PATELLAR FRACTURES
II – FRACTURES, DISLOCATIONS, NONUNIONS, AND MALUNIONS > Patella and
Tibia > CHAPTER 22 – PATELLAR FRACTURES
result in residual patellofemoral arthralgia, quadriceps weakness,
restricted knee motion, and degenerative arthritis. The goals of
surgical treatment are to reestablish continuity of the extensor
mechanism and to restore a smooth articular surface using stable
internal fixation to permit early knee motion.
By increasing the lever arm of the quadriceps mechanism, the patella
improves extensor power, particularly during the last 30° of extension.
Maquet’s proposal that the patella reduces tibiofemoral contact
stresses has been established in experimental animal studies (7,17).
Excision of the patella can cause pain, extensor weakness, extensor
lag, knee instability, and decreased flexion arc. In one series, as
many as 90% of patients undergoing patellectomy following fracture had
continued pain, and 60% complained of instability (34).
Unexpected falls can generate violent contractions of the quadriceps
muscle as a result of the effort to regain balance, and patellar
fracture may occur. Failure of the patella secondary to an imposed
tensile load can result in a displaced transverse fracture associated
with tearing of the medial and lateral retinacula. A direct blow to the
patella transmits compressive forces that can cause
a
longitudinal, stellate, or comminuted fracture of the patella. These
injuries are usually not widely displaced because of preservation of
the quadriceps expansions. Abrasions or lacerations of the skin may be
seen in fractures caused by direct forces.
forces that produce an osteochondral fracture of the articular surface
of the medial facet of the patella or of the lateral femoral condyle.
These fragments are usually less than 1 to 2 cm in diameter, but larger
fragments occasionally occur. More recently, patellar fractures are
occasionally seen as complications of total knee arthoplasty or are
secondary to the harvest of a patella graft for reconstruction of the
anterior cruciate ligament (41).
the history and physical examination. Conspicuous findings include a
history of direct trauma or an unexpected fall, with resulting pain and
swelling about the anterior knee; inability to extend the leg actively
against gravity; and a palpable defect between the patellar fragments
and in the extensor retinacula. Nondisplaced fractures may have a
similar history but lack impressive physical findings, demonstrating
only tenderness to palpation and pain with resisted motion of the knee.
A patellar dislocation is suggested by a history of a noncontact,
valgus, external rotation injury to the knee with sudden collapse,
requiring extension of the leg to relieve the incurred pain and
deformity. Subsequent giving way, locking, catching, and swelling
suggest an osteochondral fracture.
should include anteroposterior and lateral views. A tangential patellar
view with the knee in 30° of flexion is helpful in evaluating
longitudinal fractures of the patella and in locating osteochondral
fractures following patellar dislocation. Comparison radiographs of the
opposite knee may be helpful in cases of bipartite patella, which can
usually be distinguished by its superolateral location and well-rounded
margins.
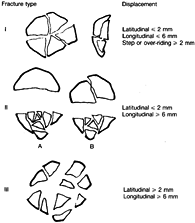
for all patellar fractures. Traditionally, they have been categorized
by degree of displacement and fracture line configuration, but this
system may fail to assess the degree of articular surface injury, which
significantly influences the outcome. Bostman classified comminuted and
displaced fractures by the degree of articular stepoff and by vertical
and horizontal displacement of major fragments in an effort to evaluate
the results of various treatment regimens (4).
displacement, the anatomic portion of the patella involved, the
fracture line configuration, the amount of comminution, and the amount
of articular incongruity. For this discussion, we recognize four groups
of patellar fractures (Fig. 22.1):
 |
|
Figure 22.1. The classification of fractures is shown. See text for details.
|
-
Transverse fractures of the patella, with and without comminution
-
Extensively comminuted and displaced patellar fractures
-
Longitudinal, marginal, and avulsion fractures of the superior and inferior poles of the patella
-
Osteochondral fractures associated with patellar dislocation.
nondisplaced—that is, one in which there is less than 2 cm of
separation, displacement, or stepoff—closed treatment is indicated if
the retinaculum is intact. Retinacular integrity can be determined by
the patient’s ability to extend the knee completely, thereby
demonstrating the intact continuity of the quadriceps mechanism.
Injection of a local anesthetic into the knee may be helpful. It is
most unusual for the extensor mechanism to be disrupted in a
nondisplaced patellar fracture. If the extensor mechanism is disrupted,
regardless of the radiographic findings of the patella, the knee should
be explored and the retinaculum and patella repaired.
However, a long leg cast made with the new lightweight fiberglass
materials may be more comfortable and prevent the downward shift and
supermalleolar irritation
that
can occur in cylinder casts. Allow 6 weeks of casting, with the knee in
a few degrees of flexion, followed by 6 weeks of progressive flexion in
a universal hinged knee brace. Quadriceps exercises with straight leg
raising can begin early, and full weight bearing is possible once
quadriceps control is established, and the fracture is healed.
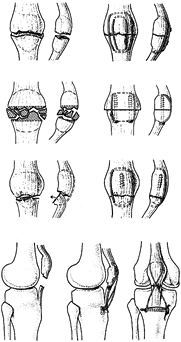
fractures with more than 2 mm of articular displacement. The specific
treatment depends on the fracture type (Fig. 22.2).
 |
|
Figure 22.2. A: A transverse fracture of the patella can be stabilized with tension band wires on the anterior surface of the patella. B:
A comminuted fracture of the patella with two large superior and inferior bony fragments can be stabilized with excision of the comminuted portion and stabilization with two 4.0 interfragmentary compression screws and a tension band. C: In a fracture of the inferior third of the patellar pole, a single 4.0 mm cancellous screw can be used in an interfragmentary compression mode and completed with a tension band wire. D: Rupture of the infrapatellar tendon can be repaired with a Tevdek suture. A figure-of-eight tension band wire protects the repair and allows for early mobilization. (From Müller ME, Allgöwer M, Schneider R, Willenegger H. Manual of Internal Fixation. New York: Springer-Verlag, 1979, with permission.) |
Fixation by a circumferential wire loop, interfragmentary screw
fixation, tension band wiring, and combinations thereof have proved
successful (4,5,13,14,24,29). Screws combined with tension band wires provide biomechanically superior fixation (8).
A circumferential wire loop (cerclage) can be placed through the soft
tissue adjacent to the patella or through holes drilled transversely or
longitudinally (Magnuson technique) in the patellar fragments. This
technique is biomechanically unsound and requires postoperative
immobilization. To eliminate postoperative immobilization and allow
early knee motion, the AO group developed tension band wiring (29).
passed around the insertions of the patellar and quadriceps tendons and
rests on the anterior surface of the patella. The wire is tightened to
close the fracture gap on the anterior surface of the patella,
potentially leaving a small gap on the posterior articular surface. A
second wire is then placed transversely inside the area of the first
wire through the proximal and distal fragments. The tension band
neutralizes the tension forces across the anterior patella so that
during flexion, quadriceps compressive forces develop at and help to
reduce and oppose the articular surface. Subsequently, to provide
better proximal and distal purchase for the tension band, two parallel
Kirschner wires (K-wires) are placed longitudinally through the
patellar fragment. Weber et al. showed the superiority of the modified
tension band wiring and Magnuson techniques in maintaining fixation of
transverse patellar fractures while allowing early motion (43).
This is now the recommended technique. Replacement of the monofilament
wire with braided cable (1 mm) provides even stronger fixation (33).
an associated tear of the medial and lateral retinacula. Repair of the
retinacula provides additional stability to the fixation.
the distal fragment, make an effort to preserve as much of the patellar
articular surface as possible. If the fracture fragments are large
enough, use interfragmentary screw fixation, which is performed and
supplemented with a tension band. If more than half of the articular
surface of the patella can be preserved, whether it is intact or
restored with interfragmentary screw fixation, then small comminuted
intraarticular fragments about the distal pole can be excised with
advancement of the patellar tendon (1,19,39).
tension band wire and its modification in treating comminuted and
displaced patellar fractures (Fig. 22.2), although
most authors recommend patellectomy when less than half of the articular surface of the patella remains intact (4).
Techniques for patellectomy include transverse primary repair,
longitudinal repair, cruciate-type repair with advancement of the
quadriceps and patellar tendon, and tubulation (12,22,32,35,37).
If patellectomy is chosen, it is important to reestablish the
continuity of the medial and lateral patellar retinacula, as well as to
ensure that tracking of the remaining tendon is normal.
tubercle osteotomy and inversions of the patella to facilitate aligning
the articular surface in comminuted fractures. All six patients he
treated this way had residual symptoms but only one had a poor result.
He believes that preservation of the patella for future reconstructive
surgery may be worthwhile in some cases.
interfragmentary screw fixation is the preferred treatment for
longitudinal, marginal, and avulsion injuries. In the case of
quadriceps or patellar tendon avulsion, supplemental cerclage wiring
can be used to diminish stresses at the repair interface. In small
marginal and longitudinal fractures that are not amenable to internal
fixation, use closed immobilization; excise the fragment or patella for
late disability and pain.
chondral flap, full-thickness chondral detachment, and osteochondral
fracture. Arthroscopy has proven useful in the treatment of these
disorders. Partial-thickness chondral injuries can be treated by
arthroscopic resection of the flap alone. Injuries that extend only to
subchondral bone require careful treatment and are discussed in Chapter 86.
lateral and two oblique radiographic views of the knee. Determine the
need for fluoroscopy, a radiolucent table, types of fixation and
instrumentation required, alternative fixation needs, and postoperative
immobilization requirements. Most patients appreciate knowing
preoperatively what to expect.
scheduled electively in outpatient surgery facilities. Preoperatively,
the knee should be splinted in extension in a well-padded knee
immobilizer to protect the soft tissues and to prevent further
articular damage.
treat the patella fracture emergently. In the polytrauma patient, the
patella fracture is a low-priority injury unless it is an open injury.
I fix all open fractures of the patella; depending on the degree of
contamination, a second surgical debridement may be required before
final skin closure.
-
Prepare and drape the patient in the routine fashion. I usually use a tourniquet.
-
Make a midline vertical incision
beginning 2 inches above the superior pole of the patella and extend it
distally to the middle of the patellar ligament. Using sharp
dissection, divide the subcutaneous tissue down to the quadriceps
retinaculum, preserving the patellar ligament periatenon. -
Raise medial and lateral skin flaps to
explore the medial and lateral extensions of the retinacular tear.
Identify the apex of the extensor retinacular tear. -
Identify the patellar fracture, separate
the two fracture fragments, irrigate the knee joint copiously, and
examine it for evidence of loose fragments and articular injury. The
anterior cruciate and the anterior horns of both menisci can be
inspected easily using this approach. Clean the fracture surfaces with
a scalpel, and dissect the retinaculum and periosteum free from the
fracture edges on the anterior border of the patella. Using gentle
curettage, remove the clotted blood and fibrous tissue from the
fracture surfaces to help ensure anatomic reduction. -
Using the 2.0 mm drill guide, place two
parallel 0.062 inch K-wires retrograde through the superior patellar
fragment. The wires will exit the superior pole of the patella and
extend through the extensor retinaculum (Fig. 22.3).
Place the wires in the midpatella to allow appropriate mechanical
stability for the tension band principle. If they are placed too close
to the articular surface, compression forces will be neutralized during
knee flexion (Fig. 22.4).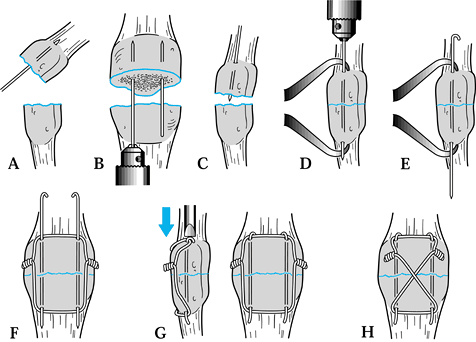 Figure 22.3. Tension band wire fixation of a patellar fracture; see text for details.
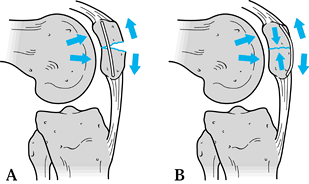
Figure 22.3. Tension band wire fixation of a patellar fracture; see text for details.![]() Figure 22.4. A:
Figure 22.4. A:
Inappropriate position of the tension band wire causes separation
fragments on the tension side of the patella during knee flexion. B:
Correct placement of the tension band wire for fixation of transverse
patellar fractures neutralizes the tension side of the patella and, on
subsequent flexion of the knee, exerts compressive forces across the
fracture at the joint surface. -
Next, use a medium-pointed reduction forceps to obtain an anatomic reduction of both fragments (Fig. 22.3D). Then, drill the previously placed K-wires through the inferior fragment to exit near the patellar ligament (Fig. 22.3E).
-
Using 18-gauge wire, with a small loop on one side,
P.729
secure the superior and inferior patellar fragments to the 0.062 inch K-wires with an oval or figure-of-eight configuration (Fig. 22.3F, Fig. 22.3G and Fig. 22.3H).
Ensure that the 18-gauge wire is in direct contact with the bone of the
superior pole of the patella and the exiting K-wire. The tendency of
allowing the quadriceps tendon and the patellar ligament to interpose
between the K-wire and the 18-gauge wire leads to loosening of the
tension band and failure of fixation. Often, small vertical incisions
are required along the line of the tendon fiber to allow the loop of
18-gauge wire to fit snugly against the exiting K-wire. Tighten the
figure-of-eight tension band wire on both the medial and lateral sides
to apply an equal distribution of tension on the wire. An alternative
is to place the tension band wire through transverse drill holes in the
patella. -
Remove the reduction forceps and bring
the knee into full extension. Palpate and inspect the articular
reduction through the medial or lateral retinacular tears. Once the
fixation is determined to be stable and anatomic, trim the excess
wires. Bend the ends of the wire proximally to a 180° loop, and drive
the wire into the bone fragment to trap the K-wire. Be certain that the
K-wires distally are long enough to prevent the 18-gauge wire from
dislodging, but not so long that they will irritate the patellar tendon. -
Next, repair the medial and lateral tears
of the quadriceps retinaculum. Begin at the apex of the tears medially
and laterally and use figure-of-eight sutures of #0 to #2 weight.
Reapproximate the tear but do not shorten it too much or the result may
be loss of knee flexion. Close the subcutaneous fat and skin. A small
drain left in the knee joint for overnight may prevent a hemarthosis. -
After surgery, apply a long leg bulky
dressing, and elevate the leg for 24 to 48 hours before the patient is
discharged from the hospital. Place the extremity in a universal hinge
brace with Velcro straps but allow no motion until the wounds are
completely healed and dry. After 10 days, begin active flexion to
between 20° and 40° and gradually advance it over the next 6 weeks. The
patient can begin isometric exercises immediately if the fixation is
secure and if he bears full weight on the site using crutches with the
hinges on the brace locked in full extension. Most fractures heal by 6
to 8 weeks, at which time protection can be discontinued and full
rehabilitation instituted.
-
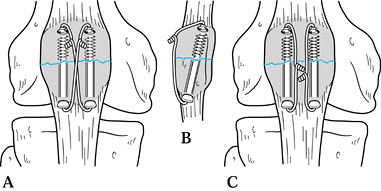
If the fracture is not conducive to
tension band wiring alone, screw fixation using 4.0 mm cancellous
screws can be done with or without a supplementary tension band wire (Fig. 22.5A, Fig. 22.5B). Screw fixation is more applicable to stellate fractures in which tension band principles are more difficult to apply.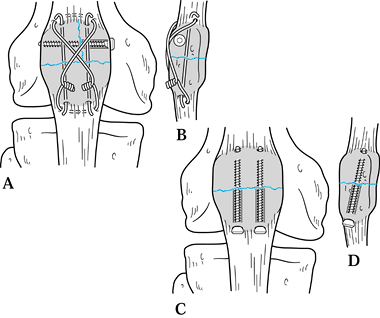 Figure 22.5. A, B: Interfragmentary compression screw and tension band wire for a comminuted fracture. C, D: Fixation with interfragmentary lag screws.
Figure 22.5. A, B: Interfragmentary compression screw and tension band wire for a comminuted fracture. C, D: Fixation with interfragmentary lag screws. -
Use the same approach for joint
irrigation and retinacular repair. Use the pointed reduction forceps
for temporary reduction before screw placement or retrograde technique
can be used as described in Fig. 22.3A, Fig. 22.3B, Fig. 22.3C, Fig. 22.3D and Fig. 22.3E. -
Using a 2.0 mm drill bit, stabilize the
two fragments using the lag technique with 4.0 mm cancellous screws
placed perpendicular to the fracture surface (Fig. 22.5C, Fig. 22.5D).
Screw fixation provides stability and compression, but it is not nearly
as reliable as when a tension band is present. I try to use a tension
band in all cases. -
Cannulated screw fixation with tension band wire techniques has gained popularity recently (Fig. 22.6).
Applying the advantage of compression screw technique and tension band
principles enhances stability and helps prevent failure of fixation at
higher loads.![]() Figure 22.6. Two different methods for combining cannulated screws with tension band wires through the screws.
Figure 22.6. Two different methods for combining cannulated screws with tension band wires through the screws. -
Stabilize the fracture using 4.0 mm cannulated screws, as described above.
-
Pass an 18-gauge wire through the holes
in the screws in a crossed wire fashion or separately for each screw.
Bend the wire twists away from the anterior skin to prevent irritation
as with all tension band techniques. Combinations of transverse or
longitudinally placed screws are acceptable, depending on the fracture
classification or direction of fracture lines. This technique does not
apply to comminuted fractures in osteoporotic bone but rather to young
patients with large fixable fracture fragments.
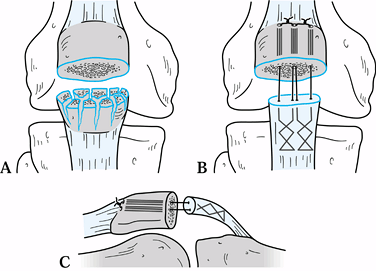
severely comminuted that internal fixation or tension band fixation
cannot be used (Fig. 22.7); in such a case, partial patellectomy is required (15).
 |
|
Figure 22.7. Marder (27) technique for partial patellectomy and repair of the patellar tendon. See text for details.
|
be reattached to the posterior aspect (articular surface) of the
remaining portion of the patella. Recent studies of the patellofemoral
contact areas and pressures in human cadavers following partial
patellectomy with reattachment
of
the patellar tendon at anterior, middle, and posterior positions on the
remaining patellar fragment have been performed. These studies have
demonstrated that regardless of the position of reattachment, there is
a decrease in patellofemoral contact area and an increase in mean
patellofemoral contact pressure following partial patellectomy (27). An anterior position of reattachment of the tendon significantly minimizes this effect, however (27). An adequate result requires strict attention to detail.
-
Prepare the extremity in the usual
fashion. Make a vertical longitudinal incision as described previously
and identify the fracture. Raise skin flaps medially and laterally to
identify the apex of the retinacular tear. -
Shell out the fragments of the inferior pole of the patella while protecting the patellar tendon.
-
On the proximal pole, remove all
articular cartilage fragmentation to provide a congruent, smooth
patellofemoral joint preventing the later migration of loose
osteochondral fragments into the patellofemoral joint. -
Using a 2.0 or 3.2 mm drill, make three
longitudinal parallel holes in the anterior third of the patella,
exiting the quadriceps tendon at the superior pole of the patella (Fig. 22.7A, Fig. 22.7B and Fig. 22.7C
). Place one hole in the center of the patella on the frontal view, and
place the medial and lateral holes parallel to and at the normal width
of the patellar tendon remaining in solid bone. -
Place two 5-0 Tevdek sutures, or
similar-weight sutures, into the patellar ligament, beginning at the
tibial tubercle; weave them in Bunnell fashion to exit the most
superior edge of the disrupted patellar tendon. Use a suture passer or
wire inserted from the superior pole of the patella through each of the
drill holes to pull the suture through the holes in the patella,
thereby securing the patellar tendon to the fractured surface of the
patella. Pass the two central sutures through the central drill hole.
Tie the two sutures to securely fasten the patellar tendon to the
fractured patella. Avoid trapping the quadriceps tendon between the
superior pole of the patella and the suture. -
Then repair the medial and lateral
retinaculum as described above in the technique for tension wire
fixation of the patella. Irrigate the wound copiously, close it in
layers over a suction drain, and place the leg in a long leg bulky
dressing with splints. -
Allow 20° of motion (0° to 20°) in a
universal brace with hinges; after 6 weeks, advance motion by 20° per
week until full flexion and extension are obtained at 12 weeks.
Encourage isometric quadriceps exercises early. Muscle electrical
stimulation may help prevent quadriceps atrophy. Full weight bearing is
possible with the hinges of the brace locked in extension.
inspected through this limited anterior approach. Use this opportunity
to look for loose osteochondral fragments and to deal with other
associated injuries.
-
The passage and recovery of K-wires and
drill points in the quadriceps mechanism and patellar tendon can be
challenging. Use a #15 blade to create a 3 to 5 mm long cruciate
incision through the soft tissues down to bone and scrape any cartilage
at the tendon attachment off bone. Use serrated drill guides to prevent
migration of wires and drills. -
Use drill points or K-wires with holes in the tip to permit passage of wires or sutures in a single step.
-
Fluoroscopic guidance is useful to less experienced surgeons or where multiple screws are placed.
-
Tension band wires are more reliable when passed through transverse drill holes or through cannulated screws.
fractures are so severe that no form of fixation will provide a
reasonable reduction. Although there have been reports of
patellofemoral pain after total patellectomy, advocates of this
procedure suggest that the degree of disability is reduced, the surgery
is less complicated, and the patients have an earlier return to
functional activities than do patients undergoing marginal fixation (15,16).
-
Approach the knee and expose the fracture as described above.
-
Shell out the comminuted fragments with a #15 blade, preserving the soft-tissue attachments as much as possible.
-
Repair the retinacular tears as described
above and carry the figure-of-eight sutures across the area of the
patellectomy. Oppose the torn surfaces firmly but do not shorten the
quadriceps mechanism any more than is necessary to obtain a good
repair. Occasionally, a Bunnell-type repair of the patellar tendon, as
described earlier for partial patellectomy, is necessary on both sides
of the tendon. -
Wound management and rehabilitation are as described above.
patellofemoral arthritis, use the following technique:
-
Expose the quadriceps mechanism and patella through an anterior midline longitudinal incision.
-
Incise the quadriceps retinaculum longitudinally in the midline over the patella with an electrocautery knife.
-
Split the patella in the midline
longitudinally by first cutting through the anterior three quarters
with an oscillating saw and then completing the fracture with an
osteotome by prying the two fragments apart. A lamina spreader can be
used as well. Avoid injury to the articular surface of the femur. -
Shell out the two fragments, preserving all soft-tissue attachments. Ensure hemostasis.
-
Repair the longitudinal split in the
quadriceps retinaculum with interrupted #1 or #2 figure-of-eight
sutures. Close the subcutaneous tissues and skin. -
Immediate protected knee motion, weight
bearing, and muscle rehabilitation are usually possible because the
quadriceps mechanism is in continuity.
the results and outcomes from treatment of patellar fractures are
retrospective studies and there is very little standardization of the
methods used to analyze results. Böaustman et al. (4)
have used the most comprehensive clinical grading scale published so
far, which includes evaluation of pain, stair-climbing, giving way, use
of aids for walking, return to work, and evaluation of range of motion,
atrophy, and presence of an effusion. They looked at 219 patients
treated nonoperatively for nondisplaced fractures. All patients had
less than 4 mm of residual articular incongruity. Fifty-four percent
had excellent results, 44% had good results, and there were only two
failures. Their results agree with those of others, showing that the
nonoperative treatment of nondisplaced fractures gives excellent
results with failure rates under 5%. Although open reduction and
internal fixation gives better results in displaced fractures, even
widely displaced fractures of the patella can be treated nonoperatively
with reasonable outcomes if surgery is contraindicated (31).
transverse fractures of the patella and more comminuted fractures,
anterior tension band wiring, particularly when combined with
cannulated screws, gives the best results. Accumulated results from
several studies show 57% excellent results, 29% good results, and 14%
poor results (4,5,22a,23a,29a,34a). Berg (3)
in 10 patients showed 70% excellent or good results based on the
hospital for special surgery knee score utilizing figure-of-eight
tension band wires placed through parallel cannulated compression
screws. Recently, heavy, nonabsorbable sutures or biodegradable,
self-reinforced polyglycolide tension bands have been used to replace
the traditionally used wire to eliminate the need for later wire
removal. These methods have proven to be equally efficacious (10,11). Smith et al. (36)
looked at the complications of operative treatment of patellar
fractures in a consecutive series of 87 fractures treated over a
five-year period. Their major complication was displacement of the
fracture of 2 mm or more which occurred in 11 fractures. They
attributed this to technical errors in five fractures and patient
noncompliance in the remainder. There were no deep infections. Two
patients had superficial infections which resolved. The high incidence
of displacement emphasizes the importance of surgical technique in
repairing displaced patellar fractures. It is important to establish,
on the operating table immediately following fixation, how much flexion
can safely be done before placing excessive stress on the repair. It is
important to make sure that patients stay within the safe range of
motion during early rehabilitation until the fracture is healed. Nine
of their patients required removal of the implants because of pain. For
that reason, consider using newer tension band techniques utilizing
cannulated screws as the profile of the wires is much lower (3). Absorbable materials for the tension band are promising as well (10,11).
Partial patellectomy with reanastomoses of the patellar tendon to the
remnant fragment produces somewhat less favorable outcomes than
restoration of the normal anatomy of the patella. Sutton et al. (38)
showed that excision of one-third of the inferior pole of the patella
resulted in an overall loss of 18° of motion. Partial patellectomy
reduces the contact area between the patella and trochlea groove. This
results in an increased incidence of anterior knee pain. However,
retention of large fragments (making up 50% or more of the patella)
improves quadriceps function compared to patellectomy and, overall, has
reasonably good outcomes of 70% or so combined good and excellent
results when a number of reports are summarized (4,29a,34a).
fractures but gives poorer results than partial patellectomy or
operative repair. Comparison is difficult, however, as these three
different treatments are applied to three entirely different fracture
patterns, each involving different levels of energy of injury. Sutton
et al. (38) showed that total patellectomy
resulted in a 40% reduction in the strength of the extensor mechanism.
This causes significant loss of ability to support body weight while
stair-climbing. Wilkinson (44) examined 31
patients with 4.5 to 13 years of follow-up after total patellectomy and
found that less than 25% of patients had an excellent result. He noted
that knee function continued to improve for approximately 3 years
before stabilizing. Einola et al. (16) followed
28 patients for an average of 7.5 years after total patellectomy and
found good results in only 6 patients. Atrophy of the quadriceps was
common, and he
found
that quadriceps power was within 75% of that of the normal knee in only
7 patients. He advised saving as much of the patella as possible. Scott
(34) found only 4 of 71 patients who were pleased with the long-term outcome of their total patellectomy. Gèagunal et al. (18) found that the results of total patellectomy could be substantially improved by advancing the vastus medialis obliquus.
practice is to fix internally the patella and retain as much patella as
possible as long as the articular surface can be reduced anatomically
or with an incongruity of less than 2 mm. If the fixation fails or the
patient has unacceptable symptoms after healing and rehabilitation,
then elective patellectomy usually gives a result similar to that of
total patellectomy done initially.
treated 79 open patellar fractures—the majority of which occurred in
patients with multiple injuries—with irrigation and debridement, open
reduction, and primary internal fixation with reconstruction of the
extensor mechanism. They performed no primary patellectomies even in
patients with severe comminution. They had only three failures of
initial fixation and one asymptomatic nonunion. Using a modified
Hospital for Special Surgery knee score they found good to excellent
results in 17 of 22 patients at an average follow-up of 3 years. In
these severe injuries, they advised thorough irrigation and debridement
with primary reconstruction of the patella and extensor mechanism
reserving total patellectomy as a salvage procedure. Torchia and
Lewallen (40) reviewed 57 open patella
fractures. They experienced somewhat less good outcomes particularly
since their rate of deep infection was 10.7% which correlated directly
with the magnitude of soft-tissue injury. They had no infections in
Type I and Type II open fractures. Their final recommendations for
treatment were similar to those of Catalano et al.
been described with each of the previously described procedures.
Certain general principles apply to all of these procedures:
-
After the repair is completed and while
the wound is still open, gently carry the knee throughout range of
motion to determine what the safe range is that does not place
excessive stress on the repair. -
Passive range of motion exercises
including continuous passive motion can begin as soon as the condition
of the wound permits. Motion helps prevent intraarticular adhesions and
tightness of the quadriceps retinaculum. -
As long as the quality of the bone and
soft tissue is good and the repair solid, most patients can begin
quadriceps isometric exercises immediately and can bear full weight in
a brace with the knee locked into full extension. -
The hinge of the brace can be adjusted to permit increasing range of motion as healing advances.
-
By 6 to 8 weeks, most patients should
have good control of their quadriceps and hamstrings, be able to raise
the leg straight against gravity, and flex the knee to 90°. If so,
full, unprotected weight bearing can begin. -
By 12 weeks, patients should be 70% to 90% rehabilitated and have good strong quadriceps function and flexion to 135°.
-
Bone repairs are slower to heal than
soft-tissue repairs and are less predictable from the standpoint of
stability. They require more cautious rehabilitation until bone union
occurs, usually between 6 and 10 weeks.
Minor degrees of loss of terminal flexion after patellar fixation have
little effect on functional outcome of the knee. Adherence to the
guidelines for rehabilitation and a cooperative patient will minimize
the risk of knee stiffness.
a well recognized, but rare, complication of inferior pole patellectomy
and reconstruction of the patellar ligament. Patients with the
condition have pain, loss of full flexion, and occasionally loss of
terminal extension. Prevent it by avoiding overshortening of the
quadriceps mechanism at the time of repair. Reconstruction requires
preoperative comparative radiographs of the contralateral flexed knee
to assess the appropriate lengthening required. The patellar tendon can
be lengthened by a Z-lengthening procedure. It is usually preferable to
a tibial tubercle osteotomy.
related to poor-quality tissues, poor fixation techniques, poor patient
compliance, and too rigorous a postoperative rehabilitation program. As
with articular reductions, the joint accommodates small degrees of gap;
however, stepoff of more than 2 mm or complete disruption may require
repeat fixation or patellectomy.
occurs most frequently with open fractures or fractures associated with
deep, neglected abrasions. Acute infections may be salvaged with
debridement, maintenance of fixation hardware, and appropriate
antibiotics. Late infections with knee-joint involvement require
aggressive debridement, removal of hardware, and an attempt at late
reconstruction. Outcomes are often poor.
fibrous union requiring no treatment. Repair or patellectomy may be required (see Chapter 30).
every effort to preserve the patella. I prefer to use cannulated screws
with supplemental tension band wire fixation. I am more likely to
perform partial or complete patellectomy in complex fractures in
sedentary middle-aged or older patients or where osteoporosis is
present. Success depends on direct supervision of the rehabilitation
program by the surgeon.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
EE. Open Reduction Internal Fixation of Displaced Transverse Patella
Fractures with Figure-Eight Wiring through Parallel Cannulated
Compression Screws. J Orthop Trauma 1997;11:573.
SC, Abhaykumar S, Elliott DS. The Use of Non-absorbable Suture in the
Fixation of Patellar Fractures: A Preliminary Report. Injury 1998;29:23.
A, Hou C, Bao J, Guo, S. Comparison of Biodegradable and Metallic
Tension-band Fixation for Patella Fractures. 38 Patients Followed for 2
Years. Acta Orthop Scand 1998;69:39.
S, Aho AJ, Kallio P. Patellectomy After Fracture. Long-term Follow-up
Results with Special Reference to Functional Disability. Acta Orthop Scand 1976;47:441.
RA, Swanson TV, Sharkey NA, Duwelius PJ. Effects of Partial
Patellectomy and Reattachment of the Patellar Tendon on Patellofemoral
Contact Areas and Pressures. J Bone Joint Surg Am 1993;75:35.
JEM. Comminuted Fractures of the Patella. Treatment of Cases Presenting
One Large Fragment and Several Small Fragments. J Bone Joint Surg 1935;17:431.
R, Vianello R. Three Cases of Patella Fracture in 1,320 Anterior
Cruciate Ligament Reconstructions with Bone-patellar Tendon-bone
Autograft. Arthroscopy 1999;15:93.