CHAPTER 50 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 50 – Combined Anterior Cruciate Ligament and Meniscal Allograft Transplantation
Jon K. Sekiya, MD
The menisci play a vital role in maintaining normal knee function. Shock absorption, stabilization, lubrication of the knee joint, proprioception, and load sharing are important functions of these cartilaginous structures. It has been demonstrated that significant joint changes follow complete or subtotal meniscectomies, and for this reason, many techniques to repair the menisci have been devised. Unfortunately, preservation of the meniscus cannot always be accomplished, and partial or total meniscectomy may be required.
The medial meniscus is an important secondary stabilizer to anterior-posterior knee translation. In the anterior cruciate ligament (ACL)–deficient knee, the medial meniscus takes on an even larger role in preventing excessive laxity. Results after ACL reconstruction in patients with deficient medial menisci are usually worse than when the meniscus is intact. Given these findings, meniscal allograft transplantation with concomitant ACL reconstruction has been performed to provide patients with a more stable knee as well as a mechanism to delay the arthritic process. This chapter outlines the senior author’s preferred technique for meniscal transplantation and concomitant ACL reconstruction in patients with combined deficiencies.
It is paramount to elicit a complete history. This includes any initial injury that may have occurred, prior treatments for the injury, activity restrictions imposed by the injury, and the patient’s expectations of treatment. Any previous arthroscopic pictures or operative reports that may be available are helpful and may obviate the need for a staging diagnostic arthroscopy.
A comprehensive physical examination is undertaken to evaluate the patient’s stance, gait pattern, and ability to squat. The overall lower extremity alignment is observed and compared with the contralateral extremity. Joint line palpation, results of the McMurray test, range of motion, and degree of quadriceps atrophy are documented. The presence of an effusion is assessed, and the ligamentous evaluation is performed to evaluate the integrity of the ACL (Lachman, pivot shift, and anterior drawer tests). An anterior drawer examination with as much anterior translation as in the Lachman test is suggestive of the loss of secondary stabilization from the posterior horn of the medial meniscus and is indicative of symptomatic medial meniscus deficiency that is compounding ACL laxity. Any prior surgical incisions are documented because these may affect surgical planning.
| • | Joint line pain; pain with squatting | |
| • | Effusion | |
| • | Full, symmetric knee range of motion | |
| • | 2+ Lachman test score, 2+ pivot shift test score, 2+ anterior drawer test score |
Magnetic Resonance Imaging (with or without Contrast Enhancement)
Other imaging modalities, such as computed tomography and technetium bone scans, may be used to assess rotational alignment (computed tomography) or any degenerative changes not visualized on initial screening radiographs (bone scan).
Indications and Contraindications
The ideal candidate undergoing concomitant ACL reconstruction and meniscal transplantation is a young patient with meniscus deficiency and full knee range of motion, pain localized to the affected joint compartment, symptoms of persistent instability, prior failed ACL surgery (particularly with medial meniscus deficiency), cartilage surfaces that are relatively intact (grade I-II, preferably confined to the meniscal weight-bearing region), and no evidence of malalignment on long-cassette radiographs. If patients are found to have malalignment (weight-bearing line falls through the affected compartment), we prefer an osteotomy to realign the weight-bearing axis through the unaffected compartment and perform a staged reconstruction (
Fig. 50-1
).
|
|
|
|
Figure 50-1 |
Contraindications to the performance of this procedure are inflammatory arthritis, history of previous infection, evidence of severe degenerative changes (either arthroscopic or radiographic), body mass index above 35, and unwillingness of the patient to cooperate with a comprehensive rehabilitation program.
Correct sizing of the meniscal allograft is critical for healing. We obtain measurements from the preoperative posteroanterior and lateral radiographs after they have been corrected for magnification. This sizing technique is similar to that of Pollard and colleagues.[10] This size is then given to the tissue bank, and an isotropic graft (graft matched for right or left knee and for medial or lateral compartment) is obtained. All meniscal allografts are sterilely harvested and fresh-frozen. None of the grafts are irradiated before transplantation.
Anterior Cruciate Ligament Allograft
For ACL reconstruction with concomitant meniscal transplantation, we prefer to use a bone–patellar tendon–bone allograft. All of our bone–patellar tendon–bone allografts are fresh-frozen and irradiated before use. We have found that use of an allograft in this setting minimizes postoperative donor site pain and can hasten the recovery of the quadriceps after surgery. Another outstanding allograft option is a tibialis anterior tendon.
Our preferred technique uses a lower extremity sciatic and femoral nerve block to assist with postoperative analgesia. Typically, the patient is also given general anesthesia (or regional if general is contraindicated) and positioned supine on a regular operating room table. A thigh tourniquet is applied as well as a lateral post just below the level of the greater trochanter. A bump is taped to the bed that will position the leg at approximately 70 degrees of knee flexion. The table is lowered to its lowest level, and once the extremity is sterilely prepared, a bump is placed between the lateral post and the thigh with the knee flexed 70 degrees on the table.
Surgical Landmarks, Incisions, and Portals
| • | Borders of the patellar tendon | |
| • | Medial-lateral joint line | |
| • | Fibular head | |
| • | Tibial tubercle and proximal medial border of the tibia |
| • | Lateral collateral ligament, peroneal nerve (lateral approach) | |
| • | Medial collateral ligament, saphenous nerve (medial approach) |
Examination Under Anesthesia and Diagnostic Arthroscopy
A thorough examination under anesthesia is performed to document anteromedial rotatory instability (in cases of medial meniscus deficiency) as well as anterior laxity (pivot shift test, Lachman test, anterior drawer test).
Diagnostic arthroscopy is performed to evaluate for other intraarticular disease as well as to critically assess the remaining meniscal rim available for placement of sutures.
Specific Steps (
Box 50-1
)
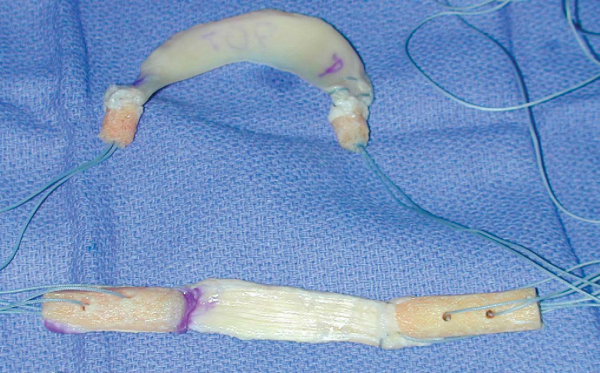
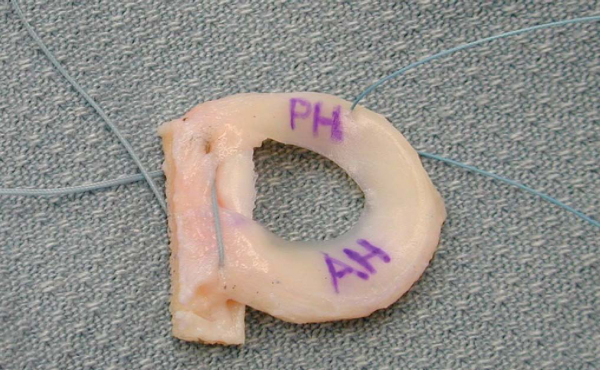
Once the diagnosis is confirmed, the allografts are thawed and washed with antibiotic solution according to the vendor’s guidelines. The patellar tendon allograft is prepared so that each bone plug measures 10 mm in diameter and 30 mm in length. All loose tissue is débrided from the tendon, and two drill holes are placed within each plug, through which No. 5 braided, nonabsorbable sutures are placed to assist with graft passage. With the meniscus allograft, a rim of the outer portion is trimmed to provide a fresh surface for repair and subsequent healing. An 8- to 9-mm diameter (5-mm length) bone plug (medial meniscus) for the anterior horn is prepared and secured with No. 5 braided, nonabsorbable suture. The posterior horn bone plug is then prepared and secured in a similar fashion. In the posteromedial corner of the medial meniscus allograft, one No. 2 braided, nonabsorbable suture is placed within the rim to assist with graft passage and fixation to the posteromedial capsule and posterior oblique ligament. For the lateral meniscus, we use a bone bridge (8 or 9 mm) secured with two No. 5 braided, nonabsorbable sutures through drill holes corresponding to the lengths made within the trough. In the posterolateral corner of the meniscus, we place a No. 2 braided, nonabsorbable suture through the rim to assist with graft passage (Figs. 50-2 and 50-3 [2] [3]).
|
|
|
|
Figure 50-2 |
|
|
|
|
Figure 50-3 |
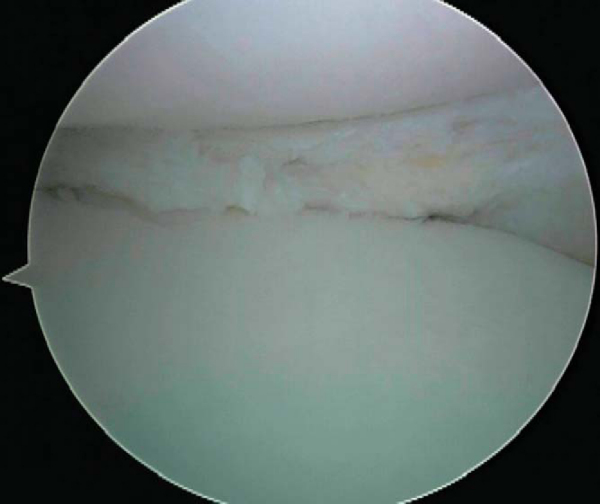
2. Preparation of Meniscal Rim
The involved posterior horns of the native menisci are trimmed to provide a bleeding surface that will support allograft healing. We prefer a 1- to 2-mm rim because this gives the sutures a more stable platform to fix the allograft. The anterior and posterior horn attachments are identified and marked. Care should be taken to maintain these anatomic landmarks (when available) because they help configure tunnel placement (
Fig. 50-4
).
|
|
|
|
Figure 50-4 |
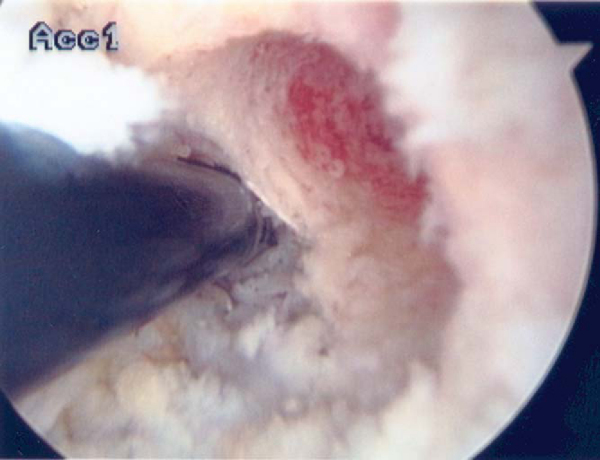
3. Tunnel Drilling for the ACL
A notchplasty is usually not necessary in our experience. For tibial guide pin placement, the tibial insertion of the ACL is identified at the intersection of the posterior border of the anterior horn of the lateral meniscus and the posterior third of the ACL stump. The ACL guide is set to 50 to 55 degrees and drilled to 10 mm. The dilators can be used to assess for the presence of any graft impingement when it is viewed arthroscopically. Extreme caution must be taken with this tibial ACL tunnel in conjunction with the trough used for lateral meniscus transplantation; these often communicate with each other, and so care must be taken in passing and securing either graft in place.
Next, attention is directed to preparation of the femoral ACL tunnel. The over-the-top position is identified at the 10-o’clock position (right knee). A 30-degree Steadman awl brought through the medial portal can be used to mark the insertion site (approximately 6 mm from the back wall, providing a 1-mm back wall after tunnel drilling;
Fig. 50-5
). We prefer drilling transtibially through the tunnel if we are able to get down the face of the femur to 10-o’clock and posterior. If we are unable to do this, with the knee flexed to approximately 115 degrees, a pin is tapped into place at the femoral insertion site through the medial portal. A 10-mm acorn drill bit is then run over the pin to a depth of 40 mm, if possible. This allows us to pull the bone-tendon-bone allograft deeper into the femoral tunnel if the tibial bone plug is too long and protruding from the tibial tunnel.
|
|
|
|
Figure 50-5 |
4. Slot Preparation (Lateral Meniscus) or Bone Plug Preparation (Medial Meniscus)
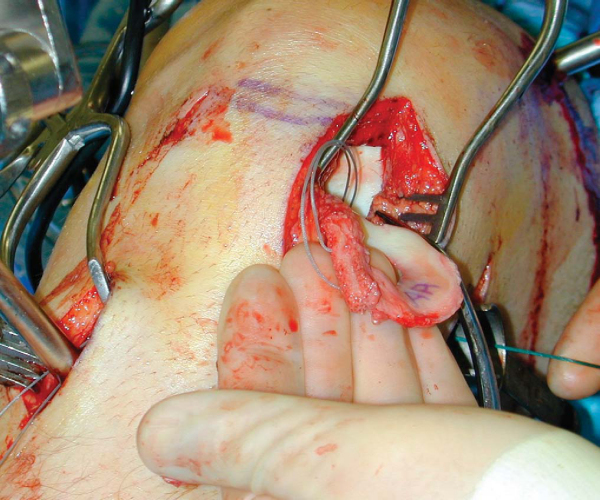
Once attention is turned to preparation of the meniscus, a femoral distractor is placed on the extremity. The joint is slightly distended so that the surgery can easily be accomplished at 70 degrees of knee flexion (
Fig. 50-6
).
|
|
|
|
Figure 50-6 |
For the lateral meniscus, we prefer a bridge and slot technique. A trough is first made in the medial aspect of the lateral tibial plateau to accept the allograft bone bridge (
Fig. 50-7
). A 1/4-inch curved osteotome is brought through the medial portal with the curve facing medially, hugging the lateral aspect of the tibial insertion of the ACL. A cut is made, making sure to keep the trough in the sagittal plane. A second cut is then made with the osteotome, lateral and parallel to the first cut. The bridging bone is then removed, and prefabricated gouges are used to finish the trough (total diameter of 8 to 9 mm). An ACL drill guide is then used to make two holes in the trough, spaced approximately 10 mm apart on the tibial surface for later fixation of the meniscal allograft. Two Hewson suture passers are placed within these holes to facilitate later graft passage.
|
|
|
|
Figure 50-7 |
For the medial meniscus, we prefer a bone plug technique for anterior and posterior horn fixation. The anterior tunnel for the anterior bone plug is drilled with the assistance of an ACL guide at the anatomic insertion of the anterior horn of the medial meniscus. Visualization is greatly aided with the use of the femoral distractor. The guide is brought through the lateral portal, and a guide pin is placed in the anatomic posterior horn of the medial meniscus and then overdrilled by 1 mm of whatever the bone plug diameter is with an acorn reamer (
Fig. 50-8
). The anterior horn can usually be made through the anteromedial arthrotomy; a blind tunnel is drilled in the anatomic insertion of the anterior horn, which is then connected to the anteromedial tibial metaphysis with a 2.0 drill. Special care needs to be taken to avoid communication of the meniscus horn tunnels and the tibial ACL tunnel during preparation.
|
|
|
|
Figure 50-8 |
Before the passage and fixation of the meniscal allograft, the ACL is passed in a retrograde fashion with the assistance of a Beath pin and suture loop. If the medial portal technique is used for femoral tunnel preparation, the Beath pin is first sent through the medial portal, up the femoral tunnel, and exits the lateral aspect of the thigh. The suture loop attached to the Beath pin is brought into the joint, and a suture grasper is used to grab it from the tibial tunnel. The sutures attached to the allograft bone plugs are then shuttled through the tibial and femoral tunnels, and the graft is secured in place. The femoral side of the graft is then fixed with a metal interference screw. The tibial bone plug is not fixed until the meniscus transplantation is completed.
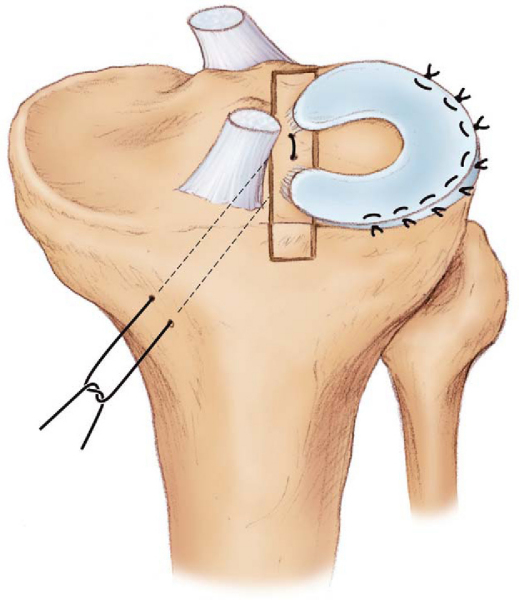
Lateral meniscus: A small lateral parapatellar arthrotomy is made in line with the previous lateral portal. Four No. 0 braided, nonabsorbable sutures are then placed in the anterior rim of the lateral meniscal remnant for later use in fixation of the anterior horn. A small posterolateral incision is made, centered over the posterior border of the lateral collateral ligament. The interval between the iliotibial band and the biceps is incised toward Gerdy’s tubercle. The posterolateral joint capsule is then exposed between the interval consisting of the lateral collateral ligament anteriorly and the gastrocnemius posteriorly. The anterior and posterior sutures of the bone bridge are threaded through the Hewson suture passers and pulled into the tunnels. The posterolateral passing suture is shuttled through the posterolateral incision and the meniscus allograft is brought into the joint, with care taken not to tangle the sutures (
Fig. 50-9
). Arthroscopic visualization then confirms that the bone bridge is in correct position, and the sutures are tied down on the medial aspect of the tibia over a 10-mm cortical bridge.
|
|
|
|
Figure 50-9 |
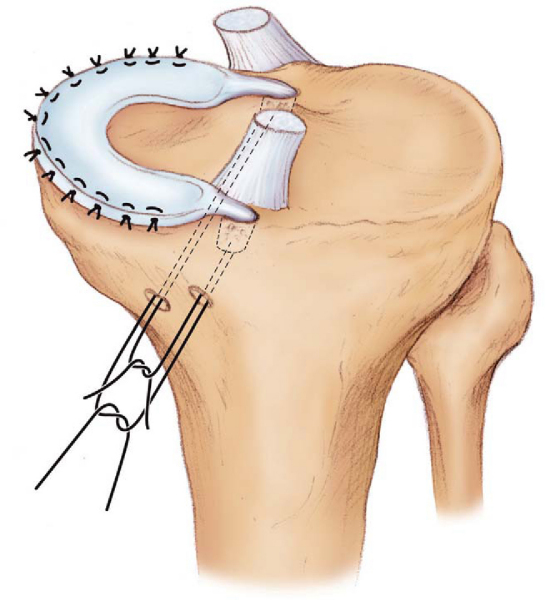
Medial meniscus: A small medial parapatellar arthrotomy is made in line with the medial portal. As for the lateral meniscus insertion, four nonabsorbable sutures are placed within the anterior horn remnant. A small posteromedial incision is then made, centered over the posterior border of the medial collateral ligament. The sartorius fascia is incised, and the interval between the semimembranosus and the medial gastrocnemius is developed, exposing the posteromedial joint capsule. This exposure will be used for inside-out meniscus repair suture techniques.
The posterior horn of the meniscus allograft is delivered through the anteromedial arthrotomy and pulled into the posterior horn tunnel. The posteromedial traction suture is used to reduce the posterior horn into the medial compartment. The posterior bone plug and sutures are pulled into their drill holes by a similar technique, and the allograft is reduced into the medial compartment (
Fig. 50-10
). Once reduction has been achieved, the sutures are tied on the lateral tibial metaphysis over a cortical bridge.
|
|
|
|
Figure 50-10 |
Lateral meniscus: The meniscal allograft is secured by arthroscopic inside-out techniques through the lateral incision. Care is taken to not fix the popliteus tendon to the meniscus during fixation. Once all of the posterior horn and body sutures have been passed, the anterior horn is secured with the nonabsorbable sutures that had been placed in the meniscal remnant. This is achieved at 70 degrees of knee flexion. Fixation of the remaining sutures is performed at 30 degrees of knee flexion after the ACL has been fixed on the tibial side (
Fig. 50-11
).
Medial meniscus: The meniscal allograft is secured by arthroscopic inside-out techniques through the posteromedial incision. The anterior horn is secured in a fashion similar to that of the lateral meniscus, and the remaining meniscus is fixed by arthroscopic inside-out techniques. Final fixation of the sutures is performed at 30 degrees of knee flexion after the ACL has been fixed on the tibial side (
Fig. 50-12
).
ACL: The ACL is fixed on the tibial surface with a metal interference screw as the knee is slightly flexed (15 degrees) and a slight posterior drawer force is applied.
Standard closure is performed for the arthrotomy and all accessory incisions.
The patient is admitted for an overnight stay in the hospital and returns to the office 6 to 8 days after the procedure for radiographs and wound observation.
| • | Patients are partial weight bearing on the affected extremity in a hinged knee brace and progress to weight bearing as tolerated during 4 weeks. | |
| • | Continuous passive motion is begun 24 hours after surgery, as are quadriceps sets, heel slides, and straight-leg raises. | |
| • | Range-of-motion goals: full extension within 1 week; 90 degrees of flexion in 4 to 6 weeks. | |
| • | Crutches are discontinued after 4 weeks. | |
| • | Rehabilitation continues for 2 to 3 months with an emphasis on restoration of full knee motion, stability, and strength. | |
| • | Low-impact aerobic activity is permitted at 8 weeks. | |
| • | Running is permitted after 5 to 6 months | |
| • | Light and moderate sports begin at 6 to 9 months. | |
| • | Strenuous sport is not recommended indefinitely. |
| • | Infection | |
| • | Arthrofibrosis | |
| • | Incomplete healing or recurrent tears of the implanted meniscus | |
| • | Neurovascular injury (saphenous or peroneal nerve) |
| PEARLS AND PITFALLS | ||||||||||||||||||||||||||||||
|
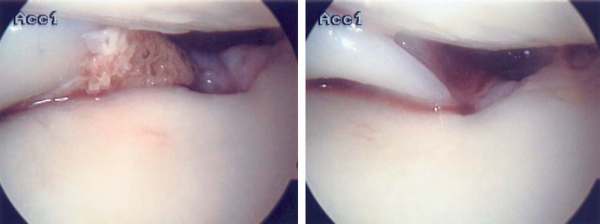
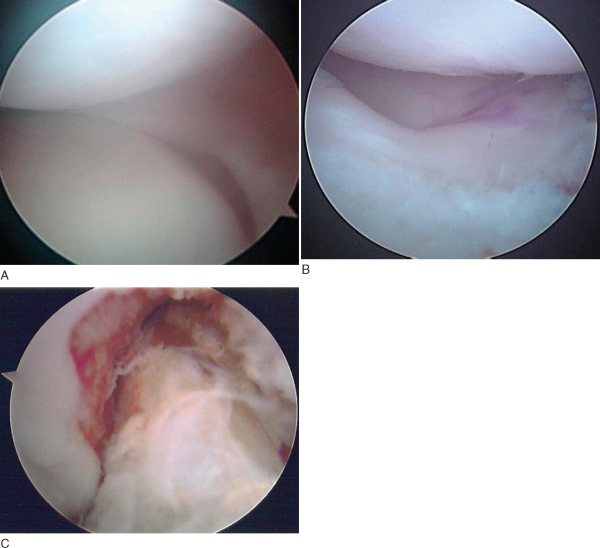
After combined ACL and meniscal transplantation surgery, good results are achieved in nearly 85% of patients (
Fig. 50-13
). The senior author’s results are presented in
Table 50-1
. Other authors’ results of meniscus transplantation are presented elsewhere in this book and referenced.
|
|
|
|
Figure 50-13 |
| Author | Study | Followup | Outcome |
|---|---|---|---|
| Sekiya et al[16] (2006) | Lateral meniscus transplantation | 3.3 years | 79% normal IKDC score |
| Graf et al[6] (2004) | ACL–medial meniscus transplantation | 8.5 years | 7/8 normal IKDC score |
| Sekiya et al[15] (2003) | ACL–meniscus transplantation | 2.8 years | 86%-90% normal IKDC score |
| Yoldas et al[21] (2003) | ACL–meniscus transplantation | 2.2 years | 95% normal IKDC score |