Fractures of the Tibia
-
For practical purposes, fractures of the tibial plateau are classified as follows:
-
Undisplaced (a vertical fracture of the plateau)
-
Split (a split fracture with displacement, with or without slight comminution)
-
Depressed (centrally depressed fracture)
-
Split and depressed with an intact tibial rim
-
Any of 1 through 4 with metaphyseal or even diaphyseal extension. The elements of these descriptions are contained within Schatzker’s system (Fig. 25-1).
-
-
Examination
is different from that for other knee injuries. It is wise to carry out
a definitive examination only after roentgenographs have been obtained.
Differential diagnosis includes a major ligamentous injury or knee
dislocation (5,6,7).
The examination should include inspection for wounds, evaluation of the
distal circulation (pulses and capillary refill), and neurologic (motor
or sensory) function. Motion and stability should not routinely be
assessed in these injuries; however, this type of injury can be
associated with ligamentous or meniscal damage (1). -
Radiographs.
Oblique films in addition to the routine anteroposterior and lateral
radiographs are often helpful in identifying fracture lines and
articular displacement. Computed tomography demonstrates minor
fractures and accurately depicts the degree of depression of the tibial
plateau; axial cuts with sagittal reconstruction are the routine. -
Magnetic resonance imaging (MRI) can be helpful when there is clinical concern for associated ligamentous injury.
-
Undisplaced fractures.
In some settings, especially when multiple injuries are involved,
fixation with two percutaneous cannulated cancellous lag screws is
advisable to ensure maintenance of reduction. For isolated injuries,
generally nonoperative management is selected. A splint is applied, and
the leg is elevated for the first 24 to 48 hours. Knee aspiration is
carried out if a significant hemarthrosis is present, and knee motion
may be started with continuous passive motion (CPM) if available. As
soon as the patient is comfortable and the range of motion is
increasing, he or she can be followed up as an outpatient. Follow-up
radiographs should be obtained shortly after motion is instituted to
ensure that the fracture remains nondisplaced. Touch-down weight
bearing should be maintained for 8 weeks to prevent displacement from
shear forces. -
Displaced fractures
-
Split fracture.
Open reduction and fixation is generally done if there is a significant
widening (lateral or medial displacement of more than 3–5 mm) of the
plateau (8,9). The
internal fixation must be rigid enough to allow movement of the joint
as soon as there is soft-tissue healing. In this situation, the authors
prefer to use the Association of the Study of Internal Fixation (ASIF)
buttress plate (Fig. 25-2) or a dynamic compression or locking plate when the patient is osteoporotic (4).
Recently, there has been a move toward use of smaller implants for all
tibial plateau fixation. Specialized 3.5-mm T- and L-buttress plates
allow the placement of more screws under the articular surface. If the
patient is young and has dense bone, then multiple percutaneous
cannulated lag screws can be inserted
P.360P.361
under
fluoroscopic and/or arthroscopic control. Percutaneous placement of a
large reduction clamp is often successful in providing reduction of the
fracture. If open reduction and internal fixation are not feasible,
then treatment should be as for comminuted fractures.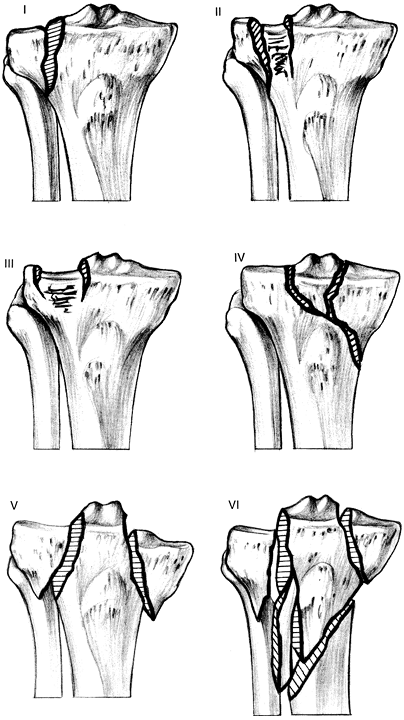 Figure 25-1.
Figure 25-1.
Schatzker’s classification system. I, split; II, split with depression;
III, depression; IV, medial condyle; V, bicondylar; VI, bicondylar with
shaft extension. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:315.)![]() Figure 25-2.
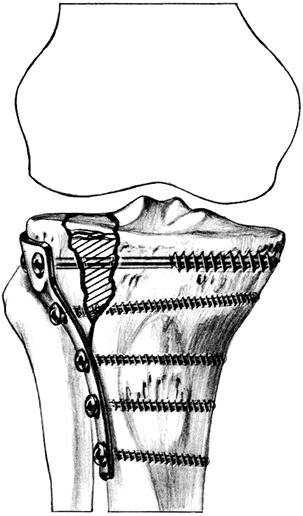
Figure 25-2.
Internal fixation of a split depression fracture of the tibial plateau
using L-buttress plate fixation with bone grafting of the elevated
segment. (From Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993: 318.) -
Central depression of the plateau.
If depression is greater than 3 to 5 mm, especially with valgus stress
instability of the knee greater than 10 degrees in full extension, then
most authors currently recommend elevation with bone grafting and
fixation (2,3,9,10).
More recently, articular reductions have been done with arthroscopic
visualization with percutaneous technique for elevation of the segment.
Autogenous bone graft remains the treatment of choice, but allograft
and cancellous substitutes such as corallin hydroxyapatite and
calcium-phosphate cements have been successfully used (9).
Generally, percutaneous lag screws are adequate for support of the
elevated joint surface and bone graft or graft substitute material. -
Split-depressed fractures
with a displacement/depression of more than 3 to 4 mm are treated with
reduction, fixation, and early motion in most young patients.
Generally, this reduction is done with an open technique with an
anterior or anterolateral approach, elevation, and bone grafting using
buttress or locking buttress plates for older patients (Fig. 25-2)
and lag screws or 3.5-mm small fragment T- or L-plates or one-third
tubular plates (as washers) in younger patients. These fractures may be
managed with arthroscopic reduction in skilled hands. Secure fixation
is critical so
P.362
that
early motion with or without CPM can be initiated. Patients are
generally limited to touch-down weight bearing for 12 weeks to prevent
late fracture settling. If the patient’s limb is stable to varus and
valgus stress in an examination under anesthesia shortly after injury,
then traction treatment with a tibial pin and early motion is an option
(10,11). The patient is placed in a cast-brace (as described in Chap. 7, III.H) or a hinged knee brace after 3 to 4 weeks (1).
This treatment is not currently recommended on a routine basis. If the
instability exceeds 10 degrees, then reduction and fixation as
described earlier is indicated (11). -
Fractures with metaphyseal/diaphyseal extension
are treated similarly to split-depressed fractures if the joint
extension is significant. Generally, buttress plate fixation and bone
grafting are required. When the injury is bicondylar, stripping the
soft tissues off both condyles from an anterior approach should be
avoided; this results in a high incidence of nonunion and deep
infection. Instead, the most unstable condyle (usually lateral) is
selected for the buttress fixation via an anterolateral approach and
the other condyle is stabilized by percutaneous screw fixation,
fixation with a posterior medial incision and small buttress plate, or
neutralization with an external fixator for 4 to 6 weeks while motion
is limited. With all tibial plateau fractures treated with operative
stabilization, it is important to examine the knee for ligamentous
stability after completing the fixation in the operating room to rule
out ligamentous injury (see II.B) (1). The functional results of treatment
are often better than the routine radiographs seem to predict. Early
motion of the knee joint and delayed full weight bearing are the keys
to maximum restoration of joint function (2,3,4).-
Apply a cast-brace (as described in Chap. 7, III.H)
off the self-hinged knee braces, which are lightweight and limit varus
and valgus stress and are more widely used. The same ambulation
protocol, touch-down weight bearing, is followed. -
In special situations, the patient is placed in a long-leg cast
until the fracture is healed. Then the patient is placed in a
rehabilitation program to regain full extension and flexion of the knee
to beyond 90 degrees. The patient is kept on protected weight bearing
for at least 3 to 4 months. This treatment is generally limited to
patients with a severe neurologic condition or significant osteopenia.
-
-
-
-
Complications
-
Significant loss of range of motion may occur, particularly if early movement is not instituted.
-
Early degenerative joint changes
with pain can occur regardless of the degree of joint reconstruction.
In some instances, the pain may be severe enough to require
arthroplasty or arthrodesis (8). -
The infection rate
following operative treatment is reduced in experienced hands. Most
infections occur because of excessive soft-tissue stripping. -
Nerve and vascular injuries that occur at the time of injury or subsequent to treatment are not uncommon (12).
Nerve injuries are usually traction injuries, and recovery is
unpredictable. Compartmental syndrome may be present and should be
treated as described in Chap. 2, III.
-
-
Classification. Proximal tibial fractures are classified similar to diaphyseal fractures (see III.C).
-
Examination.
Initial examination should be comprehensive including inspection,
palpation, and lower extremity neurovascular assessment. The integrity
and condition of the soft tissues should be carefully inspected. The
alignment of the lower extremity should also be noted. The compartments
of the leg should be palpated and passive flexion and extension of the
toes performed to assess for pain and possible compartment syndrome.
Distal pulses may be palpable despite ischemia from increased
compartment pressure. Definitive diagnosis may require measurement of
intracompartmental pressures (see Chap. 2, III). The diagnosis of a compartment
P.363
syndrome is a surgical emergency and requires prompt release of
pressure to preserve muscle and nerve viability. A careful examination
of the extremity pulses is imperative to rule out potential vascular
injury. -
Radiographs.
Although a tibial diaphyseal fracture may be obvious from clinical
examination, anteroposterior and lateral radiographs of the tibia
(including the knee and ankle joints) are needed to plan management.
Radiographs should be carefully reviewed to ensure fracture lines do
not reveal intraarticular extension. Computed tomograms or plain
tomograms can be helpful to identify intraarticular extension when
plain x-rays are difficult to interpret. -
Treatment.
Extraarticular proximal tibial fractures are often the result of high
energy trauma with displacement and comminution. Most authors agree
that operative management of such fractures is warranted to optimize
patient outcomes. However, it remains unclear which surgical option
(plate, nail, external fixator, or combination) is preferable. The
rates of nonunion between implants did not appear to differ between
treatment options (Table 25-1). Infection rates were significantly lower with intramedullary nails than with plates or external fixators (p <0.05) (13). A trend towards increased rates of malunion with intramedullary nails was identified (p
= 0.06). Pooled results across studies may be limited by heterogeneity
between studies. Results should be interpreted with caution. -
Complications.
Extraarticular fractures of the tibia are prone to infection, malunion
(i.e., valgus and procurvatum deformities), nonunion, compartment
syndrome, and implant failure (Table 25-1) (13).-
Infection: range 8% to 14% (deep infection rates 3%–5%)
-
Malunion: range 2.4% to 20%
-
Nonunion: range 2% to 8%
-
Compartment syndrome: range 2% to 6%
-
Implant failure: 8%
-
-
Epidemiology.
Tibial fractures are the most common long bone fracture. They occur
commonly in the third decade of life at a rate of 26 diaphyseal
fractures per 100,000 population annually. -
Mechanism of injury.
Five causes of injury include falls, sports related, direct blunt
trauma, motor vehicle accidents, and penetrating injuries (e.g.,
gunshots). -
Classification.
The most comprehensive classification for tibial fractures is the AO
Association for the Study of Internal Fixation/Orthopaedic Trauma
Association system that divides injury patterns into three broad
categories: unifocal, wedge, and complex fractures.-
Unifocal fractures are further described as spiral, oblique, and transverse fractures (A).
-
Wedge fractures are further described as intact spiral, intact bending, and comminuted wedge fractures (B).
-
Complex fractures (i.e., multiple fragments) can be described as spiral wedge, segmental, and comminuted fractures (C).
-
-
Examination.
Initial examination should be comprehensive including inspection,
palpation, and lower extremity neurovascular assessment. The integrity
and condition of the soft tissues should be carefully inspected. The
alignment of the lower extremity should also be noted. The compartments
of the leg should be palpated and passive flexion and extension of the
toes performed to assess for pain and possible compartment syndrome.
The diagnosis of a compartment syndrome is a surgical emergency and
requires prompt release of pressure to preserve muscle and nerve
viability (see Chap. 2, III). -
Radiographs.
Although a tibial diaphyseal fracture may be obvious from clinical
examination, anteroposterior and lateral radiographs of the tibia
(including the knee and ankle joints) are needed to plan management.
Radiographs can provide information about fracture morphology, quality
of the bone (i.e., osteopenia, osteoporosis), and gas in the tissues
suggesting an open wound. -
Treatment.
The selection of nonoperative or operative management must involve the
consideration of many factors, including associated skeletal and
ligamentous
P.364P.365
injuries,
the degree of soft-tissue injury, injuries to other organ systems, the
general condition of the patient, the skill and experience of the
treating physician, and the resources of the facility. Options for
treatment include: casting/functional bracing (nonoperative), external
fixation, plate fixation, and intramedullary nailing.-
Nonoperative management
is commonly reserved for closed tibial diaphyseal fractures with less
than 1.5 cm of shortening, axially stable transverse fractures, spiral
oblique of comminuted fractures with less than 12 mm of initial
shortening, angulations less than degrees initially, and less than 50%
displacement (15). However, acceptable degrees
of fracture shortening and translation are highly variable among
surgeons (<5 mm to >15 mm). Surgeons’ definitions of acceptable
angular malunions (rotational, varus/valgus, and
procurvatum/recurvatum) range from less than 5 degrees to 20 degrees (16). Sarmiento (17,18)
developed a below-the-knee cast [patellar tendon bearing (PTB)] and
prefabricated functional brace that allows knee motion while
maintaining stability and length in the affected leg. This PTB cast is
generally applied after 2 to 3 weeks in the long-leg bent knee cast
that is applied following a closed reduction. Prefabricated braces are
the most widely used. One of these two treatment methods should be
chosen, and the particular technique should be strictly adhered to if
the same excellent results reported in the literature are to be
expected. These cast techniques are described in detail in Chap. 4.
It must be re-emphasized that a below-the-knee total contact cast may
not be applied immediately after the fracture; one must wait until the
swelling has diminished. The authors suggest using a modified Robert
Jones compression long-leg splint during the period of acute swelling.
When the patient is ready for casting and following an appropriate
spinal or general anesthetic, nearly all tibial fractures can be
reduced by placing the leg over the end of the table. Adequate
reduction and alignment are maintained in this position while the cast
is applied. If shortening is minimal, then analgesia may suffice. The
average healing time with closed treatment is approximately 18 weeks
(range from 14.5–21.0 weeks). One of Sarmiento’s principles is that, in
general, the amount of final shortening is demonstrated on the initial
radiograph, and the patient should be so informed. Good functional
outcomes can be expected in 90% of cases (19,20,21). Closed treatment is recommended for children’s fractures except when the physis or joint is involved (22). -
Operative management
is reserved for those fractures deemed unacceptable for nonoperative
treatment. Most surgeons prefer intramedullary nails in the treatment
of closed low energy fractures (95.5%), high energy fractures (96%),
and those closed fractures with associated compartment syndrome (80.4%)
(23). The majority of surgeons prefer
intramedullary nails in the treatment of open tibial shaft fractures;
however, there is a decline in the use of intramedullary nails as the
severity of the soft tissue injury increases from Types I to IIIb (Type
I, 95.5%; Type II, 88.1%; Type IIIa, 68.4%; Type IIIb, 48.4%) (23).-
Closed fractures.
There have been three published meta-analyses evaluating treatment
alternatives for closed tibial shaft fractures: two pooling data from
primarily observational studies and one pooling data from on-use
randomized trials (21,24,25).
Littenburg and colleagues, in a comprehensive review of the available
literature, identified 2005 patients treated with a cast or brace, 474
patients treated with a plate and screws, and 407 patients treated with
intramedullary nails (21). Pooled infection
rates were lower with casts (0%) and intramedullary nails (0%–1%) when
compared to plates (0%–15%). While plate fixation achieved the fastest
time to fracture union (0%–15%). when compared to either casts (median
= 13.7 weeks) or intramedullary nails (median = 20 weeks) there were no
differences in the ultimate rates of nonunion between groups. Rates of
deep infection were lower with casts and intramedullary nails than with
plates (ranges: 0%–2%, 0%–1%, 0%–15%, respectively).In a review of prospective studies (eight observational
and five randomized trials) evaluating treatment alternatives for
tibial shaft fractures,
P.366
Coles
and Gross found plate fixation to result in the lowest nonunion rates
(2.6%) and highest infection rates (9%) compared to other treatment
alternatives (24).
Despite the apparent benefits of plate fixation in decreasing the time
to fracture healing, only 2.1% to 7.4% of surgeon respondents to a
survey preferred them in the treatment of closed tibial shaft fractures
(low energy, high energy, and those with associated compartment
syndrome). This likely reflects an assessment that the high risk of
infection with plates outweighs their relative benefit in decreasing
time to fracture union. It remains unclear whether surgeons from less
industrialized countries, who prefer plate fixation in closed tibial
shaft fractures, have similar access to intramedullary nails as those
surgeons in developed nations.A substantial proportion of respondents chose external
fixation for high energy tibial shaft fractures and those associated
with compartment syndrome. The role of external fixation in closed
tibial shaft fractures has been evaluated in an observational study (26).
Turen and colleagues, in a review of 68 closed fractures, identified a
longer fracture healing time in fractures with compartment syndrome
than those without (30.2 weeks versus 17.2 weeks, respectively)(26). Moreover, fracture healing times for closed fractures with compartment syndrome were similar to open fractures.There remains considerable variability in their
preference to ream the intramedullary canal or not. The evidence
favoring reamed or non-reamed nail insertion is suggestive but not
definitive. Bhandari and colleagues conducted a systematic review and
found nine randomized trials (n = 646 patients) comparing reamed and nonreamed intramedullary nail insertion in tibial and femoral fractures (25).
Reamed nailing resulted in a 56% reduction in the relative risk of
nonunion compared to nonreamed nailing (95% confidence interval:
7%–79%). -
Open fractures.
An international survey suggests a progressive decline in the use of
intramedullary nails as the severity of the soft tissue injury
increases from Type I to IIIb. This is related to an increased use of
external fixation with increasing soft tissue injury (3%–51%) (27). Surgeons rarely prefer plates in the treatment of open fractures (0.8%–1.1%). One study (n
= 56) suggests external fixators that significantly decrease the risk
of re-operation relative to plates (relative risk 0.13, 95% confidence
interval 0.03–0.54, p <0.01) (15). A meta-analysis found that nonreamed nails, in comparison to external fixators (five studies, n = 396 patients), reduced the risk of reoperation [relative risk (RR) 0.51, 95% confidence interval 0.31–0.69] (28).
Nonreamed nails also offered advantages in decreasing the relative risk
of malunion (RR 0.42, 95% confidence interval 0.25–0.71) and
superficial infection (RR 0.24, 95% confidence interval, 0.08–0.73).
While these studies shared methodologic limitations of lack of
concealment, blinding, and loss to follow-up, the narrow confidence
intervals make the results more definitive than those of the studies
comparing reamed versus unreamed nailing. In the open tibial fracture
trials, reamed nails, when compared to nonreamed nails, showed a trend
toward decreasing the risk of reoperation (two studies, n = 132; RR 0.75, 95% confidence interval 0.43–1.32) (6).
Because the confidence interval is very wide, the relative effect of
reamed and unreamed nails in open tibial fractures remains unresolved.
-
-
-
Complications. Most patients experience some residual disability after a tibial fracture (21,24).
-
Compartment syndrome has been discussed previously (see Chap. 2, III).
-
Joint stiffness
can be largely prevented by aggressive treatment to achieve early
union. Flexion and extension exercises to the toes must not be
neglected because these joints frequently stiffen and produce
considerable postcasting dysfunction. -
Complex regional pain syndrome (reflex sympathetic dystrophy) can occur in 30% of patients with tibial diaphyseal fractures (29). Vigorous physical therapy and sympathetic may be required (see Chap. 2).
-
Delayed union and nonunion (30)
-
The following factors are related to delayed union or nonunion:
-
Severe initial displacement of the fracture fragments (probably indicating significant soft-tissue injury)
-
Significant comminution
-
Associated soft-tissue injuries or open fractures
-
Infection
-
Open management with inadequate stabilityThese complications can be minimized by adequate
immobilization, early weight bearing (which is often delayed for 2
months if a dynamic compression plate is used), and early bone grafting
where delayed union appears certain.
-
-
Adjunctive therapies. Low-intensity pulsed ultrasound (30 mW/cm2
given at 20 minutes per day has shown potential benefits in improving
time to healing. A meta-analysis identified 138 potentially eligible
studies, of which 6 randomized trials met inclusion criteria (31).
Three trials, representing 158 fractures, were of sufficient
homogeneity for pooling. The pooled results showed that time to
fracture healing was significantly shorter in the groups receiving
low-intensity ultrasound therapy than in the control groups. The
weighted average effect size was 6.41 (95% confidence interval
1.01–11.81), which converts to a mean difference in healing time of 64
days between the treatment and control groups. Figure 25-3.
Figure 25-3.
Displaced closed fractures of the tibia shaft, when shortened more than
1 cm or considered to be unstable, are best treated with interlocking
nails. A and B: Preoperative radiographs of a shortened, unstable segmental fracture of the tibia shaft. C and D:
The interlocking nail in place. The screws placed through the holes in
the nail proximal and distal to the fracture provide length and
rotational stability for the fracture. Nearly all fractures of the
femoral shaft in skeletally mature individuals are treated with similar
interlocking nails, allowing mobilization of the patient and early
range of motion of adjacent joints.
-
-
Infection is
a complication of open fractures or the opening of a closed fracture.
The risk of infection is minimized by efficient surgical technique, by
the proper use of antibiotics, and by a delayed primary closure for
open fractures. For the most severe soft-tissue injuries, aggressive
debridement and coverage with free or rotational muscle flaps minimizes
this complication. Pin tract infection is common with the use of
external fixators. -
Revision surgery.
An observational study of 192 patients with tibial shaft fractures
identified three simple predictors of the need for reoperation within 1
year (32). Three variables predicted
reoperation: the presence of an open fracture wound (RR 4.32, 95%
confidence interval 1.76–11.26), lack of cortical continuity between
the fracture ends following fixation (RR 8.33, 95% confidence interval
3.03–25.0), and the presence of a transverse fracture (RR 20.0, 95%
confidence interval 4.34–142.86).
P.367P.368 -
and lateral radiographs and physical examination. Computed tomography
scans are helpful for assessment of displacement and for surgical
planning.
and internal fixation or percutaneous reduction with lag screw fixation
aided by arthroscopy for fractures displaced more than 2 mm (depression
or gapping). Knees that remain stable to varus/valgus stress in full
extension may be treated nonoperatively.
visualization via open reduction or arthroscopy, reduction and fixation
with lag screws and/or low profile plates and bone graft or bone graft
substitute, early range-of-motion therapy and limited weight bearing
for 8 to 12 weeks.
and lateral radiographs of the leg and clinical examination. In 10% to
20% cases there is an open wound communicating with the fracture.
for fractures that are isolated and not shortened more than 1 cm on
initial radiographs, long leg splint for 2 to 3 weeks followed by
fracture brace until fracture is united, operative stabilization for
length unstable and/or open fractures. Interlocking nail, inserted with
reaming is the procedure of choice.
Fractures close to the joint or shortened on initial radiographs
greater than 1 cm or failure to control angulation with nonoperative
technique or open fracture
Interlocking nailing, statically locked. Insert with reaming: more
reaming for larger diameter nails with closed fractures, less reaming
for open fractures.
AE, Bannister GC. The management of depressed tibial plateau fractures.
A comparison of non-operative with operative treatment using allograft
and autograft. J Orthop Trauma 1994;4:61–64.
M, Audige L, Ellis T, et al. Evidence-Based Orthopaedic Trauma Working
Group. Operative treatment of extraarticular proximal tibial fractures.
J Orthop Trauma 2003;17:591–595.
RB, Anderson JT. Prevention of infection in the treatment of one
thousand and twenty-five open fractures of long bones: retrospective
and prospective analyses. J Bone Joint Surg [Am] 1976;58:453–458.
A, Sharpe FE, Ebramzadeh E, et al. Factors influencing outcome of
closed tibial fractures treated with functional bracing. Clin Orthop 1995;315:8–25.
M, Guyatt GH, Swiontkowski MF, et al. A lack of consensus in the
assessment of fracture healing among orthopaedic surgeons. J Orthop Trauma 2002;16:562–566.
B, Weinstein LP, McCarren M, et al. Closed fractures of the tibial
shaft. A meta-analysis of three methods of treatment. J Bone Joint Surg (Am) 1998; 80:174–183.
M, Guyatt GH, Swiontkowski MF, et al. Surgeons’ preferences in the
operative treatment of tibial shaft fractures: an international survey.
J Bone Joint Surg (Am) 2001;83A:1746–1752.
C, Gross M. Closed tibial shaft fractures: management and treatment
complications. A review of the prospective literature. Can J. Surg 2000;43:256–262.
M, Guyatt GH, Tong D, et al. Reamed versus non-reamed intramedullary
nailing of lower extremity long bone fractures: a systematic overview
and meta-analysis. J Orthop Trauma 2000;14:2–9.
J, Bhandari M, Kulkarni A, et al. The effect of low intensity, pulsed
ultrasound on time to fracture healing: a meta-analysis. CMAJ 2002;166:437–441.
M, Guyatt G, Sprague S, et al. Predictors of re-operation following
operative management of fractures of the tibial shaft. J Orthop Trauma 2003;17:353–361.