Calcaneus Fractures
challenging for the orthopaedic surgeon. Calcaneal fractures account
for approximately 2% of all fractures, with displaced intra-articular
fractures comprising 60% to 75% of these injuries. Of patients with
calcaneal fractures, 10% have associated spine fractures and 26% are
associated with other extremity injuries.129,182
Ninety percent of calcaneal fractures occur in men between 21 and 45
years of age, with the majority being in industrial workers; thus, the
economic implications of this injury are substantial.1,42,62,129,160,237
Several authors have reported that patients may be totally
incapacitated for up to 3 years and partially impaired for up to 5
years postinjury.1,62,129,160,237
Although modern surgical techniques have improved the outcome in many
patients, controversy still exists regarding classification, treatment,
operative technique, and postoperative management.
Since then, a distinction between the tongue-type and
joint-depression-type fracture has been known, and treatment has often
been type specific.
suggested that an open reduction of a calcaneal fracture was
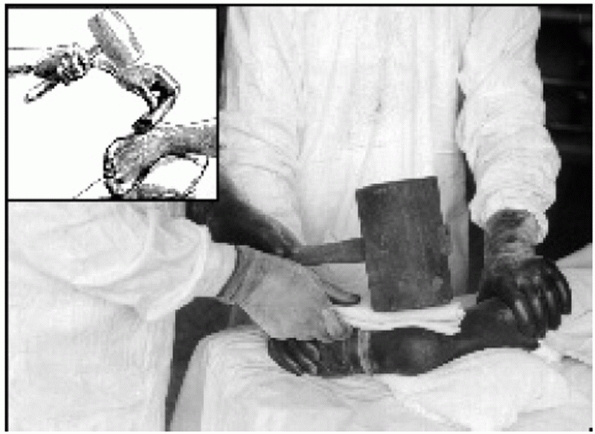
contraindicated and favored closed manipulation using a hammer to
reduce the lateral wall and “reimpact” the fracture (Fig. 59-1).
Despite his initial enthusiasm for this technique, by the 1920s he had
given up the treatment of acute fractures altogether and turned instead
to the treatment of healed malunions.40
and other French surgeons popularized this technique, alternating
between screws and bone graft for stabilization of the reduction.62,119 Böhler began to advocate open reduction of calcaneal fractures in 193118
based on his experience with the French methods. Despite this, forcible
closed reduction with tongs and hammers, or traction followed by manual
manipulation and casting, was the standard treatment of his time,
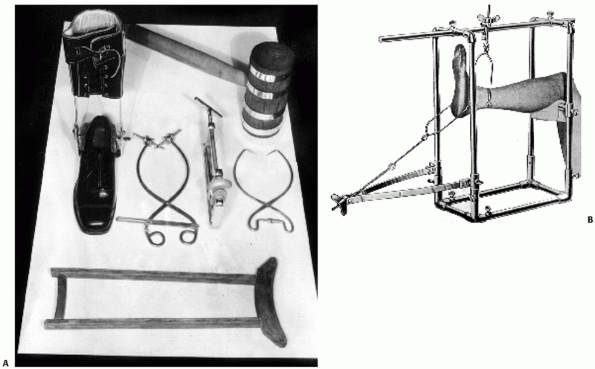
because of technical problems associated with surgery. Böhler19 popularized traction in multiple planes and improved on reduction, developing devices such as his unique clamp (Fig. 59-2).
 |
|
FIGURE 59-1 Closed reduction using a hammer. (From Cotton F. Dislocations and Joint-Fractures. Philadelphia; WB Saunders, 1910.)
|
did not believe that the midfoot should be fused, however, and in 1943
proposed subtalar arthrodesis as the definitive treatment. Given his
stature, the technique immediately became the standard for care.
 |
|
FIGURE 59-2 A. Variety of instruments to reduce the calcaneus after fracture. B. Böhler traction frame for fracture correction.
|
dissatisfied with both nonoperative management and delayed
reconstruction of these fractures and published his results of
operative treatment for acute displaced intra-articular calcaneal
fractures in 1948. Based on his understanding of the works of Lenormant
and others, and through a lateral approach, he stabilized the lateral
articular fragment with bone graft because he did not use screws. He
reported good results and stated that many of his patients were able to
return to work. Similar results were reported by Essex-Lopresti62 in 1952, who clearly stated that joint-depression-type fractures required formal open reduction and internal fixation (ORIF).
but because subtalar fusion was the easiest to perform, it became the
most commonly practiced treatment. In Canada, many of these patients
were subsequently evaluated in long-term follow-up by Lindsay and Dewar.129
Despite the fact that more than 50% of their patients were lost to
follow-up, their results indicated that primary subtalar fusions were
being unnecessarily performed, that operative intervention had many
complications,
and
that the best results occurred in patients treated nonoperatively. As a
result, operative treatment of acute calcaneal fractures once again
fell into disfavor, both in the United States and elsewhere, and during
the 1960s and 1970s most authors continued to advocate nonoperative
treatment.4,35,114,141,160,182
Over the past 25 years, however, marked advances in anesthesia,
prophylactic antibiotics, CT scanning, and fluoroscopy have allowed
surgeons to improve outcomes when operating on fractures,186 and these techniques have been applied to calcaneal fractures as well.*
Overall, operative treatment of acute fractures has become the standard
of care for many authors who, critically evaluating their results, have
concluded that good outcomes are possible. Despite these improvements,
it is recognized that operative treatment still requires an experienced
surgeon and that complications may occur.
typically the result of high-energy trauma, such as a fall from a
height or a motor vehicle accident. The pattern of fracture lines and
extent of comminution are determined by the position of the foot, the
amount of force, and the porosity of the bone at the time of impact.
Although controversy remains as to the exact mechanism of injury, there
is a general consensus among most authors.33,62,129,159,221
believed the primary fracture line was initially produced laterally by
the lateral process of the talus and the lateral edge of the talus, and
then extended medially. He believed that at the moment of impact, the
subtalar joint was forced into eversion, thus dividing the lateral wall
and body of the calcaneus at the crucial angle of Gissane. The
remaining force then dissipated into the sustentaculum medially. With
continuation of the force, the fracture line could exit through the
anterior process or calcaneocuboid joint, resulting in an anterolateral
fragment. A secondary fracture line was created with increased force.
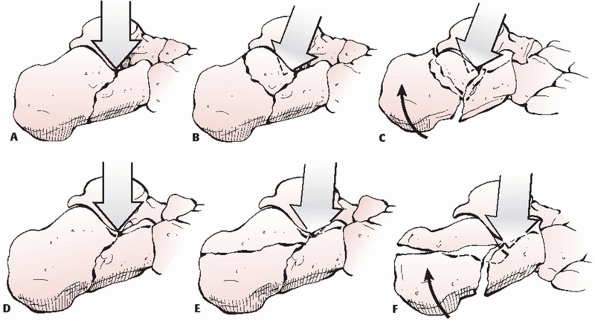
If the force was directed posteriorly, the fracture would continue both
posterior to and into the posterior facet, thereby producing a
joint-depression-type fracture. If the force was directed axially, a
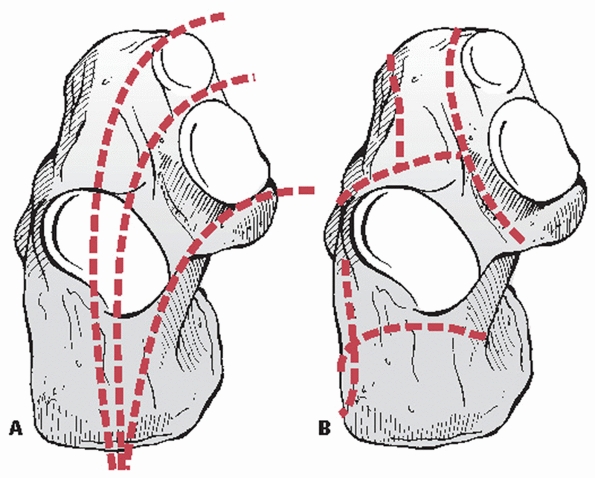
tongue-type fracture was produced (Fig. 59-3).
 |
|
FIGURE 59-3 Mechanism of injury according to Essex-Lopresti. (A-C) Joint depression. (D-F) Tongue.
|
reported on experimentally created, intra-articular calcaneal fractures
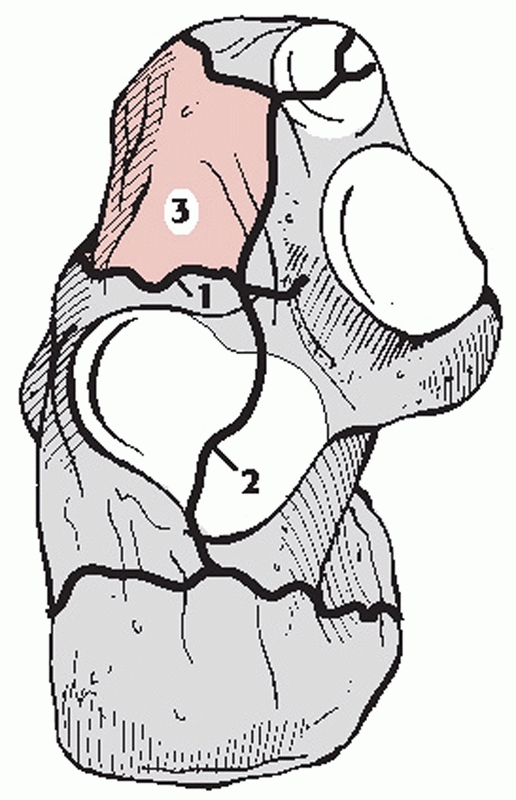
in a cadaveric model. Two primary fracture lines were identified. One
fracture line divided the calcaneus into medial and lateral portions,
with the fracture either extending into the calcaneocuboid joint or
exiting in the anterior facet. The second primary fracture line divided
the calcaneus into anterior and posterior portions, beginning laterally
at the angle of Gissane and extending medially (Fig. 59-4).
This second fracture line often continued medially to divide the middle
facet; laterally, the fracture line extended inferiorly, either toward
the plantar surface or anteriorly. These two primary fracture lines
produced a combination of fracture patterns, including both tongue-type
and joint-depression-type fractures, as well as the commonly observed
anterolateral and superomedial fragments, thus confirming the work of
Essex-Lopresti and others.62,203,244
soft tissue disruption are proportional to the amount of force and
energy involved in producing the injury. Lower-energy injuries with
minimal force produce only mild swelling and ecchymosis,
while
higher-energy injuries result in severe soft tissue disruption and may
result in an open fracture. Patients typically experience severe pain
overlying the fracture, which is related to the extent of bleeding into
the tightly enveloped soft tissue surrounding the heel. Several hours
following the injury, soft tissue swelling in the hindfoot is typically
so severe that a distinct lack of skin creases in the area is noted.
 |
|
FIGURE 59-4 Mechanism of injury according to Carr.33
|
The blister results from a cleavage at the dermal-epidermal junction,
and the fluid within the blister represents a sterile transudate. The
fluid remains clear if the dermis retains some epidermal cells. The
fluid becomes bloody if the dermis is completely devoid of epidermal
cells.77 Giordano76
prospectively evaluated various treatment methods for blister
management, including aspiration of the blister, unroofing the blister
with subsequent application of Silvadene cream or coverage with a
nonadherent dressing, or leaving the blister intact and covered by
loose gauze or exposed to air. Although there was no significant
difference in the outcome of the various soft tissue management
techniques, wound healing complications developed in 2 patients who had
incisions through blood-filled blisters. Additionally, Varela et al.232
retrospectively reviewed 53 cases and identified two cases with major
wound infections secondary to incisions passing through the blister.
They noted colonization with normal skin flora in 11 ruptured vesicles
soon after rupture of the blister, which persisted until
re-epithelialization of the area. Thus, surgical incisions should be
modified to avoid areas of blistered skin.
 |
|
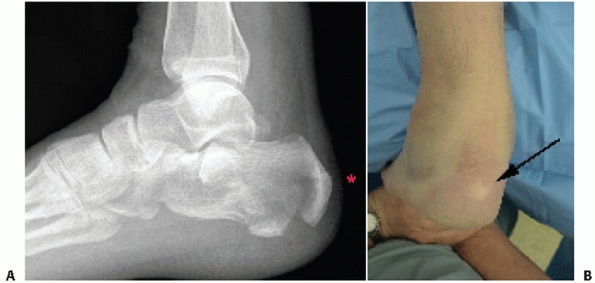
FIGURE 59-5 A. Tongue-type fracture. Note how close the tuberosity is to the skin (asterisk). B. Clinical photograph showing pressure on posterior heel.
|
lateral, central, and interosseous compartments. The central
compartment is divided into two separate compartments by a transverse
septum in the hindfoot: the superficial compartment containing flexor
digitorum brevis muscle, and the deep or calcaneal compartment
containing the quadratus plantae and the lateral plantar nerve.63 The calcaneal compartment communicates directly with the deep posterior compartment of the lower leg.136
The long-term sequelae of an unrecognized compartment syndrome in the
foot can include clawtoe deformities with permanent loss of function,
contracture, weakness, and sensory disturbances.
within a closed fascial space affects pulse pressure such that arterial
flow is decreased. This classically produces pain out of proportion to
the injury, not unlike that typically associated with a calcaneal
fracture. Thus, care must be taken to ensure that the severe pain
associated with the fracture is not caused by a compartment syndrome of
the foot, particularly in the calcaneal compartment. A self-contained
needle manometer system (Quikstik; Stryker, Kalamazoo, MI) is most
commonly used to measure compartment pressures. Most authors recommend
fasciotomy when the compartment pressure rises to within 10 to 30 mm Hg
of the patient’s diastolic pressure.63,152,155
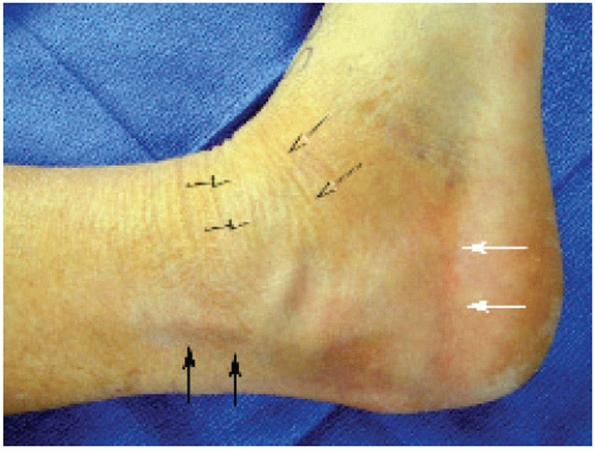
pressure on the posterior skin may occur, causing necrosis if left
untreated. Gardner et al.71 recently
presented a series of 137 tongue fractures with 21 cases exhibiting
posterior skin necrosis. In those fractures treated emergently with
percutaneous reduction, soft tissue compromise did not occur. The
authors concluded that because of the high incidence of posterior skin
compromise in tongue-type calcaneus fractures, consideration should be
given to immediate percutaneous reduction, plantarflexion splinting,
and close monitoring (Fig. 59-5).
 |
|
FIGURE 59-6 Gustilo type IIIB open calcaneal fracture.
|
They are generally associated with a higher complication rate than
their closed counterparts, including deep infection, osteomyelitis, and
possible need for amputation.15,127,153,158,190 Coughlin,42
in a review of calcaneal fractures in industrial workers, also found
that open fractures were associated with increase in the total cost of
treatment and time off from work.
reported wound complications in 13 of 18 open calcaneal fractures that
were operatively treated (72%) and calculated that patients with an
open fracture were 2.8 times more likely to develop a wound
complication than those with a closed fracture. The incidence of these
major complications also seems to increase with increasing severity of
the soft tissue injury. Siebert et al.198
reviewed the results of 36 open intra-articular fractures treated with
internal fixation with an average follow-up of 44 months. Nine of 15
(60%) type III open fractures developed osteomyelitis, resulting in
five amputations. Aggressive surgical treatment of the soft tissue
envelope and nonoperative management of the open fracture were
recommended.
reported on the results of 43 open fractures in 42 patients managed
according to a standard treatment protocol of immediate intravenous
antibiotics, aggressive surgical débridement of the wound, and
provisional limb stabilization. There were many injuries that defied
classification because of the irregular shape and size of the wound.
Definitive soft tissue coverage was completed at an average of 10.6
days; final fracture stabilization was delayed until the wound was
clean and soft tissue swelling had dissipated. All Gustilo type I open
fractures, and Gustilo type II open fractures with a medial wound, were
treated with ORIF and a lateral incision after debridement and when
tissue edema had resolved. Gustilo type II fractures with lateral,
posterior, or plantar wounds and Gustilo type IIIA fractures had
limited or no internal fixation. All Gustilo type IIIB open fractures
required vascularized free tissue transfer as soon as possible. The
overall infection rate was 37%, and osteomyelitis developed in 19%,
including 7 of 26 (27%) type III open fractures. All six amputations
occurred in patients with open type IIIB fractures. The authors
concluded that the degree of soft tissue injury was the most important
variable in predicting outcome; thus, all open type I and those open
type II fractures with a medial wound could be treated by delayed ORIF
once the soft tissues were suitable for surgery. They recommended
either external fixation or limited percutaneous fixation for those
open type II injuries with nonmedial wounds and all open type IIIA
wounds and delayed or late reconstruction for all open type IIIB wounds
and for fractures caused by penetrating trauma.
reviewed the results of 19 open calcaneal fractures treated by a
similar standard protocol at an average follow-up of 26.2 months.
Definitive fracture stabilization was completed through a lateral
approach, regardless of wound location, at an average of 7 days
following injury, at which point soft tissue swelling had adequately
dissipated. Two of 19 patients (10.5%) developed a deep infection and
subsequent osteomyelitis: one open type II fracture and one open type
IIIC fracture, the latter being the only one that went on to
amputation. Their results confirmed that open type I fractures had a
predictably good outcome with respect to soft tissue infection or
osteomyelitis, while the open type II and type III fractures were
associated with a less predictable outcome, although the overall
complication rate was considerably lower than most reported series to
date.
reviewed the results of 30 open fractures in 29 patients managed with a
standard open fracture protocol and various methods of fracture
treatment. There were 2 Sanders type II, 6 type III, and 6 type IV
fractures. There were 5 Gustilo type I fractures, 12 type II fractures,
and 13 type III fractures (9 IIIA, 2 IIIB, and 2 IIIC injuries). Most
of the open wounds occurred along the medial foot25
with two posterior injuries and three plantar wounds. There were no
lateral open wounds. Two patients with Gustilo type IIIC injuries
underwent a below knee amputation within the first 24 hours postinjury
because of massive crush injuries and dysvascular feet. Only five
fractures underwent acute ORIF. Functional outcome was evaluated using
validated assessment tools. Although the authors reported only one
superficial infection and no cases of deep infection or osteomyelitis,
most patients had only fair to poor functional results. Those with
plantar wounds had significantly worse functional outcomes relative to
those with medial wounds. They concluded that aggressive débridement of
open wounds with provisional stabilization of the limb was critical in
limb salvage, and based on their five cases, that delayed ORIF was a
safe treatment option.
more than 80% of the wounds were medial injuries, with 23% of these
associated with a significant neurovascular deficit. Five patients
required a free-tissue transfer, while two patients underwent
below-the-knee amputations as the primary treatment. The authors
stressed the need for soft tissue management and delay of definitive
internal fixation.
reviewed the results of 39 open calcaneal fractures in 38 patients
treated by open reduction and rigid internal fixation through an
extensile lateral approach as part of a large series of calcaneal
fractures. Their series included 19 open Gustilo84
type IIIA and 3 open Gustilo type IIIB fractures. Although wound
location data were not included, they reported only a 7.7% “serious”
wound complication rate, and none required amputation. They concluded
that
patient noncompliance was the single biggest issue precluding wound healing.
 |
|
FIGURE 59-7 Neutral triangle.
|
puncture wound medially from a spike of bone protruding from the medial
wall of the calcaneus or may present with a more substantial wound with
significant soft tissue disruption, typically laterally. When a
calcaneal fracture is associated with an injury to the soft tissue
envelope, it is important to categorize the wound, noting its size and
location as well as its Gustilo type.84,85
The fracture is then classified, and together these factors can give
the surgeon an estimation of the severity of the injury and its
eventual outcome, as all of these factors play a role in prognosis.5,12,14,94,117
saline and débridement of the wound with stabilization of the fracture
to protect the soft tissues. When in doubt regarding the degree of soft
tissue trauma, closed reduction and percutaneous stabilization may be
performed to realign the extremity. This may be with Kirshner wires
(K-wires), an external fixator, or both. Standard antibiotic
prophylaxis is begun, and subsequent treatment must be tailored to the
injury, but early and aggressive internal fixation should be avoided as
the additional operative trauma will compromise the limb, and
amputation may result.175 Three or
more months may be required to allow the soft tissues to heal
sufficiently before surgical salvage can be contemplated, and these
subsequent procedures are invariably for treatment of a severe
calcaneal malunion.
 |
|
FIGURE 59-8 Anatomic angles for evaluation of surgical reduction. A. Gissane angle. B. Böhler angle.
|
other associated injuries, including lumbar spine fractures or other
fractures of the lower extremities, and intuitively these associations
are more common in higher-energy trauma.35,62,182 Thordarson150
estimated that 10% of patients with calcaneus fractures also have
lumbar spine fractures, and 25% have associated lower extremity
injuries. Thus, a high index of suspicion must be maintained for these
associated injuries, and appropriate diagnostic evaluation should be
completed where necessary.
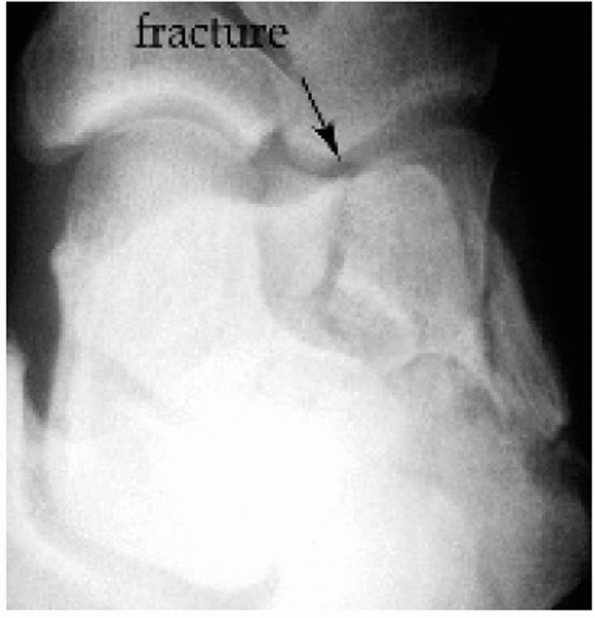
a suspected calcaneal fracture includes a lateral radiograph of the
hindfoot, an anterior posterior radiograph of the foot, a Harris heel
view, and an ankle series. In this way, all fractures, subluxations,
and/or dislocations can be diagnosed. Because of the association with
lumbar spine fractures, routine lumbar spine radiographs should also be
obtained.95 If the radiographs
reveal an intra-articular component to the calcaneal fracture, computed
tomography (CT) scanning is indicated. Multiple radiographic
projections have been described; however, most of these views are hard
to read and even more difficult to consistently reproduce.7,103,203,233 In contrast, CT evaluation, when interpreted correctly, provides a wealth of data for both diagnosis and treatment.
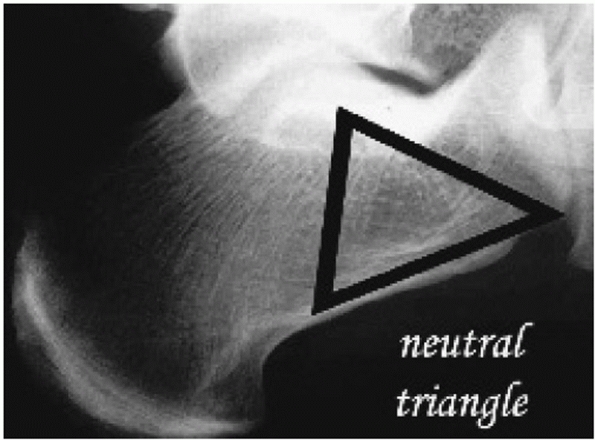
the inferior cortex of the calcaneus combine with compression
trabeculae supporting the posterior and anterior articular facets. The
area between these trabeculae creates a space known as the neutral triangle90 (Fig. 59-7).
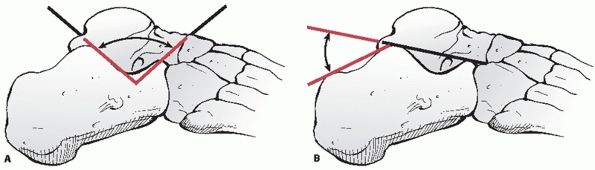
The lateral radiograph of the hindfoot demonstrates two important
angles: the tuber angle of Böhler and the crucial angle of Gissane (Fig. 59-8). The tuber angle of Böhler
is composed of a line drawn from the highest point of the anterior
process of the calcaneus to the highest point of the posterior facet
and a line drawn tangential to the superior edge of the tuberosity.18
The angle is normally between 20 and 40 degrees; a decrease in this
angle indicates that the weight-bearing posterior facet of the
calcaneus has collapsed, thereby shifting body weight anteriorly.
McLaughlin141 determined that
reduction or reversal of this angle indicates only the degree of
proximal displacement of the tuberosity and thus can be decreased in
both intra- or extra-articular fractures, limiting
its usefulness.210 The crucial angle of Gissane
is formed by two strong cortical struts extending laterally: one along
the lateral margin of the posterior facet and the other extending
anterior to the beak of the calcaneus. These cortical struts form an
obtuse angle62 and are visualized directly beneath the lateral process of the talus.194
 |
|
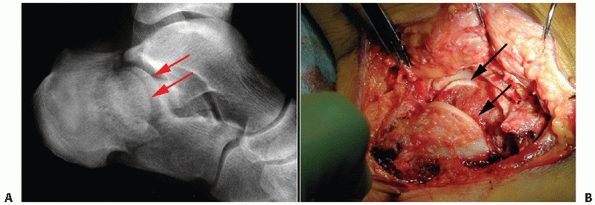
FIGURE 59-9
The “double density”; a joint-depression-type fracture where the lateral portion of the joint is impacted but both Böhler and Gissane angles are normal. A. Lateral radiograph. B. Intraoperative correlation. |
calcaneal fracture. Radiographs of intra-articular fractures usually
show a loss in the height of the posterior facet, with a decrease in
the angle of Böhler and an increase in that of Gissane, but only if the
entire facet is separated from the sustentaculum and depressed. If only
the lateral half of the posterior facet is fractured and displaced, a
split in the articular surface will be seen as a “double density” and
Böhler’s and Gissane’s angles may appear to be normal189 (Fig. 59-9).
The articular surface can be found within the body of the calcaneus;
usually, it is rotated 90 degrees in relation to the remainder of the
subtalar joint. The lateral radiograph also indicates whether the
fracture is of the joint-depression- or tongue-type according to the
classification of Essex-Lopresti.62
radiograph of the foot shows extension of the fracture line into the
calcaneocuboid joint (Fig. 59-10). This
radiograph provides very little information and usually may be omitted.
The Harris axial radiograph of the heel allows visualization of the
joint surface as well as loss of height, increase in width, and
angulation of the tuberosity fragment (Fig. 59-11). Unfortunately, this radiograph is very difficult to obtain in the acute setting because of pain.
 |
|
FIGURE 59-10 Anteroposterior view of the foot showing the calcaneocuboid joint.
|
additional information when CT is available, and they expose the
patient to increased doses of radiation.86 Deutsch et al.50 pointed out that tomograms may fail to show the extent of articular incongruity.
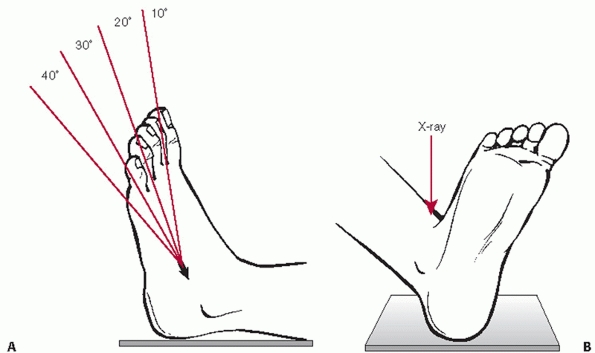
demonstrating the articular surface of the posterior facet on plain
radiographs.24 This view, known as
Broden Projection I, is obtained with the patient supine and the x-ray
cassette under the leg and the ankle. The foot is in neutral flexion,
and the leg is internally rotated 30 to 40 degrees. The x-ray beam then
is centered over the lateral malleolus, and four radiographs are made
with the tube angled 40, 30, 20, and 10 degrees toward the head of the
patient. These radiographs show the posterior facet as it moves from
posterior to anterior; the 10-degree view shows the posterior portion
of the facet, and the 40-degree view shows the anterior portion. While
this view is difficult to explain to, and
obtain from, a technician, a mortise view of the ankle will recreate this view perfectly (Fig. 59-12).
Therefore, an ankle series should be requested. Furthermore, this view
should be obtained intraoperatively using the fluoroscope and is
indispensible to verify the reduction of the articular surface.113
 |
|
FIGURE 59-11 Harris axial view of the heel.
|
 |
|
FIGURE 59-12 Broden view of the subtalar joint. A. Correct way to obtain view. B. Simplest way to obtain view is by taking a mortise view of the ankle. Note intraarticular fracture of the calcaneus (arrow). (A, Redrawn from Burdeaux BD Jr. The medical approach for calcaneal fractures. Clin Orthop Relat Res 1993;290: 96-107.)
|
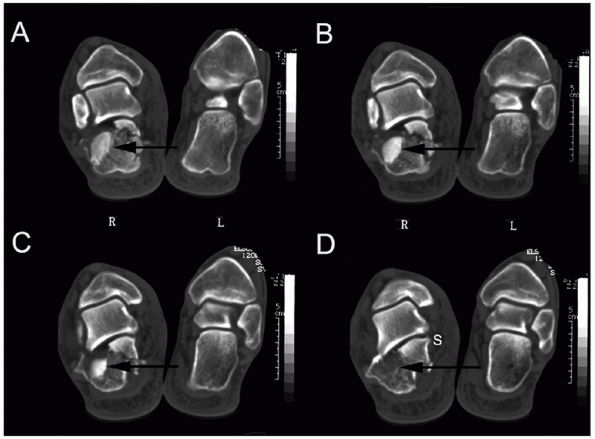
calcaneal fractures and has subsequently allowed for consistent
analysis of treatment results.* CT images are obtained in
the axial, 30-degree semicoronal, and sagittal planes. The coronal
views provide information about the articular surface of the posterior
facet, the sustentaculum, the overall shape of the heel, and the
position of the peroneal and flexor hallucis tendons. The axial views
reveal information about the calcaneocuboid joint, the anteroinferior
aspect of the posterior facet, and the sustentaculum. Sagittal
reconstruction views provide additional information as to the posterior
facet, the calcaneal tuberosity, and the anterior process (Figs. 59-13 and 59-14).
 |
|
FIGURE 59-13 Axial (coronal) CT scan views of the calcaneus. Note that the lateral fragment (arrow) gets smaller and rotates, as the sections move from posterior (A) to anterior (D). S, sustentaculum.
|
articular surface was not sufficient to assist in preoperative planning or to justify the costs. Vannier et al.231 concluded that the diagnostic value of three-dimensional CT was equivalent to that of conventional two-dimensional CT.
 |
|
FIGURE 59-14 Transverse CT scan sections showing lateral fragment (white arrow) rotated such that joint surface is parallel to calcaneocuboid joint (black arrow). *, Anterolateral wall fragment.
|
calcaneal fractures has contributed to the difficulty in treating these
injuries. Classification systems are designed to facilitate
communication among surgeons, plan operative procedures, and assist in
determining outcomes. Historically, calcaneal fracture classification
systems based on plain radiographs existed but were of limited use.62,159,182,233,237
With the advent of CT scanning, standardization of imaging techniques
has allowed for the development of modern classification systems, which
has greatly enhanced the management of calcaneal fractures.
popularized the concept of two distinct fracture patterns: a
tongue-type fracture, where the articular fragment remained attached to
a tuberosity fragment, and a joint-depression-type fracture, in which
the articular fragment was separate from the adjacent tuberosity. The
advantage of this distinction was that the surgeon could accurately
choose the correct treatment method. Unfortunately, this classification
provided little prognostic information. Several other authors described
fracture patterns and classifications, but these systems were in
essence variations of the Essex-Lopresti classification.8,72,233,237
reported on a new classification system, which was uniquely based on
the number of articular bony fragments as determined on
anteroposterior, lateral, and Harris axial heel views. First-degree
fractures were nondisplaced shear-type fractures with widening of the
joint surface. Second-degree fractures included secondary fracture
lines, resulting in a minimum of three fragments, two of which included
the articular surface. Third-degree fractures were highly comminuted
such that they could not be classified, and therefore the authors
could
not specify if the comminution referred to the body or the articular
surface of the posterior facet. Although they proposed that displaced
intra-articular fractures should be managed surgically with internal
fixation, their results could not be correlated to their classification.
however, were the first to apply information provided on CT evaluation
into a rational understanding of the injury. In his classification, the
entire calcaneus was considered, with a total of five possible
fragments, similar to the systems of Essex-Lopresti and Soeur and Remy,
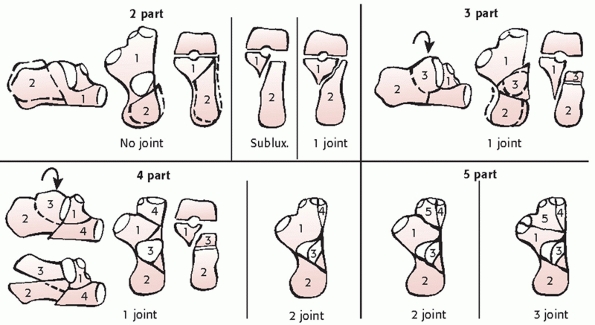
but based on CT scan data62,203 (Fig. 59-15). Although surgical outcomes were evaluated, no prognosis based on fracture classification was made.
were the first authors to correlate clinical outcome (albeit as a
result of nonoperative treatment) with a fracture classification system
based on CT evaluation. They divided their fractures into three types
based on the articular surface displacement: type I, nondisplaced; type
II, displaced; and type III, comminuted. Subsequently, Sanders
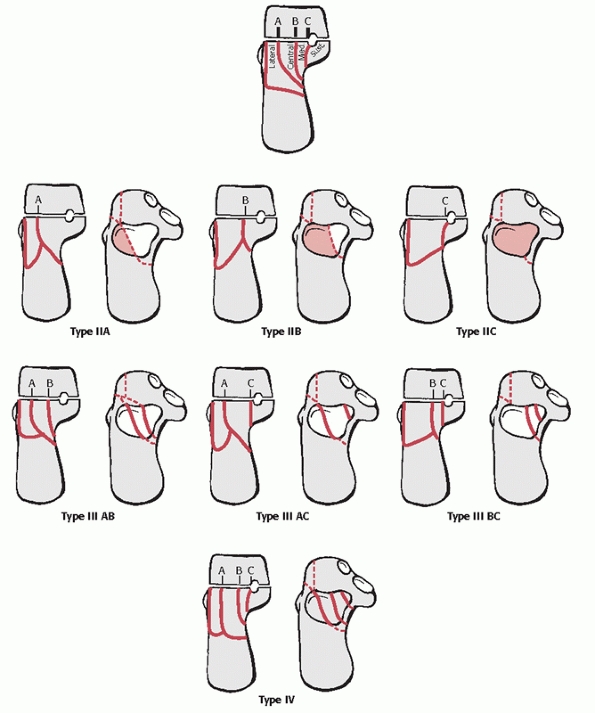
developed a scan classification system based on the number and location
of articular fracture fragments alone.187,190 This was the natural progression of fracture patterns identified by Soeur and Remy.203 The classification was found to be useful in determining both treatment methods and prognosis after surgical fixation.190 Many additional authors have since used this classification and found it to be prognostic with respect to outcome as well.* During the analysis of the results of operative treatment, it became clear to Sanders et al.190
that the body of the calcaneus could be restored surgically to virtual
anatomic shape by using a lateral approach, regardless of the degree of
comminution. Because the prognostic factor for outcome was the
articular reduction and the degree of cartilage damage, the
classification has been purposely limited to articular displacement.
 |
|
FIGURE 59-15 Zwipp CT scan classification of calcaneal fractures.
|
Although all coronal sections were analyzed, the original
classification arbitrarily used one CT scan view with the widest
undersurface of the posterior facet of the talus (in reality, the
entire CT scan should be evaluated to watch fracture lines move in and
out of plane, and to determine which are artifact, and which are real).
The talus was divided into three equal columns by two lines that were
then extended across the calcaneal posterior facet; with the addition
of a third line, just medial to the medial edge of the posterior facet,
the posterior facet of the calcaneus could be arbitrarily divided the
into three potential fragments: medial, central, and lateral. These
fragments plus the sustentaculum resulted in a total of four potential
articular pieces. All nondisplaced articular fractures (less than 2
mm), regardless of the number of fracture lines, were considered type I
fractures; type II fractures were two-part fractures of the posterior
facet. Three types—IIA, IIB, and IIC—existed, based on the location of
the primary fracture line. Type III fractures were three-part fractures
that usually featured a centrally depressed fragment. Types included
IIIAB, IIIAC, and IIIBC, and again were based on the location of the
primary fracture line. Type IV fractures, or four-part articular
fractures, were highly comminuted and often had more than four
articular fragments. While the subclassification of articular fracture
lines by medial to lateral location is important prognostically, most
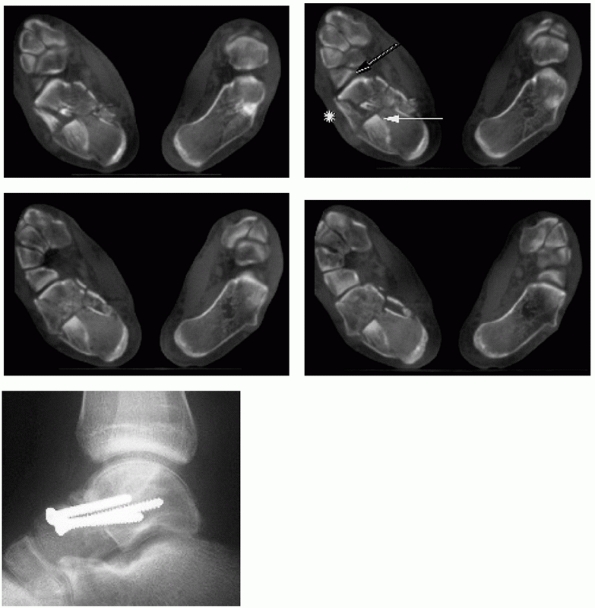
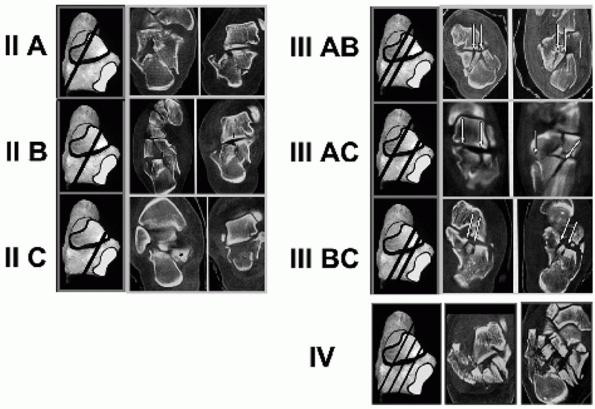
surgeons simply identify the number of articular fragments171 (Fig. 59-17).
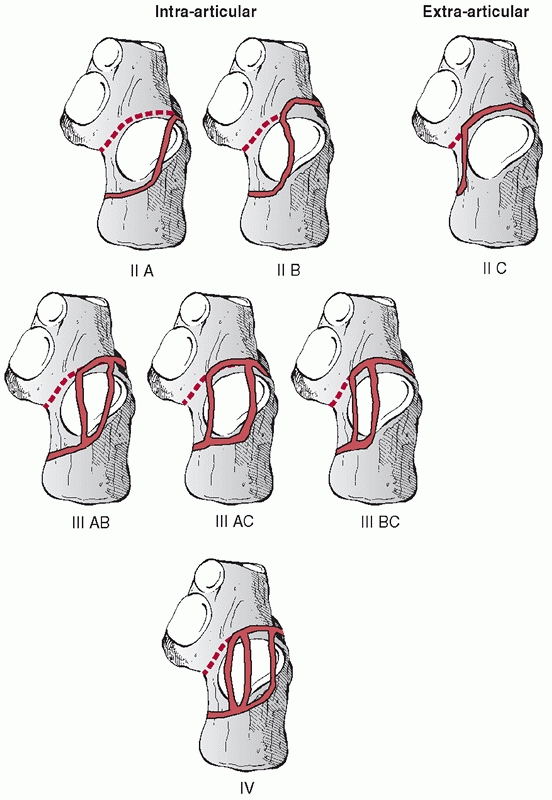
depression fractures exclusively. With the addition of the initial
lateral radiograph, however, the surgeon can determine whether the
fracture is a joint-depression- or a tongue-type fracture. Once this is
established, tongue-type fractures can be classified using this system
as well. The true extra-articular tongue is typically a type IIC, where
the entire facet is displaced but intact. If the tongue fracture
extends intra-articularly, the fracture is typically a type IIB. In
addition, tongue-type fractures with joint-depression components (mixed
fractures) can clearly be evaluated using this CT scan classification.
It is important to understand and identify these tongue variants, as
the treatment methods will be dictated by the presence or absence of an
intraarticular component (Figs. 59-18 and 59-19).
 |
|
FIGURE 59-16
Sanders CT scan classification of calcaneal fractures. (Redrawn from Sanders R. Displaced intra-articular fractures of the calcaneus. J Bone Joint Surg Am 2000;82A:225-250, with permission.) |
These typically mirror the lines that divide the articular surface and
are best seen on the transverse CT scan. Importantly, they reaffirmed
the need to obtain an anatomic reduction of the body of the calcaneus
as well as the joint. Finally, on the
transverse
CT scan, a medial-to-lateral extra-articular fracture at the level of
the anterior edge of the posterior facet can often be seen, as
originally described by Carr.33
This fracture line is important to find, as its presence indicates that
the medial component of the joint can be rotated in a plantar direction
and must be brought out from under the anterior process to obtain an
anatomic joint reduction. It is our belief that the main limitation of
this classification, as well as all CT scanning at the present time
(even with the advent of reformatting techniques), is that it cannot
determine whether the sagittally split fragment is additionally
fractured in the coronal plane. Often, this cannot be determined until
the fracture is surgically treated, and occasionally not until the
fragment separates while being repositioned.
 |
|
FIGURE 59-17 CT scans of various fracture patterns according to Sanders.
|
surface consists of three articular facets—the anterior, middle, and
posterior facets that articulate with the talus. The posterior facet is
the major weight-bearing surface and the largest facet. The middle
facet is anterior and medial, and located on the sustentaculum; it is
often contiguous with the anterior facet. The sustentaculum sits under
the talar neck and is medial to the calcaneal body. It is attached to
the talus by the interosseous talocalcaneal ligament and by the deltoid
ligament medially. The flexor hallucis longus tendon runs below the
sustentaculum. Laterally, the peroneal tendons run obliquely along the
lateral wall of the calcaneus and sit in two shallow grooves, with a
bony prominence between them known as the peroneal tubercle. The entire
calcaneal surface behind the posterior facet is known as the posterior
tuberosity. On its plantar surface, it has two processes: the lateral
and medial. The lateral process is the origin of the abductor digiti
quinti (minimi) muscle. The medial process is the origin of the
abductor hallucis muscle and the major weight-bearing structure in the
hindfoot. Finally, the Achilles tendon inserts on the posterior surface
of the tuberosity.
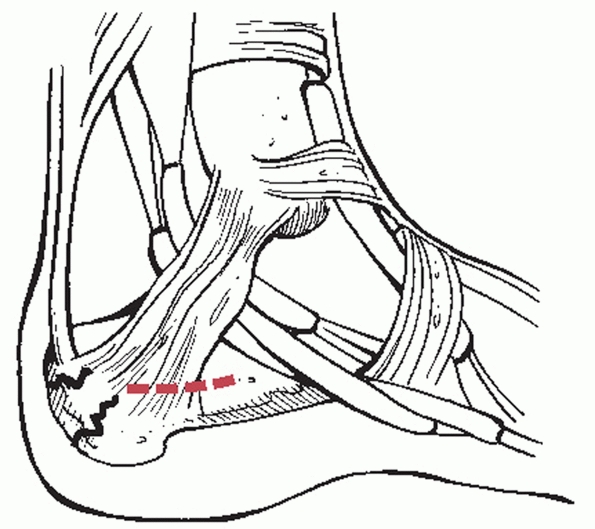
and consists of a 2- to 3-inch incision in the midportion of the medial
side of the heel, between the plantar surface and the medial malleolus,
and in line with the longitudinal axis of the os calcis (Fig. 59-21).
The incision should be centered over the site of medial displacement
and therefore may shift either anteriorly or posteriorly, based on the
fracture. The fascia is incised in line with the skin incision, with
care being taken to locate and then avoid the neurovascular bundle.
After the bundle is identified and retracted with the use of a
Penrose-type drain, the muscle of the quadratus plantae and the
abductor hallucis longus are separated down to the medial wall of the
calcaneus, and a reduction of the body is then performed.143,227 This approach was modified by Johnson,106
who developed a vertical incision, posterior to the neurovascular
bundle. This incision was directed halfway between the medial malleolus
and the Achilles tendon, and once the bundle was exposed, it could be
retracted forward to expose the fracture. The medial plantar nerve had
to be protected to avoid damage in the plantar aspect of the wound.
Zwipp and Tscherne242 published another modification that essentially combined these two approaches (Fig. 59-22).
This approach paralleled the neurovascular bundle in a large J-type
incision, much like an extended tarsal tunnel exposure. Once the nerve
and its plantar branches were identified, exposure of the fracture
could be accomplished with ease.
 |
|
FIGURE 59-18 The tongue fractures including the intra-articular variant.
|
 |
|
FIGURE 59-19
True intra-articular tongue fracture (type IIB). Plain radiographs are unable to determine whether the fracture involves the posterior facet (A,B). Semicoronal and transverse CT scans verify intraarticular displacement (C,D). Note black arrows, indicating intra-articular fracture, and white arrows, indicating the intact lateral wall component typical of tongue fractures. |
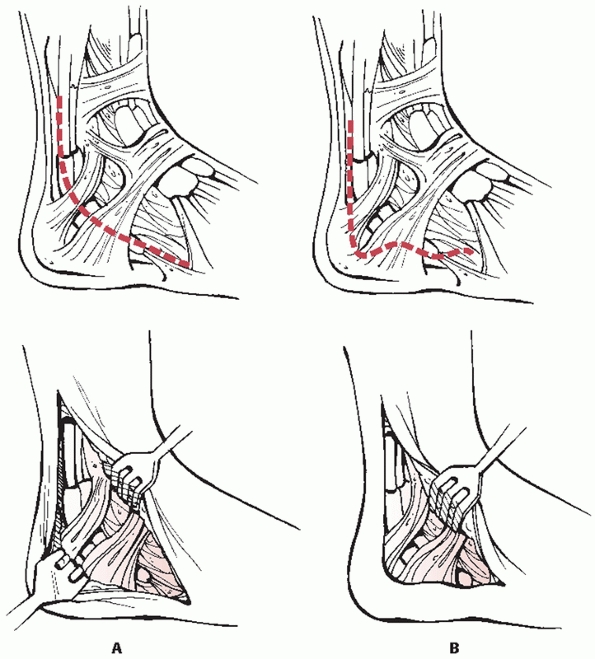
This approach offered limited access to the body of the calcaneus,
often resulted in scarring of the peroneal tendons, and frequently
damaged the sural nerve. In 1984, Fernandez64 first described the extensile posterolateral approach (Fig. 59-23A).
In this approach, an incision was made halfway between the fibula and
Achilles tendon and starting three fingerbreadths above the tip of the
lateral malleolus. This was extended around the malleolus, following
the course of the sural nerve and small saphenous vein toward the fifth
metatarsal
base.
The sural nerve was identified and protected, and then full-thickness
flaps were developed to bone. After the peroneal tendons were
dislocated over the tip of the malleolus, the calcaneofibular was cut
off the calcaneus and then retracted anteriorly such that the subtalar
joint and sinus tarsi were exposed.
 |
|
FIGURE 59-20 Miric and Patterson’s148 schematic representation of the peri-articular fracture extension lines into the anterior process (A) and around the posterior facet (B).
|
 |
|
FIGURE 59-21
Medial approach after McReynolds. (From McReynolds IS. Trauma to the os calcis and heel cord. In: Jahss M, ed. Disorders of the Foot and Ankle. Philadelphia: WB Saunders, 1984:1497-1538.) |
 |
|
FIGURE 59-22 Medial approach according to Zwipp.
|
 |
|
FIGURE 59-23 Lateral approach. A. Modified Kocher, according to Fernandez. B. Lateral approach according to Seligson. (A, Redrawn from Fernandez DL. Transarticular fracture of the calcaneus. Arch Orthop Traum Surg 1984;103:195-200. B, Redrawn from Gould N. Lateral approach to the os calcis. Foot Ankle 1984;4:218-220.)
|
The goal of the incision was to expose the entire lateral face of the
calcaneus to the level of the calcaneocuboid joint. This approach
combines the posterior approach for the ankle, described by Picot in
1924,162 with a unique plantar limb
that undulated so that the final closure could be tension free. The
incision was made just lateral to the Achilles tendon and carried
vertically to the superior pole of the calcaneus. The incision was then
curved gently following a line where the thinner skin of the lateral
side of the hindfoot met the skin of the heel pad. The incision was
carried to the base of the fifth metatarsal. The author stressed that
in the gentle curved portion of the incision, the knife should be taken
straight to bone with the skin, subcutaneous layer, and periosteum kept
as a single layer. The lateral flap was then developed as a single,
thick
flap. The peroneal tendons were subsequently elevated from the peroneal
tubercle and reflected dorsally, while the calcaneofibular ligament was
detached from the calcaneus. After subtalar capsulotomy, the entire
lateral calcaneus, calcaneocuboid, and subtalar joints were exposed.
 |
|
FIGURE 59-24
Lateral vascular anatomy. (Redrawn from Borrelli J Jr, Lashgari C. Vascularity of the lateral calcaneal flap: a cadaveric injection study. J Orthop Trauma 1999;13:73-77, with permission.) |
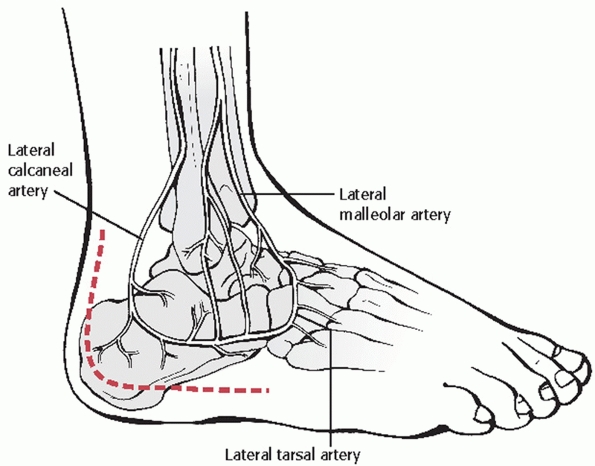
described the arterial blood supply of the subcutaneous tissues of the
lateral hindfoot and defined the relationships between these arteries
and the lateral extensile incision used for ORIF of calcaneal fractures
(Fig. 59-24). Three arteries—the lateral
calcaneal, the lateral malleolar, and the lateral tarsal artery—were
consistently found along the lateral aspect of the hindfoot. The
lateral calcaneal artery appeared to be responsible for the majority of
the blood supply to the corner of the flap and, because of its
proximity to the vertical portion of the typical incision, it appeared
most likely to be injured from inaccurate placement of the incision. As
a result of this work, and to protect the sural nerve, the authors
recommended that the vertical limb of the incision be started just
anterior to the lateral edge of the Achilles tendon and at the crease
of the heel pad and lateral foot. This study therefore supports the
original description of Seligson.82
(a) nondisplaced or minimally displaced extra-articular fractures, (b)
nondisplaced intra-articular fractures, (c) anterior process fractures
with less than 25% involvement of the calcaneocuboid articulation, (d)
fractures in patients with severe peripheral vascular disease or
insulin-dependent diabetes, (e) fractures in patients with other
medical comorbidities prohibiting surgery, and (f) elderly patients who
are household ambulators. It must be noted that chronological age is
not a contraindication to surgery, as many older patients are healthy
and active well into their 70s. Nonoperative treatment may also be
necessary when fractures are associated with (a) blistering and massive
prolonged edema, (b) large open wounds, or (c) life-threatening
injuries.
to allow dissipation of the initial fracture hematoma, followed by
conversion to a prefabricated fracture boot with the ankle locked in
neutral flexion to prevent an equinus contracture, and an elastic
compression stocking-to-minimize dependent edema. Early subtalar and
ankle joint range-of-motion exercises are initiated, and
non-weight-bearing restrictions are maintained for approximately 10 to
12 weeks, until radiographic union is confirmed.
displaced intra-articular fractures involving the posterior facet, (b)
anterior process of the calcaneus fractures with more than 25%
involvement of the calcaneocuboid articulation, (c) displaced fractures
of the calcaneal tuberosity, (d) fracture-dislocations of the
calcaneus, and (e) selected open fractures of the calcaneus. Basic
fracture patterns can be delineated with plain radiographs. A decision
can then be made regarding ancillary tests, most commonly CT scans.
Surgery should be performed within the initial 3 weeks of injury prior
to early consolidation of the fracture. Surgery should not be
attempted, however, until swelling in the foot and ankle has adequately
dissipated, as indicated by a positive wrinkle test.187
The test is performed by direct palpation and visual assessment of the
lateral calcaneal skin with dorsiflexion and eversion of the involved
foot. The test is positive if skin wrinkling is seen and no pitting
edema is evident, indicating that operative intervention may be safely
undertaken (Fig. 59-25).
the affected extremity. If the patient is seen initially in the
emergency department, immediate elevation in combination with a
Jones-type compression dressing with a posterior splint may be used,
with or without a compressive pneumatic foot pump.218 In the event of an isolated injury, the patient may be discharged
from the hospital and converted to an elastic compression stocking and
fracture boot locked in neutral flexion several days later. CT scans
and plain radiographs may be reviewed with the patient, and a
management plan outlined at that time. Full resolution of soft tissue
edema may require up to 21 days. We prefer to proceed with surgical
intervention within 2 weeks of injury, although surgery may be safely
performed up to 3 weeks from injury. Beyond this interval, early
consolidation of the fracture occurs, and the fragments become
increasingly difficult to separate and reduce. Furthermore, at the time
of attempted reduction, the articular cartilage may be left behind,
completely delaminating from the underlying subchondral bone, leaving a
facet fragment without any accompanying cartilage.
 |
|
FIGURE 59-25 Wrinkle sign. Note the wrinkling of the skin throughout (open arrows), as well as the visualization of the subluxated peroneal tendons (black arrows) and lateral edge of calcaneal heel pad (white arrows).
|
treatment of calcaneal fractures were difficult to interpret because of
inherent flaws in study design. Treatment methods, classification, and
outcome measurements were all nonstandardized, making comparison and
critical analysis difficult.* As a result, these studies
cannot be used to reach any conclusion regarding treatment or outcome,
as one would be comparing apples to oranges.188
Thus, studies published prior to the advent of CT should be considered
only from a historical perspective. Many subsequent series have been
published using modern treatment and standardized methods of outcomes
analysis. These studies can be categorized into nonoperative treatment,
studies comparing operative to nonoperative treatment, and operative
treatment.
reviewed their results of nonoperative management of calcaneal
fractures using a CT classification based on the fracture pattern
involving the posterior facet. Small or nondisplaced fractures were
classified as type I fractures, displaced fractures as type II, and
comminuted fractures as type III fractures. In their series, there were
13 type I, 10 type II, and 7 type III fractures. They reported good
results with closed treatment in all type I fractures, but poor results
in most type II and type III fractures, and suggested operative
treatment was indicated for these fractures.
reviewed fractures in 16 patients treated nonoperatively and used gait
analysis to evaluate outcome. Most patients in their series exhibited
an altered gait pattern, especially on uneven ground, thus confirming
that nonoperative management of calcaneus fractures led to at least
some persistent functional impairment.
evaluated 20 patients treated operatively over a 12-year period and
compared the results to a historical control group treated
nonoperatively over the same time period by other surgeons. They
concluded that the problems associated with internal fixation did not
justify operative treatment; however, several limitations in their
study design were apparent: only a few operative procedures were
performed each year; the surgeons did not consistently use lag screws
and never stabilized the calcaneal body with a plate or staple;
intraoperative fluoroscopy was not available; and the authors conceded
they were never able to obtain a perfect reduction. This study
illustrates many of the inherent flaws seen in the published literature
on calcaneal fractures and thus prohibits the reader from reaching
meaningful conclusions.
compared 31 displaced fractures treated nonoperatively to 25 treated
operatively. They used their own classification and fixed fractures
with K-wires through a lateral Kocher approach. No attempt was made to
reduce the calcaneal tuberosity, and they encountered difficulty in
evaluating the postoperative CT scans. Using their own scoring system,
they found no difference in clinical outcome between the two groups.
The limitations of this study include poor operative fixation
techniques and lack of assessment of the postoperative reduction by
scans.
treated 12 patients operatively and 12 patients nonoperatively. CT was
used; however, the fractures were not classified. In those treated
operatively, a Kocher incision was used with lag screw and plate
fixation. Postoperative CT evaluation was completed. Clinical outcome
was based on walking distance, subtalar motion, return to work, and
shoe size. They concluded that operative treatment was superior, but
their limited patient population precluded statistical significance.
compared 44 patients treated operatively with 19 treated nonoperatively
in a nonrandomized, retrospective study with an average follow-up of 3
years. Fractures were classified according to the Crosby and
Fitzgibbons classification. They used an extensile lateral approach,
and the reduction was held with lag screws and plate fixation. At an
average of 3-year follow-up, they reported significantly better results
in the surgical group with respect to pain, activity, range of motion,
return to work, and hindfoot swelling.
first reported on the results of nonoperative treatment of
intra-articular calcaneal fractures in 1990. Because of the poor
outcomes with the displaced and
comminuted fractures, the authors began treating displaced (type II) fractures.44,45
Results of their operative cases were then compared with their
nonoperative cases using the same outcomes assessment instrument. They
found superior results in those fractures that were treated
operatively; the difference was highly statistically significant. As a
result, they recommended operative intervention for displaced fractures.
performed a randomized, prospective trial comparing operative to
nonoperative treatment in 30 patients. Fractures were classified by CT,
and only Sanders type II and III (displaced) fractures were included in
their study. Nonoperative treatment consisted of non-weight-bearing and
early range-of-motion exercises. Operative treatment was performed by a
single surgeon and consisted of an extensile lateral approach with lag
screw and plate fixation. Clinical outcome using the American
Orthopaedic Foot and Ankle Society (AOFAS) Ankle and Hindfoot Score111
was completed in all 15 operatively treated fractures and in 11 of 15
nonoperatively treated fractures. The functional results and overall
outcome in the operatively treated group were superior to those in the
nonoperative group; the differences were statistically significant.
Despite small numbers and a relatively short period of follow-up, this
study represented the first randomized, prospective trial where many
variables were held constant, and this study confirmed that operative
intervention could lead to superior results.
first reported their matched cohort series of 34 calcaneal fractures in
1992. Seventeen fractures were treated operatively, and 17 were treated
nonoperatively. The patients were matched with respect to age, sex,
work type, and time to follow-up. They concluded that their best
results were in patients with an anatomic reduction of the posterior
facet and that, if an anatomic reduction was not possible, there
appeared to be no difference between operative and nonoperative
treatment. Unfortunately, no classification was performed, such that
fractures were not consistently classified. More important, 12
different surgeons participated in surgical treatment of the 17
patients, and all used different techniques.
performed a meta-analysis of articles between 1980 and 1996 dealing
with calcaneal fractures. Of the 1845 articles, 6 compared operative
versus nonoperative treatment for displaced calcaneal fractures using
the minimum criteria for inclusion in the meta-analysis. A statistical
summary of information across the six articles revealed a trend for
surgically treated patients to be more likely to return to the same
type of work as compared with nonoperatively treated individuals. There
also was a trend for nonoperatively treated patients to have a higher
risk of experiencing severe foot pain than did operatively treated
patients. Unfortunately, none of the other outcomes could be summarized
formally across studies using statistical techniques because of
variability in reporting across studies. Although the tendency was
always for operatively treated patients to have better outcomes
(reaching statistical significance in some of the articles), the
strength of evidence to recommend operative treatment for displaced
intra-articular calcaneal fractures remained weak.
Trauma Society performed a prospective, randomized, multicenter trial
and compared operative with nonoperative treatment of displaced
intra-articular calcaneal fractures in 424 patients with 471 fractures.28
Two hundred and eighteen patients with 262 fractures were treated
nonoperatively; 206 patients with 249 fractures underwent operative
treatment through an extensile lateral approach with screw, plate, or
wire fixation. Seventy-three percent of patients were followed for a
minimum of 2 years, with an average of 3 years. Fractures were
classified according to Sanders, and outcomes were evaluated using two
separate previously validated assessment tools. Analysis revealed
significantly better results in certain fracture groups undergoing
operative treatment, including women, younger patients, patients with a
lighter workload, patients not receiving Worker’s Compensation,
patients with a higher initial Böhler angle (less severe initial
injury), and those with an anatomic reduction on postoperative CT
evaluation. There was no difference in overall outcome between the
operative and nonoperative groups; however, those having nonoperative
treatment of their fracture were 5.5 times more likely to require a
subtalar arthrodesis for posttraumatic arthritis than those undergoing
operative treatment.
recently reported on a matched cohort study comparing patients who had
undergone initial ORIF and subsequently developed posttraumatic
arthritis requiring an in situ fusion with patients treated
nonoperatively who developed a calcaneal malunion and required a late
reconstruction and subtalar arthrodesis. The ORIF group included 36
feet in 34 patients with an average follow-up of 2.7 years. The average
interval from ORIF to late subtalar arthrodesis was 22 months, and 33
of 36 arthrodeses (91.7%) achieved initial union. The calcaneal
malunion group included 45 feet in 40 patients with an average
follow-up of 5.3 years.37 The
average interval from fracture to late reconstruction was 16.4 months,
and 37 of 40 arthrodeses (92.5%) achieved initial union. There was a
statistical trend toward a lower wound complication rate and
significantly higher outcome scores in the ORIF group. This study
suggested that the early operative restoration of calcaneal height,
length, and overall shape is beneficial to outcome. In the event the
patient developed late posttraumatic arthritis, a simple in situ
arthrodesis could be performed.
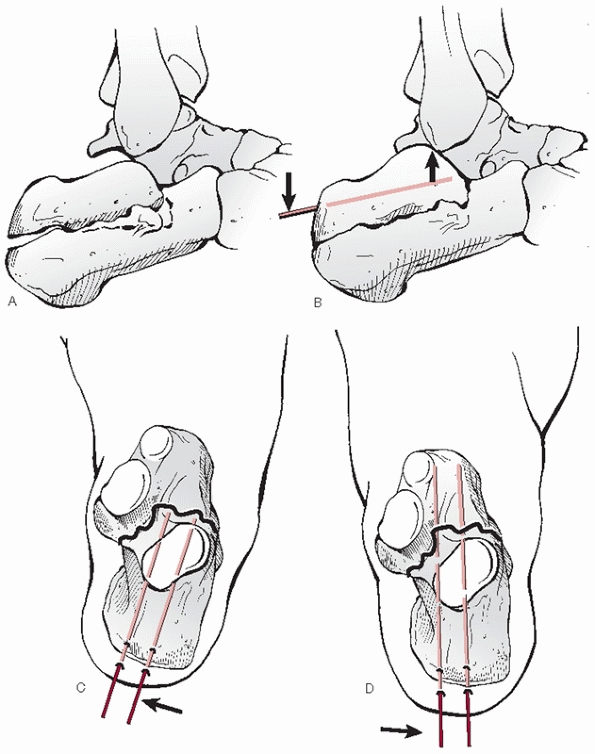
techniques for tongue-type fractures using a percutaneous “nail” were
first advocated by Westhues.236 The technique was modified by Gissane,79
who developed the Gissane Spike for this procedure. It was
Essex-Lopresti, however, who described the technique in detail and
popularized the maneuver specifically for tongue-type fractures.62
Over time, this technique was used for all types of calcaneal fractures
with poor results, and thus fell into disfavor. Recently, Tornetta224
revived the original technique, reporting on the results of 26 patients
with Sanders type IIC (extra-articular tongue-type) fractures using the
Essex-Lopresti maneuver with a modification of fixation (Fig. 59-26).
Steinmann pins were initially used for definitive fixation, but these
were changed to 6.5-mm cannulated screws later in the series. Three
patients were considered intraoperative failures, in that the technique
was abandoned in these patients in favor of traditional ORIF. The
reduction maneuver was successful in 88%. There were 86% good or
excellent results based on the Maryland Foot Score at an average
follow-up of 2.9 years.
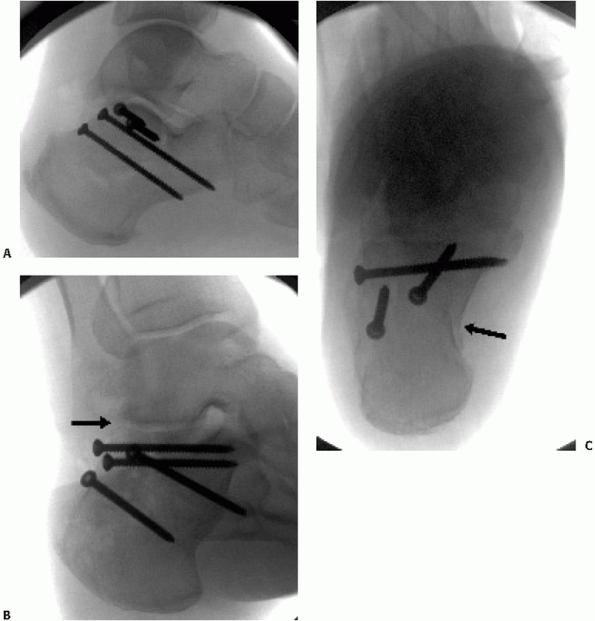
or impending soft tissue compromise from displaced fracture fragments.
Initial, closed or percutaneous reduction and external fixation
supplemented by K-wire fixation may be followed by standard open
treatment if the soft tissues are amenable within 2 to 3 weeks. For
those patients with relative contraindi-cations to open surgery, such
as heavy smokers, patients with severe peripheral vascular disease, or
patients with poorly controlled diabetes, minimally invasive approaches
may be used as definitive treatment. In general, small incisions are
used for the placement of Schantz pins and small periosteal elevators
in assisting with the reduction, followed by multiple small-fragment
screws axially and laterally (Fig. 59-27).
 |
|
FIGURE 59-26
Essex-Lopresti technique as modified by P. Tornetta, MD. Once guidepins are correctly positioned, they are exchanged for 6.5- to 8.0-mm cannulated cancellous lag screws. |
reviewed the results of 36 tongue-type calcaneal fractures managed with
a minimally invasive reduction technique and small-fragment fixation
with an average follow-up of 25.5 months. The operative technique
involved small (less than 1-cm) incisions, which were used for the
introduction of Schantz pins and small elevators for the reduction. The
fracture fragments were aligned with the Essex-Lopresti reduction
technique. All reductions were performed under fluoroscopic guidance
and were stabilized with small-fragment screw fixation. Two screws were
introduced in an axial direction, and any subsequent screws were
introduced from the lateral surface to secure the sustentaculum.
Postoperatively, patients were placed in a removable splint and range
of motion was begun postoperatively within 1 to 2 days. Weight bearing
was initiated after 2 to 3 months. There were no infections and no
cases of lost fracture reduction, and only one patient went on to
require a subtalar arthrodesis. They concluded that their technique
lowered the incidence of postoperative risks and reduced the length of
hospital stay compared to historical controls.
noted that percutaneous reduction methods play an important role in the
management of calcaneal fractures with severe soft tissue compromise,
particularly open fractures. Percutaneous reduction by pin leverage
(Westhues or Essex-Lopresti maneuver) followed by minimally invasive
screw fixation was a treatment option that yielded good to excellent
results in tongue-type fractures with posterior facet displacement
as
a whole (Sanders type IIC). The authors noted that the method could
also be applied to selected Sanders type IIA or IIB fractures if the
joint reduction was controlled arthroscopically.
 |
|
FIGURE 59-27
Percutaneous fixation for Sanders 2B split tongue-type fracture. The patient also sustained a contralateral proximal humerus fracture and a spinal cord contusion and developed a pulmonary embolus requiring anticoagulation, necessitating percutaneous reduction and fixation. A. Lateral radiograph demonstrating restoration of calcaneal height and crucial angle of Gissane. B. Broden view demonstrating anatomic reduction of posterior facet (black arrow). C. Axial view showing residual shortening and varus malalignment of tuberosity (black arrow). |
method of three-point skeletal traction applied to the tuberosity,
talus, and cuboid, using ligamentotaxis to manipulate the main
fragments. The depressed posterior facet is elevated percutaneously
with a K-wire introduced laterally. The reduction is confirmed on
fluoroscopy and the fragments are fixed with percutaneously placed lag
screws. Other authors have described percutaneous or mini-open
reduction with use of small wire circular external fixators.61,140 The use of temporary uniplanar, unilateral external fixation has also been described.132 The early results of these minimally invasive approaches are comparable to traditional open methods.
presented a technique that combined open reduction and fixation of the
joint fragments and the anterior process, with percutaneous reduction
and screw fixation of the tuberosity. A group of 24 patients with
unilateral isolated closed Sanders type II and III fractures was
treated using this technique and, compared with a similar group of 26
patients, managed by the extended approach and lateral plating. The
operation was significantly quicker (p
<0.001) in the first group, but more minor secondary procedures and
removal of screws were necessary. There were no wound complications in
this group, whereas four minor complications occurred in the second
group. According to the authors, the ultimate functional results were
equivalent in both groups. Unfortunately, despite the fact that the
authors thought postoperative CT scans were not needed, since these
were not obtained, the accuracy and maintenance of the joint reduction
using this minimal technique could not be assessed, limiting the
usefulness of this report.
reduction by traction, leverage, and compression with subsequent K-wire
or screw fixation for all types of calcaneal fractures.169,240 Stulik et al.214
reported on the treatment of 287 Sanders type II, III, and IV fractures
using minimally invasive techniques. A four-step procedure using a
traction bow, a percutaneous joint reduction using a plantar placed
punch, lateral heel compression, and percutaneous pinning was
performed. A near anatomic reduction was possible in 73.9% of
fractures, with a 4.5% loss of reduction, and a 7% superficial pin
tract infection. Using the Creighton-Nebraska score, clinical outcomes
included 29 excellent, 98 good, 26 fair, and 23 poor results. They
noted that tongue-type fractures had better results than
joint-depression fractures, but Sanders type III tongue fractures were
very difficult
to
reduce using their methods. Results also worsened with an increased
number of fracture fragments, as previously described by Sanders et al.187,190
Interestingly, at a minimum of 2-year follow-up, joint narrowing and
subchondral sclerosis were seen in 85.7% of cases, possibly indicating
the arthritic demise of a joint that was not anatomically reduced but
mobile. Nonetheless, the authors stated that 72% of patients returned
to their preinjury work and that this technique would work well in most
cases.
described their results in 28 comminuted, Sanders type III/IV calcaneus
fractures treated with closed reduction and percutaneous pinning. With
the help of a traction bow and Steinmann pin, reduction of the body was
performed. There was no attempt made to reduce the subtalar joint.
After fixation, patients were splinted and then braced with a posterior
relief ankle-foot orthosis that allowed ankle motion. Pin care was
performed 3 times a day. Patients remained non-weight bearing for 12
weeks, at which point the pins were taken out in the office and weight
bearing was initiated. Twenty-five fractures in 21 patients were
available for review with an average follow-up of 1 year. Subtalar
motion was less than 10 degrees in all cases. Twelve patients reported
minimal to no pain with full activity. These patients used normal shoes
and had no limp. Seven patients had moderate discomfort with full
activity: two had peroneal tendonitis from the lateral wall of the
calcaneus. Two patients had severe pain with activity and had
difficulties with shoe wear. They both had a shortened hindfoot with 15
degrees of varus of their calcaneus. The authors concluded that in all
their cases an anatomic, open reduction would have been the better
technique.
invasive approaches is the potential for incomplete or malreduction of
the posterior facet. Inadequate reduction and/or loss of reduction of
the articular fragments may occur in a significant number of cases.
Rammelt et al. have successfully used subtalar arthroscopy to assist in
judging the quality of articular reduction.169,170
They noted, however, that a uniform application of percutaneous
reduction and fixation methods to all types of calcaneal fractures
carried a considerable risk of inadequate joint reconstruction and
redislocation. As will be discussed later, intraoperative CT scanning
may improve the execution of minimally invasive techniques but is not
readily available in most settings. Finally, prolonged transfixation of
the subtalar and calcaneocuboid joints may be needed to maintain
reduction but should be avoided as significant subtalar stiffness may
result.62 In conclusion, minimally
invasive and/or percutaneous techniques should be reserved for
relatively simple tongue-type fracture patterns. Before attempting
these technically demanding approaches, surgeons should be thoroughly
familiar with the pathoanatomy of intra-articular calcaneal fractures
and have mastery of traditional open techniques.
Historically, many authors emphasized the correction of Böhler’s angle
and restoration of the overall morphology of the calcaneal body over
the reduction of the articular surface.* As a result,
McReynolds, Burdeaux, and others popularized the medial approach in
reconstructing the extra-articular body of the calcaneus.30,31,32,142
This approach, however, resulted in an indirect and often incomplete
reduction of the articular surface, thus leading Stephenson to use a
medial approach for reduction of the calcaneal body and a lateral
approach for reduction of the articular surface.210,211,212
on his 21-year experience with articular surface reduction from the
medial side in 1997. Sixty-one fractures classified according to the
Essex-Lopresti were managed according to a standard protocol with an
average follow-up of 4.4 years. A limited medial approach was used to
reduce the calcaneal tuberosity to the sustentaculum with a threaded
Steinmann pin. The superolateral fragment of the posterior facet was
manipulated through the medially exposed primary fracture line, and the
lateral wall was decompressed with closed, manual compression. The
articular reduction was assessed with intraoperative fluoroscopy.
Fourteen fractures (23%), however, required an additional lateral
incision to obtain a better joint reduction. Patients were allowed to
fully weight bear in a shoe at 8 weeks, and the average time to return
to work was 4.9 months. Few wound complications were reported, and the
average AOFAS ankle and hindfoot score111
was 94.7. Because CT scanning was not used, the data cannot be used for
comparison purposes. The author acknowledged the limitations of the
medial approach.
The majority of recent published series on operative treatment of
calcaneal fractures have used a lateral approach through which
reduction of the calcaneal body and restoration of calcaneal height,
length, and width was consistently reproducible, irrespective of the
extent of comminution.* Additionally, the articular
reduction, when technically possible, was attainable through this
lateral approach, such that a supplemental medial approach was rarely
needed.107 Six separate large series
of displaced intra-articular calcaneus fractures (representing 979
fractures), treated surgically through a lateral approach alone,
confirmed that good results are possible with operative treatment.15,123,190,243
reported on 132 displaced intra-articular calcaneal fractures (types II
through IV) using their CT classification system. One hundred twenty
patients returned for follow-up at an average of 29 months. All
fractures were managed through a lateral approach with lag screw
fixation of the posterior facet, plate fixation of the calcaneal body,
and no bone grafting. All patients underwent CT evaluation
preoperatively, postoperatively, and at 1-year follow-up. Clinical
outcome was based on the Maryland Foot Score190;
those cases requiring subsequent subtalar arthrodesis for posttraumatic
arthritis were immediately considered failures. Calcaneal height,
length, and width were restored to 98%, 100%, and 110% of normal,
respectively, regardless of fracture type. Böhler and Gissane angles
were reduced within 5 degrees of normal in all except three fractures.
anatomic reduction of the articular surface as verified by follow-up
evaluation, 10 had near-anatomic (within 2- to 3-mm) reductions, and
one had an approximate (within 4- to 5-mm) reduction. Clinically, 58
fractures (73%) had good or excellent results.
Eight
fractures (10%) had a fair result and 13 were considered failures, with
10 of these 21 requiring a subtalar arthrodesis. In all 10 of these
cases, arthrography, CT, and subsequent visual inspection of the joint
at time of subtalar arthrodesis verified an anatomically reduced
articular surface with damaged cartilage.
anatomic reduction of the posterior facet, 8 had near-anatomic
reductions, and 4 had approximate reductions. Twenty-one fractures had
good or excellent results, three had fair results, and there were six
failures. Of the seven fractures that ultimately required a subtalar
arthrodesis, four had been anatomically reduced.
near-anatomic, and two approximate reductions with six complete
failures (5 mm of greater step-off). Clinically, there was one good
result, two fair results, and eight complete failures; the one good and
two fair results were in the 3 patients with near-anatomic reductions.
The authors concluded that while an anatomic articular reduction was
needed to obtain a good or excellent result, it could not guarantee it,
likely because of articular cartilage injury at the moment of impact.
Furthermore, clinical prognostication was possible because good to
excellent results decreased as the number of articular fracture
fragments increased. Finally, worse results occurred at the start of
the series, while the number of good to excellent outcomes improved
each successive year. It became apparent that type II fractures were
easier to fix than type III fractures; however, with time, even type
III results improved. The results of operative intervention in type IV
fractures were not improved even after 4 years of experience.
use of CT scans, extensile lateral approaches, plate and screw
fixation, and clinical assessment using standardized tools.*
These studies all used either the Crosby and Fitzgibbons or the Sanders
classifications, and either the Maryland Foot Score or the
Creighton-Nebraska Assessment tool,44 thus allowing comparison between studies. As a result, the studies of Crosby and Fitzgibbons,45 Song et al.,206 Thordarson and Kreiger,219 Laughlin et al.,116 and Tornetta222
suggest that operative intervention, when properly executed, can
achieve good results. Additionally, classifications based on CT appear
to be prognostic: the more comminuted the articular surface, the worse
is the prognosis, thus confirming the findings of Sanders et al.190
who, dissatisfied with contemporary internal fixation techniques, used
bone graft to support the reduction of the articular surface, rather
than screws or staples. In contrast, LeTournel suggested that bone
graft was not needed when lag screws were used because the screws were
able to maintain the articular surface reduction.122,123 Stephenson211 used no bone graft and only had one late collapse, while Leung et al.125 used bone graft in all cases and thought it was needed.124,211 O’Farrell et al.157
did not use bone graft and found no cases of posterior facet collapse.
Sanders et al. did not use bone graft in 120 cases and found no cases
of subsequent loss of articular reduction.190 Longino and Buckley,130
in a prospective historical cohort study, compared patients who
received bone graft supplementation with those who had not and found no
functional or radiographic benefit to the use of bone graft in these
fractures.
appear to accelerate healing or weight bearing, several authors have
reported on the use of injectable, osteoconductive calcium phosphate
cement to assist in earlier weight bearing in the treatment of
metaphyseal and calcaneal fractures.97,115,146,157,235,239
These cements harden without producing much heat, develop compressive
strength, and are remodeled slowly in vivo. The main purpose of the
cement is to fill voids in metaphyseal bone, thereby reducing the need
for bone graft.
used Norian SRS (Synthes, Paoli, PA) in conjunction with standard ORIF
for joint depression calcaneal fractures to determine whether early
postoperative full weight bearing was possible. Cement injection
averaged 10 cm3 and could easily be
performed under fluoroscopic control. Progressively earlier full weight
bearing was achieved without loss of reduction. There was no
statistical difference in clinical outcome scores in patients with full
weight bearing before or after 6 weeks postoperatively. Biopsy samples
taken from clinically satisfactory cases showed nearly complete bone
apposition, areas of vascular penetration, and reversal lines
illustrating progressive cycles of resorption and new bone formation.
The authors concluded that calcium phosphate cement augmentation in
joint-depression calcaneal fractures allowed full weight bearing as
early as 3 weeks postoperatively.
introduction of locking plate technology has been an important advance
in the treatment of complex, periarticular fractures and fractures in
osteopenic bone. Recently, several calcaneal locking plates have been
introduced. In cadaveric models, locked plates have generally increased
the stability of fracture fixation,213 with polyaxially locked screws performing best.176,178 One study showed no biomechanical advantage with locking plate fixation in a cadaver model of Sanders type IIB fractures.174
To date, no studies have demonstrated clinical superiority of locked
calcaneal plates to nonlocked, low-profile neutralization plates. The
indications for locking plates in the treatment of calcaneus fractures
are still being defined but may include use in highly comminuted
fractures, the elderly, or those with particularly poor bone stock (Fig. 59-28).
Standard fluoroscopy has limitations in terms of precise definition of
articular reduction and implant position. For this reason, many
surgeons obtain a postoperative CT scan. In the event of articular
incongruity or implant malposition, the surgeon is forced to either
accept the result or return to the operating room. To address these
concerns, some centers are investigating the use of a mobile isocentric
C-arm with three-dimensional imaging (SIREMOBIL ISO-C-3D; Siemens,
Munich, Germany). Several studies have shown that intraoperative
three-dimensional fluoroscopy has greater sensitivity and specificity
than standard fluoroscopy for identifying articular incongruity and
implant malposition with only minimal additional operating room time.9,110,177 Three-dimensional fluoroscopy has been shown to be equivalent to CT.108
Intraoperative three-dimensional fluoroscopy may obviate the need for
postoperative CT scans and may improve outcomes in the treatment of
intra-articular calcaneus
fractures.
Its use as an adjuvant to minimally invasive approaches is particularly
appealing. Three-dimensional fluoroscopy is not yet widely available,
and further study is needed to define which fractures and surgical
approaches are best served by its use.
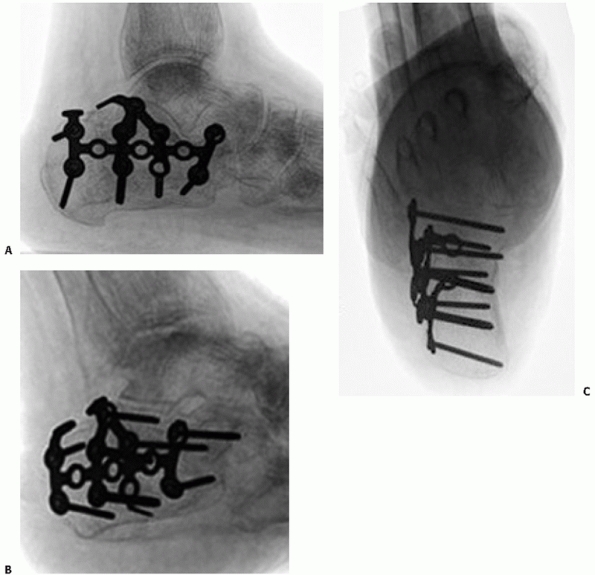 |
|
FIGURE 59-28 Locking plate fixation in patient with seizure disorder and osteopenic bone with (A) lateral, (B) Broden, and (C) axial views demonstrating satisfactory reduction and fixation.
|
however, questioned the efficacy of this method, noting that
nonoperative treatment was superior to fusion. In 1960, Hall and Pennal87
recommended ORIF for simpler fractures and primary subtalar arthrodesis
only for the treatment of highly comminuted fractures. Sanders et al.190
reported on a modification of this method in 1993, which included ORIF
of the fracture, followed by immediate primary subtalar fusion. Using
this method for highly comminuted Sanders type III and IV fractures,
the authors were able to achieve better results than with internal
fixation alone. The authors stressed that essential to achieving a good
outcome, and based on the principles of Pennal, an anatomic reduction
of the calcaneal body must first be obtained.66
By re-establishing the overall calcaneal morphology and the so-called
talocalcaneal relationship, both ankle and transverse tarsal joint
range of motion could be restored.
reviewed the results of 16 patients with severely comminuted calcaneus
fractures treated by ORIF and primary subtalar arthrodesis using an
extensile lateral approach. They used a femoral distractor
intraoperatively to assist with restoration of calcaneal height and
alignment and routinely used iliac crest autograft. Fixation included
one or more lateral plates and either a single fully threaded
cannulated screw or a “noncompressed” partially threaded cannulated
screw, thereby relying on the broad bleeding cancellous bone surfaces
to achieve arthrodesis. All fractures and arthrodeses healed, and 11 of
12 patients who were employed at the time of injury were able to return
to their original occupation at an average of 8.8 months after injury.
reported the results of ORIF and primary subtalar arthrodesis in 33
patients with Sanders type IV calcaneal fractures through an extensile
lateral approach. Ten patients had open fractures, and 16 patients had
significant other musculoskeletal injuries. Iliac crest autograft was
used in 21 fractures. A 93.3% union rate was reported. The average
scores
for
the Creighton-Nebraska Assessment tool, AOFAS Ankle and Hindfoot Score,
and Maryland Foot Score were 61 points (33 to 80), 78 points (55 to
94), and 81 points (66 to 95), respectively, at 38-month average
follow-up. By performing the ORIF and subtalar fusion in one procedure,
the authors noted that the surgeon could limit the morbidity associated
with this fracture, with patients returning to work sooner.
treated six closed, severely comminuted calcaneal fractures with ORIF
and primary fusion. Iliac crest autograft was used in four fractures.
All fractures and arthrodeses healed. Detailed radiographic analysis
revealed near complete restoration of calcaneal length, Böhler and
Gissane angles, and the talocalcaneal angle. Ankle range of motion was
restored to within 10 degrees of normal in all patients. Clinical
outcomes included five excellent and one fair result, and the average
AOFAS score was 88 at 4.9-year average follow-up. The authors concluded
that reconstruction of the calcaneus with primary fusion of the
subtalar joint led to good results.
bilateral calcaneal fractures exist in the literature. Several studies
have commented on small subgroups of patients with bilateral injuries,
and the general consensus has been that patients with bilateral
fractures have a worse prognosis than those with unilateral fractures.28,131,228
retrospectively reviewed 13 patients with bilateral calcaneal
fractures, who underwent surgical treatment of their injuries using an
extensile lateral approach and lag screw and plate fixation. Fractures
were classified according to the Sanders classification, and CT
evaluation was repeated at follow-up. They assessed functional outcome
with the Musculoskeletal Functional Assessment Score and the AOFAS
Ankle and Hindfoot Score, and compared their results with a historical
control group of patients with unilateral injuries treated surgically.
Nine of 13 patients were contacted, and follow-up clinical and
radiographic examination was completed in 6 patients at an average
follow-up of 56 months. Five of the 9 patients required secondary
surgical procedures, including 2 patients who underwent a late subtalar
arthrodesis. They found that surgical treatment of patients with
bilateral injuries resulted in lower functional outcomes compared to
those patients with unilateral injuries.
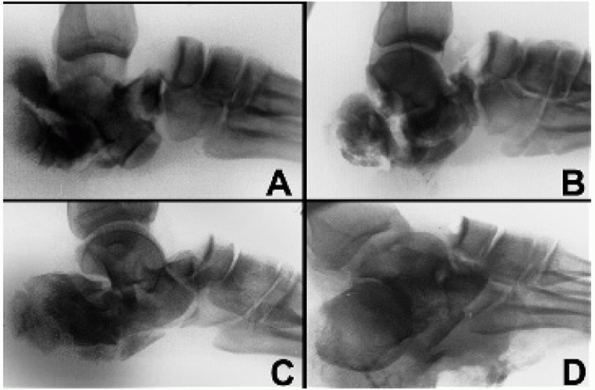 |
|
FIGURE 59-29 Transcalcaneal talonavicular dislocation.
|
compared operative and nonoperative treatment of bilateral calcaneal
fractures in 47 patients. Subjective and objective measurement tools
were used at a minimum follow-up of 2 years, and these data were
compared with those from patients with unilateral injuries. They found
that Böhler angle was significantly less, but subtalar joint range of
motion was significantly better, in the unilateral group compared to
the bilateral group. They also found no difference in subjective
outcome between the operative and nonoperative groups with bilateral
fractures; however, those patients with bilateral fractures treated
surgically were significantly less likely to require a late subtalar
arthrodesis than patients treated nonsurgically.
In this injury pattern, a severely plantarflexed foot is driven axially
toward the ankle (e.g., a plantarflexed foot on the brake pedal with
the floorboard driving through the foot). As a result, the
talonavicular joint may dislocate, with the talar head being driven
through the anterior portion of the calcaneus, and even through the
plantar skin in the most severe of cases. These may or may not be
associated with ligamentous disruptions of the ankle. Ricci et al.175 have described this injury as a transcalcaneal talonavicular dislocation (Fig. 59-29).
attempts at ORIF, the authors recommend reduction and K-wire
stabilization of the talonavicular joint and the application of an
external fixator to stabilize both the foot and the ankle. Treatment
should be delayed to allow the soft tissue envelope to heal.
Surgery
should include a late reconstruction for a calcaneal malunion. In
addition, ankle ligament instability should be repaired, as well as
peroneal tendon dislocation, if present. If the talonavicular and/or
the calcaneocuboid joints are arthritic because of the original injury,
a triple arthrodesis should be considered.
impaction of the superolateral fragment into the body of the calcaneus,
creating either a tongue-type or joint-depression-type fracture.62
Occasionally, the superolateral fragment remains part of the lateral
wall, such that the entire lateral fragment and the posterior
tuberosity dislocate laterally (see Fig. 59-29). There have been 26 reports of this injury in the literature over the past 28 years.17,43,58,59,60,172,229
In this injury, the laterally shifted posterior tuberosity drives into
the lateral malleolus, either fracturing or crushing it. The peroneal
tendons are usually dislocated. Rupture of the lateral collateral
ligament causes inversion of the hindfoot, usually seen as talar tilt.
They observed four cases where the fracture line was in the sagittal
plane with only two fragments. An anterior and medial fragment
maintained its normal relationship with the talus, but the posterior
and lateral fragment became dislocated laterally underneath the fibular
malleolus. They called this a fracture-dislocation of the calcaneus,
and suggested that treatment always be surgical by open reduction and
screw fixation. They noted that 2 of the 4 patients who were not
operated on had poor results.
described 2 patients with calcaneal fracture-dislocation where the
calcaneus split into a small anteromedial fragment and a larger
posterolateral fragment. The authors believed that closed reduction was
impossible and open reduction essential. Ebraheim et al.60
described an additional two cases. In addition to the findings already
mentioned, they also noted that the peroneal tendons were dislocated.
CT scans also showed obvious talar tilt, indicating ankle instability.
Again, these authors believed that conservative treatment by casting or
early range of motion was contraindicated, and that a lateral approach
with ORIF should be performed.
reported four cases in which radiographic features of a fracture of the
lateral malleolus and talar tilt of varying severity were associated
with a displaced fracture of the calcaneus. In two cases, the initial
diagnosis was of a primary ankle injury, which led to inappropriate
initial management. Gross fracture subluxation of the posterior
subtalar joint had occurred in all four cases but could only be fully
appreciated on CT scan. ORIF of the calcaneus led to spontaneous
reduction of the talar displacement. The authors noted that a swollen
hindfoot, talar tilt, and a flake fracture of the lateral malleolus
must alert clinicians to the possibility of a calcaneal
fracture-dislocation. Ebraheim et al.,59
in a subsequent report, evaluated another 11 calcaneal
fracture-dislocations. These injuries all had an intra-articular
calcaneal fracture, lateral subluxation or dislocation of the posterior
facet, peroneal tendon subluxation, subluxation of the talus in the
ankle mortise, and complete disruption of the anterior talofibular and
calcaneal fibular ligaments or fracture of the lateral malleolus.
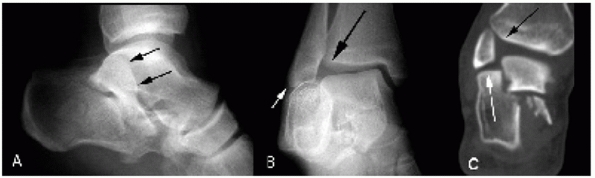 |
|
FIGURE 59-30 Fracture-dislocation of the calcaneus. A. Lateral radiograph clearly demonstrating dislocation of lateral calcaneus (black arrows). B. Mortise view of ankle demonstrating fibula abutment (white arrow) with rupture of lateral ligaments and subluxation of ankle (black arrow). C. Coronal CT scan demonstrating same findings as in (B).
|
reported on two calcaneal fractures associated with locked dislocation
of the posterior facet. Both were treated with minimally invasive open
reduction and percutaneous screw fixation of the fragment with
cannulated screws, with an uncomplicated course. Finally, Randall and
Ferretti172 recently presented a
case report of a lateral subtalar joint dislocation with an associated
calcaneal fracture that was not evident on plain film radiographs but
clearly delineated on subsequent CT scans.
suggestion that a fracture-dislocation exists is a dislocation of the
peroneal tendons, which can be palpated anterior to the fibular
malleolus. Plain radiographs may show the calcaneal pathology, but
careful inspection will reveal a small degree of varus talar tilt. CT
scans clearly show the fracture-dislocation, generally associated with
severe hindfoot varus, the peroneal dislocation, and the ankle
ligamentous disruption. All pathology must be addressed surgically
through a lateral approach.
usually a simple two-part split fracture. Because the articular
surfaces are still part of their respective tuberosity fragments, if
the dislocation can be reduced, the fracture usually will recoil into
an anatomic position. In order to accomplish this, however, reduction
must occur sooner, rather than later. Therefore, when a
fracture-dislocation is suspected, CT scans should be obtained
immediately to verify the diagnosis, and surgery should be performed
soon thereafter. If there is a significant time delay, the
fracture-dislocation will be exceedingly difficult to reduce without a
formal open reduction (Fig. 59-30).
ecchymosis overlying the anterolateral hindfoot region, along with
tenderness to palpation directly over the anterior process fragment.
Anterior process of the calcaneus fractures typically are mis-diagnosed
as ankle sprains, hence the designation “sprainfractures.”22,47,49,74,83
They often result from a forced inversion and plantarflexion injury,
which increases tension on the bifurcate ligament, and produces an
avulsion fracture.104 The fracture
line exits into the calcaneocuboid articulation and typically includes
minimal amounts of the articular surface, although varying proportions
of the joint surface may be involved. The extensor digitorum brevis
muscle may also contribute to the injury pattern. Alternatively, injury
to the anterior process region may result from forced abduction of the
foot, producing an impaction fracture of the calcaneocuboid articular
surface.100 In this instance, the
fragment is typically larger with more involvement of the articular
surface and may displace posteriorly and superiorly.
questioned this as he described cases of open beak-type fractures with
the entire Achilles tendon avulsed. These two fractures most probably
represent a spectrum of injury, resulting most commonly from a violent
pull of the gastrocnemius-soleus complex, such as with forced
dorsiflexion with a low-energy stumble and fall, producing an avulsed
fragment of varying size.
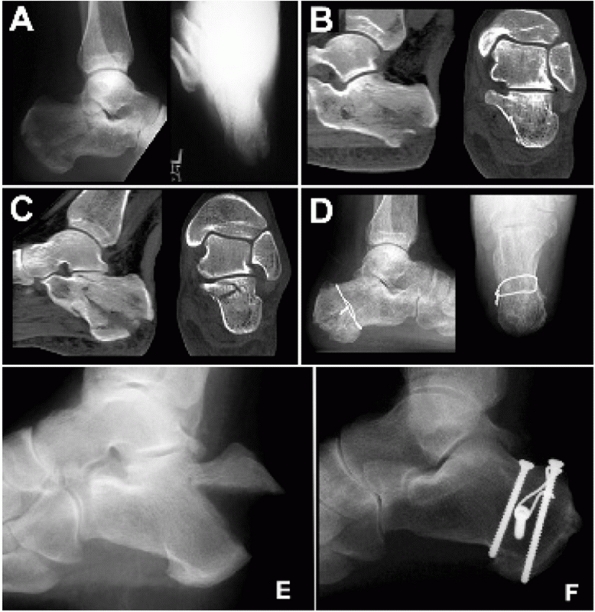 |
|
FIGURE 59-31 Extra-articular avulsion fracture. A. Lateral and axial radiographs. B. Initial CT scan sections showing nonarticular fracture. C. Further CT scan sections showing nondisplaced fracture into joint. D. Lateral and axial radiographs 1 year post simple cerclage band fixation. E. Displaced avulsion fracture. F. At 5 years post tension band with lag screw fixation.
|
present with pain and swelling in the posterior hindfoot and may also
have weakness with resisted plantarflexion because of the shortened
gastrocnemius-soleus complex. Because of the limited soft tissue
envelope overlying the tuberosity, displacement of the fragment may
endanger the surrounding skin. Thus, care must be taken to assess the
overlying skin, as expedient care of the fracture may be necessary to
avoid skin slough.71 Surgical repair
of calcaneal tuberosity avulsion fractures is indicated when (a) the
posterior skin is at risk because of pressure from the displaced
tuberosity, (b) the posterior portion of the bone is extremely
prominent and will affect shoe wear, (c) the gastrocnemius-soleus
complex is incompetent, or, rarely, (d) the avulsion involves the
articular surface of the joint.
involving the subtalar joint, probably account for 20% of all calcaneal
fractures.182,233 The mechanism of injury is identical to that of an intra-articular fracture, with the difference being that the
lines of force do not cross the posterior facet. Standard radiographs
will typically show the fracture involving the body of the calcaneus,
but a CT scan is required to determine whether an intra-articular
fracture exists, as well as the amount of displacement (Fig. 59-32).
Surgery is based on both these factors. Minimally displaced fractures
(less than 1-cm) are treated nonoperatively with early motion and
non-weight bearing for 10 to 12 weeks.53,73,195
Those with significant displacement resulting in varus/valgus
deformity, lateral impingement, loss of heel height, or translation of
the posterior tuberosity require either closed manipulation of the
fracture or ORIF.53,73,143
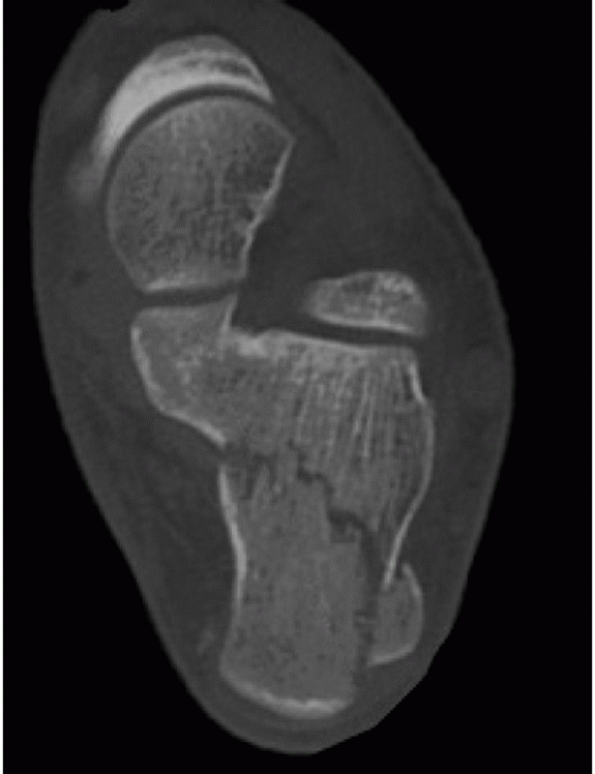 |
|
FIGURE 59-32 Body fracture. CT scan showing no intra-articular involvement.
|
posterior tuberosity are rare and usually nondisplaced. The mechanism
of injury is typically a fall directly on the tuberosity of the heel
either with the foot inverted, causing a shear fracture of the lateral
process, or with the foot in eversion, causing a fracture of the medial
process (Fig. 59-33). Usually, the heel pad is
exquisitely tender, with the area ecchymotic and swollen. The fracture
is best seen on the axial radiographic view or on the coronal CT scans.
Treatment is based on the amount of displacement. Nondisplaced
fractures can be treated with a short-leg weight-bearing cast until
they heal at 8 to 10 weeks.18,141,196 When fractures are displaced, closed manipulation may be considered.53
antibiotics prior to surgery. The operating table should be
radiolucent, preferably without side rails. If one is not available, a
wooden door can be used as a “diving board” attachment with the same
effect. Radiolucent tables with central columns will not work, as the
column will interfere with the surgeon’s location and the access needed
by the fluoroscopic unit. Additionally, a standard C-arm should be
used; it is almost impossible to perform this procedure with a “mini”
C-arm, as the “C” is too small to fit around the operating table for a
true lateral view. A pneumatic thigh tourniquet is used in all cases.
When the limb is exsanguinated, it should be performed with an Esmarch
bandage, and not an elastictype bandage, to guarantee that maximum
exsangination is obtained. The tourniquet should be inflated to 350 mm
Hg, allowing a maximum tourniquet time of 2 12 hours within which to
complete the procedure. If the procedure extends beyond that time, the
tourniquet must be released, and the remainder of the procedure
performed without it.
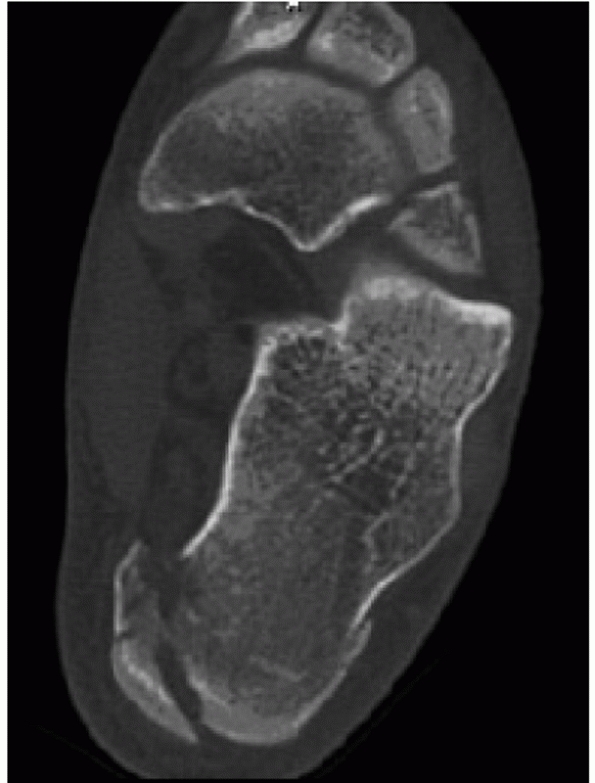 |
|
FIGURE 59-33 Medial process fracture.
|
lateral decubitus position on a beanbag. The lower extremities are
positioned in a scissor-like configuration whereby the nonoperative
“down” limb lies straight, without the knee bent, and the operative
“up” limb is bent at the knee such that the heel is positioned toward
the distal, posterior corner of the operating room table. This allows
the operator to easily approach the fracture, as well as permitting
intraoperative fluoroscopy without interference of the opposite limb.
Protective padding is placed beneath the contralateral limb to protect
the peroneal nerve, a pillow is placed between the legs, and a
“platform” is created with foam padding to elevate the operative limb (Fig. 59-34).
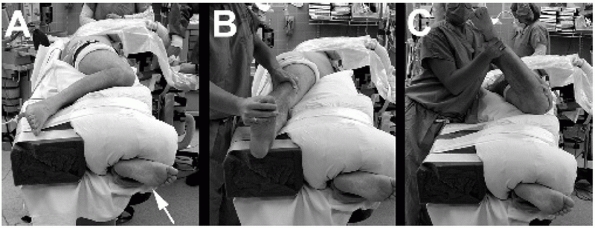 |
|
FIGURE 59-34 Positioning for lateral approach. A. Well leg in straight knee position (white arrow) with injured side on foam platform. B. External rotation allows Broden view. C. Internal rotation allows a clinical assessment of the tuberosity to determine varus/valgus.
|
The incision starts approximately 2 cm above the tip of the lateral
malleolus, just lateral to the Achilles tendon. This line is continued
vertically toward the plantar surface of the heel. It is connected to a
line drawn at the junction of the lateral foot and the heel
pad—typically when compressing the heel, a crease will appear in this
region. Posteriorly, this line connects to the vertical limb;
anteriorly, it may be curved up to follow the skin creases, ideally
centering over the middle of the calcaneocuboid joint articulation.
Whereas the two drawn lines form a right angle, this is replaced with a
gentle curve, primarily to avoid apical tip necrosis.
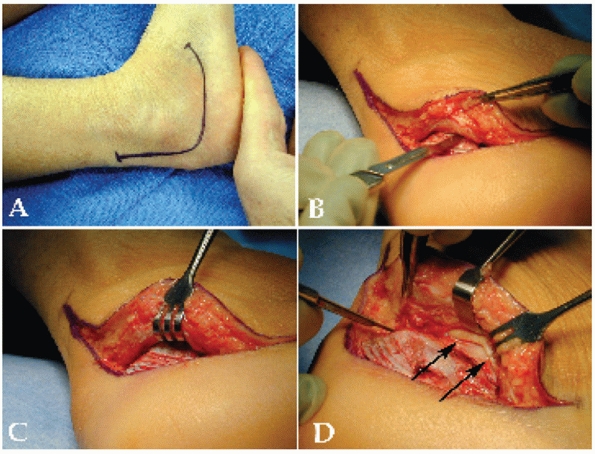 |
|
FIGURE 59-35 Lateral approach and exposure (fracture lateral, mortice, and CT scans can be seen in Figs. 59-6, 59-9, 59-10, and 59-11). A. Incision. B. No-touch full-thickness incision, using no retractors (note open Adson forceps as only means of assistance). C. Insertion of Senn retractor once subperiosteal flap has been developed in corner of incision. D. Flap development, with identification and protection of peroneal tendons (black arrows).
|
for better leverage and access to the heel. The incision is started at
the proximal part of the vertical limb, becoming full thickness once
the calcaneal tuberosity is reached. The knife should be taken
“straight to bone”82 at this level,
with care taken not to bevel the skin. As the knife rounds the corner,
pressure is relaxed and a layered incision is developed along the
plantar aspect of the foot. Once the initial incision is made,
attention is then turned to the corner of the flap, which is now raised
as a subperiosteal, full-thickness flap (Fig. 59-35B).
The surgeon should refrain from using retractors at this stage, as
these will tear the skin from the subcutaneous layer. Only once a
sizeable periosteal flap is
developed may the retractors be used (Fig. 59-35C).
At this point, the calcaneofibular ligament is encountered and peeled
off the calcaneus. The peroneal tendons are seen next. They must be
carefully retracted, and both must be visualized or, as one dissects,
the tendons will be lacerated (Fig. 59-35D).
The tendons are dissected off the peroneal tubercle and then freed from
the anterior calcaneus, using a periosteal elevator. This maneuver
should expose the entire anterolateral calcaneus.
strategically inserted to retract the flap using a “no-touch”
technique. The peroneal tendons are slightly subluxed (not dislocated!)
anterior of the lateral malleolus. A K-wire is then inserted into the
fibula to retract them and the proximal flap (Fig. 59-36A).
A second K-wire is placed in the talar neck, retracting the midportion
of the peroneal tendons and the flap. The distal peroneal tendons are
forcibly lifted with an elevator, and a third K-wire is placed in the
cuboid, thereby retracting the distal aspect of the tendons and the
flap. A small Bennett retractor can then be placed into the sinus tarsi
over the anterolateral corner of the calcaneus to complete the exposure
of the entire lateral wall.
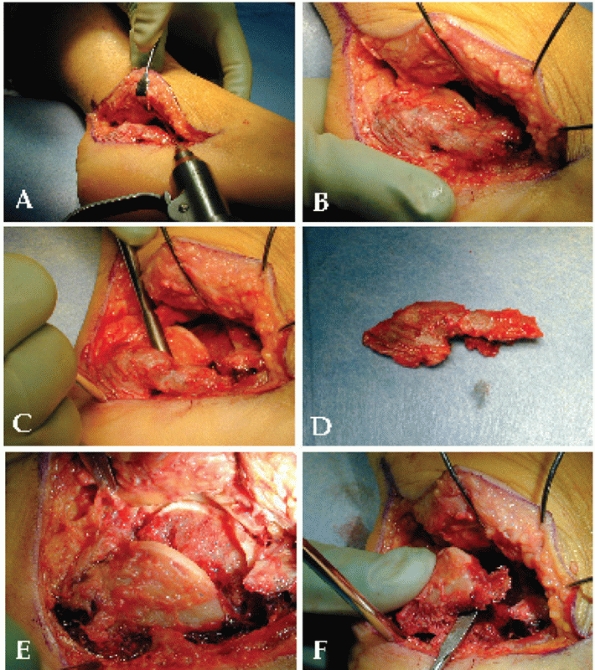 |
|
FIGURE 59-36 Exposure and disimpaction of joint. A. K-wires are inserted into fibula, subluxing peroneal tendons. B. No-touch technique, completed with three K-wires and Schanz pin in tuberosity. C. Identification and separation of lateral wall. D. Lateral wall. E. Exposure of the articular fracture displaying the pathology associated with the double density sign (black arrow = sustentacular fragment, white arrow = lateral articular fragment). F. Disimpaction of the lateral articular fragment.
|
tuberosity is then predrilled, and a short Schantz pin is placed from
lateral to medial, as described by Benirschke13 (Fig. 59-36B).
Using the Schantz pin, the heel is pulled plantarward and distracted
into varus. In fresh fractures, this will disimpact several fracture
lines within the lateral wall, making the edge of the fragment easier
to see. The lateral wall fragment is then carefully elevated in one
piece, using a knife to dissect it free from the impacted joint
fragment (Fig. 59-36C). While it can be retracted back, the authors typically resect the thin
fragment, which has no soft tissue attachment and place it in a small container with saline on the back table (Fig. 59-36D).
elevator is placed into the remaining joint and, using irrigation and
suction, all clot is removed. Once the fracture is identified,
elevation of fragments occurs (Fig. 59-36E).
Obviously, this is easier with simpler fractures, but the technique is
the same for all types. Importantly, the most plantar edge of the
depressed fragment is located. It is carefully cleaned of debris. A
small, strong periosteal elevator or Hoke osteotome is used to get
completely underneath the fragment. If a substantial amount of the
fragment is not under the operator’s control, it will splinter when
attempting to disimpact it. Care must be taken to disimpact the
fragment gradually, as it can be fairly well incarcerated, and sudden
forceful movements will cause it to become a projectile (Fig. 59-36F).
Once lifted, it should be examined for articular cartilage damage. In
the vast majority of cases, these pieces are large, free osteochondral
fragments and can be easily removed and placed on the back table. This
will afford an excellent view of the medial sustentacular component and
the posterior tuberosity, as well as the primary medial fracture line.
of the posterior tuberosity fragment, a periosteal elevator is placed
into the medial fracture line from the lateral wound, and the posterior
tuberosity is disimpacted from the sustentaculum (Fig. 59-37A).
Often, this requires force but will restore the medial wall
anatomically, unless the wall is severely comminuted. In this case, or
if the reduction is unstable, a K-wire is placed from the back of the
heel through the posterior tuberosity and into the medial sustentacular
component, making sure the wire does not interfere with subsequent
joint reduction. While this may be helpful, often the wire will
interfere with articular reduction maneuvers and may need to be removed.
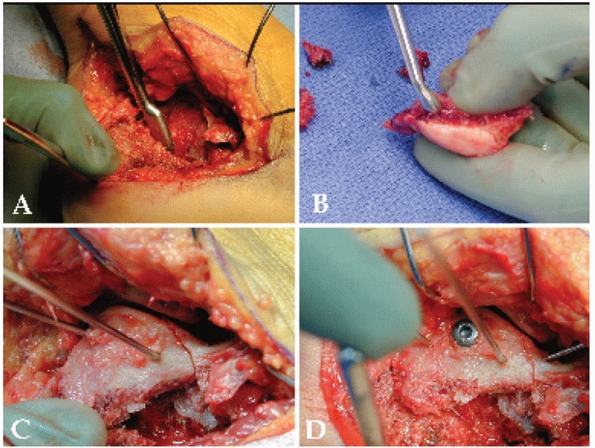 |
|
FIGURE 59-37 Joint reduction maneuvers. A. Posterior tuberosity is disimpacted. B.cleaned of clot and debris. C. Joint reduction with two K-wires. D. Lag screw fixation of joint,
|
B). If two fragments are present (type III fracture), they should be
repositioned and assembled using K-wires, followed with the insertion
of 1.5-mm resorbable poly-levoactic acid (PLLA) pins (Linvatec; ConMed,
Largo, FL) to hold the reduction. Once this is accomplished, or if the
fragment is one large piece, it is then skewered with a K-wire as a
handle and then placed into the calcaneus for reduction. While it is
impossible to describe every reduction maneuver, it is critical to
understand several key points about the reduction in general.
height, rotation, and varus-valgus alignment are correct. This will not
be possible if the inferior portion of the articular fragment bangs
into the edge of the posterior tuberosity; therefore, the posterior and
inferior path for the fragment must be free of bony obstructions. This
may require the surgeon to curette excess bone from the tuberosity,
disimpact the tuberosity with excess varus force, or remove a small
amount of tuberosity bone that is blocking the reduction with a rongeur.
before placing the articular fragment. The anterior calcaneus can be in
as many as three pieces, with the central fragment pulled up because of
its connection with the interosseous ligament. To reduce the anterior
tuberosity, a laminar spreader is often used to stretch the ligament,
thereby allowing the central piece to be more easily repositioned. The
surgeon should resist the temptation to cut the ligament as this will
destabilize the joint over time. In addition, a transverse fracture
line at the angle of Gissane may be present. This has the effect of
rotating the medial articular fragment
underneath
the medial anterior tuberosity fragment. Before reduction of the
articular fragment, therefore, this must be reduced, or the reduction
of the articular fragment of the posterior facet will be to a fragment
that is itself malpositioned. These reductions will need to be
provisionally held with the use of K-wires, placed in a manner so as
not to interfere with the subsequent reduction.
with 1.6-mm K-wires, and the posterior facet reduction is assessed
through “window” visualization (Fig. 59-37C).
At this point, the anterior-lateral “corner” of the articular fragment
should align with the anterolateral “corner” of the medial
sustentacular fragment. Similarly, after a small Hohmann retractor is
placed at the posterior edge of the joint, usually on the back of the
talar body, the corners of the two fragments should line up posteriorly
as well. Once satisfied with the reduction, at least two K-wires should
be placed across the fracture fragments (to prevent rotation of the
fragments), and further visual evaluation should be performed to assess
the joint reduction, both in the front and in the back. When satisfied,
the lateral wall and body should reduce nicely with a valgus
manipulation of the Schantz pin. The anterolateral fragment should
either fall in place or be manipulated back into position, and held in
place with K-wires. The best assessment of this reduction will be to
see that the posterior most edge of the anterolateral fragment “clicks”
into place with the anteroinferior portion of the articular fragment,
thereby recreating the angle of Gissane. At this point, the small
remnant of the lateral wall should drop into place anatomically,
verifying at least that the lateral column is anatomically reduced.
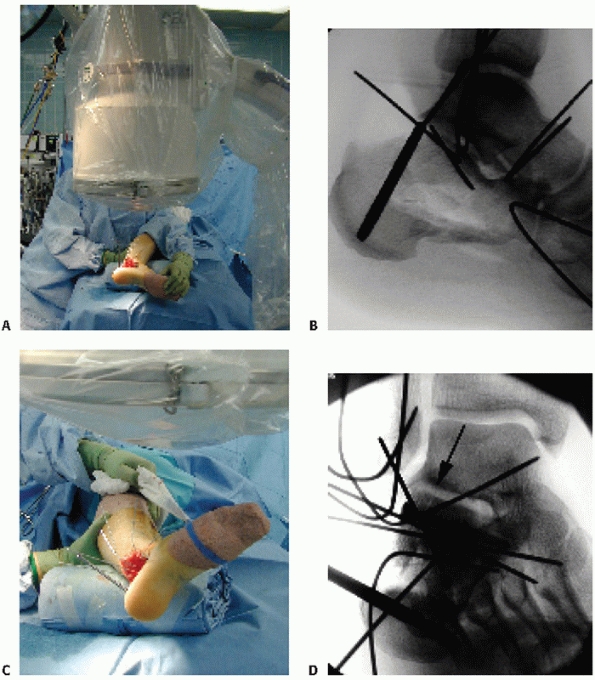 |
|
FIGURE 59-38 Intraoperative imaging. A,B. Lateral intraoperative fluoroscopic view. C,D. Broden intraoperative view. Note black arrow indicating level of fracture and an anatomic reduction.
|
obtain intraoperative lateral, Broden, and axial fluoroscopic views.
The lateral is the easiest view and is taken first. This should be a
true lateral of the talus, to delineate the calcaneus accurately (Fig. 59-38A,B).
Next, with the fluoroscope in the same position, the leg is externally
rotated 45 degrees and dorsiflexed. A mortise view of the ankle is then
obtained, showing clearly the posterior facet in a Broden view (Fig. 59-38C,D)
Thereafter, the head of the fluoroscope can be rotated to show both the
front and the back portions of the posterior facet. Finally, the foot
is externally rotated 90 degrees and maximally dorsiflexed. The
fluoroscope is then rotated so that it is directing the beam from
plantar to dorsal, at the level of the midfoot, to allow a clear axial
view of the calcaneus to be obtained. If the surgeon chooses, a 2.7-mm
sinuscope may be used without fluid to visualize the joint as well.
This is particularly helpful with extremely medial fracture lines (Fig. 59-39).
until anatomic reduction of the articular surface is confirmed.
Definitive fixation is achieved by using 3.5-mm cortical lag screws
placed from the lateral cortex aiming slightly plantarly, to avoid
violating the intra-articular surface, and distally toward the
sustentaculum. Once this is completed, the joint should be reassessed
both visually and fluoroscopically.
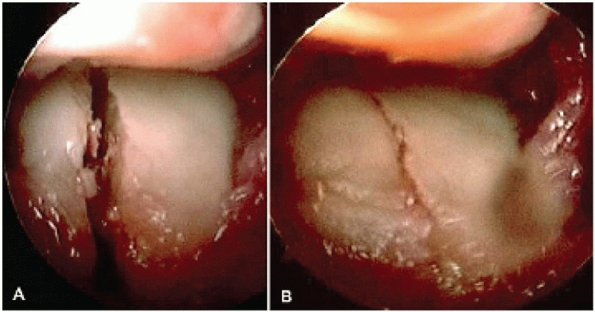 |
|
FIGURE 59-39 If the fracture line is extremely medial, a 2.7-mm sinuscope can be used to visualize the reduction. Before (A) and after (B) lag screw fixation.
|
fragment and the posterior tuberosity are realigned if needed to ensure
that the body is anatomically reduced. The small lateral wall fragment
is momentarily lifted to evaluate the defect below the joint. If a
large cavity is present, the surgeon may elect to fill the void with
either bone graft or a graft substitute. Once this is performed, the
lateral wall remnant is placed back and an appropriately sized,
low-profile lateral neutralization plate is selected and positioned (Fig. 59-40A). Bending of the plate is not recommended because the bone will come to the plate with the placement of the
screws. Furthermore, bending of the plate will throw the calcaneal tuberosity into varus.
 |
|
FIGURE 59-40 Fixation of body. A. Lateral wall replaced, and low-profile plate applied. B-D. Radiographs of final fixation, showing anatomic reduction of the articular surface, anterior process, and tuberosity.
|
These screws are placed under power, as the torque of the power driver
will cause the bone to narrow as the screw pushes the plate against the
lateral wall. The three main components of the calcaneus (as described
by Letournel122) —the anterior
process, the posterior tuberosity, and the joint—are secured to the
plate with several screws placed into each component. The final
reduction is verified fluoroscopically, and all K-wires are removed (Fig. 59-40C,D).
should fall back into their groove. If they do not or if they were
dislocated from the trauma, the tendon sheath will need to be repaired.
The tendons should be evaluated by placing a Freer elevator into the
peroneal tendon sheath at the distal inferior portion of the wound. It
should be advanced within the sheath to the level of the fibular
malleolus (Fig. 59-41A). Now, while watching the skin, the elevator is pushed forward, to see if the sheath has been torn off the fibula (Fig. 59-41B). If this is the case, the elevator will slide anterior to the fibula, and a repair must be performed.
the vertical limb of the incision, and the wound is closed in the
following layered fashion. Deep individual No. 0 absorbable sutures are
passed in a figure-of-eight stitch, starting with the apex of the
wound, and advancing to the proximal and distal edges (Fig. 59-42A).
The sutures are temporarily clamped until all deep sutures have been
placed. Once completed, the sutures are hand-tied sequentially,
starting at the proximal and distal ends and working toward the apex of
the incision. This should pull the flap together and take tension off
the apex of the incision. The skin layer is closed with monofilament
suture using the modified Allgöwer-Donati technique, again starting at
the ends and progressing toward the apex183 (Fig. 59-42B). Sterile dressings are applied and the tourniquet is deflated. A bulky cotton dressing and Weber splint are then placed.
pain control, and placed in a short-leg non-weight-bearing cast the
following morning prior to discharge. The patient is then evaluated at
3 weeks postoperatively. At that time, the cast is removed and the
incision is assessed. The sutures are removed if the incision is fully
sealed and completely dry. If not, the sutures may stay in place for
another 2 to 4 weeks. Sutures should not be removed until the wound is
healed. The patient is converted back into the elastic stocking, and
fracture boot is locked in neutral flexion. Early subtalar joint
range-of-motion exercises out of the boot are initiated at this time;
however, weight bearing is not permitted until 12 weeks
postoperatively. Additionally, we prefer that the patient sleep in the
boot until weight bearing is initiated to prevent an equinus
contracture. Once weight bearing is initiated, the patient is gradually
transitioned into regular shoes as tolerated. The patient should be
able to return to a reasonably active job by 4.5 to 6 months
postoperatively.
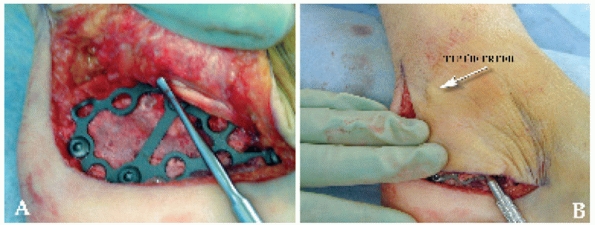 |
|
FIGURE 59-41 Peroneal tendon evaluation. A. After K-wires are removed, peroneal tendons are tested for instability by placing a probe within the tendon sheath. B. Verification that the tendons are stable. The probe is limited in its anterior excursion over the fibula.
|
fractures, most commonly Sanders type IIC fractures. The patient is
placed in the prone position on a radiolucent operating room table (see
earlier considerations). In this position, external rotation of the hip
will create the lateral position of the leg, while internal rotation
will permit access to the medial surface if needed. The leg is first
placed in neutral rotation and exsanguinated, inflating the tourniquet
to 350 mm Hg. A large bolster is placed under the foot, thereby flexing
the knee.
large terminally threaded 3.2-mm guide pins are inserted percutaneously
into the medial and lateral side of the Achilles tendon at the superior
aspect of the posterior calcaneal tuberosity. The wires are directed to
exit the fracture just below the inferior margin of the anterior
portion of the displaced posterior facet; they are not driven beyond
the facet. A posteroanterior fluoroscopic image confirms the wires to
be parallel with the axis of the tuberosity and within bone. Once the
wires are in proper position, the reduction maneuver is performed by
using one of the wires as a reduction tool (Fig. 59-43).
the foot. Reduction of the tongue fragment is confirmed
fluoroscopically while the foot is held in plantarflexion. If this is
successful, the second pin is advanced across the anterior process,
stopping just short of the plantar corner of the calcaneocuboid joint.
A Broden view is obtained (mortise view of the ankle) and reduction of
the articular surface is assessed under fluoroscopy. Placement of the
guidepin is confirmed with lateral, axial, and anteroposterior views of
the foot. Definitive fixation is achieved with a cannulated 6.5-, 7.3-,
or 8.0-mm lag screw that is inserted over the guidewire. Because the
original pin is now bent from the reduction, it is exchanged for a new
wire and measured, and another cannulated screw is placed into the
calcaneus.
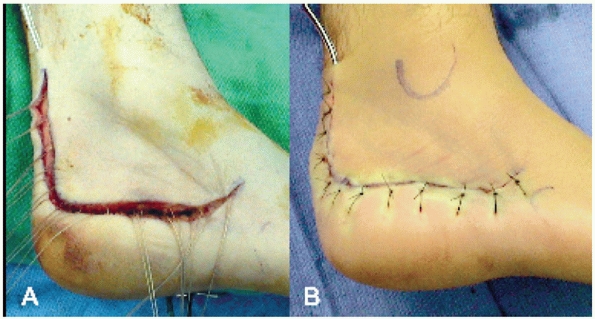 |
|
FIGURE 59-42 Wound closure. A.
Individual figure-of-eight No. 0 Vicryl sutures placed from corner of wound to ends, and then individually tied from ends to corner to relieve pressure on flap edge. B. Skin closure with 3-0 nylon using Allgower-Denoti sutures with knot on outside of incision. Note placement of drain to prevent pressure from postoperative hematoma. |
incision should be made directly over the anterior-inferior edge of the
fragment, as verified on radiography. This will invariably be at the
level of the peroneal tendons and sural nerve, so care must be taken to
only incise the skin and protect the soft tissues by spreading with a
clamp. A small periosteal elevator is then inserted under fluoroscopic
control, and the distal corner of the fragment is pried free,
disimpacting the tongue fragment. If the reduction is obtained but
cannot be held, a 1.6-mm K-wire may be inserted into the fragment and
across the subtalar joint to maintain reduction while the axial screws
are placed. Finally, if reduction is obtained in the sagittal plane but
widening between the sustentaculum and the joint fragment exists in the
coronal plane, a large reduction tong (DePuy Orthopaedics, Warsaw, IN)
is placed through the incision on the lateral side, and on the
sustentaculum on the medial side, to compress and reduce the fragments.
This may be held with a 1.6-mm wire and followed with a small-fragment
cannulated screw, inserted from the
medial
side to lag the lateral fragment, thereby narrowing the joint. The
identical postoperative protocol as described earlier is used.
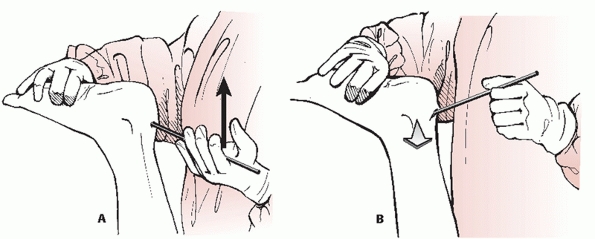 |
|
FIGURE 59-43 Percutaneous Essex-Lopresti maneuver. A. With patient prone, leverage of heavy K-wires toward the ceiling (arrow) will cause (B) disimpaction and elevation of fragment (arrow).
|
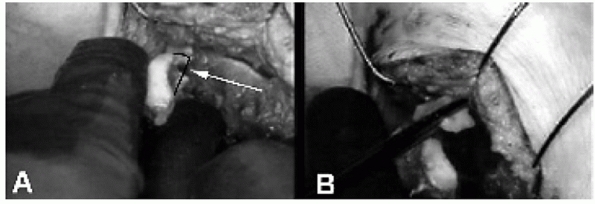 |
|
FIGURE 59-44 Split-tongue-type fracture. A. When these are opened and the tongue is disimpacted, a defect can be seen on its medial edge (black outline, white arrow). B. Further dissection reveals free osteocondral fragment (in pituitary rongeur).
|
it is virtually impossible to close reduce even a simple two-part
tongue fracture when an intra-articular fracture is also present in the
sagittal plane, such as a Sanders type IIA or IIB (Fig. 59-44).
While the fragments can be elevated, an anatomic reduction of the joint
cannot be obtained. The reason for this is that it simply impossible to
(a) clear the bone, soft tissue debris, and clot from the fracture
surfaces and (b) rotate and manipulate the fragments into a
three-dimensional anatomic position percutaneously. Tongue fractures
that are highly comminuted, such as Sanders type III or IV fractures,
will have a similar problem. In these cases, ORIF through a lateral
approach is required with certain caveats.
anatomically reduce a type IIA or IIB tongue fragment in proper
rotation in the sagittal plane may be virtually impossible because of
the constant deforming force of the Achilles tendon. Similarly, after
repositioning of the middle fragment to the sustentaculum using
resorbable pins, the surgeon attempting reduction of the lateral type
III tongue fragment will suffer the same fate. A solution to this is to
perform the Essex-Lopresti maneuver on the fragment in an open manner.
This invariably reduces the fragment anatomically in the sagittal
plane. The fragment can then be pinned to the sustentacular fragment
and the procedure completed (as described previously).
comminution, patients must be counseled beforehand about the possible
intraoperative decision to perform a primary subtalar fusion, and this
possible procedure should be added to the surgical consent.
highly comminuted intra-articular fractures, (typically severe Sanders
type III and all types IV), after attempts at internal fixation of the
posterior facet have failed because the articular surface is not
reconstructable.190 In these cases
it must be emphasized that a standard ORIF using an extensile lateral
approach is performed as earlier described, such that the best
restoration of the anatomy of the entire calcaneus is obtained. Once
the relationships between the calcaneal tuberosity, anterior process,
and posterior facet fragments have been re-established using plates and
screws, the joint is critically evaluated. If (a) the joint is poorly
reduced, (b) severe cartilage delamination exists, or (c) much of the
joint surface is absent, then a decision is made to perform a primary
subtalar fusion (Fig. 59-45).
from the surfaces of the posterior facet (calcaneus and talus) while
preserving the subchondral bone. The subchondral surfaces of the talus
are perforated with a 2.5-mm drill bit to create a bleeding surface,
and cancellous autograft or allograft is placed in the subtalar joint
space. The arthrodesis is then performed using one or two cannulated
8.0-mm lag screws, placed into the corner of the heel such that the
screws lie perpendicular to the subtalar joint and enter the dome of
the talus. If the 3.5-mm articular lag screw interferes with the
placement of the arthodesis screws, it is removed; however, care should
be taken to leave the plate screws in place so that the posterior facet
is still connected to the rest of the calcaneus via the plate and the
overall reduction is maintained. If necessary, the latter screws can be
redirected. Wound closure is standard (as previously described). The
patient is kept non-weight bearing in serial short-leg casts for 12
weeks, until radiographic healing of both the fracture and the
arthrodesis is confirmed. Progressive weight bearing is initiated
thereafter, following the same regimen as described earlier.
 |
|
FIGURE 59-45 Primary fusion for a type IV fracture.
|
usually a simple split. As such, if the dislocation can be reduced, the
fracture usually will recoil into an anatomic position. To accomplish
this, however, reduction must occur sooner rather than later.
Therefore, when a fracture-dislocation is suspected, CT scans should be
obtained immediately to verify the diagnosis, and surgery should be
performed soon thereafter. If there is a significant time delay, the
fracture will be exceedingly difficult to reduce without a formal open
reduction.
placed in the lateral position in the standard manner (as previously
noted). A fluoroscopic lateral is obtained to identify the superior
lateral edge of the displaced tuberosity fragment. A 1-cm oblique skin
incision is made directly over this area, carefully avoiding the
peroneal tendons and sural nerve. A periosteal elevator is inserted
into the wound and manipulated carefully until it is in the fracture,
hugging the medial surface of the lateral fragment. It is advanced
until it is below the talus and within the subtalar joint. Because this
displaced portion of the joint is initially wedged up against the
lateral side of the talus, positioning of the elevator should be
verified on radiography to ascertain that it is not in the ankle joint.
Once satisfied that the elevator is in the correct position, the
surgeon should attempt to lever the lateral fragment downward. As soon
as it clears the talus, it will recoil back into position.
tissue swelling is gone and fix the fracture and the remaining lateral
pathology at 10 to 21 days, or proceed with percutaneous fixation of
the fracture and repair of the collateral ligaments and peroneal
tendons at the same time. If the surgeon sees excess comminution, or is
unable to reduce the articular surface anatomically after reducing the
dislocation, a delay is advisable.
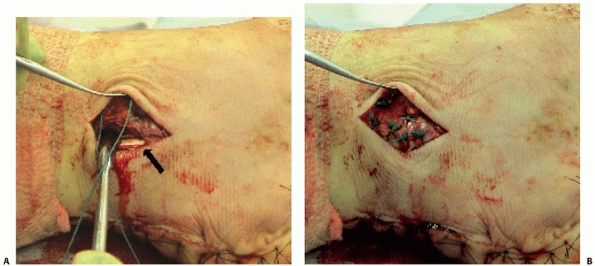 |
|
FIGURE 59-46 Evaluation of peroneal dislocation because of sheath avulsion through a separate incision. A. An incision is made over the distal fibula, and the tear is entered. B.
The tendons are relocated and the sheath is secured to the fibula with suture anchors to prevent the tendons from subluxating again. |
large periarticular reduction clamp (DePuy Orthopaedics, Warsaw, IN) is
passed through the lateral incision to grab the lateral fragment, while
the other tine is placed on the sustentaculum, medially. A clamp of
this design is needed to negotiate around the body of the calcaneus.
Once the two fragments are between the clamp tines, the clamp is slowly
closed, sliding the fragments down and together in a reduction
maneuver. The reduction is verified on intraoperative fluoroscopic
Broden views and, once acceptable, secured with percutaneously placed
1.6-mm K-wires, inserted from lateral to medial in the coronal plane.
When satisfied with the final position of the articular surface and the
K-wires, a small incision is made over each wire, and a cannulated
4.0-mm screw of appropriate length is placed. The clamp is then removed.
peroneal tendons. The initial incision is usually exactly at the level
of the pathology and can be extended in either direction to expose the
ligaments and the tendons. The tendons can typically be pushed back
into their sulcus. They should then be tested for stability by
dorsiflexing and plantarflexing the ankle. If the tendons repeatedly
sublux or dislocate, the sheath has been torn from the fibula, allowing
the tendons to slip over the lateral malleolus. Using suture anchors,
the sheath can be secured to the posterior inferior edge of the
malleolus. This will prevent the tendons from slipping out of their
groove (Fig. 59-46). At this point, the
collateral ligaments are evaluated and primarily repaired, again with
suture anchors, either in the fibula or the talus, depending on the
pathology encountered. For midsubstance tears, anchors are placed in
both the talus and the fibula, and the suture is woven through the
remnants of the ligament and then sewn to each other. Postoperatively,
the patient is placed in a padded Weber splint. This is changed for a
short leg non-weight-bearing cast for 6 weeks. Thereafter,
the
cast is exchanged for a compression stocking and fracture boot, and
range of motion of the subtalar and ankle joint is begun. Weight
bearing is permitted after radiographic determination of fracture
healing, typically at 10 to 12 weeks.
fracture that fails conservative therapy, surgical management is
indicated. A small fragment can be excised, but we prefer surgical
management of anterior process fractures if the fragment is greater
than 25% of the calcaneocuboid articulation as seen on CT scan
evaluation. The anterior process lies just distal to the sinus tarsi
and can be easily felt on palpation. The patient is placed in the
supine position with a bolster under the hip or, alternately, in a
lateral decubitus position. A lateral longitudinal incision is made
directly over the anterior process. The extensor digitorum brevis
muscle is mobilized; it is usually not necessary to mobilize the more
plantar peroneus brevis tendon. The calcaneocuboid joint is exposed,
and the fracture is identified, reduced, and provisionally stabilized
with 1.2- to 1.6-mm K-wires. The reduction is verified fluoroscopically
and is best seen on an oblique view of the foot. Definitive fixation is
achieved with small or minifragment screws. Occasionally, 1.2- or
1.5-mm resorbable PLLA pins are used instead. Comminuted fragments too
small to accept fixation may be primarily excised; however, every
attempt is made to preserve as much articular surface as possible. The
incision is closed in a layered fashion, a bulky dressing is applied,
and a wooden-soled shoe is placed. The patient may ambulate in the
wooden-soled shoe, but regular shoes are not permitted for 10 to 12
weeks postoperatively.
the anterior process are encountered. The operative approach remains
the same; treatment is based on size of fragment. If large enough to
accept a minifragment screw, attempts can be made to débride the
interface back to bleeding bone and then secure the fragment with a lag
screw. If the fragment is not repairable, excision and soft tissue
reconstruction are performed. Postoperative management is the same as
for acute injuries.
room table, with the patient in the prone position, as access to both
the medial and lateral sides of the calcaneus is needed to reduce the
fracture. If damage to the Achilles tendon insertion is severe, a
posterior approach may be needed as well. A large bolster should be
placed under the foot to flex the knee and relax the calf muscles. The
patient should be paralyzed to maximally relax the gastrocnemius-soleus
complex. After exsanguination and elevation of the tourniquet to 350 mm
Hg, the vertical limb of an extensile lateral incision is made,
centered over the fracture. On entering the fracture, it should be
cleaned of clot and loose bone. Using a periosteal elevator, enough
soft tissue should be cleared from the superior and inferior calcaneus
to allow the insertion of pointed reduction forceps. Often, a second
clamp is necessary to fully compress the fracture into an anatomic
position, and manipulation of the foot and leg may be needed to
complete the reduction. Because of the tension placed on the fracture
by the calf muscles, the reduction may take several minutes to
accomplish. Typically, if the fracture is incompletely reduced, the
surgeon waits approximately 1 minute and then compresses the clamp(s)
again. This is repeated several times over several minutes, until the
soft tissues have fatigued to the point where an anatomic reduction can
be achieved. Repositioning of the fragment, other than by closing the
clamps forcefully, is rarely needed, but a vertically oriented medial
incision, placed posterior to the neurovascular bundle, may be added to
assist the surgeon.
cancellous lag screws can be placed perpendicularly across the
fracture, late separation of the fracture can occur because of overpull
of the gastrocnemius-soleus complex. Therefore, it is our standard
treatment to add cerclage wire to the fixation (Fig. 59-47). First popularized by B. G. Weber,25
the addition of a tension band effectively neutralizes the force across
any size fracture fragment. This wire (18- or 20-gauge) should be
inserted through the lateral incision over the posterior superior
aspect of the calcaneus, anterior to the Achilles tendon, using a
curved wire passer. When the tip of the passer is palpated on the
medial skin, a small incision is made, and the wire is advanced through
the incision. The wire is clamped, and the passer is removed through
the lateral wound. It is then re-passed from lateral to medial, without
any wire, along the inferior portion of the calcaneus, in the space
just anterior to the tubercles and superior to the plantar fascial
insertion. It is manipulated to exit out of the previously made medial
incision, and the wire is then threaded into it and pulled back out of
the lateral wound. The wire should be unlooped as it is passed through
the calcaneus, so as to avoid kinking of the wire. At this point, the
wire passer is removed and the wire tightened snugly. It is bent back
flush with the lateral wall, and any excess knot is cut off with wire
cutters.
would continue to be a risk to fracture healing, a Strayer (recession
of the gastrocnemius aponeurosis) procedure may be performed.163,164
In this case, it is performed in the prone position by locating the
middle-distal third junction of the calf. A short, vertical midline
incision is made, with care to avoid the sural nerve and small
saphenous vein. The fascia is found and incised in line with the skin
incision. Selfretaining retractors are placed. A transverse incision is
then made through the muscle aponeurosis at the level of the
musculotendinous junction. With the knee extended, gentle dorsiflexion
of the foot will result in lengthening of the muscle, thus relieving
tension on the fracture repair. Closure of all wounds is standard. A
bulky cotton dressing and Weber splint are applied with the ankle in
plantarflexion, so as to neutralize the pull of the
gastrocnemius-soleus complex. The patient is converted to an elastic
stocking and fracture boot, and gentle active early range-of-motion
exercises are initiated at 2 weeks postoperatively. Weight bearing is
not begun until 8 to 10 weeks postoperatively, at which point the
patient is transitioned into regular shoe wear.
treated with non-weight bearing and early motion in a fracture boot for
10 to 12 weeks. If CT scans indicate significant displacement or
intra-articular involvement, internal fixation should be performed.
Displacement is considered to be significant when (a) the posterior
tuberosity has shifted proximally to such a degree that gastrocnemius
function is affected, (b) the lateral calcaneal wall translation causes
peroneal tendon impingement, subluxation, or dislocation, or (c) the
posterior tuberosity has settled into more than 30 degrees of varus or
40 degrees of valgus. Surgical intervention is performed using the
techniques described for intraarticular fractures.
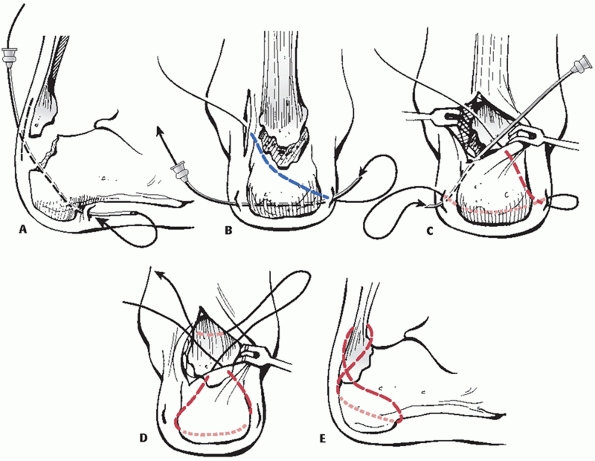 |
|
FIGURE 59-47 Cerclage of tuberosity avulsion fractures according to B. G. Weber.
|
bearing in a fracture boot until pain and swelling resolve.
Range-of-motion exercises out of the boot and weight bearing in the
boot are then begun until the fracture is healed, usually at 8 to 10
weeks. When the medial process is displaced more than 1.5 cm, a painful
heel with an altered gait may develop if not surgically corrected. A
small J-shaped incision on the inferomedial aspect of the calcaneus is
made, followed by reduction, using a K-wire to manipulate and
reposition the fragment. Once in place, this fragment is secured with a
lag screw or a resorbable PLLA pin. If the fragment is more comminuted
than anticipated, the incision is extended proximally, and a small
fragment buttress plate is added to maintain reduction. Eight to 10
weeks of non-weight bearing in an off-the-shelf boot is required before
ambulation is begun. Painful healed malunions should initially be
treated with shoe modifications. If unsuccessful, resection of any
exostoses and shaving down of the remaining prominence of the posterior
tuberosity are performed using either a medial or a lateral approach,
depending on the location of the prominence.
following nonoperative treatment because of lateral impingement, where
the displaced, expanded lateral wall subluxes the peroneal tendons
against the distal tip of the fibula, or dislocates the tendons.
Entrapment may also occur after operative treatment207 and is more common with a standard Kocher approach, because the
tendons are released from their sheath to allow access to the subtalar
joint. The extensile lateral approach has largely circumvented these
problems82,227;
however, care must be taken when operating near the fibula to sublux,
but not dislocate, the peroneal tendons when exposing the fracture.
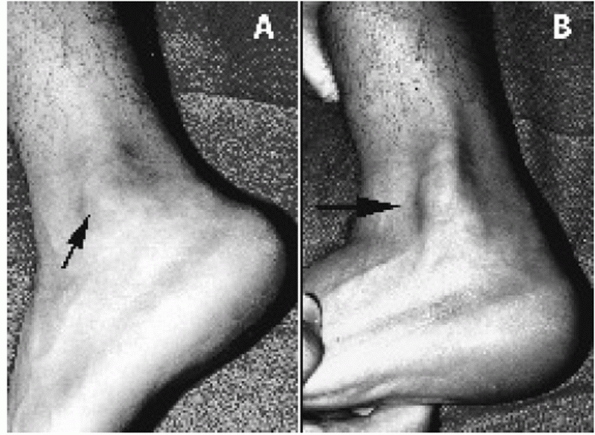 |
|
FIGURE 59-48 Peroneal tendon dislocation. A. Reduced. B. Tendons dislocated over fibula.
|
tendons, either from the surgical approach or from prominent adjacent
implants. Differential local anesthetic injections can be used to
document that the source of the pain is the peroneal tendons, but Mizel
et al.149 proposed that this may not
be completely accurate and suggested that a simultaneous injection of
contrast material be performed with the anesthetic to alert the
clinician to any lack of specificity of the anesthetic test. If the
pain is diagnosed as peroneal scarring or impingement, either tenolysis
or removal of the symptomatic implants may be needed if nonoperative
modalities, such as massage and stretching, fail to provide relief.
the peroneal tendons preoperatively, usually by palpation along the
lateral malleolus (Fig. 59-48). Although the
tendons are often reducible after the lateral wall abutment is removed,
occasionally the tendons will continue to dislocate as the surgeon
manipulates the subtalar joint after completing the reduction and
fixation of the calcaneus. In these cases, the surgeon should attempt
to reconstruct the superior peroneal retinaculum and surrounding soft
tissue envelope in order to stabilize the tendons.138,200,202,208
This is most easily performed by tacking the periosteal sleeve back
down to the posterior edge of the fibula with a staple or suture
anchor. This will prevent the tendons from redislocating into the soft
tissue defect created by the injury (Fig. 59-49).
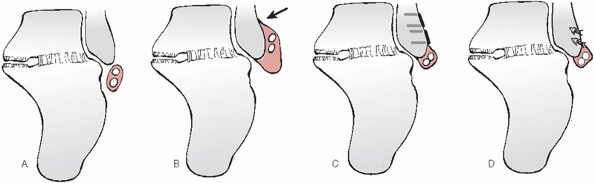 |
|
FIGURE 59-49 Peroneal tendon dislocation. A. Normal anatomy. B. Tendon sheath avulsion with tendon dislocation. C. Repair of sheath using small staples. D. Repair of sheath using suture anchors.
|
recommended sensory denervation for this problem, but their ability to
distinguish various causes of pain was limited and they performed this
procedure indiscriminately. Both Barnard and Odegard10 and Lance et al.114
recognized that plantar pain from a damaged heel pad is not improved by
operative treatment. Currently, there remains no effective treatment
for this problem.
following a calcaneal fracture. If nonoperative methods, such as heel
pads, are unsuccessful, these painful exostoses can be removed
surgically, as originally described by Cotton in 1921.40 A plantar incision should be avoided, as this is associated with painful scarring.
eversion is borne by the ankle joint because of the coupled nature of
the ankle and subtalar joint complex.194
The ankle joint, however, is not intended to bear these stresses, and
the patient experiences lateral ankle pain, most commonly in the form
of a chronic ankle sprain. These sequelae are typically managed
nonoperatively, using nonsteroidal anti-inflammatory medication,
temporary casting, or the use of a lace-up ankle brace. Patients with
recalcitrant pain may require a magnetic resonance scan to rule
out
other ankle pathology. If the pain can be localized to the
anterolateral gutter, it is the authors’ experience that an arthroscopy
will often be beneficial in removing plicae that have developed during
the immobilization period of fracture healing.
operative management of calcaneal fractures is iatrogenic injury to a
sensory cutaneous nerve. The sural nerve is the most common nerve
involved because of the frequency of use of the lateral approach, and
this complication may occur in up to 15% of cases.128
In this approach, the nerve may be injured at either the proximal or
distal portions of the incision, and the injury may vary from a stretch
neuropraxia, which may be transient or permanent, to a laceration of
the nerve. Nerve injury may also occur with the medial approach, with
the calcaneal branch of the posterior tibial nerve most commonly
involved, occurring in up to 25% of cases.158
Clinically, the patient may develop a partial or complete loss of
sensation in the affected area or a painful neuroma. Nonoperative
treatment is generally advised and may include pharmacologic management
such as gabapentin or amitriptyline, physical therapy modalities, and
soft accommodative shoe inserts or modifications. In the event of a
painful neuroma that does not respond to nonoperative treatment,
neurolysis or resection of the neuroma and stump burial into deep
tissue or bone may be considered.
management of a calcaneal fracture and typically involves entrapment or
compression of the posterior tibial nerve secondary to soft tissue
scarring, a malunited fracture fragment, or bony exostosis causing
impingement against the nerve.112,128,156
Patients experience medial-sided heel pain with associated paresthesias
in the distribution of the posterior tibial nerve, and the pain is
commonly worse at night or with activities, such as standing or
walking. Clinically, there may be a positive Tinel sign along the
course of the involved nerve. The diagnosis can be confirmed by
injection of a local anesthetic in the tarsal tunnel or by
electrodiagnostic studies. When clinical and diagnostic tests indicate
nerve entrapment, surgical neurolysis and decompression of the
posterior tibial nerve and its branches may be indicated.
regional pain syndrome type I, may occur following operative or
nonoperative management. Once present, it may result in long-term and
potentially permanent functional impairment of the patient. The
diagnosis is made clinically, and examination initially reveals burning
or aching pain out of proportion to the injury that is refractory to
narcotic pain medication, extreme intolerance to cold, and pain with
passive range of motion and light touch. Patients note irritation from
any contact with the skin, including socks and bed sheets. Later, the
patient may exhibit cold clammy skin, cyanotic discoloration, and scant
hair growth. Radiographs obtained at this point may reveal patchy,
disuse osteopenia, and three-phase bone scan frequently shows altered
uptake in the affected limb. Last, as the limb becomes atrophic, the
skin often assumes a pale, shiny, cyanotic appearance with the absence
of skin folds and significant restrictions in joint range of motion.
Radiographs will typically reveal severe osteopenia.
disease may be managed with aggressive physical therapy, including
manual desensitization and massage, and pharmacologic agents such as
gabapentin or amitriptyline. Protracted cases may require lumbar
sympathetic nerve blockade, epidural or intrathecal pain pumps,
alpha-adrenergic blockers, or other medications. Prompt referral to a
pain management specialist may be beneficial. In the absence of a
specific stimulus as a cause of the underlying pain (e.g., a prominent
screw or a neuroma), further surgical treatment should be avoided.128
treatment of a calcaneal fracture is wound dehiscence, and this may
occur in up to 25% of cases.* The incision typically will
approximate relatively easily; however, the wound later dehisces, up to
4 weeks following surgery, and most commonly at the apex of the
incision. Risk factors for wound dehiscence and wound complications in
general include smoking, diabetes, open fractures, high body mass
index, and a single layered closure.2,67
The majority of the wounds will eventually heal; deep infection and
osteomyelitis develop in approximately 1% to 4% of closed fractures12,91,98,128 and in up to 19% of open fractures.5,12,14,94
exercises should be stopped so as to prevent further dehiscence. The
limb may be placed in a cast with a window over the wound, and
damp-to-dry dressing changes or other granulationpromoting wound agents
are started on a daily basis. Alternately, the patient may be placed in
a fracture boot, and the wound managed with daily whirlpool treatments.
In either case, a course of oral antibiotics is begun. This regimen is
usually successful, so long as the wound is limited to a
partial-thickness necrosis of the skin. Once the wound is healed,
range-of-motion exercises are reinstituted. It has been the authors’
experience that recalcitrant wounds of this type (Fig. 59-50)
benefit significantly from the use of a negative-pressure device, such
as the wound-vac (Vacuum-Assisted Closure; KCI, Inc., San Antonio, TX).
If all treatment methods have failed, a low-profile fasciocutaneous
flap such as a lateral arm flap may be needed.127
serial surgical débridements and the administration of culture specific
antibiotics must be started. These problems are usually seen in the
postoperative period, and as such, most patients have not developed
diffuse osteomyelitis but rather superficial osteitis because of direct
extension from an adjacent source.36
If the infection is superficial, the plate and screws should be
retained, at least until the fracture has healed (typically a minimum
of 6 months). After the wound bed is determined to be clean, a delayed
closure, or the use of a vacuum-assisted device, is attempted if at all
possible. If the wound is too large to treat with the latter methods, a
free tissue transfer is performed. Culture-specific intravenous
antibiotics are administered for a minimum of 6 weeks. In the event of
diffuse osteomyelitis, all implants
must
be removed along with all necrotic and infected bone. In this case, an
antibiotic impregnated spacer should be placed in the wound. Following
repeated débridements and 6 weeks of culture-specific antibiotics, the
patient is readmitted to the hospital, serial débridements are
performed, wound cultures are obtained, and, if the defect is clean, a
subtalar fusion using a large structural iliac crest autograft can be
performed, based on the amount of remaining calcaneal bone stock. In
rare instances, this will not be possible and an amputation will be
required, but this is the exceptional situation.
 |
|
FIGURE 59-50 Wound dehiscence.
|
reconstruction of the joint surface of the posterior facet. Patients
will develop rapid deterioration of the joint if the reduction is
inadequate, if screws protrude into the joint, or if the articular
cartilage has been extensively damaged at the time of injury. Severe
pain and disability will certainly result.154,158,190 Poeze et al.165
showed a significant inverse correlation between institutional fracture
volume and the rate of late subtalar arthrodesis, suggesting the
presence of true learning curve.
with a truly anatomic reduction, as a result of cartilage damage at the
time of injury.187 This has been shown to be true in an experimental model by Borelli et al.,20
where the authors proved that profound and possibly irreversible
articular cartilage damage occurs after a single high-energy impact
load.
This can be accomplished by injecting a local anesthetic into the
subtalar joint. If the pain is relieved, then nonoperative measures,
such as shoe modifications, a University of California Berkeley
Laboratory orthosis, ambulatory aids, and nonsteroidal
anti-inflammatory agents, can be tried before operative treatment is
contemplated. If these fail, removal of any implants and an in situ
subtalar arthrodesis using 6.5- to 8.0-mm large cannulated lag screws
is recommended.37,168
operative intervention, most commonly if the anterolateral fragment is
not perfectly repositioned, as well as nonoperative treatment. If the
joint appears to be the area of pain, an injection of local anesthetic
can be performed to differentiate between arthritis and peroneal
tendonitis. In cases where it is the site of pain, nonoperative
treatment is offered followed by a fusion if all other methods fail.192
nonoperatively, because of either a lack of familiarity with operative
techniques or fear of potential operative complications.129,166
Nonoperative management of a displaced intra-articular calcaneal
fracture can result in equally problematic complications including (a)
posttraumatic subtalar and/or calcaneocuboid arthritis from residual
joint surface incongruity; (b) subfibular impingement because of
residual expansion of the lateral calcaneal wall and subsequent heel
widening; (c) peroneal tendon impingement, subluxation, or dislocation,
caused in part by the subfibular bony impingement, and resulting in
pain and instability; (d) loss of calcaneal height resulting in
relative dorsiflexion of the talus in the ankle mortise, leading to
anterior impingement and loss of ankle dorsiflexion; (e) residual
hindfoot malalignment resulting in altered gait patterns and shoe wear;
and (f) posterior tibial or sural neuritis.* These problems
affect function of the ankle, subtalar, and calcaneocuboid joints and
result in pain and disability in a surprisingly large number of
patients. In an effort to improve the outcome, treatment must focus on
correction of the specific sequelae of calcaneal malunions (Fig. 59-51).
identified residual problems following calcaneal fractures, accurately
describing the residual lateral wall expansion that limited subtalar
joint motion and caused painful subfibular and peroneal tendon
impingement. He performed an aggressive exostectomy of the lateral
calcaneal wall, along with an extra-articular osteotomy for heel
malalignment, resection of symptomatic plantar heel spurs, and forceful
manipulation of the subtalar joint as described by Gleich in 1893.80
The results of his technique were indeed impressive and were duplicated
by Magnuson, who used a large bone wrench to pry open the subtalar
joint.133 Kalamchi and Evans109 combined the technique of Conn38 with the Gallie fusion,70
using the lateral exostosis as autograft. They noted that the
trapezoidal slot for the graft allowed for correction of heel valgus,
thus realigning and stabilizing the heel in neutral position, and
reported good results in 6 patients. Braly et al.23
performed a lateral wall exostectomy combined with a peroneal tenolysis
as an alternative to subtalar arthrodesis in patients with calcaneal
malunions with lateral pain. They reported good results in 9 of 11
patients.
published their preliminary results with a subtalar distraction bone
block arthrodesis, which was a modification of the Gallie fusion
technique.70 They used a femoral
distractor medially and a differentially wedged tricortical iliac crest
bone graft to restore the talocalcaneal angle, thus correcting the
horizontal talus and the talonavicular subluxation. Fixation was
achieved with 6.5-mm fully threaded cancellous screws placed in nonlag
fashion to prevent compression of the autograft. Although good results
were reported in 6 of 8 patients, complications
included one nonunion and two varus malunuions. Other authors have reported similar problems using this technique. Buch et al.26 reported good results in only 7 of 14 patients, and 2 patients had varus malunions requiring reoperation. Sanders et al.191 reported four varus malunions in a series of 15 patients, of whom 2 required reoperation. Bednarz et al.11
reported on 29 feet treated with a subtalar distraction bone block
arthrodesis with a mean follow-up of 33 months. Four patients developed
a symptomatic nonunion, all of whom were smokers, while 2 went on to
varus malunion. In contrast, Trnka et al.226
reported on 41 feet managed with subtalar distraction bone block
arthrodesis, 29 of which were calcaneal malunions, at a mean follow-up
of 70 months. Although 5 patients went on to nonunion, there were no
varus malunions in their series.
 |
|
FIGURE 59-51 Calcaneal malunion. Note widened calcaneal body with fibular abutment, dislocation of peroneal tendons, and severe subtalar (A) and calcaneocuboid (B) arthritis.
|
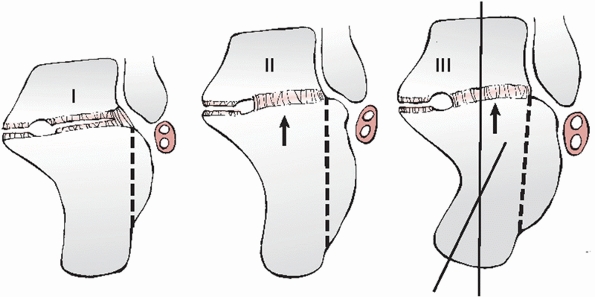 |
|
FIGURE 59-52
Calcaneal malunions according to Stephens and Sanders. Type I, lateral wall exostosis; type II, lateral wall exostosis and subtalar arthritis; type III, lateral wall exostosis, subtalar arthritis, and angular deformity. |
complex calcaneal osteotomy through the primary fracture line for
management of calcaneal malunions. The tuberosity fragment was
translated beneath the sustentacular fragment medially, thereby
restoring calcaneal height and residual varus angulation. He reported
satisfactory results in 9 of 10 feet at an average follow-up of 14
months.
Type I malunions included a large lateral exostosis, with or without
extremely lateral subtalar arthrosis. Type II malunions included a
lateral wall exostosis combined with subtalar arthrosis across the
width of the joint. Type III malunions included a lateral exostosis,
severe subtalar arthrosis, and a calcaneal body malunited in hindfoot
varus or valgus angulation.
An
extensile lateral approach was used in all patients, and treatment was
specific to malunion type: type I malunions underwent a lateral wall
exostectomy and a peroneal tenolysis, as described by Cotton41 and Magnuson133;
type II malunions underwent a lateral wall exostectomy, a peroneal
tenolysis, and an in situ subtalar arthrodesis, using the local bone as
graft as described by Kalamchi and Evans109;
and type III malunions underwent a lateral wall exostectomy, a peroneal
tenolysis, a subtalar fusion, and a calcaneal osteotomy to correct
hindfoot malalignment or shortening, as described by Dwyer.55
Their preliminary results included 26 malunions at an average follow-up
of 32 months. There were no nonunions, no varus malunions, and no deep
infections, and the classification and protocol proved to be prognostic
of outcome.
reported the intermediate- to long-term results of this protocol.
Forty-five malunions in 40 patients were available for follow-up
evaluation at a minimum of 24 months, with an average of 5.3 years
(range, 24 to 151 months). Thirty-seven of 40 arthrodeses (92.5%)
achieved initial union, with 42 of 45 malunions (93.3%) aligned in
neutral or neutralslight valgus hindfoot alignment. All 45 malunions
were plantigrade. Statistical analysis revealed no significant
difference in the Maryland Foot Score, AOFAS Ankle and Hindfoot Score,
SF-36 Health Survey subscales, lateral talocalcaneal, talar
declination, or calcaneal pitch angles among the three malunion groups.
Smoking was a significant risk factor for nonunion of the fusion and
wound complications in the series.
completed a matched-cohort study comparing patients who had undergone
initial ORIF and subsequently developed posttraumatic arthritis
requiring an in situ fusion to patients treated nonoperatively who
developed a calcaneal malunion requiring late reconstruction and
subtalar arthrodesis. The ORIF group included 36 feet in 34 patients
with an average follow-up of 2.7 years. The average interval from ORIF
to late subtalar arthrodesis was 22 months, and 33 of 36 arthrodeses
(91.7%) achieved initial union. The calcaneal malunion group included
45 feet in 40 patients with an average follow-up of 5.3 years.37
The average interval from fracture to late reconstruction was 16.4
months, and 37 of 40 arthrodeses (92.5%) achieved initial union. There
was a statistical trend toward a lower wound complication rate in the
ORIF group and significantly higher outcome scores in the ORIF group.
This suggests that initial restoration of calcaneal height, length, and
overall shape is beneficial to outcome. In the event that the patient
develops late posttraumatic arthritis, an in situ arthrodesis can be
performed.
which allows decompression of the subfibular impingement and peroneal
tendons, as well as restoration of calcaneal height through a bone
block subtalar arthrodesis, and correction of residual hindfoot
malalignment as needed. The patient is placed in the lateral decubitus
position, and a standard extensile lateral approach to the calcaneus is
used. A lateral wall exostectomy is performed for all three malunion
types. Beginning posteriorly, the saw blade is angled slightly medially
relative to the longitudinal axis of the calcaneus, leaving more
residual bone plantarly, and thereby providing decompression of the
subfibular region. Care is taken throughout the exostectomy to avoid
violation of the talofibular joint. The exostectomy is continued to the
level of the calcaneocuboid joint, and is completed with an osteotome,
thus removing the fragment en bloc as a single piece for later use as
autograft. The peroneal tendon sheath is then incised over a length of
2 to 3 cm along the undersurface of the subperosteal flap and a
tenolysis is performed.
joint is débrided of any remaining articular fragments while preserving
the underlying subchondral bone. The bony surfaces are prepared with a
2.5-mm drill bit, and the previously resected lateral wall fragment is
then placed within the joint as an autograft bone block, with the
widest portion of the autograft oriented posteromedially to avoid varus
malalignment. With the subtalar joint held in neutral to slight valgus
alignment, definitive stabilization is achieved with two large (6.5-,
7.3-, or 8.0-mm) partially threaded cannulated lag screws placed from
posterior to anterior in diverging fashion into the talar dome and
neck. A third screw may be added in the anterior process region
extending into the talar neck and head. In patients with a type III
malunion, correction of angular malalignment within the calcaneal
tuberosity is performed prior to implant placement: a Dwyer closing
wedge osteotomy is performed for those with varus malalignment, while a
medial displacement calcaneal osteotomy is used for those patients with
valgus malalignment. Routine layered closure is completed over a deep
drain. Weight bearing and early range-of-motion exercises are initiated
for type I malunions once the incision has healed, while those with
type II and III malunions are not permitted to weight bear for 12 weeks
postoperatively, until radiographic union is confirmed.
NA, Dhawan S, Gruen GS, et al. Wound-healing risk factors after open
reduction and internal fixation of calcaneal fractures. Foot Ankle Int
1998;19:856-861.
SJ, Vannier MW, Gilula LA, et al. Three-dimensional computed tomography
of the foot: optimizing the image. Comput Med Imaging Graph
1988;12:59-66.
J, Jesch AB, Helling HJ, et al. [CT morphometry for calcaneal fractures
and comparison of the Zwipp and Sanders classifications]. Z Orthop Ihre
Grenzgeb 2002;140:339-346.
W. An oblique projection for roentgen examination of the talo-calcaneal
joint, particularly regarding intra-articular fractures of the
calcaneus. Acta Radiol 1943:306-310.
K, Finkelstein J, Khoury A, et al. The use of intraoperative
three-dimensional imaging (ISO-C-3D) in fixation of intraarticular
fractures. Injury 2007;38:1163-1169.
L, Odegard JK. Conservative approach in the treatment of fractures of
the calcaneus. J Bone Joint Surg Am 1955;37A:1231-1236.
PA, Beals TC, Manoli A. Subtalar distraction bone block fusion: an
assessment of outcome. Foot Ankle Int 1997;18:785-791.
SK, Sangeorzan BJ. Extensive intra-articular fractures of the foot.
Surgical management of calcaneal fractures. Clin Orthop 1993;128-134.
GK, Stevens DG, Kreder HJ, et al. Open fractures of the calcaneus: a
review of treatment and outcome. J Orthop Trauma 2004;18:202-206.
H, Massart P, Delvaux D, et al. The operative treatment of
intraarticular calcaneal fractures. Indications, technique, and results
in 257 cases. Clin Orthop 1993;55-59.
N, Thomine JM. [Fracture-dislocation of the calcaneus. Apropos of 4
cases]. Rev Chir Orthop Reparatrice Appar Mot 1977;63:191-202.
J Jr, Torzilli PA, Grigiene R, et al. Effect of impact load on
articular cartilage: development of an intra-articular fracture model.
J Orthop Trauma 1997;11:319-326.
J Jr, Lashgari C. Vascularity of the lateral calcaneal flap: a
cadaveric injection study. J Orthop Trauma 1999;13:73-77.
BD, Myerson MS, Miller SD. Primary subtaler arthrodesis for the
treatment of comminuted calcaneal fractures. Foot Ankle Int
1996;17:61-70.
RE, Meek RN. Comparison of open versus closed reduction of
intraarticular calcaneal fractures: a matched cohort in workmen. J
Orthop Trauma 1992;6:216-222.
RE, Tough S, McCormack R, et al. Operative compared with nonoperative
treatment of displaced intra-articular calcaneal fractures: a
prospective, randomized, controlled multicenter trial. J Bone Joint
Surg Am 2002;84A:1733-1744.
BD. Reduction of calcaneal fractures by the McReynolds medial approach
technique and its experimental basis. Clin Orthop 1983;177:87-103.
B Jr. Fractures of the calcaneus. In: Chapman M, Madison M, eds.
Operative Orthopedics. St. Louis: Mosby, 1989:1723-1736.
BJ. Fractures of the calcaneus: open reduction and internal fixation
from the medial side: a 21 year prospective study. Foot Ankle Int
1997;18:685-692.
JB, Hamilton JJ, Bear LS. Experimental intra-articular calcaneal
fractures: anatomic basis for a new classification. Foot Ankle
1989;10:81-87.
JB, Hansen ST, Benirske SK. Subtalar distraction bone block fusion for
late complications of os calcis fractures. Foot Ankle 1988;9:81-86.
G. Classification and treatment of chronic osteomyelitis. In: Evarts
CM, ed. Surgery of the Musculoskeletal System. New York: Churchill
Livingstone; 1989:10-35.
MP, Lee WE III, Sanders RW. Intermediate to long-term results of a
treatment protocol for calcaneal fracture malunions. J Bone Joint Surg
Am 2005;87A:963-973.
LA, Fitzgibbons T. Computerized tomography scanning of acute
intra-articular fractures of the calcaneus. J Bone Joint Surg Am
1990;72A:852-859.
LA, Fitzgibbons TC. Open reduction and internal fixation of type II
intraarticular calcaneus fractures. Foot Ankle Int 1996;17:253-258.
M, Buckley R, Tough S, et al. Displaced intra-articular calcaneal
fractures: variables predicting late subtalar fusion. J Orthop Trauma
2003;17:106-112.
HW. Fractures of the anterior superior portion of the os calcis due to
indirect violence. J Bone Joint Surg 1930;25:629-631.
PA, Silvestre MA, Segura LF, et al. Surgery for fracture of the
calcaneus: 5 (2-8) year follow-up of 20 cases. Acta Orthop Scand
1993;64:161-164.
TJ, Morrey BF, Braun DP. Surgical excision for anterior process
fractures of the calcaneus. J Bone Joint Surg Am 1982;64:519-524.
AL, Resnick D, Campbell G. Computed tomography and bone scintigraphy in
the evaluation of tarsal coalition. Radiology 1982;144:137-140.
IL. Primary fusion of the posterior subtalar joint in the treatment of
fractures of the calcaneum. J Bone Joint Surg Br 1953;35B:375.
P, Buckley R, Tough S, et al. Bilateral calcaneal fractures: operative
versus nonoperative treatment. Foot Ankle Int 2004;25:47-52.
DM, Gregg PJ, Atkins RM. Intra-articular fractures of the calcaneum.
Part I: Pathological anatomy and classification. J Bone Joint Surg Br
1993;75B:183-188.
DM, Langkamer VG, Atkins RM. Intra-articular fractures of the
calcaneum. Part II: Open reduction and internal fixation by the
extended lateral transcalcaneal approach. J Bone Joint Surg Br
1993;75B:189-195.
DM, Maxwell AC, Atkins RM. Fracture of the lateral malleolus with talar
tilt: primarily a calcaneal fracture not an ankle injury. Injury
1993;24:109-112.
NA, Elgafy H, Sabry FF, et al. Calcaneus fractures with subluxation of
the posterior facet. A surgical indication. Clin Orthop 2000;210-216.
NA, Savolaine ER, Paley K, et al. Comminuted fracture of the calcaneus
associated with subluxation of the talus. Foot Ankle 1993;14:380-384.
DL, Koella C. Combined percutaneous and “minimal” internal fixation for
displaced articular fractures of the calcaneus. Clin Orthop
1993;108-116.
AS Jr, Infante AF, Sanders RW, et al. Subtalar arthrodesis for
complications of intra-articular calcaneal fractures. Foot Ankle Int
2000;21:392-399.
JW, Starr AJ, Early JS. Early wound complications of operative
treatment of calcaneus fractures: analysis of 190 fractures. J Orthop
Trauma 1999;13:369-372.
M. Closed reduction and percutaneous osteosynthesis: technique and
results in 265 calcaneal fractures. In: Tscherne H, ed. Major Fractures
of the Pilon, the Talus, and the Calcaneus. Berlin: Springer Verlag,
1992.
A, Stone C, Squire D, et al. Os calcis fractures: analysis of
interobserver variability in using Sanders classification. J Foot Ankle
Surg 2003;42:21-23.
MJ, Nork SE, Barei DP, et al. Secondary soft tissue compromise in
tongue-type calcaneus fractures. J Orthop Trauma 2008;22:439-445.
PW, Herzenberg J, Frank JL, et al. Compterized tomographic analysis of
acute calcaneal fractures. Foot Ankle 1986;6; no.4:184-193.
W. Discussion on “Fracture of the os calcis” (Proceedings of the
British Orthopaedic Association). J Bone Joints Surg 1947;29:254-255.
RB, Anderson JT. Prevention of infection in the treatment of one
thousand and twenty-five open fractures of long bones: a retrospective
and prospective analysis. J Bone Joint Surg Am 1976;58A:453-458.
RB, Mendoza RM, Williams DN. Problems in the management of type III
(severe) open fractures: a new classification of type III open
fractures. J Trauma 1984;24:742-746.
BH, Levinsohn EM, Fredrickson BE, et al. Computed tomography of
calcaneal fractures: anatomy, pathology, dosimetry, and clinical
relevance. Am J Roentgenol AJR 1985;145:911-919.
MC, Pennal GF. Primary subtalar arthrodesis in the treatment of severe
fractures of the calcaneum. J Bone Joint Surg Br 1960;42B:336-343.
EJ, Grujic L, Early JS, et al. Morbidity associated with ORIF of
intra-articular calcaneus fractures using a lateral approach. Foot
Ankle Int 2001;22:868-873.
KA, Infante AF, Walling AK, et al. Open fractures of the calcaneus:
soft-tissue injury determines outcome. J Bone Joint Surg Am
2003;85A:2276-2282.
KA, Buckley RE, Mohtadi NG, et al. Functional outcome measures after
displaced intra-articular calcaneal fractures. J Bone Joint Surg Br
1996;78B:119-123.
WG, Verheyen CC, Leemans R. An injectable calcium phosphate cement as a
bone-graft substitute in the treatment of displaced lateral tibial
plateau fractures. Injury 2003;34:141-144.
JL, Buckley R, McCormack R, et al. Complications following management
of displaced intra-articular calcaneal fractures: a prospective
randomized trial comparing open reduction internal fixation with
nonoperative management. J Orthop Trauma 2003;17:241-249.
F, Huebner MK. Treatment of os calcis fractures by open reduction and
internal fixation. Foot Ankle Int 1994;15:225-232.
AF, Lewis B, Heier KA, et al. Open reduction internal fixation and
immediate subtalar fusion for comminuted intra-articular calcaneal
fractures: a review of 33 cases. OTA 15th Annual Meeting, paper # 49
[Orthopaedic Trauma Association web site] 1999. Charlotte, NC. October
22-24, 1999.
MH, Kay B. An anatomic study of the anterior superior process of the os
calcis and its clinical application. Foot Ankle 1983;3:268-281.
EE, Gebhardt JS. Surgical management of calcaneal fractures using
bilateral incisions and minimal internal fixation. Clin Orthop
1993;117-124.
R, Judet J, Lagrange J. Tritement des fractures du calcaneum comportant
une disjonction astragalo-calcaneene. Mem Acad Chir 1954;80:158-160.
D, Citak M, Gardner M, et al. Three-dimensional fluoroscopy for
evaluation of articular reduction and screw placement in calcaneal
fractures. Foot Ankle Int 2007;28:1165-1171.
HB, Alexander IJ, Adelaar RS, et al. Clinical rating systems for the
anklehindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int
1994;15:349-353.
HB, Schaap EJ, Chao EY, et al. Displaced intra-articular fractures of
the calcaneus treated non-operatively. Clinical results and analysis of
motion and groundreaction and temporal forces. J Bone Joint Surg Am
1994;76A:1531-1540.
RT, Carson JG, Calhoun JH. Displaced intra-articular calcaneus
fractures treated with the Galveston plate. Foot Ankle Int
1996;17:71-78.
SJ, Grau GF. Evaluation and treatment of open calcaneal fractures: a
retrospective analysis. Orthopedics 2003;26:621-626.
E. Open reduction and internal fixation of calcaneal fractures. In
Spiegel P, ed. Topics in Orthopedic Surgery. Baltimore, MD: Aspen
Publishers, 1984:173-192.
K, Chan W, Shen W, et al. Operative treatment of intraarticular
fractures of the os calcis. J Orthop Trauma 1989;3:232-240.
KS, Chan WS, Shen WY, et al. Operative treatment of intraarticular
fractures of the os calcis—the role of rigid internal fixation and
primary bone grafting: preliminary results. J Orthop Trauma
1989;3:232-240.
KS, Yuen KM, Chan WS. Operative treatment of displaced intra-articular
fractures of the calcaneum. Medium-term results. J Bone Joint Surg Br
1993;75B:196-201.
D, Buckley RE. Bone graft in the operative treatment of displaced
intraarticular calcaneal fractures: is it helpful? J Orthop Trauma
2001;15:280-286.
C, Buckley R. Bohler’s angle: correlation with outcome in displaced
intraarticular calcaneal fractures. J Orthop Trauma 1999;13:554-558.
B, Bortolazzi R, Marangon A, et al. External fixation for displaced
intra-articular fractures of the calcaneum. J Bone Joint Surg Br
2006;88B:1474-1479.
J-F. Operative Surgery, Based on Normal and Pathological Anatomy.
Translated from French by Frederick Brittan. Philadelphia: Blanchard
and Lea, 1851.
RA. Major surgical procedures for disorders of the ankle, tarsus and
midtarsus. In Mann RA, ed. Surgery of the Foot. St. Louis: CV Mosby,
1986:284-308.
JE, McDermott FJ. Experiences with the Palmer open reduction of
fractures of the calcaneus. J Bone Joint Surg Am 1955;37A:99-106.
IS. The case for operative treatment of fractures of the os calcis. In
Leach RE, Hoaglund FT, Riseborough EJ, eds. Controversies in Orthopedic
Surgery. Philadelphia: WB Saunders, 1982:232-254.
IS. Trauma to the os calcis and heel cord. In Jahss M, ed. Disorders of
the Foot and Ankle. Philadelphia: WB Saunders, 1984:1497-1538.
G, Bereiter H, Leutenegger A, et al. Results of operative treatment for
intraarticular fractures of the calcaneus. J Trauma 1991;31:234-238.
G, Degonda F, Leutenegger A, et al. Ten-year follow-up after operative
treatment for intra-articular fractures of the calcaneus. J Trauma
1995;38:713-716.
LE, Chow LC, Friedman C, et al. The reinforcement of cancellous bone
screws with calcium phosphate cement. J Orthop Trauma 1996;10:15-20.
MS, Michelson JD, Newberg A. Peroneal tendon bupivacaine injection:
utility of concomitant injection of contrast material. Foot Ankle Int
1996;17:566-568.
MS, Miller RA, Scioli MW, et al. OKU, Orthopaedic Knowledge Update.
Rosemont, IL: American Academy of Orthopaedic Surgeons, 1998.
RD, Levine BP, Trevino SG, et al. Operative treatment of acute
displaced intraarticular calcaneus fractures. Foot Ankle Int
1995;16:57-63.
MS. Experimental decompression of the fascial compartments of the
foot—the basis for fasciotomy in acute compartment syndromes. Foot
Ankle 1988;8:308-314.
MS, Berger BI. Nonunion of a fracture of the sustentaculum tali causing
a tarsal tunnel syndrome: a case report. Foot Ankle Int 1995;16:740-742.
DA, O’Byrne JM, McCabe JP, et al. Fractures of the os calcis: improved
results with internal fixation. Injury 1993;24:263-265.
D, Hall H. Intra-articular fractures of the calcaneus. A critical
analysis of results and prognostic factors. J Bone Joint Surg Am
1993;75A:342-354.
HV, Triffitt PD, Gregg PJ. Intra-articular fractures of the calcaneum
treated operatively or conservatively. A prospective study. J Bone
Joint Surg Br 1993;75B:932-937.
SJ, Hansen ST Jr, Sangeorzan BJ. The effect on ankle dorsiflexion of
gastrocnemius recession. Foot Ankle Int 2002;23:26-29.
SJ, Sangeorzan BJ, Hansen ST Jr. Surgical anatomy of the gastrocnemius
recession (Strayer procedure). Foot Ankle Int 2004;25:247-250.
M, Verbruggen JP, Brink PR. The relationship between the outcome of
operatively treated calcaneal fractures and institutional fracture
load. A systematic review of the literature. J Bone Joint Surg Am
2008;90A:1013-1021.
JL, Kirwan OE, Jackson AM. The long term results of conservative
management of severely displaced fractures of the calcaneus. J Bone
Joint Surg Br 1984;66B:386-390.
CS, Clare MP, Sanders RW. Subtalar fusion after displaced
intra-articular calcaneal fractures: does initial operative treatment
matter? J Bone Joint Surg Am 2009;91:541-546.
S, Gavlik JM, Barthel S, et al. The value of subtalar arthroscopy in
the management of intra-articular calcaneus fractures. Foot Ankle Int
2002;23:906-916.
DB, Ferretti AJ. Lateral subtalar joint dislocation: a case with
calcaneal fracture. J Am Podiatr Med Assoc 2004;94:65-69.
JA, Kreder HJ, Stephen D, et al. Should calcaneal fractures be treated
surgically? A meta-analysis. Clin Orthop 2000;217-227.
DJ, Oliveira ML, Campbell JT, et al. A biomechanical comparison of
locking and nonlocking plates for the fixation of calcaneal fractures.
Foot Ankle Int 2006;27:196-201.
M, Droste P, Goesling T, et al. Polyaxially-locked plate screws
increase stability of fracture fixation in an experimental model of
calcaneal fracture. J Bone Joint Surg Br 2006;88B:1257-1263.
M, Geerling J, Zech S, et al. Intraoperative three-dimensional imaging
with a motorized mobile C-arm (SIREMOBIL ISO-C-3D) in foot and ankle
trauma care: a preliminary report. J Orthop Trauma 2005;19:259-266.
M, Gosling T, Zech S, et al. A comparison of plates with and without
locking screws in a calcaneal fracture model. Foot Ankle Int
2005;26:309-319.
MM. Reconstructive osteotomy of the calcaneus with subtalar arthrodesis
for malunited calcaneal fractures. Clin Orthop 1993;157-167.
ZS, Feldman F, Singson RD, et al. Peroneal tendon injury associated
with calcaneal fractures: CT Findings. Am J Roentgenol AJR
1987;149:125-129.
CR, Sakellarides H, Freeman P, et al. Fractures of os calcis: a long
term follow-up study of one hundred forty-six patients. JAMA
1963;184:920.
HC, Papp S, DiPasquale T. The effect of suture pattern and tension on
cutaneous blood flow as assessed by laser Doppler flowmetry in a pig
model. J Orthop Trauma 2008;22:171-175.
R, Benamara A, Weissman SL. Functional treatment of intra-articular
fractures of the calcaneus. Clin Orthop 1976;115:236-240.
MA, Blum L. Sensory denervation of the heel for persistent pain
following fractures of the calcaneus. J Bone Joint Surg Am
1948;30A:209-212.
R, Fortin P, DiPasquale T, et al. Operative treatment in 120 displaced
intraarticular calcaneal fractures. Results using a prognostic computed
tomography scan classification. Clin Orthop 1993;87-95.
BJ, Ringler JR. Minimally invasive reduction and small fragment
fixation of tongue-type calcaneus fractures, OTA 17th Annual Meeting,
poster # 46 [Orthopaedic Trauma Association web site] 2001. San Diego,
CA, October 18-20, 2001.
TA, Bauer TW, Josten C, et al. Open reduction and augmentation of
internal fixation with an injectable skeletal cement for the treatment
of complex calcaneal fractures. J Orthop Trauma 2000;14:309-317. J Bone
Joint Surg Am 1963;45: 863-864.
D, Marsh JL, Leiter B. Clinical application of computerized axial
tomography (CAT) scanning in calcaneus fractures. Clin Orthop Relat Res
1985;199:114-123.
CH, Hansen M, Wolter D. Follow-up evaluation of open intra-articular
fractures of the calcaneus. Arch Orthop Trauma Surg 1998;117:442-447.
P, Santavirta S, Sandelin J. Surgical treatment of chronic dislocation
of the peroneal tendons. Br J Sports Med 1988;22:16-18.
MA, Gilula LA, Oloff LM, et al. CT scanning of the foot and ankle: 2.
clinical applications and review of the literature. Am J Roentgenol AJR
1986;146:1204-1214.
MA, Gilula LA, Oloff LM, et al. CT scanning of the foot and ankle: 1.
normal anatomy. Am J Roentgenol AJR 1986;146:1192-1203.
KS, Kang CH, Min BW, et al. Preoperative and postoperative evaluation
of intraarticular fractures of the calcaneus based on computed
tomography scanning. J Orthop Trauma 1997;11:435-440.
G, Pinsger M. Treatment of peroneal tendon dislocation by transposition
under the calcaneofibular ligament. Foot Ankle Int 1994;15:107-111.
HM, Sanders R. Calcaneal malunions: results of a prognostic computed
tomography classification system. Foot Ankle Int 1996;17:395-401.
JR. Displaced fractures of the os calcis involving the subtalar joint:
the key role of the superomedial fragment. Foot Ankle 1983;4:91-101.
JR. Treatment of displaced intra-articular fractures of the calcaneus
using medial and lateral approaches, internal fixation, and early
motion. J Bone Joint Surg Am 1987;69A:115-130.
JR. Surgical treatment of displaced intraarticular fractures of the
calcaneus. A combined lateral and medial approach. Clin Orthop
1993;68-75.
K, Booth G, Rohrl SM, et al. A comparison of conventional versus
locking plates in intraarticular calcaneus fractures: a biomechanical
study in human cadavers. Clin Biomech (Bristol, Avon) 2007;22:100-105.
J, Stehlik J, Rysavy M, et al. Minimally-invasive treatment of
intra-articular fractures of the calcaneum. J Bone Joint Surg Br
2006;88B:1634-1641.
TD, Calder PR, Salisbury RD, et al. The operative management of
displaced intraarticular fractures of the calcaneum: a two-centre study
using a defined protocol. Injury 2001;32:491-496.
H, Hufner T, Schratt HE, et al. [Treatment of intraarticular calcaneal
fractures in adults. A treatment algorithm]. Unfallchirurg
1999;102:152-166.
DB, Greene N, Shepherd L, et al. Facilitating edema resolution with a
foot pump after calcaneus fracture. J Orthop Trauma 1999;13:43-46.
DB, Krieger LE. Operative vs. nonoperative treatment of intra-articular
fractures of the calcaneus: a prospective randomized trial. Foot Ankle
Int 1996;17:2-9.
DB, Triffon MJ, Terk MR. Magnetic resonance imaging to detect avascular
necrosis after open reduction and internal fixation of talar neck
fractures. Foot Ankle Int 1996;17:742-747.
H, Zwipp H. Calcaneal fractures. In Tscherne H, Schatzker J, eds. Major
Fractures of the Pilon, the Talus, and the Calcaneus. Berlin:
Springer-Verlag, 1993:153-174.
TV, Buckley R. Age, gender, work capability, and worker’s compensation
in patients with displaced intraarticular calcaneal fractures. J Orthop
Trauma 2001;15:275-279.
NS, Haidukewych GJ. Locked fracture dislocation of the calcaneus
treated with minimal open reduction and percutaneous fixation: a report
of two cases and review of the literature. Foot Ankle Int
2003;24:796-800.
MW, Hildebolt CF, Gilula LA, et al. Calcaneal and pelvic fractures:
diagnostic evaluation by three-dimensional computed tomography scans. J
Digit Imaging 1991;4:143-152.
CD, Vaughan TK, Carr JB, et al. Fracture blisters: clinical and
pathological aspects [published erratum appears in J Orthop Trauma
1994;8(1):79]. J Orthop Trauma 1993;7:417-427.
M, Lehmann O, Sagesser D, et al. Limited open reduction and internal
fixation of displaced intra-articular fractures of the calcaneum. J
Bone Joint Surg Br 2008;90B:1608-1616.
RD, Zhang H, Bronson DG. Experimental tibial plateau fractures
augmented with calcium phosphate cement or autologous bone graft. J
Bone Joint Surg Am 2003;85A:222-231.
HH, Simon CG Jr. Self-hardening calcium phosphate composite scaffold
for bone tissue engineering. J Orthop Res 2004;22:535-543.
B, Bosch P. Closed reduction and percutaneous pinning for comminuted
intraarticular fractures of the calcaneus: preliminary results, OTA
15th Annual Meeting, Paper # 50 [Orthopaedic Trauma Association web
site] 1999. Charlotte, NC. October 22-24, 1999.
MG, Karges DE. Functional outcome of patients following open reduction
internal fixation for bilateral calcaneus fractures. Foot Ankle Int
2002;23:917-921.
H, Tscherne H, Thermann H, et al. Osteosynthesis of displaced
intraarticular fractures of the calcaneus. Results in 123 cases. Clin
Orthop 1993;76-86.
