Disorders of the Rotator Cuff
area of intensive research with advances continually being made. Our
understanding of the causes of rotator cuff disease in the athlete has
grown enormously, as have surgical techniques. This chapter is intended
to provide an introduction to rotator cuff disorders. A general
overview of the anatomy and biomechanics of the rotator cuff will be
presented, followed by an overview of some of the major disorders of
the rotator cuff, including impingement, rotator cuff tears, and
calcific tendinopathy.
long been known, advancements are still being made to our knowledge of
the details of its structure. Most recently, the size and shape of the
insertions of the rotator cuff into the humeral head have been
described, which has implications for the treatment of rotator cuff
repairs.
insertions of four muscles: the supraspinatus, infraspinatus,
subscapularis, and teres minor. These muscles originate on the scapula
and insert into the tuberosities of the humeral head. The supraspinatus
originates on the supraspinatus fossa and passes under the acromial
arch to insert on the superior aspect of the greater tuberosity. It is
innervated by the suprascapular nerve, which courses under the
transverse scapular ligament in the suprascapular notch. The
supraspinatus allows abduction of the humerus. The infraspinatus
originates on the infraspinatus fossa and inserts on the posterior
aspect of the greater tuberosity. It is innervated by the continuation
of the suprascapular nerve after the nerve courses around the
spinoglenoid notch. The teres minor runs just inferior to the
infraspinatus, inserts on the posterior inferior aspect of the
tuberosity, and is innervated by the axillary nerve. Both the
infraspinatus and the teres minor are external rotators of the
shoulder. Finally, the subscapularis originates on the anterior surface
of the scapula and inserts on the lesser tuberosity. It is the most
powerful of the rotator cuff muscles, and it allows internal rotation.
The subscapularis is composed of two parts: (a) the upper portion,
which is multipennate and the greater force generator; and (b) the
lower portion, which has a parallel arrangement of fibers. The upper
portion of the muscle is innervated by the upper subscapular nerve, and
the lower portion of the muscle is innervated by the lower subscapular
nerve. The tendons of these four muscles all blend with each other and
with the underlying capsule before inserting into the humerus.
and the subscapularis is known as the rotator interval. This interval
is pierced by the tendon of the long head of the biceps. The rotator
interval is composed of a complex interweaving of fibers of the leading
edge of the supraspinatus, the superior edge of the subscapularis, and
the coracohumeral and superior glenohumeral ligaments. The
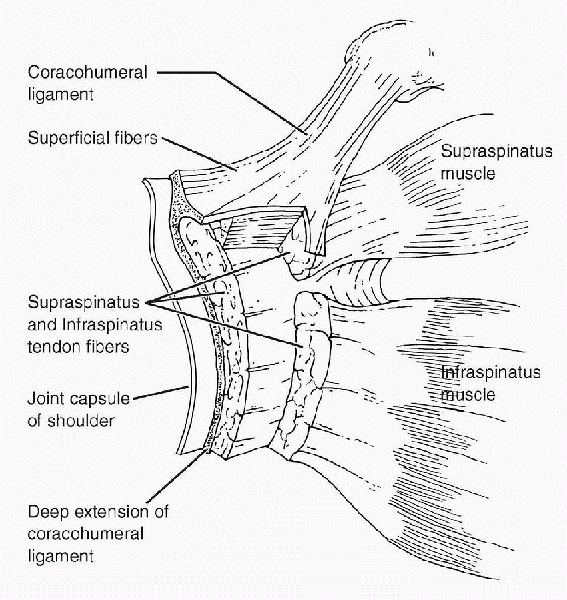
coracohumeral ligament forms layer 1 of the supraspinatus tendon as
shown in Figure 19-1.
This layer continues anteriorly to form the roof of the interval and
the superior aspect of the biceps tendon sheath. The floor of the
sheath is composed of fibers of the superior glenohumeral ligament and
subscapularis tendon.
|
TABLE 19-1 LAYERS OF THE SUPRASPINATUS AND INFRASPINATUS TENDONS
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
Figure 19-1
Schematic diagram of a transverse section through the supraspinatus and infraspinatus tendons and capsule of the shoulder. (After Clark JM, Harryman DT II. Tendons, ligaments, and capsule of the rotator cuff: gross and microscopic anatomy. J Bone Joint Surg Am 1992;74:713-725. © 1992 The Journal of Bone and Joint Surgery.) |
transition into the tendinous cuff, and this inserts into the bone of
the humeral head. The humeral head is made up of the articular surface,
the greater and lesser tuberosities, and the bicipital groove that
separates the tuberosities. The shape and size of the footprint of
insertion of the rotator cuff tendons have received interest recently
because arthroscopic techniques have allowed the diagnosis and
treatment of partial undersurface cuff tears. Knowledge of the
insertional footprint allows the surgeon to estimate the size of a
partial tear.
-
The subscapularis has the largest of the
footprints. It is, on average, comma-shaped, 40 mm long, and 19 mm
wide. The insertion initially blends with the capsule then tapers to a
well-defined tendon that is discrete from the capsule as it crosses the
joint and becomes the subscapularis muscle. -
The supraspinatus footprint is rectangular, 23 mm long, and 16 mm wide.
-
The infraspinatus has the second largest
footprint. It wraps and interdigitates with supraspinatus superiorly
and is 28 mm long and 18 mm wide. -
The teres minor has the smallest insertion. The footprint measures 28 mm × 10 mm.
-
If the right proximal humerus is viewed
from the perspective of the glenoid, the subscapularis extends from 7
to 11 o’clock. The supraspinatus goes from 11:30 to 1 o’clock. The
infraspinatus then continues from 12:30 to 3 o’clock and is followed by
the teres minor, which goes from 3 o’clock to 5 o’clock.
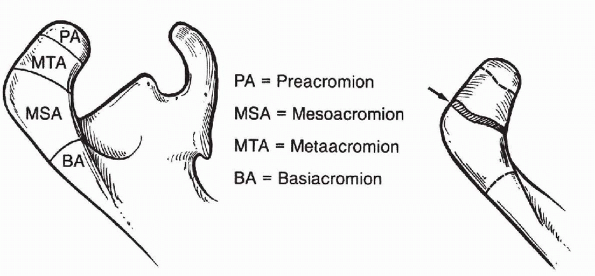
which is a continuation of the spine of the scapula. The arch is
completed by the coracoacromial ligament, which extends from the
coracoid to the anterior inferior edge of the acromion. The
supraspinatus tendon passes under the acromial arch on its way to its
insertion on the greater tuberosity. The acromial arch and the humeral
head can be thought of as forming a container. The contents of the
container are the supraspinatus tendon, the biceps tendon, and the
subacromial bursa. Reduction in the size of the container or increases
in the volume of its contents can result in there being insufficient
space for the supraspinatus tendon—a condition called “impingement.”
Absence of a fully functioning subscapularis has been shown to result
in increasing internal rotation weakness as the limit of motion is
approached. The subscapularis also acts as a restraint to anterior
subluxation of the humerus and a restraint to passive external
rotation. The infraspinatus and teres minor have been shown to provide
80% of external rotation force, and the supraspinatus provides 50% of
abduction torque output for shoulder elevation.
been thought to produce motion of the glenohumeral joint. However,
recent biomechanical studies have thrown light on the stabilizing
function of the rotator cuff, and many now believe that this may be its
primary role. The bony architecture of the shoulder provides little
stability to the glenohumeral joint. Most of its stability is provided
by the soft tissues that surround it, including the capsuloligamentous
structures. The rotator cuff provides dynamic stability to counteract
the potentially destabilizing effect of the other muscles of the
shoulder girdle, such as the effect of the deltoid muscle in abduction
of the shoulder. In the absence of the stabilizing effect of the cuff,
the deltoid will cause the humerus to migrate proximally. This destroys
the fulcrum of glenohumeral rotation, making abduction more difficult.
The rotator cuff muscles are located close to the joint. This is ideal
for performing their stabilizing function. The infraspinatus and
subscapularis co-contract to provide compression across the
glenohumeral joint. The supraspinatus works as a humeral head
depressor. Contraction of this muscle changes the resultant vector
across the joint to a more inferiorly directed force and thus
counteracts the force of the deltoid, which is directed superiorly.
rotator cuff disease, the intrinsic and extrinsic theories. The
intrinsic theory holds that tendon degeneration is the result of
changes in the mechanical properties of the tendons. This may be
because of several factors, including aging and poor vascularity. The
abnormal cuff is no longer able to perform its function to stabilize
the glenohumeral joint, which can result in a high-riding humeral head
and subacromial impingement. This then adds further trauma to the
tendons and leads to further degeneration.
the tendons are the primary cause of the disorder. Factors such as
repetitive overuse, tensile overload, and impingement begin the process
of tendon degeneration, which results in destabilization of the joint
and then further impingement. Today, we understand tendon degeneration
to be multifactorial and dependent on both intrinsic and extrinsic
causes.
from the classic subacromial process to a broad category of extrinsic
sources of injury to the rotator cuff. Impingement can now be broken
down into two main categories, external and internal.
-
External impingement refers to pathologic contact between the rotator cuff and structures outside the shoulder joint.
-
Subacromial impingement is the most
common form of external impingement. In this disorder, the undersurface
of the acromion and structures in the subacromial space are the
offending agents. -
Anterior impingement is another form of
external impingement. It occurs when the coracoid process comes into
contact with the subscapularis with internal rotation maneuvers.
-
-
Internal impingement involves abnormal contact between the rotator cuff and structures within the shoulder joint itself.
-
Posterior impingement is a form of this
and is primarily a disorder of overhead athletes. In these individuals,
abnormal contact is made between the posterior supraspinatus and
infraspinatus and the posterior superior glenoid when the arm is in the
fully cocked position.
-
impingement is by far the most common form of impingement. As the
supraspinatus tendon travels from the supraspinous fossa to the greater
tuberosity of the humerus, it travels under the acromial arch. This
arch limits the upward excursion of the tendon. Under normal
circumstances, the humeral head remains located on the glenoid, and
there is sufficient room for the tendon to travel without impingement.
In pathologic states, however, the size of the “container” —and thus
the space for the tendon—is diminished (Fig. 19-2).
his classic article, he implicated the anterior acromion, the
coracoacromial ligament, and the acromioclavicular joint. He classified
impingement into three stages: tendon inflammation, fibrosis, and cuff
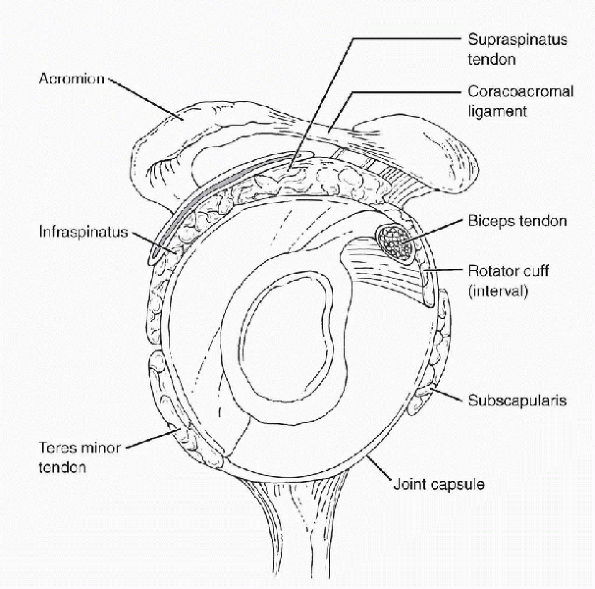
tear. Bigliani showed in cadaveric studies that there is a relationship
between the morphology of the acromion and the presence of cuff tears.
He defined three acromial shapes: type 1 (flat), type 2 (curved), and
type 3 (with an anterior hook; Fig. 19-3),
which occurred in 17%, 43%, and 40% of the specimens, respectively. Of
the specimens with rotator cuff tears, 75% of these had type 3 acromial
morphology.
shape and coracoacromial ligament hypertrophy lead to impingement. In
the younger athletic population, secondary impingement as a result of
instability is much more common. Subtle glenohumeral laxity can allow
superior migration of the humeral head with overhead activities.
Another factor that should not be overlooked in the young patient
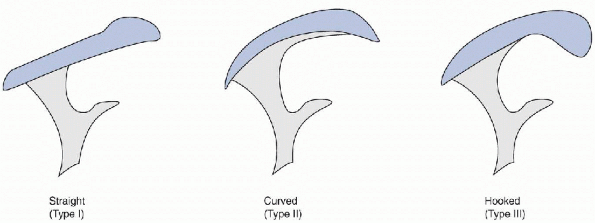
presenting with impingement is the possibility of an os acromiale. The
acromion is formed by the union of three ossification centers that are
usually fused by age 22—the preacromion, the mesacromion, and the
metacromion (Fig. 19-4). Persistent nonunion of
these centers of ossification is called an “os acromiale.” The
incidence of os acromiale in the general
population
is estimated to be between 2.7% and 6%. As many as 60% of these cases
are bilateral. Norris and Bigliani (1993) noted an association between
persistent os acromiale and impingement. The most common site of
persistent nonunion is the growth plate between the mesacromion and the
metacromion.
 |
|
Figure 19-2
Bigliani classification of acromion shape as determined on the outlet view. (After Curtis AS, Wilson P. Shoulder pain in the workplace. Orthop Clin North Am 1996;27:763-781.) |
in an inability of the cuff to generate the normal compressive forces
across the glenohumeral joint. This causes an imbalance to occur
between the stabilizing forces of the rotator cuff and the
destabilizing forces of the powerful deltoid muscle, which can result
in subacromial impingement with elevation of the arm. The loss of the
scapular stabilizing muscles, as is seen with winging of the scapula,
can cause the normal scapular rotation to be lost. The scapula will
then fail to rotate out of the way, when the arm is brought overhead,
which may also result in impingement.
 |
|
Figure 19-3 Anatomy of impingement. (After Curtis AS, Wilson P. Shoulder pain in the workplace. Orthop Clin North Am 1996;27:763-781.)
|
 |
|
Figure 19-4
Ossification centers of the acromion. The most common site of failure of ossification is between the mesoacromion and the meta-acromion. (From Butters KP. Fractures of the scapula. In: Bucholz RW, Heckman JD. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2001:1079-2263.) |
-
Patients with subacromial impingement
will complain of shoulder pain, usually over the anterior-lateral
deltoid and exacerbated by overhead activity. -
The pain can radiate down the arm but usually not below the elbow.
-
Night pain is an almost constant feature of subacromial impingement, and patients will avoid sleeping on the affected shoulder.
-
The Neer impingement sign and the Hawkins
test are both provocative tests intended to reproduce the patient’s
impingement by reducing the subacromial space.-
With a positive Neer impingement sign,
the patient’s pain is elicited by forced abduction of the humerus while
stabilizing the scapula (see Fig. 15-4 in Chapter 15). -
In the Hawkins test, the patient is made
to grasp the contralateral shoulder and the arm is abducted by
elevating the elbow (see Fig. 15-5 in Chapter 15). This forces the greater tuberosity into the acromion, causing pain.
P.248 -
-
In the Neer impingement test, the patient’s shoulder pain goes away with a subacromial injection of lidocaine.
-
A recent study has shown the value of
this test. Results of subacromial decompression in patients with a
positive impingement test were compared with those that were negative.
Patents with a positive impingement test were 28% more likely to be
improved by subacromial decompression 12 months after surgery than
those with a negative result.
-
-
Radiographs are all that is required for evaluation of subacromial impingement.
-
Standard anteroposterior x-ray is useful for assessing the bony architecture of the glenohumeral joint.
-
Calcific tendonitis can be seen in this view as can arthritis of the acromioclavicular joint.
-
A lateral downslope in the acromion can also be seen in this view.
-
The supraspinatus outlet view is taken
with the x-ray beam directed 10 degrees caudally. This shows the
acromial morphology best. -
Magnetic resonance imaging (MRI) can be
performed when a rotator cuff tear is suspected but is usually
unnecessary for isolated impingement. MRI allows an enlarged
coracoacromial ligament to be evaluated. Rotator cuff tears and
tendonitis can also be seen.
-
Treatment of impingement begins with therapy, rest, ice, and nonsteroidal anti-inflammatory drugs.
-
Therapy consists mainly of rotator cuff
strengthening exercises to better enable the rotator cuff to counteract
the proximally directed force of the deltoid and depress the humeral
head. -
Steroid injections into the subacromial space can also be used.
with subacromial decompression is indicated. Radical acromionectomy was
performed early in the treatment of impingement. This often resulted in
disability for the patient because the deltoid was rendered incompetent
by the procedure.
should be preserved. He proposed anterior acromioplasty, which requires
the removal of a wedge of bone from the acromion, with most of the
resected bone coming from the undersurface of the acromion. A high
degree of success was reported with this procedure in older patients
with percentage success in the 1980s and 1990s. In younger pitchers,
one study showed that a good functional result was achieved in only 22%
of patients, likely pointing to the different etiology of impingement
in this subset of patients.
-
Arthroscopic acromioplasty was first described by Ellman (1987). The arthroscopic approach provides many advantages.
-
The deltoid attachment is not disturbed, so the patient can undergo more aggressive rehabilitation early on.
-
The acromioclavicular (AC) joint can be inspected and co-planed if needed.
-
At the same time, the glenohumeral joint can be inspected and any other pathology can be treated if warranted.
-
Rotator cuff tears, biceps tendon pathology, and glenohumeral arthritis can all be diagnosed.
-
Results of arthroscopic decompressions are equivalent to the open procedures with few complications.
-
-
Our preferred method of acromioplasty is based on the technique described by Snyder.
-
The supraspinatus outlet view is used to plan the procedure.
-
The thickness and shape of the acromion are determined.
-
The arthroscope is introduced through a standard posterior portal.
-
The glenohumeral joint is arthroscoped first and any intra-articular pathology treated.
-
The undersurface of the rotator cuff is inspected.
-
The arthroscope is then introduced into the subacromial space.
-
A lateral portal is established in line with the posterior edge of the clavicle.
-
A shaver and arthroscopic Bovie are used to remove bursal tissue.
-
The undersurface of the acromion is then
cleared of soft tissue, and the coracoacromial ligament is peeled off
of the anterior inferior edge of the acromion but not completely
detached. -
A 4.0-mm arthroscopic burr is introduced
through a lateral portal, and a line is made in the undersurface of the
acromion just behind the acromioclavicular joint, running from medial
to lateral. -
This line marks the posterior edge of the resection and acts as a guide to further work.
-
Removal of bone begins laterally and
progresses medially with the 30-degree arthroscope oriented toward the
undersurface of the acromion. -
A flat surface is created, starting at the guide line and working forward (Fig. 19-5).
-
Care is taken not to detach the deltoid fascia.
-
The scope is then switched to the lateral portal, and the burr is brought in posteriorly.
-
Using the posterior acromion as a template, the transition zone between the posterior acromion and the anterior is smoothed.
-
Care is taken to remove the acromial facet all the way to the AC joint.
-
If the AC joint is hypertrophic, the undersurface of the clavicle can be co-planed to prevent impingement at this location.
-
pitchers. It involves the coming into contact of the undersurface of
the posterior supraspinatus and infraspinatus with the posterior
superior glenoid labrum when the arm is in the fully cocked throwing
position. The cause of this disorder is a source of controversy with
two competing theories currently under investigation.
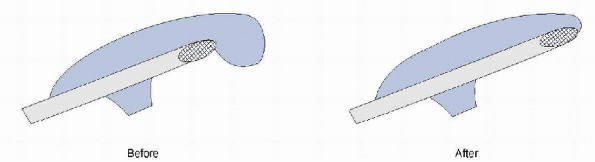 |
|
Figure 19-5
Converting a type 3 to a type 1 (flat) acromion. (After Curtis AS, Wilson P. Shoulder pain in the workplace. Orthop Clin North Am 1996;27:763-781.) |
stretched out with overuse, allowing the impingement to occur with the
arm fully externally rotated and abducted to 90 degrees.
posterior capsule that becomes tight through scar tissue formation as a
result of the eccentric overload of the posterior cuff as it
decelerates during follow-through. This tightness forces the humeral
head to rise up when the athlete assumes the cocked throwing position.
-
Patients complain of pain, usually in the
posterior shoulder. There is a loss of internal rotation and excessive
external rotation. -
A careful physical examination is important to document the patient’s arc of motion.
-
The examination is performed with the patient supine on the examining table and both arms abducted to 90 degrees.
-
The elbows are bent to 90 degrees, and
the examiner rotates the humerus of each arm to the position of maximal
internal and external rotations and compares the motion of the two arms. -
Normally, the patient will be able to touch his hand to the table in both internal and external rotations.
-
Inability to reach the table in internal
rotation and excessive external rotation are the hallmarks of a
positive physical examination.
-
-
The first line of treatment for internal impingement is physical therapy.
-
The athlete must work aggressively to regain the lost internal rotation.
-
This should be done under the supervision of a therapist experienced in the problems of overhead athletes.
-
-
For the few athletes who fail conservative treatment, arthroscopy is necessary.
-
Examination of the undersurface of the
rotator cuff may exhibit wear and tear from continued contact with the
labrum and the superior labrum may be frayed or detached. -
Repairs of the cuff and any superior labrum anterior-posterior (SLAP) lesions should be performed as indicated.
-
The glenohumeral motion problems can be
addressed with posterior capsule releases and anterior capsulorraphy as
needed to balance the shoulder.
well-defined clinical entity. Our understanding of these tears is quite
recent and owes much to the development of arthroscopic surgical
techniques. Ellman classified these tears using Neer’s classification
of rotator cuff disease as a starting point. Neer stage III rotator
cuff disease represents the torn rotator cuff, so all partial rotator
cuff tears are classified as stage III. Ellman further describes the
partial-thickness tear by location: type A is an articular surface
tear, type B is a bursal surface tear, and type C is an interstitial
tear. The tears are also classified by grade, with grade 1 including
tears less than 3 mm deep, grade 2 including tears between 3 and 6 mm
deep, and grade 3 including tears deeper than 6 mm.
side of the cuff. This is believed to be due to the relative
hypovascularity of the cuff on the articular side. Histologic studies
have shown that the collagen structure on the articular surface of the
tendon is less organized and the bundles are smaller, thus resulting in
lower mechanical strength. PTRCTs can result from severe cuff
tendinosis in which the cuff degenerates over time and then tears when
subjected to biomechanical forces. Articular surface tears in overhead
athletes can be due to internal impingement. Bursal surface tears are
often related to direct attrition of the cuff by subacromial
impingement.
-
Clinical findings with PTRCTs cover a
spectrum from the findings of simple impingement to those associated
with significant rotator cuff tears. -
In overhead athletes, subtle anterior instability of the shoulder may exist.
-
MRI is the preferred imaging modality but
it has been unreliable for PTRCTs because it can be difficult to
differentiate subtle tearing and tendinosis. -
The addition of intra-articular gadolinium can improve the results of MRI significantly.
-
Surgical options should be entertained
when nonsurgical management has failed. Surgical approaches include
debridement of the frayed cuff or completion of the tear and repair of
the cuff through either arthroscopic or open methods. -
Tendon that is partially torn on the
articular surface can be repaired though an arthroscopic transtendonous
approach. These tears are known as partial articular supraspinatus
tendon avulsion (PASTA) lesions. There are a few generally agreed-on
principles to guide the surgeon: -
Bursal surface tears should be treated
with subacromial decompression, whereas articular surface tears may be
treated with decompression if the clinical situation warrants it.-
Tears that are more than 50% of the thickness of the tendon should be repaired.
-
If the tendon is torn more than 75%, the tear should be completed and repaired.
-
-
Arthroscopic techniques have a distinct
advantage in the treatment of these lesions in that a much better
evaluation of articular surface tears can be accomplished by direct
visualization of the rotator cuff from under the surface.-
The extent of the rotator cuff tearing
can be estimated on the basis of knowledge of the footprint of
insertion of the rotator cuff. -
When the cuff is viewed arthroscopically,
the normal edge of insertion of the cuff (just off the articular
surface) can be clearly seen. -
Knowing that the supraspinatus insertion
is 12 to 16 mm wide, the width of the exposed footprint can be measured
using a probe, and an estimate of the percentage of the cuff involved
can be made.
-
-
Our approach to partial thickness rotator
cuff tears is to evaluate the patients under anesthesia for stability.
The glenohumeral joint is arthroscoped and the following performed:-
Frayed cuff is debrided back to healthy tissue.
-
The tear can then be graded for size.
-
In grade 1 and 2 tears, the shoulder is examined for associated pathologies, especially in overhead athletes.
-
-
Grade 3A tears are treated with a PASTA repair.
-
A marking suture is placed through the
lesion in articular-sided tears so the other side of the rotator cuff
can be examined. This is done by locating the lesion with a spinal
needle from the lateral acromion. -
A portal is then made, and an anchor is placed right through the lesion into the footprint.
-
Sutures are then passed retrograde through the cuff 1 cm anterior and posterior to the midline and slightly medially.
-
The sutures are tied from the bursal side of the cuff.
-
Tears more than 75% of the tendon or with
depths of 9 to 12 mm are completed into a V-shaped tear and repaired
from the bursal side using arthroscopic techniques.
-
-
Cordasco et al.
compared 105 patients at a mean of 4.5 years after surgery. Patients
had either no tear or grade 1 and 2 tears. They found patients with and
without tears did equally well, with the exception of grade 2B tears,
which had a failure rate of 38%. They suggested that grade 2B tears
might be better served by primary repair. -
Weber reported on 65 patients with grade
3 tears. Thirty-three tears were repaired by a miniopen approach, and
32 tears were repaired by debridement and decompression. The University
of California-Los Angeles shoulder score was 32 for the repaired cuffs
and 25 for the decompressed cuffs, with 6 failures. This study
supported the concept of repairing cuff tears greater than 50% of the
tendon.
can be classified by the age of the tear as acute or chronic. They may
be classified as partial or full thickness. When a rotator cuff tear
becomes full thickness, it often assumes a recognizable pattern that is
determined by the amount of detachment of the tendon and propagation
along the adjacent intervals. In many cases, the apex of the tear does
not represent the actual point of maximal retraction but instead
represents the point of maximal interval propagation. The most common
patterns are as follows:
-
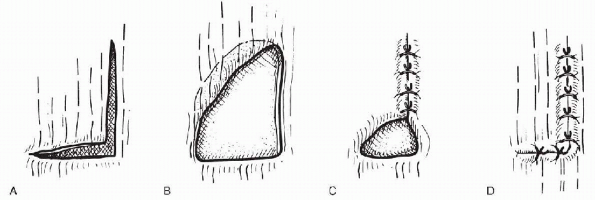
The crescent-shaped tear is pure detachment of the tendons of the supraspinatus and infraspinatus without interval propagation.
-
The L-shaped tear is lateral detachment
of the supraspinatus—and sometimes the infraspinatus as well—with
propagation along the biceps interval so that the apex of the tear
points at the base of the biceps (Fig. 19-6). -
The reverse L-shaped tear is detachment
of the tendon laterally but this time with propagation posteriorly,
between either the supraspinatus and infraspinatus or infraspinatus and
teres minor. The apex of this tear points to the base of the scapula
spine. -
With chronicity, many of these large
tears, or L-shaped tears, assume a V-shaped pattern, making recognition
of the original tear pattern difficult.
-
Rotator cuff tears can occur in healthy
tissue as the result of a traumatic event or as the end point in a
process of tendon degeneration. -
The diagnosis is usually made clinically and then supported by diagnostic studies.
-
Factors such as the age of the tear can complicate the diagnosis.
-
A tear that has slowly progressed in size
over a period of years may not present with the disabling weakness that
an acute tear of the same size would show. -
Patients with small supraspinatus tendon
tears will present with complaints similar to those of subacromial
impingement, but as the size of the rotator cuff tear increases,
weakness usually becomes more profound. -
Strength of the supraspinatus is tested
with the arm in 90 degrees of abduction. The patient is asked to resist
a downward force by the examiner. -
External rotation strength may be
affected in larger tears if the infraspinatus and teres minor are
involved. Strength is tested by having the patient hold his or her arms
at the side with the elbows bent to 90 degrees and the hands straight
out in front. The patient is then asked to rotate externally against
the resistance of the examiner. -
Subscapularis testing is done with the
liftoff test, in which the patient is asked to place his or her hand
behind the back and then lift it off of the back. -
This can be difficult for many patients,
even without a subscapularis tear. A simpler test called the belly
press test has become more popular and has been shown to isolate the
subscapularis equally well. The patient is asked to press his or her
hand against the abdomen with the wrist locked in 0 degrees of flexion.
Patients with a weak subscapularis will cheat and flex the wrist,
allowing the elbow to drop to the side. This allows the patient to
recruit accessory muscles to the task. -
Occasionally, patients will present with
pain and stiffness, as well as weakness. These patients may have
developed a frozen shoulder after an acute rotator cuff tear. This
should be carefully noted because the arthrofibrosis should be
addressed before any surgical treatment of the rotator cuff can be
successful.
 |
|
Figure 19-6 A: L-shaped rotator cuff tear. B: Elasticity of the tendon causes deformation of the L-shaped tear into a U-shaped tear. C: Closure of the vertical limb of the tear by side-to-side sutures. D:
Closure of the horizontal limb of the tear by tendon to bone sutures. (From Burkhart S. Arthroscopic management of rotator cuff tears. In McGinty J, ed. Operative Arthroscopy, 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 2003:512.) |
-
MRI has become the standard imaging modality for the diagnosis of rotator cuff tears.
-
The sensitivity and specificity of the test are reported to be above 90%.
-
MRI allows the surgeon to estimate the shape and size of the tear.
-
The entire shoulder can be evaluated, including the AC joint and the biceps tendon, which are commonly sources of pain.
-
-
Occasionally, patients cannot undergo MRI
testing because of metallic implants that could be dislodged by the
magnetic field or due to claustrophobia. Ultrasound has been shown to
be an excellent alternative to MRI for the diagnosis of rotator cuff
tears, although it is somewhat operator-dependent.
management of rotator cuff tears involves several factors: the age and
health of the patient, the size and acuteness of the tear, and the
extent of pain and disability. The clinician must attempt to estimate
the risk of progression of the tear and what the effect of progression
will be.
-
Young and active patients with any size tear are candidates for operative management.
-
Any patient with an acute tear should be considered for surgical repair.
-
Older patients and patients with chronic
massive tears may benefit from a course of nonoperative treatment and
have less to lose by delaying surgical intervention.
are available to the surgeon: the open approach, the miniopen approach,
and the arthroscopic approach.
-
The open approach is the traditional method for repairing rotator cuffs, with an excellent track record.
-
It allows good visualization of the rotator cuff and mechanically strong fixation of the tendon to bone through bone tunnels.
-
The main drawbacks of open surgery are
the detachment of the deltoid and post operative pain. Partial
detachment of the deltoid is inherent to open rotator cuff surgery.
Failure of the deltoid repair to heal is a serious complication that
can result in disability for the patient.
-
-
The miniopen technique uses arthroscopy to evaluate the rotator cuff tear and perform the acromioplasty if indicated.
-
Once this is completed, the repair is
performed through a deltoid-splitting approach that usually involves a
simple extension of the lateral portal. -
This method provides good visualization and spares the deltoid.
-
The surgeon has the option to use bone tunnels, anchors, or a combination of both for fixation.
-
-
The arthroscopic technique has the lowest postoperative pain and preserves the deltoid.
-
It is not faster than the other methods and has a long learning curve associated with it.
-
It relies on anchors for fixation.
-
The technique is relatively new and still evolving. It is gaining increased acceptance in the orthopaedic community.
-
one. We begin by creating a posterior portal and by introducing the
arthroscope into the glenohumeral joint. An anterior portal is
established to allow probing of structures and debridement if
necessary. The undersurface of the rotator cuff is examined for tears,
and some debridement of tears can be performed from within the shoulder
joint. The tear is characterized from the undersurface as to its size
and if it is partial or full thickness. The scope is than taken into
the subacromial space and a lateral portal is established. A
subacromial decompression is performed if warranted and an extensive
bursectomy to expose the bursal rotator cuff surface. The rotator cuff
tear is then classified by tear propagation pattern. This enables the
surgeon to develop a strategy for rotator cuff repair. The goal is a
tension-free repair. If there is a tear propagation interval as exists
in L- and reverse L-shaped tears, the interval can be closed with
side-to-side sutures. If this is done correctly, the tear will be
reduced back to the footprint of insertion on the tuberosity or close
to this. The final steps of the repair involve the use of anchors to
repair the torn lateral edge of the cuff back to bone (Fig. 19-6C,D).
tears develop, the ability of the rotator cuff to stabilize the
glenohumeral joint is lost. Over time, the humeral head, under the
force of the deltoid muscle, may begin to migrate proximally until it
comes to rest on the under surface of the coracoacromial arch.
Degenerative arthritis develops in the shoulder as abnormal pressures
are exerted on the cartilage by the incongruent joint. This is a
painful, disabling condition.
-
No treatment of shoulder arthropathy is ideal.
-
Relief of pain is the primary goal.
-
Debridement of the remaining cuff tissue can provide temporary relief.
-
Care must be taken not to take down the
coracoacromial ligament because this may be all that is supporting the
humeral head as it migrates into the acromion. -
Arthroplasty has been used to treat this
condition but without the stabilizing effect of the rotator cuff the
glenoid component tends to wear out quickly and so total shoulder
arthroplasty has been discouraged in the past. New total shoulder
replacement options now exist that show some promise in treating this
disorder.
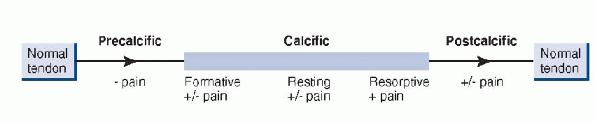
chronically painful condition that is caused by inflammation around
calcium deposits located in the rotator cuff tendons.
believed to be a cell-mediated process. Sarkar and Uthoff described the
natural history as being composed of three stages (Table 19-2 and Fig. 19-7).
|
TABLE 19-2 NATURAL HISTORY OF CALCIFIC TENDONITIS
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
Figure 19-7
Progressive stages of calcific tendonitis. (After Uhthoff HK, Loch JW. Calcific tendinopathy of the rotator cuff: pathogenesis, diagnosis and management. J Am Acad Orthop Surg 1997;5:183-191. ©1997 American Academy of Orthopaedic Surgeons.) |
-
Treatment is nonoperative in the majority of cases.
-
Nonsteroidal anti-inflammatory
medications, subacromial injections, therapy, and ultrasound have a
role in the reduction of symptoms. -
Extracorporeal shock-wave therapy has demonstrated a 70% success rate.
-
Most of the operative treatment of calcific tendonitis is done by arthroscopy.
-
The articular surface of the cuff is examined first.
-
A strawberry-colored lesion often indicates the location of the deposit.
-
The lesion can be tagged with a suture so that it can be accessed from the bursal surface of the rotator cuff.
-
The arthroscope is then introduced into the subacromial space in which a bursectomy is performed.
-
Needling of the deposit with an 18-gauge spinal needle decompresses the lesion.
-
L, Norris TR, Fischer J, et al. The relationship between the unfused
acromial epiphysis and subacromial impingement lesions. Orthop Trans
1983;7:138.
LU, Morrison DS, April EW. The morphology of the acromion and its
relationship to rotator cuff tears. Orthop Trans 1986;10:228.
SS, Morgan CD, KiblerWB. Shoulder injuries in overhead athletes: the
“dead arm” revisited. Clin Sports Med 2000;19:125-158.
JM, Harryman DT II. Tendons, ligaments and capsule of the rotator cuff:
gross and microscopic anatomy, J Bone Joint Surg Am 1992;74:713-725.
FA, Backer M, Craig EV, et al. The partial-thickness rotator cuff tear:
is acromioplasty without repair sufficient? Am J Sports Med
2002;30:257-260.
R, Stanwood WG, Bigliani LU. Arthroscopic acromioplasty: history
rationale and technique. Instr Course Lect 2004;54:13-20.
PB, Clark P, Sutherland K. An analysis of the diagnostic accuracy of
the Hawkins and Neer subacromial impingement signs. J Shoulder Elbow
Surg 2000;9:299-301.
CS II. Anterior acromioplasty for the chronic impingement syndrome in
the shoulder: a preliminary report. J Bone Joint Surg Am 1972;54:41-50.
JE, Jobe FW, Kerlan RK, et al. Shoulder impingement syndrome in
patients treated by anterior acromioplasty. Clin Orthop
1985;198:134-140.
SC. Arthroscopic debridement and acromioplasty versus miniopen repair
in the treatment of significant partial thickness rotator cuff tears.
Arthroscopy 1999;15:126-131.
