Proximal Humeral Fractures: Open Reduction Internal Fixation
fractures and occur most often as the result of a simple fall in an
older patient with osteoporosis. The proximal humerus may also be
fractured in younger patients as the result of high-energy trauma, and
evaluation and management of associated injuries to the head, spine,
chest, or other vital areas may take precedence over the shoulder
fracture.
indications for surgical versus nonoperative management of many
proximal humeral fractures. Furthermore, differences of opinion abound
regarding whether internal fixation or arthroplasty provide better
outcomes in selected fracture patterns. With the introduction of
peri-articular locked plates in the past decade, the treatment of
proximal humeral fractures has undergone a profound change.
fractures is the institution of early range of motion. Shoulder
function depends on the complex interaction of the glenohumeral and
scapulothoracic motion, as well as the interplay of 7 or more
muscle-tendon units. Soft-tissue scarring or loss of the gliding
surfaces can leave the shoulder stiff and painful and results in poor
outcomes. If a fracture of the proximal humerus is either unacceptably
displaced or too unstable to allow early motion, then operative
intervention should be considered to restore anatomy and useful
shoulder function. Whether surgery is done by open reduction and
fixation of the fracture or by prosthetic replacement depends on the
patient’s needs and expectations, fracture pattern, bone quality,
available implants, and the experience of the surgeon.
understood to treat proximal humeral fractures successfully. Fractures
of the proximal humerus occur in typical patterns that are influenced
by muscular insertions that cause predictable displacement of the
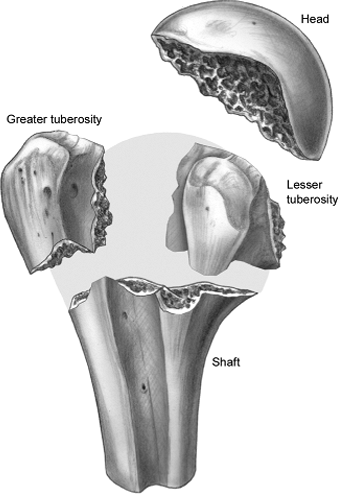
fracture fragments (Fig. 3.1). Although the
Neer classification is often used for surgical decision making,
multiple authors have shown that interobserver and intraobserver
interpretations of plain radiographs vary widely. Fractures of the
proximal humerus can involve the surgical neck and/or the tuberosities.
Also, fracture displacement affects the biomechanical function of the
shoulder
and the vascularity of the fracture fragments. The inherent stability
of the fracture is another factor affecting decision making. A fracture
is considered stable if displacement is minimal and the patient will
tolerate early functional motion. These fractures are usually treated
nonoperatively. Surgery is indicated when fracture instability prevents
early motion or when fracture displacement is sufficiently great that
functional impairment is likely.
 |
|
Figure 3.1. Drawing of the pathoanatomy of proximal humeral fractures.
|
associated with anterior shoulder dislocation, and displaced tuberosity
fragments should be reduced and fixed. Tension-band techniques with
heavy suture or wire can be utilized, or screw fixation may be
considered when comminution is minimal and bone quality is good.
Isolated lesser-tuberosity fractures are uncommon and may occur with
posterior shoulder dislocations. Large lesser-tuberosity fragments may
require open reduction and fixation if they are significantly displaced.
be nondisplaced or displaced, simple or comminuted. Displaced
surgical-neck fractures in physiologically young patients should be
treated by reduction and fixation. A number of fixation techniques have
been employed, including T-plate fixation, percutaneous pinning,
tension-band wiring, and intramedullary nailing. With the advent of
peri-articular locking plates, these methods of treatment have been
rendered obsolete (Fig. 3.2). Locked plates
dramatically increase angular stability, minimize screw toggle, and
allow early range of motion in the shoulder. Therefore, locking plates
are indicated for nearly every fracture of the proximal humerus for
which surgical treatment is necessary.
various combinations of elementary fracture patterns. Three-part
fractures generally represent the combination of surgical neck and
greater-tuberosity fractures (Fig. 3.3). For
these injuries, treatment should be based on the radiographic or
computed tomography (CT) interpretation of the fracture, such as
tuberosity or humeral-head displacement. Locking plates are ideal
implants for these
fractures because they provide stable fixation of the humeral head and a means to repair the greater or lesser tuberosities.
 |
|
Figure 3.2. Example of a displaced surgical-neck fracture in a young patient treated with locking plate fixation. A. AP and axillary lateral views of a comminuted surgical-neck fracture. B. AP, Y, and axillary views 6 months after fixation with a locking proximal-humeral plate.
|
open reduction and internal fixation for four-part fractures, and this
treatment should be considered in relatively active, young patients. It
is interesting that complications after operative repair of
valgus-impacted four-part fractures seem to be less frequent than in
other types of four-part fractures, and therefore, these
valgus-impacted injuries may be a good indication for internal
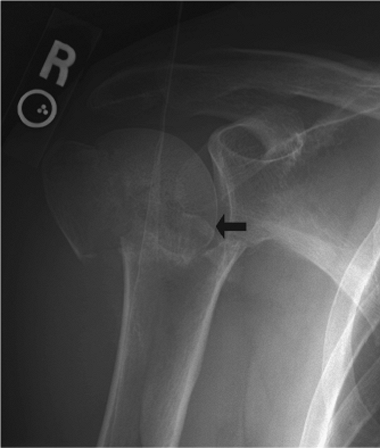
fixation. When a valgus-impacted fracture is identified, one must
carefully look for evidence of lateral displacement of the humeral-head
fragment (Fig. 3.4). If lateral displacement is
found, the medial periosteal vessels that perfuse the articular segment
may be ruptured, and avascular necrosis is more likely to result. In
the absence of lateral displacement of the humeral-head fragment, the
humeral head is likely to remain viable.
begins with a thorough assessment of the functional needs and abilities
of the patient, the presence of cognitive or physical impairments, the
fracture pattern, bone density, the patient’s expectations, and the
ability of the patient to comply with a rehabilitation program. The
goal of treatment is to
obtain
fracture union and maintain adequate function of the shoulder while
avoiding complications. The skills of the surgeon and the resources
available must also be considered.
 |
|
Figure 3.3. A three-part fracture dislocation of the shoulder following a seizure. A. AP, Y, and axillary lateral x-rays of the injury. Note the dislocation of the humeral head. B. AP and Y lateral views 4 months after open reduction and internal fixation with a locking plate.
|
understanding of the fracture geometry and morphology is essential.
Precise anteroposterior (AP) and axillary lateral radiographs of the
shoulder should be scrutinized. Occasionally, oblique, Y views or arch
views of the scapula can be helpful. If any doubt exists, a CT or
magnetic resonance imaging (MRI) scan should be obtained in
noncritically ill patients. In young patients with wide tuberosity
displacement, an MRI scan often provides useful information about the
rotator cuff. The fracture displacement should be carefully analyzed,
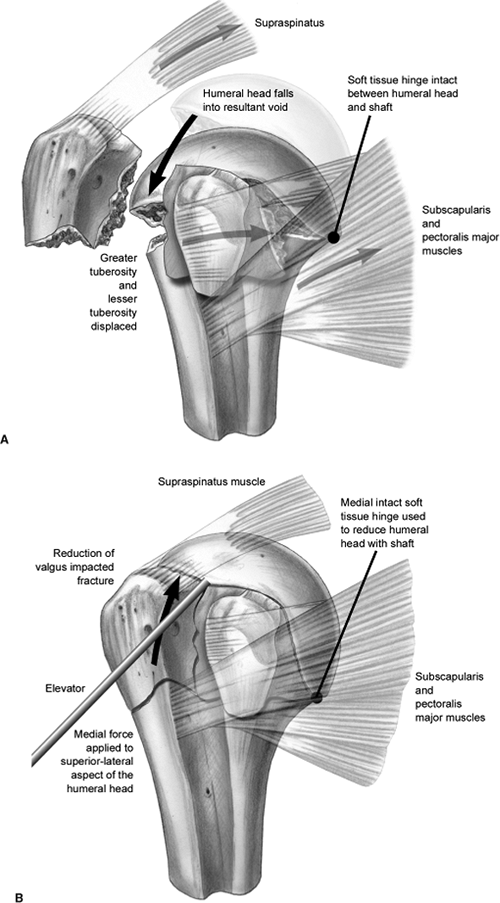
so that reduction maneuvers can be planned. For example, in a
valgus-impacted fracture, the greater tuberosity is displaced and the
humeral head falls into the resultant void. In addition, an intact,
medial, soft-tissue attachment
is
often found between the humeral head and shaft. Therefore, a
valgus-impacted fracture is reduced by applying a medial force to the
superior-lateral aspect of the humeral head and using the medial soft
tissues as a hinge (Fig. 3.5).
Once the humeral head is reduced, the greater tuberosity may be reduced
into its bed, after which it serves to maintain reduction of the
humeral head. In contrast, a humeral head that is displaced in varus
will require the opposite maneuver to reduce the articular segment.
 |
|
Figure 3.4.
A valgus-impacted fracture with more than 5 mm of lateral displacement of the humeral head. This may signify disruption of all soft-tissue attachments to the articular segment. |
is usually done through a classic deltopectoral approach. Although a
deltoid-splitting approach is normally used for isolated
greater-tuberosity fractures, the classic and splitting techniques may
be combined if the greater tuberosity is displaced posteriorly such
that reduction and fixation is difficult via the deltopectoral approach
alone. This two-incision approach may also be helpful in patients with
a large muscle envelope or significant soft-tissue swelling.
paralysis to facilitate fracture reduction. Patients should receive
prophylactic antibiotics within one hour of surgery. Multiply injured
patients should have their cervical spines cleared because of issues
with positioning of the head during surgery.
standard operating table. The patient’s torso should be at the edge of
the table, and a soft bump should be placed behind the patient’s chest
to turn the individual slightly to the side opposite the injury. This
positioning
facilitates imaging because the shoulder is slightly rotated away from
the table. A radiolucent arm and/or shoulder rest is placed along the
side of the bed. The entire upper extremity must be free to move or
manipulate during surgery.
 |
|
Figure 3.5. Drawings of reduction of a valgus-impacted fracture relying on a medial hinge.
|
 |
|
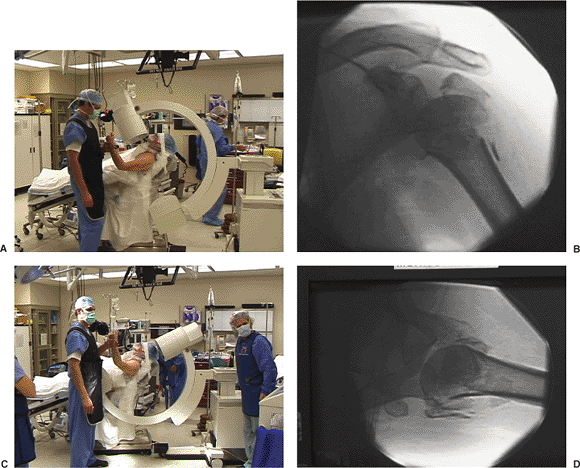
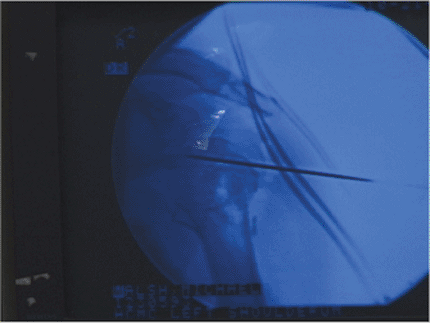
Figure 3.6. Positioning of the patient in a beach-chair position with the c-arm next to the patient’s head. A. Positioning the c-arm for AP imaging of the shoulder. B. Example of the AP image obtained. C. Positioning the c-arm for axillary lateral imaging of the shoulder. D. Example of the axillary image obtained.
|
glenoid must be possible with an image intensifier. The image
intensifier is placed parallel to the table at the patient’s head on
the injured side (Fig. 3.6). With this
arrangement, imaging in the AP and axillary planes is possible. Some
surgeons prefer to bring the c-arm from the opposite side and obtain
images in the AP and transscapular lateral planes, but this approach
does not image the humeral head quite, as well as the axillary lateral
view. In either position, trial images should be obtained prior to
prepping.
and draped. A sticky prep solution, such as DuraPrep (3M Healthcare,
St. Paul, MN), and an adherent, surgical, cover drape (Ioban, 3M
Healthcare, St. Paul, MN) facilitate draping around the shoulder.
The incision for the deltopectoral approach begins midway between the
coracoid and clavicle, and it extends distally in an oblique manner to
the deltoid insertion.
 |
|
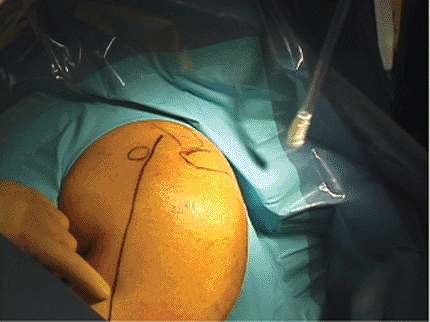
Figure 3.7. Bony landmarks outlined on the skin determine the proper placement of the skin incision.
|
 |
|
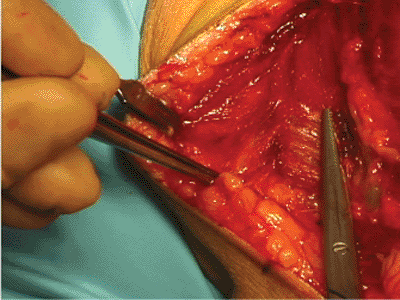
Figure 3.8.
The deltopectoral interval is opened with sharp dissection. Note the cephalic vein visible just to the right of the scissors (left shoulder shown). |
epinephrine if desired. The skin and subcutaneous tissues are divided,
and the cephalic vein is identified. The vein marks the location of the
deltopectoral interval (Fig. 3.8). The vein is
most vulnerable to injury in the proximal part of the incision. The
deltopectoral interval is deepened bluntly to the clavipectoral fascia.
During deep dissection, an important landmark is the coracoid process
and its associated strap muscles. The long head of the biceps tendon
should be identified next because it defines the rotator cuff interval.
The lesser tuberosity and subscapularis tendon lie medial to the biceps
tendon, and the greater tuberosity and supraspinatus tendon insertion
are lateral to the biceps. During the initial exposure and mobilization
of the fracture, one should keep in mind that important vascular
contributions to the articular segment are made by the ascending
(arcuate) branch of the anterior, humeral, circumflex artery that is
located along the bicipital groove. Likewise, the rotator cuff
insertions will be exposed.
Shoulder abduction during the approach relaxes the deltoid and
facilitates exposure. To facilitate exposure, reduction, and plate
placement, the anterior one third of the deltoid insertion is released
from the lateral humerus. Similarly, the upper portion of the
pectoralis major insertion on the anteromedial aspect of the humerus
may also be released. The surgeon must be cognizant of the potential
for iatrogenic injury to the axillary or musculocutaneous nerve during
surgery.
exposed. The long head of the biceps tendon is the key landmark for
identifying the tuberosities. Heavy nonabsorbable sutures are placed in
the subscapularis and supraspinatus tendons. The greater tuberosity is
often displaced posteriorly and can be retrieved with the arm abducted.
In patients with fractures more than 2 weeks old, a small, lateral,
deltoid split can be performed to retrieve and repair the greater
tuberosity; however, this type of dated injury is uncommon. Traction
sutures should be placed in the tendinous insertions to hold and reduce
fragments most securely (Fig. 3.9). Soft-tissue
attachments should be maintained, but when needed, the rotator interval
may be opened. The humeral head, as visualized via fluoroscopic
imaging, is reduced with manipulation via blunt elevators or joysticks (Fig. 3.10).
In the case of a displaced humeral head, a Kirschner (K) wire or
Schantz pin may be used as a joystick to help reduce and/or stabilize
the articular segment (Fig. 3.11).
plate with angular stable screws is utilized (Locking Proximal Humeral
Plate, Synthes USA, Westchester, PA) (Fig. 3.12). The plate is applied to the proximal lateral humerus just lateral to the biceps tendon and
held with 1 or 2 K wires. The height of the plate is evaluated with the
image intensifier to insure that the plate is not prominent superiorly (Fig. 3.13).
A standard cortical screw is placed in the oval hole in the plate,
lightly tightened and adjusted (as judged through fluoroscopy). To
insert the locking screws into the head, a triple drill guide is
threaded into the plate. A locking drill sleeve is threaded into the
plate, and based on image intensification in two planes, a guide wire
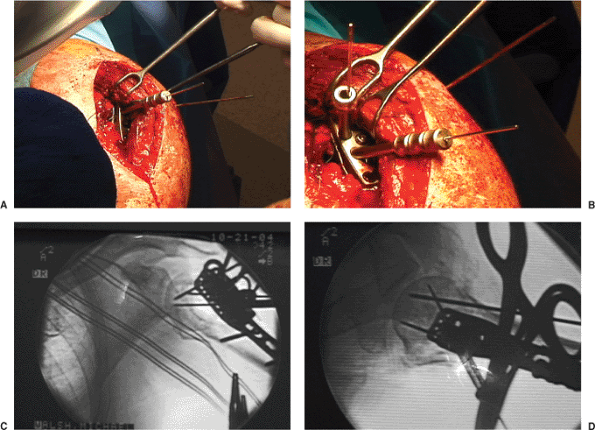
is advanced into the reduced humeral head (Fig. 3.14).
The design of the locking plate ensures that the screws appropriately
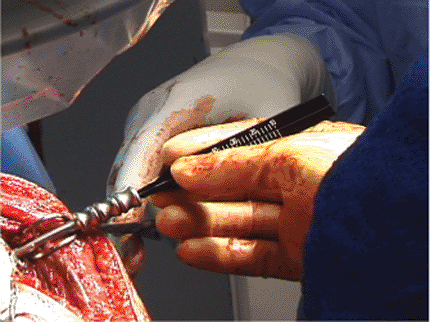
diverge within the humeral head. The screws are measured (Fig. 3.15) and inserted. The remaining screws are placed into the humeral head and shaft (Fig. 3.16).
In a recent biomechanical study, Liew et al showed that the strength of
screw fixation was related to screw position within the humeral head.
Using paired cadaveric specimens, they found that the pull-out strength
was greatest when the screws had subchondral fixation in the center of
the humeral head.
 |
|
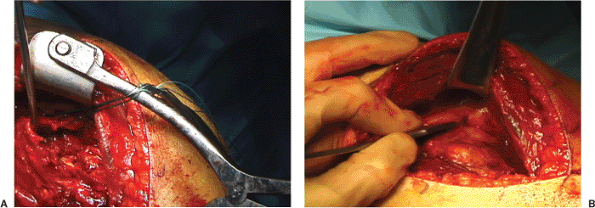
Figure 3.9. A.
With the arm abducted, a blunt retractor is used to mobilize the greater tuberosity. Here, an elevator is shown beneath the coracoacromial ligament, allowing retrieval of the greater tuberosity from the subacromial space. B. Traction sutures are placed to the greater tuberosity in the rotator cuff insertion. These facilitate reduction of the tuberosity and are later used for its reattachment. |
 |
|
Figure 3.10. A blunt elevator is used to elevate the humeral head into anatomic position. A control image taken of the c-arm is shown.
|
 |
|
Figure 3.11.
A K wire is shown maintaining the humeral head into a reduced position. The K wire can also be used to maneuver the humeral head. |
 |
|
Figure 3.12. The locking plate and drill guide are assembled.
|
 |
|
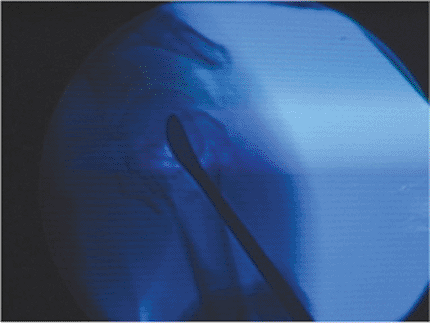
Figure 3.13.
AP c-arm image documenting correct placement of the plate on the lateral humeral shaft. To avoid subacromial impingement, the plate should not be too high. |
The sutures can be tied to the plate or to hole in the bone. It is
desirable to have sutures placed between the tuberosity and the humeral
shaft as well as in a horizontal cerclage fashion that incorporates the
plate. The tuberosities must be repaired to their anatomic position and
must be stable so that the musculotendinous unit of the rotator cuff is
restored and can tolerate early motion. While directly observing the
repair,
the surgeon brings the shoulder through a range of motion so that limits of motion are determined for postoperative exercises.
 |
|
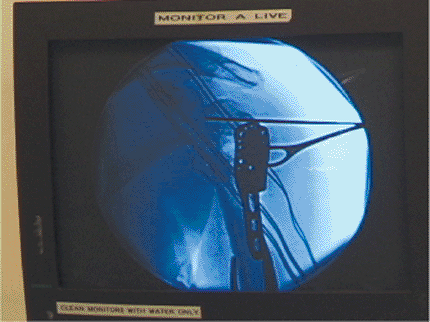
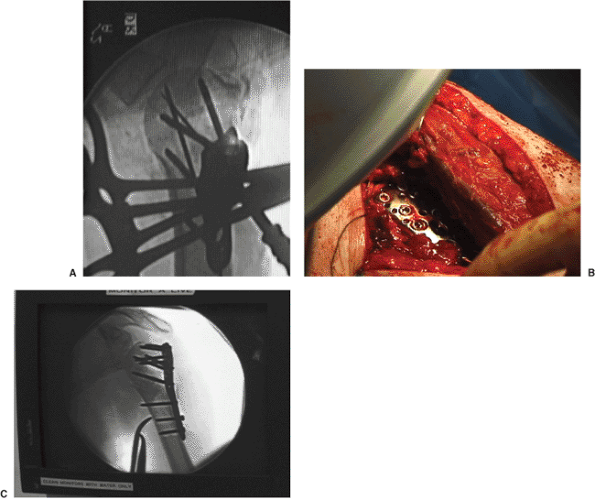
Figure 3.14. A. Intraoperative photo of the plate and the first provisional guide pins inserted into the humeral head. B. Intraoperative photo of the plate and 2 guide pins. C. Fluoroscopic AP and D. axillary lateral images documenting the correct position of the guide wires within the humeral head.
|
 |
|
Figure 3.15. Measurement of screw length using the guide pin.
|
 |
|
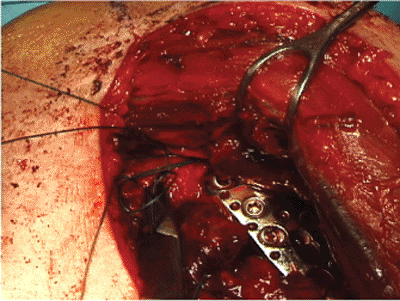
Figure 3.16. While using fluoroscopy, the surgeon inserts the remaining screws. A.
C-arm axillary view showing several screws and the guide pin for another screw. All screws are divergent and contained within the humeral head. B. Photograph of the arm showing the plate beneath the deltoid. C. AP image of the shoulder showing the final construct. |
 |
|
Figure 3.17.
Utilizing multiple sutures in the rotator cuff insertions, the surgeon repairs the tuberosities to the plate and proximal humerus. |
through imaging, of the reduction and fixation, the deltopectoral
interval is closed. Drains are not typically used.
-
To confirm adequate visualization and
reduction maneuvers, practice images with the c-arm should be taken
before the patient is prepped and draped. -
Abduction of the shoulder relaxes the deltoid and facilitates exposure of the fracture.
-
Sutures should be placed in the rotator cuff insertions to provide a means to reduce and then fix the tuberosities.
-
The ubiquitous apex-anterior angulation
of the surgical neck of the humerus is corrected by pushing toward the
floor at the fracture site while lifting up on the distal arm.
humeral fractures is focused on early movement of the extremity within
the limits of the soft-tissue repair determined at the time of surgery.
Hodgson et al found that patients who started immediate physiotherapy
had less pain and better motion compared to patients who were
immobilized for 3 weeks. Pendulum exercises are usually begun
immediately. Once the wound is healed, gentle active, assisted,
range-of-motion exercises are initiated. When the greater-tuberosity
fracture has been repaired, active abduction and external rotation
should be delayed for soft-tissue healing. After lesser-tuberosity
repair, the subscapularis must be protected from active internal
rotation or passive external rotation. In general, active motion is
begun within 4 to 6 weeks after surgery, and resistance exercises are
started in 8 to 12 postoperative weeks.
fixation of the proximal humerus fall into several broad categories
that include shoulder stiffness, osteonecrosis, and malunion
or
nonunion. Complications that are unique to internal fixation of
proximal humeral fractures include technical errors, such as inadequate
reduction, incorrectly positioned implants, screw penetration into the
joint, loss of fixation, tuberosity disruption, and nerve injury. The
use of plates with angular stability, such as blade plates or plates
with locking screws, and/or augmentation of the fracture with
polymethylmethacrylate (PMMA) or calcium phosphate cement lessens this
risk.
be partial or complete; the significance of this complication on
outcome remains controversial. Open reduction and internal fixation
with plates requires a more invasive approach and may be associated
with an increased risk of osteonecrosis. However, rigid fixation may
promote better and more rapid revascularization by creeping
substitution of the humeral head and may therefore lessen the risk of
articular collapse when osteonecrosis occurs. Wijgman et al examined 60
patients with 3- or 4-part, proximal, humeral fractures that were
managed with either plate or cerclage wire fixation at an average of 10
years after injury. Although 22 of the 60 patients (37%) had
osteonecrosis, 17 of them (77% of those with osteonecrosis) had good or
excellent functional outcomes. A correlation between the type of
fixation and the development of osteonecrosis was not found.
SC, Weinhold P, Dahners LE. Fixed-angle plate fixation in simulated
fractures of the proximal humerus: a biomechanical study of a new
device. J Shoulder Elbow Surg 2003;12:578–588.
KJ, Blair B, Takei R, et al. Surgical neck fractures of the proximal
humerus: a laboratory evaluation of ten fixation techniques. J Trauma 1996;40:778–783.
BK, Goertzen DJ, O’Brien PJ, et al. Biomechanical evaluation of
proximal humeral fracture fixation supplemented with calcium phosphate
cement. J Bone Joint Surg Am 2002;84:951–961.
AJ, Roolker W, Patt TW, et al. Open reduction and internal fixation of
three and four-part fractures of the proximal part of the humerus. J Bone Joint Surg Br 2002;84A:1919–1925.
