Physical Evaluation of the Shoulder
III – Shoulder Reconstruction > Part A – Evaluation > 29 –
Physical Evaluation of the Shoulder
by an orthopaedic surgeon. A careful physical examination can reveal a
significant amount of information about the patient’s complaint.
Shoulder pain can be due to intrinsic diseases of the shoulder joint or
pathology originating from the spine, chest, or visceral structures.
Assessment of these regions along with a detailed history is important
in the complete patient evaluation.
and can help narrow the differential diagnosis of a patient presenting
with shoulder pain. The history should include general questions about
the patient’s age, handedness, and activities, and more specific
questions about the nature of the complaint. Hand dominance can give
insight into mechanism of injury as well as determination of extent of
disability and recovery. Activities, both work and recreational, again
have important implications for cause of injury and treatment. Overhead
workers or competitive athletes will have significantly higher demands
on the shoulder compared with sedentary individuals. Age will also
provide insight into potential causes of pain, with younger patients
associated with instability and secondary impingement, and older
patients with arthritis and outlet impingement.
diagnosis of shoulder injuries. Lateral arm pain, particularly with
overhead activity, is often associated with rotator cuff pathology or
impingement. Superior discomfort, especially with cross-arm adduction,
can be associated with acromioclavicular (AC) joint pain. Deep shoulder
pain or posterior shoulder pain at the glenohumeral (GH) joint is
associated with labral pathology.
tendonitis. Neck or periscapular pain is relatively nonspecific since
many will have this secondary to abnormal compensatory scapulothoracic
(ST) movement (shrug sign).
popping, may have multiple possible causes. However, it is sometimes
possible to distinguish between subacromial crepitus (often owing to
bursitis or rotator cuff pathology) and glenohumeral clicks and pops
that may be related to labral tears or arthritis. Complaints of a
“loose” shoulder or one that “comes apart” suggest instability that is
more subtle than a frank dislocation. These may be accompanied by
reports of neurologic symptoms such as numbness, tingling, or a “dead
arm” feeling. These neurologic complaints in this context are usually
nonradicular and may be related to subtle traction on the brachial
plexus during an instability episode. Persistent pain associated with
paresthesias in a radicular distribution suggests a cervical cause. (Table 29-1)
|
TABLE 29-1 History
|
|
|---|---|
|
observe the normal bony and soft tissue contours of both shoulders,
including the scapular border, and determine any asymmetry. When
looking at the anterior view, the examiner should look for step-off
deformity of the AC joint and any bumps on the clavicle indicative of
prior fracture. Flattening of the normally round deltoid contour may
indicate an anterior shoulder dislocation or paralysis of the deltoid
muscle. A “Popeye” deformity (bulging of the upper arm) from a distally
migrated biceps can occur after biceps tendon rupture. From the
posterior view, the examiner can appreciate any atrophy of the
supraspinatus or infraspinatus muscle indicative of a compressive
neuropathy of the suprascapular nerve. Winging of the scapula in which
the medial border of the scapula moves posterior to the chest wall is
seen with long thoracic nerve injury.
side of the body with the other. Initially palpate the bony landmarks
around the shoulder starting at the sternoclavicular (SC) joint, the
clavicle, the AC joint, and the coracoid. Tenderness along these
anatomic landmarks can be indicative of arthritic changes, joint
sprains or separation, and fracture.
The
biceps tendon can also be palpated in its groove proximally.
Simultaneous palpation of bilateral biceps tendons in the groove
proximally can reveal relatively increased pain consistent with
tenosynovitis; absence would indicate proximal rupture. Tenderness
along the anterior GH joint capsule can occur with adhesive capsulitis.
range of motion to help identify side-to-side differences. If there is
a loss of active range of motion, passive motion should be evaluated.
The pattern of movement, such as an abnormal shrug sign in which
scapulothoracic motion attempts to compensate for painful glenohumeral
motion, should be noted.
-
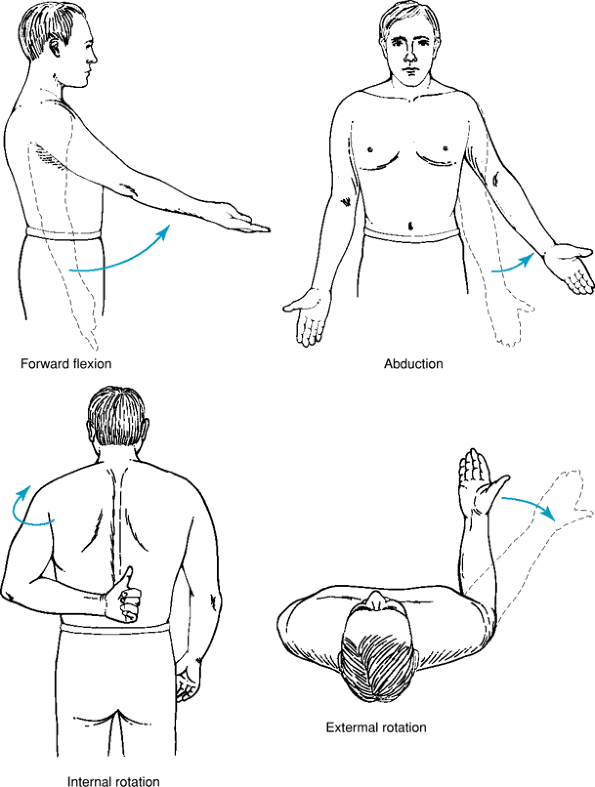
Forward flexion (normal range 150 to 180 degrees).
-
Abduction (normal range 170 to 180 degrees).
-
External rotation
-
with the elbow at the side (normal range 30 to 60 degrees)
-
With the arm abducted 90 degrees (normal range 70 to 90 degrees)
-
-
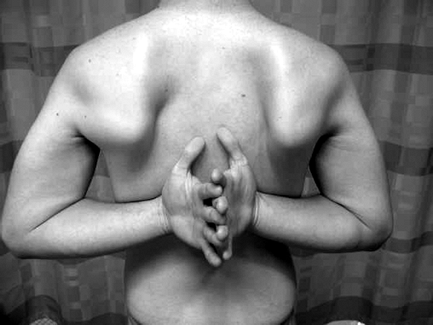
Internal rotation
-
(measured by height reached behind the back with the thumb, normal range thoracic level 4 to 8) (Fig. 29-2)
-
With the arm abducted 90 degrees (normal 30 to 60 degrees)
-
the arm abducted 90 degrees should be symmetric. It is common that
there is a relative lack of internal rotation of the dominant arm.
loss or inhibition of muscle activity, most likely owing to impingement
or other rotator cuff pathology. Pain with forward flexion and
abduction but maintained passive external rotation suggests impingement
or rotator cuff pathology. A global loss of motion (forward
flexion/abduction plus internal rotation plus external rotation)
suggests arthritis or adhesive capsulitis. Loss of external rotation
past neutral in the context of recent trauma suggests a posterior
dislocation.
-
Supraspinatus is tested with shoulders in
90 degrees of abduction. Both the “empty can” (thumbs down) and “full
can” test (thumbs up) activate the supraspinatus; the empty can test
may also trigger impingement as the greater tuberosity passes under the
coracoacromial arch. -
Teres minor/infraspinatus (external
rotators) are tested with shoulders in neutral abduction/adduction and
elbow in neutral rotation and flexed to 90 degrees. -
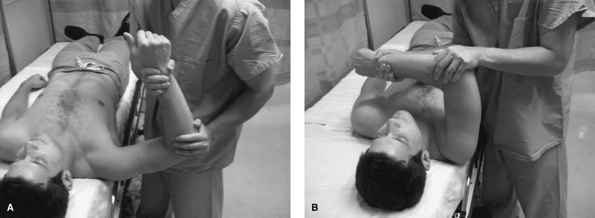
Subscapularis (lift-off test or belly-press test):
-
Belly press test: The patient presses the
hand against the stomach with the elbow brought in front of the body
and the wrist straight. Inability to maintain the elbow in front
demonstrates weakness of the upper portion of the subscapularis. (Fig. 29-3) -
Lift-off test: With the patient’s back of the hand touching his or her lower spine, the hand is lifted off against resistance (Fig. 29-4), testing the lower portion of the subscapularis.
-
pathology. The Speed test is performed by resisting forward elevation
from 90 degrees with the arm in neutral abduction/adduction and the
forearm in full supination. The Yergason test is performed with the arm
at the side and elbow in 90 degrees of flexion and resisting
supination. Pain with resisted movements during these tests is
indicative of proximal biceps tendon pathology.
subacromial impingement include the Hawkins-Kennedy and Neer
impingement signs, the painful arc sign, cross-body adduction test, and
the drop arm sign.
forward flexed by the examiner until the patient reports pain or until
full elevation is reached. Pain in the anterior or lateral part of
the shoulder in the range of 90 to 140 degrees is considered a positive test
 |
|
Figure 29-1 Range of motion.
|
 |
|
Figure 29-2 Internal rotation.
|
|
TABLE 29-2 Muscle Testing—Upper Extremity
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
Figure 29-3 Belly press.
|
 |
|
Figure 29-4 Lift off.
|
 |
|
Figure 29-5 Impingement—Neer.
|
 |
|
Figure 29-6 Impingement—Hawkins.
|
then internally rotated. The end point of rotation is when the patient
feels pain or when rotation of the scapula is felt. Pain with internal
rotation is a positive sign.
plane until full elevation is reached, and then the arm is brought down
in the same arc. The test is considered positive if the patient has
pain between 60 and 120 degrees of elevation.
adducted across the body by the examiner. The test is considered
positive with pain produced by adduction.
slowly reverse the motion. If the arm is dropped suddenly or the
patient has pain, the test is considered positive.
|
TABLE 29-3 Diagnostic Value of Clinical Tests for Impingement
|
||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
anterior posterior (SLAP) lesions. The goal is to load the biceps
tendon and transmit the force to the biceps anchor at the superior
labrum. It is performed with the arm in 10 degrees of adduction, 90
degrees of forward flexion, and thumb pointing to the floor. Forward
elevation is resisted in this plane and pain is assessed. If the
patient has pain that is resolved with supination of the arm, the test
is considered positive. Studies in the literature have shown this test
to be sensitive but not specific.
used to evaluate for posterior-superior labral tears. The patient is
positioned supine, and the arm is abducted to 90 to 120 degrees and
externally rotated. This generates internal impingement of the
posterior-superior rotator cuff against the
posterior-superior glenoid rim and labrum. Posterior pain at the GH joint line is positive.
anterior, posterior, inferior, or multidirectional. The direction of
the instability is important to determine because of the treatment
implications. When assessing for instability, the examiner should test
for generalized joint laxity with thumb to forearm flexibility or
forearm recurvatum. Instability is tested by several tests.
 |
|
Figure 29-7 Crank.
|
with the shoulder in 90 degrees of abduction and the elbow in 90
degrees of flexion, the shoulder is externally rotated. Patients with
anterior instability will have a feeling of possible anterior shoulder
dislocation, subluxation, or pain with this maneuver. For posterior
instability the arm is adducted, internally rotated, and a posterior
force is applied. If pain is elicited, this may signal a posterior
labral tear.
is performed with the shoulder in 90 degrees of abduction and 90
degrees of elbow flexion. The examiner loads the humeral head into the
glenoid and translates it anteriorly and posteriorly. This test is
graded based on the amount of translation of the humeral head on the
glenoid. Translation is 1+, 2+, or 3+ (1+, humeral head to the rim; 2+,
humeral head over the rim and reduces by itself; 3+, the humeral head
dislocates and does not reduce).
 |
|
Figure 29-8 Apprehension.
|
is performed with the arm to the side, and inferior translation of the
humeral head is assessed from the acromion. Typically, inferior
translation is maximized with internal rotation of the arm. Translation
is graded based on the amount of translation (1+, <1 cm of
translation; 2+, 1 to 2 cm of translation; 3+, >2 cm of
translation). When patients have a large sulcus sign, the examiner
should consider the diagnosis of multidirectional instability.
Alternatively, a significant SLAP tear may result in clinically evident
inferior translation.
is assessed by bringing the arm into 90 degrees of forward flexion,
internal rotating, and applying a posterior force. This may elicit pain
or apprehension, and posterior translation of the humeral head may be
appreciated. If there is pain that is relieved by bringing the arm into
90 degrees of abduction, there may be a posterior labral tear (Kim
test).
include an assessment of the cervical spine. Cervical radiculopathy can
present as shoulder pain and must be evaluated. Range of motion of the
cervical spine and a motor
and sensory evaluation of the cervical roots and dermatomes is needed for completeness.
mostly over the trapezial region, whereas pain due to primary shoulder
pathology is typically located over the deltoid. The Spurling test and
Lhermitte test can help delineate nerve root compression. The Spurling
test involves extending, laterally flexing, and rotating the neck to
the affected side with axial compression. This causes narrowing of the
neural foramina and produces nerve root compression. The Lhermitte test
involves vertical pressure on the head, which causes a shocklike
sensation in the affected extremity.
 |
|
Figure 29-9 Load and shift.
|
 |
|
Figure 29-10 Sulcus.
|
 |
|
Figure 29-11 A and B: Posterior instability—Kim test.
|
of the patient. Evaluate the neck (Spurling, Lhermitte) and palpate the
shoulders (SC, AC, biceps tendon). Have the patient go through
bilateral active forward flexion, abduction, and external rotation.
Note range of motion and if there is any dyskinesis (shrug sign,
painful arc test). If there is a lack of active motion in a plane,
evaluate passive range of motion. Perform Neer and Hawkins impingement
tests. Test resisted abduction. Test cross-arm adduction. Test for the
O’Brien sign. Test Speed and Yergason. Test active internal and
external rotation. Perform belly press test. Have patient turn around
and evaluate scapular position and motion with abduction and forward
flexion. Evaluate internal rotation. Evaluate lift-off test.
edge of the bed. Evaluate passive external rotation, sulcus sign, and
load and shift test. Abduct the arm to 90 degrees. Externally rotate
the arm, assessing for any apprehension and noting range of motion. If
there is apprehension, test relocation. Evaluate crank test. Evaluate
internal rotation at 90 degrees. Adduct the arm with the arm flexed 90
degrees and test posterior instability.
HB, Yokota A, Gill HS, et al. Diagnostic accuracy of clinical tests for
the different degrees of subacromial impingement syndrome. J Bone Joint Surg. 2005;87A:1446–1455.
