Dislocation Ligament Injuries
configuration of the bone components of the joints, provide for stable
yet mobile joints that allow the digits to perform precise movements.
These stabilizing ligaments, however, are subject to stresses that
sometimes exceed their tolerance. When this happens, they fail. The end
result is loss of stability and function due to mechanical factors and
pain. Timely recognition and appropriate treatment of these injuries is
mandatory in the management of hand injuries. Certain patterns of
injury have been identified, and the most common and clinically
significant forms of ligament injuries based on their respective joints
will be discussed. By definition, the discussion of ligament injuries
in this chapter includes joint instability, subluxation, and
dislocation. Dislocations may occur without destabilizing injury or chronic instability
to the respective ligaments involved. However, it is mandatory that the
examiner clearly distinguishes those dislocations and subluxations that
will inevitably result in instability, and those that are intrinsically
stable after reduction.
ligament injuries rather than fracture dislocations. However, some
ligament injuries may be associated with an avulsion-type fracture, but
the main focus is on the ligament injury and not the fracture. Chapter 9,
which focuses on fractures and fracture dislocations, discussed these
injuries, and the reader may recognize that some arbitrary divisions
have been made in these two chapters for the sake of convenience.
-
Dislocations of the distal joints of the fingers and thumb are relatively uncommon.
-
The distal phalanx of these joints has a
shorter lever arm, and additional stability is present due to the
adjacent insertions of the flexor and extensor tendons.
-
-
When dislocations do occur they are most
likely to be dorsal or lateral and may be open due to the comparatively
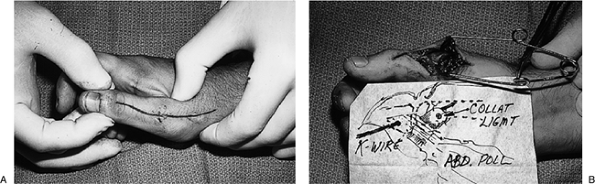
diminished skin coverage over this joint (Figure 10-1A). -
Reduction is achieved by longitudinal traction and manipulation of the base of the phalanx into its anatomical bed.
-
As in all reductions, joint stability is evaluated by gentle passive and active motion.
-
Postreduction radiographs are taken to verify the reduction.
-
The joint is splinted in a few degrees of flexion, and motion may be started in 7 to 10 days (Figure 10-1B).
-
These dislocations are usually reducible,
and reported causes for failed reduction are interposed soft tissue,
such as the palmar plate or the flexor tendon. -
Surgery is indicated for those dislocations that cannot be reduced.
likened to two coffee cups in their respective saucers that have been
placed side-by-side, with both cups and saucers firmly attached
together. This analogy serves to illustrate the fact that the
bicondylar end of the proximal phalanx (the “coffee cups”) articulates
with a saucer-like component at the base of the middle phalanx, and
thus has a certain element of stability or resistance against radial or
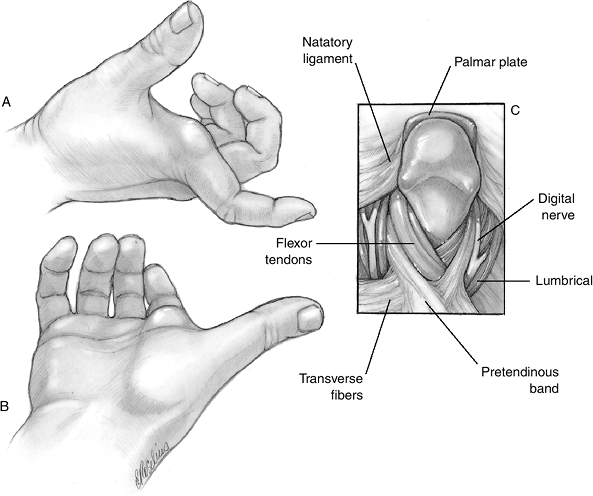
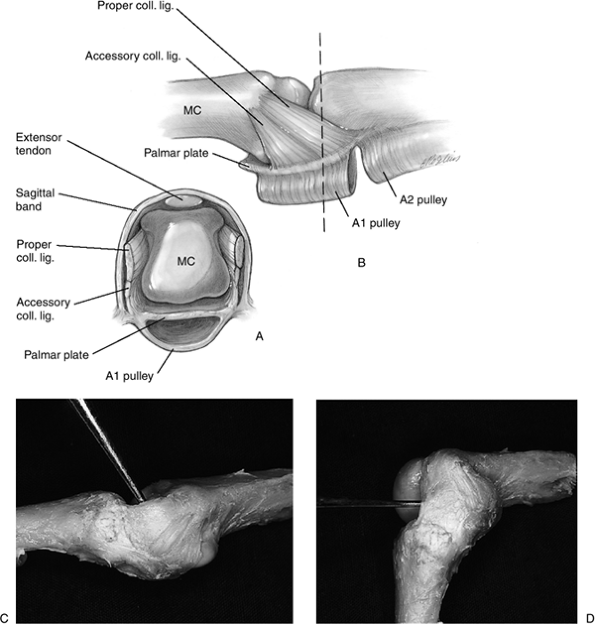
ulnar deviation. Figure 10-2 depicts the
anatomic arrangement of the PIP joint. Add to this fact that the radial
and ulnar collateral ligaments are substantial cord-like structures
that are firmly attached to the neck of the proximal phalanx and the
base of the middle phalanx. It is not surprising to recognize that the
majority of dislocations of the PIP joint occur in the dorsal (most
common) or palmar plane. Additional stability is added to the PIP joint
by the palmar plate and its proximal and distal attachments, and the
accessory collateral ligament. Figure 10-3 depicts the soft tissue anatomy of the PIP joint
 |
|
Figure 10-1 (A) X-ray appearance of a dorsal dislocation of the IP joint of the thumb. (B) X-ray appearance after reduction and splinting.
|
the end of the digit that results in an obvious deformity. The
attachments of the palmar plate are disrupted (usually distally). There
are also longitudinal but nondestabilizing tears
of the collateral ligaments in the zone between the proper (cord-like)
and accessory (fan-like) region of the collateral ligament complex.
-
These sports injuries are often reduced
shortly after the injury by the patient, a teammate, or coach, and the
patient usually presents to the examining physician with a swollen but
reduced PIP joint.![]() Figure 10-2 The bicondylar arrangement of the PIP joint accounts for its intrinsic bony stability.
Figure 10-2 The bicondylar arrangement of the PIP joint accounts for its intrinsic bony stability. -
Profile radiographs in the anterior-posterior (AP) and true lateral planes are obtained to note any fractures.
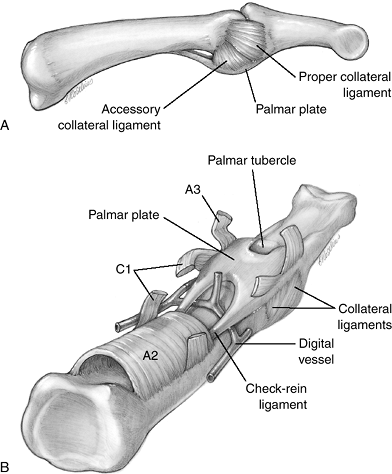 Figure 10-3
Figure 10-3
Artist’s depiction of the arrangement of the palmar plate and its
proximal and distal attachments, along with the proper and accessory
collateral ligaments.P.146![]() Figure 10-4 X-ray appearance of a dorsal PIP joint dislocation.
Figure 10-4 X-ray appearance of a dorsal PIP joint dislocation. -
In the unreduced state, these radiographs
most often reveal that the base of the middle phalanx is resting on the
dorsal neck of the proximal phalanx (Figure 10-4). -
Sometimes a small fragment of bone is
avulsed from the palmar base of the middle phalanx, which indicates
that the plane of disruption was through the base of the middle phalanx
rather than at the attachment of the palmar plate. This fragment
remains attached to the palmar plate volarly.
-
Closed reduction of the dislocation is
performed under digital block anesthesia, followed by longitudinal
traction and “pushing” the base of the middle phalanx distally. -
After reduction, stability of the joint is determined by active and passive movements of the joint.
-
Satisfactory active movement without
redislocation or deformity indicates that sufficient soft tissue
stability remains to allow early protected movement. -
Passive stability is confirmed by stress
testing of the collateral ligaments with the PIP joint in full
extension and at 30 degrees of flexion, and comparing this to an
uninjured but otherwise comparable digit. -
Increased mobility in the AP plane is
tested by gentle shear testing, by stabilizing the proximal phalanx and
moving the middle phalanx. -
This injury is seldom associated with a destabilizing
collateral ligament or other soft tissue injury, and the reduced digit
may be “buddy taped” to an adjacent digit for protected exercise. -
A large fracture fragment noted on
radiograph (usually 40% or more of the articular base of the middle
phalanx) indicates a fracture-dislocation and represents a destabilizing injury. These injuries are often treated by open reduction and fixation, or other forms of stabilization. -
Instability results due to the fact that
the majority, if not all, of the stabilizing collateral ligaments are
attached to this fragment and no longer act as stabilizers to the
middle phalanx. This topic is discussed in the chapter on Fractures and Fracture–Dislocations.
 |
|
Figure 10-5 X-ray appearance of a lateral dislocation of the PIP joint.
|
dislocation. It involves disruption of the origin or insertion of the
collateral ligament, disruption of the interval between the proper
collateral ligament and the accessory collateral ligament, and partial
disruption of the palmar plate attachment.
-
Complete lateral dislocations are clinically apparent, but subluxations may not be as obvious because of swelling.
-
Stress testing of the collateral ligament and accessory stabilizers is performed with the PIP joint in full extension.
-
An angular deformity of 20 degrees or more on the stress test is diagnostic of significant instability.
-
-
If stability is present with active and
passive flexion, and extension of the PIP joint and radiographs
demonstrate joint congruity, treatment is through protected motion by
“buddy taping” the injured digit to an adjacent digit. Surgery is
indicated for soft tissue interposition or a displaced fracture.
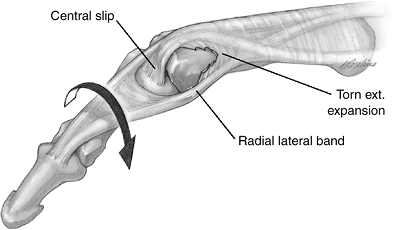
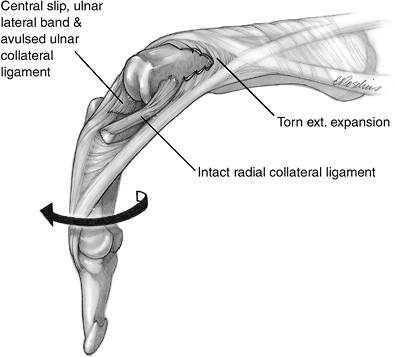
extensor mechanism between the lateral band and the central slip of the
extensor tendon, which allows the head of the proximal phalanx to enter
the separation and be trapped. The
displaced
lateral band is trapped behind the palmar aspect of the condyle,
resulting in a rotatory deformity of the middle and distal segment of
the finger (Figure 10-6).
 |
|
Figure 10-6
Rotatory subluxation of the proximal interphalangeal joint. This lesion occurs due to a longitudinal rent in the extensor mechanism between the lateral band and the central slip of the extensor tendon. This allows the head of the proximal phalanx to enter the separation and be trapped and rotated between the displaced lateral band and the central slip. |
forces, including rotation, flexion, and lateral deviation. The PIP
joint is most susceptible to torsional force at 55 degrees of flexion,
when the lateral bands shift palmar to the midaxis of the proximal
phalanx. Thus, the injury probably is sustained with the PIP joint in
moderate flexion. The term subluxation seems appropriate because the
PIP joint is not widely separated.
-
The PIP joint is in moderate flexion, the middle and distal phalanges are rotated, and there is swelling about the PIP joint.
-
A true lateral radiograph of the proximal
phalanx demonstrates partial separation of the PIP joint and obliquity
of the middle phalanx due to the rotatory component of this injury.
-
Although this condition has been reported
to be irreducible, closed reduction under appropriate anesthesia may be
attempted by simultaneous flexion of the metacarpophalangeal (MCP) and
PIP joints to relax the lateral band, followed by gradual extension
accompanied by rotation of the middle phalanx that is opposite to the
deformity. -
If this maneuver is not successful, open reduction is performed.
 |
|
Figure 10-7
Irreducible rotatory palmar dislocation of the PIP joint. The clinical appearance is characterized by almost 90 degrees of flexion at the PIP joint, supination of the distal aspect of the finger, and inability to reduce the deformity. |
the central slip, which, along with the ulnar lateral band, is
displaced palmar to the neck of the proximal phalanx (Figure 10-7).
Findings at surgery reveal the head of the proximal phalanx projecting
through an oblique tear in the extensor expansion between the central
slip and the radial lateral band. Findings also reveal the central slip
and ulnar lateral band displaced to lie together in front of the neck
of the proximal phalanx, where they act as a block to reduction. The
UCL is avulsed and the RCL is intact. As in rotatory palmar
subluxation, the mechanism of injury is a predominantly rotational
force. A common cause of injury is a full-spin clothes dryer that
catches a finger while it is still moving; the finger most often
involved is the index.
-
The clinical appearance is characterized
by almost 90 degrees of flexion at the PIP joint, supination of the
distal aspect of the finger, and inability to reduce the deformity.
-
The PIP joint is exposed through a dorsal
approach. Reduction is achieved by replacement of the displaced central
slip and lateral band, followed by repair of the rent in the extensor
mechanism.
reducible type of palmar dislocation is associated with injury to one
collateral ligament, the palmar plate, and the extensor mechanism
(usually the central slip insertion of the extensor tendon). Although
usually reducible, it is unstable because of loss of dorsal support
from the central slip. More
importantly,
if not recognized and treated properly, this results in a boutonniere
deformity because of the central slip disruption. Unilateral injury to
the collateral ligament results in a rotatory deformity because of the
suspensory effect of the intact collateral ligament. The mechanism of
injury is a varus or valgus stress followed by a palmar force that
dislocates the middle phalanx palmarly. Cadaver experiments that used
only an anterior force without varus or valgus force resulted in
avulsion of the central slip, usually with a fracture fragment and a
lesser incidence of collateral ligament rupture. Figure 10-8 depicts the x-ray appearance of reducible palmar dislocation.
 |
|
Figure 10-8 X-ray appearance of a palmar dislocation of the PIP joint.
|
-
If an anterior dislocation can be
reduced, it is important to recognize that an injury to the central
slip has occurred and requires appropriate treatment. -
It has been noted that palmar
dislocations of the PIP joint always injured the extensor mechanism
(most often a tear of the central slip), a collateral ligament, and the
palmar plate. -
The associated ligament and tendon
injury, if not treated, will result in loss of both static and dynamic
PIP joint support, which is manifested by palmar subluxation,
malrotation, boutonniere deformity, and fixed flexion contracture. Figure 10-9 Clinical and x-ray appearance of a neglected palmar dislocation of the ring finger PIP joint.
Figure 10-9 Clinical and x-ray appearance of a neglected palmar dislocation of the ring finger PIP joint.-
Figure 10-9 demonstrates the clinical and x-ray appearance of such a neglected case involving the PIP joint of the ring finger.
-
Although the joint was reduced and soft tissue reconstruction was performed, the end result was a stiff finger.
-
-
Irreducible palmar dislocations are not
usually associated with central slip disruption, and may have a more
favorable prognosis. -
Inability to reduce an anterior
dislocation is most likely due to interposition of a part of the
extensor mechanism, which can be corrected by surgery. -
There are two forms or stages of progression in rotatory injuries.
-
The first, or stage I, is a subluxation injury; the second, or stage II, is an irreducible dislocation.
-
Closed reduction of stage I injuries may be attempted in acute cases.
-
In stage II or complete dislocations, closed reduction is not advised.
-
joints of the fingers may be described as a single coffee cup that is
loosely placed in its saucer. The rounded coffee cup (the metacarpal
head) sits in its flat saucer (the base of the proximal phalanx) and
although the two joint surfaces are joined together, their shape and
ligamentous constraints permit mutiplanar movements including flexion,
extension, abduction, adduction, and limited pronation and supination (Figure 10-10).
Like the PIP joints, they are supported by primary and accessory
collateral ligaments. The MCP joint palmar plate is less rigidly fixed
proximally, and although a type of checkrein ligament exists, it is
less substantial than the one found at the PIP joint. This may explain
the normal ability of the MCP joint to hyperextend, whereas the PIP
joint is less prone to do so. One collateral ligament injury and two
dislocations have been recognized at the MCP joint finger joints.
 |
|
Figure 10-10 Anatomy of the finger MCP joint collateral ligaments. (A) A cross section of the MCP joint showing the various stabilizing structures of the joint. (B) Lateral view of the finger MCP joint. (C) Fresh cadaver dissection of the MCP collateral ligaments showing their comparatively relaxed tension in MCP joint extension. (D) Note the increased tension of the collateral ligaments in flexion.
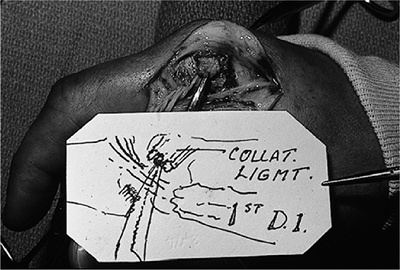
|
either the UCL or RCL of the thumb. Ruptures most often occur in the
little and index fingers, and involve the RCL. These fingers are most
commonly involved because of their position as border digits, but
finger MCP joint RCL ruptures have been reported in all the fingers.
The usual mechanism of injury is forced ulnar deviation with the
fingers flexed.
 |
|
Figure 10-11
Intraoperative appearance of a complete tear of the RCL of the index MCP joint. The curved clamp is on the proximal end of the RCL. The first dorsal interosseous muscle (1st DI) expansion was retracted, and the two ends of the ligament reapproximated with a Bunnell-type pullout suture. Excellent healing and stability was achieved. |
-
There is usually tenderness along the radial side of the joint, and pain on ulnar stress of the joint.
-
An arthrogram may aid in diagnosis.
-
Treatment should be based on functional
need, and may include primary reattachment, repair, or reconstruction
by tendon graft as needed (Figure 10-11).
The most common digit to be involved is the index, followed by the
small finger.
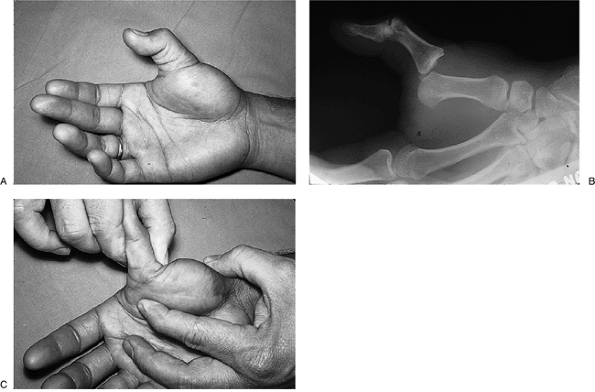
finger, often due to a fall on the outstretched hand. The proximal
attachment of the palmar plate is torn, and the suspensory effect of
the collateral ligaments allows the hyperextension force to thrust the
proximal phalanx and palmar plate dorsally to rest on the dorsal aspect
of the metacarpal.
-
Radially, the lumbrical
-
Proximally, the transverse fibers of the palmar aponeurosis
-
Ulnarly, the flexor tendons
-
Distally, the natatory ligaments and the palmar plate
-
It is important to distinguish between
complete irreducible dislocations and reducible subluxations, because a
subluxation can be converted to a complete and irreducible lesion by
inappropriate reduction maneuvers. -
In complete dislocation
(the irreducible lesion), the MCP joint is held in slight to moderate
extension; MCP joint flexion is impossible and the finger is ulnarly
deviated.-
A prominence may be palpated in the palm that corresponds to the metacarpal head, and the skin may be puckered. Figure 10-13 demonstrates the clinical appearance of complete dislocation of the MCP joint of the index finger.
-
-
In subluxation
(the reducible lesion), the findings are similar except that the
proximal phalanx is usually more hyperextended—often 60 to 80 degrees.
-
In complete dislocations, the radiographic findings may be minimal in the anteroposterior view.
-
The oblique view usually demonstrates widening of the joint space, and the lateral view may show the complete dislocation.
-
Lateral or dorsal displacement of the sesamoid in the oblique and lateral views also is an important finding.
-
A tangential or Brewerton view of the
metacarpal head may aid in the detection of an avulsion or other
fractures in the region of the metacarpal head (Figure 10-14).
-
Distinction must be made between
subluxation and complete dislocation because the former is reducible by
closed means and the latter is not.P.151![]() Figure 10-12 Complete dorsal dislocation of the index finger joint. (A–B) Extended and ulnar-deviated index finger. (C)
Figure 10-12 Complete dorsal dislocation of the index finger joint. (A–B) Extended and ulnar-deviated index finger. (C)
The head and neck of the dislocated metacarpal is trapped by the
transverse fibers of the palmar fascia, the flexor tendons, natatory
ligaments, and the palmar plate, and the lumbrical. -
In subluxation, the proximal edge of the palmar plate remains palmar to the metacarpal head.
-
If either hyperextension or traction is
used as part of the reduction technique, the palmar plate may be drawn
dorsally and result in a complete and irreducible dislocation. -
The proper reduction maneuver is
performed by flexion of the wrist, and distal and palmar force on the
base of the proximal phalanx that slides the phalanx over the
metacarpal head.
-
-
Irreducible dislocations are treated by open reduction.
-
Kaplan described a palmar approach for this condition, and others have described a dorsal approach.
-
 |
|
Figure 10-13 (A) Clinical appearance of a complete and locked dorsal dislocation of the MCP joint of the index finger. (B) Hyperextension at the MCP joint, and ulnar deviation of the index finger.
|
interposed structures that either block or trap the proximal phalanx from returning to its anatomic position.
 |
|
Figure 10-14 X-ray appearance of a dorsal dislocation of the index finger MCP joint. (A) The AP view shows only minimal changes at the MCP joint (arrow). (B) The oblique view shows a widened MCP joint space and some dorsal displacement of the proximal phalanx (arrow). (C) The lateral view shows a complete dislocation (arrow).
|
structures that suspend the proximal phalanx during flexion and
extension, it is easy to speculate that any disruption of the proximal
attachments or restraints to hyperextension may result in the proximal
phalanx going “over the top” with a sufficient hyperextension force,
and becoming locked or trapped on the dorsal surface of the metacarpal.
For this to occur, the palmar plate attachment must be disrupted either
at its proximal aspect or at its insertion into the base of the
proximal phalanx. If the palmar plate is disrupted distally, the
accessory collateral ligaments are torn, and this allows the proximal
phalanx and the collateral ligaments to swing dorsally to the top of
the metacarpal. If the palmar plate is detached proximally, it and its
imbedded sesamoid bones are carried dorsally along with the proximal
phalanx.
may be pulled along in this excursion are the adductor pollicis
aponeurosis, including the bony insertion on the ulnar base of the
proximal phalanx; the abductor expansion; and the two heads of the FPB,
which, along with the intact proper collateral ligaments, may form an
entrapment noose around the neck of the thumb metacarpal and prevent
reduction. The FPL may be entrapped in the joint but usually remains in
the sheath.
-
A radiograph that demonstrates sesamoid
bones on the dorsal aspect of the metacarpal and adjacent to the base
of the proximal phalanx usually indicates a complex irreducible
dislocation of this joint (Figure 10-15).
 |
|
Figure 10-15 Locked dorsal dislocation of the MCP joint of the thumb. (A) The sesamoid bones are resting on the dorsal aspect of the neck of the thumb metacarpal (arrow). (B) An open reduction was required to reduce this locked dislocation.
|
-
Closed reduction may be attempted, under
appropriate anesthesia, by flexing the wrist and thumb interphalangeal
joint and then pushing the hyperextended proximal phalanx distalward. -
Longitudinal traction is avoided because
it may “tighten the noose” represented by the various soft tissues
around the neck of the metacarpal and prevent reduction.![]() Figure 10-16 Clinical and x-ray appearance of an MCP thumb dorsal dislocation, and technique of reduction. (A) Note the hyperextension of the MCP joint. (B) The radiograph demonstrates that the proximal phalanx is “perched” on the dorsal aspect of the metacarpal. (C)
Figure 10-16 Clinical and x-ray appearance of an MCP thumb dorsal dislocation, and technique of reduction. (A) Note the hyperextension of the MCP joint. (B) The radiograph demonstrates that the proximal phalanx is “perched” on the dorsal aspect of the metacarpal. (C)
Reduction under suitable anesthesia is achieved by hyperextension of
the proximal phalanx and by “pushing” or “sweeping” it off the neck of
the metacarpal. -
If closed means are not successful, open reduction is indicated through a dorsal or palmar approach.
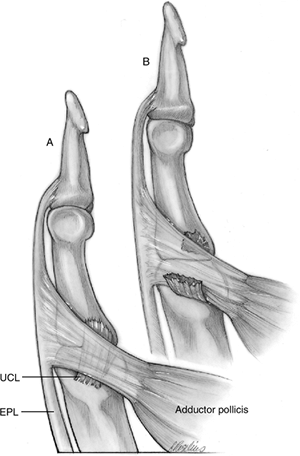
deviation (abduction) of the proximal phalanx of the thumb, often
secondary to a fall on the out stretched hand with the thumb abducted.
It may be associated with activities such as skiing or ball sports.
without a bone fragment) is five times more common than proximal tears
or disruptions. Tears in the substance of the UCL occur with less
frequency. Associated injuries include tears of the dorsal capsule,
partial avulsion of the palmar plate, or a tear in the adductor
aponeurosis. In addition to providing lateral stability to the MCP
joint, the UCL and RCL play a role in suspending the proximal phalanx.
Therefore, disruption of the UCL may result in palmar migration and
rotation (supination) of the proximal and distal phalanx on the intact
RCL.
with interposition of the adductor aponeurosis between the distally
avulsed UCL and its site of insertion. This configuration is easy to
understand based on the fact that the UCL is deep to the adductor
aponeurosis. Also, with avulsion it is carried proximally, while the
leading edge of the adductor aponeurosis is carried distally by the
deforming force of injury. When the force abates and the proximal
phalanx returns to its normal alignment, the UCL is external rather
than deep to the adductor aponeurosis. Even if this configuration did
not occur, the natural tension in the ligament and subsequent
contracture would place it well proximal to its distal attachment, and
beneath the aponeurosis. The Stener lesion is depicted in Figure 10-17.
-
The diagnosis is made by noting the
mechanism of injury; identifying tenderness, swelling, or ecchymoses
over the ulnar side of the MCP joint; and noting laxity of the UCL with
stress testing.-
Local anesthesia may be used to facilitate the stress test.
-
-
A radiograph is made as part of the
stress test to document the degree of opening of the joint. Comparison
stress films may be made of the opposite side, as needed. -
It is beyond the scope of this text to
discuss the methods of stress testing in detail, except to note that
with complete UCL disruption, the MCP joint may be opened with minimal
resistance.
 |
|
Figure 10-17 The Stener lesion. (A) The UCL lies beneath the adductor aponeurosis. (B)
Rupture of the UCL occurs with sufficient abduction force. When the MCP joint resumes its anatomic position, the proximal portions of the UCL are trapped proximal and superficial to the adductor aponeurosis. The aponeurosis must be surgically reflected, and the UCL rejoined in its anatomic position, to restore stability to the joint. |
-
The basic principle of treatment in complete ruptures of the UCL is to reattach the UCL to its anatomic site of attachment.
-
If the anatomic sites of attachment are not duplicated, there may be less range of motion than normal of the MCP joint.
the so-called avulsion fractures that may be seen with UCL injuries
marks the distal aspect of the disrupted UCL. A widely displaced
fracture fragment would indicate significant displacement of the UCL,
and would suggest the need for surgical intervention. A recent case
study reevaluated this concept and found that the location of the
fracture fragment did not always indicate the location of the ruptured
collateral ligament. The author of this study, quoting reports by
Stener in 1963 and 1969, noted that fractures of this type
are either avulsion fractures due to UCL disruption, or shear
fractures at the base of the proximal phalanx by the palmar portion of
the radial condyle of the metacarpal. If the fracture seen on
radiographs is a shear fracture, its position is unrelated to the
location of the distal end of the avulsed UCL. A displaced ligament may
occur in the presence of an undisplaced fracture.
 |
|
Figure 10-18 Radial collateral ligament disruption at the MCP joint of the thumb. (A) Positive stress test manifested by abnormal deviation of the proximal phalanx. (B)
The complete avulsion of the RCL was repaired by reattachment of its proximal origin using a small screw. The repair was protected by an oblique transarticular Kirschner wire until healing occurred. |
aponeurosis, there is no potential for soft tissue interposition (the
Stener lesion) with an RCL avulsion. In contrast to the UCL, the RCL is
torn with almost equal frequency proximally and distally, and
mid-substance disruption is more common in the RCL than in the UCL. The
abductor aponeurosis may be disrupted, in addition to the RCL.
Disruption of the RCL results in palmar migration and pronation of the
proximal phalanx and dorsoradial prominence of the metacarpal head. In
my experience, these findings may not be as noticeable immediately
after the injury, possibly because initial swelling might mask the
deformities, or because these findings may occur progressively and thus
may not be prominent in the early phase of this condition.
-
Diagnosis of the acute injury is made
based on the history of the injury, findings of ecchymosis or
tenderness, and a positive instability test. -
Figure 10-18
demonstrates a positive stress test in an acute RCL avulsion that was
repaired by reattachment of the ligament at its proximal attachment. -
In my experience, RCL injuries tend to be diagnosed late rather than early, when compared to UCL injuries.
-
This may be because a complete disruption
of the UCL results in immediate and significant disability owing to the
functional demands placed on the ulnar side of the thumb, leading to
early evaluation. -
The RCL injury and subsequent dysfunction
does not seem to be as disabling, at least in the beginning, but as
time passes, it becomes increasingly bothersome and is in fact a
significant source of patient complaint and disability.
-
-
The basic principle of treatment in
complete ruptures is to reattach the RCL to its anatomic site of
insertion or repair the tear. -
Late diagnosis may require ligament reconstruction by a tendon graft.
activities, or breaking a fall. Possible predisposing factors are an
anatomic variation in the collateral ligaments that allow greater MCP
flexion, and an area of relative thinness and weakness in the
dorsoradial capsule compared with the ulnar side of the joint.
-
The primary complaint is pain over the
dorsum of the thumb and limited use of the thumb. This diagnosis should
be considered in patients with persistent pain at
P.156the thumb MCP joint.
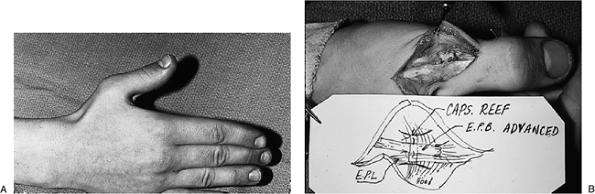 Figure 10-19 Dorsoradial capsular injury at the thumb MCP joint. (A) Flexed posture of the thumb MCP joint that represents maximum extension for this patient. (B)
Figure 10-19 Dorsoradial capsular injury at the thumb MCP joint. (A) Flexed posture of the thumb MCP joint that represents maximum extension for this patient. (B)
Repair was achieved by reefing the dorsoradial capsule of the MCP
joint, and by advancing the extensor pollicis brevis tendon about 0.5
cm distal to its insertion.![]() Figure 10-20 X-ray appearance in three views of a dorsal dislocation of the CMC joint of the ring and little fingers (arrows). Note that the dislocation is most apparent in the oblique and lateral views.P.157
Figure 10-20 X-ray appearance in three views of a dorsal dislocation of the CMC joint of the ring and little fingers (arrows). Note that the dislocation is most apparent in the oblique and lateral views.P.157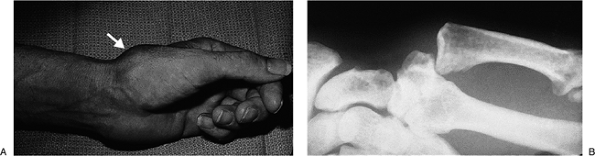 Figure 10-21 Dorsal dislocation of the thumb MCP joint. (A) Dorsal prominence at the base of the thumb metacarpal (arrow). (B) The radiograph reveals complete dislocation without fracture.
Figure 10-21 Dorsal dislocation of the thumb MCP joint. (A) Dorsal prominence at the base of the thumb metacarpal (arrow). (B) The radiograph reveals complete dislocation without fracture. -
Patients typically demonstrate tenderness
over the dorsoradial aspect of the thumb MCP joint in the absence of
laxity of either the RCL or UCL. -
In some instances, there is minimal palmar subluxation of the proximal phalanx.
-
Some patients experience loss of full active extension of the proximal phalanx.
-
Some patients can be treated successfully by immobilization if no palmar subluxation or extensor lag exists.
-
Surgery is indicated for persistent
activity-limiting complaints over the dorsoradial capsule, or if
findings of palmar subluxation and extensor lag exist. -
Findings at the time of surgery include thinning or redundancy of the dorsoradial capsule, or an obvious defect in the capsule.
-
Treatment is by reefing (imbrication) or
direct closure of the defect in the dorsoradial capsule, and
advancement of the insertion of the EPB tendon, if an extensor lag is
present. An appropriate period of immobilization to protect the repair
should follow. -
Figure 10-19 shows a patient with this lesion and the surgical intervention that was performed.
the thumb and fingers have been reported, but they are rare. Most are
fracture–dislocations, and these injuries have been discussed in the
chapter on fractures of the hand. When isolated dislocations of the CMC
joint occur, they are usually dorsal and are caused by a longitudinal
compression force that produces simultaneous flexion and compression of
the metacarpal that drives the metacarpal base from its carpal
articulation. Most occur in the little and ring fingers and are even
more rare in the thumb.
-
Figure 10-20 shows the x-ray appearance of a dorsal dislocation of the CMC joint of the ring and little fingers.
-
Figure 10-21 shows the clinical and x-ray appearance of a dislocation of the thumb CMC joint.
CHG, Tencer AF, Trumble TE. The effect of thumb metacarpophalangeal
ulnar collateral ligament attachment site on joint range of motion: an
in vitro study. J Hand Surg 1999;24A:283–287.
JL, Christian JD, Goodwin HN, et al. A simplified technique for
treating the complex dislocation of the index metacarpal joint. J Bone
Joint Surg 1975;57:683–688.
RA, Weatherwax RJ, Miller EB. Chronic post traumatic radial instability
of the thumb metacarpophalangeal joint. J Hand Surg 1980;5:221–225.
JR, Atkinson RE. Rupture of the radial collateral ligament of the
metacarpophalangeal joint of the index finger: a report of three cases.
J Hand Surg 1989;14B:248–250.
JR. Irreducible rotational anterior dislocation of the proximal
interphalangeal joint: a spin dryer injury. J Hand Surg
1993;18B:648–651.
JO, Manske PR, Mirly HL, et al. Isolated injuries to the dorsoradial
capsule of the thumb metacarpophalangeal joint. J Hand Surg
1996;21A:428–433.
M, Choi BY. Anterior dislocation of the proximal interphalangeal joint,
a cause of rupture of the central slip of the extensor mechanism. J
Bone Joint Surg 1970;52:1329–1336.
B. Displacement of the ruptured ulnar collateral ligament of the
metacarpophalangeal joint of the thumb: a clinical and anatomic study.
J Bone Joint Surg 1962;44B:869–879.
B, Stener I. Shearing fractures associated with rupture of the ulnar
collateral ligament of the metacarpophalangeal joint of the thumb.
Injury 1969;1:12–16.