture. Because some lesser
tuberosity fractures may be visible only on an axillary lateral view,
this radiograph should be included whenever possible.252
Ideally, a properly positioned axillary view should position the normal
humeral head between the acromion and the coracoid. Often, however, an
axillary lateral view is difficult to obtain in a child with an acutely
fractured proximal humerus. In these instances, transthoracic axillary
view or scapular-Y views can be obtained. In obese patients,
transthoracic views are difficult to interpret. In addition, an apical
oblique view, an AP radiograph with the x-ray beam at 45 degrees of
caudal tilt, also can provide significant information about the
proximal humerus.513 In fact, some
authors report that most shoulder trauma can be evaluated with AP and
apical oblique radiographs and that a lateral view (axillary lateral or
scapular-Y view) can be obtained if a humeral fracture is suspected.61
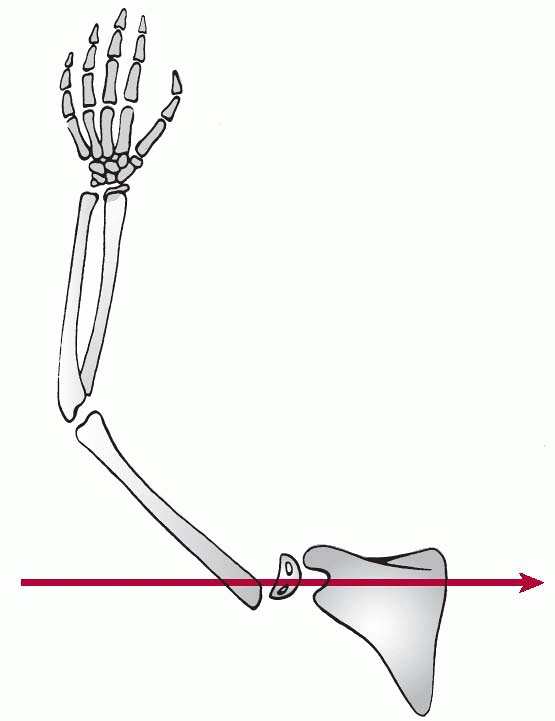 |
|
FIGURE 17-27 Vanishing epiphysis sign.
|
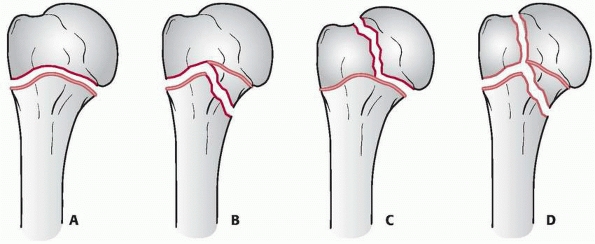 |
|
FIGURE 17-28 Physeal fractures of the proximal humerus. A. Salter-Harris type I. B. Salter-Harris type II. C. Salter-Harris type III. D. Salter-Harris type IV.
|
useful in evaluating proximal humeral fractures. CT may be especially
useful in characterizing posterior fracture-dislocations.207,545,564
If the child continues to report shoulder pain despite negative
radiographic and CT results, an occult fracture must be ruled out. For
this purpose, MRI can be diagnostic, due to its ability to identify the
intramedullary signal change of edema and the fracture plane.45,476,541
population are broadly categorized by their anatomic location. The
fractures may involve the physis, the metaphysis, the lesser
tuberosity, or the greater tuberosity. In addition, the degree of
fracture deformity (angulation and translation) plays an important role
in the overall treatment option. Other fracture characteristics that
must be evaluated include the presence or absence of open fractures,
concomitant glenohumeral dislocations, and fracture stability.
After 11 years of age, most fractures of the proximal humerus are
Salter-Harris type II injuries, with the fracture line exiting through
the metaphysis,79,124,164,435 and they occasionally are associated with an additional anterolateral bony fragment.79
Salter-Harris type III injuries with the fracture line exiting through
the epiphysis rarely occur in the proximal humerus of children124,435 and have been reported with and without concomitant glenohumeral dislocation.107,207,538,568,589
Salter-Harris type IV injuries involving both the metaphysis and the
epiphysis of the proximal humerus have not been reported in children.
This rather unexpected finding has been attributed to the rapid
metaphyseal growth that occurs during this age, which in turn results
in a relative structural weakness of the metaphysis.124
The anatomic location is described in relation to the major deforming
forces in the region, namely the insertions of the pectoralis major and
the deltoid muscles. Presence or absence of other fractures in the
ipsilateral upper extremity also must be documented, because segmental
fractures may require alternative treatments.270,357,425 Other isolated fractures of the proximal humerus may include the greater and the lesser tuberosities.174,292,300,468,577
in proximal humerus fractures is classified with respect to the shaft
diameter of the humerus.404 In grade
I injuries, there is up to 5 mm of displacement. In grade II and III
injuries, fractures are displaced by up to one third and two thirds of
the humeral shaft diameter, respectively. Displacement of greater than
two thirds of the shaft diameter is classified as a grade IV injury. In
addition to degree of displacement, fractures in this region typically
demonstrate concomitant angular deformities.
In addition to the proximal humerus, both the greater and lesser
tuberosities contain their own separate ossification centers. The
ossification center for the greater tuberosity appears at around 1 to 3
years of age, while the ossification center for the lesser tuberosity
takes form at 4 to 5 years of age.424,483
The two tuberosities typically coalesce between 5 and 7 years of age
and subsequently fuse with the humeral head at 7 to 13 years of age.424,483
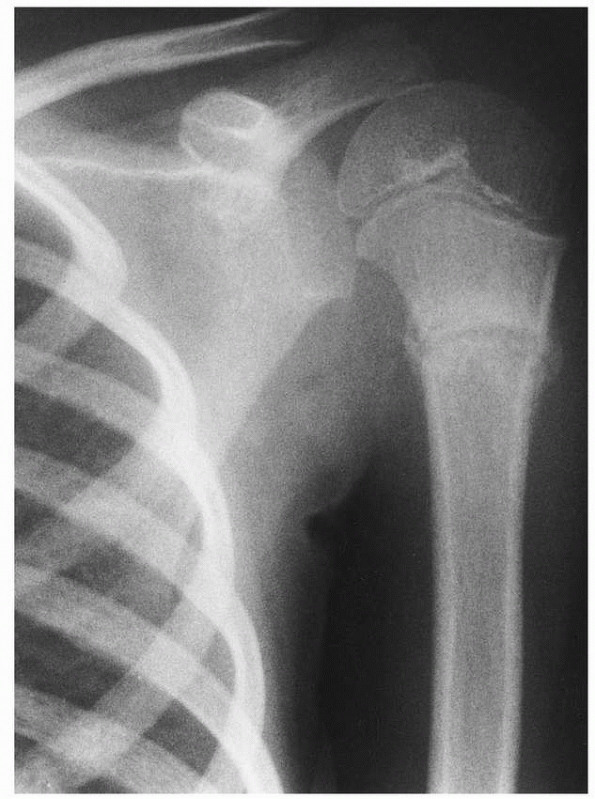 |
|
FIGURE 17-29 Healing undisplaced fracture of the proximal humerus in a 5-year-old child. Note the absence of a physeal injury.
|
active well into the teenage years and is ultimately responsible for
approximately 80% of the overall humeral growth.56,447,448,522
Interestingly, longitudinal growth at the proximal humeral physis
changes during development, such that it is responsible for only 75% of
humeral growth before age 2 but up to 90% of growth after age 11.56,447,448
For girls, this growth continues until around 14 years of age, with
subsequent fusion of the epiphysis to the shaft at 14 to 17 years of
age.56,118,522 For boys, growth continues until about age 16, when closure of the physis begins.56,447,448 For most boys, the proximal humeral physis is closed by about 18 years of age.118
The extracapsular location of the proximal humeral physis makes this
structure susceptible to injury. Physeal fractures are thought to occur
through the zone of hypertrophy and provisional calcification while
relatively sparing the cells in the resting and proliferative zones.481 Salter-Harris type I or II fractures in children have high remodeling potential and rarely result in growth arrest.38,124
most of the medial aspect of the epiphysis as well as the proximal
medial corner of the metaphysis (Fig. 17-30).
The glenohumeral joint capsule surrounds the articular surface such
that most of the medial epiphysis and the proximal medial corner of the
metaphysis are intra-articular (Fig. 17-31).
Conversely, a predominant proportion of the physis is extracapsular and
remains susceptible to injury. Most fractures of the pediatric proximal
humerus involve the physis.79,124,435
The periosteum is quite strong in the posteromedial aspect of the
proximal humerus, but the periosteum in the anterolateral aspect is
relatively weak, occasionally allowing the fractured fragment to
displace. The interposed periosteum can prevent reduction.124
number of different muscles that can influence the pattern of fracture
displacement. These muscles and their attachments form early during
development and are grossly similar to those of an adult shoulder by
the time of birth. The four muscles of the rotator cuff insert onto the
epiphysis. The subscapularis muscle inserts on the anterior aspect of
the epiphysis on the lesser tuberosity, whereas the teres minor, the
infraspinatus, and the supraspinatus muscles insert onto the superior
and posterior aspect of the epiphysis near the greater tuberosity (Fig. 17-32).
In addition to the rotator cuff muscles, the deltoid and pectoralis
major muscles can also affect fracture displacement. The deltoid muscle
attaches in the lateral aspect of the humeral shaft, whereas the
pectoralis major muscle attaches to the anteromedial aspect of the
metaphysis.
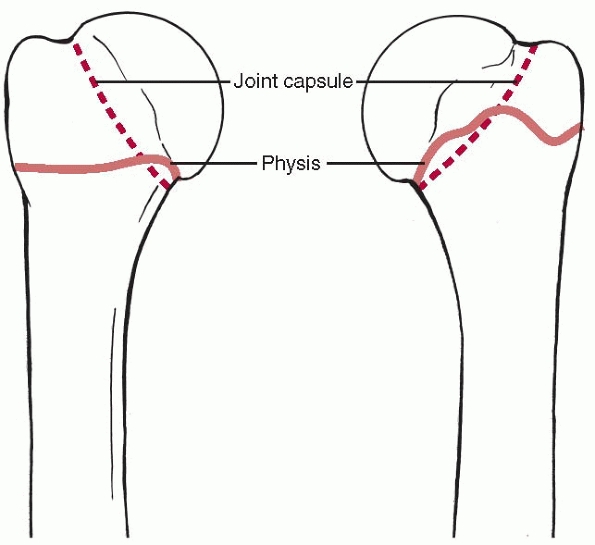 |
|
FIGURE 17-30 The anatomy of the proximal humerus.
|
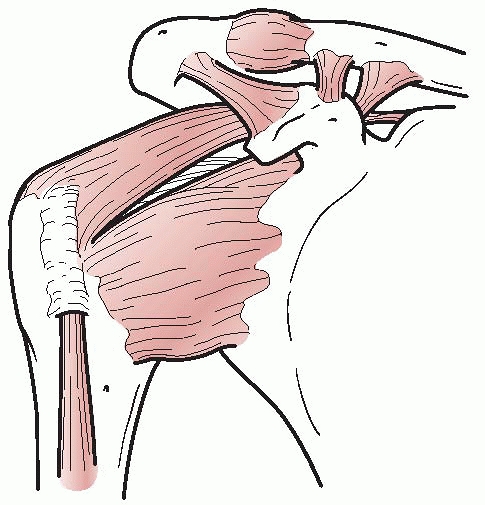 |
|
FIGURE 17-31 Glenohumeral joint capsule.
|
contribute to the degree and the overall pattern of fracture
displacement. With fractures of the physis (Salter-Harris types I, II,
and III) and metaphyseal fractures proximal to the insertion of the
pectoralis major muscle, the rotator cuff muscles displace the
epiphysis into abduction, flexion, and slight external rotation. The
distal fragment is displaced proximally by the deltoid muscle, whereas
the pectoralis major muscle displaces the fragment anteriorly and
medially. If the metaphyseal fracture occurs between the insertions of
the deltoid and the pectoralis major muscles, the proximal fragment is
adducted by the pull of the pectoralis major muscle, and the distal
fragment is pulled proximally and abducted by the deltoid muscle. If
the fracture occurs distal to the deltoid muscle insertion, the
proximal fragment is abducted by the deltoid muscle and displaced
anteriorly by the pectoralis major muscle. The distal fragment is
pulled proximally and medially by the biceps and the triceps muscles.123
the axillary artery. Distal to the pectoralis minor muscle, three
different arterial branches arise from the axillary artery before it
becomes the brachial artery to supply the upper extremity and hand. One
of these branches is the subscapular artery, which runs with the
subscapular nerve to supply the rotator cuff muscles. The remaining two
branches, the anterior and the posterior humeral circumflex arteries,
supply the proximal humerus. Most of the humeral head vascularity is
from the arcuate artery, which in turn is from the ascending branch of
the anterior humeral circumflex artery.189,312
The posterior humeral circumflex artery is a less dominant vascular
supplier of the proximal humerus because it supplies a small portion of
the greater tuberosity and posteroinferior portion of the humeral head (Fig. 17-33).189
fracture and fracture-dislocations of the proximal humerus.19,174,557
The axillary nerve is a branch of the posterior cord of the brachial
plexus. It traverses the anterior aspect of the subscapularis muscle
before passing inferior to the glenohumeral joint to the posterior
aspect of the proximal humerus (see Fig. 17-7).
The axillary nerve provides innervation to the deltoid and teres minor
muscles as well as cutaneous sensation over the lateral aspect of the
shoulder. Documentation of the normal motor and sensory function of
this nerve at the initial evaluation and prior to treatment is
essential.
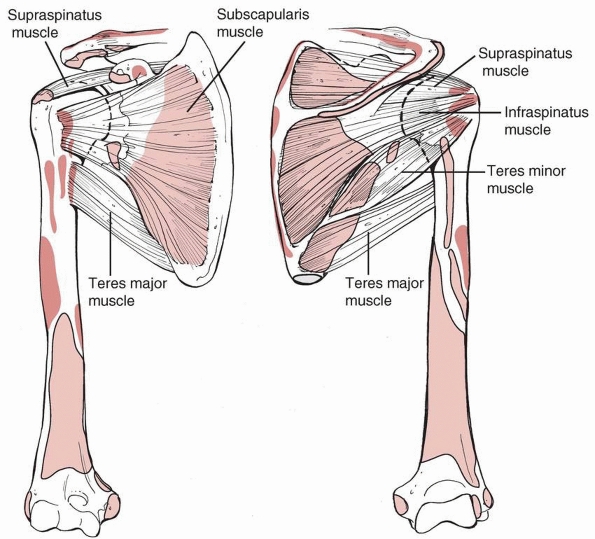 |
|
FIGURE 17-32 Origins and insertions of the cuff muscles in a child: subscapularis, teres minor, infraspinatus, and supraspinatus.
|
remodeling, fractures of the proximal humerus in children infrequently
require operative reduction and fixation (Table 17-5).
This is especially true for obstetric proximal humeral fractures in
infants. If needed, these fractures are amenable to gentle reduction
with minimal anesthesia or sedation. If desired, the adequacy of the
reduction can be evaluated via ultrasonography in infants, but due to
the incredible remodeling capability in this age group, this is not
routine. With or without anatomic reduction, the affected upper
extremity can be immobilized to the body by using a safety pin to
attach the shirt sleeve to the shirt or stockinette sling-and-swathe
that is age and size appropriate.484
Proximal humeral fractures in this age group heal quite rapidly,
typically within 1 to 3 weeks, and result in no residual functional or
cosmetic deficits.124,218,271,327,509,579
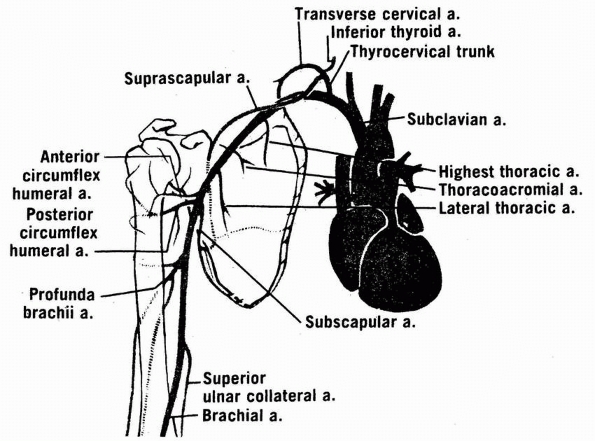 |
|
FIGURE 17-33 The arterial anatomy of the shoulder region.
|
fractures (Neer grades I and II) in older children and adolescents also
should be treated nonoperatively. Initial management of these fractures
involves sling-and-swathe immobilization (Fig. 17-34) followed by protected motion. Overall, nonoperative treatment provides excellent long-term results.82,124,174
children is significant but decreases with the increasing age of the
child; hence, the degree of acceptable displacement and angulation also
changes with the age of the child. Generally, relative greater
displacement and angulation can be accepted in younger children. For
fractures in children under the age of 11, good to excellent long-term
outcomes have been reported regardless of the fracture displacement.124,318,404,515
Various types of shoulder immobilization to maintain reduction have
been advocated and include sling-and-swathe, thoracobrachial bandage
(Velpeau), hanging arm cast, shoulder spica cast, salute position
shoulder spica cast, and “Statue of Liberty” cast.82,124,218,318,404
fracture reduction and sometimes with specialized immobilization.124,319,404,507
Multiple maneuvers exist for the reduction of pediatric proximal
humeral fractures. Most fractures can be reduced by applying
longitudinal traction to the arm while positioning it in abduction,
flexion, and external rotation. If this maneuver does not sufficiently
reduce the fracture, better reduction can be obtained by moderate
abduction, flexion to 90 degrees, and external rotation.404
Alternatively, the fracture can be reduced by direct manual
manipulation of the fragments while the arm is placed in marked
abduction (about 135 degrees), slight flexion (about 30 degrees), and
longitudinal traction.67,271,579
Despite significant efforts, however, some fractures cannot be
adequately reduced because of a barrier at the fracture site. Anatomic
structures that can prevent reduction of proximal humeral fractures
include the periosteum, the shoulder joint capsule, and the biceps
tendon.42,173,266,322,327,562
In these situations, open reduction through a small deltopectoral
incision is needed to remove the obstacles to reduction. Good
glenohumeral motion and function have been reported when severely
displaced (Neer III and IV) fractures were reduced to Neer grade I or
II displacement followed by immobilization or fixation.143
|
TABLE 17-5 Interventions for Proximal Humerus Fractures
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
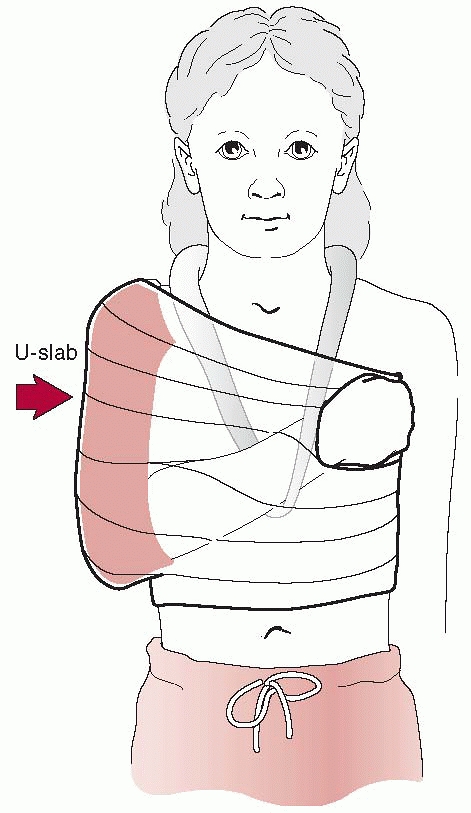 |
|
FIGURE 17-34 Sling-and-swathe for immobilization of proximal humeral fracture.
|
Salter-Harris type I and II fractures with greater than 50%
displacement, followed by immobilization with a thoracobrachial bandage
(Velpeau) or shoulder spica cast is usually sufficient (Fig. 17-35).124
An acceptable reduction of proximal humeral fractures in children over
11 years of age has been proposed by some to be less than 50%
displacement and 20 degrees of angulation.507
However, there have been no comparative outcome studies. Traditional
thinking has been that nonoperative treatment of pediatric proximal
humeral fractures has produced good to excellent results in all age
groups.124,318,404
Because of this, the reported indications for operative treatment of
pediatric proximal humeral fractures have been limited to include open
fractures, fractures associated with neurovascular injury, fractures
associated with multiple trauma, displaced intra-articular fractures
(i.e., Salter-Harris type III fractures), irreducible fractures, and
significantly displaced fractures in older adolescents.30,117,242,322,347,367,397,435,500,530,568
reported to support nonoperative treatment regimens for all patients
actually supports this method for children less than 11 years of age
and in fractures with no to minimal displacement.124,318,404
These classic references identified fractures in older children (11
years of age or older) and those with Neer grades III and IV
displacements at increased risk for less-than-optimal outcome.124,318,404
Minimal remodeling, specifically angular correction, occurs in the
older child and adolescent, which can lead to limitation of
glenohumeral motion (abduction) and pain.124,318
Case by case decisions regarding acceptable angulation and displacement
should be based on age since older patients have less capacity for
remodeling.42,143
Achieving acceptable fracture alignment can typically be accomplished
with closed manipulation of the fracture and only infrequently requires
an open reduction to remove obstructions. Immobilization of the reduced
fracture comes in two types: specialized casts or splints, or internal
fixation. Various types of external immobilization have been reported
to maintain reduction.82,124,218,318,404
Loss of reduction has been reported to be as high as 50% in one older series in which only external immobilization was used.404 Internal fixation with plates and screws, percutaneous cannulated screws, or more commonly smooth or threaded wires (Fig. 17-36)
can be used to stabilize the reduction, which obviates the need for
cumbersome immobilization such as a Velpeau bandage or spica cast.30
Intramedullary fixation from distal to proximal insertion is also a
viable option for stabilizing displaced proximal metaphyseal fractures (Fig. 17-37).95
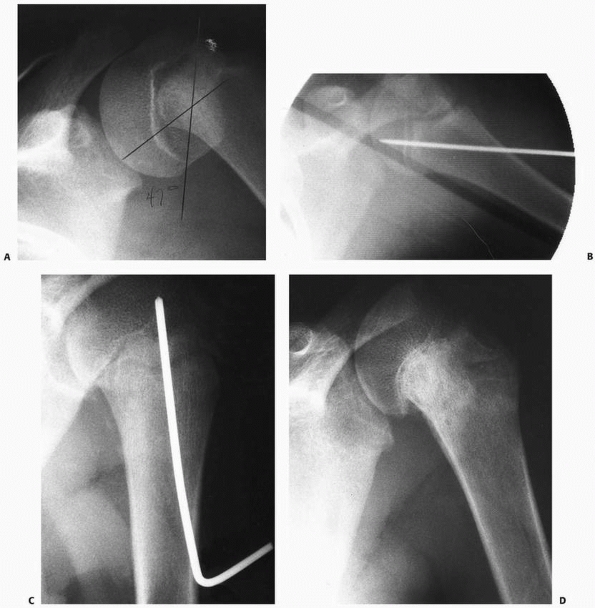 |
|
FIGURE 17-35 A. Salter-Harris type I fracture of proximal humerus. B. Intraoperative pinning through the metaphysis. C. Postoperative view. D. Healed physeal fracture.
|
epiphysis can be produced by chronic or repetitive trauma, such as
repetitive throwing, gymnastics with humeral weight bearing, or trauma
after localized radiation therapy.59,121,151,345,548,549
Because of the tremendous healing and remodeling potential in the
pediatric proximal humerus, these injuries can be successfully treated
with nonsurgical therapy.
displacement (Neer grades III and IV) and angulation in patients over
11 years of age are the fractures that typically undergo reduction to
improve fracture alignment. General anesthesia is typically necessary
for patient comfort and for adequate muscle relaxation due to the
difficulties that can be encountered
in
obtaining and maintaining an acceptable reduction. A radiolucent
operating table is optimal, but a regular operating room table can be
used if the patient’s torso is moved as far lateral as possible and
supported by a radiolucent arm table or an additional piece of
radiolucent Plexiglas. Adequate fluoroscopic imaging is essential for a
successful intervention, and the fluoroscope is set up in the AP
projection; it is not routinely moved during the procedure. A small
towel bump is placed under the medial border of the ipsilateral scapula
to elevate the shoulder away from the table to allow adequate
circumferential access to the shoulder. The sterile preparation should
be medial enough to allow the surgeon the option of performing a low
deltopectoral or axillary approach to the shoulder should closed
reduction be inadequate. Reduction is performed with longitudinal
traction on the injured limb while the arm is placed in abduction,
external rotation, and flexion to align the distal fragment with the
epiphysis. Increasing the abduction (up to 90 degrees) and flexion (up
to 90 degrees) of the distal fragment may be necessary to reduce the
fracture. For fractures requiring operative reduction, percutaneous
smooth or threaded wire stabilization is used routinely (see Fig. 17-36).
The starting point for percutaneously placed implants is at the lateral
cortex of the distal fragment, near the insertion of the deltoid
muscle, and aimed obliquely into the humeral epiphysis. By measuring
the articular cartilage height, entry can be two times the height to
safely avoid injury to the axillary nerve. Care must be taken not to
penetrate the humeral head into the joint or enter the axilla and
injure the neurovascular structures. At least two pins (0.062 or 5/64
inches), and preferentially three pins, are used and typically allow
adequate stabilization. The Kirschner wires may be cut beneath the
level of the skin or may be left through the skin and protected with
Jergens balls. The arm is placed into a shoulder immobilizer, with the
arm at the patient’s side, while the patient is under general
anesthesia. The implants can usually be removed as early as 4 weeks
after surgery after documenting healing on radiograph. Figure 17-38 from Dobbs et al.143 summarizes our approach.
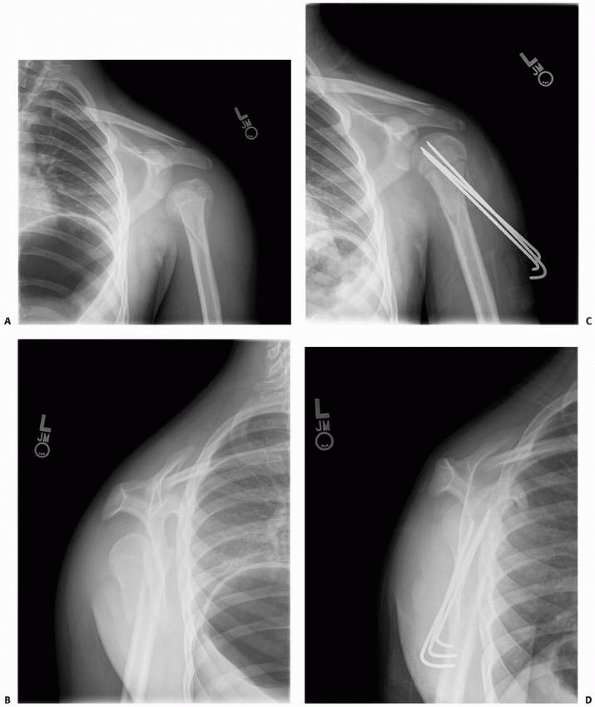 |
|
FIGURE 17-36 A.
AP radiograph of displaced fracture of the proximal humerus metaphysis with shortening with inferior subluxation of the humeral head with respect to the glenoid. B. Scapular Y-view. C,D. Postoperative films status after open reduction and fixation. The inferior subluxation has resolved. |
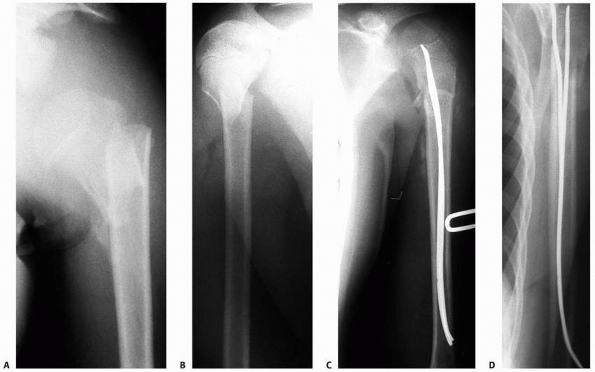 |
|
FIGURE 17-37 A. AP radiograph of displaced, shortened fracture of the proximal humerus. B. Axillary image of same. C. Intramedullary fixation using retrograde technique. Note the satisfactory restoration of alignment. D. Postoperative lateral view.
|
-
Most fractures of the proximal humeral
physis are managed nonoperatively. This includes nondisplaced and most
minimally to moderately displaced physeal injuries of the proximal
humerus, which are treated with a shoulder sling or immobilizer.
Range-of-motion exercises (pendulum) are initiated as soon as
tolerated, and the immobilization is discontinued when healing is
confirmed by radiographs and clinical examination. The great majority
of metaphyseal fractures are also treated nonoperatively, with only a
few requiring closed reduction. Because of the tremendous remodeling
potential of metaphyseal fractures in children, up to 1 cm of
displacement is acceptable if the fracture is in bayonet apposition. -
Due to the significant instability after
reduction of displaced fractures involving the humeral epiphysis or
metaphysis, we prefer to percutaneously pin the unstable fractures,
particularly those in children over 11 years of age (see Fig. 17-36).
The rationale behind reduction and percutaneous pinning of proximal
humeral physeal fractures is a more rapid return of normal active and
passive range of motion, improved patient comfort, and easier care of
the patient. There is a minimally increased, but acceptable, risk of
infection. In our opinion, this approach is more acceptable than
leaving the fracture unreduced and risking a decrease in shoulder range
of motion due to impingement with secondary shoulder pain. We prefer to
place the pin percutaneously through the metaphyseal fragment up into
the physis, similar conceptually to the pinning of a slipped capital
femoral epiphysis in the hip (see Fig.17-35). One drawback of Kirschner-wire fixation is that if the
P.654wires are left under the skin, another general anesthetic is needed to
remove the implants. In metaphyseal fractures, if the fracture is more
distal, it may not be technically feasible to place a percutaneously
placed Kirschner wire obliquely into the epiphysis. In this situation,
distal to proximal intramedullary fixation with flexible nails is an
effective method (see Fig.17-37).
Occasionally a fracture is irreducible, requiring open reduction.
Generally, the biceps is the offending structure. An anterior
deltopectoral exposure is used. -
Fracture-dislocations of the shoulder
require closed reduction of the glenohumeral joint dislocation with
appropriate anesthesia. After reduction of the glenohumeral
dislocation, radiographic confirmation of the reduction and
re-evaluation of the physeal or metaphyseal fracture is essential. If
the dislocation does not concentrically reduce or the fracture is in
unacceptable alignment, open reduction is generally done through a low
anterior or axillary approach to the proximal humerus. -
Displaced fractures of the lesser
tuberosity generally are treated with open reduction to restore the
subscapularis tendon and anterior capsule. Lag screws or suture anchors
are very useful in this region, particularly for injuries with small
bony fragments. Fractures of the greater tuberosity generally are
associated with acute dislocations of the shoulder and are typically
treated nonoperatively after closed reduction of the shoulder
dislocation. Rarely, after closed reduction of the shoulder
dislocation, the greater tuberosity fracture reduction is unacceptable,
and an open approach to repair the tuberosity fracture along with the
rotator cuff is required.
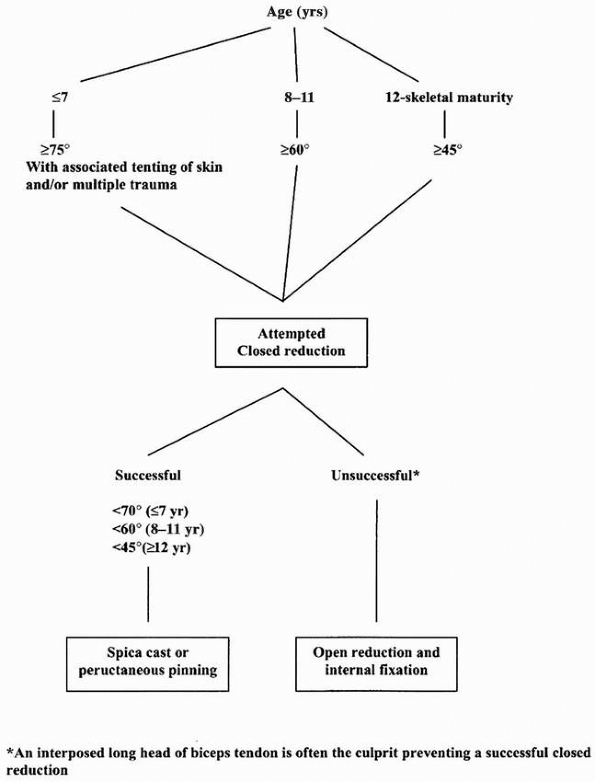 |
|
FIGURE 17-38 Algorithm for closed epiphyseal fractures of the proximal humerus. Assumed Neer Grade III or IV.
|
in a child who is asymptomatic or minimally symptomatic. This is
usually not a problem as the fracture can heal well and remodel minor
displacement with growth. In children with multiple
trauma,
the diagnosis can be delayed due to the need to focus on more life- or
limb-threatening problems and the absence of any dramatic limb
malalignment. Even after the diagnosis of proximal humeral fracture is
made, full evaluation and characterization of the fracture pattern can
remain incomplete because of inadequate radiographic studies. A high
index of suspicion, thorough physical examination, and insistence on
high-quality radiographs must all be present to ensure prompt diagnosis
and treatment of proximal humeral fractures.
Most nerve deficits can be diagnosed immediately because the clinical
signs are readily apparent. Often, the distal fracture fragment is
displaced into the axilla, with resulting adduction and valgus
malalignment and nerve compression or traction injury. There may be an
associated vascular compromise that requires emergent reduction of the
fracture to restore blood supply to the distal arm and hand.256 Rarely, however, nerve deficits from proximal humeral fractures can evolve slowly and delay the diagnosis.144 Typically, these nerve deficits are transient, and full function typically returns in 3 to 12 months.256,268,306
If the neurologic deficit persists longer than 3 to 6 months, further
evaluation with electromyography is warranted. If no evidence of nerve
recovery or regeneration is present, nerve exploration, repair, and
grafting can be considered.19,105 Salvage operations for permanent nerve deficits include proximal humeral osteotomy and muscle or tendon transfers.7,113,241,291,437
be associated with other injuries, including rib fractures and
pneumothorax.484 These fractures have been associated with disruptions and thrombosis of the axillary vessels as well in children575 and adults.344,499,533,602
Operative fixation of proximal humeral fractures with pins and wires
has been associated with hardware migration, which can be fatal.338,356 Therefore, serial radiographic monitoring of the hardware after shoulder operations is essential.
Children with humerus varus have a significant decrease in the humeral
neck-shaft angle and shortening of the upper extremity. Although
shoulder abduction may be moderately limited, most children with
humerus varus have only mild functional deficits and do not require
surgical correction of the deformity.154,317,352,546
If, however, active abduction and flexion are severely limited and
corrective growth is not possible, corrective osteotomy of the proximal
humerus can produce good results.193,517
of proximal humeral fractures. When the scarring is present in the
anterior shoulder region after an anterior deltopectoral incision, the
cosmetic deformity may be significant and psychologically damaging,
especially for girls.173,191 Therefore, many investigators have argued for the more cosmetically appealing axillary or anterior axillary incision.211,328
occurs more frequently in children treated with surgical intervention
than in those treated nonoperatively.38,124,478
This is likely due to the degree of damage to the physis at the time of
injury and not iatrogenically induced due to the surgical reduction.
The inequality is not significantly affected by the quality of initial
fracture reduction and may be more pronounced in older children (1 to 3
cm).38,404
Despite this inequality, however, these children rarely develop any
functional deficits to warrant surgical intervention. Full arrest of
physeal growth after traumatic proximal humeral fractures is extremely
uncommon.124 Although still quite rare, it does occur more frequently in children with pathologic fractures through unicameral bone cysts.239,388,413 If the functional or cosmetic deficit is significant, a limb-lengthening procedure may be of benefit for these children.492
Even after acute disruption of the vascular supply to the proximal
humeral epiphysis, subsequent remodeling and revascularization usually
occur in children and lead to excellent clinical results.568
Similarly, glenohumeral subluxation after proximal humeral fractures is
a rare complication in the pediatric population that typically results
in good clinical outcomes.594 These children are best treated with a short period of immobilization followed by early physical therapy and rehabilitation.484
displaced fractures and fractures in children 11 years old and younger;
the main area of controversy is in the treatment of displaced fractures
in the patient older than 11 years old. Two main areas of controversy
are the amount of acceptable displacement (angulation and translation)
and the optimal method of stabilization. The Neer classification is
currently the most widely accepted method for the radiographic
classification of proximal humeral fractures, but it has not been
validated as a guide for treatment.404
This system defines the fractures based on the bony translation at the
fracture site but does not integrate fracture angulation into the
schema. Multiple published reports document a high percentage of good
and excellent outcomes in Neer grade III and IV fractures.124,318,404,507
It is likely that fracture angulation, and not translation, is the more
important factor in the overall outcome of these fractures.
Unfortunately, due to the anatomy of the proximal humerus and
epiphysis, plain radiographic assessment of fracture angulation can be
very imprecise, especially in physeal fractures. This makes
preoperative and postoperative analysis of the fracture alignment
difficult, if not impossible. Further study into the role of fracture
angulation, and the ability to quantify angulation, is likely to shed
new light onto this topic by improving treatment algorithms and patient
outcomes. In addition, applying validated outcome assessments to
postfracture patients would help determine which fractures are
clinically acceptable.
reduced proximal humerus fracture has been a specialized cast or splint
designed to position the distal fracture fragment in alignment with the
proximal fragment. Improvements in intraoperative imaging and equipment
have permitted an evolution in pediatric fracture care to more
widespread use of percutaneously placed Kirschner wires, cannulated
screws, or intramedullary fixation. Hence, external immobilization is
rarely used. Both methods, external immobilization and internal
fixation, have their advantages and disadvantages in proximal humerus
fractures
(Table 17-6), but direct comparison of the techniques has not been performed to date.
|
TABLE 17-6 Treatment Pros and Cons: Proximal Humerus Fractures
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
breech presentations and with macrosomic infants. The most difficult
position is when the child’s arms have gone above the head with
maneuvers to bring the arm down after version and extraction.361
61% of all new fractures and 12% of all fractures in these unfortunate
children.348,505 Shaw et al.,505
in a retrospective review of 34 humeral shaft fractures in children
under 3 years of age, found that most occurred accidentally: only 6
were classified as caused by probable abuse. Child abuse must be part
of the differential diagnosis in children with humeral diaphyseal
fractures.426 The fractures may be spiral from a twisting injury or transverse from a direct blow.
transverse fractures from direct blows to the arm, frequently from
falls, pedestrian/vehicle accidents, gunshot wounds, and machinery.
Sports injuries are direct from contact sports or indirect from
throwing. Throwing injuries occur as a stress injury from overuse or
acutely during the throwing cycle from poor mechanics.9,76,186,200,206,235,343,321,527,548,576 A stress fracture also has been reported in an adolescent tennis player.454
Acute throwing fractures result from a sudden external rotation torque
developed on the distal humerus with concomitant proximal internal
rotation from the pectoralis major between the cocking and acceleration
phases141 as shoulder external
rotation and elbow flexion suddenly changes to shoulder internal
rotation and elbow extension. Humeral fractures may occur from arm
wrestling in older adolescents.39,351,391
Some humeral fractures are pathologic through benign lesions such as
simple bone cysts or through dysplastic bones from osteogenesis
imperfecta or fibrous dysplasia. Occasionally, pathologic fractures
occur from malignant tumors.
a diagnostic challenge. Establishing and evaluating a differential
diagnosis is the first concern. According to the history, was the
delivery normal? When was the problem noticed? Does the child move any
part of the extremity? Was there a history of maternal gestational
diabetes or of fetal macrosomia? Does the child nurse from each breast?
A broad, useful differential diagnosis consists of clavicle fracture,
proximal humeral physeal fracture, humeral shaft fracture, shoulder
dislocation, brachial plexus palsy, septic shoulder, osteomyelitis,
hemiplegia, stroke, and child abuse.
spontaneous motion of the upper extremity. Is there any hand or elbow
motion? Are there any areas of swelling, ecchymosis, or increased
warmth? Does the child move the ipsilateral lower extremity? The
clinician should carefully palpate each area of the upper extremity,
starting with the clavicle and comparing it carefully with the opposite
side for any change in soft tissue contour or tenderness. The upper
arms and shoulders should then be examined, looking for any tenderness
in the supraclavicular fossa. Lastly, the spine should be examined for
tenderness or swelling.
humeral fracture can simulate a brachial plexus palsy with
pseudoparalysis and an asymmetric Moro reflex. The fracture site is
tender and may have swelling or ecchymosis. The diagnosis is confirmed
by plain radiography.253,361
 |
|
FIGURE 17-39 A young patient with a humeral shaft fracture holding the arm tightly to his side.
|
usually evident with pain, swelling, and unwillingness to move the arm.
The arm is often supported by the opposite hand and is held tightly to
the body (Fig. 17-39). It is essential to
perform a complete neurologic and vascular examination of the extremity
before any treatment except emergency splinting.
localized tenderness but no deformity. In multiple-trauma victims,
careful evaluation should be made of the arm because the diagnosis can
be missed, especially if the patient is medically unstable.316 Humeral fractures should be sought in patients with massive upper extremity trauma.
fractures describes the location (proximal third, middle third, or
distal third, or the diaphyseal-metaphyseal junction), the pattern
(spiral, short oblique, or transverse), the direction of displacement,
and any tissue damage. Anatomically, the location is noted as proximal
to the pectoralis major insertion, between the pectoralis major and
deltoid insertions, below the deltoid insertion, or at the distal
metaphyseal-diaphyseal junction.123 Humeral shaft fractures may be segmental, with fractures of the shaft and neck,526,539 or associated with shoulder dislocation.17,34 If they are associated with fractures of the ipsilateral forearm, they result in the so-called floating elbow.69,523
but it is not as helpful in the evaluation and treatment of most
children’s humeral fractures, and like most classifications, it is
subject to some interobserver variability.182,275
shoulder, clavicle, humerus, and cervical spine. Often the shoulder,
clavicle, and humerus can be seen on a single AP view of both upper
extremities and the chest. Ultrasonography can be used to identify a
fracture of the clavicle or the proximal humeral epiphysis, a shoulder
dislocation, or a shoulder effusion by a skilled radiologist. A CT and
MRI scan may be necessary to evaluate a pathologic fracture. The
radiographic findings for each fracture are discussed in the particular
anatomic sections.
in most instances of humeral shaft fractures. In the occasional case
where the diagnosis is suspect but not readily apparent on these views,
oblique views may be useful.
usually quite apparent on AP and lateral radiographs of the humerus.
Radiographs should be taken in both the AP and lateral planes to obtain
two films perpendicular to each other to assess displacement. A true
lateral view of the distal humerus is noted by superimposition of the
posterior supracondylar ridges of the medial and lateral epicondyles.204,518
A supracondylar process of the humerus, when present, is best seen on
an oblique radiograph showing the anterior medial aspect of the distal
humerus.
marked abduction of the proximal fragment with external rotation by the
rotator cuff attachment.118,123
The distal fragment is pulled proximally by the deltoid and medially by
the pectoralis major. Displaced fractures between the pectoralis major
and deltoid insertions show adduction of the proximal fragment from the
pectoralis major and shortening by pull of the deltoid on the distal
fragment. Fractures below the deltoid insertion have abduction of the
long proximal fragment by the deltoid, but with shortening and medial
displacement of the distal fragment by the pull of the biceps and
triceps.123
Simple bone cysts are a common cause of fractures. Periostitis or
periosteal reaction of the humerus necessitates differentiating
osteomyelitis or Ewing sarcoma from a stress fracture; every effort
must be made to identify a cortical fissure using other imaging
techniques.17,34,69,523
invasion of the humerus at age 8 weeks. During the subsequent fetal
period, the humerus resembles the adult bone in both form and muscular
relationships.182,204,275,518
A bony collar is present very early with subsequent enchondral bone
formation. The secondary ossification centers at the ends are not
generally ossified radiographically until after birth.204,518
thinner, triangular shaft. Distally, this flattens and widens to form
the condylar region of the elbow. The deltoid inserts into a
protuberance midway down the shaft known as the deltoid tuberosity.
Distal to the tuberosity, the muscular spinal groove
wraps
posteriorly around the humerus. The groove gives origin to the
uppermost fibers of the brachialis. The periosteum of the humeral
diaphysis is thick and provides good remodeling potential.118,122
The main vascular foramen is at midshaft, but accessory foramina are
common—most enter the anterior surface usually below the main foramen,
but many are posterior.86,204,518
|
TABLE 17-7 Interventions for Fractures of the Humeral Shaft and Distal Humeral Diaphyseal Fractures
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
The profunda artery either accompanies the radial nerve or passes in a
second narrower groove. The nerve is protected from the humerus by a
layer of either the triceps or the brachialis until the lower margin of
the spiral groove near the lateral intermuscular septum.580
The ulnar nerve passes from anterior to posterior just distal to the
humeral midshaft. A well-formed arcade (arcade of Struthers) covers the
ulnar nerve as it passes distally.283
This arcade is always posterior to the medial intermuscular septum and
subsequently joins the medial intermuscular septum proximal to the
medial epicondyle. A few patients with a modified arcade have only
superficial fibers of the triceps medial head passing superficial to
the ulnar nerve and none deep to the nerve, making the nerve very close
to the bone and vulnerable during a fracture.283
|
TABLE 17-8 Treatment Pros and Cons: Fractures of the Humeral Shaft and Distal Humeral Diaphyseal Fractures
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
metaphyseal and diaphyseal regions of the humerus. The pectoralis major
muscle inserts laterally and distal to the bicipital groove along the
anterior aspect of the humerus. The latissimus dorsi and teres major
insert on the upper medial aspect of the humerus medial to the
bicipital groove. The deltoid originates from the clavicle, acromion,
and scapular spine to insert over a broad area of the deltoid
tuberosity. The coracobrachialis arises from the coracoid process and
inserts on the anterior medial aspect of the humerus at the junction of
the middle and lower thirds. The brachialis originates from the
anterior humerus about midway down the shaft. Knowledge of these
muscles and their orientation is essential to understand fracture
displacement and treatment.118,243
of birth injuries is an internal rotation deformity. Therefore, the
fracture can be stabilized by splinting the arm in extension. The
long-term, resultant angulation of the healed fracture is minimal due
to the child’s tremendous capacity of remodeling. Attempts at anatomic
reduction are not necessary.255
If the parents will be moving the child, the splinted arm can be bound
to the chest with a soft wrap. These fractures usually heal with some
varus and overlap that remodels. Children with arthrogryposis and
brachial plexus palsies are prone to internal rotation contractures of
the shoulder; these can be exacerbated if the birth fracture’s rotation
is not controlled.
 |
|
FIGURE 17-40 A. Fracture of the left humerus in a neonate that occurred during a difficult delivery. B. After 2 weeks of immobilization, clinical and radiographic union is evident, but with anterolateral angulation. C. At 2 months after injury, there is considerable remodeling. D,E. At 20 months, there is essentially complete remodeling of the fracture
|
does not require the precise mechanical alignment of the lower
extremity. The marked mobility of the shoulder also allows some axial
and rotational deviation without functional problems. Severe internal
rotation contractures can cause difficulties in some overhead
activities such as ball throwing and facial hygiene. Varus of 20 to 30
degrees is necessary before becoming clinically apparent (Fig. 17-41).123,295,453 Anterior bowing may be apparent with 20 degrees of angulation.295 Functional impairment does not occur with 15 degrees or less of internal rotation deformity.123 Even adolescents can correct up to 30 degrees spontaneously.123 Beaty42
gives guidelines based on the patient’s age: children under 5 years of
age tolerate 70 degrees angulation and total displacement, children 5
to 12 tolerate 40 to 70 degrees angulation, and children over 12
tolerate 40 degrees and 50% apposition. While not based on a study,
these numbers underscore the tremendous remodeling potential of the
humerus and the ability to functionally compensate for angulation.
Bayonet apposition is acceptable,171,324,422 with 1 to 2 cm of shortening well-tolerated (Fig. 17-42). Clinical appearance is more important than radiographic alignment.
 |
|
FIGURE 17-41 A,B. Radiographic appearance of a malunited humerus fracture showing 20 degrees of varus. C,D. The same patient with no clinical deformity or disability, despite her thin extremities.
|
This rarely is a functional problem. Nonoperative methods include a
sling-and-swathe, the U plaster, a hanging arm cast, a thoracobrachial
cast or dressing, a coaptation splint, functional bracing, and traction.
fractures is a sling-and-swathe. It is sufficient for patients with
minimally displaced greenstick and torus fractures.228,453 Although this treatment may yield good results in displaced fractures,520 it can be quite difficult to control anterior angulation,246 varus in an obese patient, and may be uncomfortable.
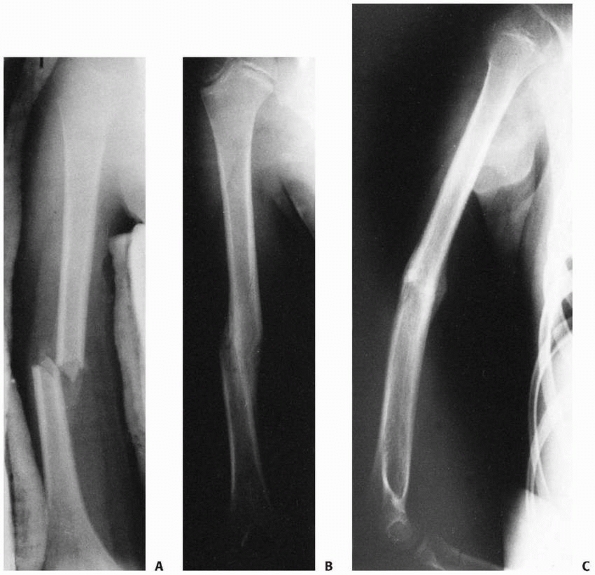 |
|
FIGURE 17-42 A. Humerus fracture allowed to heal in slight varus and bayonet apposition. B,C. The ultimate result with essentially normal alignment.
|
described a U plaster similar to the sugartong splint used on forearms.
Plaster of appropriate width for the upper arm is formed from over the
shoulder along the lateral aspect of the arm, underneath the olecranon,
and along the medial aspect of the arm to the axilla. Cotton webbing is
placed between the plaster and the skin, and the plaster is secured
using a wrap (Fig. 17-43). Results have been quite good,123 particularly in children.297 Holm244
suggested applying benzoin before the cotton webbing and using a
collar-and-cuff sling about the wrist. To prevent slippage, Shantharam502
suggested applying the splint from the base of the neck, over the
shoulder, and around to the axillary fold, with a strap securing the
proximal end to the chest. The U plaster may not control alignment
satisfactorily in more displaced fractures, which may require a
thoracobrachial cast62,244,453 or internal fixation if better alignment is necessary. Böhler62,64 actually abandoned the immediate use of the U plaster for a thoracobrachial cast because of problems with early swelling.
as a technique already in use, consists of a long-arm cast with a sling
around the neck tied to the cast along the forearm. The weight of the
cast and arm provides longitudinal traction. The position of the sling
is modified to correct anterior or posterior angulation and varus or
valgus. Rotation is difficult to control. Stewart and Hundley530 suggested not using it in children under age 12 because children cannot keep their arms in a
dependent position during sleep and often keep the arm supported rather
than hanging while awake. However, excellent results are reported in
patients under age 10.586
This is probably due to the marked remodeling and potential for good
results regardless of treatment in children. Possible complications of
the hanging cast include inferior shoulder subluxation,101 decreased external rotation,101 and shoulder stiffness,25 but these are rarely significant in children.
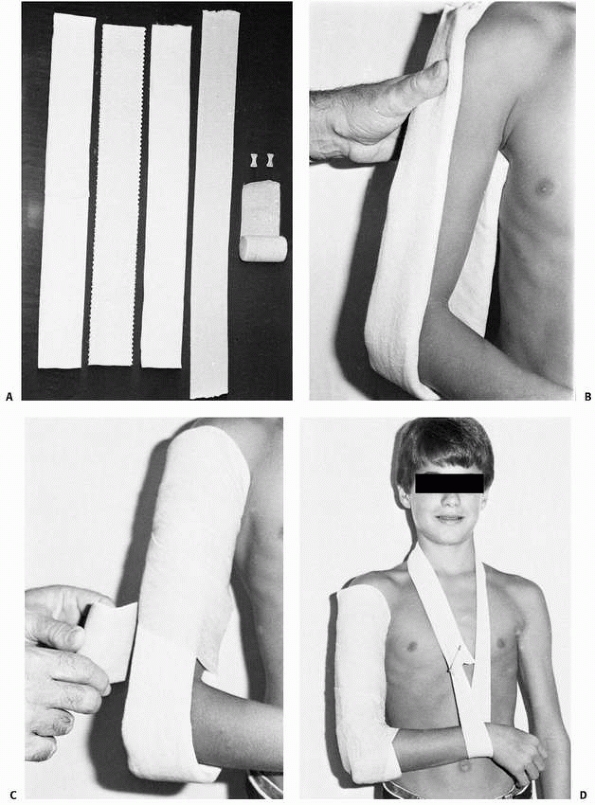 |
|
FIGURE 17-43 Coaptation splints with collar and cuff. A.
The material used for a sugartong arm splint is two pieces of cast padding rolled out to the length of the plaster-of-paris splint and applied to each side of the splint after it is wet. The splint is then brought into the tubular stockinette of the same width but 4 in longer than the splint. B. The plaster splint is applied to the arm from the axilla up to the tip of the acromion. C. As the plaster is setting, the splint is molded to the arm. An elastic bandage holds the splint in place. D. Stockinette is applied and attached to the wrist to form a collar-and-cuff sling. |
fractures uncontrollable in a hanging cast or U plaster may necessitate
extending the cast to the chest as a thoracobrachial cast or splint.62,64,244,246,453
Various types of thoracobrachial dressings are often described as a
Velpeau, but technically this is incorrect: Velpeau described a
thoracobrachial bandage with acute elbow flexion. If a thoracobrachial
cast or splint is used for a grossly unstable fracture, usually only a
few degrees of abduction is necessary.244 Distal diaphyseal fractures rarely require extension to the chest.
It may be difficult to use in children because size differences require
a customized brace for each patient or a large supply of braces;
however, modern thermoplastics can keep this economical (Fig. 17-44).43
A prefabricated brace is placed on the initial visit if possible or on
subsequent visits after placement of a U plaster or sling-and-swathe at
the initial evaluation.595 The
patient must be followed closely and the splint tightened as needed. It
should not be used in bedridden patients because of loss of gravity
support.29 Sarmiento487,488,489
noted difficulty in controlling anterior angulation and indicated that
patients should not lean on the elbow. The results in adults may be
functionally superior to those of the U plaster.503
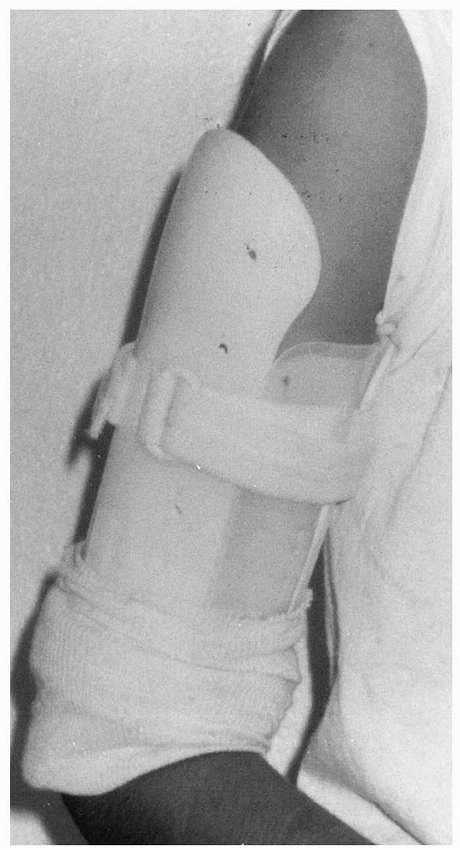 |
|
FIGURE 17-44
Light plastic functional braces are useful to maintain alignment and allow early restoration of motion, particularly in older children and adolescents. |
If olecranon skeletal traction is used, the AO method of an eye screw
in the olecranon is less likely to produce ulnar nerve irritation than
is a transolecranon pin.275,453 Excessive traction can lead to nonunion in adults236 and elbow dislocation in children.229 This technique is rarely utilized now due to economic and family considerations.
diaphyseal fractures: pinning, external fixation, intramedullary
rodding, screw fixation, and compression plating. Biomechanically,
interlocking rods are the stiffest in bending, and dynamic compression
plating is stiffest in torsion. Flexible intramedullary rods are not as
stiff as intact bone.233
and internal reduction can be performed through either a posterior
triceps-splitting approach, as advocated by the AO group,275,475
or through an anterior lateral approach between the brachialis and
brachioradialis with extension proximally between the deltoid and
pectoralis.44,166
The normal 4.5-mm dynamic compression plate does not provide adequate
stability for the adult humerus shaft. The broad 4.5-mm dynamic
compression plate is designed to allow compact screw placement without
causing excessive stress on the humerus in adults.275
At least six cortices of screw fixation proximal and distal to the
fracture site are needed. In children, smaller plates can be used, such
as small pelvic reconstruction plates and double stacked semitubular
plates depending on the size of the child. With either the
anterolateral or posterior approach, the lateral intermuscular septum
should be split in the distal third to release the tether of the radial
nerve. Interfragmentary lag screws should be used when possible. The
plate should be slipped underneath the radial nerve and vessels and
some muscle placed between the plate and the nerve. Multiple screws in
oblique fractures without a compression plate are unsatisfactory in
adults475 but may be sufficient in children. Extensively comminuted fractures may require bone graft.
rods are available. Currently, there are no indications for reamed
intramedullary nailing in children because of potential proximal
physeal damage and the small diaphyseal diameter. However, they may be
used in skeletally mature adolescents if the canal has sufficient
diameter.457 Reamed nailing has been reported in patients as young as 16.115,149 The results are generally good,115,141,219,262,299,369,450,465,554,556,596 with a low risk of nonunion and infection.24
flexible titanium rods, have been used most extensively in adults with
multitrauma. Nails or rods can be inserted via a posterior
triceps-splitting approach through a hole just above the olecranon
fossa. This can be useful for rapid management of fractures, including
open fractures in patients with multiple trauma.76,93,110,133,220
Rods should not be inserted through the greater tuberosity in children
(except under extenuating circumstances) because of risk of injury to
the proximal humeral physis and the potential for shoulder impingement.359,467,529 Inserting these relatively large rods through the epicondyles results in a high incidence of nail back-out.220
fluoroscopy is used with a tourniquet placed on the upper arm. A hole
is made just proximal to the olecranon fossa using a triceps-splitting
approach. Smooth, blunt-tipped Steinmann pins are placed up the canal
of the humerus, progressively filling the canal with smaller and
smaller pins as needed (Fig. 17-45). Results are generally good,92,137,147,234,383,433,599
although pin back-out can be a problem and care must be taken not to
distract the fracture site. The rods should be bent 90 degrees at the
cortical window.433 This technique may be useful for segmental and pathologic fractures.342
The tips of the rods should be blunt and slightly bent. These are
placed through the lateral epicondyle or through both the medial and
lateral epicondyles. A hole is made in the epicondyle, and a
blunt-tipped Steinmann pin is tapped up the diaphysis using a mallet or
passed by hand, with a drill chuck holding the pin. The bend on the tip
of the rods facilitates crossing the fracture site and manipulating the
fracture reduction. A splint is necessary postoperatively. Alignment
need be only within the tolerances for a closed reduction (Fig. 17-46). The use of flexible intramedullary nailing has also been described with good success in children and adolescents.319
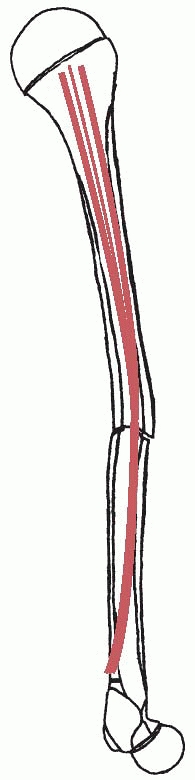 |
|
FIGURE 17-45
The Hackethal technique involves multiple smooth pins placed up the humeral shaft through a cortical window just above the olecranon fossa. The pins are placed until the canal is filled. |
external fixation techniques are occasionally useful for humeral shaft
fractures.20,129,281,289
External fixators are primarily useful for severe open fractures or as
an alternative to internal fixation. In patients with open fractures,
immediate external fixation with subsequent bone grafting yields good
results.449,514 External fixation can be combined with internal fixation for immediate stability112
and early rehabilitation. Severe open fractures with bone loss can be
treated with primary shortening followed by callus distraction479
to provide early soft tissue coverage and subsequent restoration of
humeral length. Care must be taken during pin placement to avoid radial
nerve injury. If screws are used, limited open screw placement can
prevent this injury.449 Ring fixators may be useful for reconstructing the injured humerus.78,89,90,102,259,260,508,510
Potential operative indications include open fractures, multiple
trauma, bilateral injuries, arterial injuries, compartment syndromes,
pathologic fractures, significant nerve injuries, inadequate closed
reduction, and ipsilateral upper extremity injuries or paralysis.
nonoperatively, except those with severe soft tissue injury. If
fracture reduction cannot obtain less than 30 degrees varus and 20
degrees anterior angulation in older children and adolescents—or more
importantly, if the arm appears deformed—alternatives such as internal
fixation, intramedullary rodding, external fixation, or a
thoracobrachial cast should be considered. Inadequate closed reduction
is most common in obese patients and in thin women with large breasts.475 However, obesity tends to hide the deformity of the fracture, and large breasts are seldom encountered in thin children.
1 wounds can still be managed using coaptation splints or other closed
methods. Unstable open fractures should be stabilized with internal or
external fixation to protect soft tissues.98,133,331,358,475,560
This is particularly true in patients with chest injuries, where
thoracobrachial immobilization would compromise pulmonary care.133,347,358 Excellent results have been reported with external fixation98,281,449,514; retrograde rodding using titanium, Ender, or Rush rods76; and internal fixation.44
In older adolescents, more rigid locked or unlocked intramedullary
rodding can be used for patients requiring their upper extremities for
mobility.166 However, this luxury does not exist for younger children.
Temporary vascular shunting before internal fixation allows the
orthopaedist and the vascular surgeon to work under optimal conditions.97
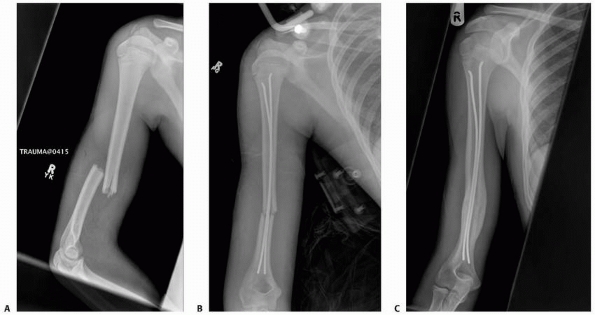 |
|
FIGURE 17-46 A. Displaced fracture difficult to align with nonoperative methods. B. Surgical treatment with tow intramedullary rods. Alignment need be only within the same tolerances as closed reduction. C. Healed fracture.
|
osteogenesis imperfecta, and simple bone cysts, can be treated
nonoperatively. Simple bone cysts are discussed in the section on
proximal humerus fractures. A report of a 6-year-old with progressive
ossifying fibrodysplasia suggests that internal fixation may prevent
stiffness after fractures in this condition.405 In fractures secondary to malignancy, intramedullary rodding is necessary if extensive cortical loss causes instability.109,149,334,529,552 Spontaneous fracture in a severely brain-injured or unresponsive cerebral palsy patient is best treated nonoperatively.557
proximal or distal humerus and of the forearm, can be difficult to
control. In adults with a floating elbow, internal fixation or elastic
nailing of the humeral fracture provides optimal results.76,315,463 This is also true for supracondylar humeral fractures in children but is not documented in diaphyseal fractures.69,523 The floating elbow is often associated with other organ system injuries; nerve injury occurs in up to 50% of these patients.438
Functional bracing is precluded in these patients because the muscles
do not function and sensation is altered. Because of the excellent
healing potential in children, they may be treated nonoperatively if
satisfactory alignment can be maintained. Older adolescents should be
treated like adults.
Primary radial nerve palsies occur at the time of the fracture;
secondary radial nerve palsies occur after manipulation of the
fracture. Many clinicians recommend exploration of secondary radial
nerve palsies42,123,181,431,444,506,555,571 and a few do for primary nerve injuries.10,119,181,245,307,311,397,431,444,464,542 The incidence of concomitant radial nerve palsy with a humeral shaft fracture ranges from 2.4% to 20.6%24,52,181,358,370,441,464,501,563 and has been reported in 4.4% of children’s humeral shaft fractures.358 Most occur with middle and distal humeral shaft fractures, but they may occur with more proximal fractures as well.370 In explored primary radial nerve palsies, the incidence of complete nerve laceration is small.204,358,431,501,518,563
Commonly, the nerve is tented over the bone, trapped in the fracture
site, or contused. The natural history is excellent, with recovery
ranging from 78% to 100%.12,52,65,66,140,181,195,431,441,444,482,501,563 Therefore, most clinicians recommend observation rather than early exploration.52,140,181,195,431,441,444,482,501,563
This is especially true in children where the periosteum can be
protective against entrapment and the nerves can recovery quickly from
contusion and traction ischemia. Open fractures resulting in severe
soft tissue injury requiring débridement should have the radial nerve
identified. If lacerated, exploration and tagging for later repair,535 or preferably, primary repair is performed.167
More severe open fractures should be stabilized using either
intramedullary rodding, internal or external fixation to provide
stability for soft tissue healing, or radial nerve recovery. Early
repair of the nerve provides the best anatomic results.49 Bostman et al.66
recommended exploration and internal fixation in patients with bayonet
apposition because the abundant callus may endanger nerve recovery. The
recommended waiting time before radial nerve exploration ranges from 8
weeks to 6 months.10,12,123,140,246,370,441,444,453,506,571 Nerve grafting up to 18 months after the injury can provide good function.49,165 Ogawa419 reported a complete radial nerve division which was repaired with a sural nerve graft resulting in full function. Seddon495
suggested a physiologic time of allowing 1 mm per day after the 1 to 2
months of Wallerian degeneration and nerve growth through the neuroma.
Nerves grow 1 to 3 mm per day,495,496,534 and this rate has been used clinically with good success.199,535
In children, healing is usually faster and signs of spontaneous
recovery are usually present by 3 months. This is noted by an advancing
Tinel sign, radial wrist extension recovery followed by central wrist
extension, digital metacarpophalangeal extension, and then thumb
retropulsion and ipsilateral extension.
 |
|
FIGURE 17-47 Radial nerve palsy secondary to a humeral shaft fracture from a low-velocity gunshot wound.
|
compelled to explore the nerve because he or she “caused” the radial
nerve injury. However, natural history studies of observed secondary
radial nerve palsies show recovery rates of 80% to 100% with
nonoperative treatment.66,181 Secondary palsies occurring after manipulation may be observed.52,140,310,432,501
If the palsy occurs after a considerable time, the nerve is probably
encased in callus and further investigation, including exploration, is
warranted.148,531 Late presentation may result in an osseous foramen containing the nerve and requiring decompression.148 Again, in children, there should be signs of recovery by 3 months, and no later than 6 months, if natural history is chosen.
recovery. To prevent an internal rotation contracture, we place the arm
in either a U plaster or a plaster coaptation splint with the palm
facing anteriorly. A soft wrap holds the arm to the body so the child
can be carried. The splint can be removed in 2 weeks. On healing, the
radiographic angulation can be quite worrisome to the parents. We like
to show them radiographs of other infants with marked remodeling, and
we keep photographs handy for this purpose.
treated nonoperatively. Torus fractures are treated with a commercial
shoulder immobilizer or a sling. Greenstick fractures and displaced
fractures in younger children are treated with a U plaster or a plaster
coaptation splint; these are usually applied in the emergency
department with mild sedation. We prefer general anesthesia if more
manipulation is needed. A careful neurologic and vascular evaluation is
performed before and after manipulation. We place a U plaster with
Webril (Covidien, Mansfield, MA) padding extending from over the
deltoid, around the olecranon, and up to the axillary fold, and secure
it with a gauze wrap followed by an elastic bandage. We have had
similar results applying plaster coaptation splints on the medial and
lateral aspects of the arm and rewrapping frequently with an elastic
wrap. We carefully pad all bony prominences and neurovascular
prominences, especially the ulnar nerve. The patient is placed in a
collar-and-cuff sling for forearm support. If alignment is
unsatisfactory, a new splint is reapplied and molded.
we prefer smooth intramedullary rodding using two 2-mm rods placed
retrograde through the epicondyles. For unstable fractures with
extensive comminution, we prefer to use a unilateral external fixator,
with small incisions made during screw placement to avoid the radial
nerve. Open fractures are treated in a similar manner. Significant bone
loss can be treated using bone transport techniques. We avoid plate
fixation because it creates a stress riser, particularly in growing
children. If a fracture occurs distal or proximal to the plate, it must
be re-explored for plate removal, necessitating re-exploration of the
radial nerve and potential nerve damage. We observe both primary and
early secondary radial nerve palsies, exploring them only after 3
months of observation, failure of anticipated recovery of at least 1 mm
per day, and if electromyography shows no return.
followed weekly for the first few weeks to ensure that alignment is
maintained. The coaptation splint or long-arm cast should be replaced
as needed. Patients with radial nerve palsies must be instructed in
finger motion to keep the fingers supple and prevent contractures.
Noncompliance requires formal hand therapy or a radial nerve outrigger.
Long-term stiffness of the shoulder and elbow is uncommon in children,
but pendulum exercises are started at 3 to 4 weeks in older children
and adolescents. Some form of immobilization is generally continued for
6 weeks. Patients should not return to contact sports until there is
adequate healing, and the family should be cautioned that refracture
may occur during the first 6 months after injury.
shaft fractures in children is excellent. Internal rotation deformity
is usually minimal, and the outlook for radial nerve palsies is good.
Loss of shoulder motion may occur but is more common in older patients.453
A few people have an abnormal arcade of Struthers in which only
superficial fibers of the triceps medial head pass superficial to the
ulnar nerve and none pass deep to the nerve, making the nerve extremely
close to the bone and vulnerable to an abduction extension mechanism of
fracture, which opens the anterior medial aspect of the humerus.283
In about 10% of the population, the median nerve crosses posterior to
the brachial artery rather than anterior, placing it closer to the
humerus. Median nerve palsy has been reported from an apex anterior
middiaphyseal fracture.360 After an
easy fracture reduction, the median nerve was caught in the fracture
between the coracobrachialis and brachialis muscles, where the nerve
crossed anteriorly. Anterior interosseous nerve palsies have not been
reported in fractures above the supracondylar region.
as strong as it is in the lower arm, making compartment syndrome less
common. Mubarak and Carroll395 reported a dorsal forearm compartment syndrome in a 9-year-old boy with a humerus shaft fracture. Gupta and Sharma212
described an adult with a triceps compartment syndrome from a middle
third minimally displaced fracture; this fracture did not disrupt the
intercompartmental boundaries.
undergoing surgery. They have not been reported in closed fractures of
the humerus in children, but have been reported in closed fractures
elsewhere.85,570
noted that the deformity visible on the AP and lateral radiographs is
generally not the maximum deformity, which is the vector sum of the two
deformities. This can be appreciated by obtaining a radiograph
perpendicular to the plane of the deformity, similar to the Stagnara
view for scoliosis.
in older adolescents, there are few reports of humeral nonunion in
children: one in a child with progeria at age 4,172 four in children with osteogenesis imperfecta,180 and three from severe trauma.97 In adults, numerous treatments have been used successfully. These include reamed nails100 and modified flexible nails.213,446
However, the best results appear to be from ASIF techniques with the
broad dynamic compression plate and autogenous bone grafting.33,91,161,226,245,397,592
Currently, treatment in children and adolescents must be extrapolated
from adult treatment. In general, the atrophic ends of the nonunion are
taken back to bleeding surfaces and apposed, a compression plate is
applied with fixation of at least six cortical screws proximally and
distally, and bone grafting is performed.226 The Ilizarov technique also reportedly produces good results.17,34,78,89,259,260,508 Electrical stimulation also has been used with success.111,156,158,497,498,532
Children with dysplastic bone, such as those with osteogenesis
imperfecta, are best treated with intramedullary rodding and bone
grafting.180
after humeral fracture occurs in about 81% of patients but is generally
minimal (<1 cm).228 Some generalized stimulus to the extremity is evident, with overgrowth of the carpals as well.490
Lengthening is rarely indicated as the humerus can tolerate 5 to 8 cm
of shortening without functional loss due to shoulder and truncal
compensation. However, lengthening has been performed in patients with
limb-length discrepancy of 3 cm or more at maturity.120,434 Unilateral or ring fixators may be used with Ilizarov’s principles.89,90
or metaphyseal-diaphyseal junction fractures. These injures are much
less common than supracondylar humeral fractures occurring in about 3%
of displaced fractures of the distal humerus.162
Fractures in this region should not be confused with supracondylar
humeral fractures. The distal diaphysis is more triangular and the
periosteum is thinner than in the supracondylar region,118,122
making these fractures generally less stable than supracondylar
fractures. The cortical bone also heals more slowly than metaphyseal
bone, requiring longer immobilization. The mobile wad, anconeus, and
flexor pronator mass originate off the epicondyles; the biceps,
brachialis, and triceps all insert distally. Therefore, forearm
position greatly affects the fracture position. Because the brachial
artery is tethered by the lacertus fibrosus, injury to the artery is
more likely than with more proximal fractures.
may be caused by transverse or longitudinal loading, torsion, or
moments generated by the forearm about the elbow. They
are
caused by direct blows and twisting more often than ulnar leverage in
the olecranon fossa. The diagnosis, made on plain radiographs, must be
differentiated from a supracondylar humerus fracture.
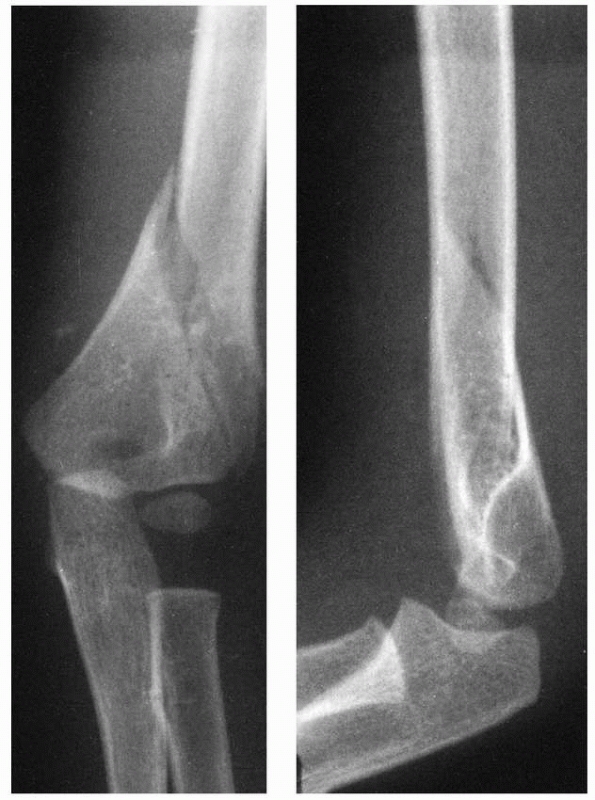 |
|
FIGURE 17-48
Distal humeral diaphyseal fracture extending to the epicondyles. This fracture was treated by casting with the forearm in pronation. |
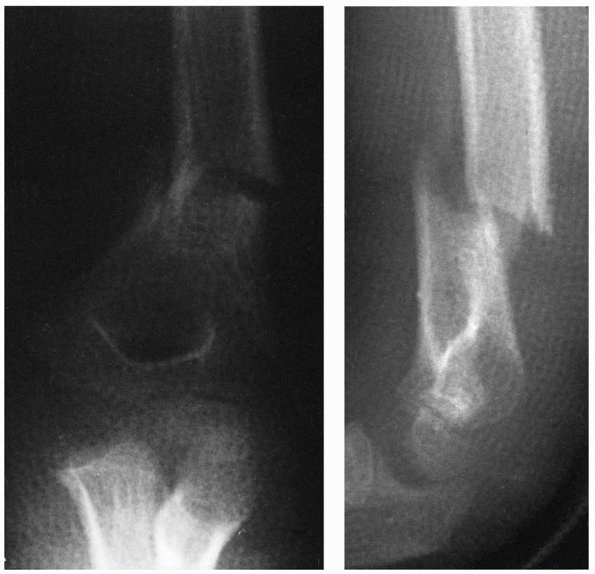 |
|
FIGURE 17-49 X-rays showing the tendency of distal humeral diaphyseal fractures toward varus malunion. The fracture required remanipulation.
|
spiral, or short oblique. Occasionally, an oblique or spiral fracture
extends distally toward or beyond the epicondyles (Fig. 17-48).
The description must include the direction of displacement, the
neurologic and vascular status, and the degree of comminution. Medial
column comminution predisposes to varus malunion.
flexion of the elbow, with potential vascular compromise, is not
required to maintain reduction. These fractures tend toward varus
malunion (Fig. 17-49),75
which may be cosmetically unacceptable, particularly in more distal
fractures. With 20% or less of humeral growth occurring distally,56,447,448
significant remodeling may not occur. Because of the proximity to the
epicondyles with their muscular origins, supination and pronation
affect fracture reduction. If one cortex is open, then the muscles
originating on that side should be tightened to reduce the fracture.16 Because of the varus tendency, this is usually by pronation.63,64,516 However, this is best checked radiographically (Figs. 17-50 and 17-51).
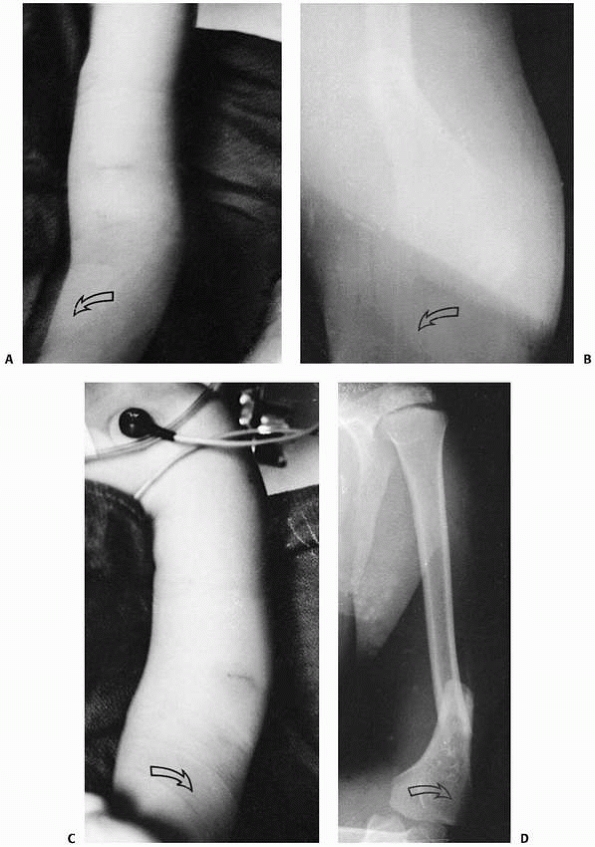 |
|
FIGURE 17-50 Influence of forearm rotation. Pronation (A,B) of the forearm produces a valgus angulation at the fracture site (arrows). Supination (C,D) creates a varus angulation (arrows).
|
 |
|
FIGURE 17-51 The same patient shown in Figure 17-50. A. The humeral coaptation splint is molded (arrows) with the forearm in neutral. B. A second forearm coaptation splint is added, and the extremity is suspended with a loop. C. Radiographs show satisfactory linear alignment. D,E. The fracture healed in bayonet apposition but with satisfactory alignment.
|
and possibly open reduction. Closed reduction and percutaneous pinning
should be performed in a similar fashion to supracondylar humerus
fractures. However, because the fracture is more proximal, it is
difficult to get the pins into the diaphysis without crossing them at
the fracture site (Fig. 17-52). The difficulty
in stabilizing these fractures has been demonstrated by a longer
operative time when compared to standard supracondylar fractures.162
In addition, transverse fractures in this region have a high incidence
of loss of fixation, reoperation, pin migration, cubitus varus
deformity, and prolonged loss of motion.162
Attempts can be made to pass the wires in intramedullary fashion up the
lateral or medial and lateral columns separately to provide stability (Fig. 17-53).453
This can be done by drilling the wires, but it is easier to create a
starting site at the epicondyles and pass blunt-tipped wires up the
columns. Holding the wires with a drill chuck helps, too. Because of
the bony anatomy and the ulnar nerve, lateral wires are easier to
place, particularly in younger children (Fig. 17-54).
However, unilateral intramedullary fixation may lead to bowing.
Alternatively, the fracture can be managed with skeletal traction until
callus forms; then either a U plaster splint or a long-arm cast can be
applied (Fig. 17-55). Brug et al.75
reported the best results with flexible intramedullary rodding. If
internal fixation with a plate is chosen, both columns need to be
stabilized.
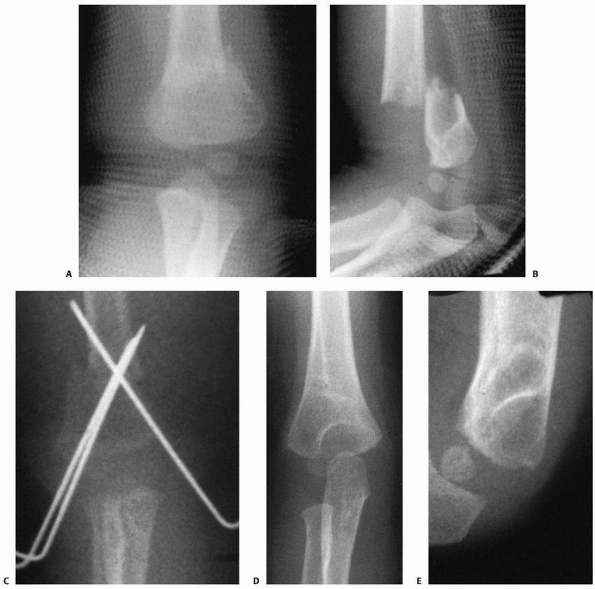 |
|
FIGURE 17-52 A,B. Distal humeral diaphyseal fracture in an 18-month-old treated with closed reduction and percutaneous pinning. C. The pins cross at the fracture site with decreased stability and some loss of position. D,E. The ultimate outcome was good.
|
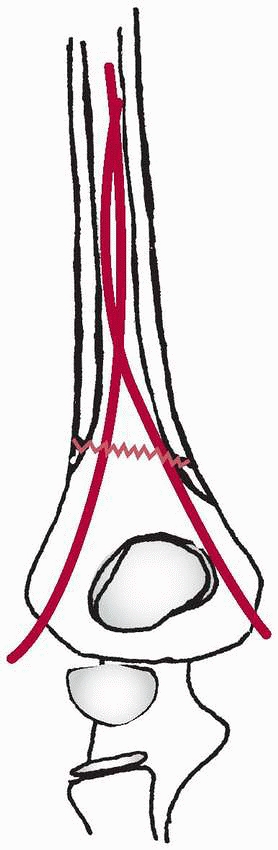 |
|
FIGURE 17-53
Ideally, pin fixation for distal humeral diaphyseal-metaphyseal junction fractures involves pins placed in intramedullary fashion up the medial and lateral columns. |
 |
|
FIGURE 17-54 Segmental distal humeral diaphyseal and supracondylar fracture in a 4-year-old boy. A,B. Both fractures could not be controlled by closed means. (continues)
|
fractures, we prefer closed treatment. Nondisplaced fractures are
treated with a long-arm cast split to allow for swelling. A double
sugartong splint is used if swelling is severe. We reduce displaced
fractures under general anesthesia. Because supination and pronation of
the forearm can affect the position, we use the image intensifier to
determine the position best for maintaining the reduction; this is
usually pronation. If the reduction obtained is unstable and cannot be
held with a cast, we do not hesitate to treat it by percutaneous
pinning with small Steinmann pins placed through the medial and lateral
epicondyles and up their respective columns, keeping the pins as
divergent as possible at the fracture site or with lateral column pins.
It is helpful to introduce them through the epicondyle and then tap
rather than drill them up the column to prevent convergence at the
fracture site. The pins are removed once good callus forms.
incidence of this process ranges from 0.1% to 2.7%, with the lower percentages in Blacks and the higher percentages in whites.32,354,407 The process extends obliquely downward and may be connected with the medial epicondyle by a tough fibrous band.32,88,281,354,407
Frequently, the foramen formed between the fibrous band and the humerus
is traversed by the median nerve and the brachial artery. They may be
entrapped by the fibrous band or the fracture. Anomalous attachments of
the coracobrachialis and the pronator teres may occur on the process (Fig. 17-56).215,299
 |
|
FIGURE 17-54 (continued) C,D. A lateral column pin acting as an internal splint is technically easier than medial column pins.
|
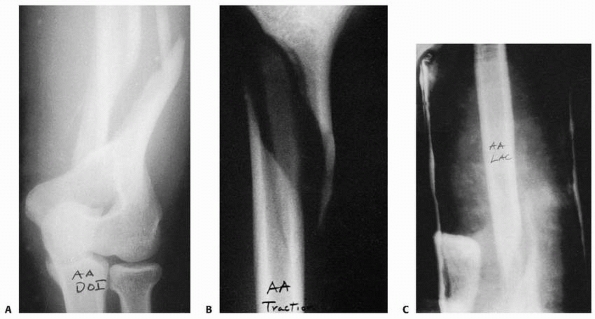 |
|
FIGURE 17-55 A comminuted distal humeral metaphyseal-diaphyseal fracture in a 14-year-old boy. Injury films (A) show multiple fragments in the metaphyseal-diaphyseal area. B. The patient was placed in traction for 2 weeks until callus appeared and then was transferred to a long-arm cast (C).
|
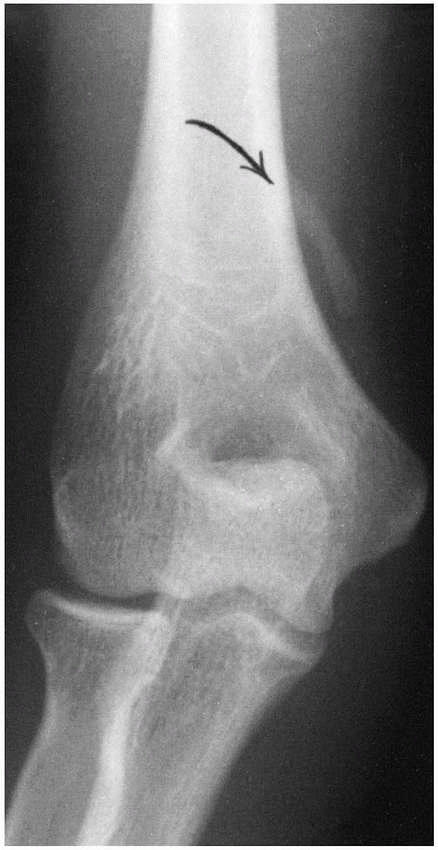 |
|
FIGURE 17-56 Radiographic appearance of a supracondylar process (arrow).
|
direct blows. There are no reports of avulsion from the anomalous
muscle attachments.
displaced or nondisplaced, with notation of median nerve or brachial
artery compromise.
and usually are caused by direct blows to the distal humeral area. They
may be quite painful and result in compression of the brachial artery
or median nerve.32,88,215,299,354,407 The process is best seen on oblique views.407
If there are no symptoms of median nerve or brachial artery
compression, they are treated by elevation, ice, and temporary
immobilization for comfort. However, if a painful nonunion or
neurovascular symptoms develop, the fragment should be excised.407 Fractures with neurologic signs or symptoms are treated by fragment excision and nerve and artery decompression.
GM, O’Phelan EM. Recurrent anterior dislocation of the shoulder: a
review of 40 athletes treated by subscapularis transfer (modified
Magnuson-Stack procedure). Am J Sports Med 1977;5:188-190.
AE, Hannafin JA. Stress fracture of the clavicle in a female
lightweight rower. A case report and review of the literature. Am J
Sports Med 2001;29(3):370-372.
H, D’Astous J, Letts J, et al. Masked rotatory subluxation of the atlas
associated with fracture of the clavicle: a clinical and biomechanical
analysis. J Bone Joint Surg Am 1998;27(5):375-380.
PL, Lee MA, Finemeier CG. Scapulothoracic dissociation: diagnosis and
treatment. Clin Orthop Relat Res 2003;416:237-244.
S, Barrios RH, Martínez-Peric R, et al. Surgical treatment of the
radial nerve lesions associated with fractures of the humerus. J Orthop
Trauma 1993;7:211-215.
K, Jensen PO, Lauritzen J. Treatment of clavicular fractures.
Figure-of-eight bandage versus a simple sling. Acta Orthop Scand
1987;58:71-74.
S, Feuilhade de Chauvin P, Camilleri A, et al. Recent fractures of the
humeral diaphysis in adults-comparison of orthopedic and surgical
treatment apropos of 252 cases [in French]. Rev Chir Orthop Reparatrice
Appar Mot 1984;70:49-61.
JA, Nasca RJ, Nelson CL. Supracondylar fractures of the humerus. The
role of dynamic factors in prevention of deformity. J Bone Joint Surg
Am 1977;59:589-595.
L, Sellier N, Kalifa G, et al. Diagnostic difficulties of isolated
symptomatic unilamellar periosteal appositions. Uncommon form of
fatigue fracture in children [in French]. J Radiol 1988;69:351-356.
JG, Regan K. Decreasing the incidence of recurrence of first-time
anterior shoulder dislocation with rehabilitation. Am J Sports Med
1984;12:283-291.
M, Salvati M, D’Andrea V, et al. Isolated lesion of the axillary nerve:
surgical treatment and outcome in 12 cases. Neurosurgery
1991;29:697-700.
B. A method for the treatment of humerus fractures in the newborn using
the S. von Rosen splint. Acta Orthop Scand 1969;40:234-236.
DP, Cassidy RH. Obstetrical paralysis and dislocation of the shoulder
in infancy. J Bone Joint Surg Am 1968;50:1447-1452.
SR, Graf P, Vidal P, et al. The risk of nonunion following closed-focus
nailing and reaming. Results of 1059 interventions using the Kuntscher
method. Int Orthop 1983;7:133-143.
SR, Steinmetz A, Wuyts JL, et al. A reliable orthopedic technic in the
treatment of humeral diaphyseal fractures in the adult: the hanging
plaster. Report of a series of 74 cases [in French]. J Chir (Paris)
1978;115:653-658.
BR Jr, O’Brien SJ, Warren RF, et al. An unusual neurological
complication of the Bristow procedure: a case report. J Bone Joint Surg
Am 1988;70:458-460.
DS, Kocher MS, Waters PM, et al. Chronic recurrent anterior
sternoclavicular joint instability: results of surgical management. J
Pediatr Orthop 2006;26(1):71-74.
G, Wilpulla E. Surgical or conservative treatment of total dislocation
of the acromioclavicular joint. Acta Chir Scand 1975;141:43-47.
GW, Mooney V, Ashby ME. Diaphyseal fractures of the humerus treated
with a ready-made fracture brace. J Bone Joint Surg Am 1982;64:11-13.
DB, Janus RB, Wade WH. Neuroarthropathy: an overuse injury of the
shoulder in quadriplegia. J Spinal Cord Med 1996;19:9-11.
A, Fernandez A, Luvizio J, et al. A combined therapeutic protocol for
aseptic nonunion of the humeral shaft: a report of 25 cases. J Trauma
1989;29:95-98.
A, Schimchak M, Carreras O, et al. Dislocation of the shoulder with
fracture of the ipsilateral shaft of the humerus. Injury
1985;16:300-302.
JB, Lim V, Mastromonaco E, et al. Axillary artery disruption secondary
to anterior dislocation of the shoulder. J Trauma 1983;23:1009-1011.
TP, Lombardo SJ, Kerlan RK, et al. The coracoid transfer for recurrent
anterior instability of the shoulder in adolescents. J Bone Joint Surg
Am 1985;67:383-387.
MP, Wiley JJ. Fractures of the proximal humeral epiphysis. Their
influence on humeral growth. J Bone Joint Surg Br 1986;68:570-573.
MJ, Beauchamp CG, Kellam JK, et al. The results of plating humeral
shaft fractures in patients with multiple injuries. The Sunnybrook
experience. J Bone Joint Surg Br 1985;67:293-296.
PE, Ofstein RA, Jackson DW, et al. MRI demonstration of
radiographically occult fractures: what have we been missing?
Radiographics 1989;9:407-436.
DC, Weiner DS, Noble JS, et al. Severely displaced proximal humeral
epiphyseal fractures: a follow-up study. J Pediatr Orthop 1998;18:31-37.
GH, McPherson JA, Reed MH. Traumatic pseudodislocation of the
acromioclavicular joint in children. A 15-year review. Am J Sports Med
1991;19:644-646.
ME, Satzman JS. Recurrent anterior subluxation of the shoulder in
athletics-a distinct entity (proceedings). J Bone Joint Surg Am
1969;51:1037-1038.
WA, Nijsten MW, ten Duis HJ. Treatment of humeral shaft fractures
related to associated injuries. A retrospective study of 237 patients.
Acta Orthop Scand 1991; 62:148-153.
S, Dahlback LO. Nerve injuries in dislocations of the shoulder joint
and fractures of the neck of the humerus. Acta Chir Scand
1970;136:461-466.
D, Curtis RJ Jr, DeHaan JT, et al. Nonunion of fractures of the
midshaft of the clavicle. Treatment with a modified Hagie
intramedullary pin and autogenous bone grafting. J Bone Joint Surg Am
1991;73:1219-1226.
DT, Pritchett JW. Straight-line graphs for the predictions of growth of
the upper extremities. J Bone Joint Surg Am 1993;75:885-892.
RE, Mah JY, Otsuka NY. Midshaft clavicle fractures associated with
atlantoaxial rotatory displacement: a report of two cases. J Orthop
Trauma 2003;17(6):444-447.
KT, Batt ME. Stress fracture of the proximal humeral epiphysis in an
elite junior badminton player. Br J Sports Med 1997;31:252-253.
O, Bakalim G, Vainionpää S, et al. Immediate radial nerve palsy
complicating fracture of the shaft of the humerus: when is early
exploration justified? Injury 1985; 16:499-502.
MA, MacDonald DA, Singh I, et al. Late fracture associated with
retained internal fixation. J Bone Joint Surg Br 1989;71:539.
MC, Mouton JN, Pierson M, et al. [Periostitis or, rather, periosteal
appositions in paediatrics (author’s translation).] J Radiol Electrol
Med Nucl 1977;58(2):119-123.
WW, Gellman H, Becker V, et al. Management of fractures of the humerus
in patients who have an injury of the ipsilateral brachial plexus. J
Bone Joint Surg Am 1990;72:1208-1210.
FH, Burbach T. Ultrasonic diagnosis of separation of the proximal
humeral epiphysis in the newborn. J Bone Joint Surg Am 1990;72:187-191.
S. Bilateral congenital pseudarthrosis of the clavicles? Case report
and review of the literature. Br J Clin Pract 1984;38:432-433.
JE, Stanley RF, Tullos HS, et al. Acromioclavicular joint dislocations:
comparative results following operative treatment with and without
primary distal clavisectomy. Am J Sports Med 1977;5:258-263.
RJ, Bosse MJ, Poka A, et al. Intramedullary stabilization of humeral
shaft fractures in patients with multiple trauma. J Bone Joint Surg Am
1986;68:960-970.
OS, Onoprienko GA, Shternberg AA, et al. Treatment of diaphyseal
pseudarthrosis with transosseous osteosynthesis [in Russian]. Vestn
Khir Im I I Grek 1977; 119:84-87.
J, Gonzales-Herranz P, Lopez-Mondejar JA, et al. Fractures of the
proximal humeral epiphysis. Int Orthop 1993;17:16-19.
WZ Jr, Rockwood CA Jr. Treatment of instability of the shoulder with an
exercise program. J Bone Joint Surg Am 1993;75:311-312.
JD, Solan M, Gidwani S, et al. Management of paediatric clavicle
fractures—is follow-up necessary? An audit of 346 cases. Ann R Coll
Surg Engl 2002;84(5):331-333.
M, Lefebvre G, Veron P, et al. Obstetrical injuries of the newborn
infant. Retrospective study apropos of 20,409 births [in Russian]. J
Gynecol Obstet Biol Reprod (Paris) 1985;14:1033-1043.
Orthopaedic Trauma Society. Nonoperative treatment compared with plate
fixation of displaced midshaft clavicular fractures. A multicenter,
randomized clinical trial. J Bone Joint Surg Am 2007;89(1):1-10.
ST, Puhl J, Watson FM, et al. Acute osteomyelitis following closed
fractures. Report of three cases. J Bone Joint Surg Am 1975;57:415-418.
C, Sweetnam R. Recurrent dislocation of the patella and of the
shoulder: their association with familial joint laxity. J Bone Joint
Surg Br 1960;42:721-727.
R, Catagni MA, Guerreschi F. Applications of the Ilizarov method in the
humerus. Lengthenings and nonunions. Hand Clin 1993;9:729-739.
R, Villa A, Catagni MA, et al. Lengthening of the humerus using the
Ilizarov technique. Description of the method and report of 43 cases.
Clin Orthop Relat Res 1990;250:117-124.
J, Brabant A, Charignon G, et al. Treatment of fractures of the humerus
by intramedullary fixation. J Chir (Paris) 1975;109:75-82.
Y, Agorastides I, Garg N, et al. Treatment of severely displaced
proximal humeral fractures in children with elastic stable
intramedullary nailing. J Pediatr Orthop B 2006; 15(1):45-50.
JC, Shen WY. Limb fracture pattern in different pediatric age groups: a
study of 3,350 children. J Orthop Trauma 1993;7:15-22.
WR Jr, Rankin JS, Bollinger RR, et al. Brachial artery reconstruction
using the heparin-bonded Sundt shunt. Surgery 1981;89:355-358.
NO. Kuntscher intramedullary reaming and nail fixation for nonunion of
the humerus. Clin Orthop Relat Res 1976;116:222-225.
C, Cervelalti C, Montanari G, et al. The Ilizarov method for the
treatment of nonunion in the humerus. Chir Organi Mov 1990;75:115-120.
RL, Milgram JW, Yawn DH. Fatal aortic perforation and cardiac tamponade
due to a Kirschner wire migrating from the right sternoclavicular
joint. South Med J 1974; 67:316-318.
LN, Narakas AO. Operative management of lesions of the axillary nerve,
isolated or combined with other nerve lesions. Clin Neurol Neurosurg
1992;94(suppl): S64-S66.
N, Simonatti R, Ramondetta V, et al. Intramedullary nailing with a rush
pin in the treatment of diaphyseal humeral fractures [in Italian]. Arch
Putti Chir Organi Mov 1990;38:395-403.
JF. Selection, evaluation, and indications for electrical stimulation
of ununited fractures. Clin Orthop Relat Res 1981;161:39-53.
P, Giancecchi F, Cavazzuti A. Internal and external fixation in complex
diaphyseal and metaphyseal fractures of the humerus. Ital J Orthop
Traumatol 1991;17:87-94.
DC, Riordan DC, Milstead ME, et al. Modification of the L’Episcopo
procedure for brachial plexus birth palsies. J Bone Joint Surg Br
1992;74:897-901.
JF. Rupture of the axillary artery complicating dislocation of the
shoulder: report of a case. J Bone Joint Surg Br 1970;52:313-317.
RJ Jr, Dameron TB Jr, Rockwood CA Jr, et al., eds. Fractures and
Dislocations of the Shoulder in Children. 3rd ed. Philadelphia: JB
Lippincott, 1991:829-919.
EJ, Banta CJ II, Murphy CP, et al. Plate fixation of the humeral shaft
for acute fractures, with and without radial nerve injuries. J Orthop
Trauma 1992;6:10-13.
Monte A, Andrisano A, Manfrini M, et al. Humeral lengthening in
hypoplasia of the upper limb. J Pediatr Orthop 1985;5:202-207.
PG, Bryan WJ. Displaced Salter-Harris type I injury in a gymnast. A
slipped capital humeral epiphysis? Orthop Rev 1994;23:538-541.
TB, Rockwood CA. Fractures and dislocations of the shoulder. In:
Rockwood CA, Wilkins KE, King RE, eds. Fractures in Children.
Philadelphia: JB Lippincott, 1984: 624-676.
JC Jr, Smith JA, Lockwood RC. A new conservative method for the
treatment of type III acromioclavicular separations. Orthop Clin North
Am 1980;11:727-733.
C, Fenoll B, Le Nen D, et al. Epiphyseal fracture-avulsion of the
distal extremity of the clavicle. Ann Radiol (Paris) 1993;36:125-128.
Bastiani G, Aldegheri R, Renzi Brivio L. The treatment of fractures
with a dynamic axial fixator. J Bone Joint Surg Br 1984;66:538-545.
Mourgues G, Fischer LP, Gillet JP, et al. Arterial intraosseous
vascularization of the humerus [Recent fractures of the humeral
diaphysis apropos of a continuous series of 200 cases, of which 107
were treated with a hanging cast alone]. Rev Chir Orthop Reparatrice
Appar Mot 1975;61:191-207.
Santa DR, Narakas AO. Fractures of the clavicle and secondary lesions
of the brachial plexus [in French]. Z Unfallchir Versicherungsmed
1992;85:58-65.
Santa DR, Narakas AO, Bonnard C. Late lesions of the brachial plexus
after fracture of the clavicle. Ann Chir Main Memb Super
1991;10:531-540.
WG Jr, Born CT, Marcelli E, et al. Ender nail fixation in long bone
fractures: experience in a level I trauma center. J Trauma
1989;29:571-576.
AF, Cooke AJ, Probhakar M. The role of the subscapularis in recurrent
anterior dislocations of the shoulder. Clin Orthop Relat Res
1967;54:35-49.
AF, Silverstein CE. Results following a modified Magnuson procedure in
recurrent dislocation of the shoulder. Surg Clin North Am
1963;43:1651-1653.
C, Safary A. The treatment of fractures of the neck and diaphysis of
the humerus by Hackethal’s bundle nailing. Acta Orthop Belg
1979;45:666-677.
Filippo P, Mancini GB, Gillio A. Humeral fractures with paralysis of
the radial nerve. Arch Putti Chir Organi Mov 1990;38:405-409.
JD, Mehlman CT, Urse JS. Fracture of the shaft of the humerus secondary
to muscular violence. J Orthop Trauma 1993;7:90-93.
JH III. Posterior dislocation and posterior fracture dislocation of the
shoulder: a report of 25 cases. South Med J 1967;60:661-666.
MB, Luhmann SL, Gordon JE, et al. Severely displaced proximal humeral
epiphyseal fractures. J Pediatr Orthop 2003;23(2):208-215.
SJ, Giddins GE, Birch R. A slowly evolving brachial plexus injury
following a proximal humerus fractures in a child. J Hand Surg Br
1995;20:24-25.
O, Beaufils P, Ouaknine M, et al. Functional treatment of recent
fractures of the humeral shaft using the Sarmiento method [in French].
Rev Chir Orthop Reparatrice Appar Mot 1989;75:292-300.
TW, Fulkerson JP. Pneumothorax complicating a closed fracture of the
clavicle. A case report. Clin Orthop Relat Res 1987;221:212-214.
RA, Gottesman MJ, Saunders KC. Hackethal stacked nailing of humeral
shaft fractures. Experience with 30 patients. Clin Orthop Relat Res
1983;179:168-174.
HL. Radial nerve in osseous tunnel at humeral fracture site diagnosed
radiographically. J Bone Joint Surg Br 1957;39:746-747.
B, Augereau B, Asselineau A, et al. Closed intramedullary nailing of
fractures of the shaft of the humerus. Int Orthop 1983;7:195-203.
BS, Libshitz HI, Cohen MA. Slipped proximal humeral epiphysis: a
complication of radiotherapy to the shoulder in children. Skeletal
Radiol 1982;9:123-125.
R, Parent H, Zeller R, et al. Traumatic scapulohumeral dislocation in
children and adolescents. Apropos of nine patients [in French]. Acta
Orthop Belg 1994;60: 204-209.
BK, Frierson MA, Raney EM, et al. Humerus varus: a complication of
neonatal, infantile, and childhood injury and infection. J Pediatr
Orthop 1994;14:479-486.
S, Kasai T, Fujii N, et al. Traumatic anterior dislocation of the
shoulder in a child. Arch Orthop Trauma Surg 1993;112: 201-202.
JL Jr, Brighton CT, Heppenstall RB, et al. Nonunion of the humerus.
Clinical, roentgenographic, scintigraphic, and response characteristics
to treatment with constant direct current stimulation of osteogenesis.
Clin Orthop Relat Res 1986;211: 228-234.
RS, Stankovits L, Domzalski ME, et al. Fractures of the distal humeral
metaphyseal-diaphyseal junction in children. J Pediatr Orthop
2008;28(2):142-146.
RJ, Dixon GL Jr, Bach AW, et al. Internal fixation of fractures and
nonunions of the humeral shaft. Indications and results in a
multicenter study. J Bone Joint Surg Am 1985;67:857-864.
RJ, Swiontkowski MF, Back AW, et al. Radial nerve palsy caused by open
humeral shaft fractures. J Hand Surg Am 1993;18:121-124.
RJ, Smith RJ. Radial nerve laceration 26 years after screw fixation of
a humeral fracture-a case report. J Bone Joint Surg Am 1984;66:959-960.
JC, Thoulon JM, Chappuis JP, et al. Injuries to the upper extremities
in the newborn diagnosed at birth [in French]. J Gynecol Obstet Biol
Reprod (Paris) 1975; 4:245-254.
JG, Rinsky LA, Strudwick J, et al. Nonunion of fractures in children
who have osteogenesis imperfecta. J Bone Joint Surg Am 1988;70:439-443.
MA, Bidstrup BP. Intrathoracic great vessel injury resulting from blunt
chest trauma associated with posterior dislocation of the
sternoclavicular joint. Aust N Z J Surg 1983;53:427-430.
DE, Jones RC, Kunkle RW. Upper extremity fractures in the acute spinal
cord injured patient. Clin Orthop Relat Res 1988;233:110-115.
WP Jr, Leberte MA, Cool TA. Recurrent fractures of the humerus in a
baseball pitcher—a case report. J Bone Joint Surg Am 1988;70:305-306.
C, Rockwood CA Jr. Subcoracoid dislocation of the lateral end of the
clavicle. A report of three cases. J Bone Joint Surg Am 1987;69:924-927.
C, Schneeberger AG, Vinh TS. The arterial vascularization of the
humeral head. An anatomical study. J Bone Joint Surg Am
1990;72:1486-1494.
G, Suren EG. Injuries of the proximal humeral epiphysis. Indications
for surgical therapy and results. Chirurgie 1983;54:406-410.
TJ, Waters P. Valgus osteotomy of the humeral neck: a technique for the
treatment of humerus varus. J Shoulder Elbow Surg 1997;6:306-310.
G, Schatten C. Incidence and potential factors in the genesis of birth
injury induced clavicular fractures [in German]. Zentralbl Gynakol
1987;109:909-912.
E, Slungaard U. Treatment of humeral fractures with and without injury
to the radial nerve-a follow-up study. Tidsskr Nor Laegeforen
1981;101:1746-1749.
NJ, Stabler J, Albert JS. Atlantoaxial rotatory fixation and fracture
of the clavicle: an association and classification. J Bone Joint Surg
Br 1990;72:72-75.
BJ, Nirschl RP, McConnell JP, et al. Arthroscopic transglenoid suture
capsulolabral repairs: preliminary results. Am J Sports Med
1993;21:656-665.
CA, Bassett GS, Sullivan S, et al. Retrosternal displacement after
physeal fracture of the medial clavicle in children treatment by open
reduction and internal fixation. J Bone Joint Surg Br
2001;83(8):1168-1172.
RM, Rogers LF, Bowerman J, et al. Osseous manifestations of elbow
stress associated with sports activities. AJR Am J Roentgenol
1980;134:971-977.
NE, Wheelhouse WW. Anterior subglenoid dislocation of the shoulder in
an infant following pneumococcal meningitis. Clin Orthop Relat Res
1978;135:125-127.
F, Naggar L, Ginalski JM, et al. Magnetic resonance imaging of
nontraumatic shoulder instability in children. Skeletal Radiol
1992;21:19-21.
L, Allouis M, Bourdelat D, et al. Fractures and slipped epiphysis of
the proximal humerus in children. Place and methods of surgical
treatment. Chir Pediatr 1983;24: 197-200.
A, Sharma S. Volar compartment syndrome of the arm complicating a
fracture of the humeral shaft—a case report. Acta Orthop Scand
1991;62:77-78.
RC, Gaur SC, Tiwari RC, et al. Treatment of ununited fractures of the
shaft of the humerus with bent nail. Injury 1985;16:276-280.
RF Jr, Pankovich AM. Ender nailing of acute fractures of the humerus. A
study of closed fixation by intramedullary nails without reaming. J
Bone Joint Surg Am 1987; 69:558-567.
RJ, Angelo RL. Glenohumeral osteoarthritis: acute complications of the
Putti-Platt repair. J Bone Joint Surg Am 1990;72:1193-1197.
RJ, Koppert G, Johnston G. Recurrent posterior instability
(subluxation) of the shoulder. J Bone Joint Surg Am 1984;66:169-174.
O. Growth stimulation of long bones after fracture or similar trauma. A
clinical and experimental study. Acta Orthop Scand Suppl 1969;122:1-134.
DM, Manoli A II, Little RE. Elbow dislocation during overhead skeletal
traction therapy: a case report. Clin Orthop Relat Res 1981;154:185-187.
M, Horoszowski H. Martinowitz U. Hemophilic arthropathy resulting in a
locked shoulder. Clin Orthop Relat Res 1986;202:169-172.
MB, Monroe M, Tencer AF. Biomechanical comparison of methods of
fixation of a midshaft osteotomy of the humerus. J Orthop Trauma
1991;5:14-20.
SP, Bush-Joseph CA, Kuo KN, et al. Throwing-induced humeral shaft
fracture in skeletally immature adolescents. Orthopedics
1999;22:621-622.
HG, Pfister U, Weller S. Influence of the treatment of fractures on the
development of pseudoarthroses of the humerus shaft. Aktuel Traumatol
1980;10: 137-142.
A, Drez D. Operative treatment of posterior shoulder dislocations by
posterior glenoidplasty, capsulorrhaphy, and infraspinatus advancement.
Am J Sports Med 1986;14:187-191.
D Jr, Fiennes AG, Allgöwer M, et al. The floating shoulder: ipsilateral
clavicle and scapular neck fractures. J Bone Joint Surg Br
1992;74:362-364.
MM, Phipps GJ. Closed reduction and tendon transfer for treatment of
dislocations of the glenohumeral joint secondary to brachial plexus
birth palsy. J Bone Joint Surg Am 1998;80:997-1001.
L, Augustini BG, Fredin H, et al. Primary anterior dislocation of the
shoulder in young patients: a 10-year prospective study. J Bone Joint
Surg Am 1996;78: 1677-1684.
L, Eriksson K, Fredin H, et al. Recurrences after initial dislocation
of the shoulder. J Bone Joint Surg 1983;65: 343-349.
L, Olofsson A, Sandström B, et al. Nonoperative treatment of primary
anterior shoulder dislocation in patients 40 years of age and younger.
a prospective 25-year follow-up. J Bone Joint Surg Am
2008;90(5):945-952.
CB, Shinwell E, Nyska M, et al. Ultrasound diagnosis of neonatal
fracture separation of the upper humeral epiphysis. J Bone Joint Surg
Br 1992;74:471-472.
FM, Shafer SJ. Injuries to the clavicle with neurovascular
complications. A study of fourteen cases. J Bone Joint Surg Am
1965;47:1335-1346.
NJ, Eloesser L. Treatment of fracture of the upper end of the humerus:
an experimental and clinical study. J Bone Joint Surg Am 1934;16:1-29.
H, Gerber C. Voluntary subluxation of the shoulder in children. A
long-term follow-up study of 36 shoulders. J Bone Joint Surg Am
1994;76:118-122.
RW, Bae DS, Waters PM. Brachial plexus palsy following proximal humerus
fracture in patients who are skeletally immature. J Orthop Trauma
2008;22(4): 286-290.
R. Fractures of the scapula involving the glenoid fossa. In: Bateman
JE, Walsh RD, eds. Surgery of the Shoulder. Toronto: BC Decker,
1984:63-66.
GA, Shevtsov VI. Bloodless compression-distraction osteosynthesis in
the treatment of pseudarthroses of the humerus [in Russian]. Voen Med
Zh 1974;6:27-31.
AM, Waters DA. Locked intramedullary nailing of humeral shaft
fractures. Implant design, surgical technique, and clinical results. J
Bone Joint Surg Br 1994;76: 23-29.
E, Hatakeyama Y, Sato T, et al. Immobilization in external rotation
after shoulder dislocation reduces the risk of recurrence. A randomized
controlled trial. J Bone Joint Surg Am 2007;89(10):2124-2131.
H, Warner JJ, Jakob RP. Percutaneous stabilization of unstable
fractures of the humerus. J Bone Joint Surg Am 1992;74:508-515.
M, Sutker A, Post M. Irreducible fracture of the middle third of the
clavicle. Report of a case. J Bone Joint Surg Am 1979;61:296-298.
P, Myllyla V, Paivansalo M. Autotraction stress roentgenography for
demonstration of anterior and inferior instability of the shoulder
joint. Clin Orthop Relat Res 1992;284:136-143.
P, Heinrich SD. Ipsilateral proximal metaphyseal and flexion
supracondylar humerus fractures with an associated olecranon avulsion
fracture. Orthopedics 1991;14: 713-716.
PO, Andersen K, Lauritzen J. Treatment of midclavicular fractures. A
prospective randomized trial comparing treatment with a figure-of-eight
dressing and a simple arm sling [in Danish]. Ugeskr Laeger
1985;147:1986-1988.
DJ, Radford WJ, Parnel EJ. Interobserver variation using the AO/ASIF
classification of long-bone fractures. Injury 1993;24:163-165.
KJ, Wiesel B, Ganley TJ, et al. Functional outcomes of early
arthroscopic bankart repair in adolescents aged 11 to 18 years. J
Pediatr Orthop 2007;27(2):209-213. Erratum in: J Pediatr Orthop
2007;27(4):483.
A, Andermahr J, Schiffer G, et al. Elastic stable intramedullary
nailing of midclavicular fractures with a titanium nail. Clin Orthop
Relat Res 2003;408:279-285.
M, Michaelson M, Waisbrod H. The use of external skeletal fixation in
the treatment of fractures of the humeral shaft. Injury 1978;9:245-248.
J, Rentis G, Varouchas G. Repair of anterior dislocation of the
shoulder using transfer of the subscapularis tendon. J Bone Joint Surg
Am 1980;62:1147-1149.
R, Landman J, Dulitzky F, et al. Fracture of the clavicle in the
newborn. An ultrasound diagnosis. J Ultrasound Med 1988;7:21-23.
R, Mahlfeld K, Heyde C, et al. Ultrasonographic imaging of fractures of
the clavicle in newborn infants. J Bone Joint Surg Br
2003;85(1):115-116.
RP, Wilson CL. Bilateral recurrent dislocation of the shoulder
(atraumatic) in a 13-year-old girl. J Bone Joint Surg Am
1961;43:553-554.
JM, Papadopoulos IA. Late treatment of brachial plexus palsy secondary
to birth injuries: rotational osteotomy of the proximal part of the
humerus. J Bone Joint Surg Am 1998;80:1477-1483.
SC, Vander Schilden JL, Park JP. Late effect of isolated avulsion
fractures of the lesser tubercle of the humerus in children. Report of
two cases. J Bone Joint Surg Am 1993;75:1691-1694.
PK, Akins CM. The “vanishing” epiphysis: sign of Salter type I fracture
of the proximal humerus in infancy. Br J Radiol 1982;55:865-867.
MS, Swischuk LE, Fagan CJ. Patterns of injury and significance of
uncommon fractures in the battered child syndrome. Am J Roentgenol
Radium Ther Nucl Med 1974;121:143-149.
R, Trillaud JM. Fracture and fracture separation of the proximal
humerus in children: report of 136 cases. J Pediatr Orthop
1983;3:326-332.
LW, Moore RD. Fractures of the supracondylar process of the humerus.
Report of two cases. J Bone Joint Surg Am 1967;49:532-534.
RU, Dronen SC. Prospective evaluation of the scapular manipulation
technique in reducing anterior shoulder dislocations. Ann Emerg Med
1992;21:1349-1352.
R, Slongo T. Operative treatment of clavicle fractures in children: a
review of 21 years. J Pediatr Orthop 2002;22(6):736-739.
JE, Blasier RB, Carpenter JE. Fractures of the acromion process: a
proposed classification system. J Orthop Trauma 1994;8:6-13.
HA, Rustemeier M. Clinical experiences in the treatment of humeral
shaft fractures with the Sarmiento brace. Unfallchirurgie
1988;14:191-198.
O, Maier R, Kutscha-Lissberg F, et al. Treatment procedure in humeral
shaft fractures with primary or secondary radial nerve damage.
Unfallchirurgie 1992;18: 168-173.
LA. Fracture patterns in children. Analysis of 8682 fractures with
special reference to incidence, etiology, and secular changes in
Swedish urban population 1950-1979. Acta Orthop Scand Suppl
1983;202:1-109.
RH, Foster RJ. Skeletal management of humeral shaft fractures
associated with forearm fractures. Clin Orthop Relat Res
1985;195:173-177.
CF, Kiaer T, Lindequist S. Fractures of the proximal humerus in
children: 9-year follow-up of 64 unoperated on cases. Acta Orthop Scand
1990;61:255-257.
P, Haumont T, Journeau P. Use and abuse of flexible intramedullary
nailing in children and adolescents. J Pediatr Orthop
2006;26(6):827-834.
HG. Operative reduction of an unusual fracture of the upper epiphyseal
plate of the humerus. J Bone Joint Surg 1944;26:401-404.
SJ, Meinhard BP, Schultz E, et al. Open reduction and internal fixation
of a glenoid fossa fracture in a child: a case report and review of the
literature. J Orthop Trauma 1997;11(6):452-454.
TR, Franta AK, Wolf FM, et al. Arthroscopic compared with open repairs
for recurrent anterior shoulder instability. A systematic review and
meta-analysis of the literature. J Bone Joint Surg Am
2007;89(2):244-254.
KS, Kwan M, Wong J, et al. Therapeutic functional bracing in upper limb
fracture-dislocations. J Orthop Trauma 1999;2:308-313.
KS, Lam TP. Open reduction and internal fixation of ipsilateral
fractures of the scapular neck and clavicle. J Bone Joint Surg Am
1993;75:1015-1018.
LS, Goldner RD, Urbaniak JR, et al. Management of severe
musculoskeletal injuries of the upper extremity. J Orthop Trauma
1990;4:432-440.
RP, Pritchard DJ, Sim FH. Treatment of pathologic fractures or
impending fractures of the humerus with rush rods and
methylmethacrylate. Experience with 55 cases in 54 patients, 1968-1977.
Clin Orthop Relat Res 1982;166:193-198.
G, Bartel HG. Unusual migration of a Kirschner wire following drill
wire fixation of a subcapital humerus fracture [in German]. Beitr
Orthop Traumatol 1987; 34:585-587.
FL, Furey JG. Obstetrical paralysis with dislocation of the shoulder: a
case report. J Bone Joint Surg Am 1953;35:227-230.
SJ, Kerlan RK, Jobe FW, et al. The modified Bristow procedure for
recurrent dislocation of the shoulder. J Bone Joint Surg Am
1976;58:256-261.
R, Ruggiero L. Left pneumothorax with subcutaneous emphysema secondary
to left clavicular fracture and homolateral obstetrical paralysis of
the arm. Minerva Pediatr 1982;34:273-276.
DA, With MA, Wurtz D, et al. Loss of external rotation following
anterior capsulorrhaphy of the shoulder. J Bone Joint Surg Am
1993;75:1185-1192.
FA, Rockwood CA Jr. Current concepts review. Migration of pins used in
operations on the shoulder. J Bone Joint Surg Am 1990;72:1262-1267.
MF. Roentgenographic evidence of median-nerve entrapment in a
greenstick humeral fracture. J Bone Joint Surg Am 1978;60:998-1000.
GS, Howard JM, Green RL. Arterial injuries complicating fractures or
dislocations: the necessity for a more aggressive approach. Surgery
1966;59:203-209.
HJ, Angel KR, Schemitsch EH, et al. The fate of traumatic anterior
dislocation of the shoulder in children. J Bone Joint Surg Am
1992;74:1242-1244.
RP, Parsons DL. Avascular necrosis of the proximal humeral epiphysis
after physeal fracture. A case report. J Bone Joint Surg Am
1997;79:760-762.
B, Käch K, Candinas D, et al. Results of intramedullary nailing in
humerus shaft fractures. Helv Chir Acta 1993;59:681-685.
JW, Spiegel PG, Harvey JP Jr, et al. Fractures of the humeral shaft. A
retrospective study of 240 adult fractures. Clin Orthop Relat Res
1975;112:254-262.
D, Van Looy F, Geens S. Recurrent anterior dislocations of the shoulder
joint treated by the Bristow-Latarjet procedure. Acta Orthop Belg
1992;58:16-22.
R Jr. Migration of a Kirschner wire from the shoulder region into the
lung: a report of two cases. J Bone Joint Surg Am 1943;25:477-483.
JP, Rab GT. Fracture of the acromion associated with an axillary nerve
deficit: a case report and review of the literature. Clin Orthop Relat
Res 1980;147:216-218.
JJ, Brief DK, Stremple JF, et al. Management of fractures with
associated arterial injury in combat casualties. J Trauma 1973;13:17-19.
DM, Gauger JU, Schmitt-Koppler A. Experiences with cluster nailing of
humeral shaft fractures. Unfallchirurgie 1985;11:70-75.
JP, Ligier JN. Surgical treatment of fractures of the long bones in
children. Interference between osteosynthesis and the physiological
processes of consolidation. Therapeutic indications. J Chir (Paris)
1984;121:527-537.
DS, Boswick JA Jr. Lesions of the brachial plexus associated with
fractures of the clavicle. Clin Orthop Relat Res 1969;64:144-149.
SP, Loyd RD. Avulsion fracture of the coracoid epiphysis with
acromioclavicular separation. Report of two casesin adolescents and
review of the literature. J Bone Joint Surg Am 1977;59:963-965.
WH III, Jobe FW. Functional outcomes in athletes after modified
anterior capsulolabral reconstruction. Am J Sports Med 1994;22:352-358.
PD, Egan TJ. Axillary artery injury in erect dislocation of the
shoulder (luxatio erecta): a case report. J Ir Orthop 1983:260-261.
ME, Allgower M, Schneider R, et al. Manual of Internal Fixation.
Techniques Recommended by the AO-ASIF Group. 3rd ed. Berlin:
Springer-Verlag, 1991.
D, Knoefel WT, Schweiberer L. The treatment of humeral shaft fractures.
Results of a prospective AO multicenter study. Unfallchirurgie
1991;94:447-454.
CS II. Involuntary inferior and multidirectional instability of the
shoulder: etiology, recognition, and treatment. AAOS Instr Course Lect
1985;34:232-238.
J, Horoszowski H, Goodman RM. Fracture in progressive ossifying
fibrodysplasia —a case report. Acta Orthop Scand 1987;58:289-291.
LF, Krufky EL, Mueller RE, et al. Locked scapula: intrathoracic
dislocation of the inferior angle. A case report. J Bone Joint Surg Am
1972;54(2):413-416.
HC. Limits of spontaneous correction of incorrectly healed fractures in
adolescence. Langenbecks Arch Chir 1969;324:78-86.
A, Petersson C. Fracture of the body, neck, or spine of the scapula. A
long-term follow-up study. Clin Orthop Relat Res 1992;283:139-144.
A, Petersson CJ. Incidence and causes of shoulder girdle injuries in an
urban population. J Shoulder Elbow Surg 1995;4:107-112.
SW, Evans DC. Contralateral shoulder instability following anterior
repair. An epidemiological investigation. J Bone Joint Surg Br
1991;73:941-946.
SW, Evans DC. Long-term results of staple capsulorrhaphy for anterior
instability of the shoulder. J Bone Joint Surg Am 1993;75:249-258.
S, Uhthoff HK. The early development and ossification of the human
clavicle. An embryologic study. Acta Orthop Scand 1990;61:330-334.
BK, Kay RM, Choi PD, et al. Complete division of the radial nerve
associated with a closed fracture of the humeral shaft in a child. J
Bone Joint Surg Br 2007;89(6): 821-824.
JA, Conlogue GJ, Bronson ML. Radiology of postnatal skeletal
development. III. The clavicle. Skeletal Radiol 1979;4:196-203.
JA, Conlogue GJ, Jensen P. Radiology of postnatal skeletal development:
the proximal humerus. Skeletal Radiol 1978;2:153-160.
W, Popiński M. Fractures of the neck and shaft of the humerus as a rare
form of double fractures in children [in Polish]. Chir Narzadow Ruchu
Ortop Pol 1974; 39:121-123.
SL, Burgess A, Levine AM. Traumatic lateral displacement of the
scapula: a radiographic sign of neurovascular disease. J Bone Joint
Surg Am 1984;66:758-763.
KG, Bell DF. Structural abnormality of the clavicle associated with
Sprengel’s deformity: a case report. Clin Orthop Relat Res
1990;258:157-159.
JW, Foster RR, Garcia A, et al. The humeral fracture with radial nerve
palsy: is exploration warranted? Clin Orthop Relat Res 1972;88:34-38.
PM, Oostvogel HJ, Bongers KJ, et al. Early functional treatment of
humerus shaft fractures by the Sarmiento method [in German]. Aktuel
Traumatol 1987;17: 150-152.
RE, Hoffmeyer P, Henley MB. Treatment of humeral diaphyseal fractures
with Hackethal stacked nailing: a report of 33 cases. J Orthop Trauma
1992;6:14-17.
HA, Madhok R, Benson JT, et al. Physeal fractures: Part 1. Epidemiology
in Olmsted County, Minnesota, 1979-1988. J Pediatr Orthop
1994;14:423-430.
GJ, Hoffer MM. Latissimus dorsi and teres major transfer to rotator
cuff for Erb’s palsy. J Shoulder Elbow Surg 1995;4:124-129.
FH, Drake D, Bovill EG, et al. Treatment of radial neuropathy
associated with fractures of the humerus. J Bone Joint Surg Am
1981;63:239-243.
F, Morace GB. Fractures of the humerus associated with paralysis of the
radial nerve. Ital J Orthop Traumatol 1988;14:455-465.
DJ, Juanteguy JM, Wilder RJ, et al. Arterial injuries of the
extremities associated with fractures. Arch Surg 1972;105:582-585.
JW. Delayed union of humeral shaft fractures treated by closed flexible
intramedullary nailing. J Bone Joint Surg Br 1985;67:715-718.
P, Lusi K, Baillon JM, et al. The treatment of fractures of the humeral
diaphysis with fasciculated intramedullary pins by the Hackethal method
apropos of 194 cases [in French]. Acta Orthop Belg 1984;50:521-538.
AA, Kuo KN. Posttraumatic cleidoscapular synostosis following a
fracture of the clavicle. J Bone Joint Surg Am 1999;81:256-258.
NM, Metz CW Jr, Hutton JE Jr, et al. Internal versus external fixation
of fractures with concomitant vascular injuries in Vietnam. J Trauma
1971;11:463-473.
BL, Buterfield SL, Daffner RH, et al. The abduction lordotic view of
the clavicle: a new technique for radiographic visualization. J Orthop
Trauma 1991;5:392-394.
BL, Foglesong ME, Burke CJ III, et al. Complications of Seidel
intramedullary nailing of narrow-diameter humeral diaphyseal fractures.
Orthopaedics 1994;17: 19-29.
CA Jr, Matsen FA, Thomas SC. Anterior glenohumeral instability. In: CA
Rockwood, FA Matsen III, eds. The Shoulder. Philadelphia: WB Saunders,
1990: 592-598.
JF, Bennett JB, Tullos HS. Management of concomitant ipsilateral
fractures of the humerus and forearm. J Bone Joint Surg Am
1984;66:552-556.
PM, Vansteenkiste F, Stappaerts KH, et al. Indications, dangers, and
results of surgical treatment of humeral shaft fractures [in German].
Unfallchirurg 1989;92: 565-570.
GJ, Love MB. Isolated avulsion fracture of the lesser tuberosity of the
humerus: report of two cases. Radiology 1989;172:833-834.
T, Moshfegh A, Pfeiffer KM, et al. Fresh fractures of the shaft of the
humerusconservative or operative treatment? Reconstr Surg Traumatol
1974;14:65-74.
RA, Lin D, Stone ML, et al. Can the need for future surgery for acute
traumatic anterior shoulder dislocation be predicted? J Bone Joint Surg
Am 2007;89(8): 1665-1674.
de Gauzy J, Vidal H, Cahuzac JP. Primary shortening followed by callus
distraction for the treatment of a posttraumatic bone defect: case
report. J Trauma 1993;34: 461-463.
M, Grujicic D, Milinkovic ZB. Radial nerve lesions associated with
fractures of the humeral shaft. Injury 1990;21:220-222.
JO, Rockwood CA Jr, Curtis RJ. Fractures and dislocations of the
humeral shaft and shoulder. In: Rockwood CA Jr, Wilkins KE, Beaty JH,
eds. Fractures in Children. Philadelphia: Lippincott-Raven,
1996:905-1021.
HN. The Moro reflex as a diagnostic aid in fracture of the clavicle in
the newborn infant. Am J Dis Child 1931;41:1304-1306.
A, Horowitch A, Aboulafia A, et al. Functional bracing for comminuted
extra-articular fractures of the distal third of the humerus. J Bone
Joint Surg Br 1990; 72:283-287.
A, Kinman PB, Galvin EG, et al. Functional bracing of fractures of the
shaft of the humerus. J Bone Joint Surg Am 1977;59:596-601.
W. [Effect of dia- and pericondylar humeral fractures on the growth of
the carpal bones in children.] Handchir Mikrochir Plast Chir
1982;14:103-105.
SA, Lawrence JF, Johnson MK. Lengthening of the humerus for upper
extremity limb length discrepancy. J Pediatr Orthop 1986;6:477-480.
L, Christel P, Duriez J, et al. Acceleration of repair of nonunions by
electromagnetic fields. Rev Chir Orthop Reparatrice Appar Mot
1981;67:11-23.
L, Christel P, Duriez R, et al. Results of nonunions treatment by
pulsed electromagnetic field stimulation. Acta Orthop Scand Suppl
1982;196:81-91.
J, Valdés F, Kramer A. Acute ischemia of the upper extremity caused by
axillary contused trauma. Report of three cases [in Spanish]. Rev Med
Child 1991;119: 567-571.
S, Lascombes P, Prevot J, et al. Centromedullary nailing in fractures
of the upper end of the humerus in children and adolescents. Chir
Pediatr 1990;31:43-46.
JJ, Bhatti NA. Radial nerve paralysis associated with fractures of the
humerus: a review of 62 cases. Clin Orthop Relat Res 1983;172:171-176.
VK, Jain Ak, Gupta RK, et al. Nonoperative treatment of fractures of
the humeral shaft: a comparative study. J Indian Med Assoc
1991;89:157-160.
BA, Murphy KM, Shaw A, et al. Humerus shaft fractures in young
children: accident or abuse? J Pediatr Orthop 1997;17:293-297.
JL, Sakellarides H. Radial nerve paralysis associated with fractures of
the humerus. A review of 45 cases. J Bone Joint Surg Am 1967;49:899-902.
VI. Outcome of treatment of pseudarthroses of the humerus by methods of
closed perosseous osteosynthesis by the Ilizarov technic. Sov Med
1977;10:75-79.
IV, Zhila IS, Rybachuk OI. Compression-distraction osteosynthesis in
pseudarthroses of long tubular bones. Vestn Khir Im I I Grek
1976;116:90-94.
KA, McLaughlin RE, Edlich RC, et al. Clavicular fractures and
acromioclavicular joint dislocations in lacrosse: preventable injuries.
J Emerg Med 1985;3:117-121.
FM. Fracture-separation of the proximal humeral epiphysis: a study of
cases seen at the Presbyterian Hospital from 1929-1953. Am J Surg
1956;91:627-635.
RF, Szilagyi E, Elliott JP Jr. Fracture of long bones with arterial
injury due to blunt trauma. Principles of management. Arch Surg
1969;99:315-324.
GJ, Patka P, van Mourik JC, et al. Treatment of fractures of the shaft
of the humerus accompanied by paralysis of the radial nerve. Injury
1987;18:404-406.
LJ, Flatow EL, Bigliani LU, et al. Articular geometry of the
glenohumeral joint. Clin Orthop Relat Res 1992;285:181-190.
CL, Micheli LJ. Simultaneous ipsilateral fractures of the arm and
forearm in children. Clin Orthop Relat Res 1980;153:218-222.
D, Trowbridge EA, Norris SH. The mechanism of clavicular fractures. A
clinical and biomechanical analysis. J Bone Joint Surg Br
1988;70:461-464.
RB, London MD, Hankin FM, et al. Fibrous dysplasia: an analysis of
options for treatment. J Bone Joint Surg Am 1987;69:400-409.
PJ, Mattingly DA, Pomeroy DL, et al. Intramedullary fixation of humeral
shaft fractures. J Bone Joint Surg Am 1984;66:639-646.
MJ, Hundley JM. Fractures of the humerus: a comparative study in
methods of treatment. J Bone Joint Surg Am 1955;37:681-692.
KM, Schmit-Neuerburg KP. Indications and clinical results of
electromagnetically induced alternating current stimulation of poorly
reacting pseudarthroses. Unfallchirurgie 1985;11:197-203.
B, Lidgren L, Norgren L, et al. Neurovascular injury complicating
displaced proximal fractures of the humerus. Injury 1987;18:423-425.
EA, Rockwood CA Jr. Fractures of the distal shaft of the humerus
associated with radial nerve palsy. Orthop Trans 1982;6:455.
PF, Stauffer AE, Crues JV III, et al. Saline magnetic resonance
arthrogaphy in the evaluation of glenohumeral instability. Arthroscopy
1993;9:550-559.
I, Donnan L. Posterior dislocation of the humeral head in association
with obstetric paralysis. J Pediatr Orthop 1998;18:611-615.
S, Floyd WE III, Waters PM. Posterior dislocation of the humeral head
in infancy associated with obstetrical paralysis. A case report. J Bone
Joint Surg Am 1993; 75:1370-1375.
DH, Slabaugh PB, Carlson PA. Injury to the axillary artery by a closed
fracture of the clavicle. A case report. J Bone Joint Surg Am
1980;62:1372-1374.
HK, Piscopo M. Anterior capsular redundancy of the shoulder: congenital
or traumatic? An embryological study. J Bone Joint Surg Br
1985;67:363-366.
den Broek JA, Vegter J. Echography in the diagnosis of epiphysiolysis
of the proximal humerus in a newborn infant [in Dutch]. Ned Tijdscr
Geneeskd 1988;132: 1015-1017.
der Ghinst M, De Geeter L, Thiry A. Treatment of collum and diaphyseal
fractures of the humerus using Kirschner wire nailing. Acta Chir Belg
1972;Suppl 2:105-116.
Griend RA, Tomasin J, Ward EF. Open reduction and internal fixation of
humeral shaft fractures. Results using AO plating techniques. J Bone
Joint Surg Am 1986;68:430-433.
J, Handelberg F, Casteleyn PP, et al. The rate of recurrence of
traumatic anterior dislocation of the shoulder. Int Orthop
1993;17:337-341.
JD, Rietberg M. Interposition of the tendon of the long head of biceps
in fracture separation of the proximal humeral epiphysis. Neth J Surg
1980;32:12-15.
VR, Hendrix RW, Rogers LF. Computed tomography of posterior
fracture-dislocations of the shoulder: case reports. J Trauma
1992;32:113-115.
T, Hartikainen-Sorri AL. Obstetric shoulder injury: associated risk
factors, prediction, and prognosis. Acta Obstet Gynecol Scand
1993;72:450-454.
P Jr, Koval KJ, Lehman W, et al. Salter-Harris type III
fracture-dislocation of the proximal humerus. J Pediatr Orthop
1997;6:219-222.
P, Bae D, Kadiyala R. Short-term outcomes after surgical treatment of
traumatic posterior sternoclavicular fracture-dislocations in children
and adolescents. J Pediatr Orthop 2003;23(4):464-469.
FM, Whitesides TE Jr. Acute hematogenous osteomyelitis complicating
closed fractures. Clin Orthop Relat Res 1976;117:296-302.
PA, Suchey JM. Epiphyseal union of the anterior iliac crest and medial
clavicle in a modern multiracial sample of American males and females.
Am J Phys Anthropol 1985;68:457-466.
B, Seife B, Alonso P. The apical oblique view of the clavicle: its
usefulness in neonatal and childhood trauma. Skeletal Radiol
1991;20:201-203.
GD, Friess DM, Getty PO, et al. Fracture of the proximal humerus with
injury to the axillary artery in a boy aged 13 years. J Bone Joint Surg
Br 2006;88(11):1521-1523.
GM, Riley LH Jr.,Isolated avulsion of the subscapularis insertion in a
child. A case report. J Bone Joint Surg Am 1985;67:635-636.
SJ, Blance CE, DiPietro MA, et al. Arthrography in evaluation of birth
injuries of the shoulder. J Can Assoc Radiol J 1987;38:113-115.
RA. Treatment of epiphyseal displacement and fractures of the upper
extremity of the humerus designed to assure deficit adjustment and
fixation of the fragments. Ann Surg 1908;47:706-708.
J, Haslam ET, Hutchinson RH. The surgical management of residual
deformities of the shoulder following birth injuries of the brachial
plexus. J Bone Joint Surg Am 1955;37:27-36.
MC, Evans EB. Fractures of the scapula: an analysis of 40 cases and a
review of literature. J Bone Joint Surg Am 1977;59:358-362.
DJ. The mechanisms producing fracture-separation of the proximal
humeral epiphysis. J Bone Joint Surg Br 1981;63B:102-107.
JM, Miller H, LaFerte AD. Evaluation of the “hanging cast” as a method
of treating fractures of the humerus. Am J Surg 1942;55:228-249.
B, Schmidt U, Nerlich M. Results of treatment of compartment syndrome
of the upper arm [in German]. Unfallchirurg 1991;94:231-235.
TW, Miller GJ, Vander Griend RA, et al. Reconstruction of the humerus
with an intramedullary fibular graft. A clinical and biomechanical
study. J Bone Joint Surg Br 1993;75:804-807.
Z, Goldberg I. Inferior subluxation of the humeral head after injury to
the shoulder. A brief note. J Bone Joint Surg Am 1989;71:751-753.
JB, Latta LL, Zych GA, et al. Diaphyseal fractures of the humerus.
Treatment with prefabricated braces. J Bone Joint Surg Am
1988;70:607-610.
R, Romano P, Rotolo F, et al. Intramedullary osteosynthesis: 3.
Kuntscher nailing in the humerus. Ital J Orthop Traumatol
1990;16:311-322.
BA, Pape HC, Gerich TG, et al. Functional outcome following
scapulothoracic dissociation. J Bone Joint Surg Am 2004;86A:2-8.
EJ Jr, Krieg JK, Rosen MJ. Open reduction and internal fixation of
clavicular fractures. J Bone Joint Surg Am 1981;63:147-151.
B, Poigenfurst J. Treatment of unstable fractures of the proximal end
of the humerus using elastic curved intramedullary wires [in German].
Unfallchirurgie 1987; 13:72-81.
GF, Sabetta E, Bungaro P, et al. The role of osteosynthesis in the
treatment of fractures of the humerus. Ital J Orthop Traumatol
1988;14:67-75.
JD, Flugstad DL, Teitz CC, et al. Axillary artery injury as a
complication of proximal humerus fractures. Two case reports and a
review of the literature. Clin Orthop Relat Res 1984;189:234-237.
JD, Matsen FA. Complications about the glenohumeral joint related to
the use of screws and staples. J Bone Joint Surg Am 1984;66:175-180.
