Acetabulum Fractures
1950s and 1960s offered conflicting recommendations regarding the
optimal care for a fracture of the acetabulum.71,122
Both nonoperative and operative treatment regimens were purported to be
best. However, much of the confusion in management recommendations can
be attributed to the fact that there was no comprehensive or accepted
acetabular fracture classification, an unsatisfactory situation that
was well recognized even at the time.140
Each investigator reporting on any sizable number of cases produced his
or her own method to describe the fracture. Fracture evaluation was
further complicated by the fact that in most instances radiographic
assessment was limited to a single anteroposterior (AP) pelvic view.
Not unexpectedly, it was stated at the time that “the surgeon must not
be surprised if, even after careful study, his preconceived idea of a
given fracture does not exactly fit the findings at operation.”71
However, there was some consistency amid the apparently disparate
recommendations: all these early investigators did agree that poor
results would follow from a hip injury that resulted in either joint
instability or a femoral head that was incongruent with the
weight-bearing dome.71,122,140,141
provided more clarity to this confused situation. In their 1964
treatise, they set out to describe, among other things, the
radiographic findings in acetabular fracture patients and to outline a
plan of treatment. Their recommendation for operative treatment was
based on 10 years of study and resulted from their disappointment with
the results of nonoperative methods.64 Over the next 3 decades, they refined a number of the aspects presented in this seminal publication.78
However, the basic concepts remain, including understanding the
surgical anatomy of the innominate bone, defining the injury via
appropriate radiographic assessment, and, by these means, determining a
suitable treatment plan.
have shown that to attain the best results, hip joint congruity and
stability must be accompanied by an anatomic (defined as less than 2 mm
of residual displacement) reduction of the
displaced
articular surface. Therefore, accurate reduction of the intra-articular
fracture fragments is critical for a successful outcome, as is
maintenance of this reduction by internal fixation. It has been
stressed that in a displaced fracture this anatomic reduction is
difficult, if not impossible, to obtain by closed means.86,87
In addition, standard plate and screw fixation constructs, which
require open surgery, have been shown to be stronger than their
percutaneous counterparts, demonstrating greater yield strength and
maximal load at failure.25
Therefore, open anatomic reduction and internal fixation continue to
serve as the mainstays in treatment of displaced fractures of the
acetabulum (Fig. 45-1).
there has been little in the way of new information regarding
acetabular fracture care. Their results are still considered the “gold
standard” of what can be obtained in the treatment of these difficult
injuries. However, there are some new trends that have developed over
the past 5 to 10 years, most of which serve to expand on principles
advocated by Letournel and Judet. Such trends include the advancements
in perioperative imaging. In the 1960s, Judet et al.64
recognized that the plane of the ilium was approximately 90 degrees to
the plane of the obturator foramen and that both of these structures
were oriented roughly 45 degrees to the frontal plane. Therefore, they
proposed that the AP pelvis and two 45-degree oblique views be used to
study the radiographic anatomy of the acetabulum.64
After understanding the radiographic landmarks on the intact dry
innominate bone, these landmarks could then be appropriately analyzed
in fracture cases and from this process came the first systematic
classification of acetabular fractures, based on the anatomic pattern
of the fracture.64 In the 1993 text, this analysis was expanded to include preoperative two-dimensional computed tomography (CT).78
Subsequent advances in CT technology have not only improved the
information provided by the two-dimensional images but now offer the
promise of useful three-dimensional images, as well as
computer-generated plain radiograph-like images created from the CT
data.13 Intraoperative imaging has
evolved from plain radiographs to C-arm image intensifier fluoroscopy
to the promise of three-dimensional imaging with image navigation.
Postoperative CT, once considered unnecessary, has become accepted as
an important evaluative tool at many centers.98
 |
|
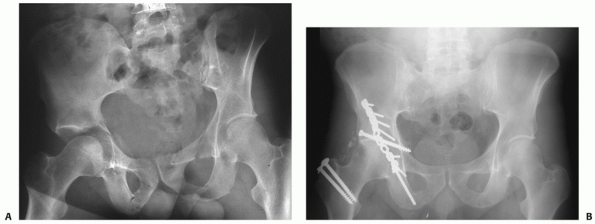
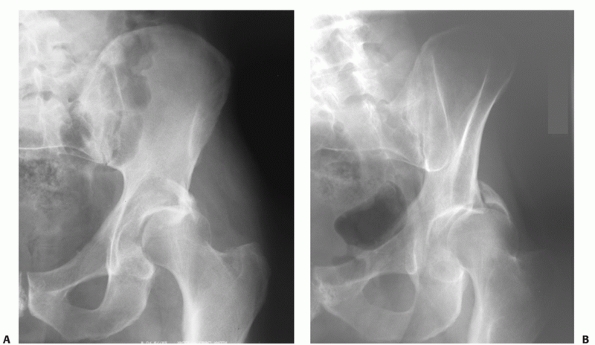
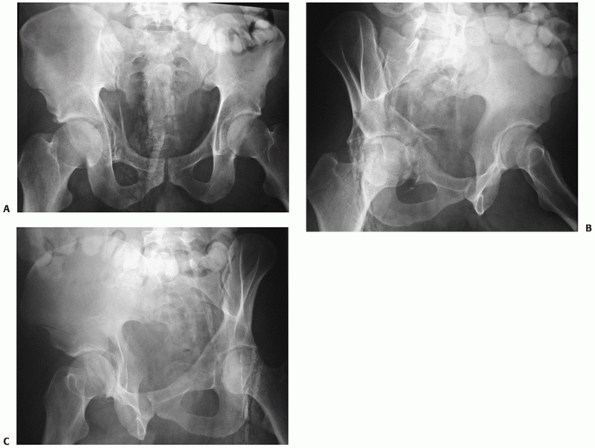
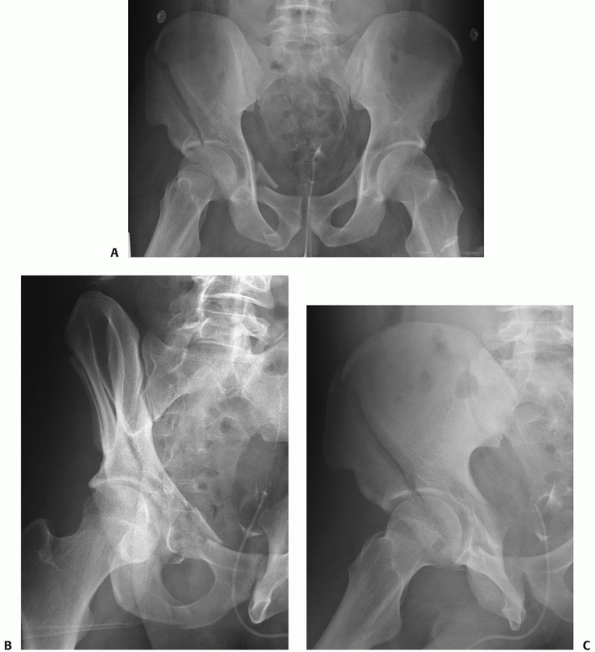
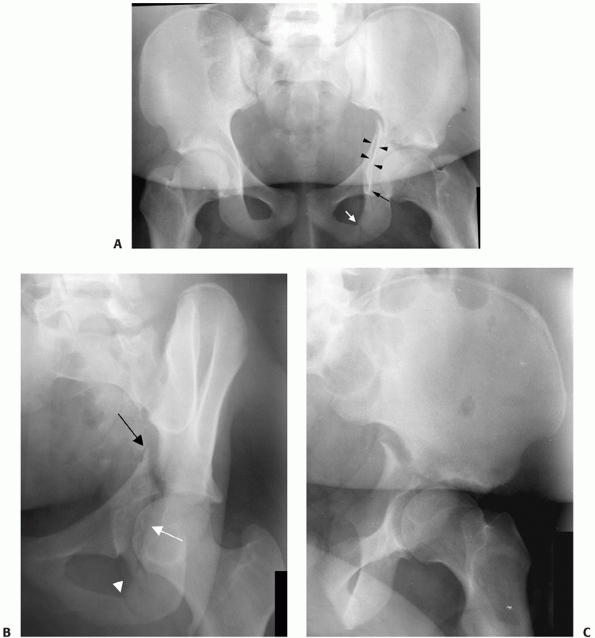
FIGURE 45-1 A.
Anteroposterior (AP) radiograph in traction of a 42-year-old man at the time of transfer to our center, 3 weeks after sustaining a displaced transverse right acetabular fracture in a motor vehicle accident. Subsequently, open reduction and internal fixation was performed. B. AP radiograph at his 20-year follow-up examination. The patient had returned to full activities within 1 year of his accident and continued to be asymptomatic regarding the right hip. (Copyright Berton R. Moed, MD.) |
described by Letournel and Judet remain the norm, the availability of
potentially useful alternative approaches has expanded over time. In
addition, the manner in which perioperative complications, such as deep
vein thromboses, are managed has evolved. Perhaps the most
controversial trend, however, is that toward percutaneous fracture
reduction and fixation techniques.137
long-term result in the treatment of a fracture of the acetabulum
fractures is dependent on restoring a congruent and stable hip joint
with an anatomically reduced articular surface. As has been noted,
these treatment objectives have been well recognized for more than half
a century. The achievement of these objectives should minimize pain,
prevent posttraumatic osteoarthrosis, and thereby improve long-term
functional outcome. However, fractures of the acetabulum continue to be
a challenge for the orthopaedic surgeon. Successful treatment of an
acetabular fracture is based on a thorough understanding of the complex
three-dimensional anatomy of the innominate bone.64,78
Although certain fracture patterns may not require surgery to have a
satisfactory outcome, in general, those with hip instability, hip
incongruity, or fracture displacement in the superior weight-bearing
area of the acetabulum should be managed with open reduction and
internal fixation. However, the surgery is complex and demanding, even
for the experienced surgeon, and has the potential for many serious
complications. Many factors, including the patient’s age, general
medical condition, and associated injuries, must be considered prior to
making definitive management decisions.146
Therefore, the operative treatment of these fractures is best performed
by specialized surgeons who routinely care for patients with these
injuries.31,65,158 All orthopaedic surgeons, however, should be capable in the diagnosis
of these fractures and able to determine which may require surgical management.
This force to the femoral head may be applied via the greater
trochanter (along the axis of the femoral neck) or from anywhere along
the long axis of the femoral shaft. Subsequently, the pattern of the
resulting acetabular fracture depends on the position of the hip at the
time of impact, as well as the location and direction of the originally
applied force78 (Table 45-1).
With the force applied along the axis of the femoral neck, external hip
rotation will produce an anterior fracture type and internal rotation
will produce a posterior fracture (Fig. 45-2).
In general, forces applied along the axis of the femur, when the hip is
flexed, drives the femoral head against the posterior articular surface
of the acetabulum. However, with the addition of adduction, the femoral
head may dislocate without causing a fracture. Whatever the hip
position or location of the applied force, however, the degree of
fracture displacement, fracture comminution, and articular impaction
further depend on the magnitude of the applied force, as well as the
strength of the underlying bone. Despite sustaining a relatively
low-energy injury, patients with osteopenic bone often sustain severely
comminuted fractures with articular impaction. A simple fall on the
greater trochanter may cause an acetabular fracture in the older,
osteopenic patient. These relatively low-energy injuries usually
produce isolated fracture trauma, whereas high-energy injuries are
often associated with additional skeletal or other system trauma.
high-energy blunt trauma. Therefore, they are frequently associated
with other musculoskeletal and visceral injuries. In some series, such
associated injuries occurred in more than 50% of patients.73,83,109,99
Specifically, in the large series reported by Matta, 35% of the
acetabular fractures were associated with an injury involving an
extremity, 19% with a head injury, 18% with a chest injury, 13% with a
nerve palsy, 8% with an abdominal injury, 6% with a genitourinary
injury, and 4% with an injury of the spine.83
Consequently, the initial evaluation, even in those patients with an
apparent isolated injury, should be part of a well-organized overall
approach. Associated injuries can be life or limb threatening and the
recommended Advanced Trauma Life Support (ATLS) evaluation sequence
should be followed.4 Disruption of
the pelvic ring may occur in association with a fracture of the
acetabulum. This pelvic injury may be an important factor regarding the
patient’s hemodynamic status at
the time of initial presentation.125
In addition, the pelvic ring injury may alter subsequent acetabulum
fracture care. Contralateral rami fractures may affect the surgeon’s
decision to use intraoperative traction, because the presence of a
peroneal post may be a deforming force on certain acetabular fractures
and possibly prevent reduction.78 A
posterior pelvic ring disruption usually must be reduced and
stabilized, recreating a stable posterior fixation point, prior to
surgical treatment of most acetabulum fractures.78
If a slight malreduction of the posterior ring injury may preclude an
anatomic acetabular fracture reduction, as is the situation when the
acetabular fracture (such as a transverse fracture type) itself
constitutes the concomitant “anterior ring” injury, the order of
fixation is often reversed.
|
TABLE 45-1 Force Applied and Hip Position versus Fracture Pattern
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 |
|
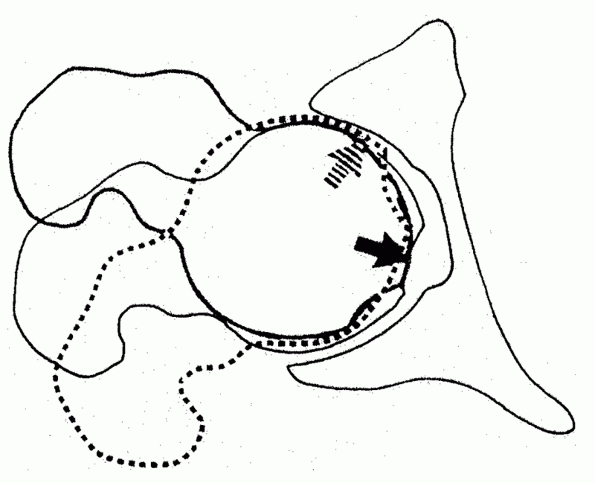
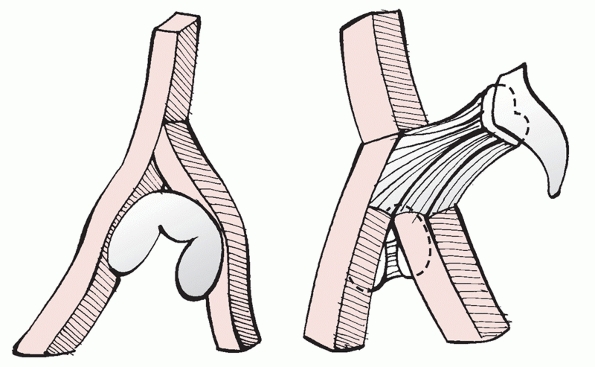
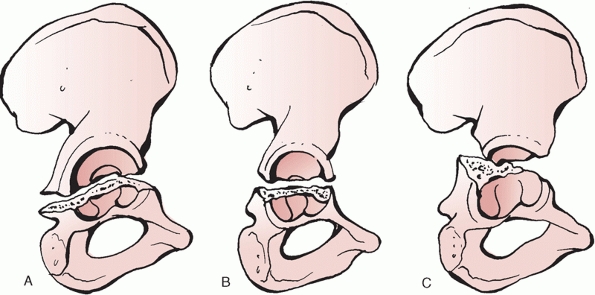
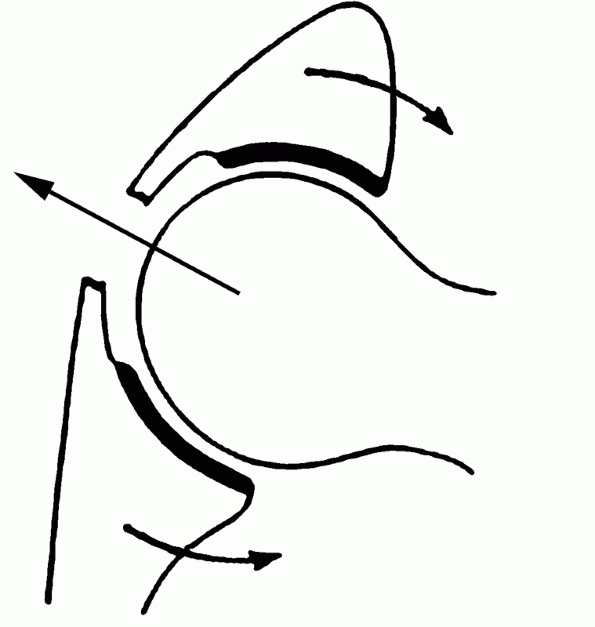
FIGURE 45-2
The type of acetabular fracture depends, in part, on the rotational position of the femoral head at the time of impact. With the force applied along the femoral neck, external rotation will produce an anterior fracture (striped arrow) and internal rotation will produce a posterior fracture (solid arrow). |
 |
|
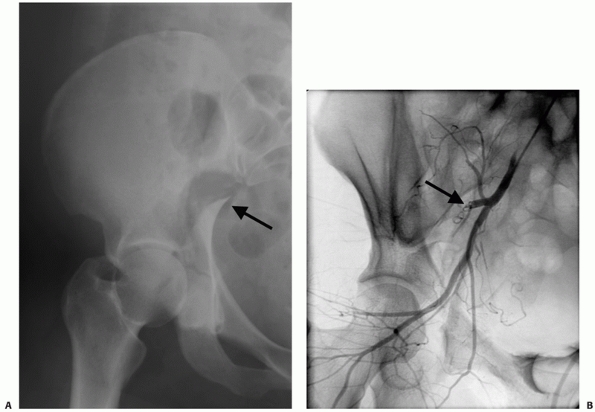
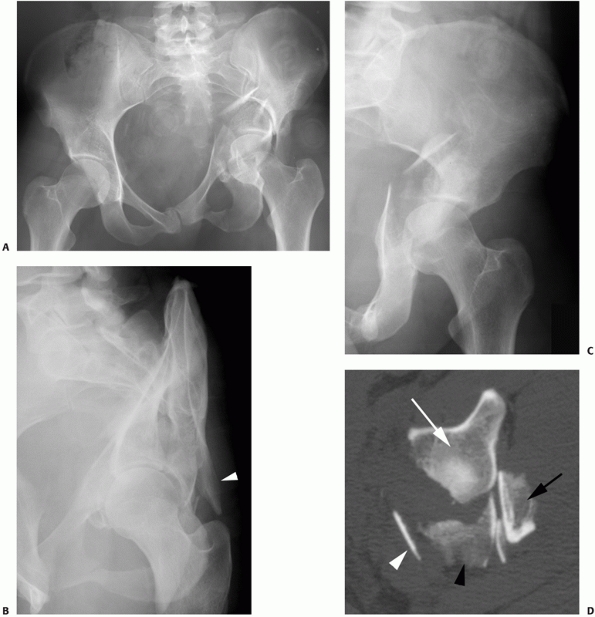
FIGURE 45-3 A 36-year-old female unrestrained driver involved in a motor vehicle accident sustained a fracture of the acetabulum (A) with wide displacement and a particularly sharp spike of posterior column at the greater sciatic notch (arrow)
became hemodynamically unstable shortly after presentation to the emergency department. Subsequent evaluation including angiography (B) revealed a superior gluteal artery injury to be the source of the bleeding, which was successfully treated by embolization (arrow). (Copyright Berton R. Moed, MD.) |
a closed fracture of the acetabulum, occurring alone or in combination
with other extremity fractures, should not be considered as the primary
cause of hypotensive shock. An alternative source of hemorrhage should
always be sought. However, laceration of the superior gluteal artery
with severe bleeding can be caused by fractures of the acetabulum
having wide posterior column displacement. One must be alert to this
possibility, which is treatable by therapeutic embolization (Fig. 45-3).
The acute evaluation and treatment of these serious life- and
limbthreatening injuries take precedence over the acetabular fracture
management. However, an orthopaedic surgeon must be involved early on,
as initial management of associated injuries often will affect the
future acetabular fracture care. Simple measures may prove to be very
important, such as locating a suprapubic catheter or colostomy so as
not to preclude a later planned surgical approach to the acetabulum.
either directly to the region of the hip or indirectly along the axis
of the femur. Therefore, associated injuries can occur locally about
the hip, distal to the hip at the location of the applied axial load,
or anywhere in between. These injuries can be occult and great care
must be taken during the initial examination and diagnostic evaluation
of the patient to elucidate their presence or absence. Fractures
involving some aspect of the femur or knee are common. The initial
management of these fractures often affects the later treatment of the
acetabular fracture. Therefore, it is important to develop treatment
strategies that achieve the best result for all associated injuries. A
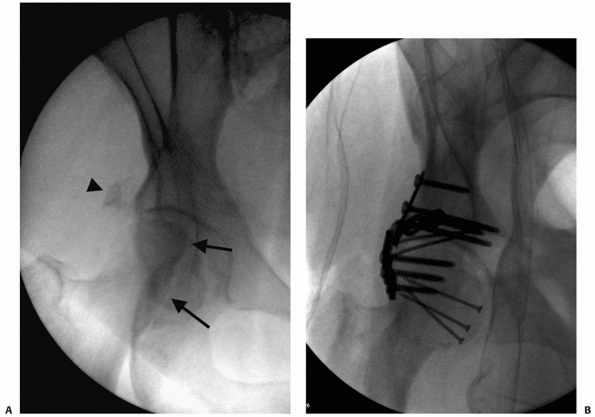
displaced fracture of the femoral head may be present, especially in
association with a posterior fracture-dislocation.73 These fractures are usually treated at the time of acetabular fracture fixation (Fig. 45-4).
dilemma, as initial femur fracture treatment may compromise the optimal
surgical approach to the acetabulum. Options include
treating
these fractures at the time of acetabular fracture fixation or planning
the staged surgical procedures so as not to interfere with optimal
acetabular fracture care. A femoral neck fracture in a young adult
patient, generally defined as those younger than 65 years, should be
treated surgically on an urgent basis.79 In this situation, it would be unusual to treat the associated acetabular fracture at the same time.73
If open reduction and internal fixation, rather than closed reduction
and percutaneous fixation, is required for treatment of the femoral
neck fracture, a Watson-Jones anterolateral approach is preferred.79,153 Alternatively, a modified Smith-Petersen anterior surgical approach can be used.110
Although the modified Smith-Petersen approach allows direct access to
the femoral neck fracture, a separate incision is required for implant
insertion.110,153
The acetabular fracture can then be addressed later, as required,
preferably through a separate, optimal approach. Unfortunately, it may
be unavoidable that the optimal surgical approach for femoral neck
fracture treatment will compromise the optimal approach for the
acetabulum. In this situation, one must choose between treating both
fractures at the same operative setting or staging the acetabulum
fracture fixation to follow acceptable healing of the femoral neck
fracture fixation wound. In contradistinction to the femoral neck
fracture in a young adult, intertrochanteric and subtrochanteric femur
fractures do not need to be operatively treated in an urgent fashion.
Therefore, the treating physician has the luxury of choosing either
staged fixation of the proximal femur fracture followed later, after
wound healing, by fixation of the acetabular fracture or appropriately
timed, delayed fixation of both fractures during the same operative
setting, using the same or separate incisions. In either case, the
treatment scheme should be planned in a way to optimize treatment of
the acetabular fracture.
 |
|
FIGURE 45-4
A 55-year-old obese woman involved in a motor vehicle accident had a right acetabular fracture and history of hip dislocation. An intraoperative fluoroscopic view (A) prior to surgical intervention shows a femoral head fracture (arrows), a small posterior wall fracture (arrowhead), and a subluxated hip joint. The intraoperative fluoroscopic view (B) after reduction and fixation of both fractures, performed at the same operative intervention using a trochanteric-flip osteotomy surgical approach35,38 is shown prior to reattachment of the trochanteric osteotomy. (Copyright Berton R. Moed, MD.) |
reaming has been shown to be an effective method for the management of
fractures of the femoral shaft. Considered the treatment of choice for
the majority of these fractures, its advantages include a rate of
fracture union approximating 98%, infrequent malunion, and a low
prevalence of infection.19,155,156,157
However, this surgical technique is not without its disadvantages,
including its potentially limited applicability in the treatment of the
femoral shaft fracture occurring in association with an ipsilateral
acetabulum fracture.108 In general,
with this combination of injuries, the femoral fracture is stabilized
first. If the femoral shaft fracture and acetabular fractures are to be
fixed in a staged fashion, once again, the treatment scheme should be
planned in a way to optimize treatment of the acetabular fracture. If
the incision for antegrade nailing will compromise the optimal surgical
approach to the acetabulum, an alternative femoral shaft fracture
treatment method should be selected, such as retrograde nailing (Fig. 45-5). When the femoral shaft and acetabular fractures are addressed as se
quential procedures during the same anesthesia, antegrade femoral
nailing still may not be the best choice. Compromised access to the
proximal femur, which may occur with a severely displaced associated
both-column fracture, or an irreducible dislocation of the femoral head
that precludes satisfactory femoral shaft fracture reduction are two
such situations. Alternatives include plating or retrograde nailing.
 |
|
FIGURE 45-5 An 18-year-old 390-pound man (A) was involved in a motor vehicle accident. Anteroposterior radiograph (B) of the hip and selected two-dimensional computed tomography section (C) show a T-type fracture of the acetabulum and an ipsilateral fracture of the femoral shaft (D). Retrograde nailing was used to stabilize the femur (E) followed by acetabular fixation 2 days later (F) using the Kocher-Langenbeck approach. (Copyright Berton R. Moed, MD.)
|
flexed knee on an automobile dashboard is a common cause of acetabular
fracture. Therefore, the knee must always be carefully evaluated for
instability, especially involving the posterior cruciate ligament.128
Often, this examination is difficult or limited because of patient
discomfort and an inability to cooperate because of the acetabular
fracture. In this situation, the knee should be examined under
anesthesia at the conclusion of any required hip surgery. Although
magnetic resonance imaging (MRI) of the knee has been advocated for all
patients with traumatic hip dislocation,128
the clinical importance of MRI findings not suspected from the initial
physical examination remains in doubt. Inability to perform an adequate
knee examination or continued knee symptoms in absence of clinical
findings indicate further evaluation is needed, such as MRI.
The prognosis for functional recovery of a sciatic nerve injury is
variable, depending on the degree of involvement of the peroneal
division. Complete or nearly complete motor and sensory recovery of an
injured tibial division can be expected in the majority of patients.39
However, patients with a severe injury of the peroneal division, in
isolation or in association with an injury of the tibial division,
cannot be expected to recover good function.39
Traumatic injury to the femoral nerve in association with a fracture of
the acetabulum is rare, having a prevalence of 0.2%, and recovery of
function can usually be expected to occur.47
Although the superior gluteal nerve and obturator nerves are
particularly at risk with some fracture patterns, it can be impossible
to assess their function in a patient with an acute fracture.
Therefore, the prevalence of their traumatic injury and subsequent
functional recovery are yet to be determined.
trauma is often very helpful, especially when determining the specific
cause of injury. As previously noted, in most cases, the patient with a
fracture of the acetabulum has sustained high-energy trauma and these
patients often will have an associated injury that must be identified
during the initial work-up. The pattern of the acetabular fracture
depends on the position of the hip at the time of impact, as well as
the location and magnitude of the applied force (see Table 45-1).
The information provided may indicate a history of axial loading
through the lower extremity at the knee with the knee flexed versus at
the foot with the knee extended or a direct blow injury. Therefore, a
history of being a passenger or driver involved in a motor vehicle
accident as opposed to being a pedestrian struck by a motor vehicle or
having experienced a fall from a height can provide an expectation of
the fracture type in addition to a tip-off to potential associated
musculoskeletal injury. If awake and alert, the patient may complain of
knee pain, being the first indication of an injury to the knee
(patellar fractures, chondral injuries, and ligamentous injuries).
Patients with a history of lower energy trauma (sports-related injury,
simple fall, etc.) in conjunction with hip pain require complete
evaluation of the hip joint. An acetabular fracture resulting from a
low-energy injury, such as a simple fall, is usually an isolated
musculoskeletal injury in underlying osteopenic bone. However, it is
important to assess the reason for the fall. A critical underlying
cardiac or neurologic medical condition may be the cause, especially in
the elderly.
with an apparent isolated injury, should be just one part of a
comprehensive and systematic approach. Detailed examination of the hip
and lower extremity is performed during the secondary survey of the
Advanced Trauma Life Support evaluation sequence.4
This detailed physical examination is a necessity. The soft tissues
should be carefully evaluated, as soft tissue injury has important
implications for subsequent surgery. Acetabular fracture surgery
through a compromised soft tissue envelope is ill advised because of
the increased risk of infection. Open wounds usually require
débridement followed by delayed wound closure. Closed degloving
soft-tissue injuries over the trochanteric region associated with
underlying hematoma formation and fat necrosis (the Morel-Lavallee
lesion) may be initially recognized by a fluid wave on palpation or may
be later identified by the presence of a fluctuant, circumscribed area
of cutaneous anesthesia and ecchymosis. These injuries, even when
closed, can be associated with the presence of pathogenic bacteria.49 Therefore, débridement followed by delayed wound closure and, subsequently, delayed fracture fixation may be required.49,78
More recently, a percutaneous method has been reported in a small
number of patients, using a plastic brush to débride the injured fatty
tissue, which is then washed from the wound with pulsed lavage.149
A medium closed-suction drain is placed within the lesion and removed
when drainage is less than 30 mL over 24 hours. Fracture fixation is
deferred until at least 24 hours after drain removal.
important, it may fail to identify a dislocation of the hip. Shortening
of the entire limb should be present if the hip is dislocated. However,
limb shortening of 1 or 2 cm is often hard to determine in this
clinical setting. The physical findings regarding limb position
commonly ascribed to a posterior dislocation of the hip (flexion,
adduction, and internal rotation of the hip with a shortened lower
extremity) may not be present.39,40
There are a few reasons for this situation. First, a dislocation may
not be present at the time the patient presents to the hospital.
Posterior wall fractures can occur with or without an associated frank
dislocation of the hip joint, and a patient initially sustaining a
posterior wall fracture-dislocation may have had the dislocation
inadvertently reduced by the emergency personnel on the scene while
being stabilized for transport to the hospital. Second, despite the
existence of a posterior hip dislocation, the presence of a larger
posterior wall fracture allows the femoral head to dislocate directly
posterior without forcing the proximal femur into the expected abnormal
position (Fig. 45-6). Therefore, the treating
physician must have a high level of suspicion of posterior wall
fracture for any lower extremity injury that potentially causes
abnormal loading to the hip joint. The absence of clinical
signs
of a dislocated hip or the lack of a history of hip dislocation does
not preclude the presence of a significant posterior wall fracture.96
 |
|
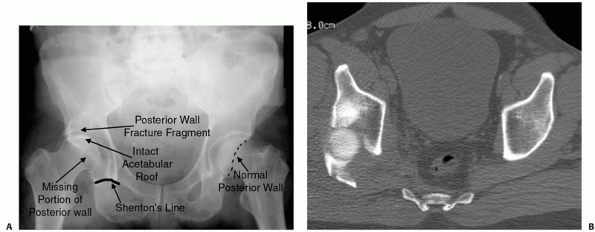
FIGURE 45-6 A.
Anteroposterior radiograph showing a dislocated hip on the right with the hip in neutral position. Radiographic signs of a posterior hip dislocation include a break in the Shenton line, proximal migration of the lesser trochanter, relatively smaller size of the affected femoral head (closer to the x-ray cassette), and a bony double density above the femoral head. The double density is the posterior wall fragment. It often sits atop the dislocated femoral head and can give the appearance of a normal joint space, potentially resulting in a misdiagnosis. B. Computed tomography shows a large displaced posterior wall fracture with the femoral head essentially fallen posteriorly through the posterior wall deficit. (Copyright Berton R. Moed, MD.) |
is extremely important both for patient prognosis and medicolegal
concerns. Sciatic nerve injury is common in fractures with a posterior
hip dislocation and fracture displacement of the posterior wall or
column.78 It is often incomplete, most often involving the peroneal division.39,60,78,99
However, depending on the particular mechanism (i.e., stretch,
impalement by fracture fragments, crush), injury can occur to smaller
components of the nerve. Therefore, isolated sensory deficits and
weakness or total loss of movement of individual muscles can occur. For
example, it is possible on physical examination to have complete loss
of tibialis anterior muscle function with the other muscles innervated
by the sciatic nerve appearing to be intact. It is no wonder why these
nerve injuries can be easily missed. Obviously, it is much better to
diagnose at the time of injury than in the postoperative period, when
the cause of the deficit could be attributed to an iatrogenic, rather
than a traumatic, cause. Therefore, a detailed examination is mandatory.
acetabular fractures are based on imaging studies that have been
derived from a thorough understanding of the anatomy of the innominate
bone.64,78
The innominate bone is formed as a condensation of pubis, ischium, and
ilium at the triradiate cartilage, which fuse at the time of skeletal
maturity. The articular surface of the acetabulum can be visualized as
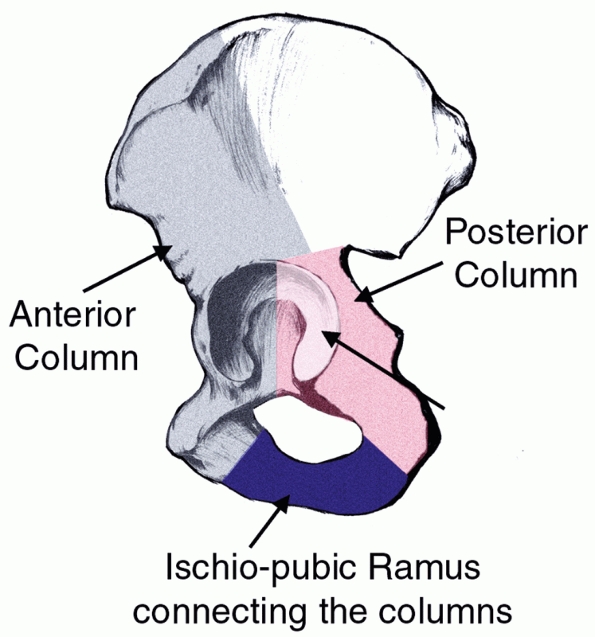
being supported between limbs of an inverted “Y” of bone (Fig. 45-7).
These columns are, in turn, connected to the sacroiliac articulation by
a thick strut of bone lying above the greater sciatic notch, known as
the sciatic buttress. Letournel was the first to describe the surgical
anatomy of the innominate bone, identifying these two limbs as the
anterior column or iliopectineal segment and posterior column or
ilioischial segment.64,78
The anterior column refers to the anterior half of the iliac wing that
is contiguous with the pelvic brim to the superior pubic ramus, as well
as the anterior half of the acetabular articular surface. The posterior
column begins at the superior aspect of the greater sciatic notch and
is contiguous with the greater and lesser sciatic notches inferiorly
and includes the ischial tuberosity (Fig. 45-8).
In addition, by recognizing that the plane of the ilium is
approximately 90 degrees to the plane of the obturator foramen and that
both of these structures are oriented roughly 45 degrees to the frontal
plane, Judet and Letournel64,78
determined that the AP pelvis and two 45-degree oblique views be used
to study the radiographic anatomy of the acetabulum. Therefore, three
radiographic projections of the pelvis are used to evaluate fractures
of the acetabulum: the AP view of the pelvis, the obturator (or
45-degree internal, Judet) oblique view, and the iliac (or 45-degree
external, Judet) oblique view.78
Interpretation of these plain films is based on the understanding of
normal radiographic landmarks of the acetabulum and disruption of these
landmarks represents a fracture involving that portion of the bone.
These landmarks are referred to as “lines,” but they are not
necessarily created by specific bony structures. Rather, they are
generated by the tangency of the applied x-ray beam to a region of
cortical bone.
 |
|
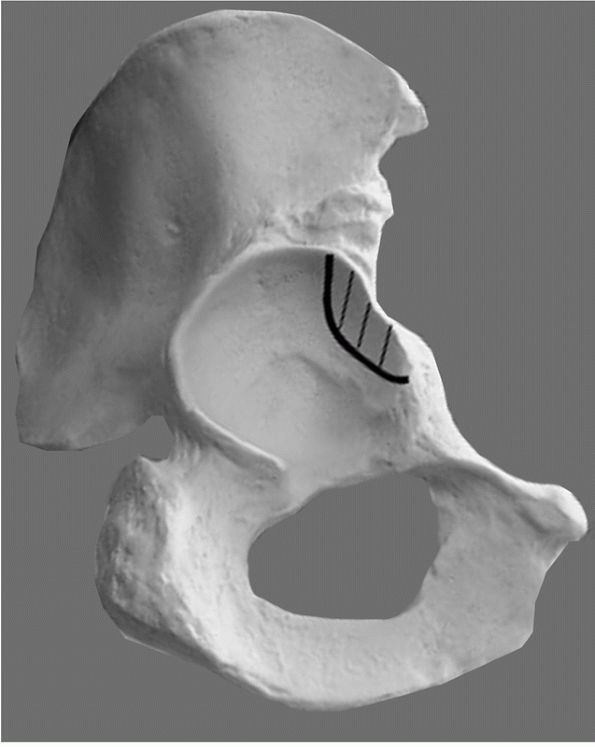
FIGURE 45-7
The acetabulum is supported by two columns in the shape on an inverted “Y.” These are in turn linked to the sacrum by the sciatic buttress. |
 |
|
FIGURE 45-8 Columns of the acetabulum as described by Letournel and Judet.76 (Copyright Berton R. Moed, MD.)
|
 |
|
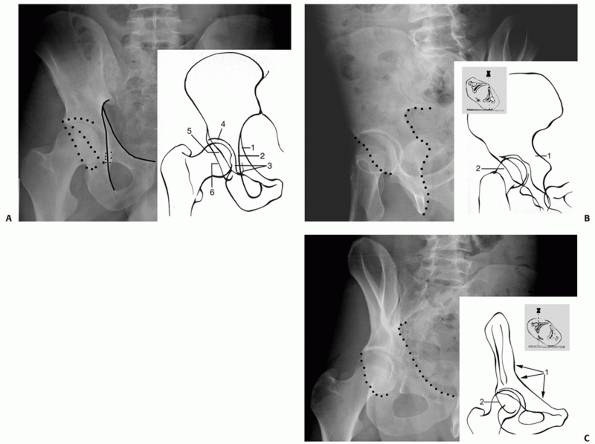
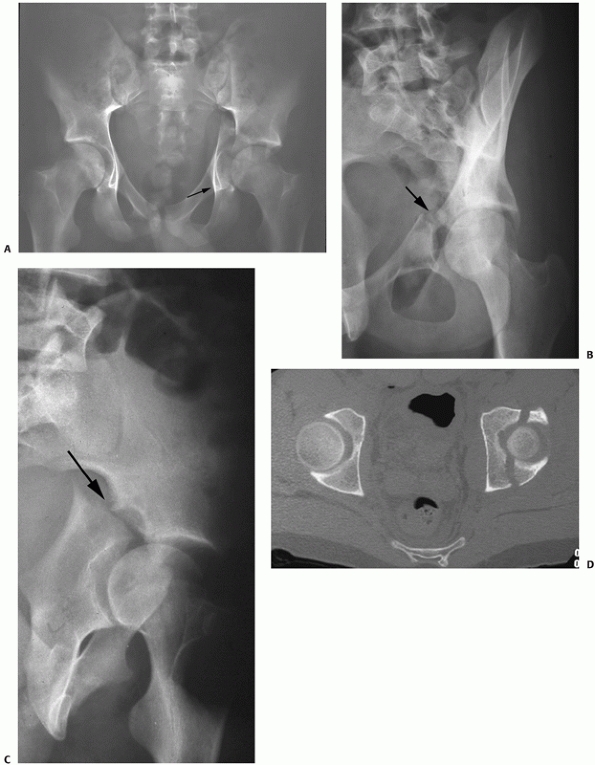
FIGURE 45-9 Radiographic lines of the acetabulum on different radiographic views. A. Anteroposterior (AP) radiograph of the pelvis. 1, Iliopectineal line; 2, ilioischial line; 3, teardrop; 4, acetabular roof; 5, anterior rim of the acetabulum; 6,
posterior rim of the acetabulum. The iliopectineal line, the anterior rim, and teardrop are landmarks of the anterior column; the ilioischial line and posterior rim are landmarks of the posterior columns. B. Iliac oblique radiograph. 1, Posterior border of the innominate bone. 2, Anterior rim of the acetabulum, which is seen best on this view. The iliac wing is seen en face, and fracture lines extending into the iliac wing are often best seen on this view. The proper amount of rotation is indicated by the tip of the coccyx lying just above the center of the contralateral femoral head. C. Obturator oblique radiograph. 1, Iliopectineal line. 2, Posterior rim of the acetabulum. The obturator ring is seen en face, and posterior wall fractures are seen best on this view. The proper amount of rotation is indicated by the tip of the coccyx lying just above the center of the ipsilateral femoral head. |
These are the iliopectineal line, the ilioischial line, the
radiographic U or teardrop, the roof of the acetabulum, the anterior
rim of the acetabulum, and the posterior rim of the acetabulum.78
The iliopectineal line is the major landmark of the anterior column.
The anterior three-quarters of the iliopectineal line represent the
pelvic brim. The posterior quarter of this line is formed by the
tangency of the x-ray beam to the internal cortical surface of the
sciatic buttress and the internal part of the roof of the greater
sciatic notch. The ilioischial line is formed by the tangency of the
x-ray beam to the posterior portion of the quadrilateral surface
(internal cortical surface of the acetabulum) and is considered a
radiographic landmark of the posterior column. The radiographic U or
teardrop consists of a medial and lateral limb and represents a
radiographic finding and not a true anatomic structure. The lateral
limb represents the inferior aspect of the anterior wall in the
acetabulum, and the medial limb is formed by the obturator
canal
and the anteroinferior portion of the quadrilateral surface. Because
the teardrop and the ilioischial line both result, in part, from the
tangency of the x-ray beam to a portion of the quadrilateral surface,
they are always superimposed on the AP pelvis view of the normal
acetabulum.64,78
Dissociation of the teardrop and the ilioischial line indicates either
rotation of the hemipelvis, or a fracture of the quadrilateral surface.84
The roof of the acetabulum is a radiographic landmark resulting from
the tangency of the x-ray beam to a narrow portion of the subchondral
bone of the superior acetabulum.78
Interruption of the radiographic line of the roof indicates a fracture
involving the superior acetabulum. The anterior rim represents the
lateral margin in the anterior wall of the acetabulum and is contiguous
with the inferior margin of the superior pubic ramus.64
The anterior rim is typically medial to the posterior rim and has a
characteristic undulation in its midcontour in the AP pelvis view. The
posterior rim represents a lateral margin in the posterior wall of the
acetabulum. Inferiorly, the posterior rim is contiguous with the
thickened condensation of the posterior horn of the acetabulum and
approximates a straight line, being more vertical than the anterior
wall.78
view) is taken with the patient rotated so that the injured hemipelvis
is tilted 45 degrees away from the x-ray beam (Fig. 45-9B).
This view shows the iliac wing in its largest dimension and profiles
the greater and lesser sciatic notches, as well as the anterior rim of
the acetabulum. Involvement of the posterior column is often best seen
on this view.78,115 Fractures of the anterior column traversing the iliac wing can also be detected.
oblique view) is taken with the patient rotated so that the hemipelvis
of interest is rotated 45 degrees toward the x-ray beam (Fig. 45-9C).
This view shows the obturator foramen in its largest dimension and
profiles the anterior column. The iliopectineal line has the same
relationship with the pelvic brim as on the AP pelvis. The posterior
rim of the acetabulum is best seen in the obturator oblique view.
Comparison of the relationship of the femoral head with the posterior
wall on the normal hip and the injured hip on the obturator oblique
view will allow the surgeon to detect subtle amounts of posterior
subluxation. A dislocated hip will become more obvious on the obturator
oblique view,17 and this view has been advocated for routine evaluation of all posterior fracture dislocations of the hip joint129 (Fig. 45-10).
Despite the potential advantages of this “obturator oblique dislocated
view,” it is prudent not to delay the reduction of a known dislocated
hip.
 |
|
FIGURE 45-10 Anteroposterior (A) and obturator oblique view (B) showing a dislocated hip with an associated posterior wall fracture. (Copyright Berton R. Moed, MD.)
|
pelvis radiograph obtained during the ATLS survey, including the
initial diagnosis of the acetabular fracture and hip dislocation (see Fig. 45-6A).
The two 45-degree oblique views ( Judet views) aid in classification of
the fracture and to identify fracture displacements that may not be
appreciable on the AP radiograph. These plain radiographs should be
obtained with the patient out of traction; otherwise, there may be a
false impression of hip joint congruity or an underestimation of
fracture displacement. The Judet views are obtained by rolling the
patient 45 degrees in relation to the x-ray beam. This may be difficult
and painful for the patient and premedication is often required. To
ensure that an appropriate oblique view is obtained, it is crucial that
the pelvis is rotated the required amount (see Fig. 45-9B, C).
Recently, CT-derived, reconstructed radiographs have been offered as an
alternative to this method of obtaining plain radiographs.13,28,143
Regardless of the method, an inadequately obtained radiograph may not
demonstrate the radiograph landmarks needed to accurately determine the
fracture pattern (Table 45-2).
assess for associated injuries. However, it does not replace the
standard radiographic evaluation.22,51,78,92
Therefore, two-dimensional (axial) and three-dimensional CT scans are
used as an adjunct to the analysis of the AP and oblique plain
radiographic projections.78,109,147 In order to obtain reliable and useful information,
the CT scan should consist of contiguous sections of no more than 3 mm
in thickness. After studying the plain films, the surgeon should use CT
to answer specific questions about the fracture that remain unanswered.
Orientation of the fracture line(s) can be very helpful in
distinguishing among fracture types (Fig. 45-11).
In addition, two-dimensional axial images are superior to plain films
in showing (a) the extent and location of acetabular wall fractures,
(b) the presence of intra-articular free fragments or injury to the
femoral head, (c) orientation of fracture lines, (d) identification of
additional fracture lines (such as the vertical portion of the “T” type
fracture and fractures of the quadrilateral plate), (e) rotation of
fracture fragments, (f) the status of the posterior pelvic ring, and
(g) marginal impaction, defined as depression of the articular surface
of the joint78,147 (Fig. 45-12).
In one study, the two-dimensional CT was shown to be superior to plain
radiographs in the detection of fracture step and fracture gap
deformities.13 However,
displacements that occur in the plane of imaging may be
underappreciated or averaged out. Although two-dimensional CT has also
been advocated as a means to determine hip joint stability,23,69,150 this has proved unreliable.95 Furthermore, CT analysis may overestimate the extent of fracture comminution.78
When reviewing a two-dimensional CT study, it is important to evaluate
the extent of the fracture fragments by following the fracture lines
sequentially through the contiguous sections of the scan. In this way,
errors of interpretation (such as mistaking the posterior inferior
extent of a transverse fracture for a separate posterior wall fracture)
can be avoided.
|
TABLE 45-2 Information Obtained from X-Ray Landmarks on Each Standard View
|
||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||
point that it is helpful in further defining the fracture pattern and,
thereby, assisting in preoperative planning. However, it does not
provide the diagnostic detail of the two-dimensional CT scan. The
three-dimensional CT scan may also assist the surgeon who is
inexperienced in interpreting the plain radiographs in developing a
better understanding of the fracture patterns. The understanding of the
fracture pattern is further enhanced by drawing the fracture lines from
the radiograph landmarks onto a dry bone model or a line drawing of the
pelvis as seen on each radiograph view. Only by understanding the
location and orientation of each fracture line can the fracture pattern
be truly appreciated.
 |
|
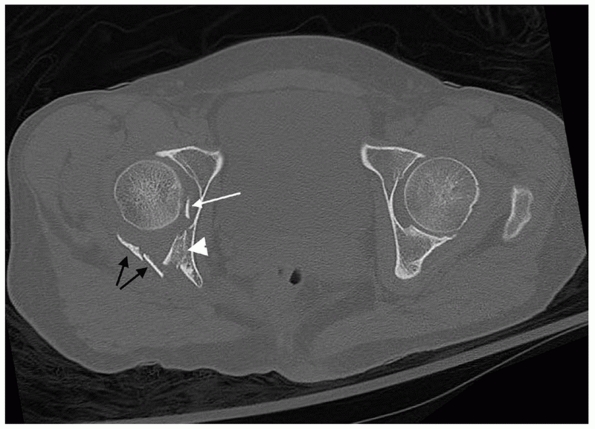
FIGURE 45-11 Orientation of fracture lines on two-dimensional computed tomography as they relate to fracture morphology. A. Fracture of one or both columns. B. Transverse fracture. C. Anterior wall. D. Posterior wall.
|
used as a clinical measure of dynamic stability and congruence of the
hip, and advocated as an adjunctive imaging study to
assess the need for operative treatment in small and intermediate fractures of the posterior acetabular wall.96,97,99,109,136,148,150 This stress examination is most applicable to fractures of the posterior wall.148
For this examination, the patient is placed supine with the hip in
neutral rotation and full extension. The hip is then gradually flexed
past 90 degrees while progressive manual force is applied through the
hip along the longitudinal axis of the femur. Simultaneously,
fluoroscopic imaging of the hip in the AP and obturator oblique
projections is performed.96,97,150
If the hip remains congruent on this assessment, the exam is repeated
with the addition of slight adduction and internal rotation
(approximately 20 degrees).96,97,150
Frank redislocation is neither required nor clinically desirable.
Posterior subluxation demonstrated in either view (indicted by a
widening medial joint space or loss of joint parallelism) is indicative
of dynamic hip instability (Fig. 45-13).
 |
|
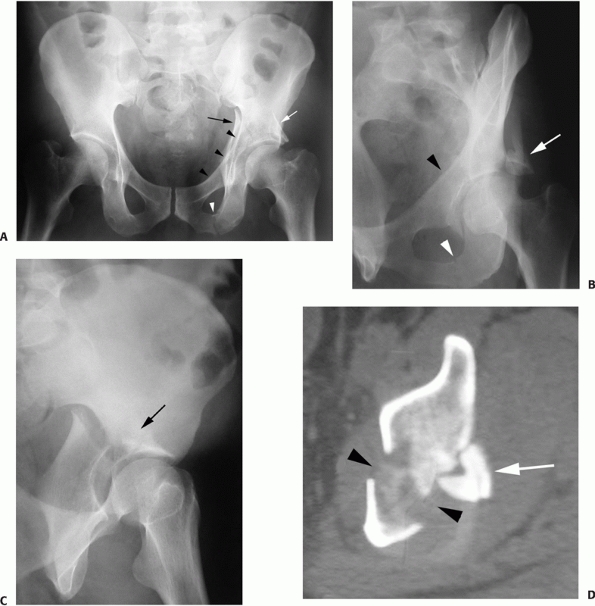
FIGURE 45-12 Axial computed tomography section through the acetabulum. The right acetabular posterior wall is fractured (black arrows). There is an intra-articular loose body between the femoral head and acetabulum (white arrow). The asymmetry of the contour of the posterior wall from side to side is secondary to marginal impaction (white arrowhead),
which occurs when a segment of the articular surface and underlying cancellous bone adjacent to a major fracture line is impacted or depressed away from the normal contour of the joint. (Copyright Berton R. Moed, MD.) |
systematic classification of acetabular fractures, initially published
as a thesis by Letournel in 1961.76
This classification is based on the anatomic pattern of the fracture.
It was derived by first understanding the radiograph landmarks on the
intact dry innominate and then analyzing these landmarks in fracture
cases.64
and offer no clinical advantage. Therefore, the “Letournel” acetabular
fracture classification continues to remain the international language
of the majority of surgeons treating these complex injuries. This
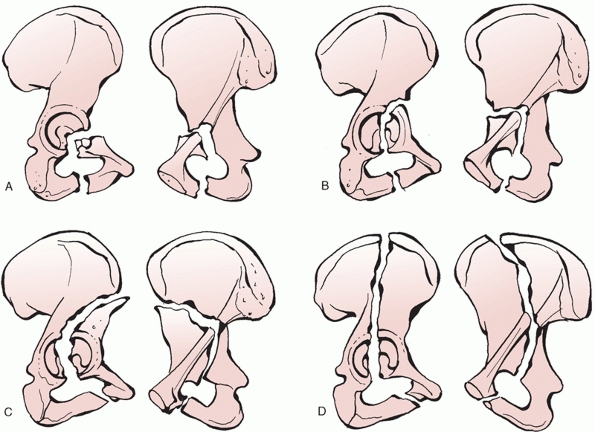
classification has 10 distinct categories, which are divided into five
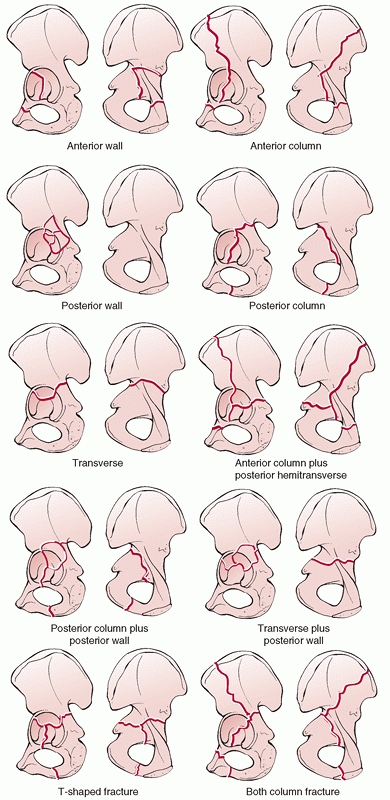
elementary types and five associated types (Fig. 45-14).
The five elementary fracture patterns are the anterior wall, anterior
column, posterior wall, posterior column, and transverse (Table 45-3).
The elementary fracture patterns are defined as those fractures that
separate all or part of a single column of the acetabulum. The anterior
and posterior column fractures separate the entire column from the
intact innominate, while the anterior and posterior wall fractures
separate only that portion of the column’s articular surface. The
transverse fracture pattern consists of a single fracture line that
traverses both the anterior and posterior columns of the acetabulum.
This fracture is included as elementary because of the fundamental
nature of the fracture pattern. The associated patterns are either a
combination of elementary patterns or an elementary pattern with an
additional fracture component. The five associated fracture patterns
are the posterior column and posterior wall, anterior column or wall
with posterior hemitransverse, transverse and posterior wall, T-shaped,
and both-column fracture (see Table 45-3).
 |
|
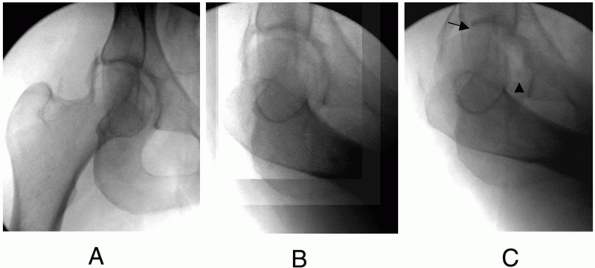
FIGURE 45-13 Fluoroscopic views showing the dynamic examination under anesthesia. A. The intraoperative obturator oblique fluoroscopic view with the hip in full extension shows a located and congruent hip joint. B.
The intraoperative obturator oblique fluoroscopic view with the hip in neutral rotation and flexed to approximately 90 degrees shows a located and a congruent hip joint. C. The intraoperative obturator oblique fluoroscopic view with the hip in neutral rotation and flexed to approximately 90 degrees with axial load applied shows gross subluxation with loss of hip joint parallelism and joint congruency (arrow) and gross enlargement of the medial clear space (arrowhead). (From Moed BR, Ajibade DA, Israel H. Computed tomography as a predictor of hip stability status in posterior wall fractures of the acetabulum. J Orthop Trauma 2009;23:7-15.) |
However, they can usually be easily integrated into the system. This
system is important not only for its ability to describe the fracture,
but it also serves as a guide for subsequent operative treatment. High
rates of interobserver and intraobserver reliability have been reported
using this classification system based purely on interpretation of the
three standard plain radiographs of the pelvis.9
the most common type of acetabular fracture, accounting for
approximately 25% of all acetabular fractures.78,83,99
The simple appearance of the posterior wall fracture on plain
radiographs underestimates its potential complexity. Rather than having
one
simple
fracture fragment, most posterior wall fractures are comminuted or have
areas where the articular surface along the margin of the primary
fracture line is impacted into the underlying cancellous bone.
Fractures of the posterior wall can be visualized on the AP and
obturator oblique radiographs with the obturator oblique providing the
best radiograph view (Fig. 45-15).
The AP pelvis radiograph will generally reveal a disruption only in the
posterior rim shadow. If the wall fragment is large enough and superior
in location, the roof shadow may also be disrupted. The obturator
oblique radiograph will demonstrate the size and multifragmentary
nature of the fracture. The iliac oblique view will reveal that the
posterior border of the innominate bone, the anterior border of the
acetabulum, and the iliac wing are uninvolved. CT scans are
particularly helpful in identifying fracture comminution and marginal
impaction (see Fig. 45-12). Marginal impaction
is a rotated and impacted osteochondral fragment that is displaced as
the femoral head dislocates and the wall fractures (Fig. 45-16). This may occur with
any fracture pattern but has been documented in up to 46% of posterior wall fractures.99
 |
|
FIGURE 45-14 Letournel acetabular fracture classification.
|
|
TABLE 45-3 Letournel Classification of Acetabular Fractures
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
FIGURE 45-15 Radiographs of a posterior wall fracture. A. Anteroposterior view shows all radiographic landmarks to be intact except the posterior rim (arrow). B. The obturator oblique view shows the displaced posterior wall fracture (arrow). C. The iliac oblique view shows an intact posterior border. (Copyright Berton R. Moed, MD.)
|
 |
|
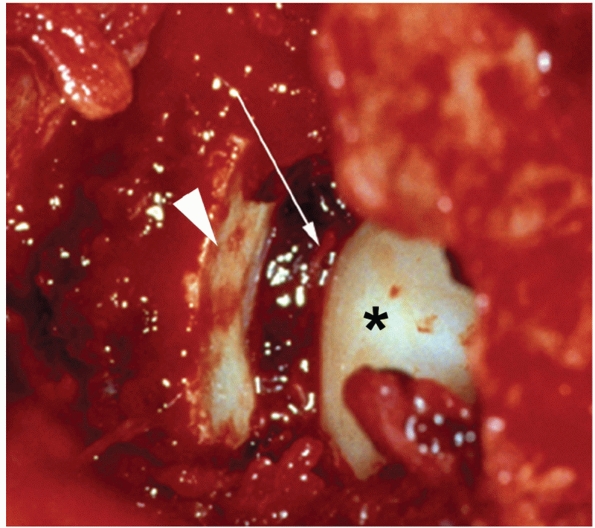
FIGURE 45-16 Intraoperative photograph shows the femoral head (asterisk), the remaining intact articular surface (white arrow), and a large marginally impacted fragment (white arrowhead).
(From Moed BR, McMichael JC. Outcomes of posterior wall fractures of the acetabulum: Surgical technique. J Bone Joint Surg Am 2008;90A(suppl 1):87-107.) |
 |
|
FIGURE 45-17 Radiographic appearance of the posterior column fracture. A. On the anteroposterior view, the displacement of the ilioischial line (arrow) is apparent while the iliopectineal line is seen to be intact (black arrowheads). As typical, the ilioischial line (arrow) is displaced relative to the radiographic U (white arrowhead). B. The obturator oblique view confirms the anterior column to be intact (arrowheads) and demonstrates the fracture of the ischial ramus (arrow). C. The iliac oblique view shows the disruption of the greater sciatic notch and the displacement of the posterior column (arrow). D. The computed tomography section shows a fracture line typical of a posterior column fracture. (Copyright Berton R. Moed, MD.)
|
the entire ischioacetabular segment from the innominate bone and
represent 3% to 5% of acetabular fractures.78,83,90
The fracture begins at the posterior border of the innominate bone,
near the apex of the greater sciatic notch. It descends across the
articular surface, quadrilateral surface, ischiopubic notch (roof of
the obturator canal), and finally across the inferior ramus. On the AP
radiograph, the ilioischial line, the posterior rim, and the inferior
ramus are disrupted. The disruption of the posterior rim will be seen
in only one location, where the fracture line crosses the rim. This is
in distinction to the posterior wall fracture where the posterior rim
will be seen to be disrupted in two locations, separating a portion of
the articular surface. The iliac oblique radiograph demonstrates the
fracture crossing the posterior border of the bone. The fracture of the
ischiopubic ramus and posterior rim are confirmed on the obturator
oblique. The iliopectineal line is preserved on all views. The femoral
head follows the displacement of the posterior column posteriorly and
medially (Fig. 45-17). The ilioischial line is typically displaced relative to the radiographic U (Fig. 45-17A).
However, when a large portion of the quadrilateral surface remains
intact with the posterior column, the radiographic U will displace with
the ilioischial line.78 Fractures of
the posterior column are notoriously unstable and skeletal traction is
frequently required to keep the femoral head reduced beneath the intact
portion of the roof. The posterior column fracture frequently involves
the greater sciatic notch at or above the location of the superior
gluteal neurovascular bundle. In widely displaced fractures, it is
common to find the neurovascular bundle in the posterior column
fracture site and it must be carefully extracted before reduction of
the fracture to prevent iatrogenic injury.
proceeds down the quadrilateral surface to the ischiopubic notch. A
secondary fracture line through the superior ramus detaches the
anterior wall portion. Anterior wall fractures are rare, and constitute
only 1% to 2% of all fractures.78,83,90
The anterior rim shadow and the iliopectineal line on the AP radiograph
will show displacement in two locations, but all posterior landmarks
will remain intact. A portion of the quadrilateral surface may be
detached with the anterior wall and this may result in an apparent
“thinning” or reduplication of the ilioischial line but some portion of
the line will remain intact. Femoral head subluxation is commonly seen
and the head will be noted to follow the anterior wall fragment,
particularly visible on the obturator oblique radiograph (Fig. 45-18).
basic fracture types, which can usually be easily integrated into the
system. In the morphologic description of the anterior wall fracture,
as detailed above, a segment of the inner table of the pelvis (the
pelvic brim) is included with the anterior rim fragment (see Fig. 45-14).
A different fracture pattern involving the anterior acetabular rim,
which does not include the inner table, has been categorized as the
“anterior wall” fracture type by the AO in their classification system.56 In addition, the 1993 publication of Letournel and Judet reveals no similarly described fracture.78
No classification system can be expected to describe every possible
variant and exceptions are the norm. However, it is quite apparent that
there is some uncertainty in the literature regarding the anterior
wall, possibly contributing to confused diagnoses and treatment
recommendations. This isolated anterior wall fracture, which does not
involve the pelvic brim, is the morphologic analogue to the posterior
wall fracture (Fig. 45-19). This variant is rare, constituting approximately 1.5% of acetabular fractures in one series.74
 |
|
FIGURE 45-18 Radiographic appearance of the anterior wall fracture, as described by Letournel and Judet.76 A. On the anteroposterior (AP) view, the disruption of the iliopectineal line is seen in two locations. B. The obturator oblique confirms this and demonstrates that the femoral head remains congruent to the anterior wall segment. C.
The iliac oblique view confirms the posterior border of the bone to be intact and that the ilioischial line disruption seen on the AP view is because of a fragment of quadrilateral surface comminution and does not represent a fracture through the posterior border of the innominate bone. This explains the normal position of the ischium despite the ilioischial line displacement. (Courtesy of Michael Stover, MD.) |
Anterior column fractures separate the anterior border of the
innominate bone from the intact ilium. The type of anterior column
fracture is named by the location where the fracture exits the anterior
aspect of the bone. High anterior column fractures exit the iliac
crest, intermediate fractures exit the anterior superior iliac spine,
low fractures exit the psoas gutter just below the anterior inferior
iliac spine, and very low anterior column fractures exit the bone at
the iliopectineal eminence (Fig. 45-20). All
anterior column fractures, regardless of where they exit the bone
superiorly, cross the pelvic brim, proceed down the quadrilateral
surface, and enter the ischiopubic notch, ultimately ending in a
fracture of the inferior ramus. Typically, the lower the fracture
crosses the anterior border of the bone, the more inferior is the site
of fracture of the ischiopubic ramus. As in the anterior wall
fractures, it is common for a portion of the quadrilateral surface to
be detached as a separate fragment but the posterior border of the
innominate bone remains intact. The iliopectineal line is disrupted in
one location on the obturator oblique and AP views. The very low
anterior column fracture can be distinguished from the typical anterior
wall fracture in that it has a fracture of the inferior pubic ramus and
a single break in the iliopectineal line. The femoral head displaces
with the anterior column fracture. The typical displacement
is an external rotation of the anterior fragment about the femoral head, allowing the head to move medial and superior (Fig. 45-21).
 |
|
FIGURE 45-19
Plastic bone model showing the anterior wall fracture variant drawn on the intra-articular surface of the acetabulum. (Copyright Berton R. Moed, MD.) |
They are the only elementary fracture pattern that breaks both the
anterior and posterior border of the innominate bone. The fracture
separates the innominate bone into two pieces: the upper iliac piece
and the lower ischiopubic segment. The upper fragment is intact to the
ilium, while the ischiopubic fragment rotates about the symphysis
pubis. This results in a medial and superior displacement of the head,
as it follows the ischiopubic segment. This rotation also typically
produces a greater translational displacement of the transverse
fracture at the posterior border rather than the anterior border of the
bone. Transverse fractures are subdivided by where the fracture crosses
the articular surface. Transtectal fractures cross the weight-bearing
dome of the acetabulum. Juxtatectal fractures cross the articular
surface at the level of the top of the cotyloid fossa. Infratectal
fractures cross the cotyloid fossa (Fig. 45-22).
As the location of the fracture moves more superior on the articular
surface, the orientation of the fracture also becomes more vertical and
the size of the intact remaining articular surface decreases. This has
definite implications for the surgical treatment of these injuries. The
AP radiograph demonstrates a disruption of both the ilioischial and
iliopectineal lines as well as the anterior and posterior rim shadows.
In transtectal fractures, the roof line will be disrupted as well.
However, the ilioischial line maintains its normal relationship with
the radiographic U, as there is no fracture at this level. The oblique
views will show disruption of the pelvic brim as well as the posterior
border of the bone. The ischial ramus will not be fractured. On CT
scan, the fracture line is oriented in an AP direction in the axial
section (Fig. 45-23).
 |
|
FIGURE 45-20 The various subgroups of the anterior column fracture: (A) very low, (B) low, (C) intermediate, and (D) high. (After Letournel E, Judet R. Fractures of the acetabulum. 2nd ed. Berlin: Springer-Verlag, 1993.)
|
combination of the two elementary fracture patterns, posterior column
and posterior wall, and makes up 3% to 4% of fractures.78,83,90 The posterior column fracture divides the posterior border of
the innominate bone and the ischium to produce a free ischioacetabular
fragment. The posterior wall component can be thought of as articular
comminution of the posterior rim where the posterior column fracture
traverses it. The femoral head is frequently dislocated on
presentation, with the femoral head following the ischioacetabular
fragment and dislocating cranially and posteriorly. The posterior wall
fragment remains with the femoral head while dislocated but typically
stays in a displaced position once the femoral head is reduced. The
posterior wall fracture may block reduction of the hip by interposition
between the head and the posterior column or by incarcerating within
the joint. Radiographically, the disrupted landmarks, as expected, are
the ilioischial line, posterior border of the innominate bone, and the
posterior rim. The radiograph roof may also be displaced depending on
how superior the posterior wall component extends. The displacement of
the posterior column may be difficult to assess on the AP radiograph as
posterior displacement of the column may result in the ilioischial line
maintaining an almost normal relationship to the radiograph teardrop (Fig. 45-24).
 |
|
FIGURE 45-21 Radiographic appearance of the anterior column fracture. A.
The AP view demonstrates the fracture from the iliac crest to the hip joint with disruption of the roof. A small area of comminution at the pelvic brim is noted. The ischial ramus fracture is also noted. B. The obturator oblique demonstrates a single break in the iliopectineal line where the anterior column fracture crosses the pelvic brim. Although difficult to see, the disruption of the ilium can be appreciated as a reduplication of the cortical lines of the internal iliac and fossa and external wing of the ilium. C. The iliac oblique view confirms the posterior border of the bone to be intact. |
 |
|
FIGURE 45-22 The various subgroups of the transverse fracture. Infratectal type (A), juxtatectal type (B), and transtectal type (C). (Redrawn after Letournel E, Judet R. Fractures of the acetabulum. 2nd ed. Berlin: Springer-Verlag, 1993.)
|
 |
|
FIGURE 45-23 Radiographic appearance of the transverse fracture. A.
The anteroposterior pelvis view demonstrates disruption of four of the six radiograph landmarks of the acetabulum with the ilioischial line maintaining its normal relationship with the radiographic U (arrow), indicating that this is a transverse fracture below the level of the roof. Note the subluxation of the femoral head away from the intact portion of the acetabular roof. B. The obturator oblique view shows a break in the iliopectineal line (arrow) and subluxation of the femoral head with the displacement of the ischiopubic segment and verifies that the ischial ramus is not broken. C. The iliac oblique shows where the transverse fracture exits the greater sciatic notch (arrow) and again confirms the subluxation of the femoral head. D. This computed tomography section shows the orientation typical of a transverse fracture. (Copyright Berton R. Moed, MD.) |
 |
|
FIGURE 45-24 Radiographic appearance of the associated posterior column and posterior wall fracture. A. The anteroposterior pelvis radiograph shows the disruption of the ilioischial (black arrow) but not the iliopectineal lines (black arrowheads), and the ischial ramus fracture is present (white arrowhead), and the posterior wall fragment can be appreciated overlying the roof of the acetabulum (white arrow). B. The obturator oblique view shows the displaced posterior wall fragment (white arrow), the ischial ramus fracture (white arrowhead), and the intact iliopectineal line (black arrowhead). C.
The iliac oblique demonstrates the disruption of the greater sciatic notch and the posterior wall fragment superimposed on the roof of the acetabulum (black arrow). D. This computed tomography section shows the posterior wall fracture (arrow) with a column fracture line typical of a posterior column fracture (black arrowheads). (Copyright Berton R. Moed, MD.) |
elementary transverse and posterior wall fracture patterns and makes up
20% of all fractures.78,83,90
As with the elementary patterns, the transverse component may be
transtectal, juxtatectal, or infratectal and the posterior wall
component may be single or multifragmentary and associated with
marginal impaction. Dislocation of the femoral head is common in these
fractures and the dislocation may be either posteriorly through the
wall defect or medially through the transverse fracture. Distinction
between the two is important because an early recognition of a
posterior dislocation is necessary to minimize such complications as
osteonecrosis, sciatic nerve injury, and femoral head damage. When the
posterior wall fragment is minimally displaced, it may be missed on the
AP pelvis radiograph, but it is commonly seen on the obturator oblique
view, as well as with axial CT (Fig. 45-25).
involve either an anterior column or a wall fracture as the primary
fracture line. An associated transverse fracture component propagates
from the anterior fracture across the articular surface to the
posterior border of the innominate bone. This posterior hemitransverse
fracture is identical to the posterior half of a transverse fracture
and may occur at any of the levels described above. The anterior plus
posterior hemitransverse group makes
up about 7% of fractures, over three quarters of which involve the anterior column rather than the wall.78,83,90
Radiographically, these fractures exhibit all the features of an
anterior wall or column fracture but with displacement of the
ilioischial line and a fracture line that crosses the posterior border
of the bone on the iliac oblique. The displacement of the
hemitransverse fracture component is generally less severe than that of
the anterior fracture. However, the internal malrotation of the
posterior column component may allow more anteromedial translation of
the femoral head and striking displacements in comparison to the
isolated anterior column fracture (Fig. 45-26).
 |
|
FIGURE 45-25 Radiographic appearance of the associated transverse and posterior wall fracture (transtectal pattern). A.
The appearance on the anteroposterior radiograph is quite similar to that of the pure transverse fracture with disruption of five of the six radiograph landmarks; only the radiographic U (which maintains its normal relationship to the ilioischial line) remains intact. The posterior wall fragment is seen as an oblique cortical line overlying the intact roof (arrowhead). B. The obturator oblique shows the transverse fracture, the subluxation of the femoral head with the ischiopubic fragment, as well as the posterior wall fragment. It is easy to see on this view how the femoral head may abrade against the fracture edge while the hip is subluxated. C. The iliac oblique view highlights the fracture line exiting the greater sciatic notch as well as the posterior wall fragment superimposed on the roof of the acetabulum (black arrow). D. This computed tomography section shows the posterior wall fracture (white arrow) with a column fracture line typical of a transverse fracture (black arrowheads). (Copyright Berton R. Moed, MD.) |
and the isolated anterior column fractures are common fracture patterns
seen in the elderly after a fall onto the hip. The fracture pattern is
often complicated by impaction of the medial roof of the acetabulum and
has been termed the “gull wing” sign based on the radiograph appearance
on the AP radiograph (Fig. 45-27). The presence of this impaction is a poor prognostic sign.5
 |
|
FIGURE 45-26 Radiographic appearance of the associated anterior wall and posterior hemitransverse fracture. A.
The anteroposterior pelvis radiograph demonstrates the medial subluxation of the femoral head with segmental displacement of the iliopectineal line. The ilioischial line displacement is noted and, unlike the anterior wall fracture, the relationship of the ischium to the ilioischial line is preserved. Wear of the femoral head is seen laterally where the head is articulating with the edge of the intact roof. B. The obturator oblique radiograph appears similar to that seen in the isolated anterior wall fracture but the fracture is seen to be multifragmentary with impaction. Disruption of the posterior rim line is appreciated. C. The iliac oblique shows the disruption of the posterior border of the innominate and displacement through the greater sciatic notch. |
 |
|
FIGURE 45-27 The “gull wing” sign represents impaction of the acetabular roof (arrow)
and is a poor prognostic sign. Maintaining reduction of the impacted fragment is difficult and fragment displacement may allow recurrent subluxation of the femoral head and an incongruous hip joint. |
fractures and involves a transverse fracture with an associated
inferior vertical fracture line known as the stem of the T.78,83,90
The vertical stem usually propagates from the transverse fracture,
across the quadrilateral surface and cotyloid fossa, then enters the
obturator foramen through the ischiopubic notch, and ends in a fracture
of the ischial ramus, typically exiting through the ischiopubic ramus.
However, it may also extend posteriorly (exiting through the ischium)
or anteriorly (exiting near the pubic body). In any case, the caudal
ischiopubic segment created by the transverse fracture component is
divided into a posterior (ischial) and an anterior (pubic) articular
segment. Radiographically, the identification of the transverse
fracture in the presence of a fracture of the ischial ramus leads the
surgeon to recognize the T-shaped fracture (Fig. 45-28).
Diagnosis of the T-shaped fracture and recognition of columnar
displacements, both in relation to the intact innominate bone and to
each other, are crucial in treating the T-shaped fracture. The T-shaped
fracture may also be associated with a posterior wall fracture. This
subgroup of fractures is generally included in the transverse plus
posterior wall pattern but has been noted to have the worst prognosis
of any subgroup of fractures. Finally, fractures of the posterior
column with anterior hemitransverse associated fractures are classified
as T-shaped.
 |
|
FIGURE 45-28 Radiographic appearance of the T-shaped fracture of the patient shown in Figure 45-5. A.
The appearance on the anteroposterior pelvis radiograph may be distinguished from the transverse fracture by the presence of the fracture of the ischial ramus (white arrow). Displacement of the stem of the T may cause the ilioischial line to appear duplicated (black arrowheads). Likewise, the relationship between the ilioischial line, which remains with the posterior column, and the teardrop, which remains with the anterior column, may be disrupted (black arrow). B. The obturator oblique shows the break in the iliopectineal line (black arrow). It also allows better visualization of the stem of the T (white arrow) as it enters the roof of the obturator foramen and is associated with the ischial ramus fracture (arrowhead). C. The iliac oblique view demonstrates the disruption of the greater sciatic notch and subluxation of the femoral head. (Copyright Berton R. Moed, MD.) |
This fracture is unique in that it represents an acetabulum completely
disconnected from the axial skeleton. By definition, all both-column
fractures have no portion of the acetabular articular
surface
remaining attached to the innominate bone and there is a split between
an anterior and a posterior column component. Within this definition,
there is room for many different fracture patterns. In its most simple
form, an anterior column fracture may be associated with a simple
posterior column fracture (see Fig. 45-14).
This is the exception and usually there are secondary fractures
involving the anterior and posterior columns. Even in very comminuted
associated both-column fractures, the acetabular labrum usually remains
intact. Therefore, as the femoral head medializes because of muscular
pull, the articular fragments may each rotate around, yet remain
congruent to, the femoral head (Fig. 45-29). This creates a situation unique to both-column fractures that is known as “secondary congruence.”78,147 The radiograph “spur sign,” when present, is pathognomonic for the associated both-column fracture.78
This is seen best on the obturator oblique projection and represents
the external cortex of the most caudal portion of the intact ilium (Fig. 45-30).
It is generally seen only in the both-column fracture because the
femoral head medializes with all portions of the acetabular articular
surface. The surgeon should recognize that transverse fractures,
transverse and posterior wall fractures, T-shaped fractures, and
anterior/posterior hemitransverse fractures all involve the anterior
and posterior columns of the acetabulum but are not “both-column”
fractures. In these four fracture types, a portion of the articular
surface remains intact with the ilium.78 It is also common for the both-column fracture to have a posterior superior wall fracture component (Figs. 45-30 and 45-31).
 |
|
FIGURE 45-29
Drawing showing how the free articular fragments in a both-column fracture may each rotate around, yet remain congruent to, the femoral head. (From Matta JM. Operative indications and choice of surgical approach for fractures of the acetabulum. Tech Orthop 1986; 1:14.) |
the most important aspects of the preoperative planning for acetabular
fracture surgery. The main determinants in the decision-making process
are the fracture type, the elapsed time from injury to operative
intervention, and the magnitude and location of maximal fracture
displacement. A single surgical approach is generally selected with the
expectation that the fracture reduction and fixation can be completely
performed through the one approach.60,78,75,88 The mainstay surgical approaches to the acetabulum are those described by Letournel and Judet78:
the Kocher-Langenbeck, the ilioinguinal, the iliofemoral, and the
extended iliofemoral. The first three provide direct access to only one
column of the acetabulum (posterior for the Kocher-Langenbeck; anterior
for the ilioinguinal and iliofemoral) and rely on indirect manipulation
for reduction of any fracture lines that traverse the opposite column.
The extended iliofemoral approach affords the opportunity for almost
complete direct access to all aspects of the acetabulum. It is most
often used in associated fracture patterns that are surgically treated
more than 21 days after injury or on certain transverse or both-column
pattern fractures with complicating features that are not amenable to
treatment by the more limited approaches.
wall fractures and posterior column fractures with or without an
associated posterior wall fracture. Transverse and T-shaped fractures,
treated within 15 days of injury, are also amenable to this surgical
approach. In addition, for T-shaped fractures, the major displacement
should be posterior, with only minor displacement occurring anteriorly
at the pelvic brim (Table 45-4).
visualization of the entire lateral aspect of the posterior column of
the acetabulum (Fig. 45-32A). The greater and
lesser sciatic notches are visualized by transecting the piriformis and
obturator internus tendons and dissecting subperiosteally into the
notches. The most caudal portion of the ilium is accessible but the
superior gluteal neurovascular bundle limits proximal exposure.
Visualization may be extended anterosuperiorly by dividing a portion of
the gluteus medius insertion or performing a transtrochanteric
osteotomy but proximal access is still largely limited (Fig. 45-32B).
Indirect access to the quadrilateral surface can be attained by the
palpating finger or the use of special instruments placed through the
greater sciatic notch (Fig. 45-32C). A
posterior capsulotomy allows limited access to the posterior aspect of
the joint surface. This access is increased without the need for a
capsulotomy in the presence of a fractured posterior wall. This
approach has a relatively high risk for sciatic nerve injury and an
intermediate risk for heterotopic ossification.78,83,87
position. However, the prone position is preferred for the more complex
fracture types. Although most surgeons are more comfortable with
lateral positioning, the weight of the operative leg tends to cause
medial displacement of the femoral head and articular fragments. In
addition, access through the greater sciatic notch for palpation or
clamp placement is impaired. Prone positioning of the patient in
traction neutralizes the weight of the leg, facilitating reduction of
transverse fracture patterns. The hip and knee position is also
controlled to minimize iatrogenic nerve injury, particularly with clamp
placement through the greater sciatic notch.14 The position of the femoral head is controlled
and improves the repositioning of free osteochondral or impacted fragments using the head as a template.
 |
|
FIGURE 45-30 Radiographic appearance of a both-column fracture. A.
Despite disruption of all six of the radiograph landmarks, the femoral head is seen to remain congruent to the roof and anterior column fragment. The position of the head on the anteroposterior radiograph is medialized as well as superiorly displaced. Fracture of the contralateral pubic body because of the displacement of the superior pubic ramus fragment is noted. B. The obturator oblique demonstrates the spur sign (arrowhead) as well as confirming the congruence between the femoral head and acetabulum. C. The iliac oblique view reveals loss of congruence between the femoral head and the posterior column; therefore, this fracture is indicated for surgical treatment. D. The computed tomography section shows the anterior column (white arrow), the superior extent of the posterior column (white arrowhead), the spur sign of the iliac wing (black arrow), and a large posterior wall fracture (black arrowhead). (Copyright Berton R. Moed, MD.) |
The proximal branch of the incision is directed toward the posterior
superior iliac spine, ending approximately 6 cm short of this bony
landmark. Distally, the incision extends approximately 15 cm along the
midlateral aspect of the thigh. The fascia lata is sharply incised and
the gluteus maximus muscle is bluntly divided toward the posterior
superior iliac spine. The innervation of the gluteus maximus muscle
comes from the inferior gluteal nerve, which runs from posterior to
anterior in the muscle. Therefore, the splitting of this muscle should
stop as soon as the first nerve trunk is met, approximately at the
mid-point between the greater trochanter and the posterior superior
iliac spine.78
Otherwise the muscle fibers anterior to the dissection will be
deinnervated. Next, the insertion of the gluteus maximus muscle into
the femur is released. This allows posteromedial retraction of the
muscle without excessive stretch on the inferior gluteal nerve. The
sciatic nerve is then located along the posterior surface of the
quadratus femoris muscle and traced proximally to the piriformis
muscle. The short external rotators and piriformis tendon are divided
and tagged with sutures to assist with retraction. Gentle retraction of
the short external rotators allows visualization of the posterior
column and retroacetabular space but provides only limited protection
of the sciatic nerve.
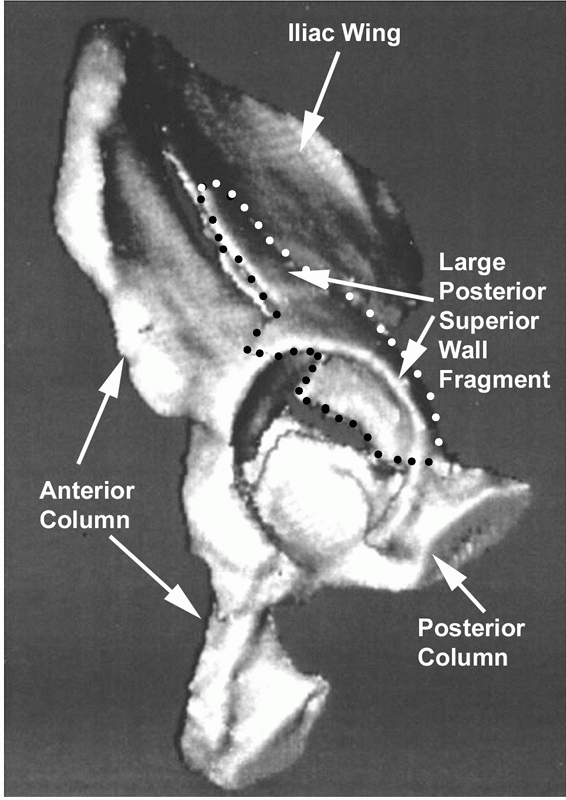 |
|
FIGURE 45-31
Three-dimensional computed tomogram in a both-column fracture showing the separate posterior wall component with the edge of the fracture line highlighted with black and white dots. (Copyright Berton R. Moed, MD.) |
approach to the hip, there are special considerations when exposing an
acetabular fracture. Transecting the piriformis and obturator internus
tendons must be performed at least 1.5 cm from the greater trochanter
to avoid injury to the ascending branch of the medial femoral
circumflex artery.55 Dissection
caudal to the inferior gemellus on the femur must be avoided, also to
preserve the blood supply to the femoral head (Fig. 45-34).
If more distal exposure of the ischium is necessary, elevation of the
quadratus femoris muscle can be performed from its ischial attachment
rather than its femoral side. Excessive superior and lateral retraction
of the abductors can place harmful tension on the superior gluteal
neurovascular bundle. If additional superior and anterior exposure is
required, to secure buttress plate fixation for a superiorly located
posterior wall fracture for instance, anterior extension of the
exposure can be accomplished without excessive traction on the
abductors or superior gluteal neurovascular pedicle by using a standard
or a flip osteotomy of the greater trochanter.16,35,131
As opposed to the situation for posterior approaches to the hip for
total hip arthroplasty, during acetabular fracture surgery the sciatic
nerve must be directly visualized and protected. Therefore, it is
important to recognize the normal potential variability in the
relationship between the sciatic nerve and the piriformis muscle.
Typically (about 84% of the time), the sciatic nerve runs deep to the
piriformis muscle, appearing in the buttock at the inferior border of
this muscle.45 Three variations of this “normal” anatomy have been reported, and others probably exist.45
The most common variation (12%) is for one part of the nerve (the
peroneal division) to pass through the muscle and the other part (the
tibial division) to appear below the muscle. The entire nerve also may
pass through the muscle (1%). These two variations result in a split
piriformis muscle with two tendons of insertion. The third variation is
passage of the peroneal division above the piriformis and the tibial
division below it (3%). With enough operative cases, one will
eventually encounter one of these anatomic anomalies (Fig. 45-35).
Knowledge of the anatomic variability of this area and the prior
identification of the sciatic nerve on the posterior surface of the
quadratus femoris muscle will prevent intraoperative confusion and
decrease the risk of iatrogenic sciatic-nerve injury.
|
TABLE 45-4 Choice of Surgical Approach for Each Fracture Pattern
|
||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||
approach does not allow access medial to the iliopectineal eminence.
Therefore, this approach is satisfactory for atypical fractures of
the anterior wall (see Fig. 45-19).
Although the ilioinguinal is usually the better choice, the iliofemoral
approach may be sufficient for high anterior column fractures in which
the main displacement is cephalad to the hip joint (see Table 45-4).
The patient is placed supine on the operating room table. The incision
extends from just posterior to the gluteus medius tubercle, paralleling
the iliac crest to the anterior superior iliac spine and then coursing
distally for approximately 15 cm along the lateral aspect of the
sartorius muscle (Fig. 45-36). The iliopsoas
muscle is elevated off the inner aspect of the iliac crest. The
sartorius origin and inguinal ligament are released from the anterior
superior iliac spine. The interval between the sartorius and the tensor
fascia lata is developed to allow exposure of the anterior hip joint
capsule, the anteroinferior iliac spine, and the anterior column as far
medial as the iliopectineal eminence. Removal of the muscles of the
outer surface of the pelvis should be undertaken only if absolutely
required and with great care to not devitalize the anterior column
fracture fragment. This approach is fairly simple and low risk.
However, access to the anterior column is quite limited. The lateral
femoral cutaneous nerve or some portion thereof is commonly injured
with this approach.
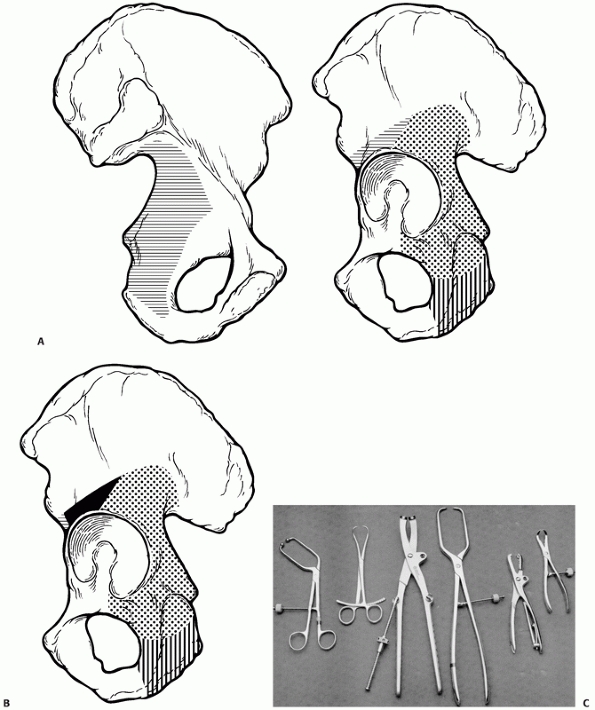 |
|
FIGURE 45-32 A. Access provided by the Kocher-Langenbeck approach. Dots delineate the available area of direct visualization. Horizontal lines delineate the area of indirect access. Vertical lines delineate the area of visualization and access extended by release of the quadratus femoris muscle. B. Access provided by extension of Kocher-Langenbeck approach or use of the modified Gibson approach. Dots delineate the available area of direct visualization. Horizontal lines delineate the area of indirect access. Vertical lines delineate the area of visualization and access extended by release of the quadratus femoris muscle origin. Solid black area shows area of extended visualization and access. C. Examples of various reduction clamps. From left to right:
oblique reduction forceps with pointed ball tips, large reduction forceps with points, Jungbluth reduction clamp, extra large pelvic reduction forceps with points, Farabeuf reduction forceps, and large serrated bone forceps. (A,B. Copyright Berton R. Moed, MD. C. From Moed BR, Karges DE: Techniques for reduction and posterior fixation of pelvic ring disruptions through the posterior approach. Clin Orthop 1996;329:107.) |
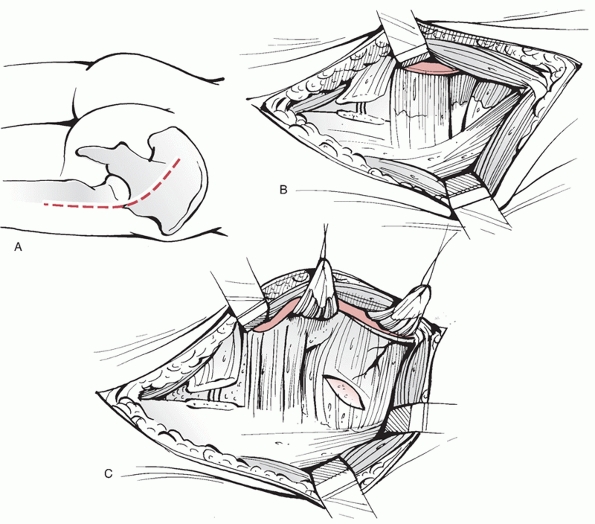 |
|
FIGURE 45-33 The Kocher-Langenbeck approach. A. The skin incision. B.
The fascia lata and gluteus maximus have been split. The short external rotators are seen with the sciatic nerve lying on the dorsal surface of the quadratus femoris. The gluteus maximus tendon has been transected. C. The retroacetabular surface is exposed by transecting the tendons of the piriformis and obturator internus and reflecting them back toward the sciatic notches. A capsulotomy is shown but is not often used clinically. |
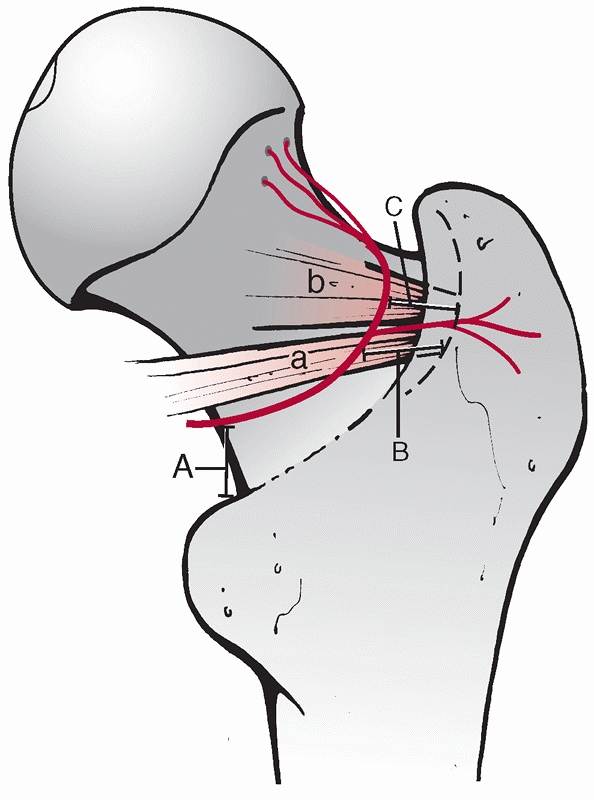 |
|
FIGURE 45-34 Diagram showing the course of the deep branch of the medial femoral circumflex artery with respect to the tendons of the (a) obturator externus and (b)
obturator internus. Shown are the distances of the deep branch of the artery to the trochanteric crest at the level of the lesser trochanter (A = 18.2 mm), insertion of the obturator externus (B = 8.8 mm), and the insertion of the obturator internus (C = 1.24 mm). (Redrawn after Helfet DL, Beck M, Gautier E, et al. Surgical techniques for acetabular fractures. In: Tile M, Helfet DL, Kellam JF, eds. Fractures of the Pelvis and Acetabulum. 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 2003:537.) |
and anterior column fractures as well as for most anterior column plus
posterior hemitransverse fractures. Transverse fractures in which the
major displacement is anterior with minimal posterior displacement and
both-column fractures having a noncomminuted posterior column fragment
can also be managed using this approach. These complex fracture types
must not have displacement in the anatomic roof and must be treated
within 15 days of injury; otherwise an alternate, more extensive, surgical approach will be required (see Table 45-4).
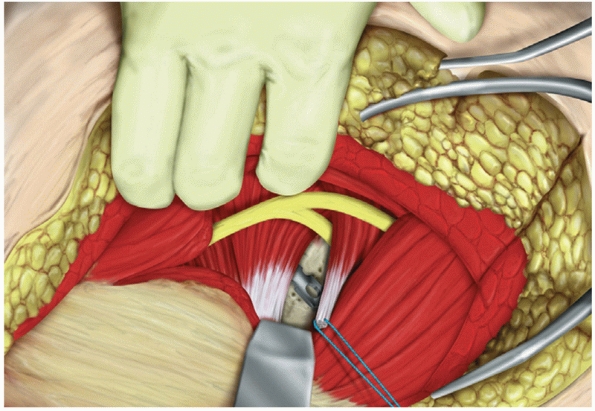 |
|
FIGURE 45-35
Drawing showing a split sciatic nerve with the peroneal division above the piriformis muscle and the tibial division below the piriformis muscle. (From Moed BR. Acetabular fractures: the Kocher-Langenbeck approach. In: Wiss DA, ed. Master Techniques in Orthopaedic Surgery: Fractures. Philadelphia: Lippincott Williams & Wilkins, 2006:699.) |
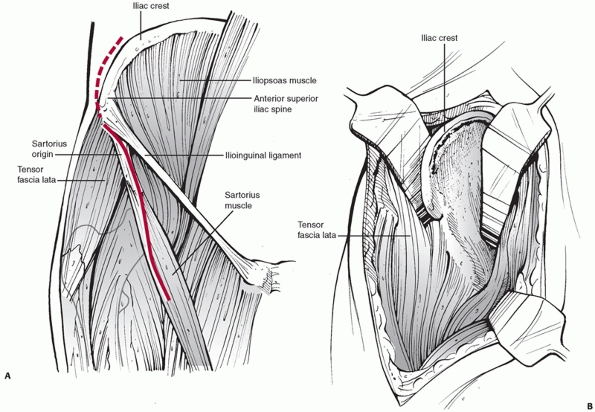 |
|
FIGURE 45-36 The iliofemoral approach. A. Skin incision. B.
Deep dissection by elevation of muscles of the inner surface of the pelvis and release of the sartorius origin and Ilioinguinal ligament. Removal of the muscles of the outer surface of the pelvis, as shown, should be undertaken only if needed and with great care to not devitalize the anterior column fracture fragment. |
aspect of the innominate bone from the sacroiliac joint to the
symphysis pubis (Fig. 45-37). Direct
visualization of the internal iliac fossa, pelvic brim, superior pubic
ramus, and a portion of the quadrilateral surface is achieved. Indirect
access to the inferior portion of the quadrilateral surface can be
attained by the palpating finger or the use of special instruments.
Limited access to the external aspect of the iliac wing is possible by
release of the abductor origin.
table. The skin incision extends from just posterior to the gluteus
medius tubercle, paralleling the iliac crest to the anterior superior
iliac spine and then coursing medially to the midline ending two
fingerbreaths above the pubic symphysis78 (Fig. 45-38).
The iliacus muscle is elevated from the internal iliac fossa. The
aponeurosis of the external oblique muscle (along with the anterior
aspect of the sheath of the rectus abdominis) is then incised from the
anterior superior iliac spine to the midline, passing at least 1 cm
superior to the superficial inguinal ring. The aponeurosis is reflected
distally revealing the spermatic cord in the male and the round
ligament in the female. This structure is
bluntly
isolated along with the ilioinguinal nerve and retracted using a rubber
sling. The now exposed inguinal ligament is split through its entire
length, revealing the laterally located lacuna musculorum contents
(lateral femoral cutaneous nerve, the iliopsoas muscle mass, and
femoral nerve) and the medially located lacuna vasorum containing the
external iliac vessels and lymphatics.78
The iliopectineal fascia, which separates these lacunae, must be
incised to allow access to the quadrilateral plate and true pelvis.
Separate rubber slings are placed around the lacuna musculorum contents
and the external iliac vessels. In this way, three surgical access
“windows” are created.
 |
|
FIGURE 45-37 Access provided by the ilioinguinal approach. Dots delineate the available area of direct visualization. Horizontal lines delineate the area of indirect access. Vertical lines
delineate the area of visualization and access extended by release of the tensor fasciae latae muscle. (Copyright Berton R. Moed, MD.) |
elevation of the iliacus muscle from the internal iliac fossa) allows
exposure of the iliac crest and the internal iliac fossa medially to
the sacroiliac joint and distally to the pelvic brim. The middle window
(created by the release of the iliopectineal fascia and retraction of
the iliopsoas and femoral nerve laterally and the external iliac artery
and vein medially) allows exposure of the anterior wall, pectineal
eminence, pelvic brim, and quadrilateral surface. Prior to retraction
of the vessels, care must be taken to look for an anomalous origin of
the obturator artery, known as the corona mortis, or other anastamoses
between the obturator and the external iliac systems44 (Fig. 45-39).
The medial window, created by lateral retraction of the vessels with
either medial or lateral retraction of the spermatic cord (or round
ligament), provides exposure to the superior pubic ramus and pubic
symphysis. The ipsilateral rectus abdominis tendon may be transected to
allow additional access to the space of Retzius (retropubic space) and
exposure to the pubic symphysis.
The lateral femoral cutaneous nerve, the femoral nerve, the external
iliac vessels, and the inguinal canal contents are all at risk for
injury. The lateral femoral cutaneous nerve must be identified and
protected throughout the procedure. While working within the middle
window, the pulse in the external iliac artery should be frequently
checked as thrombosis or intimal injury may occur with prolonged
tension on the artery.
and for surgery delayed more than 2 weeks following injury (see the
earlier section on timing of surgery). These include transverse plus
posterior wall fractures if the surgeon expects unusual difficulties
with reduction.78,83
Examples include a transtectal transverse component with an extended
posterior wall fracture (involving the posterior border of the bone), a
T-shaped plus posterior wall fracture, and those associated with
dislocation of the symphysis pubis or fracture of the contralateral
pubis ramus.78,83
Select T-shaped fractures include those with a transtectal transverse
component, those with a wide separation along the vertical stem of the
T, and those associated with dislocation of the symphysis pubis or
fracture of the contralateral pubic ramus.78,83
Select both-column fractures include those having a complex fracture of
the posterior column, a displaced fracture line crossing the sacroiliac
joint, or a wide separation of the anterior and posterior columns at
the rim of the acetabulum.83
Letournel as a surgical approach to the external aspect of the
acetabulum and innominate bone (Fig. 45-40).
The approach, derived from the Smith-Petersen approach, provides
maximum simultaneous access to both columns of the acetabulum. The
entire lateral aspect of the iliac wing, the anterior column to the
level of the iliopectineal eminence, the retroacetabular surface, and
the interior of the hip joint are accessible.
knee maintained in a flexed position to relax the sciatic nerve. An
inverted J incision is used, extending from the posterior superior
iliac spine along the iliac crest to the anterior superior iliac spine
and then continued distally to the midpoint of the thigh angling toward
a point 2 cm lateral to the lateral aspect of the patella
(Fig. 45-41).
The gluteal and tensor fascia lata muscles are elevated from the
external surface of the ilium and are hinged on the superior gluteal
neurovascular bundle. The hip abductors are released from their
insertion into the greater trochanter. Alternately, the greater
trochanter may be osteotomized. Next, the short external rotators are
released from their insertion into the greater trochanter to complete
the exposure of almost the entire external surface of the bone. Release
of the reflected head of the rectus femoris combined with a
circumferential capsulotomy at the acetabular rim provides direct
visualization of the hip joint. The exposure can be extended medially
by release of the sartorius and rectus femoris origins and elevation of
the iliacus from the internal iliac fossa. However, this additional
muscle stripping creates added risk of iliac wing and acetabular dome
devascularization and increased risk of infection.57
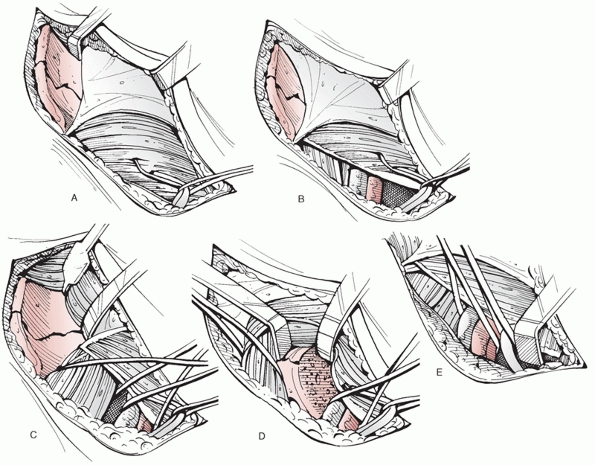 |
|
FIGURE 45-38 The ilioinguinal approach. A.
The skin incision extends from just posterior to the gluteus medius tubercle, paralleling the iliac crest to the anterior superior iliac spine and then coursing medially to the midline ending two finger-breaths above the pubic symphysis. B. The iliacus muscle has been dissected subperiosteally from the internal iliac fossa, and the external oblique aponeurosis has been incised from the anterior superior iliac spine to the midline, passing at least 1 cm superior to the superficial inguinal ring, and reflected distally. The spermatic cord in the male or the round ligament in the female is bluntly isolated along with the ilioinguinal nerve and retracted using a rubber sling. The now-exposed inguinal ligament is split through its entire length and the iliopectineal fascia is seen to be separating the femoral nerve and iliopsoas from the external iliac vessels. C. The iliopectineal fascia has been released and the exposure is complete. The lateral window exposes the internal iliac fossa to the sacroiliac joint and pelvic brim. D. The middle window exposes the pelvic brim to the pectineal eminence, the quadrilateral surface, and the anterior wall. E. The medial window is shown here with retraction of the spermatic cord laterally. The rectus abdominis tendon has been transected. The space of Retzius, superior ramus, and symphysis pubis are visualized. |
the posterior Kocher-Langenbeck approach can be combined and performed
simultaneously or sequentially.52,123
For two simultaneous approaches, the patient is positioned laterally.
Two simultaneous approaches theoretically allow access to both the
anterior and posterior columns without the morbidity of the
extended
approach. The combined access, however, does not include the exposure
of the external surface of the posterior-superior ilium that the
extended iliofemoral approach allows. In addition, the lateral patient
positioning frequently compromises both exposures. Frequently only the
lateral window of the ilioinguinal can be used. Simultaneous
iliofemoral and Kocher-Langenbeck surgical approaches performed by two
surgical teams operating concurrently has been used successfully for
both-column fractures with associated posterior wall fractures,
comminuted transverse transtectal fractures, transverse plus posterior
wall fractures with wide displacement, and T-shaped fractures.52 More commonly, sequential ilioinguinal
and Kocher-Langenbeck approaches are used for anterior plus posterior
hemitransverse, T-shaped, or associated both-column fractures when the
surgeon is able to achieve a reduction of only one column though the
first approach. In either situation, care should be taken to maximize
the skin bridge between the two approaches and avoid undermining the
subcutaneous tissues between the exposures.
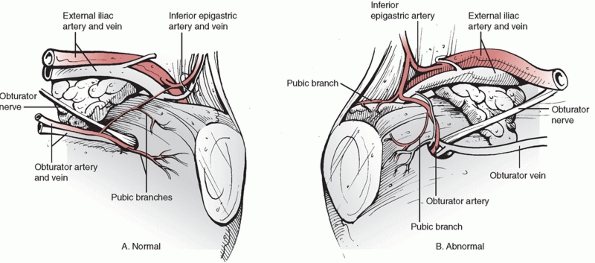 |
|
FIGURE 45-39 A. Illustration of the commonly occurring small-caliber anastamoses between the obturator and external iliac systems. B. Illustration of the true “corona mortis,” aberrant origin of the obturator artery from the external iliac system.
|
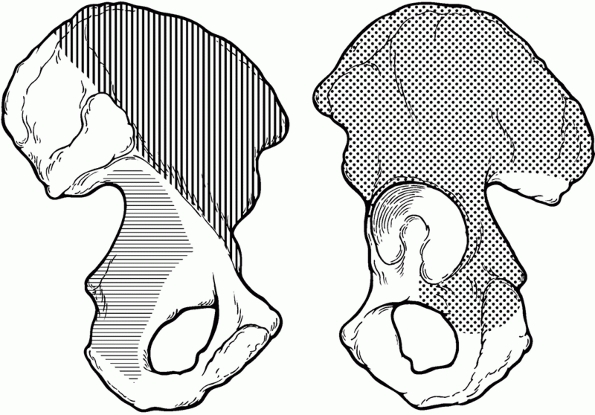 |
|
FIGURE 45-40 Access provided by the extended iliofemoral approach. Dots delineate the available area of direct visualization. Horizontal lines delineate the area of indirect access. Vertical lines
delineate the area of visualization and access extended by elevation of the iliacus from the internal iliac fossa. (Copyright Berton R. Moed, MD.) |
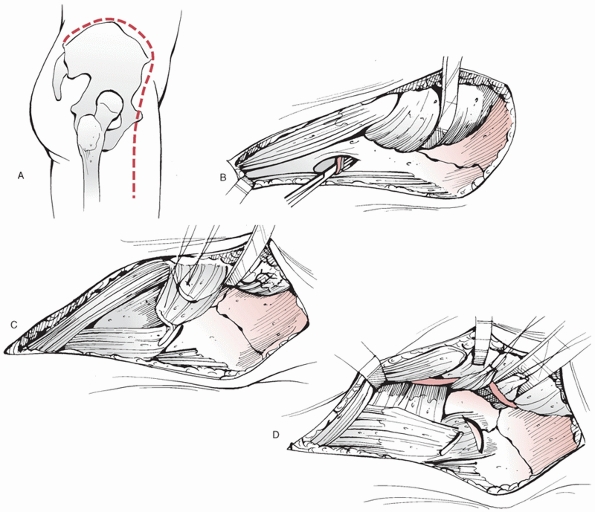 |
|
FIGURE 45-41 The extended iliofemoral approach. A.
The skin incision runs from the posterior superior iliac spine to the anterior spine and then curves to lie on the anterior-lateral thigh. B. The abductors have been reflected subperiosteally from the external ilium and reflected posteriorly with the tensor fascia lata muscle. The fascia separating the tensor from the rectus is split and the ascending branch of the lateral femoral circumflex vessels is ligated. C. The abductor tendons are here transected from the greater trochanter. Alternately a trochanteric osteotomy can be performed. D. The piriformis and obturator internus tendons have been transected and the exposure to the external ilium is completed. A capsulotomy is shown. |
osteotomy is a variation of the Kocher-Langenbeck approach that is used
to attain additional anterosuperior exposure (see Fig. 45-32B) and to facilitate intraoperative dislocation of the femoral head for inspection of the joint.35,131 Although the patient is usually in the lateral position for this approach,35 the patient also can be placed in the prone position.131
Indications potentially include combined femoral head-posterior wall
acetabular fractures, posterior wall, and column fracture types, as
well as certain transverse or T-shaped fractures.131
of the greater trochanter and exits anteriorly just medial to the
gluteus medius and minimus insertions (Fig. 45-42).
Some fibers of the gluteus minimus tendon are transected from the
anterior trochanter, but the majority of the tendon insertion remains
with the trochanteric fragment. This is also referred to as a digastric
osteotomy because both the abductor and vastus lateralis insertions
remain on the trochanteric fragment. The insertion of the piriformis
tendon remains on the intact proximal femur. This protects the blood
supply to the femoral head from the ascending branch of the medial
femoral circumflex artery. Anterior exposure is then facilitated by
retraction of the trochanteric fragment anteriorly. Cranial exposure is
still limited by the superior gluteal neurovascular bundle, and if more
cranial
exposure of the posterior iliac wing is thought to be necessary, an extended approach should be chosen primarily.
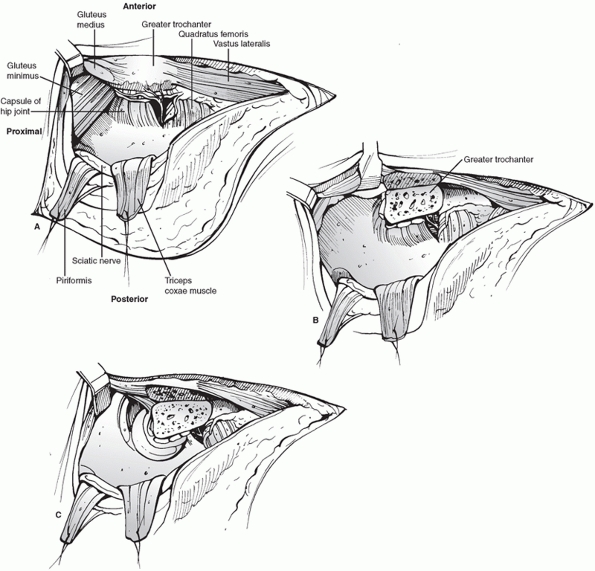 |
|
FIGURE 45-42 The trochanteric flip osteotomy using a Kocher-Langenbeck approach. A. Exposure without trochanteric osteotomy. B. Exposure of the supra-acetabular area after osteotomy with anterior retraction of the osteotomized trochanter. C.
Posterior dislocation of the femoral head, which is facilitated by the trochanteric osteotomy. (Redrawn from Siebenrock KA, Gautier E, Ziran BH, et al. Trochanteric flip osteotomy for cranial extension and muscle protection in acetabular fracture fixation using the Kocher-Langenbeck approach. J Orthop Trauma 1998;12:387-391.) |
differs from the Kocher-Langenbeck approach in its proximal dissection.
The interval between the gluteus maximus and tensor fasciae lata
muscles is developed, rather than splitting the gluteus maximus muscle.106
In this way, the neurovascular supply to the anterior portion of the
gluteus maximus muscle is not at risk. In addition, anterosuperior
visualization and access are extended (see Fig. 45-32B).
Having a straight, rather than angled, skin incision may make the
modified Gibson more cosmetically appealing, especially in obese female
patients.38 The modified Gibson approach can be combined with a trochanteric flip osteotomy.38
Stoppa intrapelvic approach has been advocated to treat a number of
fracture types, including anterior wall and column, transverse,
T-shaped, anterior column (or wall) and posterior hemitransverse, and
both-column fractures.27 Although
this approach has not gained wide acceptance, it is especially useful
for fractures requiring buttress plating of the quadrilateral plate.118
position. A transverse skin incision is made 2 cm above the pubic
symphysis extending approximately from one external inguinal ring to
the other. Deep dissection is performed through the linea alba (Fig. 45-44).
With this approach, it is often necessary to make a second approach
through a skin incision along the iliac crest for fracture reduction or
hardware insertion, essentially using the equivalent of the lateral and
medial “windows” of the ilioinguinal approach. Similar to the
ilioinguinal approach, this approach requires indirect reduction of
posterior fracture lines. The advantage over the ilioinguinal is that
dissection of the iliac vessels is not required. However, this lack of
access
to the ilioinguinal middle “window” is also its disadvantage. With this
approach, it is particularly important to locate the obturator nerve.
 |
|
FIGURE 45-43 Modified Gibson approach. A. Straight skin incision. B. Fascial incision showing underlying anatomic structures. C. Deep dissection with the gluteus maximus muscle reflected and a retractor in the lesser sciatic notch (asterisk)
showing posterior exposure similar to the Kocher-Langenbeck. Anterior retraction of the gluteus medius muscle without the presence of any overlying gluteus maximus muscle facilitates anterosuperior access. (Copyright Berton R. Moed, MD.) |
medially, across the midline, and a modified Stoppa midline approach
made through the linea alba between the rectus muscles.83,84,85,86
As noted earlier, this has the added advantage of allowing improved
visualization of the quadrilateral surface to the lesser and greater
sciatic notches. The ilioinguinal approach also can be modified to
allow extended access. Weber and Mast154
described improved access to the external aspect of the ilium by
positioning the patient in the semilateral position and extending the
skin
incision
to the posterior superior iliac spine. The posterior aspect of the
abductor origin and a portion of the gluteus maximus origin are
detached from the external aspect of the ilium. If there is a
sacroiliac fracture-dislocation component to a both-column fracture,
this may be helpful. Kloen et al.70
described a modification of the classic ilioinguinal approach to
develop the plane between the sartorius and tensor fascia lata muscle
distal to the inguinal ligament. This allows access to the anterior hip
capsule for capsulotomy and may improve visualization of small anterior
rim fracture fragments. The standard skin incision may be used but is
typically moved a few centimeters distally to facilitate this exposure.
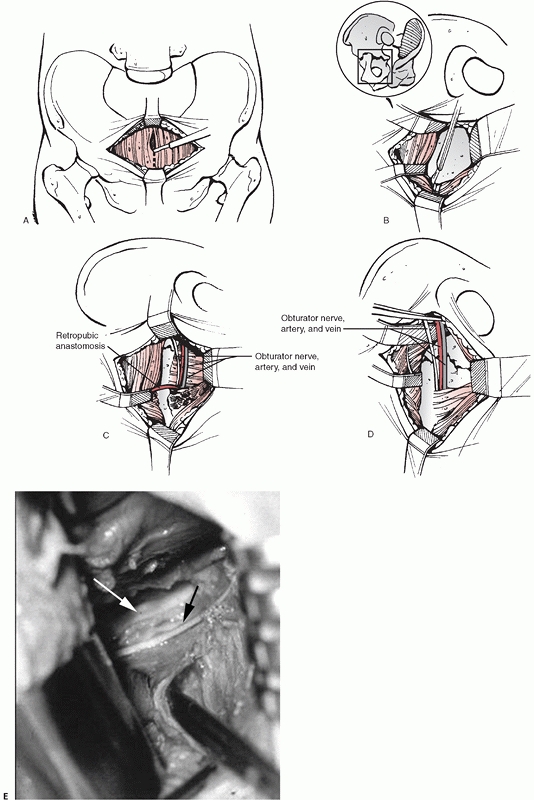 |
|
FIGURE 45-44 Modified Stoppa intrapelvic approach. A.
A transverse incision is made 2 cm above the symphysis. The linea alba is incised at the midline and split vertically from inferior to superior with care taken to remain extraperitoneal in the proximal portion. B. Protecting the bladder, the rectus abdominis muscle is then retracted upward. Sharp dissection is used to elevate the rectus to expose the symphysis body and pubic ramus. C. The rectus and neurovascular structures are subsequently retracted laterally and anteriorly so that they are protected. Any anastomotic vessels between major arteries, such as the inferior epigastric and obturator vessels, are ligated, as required. D. Full access is then developed from anterior to posterior along the pelvic brim, sharply dividing and elevating the iliopectineal fascia superiorly and the obturator fascia inferiorly and exposing the medial wall of the acetabulum, the fracture, and the pelvic brim. It is imperative to pay strict attention at all times to the location of the obturator neurovascular bundle and lumbosacral trunk which traverse the operative field. E. Cadaver dissection showing a scissors opening the obturator fascia. The obturator nerve (black arrow) is seen traversing the operative field just below the pelvic brim (white arrow). (A-D. Modified from Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop 1994;305: 1154. E. Copyright Berton R. Moed, MD.) |
are the same as for the extended iliofemoral. The exposure achieved is
also similar, perhaps increasing access to the ischial region in obese
patients and those with indurated soft tissues. The skin incision was
changed to a T shape to facilitate possible later total hip
arthroplasty.119 The abductor and
sartorius muscles are mobilized via multiple osteotomies rather than
soft-tissue release, theoretically allowing increased security of
reattachment. However, clinical advantage has yet to be demonstrated.
Furthermore, osteotomy of the iliac crest decreases the bone stock
available for implant placement, which is especially important in
both-column fracture fixation.
also has indications similar to those for the extended iliofemoral.
However, the exposure is more limited, lacking complete visualization
of the iliac crest. The skin incision is Y-shaped, with the posterior
limb being nearly identical to the Kocher-Langenbeck incision. The
anterior limb of the incision extends from the greater trochanter to
the anterior superior iliac spine. The skin incision is deepened
through the fascia. Posteriorly, the approach is the same as the
Kocher-Langenbeck. A trochanteric osteotomy is performed to release the
abductor insertion, and the glutei and tensor muscles are elevated from
the external surface of the ilium. The triradiate approach can be
performed when the surgeon cannot address the fracture through an
initial Kocher-Langenbeck approach. Some view this extension of the
Kocher-Langenbeck to a triradiate as a desirable safety net. Others see
it as the result of poor preoperative planning, inappropriate lateral
patient positioning, and surgical inexperience. Whatever the case,
clinical advantage of the triradiate approach has not been demonstrated.3
fractures not involving the superior acetabular dome can be considered
for nonoperative management.54,86,115,122,147
This group of fractures includes nondisplaced and minimally displaced
fractures, fractures in which the intact part of the acetabulum is
large enough to maintain stability and congruity, and those with
secondary congruence (Table 45-5). Nonoperative
management may also be selected for patients with severe osteopenia or
severe underlying medical problems that preclude surgical intervention.
This is a relatively small group, consisting mainly of elderly patients.
|
TABLE 45-5 Acetabular Fractures Amenable to Nonoperative Treatment
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||
first recognized the condition of the superior dome of the acetabulum
to be a significant prognostic indicator of clinical outcome. The
superior dome of the acetabulum is described as the superior third of
the weight-bearing area of the acetabulum and has been further
quantified by other investigators. Olson and Matta115
demonstrated that axial CT sections of the superior 10 mm of the
acetabular articular surface are equivalent to the weight-bearing dome
region and can also be useful in determining if acetabular fracture
lines involve this region. Although controversy exists regarding the
exact amount of displacement that is considered acceptable when the
superior dome of the acetabulum is involved, most authors recommend
surgical intervention if displacement exceeds 2 mm.54,78,83,115
developed roof arc measurements to determine whether an acetabular
fracture has violated the weight-bearing dome. This measurement has
been used to determine if the remaining intact acetabulum is sufficient
to maintain a stable and congruous relationship with the femoral head.
In this way, operative verses nonoperative treatment can be selected.
The roof arc is measured on all three radiograph views with the leg out
of traction. The medial roof arc is measured on the AP view. The
anterior roof arc is measured on the obturator oblique, and the
posterior roof arc is measured on the iliac oblique. To obtain these
measurements, the first line is a vertical line through the center of
the femoral head and the second line is drawn from the center of the
femoral head to the fracture location at the articular surface (Fig. 45-45).
Roof arc measurements are not applicable to both-column fractures or
those with a fracture of the posterior wall. The previous
recommendations were that roof arc measurements greater than 45 degrees
on the AP (medial roof arc), iliac oblique (posterior roof arc), and
obturator oblique radiographs (anterior roof arc) indicate preservation
of the weight-bearing dome, and these patients should be considered for
nonoperative management.87,115 More recently, however, biomechanical study151
has produced different criteria; fractures with a medial roof arc angle
of greater than 45 degrees, an anterior roof arc angle of greater than
25 degrees, and a posterior roof arc angle of greater than 70 degrees
have sufficient intact acetabulum for nonoperative treatment (see Fig. 45-45). Therefore, displaced low anterior column, low transverse, and low T-shaped acetabular fractures are amenable to nonoperative
treatment, if, as expected, the fracture position is stable and the joint remains congruent54,78,115,122 (see Table 45-5).
 |
|
FIGURE 45-45 A. Anteroposterior (AP), B. obturator oblique, and C.
iliac oblique radiographs of a transverse fracture of the acetabulum showing roof arcs of approximately 50 degrees each, indicative of a stable hip joint by the initial recommendations (greater than 45 degrees on each view).87 D. AP radiograph of the patient obtained 3 weeks later showing gross medial subluxation of the hip, which would have been expected using the updated criteria for stability of Vrahas et al. 1999 (greater than 45 degrees on AP, greater than 25 degrees on obturator oblique, greater than 70 degrees on iliac oblique). (Copyright Berton R. Moed, MD.) |
fractures because there is no intact portion of the acetabulum to
measure. Instead, displaced both-column fractures of the acetabulum may
be considered for nonoperative management in the presence of secondary
congruence (Fig. 45-46), defined as congruency
between the femoral head and the displaced acetabular articular
fragments without skeletal traction being applied.78
Parallelism between the femoral head and acetabular articular surface
must be maintained in all three radiographic views, especially in a
young patient. However, secondary congruence is a necessary, but not a
sufficient, criterion for nonsurgical treatment. In addition, articular
fragment displacement and medial joint displacement should not be so
excessive as to limit motion and limb shortening must be acceptable. It
must be recognized that fractures with secondary congruence do not have
as good a prognosis as those reduced in anatomic position.78,83
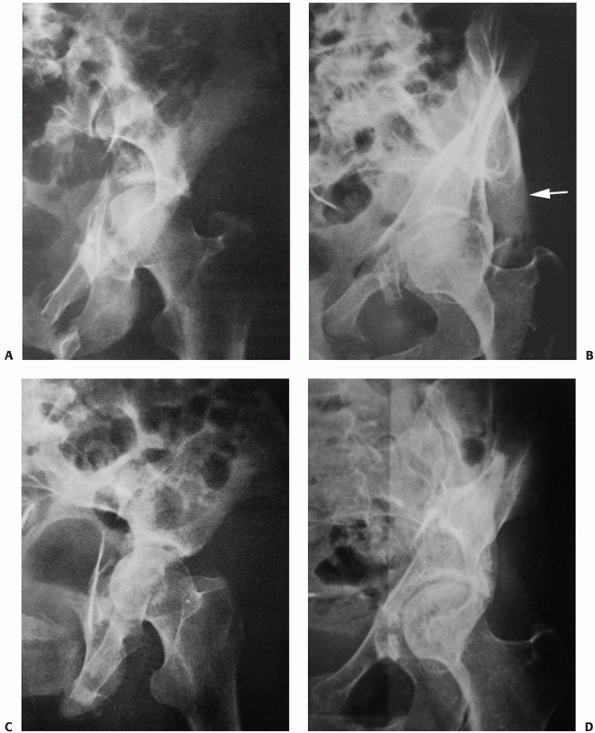 |
|
FIGURE 45-46 Both-column fracture showing secondary congruence. A. Anteroposterior, B. obturator oblique, with white arrow showing the spur sign, and C. iliac oblique radiographs at time of injury. D.
Obturator oblique radiograph 14 years later in a patient with an excellent clinical result. (From Tile M, Helfet DL, Kellam JF. Fractures of the pelvis and acetabulum. Philadelphia: Lippincott Williams & Wilkins, 2003:507-508.) |
fractures of the posterior wall. Fractures involving the acetabular
walls should be treated nonoperatively only if the hip joint remains
completely stable. When in doubt, it is safest to assume that all of
these fractures are unstable until proved otherwise. Therefore,
clinical evaluation of stability is mandatory if nonoperative treatment
is being considered. As noted previously, this examination is best
performed using fluoroscopic visualization of the hip joint with the
patient under general anesthesia.97,148 Frank
redislocation is neither required nor clinically desirable. An
acetabular wall fracture presenting in the absence of known hip
dislocation is no guarantee of hip stability.97
displaced acetabular fractures should be considered for nonoperative
management. However, there have been advocates for percutaneous
fracture fixation in this group of patients.29,67,138
The concern centers on the questionable stability of these fractures
with the contention that a certain percentage will displace. Therefore,
early percutaneous fixation would avoid a subsequent more extensive
open procedure or prevent the disaster of early traumatic arthrosis in
those (for whatever reason) not having the benefit of further
treatment. However, only a very small number (less than 7%) of these
nondisplaced and minimally displaced fractures are potentially unstable
and will significantly displace without traction.148
Rather than unnecessarily operating on a large number of fractures to
prevent problems in these few or subject all of these patients to
prolonged bedrest in traction, it makes more sense to try to identify
those at risk for fracture displacement. Dynamic fluoroscopic stress
examination with the patient under general anesthesia, as noted
earlier, is one proposed method of identifying these fractures at risk.148
However, the exact technique for performing this examination is ill
defined for fractures other than the posterior wall. Another method is
to closely observe all patients presenting with nonoperative parameters
via weekly radiographic follow-up, being prepared to shift immediately
to operative management (percutaneous or otherwise) should joint
instability or incongruency be detected.
fractures include both intact roof arc measurements and congruence of
the femoral head to the intact acetabulum on AP and Judet radiographs
taken out of traction. Patient-related factors such as age, preinjury
activity level, functional demands, and medical comorbidities also must
be considered when determining whether a patient is best served by
surgical or nonsurgical treatment. Nonsurgical treatment of elderly or
infirm patients, with planned subsequent arthroplasty if symptomatic
arthritis develops, may be appropriate—particularly if the fracture
displacement is minimal.61,130,133
for nonoperative management, treatment mainly consists of bedrest with
joint mobilization and eventual progression to full weight-bearing
activity. Bed rest is necessary in the acute injury phase only for
symptomatic relief. Mobilization of the patient and the hip joint
should follow as soon as symptoms allow. Patients should begin with
touch-down partial weight bearing of the affected extremity (less than
10 kg). AP and oblique radiographs should be obtained at frequent
intervals (weekly for the first 4 weeks) to confirm maintenance of
satisfactory position. When there is adequate fracture healing, usually
by 6 to 12 weeks, the patient should gradually progress to full weight
bearing. Joint mobilization should be continued throughout the
rehabilitation period. The use of formal physiotherapy or continuous
passive motion modalities should be tailored to the individual.
those patients with operative indications related to fracture
displacement but having medical contraindications. In these cases,
traction should be maintained until fracture healing is sufficient to
allow progressive weight-bearing ambulation and may range from 4 to 12
weeks.144,147
be treated nonoperatively with good results. In the study by Rowe and
Lowell in 1961,122 the 49 patients
with nondisplaced linear fractures or displaced medial wall fractures
not involving the superior dome were treated without surgery. At an
average of 6 years follow-up, all patients with linear nondisplaced
fractures and 26 of 28 patients with medial wall fractures demonstrated
good or excellent clinical results. However, fractures of the superior
acetabular dome or posterior acetabulum yielded variable results.
Nondisplaced superior dome fractures treated by closed means yielded
75% good or excellent clinical results, while displaced fractures
yielded 75% poor clinical results. Sixty-seven percent of posterior
acetabular fractures treated nonoperatively had a poor clinical
outcome. Delayed reduction of the hip dislocation, injury to the
femoral head, and continued instability were all factors contributing
to a poor outcome in patients with posterior acetabular fractures.
reported 83% good or excellent results in cases in which congruency
could be obtained and maintained by closed means, with an average
follow-up of 10 years. However, considerably worse results were
observed in patients with unsatisfactorily reduced fractures involving
the weight-bearing dome. Tornetta148
also demonstrated that satisfactory results could be achieved with
nonoperative management provided joint congruence and stability are
maintained. Thirty-eight patients with stable and congruent fractures
as documented by dynamic fluoroscopic stress views were treated
nonoperatively and followed for an average of 2.7 years. The results
were good or excellent in 35, and the three fair results were
attributable to other, associated injuries.
fractures that result in hip joint instability and/or incongruity,
regardless of the classification type. This statement applies to
displaced fractures as well as to those with occult findings. Posterior
and anterior wall fractures with instability of the hip joint require
operative fixation, as do injuries with fragments of bone or soft
tissue incarcerated within the hip joint resulting in joint incongruity
(Fig. 45-47). Open reduction and removal of the
loose body or obstructive tissue is indicated to prevent early onset of
traumatic arthrosis. Internal fixation should be performed in this
setting as dictated by hip joint stability parameters. Recurrent
dislocation (with attendant disastrous consequences for the hip joint)
is inevitable if stability is not restored.31 As has been previously described, two-dimensional CT as a means to determine hip joint stability has proved to be unreliable.97
Therefore, it is safest to assume that all of these fractures are
unstable unless proved otherwise by dynamic stress examination. There
is no need to stress an obviously unstable hip.
in joint incongruity and constitutes one of the main indications for
open reduction and internal fixation. As described earlier, plain
radiography and CT can be effectively used to determine whether an
acetabular fracture violates the weight-bearing
dome.87,115,151 A both-column fracture may exhibit significant displacement but with secondary congruence may not require operative treatment (Fig. 45-46).
However, loss of parallelism between the femoral head and acetabular
articular surface noted on any of the three radiographic views is an
indication for operative management (see Fig. 45-30).
 |
|
FIGURE 45-47 Initial (A) and postreduction (B) anteroposterior radiographs of the right hip in a 34-year-old man. The postreduction view (B) demonstrates an incongruent hip joint with a probable intra-articular osteochondral fragment (arrow). (Copyright Berton R. Moed, MD.)
|
acetabular fractures are varied in the literature and difficult to
interpret. However, the three largest series reporting outcomes after
acetabular fractures treated within 3 weeks of injury all reported good
or excellent results in 75% to 81% of fractures at long-term follow-up.78,83,90
The instrument used in the assessment of acetabular fracture outcome
has been a clinical measure, the modified rating scale of Merle
d’Aubigné and Postel.78,83,98,99
This scale rates pain, walking, and range of motion each on a 6-point
scale. A score of 18 is excellent; 17 is very good; 16 and 15 are good;
14 and 13 are fair; and less than 13 is poor (Table 45-6).
The scores are usually dichotomized into good-to-excellent (15 to 18)
and fair-to-poor (14 or less) groups for reporting purposes.
obtain an anatomic reduction of the articular surface, and clinical
outcome strongly correlates with the adequacy of fracture reduction.78,83
In Letournel and Judet’s series of 492 acetabular fractures treated
operatively, anatomic reduction was achieved in 366 patients (74%).
Eighty-one percent of patients demonstrated a good, very good, or
excellent result using their modification of the d’Aubigné-Postel hip
score.78 In contradistinction,
approximately 64% (81 of 126) of patients with an imperfect reduction
achieved a good to excellent clinical result. Posttraumatic arthritis
was observed in 10% of cases where anatomic reduction was achieved and
36% of cases where reduction was imperfect.78 Even when posttraumatic arthritis was seen after a perfect articular reduction, Letournel and Judet78
found that 50% of the time, the arthritis presented between 10 and 25
years after injury. In contrast, after imperfect reduction, 80% of the
cases of arthritis appeared within the first 10 years after injury.78
demonstrated the importance of achieving an anatomic reduction (defined
as up to 1 mm of residual displacement) as the main outcome determinant
for acetabular fracture surgery. Two hundred sixty-two patients with
displaced acetabular fractures treated operatively were evaluated at
average follow-up of 10.9 years. Interestingly, he obtained results
that were essentially identical to those of Letournel and Judet.
Eighty-one percent (150 of 185) of patients with anatomic reduction
achieved a good or excellent clinical result, whereas only 64% (49 of
77) of patients with nonanatomic reduction achieved a good or excellent
clinical result.78 An important
difference between those with an anatomic reduction versus those with
an imperfect reduction (defined as 2 to 3 mm of residual displacement
and previously called “satisfactory”) was demonstrated. To maximize the
patient’s quality of life following injury, the surgeon must strive for
an inframillimetric reduction with every fracture.
decrease with increased fracture complexity, patient age, and time
delay to fracture fixation.83 Time delay to fracture fixation dramatically affects results. In Letournel and Judet’s78
series of 138 patients treated after a 3-week delay, the rate of good
to excellent results dropped to 54%. Similarly, Johnson et al.63 reported 65% good to excellent results in 187 patients. In a series of 237 patients, Madhu et al.80 found that an anatomic reduction was
more likely if surgery was performed within 15 days for elementary
fracture types and 5 days for associated fracture types. A
good-to-excellent clinical outcome was more likely when surgery was
performed within 15 days for elementary fracture types and within 10
days for associated fracture types.80
|
TABLE 45-6 The Modified Merle d’Aubigné and Postel Clinical Grading System*
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Both-column fractures are complex injuries and technically demanding.
However, they have a generally better outcome than many fracture types,
despite a higher rate of nonanatomic reduction. Matta83
obtained anatomic reduction in only 57% of cases, yet still achieved a
good-to-excellent result in 77%. Posterior wall fractures present as a
straightforward treatment problem with excellent anatomic reduction
rates reported as high as 100%.83 However, despite the anatomic reduction obtained in all 22 treated fractures, a 32% clinical failure rate was reported.83 This was higher than for any other fracture type in the series. Similar findings have been reported by Aho et al.1 and Chiu et al.26 However, others have reported clinical results (more than 80% good to excellent) similar to other acetabular fracture types.41,78,99 It was suggested by Letournel and Judet78 and later shown by Moed et al.98
that the disparity between clinical results and apparent anatomic
reduction, as determined by plain radiography, is due, in large part,
to the inadequacy of radiographs in assessing the quality of the
postoperative posterior wall reduction. In this series of Moed et al.,98
fracture reductions were graded as perfect in 65 and imperfect in 2
(97%), as determined with use of plain radiography. However,
postoperative CT revealed the articular surface reduction to be perfect
in only 15 (22%). Postoperative CT, therefore, appears to be a more
accurate means of documenting the articular reduction after posterior
wall fracture.13,98
has been proposed to prevent potential further fracture displacement
and for elderly patients with displaced acetabular fractures in whom a
less than anatomic reduction could be accepted, as well as for simple
fractures with minimal displacements, and for the morbidly obese.40,46,66,116,126,138 Percutaneous fixation has also been proposed as an adjunct to standard open reduction and internal fixation techniques.130,138
In addition, it has been offered as an option in conjunction with
limited open surgery for displaced fractures in the elderly as a
staging procedure for total hip arthroplasty and in young patients with
severe injuries that prevent formal open reduction and internal
fixation of the fracture.29,126,137
The potential benefits of percutaneous surgery are self-evident.
However, the indications for the use of this technique are yet to be
determined.126
data demonstrating clinical outcome in these patients. In addition,
there are no data comparing percutaneous methods to standard open
reduction and internal fixation in a similar group of patients. Most
series have a very small number of patients with little or no follow-up.18,40,66,116 In the largest series, Starr et al.137
reported on 24 patients. Thirteen elderly patients with displaced
fractures had medical problems and anatomic fracture reduction was not
thought to be a necessity. There were also 11 young patients with
minimally displaced elementary fracture patterns. Closed or limited
open reduction was thought to be successful in 23 patients. In one
obese young patient, the percutaneous surgery was aborted and an open
procedure was performed. Postoperatively, average residual articular
displacement as measured on plain radiographs was 3 mm in the 13
elderly patients and 1 mm in the 10 young patients. After an average of
1 year of follow-up, 5 of the 11 elderly patients available for
follow-up had already undergone total hip arthroplasty and there were
incomplete data reported for the 10 young patients.137
In a follow-up from this center, the investigators reviewed their first
18 patients over the age of 60 years with displaced acetabular
fractures treated with closed or limited open reduction and
percutaneous screw fixation.126 All
18 fractures were reduced to within 5 mm with minimally invasive
techniques, and stabilized percutaneously and followed for a mean of 27
months. Four patients experienced early loss of reduction. Of these
four, two had total hip arthroplasty within 1 year and one died of
unrelated causes. Three additional patients died and two of the
remaining 11 patients progressed to total hip arthroplasty. Based
on
these results, without any comparison to other standard operative or
nonoperative treatments, it is difficult to provide any recommendations
regarding this technique.
|
TABLE 45-7 Clinical Results of Operative Management of Acetabular Fractures
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
specific fracture pattern, the amount of fracture displacement, and the
relative stability and congruency of the hip joint. The initial AP
radiograph of the pelvis provides substantial diagnostic information in
this regard and may reveal the need for emergency treatment (Table 45-8; see Fig. 45-6A).
This radiograph is supplemented as soon as possible after reduction of
any associated dislocation by oblique plain films and CT to define the
injury completely. After careful physical examination and pertinent
radiographic examination, the appropriate treatment approach is
determined.
and requires prompt reduction as the rate of osteonecrosis increases
significantly if reduction is not performed within 12 hours of the
injury.1,99,109
With adequate sedation and pain medication, the reduction maneuver can
often be performed in the emergency department setting. Subsequent
failed closed reduction, pre-existing contraindications to conscious
sedation, or physician preference constitutes an indication for closed
reduction using general anesthesia. Immediately following reduction,
confirmatory radiographs are obtained. There is no need to stress an
obviously unstable hip and redislocation may be injurious. Only when
the fracture pattern suggests that the hip joint should be stable or
stability is equivocal (such as with a small posterior wall fracture)
should the hip be taken through a full range of motion to evaluate
postreduction stability. As a diagnostic procedure, this examination is
best performed using fluoroscopic visualization of the hip joint with
the patient under general anesthesia.97,99,109
|
TABLE 45-8 Indications for Emergency Acetabular Fracture Fixation
|
||||||
|---|---|---|---|---|---|---|
|
skeletal traction. However, there are notable situations in which
skeletal traction (preferably using a distal femoral, rather than a
proximal tibial, traction pin) is either mandatory or desirable.
Unstable fracture-dislocations require skeletal traction following
reduction to prevent recurrent dislocation. When hip stability is in
doubt, it is also prudent to use traction, pending further evaluation.
Preoperative skeletal traction is also important to prevent further
femoral head articular surface damage from abrasion by the raw
acetabular bony fracture surfaces and may occasionally improve fracture
position (Fig. 45-48). A reasonable initial
traction amount is 15% of body weight, followed by radiographdirected
weight adjustments to attain the desired distraction
of
the femoral head. Skin traction is ineffective and should not be used.
Skeletal traction using a trochanteric pin is contraindicated because
of its associated high infection risk and ineffectiveness in fracture
reduction.147
In general, fractures with minimal or no displacement, both-column
fractures in which the hip joint remains congruent and in acceptable
position (secondary congruence), and other displaced fractures not
meeting operative criteria initially require only bedrest with
symptomatic treatment. However, these patients, as well as those with
fractures meeting operative criteria who do not require skeletal
traction for fracture management, may benefit from skeletal traction
for pain relief.
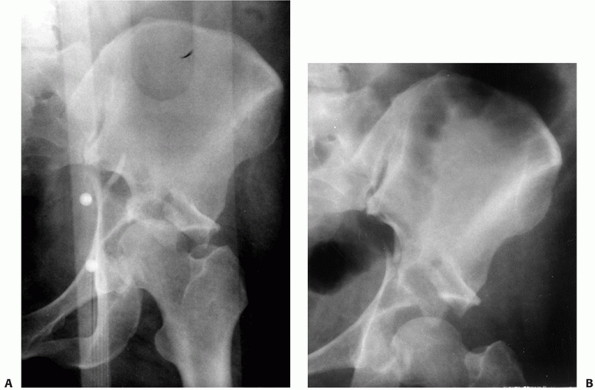 |
|
FIGURE 45-48 Anteroposterior hip radiographs before and after the application of traction. A.
Without traction, the femoral head is medially subluxed, rubbing against the sharp corner of the superior acetabular fracture surface in this displaced transtectal fracture. B. The hip joint is distracted with the application of traction pulling the articular cartilage of the femoral head a safe distance away from the acetabular fracture surface. |
required to successfully treat an acetabular fracture. To accomplish
this, the imaging studies must be systematically scrutinized. First,
the lines on the AP radiograph (see Fig. 45-49A)
should be carefully analyzed in turn. Is the iliopectineal line
disrupted? If so, the fracture possibilities include the anterior wall,
anterior column, transverse types, T-shaped, anterior column with
posterior hemitransverse, and both-column. If the ilioischial line is
disrupted, possibilities include the posterior column types, transverse
types, T-shaped, anterior column with posterior hemitransverse, and
both-column. With both lines disrupted, the possibilities are reduced
to transverse types, T-shaped, anterior column with posterior
hemitransverse, and both-column. Is the line along the posterior rim
disrupted? If so, this will add the possibility of a posterior wall
fracture. Is the ilioishial line displaced from its normal relationship
to the teardrop? If so, this would indicate, in general, that the two
columns are separated from each other.
This view will refine the diagnosis made from the AP view. A suspected
posterior wall component will become obvious, as well as disruption
involving the anterior wall or column. Is the obturator ring fractured?
If so, this, again, would suggest that the two columns are separated
from each other. The
presence of a spur sign (see Fig. 45-30) is pathognomonic for a both-column fracture. The iliac oblique is viewed next (see Fig. 45-9B).
Injury to the posterior column is further defined, as well as the
presence and location of fractures involving the iliac wing (e.g.,
anterior column, anterior column plus posterior hemitransverse, and
both-column fractures).
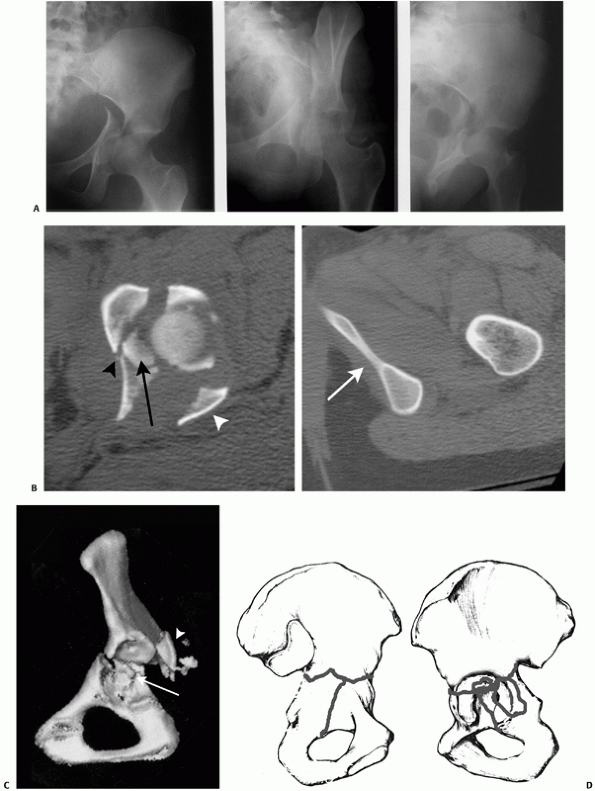 |
|
FIGURE 45-49 A.
Anteroposterior and oblique radiographs show a juxtatectal transverse acetabular fracture with an associated posterior wall fracture. B. Selected axial computed tomography sections show an intra-articular free fragment (black arrow), the posterior wall fracture (white arrowhead), and an additional vertical fracture line through the quadrilateral plate (black arrowhead), which does not propagate through the obturator ring (white arrow shows intact ring). C. Three-dimensional computed tomography scan shows the main transverse fracture line, posterior wall fragments (white arrowhead), and intra-articular free fragment (white arrow). However, the vertical (incomplete “T” component) is not apparent. D. Drawing of the fracture as part of preoperative planning. (A. From Moed BR. Acetabular fractures: the Kocher-Langenbeck approach. In: Wiss DA, ed. Master Techniques in Orthopaedic Surgery: Fractures. Philadelphia: Lippincott Williams & Wilkins, 2006: 688. B-D. Copyright Berton R. Moed, MD.) |
information described previously. After this analysis, the plain films
should be revisited to refine the diagnosis for fracture subtypes
(e.g., the level of transverse fracture or the path of the stem of the
T-shaped fracture). If the diagnosis continues to be unclear, the
three-dimensional CT scan can prove helpful. However, as noted earlier,
the three-dimensional CT scan has its limitations.
fracture is not an emergency. A delay of 3 to 5 days is commonly used
to allow for evaluation of any underlying medical problems or
associated injuries and for preoperative planning. Much of the
intraoperative maneuvering for acetabular fracture reduction is
performed indirectly, without direct exposure or complete visualization
of the fracture fragments. These techniques rely on the presence of
relatively mobile fracture fragments. Ten days following injury, early
fracture healing begins to limit this type of fracture mobilization.
Two weeks following injury, healing has often progressed to the point
that this fracture mobility has been lost and a more extensive surgical
approach is required for certain fracture types, such as the
transverse, T-shaped, anterior column with posterior hemitransverse,
and both-column patterns.78 After 3 weeks, callus formation is extensive to the point that the fracture is no longer considered to be an acute injury.78 Previous data has indicated that delay in surgical treatment beyond 3 weeks is associated with compromised outcome.31,63,78
More recently, it has been shown that a good-to-excellent clinical
outcome is more likely when surgery was performed within 10 to 15 days.80
This compromised outcome is probably related to many factors beyond the
more extensive surgical exposure with its attendant higher complication
rate, such as acetabular cartilage damage and femoral head erosion.31,63
In any case, the time to surgery has been shown to be a significant
predictor of radiologic and clinical outcome and, if possible, should
not be delayed beyond 15 days for elementary fractures and 10 days for
associated types.80 Indications for emergency operative treatment are uncommon (see Table 45-8).
Situations that demand emergency surgery include persistent instability
following reduction that cannot be controlled by traction and
irreducible hip dislocations. Progressive sciatic nerve deficit
following closed reduction of a dislocated hip is also an indication
for emergency surgery despite the fact that the return of nerve
function is variable.92,95,147
should allow the surgeon to classify the fracture type and to achieve a
precise understanding of the “personality” of the fracture.147
The three-dimensional CT reconstruction may obscure some fracture
lines. However, this study can be very helpful in visualizing the
fracture pattern in the mind’s eye. Drawing the fracture on paper or on
a whole bone specimen is also very instructive (see Fig. 45-49). In this way, the appropriate surgical approach (see Table 45-4),
reduction technique, and hardware configuration can be planned with
confidence that the required anatomic reduction and stable fixation
will be accomplished.
An oscillating drill is helpful for placing screws deep within the
wound. The implants of choice are 3.5-mm reconstruction-type plates,
either curved or straight, that can be contoured intraoperatively to
match the complex three-dimensional shape of the innominate bone.
Cortical screws of 3.5- and 4.5-mm diameter should be available in
lengths at least up to 100 mm. Longer or smaller diameter (2.7- or
2.0-mm) screws may be required, depending on the fracture configuration
or comminution.
position for acetabular fracture surgery is dictated by the fracture
type, the particular characteristics of the individual fracture, and
the selected surgical approach. However, the full extent of the four
standard surgical approaches can only be realized by using specific
patient positioning: prone for the Kocher-Langenbeck, supine for the
iliofemoral and ilioinguinal, and lateral for the extended iliofemoral.
Intraoperative traction is very important in obtaining fracture
reduction. Therefore, purpose-specific traction tables, such as a
Judet-type fracture table (Tasserit, Gron, France; PROfx Orthopedic
Surgical Table, OSI, Union City, CA) or the Jackson table (OSI), is
preferred.78,83,94 The operating table should be radiolucent (Fig. 45-50).
Although the Tasserit table is no longer available in North America as
a new item, refurbished models are still available (Medrecon, Inc.,
Garwood, NJ). In any case, if one of these purpose-specific traction
tables is not available, an AO/ASIF femoral distractor, or manual
traction delivered through a Schanz pin placed in the greater
trochanter, can be used to provide the intraoperative traction in
combination with a standard radiolucent operating room table.
High-quality intraoperative C-arm fluoroscopy can then be used to
assess fracture reduction and hardware location, allowing the surgeon
to check the extra-articular location of fixation close to the
articular surface as well as to check portions of the articular
reduction that are not directly visualized.95,114
determinant for clinical outcome, and for an excellent result the
fracture must be reduced to within 1 mm and then held there until
healing.78,83
Therefore, fracture reduction is critical. Unfortunately, fracture
reduction is the most difficult aspect of acetabular surgery, even with
excellent surgical exposure. Reduction is facilitated by many tactics,
including traction and special clamps (see Fig. 45-32C).
Traction is important in that it not only unloads the hip joint to
allow better joint visualization and facilitate direct manipulation of
the displaced fracture fragments but also can be used to effect at
least a partial reduction of the displaced columns. Traction
may
often need to be steady and prolonged. For these reasons, as noted
earlier, traction through a table is preferred to manual methods.
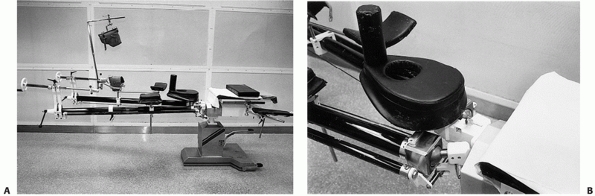 |
|
FIGURE 45-50 A. The Judet fracture table made by Tasserit. B.
A detailed view shows the padded perineal post and the padded support with perineal cutout for male patients. The separation between the chest and padded perineal support serves to reduce abdominal pressure without requiring additional padding or chest rolls. (From Moed BR. Acetabular fractures: the Kocher-Langenbeck approach. In: Wiss DA, ed. Master Techniques in Orthopaedic Surgery: Fractures. Philadelphia: Lippincott Williams & Wilkins, 2006:692.) |
standard fracture reduction sequence is to first reduce and stabilize
the displaced columns, if present, and then reduce any wall fracture
that may be present. After definitive fixation of the reduced
fragments, the entire construct is stabilized with buttress plates. For
the both-column fracture (which may have a posterior superior wall
fracture component; Figs. 45-30 and 45-31),
the sequence is to first reduce and stabilize one of the columns to the
axial skeleton (iliac wing), then the other column, and then, if
present, the wall component. After definitive fixation of the reduced
fragments, the entire construct is stabilized with buttress plates.
Although columns may be stabilized in young, healthy bone using screws
alone, osteopenic bone and all wall fractures require buttress plating.
posterior wall, the surgeon must be cognizant of the capsular blood
supply to the articular fragments. Limiting periosteal elevation to the
fracture site helps to avoid further devascularization and under no
circumstances should any fragment be released from its capsular
attachment. Rotating the fragments on their capsulolabral attachments
still allows visualization of the fragments, the articular surface, and
the joint itself. The femoral head is distracted and free osteochondral
fragments are removed from the joint. The position and orientation
should be noted as it may help the surgeon in figuring out where to
replace each fragment. The ligamentum teres is débrided from the
cotyloid fossa and the joint is thoroughly irrigated to ensure that all
debris has been removed. The rationale behind débriding the ligamentum
is that the tissue, once torn by the dislocation, may be interposed
between the femoral head and the intact acetabulum. If this causes the
femoral head to sit incongruently in the joint during reduction of the
posterior wall fragments, the joint may be reconstructed incorrectly.
that the hip be subluxated temporarily. The fracture table is very
helpful in this regard. If a fragment of the posterior wall is
incarcerated within the joint, the capsular attachments should not be
sacrificed to retrieve the fragment. The capsular hinge is usually at
the anterior aspect of the wall fragment, which may be difficult to
access though a Kocher-Langenbeck approach. Instead, a modified Gibson
or possibly a trochanteric flip will be needed to retrieve the fragment
with its blood supply intact. Both of these situations should be
anticipated from the preoperative planning. A lateral patient position
may be required.
acetabular cartilage. This allows the femoral head to be used as a
template for the reduction of free articular fragments and marginal
impaction. Impacted fragments should be mobilized with underlying
cancellous bone, reduced against the head, and held provisionally in
place while any remaining underlying bony defect is filled with
structural graft. Bone graft is most often easily obtained from a
window in the greater trochanter. However, freeze-dried cancellous
allograft bone is preferred (Fig. 45-51). Once
these fragments are reduced, it is difficult to hold them in their
positions while reducing the overlying main wall fragment(s). It is
useful to provisionally fix the articular fragments with 1.6-mm K-wires
and to exchange these for subchondral mini screws or bioabsorbable pegs
(Fig. 45-52). Final reduction of the fragments
is performed using a ball-spiked pusher and direct visualization of the
reduction on the retroacetabular surface.
with lag screws, with at least one screw in each articular fragment.
Smaller fragments may require 2.4- or 2.7-mm lag screws. Very small rim
fragments may require the use of a spring plate. Because the direction
of the lag screws can rarely be perpendicular to the fracture,
excessive tightening of the screws can displace the wall fragments. The
lag screws must
be supplemented with a buttress plate that spans the posterior wall fragments from the ischium to the intact ilium.99
Following plate application, the lag screws in the wall can be fully
tightened. This method of fixation has been termed “two-level
reconstruction.”41 Lag screws placed
close to the posterior rim can be confirmed to be extra-articular by
using C-arm visualization directly down the long axis of the screw or
tangential to the screw to confirm that the screw is placed in an
extra-articular location but should be performed prior to buttress
plate fixation obscuring the view.24
The buttress plate should be slightly undercontoured so as to provide
compression to the posterior wall when tightened. Excessive
undercontouring can cause the fragment to be overreduced, which may
prevent the femoral head from fully seating into the acetabulum. The
buttress plate is best placed parallel and close to the rim of the
acetabulum, where it can provide the best buttress for the wall
fragments (Fig. 45-53).
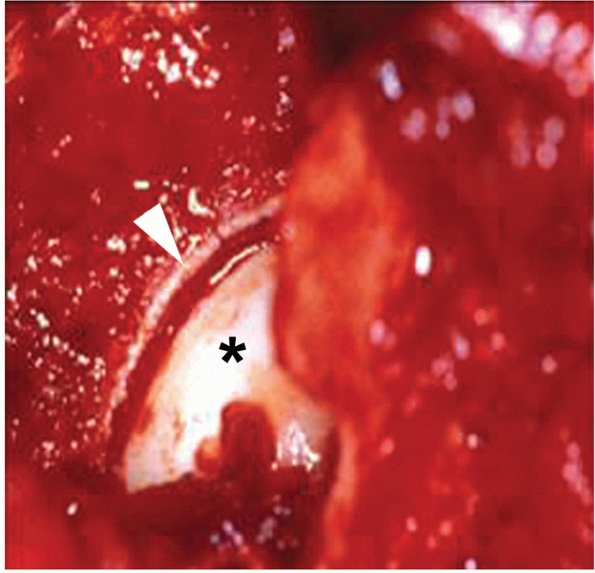 |
|
FIGURE 45-51 Intraoperative photograph demonstrating elevation of the marginal impaction (white arrowhead) with the femoral head (asterisk) used as a template and the filling of the residual osseous cavity with allograft cancellous bone from the patient shown in Figure 45-16.
(From Moed BR, McMichael JC. Outcomes of posterior wall fractures of the acetabulum: surgical technique. J Bone Joint Surg Am 2008;90A[suppl 1]: 87-107.) |
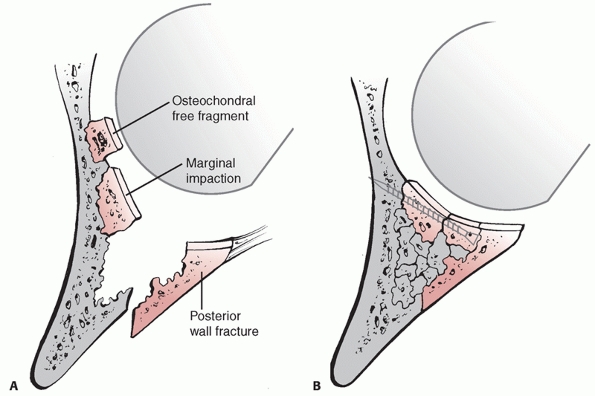 |
|
FIGURE 45-52 A.
Schematic drawing of a hip showing a posterior wall fracture, marginal impaction, and an osteochondral free fragment. (Reproduced, with modification, from Letournel E, Judet R. Fractures of the Acetabulum. New York: Springer, 1993: 418. Permission granted.) B. Drawing of the hip after fracture fragment repositioning, bone-grafting, and stabilization with use of a subchondral mini screw. (Redrawn after Moed BR, McMichael JC. Outcomes of posterior wall fractures of the acetabulum: surgical technique. J Bone Joint Surg 2008; 90A:87-107. Permission granted.) |
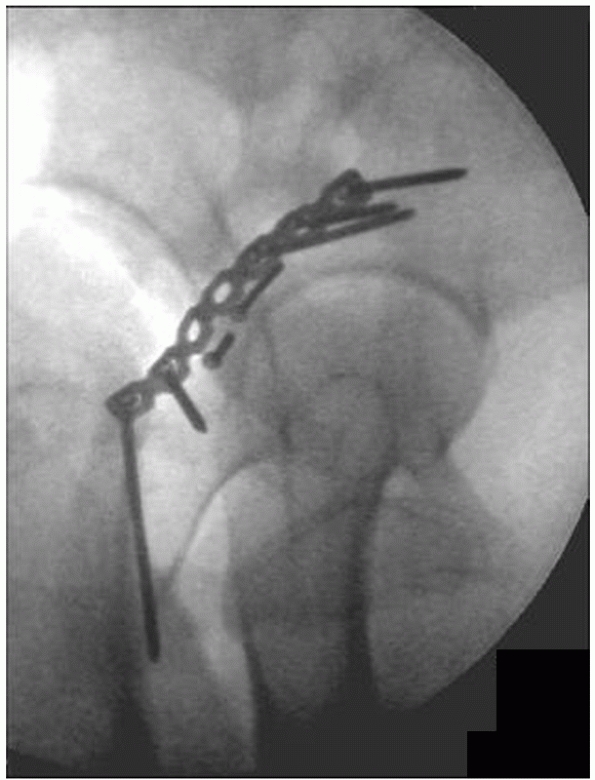 |
|
FIGURE 45-53
Intraoperative C-arm fluoroscopy showing extra-articular placement of two 2.7-mm lag screws and the buttress plate appropriately positioned for a small posterior wall fragment. (Copyright Berton R. Moed, MD.) |
involved, as it is in most fracture types (posterior column, posterior
column and wall, transverse, transverse and posterior wall, T-shaped,
anterior and posterior hemitransverse, and both-column), there is a
rotational as well as translational displacement of this component.
Insertion of a Schanz screw into the ischium is an important first step
in correcting this multiplanar displacement (Fig. 45-54A).
For fractures that involve only the posterior column (posterior column
with or without a posterior wall component), one additional reduction
clamp is usually required to complete the reduction. This reduction
clamp is placed on the retroacetabular surface on either side of the
fracture line. If there is no comminution in the column, a standard
pointed reduction clamp can be used (Fig. 45-54B).
If comminution is present, requiring the length of the column to be
restored, a clamp that has distraction capabilities, such as a
Jungbluth, should be used (see Fig. 45-32C).
The reduction is visualized on the intact retroacetabular surface and
is palpated on the quadrilateral surface through the greater sciatic
notch. The posterior column fracture is then secured to the intact
ilium with interfragmentary screw fixation directed toward the pelvic
brim. Secure lag screw fixation is critical to maintain the reduction
and is easily performed perpendicular to the fracture plane in all
except the lowest posterior column fractures. Although the patient may
be positioned prone or lateral, prone is preferred as it controls the
position of the leg, allows the sciatic nerve to remain relaxed during
manipulation through the greater sciatic notch, and improves the
ability to place lag screws. The lag screws are supplemented with a
buttress plate on the retroacetabular surface but in distinction to the
posterior wall, here the plate contour should exactly match the bone.
If the lag screw fixation is not secure, an undercontoured plate can
“pull” the posterior column fracture to the plate, resulting in a loss
of the articular reduction.
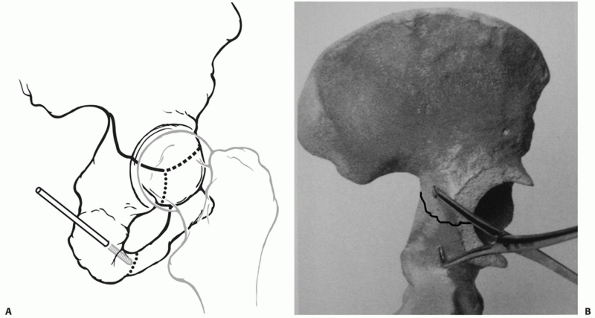 |
|
FIGURE 45-54 A.
Drawing of a hemipelvis showing a Schanz screw in the ischium, which is used to control rotational, as well as translational, displacement of the posterior column seen in a number of fracture types. B. Plastic bone model showing a fracture of the posterior column with a pointed reduction clamp applied. (A. Copyright Berton R. Moed, MD. B. Modified from Tile M, Helfet DL, Kellam JF. Fractures of the Pelvis and Acetabulum. Philadelphia: Lippincott Williams & Wilkins, 2003:688.) |
posterior approach is similar to the reduction of the posterior column
fracture. Derotation of the fracture around the vertical axis through
the symphysis and correction of medial displacement are difficult to
achieve from a posterior approach without the patient being prone.
Often a number of reduction tools are required. Initially, a Jungbluth
clamp alone is sufficient. Experience will improve positioning of the
reduction screws and the ability to obtain reduction. Reduction of the
anterior column can be assessed by palpation of the quadrilateral
surface and pelvic brim through the greater sciatic notch. In
transtectal and some juxtatectal fractures, only a small portion of the
anterior fracture line can be palpated. Intraoperative fluoroscopy may
assist in judging the reduction of the anterior column. Residual
displacement at the pelvic brim is caused by continued displacement of
the fracture around its horizontal axis. Reduction can be completed
with the use of a Schanz screw in the ischium or by angled reduction
clamps introduced through the greater sciatic notch (Fig. 45-55AB). Often, all three methods are required (Fig. 45-55C).
Lag screw fixation of the anterior column of the transverse is
accomplished initially, followed by screw fixation across the posterior
column. An accurately contoured neutralization plate is then applied,
resulting in a biomechanically sound initial internal fixation. It is
important
to
realize that the anterior column screw can only be placed at a certain
angle through the Kocher-Langenbeck approach, which causes it to exit
near the pectineal eminence (Fig. 45-56).
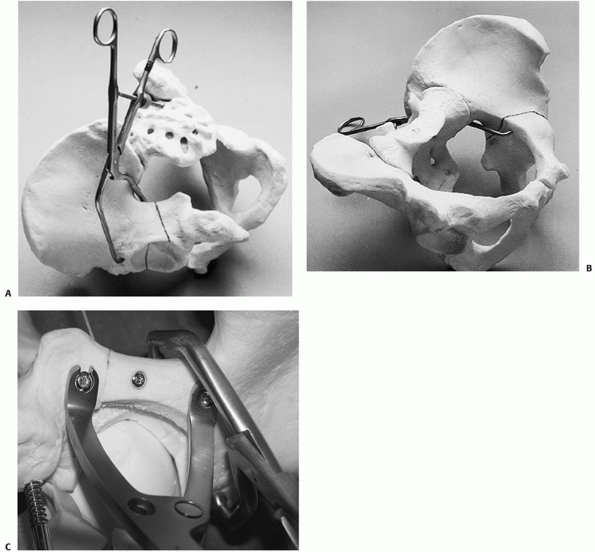 |
|
FIGURE 45-55
Plastic bone model of a transverse fracture showing positioning of a pointed reduction clamp applied through the greater sciatic notch. A. External view. B. Internal view. C. Plastic bone model showing the use of all three methods-clamp through the greater sciatic notch, clamp between two screws in the retroacetabular surface, and a Schanz screw in the ischium-to accomplish reduction. (A,B. From Moed BR. Acetabular fractures: the Kocher-Langenbeck approach. In: Wiss DA, ed. Master Techniques in Orthopaedic Surgery: Fractures. Philadelphia: Lippincott Williams & Wilkins, 2006:687.) |
ilioinguinal approach is achieved by applying lateral and caudal
pressure on the pelvic brim using a ball-spiked pusher through the
middle window. The reduction can then be maintained using a two-screw
technique or an angled reduction clamp introduced through the lateral
or middle window. Fixation proceeds in the same sequence, with screw
fixation of the posterior column accomplished through the
neutralization plate along the pelvic brim. If the transverse fracture
exits low on the pelvic brim, there may not be adequate bone for a lag
screw to be placed. In this circumstance, use of the ilioinguinal
approach is not recommended, as it is very difficult to maintain the
reduction and apply a well-contoured plate simultaneously.
fractures is complicated by several factors. Secure clamp placement is
difficult and usually requires a small quadrangular clamp introduced
entirely within the middle window. This in turn interferes with
contoured plate placement. Interfragmentary screw fixation is often not
possible without violating the hip joint. A screw placed very close to
the pelvic brim and paralleling the quadrilateral surface may suffice
to hold the wall fracture but will often be intra-articular within the
cotyloid fossa. Once a lag screw is obtained (if possible), a buttress
plate is added with screws secured into the superior ramus below and
the ilium above the wall fracture (Fig. 45-57).
reduced through the ilioinguinal approach with a combination of pelvic
clamps positioned at the iliac crest, interspinous notch, and pelvic
brim. Occasionally, the anterior column
fracture
is found to be incomplete with the fracture line not exiting the iliac
crest. The displacement of the column occurs through comminution or
plastic deformation in the very thin central portion of the iliac wing.
It is often not possible to achieve a complete reduction of the
anterior column in this situation without completing the fracture by
osteotomizing the iliac crest. This improves the mobility of the
anterior column fragment for reduction. The reduction of the anterior
column is assessed primarily through the lateral and middle windows.
Care must be taken to restore the normal concavity to the internal
iliac fossa. Residual external rotation or flexion of the anterior
column fracture is appreciated as a gap in the fracture site at the
pelvic brim. When the rotation of the anterior column is correct, the
anterior inferior iliac spine should be aligned with the nutrient
foramen of the ilium. Residual flexion of the anterior column may be
improved by a two-screw technique at the pelvic brim or a quadrangular
clamp between the quadrilateral surface and the anterior wall. Fixation
of the anterior column can often be performed with lag screw fixation
alone. Lag screws started just lateral to the pelvic brim and directed
toward the sciatic notch or retroacetabular surface help to control the
external rotation and flexion of the anterior column. A lag screw
placed between the tables of the ilium at the iliac crest as well as
one directed from the interspinous notch toward the posterior superior
iliac spine completes the fixation. Inadequate screw purchase,
osteoporotic bone, or screw fixation placed obliquely to the anterior
column fracture line may require buttress plate supplementation as well
(Fig. 45-58).
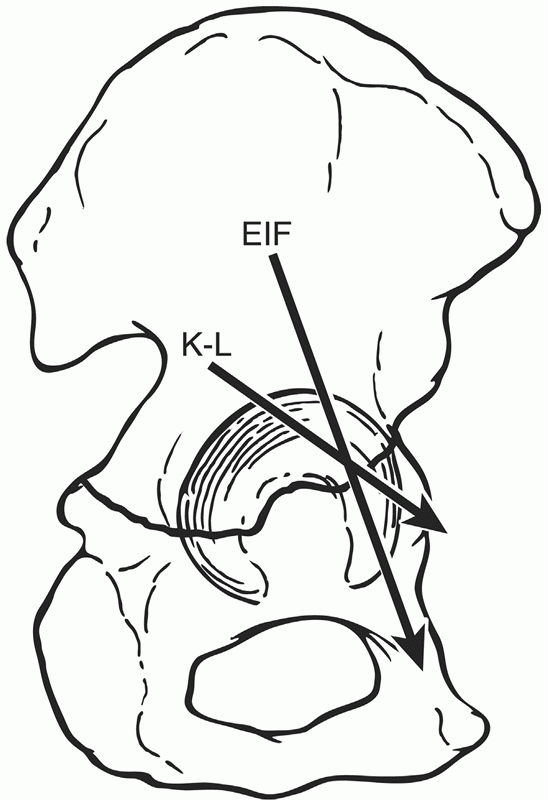 |
|
FIGURE 45-56
Drawing showing the possible angles for insertion of an anterior column lag screw using the Kocher-Langenbeck (K-L) versus the extended iliofemoral (EIF). The angle of the EIF without using this exposure can also be attained by using percutaneous techniques. (Copyright Berton R. Moed, MD.) |
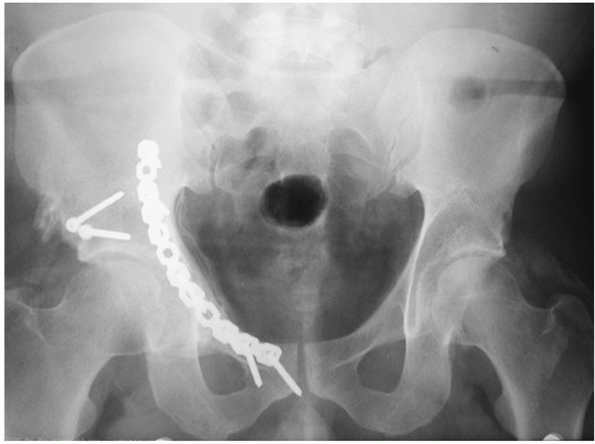 |
|
FIGURE 45-57 Radiographic appearance at 8 months of the patient seen in Figure 45-18.
Two interfragmentary screws have been supplemented by a buttress plate that spans from the intact internal iliac fossa to the superior ramus. The central hole in the plate was used for a screw paralleling the quadrilateral surface. |
with anterior sacroiliac joint opening and external rotation of the
“intact” portion of the ilium. This should be reduced prior to
attempting reduction of the anterior column and may be internally fixed
with a single two-hole plate—one screw in the sacrum and one in the
ilium. Additional stability
for this rotational injury results from the fixation of the anterior column fracture.
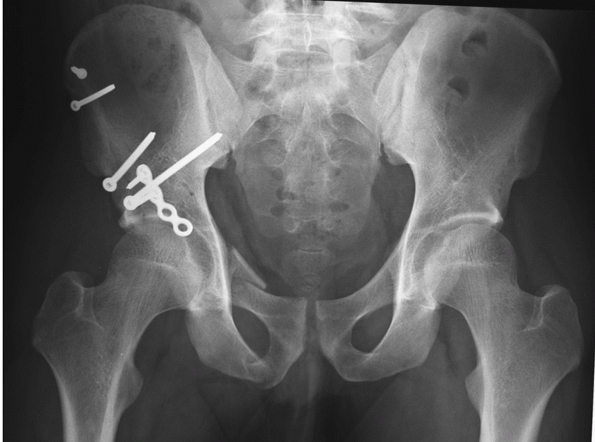 |
|
FIGURE 45-58 Radiographic appearance at 6 months of the patient whose injury films are seen in Figure 45-21.
The anterior column has been fixed at the crest and interspinous notch with interfragmentary screws. A separate fragment of anterior wall comminution was buttressed with a “push” plate that buttresses the anterior wall without actually spanning to the superior ramus. The comminuted superior ramus fracture has been left to heal unfixed. |
column plus posterior wall fracture is generally treated through the
Kocher-Langenbeck approach with the patient positioned prone. The
reduction begins with the posterior column fragment exactly as
previously described. Large posterior wall fractures, however, may
contain much of the retroacetabular surface and preclude stable
interfragmentary fixation of the column. In this circumstance, a small
plate along the border of the greater sciatic notch may be useful in
maintaining the reduction of the posterior column. The posterior wall
component is then reduced along with any marginal impaction that may be
present. Interfragmentary screws in addition to buttress plate fixation
are necessary to maintain reduction of the posterior wall. The buttress
plate on the posterior wall will now serve as additional fixation for
the posterior column fracture as well. Unless the caudal screws in the
plate cross the ischial ramus fracture, however, the stability of the
posterior column is dependent on accurate contouring of the buttress
plate and the interfragmentary column screws.
transverse fracture proceeds as previously described. The addition of a
posterior wall component adds technical complexity to the reduction and
fixation. The transverse fracture is reduced first and held in place
with interfragmentary screw fixation if possible. If the posterior wall
fracture is large, sufficient retroacetabular surface may not be
available for screw placement. In this circumstance, a small plate
adjacent to the posterior border of the innominate bone may suffice.
The posterior wall fracture is then reduced in the standard fashion and
fixed with interfragmentary screw and buttress plate fixation. Less
undercontouring of the posterior wall plate is desirable than for the
isolated posterior wall fracture; otherwise, the plate may cause a loss
of reduction of the transverse fracture line as it is tightened to the
bone. With operative treatment at less than 2 weeks, the
Kocher-Langenbeck is usually sufficient (Fig. 45-59A). Otherwise, an extended approach may be required (Fig. 45-59B).
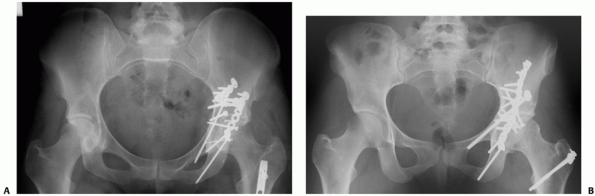 |
|
FIGURE 45-59 A. Radiographic appearance at 1 year of the patient whose injury films are seen in Figure 45-25.
The fracture was treated within a few days of injury through the Kocher-Langenbeck. A short plate was used posteriorly for the transverse component and the anterior column lag screw was inserted percutaneously using C-arm guidance. The comminuted posterior wall was buttressed separately. Also seen is the tip of a retrograde femoral nail. B. Radiographic appearance at 6-year follow-up of the patient whose injury films are shown in Figure 45-49. The fracture was treated 22 days after injury through the extended iliofemoral approach. (Copyright Berton R. Moed, MD.) |
The anterior column is reduced through the ilioinguinal approach as
described earlier. Once the anterior column reduction is achieved,
interfragmentary screw fixation from the internal iliac fossa to the
sciatic buttress is frequently helpful but must be positioned to avoid
crossing the fracture line of the unreduced posterior column fracture.
This is supplemented with screw placement between the tables of the
ilium at the iliac crest. Alternately, plate and screw techniques can
be used at the iliac crest if screw placement alone is inadequate. The
posterior column fracture may now be reduced using an angled clamp
placed around the iliopsoas from the quadrilateral surface portion of
the posterior column fragment to the supracetabular ilium. An
intrapelvic rotational reduction of the posterior column is achieved.
The reduction is assessed by palpation of the quadrilateral surface and
image-intensifier visualization of the ilioischial line on the AP view.
It is important to recognize that the reduction of the articular
surface is never directly visualized. By anatomically reducing the
internal contour of the innominate bone in combination with
intraoperative fluoroscopy, an anatomic reduction of the articular
surface is obtained. The posterior column fracture is frequently
internally fixed with a screw placed from the outer cortex of the ilium
to the quadrilateral surface. Additionally, a screw placed from the
internal iliac fossa is directed down the length of the posterior
column to exit the ischium or lesser sciatic notch. In many cases,
screws alone may be used for fixation of the anterior column and
posterior hemitransverse fracture. However, buttress plates along the
pelvic brim should be added for comminuted fractures or osteopenic
patients. Anterior wall fracture components may require additional
buttress plate fixation (Fig. 45-60).
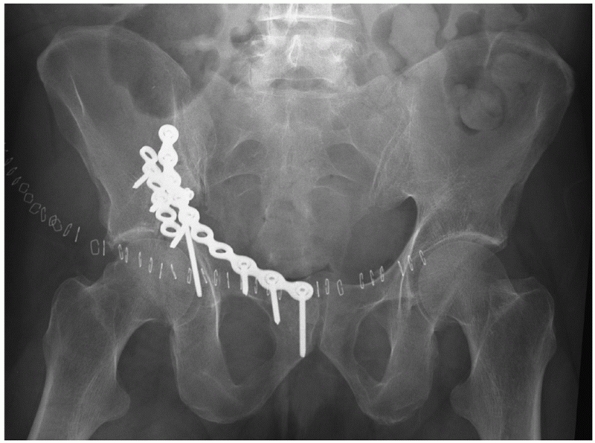 |
|
FIGURE 45-60 Postoperative radiograph of the patient seen in Figure 45-26.
The wear defect in the femoral head is again noted. Long buttress plate fixation has been supplemented by a second push plate buttressing the lateral portion of the anterior wall fragments. The posterior hemitransverse is fixed by posterior column screws inserted into the plate applied to the pelvic brim. The joint space is seen to be subtly widened. This appearance may be seen if the anterior wall fragment is slightly overreduced and causes a partial extrusion of the femoral head. The prognosis for the hip joint is guarded. |
on through the Kocher-Langenbeck approach with the patient in the prone
position. The reduction of the anterior column fracture is performed by
displacing the posterior column fracture and placing a clamp across the
stem of the T between the anterior column fracture and the intact
ilium, as in Figure 45-55A,B. The reduction is
assessed radiographically as well as directly visualized on the
articular surface with the femoral head distracted. Internal fixation
with lag screws down the long axis of the anterior column is performed.
The posterior column fracture is then reduced and internally fixed as
described in the posterior column section (Fig. 45-61).
Another option is the reduction and lag screw fixation of the posterior
column fracture first. This is made more complicated by the need to
keep the posterior column fixation completely out of the anterior
column fracture and the stem of the T. Placement of clamps through the
greater sciatic notch then allows reduction of the anterior column
fracture. With either of these techniques, if the anterior column
fracture cannot be reduced, a subsequent anterior approach may be
required. T-shaped fractures with significant displacement of the
vertical stem at the obturator notch are very unlikely to be reduced
with a single nonextensile approach and are best treated initially
through an extensile approach or combination of approaches that allows
simultaneous access to both columns. Alternately, planned sequential
Kocher-Langenbeck and ilioinguinal approaches may be used.
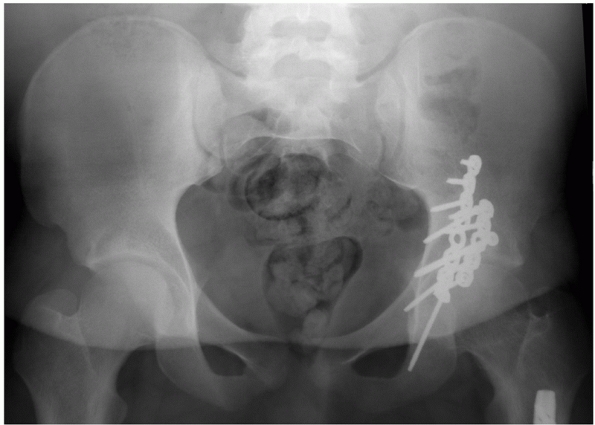 |
|
FIGURE 45-61 Radiographic appearance at 2 years of the patient whose injury films are seen in Figure 45-28.
This patient was treated in the prone position through the Kocher-Langenbeck approach. Due to the patient’s large size, two lag screws were placed into the anterior column and two plates were applied to the posterior column. (Copyright Berton R. Moed, MD.) |
Kocher-Langenbeck approach alone, direct plate fixation on both columns
is not necessary. A single well-contoured plate on the retroacetabular
surface with lag screws across both the anterior and posterior column
fractures can suffice.132
the reduction and fixation of the T-shaped fracture. This is most
common when the stem of the T is anterior, close to the pelvic brim.
This configuration typically leaves a large portion of the
quadrilateral surface intact to the posterior column fragment, allowing
the surgeon sufficient access for the reduction. Analogous to the
situation just described, if the reduction of the posterior column is
not successful through the ilioinguinal approach, a staged subsequent
Kocher-Langenbeck would be required for the direct reduction and
fixation of the posterior column.
significant complexity to the fracture reduction. Stable fixation of
the posterior column and wall without crossing into the stem of the T
or the anterior column fracture line may no longer be possible.
Therefore, the anterior column fracture must be reduced and fixed
first. Unfortunately, the ideal starting point for the anterior column
lag screws is often obscured by the posterior wall fracture. Obtaining
reduction and fixation of the anterior column first through either an
anterior approach or through the extended approach makes the reduction
and fixation of the posterior column and wall more feasible. However,
it is very difficult to obtain stable fixation of the anterior column
fracture without the screws inadvertently crossing the stem of the T,
the posterior column fracture line, or the posterior wall fracture or
penetrating the hip joint. These technical considerations may explain
why the T-shaped fracture with an associated posterior wall had the
lowest rate of excellent reductions of any type or subtype of fractures
in the series of Letournel and Matta and colleagues.78,83
through the ilioinguinal approach is frequently similar to that of the
anterior plus posterior hemitransverse fracture. The entire internal
contour of the innominate bone must be reconstructed to ensure anatomic
reduction of the acetabulum. Comminution or plastic deformation of the
thin cortical bone of the internal iliac fossa is common, making
assessment of reduction impossible in this location. Frequently,
comminution
at the pelvic brim is seen, and if this is not reduced, the anterior
column reduction can be assessed only at the iliac crest. The tendency,
then, is for the surgeon to leave the anterior column with a residual
flexion and adduction deformity, making perfect reduction of the joint
impossible. As with nonperatively treated both-column fractures,
operative malreduction may lead to secondary surgical congruence if all
the fracture fragments remain congruent to the femoral head. Although
this may be better tolerated than other malreductions of the
acetabulum, it is still undesirable.
A large reduction clamp placed across the anterior border of the
innominate bone can be used to reduce the posterior wall. This fracture
can be fixed with obliquely oriented screws placed from just lateral to
the pelvic brim and directed posteriorly toward the superior iliac
extension of the wall fragment (Fig. 45-62).
encountered. This is especially frequent with initial medial
displacements of the femoral head causing an impaction of the medial
roof. Lateral traction via a trochanteric pin may be used to position
the femoral head beneath the intact segment of articular surface. The
femoral head may then be used as a mold for the reduction of the
impacted segments. The disimpaction of such fragments is usually
performed through the anterior column or quadrilateral surface fracture
lines. In some circumstances, the impacted roof fragment may not be
accessible though a primary fracture line and a cortical window may
have to be created in the internal iliac fossa, allowing insertion of a
bone tamp and disimpaction of the fragment with radiographic assessment
of the reduction. When roof impaction is reduced, screw fixation just
above the fragment may help to prevent reimpaction during healing.
These screws are naturally close to the articular surface and, if
displacement does occur, may come in contact with the femoral head,
contributing to articular wear and loss of the joint (Fig. 45-63).
fractures, many associated both-column fractures may be amenable to lag
screw fixation alone. A long contoured plate applied to the pelvic brim
adds additional stability and should always be used if there is any
question of the stability of the screw-only construct.
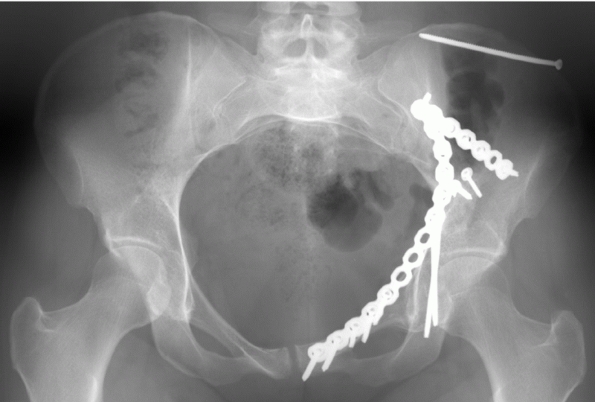 |
|
FIGURE 45-62 Radiographic appearance at 2 years of the patient whose injury films are seen in Figure 45-30.
This patient was treated through the Ilioinguinal approach. Obliquely oriented screws were placed from just lateral to the pelvic brim and directed posteriorly toward the superior iliac extension of the posterior wall fragment. (Copyright Berton R. Moed, MD.) |
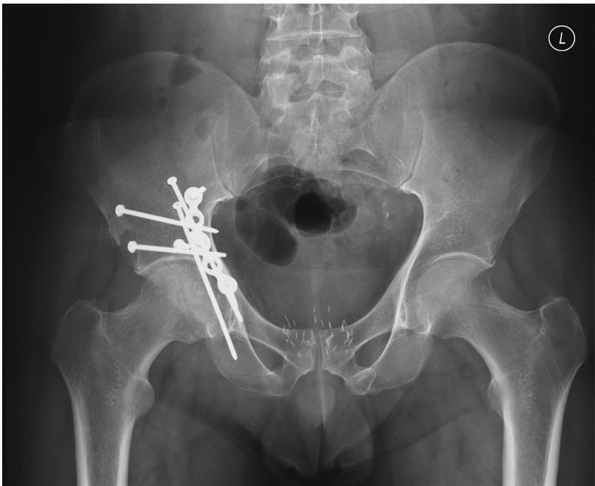 |
|
FIGURE 45-63 Six-month radiograph of the patient seen in Figure 45-27.
The “gull wing” impacted fragment has been reduced using the femoral head as a template. A lag screw placed from outside the bone to the quadrilateral surface passes directly above the fragment to buttress it, and a second anteroposterior screw is placed just above this fragment to prevent the first screw from losing fixation and allowing displacement of the fragment. A slight imperfection in the roof can be appreciated where the impacted fragment was reduced. |
time prior to their procedure or have prolonged delays until surgery
may have an alteration of their skin flora because of inadequate
ability to effectively cleanse the perineum. For this reason,
prophylactic antibiotic coverage with a first generation cephalosporin,
administered preoperatively and continued at least 24 hours
postoperatively, is often supplemented by Gram-negative coverage.
Suction drainage is used and continued for 48 hours or until drainage
has ceased.
high risk for thromboembolic disease. Currently, no prophylactic
treatment consensus exists. Our approach consists of mechanical
sequential compressive devices applied on hospital admission to both
lower extremities, low-molecular-weight heparin for chemical
prophylaxis as soon as the patient is hemodynamically stable, and
screening using duplex color Doppler ultrasound. For patients who
require operative intervention, the low-molecular-weight heparin is
discontinued on the night prior to surgery and resumed within 36 hours
after surgery. Those positive preoperatively for deep vein thrombosis
receive a vena cava filter. After discharge from the hospital, the
patients are maintained on chemical prophylaxis until they have
regained an active ambulatory status, usually 6 to 12 weeks
postoperatively.10 Vena cava filters
are reserved for those high-risk patients having contraindications to
chemical prophylaxis and those with preoperatively diagnosed deep vein
thrombosis or pulmonary embolism.
|
TABLE 45-9 Recommendations for Heterotopic Ossification Prophylaxis
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||
approaches that involve stripping of muscle from the external surface
of the ilium and is a particular risk of extended surgical approaches.
Based on a review of the current evidence available in the literature,100 recommendations have been made regarding the use of heterotopic ossification prophylactic treatment (Table 45-9).
Indomethacin is inexpensive, simple, and safe and probably works. Our
approach is to use 25 mg three times daily beginning within 24 hours of
surgery and continued for 4 to 6 weeks. As with other nonsteroidal
anti-inflammatory drugs, gastric and duodenal mucosal lesions may
occur. In addition, gastrointestinal prophylaxis (such as misoprostol
or a proton pump inhibitor) should be considered to decrease the risk
of these drug-induced lesions.7,43,124,127
However, the use of this drug, or that of any other gastroduodenal
mucosal protective agent, in patients with an acetabular fracture
receiving indomethacin for heterotopic ossification prophylaxis has not
been studied. Irradiation with 700 cGy is considered in high-risk cases
(e.g., head injured) and for adult patients (women beyond childbearing
age) requiring an extended surgical approach (see Complications).
radiographs should be obtained. A postoperative CT scan should be
considered if there is concern for inadequate or loss of reduction.56
The patient is mobilized as quickly as the associated injuries will
allow. Sitting up on the first postoperative day is followed by formal
physical therapy for active range-of-motion exercises on subsequent
postoperative days. Total hip arthroplasty precautions should not be
needed, as internal fixation has rendered the hip joint stable. Partial
toetouch weight bearing of 10 to 15 kg with crutches or a walker is
required for 10 to 12 weeks. However, progression to full weight
bearing must be tailored to the individual. Formal physical therapy
should begin at 6 weeks postoperatively for muscle strengthening and
continue until muscle strength and range of motion are regained or a
plateau is reached.
The risk of infection is increased in patients with open fractures and
local soft-tissue injuries such as Morel-Lavallee lesions49 (Fig. 45-64).
Gastrointestinal or urologic injuries are also associated with
increased infection rates. Appropriate antibiotics, lessextensive
surgical approaches, and aggressive débridement of open wounds can help
to decrease the rate of infection. Infection has also been reported in
conjunction with postoperative irradiation. Haas et al.48
reported infection in (9%) 6 of 66 patients who were treated with
postoperative radiation to diminish heterotopic ossification. This is
one of the highest reported rates of infection after acetabular
fracture. Other authors have reported lower rates of infection after
extended approaches and irradiation.102,139
intra-articular wound infection cannot be minimized. Complete joint
destruction can be expected in 50% of these cases.83,90
However, the results are somewhat dependent on the surgical approach.
If an infection involves the joint itself, the results are uniformly
bad. This is usually the case when a surgical approach is used that
exposes the joint directly, such as the Kocher-Langenbeck or an
extended approach. In contradistinction, patients treated operatively
via the ilioinguinal approach who become infected have a much better
chance at a good outcome. This is likely because there is less
devitalization from stripping of muscle from the innominate bone and
the reduction of the joint is indirect. Therefore, the local blood
supply is less impaired and deep infection may remain extra-articular,
sealed off from the joint by the fracture reduction and healing.
anatomic regions. If the infection is early, then hardware preservation
is attempted to maintain the stability of the hip until union; then it
is removed. Late infection is treated with hardware removal. In all
cases, long-term culture-specific antibiotics, usually an empiric
course of 6 weeks, is used.
known prevalence of these injuries is low. However, iatrogenic damage
to the sciatic nerve is one of the major complications encountered in
acetabular fracture management. These injuries are most commonly
associated with the posterior and extended surgical approaches that
involve direct exposure and retraction of the sciatic nerve.78,152 Injury at the time of indirect reduction of posterior column displacement through an anterior surgical approach can also occur.33,60,78
Intraoperative sciatic nerve monitoring has been advocated by some
authors as a method to decrease the incidence of sciatic nerve injury.
However, the rate of nerve injury appears to decrease as surgeon
experience increases. Matta and colleagues reported a 9% prevalence in
their retrospective series,86 decreasing to 5% in the subsequent prospective series,84 and further diminished to 3% without the aid of nerve monitoring.83
These numbers compare favorably with those of a series using
somatosensory evoked potential monitoring systems that report a 2% to
7% prevalence.8,58,60,152
The question is whether somatosensory evoked potential monitoring,
while feasible, is of real clinical value. It has been shown that
iatrogenic injury may occur despite normal somatosensory evoked
potential tracings.104,152 Furthermore, Middlebrooks et al.93
demonstrated no substantial reduction in the rate of iatrogenic nerve
injury with the use of intraoperative somatosensory evoked potential
monitoring. At present, there are no clear data indicating that nerve
monitoring actually reduces the overall rate of iatrogenic sciatic
nerve injury. Currently, there is no substitute for attention to detail
in the operating room with careful patient positioning, maintaining the
knee flexed during posterior approaches to relax the sciatic nerve,
cautious placement of retractors, and limited traction on the nerve
during fracture reduction.
 |
|
FIGURE 45-64 Example of a Morel-Lavallee lesion in a patient with combined pelvic and acetabular fractures. (Copyright Berton R. Moed, MD.)
|
The most common neurologic injury after treatment of an acetabular
fracture is to the lateral femoral cutaneous nerve after the
ilioinguinal approach.32,77,85
Despite taking all appropriate measures to protect the nerve, during
even a routine surgery the nerve may become stretched or attenuated.
Clinically, most patients experience a region of cutaneous anesthesia
in the nerve distribution that becomes dysesthetic over time but
ultimately resolves. Warning the patient of this likelihood
preoperatively is important because even though the symptoms are
generally well tolerated by the patient, they are nevertheless bothered
enough by their symptoms to seek reassurance that they will resolve.
intra-articular placement of screws is a documented and often
destructive complication of acetabular fracture surgery. Letournel and
Judet78 originally proposed taking
the hip through range of motion in complete silence in the operating
room to listen for crepitus as a method for detecting intra-articular
hardware. Anglen and DiPasquale6
recommended use of a sterile esophageal stethoscope for the same
purpose. Other authors have recommended careful intraoperative and
postoperative radiography (fluoroscopy, plain radiography, and/or CT)
to ensure that the hardware has been placed outside the joint.6,114 Currently, it appears that intraoperative fluoroscopy is the best method.24
If hardware has been placed within the joint, it is imperative that the
offending implant(s) be removed. Otherwise, posttraumatic arthrosis
will almost certainly ensue.
significant problem in acetabular fracture patients. Proximal deep vein
thrombosis was identified using magnetic resonance venography in 34% of
acetabular fracture patients.112 Letournel and Judet78
reported 13 deaths (2.3%) after acetabular fracture surgery, 4 of which
were caused by massive pulmonary embolism. Therefore, some form of
mechanical or chemical prophylaxis is recommended to decrease the risk
of thromboembolic complications. One study indicated that early (at the
time of hospital admission) mechanical prophylaxis with foot pumps and
the addition of enoxaparin on a delayed basis (5 days after admission)
is a very successful strategy for prophylaxis against venous
thromboembolic disease following serious musculoskeletal injury.134
For any patient who was required to return to the operating room, the
enoxaparin was discontinued on the night prior to surgery and was
resumed within 12 hours after surgery. Despite the use of prophylactic
treatment, the prevalence of posttraumatic and postoperative
thromboembolism approximates 11%,11,134,135 and the value of screening, using Doppler ultrasound or magnetic resonance venography, remains controversial.11 The placement of prophylactic vena caval filters is controversial but may be indicated in selected high-risk patients.11,121
in as many as 90% of patients after acetabular fracture surgery (range,
18% to 90%) with severe involvement as high as 50% in some patient
groups.15,92
The terminology “severe heterotopic ossification” is often used to
describe the amount of heterotopic ossification necessary to impair
function. Greater than 20% loss of total hip motion is thought to be
the best clinical definition for severe heterotopic ossification.83
Many reports have used the Brooker classification, which relies solely
on the AP radiographic view of the hip, for this determination.15,92,103
However, this radiographic method does not consistently correlate with
hip joint motion and generally overestimates the clinical severity of
heterotopic ossification.78,107,95
A radiographic classification that would accurately correlate with
significant limitation of hip motion should be useful in evaluating the
independent effect of heterotopic ossification on functional outcome in
patients after acetabular fracture surgery. Adding the standard Judet
oblique views (which would routinely be obtained in the course of the
patient’s postoperative evaluation) to the AP view and reading them in
a logical specified sequence appear to give a more reliable indication
of the restriction of motion that can be attributed to heterotopic
ossification.107 Using this modified system, classes 0, I, and II typically demonstrate unimpaired range of motion.107
ossification is stripping of the gluteal muscles from the external
surface of the ilium.15,78,83,92,103
In his series, in which significant heterotopic bone formation was
defined as motion limited by greater than 20% and patients were not
given prophylactic treatment, Matta83 reported the following prevalence figures: Kocher-Langenbeck, 9 of 112 (8%); extended iliofemoral, 12
of 59 (20%); ilioinguinal, 2 of 87 (2%). From retrospective studies, it
appears that the rate of heterotopic ossification can be reduced with
the use of indomethacin and radiation therapy.15,62,78,101,102,103 In a prospective randomized study comparing indomethacin and radiation therapy, Moore et al.111
demonstrated both to be safe and effective prophylactic agents.
Noncompliance was the problem with indomethacin; radiation was
strikingly more expensive. In a follow-up to this study, Burd et al.21
performed a comparable study in a larger group of patients and their
findings were similar. Use of a combination of irradiation and
indomethacin essentially eliminated postoperative heterotopic
ossification in a series reported by Moed and Letournel and no
progression of heterotopic ossification was noted, even when early
ossification was seen on preoperative radiographs.102
Matta and Siebenrock reported a randomized prospective trial indicating
that indomethacin was not effective. However, the numbers were too
small to be definitive, having a low power (only 10%) to detect a
significant difference between treatment and no treatment groups.89
postoperative complication of acetabular fracture surgery and
prophylactic therapy is desirable. However, one must weigh the risk of
prophylaxis and its potential for failure against the actual risk of
occurrence in each particular clinical situation. A recent study in
acetabular fracture patients has shown that the use of indomethacin
increases the risk of long bone nonunion.20
The possibility of induced malignant disease is the main concern with
low-dose radiation therapy, although genetic alterations in offspring
may also be at issue.30 When
deciding on prophylactic therapy, the actual expected rates of
functionally important heterotopic ossification should always be kept
in mind: 8% for Kocher-Langenbeck, 20% for extended iliofemoral, and 2%
for ilioinguinal.78
acetabulum is posttraumatic arthrosis. The quality of the fracture
reduction appears to be the main determinant for clinical outcome and
for the risk of late traumatic arthrosis.78,83,90
Long-term studies have demonstrated that fracture reductions to within
1 mm of residual displacement have better long-term outcome and a lower
prevalence of arthritis than those with greater than 1 mm of
displacement. In addition, if arthritis develops after a perfect
reduction, the onset tends to be later and the progression slower than
arthritis that develops after a poor reduction.78 Damage to the femoral head at the time of initial injury is another important factor.83
Osteonecrosis of the femoral head is known to result from acetabular
fracture associated with hip dislocation and can also result in
posttraumatic arthrosis. However, posttraumatic arthrosis is more
commonly because of wear of the femoral head against a malreduced
fracture and may often be incorrectly attributed to osteonecrosis.78,83 Total hip arthroplasty or arthrodesis is indicated for patients with posttraumatic arthrosis and disabling pain.
reported using the modified rating scale of d’Aubigné and Postel, which
is a clinical grading system. As noted earlier, with sufficient
training and experience, good-to-excellent long-term clinical results
in 75% to 81% of fractures should be expected, as measured by this
evaluative tool. Despite the common practice of using such clinical
measures to evaluate the outcomes in patients with orthopaedic
conditions, a validated, self-reported patient questionnaire is most
useful for determining health status.117,142
The Musculoskeletal Function Assessment, a validated well-designed
self-reported patient questionnaire, is a useful outcome instrument for
patients with musculoskeletal disorders.37,82
Studies using this functional outcome instrument as the evaluative
measure of health status after acetabular fracture surgery paint a
different picture.72,105,109
In a series of studies, Moed and coworkers found that complete recovery
after a fracture of the acetabulum is uncommon, with residual
functional deficits involving wide-ranging aspects of everyday living
that do not necessarily have an obvious direct connection to hip
function.105,109
Although a correlation was found between the modified Merle d’Aubigné
and Postel and the Musculoskeletal Function Assessment scores, the
relatively worse Musculoskeletal Function Assessment scores for these
patients with an acetabular fracture, compared with those in the normal
population, indicate that a complete return to a preinjury functional
level is uncommon for these patients despite a good-to-excellent Merle
d’Aubigné clinical score.105,109
Similarly, Kreder et al. found relatively worse Musculoskeletal
Function Assessment scores for patients with an acetabular fracture
compared with those in the normal population.72
Despite some differences among these studies, the overall data and the
importance of the emotional category of the Musculoskeletal Function
Assessment score as a negative determinant of functional outcome were
consistent. Interestingly, these findings are similar to those of a
small series of patients with hip and femur fractures.36
Although the modified Merle d’Aubigné score may be useful for
evaluating isolated hip function in patients with a fracture of the
acetabulum, it appears to have limited usefulness as a method for
evaluating the overall functional outcome in these patients. It
certainly is possible for your patient to have minimal hip pain, walk
without a limp, and have a good-looking radiograph but not be doing
well.
the early 1960s, significant strides have been made in the treatment of
acetabular fractures. There is no doubt that excellent clinical results
can be obtained by experienced surgeons and the expansion of
educational activities specific to acetabular fracture care has
increased the number of experienced surgeons. However, acetabular
fracture fixation remains extensive surgery with a significant
potential complication rate. The results of Letournel and Judet (1993)
remain the “gold standard.”
result, related mainly to residual fracture displacement, infection,
nerve injury, thromboembolic disease, and heterotopic ossification. In
addition, not all fractures are perfectly reconstructable, and there
are some patients for whom the operative morbidity may not be justified
given the expected result. Fractures complicated by extreme osteopenia,
pre-existing arthritis, or large degrees
of articular impaction continue to routinely fail current reconstructive techniques.5,61,133
Elderly patients with significant medical comorbidities may not
tolerate an extensive reconstructive procedure and may not be able to
comply with the postoperative weight-bearing restrictions. Some of
these patients will be better served with total hip arthroplasty.
Unfortunately, primary arthroplasty to treat acetabulum fracture has
been associated with a significantly higher complication rate and
poorer outcomes than standard primary arthroplasty.50,92,113,145
The indications for primary arthroplasty are still to be determined and
the techniques to avoid higher complication rates need to be refined.
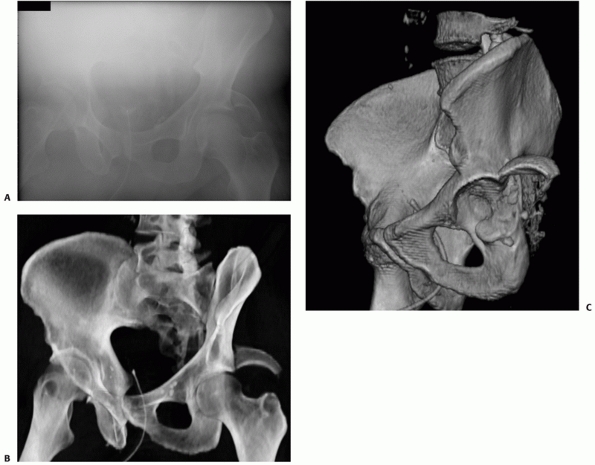 |
|
FIGURE 45-65 An obese 57-year-old man sustained multiple injuries, including an acetabular fracture, in a motor vehicle accident. A. After a number of tries, this obturator oblique radiograph was considered acceptable. B. Obturator oblique radiograph generated from the computed tomography scan obtained on the day of injury. C. Selected three-dimensional computed tomography example in this patient. (Copyright Berton R. Moed, MD.)
|
techniques and improved prophylactic measures. Thromboembolic disease
remains an issue. Deep venous thrombosis continues to occur despite our
currently used measures.11,134,135 Furthermore, our screening measures continue to be unreliable.11
Hopefully, we can look forward to better means of prophylaxis and
improved diagnostic methods. Prophylaxis for heterotopic ossification
remains controversial. Indiscriminate use of irradiation seems ill
advised. However, indomethacin may not really be as effective as the
retrospective studies indicate and it has its own set of potential
complications.
offers the potential of obtaining the radiographs needed for diagnosis
without the usual bother to the patient or the treating surgeon. It
remains to be seen whether these studies, or improved three-dimensional
studies, can provide information equivalent to, or better than, that
derived from plain radiographs (Fig. 45-65).
More information is also needed regarding the determination of joint
stability, for both posterior wall fractures and nondisplaced fractures
that have “potential” to displace. However, the most controversial area
of acetabular fracture treatment is determining the place for
percutaneous surgery. The placement of percutaneous screws across
acetabular fractures is not particularly challenging, particularly when
aided by fluoroscopic visualization or computer-assisted surgical
navigation. The challenge for future development is the ability to
obtain, and maintain, an anatomic articular reduction in a minimally
invasive fashion. Furthermore, the data are limited regarding its use
as a staging procedure in the elderly for total hip arthroplasty.
Percutaneous fixation of acetabular fractures does appear to reduce the
rate of approach-related complications. However, it is yet to be
established whether these techniques improve on the standard
nonoperative and operative methods. Future studies evaluating
intraoperative, fluoroscopically-based three-dimensional image
navigation
systems, along with improved instrumentation for fracture reduction and
fixation through limited incisions, are needed to determine if
percutaneous surgery can better these results.
JE, Volgas DA, Giordano V, et al. A review of the treatment of hip
dislocations associated with acetabular fractures. Clin Orthop
2000;377:32-43.
JE, Davila R, Bradly E. Extended iliofemoral versus triradiate
approaches in management of associated acetabular fractures. Clin
Orthop 1994;305:81-87.
College of Surgeons Committee on Trauma. Advanced Trauma Life Support
Program for Doctors. 7th Ed. Chicago, IL: American College of Surgeons,
2004:11-40.
JO, Burd TA, Hendricks KJ, et al. The “gull sign”: a harbinger of
failure for internal fixation of geriatric acetabular fractures. J
Orthop Trauma 2003;17:625-634.
JO, DiPasquale T. The reliability of detecting screw penetration of the
acetabulum by intraoperative auscultation. J Orthop Trauma
1994;8:404-448.
KD, Bjarnason I, Scott DL, et al. (1993). The prevention and healing of
acute non-steroidal anti-inflammatory drug-associated gastroduodenal
mucosal damage by misoprostol. Br J Rheum 1993;32:990-995.
MR, Wegner D, Booke J. (1994). Somatosensory evoked potential
monitoring during pelvic and acetabular fracture surgery. J Orthop
Trauma 1994;8: 127-133.
PE, Dorey FJ, Matta JM. Letournel classification for acetabular
fractures: assessment of interobserver and intraobserver reliability. J
Bone Joint Surg Am 2003;85A:1704-1709.
BT, Gudmundsen TE, Dahl OE. Frequency and timing of clinical venous
thromboembolism after major joint surgery. J Bone Joint Surg Br
2006;88B:386-391.
DS, Starr AJ, Reinert CM. The effect of screening for deep vein
thrombosis on the prevalence of pulmonary embolism in patients with
fractures of the pelvis or acetabulum: A review of 973 patients. J
Orthop Trauma 2005;9:92-95.
J, Goldfarb C, Catalano L, et al. Assessment of articular fragment
displacement in acetabular fractures: a comparison of computerized
tomography and plain radiographs. J Orthop Trauma 2002;16:449-456.
J Jr, Peelle M, McFarland E, et al. Computer-reconstructed radiographs
are as good as plain radiographs for assessment of acetabular
fractures. Am J Orthop 2008;37:455-460.
J Jr, Kantor J, Ungacta F, et al. Intraneural sciatic nerve pressures
relative to the position of the hip and knee: a human cadaveric study.
J Orthop Trauma 2000;14:255-258.
MJ, Poka A, Reinert CM, et al. Heterotopic ossification as a
complication of acetabular fracture: prophylaxis with low-dose
irradiation. J Bone Joint Surg Am 1988;70A:1231-1237.
TJ, Esser M, Fulkerson L. Osteotomy of the trochanter in open reduction
and internal fixation of acetabular fractures. J Bone Joint Surg Am
1987;69A:711-717.
GA, Willis, MC, Firoozbakhsh K, et al. Computed tomography image guided
surgery in complex acetabular fractures. Clin Orthop 2000;370:219-226.
RJ, Uwagie-Ero S, Lakatos RP, et al. Intramedullary nailing of femoral
shaft fractures. J Bone Joint Surg Am 1988;70A:1453-1462.
TA, Hughes MS, Anglen JO. Heterotopic ossification prophylaxis with
indomethacin increases the risk of long-bone nonunion. J Bone Joint
Surg Br 2003;85B:700-705.
TA, Lowry KJ, Anglen JO. Indomethacin compared with localized
irradiation for the prevention of heterotopic ossification following
surgical treatment of acetabular fractures. J Bone Joint Surg Am
2001;83A:1783-1788.
DL Jr, Mears DC, Kennedy WH, et al. Three-dimensional computed
tomography of acetabular fractures. Radiology 1985;155:183-185.
MS, Zych G, Latta L, et al. Computerized tomography evaluation of
stability in posterior fracture dislocations of the hip. Clinical
Orthop 1988;227:152-163.
DB, Moed BR, McCarroll K, et al. Accuracy of detecting screw
penetration of the acetabulum with intraoperative fluoroscopy and
computed tomography. J Bone Joint Surg Am 2001;83A:1370-1375.
JK, Gill SS, Zura RD, et al. Comparative strength of three methods of
fixation of transverse acetabular fractures. Clin Orthop
2001;392:433-441.
JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa
limited intrapelvic approach. Description of operative technique and
preliminary treatment results. Clin Orthop 1994;305:112-123.
G, O’Toole RO, Shanmuganathan K, et al. Computerized
tomographic-generated images improve diagnostic accuracy in acetabular
fractures and are adequate for planning surgical approach. Presented at
the 22nd Annual Meeting of the Orthopaedic Trauma Association, Phoenix,
AZ, October 5-7, 2006.
AC, Kahler DM. Closed reduction and percutaneous fixation of anterior
column acetabular fractures. Comput Aided Surg 2002;7:169-178.
SC, Reeves G, Key T, et al. Mortality in a cohort of women given x-ray
therapy for metropathia haemorrhagica. Int J Cancer 1994;56:793-801.
DB, Moed BR. Late salvage of failed open reduction and internal
fixation of posterior wall fractures of the acetabulum. J Orthop Trauma
2009;23:180-185.
Ridder VA, de Lange S, Popta JV. Anatomical variations of the lateral
femoral cutaneous nerve and the consequences for surgery. J Orthop
Trauma 1999;13:207-211.
RP Jr, Gardner MJ, Cunningham B, et al. Sciatic nerve entrapment in
associated both-column acetabular fractures: a report of 2 cases and
review of the literature. J Orthop Trauma 2009;23:80-83.
NA, Savolaine ER, Hoeflinger MJ, et al. Radiologic diagnosis of screw
penetration of the hip joint in acetabular fracture reconstruction. J
Orthop Trauma 1989;3:196-201.
TJ, Beck M. Trochanteric osteotomy for acetabular fractures and
proximal femur fractures. Orthop Clin North Am 2004;35:457-461.
R, Martin DP, Agel J, et al. Musculoskeletal function assessment:
reference values for patient and non-patient samples. J Orthop Res
1999;17:101-109.
R, Martin DP, Agel J, et al. Musculoskeletal Function Assessment
instrument: criterion and construct validity. J Orthop Res
1996;14:182-192.
N, Beck M, Rothenfluh DA, et al. Treatment of femoro-acetabular
impingement: preliminary results of labral refixation: Surgical
technique. J Bone Joint Surg Am 2007;89(suppl 2, pt 1):36-53.
PR, Swiontkowski MF, Kilroy AW, et al. Injury of the sciatic nerve
associated with acetabular fracture. J Bone Joint Surg Am
1993;75A:1157-1166.
SB, Sistrom C, Wang GJ, et al. Percutaneous screw fixation of
acetabular fractures with CT guidance: preliminary results of a new
technique. AJR Am J Roentgenol 1992; 158:819-822.
PV, Tzioupis CC, Moed BR. Two-level reconstruction of comminuted
posterior-wall fractures of the acetabulum. J Bone Joint Surg Br
2007;89B:503-509.
JT, Powell JN, Tile M. Lateral extension of the ilioinguinal incision
in the operative treatment of acetabular fractures. Injury
1995;26:207-212.
DY, White RH, Moreland LW, et al. Duodenal and gastric ulcer prevention
with misoprostol in arthritis patients taking NSAIDs: Misoprostol Study
Group. Ann Intern Med 1993;119:257-262.
T, Jacob AL, Messmer P, et al. Transverse acetabular fracture: hybrid
minimal access and percutaneous CT-navigated fixation. AJR Am J
Roentgenol 2004;183:1000-1002.
ML, Kennedy AS, Copeland CC, et al. Utility of radiation in the
prevention of heterotopic ossification following repair of traumatic
acetabular fracture. Int J Radiat Oncol Biol Phys 1999;45:461-466.
DJ, Olson SA, Matta JM. Diagnosis and management of closed internal
degloving injuries associated with pelvic and acetabular fractures: the
Morel-Lavallé lesion. J Trauma 1997;42:1046-1051.
MA, Althausen P, Kellam JF, et al. Simultaneous anterior and posterior
approaches for complex acetabular fractures. J Orthop Trauma
2008;22:494-497.
M, Oostvogel HJM, Klasen HJ. Conservative treatment of acetabular
fractures: the role of the weight-bearing dome and anatomic reduction
in the ultimate results. J Trauma 1987;27:555-559.
DL, Beck M, Gautier E, et al. Surgical techniques for acetabular
fractures. In: Tile M, Helfet DL, Kellam JF, eds. Fractures of the
Pelvis and Acetabulum. 3rd Ed. Philadelphia: Lippincott Williams &
Wilkins, 2003:533-603.
DL, Bartlett CS. Acetabular fractures: evaluation/classification
treatment concepts and approaches. In: Reudi TP, Murphy WM, eds. AO
Principals of Fracture Management. New York: Thieme, 2001:419-443.
DL, Bartlett CS, Malkani AL. Acetabular fractures: extended iliofemoral
approach. In: Wiss DA, ed. Master Techniques in Orthopaedic Surgery:
Fractures. Philadelphia: Lippincott-Raven, 1998:675-695.
DL, Anand N, Malkani AL, et al. Intraoperative monitoring of motor
pathways during operative fixation of acute acetabular fractures. J
Orthop Trauma 1997;11:2-6.
DL, Schmeling GJ. Management of complex acetabular fractures through
single nonextensile exposures. Clin Orthop 1994;305:58-68.
DL, Schmeling GJ. Somatosensory evoked potential monitoring in the
surgical treatment of acute, displaced acetabular fractures: results of
a prospective study. Clin Orthop 1994;301:213-220.
DL, Borrelli J Jr, DiPasquale T, et al. Stabilization of acetabular
fractures in elderly patients. J Bone Joint Surg Am 1992;74A:753-765.
EE, Kay RM, Dorey FJ. Heterotopic ossification prophylaxis following
operative treatment of acetabular fracture. Clin Orthop 1994;305:88-95.
EE, Matta JM, Mast JW, et al. Delayed reconstruction of acetabular
fractures 21-120 days following injury. Clin Orthop 1994;305:20-30.
R, Judet J, Letournel E. Fractures of the acetabulum. Classification
and surgical approaches for open reduction. J Bone Joint Surg Am
1964;46A:1615-1638.
FA, Bone LB, Border JR. Open reduction internal fixation of acetabular
fractures: Heterotopic ossification and other complications of
treatment. J Orthop Trauma 1991;5:439-445.
DM, DeGrange D, Wang G-J. Percutaneous fixation of selected acetabular
fractures using computed tomographic guidance. Orthop Transpl
1996;20:83.
JE, Brashear HR, Guilford WB. Stability of posterior fracture
dislocations of the hip: quantitative assessment using computed
tomography. J Bone Joint Surg Am 1988;70A:711-714.
HJ, Rozen N, Borkhoff CM, et al. Determinants of functional outcome
after simple and complex acetabular fractures involving the posterior
wall. J Bone Joint Surg Br 2006;88B:776-782.
PJ, Templeman D. Associated injuries complicating the management of
acetabular fractures: review and case studies. Orthop Clin North Am
2002;33:73-95.
CJ, Moed BR. Atypical anterior wall fracture of the acetabulum: case
series of anterior acetabular rim fracture without involvement of the
pelvic brim. J Orthop Trauma 2007;21:515-522.
R, Kotnis R, Al-Mousawi A, et al. Outcome of surgery for reconstruction
of fractures of the acetabulum. The time dependent effect of delay. J
Bone Joint Surg Br 2006;88B:1197-1203.
JL, Slongo TF, Agel J, et al. Fracture and dislocation classification
compendium: 2007. J Orthop Trauma 2007;21(10 suppl):S1-S163.
DP, Engelberg R, Agel J, et al. Development of a musculoskeletal
extremity health status instrument: the Musculoskeletal Function
Assessment instrument. J Orthop Res 1996;14:173-181.
J. Fractures of the acetabulum: accuracy of reduction and clinical
results in patients managed operatively within three weeks after the
injury. J Bone Joint Surg Am 1996;78A:1632-1645.
JM. Operative treatment of acetabular fractures through the
ilioinguinal approach. A 10-year perspective. Clin Orthop
1994;305:10-19.
JM, Letournel E, Browner BD. Surgical management of acetabular
fractures. In: Anderson LD, ed. Instructional Course Lectures, Volume
XXXV. St. Louis: Mosby, 1986:382-397.
JM, Siebenrock KA. Does indomethacin reduce heterotopic bone formation
after operations for acetabular fractures? A prospective randomised
study. J Bone Joint Surg Br 1997;79B:959-963.
KA. Open reduction and internal fixation of fractures of the
acetabulum. Results in 163 fractures. Clin Orthop 1994;305:31-37.
DC, Velyvis JH. Acute total hip arthroplasty for selected displaced
acetabular fractures: two to twelve-year results. J Bone Joint Surg Am
2002;84A:1-9.
ES, Sims SH, Kellam JF, et al. Incidence of sciatic nerve injury in
operatively treated acetabular fractures without somatosensory evoked
potential monitoring. J Orthop Trauma 1997;11:327-329.
BR. Acetabular fractures: the Kocher-Langenbeck approach. In: Wiss DA,
ed. Master Techniques in Orthopaedic Surgery: Fractures. 2nd Ed.
Philadelphia: Lippincott Williams & Wilkins, 2006:685-709.
BR. Posterior wall acetabular fractures: diagnosis, treatment, and
results. Retrieved February 23, 2009, from
http://www5.aaos.org/oko/description.cfm?topic=TRA026.
BR, Ajibade DA, Israel H: Computed tomography as a predictor of hip
stability status in posterior wall fractures of the acetabulum. J
Orthop Trauma 2009;23:7-15.
BR, Carr SEW, Gruson K, et al. Computed tomography assessment of
fractures of the posterior wall of the acetabulum after operative
treatment. J Bone Joint Surg Am 2003;85A:512-522.
BR, Carr SEW, Watson JT. Results of operative treatment of fractures of
the posterior wall of the acetabulum. J Bone Joint Surg Am
2002;84A:752-758.
BR, Israel H. Heterotopic ossification prevention and treatment: what
is the best way to prevent heterotopic ossification following
acetabular fracture fixation? In: Wright JG, ed. Evidence-Based
Orthopaedics. Philadelphia: Saunders Elsevier, 2009:353-359.
BR, Karges DE. Prophylactic indomethacin for the prevention of
heterotopic ossification after acetabular fracture surgery in high-risk
patients. J Orthop Trauma 1994;8:34-39.
BR, Letournel E. Low-dose irradiation and indomethacin prevent
heterotopic ossification after acetabular fracture surgery. J Bone
Joint Surg Br 1994;76B:895-900.
BR, Maxey JW. The effect of indomethacin on heterotopic ossification
following acetabular fracture surgery. J Orthop Trauma 1993;7:33-38.
BR, Maxey JW, Minster GJ. Intraoperative somatosensory evoked potential
monitoring of the sciatic nerve: an animal model. J Orthop Trauma
1992;6:59-65.
BR, McMichael JC. Outcomes of posterior wall fractures of the
acetabulum: Surgical technique. J Bone Joint Surg Am 2008;90A(suppl
1):87-107.
BR, Smith ST. Three-view radiographic assessment of heterotopic
ossification after acetabular fracture surgery. J Orthop Trauma
1996;10:93-98.
R, Routt M. Open reduction of intracapsular hip fractures using a
modified Smith-Petersen surgical exposure. J Orthop Trauma
2007;21:490-494.
KD, Goss K, Anglen JO. Indomethacin versus radiation therapy for
prophylaxis against heterotopic ossification in acetabular fractures: a
randomised, prospective study. J Bone Joint Surg Br 1998;80B:259-263.
KD, Potter HG, Helfet DL. The detection and management of proximal deep
vein thrombosis in patients with acute acetabular fractures: a
follow-up report. J Orthop Trauma 1997;11:330-336.
E, Garofalo R, Borens O, et al. Acute total hip arthroplasty for
acetabular fractures in the elderly: 11 patients followed for 2 years.
Acta Orthop Scand 2002;73:615-618.
BL, Hahn DH, Bosse MJ, et al. Intraoperative fluoroscopy to evaluate
fracture reduction and hardware placement during acetabular surgery. J
Orthop Trauma 1999;13:414-417.
SA, Matta JM. The computerized tomography subchondral arc: a new method
of assessing acetabular articular continuity after fracture (a
preliminary report). J Orthop Trauma 1993;7:402-413.
AA, Archdeacon MT, Jenkins MA, et al. Infrapectineal plating for
acetabular fractures: a technical adjunct to internal fixation. J
Orthop Trauma 2004;18:175-178.
CM, Bosse MJ, Poka A, et al. A modified extensile exposure for the
treatment of complex or malunited acetabular fractures. J Bone Joint
Surg Am 1988;70A:329-337.
RP, Matta JM. Unrecognized posterior dislocation of the hip associated
with transverse and T-type fractures of the acetabulum. J Orthop Trauma
1993;7:23-27.
FB, Shackford SR, Ricci MA, et al. Prophylactic vena cava filter
insertion in selected high-risk orthopaedic trauma patients. J Orthop
Trauma 1997;11:267-272.
ML Jr, Swiontkowski MF. Operative treatment of complex acetabular
fractures. Combined anterior and posterior exposures during the same
procedure. J Bone Joint Surg Am 1990;72A:897-904.
A, Alvisi A, Blasi A, et al. Misoprostol prevents NSAID-induced
gastroduodenal lesions in patients with osteoarthritis and rheumatoid
arthritis. Ital J Gastroent 1991; 23:119-123.
A, Teixeira PGR, DuBose J, et al. Predictors of positive angiography in
pelvic fractures: a prospective study. J Am Coll Surg 2008;207:656-662.
MB, Starr AJ, Reinert CM, et al. Percutaneous screw fixation of
acetabular fractures in elderly patients. Curr Opin Orthop
2006;17:17-24.
JM. Nonsteroidal anti-inflammatory drugs, aspirin, and gastrointestinal
prophylaxis: an ounce of prevention. Rev Gastroenterol Disord
2005;5(suppl 2):S39-S49.
GL, Sciulli R, Altman GT. Knee injury in patients experiencing a
high-energy traumatic ipsilateral hip dislocation. J Bone Joint Surg Am
2005;87A:1200-1204.
DM, Siboto GM. Posterior fracture dislocation of the hip joint: the
value of the obturator-oblique view with the hip still dislocated. J
Orthop Trauma 2002;16:374-378.
A, Broos P, Vanderschot P. Total hip replacement for acetabular
fractures. Results in 121 patients operated between 1983 and 2003.
Injury 2008;39:914-921.
KA, Gautier E, Ziran BH, et al. Trochanteric flip osteotomy for cranial
extension and muscle protection in acetabular fracture fixation using
the Kocher-Langenbeck approach. J Orthop Trauma 1998;12:387-391.
PT, Routt ML Jr, Harrington RM, et al. The acetabular T-type fracture.
A biomechanical evaluation of internal fixation. Clin Orthop
1995;314:234-240.
JP, LopezBen RR, Volgas DA, et al. Prophylaxis against deep-vein
thrombosis following trauma: a prospective, randomized comparison of
mechanical and pharmacologic prophylaxis. J Bone Joint Surg Am
2006;88A:261-266.
JP, Singhania AK, LopezBen RR. et al. Deep-vein thrombosis in
high-energy skeletal trauma despite thromboprophylaxis. J Bone Joint
Surg Br 2005;87B:965-968.
AS, Moed BR: Acetabular fractures: definitive treatment and expected
outcomes. In: Baumgaertner MR, Tornetta PIII, eds. Orthopaedic
Knowledge Update Trauma 3. Rosemont, IL: American Academy of
Orthopaedic Surgeons, 2005:271-280.
AJ, Jones AL, Reinert CM, et al. Preliminary results and complications
following limited open reduction and percutaneous screw fixation of
displaced fractures of the acetabulum. Injury 2001;32(suppl 1):45-50.
AJ, Reinert CM, Jones AL. Percutaneous fixation of columns of the
acetabulum: a new technique. J Orthop Trauma 1998;12:51-58.
AJ, Watson JT, Reinert CM, et al. Complications following the “T
extensile” approach: a modified extensile approach for acetabular
fracture surgery—report of forty-three patients. J Orthop Trauma
2002;16:535-542.
MF, Buckwalter JA, Keller RB, et al. The outcomes movement in
orthopaedic surgery: where we are and where we should go. J Bone Joint
Surg Am 1999; 81A:732-740.
R, Mast A, Coats A. Comparison of Judet radiographs to CT-reconstructed
Judet images for the diagnosis of acetabular fractures. Presented at
the 22nd Annual Meeting of the Orthopaedic Trauma Association, Phoenix,
AZ, October 5-7, 2006.
DC, Olson S, Moed BR, et al. Surgical treatment of acetabular
fractures. In: Zuckerman JD, ed. Instructional Course Lectures, Vol.
48. Rosemont, IL: AAOS, 1999:481-496.
J, Blomfeldt R, Ponzer S, et al. Primary total hip arthroplasty with a
Burch-Schneider antiprotrusion cage and autologous bone grafting for
acetabular fractures in elderly patients. J Orthop Trauma
2003;17:193-197.
P III: Nonoperative management of acetabular fractures: the use of
dynamic stress views. J Bone Joint Surg Br 1999;81B:67-70.
JC, Hurwitz S, Wiesel SW. Posterior acetabular fracture dislocations:
fragment size, joint capsule, and stability. J Trauma 1989;29:1494-1496.
MS, Widding KK, Thomas KA. The effects of simulated transverse,
anterior column, and posterior column fractures of the acetabulum on
the stability of the hip joint. J Bone Joint Surg Am 1999;81A:966-974.
M, Gordon RG, Mears DC, et al. Intraoperative somatosensory evoked
potential monitoring of pelvic and acetabular fractures. J Orthop
Trauma 1992;6:50-58.
RA, Hansen ST Jr, Clawson DK. Closed intramedullary nailing of femoral
fractures. A report of five hundred and twenty cases. J Bone Joint Surg
Am 1984;66A:529-539.
DA, Brien WW, Stetson WB: Interlocked nailing for treatment of
segmental fractures of the femur. J Bone Joint Surg Am 1990;72A:724-728.
DA, Fleming CH, Matta JM, et al. Comminuted and rotationally unstable
fractures of the femur treated with interlocking nail. Clin Orthop
1986;212:35-47.
R, Barrett K, Christie MJ, et al. Acetabular fractures: long-term
follow-up of open reduction and internal fixation. J Orthop Trauma
1994;8:397-403.
