Pediatric Hip
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > V – Pediatric Fractures and Dislocations > 47 – Pediatric Hip
47
Pediatric Hip
PEDIATRIC HIP FRACTURES
Epidemiology
-
Hip fractures are rare in children, occurring less than 1% as often as in adults.
Anatomy
-
Ossification (Fig. 47.1)
-
Proximal femur: week 7 in utero
-
Proximal femoral epiphysis: age 4 to 8 months
-
Trochanter: 4 years
-
-
The proximal femoral epiphysis fuses by age 18 years, the trochanteric apophysis by age 16 to 18 years.
-
The proximal femoral physis contributes
significantly to metaphyseal growth of the femoral neck and less to
primary appositional growth of the femoral head. Thus, disruptions in
this region may lead to architectural changes that may affect the
overall anatomic development of the proximal femur. -
The trochanteric apophysis contributes
significantly to appositional growth of the greater trochanter and less
to the metaphyseal growth of the femur. -
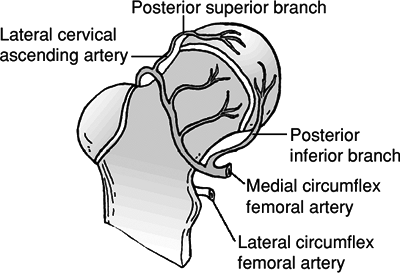
Blood is supplied to the hip by the
lateral femoral circumflex artery and, more importantly, the medial
femoral circumflex artery. Anastomoses at the anterosuperior portion of
the intertrochanteric groove form the extracapsular ring. Ascending
retinacular vessels go to the epiphysis (Fig. 47.2). -
By 3 or 4 years of age, the lateral
posterosuperior vessels (branches of the medial femoral circumflex)
predominate and supply the entire anterolateral portion of the capital
femoral epiphysis. -
Vessels of the ligamentum teres contribute little before age 8 years and approximately 20% in adulthood.
-
Capsulotomy does not damage the blood
supply to the femoral head, but violation of the intertrochanteric
notch or the lateral ascending cervical vessels can render the femoral
head avascular.
Mechanism of Injury
-
Axial loading, torsion, hyperabduction,
or a direct blow can result in a hip fracture. Severe, direct trauma
(e.g., motor vehicle accident) accounts for 75% to 80% of pediatric hip
fractures. -
Pathologic: Fracture occurs through bone cyst, fibrous dysplasia, or tumor.
-
Stress fractures: These are uncommon.
Clinical Evaluation
-
The patient typically presents with a shortened and externally rotated lower extremity.
-
Range of hip motion is painful with variable crepitus.
-
Swelling, ecchymosis, and tenderness to palpation are generally present over the injured hip.
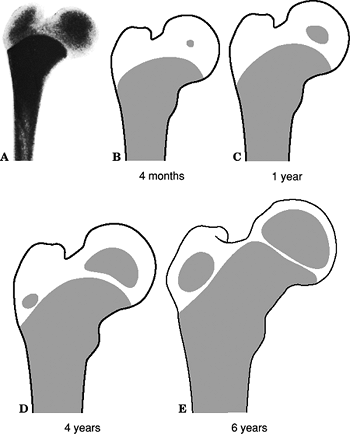 Figure
Figure
47.1. The transformation of the preplate to separate growth zones for
the femoral head and greater trochanter. The diagram shows development
of the epiphyseal nucleus in the proximal end of the femur. (A) X-ray
of the proximal end of the femur of a stillborn girl, weight 325 g.
(B–E) Drawings made on the basis of x-rays.(From Edgren
W. Coxa plana: a clinical and radiological investigation with
particular reference to the importance of the metaphyseal changes for
the final shape of the proximal part of the femur. Acta Orthop Scand 1965;84(suppl):24.) -
A careful neurovascular examination should be performed.
P.572
Radiographic Evaluation
-
Anteroposterior (AP) views of the pelvis
and a cross-table lateral view of the affected hip should be obtained,
with the leg extended and internally rotated as far as is tolerable by
the patient. -
Developmental coxa vara should not be
confused with hip fracture, especially in patients <5 years of age.
Comparison with the contralateral hip may aid in the distinction. -
Computed tomography may aid in the diagnosis of nondisplaced fractures or stress fractures.
![]() Figure
Figure
47.2. Arterial supply of the proximal femur. The capital femoral
epiphysis and physis are supplied by the medial circumflex artery
through two retinacular vessel systems: the posterosuperior and
posteroinferior. The lateral circumflex artery supplies the greater
trochanter and the lateral portion of the proximal femoral physis and a
small area of the anteromedial metaphysis.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
A radioisotope bone scan obtained 48 hours after injury may demonstrate increased uptake at the occult fracture site.
-
Magnetic resonance imaging may detect occult fractures within 24 hours of injury.
P.573
Classification
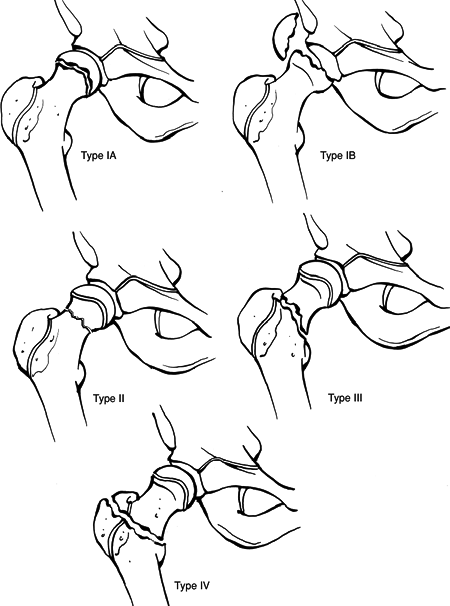
Delbert Classification of Pediatric Hip Fractures (Fig. 47.3)
| Type I: | Transepiphyseal fracture |
|
|
| Type II: | Transcervical fracture |
|
|
| Type III: | Cervicotrochanteric fracture |
|
|
| Type IV: | Intertrochanteric fracture |
|
P.574
Treatment
 |
|
Figure
47.3. Delbet classification of hip fractures in children. Type I, transepiphyseal, with (Type IB) or without (Type IA) dislocation from the acetabulum; Type II, transcervical; Type III, cervicotrochanteric; and Type IV, intertrochanteric. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
| Type I: | Closed reduction with pin fixation is indicated, using threaded pins in an older child and smooth pins in a younger child. Open reduction and internal fixation may be necessary if the fracture is irreducible by closed methods. |
| Type II: | Nondisplaced: The choice is abduction spica cast versus in situ pinning; these fractures may go on to coxa vara or nonunion. Displaced: Closed reduction and pinning (open reduction if necessary) are indicated; transphyseal pinning should be avoided. |
| Type III: | Nondisplaced: Traction is indicated, then spica cast versus immediate abduction spica versus in situ pinning. Displaced: Open reduction and internal fixation are recommended, with avoidance of transphyseal pinning. |
| Type IV: | Two to 3 weeks of traction are indicated, then abduction spica for 6 to 12 weeks. Open reduction and internal fixation may be necessary for unstable fractures or if one is unable to achieve closed reduction. |
P.575
Complications
 |
|
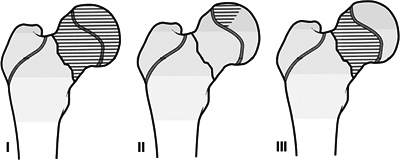
Figure 47.4. Three types of osteonecrosis.
(From Ratliff AHC. Fractures of the neck of the femur in children. J Bone Joint Surg Br 1962;44:528.)
|
-
Osteonecrosis: The overall incidence is
40% after pediatric hip fracture. This is directly related to initial
fracture displacement and fracture location. Ratliff described three
types (Fig. 47.4):Type I: Diffuse, complete head involvement, and collapse; poor prognosis (60%) Type II: Localized head involvement only; minimal collapse (22%) Type III: Femoral neck involved only; head sparing (18%)
-
Premature physeal closure: The incidence
is ≤60%, with increased incidence with pins penetrating the physis. It
may result in femoral shortening, coxa vara, and short femoral neck.
The proximal femoral epiphysis contributes to only 15% of growth of the
entire lower extremity. The presence of premature physeal closure in
association of osteonecrosis may result in significant leg length
discrepancy. -
Coxa vara: The incidence is 20%, usually
secondary to inadequate reduction. Open reduction and internal fixation
are associated with a reduced incidence of coxa vara. -
Nonunion: The incidence is 10%, primarily
owing to inadequate reduction or inadequate internal fixation. It may
require valgus osteotomy with or without bone graft to achieve union.
P.576
DISLOCATION OF THE HIP
Epidemiology
-
More common than hip fractures.
-
Bimodal distribution: The incidence is
greater between 2 and 5 years, owing to joint laxity and soft pliable
cartilage, and between 11 and 15 years of age as athletic injuries and
those associated with vehicular trauma become more common. -
Posterior dislocations: These occur ten times more frequently than anterior dislocations.
Mechanism of Injury
-
Younger patients (age <5 years): may occur with relatively insignificant trauma such as a fall from a standing height.
-
Older patients (>11 years): These
injuries tend to occur with athletic participation and vehicular
accidents (bicycles, automobiles, etc.). In this age group, there is a
higher association with acetabular fractures. -
Posterior dislocations are usually the
result of an axial load applied to a flexed and adducted hip; anterior
dislocations occur with a combination of abduction and external
rotation.
Clinical Evaluation
-
In cases of posterior hip dislocation,
the patient typically presents with the affected hip flexed, adducted,
and internally rotated. Anterior hip dislocation typically presents
with extension, abduction, and external rotation of the affected hip. -
A careful neurovascular examination is
essential, with documentation of integrity of the sciatic nerve and its
branches in posterior dislocations. Femoral nerve function and limb
perfusion should be carefully assessed in anterior dislocations. This
examination should be repeated after closed reduction. -
Ipsilateral femur fracture often occurs and must be ruled out before hip manipulation.
Radiographic Evaluation
-
AP views of the pelvis and a lateral view
of the affected hip should be obtained. Pain, swelling, or obvious
deformity in the femoral region is an indication for femoral
radiographs, to rule out associated fracture. -
Fracture fragments from the femoral head
or acetabulum are typically more readily appreciated on radiographs
obtained after reduction of the hip dislocation because anatomic
landmarks are more clearly delineated. -
Following reduction, computed tomography
should be obtained to delineate associated femoral head or acetabular
fracture, as well as the presence of interposed soft tissue.
Classification
P.577
Treatment
Nonoperative
-
Closed reduction using conscious sedation may be performed for patients presenting less than 12 hours after dislocation.
-
Skeletal traction may be used for
reduction of a chronic or neglected hip dislocation, with reduction
taking place over a 3- to 6-day period and continued traction for an
additional 2 to 3 weeks to achieve stability.
Operative
-
Dislocations more than 12 hours old may
require reduction with the patient under general anesthesia. Open
reduction may be necessary, if irreducible, with surgical removal of
interposing capsule, inverted limbus, or osteocartilaginous fragments. -
Open reduction is also indicated in cases of sciatic nerve compromise in which surgical exploration is necessary.
-
Hip dislocations associated with
ipsilateral femoral shaft fractures should initially be addressed with
reduction of the dislocation. If manipulative closed reduction is
unsuccessful, skeletal traction may be applied to the trochanteric
region to allow control of the proximal fragment. Internal or external
fixation of the femoral shaft fracture may then be performed.
Occasionally, operative fixation of the femoral shaft fracture is
necessary to achieve stable reduction of the hip. -
Postoperatively, the patient should be placed in skeletal traction or spica cast for 4 to 6 weeks to achieve hip stability.
Complications
-
Osteonecrosis (8% to 10%): This has a
decreased incidence with patient age <5 years and an increased
incidence with severe displacement and delay in reduction. -
Epiphyseal separation: Traumatic physeal injury may occur at the time of dislocation and may result in osteonecrosis.
-
Recurrent dislocation: In traumatic
cases, it may result from absolute capsular tears or capsular
attenuation. It is also associated with hyperlaxity or congenital
syndromes (e.g., Down syndrome). It may be addressed with surgical
“tightening” of the hip, with capsular repair, or with plication as
well as spica casting for 4 to 6 weeks postoperatively. -
Degenerative joint disease: This may
result from nonconcentric hip reduction secondary to trapped soft
tissue or bony fragments or from the initial trauma. Articular
incongruity secondary to associated femoral head or acetabular
fracture, or entrapped osteochondral fragments, may exacerbate
degenerative processes. -
Nerve injury (2% to 13%): Sciatic nerve
injury can occur with posterior dislocation and is typically a stretch
injury. Treatment is usually expectant, unless laceration or
incarceration in the joint is suspected. -
Chondrolysis (6%): Injury occurs at the
time of hip dislocation. Management is symptomatic treatment with
nonsteroidal antiinflammatory drugs and weight-relieving devices as
needed.