Head Blocks
the head performed under regional anesthesia in the United States is
the partial maxillectomy performed on President Grover Cleveland in
1893. This chapter is presented according to the anatomic sites and
types of nerves (scalp and face, facial nerves, trigeminal nerve,
midface, and mandibular nerve). For each site, the relevant anatomy and
the corresponding blocks will be described. Since most head blocks
involve cranial nerves or their branches, consideration will also be
given to the bony anatomy and especially the neural foramina. All of
these blocks can be performed with the patient in the sitting or supine
position depending on the block and the condition of the patient.
Blocks of the cutaneous nerves supplying the scalp are indicated in the
emergency room and for plastic surgery to avoid tissue distortion.
Blocks of the frontal branch of the supraorbital and infraorbital
nerves are indicated for anesthesia in or around the eye. These blocks
are indicated for blepharoplasty or for other lid procedures, including
traumatic and posttraumatic reconstructive surgical procedures. Blocks
of the auriculotemporal, greater auricular nerves, and minor occipital
nerves are indicated for ear surgery.
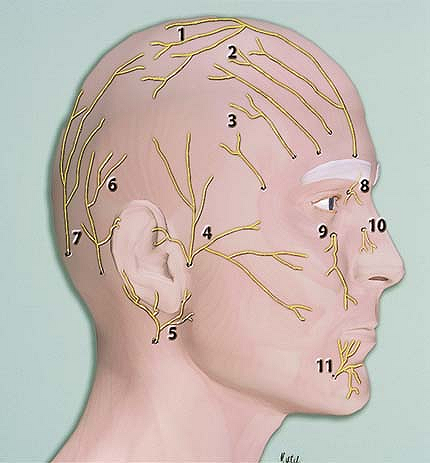
1, frontal nerve; 2, supraorbital nerve; 3, zygomaticotemporal nerve
(V2); 4, auriculotemporal nerve (V3); 5, greater auricular nerve; 6,
minor occipital nerve; 7, greater occipital nerve; 8, supra- and
infratrochlear nerve; 9, infraorbital nerve; 10, external nasal
branches of the ethmoid nerve; 11, mental nerve.
The appropriate site is identified, and 0.5 to 1.0 mL of 1% lidocaine
with 1/100,000 epinephrine is injected subcutaneously in small
increments up to 2 mL per nerve to obtain adequate anesthesia.
-
Originally, these blocks were directed at
specific cutaneous nerves to block their sensory distribution. However,
as epinephrine came into general use, its hemostatic effects on the
scalp became a great aid to neurosurgeons. Therefore, instead of
electively blocking these nerves, surgeons started to infiltrate the
scalp around their proposed incision sites.
 |
|
Figure 23-1. Cutaneous nerves supplying the scalp and face.
|
Blocks of the facial nerve are indicated when cosmetic procedures are
planned that require the injection of botulin toxin-A to produce nerve
paralysis with subsequent removal of forehead rhytides. It is of utmost
importance to test the effect of blocking the zygomaticotemporal branch
of the facial nerve using a short-acting local anesthetic. If the
botulin injection is not performed correctly, and the botulin toxin is
infiltrated lower, then a paralysis of the eyelids occurs that can last
2 to 3 months (temporary motor denervation). Blocks of the facial nerve
are also used for plastic surgery (to produce a temporary paralysis of
the eyelids when performing CO2 laser resurfacing or dermabrasion) and for traumatic repairs as well as posttraumatic reconstructive surgery.
1% lidocaine with 1/100,000 epinephrine is injected in small increments
(up to 2 mL) along the orbit posterior to the rim, laterally and
inferiorly. The needle can come close to the midline without causing
paralysis and affecting eye closure. The effects are not long lasting
and can be used as a good test prior to injecting the botulin toxin.
-
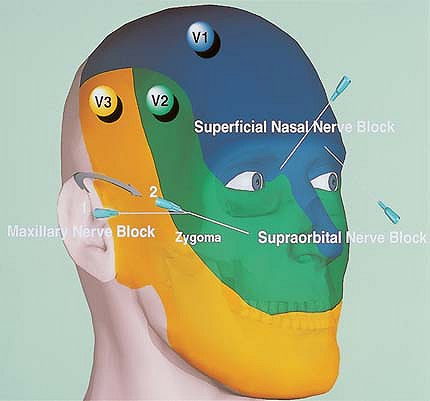
The combination of a supraorbital nerve block and an infraorbital nerve block provides complete anesthesia of the periorbita (Fig. 23-2).
-
The advantages of this technique over
infiltrating techniques are that the volume of the soft tissues is not
augmented by these injections and that there is no soft tissue
distortion. Therefore, the surgeon has much better perspective to plan
and carry out the repairs.
 |
|
Figure 23-2. The combination of a supraorbital nerve block and an infraorbital nerve block provides complete anesthesia of the periorbita.
|
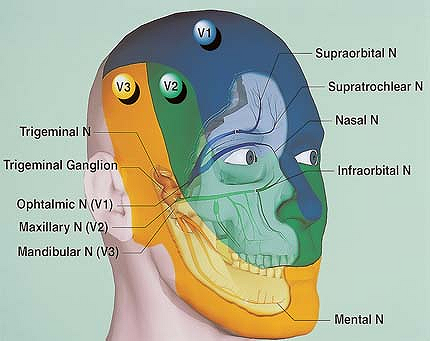
rise to the supraorbital nerve, which exits the brain through the
supraorbital fissure. This branch gives sensation to the forehead and
parietal scalp. The second division (V2) exits through the infraorbital
fissure to exit into the face through the infraorbital foramen, located
at approximately the midpoint of the infraorbital rim. Figure 23-3 depicts the cutaneous dermatomes associated with the different sensory branches of the trigeminal nerve.
The ophthalmic nerve cannot be blocked directly because it is posterior
to its branches (the lacrimal, nasociliary, and frontal nerves). The
nasociliary nerve insinuates itself through the annulus of Zinn into
the apex of the orbit and innervates
the
eye. Its two branches, the posterior and anterior ethmoids, leave the
orbital apex and pass into the posterior and anterior ethmoid foramina.
The frontal and lacrimal branches are not accessible to blocks in the
posterior orbital apex because they lie entirely outside of the apex of
the orbital wall.
 |
|
Figure 23-3. Cutaneous dermatomes associated with the different sensory branches of the trigeminal nerve.
|
With a needle pointing to the anterior ethmoid foramen, the anterior
and posterior ethmoid nerves are blocked, which innervates the
conjunctiva. Up to 2 mL of 1% lidocaine with 1/100,000 epinephrine is
then injected near the superior orbital fissure. With the insertion of
the needle, the globe elevates as digital pressure increases. With a
needle pointing to the posterior ethmoid foramen, the frontal and
lacrimal nerves are blocked by injecting up to 2 mL of the same local
anesthetic solution. The frontal nerve may be blocked forward, above
the bulb.
-
The portions of the orbit that are
straighter are best to guide the needle when blocking the orbital apex.
These conditions are best exemplified along the lateral wall of the
orbit and the superomedial wall. The lateral point of injection lies
immediately above the outer canthus of the eye. The needle is passed
with its point constantly in contact with the bone to an approximate
depth of 4.5 to 5.0 cm. -
To block the ciliary nerves and ciliary
ganglion, the local anesthetic solution needs to be injected in the
muscle boundaries. As a rule, the optic nerve is unaffected. After
injection, a transient mild proptosis is not uncommon. -
Finally, to obtain transient sensory
de-innervation of the bulb, the injection must be made in the muscle
boundaries to block the ciliary nerves and ciliary ganglion. As a rule,
the optic nerve is unaffected. After injection, a transient mild
proptosis is not uncommon.
For incision and drainage of dental abscesses in the outpatient
setting, to remove hardware used in repairing maxillofacial fractures,
and, occasionally, in sinus surgery in the elderly and in closed
reduction of nasal fractures. Palatal blocks are also indicated to
excise cysts, small benign tumors, and bony exostoses. They are also
occasionally used as a conduit to the pterygopalatine foramen either to
block V2 at the foramen rotundum or to therapeutically obtain
hemostasis in posterior nosebleeds by placing the internal maxillary
artery in spasm and using the hydrostatic pressure for vessel
compression against the bony canal. Blocking the sphenopalatine
ganglion is also valuable in evaluating contact neuralgia (Sluder type)
prior to any definitive surgical procedure.
To provide a complete block of the region it is necessary to block the
peripheral branches of the second division of the trigeminal nerve (the
infraorbital and superior, posterior, and medial alveolar nerves). The
infraorbital nerve is approached by introducing the needle directly to
the midpoint of the inferior orbital rim and infiltrating the area with
approximately 1 to 2 mL of 1% lidocaine with 1/100,000 epinephrine.
This block produces anesthesia of the lower eyelid, the upper lip, a
large part of the nose, a part of the skin and mucosa of the cheek, the
anterior portion of the superior alveolar process and its periosteum,
the anterior wall of the maxilla, and the upper central and lateral
incisors.
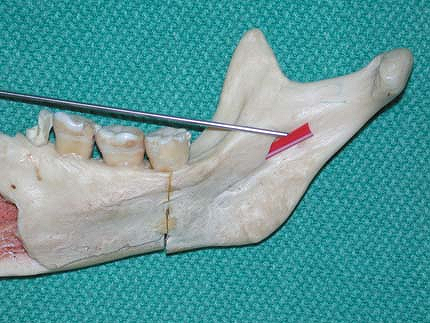
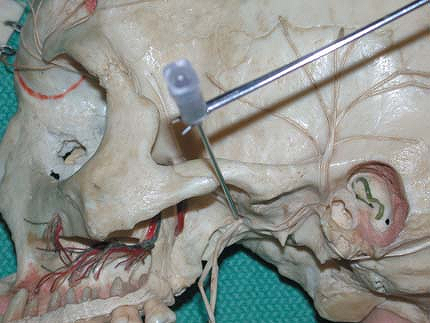
nerve (V2) may be carried out externally by passing a 22-gauge, 89-mm
spinal needle just below the zygomatic arch along the posterior surface
of the ascending ramus of the mandible into the most superior portion
of the pterygopalatine fossa. The point of insertion of the needle lies
immediately behind the lower palpable angle of the malar bone (Fig. 23-4).
First, a small amount of 1% lidocaine with 1/100,000 epinephrine is
injected into the skin itself. From this point, the needle is pressed
inward and upward. Its point passes through the masseter muscle until
it comes in contact with the superior maxillary tubercle, and it is
slid along this surface. Occasionally, the point of the needle strikes
the wing of the sphenoid, in which case, the direction of the needle is
changed, or, if necessary, withdrawn altogether, and another point of
entrance made just posterior to the midpoint of the zygomatic arch. The
appropriate location is assumed once the needle suddenly passes deeper
into the pterygopalatine fossa and reaches the nerve at an approximate
depth of 5 to 6 cm. Once the needle is in the appropriate position, the
patient complains of radiating pain in the face. The needle is then
withdrawn slightly, and 5 mL of 1% lidocaine with 1/100,000 epinephrine
is injected, moving the needle back and forth.
 |
|
Figure 23-4. The point of insertion of the needle lies immediately behind the lower palpable angle of the malar bone.
|
-
In the past, these blocks have been used for major surgery of the head.
-
When performing these blocks, it is very
important not to perform an intraneural injection (a sharp
“electric-like” pain during the injection), and therefore the patient
should remain awake during the block.
Anesthesia of the lower third of the face. Mostly used by dentists and
maxillofacial surgeons in the emergency room setting for repair of
facial lacerations, animal bites, incision and drainage of dental or
salivary gland abscesses, probing of salivary gland ducts, or in
radiology. Indications also include biopsies of the tongue, labiodental
sulcus, or inner table of the mandible, manipulation of the mandible in
cases in which mandible fractures are suspected and the patient is
uncooperative to intraoral exam because of pain, and in removal of
hardware inserted for repair of Le Fort fractures. It is also useful in
performing a number of cosmetic procedures on the lower third of the
face.
alveolar and lingual nerves intraorally by injecting the inner surface
of the ascending ramus of the mandible into the region of the lingula.
This route is the one most commonly performed. The second method is by
directly blocking the nerve trunk in the foramen ovale.
lingual nerve blocks), the index finger is passed intraorally until it
touches the ascending ramus of the mandible. At about 1.5 cm lateral to
the third molar, the sharp edge of the coronoid process can be
palpated. This runs inferiorly along the side of the third molar and
becomes lost in the oblique line. Medially, from this edge, there is a
small, concave bony area, with three corners, directed forward and
inward and medially bounded by a bony ridge. This area is occasionally
referred to by head and neck surgeons as the retromolar trigone.
With the mouth closed, this area lies to the inner side of the third
molar. With the mouth open, it lies laterally to the upper and lower
teeth and is easily accessible. The lingual nerve lies immediately
under the mucosa, and the inferior alveolar nerve is 1.5 cm in back of
this point. A long 22-gauge, 89-mm spinal needle is introduced
intraorally and is directed from opposite the lateral incisors toward
the point of injection and held parallel to the biting surface of the
lower teeth. The needle is then inserted 1 cm above and lateral to the
biting surface of the last molar, into the retromolar trigone. The bone
should be immediately felt. If this is not the case, then the point of
the needle is too far from the median line, in which case the needle
must be directed more to the median line until the border is felt. The
needle is passed along the inner surface of the ascending ramus of the
mandible into the deeper parts for approximately 2.0 to 2.5 cm. Once
the needle is proximate to the lingual nerve, about 5 to 10 mL of 1%
lidocaine with 1/100,000 epinephrine is injected. A long needle is
always used so that the injection site is under direct visualization at
all times.
the trigeminal nerve) has the advantage of providing a complete block
of the branches originating from the main trunk of the trigeminal
nerve, except for the lingual nerve. For the external approach to the
foramen ovale, once again a long spinal needle is used. The point of
injection is chosen
by
marking the inferior border of the zygomatic arch at its midpoint, and
the needle is inserted almost in transverse fashion. At a depth of 4 to
5 cm, the end of the needle touches the pterygoid process. In this
injection, the needle is approximately 1 cm anterior to the foramen
ovale. The depth is then marked on the needle. The needle is then
withdrawn to the subcutaneous tissue and is once again passed medially
at a slight posterior angle and to the same depth or a few millimeters
more. The characteristic radiating pains will then occur. At this
point, the needle is withdrawn a few millimeters and the injection
proceeds by instilling approximately 5 to 10 mL of 1% lidocaine with
1/100,000 epinephrine (Fig. 23-5).
 |
|
Figure 23-5.
The needle is withdrawn a few millimeters and the injection proceeds by instilling approximately 5 to 10 mL of 1% lidocaine with 1/100,000 epinephrine. |
-
To provide a complete block of the
branches originating from the trigeminal nerve, it is necessary to
occasionally add a block of the distal branches, which exit through the
mental foramina.
Y, Okuda K, Shinohara M, et al. Use of computed tomography for
maxillary nerve block in the treatment of trigeminal neuralgia. Reg Anesth Pain Med 2000;25:417–419.
