Hip Hemiarthroplasty
hemiarthroplasty remains one of the most commonly performed orthopedic
operations still in use today. Most hip hemiarthroplasty procedures are
carried out for femoral neck fractures in elderly patients. Over the
decades, however, hemiarthroplasty has been used for many other
indications including initial usage for osteoarthritis and as a
temporizing measure for the young patient with osteonecrosis.
Hemiresurfacing procedures have been used to provide a conservative
alternative to total hip arthroplasty in young patients. As longer-term
data have become available, the future trends in the use of hip
hemiarthroplasty and more specifically hemiresurfacing arthroplasty
remain to be seen. This chapter outlines three categories of
indications and patient types in which hemiarthroplasty is widely used.
First is the use of hemiarthroplasty for the treatment of acute femoral
neck fracture. Second, the use of hip hemiarthroplasty for indications
other than femur fracture is reviewed. Third, the history and continued
use of hemiresurfacing techniques will be analyzed. The future of this
technique for indications other than proximal femur fracture will be
written by long-term studies comparing and contrasting the
effectiveness of hemiarthroplasty with the now available long-term
results of total hip arthroplasty in these three patient groups.
the population ages, and the larger middle-age generation reaches
elderly ages, this trend will no doubt continue. Optimal treatment of
nondisplaced fractures includes internal fixation with bone screws and
has been described as successful in multiple reports. Treatment of
nondisplaced fractures with hemiarthroplasty has been associated with
increased mortality; hemiarthroplasty and should be reserved for
displaced fractures, which carry a higher rate of failure when treated
with internal fixation. Once fracture displacement has occurred, the
optimal treatment for the fracture has not been defined. Current
controversy revolves around the use of cemented versus cementless
femoral stem fixation, unipolar versus bipolar articulations, and the
use of acute total hip arthroplasty (THA) versus hemiarthroplasty.
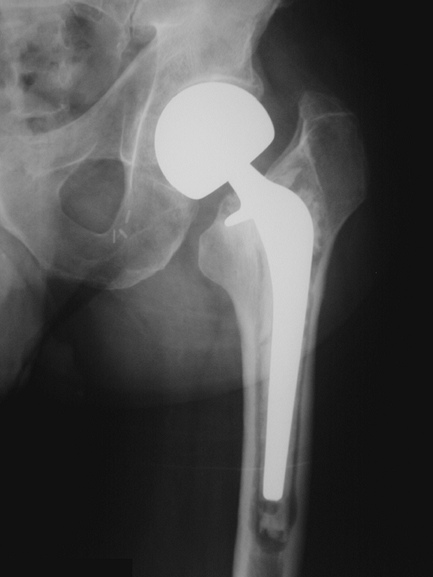
uncemented unipolar hemiarthroplasty, such as the Austin Moore
hemiarthroplasty (Fig. 11-1), have been reported to be inferior to those of other treatment options. Blomfeldt et al. 1
examined the functional outcomes of internal fixation and monoblock
uncemented unipolar arthroplasty in a series of 60 patients with an
average age of 84 years. In this group with displaced fractures, the
overall mortality and complication rates were not statistically
different between treatment options. There was a trend toward more
reoperations in the internal fixation group, however, with 33% of the
internal fixation group and 13% of the hemiarthroplasty group requiring
subsequent surgery. The quality of life outcomes measures used in this
study did demonstrate a clear superiority in those patients who lived
longer than 2 years after index surgery and had undergone internal
fixation. The authors concluded that when compared with internal
fixation, there are few data to recommend the use of a low-demand
uncemented monoblock unipolar design in elderly patients. This view has
been supported elsewhere. In a randomized controlled series, El-Abed et
al. 2 demonstrated superior
functional results in their group of patients treated with internal
fixation when compared with hemiarthroplasty. No difference in revision
rates was seen, but both the patients’ and the physicians’ perception
of outcome was better in the internal fixation group. The superiority
of internal fixation seen in some studies should be tempered by the
high rates of failure seen in other series. In the hands of experienced
trauma surgeons, the failure rate and subsequent surgical rate is as
high as 35% with only 67% of fractures achieving bony union without
avascular necrosis at 2 years following surgery. In a separate report,
nonunion is reported to occur in up to 30% of
cases
with an additional rate of avascular necrosis occurring in up to 30% of
displaced femoral neck fractures treated with internal fixation.
 |
|
Figure 11-1 Photograph of an Austin-Moore hemiarthroplasty femoral component.
|
the same implant design concluded that its use should be avoided in
younger active patients. Taken together, these data raise the question
of the utility of either internal fixation or this type of uncemented
monoblock unipolar design in the treatment of femoral neck fractures.
Instead, other more durable designs and surgical options are indicated.
reviewed the clinical and radiographic outcomes of 256 cemented
hemiarthroplasty devices inserted for acute femoral neck fracture over
a 2-year period. All of the patients were older than 65 years of age.
At an average of 3.5 years after surgery, there were two stem revisions
and six cases converted to THA for recalcitrant groin pain. They
concluded that cemented hemiarthroplasty is a viable treatment option
with good midterm results in these elderly patients. Clearly, this 97%
success far outweighs even the best reports of internal fixation or
Austin Moore–type hemiarthroplasty for displaced femoral neck
fractures. The use of a cemented device for hemiarthroplasty has been
demonstrated to provide earlier and superior pain relief and return of
function in some series. Further support for the use of a cemented
hemiarthroplasty is provided by Dixon and Bannister. 5
In a review of 53 cemented bipolar hemiarthroplasties, they report that
almost 70% of patients who were able to walk 1 mile before fracture
were able to do the same at the time of final follow-up. Moreover, only
two failures were noted in the series with 32-month follow-up. Nearly
three decades ago, Beckenbaugh et al. 6
concluded that cemented hemiarthroplasty is indicated in the treatment
of acute femoral neck fracture in the elderly. The cemented
hemiarthroplasty still appears to be the standard to which other
treatment options for displaced femoral neck fractures should be
compared.
femoral device in the treatment of femoral neck fractures has been
associated with an increased risk of death within 30 days of the
surgery. Other risk factors associated with increased mortality
following hip fracture treatment include female gender, advanced
elderly age, pre-existing heart and lung conditions, and
intertrochanteric-type fractures. It would seem prudent to weigh the
possible increased risk of mortality with the benefit of earlier
functional recovery when considering the use of cemented or cementless
devices. Unfortunately, many of the low-demand, fracture-type stems are
designed to be implanted either with or without cement, are made of
cobalt-chrome, and do not have the same porous coatings that have
proven to provide longevity in cementless applications. When these
types of stems are implanted in a cementless fashion, the results will
probably be inferior to those of cemented designs or modern porous
coated stems (Fig. 11-2).
decade, primary femoral components with long-term excellent results
should be the implant of choice when hemiarthroplasty is carried out
for fracture. Certainly, in the younger, more active patient, this
holds true.
unipolar and a bipolar prosthesis for use in hemiarthroplasty. The
theoretical decrease in articular cartilage wear and increased range of
motion with the bipolar device are frequently cited as the benefits
obtained by choosing a bipolar design. Most frequently, cost
containment is cited as the primary indication for use of a unipolar
device.
approach to the surgical treatment of a displaced femoral neck
fracture. More than 70% of people regain prefracture levels of
ambulation, and 80% report mild or no pain at 1 year following surgery.
Up to 80% survivorship at 7 years has been published with unipolar
arthroplasty. There have been indications that stiffness, groin pain,
cartilage degeneration, and acetabular protrusio are more frequent with
unipolar designs compared with bipolar designs.
In
older patients who are active, higher demands place increased stresses
on the implant and articular surfaces leading to lower satisfaction
with the surgical results in these cases.
 |
|
Figure 11-2
Radiograph of a 62-year-old man who presented with a left hip cemented hemiarthroplasty for treatment of fracture that had failed after 3 years secondary to stem loosening and subsidence. |
unipolar designs in some series. Although groin pain can and does still
occur in some patients, a large meta-analysis of the literature
revealed that 85% of patients report mild or absent pain and 85% regain
functional mobility in the first 2 years after surgery. In a separate
prospective series, no advantage to bipolar over unipolar designs was
seen in elderly patients treated for femoral neck fracture.
the bipolar design, and this remains a significant motivator for its
use. When the bipolar does dislocate, it more frequently requires open
reduction than does unipolar hemiarthroplasty. In addition, there are
several reports of wear, osteolysis, and loosening associated with the
polyethylene articulation in bipolar arthroplasty. Taking the above
noted information into account, it would appear that a well-designed
cemented or porous coated femoral stem combined with a unipolar
articulation would be the treatment of choice for the elderly,
low-activity patient with a displaced femoral neck fracture. Total hip
arthroplasty in the treatment of these fractures has been suggested to
be the ideal treatment in younger patients and may eventually prove to
be the ideal treatment for all patients with displaced fractures.
arthroplasty for femoral neck fracture, some investigators have
attempted to use these devices as a conservative option when treating
young patients with osteonecrosis (ON) of the femoral head. It is
believed by some that not preparing the acetabulum and placing an
acetabular component may be a beneficial option in these cases. This
philosophy has been tested for several decades. In 1977 Beckenbaugh et
al. 6 reported inferior results
using the Thompson femoral endoprosthesis and cemented fixation in
cases of ON. Again in the 1980s Lachiewicz and Desman 7
reported 52% fair and poor results using a bipolar endoprosthesis as a
conservative option in young patients with ON. They further noted that
younger age and increasing severity of the ON carried increased risk
for failure.
these negative results in a small meta-analysis highlighting the
long-term results of cemented and uncemented bipolar hemiarthroplasties
in contrast to THA. He noted that femoral loosening was not prevented
by a bipolar design and that the results of THA in ON were far superior
to those of the bipolar device. There were higher rates both of
complications and reoperations in the hemiarthroplasty group. Lee et
al. 9 prospectively compared the
results of bipolar hemiarthroplasty versus THA using an identical
modern cementless femoral component. They noted a significantly better
pain score in the THA group. Groin pain occurred significantly more
often in the bipolar group as did buttocks pain. In addition, 23% of
the bipolar group demonstrated superior head migration and acetabular
degeneration. Interestingly, the incidence of dislocation, thought to
be a concern with THA for acute fracture, was the same in both groups.
The conclusion of this series was that THA is a better procedure in
patients with ON.
who studied hemiarthroplasty in renal transplant patients suffering
from ON. In their series of 22 cemented bipolar hemiarthroplasties, all
patients had improvements in pain and 21 of the 22 had good to
excellent results. One case of aseptic loosening and one acetabular
complication necessitated revision at an average of 40 months
follow-up. Takaoka et al. 11 echoed
these acceptable results at early follow-up with the use of a bipolar
device in ON. In a comparison of bipolar hemiarthroplasty with
contralateral THA in the same patient, satisfactory results were equal
between the sides. No statistical differences were noted in any of the
clinical outcomes measured. The authors concluded that in young
patients with Ficat stage III disease, a bone in-growth stem and
bipolar arthroplasty is the treatment of choice. Excellent results have
also been shown with the use of a bipolar device and an uncemented stem
in young active patients with ON associated with sickle cell disease.
Caution should be used in these cases and any scenario where acetabular
bone stock may be involved because protrusion can occur, complicating
conversion to THA when necessary. It appears that in selected cases of
young patients with AVN, a bipolar articulation combined with a modern
cementless femoral component can provide acceptable results for several
years.
gained and lost popularity several times in the relatively short
history of hip arthroplasty. With more advanced bearing options,
improved implantation techniques, and stringent patient selection,
these procedures are enjoying a tremendous resurgence of interest
worldwide. As total resurfacing initially fell from favor, owing to
thin polyethylene acetabular surfaces and fixation issues,
hemiresurfacing has remained a viable option in young patients with ON.
attractive in the young active patient with ON, there have been
negative reports in the literature. Cuckler and Tamarapalli 12
reported poor results but recommended this procedure in patients with
ON if younger than 30 years of age as the conversion to THA is
straightforward. Adili and Trousdale 13
reported similar poor results with overall survivorship of 76% at 3
years. Only 62.5% of cases reported satisfaction and good pain relief
with this procedure.
of selected hemiresurfacing has been questioned. Total resurfacing hip
arthroplasty in ON has enjoyed renewed interest as results of this
procedure are now being reported in a more favorable light. Beaulé et
al. 14 have reported better
functional results and better pain relief with the use of a
metal-on-metal resurfacing than with hemiresurfacing alone.
the treatment of displaced femoral neck fracture in the elderly
patient. Although some authors believe that total hip arthroplasty may
be a better option, complications such as dislocation and increased
operative time and blood loss may outweigh these benefits in the
elderly low-demand patient. Both cemented and cementless fixation have
shown good long-term results as have unipolar and bipolar designs.
Advantages and drawbacks to each combination should stimulate personal
investigation by the orthopedic surgeon as to his or her own outcomes.
Hemiresurfacing arthroplasty has attractive theoretical advantages, but
with alternative bearings and improved implant fixation options this
procedure has decreasing and now very limited application.
R, Tornkvist H, Ponzer S, et al. Internal fixation versus
hemiarthroplasty for displaced fractures of the femoral neck in elderly
patients with severe cognitive impairment. J Bone Joint Surg Br. 2005;87(4):523–529.
K, McGuinness A, Brunner J, et al. Comparison of outcomes following
uncemented hemiarthroplasty and dynamic hip screw in the treatment of
displaced subcapital hip fractures in patients aged greater than 70
years. Acta Orthop Belg. 2005;71(1):48–54.
HP, Shah AR, Harding SH, et al. Cementless bipolar hemiarthroplasty for
displaced femoral neck fractures in the elderly. J Arthroplasty. 2004;19(7 suppl 2):73–77.
S, Bannister G. Cemented bipolar hemiarthroplasty for displaced
intracapsular fracture in the mobile active elderly patient. Injury. 2004;35(2):152–156.
RD, Tressler HA, Johnson EW Jr. Results after hemiarthroplasty of the
hip using a cemented femoral prosthesis. A review of 109 cases with an
average follow-up of 36 months. Mayo Clin Proc. 1977;52(6):349–353.
K, Nishina T, Ohzono K, et al. Bipolar prosthetic replacement for the
treatment of avascular necrosis of the femoral head. Clin Orthop Relat Res. 1992;277:121–127.
PE, Amstutz HC, Le Duff M, et al. Surface arthroplasty for
osteonecrosis of the hip: hemiresurfacing versus metal-on-metal hybrid
resurfacing. J Arthroplasty. 2004;19(8 suppl 3):54–58.
PE, Amstutz HC, Le Duff M, et al. Surface arthroplasty for
osteonecrosis of the hip: hemiresurfacing versus metal-on-metal hybrid
resurfacing. J Arthroplasty. 2004;19(8 suppl 3): 54–58.
HP, Shah AR, Harding SH, et al. Cementless bipolar hemiarthroplasty for
displaced femoral neck fractures in the elderly. J Arthroplasty. 2004;19(7 suppl 2):73–77.
M, Devereaux PJ, Swiontkowski MF, et al. Internal fixation compared
with arthroplasty for displaced fractures of the femoral neck: a
meta-analysis. J Bone Joint Surg. 2003;85A:1673–1681.
GL, Keller RB, Littenberg B, et al. Outcomes after displaced fractures
of the femoral neck. A meta-analysis of one-hundred and six published
papers. J Bone Joint Surg. 1994;76A:15–25.
RA, Koval KJ, Aharonoff GB, et al. Modular unipolar versus bipolar
prosthesis: a prospective evaluation of functional outcomes after
femoral neck fracture. J Orthop Trauma. 1995;9:298–302.
