Hand Fractures and Dislocations
most frequently encountered musculoskeletal injuries. In Canada, the
annual incidence was found to be 29 per 10,000 in people older than 20
years of age, and 61 per 10,000 in people younger than 20 years of age.48 Males had a 2.08 times greater risk until after age 65, when females become at greater risk.48,145
The 1998 U.S. National Hospital Ambulatory Medical Care Survey found
phalangeal (23%) and metacarpal (18%) fractures to be the second and
third most common fractures below the elbow, peaking in the third
decade for men and the second decade for women.25
Another series of 1358 fractures reported the distribution as 57.4% for
proximal phalanx, 30.4% for middle phalanx, and 12.2% for metacarpal.86
Of 502 phalangeal fractures, 192 were at the proximal phalanx (P1), 195
were at the middle phalanx (P2), and 115 were at the distal phalanx
(P3).165 The small finger axis is the most commonly injured, constituting as high as 37% of total hand fractures.145
underappreciated and difficult to measure. No statistically significant
correlation could be drawn in a study comparing the American Medical
Association impairment rating with the Disability of the Arm, Shoulder,
and Hand (DASH) questionnaire.166 In
a series of 924 hand fractures, overall results were excellent or good
in 90% of thumbs but only 59% to 76% of fingers, citing comminution and
open or multiple fractures as poor prognostic indicators.86
The most common complication is stiffness. Intra-articular extension
appears to confer a worse prognosis with total active motion (TAM) of
169 degrees compared with a TAM of 213 degrees in fractures without
intra-articular extension.62 Only a
few patterns of dislocation lead to residual instability. Fractures,
however, can easily result in malunion. Some practitioners perceive a
direct tradeoff between stiffness and either residual instability or
malunion. This is not necessarily the case. As the understanding of
these difficult injuries improves along with new surgical techniques,
it is becoming increasingly possible to achieve good hand function
while avoiding complications for most isolated fractures and
dislocations. Major hand trauma is another matter.
that the negative effects of surgery on the tissues should not exceed
the negative effects of the original injury. Accordingly, nonoperative
treatment plays a significant role in the management of fractures and
dislocations of the hand. A corollary to this principle is that even
though fractures and dislocations are fundamentally skeletal injuries,
most of the difficult decision-making centers on management of the soft
tissues. The injured part must not be considered in isolation. The
multiple joints of the hand are maintained in a delicate balance by the
intrinsic and extrinsic tendon systems such that a disturbance in one
set of tissues will often significantly affect others.
magnitude, direction, point of application, and type of force that
caused the injury. A high degree of variation in mechanism of injury
accounts for the broad spectrum of patterns seen in skeletal trauma
sustained by the hand. Axial load or “jamming” injuries are frequently
sustained during ball sports or sudden reaches made during everyday
activities such as to catch a falling object. Patterns frequently
resulting from this mechanism are shearing articular fractures or
metaphyseal compression fractures. Axial loading along the upper
extremity must also make one suspicious of associated injuries to the
carpus, forearm, elbow, and shoulder girdle. Diaphyseal fractures and
joint dislocations usually require a bending component in the mechanism
of injury, which can occur during ball-handling sports or when the hand
is trapped by an object and unable to move with the rest of the arm.
Individual digits can easily be caught in clothing, furniture, or
workplace equipment to sustain torsional mechanisms of injury,
resulting in spiral fractures or more complex dislocation patterns.
Industrial settings or other environments with heavy objects and high
forces lead to crushing mechanisms that combine bending, shearing, and
torsion to produce unique patterns of skeletal injury and significant
associated soft tissue damage.
trauma. If the injury is reducible at all, gentle manipulation will
accomplish the reduction far more successfully than forceful
longitudinal traction. The principle is relaxation of deforming forces
through proximal joint positioning such as metacarpophalangeal (MP)
joint flexion to relax the intrinsics or wrist flexion to relax the
digital flexor tendons. Often, a gentle back-andforth rotatory maneuver
is necessary to free a bony prominence from soft tissue entrapment. The
mobile distal part is then reduced to the stable proximal part.
possible and allow unrestricted motion of all other joints. One
controversial point concerns the need to immobilize the wrist. Setting
appropriate length-tension relationships in the extrinsic motors (in
cases where they are deforming forces) is most easily accomplished
through immobilization of the wrist in 25 to 35 degrees of extension.
This is extremely helpful in patients with low pain tolerance who tend
to place the hand in a characteristic dysfunctional posture of wrist
flexion-MP joint extension-interphalangeal (IP) joint flexion (the
“wounded paw” position). Other patients who are capable of avoiding
this position on their own often do not need wrist immobilization. A
simple splint that is useful for injuries ranging from the
carpometacarpal (CMC) joints proximally to P1 fractures distally
consists of a single slab of plaster or fiberglass applied dorsally.
With a foundation at the forearm, the splint runs out to the level of
the proximal interphalangeal (PIP) joints distally with the wrist
extended and the MP joints fully flexed. Full motion of the IP joints
should be encouraged throughout the healing process. The total duration
of immobilization should rarely exceed 3 to 4 weeks. Hand fractures are
stable enough by this time to tolerate active range of motion (AROM)
with further remodeling by 8 to 10 weeks.15
of coordination. Numbness and tingling signify associated nerve
involvement (either direct injury to the nerve or as a secondary effect
of swelling). Signs include tenderness, swelling, ecchymosis,
deformity, crepitus, and instability. A better skeletal examination can
often be obtained with the aid of anesthesia applied directly at the
injury site or regionally. Isolated MP joint dislocations and
metacarpal fractures can be treated with direct injection of anesthetic
into the injury site. More distal injuries are easily anesthetized with
a digital block. More global pain relief can be obtained through nerve
blocks performed at the wrist to include the median nerve, ulnar nerve,
and dorsal cutaneous branches of the radial and ulnar nerves. The time
following administration of the anesthetic can be used to cleanse any
superficial wounds and to prepare splinting supplies. Pain-free
demonstration of tendon excursion and fracture and ligament stability
can then be performed. At the conclusion of the anesthetized skeletal
exam, the injury can be promptly reduced and splinted.
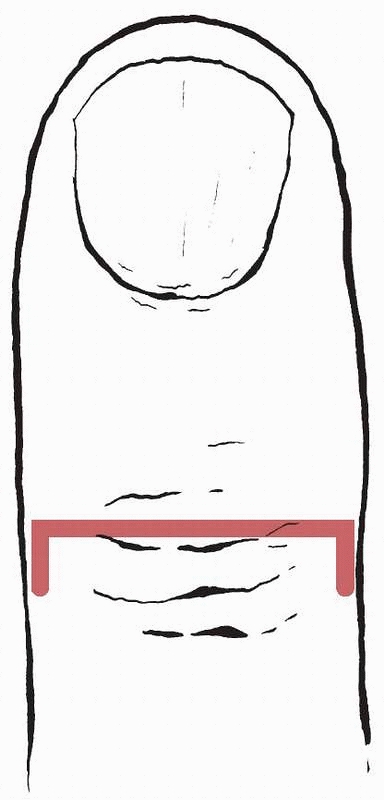
presence of rotational deformity. The examiner must understand the
appropriate method of assessment. The bones of the hand are short
tubular structures. Malrotation at one bone segment is best represented
by the alignment of the next more distal segment. This alignment is
best demonstrated when the intervening joint is flexed to 90 degrees.
Comparing nail plate alignment is an inadequate method of evaluating
rotation. Other unique physical examination findings will be discussed
in association with specific injuries.
common. Open wounds should not be probed in the emergency department;
doing so only drives surface contaminants deeper and rarely yields
useful information. The need for prophylactic antibiotics in open hand
fractures is controversial. The previous standard administration of
Ancef no longer appears applicable with methicillin-resistant Staphylococcus aureus
(MRSA) dominating most community-acquired infection profiles.
Clindamycin, vancomycin, Bactrim, and the quinolones are useful agents
against MRSA. Aminoglycosides are added for contaminated wounds, and
penicillin for soil or farm environments. No hard evidence exists to
support continuation of antibiotics beyond the initial 24 hours. The
exception to this may be bite wounds, whose potential for osteomyelitis
is significant if the tooth directly penetrates the cortex, allowing
the saliva into the cancellous structure. Aggressive and early surgical
debridement is needed for all bite wounds.
With substantial displacement of the dorsal cortex, nail matrix
disruption should be expected and direct repair planned. Reconstruction
of residual open wounds overlying skeletal injury sites requires the
use of flaps. Frequently transposition flaps will suffice. Less
frequently, pedicle or free flaps will prove necessary.75,76
The greatest challenge in the hand, and particularly the digit, is to
achieve both thin and supple tissue coverage. A fascial flap covered
with a split-thickness skin graft provides this combination of
features, except at the volar pulp, where a directly innervated
glabrous cutaneous flap is needed (Fig. 28-1).
may accompany dislocations. Prime examples are terminal tendon ruptures
sustained in association with distal interphalangeal (DIP) joint
injuries and central slip ruptures sustained in association with PIP
joint injuries. Initial examination of the traumatized hand must
include a survey that inventories each potential tendon injury. Apart
from these, tendon damage usually only occurs with an associated
laceration or in open combined injuries.
rarely injured as part of simple fractures and dislocations of the
hand. In major open hand trauma, there is usually a significant zone of
injury. Appropriate treatment includes excision of the devitalized
tissues in the zone of injury including nerve and vessel tissues
followed by reconstruction with autogenous grafts or adjacent transfers.
fracture with injury to at least one of the soft tissues listed above.
These are most often open injuries with the soft tissue component of
greatest significance being the injury to flexor tendons, extensor
tendons, or both. The occurrence of this combined pattern of injury
directly impacts the treatment strategy for the fracture itself. Many
fracture patterns presenting as an isolated injury would be best cared
for nonoperatively or with closed reduction and internal fixation
(CRIF) using smooth stainless steel Kirschner wires (K-wires). The open
wound leading to the fracture site automatically changes the surgical
approach to open reduction, usually with internal fixation (ORIF). The
presence of an adjacent tendon repair site necessitates achieving
skeletal stability sufficient to withstand the forces of an immediate
tendon glide rehabilitation program. This often means the use of rigid
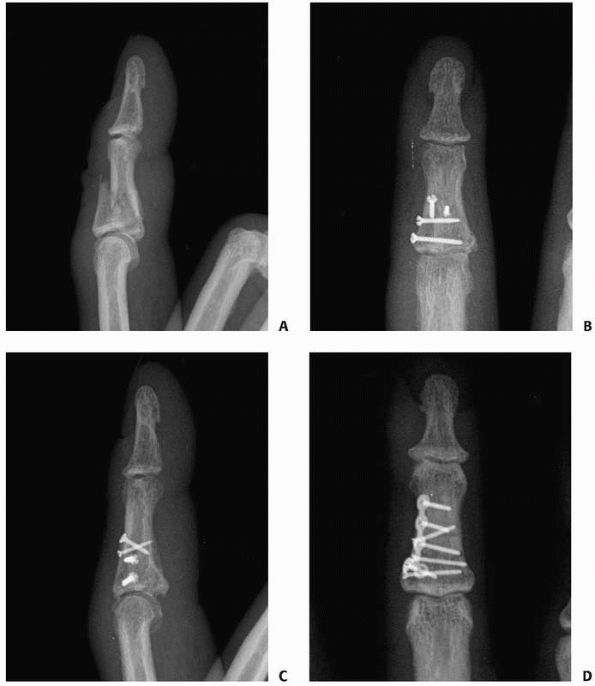
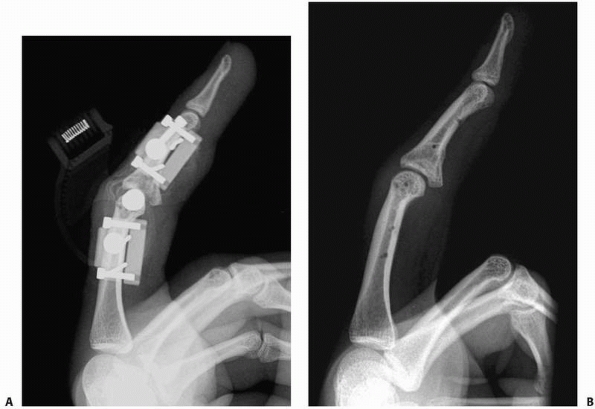
internal fixation (Fig. 28-2). In a study
limited to ORIF of intra-articular fractures, comminution and an
initial open injury were identified as independent variables leading to
a worse prognosis.154 Only 6 of 16
patients in another study of comminuted phalangeal fractures and
associated soft tissue injuries achieved greater than 180 degrees of
TAM.29 The remainder of this chapter
describes the most appropriate techniques for managing fractures and
dislocations of the hand as isolated injuries. The term combined injuries
will be found associated with the more stable fixation options as part
of the “Indications for Treatment” tables listed throughout the chapter.
massive hand trauma merits a textbook in its own right and is beyond
the scope of this chapter. The majority of the complex decision-making
in these injuries occurs with respect to the strategy chosen for the
soft tissues (Fig. 28-3). With true degloving injuries and exposed bone and tendon, either pedicle or free flaps are required for coverage.75,76 Pedicle flaps are simpler and faster but are limited in size and reach and are associated with
a higher complication rate than thin fascial free flaps that can cover a defect of any size and shape.75,76
Clinical evaluation of these injuries is quite difficult because the
patient is often unable or unwilling to do very much with respect to an
interactive examination. Much of the determination regarding the extent
of injury is made intraoperatively. Good-quality radiographs are rarely
obtained initially and usually consist of semioblique views of the hand
with a high degree of bone overlap. Every effort should be made within
the scope of total patient management to obtain additional radiographic
views that can be set up properly so that associated injuries are not
missed. More often than not, the opportunity for these views first
presents itself in the operating room. A very easy pitfall is to draw
attention to the most obvious radiographic findings without taking the
time to search for more subtle injuries. Radiographic evidence of
foreign matter embedded in the hand should be sought as well as its
absence at the conclusion of the debridement.
 |
|
FIGURE 28-1 Thin supple coverage of open hand trauma wounds can be accomplished with (A) thinner fascial flaps covered with a split-thickness skin graft or (B) bulkier cutaneous or fasciocutaneous flaps. C.
Fasciocutaneous flaps at the digital level may demonstrate an even more substantial difference compared with the thinness and flexibility of a grafted fascial flap (D,E). |
 |
|
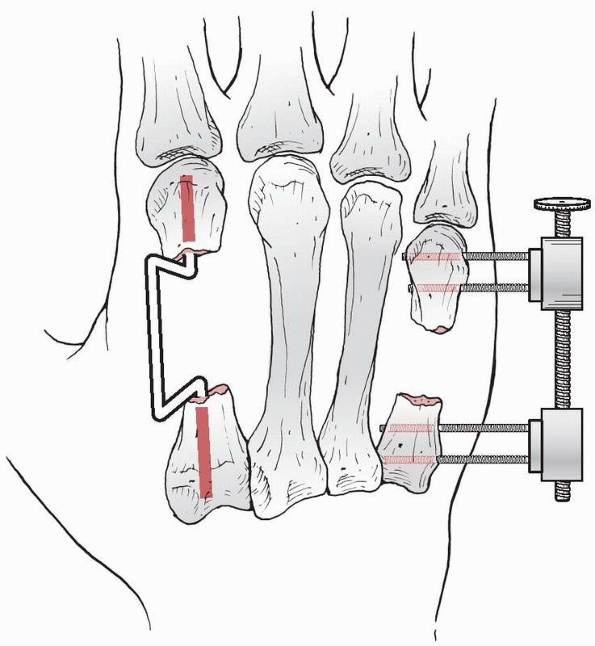
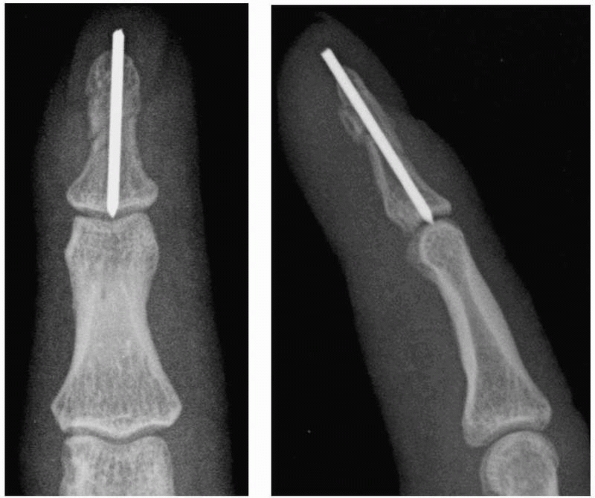
FIGURE 28-2
Major open hand trauma frequently requires the most stable forms of fixation to facilitate an aggressive early motion rehabilitation program focusing on tendon gliding. |
 |
|
FIGURE 28-3
Massive crushing trauma to the hand usually causes its most devastating effects, not to the skeletal elements themselves, but rather diffusely through devitalization of the soft tissues covering the bone. |
modified for the hand by reducing the 10-cm wound length threshold to 2
cm. The validity of the classification is supported by 62.5% normal
hand function found after type I injuries compared with 21% following
type III fractures.111 Another series found 92% poor results associated with grade III B and C injuries.39 From a series of 200 open hand fractures, Swanson151
differentiated type II wounds from type I wounds by three criteria:
contamination at initial presentation, open for more than 24 hours
before treatment, or in patients with systemic illness. Type II wounds
are not recommended for primary closure.
in massive hand injuries. Standard indications for external fixation
include gross contamination of the original wound, segmental bone loss
or comminution, or the lack of availability of good
soft tissue coverage.37
The biomechanics of external fixation in the hand are the same as
elsewhere in the body with pin diameter constituting the chief
determinant of fixator stiffness. Four pins, two proximally and two
distally, are sufficient for most hand applications. A given hand
injury may best be fixed by all internal, all external, or a
combination of the two methods of fixation. An improved understanding
and a wider array of elegant soft tissue coverage techniques have
overcome previous concerns regarding exposure of hardware with internal
fixation.75,76
(especially with crush injuries), the thumb and index metacarpals
should be pinned into abduction to prevent a first web space
contracture. No matter how the injury is managed, the strategy should
plan for rehabilitation to begin, unobstructed by bulky external
dressings, by 72 hours after surgery. In one series, 72 metacarpal and
phalangeal fractures with severe associated soft tissue injury were
treated with plates and screws yielding 46% good, 32% fair, and 22%
poor results by the American Society for Surgery of the Hand (ASSH)
criteria of total active motion.21
The overall results for treatment of these severe injuries are most
closely related to the soft tissue component rather than the status of
the skeletal injury.65 In 245 open
injuries studied prospectively, extensor tendon injury alone had 50%
poor results, but flexor tendon or multiple soft tissue injuries
produced 80% poor results.24 A
series of 140 open fractures demonstrated better results at the
metacarpal compared with the phalangeal level with the worst outcomes
occurring for injuries at the P1 and PIP level, especially when
associated with an overlying tendon injury.39
hand injuries. Once the wound has been rendered clean through either a
single or multiple débridements, bone grafting is appropriate using
corticocancellous iliac crest, shaped and sized to match the curvature
of the missing segment. If only mild comminution is present without
loss of structural stability, cancellous graft alone is sufficient.
Stable fixation is achieved with either internal plate (Fig. 28-4)
or external fixator application. With proper débridement, immediate
primary bone grafting is safe. A series of 12 patients with type III
open fractures and another 20 patients with low-velocity gunshot
phalangeal fractures both demonstrated 0% infection rates with the use
of an immediate autograft.62,133
If delayed bone grafting is planned, a temporary spacer may be used to
preserve the volume that will later be occupied by the graft (Fig. 28-5).
Bone loss that includes the articular surface represents an entirely
different and much more complex problem. Strategies that have been
advocated include autografts of metatarsal head, second, and third CMC
joints; immediate Silastic prosthetic replacement; osteoarticular
allografts; primary arthrodesis; and free vascularized composite whole
toe joint transfer.87
dislocations of the hand is to achieve sufficient stability of the bone
or joint injury to permit early motion rehabilitation without resulting
in malunions for fractures or residual instability for dislocations.
The correct treatment option is the least invasive technique that can
accomplish these goals. When multiple injuries are present, one must
determine treatment for the primary injury upon which the management of
the other injuries will be based. There are essentially five major
treatment alternatives: immediate motion, temporary splinting, CRIF,
ORIF, and immediate reconstruction.91,97,146,154,156
The general advantages of entirely nonoperative treatment are assumed
to be lower cost and avoidance of the risks and complications
associated with surgery and anesthesia. The generally presumed
disadvantage is that stability is less ensured than with some form of
operative fixation. CRIF is expected to prevent overt deformity but not
to achieve an anatomically perfect reduction. Pin tract infection is
the prime complication that should be mentioned to patients in
association with CRIF. Open treatments are considered to add the
morbidity of surgical tissue trauma, titrated against the presumed
advantages of achieving the most anatomic and stable reduction.
operative treatment are the assessments of rotational malalignment and
stability (Fig. 28-6). If carefully sought, rotational discrepancy is relatively easy to determine.140
Defining stability is somewhat more difficult. Some authors have used
what seems to be the very reasonable criterion of maintenance of
fracture reduction when the adjacent joints are taken through at least
30% of their normal motion.24
Contraction of soft tissues begins approximately 72 hours following
injury. Motion should be instituted by this time for all joints stable
enough to tolerate rehabilitation.28 Elevation and elastic compression promote edema control.109
The more aggressive the surgeon’s management of the injury has been,
the more aggressive must be the rehabilitation. Low-energy isolated
injuries have far less risk of stiffness than those created by
high-energy trauma with large zones of injury.
should be made in accordance with the fundamental principles of patient
evaluation and management. A well-taken history should be followed by a
thorough examination that is followed by imaging studies. The set of
combined information from these three sources creates a profile of the
individual patient’s unique problem that then leads to all subsequent
management decisions. The history should include a description of the
environment where the injury occurred. If the injury is open, expected
contaminants from different environments would dictate different
choices for prophylactic antibiotics. A clear history of the mechanism
of injury should be obtained. The patient should be questioned
regarding visible deformity immediately following injury and whether
any immediate reduction maneuvers were performed at the site of injury
or subsequently in an emergency department. The degree and duration of
swelling should be described with specific reference to exact location.
The patient’s current symptoms and chief complaint are essential and
often the best clues to uncovering associated injury patterns. Physical
examination includes assessment of all tissue layers beginning with the
integument and including flexor and extensor tendons, nerves, vessels,
and, ultimately, the skeletal structure.
 |
|
FIGURE 28-4 When segmental bone loss occurs (A), shortening may be prevented by temporary stabilization (B). Subsequent internal fixation (C, D) and bone grafting can restore the original anatomic parameters of the skeletal unit.
|
projections with the beam centered at the level of interest. A third
oblique view is often quite instructive, revealing displacement not
evident on the standard posteroanterior (PA) or lateral. Rarely are
other imaging studies necessary in evaluating fractures and
dislocations of the hand. In complex periarticular fractures, such as
“pilon” fractures at the base of P2, computed tomography (CT) scans
assist some surgeons with operative planning. Foreign bodies may not
always be detected by standard radiographic projections. Glass or
gravel is best seen with soft tissue technique. CT scans may detect
plastic, glass, and wood. Ultrasound can detect objects that lack
radiopacity. Magnetic resonance imaging (MRI) remains a more expensive
backup for all types of foreign materials.
has not been written in accordance with any defined classification
scheme, and true comparisons are difficult to make. Descriptions
of
fractures have been based largely on the location within the bone
(head, neck, shaft, base) and further modified by the direction of the
fracture plane (transverse, spiral, oblique, comminuted) and the
measurable degree of displacement. Dislocations have been described by
the direction the distal segment travels (dorsal, volar, rotatory) and
further modified by the capacity (simple) or incapacity (complex) for
closed reduction. In the sections that follow regarding each injury, it
will be assumed that the above-stated designations are in effect unless
specific exceptions are noted.
 |
|
FIGURE 28-5
When extensive contamination precludes the use of internal fixation or when bone reconstruction is to be done at a later date, the use of spacer wires or the application of an external fixator with distraction and compression capabilities can be useful. |
the distal phalanx experiences stress loading with nearly every use of
the hand. The soft tissue coverage is limited and local signs of
fracture can usually be detected at the surface. When fractures
accompany a nail bed injury, hematoma can be seen beneath the nail
plate. When the seal between the nail plate and the hyponychium is also
broken, the fracture is open and should be treated as such. The
mechanism of injury often involves crushing, and the soft tissue injury
is frequently of greater significance for long-term prognosis than the
fracture. When one is suspicious of a distal phalanx fracture,
radiographs should be taken as isolated views of the injured digit.
 |
|
FIGURE 28-6
Pronation of the ring finger proximal phalanx is easily demonstrated by the angular discrepancy of the middle phalanges viewed with the proximal interphalangeal joints flexed 90 degrees. |
ligaments that pass from the distal margin of the widened lateral base
to the expanded proximal margins of the tuft. Small branches of the
proper digital artery that supply the dorsal arcade just proximal to
the nail fold pass under these ligaments very close to the base of the
shaft of the distal phalanx. The tuft is an anchoring point for the
specialized architecture of the digital pulp, a honeycomb structure of
fibrous septae that contain pockets of fat in each compartment. The
proximal part of the pulp is thicker and more mobile than the distal
pulp. The proximal portion of a tuft fracture may become entrapped in
the septae of the pulp and prove irreducible.5
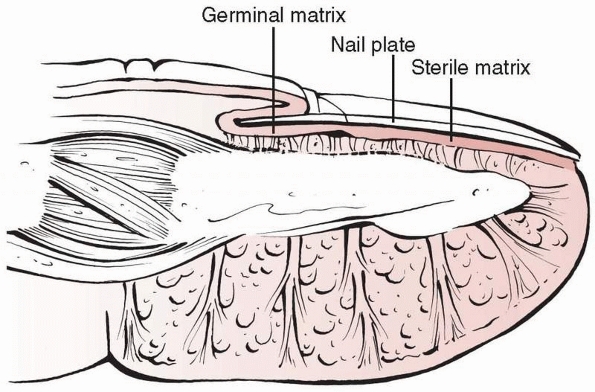
The dorsal surface of the distal phalanx is the direct support for the
germinal matrix and sterile matrix of the nail. The bone volarly and
the nail plate dorsally create a three-layer sandwich with the matrix
in the middle (Fig. 28-7).
The two mechanisms of injury experienced most frequently are a sudden
axial load (as in ball-handling sports) or crush injuries. Crush
fractures of the tuft are often stable injuries held in place by the
fibrous network of the pulp volarly and the splinting effect of the
nail plate dorsally. Proximally, the digital flexor and terminal
extensor tendons insert on the volar and dorsal bases of the distal
phalanx. Since these are the last tendon attachments in the digit, all
fracture planes occurring distal to these tendon insertions have been
separated from any internal deforming forces. In contrast, volar and
dorsal base fractures are unstable, with the entire force of a tendon
pulling
the
small base fragment away from the remainder of the bone. Controlling
rotation in these small pieces may be particularly difficult. Dorsal
base intra-articular fractures because of the shearing component of an
axial load injury should be distinguished from avulsion fractures
occurring under tension from the terminal tendon. The latter are
smaller fragments with the fracture line perpendicular to the line of
tensile force in the tendon, whereas the former are larger fragments
comprising a significant (greater than 20%) portion of the articular
surface with the fracture line being perpendicular to the articular
surface. These are very different injuries with different treatment
requirements.104
In a similar fashion, the majority of bone flakes at the volar base of
P3 are really flexor digitorum profundus (FDP) tendon ruptures
occurring through bone. A small percentage of volar base fractures,
especially when large in size, are not FDP avulsions but rather
shearing fractures that are amenable to extension block splinting.
 |
|
FIGURE 28-7
An intimate relationship exists between the three layers of the dorsal cortex of the distal phalanx, the nail matrix (both germinal and sterile), and the nail plate. |
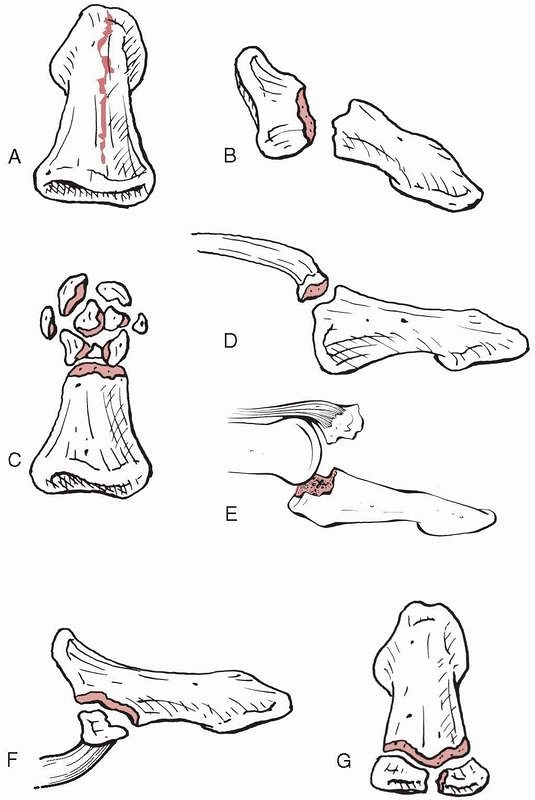 |
|
FIGURE 28-8 Fracture patterns seen in the distal phalanx include (A) longitudinal shaft, (B) transverse shaft, (C) tuft, (D) dorsal base avulsion, (E) dorsal base shear, (F) volar base, and (G) complete articular.
|
The splint should leave the PIP joint free but usually needs to cross
the DIP joint simply to gain enough foundation to provide adequate
stability. The splint may be removed daily to perform active DIP
joint-blocking exercises. Aluminum and foam splints or plaster of Paris
are common materials chosen. The significance of lingering symptoms
with fractures of the distal phalanx remains underappreciated (Table 28-1).
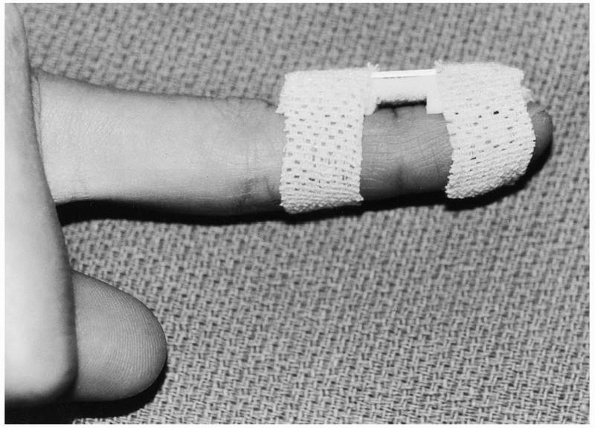 |
|
FIGURE 28-9
Dorsal splinting of the distal phalanx and the distal interphalangeal joint is easily accomplished with an aluminum and foam splint. Cutting out the foam over the dorsal nail fold skin relieves direct pressure where the skin is at greatest risk for ischemic necrosis. |
phalanx that supports the nail matrix has a significant step-off,
especially with a concomitant nail plate avulsion, the fracture should
be restored to a level surface and pinned to render support to the
surgical repair of the nail matrix. Conversely, if the nail plate has
maintained its seal at the hyponychium and the dorsal surface of the
distal phalanx is level, formal removal of the plate to perform a nail
matrix repair is not necessary despite any measured percentage of
hematoma occupying the area under the nail. Matrix defects should be
split-thickness grafted from the adjacent or a distant nail bed.
Following repair, the dorsal nail fold should be stented to prevent
adherence to the matrix but still allow fluid drainage. The patient
should be warned of the potential for nail deformity and the time
required (4 to 5 months) for regrowth.
that nonoperative management is appropriate. Active motion of the DIP
joint can be pursued from the outset since the forces of the flexor
digitorum profundus and the terminal extensor tendon are not acting
across the fracture site. Only externally applied forces such as pinch
will deform the fracture. Shaft fractures with wide displacement are
headed for a nonunion without closer approximation of the fragments.
CRIF is usually sufficient for these fractures unless there is
interposed tissue blocking the reduction (Fig. 28-10).
Kirschner wire fixation may also be preferable (0 of 5 malunions)
compared with splinting (3 of 18 flexion malunions) when the fracture
is transverse, extra-articular, and located at the base of the distal
phalanx.4
surface had mean flexion of 77 degrees with a four-degree extensor lag and two losses of reduction.80
The difficulty in comparing the published outcomes for these injuries
is that the literature has usually failed to distinguish between dorsal
fractures that are merely bony variants of terminal tendon injuries and
those that are the more significant intra-articular fractures discussed
in this section.
|
TABLE 28-1 Distal Phalanx Fractures
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||
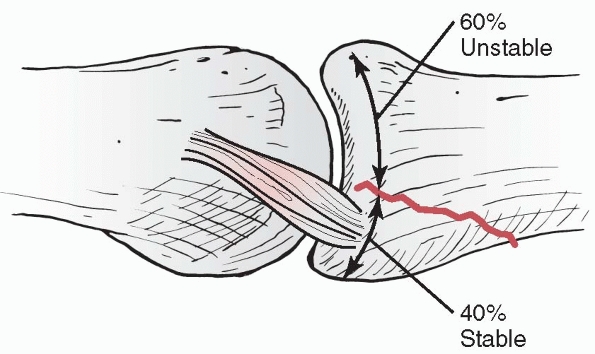
subluxation has been cited as a reason to perform ORIF, a biomechanical
study showed that subluxation was not seen whenever the smaller
fragment carried less than 43% of the articular surface.84 Thirty-three patients with K-wire ORIF had a mean arc of 4 to 67 degrees of final motion.153
As an alternative method of ORIF, nine patients were treated with a
custom “hook plate” formed by cutting a 1.3-mm modular straight plate
and achieved an average of 64 degrees of ROM at the DIP joint with no
extensor lag.155 One method of
avoiding the complications potentially associated with open DIP joint
surgery (0 of 19) might be the 5 weeks of external fixation employed in
19 patients resulting in 70 degrees of flexion with a two-degree
average extensor lag.88
 |
|
FIGURE 28-10
Shaft fractures should first be axially compressed then stabilized with a longitudinal K-wire that is drilled just short of the subchondral bone plate then axially tapped into the subchondral bone without spinning the wire. |
FDP functional integrity. If the volar FDP fragment is large enough, it
may be fixed with a compression screw. Extension block pinning is
another rarely used alternative. The remainder of small bone flakes
located at the volar base of the distal phalanx are tendon avulsions
and should be treated in accordance with modern principles of flexor
tendon reinsertion.
 |
|
FIGURE 28-11
Dorsal base fractures from axial impaction with shearing rather than a traction avulsion injury may demonstrate subluxation of the volar fragment with rotation into extension of the smaller dorsal fragment. These features are consistent with operative management of the injury. |
Transverse shaft fractures may take 3 to 4 months before being able to
resist maximum pinch force. For stable tuft and longitudinal fractures,
splints may be removed and functional use of the hand instituted as
soon as tolerated. Dorsal base fractures usually have the Kirschner
wires removed by 4 weeks with continued external protection for 2 to 3
more weeks when using traditional pinning techniques. The dorsal base
extension block method works through the institution of passive
extension exercises beginning at 4 weeks and coinciding with wire
removal. The more distal the injury is in the digit, the more
hypersensitivity to surface contact the patient is likely to have.
Desensitization through progressively more stimulating contact is the
earliest component of the rehabilitation program, with the goal of
reincorporating the fingertip into as many activities of daily living
as possible.
 |
|
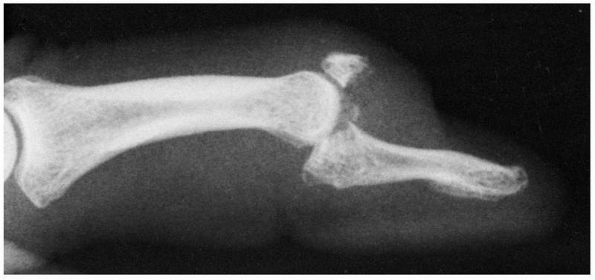
FIGURE 28-12 Dorsal base shearing articular fractures (A) can be stabilized by the extension block pinning technique (B) using two 0.045-inch K-wires.
|
 |
|
FIGURE 28-13 The steps of the extension block pinning method begin with (A) hyperflexion of the distal interphalangeal joint to draw the smaller dorsal fragment volarly where it is (B) blocked from returning into further extension by the first 0.045-inch K-wire. The larger volar fragment is then reduced (C) first at the articular surface to meet the dorsal fragment followed by (D) extension of the shaft to approximate the metaphysis, and maintained by the second K-wire (E).
|
and foam splint for a duration determined by the patient’s symptoms
alone. The time course for healing of the associated soft tissue injury
may well determine the total duration of disability far more than that
of the fracture itself. When the seal of the nail plate with the
hyponychium has been broken and the tuft fracture is displaced, this
represents an open fracture that should be treated on the day of injury
with direct nail bed repair. If the distal fragment is of substantial
size, the dorsal cortex of the distal phalanx that supports the nail
bed will provide a more level surface if pinned with one or more
0.035-inch K-wires for 4 to 6 weeks.
with CRIF with oblique 0.028- to 0.035-inch K-wires being used for the
rare displaced fracture. For unstable transverse shaft fractures, the
surrounding tissues usually impart enough rotational stability that a
single axial wire is sufficient. Depending on the size of the phalanx,
either a 0.045-or 0.035-inch Kirschner wire is appropriate. Care should
be taken to avoid penetration of the nail matrix tissues with the wire.
If the fracture is at mid-shaft level or more distal, the wire will
provide enough stability if driven to the subchondral base of the
distal phalanx only. Fractures occurring at the metadiaphyseal junction
may need to have the wire passed across the DIP joint to achieve
sufficient stability. Distraction at the shaft fracture site can easily
occur and should be avoided to diminish the possibility of nonunion.
One way to overcome this is with axial compression provided by a
variable pitch headless screw now offered in a micro size (Fig. 28-14).
This same technique can be used percutaneously to treat a fibrous
nonunion of a previous shaft fracture. The old standard had been to
leave pins emerging from the hyponychium for ease of removal later in
the office, but in the MRSA era, cutting them below the skin surface
guards against pin tract infection. The distal phalanx heals slowly,
often taking up to 8 weeks or longer. Fortunately, DIP joint
rehabilitation may proceed since the fracture is only deformed by
external application of pinch forces.
triangular dorsal fragment that is extended and translated by the pull
of the terminal tendon. With proper collateral ligament damage, the
larger articular fragment that is in continuity with the remainder of
the phalanx may sublux volarly. ORIF adds excessive surgical trauma to
this delicate set of tissues and the dorsal fragment is usually too
small to accommodate fixation devices passing directly through it
without experiencing comminution. The injury is best addressed by
extension block pinning. The DIP joint is hyperflexed, drawing the
dorsal fragment volarly to reach its natural position in relation to
the head of the middle phalanx. A 0.045-inch K-wire is then inserted at
the dorsal margin of the fragment (but not through the fragment) to
block it from returning to the retracted position under the influence
of the terminal extensor tendon (see Fig. 28-13).
The remainder of the distal phalanx consisting of the volar articular
fragment and shaft is then extended to meet the blocked smaller
fragment and restore articular congruity. A second 0.045-inch K-wire is
passed from P3 across the DIP joint into the middle phalanx. The wires
are retained for 4 weeks. Upon removal, passive extension exercises
further compress the two fragments and assist in the final stages of
cancellous bone healing. The treatment can still be executed up to 4 to
5 weeks after the initial injury, but the early callus that has formed
between the two fragments must be dispersed or satisfactory
approximation will not be achieved.
 |
|
FIGURE 28-14
Shaft fractures can be axially compressed to avoid nonunion resulting from distraction by using a variable pitch headless compression microsized screw placed over a guidewire. |
fractures represents a tense three-dimensional hydrodynamic unit that
will tend to expand when injured and forcibly distract fracture
fragments from each other resulting in nonunion frequently seen at this
level. The most common direction of displacement is in distraction.
Smooth sided K-wires are the most common fixation devices used for P3
fracture fixation but they can allow the fracture fragments to slide
along the surface of the wires. The best way to defeat this is to place
the wires as obliquely as possible and to use converging and diverging
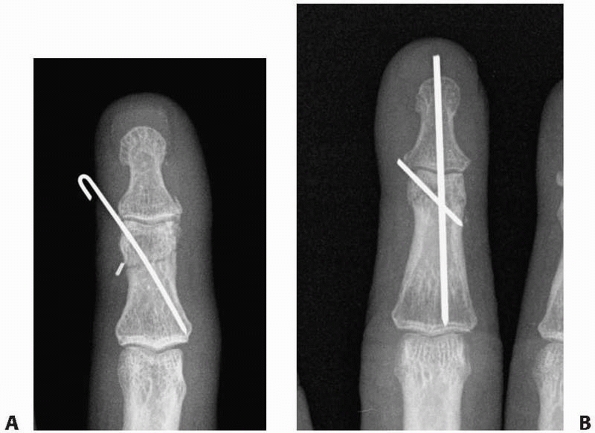
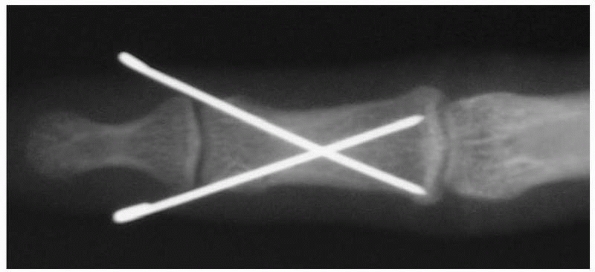
patterns (Fig. 28-15). When performing the
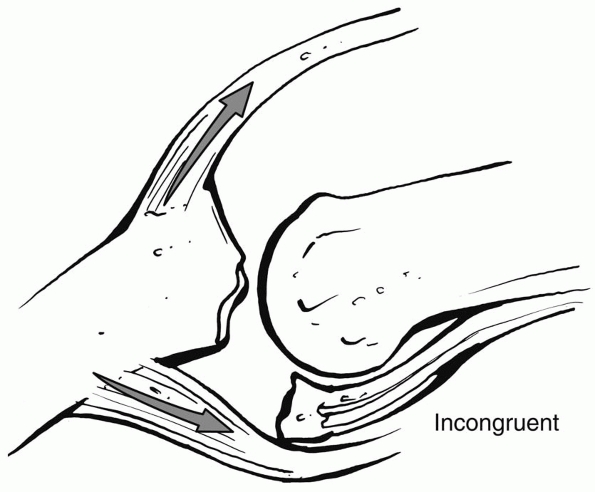
extension block pinning technique for dorsal base fractures, achieving
a truly congruent joint is difficult. There are two typical problems:
rotation of the smaller fragment into extension under the influence of
the terminal extensor tendon and cantilevering of the volar
articular-shaft fragment. A method to overcome the first problem is to
insert another K-wire percutaneously to hold pressure on the dorsal
cortex of the small fragment while placing the extension block wire.
The flat side of the wire rather than the sharp tip should be used for
this reduction maneuver. The surgeon holding the distal phalanx shaft
fragment manually and applying the extension force for reduction
creates the second problem. Instead of achieving a congruent joint
reduction, the larger fragment cantilevers and reduces at the
metaphyseal level but leaves an incongruent articular gap. Placing an
instrument handle, such as a Freer elevator, transversely across the
volar base just distal to the flexion crease and using the instrument
to apply the extension force directly at the level of the joint can
overcome this second problem. The reduction will first occur
congruently at the joint and then secondarily at the metaphysis.
opening of a fracture site, particularly at the base of the germinal
matrix. If reduction of a distal phalanx fracture with a visible dorsal
cortical gap on the lateral radiograph is not forthcoming, this
possibility must be considered and matrix extrication performed to
prevent both nonunion and nail deformity. Suturing the nail matrix can
be difficult. Friable nail matrix tissue is easily torn as the needle
is pushed rather than rolled along its axis during repair, a problem
that is compounded by the needle tip’s tendency to catch on the dorsal
cortex during the bottom of the stroke. These problems are overcome by
using a special 7-0 chromic suture with a spatula tipped needle that
can be passed with a rolling motion of the fingers when loaded on a
Castro-Viejo needle driver.
 |
|
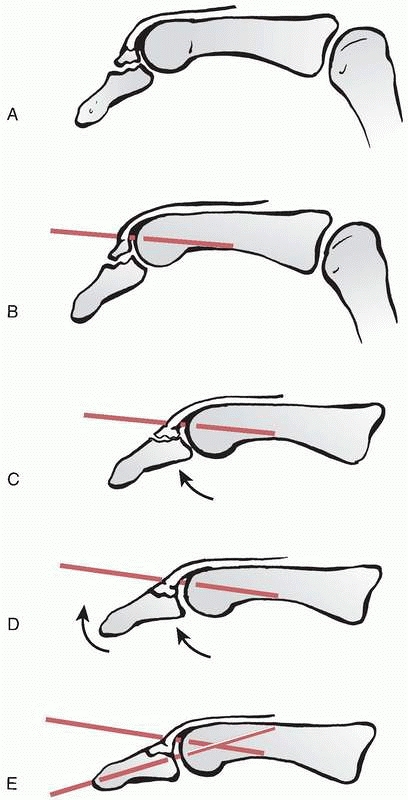
FIGURE 28-15 Fracture fragment sliding along the smooth shaft of the K-wire is prevented by (A) maximum oblique placement from one lateral edge of the tuft to the opposite far lateral corner of the base, (B) two wires targeting the lateral corners of the base, (C) converging wire patterns, or (D) diverging wire patterns.
|
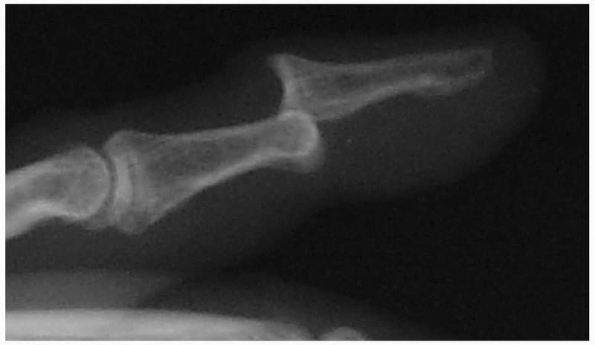
underappreciation and late presentation. Injuries are considered
chronic after 3 weeks. Pure dislocations without tendon rupture are
rare, usually result from ball-catching sports, are primarily dorsal in
direction, and may occur in association with PIP joint dislocations (Fig. 28-16). Transverse open wounds in the volar skin crease are frequent (Fig. 28-17). Injury to a single collateral ligament or to the volar plate alone at the DIP joint is rare.
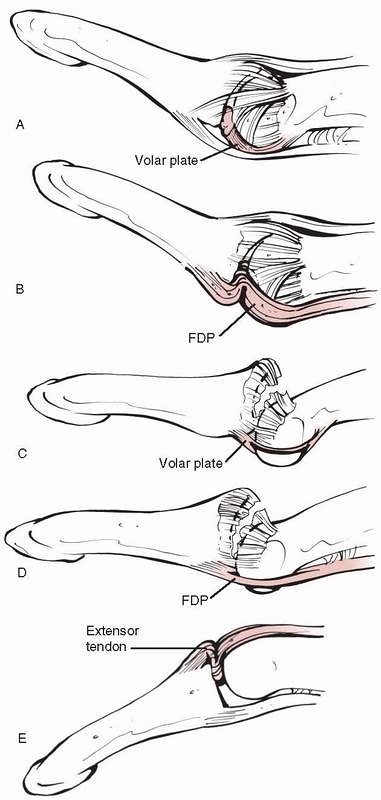
stabilized on each side by proper and accessory collateral ligaments
and the volar plate (Fig. 28-18). The proper
collateral ligaments insert on the lateral tubercles at the base of P3,
which also serve as the origin for the lateral ligaments to the tuft.
The accessory collateral ligaments attach distally to the lateral
margins of the volar plate. The volar plate of the DIP joint has a
proximal attachment weakly confluent with the distal extent of the
flexor digitorum superficialis (FDS) tendon but has no strong
check-rein ligaments like those at the PIP joint. This is in keeping
with the clinical observation of proximal volar plate detachment with
dorsal dislocation. The joint is inherently stable owing to articular
congruity and the dynamic balance of flexor and extensor tendons.
However, the DIP/IP joint is not as intrinsically stable as the PIP
joint and depends to a greater degree on its ligaments.
 |
|
FIGURE 28-16 Dislocations of the distal interphalangeal joint are nearly always dorsal.
|
axial rotation that are different for each finger and designed to
ensure conformity when the hand surrounds an object. The capacity for
passive DIP hyperextension is unique to modern humans, but the role
this plays in the etiology of dislocation is unclear. Irreducible
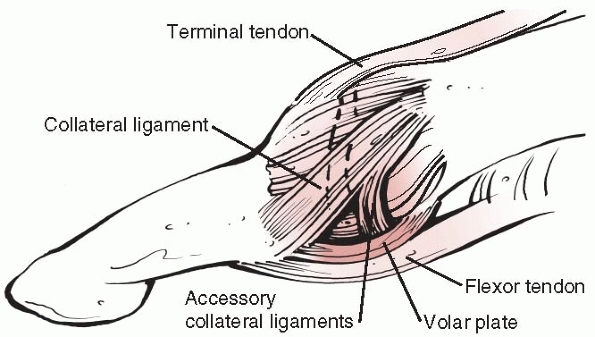
dorsal dislocations are thought to occur through a variety of different
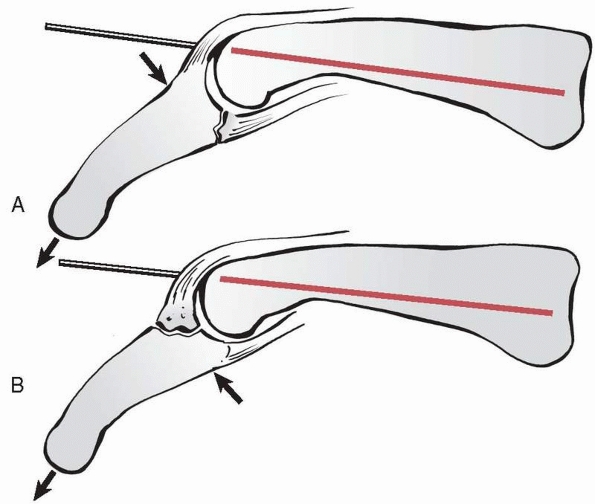
anatomic circumstances (Fig. 28-19). Reasons
include a trapped volar plate, the FDP being trapped behind a single
condyle of the middle phalanx (marked lateral displacement), the middle
phalanx buttonholed through the volar plate or through a rent in the
FDP. Volar dislocations may
also
be irreducible with the extensor tendon displaced around the head of
the middle phalanx. Thumb sesamoids or the volar plate may render an IP
joint dislocation irreducible.46,131
 |
|
FIGURE 28-17
Dorsal distal interphalangeal dislocations are often open with a transverse rent in the flexion crease from tearing rather than direct laceration. The wound should be débrided before reduction if possible. |
 |
|
FIGURE 28-18
The balanced forces of the terminal extensor tendon and the long flexor tendon dynamically stabilize the distal interphalangeal joint. The proper and accessory collateral ligaments and the volar plate provide static stability. |
AROM. The rare unstable dorsal dislocation should be immobilized in 20
degrees of flexion for up to 3 weeks before instituting AROM. The
duration of the immobilization should be in direct proportion to the
surgeon’s assessment of joint stability following reduction. Complete
collateral ligament injuries should be protected from lateral stress
for at least 4 weeks. When splinting at the level of the DIP/IP joint,
extreme caution must be exercised with regard to the vascularity of the
dorsal skin between the extension skin crease and the dorsal nail fold.
It is not only direct pressure but merely the angle of hyperextension
that can “wash out” the blood supply to this skin, potentially
resulting in full-thickness necrosis. This complication is thought to
occur at an angle representing 50% of the available passive
hyperextension of the DIP joint and can be identified by blanching of
the skin (Table 28-2).
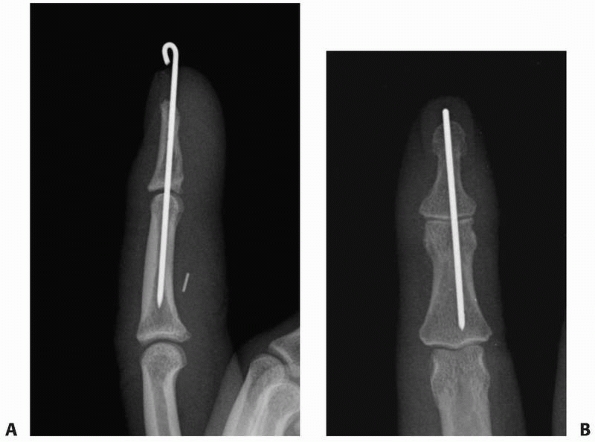
instability is great enough to require a brief period (3 to 4 weeks) of
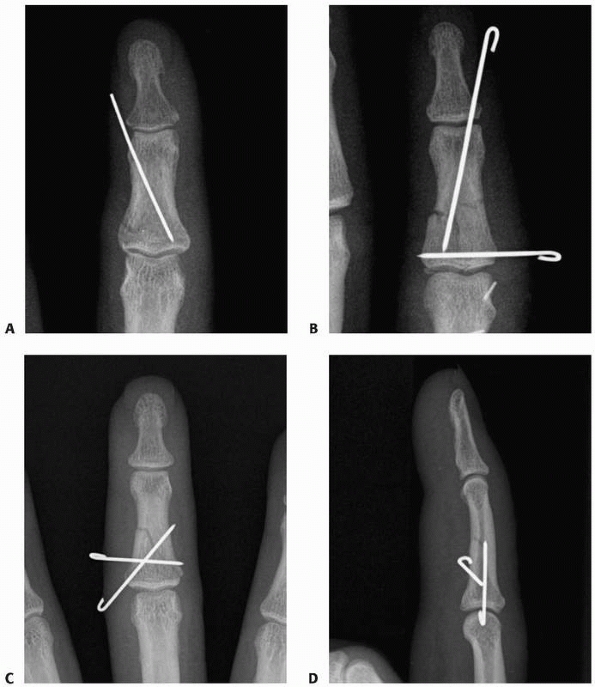
0.045-inch K-wire stabilization across the joint (Fig. 28-20). The need for added stabilization occurs primarily when aggressive rehabilitation is required for adjacent hand injuries.
joint may require open reduction to resect scar tissue and permit a
congruent reduction, but can result in additional postoperative
stiffness. In one study, 10 patients with chronic dorsal
fracture-dislocations of the DIP and IP joints (average, 8 weeks)
underwent a volar plate arthroplasty with 4 weeks of K-wire fixation
yielding a 42-degree average arc of motion for finger DIP joints and 51
degrees for thumb IP joints with an average flexion contracture of 12
degrees.126 Open dislocations
require thorough débridement to prevent infection. The need for
fixation with a K-wire should be based on the assessment of stability
and fixation is not necessarily required for all open dislocations. The
wire may be placed either longitudinally or on an oblique path. The
duration of pinning should not be longer than 4 weeks. The advantage of
longitudinal pinning is the absence of any lateral wire protrusion to
contact adjacent digits. The advantage of oblique pinning is the
ability to remove both sections of the wire should breakage across the
joint occur. When open reduction of the joint is required, a transverse
dorsal incision
at
the distal joint crease from midaxial line to midaxial line provides
ample exposure. Should additional exposure be required, midaxial
proximal extensions can be made.
 |
|
FIGURE 28-19 Irreducible dislocations of the distal interphalangeal joint occur due to (A) volar plate entrapment, (B) the flexor digitorum profundus being trapped behind a single condyle of the middle phalanx, (C) the middle phalanx being buttonholed through the volar plate, (D) the middle phalanx being buttonholed through a rent in the flexor digitorum profundus, and (E) the extensor tendon being displaced around the head of the middle phalanx.
|
|
TABLE 28-2 Distal Interphalangeal Joint and Thumb Interphalangeal Joint Dislocations
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||
treatment for most injuries. Should added pin stabilization prove
necessary because of recurrent instability, a single longitudinal
0.045-inch K-wire is sufficient. Closed reduction may seem to be
impossible. Interposed tissue is usually the cause and may include
volar plate, collateral ligament, or tendon. Longitudinal traction
rarely is successful in overcoming the blockade. Instead, proximal
joint positioning to relax the involved tendons and gentle rotation may
allow the interposed tissue to slip out of the joint.
 |
|
FIGURE 28-20 Closed reduction and internal fixation of the distal interphalangeal joint should ensure (A) a congruent articulation in neutral on the lateral view and (B) neutral pin placement on the anteroposterior view.
|
The most distal of the major extensor creases corresponds to the joint
level. Proximal extensions of 5 mm made in the midaxial lines create a
small trapdoor effect that gives ample exposure for any procedure. The
terminal extensor tendon or extensor pollicis longus should be
protected. Using a single-prong skin hook is a gentle method to control
the tendon without grasping and crushing its fibers with forceps while
working to achieve reduction. One must search for small chondral or
osteochondral injuries primarily for the purpose of removing the
fragments from the joint to prevent subsequent third body wear.
are impaired wound healing and hypersensitivity. Dissecting and
preserving longitudinal venous channels during the surgery facilitates
venous drainage of the narrow skin flap between the wound and the
dorsal nail fold. There is usually one major group of veins directly in
the midline overlying the extensor tendon and one major group at each
dorsolateral corner. The lateral venous groups are accompanied by the
distal branches of the dorsal digital nerves. Transection of these
small nerve branches with the subsequent formation of small neuromas
adherent to the wound may be one
reason
for the high incidence of hypersensitivity in this region. The initial
surgical incision should be just through dermis only, followed by
careful longitudinal dissection of these neurovascular structures under
magnification before proceeding with the remainder of the surgery. An
additional nonoperative pitfall is the development of imbalance
following splinting, perhaps as a result of failure to monitor the
physical examination at each time point during healing.
 |
|
FIGURE 28-21
The safest surgical approach to the distal interphalangeal joint with respect to skin blood supply is transverse in the distal extensor crease with midaxial proximal extensions as needed not exceeding 5 mm. |
the intraarticular fractures that occur at the base of the middle
phalanx. These are perhaps the most functionally devastating of all
fractures, and dislocations of the hand and the most technically
difficult to treat. Many other fracture patterns that occur in the
middle phalanx are the same as those patterns seen in the proximal
phalanx. The literature rarely distinguishes between P1 and the middle
phalanx when reporting on the phalangeal fractures, and the majority of
the published data on this subject is covered in the section on
proximal phalanx fractures later in the chapter.
 |
|
FIGURE 28-22 Fracture patterns of the middle phalanx other than the specific base patterns discussed later include (A) intra-articular fractures of the head, (B) oblique shaft fractures, (C) longitudinal shaft fractures, and (D) transverse shaft fractures.
|
Tendon insertions that play a role in fracture deformation include the
central slip at the dorsal base and the terminal tendon acting through
the DIP joint. The flexor digitorum superficialis has a long insertion
along the volar lateral margins of the shaft of the middle phalanx from
the proximal fourth to the distal fourth. Fractures at the neck of the
middle phalanx will usually angulate apex volar as the proximal
fragment is flexed by the FDS and the distal fragment is extended by
the terminal tendon (Fig. 28-23). Those at the
base will usually angulate apex dorsal as the distal fragment is flexed
by the FDS and the proximal fragment is extended by the central slip.
Despite the theoretical resolution of these force vectors, actual P2
are less predictable and subject to any variety of displacement
patterns. Axial loading patterns of injury may produce unicondylar or
bicondylar fractures of the head or intra-articular fractures of the
base. Base fractures can be divided into partial articular fractures of
the dorsal base, volar base, and lateral base or complete articular
fractures that are usually comminuted and often referred to as “pilon”
fractures.
“Pilon” fractures are unstable in every direction including axially.
 |
|
FIGURE 28-23
The insertions of the flexor digitorum superficialis, the flexor digitorum profundus, and the components of the extensor apparatus typically cause fractures in the distal fourth of the middle phalanx to angulate apex volar and those in the proximal fourth of the middle phalanx to angulate apex dorsal. |
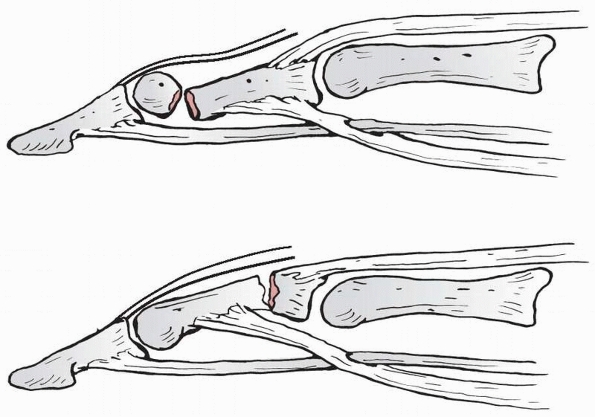
challenging ones in which to restore function, the force vectors of
volar base fractures are perhaps more interesting. Fractures at the
volar base of the middle phalanx can be particularly unstable in direct
relation to the percentage of articular surface involved. When the
volar fragment constitutes greater than around 40% of the articular
surface, this fragment carries the majority of the proper collateral
ligament insertion in addition to the accessory ligament and volar
plate insertions (Fig. 28-24). The dorsal
fragment and remainder of the middle phalanx will thus sublux
proximally and dorsally with displacement being driven by the pull of
the FDS and the central slip (Fig. 28-25). The
joint then hinges rather than glides, pivoting on the fracture margin
of the dorsal fragment and destroying articular cartilage on the head
of P1.
The presence of comminution alone does not necessitate surgery. When
crushing is the mechanism of injury, the periosteal envelope may remain
relatively intact as long as fracture displacement is not significant.
Degree of displacement is more related to inherent stability than the
direction or number of fracture planes. Nevertheless, certain patterns
are more stable than others. Transverse fractures are more stable than
long oblique or spiral fractures, both of which tend to shorten and
either laterally deviate or rotate to cause interference patterns with
neighboring digits. Splinting is confined to the digit alone with
dorsally applied aluminum and foam or custom orthoplast splints. Motion
rehabilitation should be initiated by 3 weeks postinjury with interim
splinting until clinical signs of healing are present (but not longer
than 6 weeks).20 Side strapping to an adjacent digit usually provides sufficient protection from external forces after the first 3 weeks.
 |
|
FIGURE 28-24
When the volar fragment of the base of the middle phalanx comprises more than 40% of the joint surface, the collateral ligaments attach to the volar, rather than the dorsal, fragment rendering the dorsal fragment with the shaft unstable in extension. |
 |
|
FIGURE 28-25
The central slip of the extensor tendon and the flexor digitorum superficialis serve as prime deforming forces for dorsal subluxation in volar base P2 fractures. |
base fractures is extension block splinting. Fractures at the volar
base of the middle phalanx that involve less than 40% of the articular
surface can usually be managed effectively with extension block
splinting. The key to success with this treatment is absolute
maintenance of a congruent reduction, avoiding the hinge motion that
occurs with dorsal and proximal subluxation of the major fragment.
Correct application of a dorsal extension block splint requires
maintenance of contact between the dorsum of the proximal phalangeal
segment and the splint. If the digit is allowed to “pull away” from the
splint volarly, the PIP joint can extend beyond the safe range,
subluxate, and negate the desired effect of the splint. Once the splint
is in place, weekly follow-up with a true lateral radiograph of the PIP
joint is mandatory to monitor the advancement of extension at a rate of
around 10 degrees per week (see later for details of extension block
splinting).
the condyles to maintain a level distal articular surface at the DIP
joint. A second wire passed obliquely to the diaphysis of the opposite
cortex will prevent lateral migration of the condylar fragment along
the smooth shaft of the first wire, which would create an articular gap
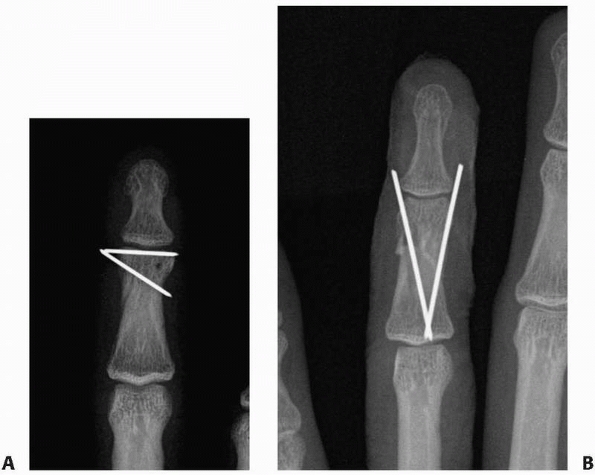
(Figs. 28-26 and 28-27).
This second wire also controls the rotation of the fragment in the
sagittal plane that can occur with single-wire fixation alone. If the
patient presents late or soft tissue lies interposed in the fracture
plane between condyles, achieving an accurate closed reduction is
unlikely and open reduction may be required. Once opened, the
opportunity for threaded lag screw fixation exists as opposed to smooth
K-wire fixation. If the condylar fragment does not have a diaphyseal
extension, then the location for lag screw placement is directly
through the collateral ligament, which may negate the screw’s
theoretical advantage over two diverging K-wires in terms of early
motion.
|
TABLE 28-3 Middle Phalanx Fractures Not Involving the Proximal Interphalangeal Joint
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||
|
TABLE 28-4 Volar Base Fracture Dislocations of the Middle Phalanx at the Proximal Interphalangeal Joint
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
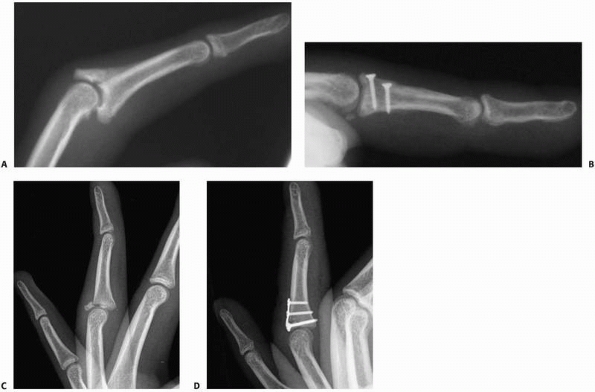
Kirschner wires that cross in the middle of the shaft produce a less
stable pattern of fixation particularly if the fracture is located at
the level where the wires cross. For transverse or short oblique
patterns, K-wire placement other than the crossing pattern may be
difficult to achieve without violating either the DIP or PIP joint or
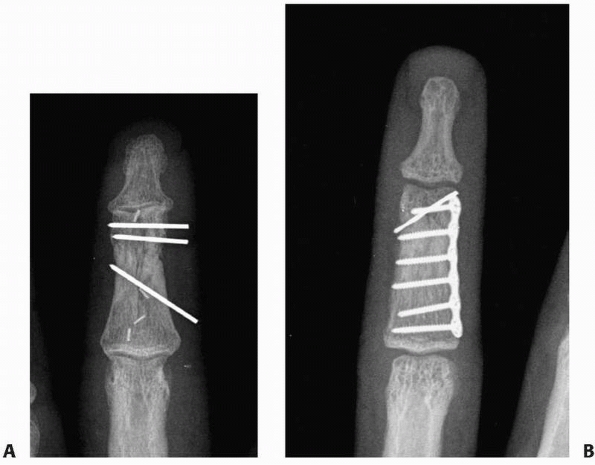
directly penetrating a tendon (Fig. 28-29).
Long oblique or spiral shaft fractures are amenable to relatively
transverse placement of K-wires without joint or tendon penetration.
When rotational alignment cannot be effectively
restored
by closed means, interfragmentary lag screw fixation is usually quite
effective for spiral fractures. When comminution or axial instability
is present, a limited number of P2 fractures may actually be most
appropriately treated with plate and screw fixation (Fig. 28-30).
|
TABLE 28-5 “Pilon” Complete Articular Fractures of the Base of the Middle Phalanx
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||
An average PIP joint ROM of 91 degrees was achieved following CRIF of
dorsal base fractures despite an extensor lag of over 10 degrees in 5
of 9 patients.127 Extension block
pinning for 3 weeks or even longer to treat volar base fractures has
been used with success in limited numbers of patients.162,167
Ten patients with 16-year follow-up of transarticular pins for 3 weeks
with 2 additional weeks of extension block splinting achieved an
average 85-degree arc of motion with an 8-degree flexion contracture
and no severe degenerative changes.115
Another study compared transarticular fixation (eight patients) to ORIF
with lag screws (six patients) or ORIF with cerclage wires (five
patients). At 7-year mean follow-up, cerclage wires produced the
smallest arc of motion (median, 48 degrees) compared with pinning
(median, 75 degrees). Eleven of the 19 total patients healed with some degree of incongruence or frank subluxation.2
 |
|
FIGURE 28-26
Condylar fractures at the head of the middle phalanx tend to slide along the pin interface producing an articular gap and/or step-off. A. Unicondylar fractures require diverging wires to prevent fragment separation. B. In bicondylar fractures, converging wires are used to prevent fragment separation. |
 |
|
FIGURE 28-27 More complex bicondylar fractures can be stabilized by either (A) multiple wires in different planes or (B) a lateral plate and screws.
|
 |
|
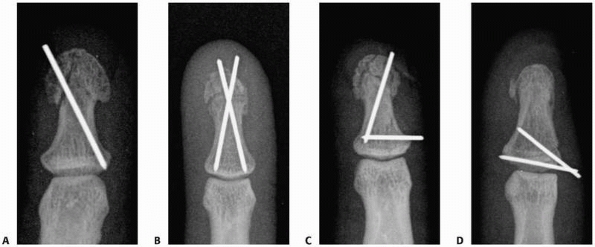
FIGURE 28-28 Fractures of the neck of the middle phalanx can be pinned with (A)
a single oblique pin only when local soft tissues and the geometry of the fracture itself add some inherent stability. Correct placement is from the collateral recess distally to the opposite corner of the metaphyseal base. B. If there is a concomitant zone II extensor tendon repair needing protection, pinning can include the distal interphalangeal joint with an oblique wire in the middle phalanx to prevent axial rotation. |
 |
|
FIGURE 28-29 Shaft fractures of the middle phalanx can be stabilized with (A) a single oblique pin from the collateral recess to the opposite base if relatively stable upon reduction, (B) converging wires in different planes when added stability is needed, or (C,D) diverging wires.
|
base fractures is a force couple device that works to dynamically
reduce the tendency for dorsal subluxation of the middle phalanx17 (see Table 28-4).
Acute volar base fractures involving more than 40% of the joint surface
and those with subacute or chronic residual subluxation can be treated
with volar plate arthroplasty.36
Seventeen patients followed at 11.5 years demonstrated a TAM of 85
degrees when operated on within 4 weeks of injury and 61 degrees when
operated on later than 4 weeks from injury.36
A series of 56 patients with volar base fracture-dislocations treated
by either volar plate arthroplasty (23 of 56) or ORIF (33 of 56)
yielded at 46-month follow-up minimal pain in 83% but radiographic
evidence of degenerative changes in 96%.34
Seven patients undergoing lag screw fixation within 2 weeks of injury
achieved an average PIP joint ROM of 100 degrees with a similar group
of seven patients operated after 2 weeks achieving an average of 86
degrees.66 Another 12 digits followed-for an average of 8.7 months after lag screw ORIF demonstrated combined PIP
and DIP motion arcs that averaged 132 degrees.96
When followed at an average of 42 months from surgery, 9 similar
patients demonstrated an average PIP range of 70 degrees with a
14-degree flexion contracture.68
Even displaced fractures more than 5 weeks from injury can be carefully
corrected at the articular surface and supported by bone graft using
the volar “shotgun” exposure.32 An interesting alternative procedure offered by Weiss172
and performed through the same “shotgun” volar exposure is that of
cerclage wiring of the base of the middle phalanx, which resulted in an
average PIP ROM of 89 degrees for 12 patients. When comminution is
excessive, restoration of the volar buttress with true hyaline
cartilage is possible using a hemi-hamate osteochondral autograft.
Thirteen patients treated with this strategy at an average of 45 days
postinjury for comminution of the volar 60% of the the middle phalanx
base had an average PIP 85-degree arc of motion at 16-month follow-up.175
 |
|
FIGURE 28-30 More complex shaft fractures (A) can be stabilized by (B,C) multiple lag screws or (D) a lateral plate and screws.
|
 |
|
FIGURE 28-31
Extension block pinning includes at least one K-wire placed into the intercondylar notch of the proximal phalanx to prevent dorsal displacement of the base of the middle phalanx and a second interfragmentary wire may be added in the base of the middle phalanx itself. |
 |
|
FIGURE 28-32 Extension block pinning is a closed strategy for managing (A) volar base fractures of the middle phalanx and (B) dorsal base fractures of the middle phalanx.
|
 |
|
FIGURE 28-33 Volar base fractures of the middle phalanx allow the shaft and dorsal base fragment to (A) sublux dorsally and proximally resulting in hinge, rather than gliding, motion. Fixation of the volar base fragment must (B) restore the volar lip buttress against subluxation and recreate a congruent articulation.
|
 |
|
FIGURE 28-34 Strategies for managing “pilon” fractures at the base of the middle phalanx include (A) an adjustable unilateral hinged external fixator with distraction capabilities, (B) a wire spring construct, (C) the original configuration of pins and rubber bands, and (D)
the same foundation augmented with an additional transverse wire across the metaphyseal base of the middle phalanx to resist dorsal subluxation. |
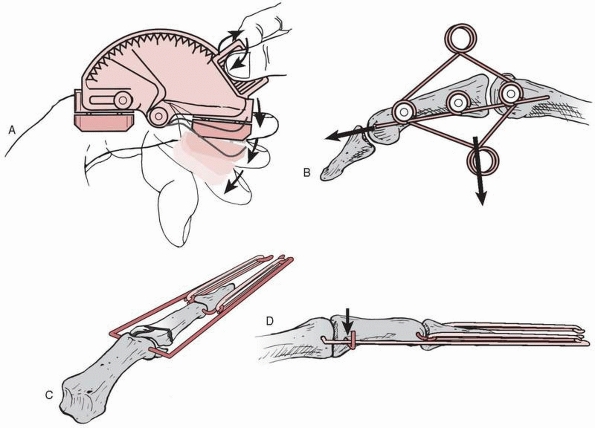
joint are “pilon” fractures that involve the complete articular surface
combined with metaphyseal compaction (Table 28-5).
These are highly unstable injuries refractory to standard surgical
techniques. Although other adverse events such as pin tract infection
may intercede, the primary complication is stiffness. Unique forms of
treatment have been devised for these injury patterns involving
“dynamic traction.”8,42,106,129,134,152,157 An alternative design uses a dorsal spring mechanism.45
The general principle is to establish a foundation at the center of
rotation in the head of P1. From this foundation, traction (adjustable
or elastic) is applied along the axis of the middle phalanx to hold the
metaphyseal component of the fracture out to length while allowing
early motion to remodel the articular surface (Fig. 28-34).
Dynamic traction with pins and rubber bands in 14 patients followed for
2.5 years produced average PIP motion of 74 degrees and a TAM of 196
degrees.106 Dynamic fixation with
wires but not elasticity in eight patients yielded a final average
motion of 12 to 88 degrees following wire removal at 6 weeks.85 Ideally, the patient should begin treatment acutely compared with delayed
application of the device.23 Many types of device constructs are possible (Fig. 28-35).
The simplest constructs involve only K-wires and rubber bands.
Thirty-four patients from the armed services achieved a final average
arc of motion at the PIP joint of 88 degrees and the DIP joint of 60
degrees using such a device with eight pin tract infections.129 Another group of nonmilitary personnel achieved average PIP arcs of 64 degrees and DIP arcs of 52 degrees.157
With the traction left in place for only 3.5 weeks on average, an
average PIP arc of 94 degrees and thumb IP arc of 62.5 degrees was
achieved in six total patients.134
Another six patients having the device removed between 3 and 4 weeks
achieved average PIP range from 5 degrees to 89 degrees with two pin
tract infections.8 In another
series, by an average of 26 months postoperatively, five of eight
patients already demonstrated step-off deformities or arthritis.42
 |
|
FIGURE 28-35 A hinged external fixator can be used to control “pilon” fractures beginning with (A)
the placement of a transverse K-wire through the center of proximal interphalangeal rotation in the head of the proximal phalanx, followed by assembly of the device around that foundation wire. If performed correctly, the result will be (B) a congruent joint when healed. |
digital splints for 3 weeks or less and protected early motion
thereafter with side strapping to an adjacent digit until clinically
healed. Unstable but not comminuted fractures of the shaft can be
treated well by temporary (3 weeks) closed pinning (Fig. 28-36).
There are a few spiral fractures for which closed reduction will not
achieve satisfactory control of rotation such that lag screw fixation
with 1.2-mm screws is preferable to closed pinning techniques. These
treatment strategies are also used in proximal phalanx fractures and
more detail may be found in that subsequent section of the chapter.
block pinning is an excellent treatment. The principles are all the
same as described above for extension block pinning of dorsal base
fractures in the distal phalanx. At the base of the middle phalanx, the
larger dorsal fragment (compared with the base of P3) is easier to work
with and manipulate, but the PIP joint (compared with the DIP joint)
imposes greater demands for a perfectly congruent joint reduction
because of its more important role in overall digital function. The
volar articular and shaft fragment is almost always subluxated
proximally
and volarly. When more than 10 to 14 days have passed since injury, it
can be quite difficult (because of early soft tissue contracture) to
achieve a closed reduction of this fragment relative to the head of P1.
It is for these reasons that late presenting dorsal base fractures are
often better managed with ORIF to ensure the clearance of consolidating
hematoma from between the fragments and exact approximation of the
articular reduction (Fig. 28-37).
In this setting, fixation with two 1.2-mm lag screws affords enough
stability to pursue early motion. Use of the countersink tap is
important to minimize dorsal prominence of the screw heads and to avoid
pressure concentration that might comminute the still relatively small
dorsal fragment. Even though the surgical procedure occurs distal to
extensor zone IV, a priority still must be placed on active extensor
tendon excursion during rehabilitation to avoid a long-term extensor
lag. Intraoperative assessment of the stability of the fixation will
guide the progression of rehabilitation to ensure against fixation
failure, recognizing the small size of the thread purchase in
cancellous rather than cortical bone at the metaphyseal base of the
middle phalanx.
 |
|
FIGURE 28-36
The relative biomechanical inferiority of K-wires crossing at the midshaft of the phalanx is offset by the lesser demands placed on the middle phalanx during rehabilitation than on the proximal phalanx and the advantage of avoiding articular penetration to achieve a closed pinning. |
of the joint surface rarely require surgery unless presenting late with
an incongruent joint. When seen acutely, these fractures are well
managed with extension block splinting that begins at around 40 degrees
and advances 10 to 15 degrees per week for the first 3 weeks. If the
extension block splint cannot be eliminated in 3 weeks’ time, this
treatment strategy may not be appropriate. Fractures constituting more
than 25% but less than 40% of the joint surface pose a difficulty in
treatment planning as they constitute an intermediate group where the
disadvantages of the two primary options are relatively well matched.
It is difficult to predict in advance how the disadvantages will play
out over the course of treatment for an individual patient. The
disadvantage of extension block splinting or pinning is that with a
greater amount of joint surface involved, the blocking must begin at a
higher angle and it will take longer to achieve full extension. A
permanent fixed flexion contracture is the consequence to be avoided.
This must be compared with the overall tendency for loss of joint
motion associated with ORIF or open reconstruction.
 |
|
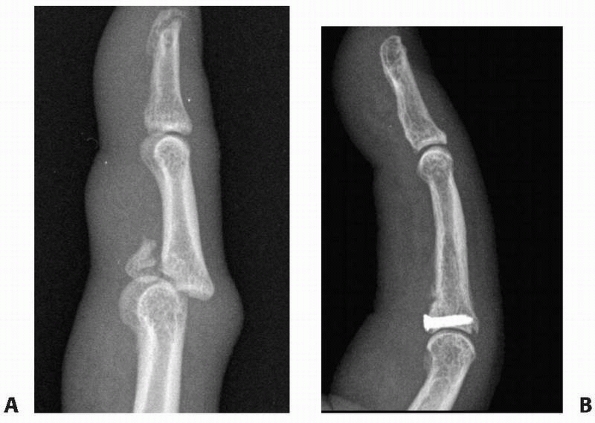
FIGURE 28-37 Dorsal base fractures allow (A) the volar articular fragment and the attached shaft of the middle phalanx to sublux volarly and proximally. (B)
A congruent joint is restored with sufficient stability to initiate early rehabilitation by lag screw fixation. An alternative fixation strategy is (C,D) a small custom-cut hook plate. |
of the joint surface, an open procedure offers the greatest assurance
of achieving a congruent joint as a final result. The distinction
between ORIF for one or two relatively large fragments or open
reconstruction for highly comminuted multiple fragments cannot often be
made until the time of surgery. One should always be prepared for both
possibilities in the preoperative planning discussions with the
patient. Dorsal base fractures usually provide a single fragment of
reasonable size for direct lag screw fixation. Volar base fractures are
not so easy. One or two large fragments that facilitate lag screw
fixation are the exception rather than the rule. In this case, two
1.2-mm lag screws are appropriate. Placement is side by side with one
screw in the radial half of the base fragment
and
other in the ulnar half. If two separate radial and ulnar volar base
fragments are found, this strategy is still acceptable provided that
the fragment diameter is at least three times the screw diameter and
compression can be achieved without causing fragment comminution. The
countersink tap is useful in this regard. The operative approach is the
same as described for reconstruction of a collection of comminuted
fragments.
second over the middle phalanx. The flexor tendon sheath is reflected
as a single rectangular flap hinging on its lateral margin between the
distal margin of the A2 pulley and the proximal margin of the A4
pulley. The FDS and FDP are retracted laterally, one to either side,
and the collateral ligament origins are dissected as a sleeve from the
lateral surfaces of the head of P1. Release of the volar plate allows
complete hyperextension of the PIP joint and presentation of both joint
surfaces toward the surgeon. This is the so-called “shotgun” approach,
and its variations center on the management of the volar plate. This
approach is also used for volar plate arthroplasty and ORIF. In the
former procedure, the volar plate is released distally so that it may
be advanced to replace the defect in the volar articular surface. In
the latter, it should remain attached to the fragments as an important
source of blood supply. When performing a reconstruction of irreparable
comminution, the volar plate may be released along its distal margin.
The defect in the volar articular surface may range anywhere from 40%
up to almost 90%, often with irregular margins. A small saw or burr
should be used to straighten the irregular margins into sharp
orthogonal cuts that define a clear bed of cancellous bone in the
metaphysis that can be accurately measured for reconstruction. The
articular surface at the base of the middle phalanx has a sagittally
oriented ridge that interdigitates with the recession between the two
condyles at the head of P1. This relationship is important not only for
preserving joint congruence but for maintaining stability in the
setting of the collateral ligament releases. An excellent geometric
match has been found in the distal articular surface of the hamate at
the ridge that separates the ring from the small finger CMC joints. The
measurements taken from the defect at the base of the middle phalanx
are transposed to the hamate and a small saw and osteotomes are used to
remove the osteochondral graft from its donor site. The graft is then
exactly trimmed to match the defect and secured with two 1.2-mm lag
screws (Fig. 28-38). The joint is checked
clinically and radiographically for maintenance of congruence through a
full ROM. The flexor sheath is reapproximated with 6-0 monofilament
sutures and the PIP joint splinted for protection. Immediate active
motion rehabilitation is begun within days of surgery.
phalanx may be treated by entirely closed reduction and stabilization.
If significant metaphyseal bone loss is present or if the articular
fragments at the base of the middle phalanx do not reduce sufficiently
with traction alone, a small incision can be made through which
cancellous bone graft can be added to fill the metaphyseal void and to
assist in supporting a reduction of the articular fragments. Transverse
0.035-inch K-wires may be placed at the subchondral level to maintain
the articular relationships. The fracture must then be reduced at the
metaphyseal level and undergo stabilization sufficient to withstand the
rigors of early motion that must accompany the rehabilitation of
articular fractures. It is at this point that the significant
variations in technique arise along with different devices available
for stabilization. My preference is for an off-the-shelf unilateral
hinged external fixator with a manual adjustment for longitudinal
traction. The device itself allows either free AROM with a gear
disengaged or passive range of motion (PROM) with the gear engaged (see
Fig. 28-35). Active motion with the device in
place should be checked with fluoroscopy to ensure that congruent
motion rather than hinge motion is occurring at the PIP joint. For this
reason, these cases should be done under digital block, and the need
for AROM by the patient should be explained before the procedure.
Motion rehabilitation is initiated immediately and continued until
final healing. The patient’s performance of hourly motion exercises
often causes significant pin irritation to the point of necessitating
an early removal before the planned 4 weeks. Any external fixator
device for a “pilon” fracture is not well appreciated by the patient.
Some “pilon” fractures are amenable to ORIF, and this is a
well-received option by patients provided that stable fixation is
achieved and the result maintained during the stress of therapy (Fig. 28-39).
steps in performing volar base osteochondral graft reconstructions. The
first is to establish sharp and flat borders in the metaphyseal defect
to receive and inset the graft stably with broad cancellous surfaces
for rapid bone healing. The second critical step is trimming the
graft
to fit this bed. The common pitfall is to set the graft’s articular
surface perpendicular to the neutral axis of the bone. This fails to
reestablish the volar buttress and a truly congruent joint surface. If
the graft is cut correctly, once inset it should replicate the
buttressing function of the native volar base and prevent dorsal
dislocation.
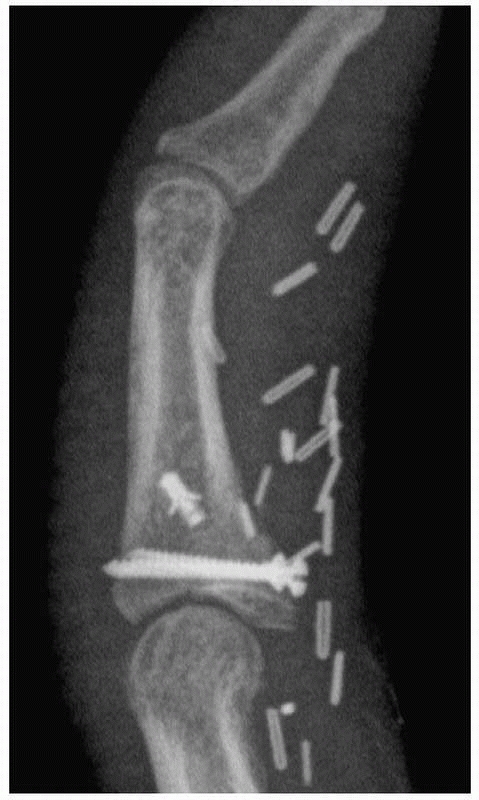 |
|
FIGURE 28-38
Volar base fractures with comminution of a substantial portion of the articular surface and subluxation can be reconstructed with an osteochondral graft from the hamate with particular emphasis placed on recreating the volar lip buttress and a truly congruent reproduction of the radius of curvature. |
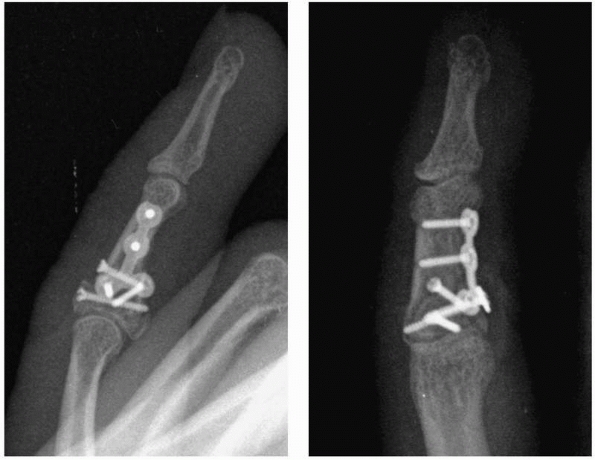 |
|
FIGURE 28-39
Some “pilon” fractures are amenable to open reduction and internal fixation, which then avoids the complications of pin tract infection associated with the dynamic traction strategies. |
the unilateral hinged fixator, repeated checks on orientation of the
device as a whole are needed to prevent progression to malunion. The
majority of the mistakes cause the hinge on the device to rotate along
a different axis than the joint itself.
from the neutral axis of the bone at the P1 level than the the middle
phalanx level or to have the pins entering the phalanges obliquely
rather than in the true mid-axial plane. Above all, the surgery should
be performed under a local anesthetic with the patient demonstrating
true active PIP joint motion under fluoroscopy to judge the maintenance
of congruence throughout the ROM. Finally, there must be no tension in
the skin around the pins, as the hourly motion performed in
rehabilitation will promote pin tract infections.
diagnoses that are passed off as “sprains.” Although a large number of
incomplete injuries occur (especially in ball-handling sports),
complete disruptions of the collateral ligaments and the volar plate
are also frequent. Since dramatic swelling is often present even with
minor injuries to the PIP joint, this sign may often get dismissed by
initial examiners of the patient. Careful palpation for localized
tenderness may direct attention to one of the collateral ligaments, the
volar plate, or the insertion of the central slip. The capacity for
active PIP extension against resistance from a starting position of PIP
flexion confirms the integrity of the central slip. Limitation of
passive DIP flexion while the PIP joint is held in extension may appear
several weeks following the initial injury and signify a developing
boutonnière deformity. Congruence on the lateral radiograph is the key
to detecting residual subluxation. Correct axial rotational alignment
is demonstrated when both P1 and the middle phalanx are seen in a true
lateral projection on the same film.
as opposed to fracture-dislocations where it is the chief issue at
stake. It manifests as hyperextension laxity following volar plate
injuries managed with an inadequate initial degree of extension
blocking. Correction of hyperextension instability can be performed
with either delayed reattachment of the volar plate or a
capsulotenodesis reconstruction. In pure dislocations, stiffness is the
primary concern. Stiffness can occur following any injury pattern and
responds best at the late stage to complete collateral ligament
excision.33,100
Chronic missed dislocations require open reduction with a predictable
amount of subsequent stiffness. Patients should be counseled to expect
permanent residual enlargement of the joint and for the final
resolution of stiffness and aching to take as long as 12 to 18 months.
metacarpal. There is no cam effect. The head is bicondylar, and the
collateral
ligaments
originate from the center axis of joint rotation. Never theless, the
accessory collateral ligaments and volar plate are lax in flexion and
will become contracted if immobilized in that position. At the volar
base of the middle phalanx, there are tubercles for the confluence of
the proper and accessory collateral ligaments with the volar plate.
This junction is referred to as the “critical corner.” This three-sided
box design provides excellent inherent joint stability (Fig. 28-40).
The volar plate anatomy is unique at the PIP joint with the presence of
strong check-rein ligaments that originate inside the margins of the A2
pulley confluent with the C1 pulley fibers and the oblique retinacular
ligament. The distal insertion of the volar plate is strong only at its
lateral margins. The undersurface of the central slip has an
articulating fibrocartilage that may aid in stabilization, prevent
central slip attenuation, and increase the extensor moment arm.
Although primarily a hinge, the PIP joint accommodates 7 to 10 degrees
of lateral deviation and slight axial rotation. The normal ROM may be
up to 120 degrees of flexion. In contrast to the other small joints of
the hand, PIP joint volar plate disruptions usually occur distally. The
proper collateral ligaments are the primary stabilizers to lateral
stress, and a greater than 20-degree opening signifies complete
disruption. Collateral ligament disruption is usually proximal, but the
fibers traditionally stay positioned over their anatomic origin for
subsequent healing.
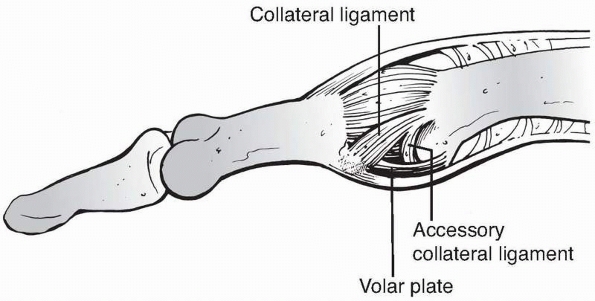 |
|
FIGURE 28-40
The proximal interphalangeal joint receives static stability from the proper and accessory collateral ligaments and the volar plate, supplemented by the dynamic stability of the dorsal plate and other balanced tendon forces acting across the joint. |
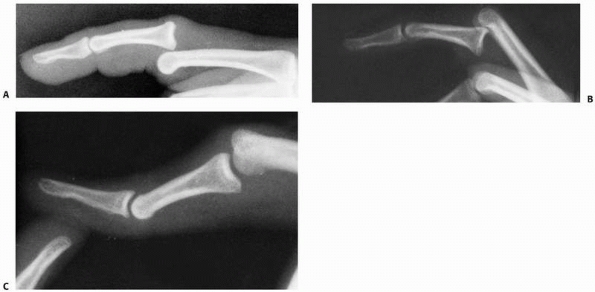 |
|
FIGURE 28-41 Three variants of proximal interphalangeal dislocation are seen. A. The most common, dorsal, (B) pure volar with central slip disruption, and (C)
volar rotatory (note that the middle phalanx is seen as a true lateral, whereas the proximal phalanx is seen in oblique profile). |
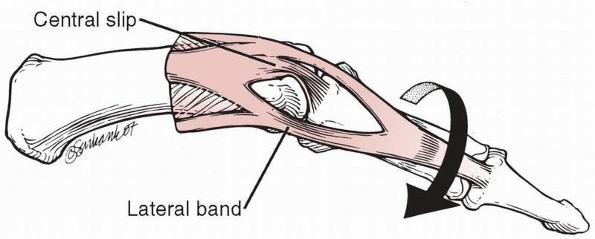 |
|
FIGURE 28-42
In volar rotatory dislocations, the head of the proximal phalanx protrudes between the intact central slip and one lateral band, which create a noose effect, preventing reduction, especially if longitudinal traction is applied. |
collateral ligament injury are dorsal dislocation, pure volar
dislocation, and rotatory volar dislocation (Fig. 28-41).
Dorsal dislocations involve volar plate injury (usually distally, with
or without a small flake of bone). For pure volar dislocations the
pathologic findings are consistently damage to the volar plate, at
least one collateral ligament, and the central slip. Rotatory volar
dislocation occurs as the head of P1 passes between the central slip
and the lateral bands, which can form a noose effect and prevent
reduction (Fig. 28-42). Irreducible dislocations obstructed by the volar plate or flexor tendons are uncommon injuries.
(strapped to an adjacent digit) AROM (Table 28-6).
Fortunately, the majority of hyperextension injuries remain congruent
even at full extension and do not require extension block splinting.
However, one must consider that the distal volar plate is poorly
vascularized, and a lack of early healing may lead to chronic
hyperextension laxity. Lower-profile digitally based splints or buddy
taping may effectively prevent the full extension that could threaten
sound volar plate healing. When formal extension block splinting is
chosen (usually only in the situation of fracture-subluxation), the
rate of progression each week is determined by the severity of the
initial injury but should reach full extension no later than 4 weeks
from injury.
|
TABLE 28-6 Proximal Interphalangeal Joint Dislocations
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||
occurs and will result in a boutonnière deformity if not treated
properly. Careful examination consisting of PIP extension against
resistance from a starting position of full flexion will prevent
missing the diagnosis of a central slip disruption. Limitation of
passive DIP flexion is an early sign of a developing boutonnière
deformity. Even when identified late, the treatment of choice is
extension splinting at the PIP joint with immediate active DIP blocking
exercises. Active DIP flexion pulls the whole extensor mechanism
(including the ruptured central slip) distally through the intact
lateral bands. The duration of PIP extension splinting is usually 4 to
6 weeks with a transitional period of night splinting for several
additional weeks.
trapped between the central slip and lateral band may be difficult to
reduce owing to the noose effect exerted by these two soft tissue
structures. The key to closed reduction (if it is possible at all) is
to relax both structures. Wrist extension relaxes the extrinsic
component, and full metacarpophalangeal joint flexion relaxes the
intrinsic component. A gentle rotating maneuver that avoids excessive
longitudinal traction stands the highest chance of success. A few of
these dislocations remain irreducible even in the most skilled hands.
When a reduction can be achieved, early mobilization is then instituted
with buddy taping to an adjacent digit (usually the more radial) in an
attempt to prevent stiffness.
A midaxial (or dual midaxial) incision allows for management of both
dorsal and volar dislocations. Controversy remains as to the need for
direct repair of complete collateral ligament ruptures and volar plate
injuries. Direct repair is probably only functionally necessary in the
long term for the radial collateral ligament of the index finger.
Chronic reconstruction of collateral ligament deficiency is an even
more technically demanding procedure with a high propensity
for generating stiffness but may be accomplished by a variety of techniques.
 |
|
FIGURE 28-43
Entrapment of a collateral ligament can prevent reduction of the proximal interphalangeal joint; lateral stress examination demonstrates the high degree of instability in this situation. |
collateral ligament ruptures, and dorsal dislocations congruent in full
extension on the lateral radiograph can all begin immediate AROM with
adjacent digit strapping. Dorsal dislocations that are subluxated on
the extension lateral radiograph require a few weeks of extension block
splinting before progressing (however, this is an almost unheard of
situation with pure dislocation and no fracture component). Volar
dislocations with central slip disruptions require 4 to 6 weeks of PIP
extension splinting followed by nighttime static extension splinting
for 2 additional weeks. The DIP joint should be unsplinted and actively
flexed throughout the entire recovery period.
in the skin at the flexion crease. Debridement of this wound should
precede reduction of the dislocation. Any joint debris should be
cleared out to prevent third body wear. The “critical corner” warrants
particular attention. For closed irreducible joints, unilateral or
bilateral midaxial incisions allow excellent access to both volar and
dorsal structures without violating the extensor mechanism.
Postoperative management follows the same time courses stated earlier
for nonoperative management based on the injury pattern and severity.
answer to accomplishing a reduction and certainly is the surest way to
fail at the PIP joint. Relaxation of the most powerful tendon forces
acting across the joint is the key to facilitating a smooth reduction
that does not cause additional hyaline cartilage damage. Postreduction
clinical and radiographic assessment is crucial with an emphasis on the
lateral radiograph in full extension to assess congruence. The patient
should be able to move the finger through a near full ROM under the
influence of the digital block used to accomplish the reduction. Open
dislocations should be taken seriously for their potentially high rate
of complications and debrided before reduction.
recognized include intra-articular fractures of the head,
extra-articular fractures of the neck and shaft, and both
extra-articular and intraarticular fractures of the base (Fig. 28-44).
Further describing the pattern of the fracture as transverse, short
oblique, long oblique, or spiral for shaft fractures and partial or
complete articular for intra-articular fractures (along with the degree
and direction of displacement) provides the necessary information on
which to base treatment decisions. A specific fracture pattern that
risks extreme PIP limitation is that of the neck of the proximal
phalanx, where a volar spike of bone from the proximal fracture
fragment impinges into the subcapital recess volar to the neck of P1 (Fig. 28-44B).
If the fracture heals in this position, full PIP flexion is prevented
by obstruction of the space for volar plate in-folding. This pattern is
best identified on an individual digital lateral radiograph and
warrants operative treatment to prevent a functionally disabling
malunion.
The prime reason is the local soft tissue anatomy. While the metacarpal
has only a cordlike extensor tendon running well dorsal to it, the
proximal phalanx is closely invested by a sheetlike extensor mechanism
with a complex array of decussating collagen fibers (Fig. 28-45).
Surgical disturbance of the fine balance between these fibers can
permanently alter the long-term function of the digit. The operative
approach to P1 can be either dorsal or lateral. The dorsal approach may
be technically simpler but transgresses the extensor mechanism. The
lateral midaxial approach allows the fracture to be fully exposed and
hardware placed in its proper lateral position (if hardware is
indicated) without directly violating the extensor mechanism.73
If prominent hardware is to be placed, the intrinsic tendon on that
side (usually ulnar) may be resected. The proximal phalanx is not a
cylinder but rather highly elliptical (in fact, tunnel shaped) in cross
section, with a thicker dorsal cortex.
extrinsic tendon forces deform the fracture. They result in a
predictable apex volar deformity for transverse and short oblique
fractures. These forces can be used with benefit during rehabilitation.
If the MP joints are maximally flexed (the intrinsic plus position),
the intrinsic muscle forces acting through the extensor mechanism
overlying P1 create a tension band effect that helps to maintain
fracture reduction (Fig. 28-46). Active PIP
joint motion will heighten this effect and forms the basis for
nonoperative fracture management. Spiral and long oblique fractures
tend to shorten and rotate rather than angulate. These fractures also
have more complex patterns of deformity that are not so easily
controlled through the joint positioning just described.
joint for each millimeter of shortening and 1.5 degrees of extensor lag
for each degree of apex palmar fracture angulation.163
fractures deform through apex volar bending. Laboratory investigation
has shown the biomechanical inefficiency of dorsally applied plates in
an apex volar bending model that correlated with the clinical forces
experienced at the P1 level.103 Even with plate fixation, the soft tissue envelope has been shown to add stability under load application.120 This is particularly true in the most proximal 6 to 9 mm at the base of P1.174
The most valuable foundation in a fixation paradigm is a well placed
lag screw across a noncomminuted fracture interface, although some
surgeons have bypassed the step of lagging the screw in favor of less
labor intensive bicortical screws.128
Long oblique and spiral proximal phalanx fractures demonstrate less
angular deformity than transverse fractures, instead shortening and
axially rotating.
 |
|
FIGURE 28-44 Fracture patterns appearing in the proximal phalanx include (A) complete articular fractures of the head, (B) subcapital fractures with impingement in the volar plate recess, (C) transverse fractures of the shaft or base, (D) oblique fractures of the shaft, and (E) articular fractures of the base.
|
fractures that are either minimally displaced or easily rendered stable
by reduction (Table 28-7). Transverse fracture
patterns will generally prove to be stable after reduction compared
with oblique, spiral, or comminuted fractures. Stable proximal
phalangeal fractures are ideal candidates for dorsal splinting with the
MP joint in flexion. Only 4 of 45 patients treated in intrinsic plus
splints failed to achieve full motion by 6 weeks.41
The splint should be able to be discontinued at 3 weeks and followed by
AROM exercises without resistance. Stable, nondisplaced fractures may
even be treated by a program of immediate AROM, protected only with
adjacent digit strapping. The take-home message for nonoperative
management is that a carefully formed splint and/or adjacent digit
strapping can effectively maintain an existing and reasonably stable
reduction. What splints and strapping cannot accomplish is a reduction
in their own right. In case this fact is not appreciated at the initial
encounter, all patients undergoing nonoperative management should be
seen back in the office at a week to verify maintenance of reduction
radiographically.
reducible but unstable isolated fractures, both extra-articular and
some intraarticular. A higher degree of care must be exercised when
pursuing CRIF in the phalanges compared with the metacarpals because
of
the close investment by the broad extensor mechanism. Pin entry sites
should be chosen carefully to minimize tethering of the extensor
mechanism. In the proximal two thirds of P1, this is virtually
impossible. As one approaches the distal third, a direct lateral
approach can be made volar to the interosseous tendon. For long oblique
and spiral fractures, three K-wires (0.045 or 0.035 inch) are placed
perpendicular to the fracture plane (Fig. 28-47). For neck fractures, retrograde pinning may be necessary (Fig. 28-48). For short oblique and transverse fractures, longitudinal K-wires (0.045-inch) are placed through the MP joint (Fig. 28-49).
Twelve patients achieved an average TAM of 265 degrees with two
longitudinal pins placed across the MP joint and down the shaft of the
proximal phalanx.81 Trocartipped
K-wires rather than diamond-tipped or surgeon-cut wires should be used.
The wire should be passed through the soft tissues and down to bone
before activating the wire driver. Pins should be cut just below the
skin surface to prevent pin tract infection or left protruding for ease
of removal at the surgeon’s discretion. Absolute parallelism of the
K-wires for oblique fractures risks the fracture displacing as it
slides along the wires. Some degree of convergence or divergence of the
wires will help to prevent this consequence of using smooth wires. The
procedure of CRIF is made more difficult than it may initially appear
by the challenge of obtaining a truly accurate reduction by closed
means. Commercially available devices have been specially designed for
closed intramedullary rodding of the phalanx (Fig. 28-50).
Routinely, pins should be removed by 3 weeks. When this is done, any
final limitations of motion are most likely because of the injury
itself rather than the pins. In 35 fractures of the proximal phalanx
treated by percutaneous pinning, 32% developed a PIP flexion
contracture averaging 18 degrees.43 A slight variation on the theme is “intrafocal” pinning used in five patients to achieve an average PIP range of 90 degrees.27
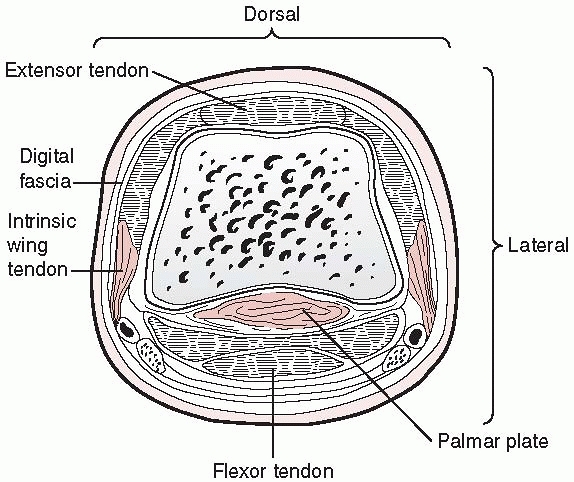 |
|
FIGURE 28-45
The proximal phalanx is closely invested by the sheet of the zone IV extensor tendon dorsally, the blending of the intrinsic wing tendons laterally and volarly, and the flexor tendons and flexor sheath direct volarly. |
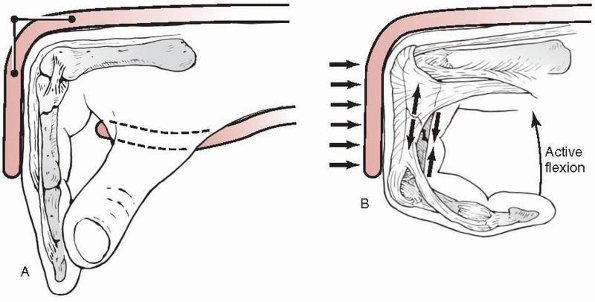 |
|
FIGURE 28-46
Flexing the MP joints fully causes the extensor apparatus to function as a tension band to a transverse fracture in the proximal phalanx shaft, helping to reduce the deformity and stabilize the fracture when the proximal interphalangeal joint is actively flexed. |
fractures with multiple associated soft tissue injuries and for
patients with multiple fractures (within the same hand or polytrauma
patients). It is also the technique of choice for intra-articular
fractures with displacement in P1. In a series of 38 distal unicondylar
fractures of P1, five of seven initially nondisplaced and unfixed
fractures and four of ten fixed with a single K-wire went on to
displace.173 Displaced fractures at
the intra-articular base of P1 with more than 20% articular involvement
should be internally fixed. Using a volar A1 pulley approach, 10
patients had fixation of lateral base fractures with full motion
recovery, good stability, and over 90% contralateral grip strength.92
The role of ORIF for an isolated, noncomminuted, extra-articular
fracture of the phalanx is clearly defined only for the rare
irreducible fracture. Spiral fractures may benefit from ORIF with lag
screws to achieve precise control over rotation, provided that surgeons
experienced in this specific technique can minimize soft tissue
disruption. Most surgeons will be more comfortable with CRIF for those
fractures that can be reduced. The 40-month follow-up of 32 patients
prospectively randomized to percutaneous pinning versus lag screw
fixation for long oblique and spiral shaft fractures found no
differences in function, pain scores, ROM, or grip strength, but with a
mean loss of active extension of 8 degrees in the pinning group and 27
degrees in the screw fixation group.82
Surgical technique was such that there were 8 malunions of the 15 lag
screw patients using screws as large as 2.0 mm. Three of the 17 K-wire
patients required subsequent formal extensor tenolysis for tethering
but none of the lag screw patients did.82 ORIF with screws and/or plates is
considerably more technically demanding than in the metacarpal for a
number of reasons including the proximity of the extensor mechanism,
the origins of the fibro-osseous flexor tendon sheath, and the size and
consistency of the bone. More than just the technical complexity of
ORIF is the problem of the postoperative response of the surrounding
soft tissues to the surgical dissection and the presence of hardware.
|
TABLE 28-7 Proximal Phalanx Fractures
|
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||
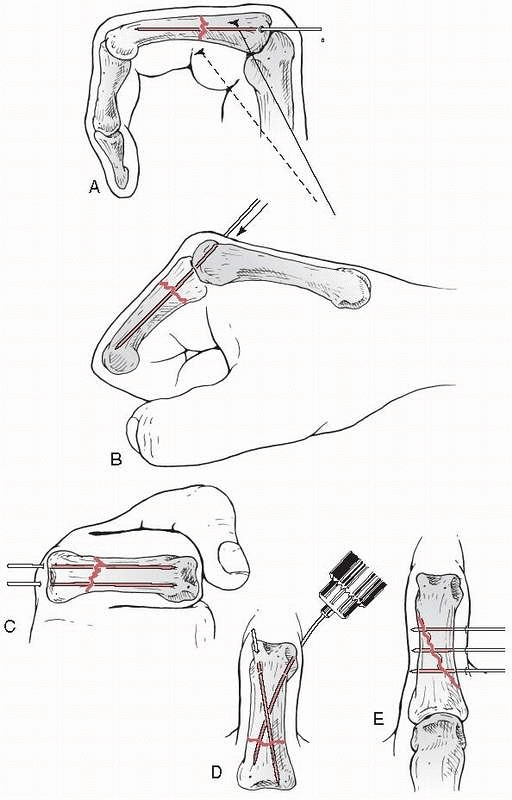 |
|
FIGURE 28-47 Closed reduction and internal fixation of P1 shaft fractures can be accomplished (A) longitudinally through the metacarpophalangeal joint but not the metacarpal head, (B) or through the metacarpal head, (C) with the wires for either of these options running parallel in the phalanx, or (D) entering at the collateral recess and crossing, or (E) passing transversely.
|
The familiarity of the surgeon with the specific technique is probably
the most important factor in the selection of a method. Of 30 patients
followed for 2.3 years after tension band wiring, 17 had a TAM of over
195 degrees and 13 had a TAM of between 130 and 195 degrees.132 More recently, attention has increasingly turned to the use of screw and plate technology (Figs. 28-53 and 28-54).
The relative bulkiness of plates at the phalangeal level compared with
the metacarpals can result in the need for their removal even with
initially excellent results. The results of internal fixation are
intimately related to the associated injuries present. The gravest
danger, however, occurs when the surgeon elects ORIF but is then unable
to secure rigid fixation of the fracture. In this situation, the
patient has been subjected to the “worst of both worlds,” and a poor
outcome can be reliably predicted.
phalangeal head, unicondylar (partial articular fracture), or
bicondylar (complete articular fracture). The condylar fragments
usually are extremely small, can be fragile, and receive their blood
supply from the attached collateral ligament. Fixation of a single
condyle is most rigid when accomplished with a compression screw placed
transversely, entering near the collateral ligament origin (Fig. 28-55). This can be quite challenging technically, and the bone stock may only tolerate K-wire or composite wiring techniques (Fig. 28-56).
When the unicondylar fragment has a solid extension to the shaft level
cannulated microsized headless compression screws can be used.58 Triplane fractures of the head of the proximal phalanx are
well managed with 1.2-mm lag screws (Fig. 28-57).22
Complete articular fractures can be fixed with screws only if one of
the two condyles has an extended spike. If not, minicondylar or locking
plate fixation may be necessary to achieve excellent rigidity. Again,
the bone stock may not tolerate the application of this device, and
wiring techniques remain an alternative strategy.
 |
|
FIGURE 28-48 Fractures of the proximal phalangeal neck that are angulated apex volarly (A), can be stabilized by (B) antegrade pinning with a rotational control cross wire if the fracture is sufficiently proximal, but very distal fractures (C,D) usually require retrograde pinning.
|
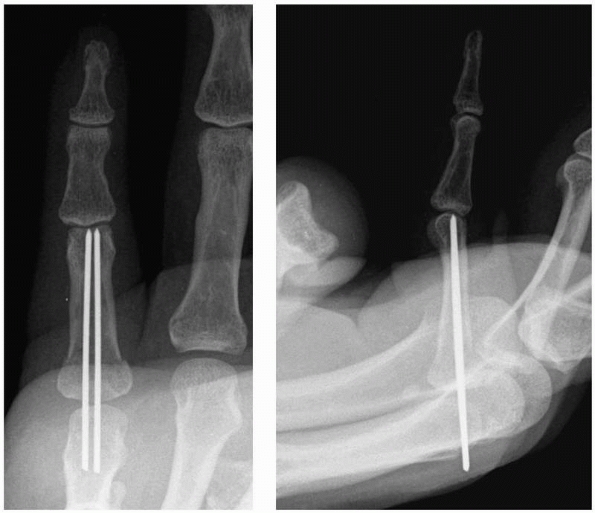 |
|
FIGURE 28-49
Transverse shaft fractures of the proximal phalanx are best stabilized by 0.045-inch K-wires passed longitudinally through the metacarpal head and removed at 3 weeks. |
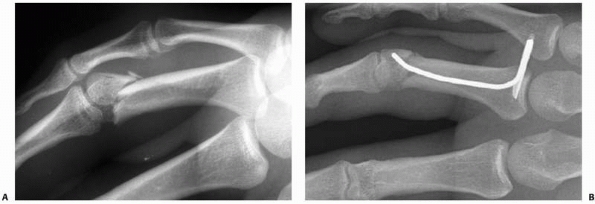 |
|
FIGURE 28-50 A. Proximal phalanx fractures can be stabilized by closed placement of a specially designed device that achieves (B) three-point fixation with a rotational locking sleeve proximally.
|
the lateral corner of the phalangeal base, which are particularly
amenable to the technique of tension band wiring (see Fig. 51C). An
alternative is a volar approach to lateral base P1 fractures using a
single lag screw for fixation to achieve full motion by 3 weeks.137
Comminuted intra-articular fractures of the proximal phalangeal base
can be stabilized by a small volar plate placed through the A1 pulley
approach.72 A specific subset of
proximal phalangeal base fractures that are purely impactions by nature
may be treated by supporting the impacted fragments with packed
cancellous bone only; in one series of 10 patients followed for 32
months, there was no secondary displacement and an average PIP joint
flexion of 88 degrees was achieved.150
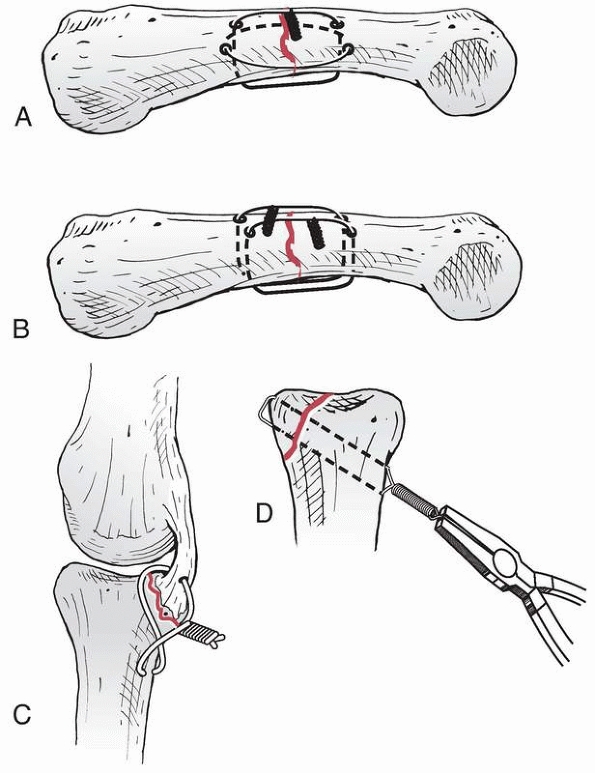 |
|
FIGURE 28-51 A malleable intraosseous wire alone can be applied in its strongest configuration of (A) two loops at 90 degrees to each other, (B) two parallel loops, (C) a figure-of-eight tension band, and (D) a single loop to compress a smaller fragment against the larger fragment.
|
weeks followed by AROM that can include adjacent digit strapping if
necessary. Similarly, CRIF should allow for pin removal at 3 weeks,
with AROM beginning no later than this time. If ORIF is chosen, AROM
should begin within 72 hours of surgery and edema control should be
foremost in the treatment plan using cohesive elastic bandages.53
AROM alone may be insufficient to counteract extensor lag at the joint
distal to the site of fixation. Rapidly accelerating the extensor
tendon concentrically without resistance best limits local adhesion
formation77 (Fig. 28-58).
These exercises can be supplemented with the use of electrical muscle
stimulation during outpatient therapy sessions. Night splinting with
the PIP joint in extension can be helpful but will not in and of itself
overcome an extensor lag.
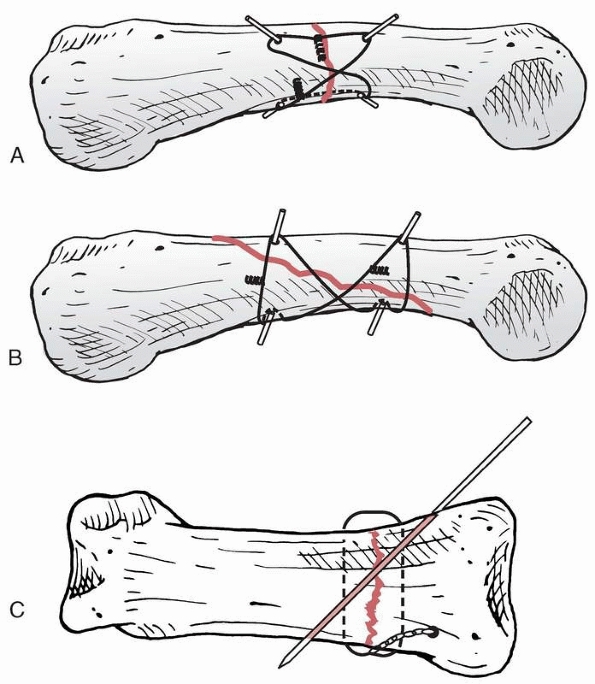 |
|
FIGURE 28-52
Composite wiring techniques may involve any configuration or combination of nonflexible fixation with a malleable wire that is twisted to achieve compression across the fracture site. |
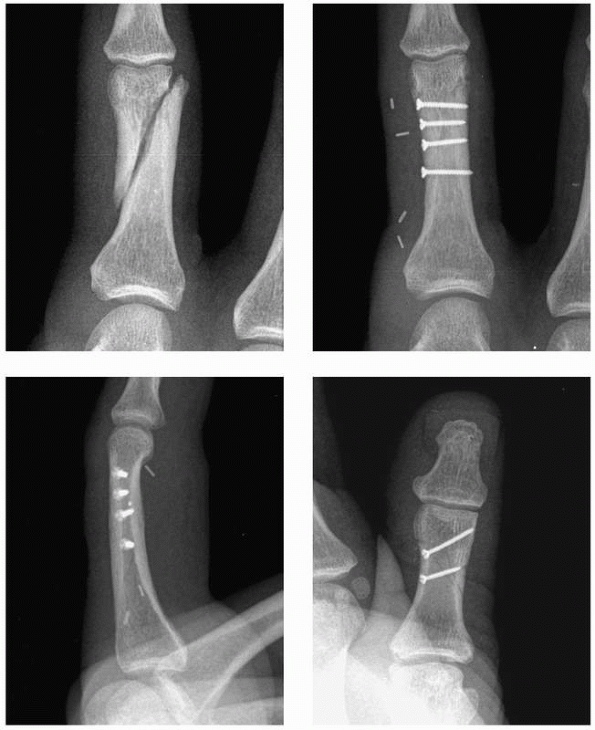 |
|
FIGURE 28-53
In long oblique fractures of the shaft with shortening, an exact reduction and stability sufficient to withstand early motion can be achieved through lag screw fixation only. |
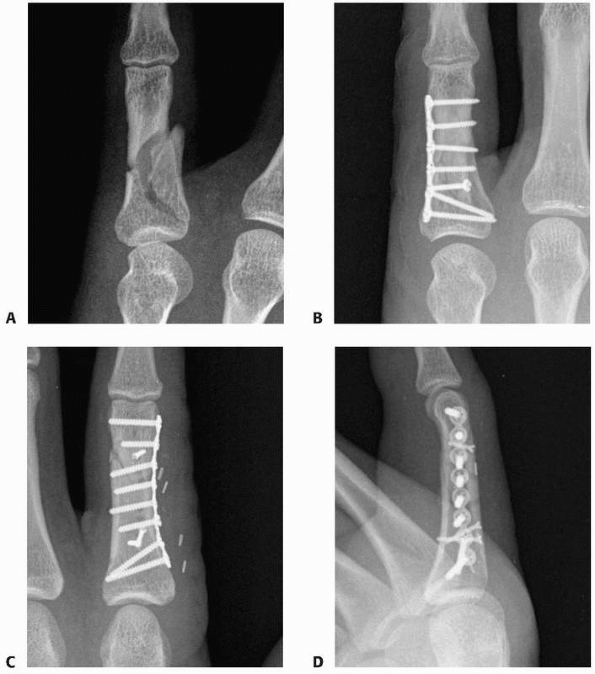 |
|
FIGURE 28-54 More complex fractures of the shaft (A) can be well stabilized by (B) lateral plating. Specific care should be taken to (C) contour the plate meticulously to fit the cortex and to place the hardware in (D) the true midlateral position.
|
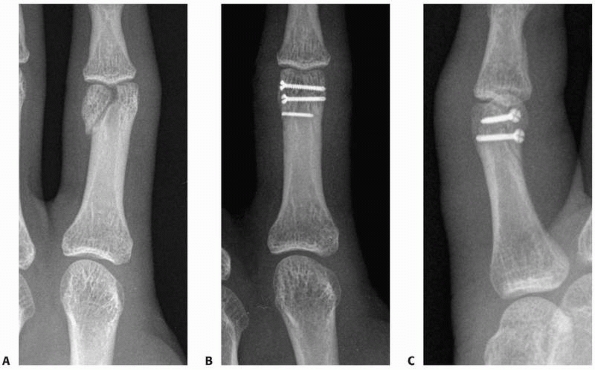 |
|
FIGURE 28-55 A. Unicondylar fractures of the head of the proximal phalanx benefit from compression between the articular fragments through (B,C) lag screw fixation.
|
Longitudinal pinning with two K-wires passing through the metacarpal
head with the MP joint flexed 80 to 90 degrees has yielded reliable
results.74 In larger patients, two
0.045-inch K-wires can both be fit through the medullary canal. In
smaller patients, one 0.045-inch and one 0.035-inch wire may be more
compatible. When rotational interlock is felt between the fragments,
one wire can be used. The wires are placed one each on either side of
the thick central extensor tendon dorsal to the MP joint, thus passing
through the sagittal band fibers. The wires are then passed through the
base fragment, across the fracture site, and down the distal shaft of
the phalanx to the head. Care must be taken to not power drill the
wires through the subchondral bone of the phalangeal head, creating a
pin tract into the PIP joint. If such a passage exists, the wire may
migrate distally into the PIP joint during early rehabilitation and
cause hyaline cartilage damage to the
base
of the middle phalanx. Instead, the wire should be drilled up to but
not into the subchondral bone. After cutting the wires dorsally, they
may be manually impacted a few millimeters further into the subchondral
bone, conferring an added degree of stability.
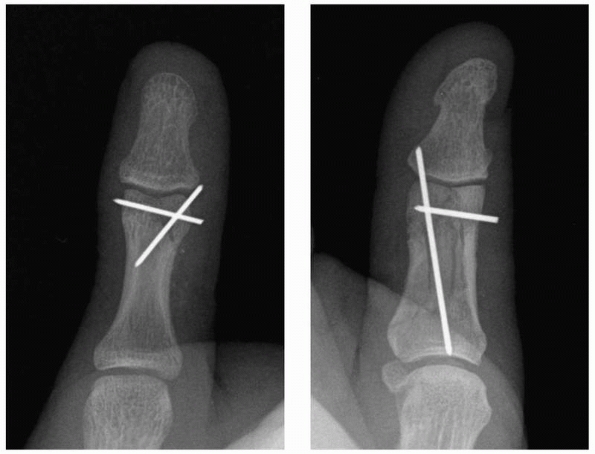 |
|
FIGURE 28-56
When a unicondylar fracture of the head of the proximal phalanx has a proximal shaft extension on the smaller fragment, K-wire fixation in a diverging pattern can prevent migration of the fragment that would otherwise occur with a single smooth K-wire as the only fixation. |
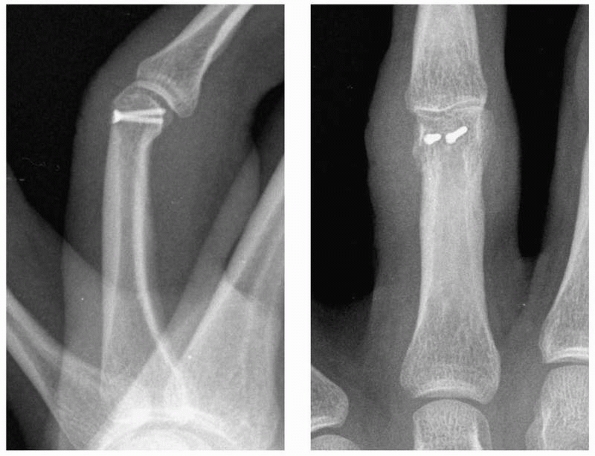 |
|
FIGURE 28-57 Triplane fractures of the proximal phalangeal head can be well stabilized by two small lag screws (1.2-mm to 1.5-mm).
|
nondisplaced fractures at the head of P1. Both a transverse pin
connecting the two condyles and an oblique pin from the condyle to the
opposite diaphyseal cortex should be used for a unicondylar fracture.
For bicondylar fractures, two oblique pins are needed. The oblique pins
are best cut for retrieval proximally rather than distally as their
passage through the periarticular soft tissues will interfere with PIP
joint motion. Closed pinning also represents a reasonable treatment
option
for
nondisplaced long oblique or spiral fractures that are suspected of
subsequent displacement when subjected to the stress of motion
rehabilitation. However, practically I have not found this fracture
pattern to exist. I see either truly nondisplaced fractures that I
expect to remain stable, and I treat them nonoperatively, or displaced
long oblique and spiral fractures that I prefer to treat with open
reduction.
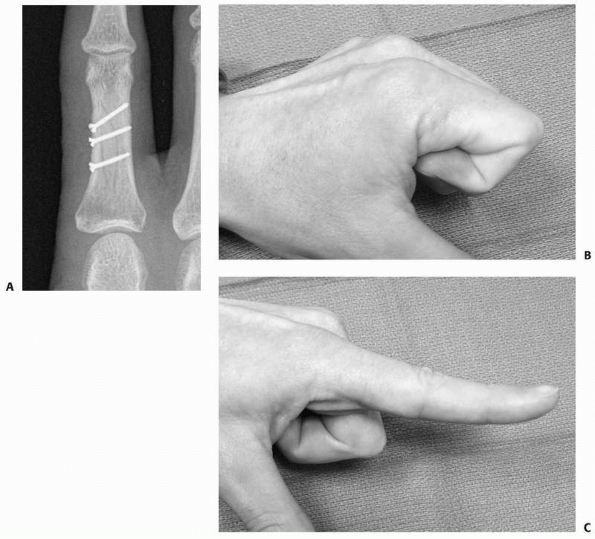 |
|
FIGURE 28-58 Following (A) lag screw fixation of a shaft fracture in the proximal phalanx, (B) complete proximal interphalangeal joint flexion and (C)
proximal interphalangeal joint hyperextension are achievable with an aggressive special therapy program of resisted zone IV extensor tendon preload followed by sudden release with follow-through. |
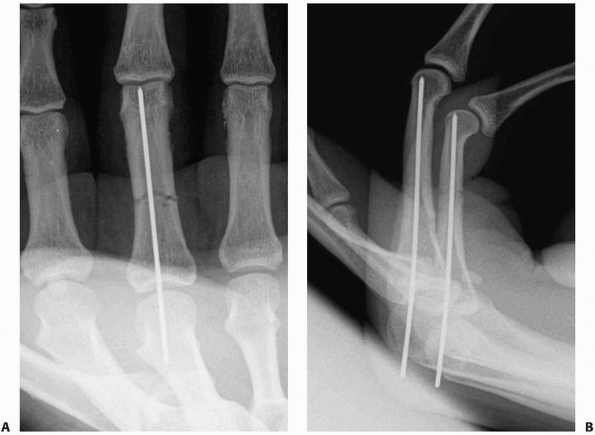 |
|
FIGURE 28-59 A.
Transverse proximal phalanx fractures without comminution should achieve sufficient interfragmentary stability to have axial rotational control with a single wire alone that targets the (A) intercondylar notch and extending (B) all the way to the subchondral bone. |
I have found it difficult through closed means alone to correct all the
shortening and rotation of long oblique and spiral fractures. There is
a natural tradeoff between the undeniable added surgical trauma of an
open approach and the benefits of an anatomically precise reduction.
When lag screws alone are used for fixation, full motion rehabilitation
can begin immediately.73,77
This is not the case with K-wires that tether soft tissues, limiting
motion and risking pin tract infection. Performing the open fixation
gently and precisely to minimize soft tissue trauma is more easily
described than executed. The first principle is to carefully evaluate
fracture geometry. In a simple two-fragment diaphyseal fracture, there
will be inherent stability between the bone edges once the fracture has
been reduced. The role of internal fixation is then to exploit this
inherent stability by further compressing the fracture line. Fixation
involving the use of lag screws achieves the maximum compression
possible. One must always heed the ground rules for screw-only
fixation: fracture length is at least two times the bone diameter, and
fragment width is at least three times the screw diameter. For all of
the above techniques, adherence to strict principles is mandatory;
multiple drill bit passes are not well tolerated by the phalanx. Screws
of 1.2- to 1.5-mm diameters are appropriate for P1. Biomechanically, it
is desirable to have at least one screw placed perpendicular to the
neutral axis of the bone. The remaining screws should be perpendicular
to the fracture plane. In a spiral fracture, one screw can satisfy both
of these requirements simultaneously and is termed the “ideal” screw.
In an oblique fracture, this will not be the case.
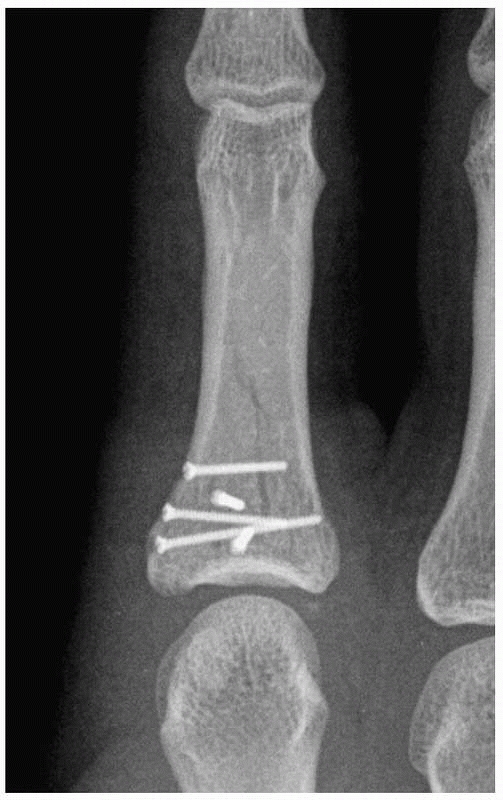 |
|
FIGURE 28-60
Partial articular fractures that can be rendered stable by interfragmentary compression are excellent candidates for lag screw fixation. |
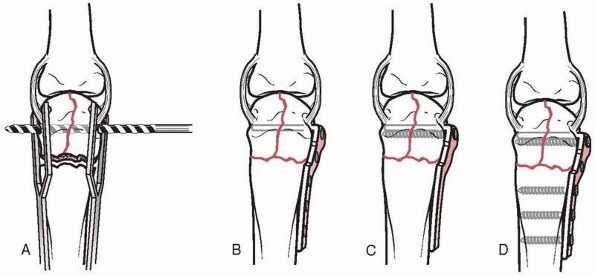 |
|
FIGURE 28-61 After reduction of the condylar fragments to each other and the shaft, (A) the hole for the condylar blade is drilled and its depth is measured. B. The blade is cut to size and inserted to evaluate the accuracy of the plate contouring. C. The condylar screw is inserted, along with (D) the shaft screws.
|
of their bulk and propensity for tendon adherence, and I avoid using
them whenever possible. This is my treatment of choice for fractures
with comminution and bone loss and complete articular fractures of the
phalangeal head that are unstable (Fig. 28-61).
Since the biomechanics of P1 fractures create an apex palmar sagittal
plane deformity, the plate would (impossibly so) have to be applied to
the volar surface of the bone to have its optimum tension band effect.
Lateral placement is then the next most desirable option, and this
corresponds well to the surgical access that is least harmful to the
soft tissues.73 A midaxial incision
is carried volar to the margin of the extensor mechanism, straight
through periosteum and the entire soft tissue sleeve is elevated as a
single unit, avoiding any dissection of planes surrounding the extensor
tendon.73 When plates are used, one should attempt to place screws as perpendicular to the surface of the plate as possible (Fig. 28-62).
The heads of obliquely placed screws have a prominent edge. Plates
should also be painstakingly contoured to ensure both the lowest
profile as well as proper biomechanical function (preload, dynamic
compression, and a buttress effect). If more than 50% of the
cross-sectional area of the bone is comminuted or lost, bone graft will
be required.
 |
|
FIGURE 28-62
Plate fixation in the proximal phalanx must be contoured meticulously to restore the normal anatomic shape of the bone. The condylar blade plate can also be used at the metaphyseal base of a proximal phalanx. An oblique screw is often advantageous to achieve an extra point of compression in the metaphyseal fragment. |
preferred treatment section. The details of the difficult open fixation
procedures at the proximal phalanx level will be covered here. I prefer
to operate on closed fractures around postinjury day 3 to 5 when even
adult periosteum will thicken dramatically in response to injury and
can be surgically manipulated as a tissue flap. Posttraumatic swelling
will have begun to subside by this time. A true midaxial incision is in
the neutral tension lines of the skin and brings the approach down to
the volar leading edge of the intrinsic wing tendon. One of the most
important principles in open fixation of a P1 fracture is to not create
planes of surgical dissection either superficial or deep to the zone IV
extensor tendon (Fig. 28-63). The only
dissection that should occur at the subcutaneous level is to identify
dorsal cutaneous nerve branches passing obliquely from the proper
digital nerves and to mobilize them effectively to avoid neuromas.
Other than this, the approach should create a single tissue flap from
skin through periosteum to bone.73 A
sharp blade is needed to carefully preserve the periosteum for later
repair using fine monofilament resorbable sutures. This creates an
additional gliding layer of protection for the extensor mechanism. A
finetipped curette must be used to clear the fracture interface of all
clot and soft tissue or a truly anatomic interdigitated reduction will
not be possible. Although provisional fixation of the fracture with
K-wires has been recommended by others, I have found that the
absoluteness of a perfect reduction is not well maintained by smooth
wires, which invariably allow the reduction to slip a little bit. This
ensures that the drill path will not be exactly in the desired location
and that final placement of the screw or plate will thus be imperfect.
I prefer to hold the reduction manually with either a bone clamp
specialized for the short tubular bones of the hand or with Brown-Adson
forceps. Caution must be used to drill at lower speeds as high speeds
can introduce an eccentric “whip” to the tip of these small drill bits,
resulting in a larger drill path than desired. I strongly prefer a
“pencil grip” microdrill over a “pistol grip” driver for the sake of
accuracy in drilling a straight path.
provisional stabilization are core drilling followed by countersinking
the near bone surface (Fig. 28-64). Countersinking not only recesses the
screw head but also distributes the force of compression, lessening the
chance of propagating a new fracture line. Measuring for screw length
is done next, and the time for the scrub technician to procure the
correct screw can be used to drill the gliding hole. Self-tapping
screws are a little difficult to start into bone as some axial load is
necessary to get them to bite, but application of this load off the
true axis will toggle the screw. A fine touch must be learned over the
course of many cases using these implants. Screws are tightened with a
“chuck” pinch on the screwdriver using three fingers, not with the more
forceful key pinch that may shear the head off the shaft of the screw.
All plates must be meticulously and often painstakingly contoured
before application (Fig. 28-65).
One must not hesitate to remove a plate and recontour it after the
first two screws have been placed if it is clear that the shape is not
correct. Application of an incorrectly contoured plate guarantees an
imperfect fracture reduction. A common error is with plates ending near
the metaphyseal flare that must have a small bend at the last hole to
accommodate the curvature of the bone at this level. Since the last
edition of this text, locking plate technology has found its way down
to the size range for the small bones of the hand. This is a huge
advantage over the sole previously available implant that offered fixed
angle stability, the minicondylar plate. The minicondylar plate could
not be fully contoured to the bone surface before placing the blade; a
locking plate can.
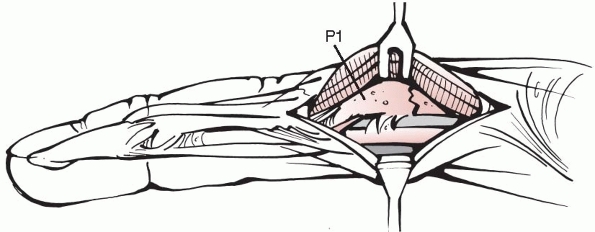 |
|
FIGURE 28-63
The lateral approach to the proximal phalanx should not create layers of dissection around the extensor tendon but rather pass volar to the leading edge of the intrinsic wing tendon and through periosteum to bone, leaving skin, extensor tendon, and periosteum as a single tissue flap for retraction. |
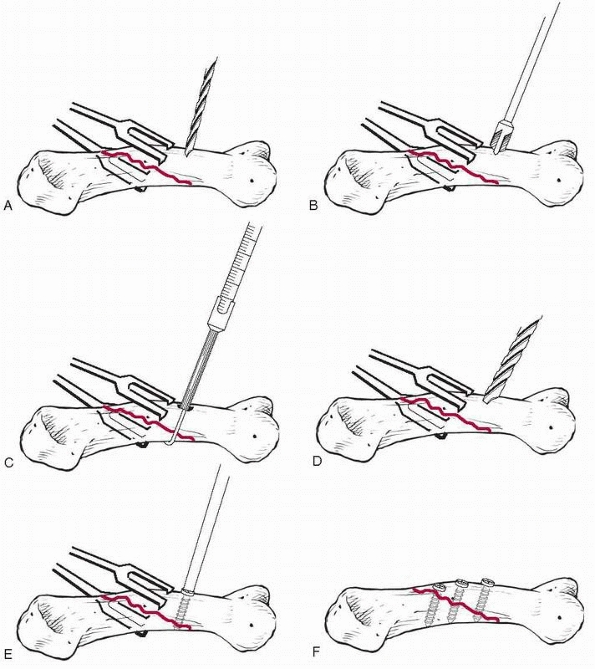 |
|
FIGURE 28-64 After stabilized reduction of a shaft fracture, lag screw fixation is accomplished by (A) drilling with the smaller core bit, (B) countersinking the near cortex, (C) measuring the correct length, (D) drilling the gliding hole, (E) tightening the lag screw with light three finger tip pressure, and (F)
ensuring all distances between screws and fracture edges are sufficient to avoid propagation of new fracture lines under the pressure of screw tightening. |
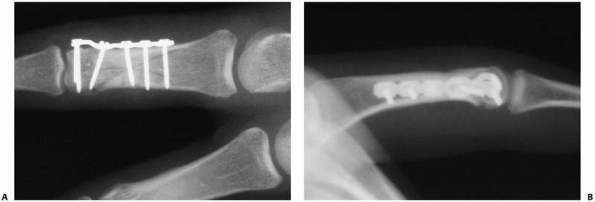 |
|
FIGURE 28-65 Comminuted fractures involving the head and shaft of the proximal phalanx (A) can be stabilized for early motion with a condylar blade plate (B) placed laterally in the midaxial plane.
|
dislocations are reducible and present with a hyperextension posture.
They are really subluxations, as some contact remains between the base
of P1 and the metacarpal head (Fig. 28-66). The
volar plate stays volar or distal to the metacarpal head. Reduction
should be achieved with simple flexion of the joint; excessive
longitudinal traction on the finger should be avoided. Wrist flexion to
relax the flexor tendons may assist reduction. The other variety of MP
joint dislocation is a complex dislocation, which is by definition
irreducible, most often because of volar plate interposition (Figs. 28-66B and 28-67).
Complex dislocations occur most frequently in the index finger.
Longitudinal traction can convert a simple into a complex dislocation.
A pathognomonic radiographic sign of complex dislocation is the
appearance of a sesamoid in the joint space. Concomitant injuries
include small chip fractures on the dorsum of the metacarpal head that
have been sheared off in complex dislocations by the volar base of P1.67,79 Other difficult fractures to detect are bony collateral ligament avulsions.
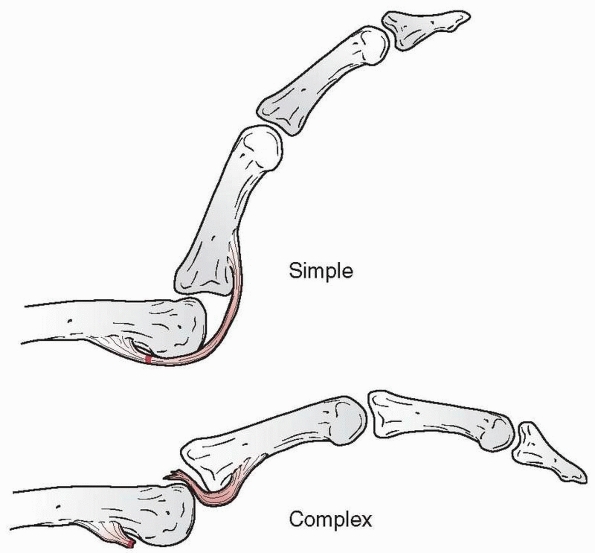 |
|
FIGURE 28-66
Simple metacarpophalangeal joint dislocations are spontaneously reducible and usually present in an extended posture with the articular surface of the proximal phalanx sitting on the dorsum of the metacarpal head. Complex dislocations have bayonet apposition with volar plate interposition that prevents reduction. |
reduction and do not need surgical repair of the ligaments or volar
plate. Volar dislocations are rare but particularly unstable. Volar
dislocations risk late instability and should have repair of the
ligaments.113 Obstructions to
reducing volar dislocations include the volar plate, collateral
ligament, and dorsal capsule. Open dislocations may be either reducible
or irreducible. Small fracture fragments at the collateral insertions
(base of P1 or metacarpal head) need special consideration as such
injuries share the features of ligament instability and the
consequences of an intraarticular fracture.135,137,138
Isolated collateral ligament injuries are more common on the radial
aspect of the small finger followed by the index finger. A differential
diagnosis to consider with posttraumatic swelling at the MP joint level
is rupture of the sagittal bands (confirmed by visible or palpable
ulnar subluxation of the zone 5 extensor tendon), which requires
protection in extension for 4 weeks. A rare variant injury to the MP
joint is a dorsal capsular tear (Boxer’s knuckle) that can prove
persistently symptomatic. In a series of 16 patients that included
extensor tendon dislocation in 7, surgical closure of the rent found in
the dorsal capsule or extensor hood was reported to be successful in
all cases.6
of the thumb MP joint is a common injury that less frequently may
accompany a full MP joint dislocation (Fig. 28-68).
Circumferential palpation of the MP joint can often localize pain to
the UCL, radial collateral ligament (RCL), volar plate, or combinations
of these. Following joint injection with local anesthetic,
stress
testing in full extension and 30 degrees of flexion (eliminates the
false-negative conclusion of stability in the setting of a ruptured
proper collateral ligament but an intact volar plate) should reveal any
instability (Fig. 28-69A). If clinical uncertainty remains, stress radiography may also be performed (Fig. 28-69B).
Finding a consistent role for MRI in the diagnosis of the Stener lesion
(a distally ruptured ulnar collateral ligament blocked from healing by
the interposed adductor aponeurosis) has yet to occur.78
In a series of 24 patients, a palpable tender mass on the ulnar side of
the MP joint was used as the sole diagnostic criterion for the Stener
lesion. Operative treatment was performed for those thought to have the
lesion and nonoperative management for those who did not, resulting in
only a single case of long-term instability.1
 |
|
FIGURE 28-67
The typical complex dorsal dislocation of the metacarpophalangeal joint presents with complete overriding of the phalanx on the metacarpal. |
sport in the etiology of acute UCL injuries. The interaction between
the thumb and first web space with ski pole grips has been blamed for
the association of UCL ruptures in this sport. Not all fracture
fragments seen on the ulnar aspect of the MP joint represent the
anatomic insertion of the UCL. Some of these fragments may be attached
to the volar plate insertion, separate from the collateral ligament.
The differential diagnosis of sesamoid fracture must also be considered
when volar tenderness is present. Oblique radiographs may be helpful in
this respect when considering the frequent incomplete ossification of
the sesamoids. Special mention should be made of irreducible
dislocations. Irreducible volar dislocations have been reported with
the radial condyle of the metacarpal trapped in a rent dorsal to the
accessory collateral-volar plate complex.79
Other causes of volar trapping may involve the extensor pollicis longus
and brevis. The flexor pollicis longus may block reduction of a dorsal
dislocation.83
 |
|
FIGURE 28-68 Metacarpophalangeal joint dislocation in the thumb, like the fingers, is typically dorsal.
|
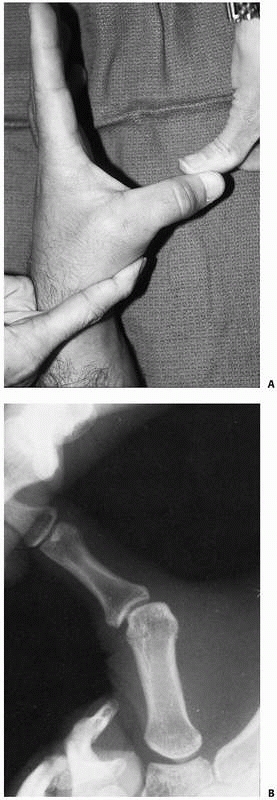 |
|
FIGURE 28-69 A.
Clinical stress testing of the ulnar collateral ligament in 30 degrees of flexion prevents reaching a false-negative conclusion when an intact volar plate obscures the instability of a complete proper ulnar collateral ligament rupture. B. Radiographic stress testing is also useful when there is clinical uncertainty. |
box previously presented for the PIP joint, composed of the proper
collateral ligaments, the accessory collateral ligaments, and the volar
plate (Fig. 28-70). The radial and ulnar proper
collateral ligaments are the primary stabilizers to motion in all
planes, including distraction, dorsopalmar translation,
abduction-adduction, and supination-pronation. The accessory collateral
ligaments supplement adduction-abduction stability. The volar plates
are connected to each other by the deep transverse intermetacarpal
ligament. The MP collateral ligaments have an origin dorsal to the
center axis of joint rotation. This feature combines with two others (a
greater width of the metacarpal head volarly and a greater distance
from the center of rotation to the volar articular surface than the
distal articular surface) to maximize tension in the true collateral
portion of the ligament when the joint is in full flexion.
Consequently, stress testing to determine the presence of instability
must be performed in full flexion.
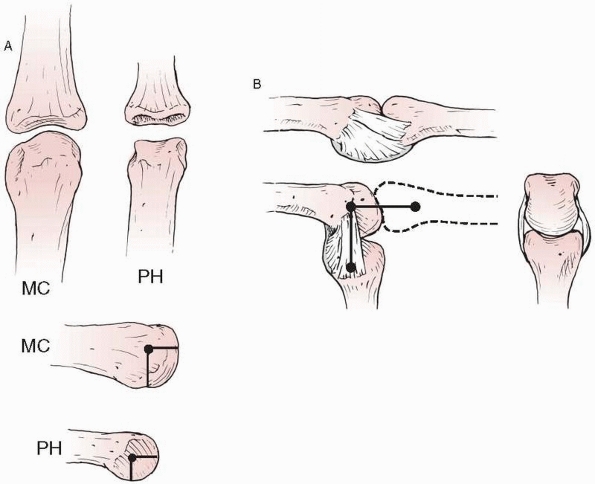 |
|
FIGURE 28-70 A.
The anatomy of the metacarpophalangeal (MP) joint differs from that of the proximal interphalangeal joint in the unicondylar head of the metacarpal (MC) versus the bicondylar head of the phalanx (PH), the cam effect in the sagittal plane unique to the metacarpal, and (B) the collateral origin offset dorsally from the center of rotation in the metacarpal. |
topic of great controversy. Central MP joints can be approached either
dorsally or volarly. Although the volar plate is the most commonly
noted structure in the prevention of reduction, the flexor tendons,
lumbricals, deep transverse intermetacarpal ligaments, juncturae
tendinae, and dorsal capsule have all been implicated.122
In a series of 10 operatively treated ligament ruptures, most were
distal with the ligament occasionally trapped between the intrinsic
tendon and the sagittal band, including two associated dorsal
interosseous ruptures at the phalangeal insertion.31
flexion and extension, allows abduction-adduction and a slight amount
of rotation (pronation with flexion). The range of flexion and
extension has a wide natural variation that may be related to the
flatness of the metacarpal head and may also play a role in
predisposition to injury for those with less motion. With a one-sided
collateral ligament injury, the phalanx tends to subluxate volarly in a
rotatory fashion, pivoting around the opposite intact collateral
ligament. The ulnar collateral ligament may have a two-level injury
consisting of a fracture of the ulnar base of P1 with the ligament also
rupturing off the fracture fragment.59
Of particular importance is the proximal edge of the adductor
aponeurosis that forms the anatomic basis of the Stener lesion. The
torn UCL stump comes to lie dorsal to the aponeurosis and is thus
prevented from healing to its anatomic insertion on the volar, ulnar
base of the proximal phalanx (Fig. 28-71). The
true incidence of the Stener lesion remains unknown because of widely
disparate reports. The abductor pollicis brevis also sends fibers to
the extensor mechanism, but a discrete edge capable of preventing
healing of the radial collateral ligament does not
exist;
therefore, there is no correlate to a Stener lesion on this side of the
joint. Radial collateral ligaments injuries have been found to occur at
the phalangeal insertion in 13 of 38 cases and at the metacarpal origin
in 25 of 38.26
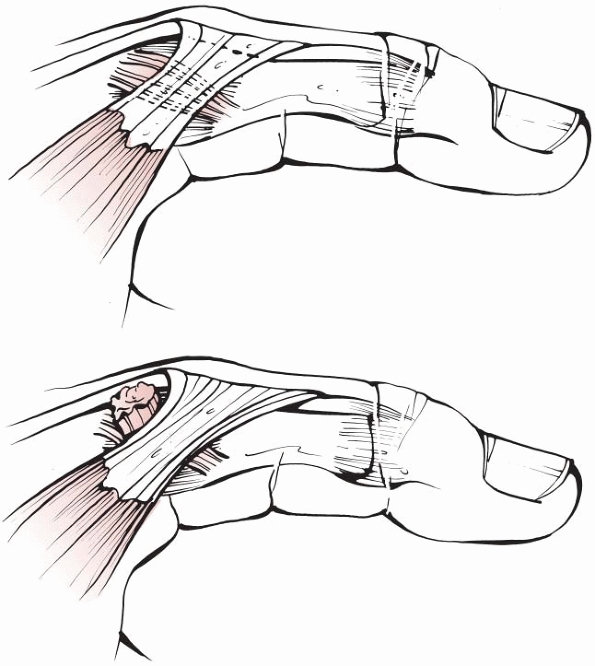 |
|
FIGURE 28-71
The Stener lesion. The proximal edge of the adductor aponeurosis functions as a shelf that blocks the distal phalangeal insertion of the ruptured ulnar collateral ligament of the thumb metacarpophalangeal joint from returning to its natural location for healing after it comes to lie on top of the aponeurosis. |
Collateral ligament injuries should be immobilized in incomplete
flexion (50 degrees) for 3 weeks followed by AROM while the digit is
strapped to an adjacent digit to resist lateral deviation stress. Even
with fracture fragments constituting up to 25% of the width of the
phalangeal base, early active mobilization using side strap protection
led to normal motion and grip strength in 6 of 7 patients with a mean
DASH score of 3.1.135 Dorsal
dislocations will normally prove stable during early AROM. Only in an
exceptional case would the use of extension block splinting of 20
degrees or so for 2 to 3 weeks be required. In a high-demand patient
the radial collateral ligament of the index MP joint should be
considered for operative repair.
|
TABLE 28-8 Metacarpophalangeal Joint Dislocations
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
thumb MP joint injuries. Only the complete UCL injury with a Stener
lesion and volar dislocations require more aggressive treatment. The
standard treatment consists of 4 weeks of static MP joint
immobilization with the IP joint left free. Management in the presence
of a fracture at the ulnar base of P1 is more controversial. Nine
patients with less than 2-mm displacement of such a fragment treated
nonoperatively all had chronic pain with pinch strength rated at 36% of
normal. Following operative treatment, pinch improved to 89% of normal
with symptom resolution.35
Conversely, 28 patients with ulnar base fractures but with a joint
clinically assessed as stable to stress testing were managed
nonoperatively resulting in equivalent grip and pinch strengths to the
contralateral side and 93% were pain free despite a 60% rate of fibrous
union.142 Radial collateral ligament
disruptions and pure dorsal dislocations can be successfully managed by
a 4-week period of MP joint immobilization. Sesamoid fractures also are
managed primarily by 3 to 4 weeks of immobilization in partial flexion.
collateral ligament disruptions associated with large bone fragments
should be treated with open reduction and repair (Fig. 28-72).
Radial collateral ligament injuries repaired late risk a higher
incidence of pinch weakness and should be attended to promptly. Open
repair or reconstruction with a free tendon graft may also be required
in chronic cases with persistent symptoms following initial
nonoperative management. Of 33 patients with MP collateral ligament
avulsion fractures from the base of the proximal phalanx, the eight who
were treated nonoperatively
initially all went on to symptomatic nonunion requiring subsequent surgery.137
In a similar series of 19 patients with the avulsion occurring at the
metacarpal head, successful results occurred in the 11 displaced
fragments internally fixed through a dorsal approach but 3 of 7
initially nondisplaced fragments went on to symptomatic nonunion
requiring surgery.138 Volar MP
dislocations should have repair of the collateral ligaments and volar
plate to prevent late instability. Either a dorsal or a volar approach
is acceptable, and the one that provides access to the major pathology
should be chosen based on the individual patient’s preoperative
findings. Dorsally, a midline longitudinal incision provides good
access to manage any associated osteochondral fractures. One may have
to split the volar plate longitudinally and draw it around the sides of
the metacarpal head to accomplish a reduction. The volar approach
avoids splitting the volar plate but risks injury to digital nerves
which are tented over the deformity and lying directly under the
dermis. Volarly, the volar plate can be pulled back out of the joint
and reduced without splitting it.
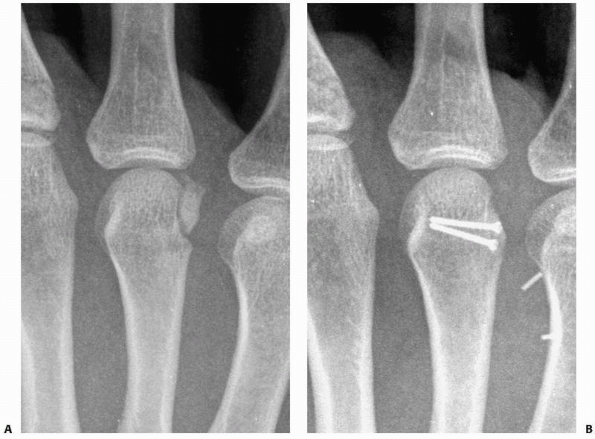 |
|
FIGURE 28-72 Collateral ligament injuries that (A) avulse a large bone fragment at the metacarpal head can be stabilized by direct bone fixation (B).
|
proportion to the surgeon’s assessment of instability following
reduction. While most patients may begin AROM immediately, those
injuries that demonstrate an extra degree of instability during the
postreduction assessment should be immobilized in partial flexion for 3
weeks. Whether simple or complex, the dislocations should be
immobilized in only partial (50-degree) flexion to allow ligament
healing under appropriate tension. After 3 weeks, AROM is progressed
until 6 weeks, when full passive motion including hyperextension is
allowed.
largely limited to UCL disruptions with a Stener lesion and volar or
irreducible MP dislocations.83 The results of acute repair of the radial
collateral ligament equal those of chronic reconstructions. This makes
a very weak case for early operative repair considering that no Stener
lesion exists on the radial side of the joint. Determining the presence
of a Stener lesion on the ulnar side of the joint remains an inexact
science; therefore, open management can be argued to be the treatment
of choice for all widely unstable ulnar-sided disruptions. Pure
ligamentous midsubstance ruptures can be repaired by direct suture. The
usual site of disruption is distally at the phalangeal insertion where
bone anchors can be used for ligament reinsertion. Thirty-six patients
with suture anchor repairs healed with loss of 10 degrees of MP joint
motion and 15 degrees of IP joint motion.170
Overtensioning should be avoided as insertion sites malpositioned
volarly or distally on the proximal phalanx will cause loss of motion.9 Arthroscopic reduction of the Stener lesion has been reported in eight patients.130
With bony avulsion fragments, tension band wiring, intraosseous wiring,
or fragment excision with ligament anchorage may all be used at the
surgeon’s discretion.
degeneration of the tendon substance has occurred) may require
reconstructive methods.47 Twenty-six
patients with tendon reconstruction for the thumb UCL followed for 4.5
years had 85% normal ROM and key pinch strength equal to the opposite
side at 20 pounds.60 High-grade
radial collateral ligament tears that are widely unstable may benefit
from direct soft tissue advancement and repair with 38 patients at
10-month follow-up achieving 92% of normal pinch and 87% were symptom
free.26
metacarpal head should identify any chondral or osteochondral
fractures. There are three strategies to manage these fractures. If the
fragment is small and extremely unstable, it should be excised. If the
fragment has a large subchondral bone base, it can be fixed with a
countersunk screw. If fixation is not possible but the fragment can be
stably trapped in its bed by the congruent opposing joint surface, it
can be further restrained with fine resorbable sutures. For collateral
ligament injuries associated with bone fragments, there are two
options. If the bone fragment is both large and solid enough to receive
definitive fixation, ORIF may be performed with a tension band wire or
lag screw. Twenty-five patients with base of P1 ligament avulsion
injuries were reported to have recovered full motion by 3 weeks
following volar approach single lag screw fixation.137
If the bone fragment is too small or too comminuted, the bone can be
excised and the end of the ligament reinserted to the cancellous bed of
either the metacarpal head or the base of the proximal phalanx. This
can be accomplished with a mini-bone anchor (many models are currently
available) or by transosseous suture. Surgery may not always be
necessary to achieve grip and key pinch strength in avulsion fractures
of the lateral base of P1. For example, 27 of 30 nonoperatively treated
patients achieved clinical stability despite a 25% incidence of
radiographic nonunion, but with only 19 of 30 reporting no pain.95
both finger and thumb MP joint ligament injuries indicates that the
clinical assessment of instability is paramount in planning subsequent
treatment. Local anesthetic injection into the MP joint allows vigorous
stress testing of the ligament to be performed without fighting the
patient or causing undue pain. Testing in both extension and flexion
reveals the absolute value of deviation as well as the discrepancy
compared with the uninjured side. The feel at the end point is also a
significant piece of information. A greater than 15-degree difference
side to side and a soft end point are stronger indicators of complete
ligament disruption than the absolute value of the joint angle when
stressed. The integrity of the volar plate should be assessed along
with the appearance of rotatory subluxation. I use a combination of the
clinical degree of instability and the presence of a palpable Stener
lesion to choose direct repair of the thumb UCL, the index RCL, and
large bony avulsion injuries. Thumb radial collateral ligament and
other finger MP joint injuries are managed nonoperatively. Volar
dislocations risk late instability if not surgically repaired. When the
patient presents late following a complete ligament rupture, direct
repair is rarely possible. The simplest reconstruction is then to
create a proximally based flap of retracted ligament and advance it
back to the anatomic insertion at the volar base of the proximal
phalanx. This tissue is not always of sufficient quality. When that is
the case, a free tendon graft (plantaris or palmaris longus) can be
placed through drill holes to reconstruct the ligament. With
appropriate rehabilitation, these patients can still achieve near
normal motion.
easily be approached with a midaxial incision that offers all the
advantages that are proposed for both volar and dorsal approaches.
Cartilage injuries on the metacarpal head can be well visualized, the
digital nerves are easily protected, and the volar plate can be guided
back into its correct position. For the long and ring fingers, I prefer
a transverse incision made at the level of the distal portion of the
metacarpal head. This level can reliably be found at the dorsal apex of
the sloping V shape of the web commissure. The sagittal bands do not
need to be divided but rather they can be retracted distally to access
the joint. The volar plate can be reduced without dividing it through a
combination of wrist flexion to relax the extrinsic flexor tendons and
MP hyperextension. A Freer elevator then guides the volar plate to the
distal surface of the metacarpal head before attempting to reduce the
joint itself. For the radial collateral ligament of the index, an
absorbable 1.3-mm bone anchor can be used for repair of insertional
ruptures and a 4-0 absorbable monofilament suture for midsubstance
ruptures. Pinning of the joint is not necessary in fingers as adjacent
digit strapping provides enough restraint to excessive coronal plane
deviation to protect the healing repair. The exception to this is the
rare high energy volar dislocation that is so unstable as to require 3
weeks of transarticular pin fixation.
over the ulnar aspect of the MP joint ensuring adequate volar exposure
at the base of the proximal phalanx. Care must be taken with the
superficial branches of the radial nerve to avoid neuroma formation.
There is usually one large branch passing through the surgical field
that is best mobilized dorsally. An incision in the adductor
aponeurosis is made just ulnar to the extensor pollicis longus tendon
with a cuff being left for repair. Reflection of this layer reveals the
joint capsule and torn collateral ligament (Fig. 28-73).
While all patterns of disruption have been reported, the most frequent
is that of distal avulsion from the base of the proximal phalanx. Often
there is a transverse rent in the dorsal capsule and
evidence
of volar plate injury as well. Direct repair is easiest with an
absorbable 1.3-mm bone anchor placed at the true insertion site on the
volar lateral tubercle to restore normal anatomy and reduce the
rotatory subluxation of the joint. The repair may include a suture
through the volar plate margin to recreate the “critical corner.” The
joint is pinned with a 0.045-inch K-wire before tying the anchor
sutures to prevent inadvertent radial deviation and early rupture of
the repair during the first 4 weeks postoperatively. A large bone
fragment carrying the point of ligament insertion can be stabilized
with one or two lag screws (Fig. 28-74).
The IP joint should be left free for motion at all times. Motion at the
MP joint can begin in a protected fashion at 4 weeks following pin
removal and then in an unprotected fashion by 6 weeks. Power pinch
activities that stress the ligament in the coronal plane of the thumb
should be avoided for up to 3 months after repair.
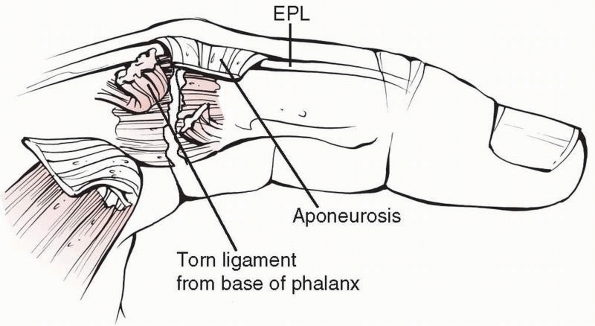 |
|
FIGURE 28-73
The approach to the ulnar side of the MP joint must protect dorsal digital nerve branches, leave a cuff for aponeurosis repair to the extensor pollicis longus (EPL), and provide adequate exposure to reach the true volar location of the tubercle at the base of the phalanx that represents the anatomic point of proper collateral ligament insertion or the “critical corner.” |
as for simple repair. The correct anatomic sites of ligament origin at
the metacarpal head and insertion at the phalangeal base should be
easily discernable, having remnants of the original ligament fibers.
Drill tunnels are made from each of these points obliquely directed
away from the joint with a 2.5-mm bit. Free tendon graft may be
harvested by conventional methods from either the palmaris longus
(within the operative field) or the plantaris (a more appropriate size
match). The tendon is passed through each of the drill holes and out
the opposite cortex where it may be grasped for tensioning of the
reconstruction (Fig. 28-75). The joint is
pinned with a 0.045-inch K-wire before setting the final tension. The
graft tension may be secured in any number of ways, but a simple method
involves the use of two absorbable 1.3-mm bone anchors. One anchor is
drilled adjacent to each bone tunnel, further away from the joint. The
tendon graft is captured by the sutures from the anchor at the margin
of the bone tunnel, thus fixing the tension in the graft between these
two points.
are often considered the banes of hand surgery. Although never totally
avoidable, these unwanted complications can be minimized by a thorough
knowledge of the branching patterns of the cutaneous nerves and
meticulous attention to detail at the time of surgery. The dorsal
digital nerve along the ulnar side the thumb MP joint is at high risk
of injury. It should be mobilized dorsally for the procedure and
checked each time before drilling. Perhaps the greatest risk is during
closure of the adductor aponeurosis along the margin of the extensor
pollicis longus tendon. It is quite easy to simply capture the nerve
branch with one of these sutures if it is not visualized to be clear
with each suture pass.
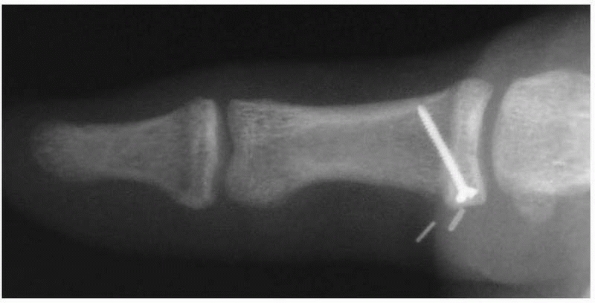 |
|
FIGURE 28-74
When a substantial bone fragment accompanies an ulnar collateral ligament injury to the MP joint, lag screw compression provides excellent stability through direct bone healing provided that there is not a multilevel injury of the ligament separating it from the bone fragment as well. |
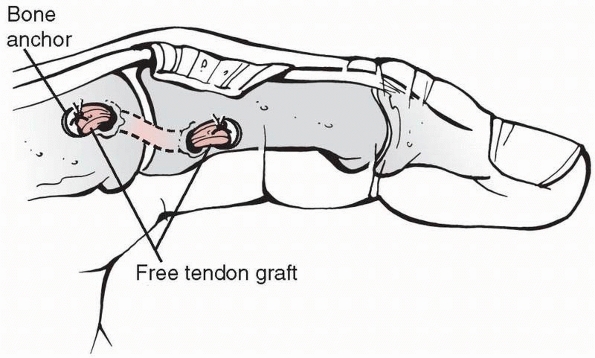 |
|
FIGURE 28-75
Free tendon graft reconstruction of the thumb metacarpophalangeal ulnar collateral ligament uses the same surgical approach as for direct ligament repair. Drill holes are made obliquely through the metacarpal and the phalanx from the points of anatomic ligament attachment so that a free tendon graft can be passed and tensioned. The graft may be secured by bone anchors adjacent to the bone tunnels. |
immobilization of any hand injury and especially when the injury is
located in the first web space. Since the first web is located at the
level of the MP joint, all positioning forces designed to prevent
contracture act on the proximal phalanx and across the MP joint. The
value of pinning the thumb MP joint with a 0.045-inch K-wire during the
4-week period of immobilization in a thumb spica splint is that the
splint may be appropriately molded to abduct the thumb and avoid web
space contracture.
metacarpal head, neck, and shaft. Intra-articular fractures of the
metacarpal base are covered in the next section on CMC joint
fracture-dislocations. Metacarpal head fractures present in a variety
of patterns requiring different treatment strategies aimed at restoring
a smooth congruent joint surface. Transverse metacarpal neck and shaft
fractures will typically demonstrate apex dorsal angulation. The normal
anatomic neck to shaft angle of 15 degrees should be recalled when
assessing the amount of angulation in subcapital fractures
radiographically. Radiographic assessment of apex dorsal angulation has
a high interobserver and intraobserver variability.99
Pseudoclawing is a term used to describe a dynamic imbalance manifested
as a hyperextension deformity of the MP joint and a flexion deformity
of the PIP joint (Fig. 28-76). This occurs as a
compensatory response to the apex dorsal angulation of the metacarpal
fracture (usually at the neck) and represents a clinical indication for
correcting the fracture angulation. Oblique and spiral fractures
tend to shorten and rotate more than angulate (Fig. 28-77).
As with all hand fractures, evaluation of rotation remains one of the
most critical assessments to make in order to avoid a functionally
disabling malunion. Ten degrees of malrotation (which risks as much as
2 cm of overlap at the digital tip) should represent the upper
tolerable limit. The problem of overlapping bone shadows has led to the
development of a number of specialized radiographic views (Fig. 28-78).
The Brewerton and Mehara views may show otherwise occult fractures at
the metacarpal bases. The reverse oblique projection allows a more
accurate estimation of angulation at the second metacarpal neck. The
skyline view may show vertical impaction fractures of the metacarpal
head not appreciable in any other projection.
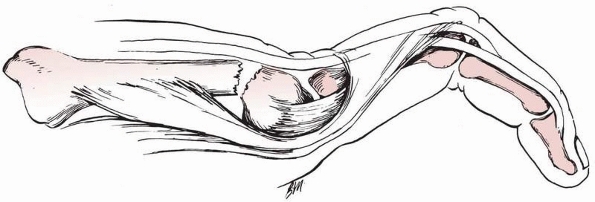 |
|
FIGURE 28-76
Pseudoclawing is an imbalance of compensatory metacarpophalangeal joint hyperextension and proximal interphalangeal joint flexion that occurs on attempted digital extension in proportion to the degree of apex dorsal angulation at the metacarpal fracture site and represents one indication for surgery. |
There are two transverse arches that exist at the CMC and MP joint
levels. The metacarpals themselves are longitudinally arched with a
fairly broad convex dorsal surface. Intramedullary geometry is highly
variable but with a consistently 20% thicker volar cortex. Surgical
access to the metacarpals is easily achieved through incisions placed
over the intermetacarpal valleys and curved distally to avoid entering
the digital web commissures.
 |
|
FIGURE 28-77 Long oblique and spiral fractures of the metacarpal shaft tend to shorten and rotate more than angulate.
|
strong interosseous ligaments at their bases and by the deep transverse
intermetacarpal ligaments distally. These connections help to maintain
the transverse arches of the hand, but flattening can occur with
multiple metacarpal fractures or crushing injuries. Shortening of
individual metacarpal fractures is limited by these same ligaments
(more effectively for the central metacarpals than for the border
metacarpals). For each 2 mm of metacarpal shortening, 7 degrees of
extensor lag can be expected.148 One of the weakest points in the metacarpal is the volar aspect of the neck, where comminution is often present (Fig. 28-80).
In the sagittal plane the primary deforming forces are the intrinsic
muscles, which can be counteracted through MP joint flexion, an
important component of the reduction maneuver for metacarpal fractures.
Correction of apex dorsal angulation and rotational control is achieved
indirectly by grasping the finger to exert control over the distal
metacarpal fragment. Flexion of the PIP joint for reduction, as has
been long recommended, is an unnecessary maneuver that actually
encumbers the reduction process by tensioning the intrinsics (Fig. 28-81).
The majority consists of cadaver studies evaluating different fixation
constructs in materials testing machines using transverse or oblique
osteotomies, cantilever, torsion, three- or four-point bending, and
producing load-displacement data. The inherent flaw in this whole
approach is that the stiffness of the implant is not the important
factor for the surgeon to consider. More important is the implant’s
fatigue failure properties in response to cyclic stress. Nevertheless,
the conclusions reached by nearly all the authors support the
following: (a) The interfragmentary lag screw is, biomechanically, one
of the most effective tools available to the surgeon. When applied
alone or with a plate, it can even resist nearly the same failure loads
as intact bone. (b) Self-tapping screws are as strong as standard
screws that require a separate step of advance tapping. (c) Plates
function most effectively as tension bands (which dictates dorsal
placement for metacarpal fractures). (d) Intraosseous wire constructs
placed in orthogonal planes (90 degrees/90 degrees) are not improved
with the addition of K-wires and are the only intraosseous wire
constructs that can compete with plates and screws. (e) All other
intraosseous wire designs are less rigid than screws and/or plates but
stronger than K-wires alone, which tend to slide through bone and
loosen. Modern plating systems tolerate applied loads in cadaver
specimens sufficient for immediate full active motion rehabilitation.141 Locking intramedullary nails can be used in special cases such as following gunshot wounds.7 External fixation has been reported even for closed fractures.108
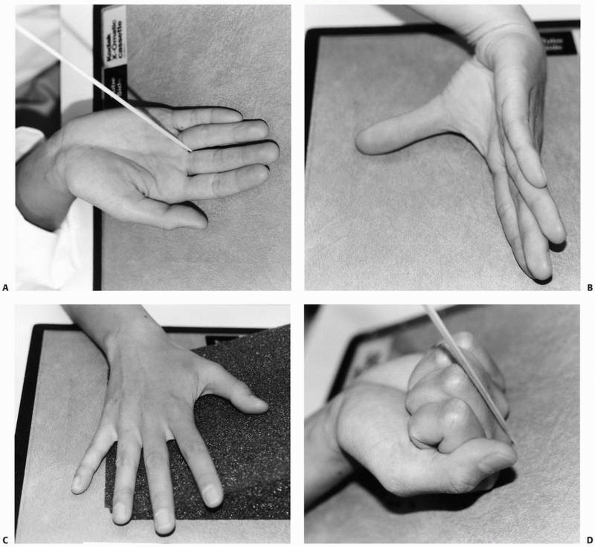 |
|
FIGURE 28-78 Specialized radiographic views may help to define injury patterns in the metacarpal including (A) the Brewerton view for the metacarpal bases, (B) the Mehara view for the index carpometacarpal relationships, (C) the reverse oblique view for angulation in the index metacarpal neck, and (D) the skyline view for vertical impaction fractures of the metacarpal head.
|
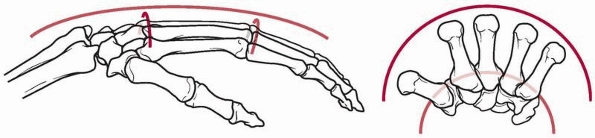 |
|
FIGURE 28-79
The three arches of the hand are the longitudinal arch and two transverse arches (one at the metacarpal bases and the other at the metacarpal neck level). |
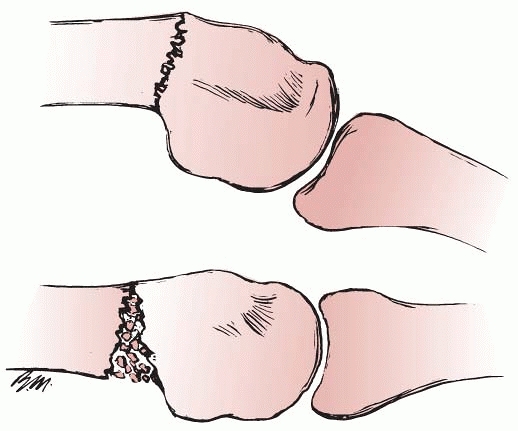 |
|
FIGURE 28-80
Fractures of the metacarpal neck frequently experience volar comminution and lack the inherent stability to resist apex dorsal angulation. |
Twenty-seven small finger metacarpal fractures with initial angulation
of 40 degrees were reduced and treated in a short hand cast for 4 weeks
with only 3 patients losing reduction beyond 15 degrees.30
Intra-articular fractures of the head and base may also be treated
nonoperatively provided the fracture plane is both stable and minimally
displaced. Metacarpal fractures with significant rotation or shortening
cannot be effectively controlled through entirely nonoperative means.
An externally applied splint exerts indirect (but not direct) control
over fracture position through positioning and reduction of
myotendinous deforming forces. A splint is able to preserve a fracture
position that is inherently stable but is not capable of reducing and
maintaining an unstable position. The stability of a metacarpal
fracture is determined primarily by the adjacent structures
(periosteum, adjacent metacarpals, deep transverse intermetacarpal, and
proximal interosseous ligaments) as well as the degrees of initial
displacement and comminution. Splinting should be directed at pain
control and neutralization of deforming forces. Surface contact should
be as broad as possible with an appropriate amount of padding. The
splint may be discontinued as soon as the patient can comfortably
perform ROM with the hand and not later than 3 weeks. Interphalangeal
joint motion should begin immediately following injury. A dorsal splint
in full MP joint flexion meets the patient’s needs well but may be more
than is required. Even less restrictive methods of functional bracing
have been advocated. Compared to simple adjacent digit strapping in 73
patients, a molded metacarpal brace for less than 40-degree angulated
fractures of the small finger metacarpal neck yielded similar clinical
results with less pain.70 Extending this concept, some have advocated functional mobilization for metacarpal fractures without splinting at all.14
Defining the acceptable limits of deformity for each injury location is
the subject of much controversy. Functionally, pseudoclawing is
unacceptable. Also, the patient may be troubled by the appearance of a
dorsal prominence at the fracture site or a shift in the metacarpal
head from its dorsally visible position toward the palm. Only rarely
will the shift toward the palm create a functional problem. Each
patient may have different degrees of deformity that he or she is
willing to tolerate. A correlation between deformity and symptoms has
not been clearly established. Greater degrees of angulation are
tolerable in neck fractures than in shaft fractures. Greater angulation
is tolerable in the ring and small metacarpals than in the index and
long metacarpals because of the increased mobility of the ulnar-sided
CMC joints. Biomechanically significant decay in flexor tendon
efficiency because of slack in the flexor digiti minimi and third volar
interosseous occurs with angulations over 30 degrees in the fifth
metacarpal neck, the site of greatest allowable angulation.3,12
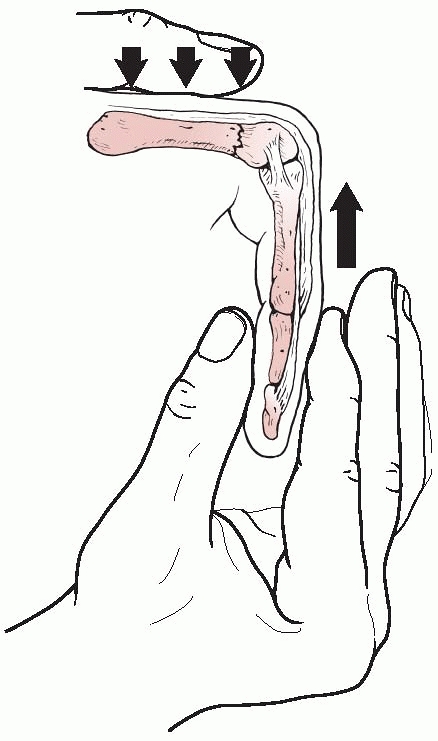 |
|
FIGURE 28-81
Reduction of metacarpal fractures can be accomplished by using the digit to control the distal fragment but the proximal interphalangeal joint should be extended rather than flexed. |
Twenty-five patients with small finger metacarpal fractures achieved
excellent functional results following stabilization with 3 transverse
K-wires and demonstrated no shortening, appreciable angulation, or
complications.56 A comparison
between transverse and intramedullary K-wires in 59 patients failed to
show any differences in outcome with no complications in either group.176
CRIF may be used for both extra-articular and intra-articular fractures
provided that the fracture is anatomically reducible and stable to the
stress of motion with only K-wire fixation (Fig. 28-83). CRIF is the minimum treatment necessary for metacarpal base fractures that cannot be held reduced by nonoperative means.
transverse and short oblique fracture patterns and include a single
large-diameter rod such as a Steinmann pin, an expandable
intramedullary device, multiple prebent K-wires, or specially
manufactured devices inserted at the metacarpal base designed
to achieve three-point intramedullary fixation52,63,64,102,107,116 (Fig. 28-84).
A single Steinmann pin may be inserted open through the fracture site
with the two fragments then impacted over it. Rotational control is
achieved by fracture fragment interlock, and motion can be started
immediately. The strategy of multiple, stacked prebent wires has
received broader acceptance than the other two strategies, perhaps
owing to the closed technique used for introduction.52,64,102,107
The wires are to be prebent such that three-point contact is obtained
dorsally at the proximal and distal ends of the metacarpal and volarly
at the mid-diaphysis (Fig. 28-85). This bow
opposes the natural dorsal convexity of the metacarpal and is the basis
for the apparently secure fixation achieved with this technique. The
pins are to be stacked into the canal, filling it and imparting
improved rotational control; as many as three to five 0.045-inch
K-wires may be required. Excellent results with multiple wires have
been reported primarily for fractures at the metacarpal neck level.52,107 One series of 20 patients with 5-year follow-up reported essentially no complications.107
Another series of 66 patients with 4.5-year follow-up noted eight
incomplete reductions (average 18-degree deformity) and 12 patients
with MP joint extensor lags of 10 to 15 degrees.52
|
TABLE 28-9 Metacarpal Fractures Not Involving the CMC Joints
|
|||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||
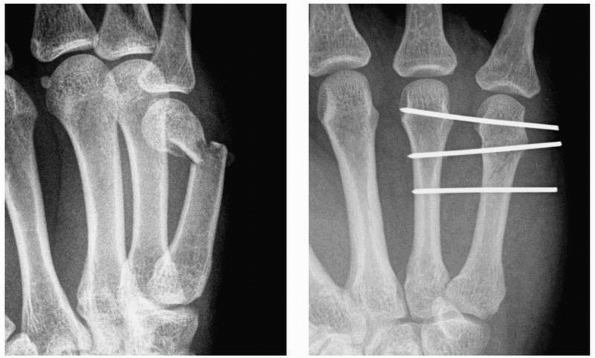 |
|
FIGURE 28-82
Closed reduction and internal fixation is effective for metacarpal neck fractures despite the smaller size of the head fragment and the need to achieve separation of the two wires that pass through it for control of fragment rotation in the sagittal plane. |
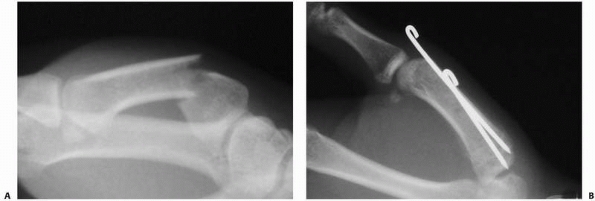 |
|
FIGURE 28-83 Extra-articular fractures of the thumb metacarpal (A) can be effective managed by (B) retrograde longitudinal pinning across the fracture into the base fragment.
|
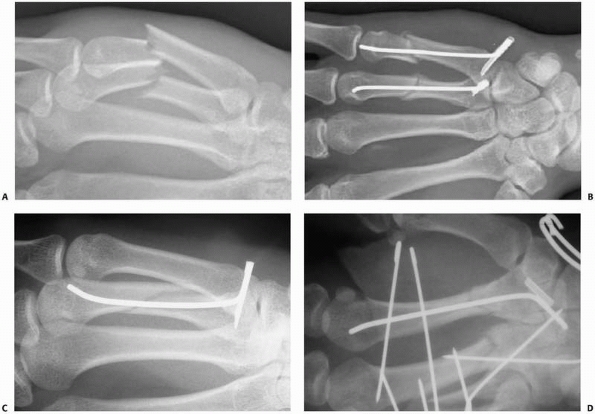 |
|
FIGURE 28-84 Fractures of the metacarpal at the same level that cannot be treated by transverse pinning (A) can be stabilized by (B)
a specially manufactured device shaped for three-point fixation and closed intramedullary application with a rotational locking sleeve used proximally. This device is also effective (C) in oblique fracture patterns and (D) fractures near the base. |
fractures that cannot be reduced and held by closed means. Internal
fixation is also required for multiple fractures without inherent
stability and for open fractures especially when associated with tendon
disruptions.54 Internal fixation can be accomplished with intraosseous wiring, composite wiring, screws only, or screws and
plates (Fig. 28-86).
Wiring techniques have traditionally held the advantage over plate and
screw application in terms of technical ease and availability of
materials. However, with the modular plating systems now available
specifically for use in hand surgery, lower profile fixation can be
achieved with greater rigidity (Fig. 28-87).
The most important consideration is that the surgeon should choose the
method of internal fixation with which he or she is the most
comfortable.
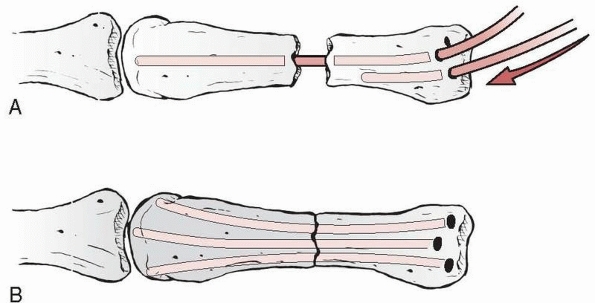 |
|
FIGURE 28-85
An alternative antegrade intramedullary fixation strategy includes multiple prebent 0.045-inch K-wires “stacked” into the canal in an attempt to achieve both rotational and angular control over the fracture. |
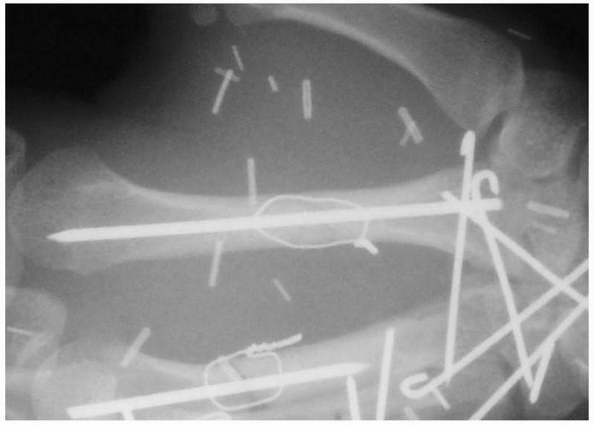 |
|
FIGURE 28-86
When rotational control is not sufficient with intramedullary fixation alone, composite wiring is useful and also adds a compressive force across the fracture site. |
screw-only fixation is the treatment of choice. If sufficient interlock
of bone spicules occurs, a single 1.2- to 1.5-mm countersunk screw can
control rotation of the fragment. If interlock is not effective, two
screws are preferred even if this means downsizing the screw diameter
to accommodate both of them in the fragment without causing comminution
(Fig. 28-88). For complete articular head
fractures, the condylar blade plate used to be required, but it is the
most technically demanding plate to apply. It is applied laterally with
the blade dorsal and the condylar screw hole volar. The drill hole for
the blade is round but the blade is rectangular in cross-sectional
area. This makes manual insertion of the blade into its hole difficult,
and a fine touch is required to not further comminute the metacarpal
head. More importantly, the exact angle of the drill path for the blade
must be determined in advance relative to the cortical surface of the
more proximal shaft against which the plate will be applied. The
condylar screw hole of the plate usually needs to be bent to avoid
prominence on its volar edge. Since the last edition of this text,
locking plate technology has become available in the size range for
small hand fracture plates. This allows fixed angle support of
comminuted periarticular fractures with the ability to contour the
plate first and avoid the complexity associated with inserting the
blade plate (Fig. 28-89).
 |
|
FIGURE 28-87
Plates are indicated for use with comminuted fractures lacking inherent stability and open fractures with associated soft tissue injury requiring immediate aggressive rehabilitation. |
direct proportion to the magnitude of the injury or the surgical
procedure performed.112 The more
tissue damage that is present, the more aggressive must be the motion
program. One frequently overlooked factor that greatly confounds
progress in therapy is edema control. External compression wraps to the
zone of injury with cohesive elastic bandages work to minimize the
presence of edema from the outset. When internal fixation has been
required, one must anticipate the development of an extensor lag at the
MP joint. Specific attention should be given to extensor tendon gliding
in zone VI to overcome a developing lag. Rapid tendon activation has
been successful in breaking free developing adhesions between the
peritendinous tissues and their surroundings77 (Fig. 28-90).
Patients should be allowed to use the hand for light activities
throughout the healing period. Light resistance activities can begin at
6 weeks. Extremely forceful use patterns should be deferred until 3
months.15
which are categorized as stable by virtue of having over 30% normal ROM
without motion at the fracture site, can be managed with entirely
nonoperative means using temporary splinting. Patients with entirely
nondisplaced fractures that have excellent inherent stability do not
require any external immobilization at all and can begin immediate
AROM, usually with the added protection of adjacent digit strapping.
Patients with stable metacarpal shaft fractures can be returned to
nearly all light activities in a hand-based splint that is continued
for a maximum of 3 weeks. Stable neck and intra-articular head
fractures are more effectively protected by support that covers from
the PIP level to the forearm
with
the MP joints in full flexion. At least one adjacent digit is included
with the affected ray. Interphalangeal joint motion should begin
immediately with all strategies.
 |
|
FIGURE 28-88 Metacarpal head fractures consisting of only a few fragments are best stabilized by countersunk small lag screws.
|
 |
|
FIGURE 28-89 Metacarpal head fractures with (A) high degrees of comminution and inherent instability may require (B) plate stabilization to avoid collapse.
|
 |
|
FIGURE 28-90 Even following open reduction and internal fixation, when a properly designed rehabilitation program is administered, (A) complete flexion and (B) hyperextension are possible.
|
treatment of choice for all unstable closed metacarpal fractures except
multiple adjacent fractures at the same level that include a border
digit (Fig. 28-91). The biomechanics of the
transverse pinning strategy is that of external fixation. Four points
of control are needed. The two points closest to the fracture site on
either side should be as close together as possible. The two farthest
from the fracture site should be as far apart as possible. The proximal
intermetacarpal and CMC ligaments are stout enough to qualify as the
most proximal point of fixation such that only one 0.045-inch K-wire is
required proximal to the fracture site. The distal most pin should
avoid transgression of the sagittal bands if at all possible. This must
be titrated clinically against the goal of placing the point of
fixation as far from the fracture site as possible. The transverse
pinning strategy works equally well for central (long and ring) and
border (index and small) metacarpals. If the four finger metacarpals
are conceived of as occurring in two columns (a radial column for index
and long and an ulnar column for ring and small), then most
combinations of multiple metacarpal fractures can still be fixed with
this strategy, and it can always be used if there is only one fracture
per column. If both metacarpals in the column are fractured, but at
different levels, they can be used to reciprocally stabilize each other
(Fig. 28-92). The specific requirement for
reciprocal stabilization to be effective is that there is a zone in the
diaphysis of both bones where two pins can be placed with adequate
spacing from each other (distal to one fracture site and proximal to
the other). At the conclusion of the procedure, one has the choice of
leaving the pins protruding through the skin or cutting them off
beneath the skin. In previous editions of this chapter I had advocated
allowing pins of less than 4 weeks’ duration to be left outside the
skin for ease of removal, but I now cut nearly all pins below the skin
level given the prevalence of MRSA in the community. The hand is
initially splinted in full MP flexion to resist the development of
contractures. Early motion can proceed while the pins are still in
place.
 |
|
FIGURE 28-91
Transverse closed reduction and internal fixation functions under the same biomechanical principles as external fixation. Note the distal wire is placed just proximal to the collateral recess of both bones and has also avoided tethering the sagittal bands. |
multiple fractures not meeting the criteria for reciprocal transverse
stabilization. When fracture plane interlock between bone spicules is
present, intraosseous wiring, composite wiring, screw-only, or screw
and plate fixation may all be considered. I prefer lag screw fixation
for long-oblique or spiral
fractures since CRIF cannot control the reduction of these patterns nearly as well as transverse fractures (Fig. 28-93).
To select screw-only fixation, the ratio of the length of the oblique
or spiral fracture plane to the bone diameter must be at least 2:1.
Furthermore, to avoid comminution, the screws must pass through an area
in the bone spike where the screw outer diameter is less than one-third
the width of the spike. The screw sizes most appropriate for a
metacarpal are 1.5 and 1.7 mm. Multiple open transverse or short
oblique fractures of the mid-diaphysis from open crushing injuries are
nicely managed with intramedullary pins. Rotational control can be
supplemented with a composite wire loop. When interfragmentary
compression cannot be achieved owing to the presence of comminution or
bone loss, plates and screws are indicated.
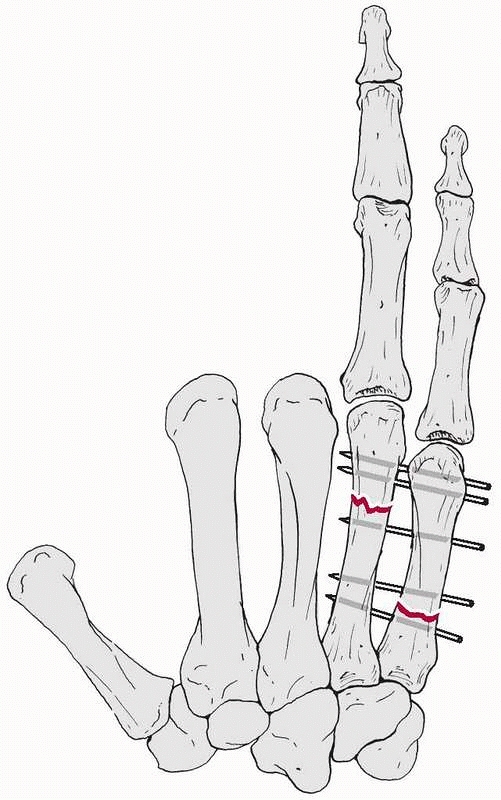 |
|
FIGURE 28-92
Reciprocal transverse stabilization of adjacent metacarpal fractures is possible when the levels of the two fractures are separated enough to be able to place two pins that fall distal to the first fracture and proximal to the second such that the first metacarpal is sufficiently stabilized to in turn provide stability to the other metacarpal. |
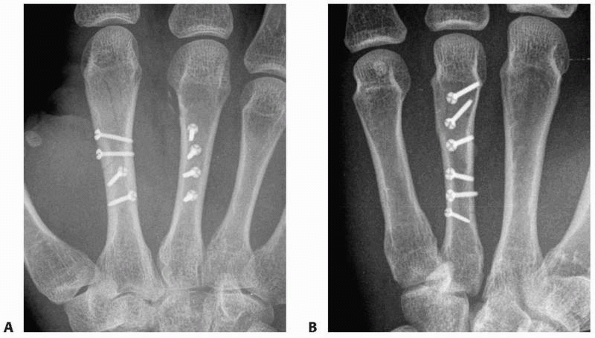 |
|
FIGURE 28-93 Interfragmentary lag screws allow stable fixation of (A) adjacent metacarpals and (B) three fragment fractures with an intermediate butterfly fragment sufficient to permit full, immediate motion rehabilitation.
|
essential to cover the hardware with periosteal closure to provide a
separate gliding layer. I prefer to operate 3 to 5 days following
injury so that the periosteum will have thickened in response to injury
and both can be dissected as a discrete tissue flap and closed with
solid suture purchase. Unlike over the proximal phalanx, the extensor
tendons at this level are discrete cords, and placement of the hardware
away from them should be possible in most cases. Placement of the plate
dorsally puts it on the tension cortex of the bone, but in this
position it interferes most directly with the extensor tendons.
Placement of the plate in a true lateral position allows sagittal plane
forces to be resisted by the width of the plate rather than its
thickness, and doing so is almost always possible, just technically
more difficult. This is my choice for plate placement unless
extenuating circumstances dictate dorsal placement. One such
circumstance is fracture comminution extending all the way to the base
of the metacarpal. All the technical comments made in the section on
proximal phalangeal fractures apply equally here.
Rotational malunions here will be the most obvious and functionally
disabling. In large part, the management of metacarpal fractures is all
about ensuring that rotation is correct. Length and angulation are, of
course, not to be forgotten. The assessment of rotation both
preoperatively and intraoperatively merits discussion. In both cases,
the examiner should not touch the digit during the assessment. The
awake, preoperative patient may require an anesthetic block to relieve
enough pain so that he or she is capable of flexing sufficiently to
demonstrate the rotational status of the digit. In the anesthetized
patient, tenodesis driven by full-range wrist motion produces
sufficient flexion and extension of the digit that rotational alignment
can be accurately judged.
intraoperative imaging will effectively demonstrate depth of pin
penetration and coronal plane fracture orientation. Metacarpal overlap
obscures any individual metacarpal lateral view. Ensuring that the pins
have penetrated both cortices of both metacarpals cannot be judged
radiographically and must be determined by feel at the time of
placement. If the reduction is difficult to obtain closed or tends to
slip as the pins are driven, the case does not have to be converted to
a full open reduction. A small instrument such as a
dental
pick or microelevator can be placed percutaneously at the fracture site
to directly control reduction while the surgeon proceeds with the
otherwise entirely closed pinning. Compared with plating of phalangeal
fractures, there is even greater risk of inducing an iatrogenic
rotational malunion when tightening down the screws. If a metacarpal
plate has not been axially contoured correctly, when the screws are
tightened, the plate will actually rotate the distal fragment out of an
otherwise previously correct reduction. For this reason, no matter how
many times the reduction has already been clinically evaluated, it must
be evaluated at least one more time upon final placement of all
fixation.
joints are usually high-energy injuries with involvement of associated
structures, often neurovascular (Fig. 28-94).
Particular care must be given to the examination of ulnar nerve
function, especially motor, because of its close proximity to the fifth
CMC joint. Frequently, the pattern is one of fracture-dislocation
involving the metacarpal bases, the distal carpal bones, or both.93
Overlap on the lateral radiograph obscures accurate depiction of the
injury pattern, and most authors recommend at least one variant of an
oblique view.177 The Brewerton view
may be helpful in this respect, profiling individual metacarpal bases.
Another special view has been described for the second metacarpal base.240
When fracture-dislocations include the dorsal cortex of the hamate, CT
or polytomography may be necessary to fully evaluate the pathoanatomy.
Another pattern to recognize is dislocation of one CMC joint with
fracture of an adjacent metacarpal base. Shortening can be evaluated by
noting a disruption in the normal cascade seen distally at the MP
joints. Volar CMC dislocations are rare.
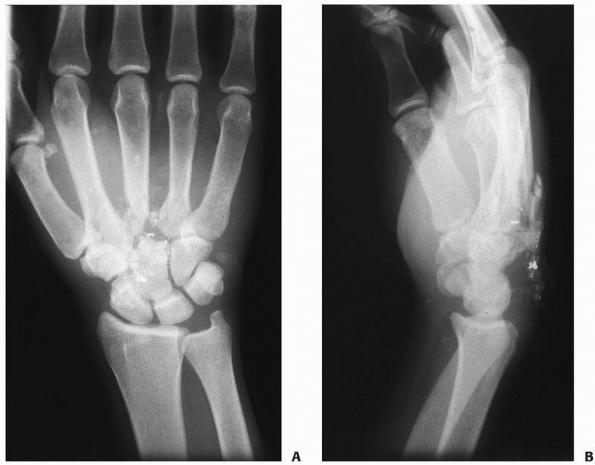 |
|
FIGURE 28-94 Fractures of carpometacarpal joints (A) are typically high-energy injuries with (B) comminution of both the metacarpal base and the distal carpal row.
|
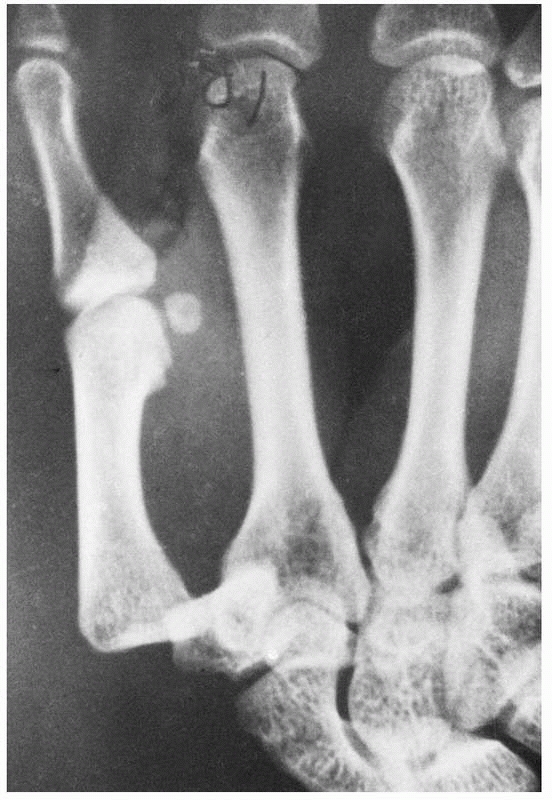 |
|
FIGURE 28-95 Pure dislocations of the thumb carpometacarpal joint are rare injuries and typically occur dorsoradially.
|
Motorcyclists may be uniquely prone to sustaining this rare injury and
to having the injury missed on initial evaluation. The injury will
often be reduced before being seen by the surgeon. Clinical diagnosis
is then based on identifying the residual instability. Differentiating
complete from incomplete ligament rupture is essential, as initial
operative treatment is appropriate
only
for complete disruptions. Instillation of local anesthetic into the
joint may be required to allow an unimpeded examination. Manual stress
testing compared with the contralateral side should allow diagnosis in
most cases.
The majority of thumb CMC joint injuries are fracture-dislocations
rather than pure dislocations. The smaller fracture fragment at the
thumb metacarpal volar base is deeply placed and not palpable. Eponyms
associated with these fracture-dislocations are Bennett (partial
articular), and Rolando (complete articular) fractures. Specific
radiographs must be obtained in the true AP and lateral planes of the
thumb (not a series of hand radiographs) if injuries along this axis
are to be correctly identified (Fig. 28-97).
system of four ligaments. There is a high degree of variation with
dorsal, multiple palmar, and two sets of interosseous ligaments (only
one between the long and ring metacarpals).40,114
The interosseous ligaments are the strongest and have a V-configuration
with the base of the V oriented toward the fourth metacarpal. Range of
motion of the index and long CMC joints is limited to less than 5
degrees, with 15 degrees at the ring, and up to 25 to 30 degrees at the
small finger. Small finger CMC motion is reduced 28% to 40% when the
ring finger is immobilized.44 The
axis of motion is located near the base of the metacarpal. The index
metacarpal has a particularly stable configuration through its
wedge-shaped articulation with the trapezoid. The small finger CMC
joint is the only joint not having a gliding configuration but instead
is a modified saddle-shaped joint. The increased mobility on the ulnar
side of the hand may predispose to its greater frequency of injury.
Critical soft tissue relationships to appreciate during treatment of
injuries to the CMC joints are the positions of the motor branch of the
ulnar nerve directly in front of the fifth CMC joint and the deep
palmar arch in front of the third CMC joint. Of all hand fractures and
dislocations, injury at the CMC level requires the highest degree of
vigilance regarding associated neurologic injury. The high-energy
mechanism of these injuries and profound degrees of swelling may lead
to worsened outcomes through residual long-term nerve compression.
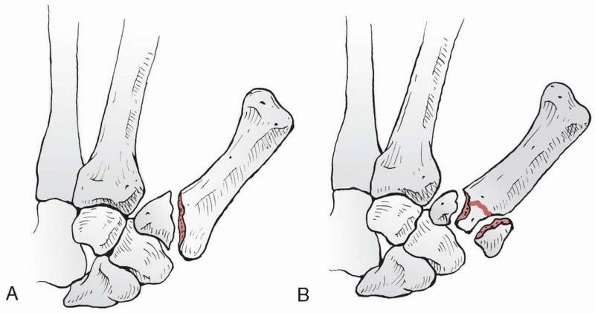 |
|
FIGURE 28-96 The most recognized patterns of thumb metacarpal base intra-articular fractures are (A) the partial articular Bennett fracture and (B) the complete articular Rolando fracture.
|
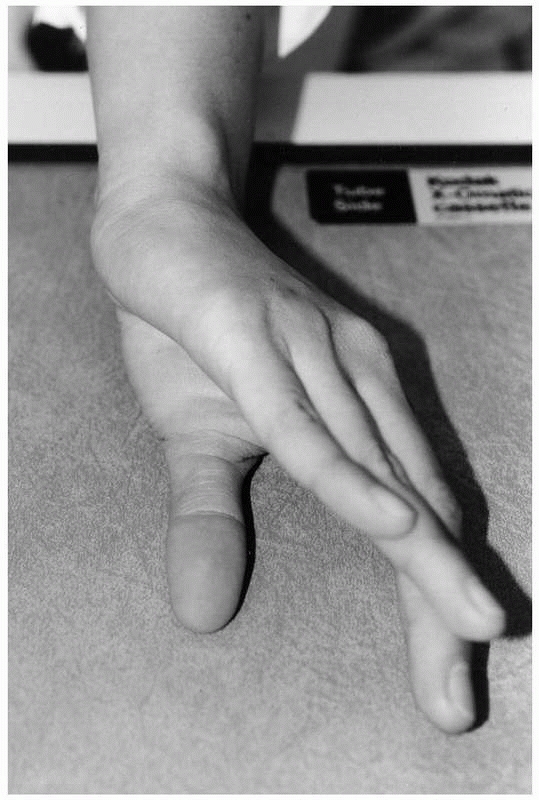 |
|
FIGURE 28-97
The thumb does not reside in the same plane as the rest of the hand. A true AP view of the thumb can be obtained with the Robert view. |
superficial radial nerve ramify throughout the region of the thumb base
on the radial side. Three tendons pass through this region: the
abductor pollicis longus (APL), extensor pollicis brevis (EPB), and
extensor pollicis longus (EPL). The radial artery passes beneath the
APL and EPB on its course to the first web space and lies just proximal
to the CMC joint. The joint anatomy includes reciprocal saddle-shaped
surfaces of the distal trapezium and proximal metacarpal. The axis of
this concavoconvex joint is then itself curved in a third plane with
the convexity lateral. The normal ROM at the thumb CMC joint is around
50 degrees of flexion-extension, 40 degrees of abduction-adduction, and
15 degrees of pronation-supination. There is consensus as to which
ligaments are anatomically present at the trapeziometacarpal joint (Fig. 28-98). They are the superficial
anterior oblique, deep anterior oblique (beak), ulnar collateral, intermetacarpal, posterior oblique, and dorsoradial ligaments.10
A point of confluence exists at the palmar ulnar tubercle of the first
metacarpal base. There was a period of disagreement regarding the
primary stabilizing ligament in preventing dislocation between the deep
anterior oblique and the dorsoradial ligament. Although the deep
anterior oblique was previously considered the primary stabilizer, more
recent research has effectively demonstrated that the dorsoradial
ligament is the prime restraint to dislocation. The dorsoradial
ligament is the shortest ligament in the group and the first to become
taut with dorsal or dorsoradial subluxation.10 Selective ligament sectioning showed that deficiency of the dorsoradial ligament led to the greatest degree of subluxation.164
Dorsal dislocation usually occurs through rupture of the dorsal
ligaments with a sleevetype avulsion of the anterior oblique ligament
as it peels off the volar surface of the first metacarpal.148
Supination may also play a significant role in the mechanism of this
injury. Deformation of fractures at the base of the thumb metacarpal
occurs with a complex motion (Fig. 28-99). The
distal metacarpal is adducted and supinated by the adductor pollicis.
At the same time, the APL pulls the metacarpal radially and proximally.
Reduction maneuvers must attempt to counteract each of these forces.
Probably the most difficult aspect of the reduction to maintain through
splinting is the radial displacement of the base.
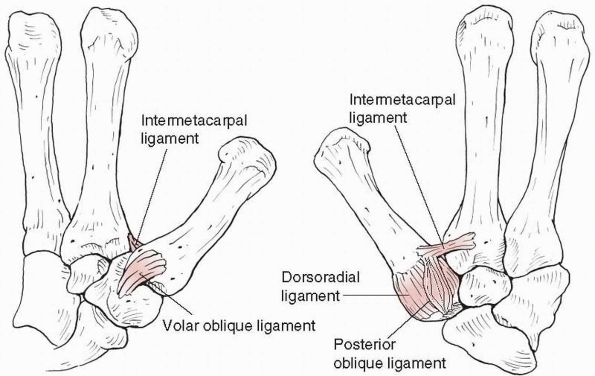 |
|
FIGURE 28-98
The primary stabilizing ligaments of the thumb carpometacarpal joint include the deep anterior oblique, dorsoradial, posterior oblique, and intermetacarpal ligaments. The superficial anterior oblique and ulnar collateral ligaments are not primary stabilizers. |
Dorsal finger CMC fracture-dislocations usually cannot be held
effectively by external means alone. Although usually acceptable as the
least invasive method of treatment for most injuries, entirely
nonoperative management of pure thumb CMC dislocations does not provide
sufficient stability for accurate healing of the ligaments. It is not
possible through external means to completely maintain control over the
reduction of a widely displaced intra-articular fracture-dislocation at
the base of the thumb throughout the entire period of healing. However,
the need to achieve anatomic union in these fractures has been
questioned. Although no one study is definitive, the risk of
significant malunion when managing an initially widely displaced
intra-articular fracture is too great to warrant entirely nonoperative
management.
is the treatment of choice. The technique involves restoration of
anatomic length to the shortened and dislocated metacarpals through the
combined application of traction and direct pressure at the metacarpal
bases. Manual reduction is then followed by placement of 0.045-inch
K-wires across the metacarpal shaft and into either the carpal bones or
into adjacent stable metacarpals (Fig. 28-100).
Adequacy of reduction as well as stability should be evaluated both
radiographically and clinically. Pins should remain for 6 weeks. Unlike
most other hand fractures, residual instability rather than stiffness
is the risk with this injury.
Initially
open fractures and those with tissue interposition preventing reduction
will require ORIF. Open reduction is much more likely to be required in
cases presenting late and may be accomplished as long as three months
after the initial injury (Fig. 28-101).
The stabilization strategy is the same as for CRIF with the open part
of the procedure being used strictly for reduction purposes.51,136
Excellent long-term stability without pain is achieved in the majority
of cases. In more severe cases, immediate arthrodesis of the CMC joints
may be required.69
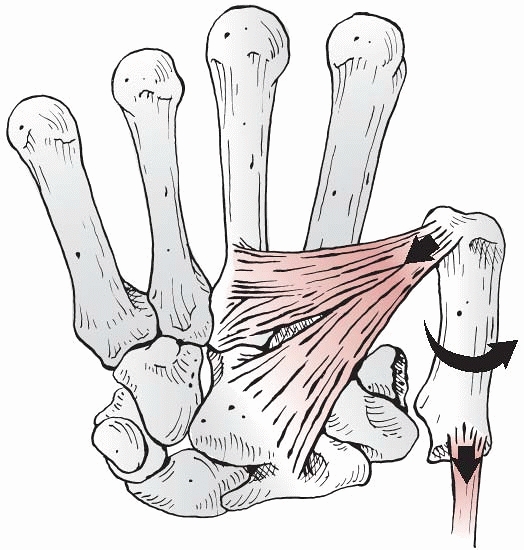 |
|
FIGURE 28-99
Displacement of Bennett fractures is driven primarily by the abductor pollicis longus (proximal migration) and the adductor pollicis (adduction and supination). |
|
TABLE 28-10 Carpometacarpal Joint Dislocations and Fracture Dislocations
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||
 |
|
FIGURE 28-100
Isolated carpometacarpal fracture dislocations can be reduced and pinned closed to a stable adjacent metacarpal and to the distal carpal row. |
sufficient to consistently prevent long-term symptoms of instability
and arthritis in pure thumb CMC dislocations. In a series of eight
dislocations pinned for 6 weeks and immobilized for a total of 7.4
weeks, four required ligament reconstruction (three for symptomatic
instability and one for progression of early posttraumatic arthritis).139
Based on these poor results, the same authors subsequently treated the
next nine patients with early ligament reconstruction, resulting in no
late symptoms, full motion, and normal grip strength139 (Fig. 28-102).
stabilization is the treatment of choice for nearly all Bennett
fractures and some Rolando fractures (Fig. 28-103).
A series of 32 patients followed for 7 years with intra-articular
step-offs of less than 1 mm found no difference between closed pinning
and ORIF for Bennett’s fractures with the exception of a higher
incidence of adduction contracture in the pinning group.105 Advocates of internal fixation may choose to manage less comminuted Rolando’s fractures and some Bennett’s fractures with ORIF.101
When there are reasonably large fragments that will support purchase of
at least one solid screw per fragment, one may consider plate and screw
stabilization of a Rolando fracture (Fig. 28-104).
However, ORIF of a Rolando fracture is not for the occasional hand
surgeon. Comminution is the rule rather than the exception, and
restoration of normal anatomy is quite difficult. The combination of
limited internal fixation and external fixation to support the length
and unload the articular reduction may be helpful in complex Rolando’s
fractures. A series of ten patients managed this way and followed at 35
months showed 88% key pinch strength compared with the contralateral
side with 9 of 10 patients having good or fair overall satisfaction.19 While some series have deemphasized the role of anatomic reduction in improving long-term results, others have stressed its
role. Eighteen patients followed to 10.7 years showed a clear
correlation between the quality of reduction and posttraumatic
arthritis.159
A similar series with over 7-year follow-up demonstrated a clear
correlation between radiographic post-traumatic arthritis and greater
than 1-mm step-off in the final reduction.158
Twenty-one patients achieved 80% of normal grip strength despite
radiographic signs of degeneration in 16 that did not correlate to
clinical outcome.16 Thirty-one
patients followed at 7.3 years demonstrated a correlation of both
radiographic signs of osteoarthritis and (more important) symptoms of
pain with the final residual displacement when healing occurred with
more than a 2-mm articular step-off.90
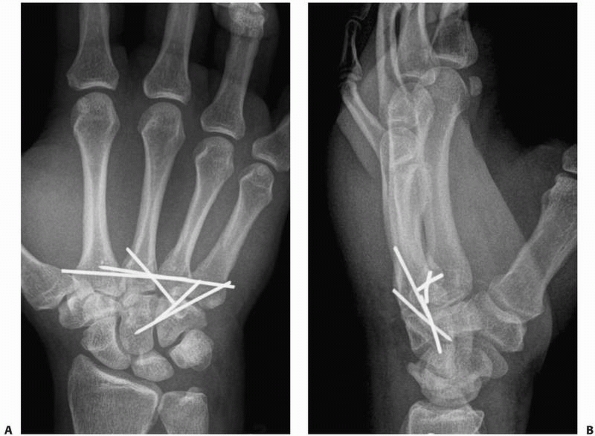 |
|
FIGURE 28-101 Multiple highly unstable carpometacarpal dislocations are at high risk of incomplete reduction and require (A) multiple points of fixation and (B) a careful check on the lateral radiograph to identify any residual dorsal subluxation.
|
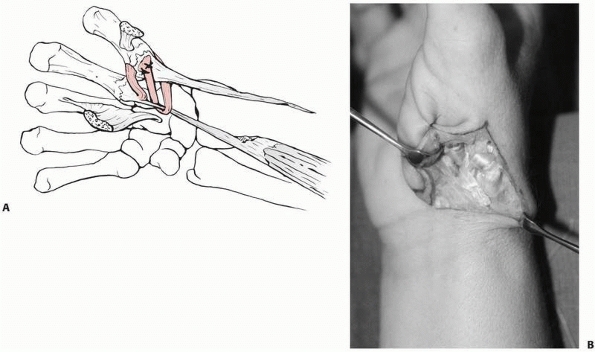 |
|
FIGURE 28-102 Reconstruction of the thumb carpometacarpal ligaments can be performed with (A)
a split flexor carpi radialis graft woven through a bone tunnel in the thumb metacarpal base, exiting the dorsal cortex, passing deep to the abductor pollicis longus, around the intact remaining flexor carpi radialis, and back to the volar radial aspect of the metacarpal base. B. This procedure is accomplished through a traditional Wagner approach. |
 |
|
FIGURE 28-103 A. Bennett fractures can be stabilized with (B) closed pinning to the index metacarpal base and across the carpometacarpal joint into the trapezium.
|
orthoplast splint. The primary problem with finger CMC joint injuries
is residual instability, not joint stiffness. The MP joints should be
left free throughout the aftercare period with attention paid to
excursion of the common digital extensor tendons. For thumb CMC joint
injuries, immobilization is continued for 6 weeks in a thumb spica
splint. The IP joint should be left free throughout the postoperative
period. Following cast removal the patient undergoes a standard
progression of ROM exercises that graduates as tolerated into
functional use by 8 to 10 weeks. Forceful pinch loading is avoided for
3 months after surgery.
 |
|
FIGURE 28-104
Rolando fractures are highly unstable and require techniques such as fixed angle plates adjacent to the subchondral bone to resist collapse and sometimes even a smaller second plate placed at 90 degrees to the primary plate. |
either the metacarpal bases or carpal bones of the distal row. However,
the absence of such fractures creates an opportunity for successful
management by CRIF. The metacarpal bases must both be felt to engage
their articulations fully and demonstrate complete congruence on
radiographs. This is one injury pattern where the added time invested
in obtaining true radiographs rather than fluoroscopy alone is
worthwhile to assure this congruence. Only when the x-ray beam passes
tangentially through the joint can an accurate assessment be made. It
is practical to use the fluoroscope to determine the angle of
projection that best demonstrates the reduction and then try to
reproduce the shot with the plain radiograph. K-wires are retained for
6 weeks outside the skin with an additional 2 weeks of splint
protection before initiating wrist and CMC rehabilitation. All other
joints remain mobile throughout the postoperative period.
an excellent choice. Cases seen many days after injury or those with
tissue interposition will likely require ORIF to achieve accurate
reduction. The approach may be dictated by the presence of an open
traumatic wound. Otherwise, a dorsal transverse incision at the level
of the joint is best. Branches of the superficial radial nerve and
dorsal cutaneous branch of the ulnar nerve must be identified and
protected not only from the surgical approach to reach the injury site
but also during pin placement. The common extensor tendons overlie the
central metacarpal bases, and the wrist extensor tendons insert on the
border metacarpals. Incision of the extensor retinaculum increases the
lateral mobility of these tendons, allowing the surgeon to work around
them. Bone and cartilage fragments too small for fixation but large
enough to create third body wear in the joint should be
removed.
Fixation is founded upon 0.045-inch K-wire passage from the metacarpal
bases across the CMC joints into the distal carpal row. If adjacent
metacarpals are stable without CMC joint injury, transverse
stabilization between metacarpal bases is an excellent addition.
Evaluation of the dorsal cortices of the hamate and capitate should be
performed on each case as these are often also fractured. Large bone
fragments should be restored to their cancellous beds and fixed with
countersunk compression screws. Small bone fragments should be excised.
Index or long finger CMC joints with extensive articular cartilage
damage are good candidates for primary arthrodesis. Motion in the ring
and small finger CMC joints should be preserved if possible but
arthrodesis remains an acceptable method of management as a last resort.
treatment for this injury despite basic principles that should allow
this method to produce satisfactory results. Although some articles
suggest that one needs to perform immediate free tendon graft
reconstruction of complete thumb CMC dislocations, this has not been my
experience. I have consistently found open ligament repair to produce
stable and pain-free motion. The reproducible surgical findings are a
sleevelike avulsion of the deep anterior oblique ligament from the
volar surface of the metacarpal and a rupture of the dorsoradial and
posterior oblique ligaments. The rupture has usually been distally from
the metacarpal insertion. The procedure is easily accomplished by
inserting a series of 1.3-mm bone anchors around the margin of the
metacarpal base and using the sutures for anatomic repair of the dorsal
ligaments. The joint should be pinned in a reduced position before
tying down the dorsal ligaments. The deep anterior oblique ligament
comes to lie flush with the metacarpal surface when the joint is
reduced and stabilized. Pins are retained for 6 weeks with thumb CMC
joint motion being instituted at that time. Light pinch is also allowed
with progression to power pinch by 3 months postoperatively.
the remainder augmented with small openings to control small articular
fragments or pack bone graft into the metaphysis, and the final
minority with full ORIF. The soft tissue anatomy of this region should
be taken into account when placing pins. The drill should not be
activated until the pin is solidly placed down to bone. Bennett
fractures can be stabilized with either one or two pins. The primary
pin reduces and stabilizes the shaft of the metacarpal to the
trapezium. An alternative to trapezium pinning is to pin the thumb to
the index metacarpal or to both. A second pin may be placed across the
two fragments to prevent the development of an articular step-off, but
this pin will not hold the fracture surfaces opposed. Many surgeons do
not even use this second pin.
different. The primary aim is to provide distraction to allow healing
through the often-comminuted metaphyseal zone. This is best
accomplished by pinning the thumb metacarpal (with two 0.062-inch
K-wires) to the index metacarpal rather than to the trapezium. It is in
the complete articular cases with comminution that making a small
opening to place an elevator into the metaphysis may prove useful. The
articular fragments can be molded against the distal surface of the
trapezium and kept there by either packing bone graft in behind them or
with additional smaller-caliber (0.035-inch) pins placed transversely
at the subchondral level to maintain articular congruity. The advantage
of plate and screw stabilization of an intra-articular fracture in
general is usually to allow early motion of the joint for the sake of
cartilage nutrition and preservation of long-term ROM. The small
fragments at the base of the thumb metacarpal are more at risk of
devascularization with a widely open procedure that includes periosteal
stripping to place a small titanium plate. I have not experienced that
long-term loss of motion is a problem at the trapeziometacarpal joint
following 6 weeks of pin immobilization for these fractures. I have
observed that the presence of the plate results in adherence of the
extensor pollicis longus and brevis tendons and can cause long-term
loss of motion of both the MP and IP joint, which is a clinically
relevant problem.
along the glabrous/nonglabrous border of the thumb base may be curved
in a volar and transverse direction to expose the thenar muscle group (Fig. 28-102B).
Reflection of these muscles reveals the joint capsule volar to the
insertion of the APL. Arthrotomy reveals the intra-articular fracture,
and subperiosteal dissection along the shaft allows for placement of a
plate. Stable internal fixation of Rolando’s fractures is only possible
when the fragments are large enough to accept the purchase of
individual screws. My current fixation of choice in this situation is a
titanium locking condylar plate (either 1.7-mm or 2.3-mm depending on
the size of the patient). Eccentric drilling of the condylar holes can
add transverse compression between the articular base fragments. If
ORIF is chosen for a Bennett’s fracture, a smaller version of the same
approach is used to allow sufficient access to compress the reduction
and place an interfragmentary lag screw from dorsal to volar. Recently,
micro-sized variable pitch headless screws have become available and
are well suited to the fragment sizes seen in a Bennett’s fracture.
provides ample opportunity for the occurrence of two complications
frequent in hand surgery: injury to cutaneous nerves and pin tract
infections. The injury to cutaneous nerves is likely to occur by a pin
rather than during dissection and particularly when approaching the
radial side of the thumb base. Pins are retained longer here (6 weeks)
than for stabilization of metacarpal (removed by 4 weeks) or phalangeal
(removed by 3 weeks) fractures. There is thus more time for a pin tract
infection to develop. The pearls and pitfalls for finger CMC joint
fracture-dislocations are contained in two statements: Be sure the
joint is fully reduced, and do not miss associated carpal bone
fractures of significant size. Although most isolated single ray CMC
fracture-dislocations occur in the small finger axis, there is a
reproducible pattern that will occasionally be seen for the index ray
where the articular base is split into two good quality fragments very
amenable to a percutaneous headless compression screw fixation (Fig. 28-105).
difficult injuries to treat but are made much simpler by approaching
their management as follows: Conceive of where the shaft of the thumb
metacarpal lies when in a correct functional position relative to the
rest of the hand and pin it there (to the index metacarpal) with two
0.062-inch K-wires. Then make the articular surface of the metacarpal
base congruent with supportive bone graft and/or small subchondral
wires through a limited opening. What originally appeared as an
impossible undertaking now becomes a relatively simple two-step process.
 |
|
FIGURE 28-105
An isolated index metacarpal carpometacarpal fracture-dislocation can be percutaneously reduced and stably fixed with a headless variable pitch compression screw. |
internal fixation are high and often attributable to the complex nature
of the injuries for which this treatment method is selected. In a
series of 41 metacarpal and 27 phalangeal fractures, complications
related to hardware (45%), extensor lag (19%), and infection (12%) were
seen.119 Another series of 37
phalangeal fractures reported a 92% complication rate including 60%
extensor lag, and 38% fixed flexion contracture.121
Increased complication rates were associated with
intra-articular/periarticular locations with extension to the shaft,
open injuries, associated soft tissue injury, and the need for bone
graft. As long as 18 months may be required for soreness and stiffness
to abate following small joint dislocations. In 490 severe phalangeal
fractures, there were 31 (6%) nonunions, 44 (9%) malunions, and 8 (2%)
infections.166
infections, 18 malunions, 17 delayed unions or nonunions, 23
fixationrelated complications, and two late amputations.151
These complications were usually associated with Swanson type II wounds
(14% compared with 1.4% in type I wounds) but not with the use of
internal fixation, high-energy injury, large wound size, or associated
soft tissue injury.
An 11% infection rate occurred in 146 open hand fractures, all in
Gustilo type II or III injuries, and in association with a crushing
component.13 Preoperative wound cultures were of no help, and S. aureus
was the most commonly isolated species. In current practice, MRSA is
the most commonly isolated species. The role of antibiotics in reducing
the infection rate in noncontaminated open wounds with intact vessels
has not been supported. When 198 patients were randomized in a
double-blind placebo-controlled study with flucloxacillin for open
distal phalangeal fractures, there were seven superficial and no deep
infections (three with antibiotic, four without).147
of the most common following a fracture or dislocation of the hand is
stiffness. Twenty-two of 54 patients failed to achieve TAM over 180
degrees following plate fixation of phalangeal fractures.94
Stiffness is a product of the magnitude of the original trauma, the age
and genetic composition of the patient, the duration of immobilization,
the position of immobilization, and the invasiveness of any surgical
intervention. The primary factors influencing stiffness are the
associated soft tissue injury and the age of the patient.24,173
Too often the position of immobilization violates the fundamental
principles of splinting ligaments at full length and balancing tendon
forces that act across the fracture site.53
First web space contractures are common and can be minimized by pinning
or splinting the thumb metacarpal in maximum abduction. Active versus
passive motion discrepancies most commonly appear in the form of an
extensor lag. The overlying extensor tendon becomes adherent to the
fracture site and its subsequent failure of excursion produces an
extensor lag at the next most distal joint. This is most common at the
PIP joint following fractures of P1 with adherence of the flat and
broad extensor tendon in zone IV. Only 11% of phalangeal fractures
fixed with plates had a TAM of greater than 220 degrees.121
A focused rehabilitation technique that uses the differential
viscoelastic properties of tendon and scar tissue can be used to
maximize extensor excursion over both phalangeal and metacarpal
fractures.77 Once a fixed
contracture has been established by the time of tissue homeostasis
following the initial trauma, tenocapsulolysis is required if the
patient desires to improve motion.100
One of the chief concerns with operative management of thumb MP
ligament disruptions has been the loss of motion. Loss of motion may be
more significant in patients undergoing late reconstructions as
occurred in 21 patients from a series of 70 after free tendon graft.95
little padding between the surface and a complex array of small-caliber
nerve branches. There are very few locations for either surgical
incisions or percutaneous pins where small nerve branches are more than
1 cm away. Hypersensitivity is a frequently seen consequence of the
mechanism of injury itself. Crush injuries are almost invariably
accompanied by some degree of hypersensitivity. When surgical
management is performed soon after the injury, the procedure itself is
often erroneously blamed for causing
the
hypersensitivity. Some areas are at higher risk than others. Neuroma
formation through direct injury or nerve encasement in postoperative
scar should be guarded against when one is operating along the ulnar
side of the thumb MP joint with its high concentration of small dorsal
digital nerve branches and at the radial side of the wrist near the
superficial radial nerve. Treatment is based on a combination of
specific medications designed to reduce nerve pain such as gabapentin,
amitriptyline, or pregabalin and a progressive contact desensitization
therapy program. Gentle surface contact essentially trains the
sensitive nerve fibers to tolerate that level of stimulation before
then progressing to more intense stimulation. Eventually, the patient
works his or her way up to normal use of the hand over a period of
weeks. In the meantime, overstimulation of the nerve pain by traction
and motion must be avoided even if this means slower progress in the
motion program. Failure to heed this principle will result in
progression from straightforward hypersensitivity to complex regional
pain syndromes and a downward spiral of worsening pain and function
that far exceeds the simple early reduction in motion.
 |
|
FIGURE 28-106
Malunion of proximal phalanx fractures is typically apex volar with a compensatory loss of extension at the proximal interphalangeal joint correctable only with osteotomy. |
hand fractures owing to a lack of understanding regarding hand
biomechanics, to an unfounded belief that all hand fractures do well
with nonoperative treatment, or to a noncompliant patient. Malunions
are managed with corrective osteotomy. Each aspect of the deformity
must be well understood from angular to rotational to length
considerations. The decision is whether to place the osteotomy at the
site of original deformity or to make a compensatory osteotomy that
produces reciprocal deformities. Fundamentally, it is best to make the
correction at the site of the original deformity. The problem is
hardware interference with soft tissues. The plate and screws usually
necessary to stabilize the correction may not fit well at the site of
original deformity. Another consideration is the healing potential of
metaphyseal as compared with diaphyseal regions particularly if the
diaphyseal bone has been stripped of its blood supply during prior
procedures. A popular location for rotational corrections in particular
is the metacarpal base for the above reasons.
apex volar usually occurs because of failure to splint the hand in the
position of full MP flexion that will correct the dynamic imbalance
across the fracture site (Fig. 28-106).
Rotational malunion is usually the result of improper choice of
nonoperative treatment when direct fixation was needed to control
rotation. Spiral fractures are difficult to correctly reduce closed,
and rotational malunions can easily result from CRIF especially at the
level of the proximal phalanx. Using nail plate alignment is an
inadequate method of assessing rotation, which should be judged by
parallelism of the short tubular bone segment distal to the injured one
with the intervening joint flexed to 90 degrees. Corrective osteotomy
is more successful at the metacarpal level than the phalangeal level61 (Fig. 28-107). Correction of a sagittal plane or multidirectional malunion is best accomplished at the site of the original fracture.98,161
Significant stiffness often accompanies the malunion. A concomitant
tenocapsulolysis can be performed if rigid fixation of the osteotomy is
achieved. The alternative is to break the solution down into two parts:
stage 1 achieves correction of the skeletal deformity through
osteotomy, and stage 2 improves motion through tenocapsulolysis. These
patients achieve the greatest gains in motion even though the measured
final range may be less than that of other patients with less severe
injuries.18,159
Tenolysis alone improves extensor lag, but when a dorsal capsulotomy is
required to regain flexion, the lag may actually increase. For mild to
moderate malunions, a realistic assessment regarding the expected
improvement in function must be weighed carefully against the predicted
degree of digital stiffness created by the osteotomy procedure itself
and the hardware used.163,178 Intra-articular osteotomy is an extremely demanding undertaking and should be restricted to carefully selected patients (Fig. 28-108).
Five patients undergoing extra-articular osteotomy for malunited
unicondylar fractures of the proximal phalanx saw an increase in
average PIP motion from 40 degrees preoperative to 86 degrees
postoperative.71 Surgery may be performed as late as several months after the initial injury through the original fracture plane.
apex dorsal sagittal plane deformity. Patients may complain of the
cosmetic deformity, pain at the dorsal prominence, or grip
discomfort
with a prominent metacarpal head in the palm. Patients should be
counseled to evaluate their deformity and decide if their
dissatisfaction is sufficient to warrant undergoing corrective
osteotomy. The osteotomy should be delayed until tissue homeostasis has
been achieved unless an opportunity for early intervention (less than 6
weeks) exists (Fig. 28-109).
Correction is best achieved through the site of the original fracture
with rigid internal fixation followed by immediate motion. In choosing
between opening wedge, closing wedge, pivot osteotomy, or oblique
osteotomy, the exact pattern of deformity needs to be assessed and the
osteotomy designed to most closely restore normal anatomy. This will
demand a different cut for each patient, but the simpler the intended
osteotomy, the more likely it is that the surgeon can achieve a good
result. Shortening must be considered if a closing wedge is planned. An
extensor lag at the MP joint of 7 degrees can be predicted for every 2
mm of shortening.148 Rotational
malunion in a metacarpal may also occur, causing digital overlap.
Osteotomy can be performed at the site of original injury or at the
metacarpal base. Rotational osteotomy performed at the base of the
metacarpal offers broader cancellous surfaces for healing and can
correct up to 25 to 30 degrees of rotation. If the plane of deformity
is more complex than pure rotation, it may be wiser to attempt
multiplanar correction through the original fracture site.
 |
|
FIGURE 28-107
Corrective osteotomy often requires prolonged healing and bone graft and is best supported by a laterally placed locking plate at both the (A) metacarpal and (B) phalangeal level. |
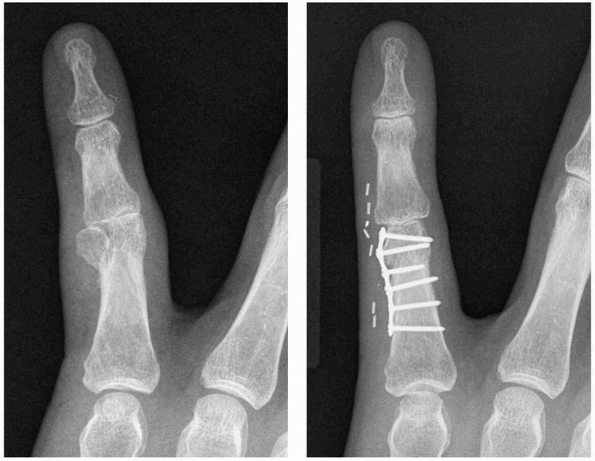 |
|
FIGURE 28-108
Intra-articular corrective osteotomy is a demanding undertaking but can produce excellent results when precise attention is given to restoring articular congruence. |
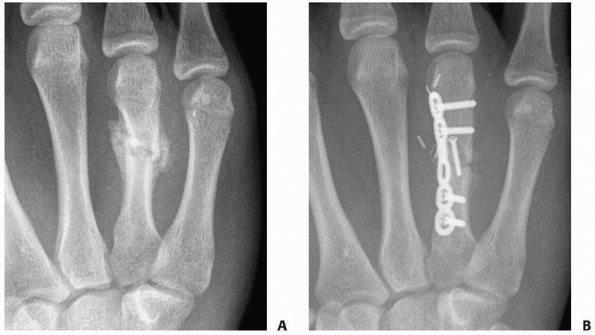 |
|
FIGURE 28-109
Nascent malunions that have healed by callus but where the original fracture plane can be cut with an osteotome by hand rather than a saw (A) are excellent opportunities to achieve a true anatomic restoration as opposed to a close approximation (B). |
infrequent indications, as correction of an intra-articular malunion is
extremely difficult. In long-term follow-up, intra-articular malunion
at the metacarpal base leads to osteoarthritis (65%), decreased grip
(49%), and pain (38%).89 Arthrodesis
is the preferred solution for these problems, even for the fifth
metacarpal. It reliably improves grip strength with the elimination of
pain. Compensatory triquetrohamate motion may alleviate the effect of
arthrodesis on the mobility of the ulnar side of the hand.
the exception of distal phalanx fractures, when CRIF has caused
distraction, or in fractures treated with ORIF where excessive
periosteal stripping has occurred. Nonunions are treated no differently
than anywhere else in the body. Hypertrophic nonunions may be addressed
by compression alone using a dynamic compression plate. Nonunions with
bone loss or inadequate vascular supply require supplementary bone
grafting in addition to stable fixation. Tuft fractures of the distal
phalanx rarely achieve osseous union, going on instead to fibrous
union. Transverse shaft fractures of the distal phalanx left without
support too early may result in an apex volar malunion or nonunion
after being repeatedly subjected to pinch forces. Microsized headless
variable pitch compression screws are now available to treat P3 shaft
nonunions, but caution is still required in assessing the relationship
of the screw to the sagittal plane dimension of P3, risking both
fracture extension and damage to the overlying nail apparatus171 (Fig. 28-110). Four nonunions were seen in a series of 52 unstable hand fractures, of which 61.5% were open.24
A treatment for phalangeal nonunion consisting of a Herbert screw
placed through the distal joint has been proposed based on the results
in four patients.171 If no bone loss
is present, simple compression across a hypertrophic nonunion site with
a short plate should be sufficient to achieve healing. If bone loss is
present, a longer plate and corticocancellous or cancellous bone graft
may be required. Osteonecrosis of the metacarpal head remains a concern
in periarticular fractures that may lack an independent blood supply.
distally but more common proximally. All five carpometacarpal joints
are quite subject to recurrent instability particularly with pure
dislocation patterns rather than fracture-dislocations. The reason is
that in pure dislocation, all the ligaments are ruptured and require
ligament-to-bone or ligament-to-ligament healing. Fracture-dislocations
usually occur with one or more key stabilizing ligaments remaining
attached to the smaller fragment that remains at the joint while the
larger articular fragment dislocates. If properly reduced and
stabilized, bone-to-bone healing will restore joint stability. In one
series, redislocation occurred in 6 of 56 dorsal fracture-dislocations
of the PIP joint.34 Chronic
instability following closed treatment of a complete MP joint radial
collateral ligament injury may need to be treated surgically. A small
population of patients exists with chronic hyperextension laxity at the
thumb MP joint that may be either passive (volar plate only) or active
(involving the intrinsics) and may in a few instances require surgical
advancement of the volar
plate
for reconstruction and restoration of stability. Late symptomatic
(painful) instability after finger CMC fracture-dislocation can be
evaluated with lidocaine injection into the joint. If relief is
provided, arthrodesis is a reliable way to eliminate the pain. The
fifth CMC joint may be fused in 20 to 30 degrees of flexion with little
long-term loss of hand motion, apparently through increased
compensatory triquetrohamate motion. Thumb CMC painful residual
instability is treated by ligament reconstruction rather than
arthrodesis.
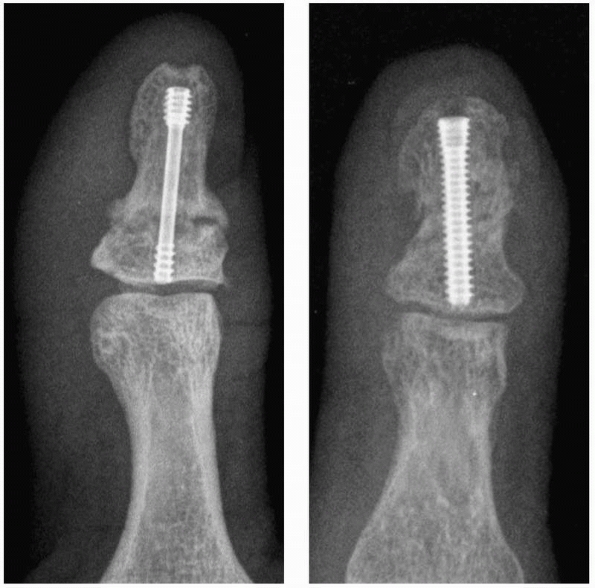 |
|
FIGURE 28-110
Nonunions of the distal phalanx shaft can be managed by adding compression across the nonunion site with a headless variable-pitch cannulated microscrew; healing is prolonged. |
intra-articular fractures and residual joint instability may cause
accelerated hyaline cartilage wear and lead to posttraumatic arthritis.
A poor correlation exists between the radiographic appearance of
posttraumatic arthritis and clinical loss of function and pain.
Patients should be managed for the arthritis on the basis of clinical
deficits and not based on radiographic abnormality. Posttraumatic
arthritis of the thumb MP joint can be successfully managed by
arthrodesis with excellent overall hand function. Few other joints in
the hand can be fused with so little impact on function (index and long
finger CMC joints). Finger MP and PIP joint fusions result in
tremendous loss of function.
internal fixation of hand fractures and occasionally for stabilizing
dislocations, but they can demonstrate complication rates as high as
15%.144 Pin tract infections are the
most common complication seen. Infections used to be rare when pins
were left in for less than 4 weeks and usually responded well to
removal of the pin and administration of oral antibiotics. With the
increasing prevalence of MRSA in the community, that no longer seems to
be true, and pins may be more safely cut below the skin level. Another
hardware complication is simply irritation of adjacent tissues such as
overlying tendons by the presence of prominent hardware. Given the
delicate and thin tissues of the hand, even implants measuring several
millimeters thick are enough to produce persistent symptoms for many
patients. In one series, 7 of 57 patients required plate removal.117
Another series reported a complication rate of 82% following plate
fixation for phalangeal fractures compared with 31% for metacarpal
plates.160 A unique concern with
plates, however, is the potential for delayed or nonunion in transverse
metacarpal fractures (30%) as opposed to fracture sites with a broader
interface (7%).55
dislocations of the joint adjacent to the site of tendon insertion.
Failure to recognize this associated injury may occur with an
inadequate examination. The consequence is usually a deformity posture
such as mallet finger at the DIP joint or a Boutonniere deformity at
the PIP joint. Open reconstructions of chronic terminal tendon ruptures
with either local tissues or free tendon grafts have not proven
particularly successful. For disabling terminal tendon deficiencies in
a high angle of flexion, arthrodesis of the DIP joint is a permanent
and durable solution to the problem. The loss of motion associated with
arthrodesis is not as well tolerated at the PIP joint where every
effort should be made to restore active extension. Mild deformities
especially when identified reasonably early may respond to a program of
PIP extension splinting and DIP joint flexion exercises. Success is
dependent on the natural tendency of collagen-based scar to contract.
For more substantial deficiencies, surgical reconstruction with local
tissues or a free tendon graft may be required once passive motion has
first been regained through either rehabilitation or a previously
staged surgical capsulectomy.
the delicate matrix tissues. Temporary or permanent passage of fixation
devices through the region of the germinal matrix should be avoided,
and sterile matrix penetration should be either temporary or by suture
material. A rare but troublesome complication is entrapment of the
germinal matrix in a transverse fracture gap (which can occur with a
reasonably normal external appearance of the digit) that both prevents
fracture healing and results in permanent nail deformity.
technical methods of reduction and fixation for fractures and
dislocations of the hand. Controversy is much greater when it comes to
deciding how specific fractures and dislocations should be managed.
Most surgeons understand and accept the basic principle that the least
invasive method should be used that will result in stable, anatomically
correct healing and still permit enough motion rehabilitation to
achieve a useful and functional final result. The problem lies in the
fact that the data simply do not exist anywhere in the published
literature to definitively link specific treatment strategies to the
many different fracture patterns that exist. Each of the various small
bones in the hand (P3, P2, P1, metacarpal) responds to treatment
differently. There are numerous varieties of just the fracture pattern
alone in each of these bones, not to mention the associated soft tissue
injuries that impact final outcome substantially. No study has used
rigorous enough statistics to separate all the groups and stratify the
results. The same holds true for dislocations.
difficult is that of coordinating more complex reconstructions that
involve multiple tissues. When the original management of skeletal
trauma to the hand yields unsatisfactory results, secondary surgery may
be required. The timing and order of events are very much a matter of
individual surgeon experience and preference. The foundation for good
hand function is a stable inner skeletal structure and a
well-vascularized and supple outer envelope of integument. These are
the first steps to be accomplished in any reconstruction. The next step
is to ensure passively supple joints that are also stable. This
infrastructure is then powered by three groups of tendons responsible
for active motion in the hand: the extrinsic extensors, the extrinsic
flexors, and the intrinsics. Good motion facilitates interaction with
the environment, a function that also requires sensibility.
Reconstructive surgery of nerves is well timed to coincide with tendon
procedures. Three stages have been outlined here, but this does not
necessarily mean that three distinct surgical procedures are required.
Judging which combinations of procedures will yield the best results is
the province of an experienced revision hand surgeon. In general,
procedures that require the same type of rehabilitation may be
combined, whereas those that have disparate therapy goals should be
separated as distinct surgical events. When a series of surgical
procedures is staged, tissue homeostasis after the former procedure
should be achieved before executing the subsequent procedure.
microvascular whole joint transfer was previously implantation of a
Swansontype one piece silicone prosthesis with the attendant high rates
of prosthetic fracture and generation of silicone debris leading to
osteolysis. Since earlier editions of this text, new prosthetic
implants have become available for total joint replacement of the MP
and PIP joints. There are models with metal on polyethylene bearing
surfaces as well as pyrolytic carbon-bearing surfaces. Rates of
loosening, osteolysis from debris, and prosthetic breakage will
determine if these models offer a new opportunity for improved hand
motion and function to those with posttraumatic arthritis in the MP and
PIP joints.
locations or in the diaphysis. Diaphyseal loss is by far the more
straightforward issue. Current controversies relate to the choice of
purely cancellous graft with bridge plating as opposed to
corticocancellous grafts. Additional controversy exists regarding the
timing of bone grafting for open fractures. The traditions have been
corticocancellous grafts with delay. New trends are for immediate
grafting after extensive debridement and using purely cancellous graft.144
Osteoarticular defects can be replaced with nonvascularized
osteoarticular autografts as long as the defect only involves at most
one half of a joint.87 Partial toe
joint osteochondral grafts to the PIP joint of the hand resulted in
significant motion loss in three of five cases and resorption in one.57
The most common sites requiring partial osteoarticular grafts are
single condyles at the head of P1 and the volar base of the middle
phalanx. Toe PIP joints provide well-matched condyle donor sites. The
dorsal portion of the hamate provides an excellent donor site for the
volar base of the middle phalanx. Nonvascularized whole joint transfers
have been unsuccessful. If an entire joint requires autogenous
replacement, a vascularized whole joint transfer from the foot is
required. Unique cases offer the opportunity to create a pedicled,
vascularized whole joint transfer from one unsalvageable digit to an
adjacent digit.
other reconstruction. It is often performed at the same time as
skeletal reconstruction and should be performed before most other
reconstructions except first-stage tendon grafting. Methods of wound
reconstruction include primary closure, secondary closure, split- or
full-thickness skin grafts, transposition flaps, pedicle flaps, and
free flaps. The simplest strategy that provides for optimum gliding of
subjacent structures without contracture formation should be chosen.
The challenge for more complex wounds that require flap reconstruction
in the hand is finding tissue that is both supple and thin. Current
trends are for earlier applications (within 72 hours) of increasingly
thinner flaps. A useful strategy involves fascial flaps that are
covered with split-thickness skin grafts. The lateral arm flap inverted
to orient the muscular surface to receive the skin graft has performed
particularly well in this respect.76
The fascia overlying the serratus anterior is thin with a reliable,
large, and long pedicle. One criticism of skin-grafted fascial flaps is
that they are slightly more difficult to operate through at the time of
further revision compared with cutaneous flaps. The current trend in
microsurgery for perforator flaps has spawned a number of cutaneous
flaps thin enough for use around the hand, wrist, and forearm but not the digits.
showed maintenance of strength for 8 weeks comparable to titanium but
then degraded with loss of strength over 12 weeks under four-point
bending stress.13 Testing in 112
fresh-frozen cadavers of 2-mm poly-L/DL-lactide plates demonstrated an
overall stability comparable to that of 1.7-mm titanium plates. There
have been studies such as these in the literature,168,169
but the regular use of bioabsorbable implants in the hand simply has
not caught on clinically. One concern may be reports of sterile abscess
formation around implants of the same materials used in other
orthopaedic applications. The soft tissues of the hand have little
tolerance for any process that might cause additional inflammation at
the site of skeletal trauma.38 At
the same time, there is no doubt that the physical presence of a plate
(even when 1.3 to 2.0 mm in thickness) along the surface of a short
tubular bone can create significant problems for tendon adherence and
obstructed motion. Since the last edition of this text, there has been
no apparent advance toward greater use of bioabsorbable implants for
hand fractures.
diverse group of injuries that share a common theme in management. The
hand is a delicate organ that requires both stability and flexibility;
function follows form. Although rough guidelines can be drawn from the
published literature, it remains the responsibility of individual
surgeons to judge which fractures and dislocations can be managed by
each of the various methods discussed in this chapter. There are three
basic treatment options for most fractures and dislocations of the
hand: splinting, CRIF, and ORIF. Many fractures and the majority of
dislocations of the hand have enough inherent stability to be managed
nonoperatively. Testing for inherent stability in the office setting
using active motion under the protection of injectable anesthetics
should demonstrate those fractures and dislocations that can safely be
managed without surgery. Malrotated, multiple, high-energy, and open
fractures are usually treated operatively. CMC dislocations and
fracture-dislocations (unlike MP and PIP joint injuries) are usually
treated operatively. The majority of operatively treated hand fractures
and dislocations are closed and isolated injuries for which CRIF is
usually an appropriate method. The exceptions to this are noted
throughout the chapter. A few select injury patterns such as
intra-articular P2 base fractures have specific and unique treatments
that must be remembered and used according to the indications
described. Once underway with treatment, one should stay focused on
edema control and promoting early motion. The final steps to a
successful outcome lie in avoiding complications such as nerve
hypersensitivity and pin tract infections. When complications do occur,
the key is in planning a well-thought-out correction in terms of
risk-benefit analysis and staging. Finally, patients should be
counseled regarding expectations, which are that fractures and
dislocations of the hand produce swelling, stiffness, and aching that
frequently takes more than 1 year to overcome.
S-O, Sollerman C, Lundborg G, et al. Diagnosis of displaced ulnar
collateral ligament of the metacarpophalangeal joint of the thumb. J
Hand Surg 1990;15A: 457-460.
A, Davis TRC. Dorsal fracture-dislocation of the proximal
interphalangeal joint: a comparative study of percutaneous Kirschner
wire fixation versus open reduction and internal fixation. J Hand Surg
2005;30B:120-128.
Extra-articular transverse fractures of the base of the distal phalanx
(Seymour’s fracture) in children and adults. J Hand Surg
2001;26B:201-206.
K, Toh S, Nakahara K, et al. Treatment of soft tissue injuries to the
dorsum of the metacarpophalangeal joint (Boxer’s knuckle). J Hand Surg
2002;27B:90-95.
HG, Gonzales MH, Hall Jr RF. Locked intramedullary nailing of
metacarpal fractures secondary to gunshot wounds. J Hand Surg
2006;31A:1083-1087.
A, Riano F, Ravikoff J, et al. Dynamic intradigital external fixation
for proximal interphalangeal joint fracture dislocations. J Hand Surg
2005;30A:154-160.
CHG, Tencer AF, Trumble TE. The effect of thumb metacarpophalangeal
ulnar collateral ligament attachment site on joint range of motion: an
in vitro study. J Hand Surg 1999;24:283-287.
PC, Linscheid RL, Berger RA, et al. An anatomic study of the
stabilizing ligaments of the trapezium and trapeziometacarpal joint. J
Hand Surg 1999;24: 786-798.
BT, Hanel DP. Self-tapping versus standard tapped titanium screw
fixation the upper extremity. J Hand Surg 1998;23A:308-311.
MS, Daley R, Greenwald DP. Metacarpal fracture angulation decreases
flexor mechanical efficiency in human hands. Plast Reconstr Surg
1997;99:1079-1083.
KJ, Perez LE, Wilson DR, et al. Mechanical testing of bioresorbable
implants for use in metacarpal fracture fixation. J Hand Surg
2001;26:755-761.
J, Bednarski M, Niedzwiedz Z, et al. The results of operative treatment
of fractures of the thumb metacarpal base. Acta Orthop Belg
2001;67:368-373.
RT. Mechanical requirements for application and modification of the
dynamic force couple method. Hand Clin 1994;10:221-228.
U, Gupta A, Ruf S. Corrective osteotomy for posttraumatic malunion of
the phalanges of the hand. J Hand Surg 1996;21B:33-42.
U, McCollam SM, Oppikofer C. Comminuted fractures of the basilar joint
of thumb: combined treatment by external fixation, limited internal
fixation, and bone grafting. J Hand Surg 1991;16A:556-560.
KC, Spilson SV. The frequency and epidemiology of hand and forearm
fractures in the United States. J Hand Surg 2001;26:908-915.
MP. Grade III radial collateral ligament injuries of the thumb
metacarpophalangeal joint: treatment by soft tissue advancement and
bony reattachment. J Hand Surg 2003;28:14-20.
CD, Saing M, Raphael J. Intrafocal pinning for juxta-articular phalanx
fractures. Tech Hand Up Extrem Surg 2005;9:169-171.
UK, Nassab RS, Oni JA, et al. A prospective study of the treatment of
fractures of the little finger metacarpal shaft with a short hand cast.
J Hand Surg 2004;29B: 214-217.
OP, Suttor PM, Degolla R, et al. Early surgical treatment for
collateral ligament rupture of metacarpophalangeal joints of the
fingers. J Hand Surg 2003;28:309-315.
Pinal F, Garcia-Bernal FJ, Delgado J, et al. Results of osteotomy, open
reduction, and internal fixation for late-presenting malunited
intra-articular fractures of the base of the middle phalanx. J Hand
Surg 2005;30A:1039e1-e14.
E, Eaton RG. Total collateral ligament excision for contractures of the
proximal interphalangeal joint. J Hand Surg 1993;18A:395-402.
MA, Kiefhaber TR, Comisar R, et al. Dorsal fracture dislocations of the
proximal interphalangeal joint: surgical complications and long-term
results. J Hand Surg 1999; 24:914-923.
M, Trumble T, Hanel D, et al. Failure of cast immobilization for thumb
ulnar collateral ligament avulsion fractures. J Hand Surg
1997;22A:1057-1063.
E, Eaton RG. The long-term outcome of volar plate arthroplasty of the
proximal interphalangeal joint. J Hand Surg 2000;25:429-437.
C, Fuchs M, Burchhardt H, et al. Clinical results of absorbable plates
for displaced metacarpal fractures. J Hand Surg 2007;32A:491-496.
RW, Freeland AE, Jabaley ME, et al. Open hand fractures: an analysis of
the recovery of active motion and of complications. J Hand Surg
1993;18A:387-394.
WW, Matloub HS, Yan J-G, et al. Anatomy of the intermetacarpal
ligaments of the carpometacarpal joints of the fingers. J Hand Surg
1997;22:931-934.
T, Erhard N, Kinzl L, et al. Dynamic treatment of displaced proximal
phalangeal fractures. J Hand Surg 1999;24:1254-1262.
SJ, Cheng R, Prokopis P, et al. Treatment of proximal interphalangeal
dorsal fracture-dislocation injuries with dynamic external fixation: a
pins and rubber band system. J Hand Surg 2007;32A:1242-1250.
MW, Elmaraghy AW, Richards RS, et al. Transmetacarpal intramedullary
K-wire fixation of proximal phalangeal fractures. Ann Plast Surg
1998;41:125-130.
M, Nakamura K, Patterson RM, et al. Three-dimensional kinematic
analysis of the second through fifth carpometacarpal joints. J Hand
Surg 2001;26: 1030-1035.
N, Khan W. The S-Quattro in the management of acute intra-articular
phalangeal fractures of the hand. J Hand Surg 2006;31:79-92.
JM. Irreducible thumb interphalangeal joint dislocation due to a
sesamoid and palmar plate: a case report. J Hand Surg 1995;20:490-491.
M, Hansen L. Treatment of “gamekeeper’s thumb” by reconstruction of the
ulnar collateral ligament. J Hand Surg 2003;27B:542-545.
LM, Sheps SB. Incidence and demographics of hand fractures in British
Columbia, Canada: a population-based study. J Hand Surg
2006;31A:1068-1074.
KK, Moneim MS, Howey T, et al. Comparative fatigue strengths and
stabilities of metacarpal internal fixation techniques. J Hand Surg
1993;18A: 1059-1068.
KJ, Bastidas JA, Provenzano DA, et al. Low-profile versus conventional
metacarpal plating systems: a comparison of construct stiffness and
strength. J Hand Surg 1999;24:928-934.
C, Della Santa DR. Influence of fracture pattern on consolidation after
metacarpal plate fixation. Chir Main 2004;23:32-36.
I, Aliquizakis A, Katonis P, et al. Treatment of closed unstable
metacarpal fractures using percutaneous transverse fixation with
Kirschner wires. J Trauma 2003; 55:509-513.
JS. Articular fractures of the proximal interphalangeal joint with
missing elements: repair with partial toe joint osteochondral
autografts. J Hand Surg 1999;24:78-85.
H, Martin J. The two-level ulnar collateral ligament injury of the
metacarpophalangeal joint of the thumb. J Hand Surg 2003;28B:92-93.
SZ, Malerich M, Pearce SM, et al. Ligament replacement for chronic
instability of the ulnar collateral ligament of the metacarpophalangeal
joint of the thumb. J Hand Surg 1993;18A:930-941.
MH, Hall M, Hall RF Jr. Low-velocity gunshot wounds of the proximal
phalanx: treatment by early stable fixation. J Hand Surg
1998;23A:142-149.
TJ. The exploded hand syndrome: logical evaluation and comprehensive
treatment of the severely crushed hand. J Hand Surg 2006;31A:1012-1023.
I, Berger AC, Tham SK. Internal fixation of unstable fracture
dislocations of the proximal interphalangeal joint. J Hand Surg
2005;30:492-498.
Y, Sairyo K, Tonogai I, et al. Irreducible fracture dislocation of a
finger metacarpophalangeal joint: A case report. Hand 2008;3:76-78.
SC, Stern PJ, Fassler PR, et al. Miniscrew fixation for the treatment
of proximal interphalangeal joint dorsal fracture-dislocations. J Hand
Surg 2006;31A: 1349-1354.
IJ, Parry D, Barrington RL. The use of a moulded metacarpal brace
versus neighbour strapping for fractures of the finger metacarpal neck.
J Hand Surg 2001; 26B:261-263.
NG, Chen A, Jupiter JB. Extra-articular osteotomy for malunited
unicondylar fractures of the proximal phalanx. J Hand Surg 2005;30A:
566-572.
Y, Doi K, Sakamoto S, et al. Volar plating for intra-articular fracture
of the base of the proximal phalanx. J Hand Surg 2007;32A:1299-1303.
MH. Soft tissue sleeve approach to open reduction and internal fixation
of proximal phalangeal fractures. Tech Hand Up Extr Surg 2008;12.
MH. Fractures of the proximal phalanx and metacarpals in the hand:
preferred methods of stabilization. J Am Acad Orthop Surg 2008;16.
MH. Specific complications associated with different types of intrinsic
pedicle flaps of the hand. J Reconstr Microsurg 2008;24.
MH. Degloving combined with structural trauma at the digital level:
functional coverage with fascial free flaps. J Reconstr Microsurg
2007;23:59-62.
DH, Erickson SJ, Chamoy L, et al. Ulnar collateral ligament of the
thumb: MR findings in cadavers, volunteers, and patients with
ligamentous injury (gamekeeper’s thumb). AJR Am J Roentgenol
1994;163:1431-1434.
H, Tsujii M, Nakao E. Locking of the metacarpophalangeal joint of the
thumb caused by a fracture fragment of the radial condyle of the
metacarpal head after dorsal dislocation. J Hand Surg 2006;31B:635-636.
EE, Cohen MS. Closed reduction and percutaneous pinning of fractures of
the proximal phalanx. J Hand Surg 2003;26B:45-49.
TC, Hatton M, Davis TRC. A prospective randomized controlled study of
fixation of long oblique and spiral shaft fractures of the proximal
phalanx: closed reduction and percutaneous Kirschner wiring versus open
reduction and lag screw fixation. J Hand Surg 2003;28B:5-9.
SN, Dietz JF, Kalainov DM, et al. A biomechanical study of distal
interphalangeal joint subluxation after mallet fracture injury. J Hand
Surg 2008;33:26-30.
MC, Giddins GEB. Dynamic external fixation for pilon fractures of the
interphalangeal joints. J Hand Surg 2001;26B:122-124.
K, Jurik AG, Peterson LK. Intraarticular fractures at the base of the
fifth metacarpal. A clinical and radiographic study of 64 cases. J Hand
Surg 1992;17B: 144-147.
SH, Thoder JJ, Lieberman G. Operative treatment of metacarpal and
phalangeal shaft fractures. J Am Acad Orthop Surg 2000;8:111-121.
KM, Khiem DD, Shin AY. Volar A1 pulley approach for the fixation of
avulsion fractures of the base of the proximal phalanx. J Hand Surg
2001;26:762-771.
R, Malhotra R. Divergent fracture-dislocation of the second
carpometacarpal joint and the three ulnar carpometacarpal joints. J
Hand Surg 2001;26:123-129.
JE, Husband JB, Tokar N, et al. Outcome of avulsion fractures of the
ulnar base of the proximal phalanx of the thumb treated nonsurgically.
J Hand Surg 1999;24: 275-282.
JYL, Teoh LC. Dorsal fracture dislocations of the proximal
interphalangeal joint treated by open reduction and interfragmentary
screw fixation: indications, approaches, and results. J Hand Surg
2006;31B:138-146.
YL, Beredjiklian PK, Monaghan BA, Bozentka DJ. Radiographic assessment
of small finger metacarpal neck fractures. J Hand Surg 2002;27:443-448.
KH, Chan BK, Low CO. Metacarpal and proximal phalangeal
fractures-fixation with multiple intramedullary Kirschner wires. Hand
Surg 2000;5:125-130.
RE. A comparative mechanical analysis of plate fixation in a proximal
phalanx fracture model. J Hand Surg 1996;21A:1059-1064.
M, Sailer R, Zimmerman R, et al. Closed reduction transarticular
Kirshner wire fixation versus open reduction internal fixation in the
treatment of Bennett fracture dislocation. J Hand Surg 2003;28B:142-147.
S, Peck F, Watson JS, et al. Lessons learned from the management of
complex intra-articular fractures at the base of the middle phalanges
of fingers. J Hand Surg 2003;28B:559-565.
K. External fixation of closed metacarpal and phalangeal fractures of
digits. A prospective study of 100 consecutive patients. J Hand Surg
2006;31B:30-40.
HS, Jensen PL, Sanger JR, et al. Spiral fracture fixation techniques. A
biomechanical study. J Hand Surg 1993;18B:515-519.
T, Morimoto H, Yoshikawa H. Palmar dislocation of the
metacarpophalangeal joint of the finger. J Hand Surg 2004;29B: 90-93.
K, Patterson RM, Viegas SF. The ligament and skeletal anatomy of the
second through fifth carpometacarpal joints and adjacent structures. J
Hand Surg 2001;26: 1016-1029.
DP, Davis TRC, Barton NJ. The treatment of dorsal fracture-dislocation
of the proximal interphalangeal joint by closed reduction and Kirschner
wire fixation: a 16-year follow up. J Hand Surg 2002;27B:537-540.
JL, Indriago I, Gonzales E, et al. Percutaneous fixation of metacarpal
fractures. Oper Tech Plast Reconstr Surg 2002;9:138-142.
ST, Limantzakis G, Kay SP. The role of low-profile titanium miniplates
in emergency and elective hand surgery. J Hand Surg 1999;24B:347-349.
K, Fukuda K, Hamanishi C. An unusual dorsal fracture-dislocation of the
proximal interphalangeal joint. J Hand Surg 2007;32E:193-194.
EA, Dennis JJ, Latta LL, et al. The role of soft tissues in plate
fixation of proximal phalanx fractures. Clin Orthop 2004;418:213-218.
SM, Stern PJ. Complications and range of motion following plate
fixation of metacarpal and phalangeal fractures. J Hand Surg
1998;23A:827-832.
MR, Bassini L. Irreducible palmar Metacarpophalangeal joint dislocation
due to juncture tendinum interposition: a case report and review of the
literature. J Hand Surg 2000;25:166-172.
L, Toh S, Arai K, et al. The Ishiguro extension block technique for the
treatment of mallet finger fracture: indications and clinical results.
J Hand Surg 2003;28B:15-17.
CD. Comparative biomechanical stability of titanium bone fixation
systems in metacarpal fractures. Ann Plast Surg 1995;35:6-14.
CD, Eppley BL, Jackson JR, et al. Mini- and micro-plating of phalangeal
and metacarpal fractures: a biomechanical study. J Hand Surg
1995;20:44-49.
BE, Glickel SZ, Lane LB, et al. Palmar fracture dislocation of the
proximal interphalangeal joint. J Hand Surg 1998;23A:811-820.
RT, Hogan CJ, Cannon DL, et al. Use of dynamic distraction external
fixation for unstable fracture-dislocations of the proximal
interphalangeal joint. J Hand Surg 2008;33:19-25.
J, Fagan R. Arthroscopic treatment of acute complete thumb
metacarpophalangeal ulnar collateral ligament tears. J Hand Surg
1995;20A:1037-1042.
SR, Bose VC, Rex C. Irreducible dislocation of the interphalangeal
joint of the thumb due to sesamoid bone interposition: a case report. J
Hand Surg 1995;20: 487-489.
M, Miranda D, Gonzalez R, et al. Immediate corticocancellous bone
autografting in segmental bone defects of the hand. J Hand Surg
2006;31B:168-177.
I, Goitz RJ, Sotereanos DG. Dynamic traction and minimal internal
fixation for thumb and digital pilon fractures. J Hand Surg
2004;29A:39-43.
N, Kulikov Y, Giddins GEB. Outcome following conservative treatment of
metacarpophalangeal collateral ligament avulsion fractures of the
finger. J Hand Surg 2007; 32B:102-104.
J, Klasen HJ. Open reduction and internal fixation of combined fourth
and fifth carpometacarpal fracture dislocations. J Trauma
1997;42:1052-1055.
DJ, Thomas RH. Collateral ligament avulsion fractures from the heads of
the metacarpals of the fingers. J Hand Surg 2006;31B:537-541.
PT, Trumble TE. Traumatic dislocation of the thumb carpometacarpal
joint: early ligamentous reconstruction versus closed reduction and
pinning. J Hand Surg 1996;21A:802-806.
ED, Goodwin DR. Nonoperative treatment of displaced avulsion fractures
of the ulnar base of the proximal phalanx of the thumb. Scand J Plast
Reconstr Surg Hand Surg 2003;37:225-227.
S, Lerner A, Kaufman T. Immediate autografting of bone in open
fractures with bone loss of the hand: a preliminary report. Case
reports. Scand J Plast Reconstr Surg Hand Surg 1999;33:117-122.
S, Schwartz O. Complications of K-wire fixation of fractures and
dislocations in the hand and wrist. Arch Orthop Trauma Surg
2001;121:527-530.
J, McNaughton G, Riley J. The use of prophylactic flucloxacillin in
treatment of open fractures of the distal phalanx within an accident
and emergency department: a double-blind randomized placebo-controlled
trial. J Hand Surg 2003;28B:388-394.
RJ, Behrman MJ, Rosenwasser MP. Acute dislocation of the
carpometacarpal joint of the thumb: an anatomic and cadaver study. J
Hand Surg 1994;19:93-98.
RJ, Rosenwasser MP, Lunt JG. Metacarpal shaft fractures: the effect of
shortening on the extensor tendon mechanism. J Hand Surg
1998;23:519-523.
M, Nagy L, Buchler U. Rigid internal fixation of basilar fractures of
the proximal phalanges by cancellous bone grafting only. J Hand Surg
2001;26B:455-458.
AA, Agarwal M, Boome R. Dynamic external fixation for pilon fractures
of the proximal interphalangeal joints: a simple fixator for a complex
fracture. J Hand Surg 2003;28B:137-141.
H, Takahashi S, Ando M. Operative treatment of mallet finger due to
intra-articular fracture of the distal phalanx. Arch Orthop Trauma Surg
2000;120:9-13.
V, Beredjiklian PK, Weiland AJ. Intra-articular fractures of the hand:
treatment by open reduction and internal fixation. J Orthop Trauma
2005;19:518-523.
K, Pollock J, Rajaratnam V. Proximal interphalangeal joint fractures of
the hand: treatment with an external dynamic traction device. Ann Plast
Surg 2007; 58:625-629.
EJF, Blokhuis TJ, Maas M, et al. Long-term evaluation of Bennett. A
comparison between open and closed reduction. J Hand Surg
1994;19B:373-377.
C, Morganti A, Casiraghi A, et al. Low-severity metacarpal and
phalangeal fractures treated with miniature plates and screws. Arch
Orthop Trauma Surg 2004; 124:675-680.
RS, David HG. The doorstop procedure. A technique for treating unstable
fracture dislocations of the proximal interphalangeal joint. J Hand
Surg 1993;18B: 714-715.
JW, Wegner DA, Hastings H II. Effect of proximal phalangeal fracture
deformity on extensor tendon function. J Hand Surg 1998;23A:673-681.
Brenk B, Richards RR, Mackay MB, et al. A biomechanical assessment of
ligaments preventing dorsoradial subluxation of the trapeziometacarpal
joint. J Hand Surg 1998; 23:607-611.
Oosterom FJT, Brete GJV, Ozdemir C. Treatment of phalangeal fractures
in severely injured hands. J Hand Surg 2001;26B:108-111.
SF. Extension block pinning for proximal interphalangeal joint fracture
dislocations: preliminary report of a new technique. J Hand Surg
1992;17A:896-901.
E, Ashammakhi N, Happonen H, et al. Bioabsorbable miniplating versus
metallic fixation for metacarpal fractures. Clin Orthop
2003;410:310-319.
E, Ashammakhi N, Raatikainen T, et al. Self-reinforced bioabsorbable
versus metallic fixation systems for metacarpal and phalangeal
fractures: a biomechanical study. J Hand Surg 2002;27:902-909.
AJ, Berner SH, Hotchkiss RN, et al. Repair of acute ulnar collateral
ligament injuries of the thumb metacarpophalangeal joint with an
intraosseous suture anchor. J Hand Surg 1997;22A:585-591.
AD, Ladas CS. Anatomical attachments to the proximal phalangeal base: a
case for stability. Scand J Plast Reconstr Surg Hand Surg 2001;35:85-90.
RMM, Kiefhaber TR, Sommerkamp TG, et al. Treatment of unstable dorsal
proximal interphalangeal fracture/dislocations using a hemi-hamate
autograft. J Hand Surg 2003;28:856-865.
T-C, Ip FK, Yeung SH. Comparison between percutaneous transverse
fixation and intramedullary K-wires in treating closed fractures of the
metacarpal neck of the little finger. J Hand Surg 2006;31B:61-65.
R, Shah MA, Patterson RM, et al. Anatomy and pathomechanics of ring and
small finger carpometacarpal joint injuries. J Hand Surg
2003;28:1035-1043.
FC, Tan SH, Tow BPB, et al. Trapezoid rotational bone graft osteotomy
for metacarpal and phalangeal fracture malunion. J Hand Surg
2007;32B:282-288.
