Indications for Upper Extremity Blocks
II – Single-Injection Peripheral Blocks > A – Upper Extremity > 5
– Indications for Upper Extremity Blocks
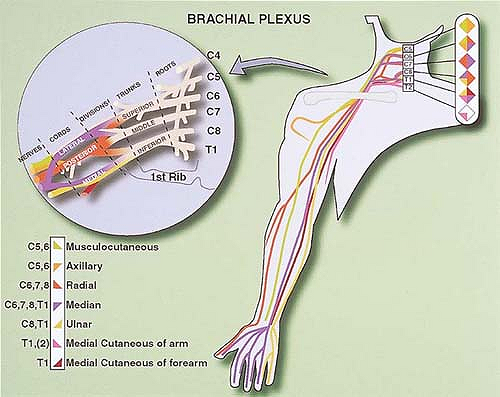
frequently based on either a block of the brachial plexus
(interscalene, supraclavicular, and classical infraclavicular) or a
block of terminal nerves (median, ulnar, radial, and musculocutaneous
nerves) at either the axilla (axillary block) or proximal part of the
humerus (high-humeral approach). The choice of the approach often
depends on the patient’s condition, the surgical indication, and the
anesthesiologist’s experience. In this regard, it is important to
recognize that for surgeries at the wrist and fingers scheduled for
less than 30 minutes, a more distal approach either at the elbow or the
wrist may satisfy all surgical requirements and allow for specific
blocking of the nerve(s) implicated as well as for a preferential
sensory block (at the wrist), preserving the motor function and
allowing the patient to move his or her fingers at the request of the
surgeon (release of trigger fingers). This “hyperselective” approach to
regional anesthesia has been proven to be safe and effective and to
facilitate rapid patient discharge after ambulatory surgery. For
example, a short procedure on the fifth finger can be performed using a
block of the ulnar nerve at the wrist. This technique is very quick to
perform, satisfies all surgical requirements, provides effective
postoperative analgesia, and allows the preservation of motor function
not only of the thumb, index finger, and middle finger, but also of the
fourth and fifth fingers. This chapter focuses on providing some
rationales for choosing the most appropriate strategy for anesthesia
and postoperative analgesia in patients undergoing upper extremity
surgery.
innervation is essential to define the minimum anesthetic and analgesic
requirements for a given indication, even if a more global approach is
chosen because of other considerations (i.e., the anesthesiologist’s
experience and the length of surgery), and even if ultimately the
surgeon determines the technique. For example, a median, ulnar, and
lateral cutaneous nerve block at the wrist represents the minimum
requirement for anesthesia for carpal tunnel release, even if an
axillary block is often performed.
|
Table 5-1. Most Common Anastomoses Between the Brachial Plexus Nerves
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
role of anatomy in performing a peripheral block of the upper
extremity: the level at which the nerves branch, anastomosis between
nerves, and global innervation.
branch and a motor branch below the axilla, with a number of
collaterals. For example, the radial nerve divides into a sensory and
motor branch above the elbow crease, with the sensory branch running
more superficially. The median and ulnar nerve divide into a sensory
and motor branch above the wrist, whereas the musculocutaneous nerve
supplies a motor branch to the biceps muscle and remains sensory
thereafter. Consequently, a radial nerve block performed in the axilla
results in a sensory and motor block of the posterolateral aspect of
the forearm. In contrast, when the radial nerve is blocked at the elbow
and below, the nerve has already divided into motor and sensory
branches. Therefore, it is important to block the radial nerve 2 to 3
cm above the elbow crease, especially when using a nerve stimulation
technique. The same is true when blocking the median nerve at the
wrist: The motor and sensory fibers are distinctly separated. In
addition, at the wrist, the median and ulnar nerves provide collateral
sensory fibers to the anterior and medial aspects of the wrist,
respectively, which originate above the wrist. Consequently, blocking
these nerves at the level of the wrist crease produces only incomplete
blocks. Wrist blocks need to be performed at least 4 cm above the wrist
crease.
plexus is frequent and may explain, at least in part, individual
variations after a nerve block. To increase the reliability of the
block, it is necessary to take this factor into consideration,
especially when considering the use of specific distal blocks (see Table 5-1, which lists the most frequent nerve anastomoses).
innervation is based on superficial distribution, it is important to
recognize that the muscular and bone innervation is not strictly
superimposed (Fig. 5-1).
The only location at which a single nerve innervates all structures is
the lateral edge of the hand and the fifth finger, both of which are
innervated by the ulnar nerve. There are some significant differences
between the superficial, muscular, and skeletal innervations. These
differences must be taken into account in determining the most
appropriate block(s) for a specific surgical procedure. Thus, the
surgical exploration of a second interdigital wound requires radial and
median blocks, whereas an ulnar block is also necessary if interosseous
muscle exploration is indicated.
the level of the brachial plexus or the individual nerves. Approaches
to the brachial plexus include the interscalene, subclavicular,
infraclavicular,
and axillary blocks. Other blocks of the upper extremity are high
humeral, elbow, wrist, and digital blocks. Each injection site is
associated with a defined probability of achieving a complete block for
a given nerve. The orientation of the plexus vis-à-vis the injection
site is an important factor to take into consideration. Although
experience is an important determinant of success, the extent of the
sensory and motor blocks also depends on the site at which the block is
performed. To maximize the correlation between the block resulting from
the use of a given approach and the surgical requirements, it is
important to choose an approach with the highest probability of
producing a complete block in the surgical territory. This can only be
achieved by gaining experience in the different approaches. Finally,
when using peripheral nerve blocks as the main anesthesia technique, it
is also important to account for all surgical requirements, such as the
prevention of tourniquet pain, especially if the tourniquet is placed
at the level of the arm and the surgery lasts more than 30 minutes.
 |
|
Figure 5-1. Upper extremity innervation.
|
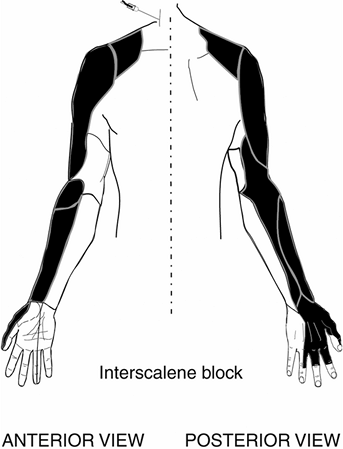
approached at the level of the trunks or roots. The anatomy of the
plexus relative to the site of injection with this approach explains
why the upper (C5-6) and middle (C7) trunks are preferentially blocked.
The lower trunk (C8-T1), which is more posterior, is often blocked
incompletely. Consequently, the shoulder and the lateral aspect of the
upper arm represent the territory with the highest probability of
block. In addition, the proximity of the phrenic nerve, the large
volume of local anesthetic usually injected (40 to 50 mL), and the
diffusion of the local anesthetic solution toward the cervical region
explain why the phrenic nerve, which runs anterior, is also almost
always blocked and why the sensory block may extend up to C2 (Fig. 5-2).
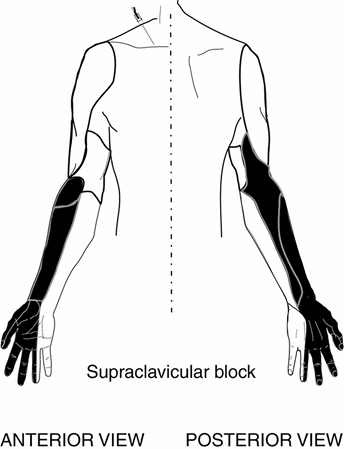
supraclavicular and infraclavicular approaches are associated with the
greatest diffusion of local anesthetic solution after a single
injection because, at these levels, the brachial plexus is the most
compact. However, supraclavicular injection preferentially blocks the
axillary, radial, and musculocutaneous nerves. Because at this level
the middle trunk is deeper, blockade of the median and, more
importantly, the ulnar nerves requires a longer onset time and is often
incomplete (Fig. 5-3).
 |
|
Figure 5-2. Anterior and posterior view of an interscalene block.
|
 |
|
Figure 5-3. Anterior and posterior view of a supraclavicular block.
|
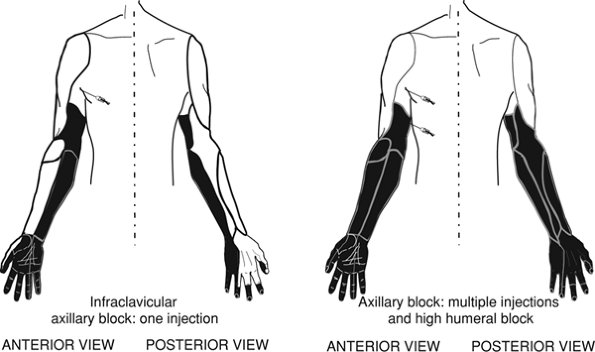
brachial plexus are individualized. As with the other sites, a single
injection does not produce complete upper limb anesthesia because (a)
the axillary and musculocutaneous nerves have already left the plexus
sheath, and (b) diffusion of the local anesthetic solution can be
incomplete. Although there is no anatomically defined separation
between the nerves, the presence of fibrous septa limits diffusion of
the local anesthetic solution. Therefore, it is difficult to achieve a
complete block with a single injection. However, the extent of the
block and the success rate can be increased by a multiple-injection
technique around the axillary artery (>90%). In this technique, the
use of a nerve stimulator greatly facilitates individual nerve
localization (Fig. 5-4).
 |
|
Figure 5-4.
Anterior and posterior view of an axillary block using one injection and an anterior and posterior view of an axillary block using multiple injections. |
vasculonervous anatomic space exists only between the brachial artery
and the median nerve. The other nerves (i.e., radial, ulnar, and
musculocutaneous) are completely separated. Therefore, such an approach
allows each nerve to be blocked according to the surgical requirement.
In practice, the extent and success rate achieved with this approach
are comparable with those in a multiple-injection axillary block.
wrist, multiple injections are required. At the elbow, six nerves need
to be blocked. Three of these nerves are superficial (musculocutaneous,
posterior cutaneous nerve of the forearm, and middle cutaneous of the
forearm) and three are deep (median, ulnar, and radial). At the wrist,
or more precisely, at the lower third of the forearm, eight nerves
provide innervation of the hand and the wrist. Four are superficial
(musculocutaneous, cutaneous middle of the forearm, superficial radial,
and posterior cutaneous nerve of the forearm) and four are deep
(median, ulnar, anterior interosseous, and posterior interosseous). At
the wrist, the use of epinephrine solutions is contraindicated.
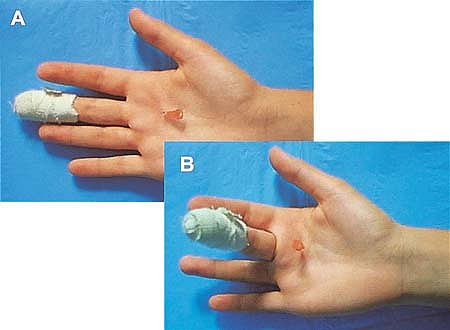
To be effective, it is necessary to block the dorsal and palmar
collateral nerves. The use of epinephrine solutions is contraindicated.
In addition, for the second, third, and fourth fingers, the palmar
collateral nerves provide innervation to the whole finger on the palmar
side and the first two phalanges on the dorsal side (Fig. 5-6).
An injection at or above the flexion tendon sheath facing the
metacarpophalangeal joint produces a block of the collateral palmar
nerves, thus providing anesthesia of three-fourths of the finger with a
single injection. The dorsal surface of the thumb is innervated by the
superficial radial
nerve,
which can be blocked through an injection in the flexor sheath. For the
fifth finger, an upper branch of the ulnar nerve innervates the entire
dorsal side. In this case, rather than two injections (one in the
sheath and one at the level of the ulnar upper branch), it is easier to
make a single injection and block the ulnar nerve 5 cm above the wrist.
 |
|
Figure 5-5. Interdigital block.
|
 |
|
Figure 5-6.
The palmar collateral nerves provide innervation to the whole finger on the palmar side and the first two phalanges on the dorsal side. |
established, the location, extent of the surgery, and expected
tourniquet duration guide the choice for the most appropriate technique.
shoulder surgery. It can be performed in the absence of general
contraindications, including (a) absolute contraindications (e.g.,
allergies to local anesthetics, infections at the injection site,
uncontrolled seizure disorder, major coagulation abnormality,
uncooperative patient); (b) relative contraindications (e.g.,
neurologic abnormalities in the territory affected by surgery); and (c)
specific contraindications (e.g., respiratory insufficiency). If the
surgical site also includes the supraclavicular region, a superficial
cervical plexus block is also required. Although interscalene block
alone is adequate for shoulder surgery, consideration should also be
given to its combination with general anesthesia, especially when the
surgery is expected to last for more than 2 hours. In these cases, the
block minimizes the requirement for opioids during surgery and the
immediate postoperative period. However, to minimize the risk for
complications (intravascular and epidural injections), it is highly
recommended that the block be performed before the induction of
anesthesia, while the patient is awake and under minimum sedation. If
the postoperative pain is expected to last more than 24 hours (rotator
cuff repair, total shoulder replacement, Bankart repair), the placement
of a catheter is indicated.
interscalene, supraclavicular, and infraclavicular blocks are equally
indicated for patients undergoing surgery below the shoulder and above
the elbow, the use of supraclavicular and infraclavicular blocks are
most likely to result in a higher success rate. However, the risk for
pneumothorax (immediate or delayed) represents a relative
contraindication of the supraclavicular block approach, especially for
ambulatory surgery. If prolonged postoperative pain control is
required, the placement of a catheter is indicated with an
infraclavicular approach.
high-humeral approach yield the best results for surgery at or below
the elbow. In contrast, interscalene blocks are not advised given their
insufficient extension in the C8–T1 territory. The use of a
supraclavicular block is possible, but the risk for pneumothorax needs
to be balanced against the specific benefit of such an approach. On the
other hand, the infraclavicular placement of a catheter for continuous
infusion may represent a viable alternative, especially in trauma cases
in which upper limb mobilization makes access difficult. Sometimes,
forearm surgery can also be performed with elbow blocks, allowing
anesthesia to be provided only to the surgical territory. This requires
an appropriate evaluation of the surgical field and knowledge of the
innervation, not only superficial but also muscular and skeletal.
However, the requirement for multiple injections may not always be well
tolerated by the patient.
performed initially at a higher level (interscalene, supraclavicular,
infraclavicular, axillary, and even high humeral).
for hand and wrist surgery. In addition, the use of a high-humeral
approach also allows the local anesthetic solution to be selected for
each nerve according to the surgical need. For example, 0.5% to 0.75%
ropivacaine may be used to block nerves directly involved with the
surgical territory for both anesthesia and immediate postoperative
analgesia, whereas 1.5% mepivacaine or lidocaine may be used to produce
a short-lasting sensory block to prevent tourniquet pain. This may also
limit the duration of the motor block while providing adequate
postoperative analgesia. Individual nerve blocks at the elbow and at
the wrist may also be indicated to complete a block in a specific
territory. Although these distal blocks have the reputation of being
more prone to inducing nerve damage, this has never been established.
|
Table 5-2. Most Common Upper Limb Procedures and Their Proposed Peripheral Blocks
|
||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
consideration. First, the tourniquet can be placed at different levels:
arm, forearm, and even fingers. Tourniquets are usually well tolerated
by the patient as long as the inflation is not too high and they are
inflated for less than 30 minutes. After that, it is necessary to block
the patient accordingly. For example, a subcutaneous injection of
lidocaine 1% along the medial aspect of the arm to block the
intercostobrachial and medial cutaneous nerves of the arm may be used
to prevent pain from a tourniquet placed at the level of the arm.
outpatient procedures. In this environment, it is important to provide
adequate postsurgical analgesia even after discharge. This requires
educating the patient about the risks and symptoms of a persistent
sensory or motor block (e.g., vascular or nerve compression). An
alternative approach can be to perform a short-duration axillary block
using mepivacaine or lidocaine completed by either an elbow or wrist
block with ropivacaine for immediate postoperative analgesia.
fingers can be performed using a hyperselective technique at the wrist
(carpal tunnel release, trigger finger release, open
reduction,
and internal fixation of the fifth finger). These blocks are better
suited for ambulatory surgery. They preserve the mobility of the
fingers, allow early discharge, and are also better accepted by
patients. However, these blocks should be restricted to procedures
involving less than 20 to 30 minutes of tourniquet time, and they
require good cooperation among the patient, the anesthesiologist, and
the surgeon.
