ARTHRODESES OF THE FOOT AND ANKLE
painful, deformed, or unstable joint to produce a painless plantigrade
foot. This is achieved by resecting the articular surfaces, correcting
malalignment, and then using an appropriate method of internal fixation
to provide interfragmentary compression at the arthrodesis site. The
use of bone graft is usually not necessary in doing an arthrodesis
unless a defect is present. Adequate postoperative immobilization is
necessary to ensure that fusion occurs.
articular surfaces of the bones comprising a joint are removed and bone
union (fusion) is attempted, thereby effectively eliminating the motion
that normally occurs in the joint. Mobility of the adjacent joints
should be maintained whenever possible. Mobility of the joints of the
foot and ankle aids in shock absorption at the time of initial ground
contact and in producing stability within the foot at the time of heel
rise and toe off. Shock absorption within the ankle occurs through
dorsiflexion and plantar flexion, in the subtalar joint by eversion at
the time of initial ground contact, and at the transverse tarsal joint
by its flexibility at initial ground contact. Even the tarsometatarsal
joints have some motion that helps to absorb stress.
patient’s problem, the extent of the fusion should be minimized. If
only the subtalar joint is involved, then only the subtalar joint
should be fused rather than performing a triple arthrodesis. The motion
of the subtalar joint depends on movement within the talonavicular and
calcaneocuboid joints (transverse tarsal joint). If the talonavicular
joint is arthrodesed, motion of the subtalar joint is effectively
eliminated (10). An isolated calcaneocuboid
joint arthrodesis still permits about two thirds of subtalar motion. An
arthrodesis of the subtalar joint, however, permits
motion
to occur within the transverse tarsal joint (abduction–adduction).
Although the degree of motion within the midfoot area, namely the
intertarsal and tarsometatarsal joints, is minimal, arthrodesis in
these joints creates a rigid midfoot and forefoot so that there is
little or no accommodation of the forefoot to the ground during stance
phase. Therefore, in attempting a fusion of this type, line up the
forefoot as anatomically as possible to create a plantigrade forefoot.
painful joint, to correct a deformity, to produce stability, or a
combination of these. The pain in the joint is usually caused by
arthrosis, whether it be degenerative, traumatic, rheumatoid, or of
undetermined etiology. When the articular surfaces are no longer
congruent, or the articular cartilage has deteriorated, intractable
pain often results. Because the foot is a weight-bearing structure with
stress constantly applied to it, the pain may result in considerable
disability. Although some of these problems can be managed
conservatively with an orthotic device, eventually an arthrodesis is
required.
the foot or ankle to produce a plantigrade foot. At times the deformity
may cause pain resulting from an abnormal weight-bearing pattern that
places too much stress on a localized area of the foot. Sometimes after
trauma, such as a severe calcaneal fracture, an explosive-type fracture
of the navicular, or a Lisfranc fracture-dislocation, a significant
deformity may result that can be corrected with an arthrodesis.
Charcot-Marie-Tooth disease, a dropfoot secondary to a peroneal nerve
palsy, or a deficit following a compartment syndrome or poliomyelitis
may produce instability about the foot so that the foot cannot support
the body weight. The instability may be produced by rupture of a
tendon, such as the posterior tibial or the peroneal tendon. In such
cases, a significant degree of instability and possibly a deformity may
result that again may cause pain because of instability. In all of
these cases, an arthrodesis may be used to realign the architecture of
the foot to produce a plantigrade foot that will enable the patient to
ambulate with increased stability and little or no pain.
contemplated, several factors must be carefully considered. The soft
tissue covering the foot and ankle is such that there is often little
or no fatty tissue present. Therefore, the surgical approach must be as
precise as possible to avoid having to place undue tension on the skin
at the time of surgery, for fear that a slough might occur. The skin
flaps created must be full thickness with as little undermining as
possible. Keep in mind the location of the cutaneous nerves about the
foot and ankle. A technically good arthrodesis may not satisfy the
patient if a cutaneous nerve is caught up within the scar tissue or
sensation is impaired distally as the result of a cut nerve, making it
difficult for the patient to wear shoes comfortably. The major mixed
nerves running into the foot are susceptible to being cut or stretched,
resulting in loss of function.
fusion, no change in the overall position of the extremity is made;
when realignment is required, the deformed extremity must be carefully
examined and compared with the normal side. In this way, the overall
alignment of the limb (in regard to the varus–valgus alignment of the
hindfoot and forefoot) and the degree of rotation (internal and
external) of the extremity are determined. When an arthrodesis is
performed, restore normal alignment as much as possible.
ankle is the same as that for other joints: to ensure the best possible
chance for fusion, broad surfaces of cancellous bone must be brought
into apposition. When a realignment arthrodesis is being performed,
achieving broad bony surfaces is not difficult because a sufficient
amount of bone is removed during realignment of the joints. If,
however, an isolated talonavicular or calcaneocuboid joint fusion is
carried out and too much bone is removed from one side of the foot, a
forefoot deformity could result because of shortening of the medial or
lateral column. In this situation, adequate bony contact may be
impossible without incorporation of some type of bone graft.
bone graft, obtained either locally or from the iliac crest. Local bone
graft may be obtained just above the medial malleolus and from the
calcaneus. This is preferable to an iliac crest bone graft. The graft
may be in the form of a dowel or a rectangle of bone to be inlaid or
fragments placed between the bone surfaces. Regardless of the type of
fusion contemplated, the most important factor is careful surgical
technique to remove the cartilage and subchondral bone so that there is
good cancellous bone contact, which, with good internal fixation,
should then proceed to a satisfactory fusion.
internal fixation is usually necessary, such as pins, plates, staples,
or screws. The type of fixation depends on the surgeon’s preference and
the type of fusion. The following sections on each specific fusion
discuss our own methods, but there are many ways to carry out an
arthrodesis and insert internal fixation. Ours is based on our
experience as foot and ankle surgeons.
the foot and ankle involves careful assessment of the patient’s
problem. After obtaining a history from the patient
regarding
the complaint, perform a physical examination to look at the alignment
of the entire lower extremity. Assess the range of motion of the ankle,
subtalar, transverse tarsal, and metatarsophalangeal joints. Observe
the posture of the foot to see if the foot is plantigrade and, if not,
the reason for the abnormality. There may be multiple joint
involvement, as in the rheumatoid patient with involvement of the knee,
ankle, subtalar, and transverse tarsal joints. Assess the quality of
the skin because adherent skin or multiple scars may make it difficult
to expose the arthrodesis site safely. Last, assess the neurovascular
status of the foot and, if there are questions about the adequacy of
the circulation, do arterial Doppler studies.
usually requires an ankle–foot orthosis to immobilize a joint or
accommodate a deformity. As a general rule, however, most patients with
significant arthrosis are not comfortable in the long term with an
orthotic device and will usually require fusion.
important. Assess the involved joint or joints and decide on the extent
of fusion required. Minimize the number of joints to be fused to
maintain maximum flexibility of the foot and ankle. Decide whether an in situ fusion will be adequate or if some type of correction of a deformity needs to be achieved to create a plantigrade foot.
surgical procedure, including the possibility of failure of the
procedure, particularly of a nonunion.
arthrosis of the joint, malalignment, or both. There are many ways to
carry out an arthrodesis of the ankle joint; the one we describe here
is the transfibular approach, which we believe is the most utilitarian
type of fusion (1,7,23,24 and 25). Some authors advocate doing an in situ fusion arthroscopically, but this should be attempted only by a very experienced arthroscopist (5,6,12,26).
Most authors who initially touted this method of fusion now utilize a
limited approach to the ankle joint rather than carrying it out
arthroscopically. The most important factor in carrying out an ankle
arthrodesis is the alignment. The alignment of the ankle joint should
always be matched to the uninvolved normal side. The planes of
alignment include (a) dorsiflexion–plantar flexion, (b) internal and
external rotation, (c) varus–valgus, (d) medial–lateral displacement,
and (e) anterior–posterior displacement (3). These five planes must be taken into consideration when carrying out an ankle arthrodesis.
-
Approach the ankle joint through a
transfibular approach, which starts over the lateral aspect of the
fibula approximately 10 cm above the tip of the malleolus and carries
distally along the lateral side of the foot toward the base of the
fourth metatarsal (Fig. 115.1A). Create
full-thickness dorsal and plantar flaps in this inter nervous plane
down to bone. Continue subperiosteal dissection over the anterior
aspect of the tibia and ankle joint to the neck of the talus.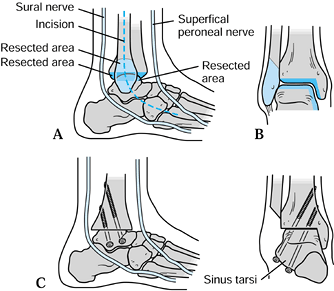 Figure 115.1. Ankle arthrodesis. A:
Figure 115.1. Ankle arthrodesis. A:
Placement of the incision between the superficial peroneal nerve and
the sural nerve. Note that the incision ends near the base of the
fourth metatarsal. B: Cuts made in the
fibula, distal end of the tibia, and talus. This creates the flat, bony
surfaces at the arthrodesis site. The fibular cut ends approximately
1.5 to 2.0 cm proximal to the level of the ankle joint. C:
Placement of 6.5-mm screws across the arthrodesis site. Note that the
screws are placed as longitudinally as possible and engage the cortex
on the medial aspect of the tibia. -
Posteriorly expose the fibula, releasing the peroneal tendons.
-
Distally identify the posterior facet of the subtalar joint as well as the tarsal sinus.
-
Excise the distal fibula by making an oblique cut in the fibula ending 1.5 cm proximal to the joint line (Fig. 115.1B).
-
Expose the posterior aspect of the tibia
by making an incision along its posterior aspect. Strip the soft tissue
along the posterior tibia distally to the calcaneus. Place malleable
retractors anterior and posterior to the tibia. -
Use an oscillating saw to remove the
articular surface of the tibia by transecting the tibia just proximal
to the subchondral bone, remaining as perpendicular as possible to the
long axis of the tibia. Cut from lateral to medial but not so far
medially that the medial malleolus is fractured by using first a short
wide and then a long wide saw blade. -
Remove approximately 2 to 3 mm of distal tibia, taking care to prevent fracturing the medial malleolus.
-
If it appears that the cut fragment is
too thick and a fracture of the medial malleolus may occur, make a
second approach along the anterior medial aspect of the joint. Make an
anterior medial longitudinal incision over the ankle joint and carry it
distally and obliquely around the medial malleolus. -
Expose the ankle joint, avoiding injury to the saphenous vein and nerve.
-
Use a 6-mm osteotome along the lateral
aspect of the medial malleolus to free up the distal tibial fragment to
prevent fracture of the medial malleolus when this bone fragment is
removed. Return now to the lateral wound and remove the distal tibial
fragment in its entirety. It is important that this cut be brought all
the way across to the lateral aspect of the medial malleolus. -
Place the foot into a plantigrade position, insofar as dorsiflexion–plantarflexion and varus–valgus are concerned.
-
If at this time there is a gap between
the talus and the distal tibial cut, the medial malleolus is likely
keeping the joint space from collapsing. In this situation, remove the
distal 6 to 8 mm of medial malleolus by cutting all soft tissue
attachments, avoiding injury to the posterior tibial tendon, artery,
and nerve. Once this piece of medial malleolus has been removed, the
joint space will readily collapse. -
With the foot held in neutral
dorsiflexion–plantarflexion and about 5° of valgus, excise the dome of
the talus with a saw cut that parallels the cut surface of the distal
tibia. Excise approximately 3 to 4 mm of talus. Once this has been
achieved, there should be a good bony apposition between the two cut
surfaces, and the foot should be in a plantigrade position. -
Remove the remaining articular cartilage along the lateral side of the medial malleolus and medial side of the talus.
-
If the bone in the distal tibia or talus
is sclerotic, make multiple drill holes. Bring the two broad, flat
surfaces of the tibia and talus together so that the anterior cut of
the tibia matches the anterior aspect of the cut in the talus. In this
way, the normal posterior contour of the heel is achieved. -
Check rotation by palpating the patella
and rotating the foot into the predetermined degree of external
rotation as well as the varus and valgus position of the hindfoot. Use
two 0.062-in. K-wires for preliminary fixation of the arthrodesis.
-
Remove the two K-wires and stress the fixation. There should be little or no motion present.
-
If there is some motion, insert a third
screw from the tibia, either medially or laterally, into the talus. If
the bone is soft, use washers. -
If there is lateral displacement at the
ankle, remove the medial malleolus, center the talus on the tibia, and
use multiple staples along the medial side for added internal fixation.
-
For internal fixation, we prefer two
interfragmentary screws, one starting in the sinus tarsi area and
inserted obliquely into the medial aspect of the distal tibia and the
other starting in the region of the lateral process of the talus almost
paralleling the screw in the sinus tarsi and again exiting along the
medial aspect of the tibia (20,21) (Fig. 115.1C). -
Insert the screw by first drilling a hole
with a 3.2-mm drill bit in the sinus tarsi at as oblique an angle as
possible to obtain the maximum amount of compression across the ankle.
It is important that the medial aspect of the tibial cortex is drilled.
Leave the drill bit in place and use a second drill bit to make the
hole in the lateral process. Be certain to leave sufficient bone along
the lateral side of the talus to provide adequate screw purchase in the
bone. The second drill hole should almost parallel the first, and
insert it at as longitudinal an angle as possible to gain the maximum
amount of compression across the arthrodesis. Once these two drill bits
have been inserted, there is good stabilization of the arthrodesis site. -
Remove the first drill bit, measure and
tap the hole, and insert a 6.5-mm long threaded screw. The screw must
engage the medial cortex of the tibia to gain maximum interfragmentary
compression. -
Next, remove the second drill bit and insert the next screw.
short-leg compression dressing incorporating plaster splints.
Approximately 10 days following surgery, remove the dressing. Remove
the sutures and apply a short-leg, non-weight-bearing cast for 6 weeks.
At 6 weeks, if on radiographs the arthrodesis site appears to be making
satisfactory progress. Apply a short-leg weight-bearing fiberglass
cast for another 6 weeks. As a general rule, the arthrodesis is solidly healed by 12 to 16 weeks (Fig. 115.2).
 |
|
Figure 115.2. Radiographs demonstrating ankle arthrodesis utilizing the technique described in the text. On the AP view (B),
note that the screws engage the medial cortex to maximize interfragmentary compression. It is also important that the threads are past the fusion site. |
arthrosis of the subtalar joint secondary to trauma, rheumatoid
arthritis, or a subtalar coalition (19,22,27,29).
Sometimes a subtalar arthrodesis is necessary to treat instability of
the subtalar joint secondary to rupture of the posterior tibial or
peroneal tendons or because of a marked valgus deformity secondary to
collapse of the telonavicular joint as a result of rheumatoid arthritis.
fracture, evaluate whether any lateral impingement is present between
the calcaneus and fibula so that it can be corrected at the same time.
fusion without the addition of bone graft from another site, although
sometimes when attempting to correct a severe valgus deformity of the
subtalar joint, a bone graft may be required to fill the gap created
along the lateral aspect of the joint. In the occasional patient with
severe collapse of the calcaneus secondary to trauma, we insert a bone
block to restore the anatomic relationship between the talus and
calcaneus.
-
Begin the skin incision at the tip of the fibula and carry it distally just proximal to the base of the fourth metatarsal (Fig. 115.3).
The incision should be dorsal to the sural nerve, although a smaller
anterior branch may be present that should be looked for and protected.
Carry the incision down to the fascia overlying the extensor digitorum
brevis muscle. Detach the origin of the muscle from the lateral aspect
of the subtalar joint and reflect it distally to the level of the
calcaneocuboid joint.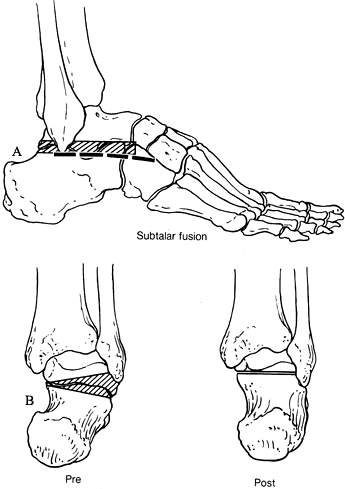 Figure 115.3. A: Incision for subtalar fusion; shaded area indicates bone to be resected. B: Correction of varus deformity.
Figure 115.3. A: Incision for subtalar fusion; shaded area indicates bone to be resected. B: Correction of varus deformity. -
Visualize the subtalar joint by removing
the fat pad from the sinus tarsi and stripping the joint capsule along
the lateral side of the posterior facet to delineate the posterior
facet and posterior aspect of the subtalar joint. -
Facilitate exposure of the posterior
facet by using a lamina spreader in the sinus tarsi to open the joint.
Use a sharp curet to methodically remove the articular cartilage from
the entire posterior facet and by reaching across the sinus tarsi, the
middle facet. -
Remove the lamina spreader and assess the
alignment of the subtalar joint. The fusion should place the subtalar
joint in 5° to 7° of valgus in relation to the long axis of the lower
extremity. -
If in situ
fusion is to be achieved, feather the bone with a small osteotome and
insert internal fixation. If a varus deformity needs to be corrected,
remove a wedge of bone 3 to 5 mm in width from the lateral aspect of
the posterior facet to realign the hindfoot. If a valgus
P.3062
deformity is to be corrected, a piece of iliac crest bone used as a strut in the subtalar joint may be necessary. -
When an in situ
fusion is done, local bone graft can be acquired by harvesting the
anterior process of the calcaneus, avoiding the articular surface of
the calcaneocuboid joint. This can be morselized and packed into the
sinus tarsi. If more bone graft is required, then we obtain the graft
above the medial malleolus. -
Feather the bone surfaces of the
posterior and middle facets and sinus tarsi with a 4- or 6-mm
osteotome. This elicits a healing response, increases the bony
surfaces, and increases the chances of successful fusion. -
For internal fixation, we prefer a 7.0-mm
fully threaded cannulated screw inserted from the posterior aspect of
the calcaneus just off the weight-bearing area to the neck of the
talus. We overdrill the calcaneus with a 7.0-mm drill to create a glide
hole to achieve intrafragmentary compression between the talus and
calcaneus. -
Insert a guide pin from the posterior
inferior aspect of the calcaneus about 1 cm above the weight-bearing
area utilizing an anterior cruciate guide device to direct the guide
pin into the posterior facet of the subtalar joint approximately in the
midline and about 3 to 5 mm posterior to the anterior edge of the
posterior facet. This ensures that the screw remains within the
posterior facet rather than traversing the sinus tarsi. -
Once the guide pin has been placed in the
calcaneus, remove the anterior cruciate guide, manipulate the calcaneus
into 5° of valgus, and insert the guide pin into the neck of the talus.
Use fluoroscopy to ensure proper placement of the guide pin. The guide
pin should be entirely within the posterior facet of the subtalar joint
and in the neck of the talus. The advantage of this technique is that
with only a guide pin in place, the alignment of the subtalar joint can
be checked to be certain that it is correct. If the alignment is not
satisfactory, back out the guide pin, reposition the calcaneus, and
reinsert the guide pin. -
Once the alignment is satisfactory, make
a transverse incision on the heel along the pin in the calcaneus. Make
this incision large enough to easily seat a washer without crushing the
surrounding fatty tissue. Measure for screw length and then drill the
guide pin through the skin on the anterior aspect of the ankle. This
permits the guide pin to be gripped so that it is not accidentally
withdrawn during the drilling of the hole. Use a 4.5-mm drill to drill
a hole through the calcaneus and talus, following with a 7.0-mm drill
to create the glide hole only in the calcaneus. -
Tap the talus and insert a 7.0-mm fully threaded screw with a washer, achieving excellent interfragmentary compression.
-
If by chance there is any rocking or
motion at the subtalar joint, insert a 1/8-inch smooth Steinmann pin
for additional fixation. This is very rarely needed. -
Check the length of the screw by fluoroscopy, and if it is satisfactory, remove the guide pin.
-
Pack bone graft into the sinus tarsi.
-
Suture the extensor digitorum brevis back to its origin and close the skin.
-
Apply a short-leg compression dressing incorporating plaster splints.
-
Under certain circumstances following a
calcaneal fracture, when there is lateral impingement of the calcaneus
against the fibula, the lateral wall of the calcaneus is removed in
line with the lateral aspect of the articular surface of the talus. In
this way, the peroneal tendons are decompressed. This bone can be
utilized for bone graft if necessary.
cast. Remove sutures and apply a short-leg non-weight-bearing cast,
which is kept in place for 6 weeks. At 6 weeks, if satisfactory healing
of the arthrodesis is seen on radiographs, permit walking in the
short-leg walking cast for another 6 weeks. Solid fusion usually occurs
by 10 to 12 weeks (Fig. 115.4).
 |
|
Figure 115.4. Radiograph demonstrating a subtalar fusion utilizing the technique described in the text.
|
the talonavicular joint that may be caused by trauma or degenerative or
rheumatoid arthritis (11). Subluxation of the
talonavicular joint secondary to rheumatoid arthritis or posterior
tibial tendon dysfunction is also an indication for an isolated
talonavicular fusion (9,15).
As a general rule, if the patient is older than 50 years of age, an
isolated fusion is probably adequate. If the patient is younger than 50
years old or is very active, the calcaneocuboid joint should be
included for increased stability. Careful evaluation is necessary to
determine whether an isolated talonavicular fusion will achieve
satisfactory realignment of the foot or whether the calcaneocuboid
and/or subtalar joints should also be incorporated. If it seems that
too much bone will be removed from the medial column when doing the
talonavicular fusion, thereby producing an adducted position, always
include the calcaneocuboid joint so that a balanced foot will result.
Keep in mind that fusion of the talonavicular joint renders the
subtalar joint nonfunctional. Therefore, it is essential that the
subtalar joint be placed in 5° of valgus when the talonavicular joint
is fused; otherwise a nonplantigrade foot will result.
-
Approach the talonavicular joint
medially. Start the incision about 1 cm distal to the tip of the medial
malleolus and carry the incision along the midline of the foot to the
naviculocuneiform joint (Fig. 115.5). In this
area there are no superficial nerves of significant concern. Some
surgeons prefer to make a slightly dorsally curved incision to approach
the talonavicular joint, which is also satisfactory. When making a
slightly dorsally curved incision, avoid injury to the saphenous nerve,
which accompanies the saphenous vein.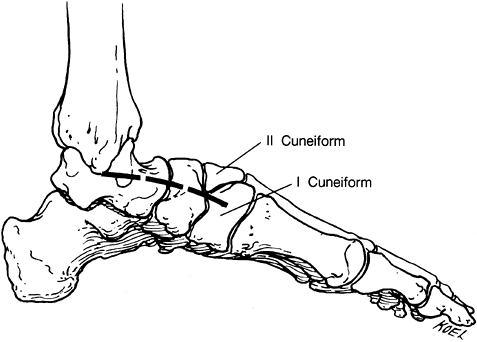 Figure 115.5. Incision for talonavicular fusion.
Figure 115.5. Incision for talonavicular fusion. -
Palpate the talonavicular joint to be
certain the proper joint is being exposed, because confusion can arise
in this area. Once the talonavicular joint is identified, strip the
capsular tissue along its medial aspect and then onto its dorsal and
plantar aspects. -
If dorsal spurs are present, remove them.
Decortication of the talonavicular joint is sometimes difficult because
of limited exposure. It is often helpful to place a large towel clip
into the medial aspect of the navicular and pull the foot into a
slightly adducted position, which facilitates exposure of the joint.
-
In a large person, a 7.0-mm cannulated screw can be utilized.
-
Where poor bone stock is present, multiple staples from a power stapilizer can be used.
-
Meticulously remove all of the articular cartilage. Once this is achieved, heavily feather the talar head and the navicular.
-
Manipulate the foot to assure that there
will be adequate bony apposition when the foot is placed into a
plantigrade position. If too much adduction will occur without bone
grafting, insert bone graft or include the calcaneocuboid joint in the
fusion. -
We prefer fixation with two 4.0-mm
cannulated screws inserted from the naviculocuneiform joint. Place the
foot in a plantigrade position with the subtalar joint in 5° of valgus
and the forefoot in neutral abduction–adduction. Correct any forefoot
varus by plantarflexing the navicular on the head of the talus. -
Insert a guide pin across the
talonavicular joint and a second guide pin just inferior to it. Verify
the position on fluoroscopy. -
Insert two 4.0-mm cannulated screws with washers, which produce good interfragmentary compression.
-
Close the wound in layers and apply a short-leg compression dressing incorporating plaster splints.
approximately 10 days and place the patient into a short-leg
non-weight-bearing cast, which is changed 6 weeks after surgery. If
there is radiographic evidence of healing at that time, allow
ambulation in a short-leg walking cast for another 6 weeks. As a
general rule, fusion occurs by 12 to 16 weeks (Fig. 115.6).
 |
|
Figure 115.6. Talonavicular arthrodesis using 6.5-mm screw and two small staples. A: Arthrosis of the talonavicular joint. B: Method of internal fixation. C: Degenerative arthritis of the talonavicular joint, anteroposterior radiograph. D: Fixation of talonavicular joint using compression screw and staple.
|
and calcaneocuboid joints. It is indicated when there is deformity
secondary to rupture of the posterior tibial tendon or after trauma in
which the transverse tarsal joints (talonavicular and calcaneocuboid)
have been disrupted without involvement of the subtalar joint (4,8).
Consider doing a double arthrodesis when an active patient who
otherwise would require only an isolated talonavicular or
calcaneocuboid joint fusion will be placing a great deal of stress on
the foot. A more stable foot results. A single arthrodesis can give a
most satisfactory result, but we believe that in the higher-performance
patient, adding the other joint enhances the stability of the foot and
thus makes it more functional. Performing a double arthrodesis
essentially eliminates all subtalar joint motion because subtalar
motion depends on rotation of the navicular on the talus and to a
lesser degree the calcaneocuboid joint. The advantages of a double
arthrodesis over a triple arthrodesis are that the former has decreased
morbidity and there is one less joint to fuse.
-
Approach the talonavicular joint as
previously described. Approach the calcaneocuboid joint through a
longitudinal incision centered over the calcaneocuboid joint; make this
incision cautiously because the sural nerve is in the area. Carefully
identify and retract the sural nerve if possible. Deepen the incision
to expose the calcaneocuboid joint and expose the joint
subperiostially. Sometimes the lateral aspect of the talonavicular
joint can be decorticated through this incision as well. -
If the procedure is to be done in situ,
the alignment of the foot is not a significant problem, but if there is
deformity, the joint surfaces must be realigned. Decorticate and
feather the joint surfaces with a 4- or 6-mm osteotome, as previously
described. -
Before internal fixation, a plantigrade
foot must be achieved because there will be no functional subtalar
joint motion following the double arthrodeses. Place the subtalar joint
in 5° of valgus, place the forefoot in neutral abduction–adduction, and
correct any forefoot abnormality, particularly varus, by plantarflexing
the navicular on the head of the talus. -
Fix the talonavicular joint as described
previously with two 4.0-mm cannulated screws or a 7.0-mm cannulated
screw, or with multiple staples. We fix the calcaneocuboid joint with
two 4.0-mm cannulated screws or multiple staples, depending on the
quality of the bone. -
After surgery, keep the patient in a short-leg compression dressing incorporating plaster splints.
remove sutures, and apply a short-leg, non-weight-bearing cast for 6
weeks. At this point, if there is radiographic evidence of healing,
place the patient into a short-leg walking cast for another 6 weeks.
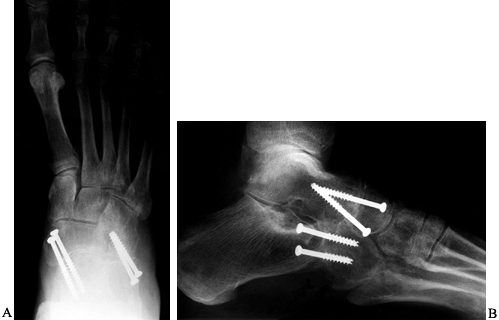
Fusion usually occurs by 12 to 16 weeks (Fig. 115.7).
 |
|
Figure 115.7. AP (A) and lateral (B) radiographs following a double arthrodesis utilizing 4.0-mm cannulated screws.
|
arthrosis, or a deformity caused by rheumatoid arthritis or trauma (2,13,14,30). The triple arthrodesis involves fusion of the subtalar, talonavicular, and calcaneocuboid joints. The fusion may be an in situ
arthrodesis, which is relatively simple to achieve; however, when
realignment of the foot is required, this procedure can be technically
extremely difficult. It can be used to correct a cavus deformity as
well as a flat foot deformity. It is not within the scope of this
section, however, to discuss all of the various types of triple
arthrodeses.
-
Use two skin incisions to adequately
expose the joints to be fused. Expose the subtalar and calcaneocuboid
joints through a longitudinal incision starting at the tip of the
fibula and carried toward the base of the fourth metatarsal (Fig. 115.8A).
Expose the talonavicular joint through a longitudinal incision
beginning at the tip of the medial malleolus and extended to the area
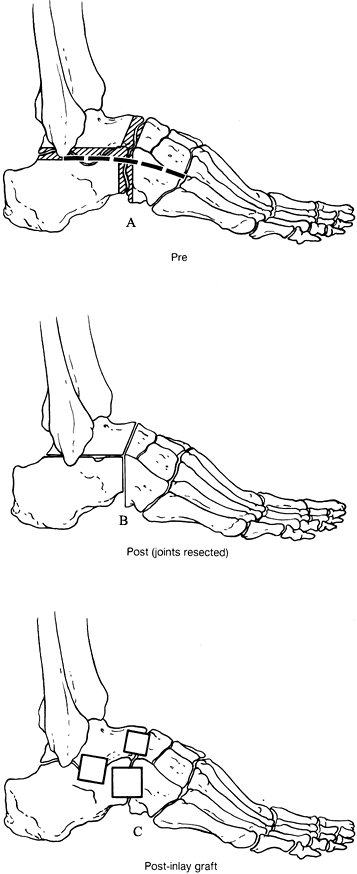
of the naviculocuneiform joint (Fig. 115.5).![]() Figure 115.8. Triple arthrodesis. A: Dashed line indicates incision; shaded area is bone to be resected. B: Appearance of the joint after preparation of the surfaces. C:
Figure 115.8. Triple arthrodesis. A: Dashed line indicates incision; shaded area is bone to be resected. B: Appearance of the joint after preparation of the surfaces. C:
An alternative technique involves stabilizing the joints with
rectangular bone graft inlays; this may be combined with the procedure
shown in Fig. 115.3B. -
Once the joints are exposed, decorticate
them as previously described. As a rule, when performing a triple
arthrodesis, we prefer to decorticate the surfaces to obtain good bony
apposition; others, however, prefer to inlay dowels or rectangular
pieces of bone from the iliac crest (Fig. 115.8B, Fig. 115.8C).
Both techniques produce satisfactory results; however, we prefer not to
use iliac crest bone graft if possible because of increased morbidity. -
If there is malalignment that needs
correction, some bone may have to be resected to produce a plantigrade
foot. The decortication of the subtalar joint is the same as previously
described for subtalar joint fusion. The decortication of the
talonavicular and calcaneal joints is the same as for a double
arthrodesis. -
Once the joint surfaces have been
prepared, place the foot into a plantigrade position with the hindfoot
in 5° of valgus and the transverse tarsal joint in neutral
abduction–adduction and correct any forefoot deformity, particularly
forefoot varus, by plantar flexing the navicular on the head of the
talus. If a plantigrade foot cannot be achieved, then resect bone as
necessary to correct the deformity. Heavily feather and then internally
fix the joints. -
Fix the subtalar joint with a 7.0-mm
cancellous screw, as described previously, and then stabilize the
talonavicular joint followed by the calcaneocuboid joint. After
surgery, keep the patient in a short-leg compression dressing
incorporating plaster splints for about 10 days, followed by a
short-leg, non-weight-bearing cast.
radiographs, and, if early union is occurring, place the patient into a
short-leg walking cast. Fusion usually occurs by 12 to 16 weeks (Fig. 115.9).
 |
|
Figure 115.9. Radiographs of a triple arthrodesis. A: Fixation of the triple arthrodesis utilizing screws. B:
Triple arthrodesis utilizing staples and screws in a patient whose bone stock was not sufficient to obtain adequate fixation utilizing only screws. |
arthrodesis, usually at the talonavicular joint. If symptomatic, it
should be surgically repaired. This is most easily accomplished by
inlaying or rotating a block of bone within the nonunion site.
too much varus or valgus or the forefoot is placed into too much
adduction, abduction, pronation, or supination. This results in
abnormal weight bearing, and it usually cannot be compensated for with
an orthotic device or shoe modification, so a revision of the triple
arthrodesis may be necessary. The revision is done with the same
surgical approach as outlined for the triple arthrodesis. If the
forefoot is in too much abduction or adduction, shorten the medial or
lateral column of the foot by resecting more bone from the appropriate
side to realign the foot. If a pronation or supination deformity of the
forefoot also exists, realign by rotation through the transverse tarsal
joint. Careful alignment of the forefoot to the hindfoot is needed to
obtain a plantigrade foot.
performed for primary arthrosis or posttraumatic arthrosis. Arthrodeses
in the tarsometatarsal area may involve a single joint, such as the
first metatarsocuneiform joint, or multiple joints (16). An in situ fusion may be all that is required. If there is deformity, correct it.
the arthrodesis need include only the metatarsal and cuneiform joints.
If, however, the cuneiforms have also been disrupted, then a block
fusion incorporating the cuneiforms and metatarsals is needed.
Sometimes after a Lisfranc fracture dislocation, the fourth and fifth
metatarsal cuneiform joints are involved, and thus, fusion of these
joints must be included.
arthrodesis are that there is little soft-tissue coverage, and the
nerves over the dorsum of the foot are extremely sensitive to pressure.
Even when the nerves are identified during the surgical approach, the
pressure from a retractor may cause a neuropraxia, which often will
resolve.
tarsometatarsal joint. These may involve decortication of the bony
surfaces and internal fixation; others recommend using various types of
dowels (17). We prefer to decorticate the bony surfaces, perform a reduction, and insert internal fixation (18,28).
-
If only a first metatarsocuneiform
arthrodesis is to be done, use a medial approach to expose the first
metatarsocuneiform joint. Center the incision over the first
metatarsocuneiform
P.3068
joint
and carry it down through the subcutaneous tissue to expose the bone.
There is no nerve in the way when a direct medial approach is used, but
if a dorsal medial approach is used, carefully identify and retract the
dorsal medial cutaneous nerve. Once the first metatarsocuneiform joint
is identified, reflect the capsule along the dorsal, medial, and
plantar aspects. -
Meticulously decorticate the first
metatarsocuneiform joint, which is a sinusoidal shape so that sometimes
debriding the plantar aspect of the joint is difficult. Once this has
been achieved, place the joint in the same degree of
abduction–adduction and plantarflexion as on the uninvolved foot.
Usually the joint will fall into place once all of the soft tissues
have been released and the joint surfaces are decorticated. If a
deformity is present, some bone may need to be removed to realign the
joint, but this is rarely necessary. Then heavily feather the joint
surfaces with a 4-mm osteotome. -
There are several ways to fix the joint,
but we prefer to utilize 4.0-mm cannulated screws, one from the
metatarsal into the cuneiform and the other from proximally in the
cuneiform into the first metatarsal. This pattern of screws gives
rather rigid fixation of the joint. -
If multiple metatarsocuneiform joints
need to be arthrodesed, or if the fusion mass needs to include the
cuneiforms themselves, then two incisions are used. The first incision
is the medial incision just described, and the second incision is
placed just along the lateral aspect of the second metatarsal. The
lateral approach to the second metatarsocuneiform region must be made
cautiously because the neurovascular bundle lies just lateral to the
extensor hallucis longus tendon. After the skin incision is made and
the superficial fascia is opened, take care to expose the cutaneous
nerves. We have found it simplest to approach this area by working
through the medial incision and stripping the soft tissues over the
dorsum of the foot as far as possible. Usually this dissection can be
carried along the skeletal plane, thereby passing beneath the
neurovascular bundle to about the lateral side of the middle cuneiform.
When the lateral incision is deepened to the level of the skeletal
plane, most of the soft tissues will have already been elevated,
protecting the neurovascular bundle. -
Once all the involved joints have been
decorticated, reduce the first metatarsocuneiform joint. Following
this, carefully check the alignment of the remainder of the joints to
see whether any bone needs to be removed. Usually bone does not need to
be removed because most deformities can be corrected by fully
mobilizing the tarsometatarsal joints. Feather all of the joints to be
arthrodesed with a 4-mm osteotome. -
Fix the first metatarsocuneiform joint with two crossed 4.0-mm cannulated screws as previously described.
-
Next, reduce and fix the second
metatarsocuneiform joint, starting the screw distally in the metatarsal
and inserting it proximally across the metatarsocuneiform joint into
the second cuneiform. If the cuneiform joints are included in the
fusion mass, place a transverse screw from medial to lateral across the
cuneiforms. If the third metatarsocuneiform joint is to be included,
insert an oblique screw from distally in the third metatarsal and
proximally into the third cuneiform. Occasionally, in a large person or
one in whom some instability still seems to be present after the screws
have been inserted, place a crossing screw from the first metatarsal
into the cuneiform or occasionally a screw from the medial cuneiform
into the third metatarsal base. Sometimes arthrosis is present at the
naviculocuneiform joint, which then needs to be incorporated into the
fusion. -
As a general rule, fusion of
metatarsocuneiform joints 1, 2, and 3 is adequate. If the fourth and
fifth metatarsal cuboid joints need to be arthrodesed, then try not to
fuse from the cuboid to the lateral cuneiform so that motion can still
be present between the medial and lateral arches of the foot. If,
however, severe arthrosis is present in this area, then it must be
included in the fusion, but a stiffer foot will result. -
On completion of the arthrodesis, the
wounds need to be carefully closed because the skin over the dorsum of
the foot is extremely thin and sensitive to pressure. -
After surgery, place the foot into a short-leg compression dressing incorporating plaster splints.
non-weight-bearing cast for approximately 1 month. If radiographic
union seems to be occurring, use a short-leg walking cast until fusion
is complete at 10 to 12 weeks (Fig. 115.10).
 |
|
Figure 115.10. Radiographs following tarsometatarsal fusions. A: Arthrosis of the second tarsometatarsal joint. B,C: Arthrodesis of the second tarsometatarsal joint utilizing 4.0-mm screws. D: Preoperative radiograph demonstrating primary arthrosis of the tarsometatarsal joints 1, 2, and 3. E: Postoperative radiograph demonstrating realignment and fusion. F: Preoperative radiograph demonstrating advanced arthrosis of the first tarsometatarsal joint. G: Postoperative radiograph following arthrodesis, demonstrating improvement in the height of the longitudinal arch.
|
the arthrodesis with 0.25% plain bupivacaine (Marcaine). This provides
the patient with some initial postoperative analgesia. Once the patient
is in the recovery room, have the anesthesiologist do a popliteal
block. This provides the patient with anesthesia below the knee that
lasts from 18 to 36 hours. Controlling the initial postoperative pain
reduces narcotic requirements significantly. If the patient has too
much pain the day following surgery, which occurs in about 10% to 15%
of cases, do a second popliteal block. By utilizing this type of
analgesia, most of our arthrodeses are carried out as outpatient
procedures with a minimum amount of patient morbidity.
amount of trauma to the tissues, particularly in the hindfoot and
midfoot. Unfortunately, there is not a great deal of soft tissue
coverage in this area, so swelling must be carefully controlled with
the postoperative dressing. Use a firm compression dressing along with
splints for the immediate postoperative period. This firm dressing
helps control the initial swelling but also permits expansion, which is
important to accommodate the postoperative swelling. Following the
initial postoperative period, after the sutures are removed, a firm,
well-fitting cast may be applied. The patient should be kept from
weight bearing on the foot until union is well under way in the
presence of good internal fixation—about 6 weeks.
infection, nonunion, malalignment, skin slough, and nerve entrapment,
among others.
arthrodesis is performed may help decrease the incidence of infection,
but good surgical technique and careful handling of tissues are the
most important factors in minimizing the risk of infection.
Unfortunately, about 0.5% to 1% of cases become infected following
surgery and need to be treated vigorously with debridement and
antibiotic therapy.
Minimize the risk by proper preparation of the bone surfaces and
adequate internal fixation, using good postoperative immobilization.
Sometimes dysvascularity of the bone prevents satisfactory arthrodesis.
This may occur at the talonavicular joint if the navicular is avascular
secondary to an old crush injury or when an ankle or subtalar
arthrodesis is done if the body of the talus has avascular necrosis.
Rather than attempting to fuse to a bone that appears avascular, excise
the avascular bone and graft into bones that have normal blood supply.
If a nonunion occurs and is symptomatic, revision is necessary with
excision of the nonunion site and either bone grafting or
reestablishing adequate bone apposition along with internal fixation.
there is little soft tissue coverage about the foot and ankle, a skin
slough may occur because of excessive pressure from retractors or
because of marginal skin from previous surgery or trauma. Too tight a
postoperative dressing can compromise skin as well. The best treatment
is prevention. When a skin slough occurs, debridement may be necessary,
followed by a skin graft or pedicle to close the defect if it is too
large. Small marginal sloughs will heal on their own with serial
dressing changes.
the patient’s shoe puts pressure against the involved area. The patient
may then be unhappy in spite of a satisfactory arthrodesis. For
persistent pain and disability, excise the neuroma and resect the nerve
back to normal soft tissues if possible. Because there is little soft
tissue coverage about the foot, it may be necessary to place the end of
the nerve into the bone to relieve symptoms.
for both patient and surgeon. Careful preoperative planning is
necessary to prevent malalignment. Carefully assess the alignment of
the entire lower extremity before attempting fixation of the
arthrodesis site. Take into account the alignment of the foot with the
patella because aligning the foot only to the distal tibia may result
in mal alignment. Malalignment that cannot be compensated for by the
use of an orthosis or shoe modification necessitates a revision of the
arthrodesis site.
procedures, take great care to realign the forefoot to the hindfoot. It
is not enough to align the hindfoot with the leg and not take into
account the alignment of the forefoot on the hindfoot.
relief and create a plantigrade foot. There are many pitfalls,
unfortunately, along the way to obtaining a satisfactory fusion, but
with careful preoperative planning, meticulous surgery, and rigid
internal fixation, a satisfactory outcome can usually be achieved. In
our experience, the patients who are least satisfied are the ones who
have malalignment of the extremity resulting in a nonplantigrade
foot. The possibility of nonunion is always present but can usually be avoided by good surgical technique.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
JH, Kirkos JM, Provellegios SM, Zachos AD. Long-Term Result of Triple
Arthrodesis: Forty-two Cases Followed for Twenty-Five Years. Foot Ankle Int 1994;15:548.
RA, Prieskorn D, Sobel M. Midtarsal and Tarsometatarsal Arthrodeses for
Primary Degenerative Osteoarthrosis or Osteoarthrosis after Trauma. J Bone Joint Surg 1996;78A:1376.