Anatomy of the Lumbar and Sacral Plexus
II – Single-Injection Peripheral Blocks > B – Lower Extremity >
11 – Anatomy of the Lumbar and Sacral Plexus
essential to perform peripheral nerve blocks, it is important to
recognize that variations are frequent and that “normal anatomy” is
found in only 50% to 70% of cases.
the anterior roots from L1 to L3 and the greater part of L4. It has a
triangular form, with its base resting against the lumbar vertebrae and
veretrebral transverse process and its apex formed by the union of the
third roots with the ascendant rami of the fourth. There is frequent
anastomosis between the upper part of the plexus with the subcostal
nerve and between the L4 rami and the lumbosacral trunk. As with the
brachial plexus, we can describe a pre- or a postfixed plexus with
respect to the main anastomosis; however, an important characteristic
of lumbar plexus anatomy is its great variability and frequent
asymmetry. The best definition is given by Bonniot: “The superior limit
corresponds to the first roots where the first collateral of the lumbar
plexus originate, and the inferior part is defined by the first roots
entirely distributed to the sacral plexus” (1922).
fibers for the three main trunks of the lower limb: the femoral,
obturator, and sciatic nerves (lumbosacral trunk). This may explain the
effectiveness of the posterior approach of the lumbar plexus at the L4
level for hip surgery.
process between the two parts of the psoas muscle. All of the branches
of the lumbar plexus emerge from the psoas muscle and all leave the
pelvis, though, not all by the same path. Near the vertebral body, the
psoas muscle is divided into two planes: a superficial plane that
arises from the lateral faces of the vertebral bodies from T12 to L4
and a deep plane arising from the transverse process
of
L1 to L5. Within these two planes lie the trunks of the lumbar plexus
and the ascending lumbar vein. In addition, the lumbar arteries, which
supply the psoas muscle, provide branches for the plexus. The two parts
of the muscle then fuse to form the psoas major.
 |
|
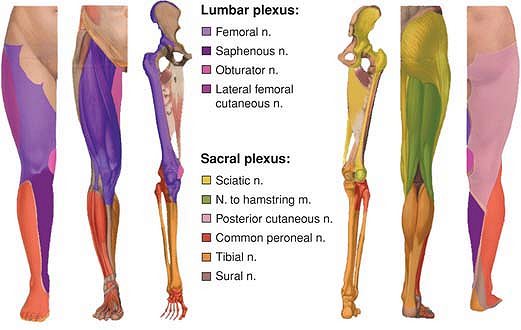
Figure 11-1. Lumbar plexus and sacral plexus nerves.
|
and the psoas muscles—six branches originate from the lumbar plexus.
They are classified either as collateral or terminal branches.
psoas muscle and runs down and laterally along the anterior face of the
quadratus lumborum muscle. Close to the iliac crest, it runs between
the transversus abdominis and the oblique muscles. It leaves a lateral
branch for the anterosuperior part of the buttock, supplying the skin
as far as the greater trochanter (55% of cases). Variations are
possible, however, including a shorter branch that does not reach the
greater trochanter (20%) and a longer branch that extends beyond it
(15%). The nerve divides into two branches: an abdominal branch, which
supplies the muscles and skin of the inferior part of the abdomen, and
an inguinal branch, supplying the skin of the pubis and the scrotum
(men) or labium majus (women). The inguinal branch perforates the
internal oblique muscle and then runs between the oblique muscles.
nerve. Its diameter is inversely proportional to that of the
iliohypogastric nerve, and it may be absent in some cases. It gives
rise
to
an abdominal branch, which is frequently anastomosed with the abdominal
branch of the iliohypogastric nerve, and the inguinal branch, which
supplies the skin of the superior and medial aspects of the thigh and
the genital area. It can replace the genital branch of the
genitofemoral nerve and all or part of the lateral femoral cutaneous
nerve.
 |
|
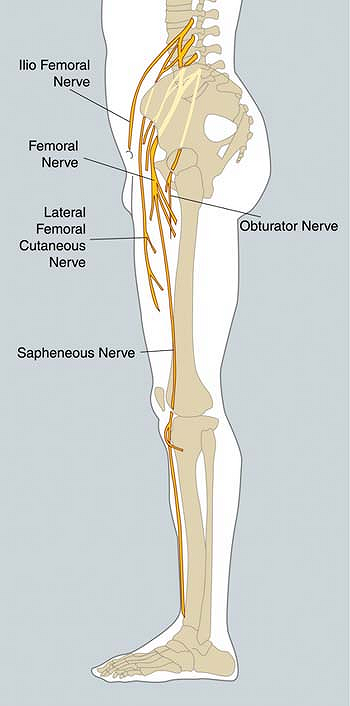
Figure 11-2. Lumbar plexus collateral and terminal nerves.
|
its anterior face before dividing into genital and femoral branches.
The genital branch passes through the inguinal canal and supplies the
cremaster muscle and the skin of the pubis and scrotum (or labium
majus). The femoral branch enters the thigh under the inguinal ligament
in the femoral sheath and then supplies the skin of the upper part of
the femoral triangle. This branch is probably the most variable of the
lumbar plexus. It supplies an important part of the anterior aspect of
the thigh. In some cases, it receives an anastomosis from T12, and
sometimes it is completely absent, in which case it is replaced by the
ilioinguinal and the lateral femoral cutaneous nerve.
cutaneous nerve follows an oblique and lateral course between the iliac
muscle and the fascia iliaca in the direction of the anterosuperior
iliac spine. It provides branches for the peritoneum. It then enters
the thigh by passing through or under the inguinal ligament and then
divides into a posterior branch, which supplies the skin of the
superior and lateral aspects of the thigh, and an anterior branch,
which supplies the anterolateral part of the thigh as far as the knee.
Variations in the course of this nerve are described in 25% of cases,
and it may arise directly from the femoral nerve in 18% of cases.
Variability also exists with respect to the superficial territories
supplied by this nerve. In 31% of cases, this innervation may extend
medially as far as the anterior surface of the thigh. This may
represent a possible explanation for failure of anesthesia in this
region after femoral block in some patients. The lateral femoral
cutaneous nerve is considered by some as a branch of the femoral nerve
that leaves the femoral nerve after its origin.
their courses and their extension territory. These variations explain
why anesthesia of the anterior face of the thigh is difficult to
anticipate both with a femoral block and with a posterior approach.
However, it is important to recognize that all of the cutaneous
branches of these nerves are mainly subaponeurotic and therefore can be
blocked with a subcutaneous injection at the level of the inguinal
crease.
of the sacroiliac joint. It runs outward and downward close to the
ureter and the internal iliac artery. Its position in the pelvis, after
it leaves the psoas muscle, explains why extension of anesthesia to
this nerve after an anterior approach (three-in-one or iliofascial
block) is unlikely. It reaches the obturator groove at the upper part
of the obturator foramen and then enters the thigh. It then divides
into an anterior and a posterior branch. In 50% of cases, this division
occurs in the obturator groove, but it may also occur before or after
the groove. In the pelvis, it sometimes provides a ramus for the
articular capsule of the hip joint. This represents an additional
argument for using a posterior lumbar plexus approach for hip surgery.
adductor magnus muscles and behind the adductor longus. It innervates
the pectineus, adductor longus, gracilis, and adductor brevis muscles.
It typically supplies a limited skin territory at the medial surface of
the thigh and the knee. However, there are important variations in the
location and extent of this area. The frequent anastomosis of the
anterior branch with the saphenous and anterior femoral cutaneous
nerves in the adductor canal (the subsartorial plexus) is responsible
for significant overlaps. It has been established that an effective
block of the obturator nerve is associated with no sensory block in 57%
of patients in the presence of a reduction of the adduction motor
function. For German anatomists the specific sensitive area of the
obturator nerve corresponds to a small posteromedial territory at the
distal third of the thigh between the adductor gracilis and the
adductor magnus. This explains why the determination of the intensity
of an obturator block based only on sensory assessment is difficult in
the absence of simultaneous assessment of motor function.
adductor magnus muscles. It supplies the obturator externus, adductor
magnus and adductor brevis muscles, and produces articular branches for
the hip and the knee joints.
the same course as the obturator nerve, except that it enters the thigh
over the pubic anterior branch. It supplies the obturator and the
pectineus muscles and gives rise to a branch for the hip joint.
 |
|
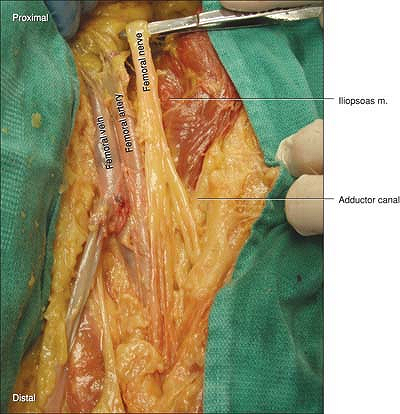
Figure 11-3.
The femoral nerve to artery relationship is one of the most consistent in the body. The relationship of the nerve lateral to the artery is best approached superior to the extensive branching (arborization) at or just below the inguinal crease. |
plexus. It exits the lateral side of the psoas muscle and runs in the
iliopsoas groove toward the inguinal ligament, beneath which it enters
the thigh. In the pelvis, it produces branches for the psoas and iliac
muscles. Generally, it divides in four terminal branches at the level
of or immediately below the inguinal ligament, although in some cases
the division occurs before. In the femoral triangle, there are two
planes to be considered. The anterior femoral nerve is located within
the anterior plane, which innervates the skin over the front and medial
sides of the thigh and also contributes to the subsartorial plexus and
branches to the sartorius, pectineus, and sometimes part of adductor
longus muscles. The posterior plane consists of the quadriceps femoris
and the saphenous nerve. The saphenous nerve also contributes to the
subsartorial plexus. It supplies the skin of the medial part of the
knee and the anteromedial part of the leg as far as the foot, although
in some cases it may extend as far as the base of the first toe.
Additionally, the saphenous nerve also plays an important role in the
innervation of the knee joint.
regions supplied by some branches of the lumbar plexus, especially the
lateral femoral cutaneous and the femoral branch of the genitofemoral
nerves, which may explain instances of incomplete superficial blocks.
from S1 to S3, and the lumbar roots from L5 are associated with an
anastomotic branch from L4 (furcal nerve). The L5 roots and the L4
anastomotic branch form the lumbosacral trunk. The lumbosacral trunk
and the sacral roots converge toward the sciatic foramen and merge
before entering the buttock. The sacral plexus is shaped like a
triangle, with its base lying against the anterior sacral foramina and
its vertex corresponding to the anteromedial border of the sciatic
foramen. The sacral plexus transverses the sciatic foramen lying
anterior to the piriformis muscle and is covered by the pelvic
aponeurosis (corresponding to the fascia of the pelvic muscles), which
separates it from the visceral structures of the pelvis. In this
section only the collateral branches of the sacral plexus for the lower
limb are described.
nerves supplying the muscles of the region. Some are more relevant for
regional anesthesia.
crosses the sciatic foramen. It supplies the gluteus medius and gluteus
minimus muscles and finishes its course in the tensor fasciae latae
muscle. In this regard, it is important to note that it is a branch of
the lumbar plexus that provides sensory innervation of the skin over
the tensor fasciae latae muscle before it leaves a branch for the hip
joint.
foramen. In addition to supplying these two muscles, it also produces a
small ramus for the hip joint.
S2. It penetrates the buttock through the lateral border of the sciatic
foramen. It may have a common origin with the posterior cutaneous nerve
of the thigh, but frequently these two nerves are separated. Beyond the
piriformis muscle, the inferior gluteal nerve hooks around the inferior
border of the gluteus maximus muscle and supplies it.
inferior gluteal nerve, it penetrates the buttock just beyond the
piriformis muscle, and it gives rise to branches for the inferior part
of the buttock (inferior gluteal nerve) and the perineal region. It
runs between the posterior muscles of the thigh immediately under the
fascia lata and gives branches that perforate the fascia and supply the
skin of the posterior surface of the thigh as far as the popliteal
region. In the popliteal region, it pierces the fascia and divides into
two branches: one for the posterior and upper surface of the thigh; and
one that follows the small saphenous vein as far as the middle of the
calf, where it is anastomosed with the sural nerve.
 |
|
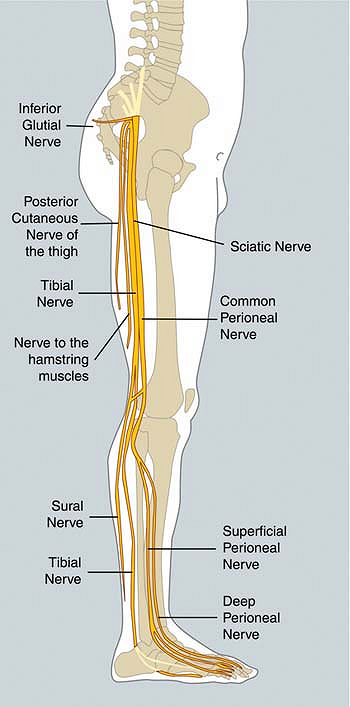
Figure 11-4. Branches collateral and terminal nerves.
|
muscle, the sciatic nerve, the inferior gluteal muscle, and the
posterior cutaneous nerve of the thigh are close to each other.
body. Although it may be considered the solitary terminal branch of the
sacral plexus, at this level it is already composed of two distinct
contingents reunited in a common sheath. After passing through the
sciatic foramen, it inclines laterally under the gluteus maximus
muscle. On its medial side, it is accompanied by the posterior
cutaneous nerve of the thigh and the inferior gluteal vessels. It runs
anterior to the piriformis muscle, and, at the midpoint between the
greater trochanter and the ischial tuberosity, it turns downward toward
the thigh. In the thigh, it runs between the biceps femoris muscle
(laterally) and the semi-tendinous and semi-membranous muscles
(medially) and just behind the adductor magnus. At the vertex of the
popliteal fossa or even higher, it separates into tibial and common
peroneal nerves. In 15% of cases, division of the sciatic nerve occurs
at the level of the piriformis muscle. Several anatomic modalities can
be observed, which are classified into three types: (a) both
contingents pierce the pyramidal muscle; (b) only the common peroneal
contingent pierces the muscle; and (c) one contingent passes over the
muscle.
the posterior part of the hip joint capsule. The medial part of the
sciatic nerve (tibial contingent) provides a branch that
innervates
the semi-tendinous and semi-membranous muscles, the long head of the
biceps femoris muscle, and the ischiocondylar part of the adductor
magnus muscles. In the middle of the thigh, the lateral part of the
sciatic nerve (common peroneal contingent) has two branches: one for
the short head of the biceps femoris and the other for the posterior
and lateral part of the knee joint capsule.
 |
|
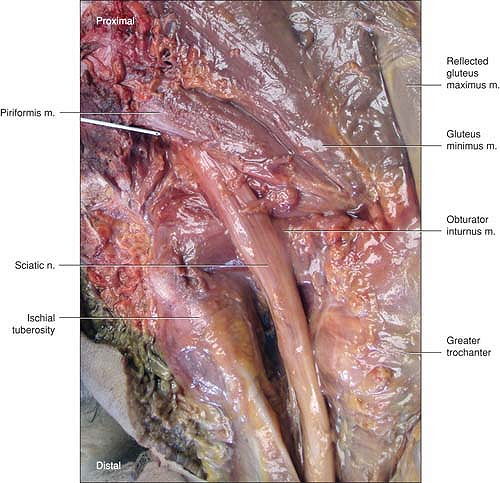
Figure 11-5.
This is a fresh tissue dissection of the sciatic nerve from its origin at the sacrum. The pen is at the level of the PSIS which is circled. The needle is 7 cm from that point at the exit of the sciatic nerve. The gluteus maximus has been reflected so the exit of the sciatic nerve is just caudal to the piriformis muscle. As the nerve exits the buttocks it is between the ischial tuberosity and greater trochanter. |
through the popliteal fossa and the leg. In the popliteal fossa, it
runs laterally to the vessels and follows the median axis of the
popliteal fossa. In the leg, it passes downward in an oblique and
medial direction, lying between the tibialis posterior muscle, then the
flexor digitorum muscles in front and the soleus muscles behind. In the
distal third of the leg, the nerve is covered only by skin and fascia.
It curves medially behind the medial malleolus and produces two
branches: the medial and lateral plantar nerves. In the popliteal
fossa, it leaves a branch for the capsule of the knee joint, gives rise
to a part of the sural nerve (medial sural cutaneous nerve), and
supplies the muscles of the calf. In the leg, it leaves articular
branches for the ankle, the
tibiofibular
joint and bone, and innervates the flexor muscles of the foot and toes.
In the ankle and foot region, it supplies the skin of the sole and the
intrinsic muscles of the foot.
 |
|
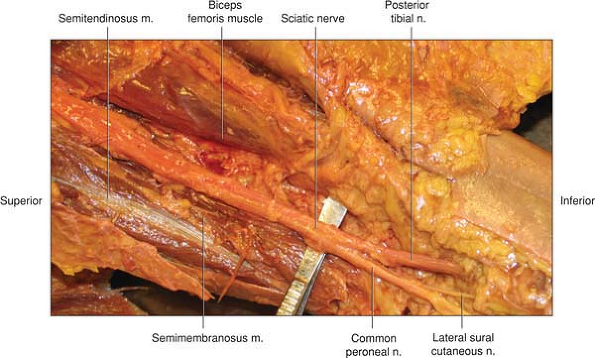
Figure 11-6.
This unaltered fresh tissue dissection is to illustrate the straight course the sciatic nerve takes though the leg. Note that there is no vascular bundle as the artery is much closer to the femur than the sciatic nerve. Just above the knee the branches into the posterior tibial and common peroneal are seen. This branching is usually within 10 cm of the crease of the knee. |
border of the popliteal fossa and gives a branch to the sural nerve. It
winds around the head of the fibula, passes over the neck of the
fibula, and then divides into a superficial and a deep branch. The
superficial peroneal nerve descends along the lateral aspect of the leg
and supplies the skin of the anterior and lateral face of the leg and
the dorsum of the foot and lateral peroneal muscles. The deep peroneal
nerve supplies the tibialis anterior and extensor muscles. It
penetrates the foot between the tendon of the extensor digitorum longus
and the extensor hallucis longus muscles, and supplies contiguous sides
of the first and second toes.
peroneal nerves provide a medial and a lateral sural cutaneous nerve,
respectively. The lateral sural nerve has a communicating branch that
joins the medial sural cutaneous nerve to form the sural nerve. The
lateral sural cutaneous nerve supplies the skin of the lateral aspect
of the leg while the sural nerve supplies the skin of the
posterolateral part of the leg and the lateral border of the foot.
medial sural cutaneous nerve and the communicating branch can occur at
variable levels, and in some cases can even be absent. In such cases,
the communicating branch supplies the lateral malleolus and the
external face of the heel. Moreover, the proportion of fibers
originating from the medial sural cutaneous nerve and the communicating
branch is variable. For this reason, it is probably preferable to
consider the sural nerve as an independent nerve formed by the union of
two roots: a medial root from the tibial nerve and a lateral root from
the common peroneal nerve.
rib, laterally by the external border of the quadratus lumborum muscle,
medially by the vertebral body, and on its lower border by the iliac
crest. As previously described, the lumbar plexus lies between the two
parts of the psoas muscle. After their origin from L1, the
iliohypogastric and the ilioinguinal nerves immediately leave the
posterior psoas muscle posteriorly. This may explain why a posterior
approach of the lumbar plexus at the level of L4-5 may not result in a
block of these nerves. The genitofemoral nerve (from L2) has a more
prolonged course in the psoas muscle and leaves it anteriorly. Thus, a
block of this nerve is probably more likely to be achieved by using a
posterior approach. Concerning the three main trunks of the lumbar
plexus, dissections have found a fan disposition in the muscle: The
lateral femoral cutaneous nerve is lateral, the obturator nerve is
medial, and the femoral nerve lies in between, usually in the same
plane. However, variations are common. Although the lateral femoral
cutaneous and femoral nerves have a constant relationship with one
another, the presentation of the obturator nerve is more variable, and
frequently it is in a different plane from the one enclosing the other
nerves. This variability might explain a limited extension to the
obturator nerve, even with a posterior approach.
plexus blocks for two reasons. First, the landmarks are easy to
identify, and second, the L4 roots provide fibers for the trunks of
both the lumbar and sacral plexus. Moreover, it seems that this
approach is associated with a lower rate of complications. One of the
landmarks used is the iliac crest, which usually corresponds to the
L4-5 space. However, it is important to remember that this line is not
an absolute reference: The rate of inaccuracy is close to 50% and
corresponds to the normal distribution of an anthropometric variable.
Palpation and drawing of the spinal processes are important aids to
confirming the correct position of this line. The second line parallel
to the spine passes through the posterosuperior iliac spine. Although,
the needle is classically introduced at the junction of these two
lines, the junction of the lateral one third and medial two thirds
between the lines of the spinous process and the posterior iliac spine
on the iliac crest line has also been advocated. This modification is
important to take into account for two reasons. First, this approach is
strictly parallel to the vertebral column, whereas a more lateral
approach would require the needle to be redirected medially to reach
the plexus (as recommended by Winnie). Such redirection of the needle
increases the risk of peridural or spinal placement of the needle.
Second, although there is great individual variation in the distance
between skin and lumbar plexus (55 mm to 110 mm), the distance between
the transverse process and the lumbar plexus is relatively constant at
around 18 mm. Therefore, the contact with the transverse process
constitutes an important safety marker.
plexus, the risk of epidural and even intrathecal extension of a lumbar
plexus block cannot be completely eliminated, even with meticulous
technique. Moreover, prolongations of the spinal dura mater surrounding
the roots may favor an intrathecal diffusion despite a correct
approach. This risk must be taken into account when performing this
block.
performed using a “loss of resistance” technique (psoas compartment
block), the use of a nerve stimulator has increased the reliability of
this approach. The optimal muscular response is a contraction of the
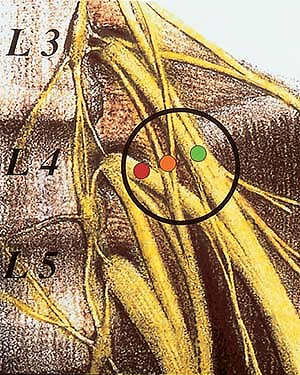
quadriceps with ascension of the patella (Fig. 11-7, green dot). A contraction of the adductor muscles (Fig. 11-7, orange dot)
suggests that the needle position is too medial and that the needle
should be redirected laterally in search of the proper motor response.
In some cases (obese patients) the contraction of the adductor muscles
may simulate a stimulation of the femoral nerve. In such patients, only
palpation allows the proper diagnostic confirmation. Simultaneous
contraction of the quadriceps and adductor muscles suggest that the
needle is paravertebral (Fig. 11-7, red dot) with an increased risk of epidural diffusion.
 |
|
Figure 11-7. The patellar (green dot), adductor muscles (orange dot), and quadriceps (red dot).
|
of L3 at the right and L2-3 vertebral discs at the left. The location
of the kidneys explains why renal subcapsular hematomas have been
described with a high posterior approach at the L3 level.
the femoral triangle, and it is at this level that the femoral nerve is
approached. The femoral triangle is limited laterally by the sartorius
muscle and medially by the border of the adductor longus and pectineus
muscle. The junction of the sartorius and the adductor longus muscles
corresponds to the vertex of the triangle. From the surface downward,
there is a subaponeurotic plane, containing lymphatics and vessels,
followed by two aponeurotic planes: the fascia lata, stretching between
the sartorius and adductor longus muscle, and the aponeurosis of the
psoas major, iliacus, and pectineus muscles: the fascia iliaca. Because
it is pierced with several openings through which vessels and nerve
pass, the fascia lata in the femoral triangle is also known as the
cribriform fascia. The femoral nerve is under the fascia iliaca, but
the femoral artery and vein lie between the two fasciae. Therefore
there is no common vascular–nervous sheath at this level. It is also
important to recognize that although the femoral nerve and vessels are
clearly separated in the femoral triangle, there are superficial
(subaponeurotic) and deep (between fascia lata and fascia iliaca)
circumflex iliac vessels that cross over the femoral nerve and can be
punctured during the performance of a femoral block.
iliaca compartment, and three-in-one blocks. However, for each of these
approaches the goal is to inject the local anesthetic solution under
the fascia iliaca using one of two techniques: either with a nerve
stimulator to localize the femoral nerve or by feeling the penetration
of the two fasciae. Anatomically, these three techniques are similar.
the femoral nerve using the nerve stimulator. The approach is most
frequently immediately lateral to the femoral artery at the level of
inguinal crease. At the level of the inguinal ligament, and especially
when the needle is introduced cephalad, the femoral nerve can be missed
because the orientation of the nerve at this level is anteroposterior
in the direction of the psoas muscle, rather than cephalad to caudal.
The appropriate motor response is a contraction of the quadriceps
muscle associated with movement of the patella. A contraction of the
vastus medialis indicates that the needle needs to be redirected
laterally and slightly deeper, whereas a direct contraction of the
sartorius muscle
suggests
a medial redirection of the needle. Again, at times, it may be
difficult to distinguish between the contraction of the sartorius
muscle and contraction of the vastus medialis muscle.
introduced just below the inguinal ligament immediately to the medial
border of the sartorius muscle. A short bevel needle is used to feel
the passage of the fasciae lata and iliaca (“double click”). This
approach is based on the concept of a diffusion of the local anesthetic
solution under the fascia iliaca. Generally, the femoral nerve fans out
in its different branches quickly below the inguinal ligament, but
there are frequent anatomic variations. Consequently, the risk of
femoral nerve injury exists even if the needle is introduced along the
medial border of the sartorius muscle.
local anesthetic solution. Indeed, Winnie postulated that, with firm
compression immediately below the needle and a sufficient volume of
local anesthetic, it is possible for the local anesthetic solution to
diffuse toward the psoas muscle and consequently produce a block of the
femoral, obturator, and lateral femoral cutaneous nerves. However, two
studies, one radiographic and one using magnetic resonance imaging,
have shown that such diffusion to the psoas compartment is exceptional.
Although a diffusion of local anesthetic toward the lateral femoral
cutaneous nerve frequently occurs, especially after fascia iliaca
block, the block of the obturator nerve is unlikely. Only one study has
made a correct evaluation of the block of the obturator nerve after a
three-in-one block using electromyographic techniques, and this study
confirmed that the obturator nerve is practically never blocked after
performing a three-in-one block.
three-in-one, or fascia iliaca compartment blocks) the end point is the
same: injection of the local anesthetic under the fascia iliaca. In
fact, the most logical approach is to localize the femoral nerve with a
nerve stimulator after feeling the two “clicks.” In addition, the
“quest” for a complete lumbar plexus block through an anterior approach
is unlikely to succeed. With an anterior approach, even in the best
cases, it is more likely to obtain a two-in-one block. More frequently,
just a femoral block or less (when the territory of the lateral femoral
extends until the anterior face of the thigh) can be observed.
pelvis and enters the buttock through the greater sciatic foramen. From
an anesthetic point of view, this region can be compared to the
supraclavicular region for the brachial plexus in that, at this level,
all the nerves of the plexus are close to each other and, therefore,
all can be blocked with a relatively small volume. Furthermore, the
possibility of an extension to the obturator nerve has been postulated;
however, such an extension seems unlikely considering that there is a
pelvic fascia between the sacral plexus and the obturator nerve.
Nevertheless, the excellent extension of the block to the sacral plexus
territory is real, but this advantage must be balanced by the
theoretical risk of injury to the internal iliac vessels, ureter, or
rectum if the needle is introduced beyond the plexus.
classic approach correspond to the inferior border of the piriformis
muscle. At this level, the sacral plexus has already fanned out in its
different branches, and only the sciatic nerve, the posterior cutaneous
nerve of the thigh, and probably the inferior gluteal nerves can be
reliably blocked with such an approach. The superior gluteal nerve and
the nerve to the quadratus femoris muscle are unlikely to be blocked
with this approach. This distinction may be important to recognize,
especially for hip surgery, because these two nerves supply a part of
the posterior hip joint capsule. At this level, the sciatic nerve, the
inferior gluteal nerve, and the posterior cutaneous nerve of the thigh
are close enough together for all to be blocked, providing adequate
anesthesia for any surgery being performed from the thigh to the foot,
including those requiring the use of a tourniquet for more than 30
minutes. Moreover, if the needle misses
the
sciatic nerve, its course is stopped by bone. The major risk of this
approach is limited to a puncture of the inferior gluteal vessels.
However, a more distal approach at the buttock progressively increases
the risk of missing the posterior femoral cutaneous nerve. Even though
the inferior gluteal and the posterior cutaneous nerves are frequently
merged at this level (40% of cases), it is not necessary to block the
inferior gluteal nerve to guarantee extension to the posterior femoral
cutaneous nerve for two reasons: (a) localization of the sciatic nerve,
especially with a two-stimulation technique (tibial and common peroneal
responses) is sufficient to ensure anesthesia in this territory; and
(b) the inferior gluteal nerve pursues a circular course and can be
stimulated superficially as a possible means of extension to the
posterior femoral cutaneous nerve. The size of the sciatic nerve and
the possibility that its division can occur high, justify the use of a
multi-stimulation technique.
level. Extension to the posterior cutaneous nerve of the thigh is
unpredictable. Two approaches are generally described: an anterior and
a lateral approach. In all cases, the sciatic nerve is approached at
the level of the lesser trochanter. These approaches are frequently
associated with a direct contact of the femoral shaft before reaching
the nerve. Moreover, the nerve is deep (8 to 12 cm). Therefore, it is
generally difficult to reorient the needle to perform a two-stimulation
technique. In the anterior approach, because the needle approaching the
sciatic nerve comes close to the femoral nerve, it is necessary to
immediately switch on the nerve stimulator after passing the skin. One
of the problems encountered with the anterior approach is the
difficulty in reaching the nerve when it is located under the femoral
shaft. It has been shown that when the needle is inserted at the level
of the lesser trochanter, an internal rotation of the leg facilitates
the approach to the sciatic nerve.
corresponding to the popliteal crease and limited medially by the
semi-tendinous and semi-membranous muscles and laterally by the biceps
femoris muscle and its tendons. Different approaches to the sciatic
nerve have been described, and all can be grouped into posterior and
lateral approaches. Of the various posterior approaches to the
popliteal fossa, high approaches are most logical. There is no risk of
vessel puncture above the adductor hiatus because it is not close to
any vessels there; below the adductor hiatus, the risk of puncturing
popliteal vessels increases as the approach becomes lower and the
distance between the nerve and the vessels decreases. Moreover, the
higher is the approach and the closer are the two branches of the
sciatic nerve. This is especially important when a perineural catheter
is placed. The posterior approaches near the popliteal crease must be
avoided because popliteal vessels lie immediately anterior or behind
the tibial nerve, thus increasing the risk of vessel puncture. For the
lateral approach, there is also a theoretical risk of popliteal vessel
puncture, but this risk is limited if the needle is directed at a 25°
to 30° angle.
comprises the sural nerve may occur at different levels in the
popliteal region. Consequently, at the level of the popliteal fossa,
the block of the sural nerve is sometimes incomplete.
CR. Development and variation of the nerves and the musculature of the
inferior extremity and of the neighboring regions of the trunk in man. Am J Anat 1906–1907;6:259–390.
X, Biboulet P, Bouregba M, et al. Comparison of the three-in-one and
fascia iliaca compartment blocks in adults: clinical and radiographic
analysis. Anesth Analg 1998;86:1039–1044.
X, Macaire P, Dadure C, et al. Continuous psoas compartment block for
postoperative analgesia after total hip arthroplasty: new landmarks,
technical guidelines, and clinical evaluation. Anesth Analg 2002;94:1606–1613.
Ridder VA, de Lange S, v. Popta J. Anatomical variations of the lateral
femoral cutaneous nerve and the consequences for surgery. J Orthoped Trauma 1999;13:207–211.
H, Vloka J. A comparison of the posterior versus popliteal approaches
to the block of the sciatic nerve in the popliteal fossa. Anesthesiology 1998;88:1480–1486.
M, Kikuchi S, Sakuyama Y, et al. Anatomic study of the interrelation
between lumbosacral nerve roots and their surrounding tissues. Spine 1983;8:50–58.
R, Maigne JY. Syndrome des branches perforantes latérales des nerfs
sous-costal et ilio-hypogastrique. Une cause méconnue de douleurs de
hanche. Revue du Rhumatisme 1986;53:307–311.
P, Nasel C, Sitzwohl C, et al. Magnetic resonance imaging of the
distribution of local anesthetic during the three-in-one block. Anesth Analg 2000;90:119–124.
JD, Hadzic A, Drobnik L, et al. Anatomical landmarks for femoral nerve
block: a comparison of four needle insertion sites. Anesth Analg 1999;89:1467–1470.
