Peribulbar Block
Editors: Chelly, Jacques E.
Title: Peripheral Nerve Blocks: A Color Atlas, 3rd Edition
Copyright ©2009 Lippincott Williams & Wilkins
> Table of Contents > Section
II – Single-Injection Peripheral Blocks > C – Miscellaneous Blocks
> 17 – Peribulbar Block
II – Single-Injection Peripheral Blocks > C – Miscellaneous Blocks
> 17 – Peribulbar Block
17
Peribulbar Block
Didier Sciard
Anterior eye segment surgery—cataract, trabeculectomy; posterior eye
segment surgery—vitreoretinal surgery; conjunctival surgery, scleral
buckle.
Inferotemporal orbit injection—third inferolateral border of the orbit;
superonasal orbit injection—third superomedial border of the orbit.
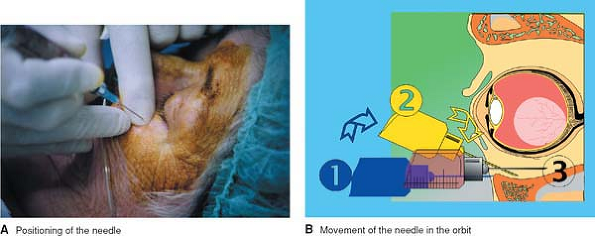
For an inferotemporal periconal injection, the needle is introduced
perpendicular to the skin. After contact with the bony rim, the needle
is moved slightly in the cranial direction to lose this bone contact,
angled 30°, and introduced another 5 mm to a new periosteum contact.
The needle is then moved back to the perpendicular position and
progressively inserted to its full extent. After a negative blood
aspiration, 6 to 8 mL of local anesthetic solution is injected. A good
sign is a relative protrusion of the eye with a downward movement of
the superior eyelid during the injection. Ocular tonicity must be
checked continuously during the procedure (Fig. 17-1).
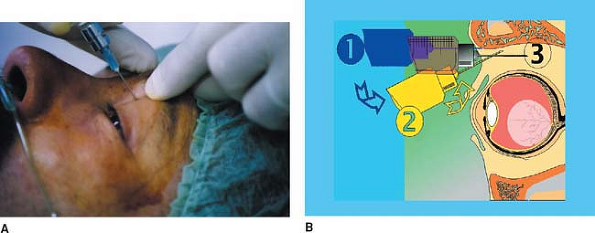
For a superonasal periconal injection, the technique is
similar to the one described for the inferotemporal injection. The
needle is moved slightly in the caudal direction, and 2 to 4 mL of
local anesthetic solution is injected (Fig. 17-2).
similar to the one described for the inferotemporal injection. The
needle is moved slightly in the caudal direction, and 2 to 4 mL of
local anesthetic solution is injected (Fig. 17-2).
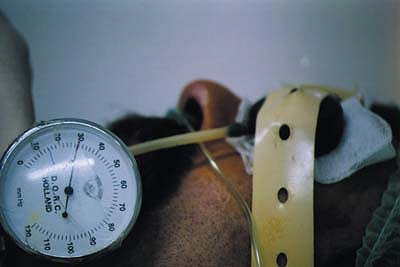
After these injections, the globe is compressed for 5 to
10 minutes with a special device such as a Hoonan balloon. The
low-pressure cuff allows for ocular compression of less than 30 mm Hg (Fig. 17-3).
10 minutes with a special device such as a Hoonan balloon. The
low-pressure cuff allows for ocular compression of less than 30 mm Hg (Fig. 17-3).
P.170
 |
|
Figure 17-1. Inferotemporal periconal injection.
|
Evaluation of the Block
The potency of the motor block is evaluated using the
akinesia score: the patient is asked to open his or her eye (0 to 2),
to look up (0 to 2), to look down (0 to 2), and to move laterally on
one side (0 to 2) and on the other side (0 to 2). The total score
varies from 0 to 10. A block with a score of at least 8 is considered
satisfactory. The quality of the sensory blockade can be verified by
testing conjunctival sensitivity to touch or topical drugs.
akinesia score: the patient is asked to open his or her eye (0 to 2),
to look up (0 to 2), to look down (0 to 2), and to move laterally on
one side (0 to 2) and on the other side (0 to 2). The total score
varies from 0 to 10. A block with a score of at least 8 is considered
satisfactory. The quality of the sensory blockade can be verified by
testing conjunctival sensitivity to touch or topical drugs.
Complications
Ocular Perforation
Patients with large eyes are at an increased risk of
ocular perforation. In addition, in patients with a small orbital
cavity, the risk of ocular perforation is especially increased during
the superonasal injection.
ocular perforation. In addition, in patients with a small orbital
cavity, the risk of ocular perforation is especially increased during
the superonasal injection.
 |
|
Figure 17-2. Superonasal periconal injection.
|
P.171
 |
|
Figure 17-3. Low-pressure cuff.
|
Retrobulbar Hemorrhage
The risk for retrobulbar hemorrhage is increased in
elderly patients treated with steroids or aspirin and other
nonsteroidal anti-inflammatory drugs.
elderly patients treated with steroids or aspirin and other
nonsteroidal anti-inflammatory drugs.
Infection
The risk of infection after peribulbar block is minimal
because of the bacteriostatic property of the local anesthetic solution
and the use of aseptic technique.
because of the bacteriostatic property of the local anesthetic solution
and the use of aseptic technique.
Paresis
There is a slight risk of paresis of the upper eyelid with the superonasal approach.
Central Nervous System Side Effects
The risk of injection into the optic nerve sheath
(resulting in unexpected intradural injection, requiring general
anesthesia and tracheal intubation) or intravascular injection
(producing centrally mediated cardiovascular or respiratory depression)
is minimal with this approach.
(resulting in unexpected intradural injection, requiring general
anesthesia and tracheal intubation) or intravascular injection
(producing centrally mediated cardiovascular or respiratory depression)
is minimal with this approach.
-
The peribulbar block allows for most
types of intraocular surgery to be performed with a lower risk of
neural optic damage or intradural or intravascular injection than the
retrobulbar block. Use of the retrobulbar block should be reserved to
ophthalmologists. -
Sedation: The use of sedation before
injection is indicated to decrease anxiety and minimize recall. During
the procedure, patient cooperation is important, and therefore
excessive use of sedative drugs is not advisable. However, in patients
with major respiratory or neuromuscular diseases, sedation is
contraindicated. In this instance, the use of topical anesthesia with a
transconjunctival injection represents an alternative. -
Needle: (a) The normal bevel increases
the penetration power of the needle (less painful) and does not
increase the risk of ocular perforation. In addition, in case of
perforation, the damage done to the globe is decreased. (b) The length
of the needle must be less than 30 mm to lower the risk of neural optic
damage (unexpected retrobulbar injection). -
Drugs: Mepivacaine 2% results in a good
motor block and can be used alone instead of the mixture of lidocaine
and bupivacaine. When a prolonged sensory block is
P.172
required
(vitreoretinal surgery), 1 mg/kg clonidine can be added to the solution
of local anesthetic. Ropivacaine 0.75% can also be used as a
long-acting local anesthetic. -
Medial canthus (caruncula) approach: This
approach can be used to complement an incomplete peribulbar block. The
puncture is done just above the caruncula, in the semilunaris fold. The
needle is directed primarily to the nose and is inserted perpendicular
to the eye with a constant pressure, producing a slight attraction of
the eye. During the introduction of the needle, a loss of resistance is
indicated by the eye returning to a central position. After a negative
blood aspiration, 6 to 10 mL of the local anesthetic solution is
injected. The caruncula approach can also be used as the sole approach
for a peribulbar block. However, there is an increased risk of paresis
of the medial rectus muscle, which is temporary most of the time but
requires physical therapy in a few cases.
Suggested Readings
Brydon
CW, Basler M, Kerr WJ. An evaluation of two concentrations of
hyaluronidase for supplementation of peribulbar anaesthesia. Anaesthesia 1995;50:998–1000.
CW, Basler M, Kerr WJ. An evaluation of two concentrations of
hyaluronidase for supplementation of peribulbar anaesthesia. Anaesthesia 1995;50:998–1000.
Crawford M, Kerr WJ. The effect of hyaluronidase on peribulbar block. Anaesthesia 1994;49:907–908.
Davis
DB II, Mandel MR. Efficacy and complication rate of 16,224 consecutive
peribulbar blocks: a prospective multicenter study. J Cataract Refract Surg 1994;20:327–337.
DB II, Mandel MR. Efficacy and complication rate of 16,224 consecutive
peribulbar blocks: a prospective multicenter study. J Cataract Refract Surg 1994;20:327–337.
Dick B, Jacobi FK. Cataract surgery and anticoagulation current status. Klin Monatsbl Augenheilkd 1996;209:340–346.
Gomez RS, Andrade LOF, Rezende Costa JR. Brainstem anaesthesia after peribulbar anaesthesia. Can J Anaesth 1997;44:732–734.
Haimeur C, Syah S, Driss N, et al. Peribulbar anesthesia for cataract surgery. Cah Anesthesiol 1995;21:16–20.
Hamilton RC. Complications of retrobulbar and peribulbar blocks. Reg Anesth 1990;15:106–107.
Hamilton RC. Techniques of orbital regional anaesthesia. Br J Anaesth 1995;75:88–92.
McCombe M, Heriot W. Penetrating ocular injury following local anaesthesia. Aust N Z J Ophthalmol 1995;23:33–36.
Ripart
J, Lefrant JY, de La Coussaye JE, et al. Peribulbar versus retrobulbar
anesthesia for ophthalmic surgery: an anatomical comparison of
extraconal and intraconal injections. Anesthesiology. 2001;94:56–62.
J, Lefrant JY, de La Coussaye JE, et al. Peribulbar versus retrobulbar
anesthesia for ophthalmic surgery: an anatomical comparison of
extraconal and intraconal injections. Anesthesiology. 2001;94:56–62.
Ripart J, Lefrant JY, Eledjam JJ. Medial canthus (caruncle) single injection periocular anesthesia. Anesth Analg 1996;83:1234–1238.
Ripart
J, Lefrant JY, Vivien B, et al. Ophthalmic regional anesthesia: medial
canthus episcleral (sub-tenon) anesthesia is more efficient than
peribulbar anesthesia: a double-blind randomized study. Anesthesiology 2000;92:1278–1285.
J, Lefrant JY, Vivien B, et al. Ophthalmic regional anesthesia: medial
canthus episcleral (sub-tenon) anesthesia is more efficient than
peribulbar anesthesia: a double-blind randomized study. Anesthesiology 2000;92:1278–1285.
Rubin AP. Complications of local anaesthesia for ophthalmic surgery. Br J Anaesth 1995;75:93–96.
