Lumbar Spine Anatomy and Examination
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Lumbar Spine Anatomy and Examination
Lumbar Spine Anatomy and Examination
Rohit Robert Dhir BA
A. Jay Khanna MD
Description
-
The spine is a complex system composed of
bony elements, articulations, ligaments, muscles, spinal cord, and
peripheral nerves divided into anterior, middle, and posterior columns. -
The vertebral body, lamina, and the spinous process protect the spinal cord.
-
The lumbar spine (Fig. 1) contains 5 vertebrae and 5 nerve roots.
-
Most lumbar spines have a lordotic secondary curvature acquired when an infant begins walking (1).
-
The defining characteristics of the
lumbar spine include a substantially large, kidney-shaped vertebral
body, long and slender transverse processes (with accessory processes
on the posterior base), and short and sturdy spinous processes (1).
-
-
The thick intervertebral discs, large articular surfaces, and the lack of rib attachments give the lumbar spine a wide ROM.
-
This freedom of motion allows for lumbar flexion, extension, lateral bending, and trunk rotation.
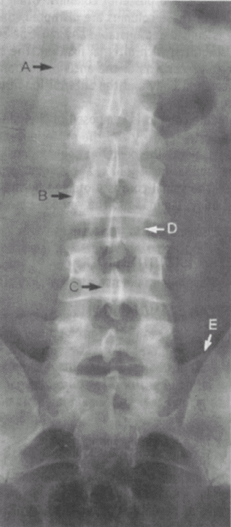 Fig. 1. Roentgenogram of normal lumbosacral spine. A: Transverse process. B: Pedicle. C: Posterior spinous process. D: Lamina. E: Sacrum. (From Steinberg GG, Akins CM, Baran DT. Orthopaedics in Primary Care, 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 1999, with permission.)
Fig. 1. Roentgenogram of normal lumbosacral spine. A: Transverse process. B: Pedicle. C: Posterior spinous process. D: Lamina. E: Sacrum. (From Steinberg GG, Akins CM, Baran DT. Orthopaedics in Primary Care, 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 1999, with permission.) -
The lumbar spine also functions to
support the lumbosacral nerve roots (cauda equina), transmit weight to
the pelvis and legs, and support the upper body.
-
Signs and Symptoms
Physical Exam
-
Gait: Look for:
-
Antalgic (painful) gait
-
Muscle wasting and weakness
-
Signs of hip or knee problems
-
Trendelenburg sign (abductor weakness with an ipsilateral pelvic tilt when the leg is lifted off the ground)
-
-
Inspection:
-
As the patient disrobes, pay attention to fluidity of motion and any associated pain.
-
Inspect the back for clues to underlying
bone or neurologic pathology: Areas of redness, hair patches,
birthmarks, or skin markings such as café-au-lait spots (2). -
Analyze the patient’s posture and inspect the curvature of the lumbar spine.
-
A slight lordotic curve is normal, but
normal lordosis can be absent in cases of paravertebral muscle spasm,
and occasionally an extreme kyphosis (Gibbus deformity) is present.-
A weak anterior abdominal wall generally leads to an exaggerated lordosis (2).
-
-
Structural scoliosis:
-
A patient’s tendency to favor 1 side while standing may indicate structural scoliosis (2), which is characterized by a fixed curve and no change with flexion or recumbency.
-
-
Sciatic scoliosis:
-
Characterized by a more diffuse curve that worsens with flexion and by limited flexion that disappears with recumbency
-
-
Spondylolisthesis:
-
A palpable “step” from 1 spinous process to another may indicate spondylolisthesis.
-
May also present with segmental tenderness or nerve root injury (2)
-
-
NF:
-
May impinge on the spinal cord and roots
-
Often accompanied by café-au-lait spots (2)
-
-
Spina bifida:
-
Absence of spinous processes, along with birthmarks, excessive port wine marks, or a tuft of hair, may indicate spina bifida (2).
-
-
AS:
-
Usually begins with pain and stiffness in
the SI joints, spreads to the spine, and eventually leads to the
ossification of spinal ligaments; eventually, the spine may fuse.
-
-
-
Palpation:
-
Bony (anterior):
-
Vertebral body and disc: L4, L5, S1 (abdominal palpation: below aortic bifurcation)
-
Sacral promontory: L5–S1 (abdominal palpation through the linea alba below the umbilicus)
-
-
Bony (posterior):
-
Spinous processes of the lumbar region
-
Spinous processes of the sacral region
-
Iliac crest: L4–L5
-
Posterior superior iliac spine: S2
-
-
Soft tissue
-
-
ROM evaluation:
-
Substantial motion in the lumbar spine
-
Motion between L5–S1 >motion between L1–L2
-
Flexion:
-
Anterior longitudinal ligament relaxes as
the supraspinous and interspinous ligaments, ligamentum flavum, and
posterior longitudinal ligament stretch (2).
-
-
Extension:
-
Posterior ligaments relax as the anterior longitudinal ligament stretches (2).
-
-
Lateral bending
-
Rotation
-
Resisted movement tests of flexion, lateral bending, and rotation (3)
-
Passive movement tests:
-
Conduct when a patient does not have full ROM.
-
Do not test for passive flexion because of possible aggravation of a disc herniation.
-
-
Root irritation from disc herniation: Deviation to painful side with spine flexion
-
-
Waddell signs: 3 of the following 5 signs indicate a malingering patient (2):
-
Nonanatomic superficial tenderness
-
Simulation tests (pain with axial loading or rotation of the spine)
-
Nonanatomic weakness and sensory findings
-
Overreaction: “Cogwheeling” or jerky muscle relaxation
-
Inappropriate response to provocative maneuvers with distraction (i.e., supine versus seated straight-leg-raise test)
-
-
Rectal examination checks for:
-
Tone
-
Volition
-
Anal wink (stroke perianal skin, feel anal sphincter contraction around finger)
-
Bulbocavernosus maneuver: Signals end of
spinal shock (Pull on Foley catheter in urethra or pull on glans penis;
feel anal wink.) -
Light touch and pin-prick perianal
sensation: S2–S4 (If sensation is absent, a mass lesion such as a disc
or tumor may be pressing on the nerve roots.)Table 1 Motor Examination of the Lumber SpineRoot Muscle Group Action T12, L1–L3 Iliopsoas Hip flexion L2–L4 Quadriceps Knee extension L4 Tibialis anterior Foot dorsiflexion L5 Extensor hallucis longus Big toe extension S1 Gastrocnemius Foot plantarflexion
-
-
Upper motor neuron disorders:
-
Hoffman sign:
-
Nip the nail of the patient’s middle finger.
-
A positive reaction produces flexion of the terminal phalanx of the thumb and of the 2nd and 3rd phalanx of another finger.
-
-
Babinski sign:
-
Stroke the plantar lateral foot.
-
A positive test (extended great toe while other toes plantarflex and splay) indicates an upper motor neuron lesion.
-
Use to rule out cervical or thoracic myelopathy (2).
-
-
Loss of any of the superficial reflexes,
such as the abdominal, cremasteric, or anal reflex, suggests an upper
motor neuron lesion. -
Sustained clonus of the patellar or Achilles reflex or hyperreflexia indicates an upper motor neuron lesion (4).
-
P.237
Tests
-
Motor examination (Table 1):
-
Systematically examines the nerve roots
-
Muscle wasting and weakness suggests nerve root compression.
-
-
Reflex tests (Table 2):
-
Loss of the patellar or Achilles reflex suggests ipsilateral nerve root compression.Table 2 Reflex Tests of the Lumbar Spine
Disc Root Reflex Muscles L3–L4 L4 Patellar reflex Anterior tibialis L5–S1 S1 Achilles reflex Peroneus longus and brevis Table 3 Sensation Tests of the Lumbar SpineNerve Root Area of Skin Innervation L–1 Groin, upper anterior thigh, posteromedial leg L–2 Anterior mid-thigh; lateral groin L–3 Anterior thigh above knee cap, posterolateral lower leg L–4 Anteromedial shin L–5 Dorsum of foot, anterior aspect lower leg S–1 Lateral foot S2–S5 Perianal
-
-
Sensation tests (Table 3):
-
Pin-prick testing compares 2-point discriminatory sensibility on the lower extremities.
-
Vibration sensibility and temperature sense also are tested.
-
-
Nerve root tension tests:
-
Straight-leg-raise test:
-
Raise the leg of the supine patient slowly by supporting the foot slightly above the malleoli and keeping the knee extended (2).
-
Differentiating radiculopathy from tight hamstring pain is important (3).
-
This procedure reproduces the
sciatic-type radicular leg pain that is relieved when the knee is bent
and is exacerbated by foot dorsiflexion. -
Cross-leg straight-leg-raise test is less
sensitive than the straight-leg-raise test but a more specific physical
examination finding for lumbar disc herniation (5). -
A positive test (flexion of 1 leg with
pain in the contralateral leg or buttocks [5]) suggests disc herniation
axillary or medial to the root.
-
-
Femoral nerve stretch test:
-
The patient is prone, and the hip is extended with the knee slightly flexed.
-
Pain radiating down the front of the thigh indicates L3–L4 nerve root irritation.
-
-
Patrick (FABER) test:
-
Test the SI joint by Flexing, ABducting, and Externally Rotating the hip to reproduce SI joint pain.
-
Pain usually is associated with pelvic trauma or infectious disease (2).
-
-
-
Muscle strength grading:
-
5: Normal strength
-
4: Weakness with resistance, full movement against gravity
-
3: Full ROM against gravity but marked weakness against resistance
-
2: Full ROM with gravity eliminated
-
1: Flicker of tendon unit
-
0: No movement
-
Imaging
-
Imaging confirms or supports the diagnosis of disorders suspected from the history and physical examination.
-
Radiographs should show normal alignment of the vertebrae, the presence of bony landmarks, and maintenance of the disc spaces.
-
False-positive MRI scans occur in 35% of patients <40 years old and in 93% of patients >60 years old (6).
-
SPECT is more sensitive in detecting
isthmic spondylolisthesis than technetium-99m methylene diphosphonate
bone scintigraphy, and plain radiographs (7).
References
1. Moore KL, Agur AMR. Back. In: Essential Clinical Anatomy. Philadelphia: Lippincott Williams & Wilkins, 2002:275–313.
2. Hoppenfeld
S. Physical examination of the lumbar spine. In: Physical Examination
of the Spine and Extremities. Norwalk, CT: Appleton-Century–Crofts,
1976:237–263.
S. Physical examination of the lumbar spine. In: Physical Examination
of the Spine and Extremities. Norwalk, CT: Appleton-Century–Crofts,
1976:237–263.
3. Albert
TJ, Vaccaro AR. Physical examination of the lumbosacral spine. In:
Physical Examination of the Spine. New York: Thieme, 2005:89–121.
TJ, Vaccaro AR. Physical examination of the lumbosacral spine. In:
Physical Examination of the Spine. New York: Thieme, 2005:89–121.
4. Kahanovitz N. Physical examination. In: Diagnosis and Treatment of Low Back Pain. New York: Raven Press, 1991:31–42.
5. Engstrom
JW. Back and neck pain. In: Kasper DL, Fauci AS, Longo DL, et al., eds.
Harrison’s Principles of Internal Medicine, 16th ed. McGraw-Hill
Medical Publishing Division, 2005: 94–104.
JW. Back and neck pain. In: Kasper DL, Fauci AS, Longo DL, et al., eds.
Harrison’s Principles of Internal Medicine, 16th ed. McGraw-Hill
Medical Publishing Division, 2005: 94–104.
6. Boden
SD, McCowin PR, Davis DO, et al. Abnormal magnetic-resonance scans of
the cervical spine in asymptomatic subjects. A prospective
investigation. J Bone Joint Surg 1990;72A:1178–1184.
SD, McCowin PR, Davis DO, et al. Abnormal magnetic-resonance scans of
the cervical spine in asymptomatic subjects. A prospective
investigation. J Bone Joint Surg 1990;72A:1178–1184.
7. Logroscino G, Mazza O, Aulisa AG, et al. Spondylolysis and spondylolisthesis in the pediatric and adolescent population. Childs Nerv Syst 2001;17:644–655.
Additional Reading
McCulloch J, Transfeldt E. Musculoskeletal and neuroanatomy of the lumbar spine. In: Macnab’s Backache, 3rd ed. Baltimore: Williams & Wilkins, 1997:1–74.
FAQ
Q: Which reflex evaluates the L5 nerve root?
A:
No reflex exists for L5. The patellar reflex evaluates the L4 nerve
root, and the Achilles reflex evaluates the S1 nerve root.
No reflex exists for L5. The patellar reflex evaluates the L4 nerve
root, and the Achilles reflex evaluates the S1 nerve root.
Q:
Which test is more specific for a lumbar disc herniation at the L4–L5
level: the straight-leg-raise test or the contralateral
straight-leg-raise test?
Which test is more specific for a lumbar disc herniation at the L4–L5
level: the straight-leg-raise test or the contralateral
straight-leg-raise test?
A: The contralateral straight-leg-raise test.
