Complications
spinal surgery has been reduced, complications can be serious and
potentially life-threatening. The complications can be categorized by
the period of time during which they occur relative to the surgical
procedure, as follows:
-
Intraoperative, which occur in the operating room
-
Perioperative (early postoperative), which occur within a few days after surgery, usually during hospitalization
-
Delayed postoperative, which occur weeks to years after surgery
-
Patient positioning
-
Technical aspects of surgical exposure
-
Insertion of spinal instrumentation
-
Harvesting of autograft bone
-
Superficial wound infections
-
Deep venous thrombosis
-
Pulmonary embolism
-
Urinary retention
-
Malnutrition
-
Late postoperative instability
-
Infection
-
Deformity
-
Pseudarthrosis
-
Adjacent segment disease
-
Epidural fibrosis
-
Arachnoiditis
on the operating table. Care must be taken to ensure that the airway is
protected when the patient is transferred from a stretcher to the
operating table, especially if the patient is being turned from a
supine to a prone position. In the prone position, the face must be
padded evenly to avoid pressure ulceration. Direct pressure on the eye
must be avoided to prevent catastrophic retinal artery occlusion and
loss of vision. Direct pressure applied to the scalp has been
associated with alopecia, usually reversible, but occasionally
permanent.
elbows, hips, and knees, helps prevent injuries to the ulnar, lateral
femoral cutaneous, and common peroneal nerves. The brachial plexus can
be at risk in the lateral decubitus or prone position. An axillary roll
(which is placed 5 to 10 cm distal to the axilla) and avoidance of
excessive abduction of the shoulder can help reduce the incidence of
postoperative brachial plexopathy.
positioning. The abdomen should remain free to prevent vena cava
compression. Decreased venous return can lead to loss of cardiac
preload and subsequent hypotension. Batson showed that obstruction of
caval flow can produce increased venous pressure around the epidural
sinusoids of the spine, which may lead to increased blood loss.
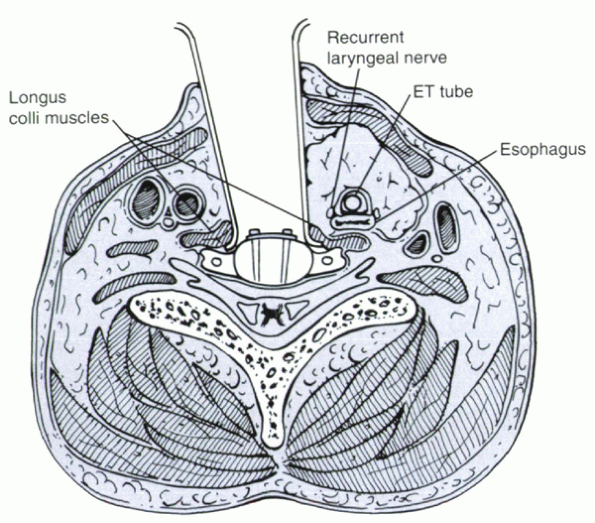
anterior surgery on the cervical spine may occur. Meticulous atraumatic
dissection and careful placement of deep retractors can minimize these
complications. The recurrent laryngeal nerve runs between the esophagus
and the trachea. When deep retractors are placed, the recurrent
laryngeal nerve can be pinched between the retractor and the
endotracheal cuff (Fig. 29-1). Some authors
believe that it is important to deflate the endotracheal cuff to lower
pressure of the recurrent laryngeal nerve. Releasing the endotracheal
cuff and reinflating the cuff at a lower tension decreases the pressure
on the recurrent laryngeal nerve and decreases the incidence of
postoperative vocal cord paralysis. The airway must be maintained clear
of secretions, however, to avoid retrograde flow or aspiration into the
lungs.
posterior approaches. It is at particular risk during placement of C1-2
transarticular screws. Most vertebral artery lacerations
can
be treated by packing with thrombin-soaked absorbable gelatin sponges.
In rare cases, ligation may be required for hemostasis. Although most
patients tolerate unilateral vertebral artery ablation, a small
percentage have symptomatic vertebrobasilar symptoms, such as syncope,
nystagmus, dizziness, or Wallenberg syndrome (ipsilateral loss of
temperature and pain sensation of the face and contralateral loss in
the extremities and trunk, dysphagia, dysarthria, and nystagmus). If
possible, repair of an injured vertebral artery might be considered.
 |
|
Figure 29-1
Cross-sectional anatomy of the cervical spine during anterior cervical spine surgery. The retractors are shown under the longus colli muscles. The recurrent laryngeal nerve lies between the retractor blade and the trachea. ET, endotracheal. (From Apfelbaum RI, Kriskovich MD, Haller JR. On the incidence, cause, and prevention of recurrent laryngeal nerve palsies during anterior cervical spine surgery. Spine 2000;25:2906-2912.) |
incidence of deep infection. Palpation of the nasogastric tube can help
identify the location of the esophagus. Subperiosteal elevation of the
longus colli muscles from the anterolateral vertebral bodies with
placement of deep retractors under the elevated muscle edge can help
prevent injury. The most frequently occurring symptoms are neck pain,
odynophagia, dysphagia, and hoarseness. Cervical osteomyelitis or
cervical abscess develops in about half of patients. Clinical findings
include fever, cervical tenderness and induration, weight loss,
tachycardia, crepitus from emphysema, and hematemesis. A combination of
endoscopy and a swallow study is regarded by most authors to have the
highest diagnostic yield.
Nonoperative management, including observation, intravenous nutrition,
feeding tube or gastrostomy, appropriate antibiotic coverage, and
aspiration precautions, should be reserved for small perforations in
patients otherwise too sick to undergo surgery. The literature
indicates high morbidity and mortality with nonoperative management of
all but the smallest of perforations, especially with tears of the
lower esophagus. Consultation with a thoracic or esophageal surgical
specialist is recommended in all cases. The esophagus should be
examined carefully after any anterior cervical spinal operation before
closure. Any esophageal injury noted in the operating room should be
repaired by an experienced surgeon. The repair can be augmented, if
necessary, with a muscle flap, such as a proximally based
sternocleidomastoid rotational flap. This augmentation is of particular
utility in cases of delayed diagnosis and of large defects that are not
amenable to primary repair.
by pneumothorax, hemothorax, and chylothorax. Massive hemothorax may
occur from profuse vertebral body bleeding. This condition may require
surgical tamponade of venous sinuses in the vertebral body with bone
wax or ligation of the respective segmental arteries.
the physician to the possibility of a thoracic duct injury. The
thoracic duct has a winding course along the spine. In the lower
thoracic spine, it lies anterior and slightly to the right of the spine
between the aorta and azygos vein and behind the esophagus. In the
upper spine, it crosses over to the left side, behind the aortic arch.
Iatrogenic chyle leaks have been reported after spinal surgery. Most
leaks are clinically insignificant and heal spontaneously. If a
chylothorax is suspected postoperatively, diagnostic thoracentesis and
tube thoracostomy should be done. Oral intake should be discontinued
because even low-fat clear liquids markedly increase chyle flow.
Traditionally, continued chylous chest drainage for more than 6 weeks
is an indication for open surgical intervention. Some authors recommend
surgical treatment within 2 weeks to prevent ongoing protein and
lymphocyte losses and to minimize the risk of infection.
sensitive to the effects of mild ischemia. Anterior procedures of the
spine often require mobilization or ligation of the segmental vessels
over numerous levels. In most cases,
ligation
of multiple ipsilateral segmental arteries can be performed without
neurologic compromise. In some cases, especially in the setting of
congenital deformity correction, segmental artery disruption may lead
to neurologic compromise.
retroperitoneal or, less commonly, the transperitoneal approach. If the
location of the pathology does not necessitate one side or the other, a
left-sided approach is preferred because the aorta is easier to
mobilize than the thin-walled vena cava. The left common iliac vein is
the vessel most at risk during left-sided retroperitoneal and
transperitoneal exposures. Regardless of approach, instrumentation
should be placed on the lateral side of the vertebral body and should
not contact the great vessels. The ureters and great vessels are at
risk in retroperitoneal dissections, especially in the revision
setting. Consideration should be given to preoperative ureteral
stenting before revision procedures. Injury to the sympathetic plexus
overlying the anterior aspect of the lower lumbar and upper sacral
vertebrae may lead to retrograde ejaculation in men.
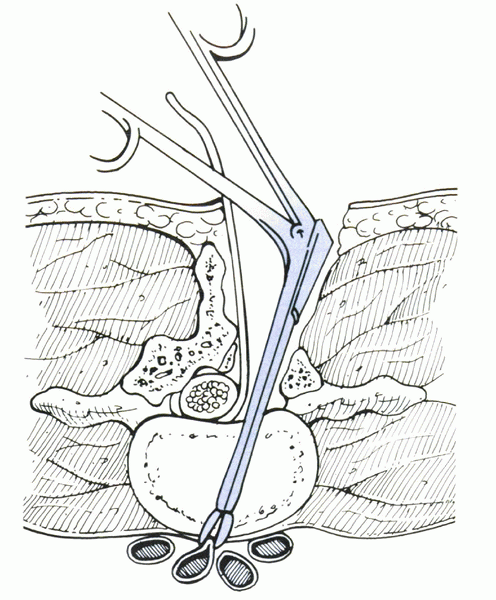
surgery are uncommon. Vascular injury may occur during discectomy if
the anterior longitudinal ligament is violated. The pituitary rongeur
is the most frequent culprit (Fig. 29-2).
Unless acute hypotension occurs intraoperatively, these injuries
initially may go unnoticed. Late abdominal rigidity, abdominal pain,
tachycardia, and anemia should alert the physician to the possibility
of this complication.
headache, wound complications, meningitis, arachnoiditis, and
pseudomeningocele. Postoperatively, persistent CSF leaks lead to clear
drainage from the wound or a subcutaneous fluid collection. Severe
headache exacerbated by upright posture may be noted. Large volumes of
fluid can be seen because the choroid plexus produces more than 20 mL
of CSF hourly. If it is unclear whether drainage is CSF, testing for β2-transferrin
can be useful. A pseudomeningocele may develop if a dural tear occurs
and is not repaired in a watertight fashion. A pseudomeningocele may
occur days to months postoperatively.
dural rent. The goal is a watertight repair that is tension-free.
Usually this repair can be accomplished with 6-0 polypropylene suture
placed in a running locking stitch. A Valsalva maneuver to 40 torr may
be simulated by the anesthesiologist after repair to assess for
residual leak. If leakage occurs after repair, augmentation with
additional suture, gelatin sponge, autogenous fat, or fibrin glue is
advised. More complex tears may require grafting with fascia lata or
with commercially available dural patches. Meticulous watertight
fascial closure is as important as the dural repair itself because the
healing of the fascial barrier is important in preventing durocutaneous
fistulas. Most surgeons avoid the use of wound drains in the presence
of a dural tear because negative pressure may encourage a persistent
leak.
 |
|
Figure 29-2
The pituitary rongeur may injure anterior vessels during discectomy, particularly if the anterior longitudinal ligament is disrupted. (From Garfin SR. Complications of spine surgery. Baltimore: Williams & Wilkins, 1989.) |
result. Systems employing rods and hooks can fail from hook pullout,
hook-rod disengagement, or rod fracture. Hook pullout occurs commonly
if used in osteoporotic bone or at the apex of a kyphotic segment.
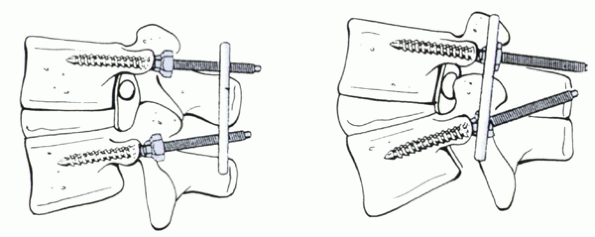
reliability and versatility of spinal fixation; however, the potential
complications can be significant. A short screw or a screw placed too
lateral can have suboptimal fixation. A medially and inferiorly placed
screw may violate the canal or foramen and cause a dural tear or
neurologic injury. A screw that is excessively long may violate the
anterior aspect of the vertebral body with potentially life-threatening
perforation of the great vessels. Similarly, excessive compression of
the reconstructed segments can lead to foraminal encroachment (Fig. 29-3).
In experienced hands, the rate of complications is low. In a large
series, only 0.2% of screw fixations needed reoperation for nerve root
irritation and 0.5% of screws were fractured at follow-up.
with its harvest. The most common complication is persistent pain at
the donor site. Often this pain is more bothersome and lasts longer
than the pain associated with the principal procedure. Although there
is no accepted method to avoid donor site pain, most authors agree that
limited muscle dissection and periosteal stripping is helpful.
 |
|
Figure 29-3 Foraminal encroachment of the nerve root by hyperextension with pedicle screw instrumentation. (From Richardson WJ. Complications in spinal surgery. Curr Opin Orthop 1993; 4:155-159.)
|
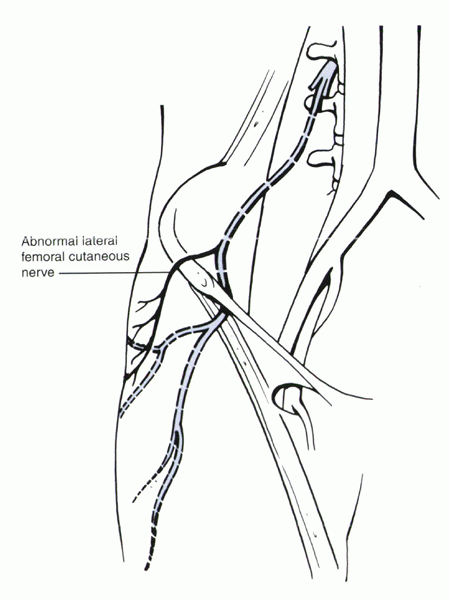
harvesting is injury to the lateral femoral cutaneous nerve leading to
meralgia paresthetica. The lateral femoral cutaneous nerve is a sensory
branch of the lumbar plexus that supplies the lateral aspect of the
thigh. It emerges from the lateral border of the psoas muscle and
crosses the anterior border of the iliacus muscle to reach the anterior
superior iliac spine. It passes into the thigh usually inferior to the
inguinal
ligament and medial to the anterior superior iliac spine. Retraction of
the iliacus muscle may traumatize the nerve, particularly if an inner
table graft is taken. Some patients have an anomalous anatomy path in
which the nerve may be located as far lateral as 2 cm from the anterior
superior iliac spine, above the inguinal ligament (Fig. 29-4). Careful visualization of this potential variant is required during dissection.
 |
|
Figure 29-4
Anteroposterior view of the right hemipelvis showing an anomalous course of the lateral femoral cutaneous nerve, which may be 2 cm lateral to the anterior superior iliac spine. (From Garfin SR. Complications of spine surgery. Baltimore: Williams & Wilkins, 1989.) |
posterior iliac crest harvesting. The superior gluteal artery branches
off the internal iliac artery and enters the gluteal region through the
most superior aspect of the sciatic notch. These structures may be
injured during subperiosteal dissection with elevators or inadvertent
penetration by a toothed retractor. If the artery is transected, it
tends to retract into the pelvis. Hemostasis may require further bone
resection to expose the stump, embolization, or anterior exploration
and ligation.
harvesting and are likely due to a stress riser created in the ilium at
graft acquisition. This phenomenon is most likely to occur in older
osteoporotic patients with long lumbosacral fusions. Protected weight
bearing typically is adequate for resolution of symptoms.
3%. Simple lumbar discectomy has less than a 1% infection rate, whereas
combined fusion and instrumentation is associated with rates of 4% to
8%. Risk factors include the following:
-
Increased age
-
Obesity
-
Diabetes
-
Smoking
-
Immunosuppression
-
Duration of preoperative hospitalization
-
Spinal dysraphism
-
Myelodysplasia
-
Revision surgery
-
Operative time
-
Use of instrumentation, bone graft, or methyl methacrylate
prevent infection is widespread. Patients with instrumented fusions
have a decreased infection rate with the use of prophylaxis compared
with patients having surgery without prophylaxis. Commonly the
antibiotic dose is administered before the incision and for 24 hours
postoperatively, although some surgeons prefer to administer
antibiotics until suction drains or catheters are removed. The choice
of antibiotic is guided by consideration of multiple factors, including
host immunocompetence; the bacterial flora common in the region; and
procedure type, cost, and side-effect profile. Most commonly a
cephalosporin is used. With increasing concerns regarding the
development of bacterial resistance, drugs such as vancomycin should be
discouraged and reserved only for patients at increased risk of
methicillin-resistant staphylococci infections; this includes patients
with lymphopenia, recent or current hospitalization, postoperative
wound drainage, and alcohol abuse.
antibiotics and local wound care. Nonresponsive superficial infections
require early surgical intervention. The débridement should proceed in
a systematic fashion. Each layer is débrided and cultured before
advancing deeper with the dissection. In most cases, the infection
tracks to the bone or hardware, and deep débridement should be
performed.
in place in the early postoperative period, all other foreign bodies,
such as bone wax and collagen sponges, must be removed. Hematomas
should be evacuated. Adherent bone graft may be retained, whereas loose
and necrotic graft is removed. Susequent bone grafting may be performed
at a later débridement after the infection is controlled better.
Primary wound closure over drains, often with retention sutures to
prevent dehiscence, is favored. Depending on the amount of devitalized
tissue, routine serial débridements often are required. Complex wound
infections may require musculocutaneous flaps. Postoperatively,
antibiotic therapy is required for at least 10 to 14 days for
superficial infections. Six weeks of parenteral antibiotic treatment is
recommended in cases of bone involvement, deep infection, or retained
foreign bodies (e.g., metal, graft).
significant effects on morbidity and mortality. The degree of
malnutrition is related to the number of spinal levels treated.
Prospective studies have shown that patients undergoing sixlevel
fusions require at least 6 weeks to recover, whereas patients
undergoing 13-level fusions require at least 12 weeks. Perioperative
malnutrition is especially problematic in patients undergoing staged
anterior and posterior procedures. There is often little or no enteral
intake between stages. Combined with the catabolic state after major
surgery, patients often have deleterious malnutrition leading to higher
rates of postoperative complications, such as wound infection, sepsis,
and pneumonia. Total parenteral nutrition between stages of anterior
and posterior procedures may lower rates of pneumonia, urinary tract
infections, and wound complications.
The incidence of urinary retention can be 38%, however. Advanced age
and preoperative use of β-blockers are risk factors for this problem.
Patients undergoing lumbar laminectomy are at higher risk than patients
undergoing simple discectomy or cervical spinal surgery. Prolonged
bladder catheterization leads to a higher risk of urinary retention,
possibly by mechanical irritation of the trigone, which serves to
straighten and shorten the bladder neck. When the patient can stand,
the catheter is removed. Straight catheterization is performed every 6
hours for urinary retention.
noninstrumented fusions. Rates of pseudarthrosis after posterior spinal
fusion vary widely in the literature from 0% to 50%. The most common
sequela of pseudarthrosis is pain. Diagnosis can be challenging.
Instrumentation often obscures radiographic evaluation, and back pain
often persists even in patients with a solid fusion. Screw fracture or
lucency around screws suggests fusion failure.
attempted fusion levels. Tobacco use, advanced age, malnutrition, and
use of nonsteroidal antiinflammatory drugs have been associated with
decreased rates of fusion. If patients stop smoking for at least 6
months after lumbar fusion surgery, the rate of nonunion may be
comparable to that of nonsmokers.
degeneration that occurs above and below the level of a fusion.
Instrumented fusions seem to be more prone to this phenomenon than
fusions without instrumentation. The cause of adjacent segment disease
is unclear. Possible causes include direct impingement of
instrumentation on the facet joints or denervation of the surrounding
tissues, especially the facet capsule, leading to neuropathic
destruction of the facet. The facet joint adjacent to the fusion site
should be protected. One should avoid ending a fusion at a region of
stenosis, spondylolisthesis, or posterior column deficiency.
subset of patients who have poor clinical outcomes after lumbar
procedures. It is likely that some of these cases are a result of
epidural scarring. With the advent of magnetic resonance imaging (MRI),
exuberant epidural fibrosis is recognized after spinal surgery.
concerning the importance of epidural fibrosis. Several studies have
failed to show a correlation between epidural scarring and clinical
outcome. A large multicenter, randomized, double-blind, prospective
clinical trial showed, however, that the presence of epidural scar
increases the likelihood of a poor outcome after lumbar surgery. In a
study of 197 patients undergoing contrast-enhanced MRI after
single-level laminotomy and discectomy, patients with extensive
peridural scar were 3.2 times more likely to have recurrent radicular
pain that patients with less extensive scarring. These findings suggest
that epidural scar formation increases the likelihood of a poor outcome
after lumbar disc surgery.
studied. Barriers such as absorbable gelatin sponge (Gelfoam), gelatin
films, collagen sponges, and cellulose sponges have been shown to be
ineffective in preventing epidural scar formation. Fat grafts,
polyglactin 910 (Vicryl) meshes, and fibrin glue have moderate
inhibitory effects on scar formation but do not affect clinical
outcomes. More contemporary barriers include viscous
carboxymethylcellulose, carbohydrate polymer sheets, collagen sealant,
and silicone tubing. These barriers have been shown to decrease scar
formation in animal models.
piaarachnoid membrane surrounding the spinal cord, cauda equina, or
nerve roots. It is an intradural process. There is a continuum of
involvement, ranging from mild membrane thickening to dense scarring
that can block CSF flow. Patients show a wide constellation of pain and
neurologic symptoms. The causes of arachnoiditis are variable.
Oil-based intrathecal contrast media used for myelography and meningeal
infections were the main causes of this disease until more recently.
Failed back surgery syndrome, marked by persistent pain, numbness, and
weakness after spinal surgery, is thought to be due in part to
arachnoiditis. Arachnoiditis is more frequent in patients who have had
extensive procedures, repeated procedures, postoperative spinal
infections, or intraoperative dural tears.
arachnoiditis using a three-group classification system. Group 1 showed
conglomerations of adherent nerve roots residing centrally within the
thecal sac. Group 2 showed nerve roots adherent peripherally to the
meninges, giving rise to an “empty sac” appearance. Group 3 showed a
soft tissue mass replacing the subarachnoid space. MRI resulted in
accurate diagnosis and had excellent correlation with computed
tomography-myelography and plain film myelographic findings.
(antiinflammatory, nerve stabilizing, and narcotic) combined with
activity modification and physical therapy. Intrathecal infusion of
morphine, transcutaneous nerve stimulation, and dorsal column
stimulators have produced variable results. Surgery involving extensive
microsurgical dissection and lysis of fibrotic tissue produces good
short-term results in selected patients, but these results diminish
greatly with time, and surgery rarely is indicated. Given the
challenges of treatment, concentrated effort at avoiding this problem
is warranted.
challenging. Complications may occur during various periods of surgical
treatment. Intraoperatively, meticulous technique guided by known
potential risks of each procedure is essential. Perioperatively, wound
care, pulmonary toilet, bladder care, and nutrition must be diligent.
Postoperatively, pseudarthrosis, adjacent segment disease, kyphosis,
epidural fibrosis, and arachnoiditis may develop months to years after
surgery. Regular follow-up and prompt recognition of potential
complications provide a better opportunity for effective treatment.
RI, Kriskovich MD, Haller JR. On the incidence, cause, and prevention
of recurrent laryngeal nerve palsies during anterior cervical spine
surgery. Spine 2000;25:2906-2912.
NM, Mian FS, Rodriguez D, et al. Urinary retention following routine
neurosurgical spine procedures. Surg Neurol 2001;55: 23-28.
CW, Orme TJ, Richardson HD. The rate of pseudarthrosis (surgical
nonunion) in patients who are smokers and patients who are nonsmokers:
a comparison study. Spine 1986;11:942-943.
RB, Ross JS, Masaryk TJ, et al. Diagnosis of lumbar arachnoiditis by
magnetic resonance imaging. Spine 1990;15:304-310.
SD, Anagnost SC, Parker A, et al. The effect of cigarette smoking and
smoking cessation on spinal fusion. Spine 2000;25: 2608-2615.
LG, Bridwell KH, Blanke K, et al. Prospective analysis of nutritional
status normalization after spinal reconstructive surgery. Spine
1995;20:1359-1367.
JS, Obuchowski N, Modic MT. MR evaluation of epidural fibrosis:
proposed grading system with intra- and inter-observer variability.
Neurol Res 1999;21:S23-S26.
