Examination of the Patient With Visual Symptoms
Authors: Lewis, Steven L.
Title: Field Guide to the Neurologic Examination, 1st Edition
Copyright ©2004 Lippincott Williams & Wilkins
> Table of Contents > Section 3
– Neurologic Examination in Common Clinical Scenarios > Chapter 49 –
Examination of the Patient With Visual Symptoms
– Neurologic Examination in Common Clinical Scenarios > Chapter 49 –
Examination of the Patient With Visual Symptoms
Chapter 49
Examination of the Patient With Visual Symptoms
GOAL
The goal of the history and examination of the patient
with visual symptoms is to determine whether the symptoms are due to
vision loss or diplopia and to determine the most likely cause of that
dysfunction.
with visual symptoms is to determine whether the symptoms are due to
vision loss or diplopia and to determine the most likely cause of that
dysfunction.
PATHOPHYSIOLOGY OF VISUAL DYSFUNCTION
Visual dysfunction, whether transient or persistent, can occur as a result of one of two main mechanisms: vision loss or diplopia.
-
Vision loss can occur due to dysfunction
anywhere along the sensory visual pathway that begins in the eyes and
ends in the occipital cortex (see Chapter 13, Visual Field Examination, and Fig. 13-1). -
Diplopia is the illusion of seeing two
objects when there is really only one and occurs when there is
dysfunction of normal conjugate eye movements so that the eyes no
longer move appropriately in synchrony. The presence of diplopia
implies dysfunction of the motor pathways that move the eyes, anywhere
from the brainstem to the extraocular muscles. Because the illusion of
diplopia requires two eyes, patients who are blind in one eye cannot
have diplopia.
TAKING THE HISTORY OF A PATIENT WITH VISUAL DYSFUNCTION
Listed below are important features of the history that
can be helpful in the evaluation of patients who present with symptoms
due to vision loss or diplopia.
can be helpful in the evaluation of patients who present with symptoms
due to vision loss or diplopia.
Vision Loss
Monocular Vision Loss
-
Monocular vision loss
may be transient or persistent. When patients present with transient
visual symptoms that they attribute to one eye, for you to be more
certain that your patient’s symptom was truly monocular and not a
hemianopic disturbance, the patient would have had to have covered the
bad eye during the event to confirm that the vision was intact in the
good eye. Some patients do initiate this test on their own during an
episode of vision loss, but you may need to specifically inquire if the
patient did this. -
Patients with monocular visual problems
do not usually present with significant functional deficits from their
vision loss, as long as the remaining eye has intact visual fields. In
other words, unlike patients with hemianopsias, patients with purely
monocular vision loss are less likely to bump into objects because of
their visual dysfunction. -
Amaurosis fugax (meaning fleeting blindness)
is an important kind of transient monocular vision loss that may be
seen in patients with retinal ischemia, such as can be associated with
carotid stenosis or temporal arteritis. Patients describe a brief
(seconds or minutes) loss of vision in
P.167
one eye as “like a shade coming down.” As the symptoms resolve, the patient may describe the shade coming back up. -
Patients with optic neuritis usually
present with monocular vision loss that progresses over a period of
days and lasts for weeks, and it is often associated with pain on eye
movement.
Visual Field Loss
-
Patients with visual field loss
often do not recognize the concept of a visual field or a visual field
deficit. They may misinterpret their homonymous visual field deficits
as monocular (i.e., a patient may interpret a left homonymous
hemianopsia as a visual problem involving the left eye alone). -
Patients with hemianopic visual field
cuts sometimes present with symptoms of the consequences of their
deficits, rather than with a primary visual complaint. They may tell
you they consistently bump into objects on one side, or they may have
been involved in a motor vehicle collision because of their visual
deficit. -
Patients with hemianopsias may present
with a vague visual complaint that they have difficulty describing.
Those with left homonymous hemianopsias may complain of difficulty
reading, not recognizing that their difficulty is due to consistently
missing the first (left) parts of sentences. Patients with bitemporal
field loss may complain of difficulty with their peripheral vision. -
A common form of transient hemianopic
field deficit is the visual disturbance of a migraine aura. Migrainous
visual disturbances typically present as a scintillating (shining)
zigzag or herringbone-like pattern, sometimes in the form of a C,
occurring in the left or right visual field and gradually growing over
approximately a 15-minute period before resolving. This migrainous
visual disturbance may or may not be followed by a headache. -
Patients with complete bilateral vision
loss due to bilateral occipital lobe infarcts can actually be unaware
that they are blind and deny the existence of their blindness. This is
known as Anton’s syndrome.
Diplopia
-
Patients with diplopia usually are aware
of seeing two objects, which (depending on the cause) can be side by
side, vertical, or diagonal. Horizontal diplopia would be particularly
likely from sixth nerve lesions or disorders affecting the lateral or
medial rectus muscles alone. Vertical or diagonal diplopia would be
expected with lesions causing the eyes to diverge vertically or
diagonally but is otherwise not specific in terms of localization. -
Diplopia should completely resolve when
the patient covers either eye. Some patients instinctively perform this
test themselves, but you may need to specifically ask if they did,
especially if the diplopia was transient and is no longer present
during your examination. -
Some patients who have diplopia complain
only of a vague blurriness of vision, unaware that their difficulty is
actually due to two partially superimposed images. In this case, the
historical clue that the visual symptom is actually diplopia rests on
the finding that the symptoms resolve with covering either eye. -
Diplopia due to myasthenia gravis usually
waxes and wanes like any other weakness associated with this
neuromuscular junction disease. The diplopia may be worse at the end of
the day and may be associated with eyelid drooping.
P.168
EXAMINING THE PATIENT WITH VISUAL DYSFUNCTION
The following are important features of the examination of patients who present with symptoms due to vision loss or diplopia:
Vision Loss
Monocular Vision Loss
-
In patients with monocular vision loss
due to optic nerve dysfunction (such as optic neuritis), the visual
field in the affected eye may be a central scotoma. This is easily
detected by asking the patient to cover the good eye and look directly
at your face with the bad eye. The patient with a central scotoma
describes inability to see the central part of your face but is able to
see the periphery. -
On pupillary examination, patients with
monocular vision loss due to optic nerve dysfunction also usually have
an afferent pupillary defect (see Chapter 10, Examination of the Pupils). -
Acute monocular vision loss due to optic nerve demyelination or inflammation may be associated with optic disc swelling (see Fig. 11-2)
if the process involves the optic nerve head itself (papillitis);
however, the optic disc will appear normal if the disease process is
behind the eye (retrobulbar optic neuritis). Long-standing monocular
vision loss from severe optic nerve dysfunction is often associated
with significant pallor of the optic disc due to optic nerve atrophy
(see Fig. 11-4). -
Patients with transient monocular vision
loss (amaurosis fugax) from carotid stenosis may or may not have other
evidence for carotid disease on examination, such as a bruit. They may
also rarely have refractile (bright) embolic material at the branch
points of one or several retinal arterioles visible on funduscopy,
called Hollenhorst plaques (Fig. 49-1).
Hemianopsia
-
In patients with symptoms suggestive of a visual field cut, confrontational visual field testing (see Chapter 13,
Visual Field Examination) will usually easily detect a deficit (i.e., a
left or right homonymous hemianopsia, quadrantanopsia, or bitemporal
hemianopsia). -
Pupillary responses should be normal in
patients with hemianopic visual field deficits (as well as in patients
with complete vision loss due to bilateral occipital pathology) because
the lesion is posterior to the optic chiasm.
Diplopia
-
While examining a patient with diplopia,
ask the patient to describe the characteristics of the two images to
you. This may require the patient to look at an object in the room and
tell you whether the two images are side by side (horizontal diplopia),
up and down (vertical diplopia), or diagonal. -
Confirm that the diplopia resolves when
the patient covers either eye; this simply further confirms that the
patient’s symptoms fit with diplopia. -
Look at the resting position of the eyes
as the patient looks straight ahead. The affected eye of patients with
third nerve palsies, for example, characteristically deviates laterally
and downward (see Fig. 10-1).P.169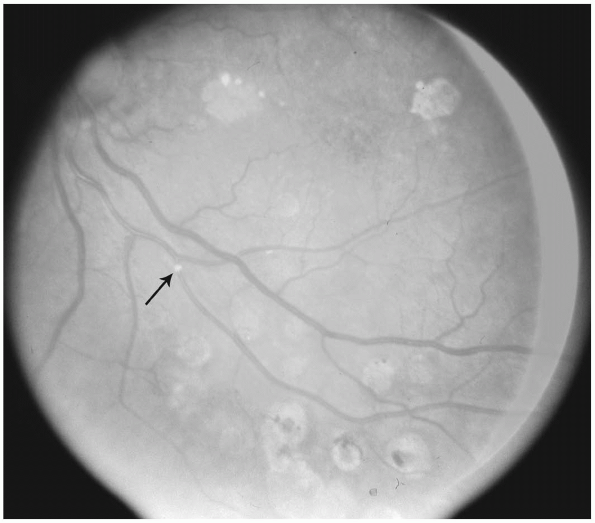 Figure 49-1 Retinal artery embolus (arrow) in a patient with carotid atherosclerosis.
Figure 49-1 Retinal artery embolus (arrow) in a patient with carotid atherosclerosis. -
Look closely at the extraocular movements. Particularly, look for evidence of a third or sixth cranial nerve palsy (see Chapter 14, Examination of Eye Movements), and look for pupillary findings suggestive of a third nerve palsy (see Chapter 10, Examination of the Pupils). Also look for evidence of an internuclear ophthalmoplegia (see Fig. 14-2).
-
Patients with fourth nerve palsies are
recognized more by the characteristic head tilt they adopt (as a
compensation for the diplopia that would occur if they didn’t hold
their head in that position) than the subtle eye movement changes that
would be expected from weakness of the superior oblique muscle.
Patients with fourth nerve palsies usually tilt their head away from
the side of the fourth nerve lesion (i.e., a left fourth nerve palsy
would likely cause a head tilt to the right). -
The finding of proptosis in a patient
with diplopia suggests that the lesion is within the orbit or involves
the eye muscle itself. -
If myasthenia gravis is suspected as a cause of diplopia, look for fatigability of the eye muscles as follows:
-
Ask the patient to follow your finger with his or her eyes upward as you raise your finger up to test upward gaze.
-
Continue holding your finger above the
patient’s head as you observe the patient perform a prolonged upgaze.
Watch for a minute or two (your arm may get tired before the patient
does) while you observe the patient’s eyes. -
The finding of fatigability of upgaze or
worsening ptosis with this procedure can be a helpful clue to the
diagnosis of myasthenia gravis even if eye muscle weakness or ptosis is
not seen on routine testing.
-
