CHAPTER 46 –
Cole & Sekiya: Surgical Techniques of the Shoulder, Elbow and Knee in Sports Medicine, 1st ed.
Copyright ©
2008 Saunders, An Imprint of Elsevier
CHAPTER 46 – Arthroscopic Meniscus Repair: All-Inside Technique
David Diduch, MD
The all-inside technique for meniscal repair was first introduced in 1991. Since then, several generations of change have taken place with improvements in implant designs and technique. Inherent advantages of an all-inside technique are the avoidance of accessory incisions and their potential risks, the decrease in operative time, and the ease of insertion compared with other meniscal repair techniques.
The success of an all-inside repair is directly related to its ease of use and its ability to restore stability and to re-create normal anatomy. It must compare favorably with traditional arthroscopic methods of meniscal repair, such as suture repair by the inside-out technique. Potential complications, such as device breakage, pullout, and chondral damage, must be avoided.
This chapter briefly discusses the first three generations of all-inside meniscal repair and concentrates on the surgical techniques associated with the latest fourth-generation implants, specifically the FasT-Fix (Smith & Nephew, Inc., Andover, Mass) and the RapidLoc device (Mitek Worldwide, Westwood, Mass).
Meniscal injury commonly occurs with a twisting injury to the knee and, at times, in conjunction with knee ligamentous injury. There are usually joint line tenderness and mechanical symptoms that include catching, locking, and giving way. Swelling typically occurs overnight in the acute setting and on an intermittent, activity-related basis with a chronic tear.
| • | Full knee evaluation bilaterally | |
| • | Rule out any hip, pelvic, or back disease that may be contributing to “knee” pain |
Key examination elements for meniscal tears include the following:
| • | Presence of an effusion | |
| • | Extension deficit (which may indicate a locked meniscal fragment) | |
| • | Joint line tenderness | |
| • | Positive results of McMurray test and Apley test |
Positive findings suggest a meniscal tear.
Plain radiographs are helpful in assessing for gonarthrosis as well as limb alignment.
| • | Standing anteroposterior and posteroanterior flexed views | |
| • | Lateral and sunrise views |
Magnetic resonance imaging can be more than 90% accurate in identifying meniscal lesions and may be used to help confirm their presence. However, it is not as helpful in predicting whether a tear is reparable. The decision for repair versus partial resection usually requires arthroscopic assessment.
Indications and Contraindications
Many factors play a role in meniscal treatment decision-making. Age of the patient, presence of meniscal degeneration, tear size, tear pattern, vascularity, associated instability, chronicity of the tear, and integrity of the meniscal body must be taken into account. Longitudinal, peripheral (vascular) tears are the most amenable to repair. If there is ligamentous instability, it should be addressed at the time of meniscus repair, if possible, or in the near future if the procedure must be staged. As with other forms of repair, the all-inside technique yields better results with acute, traumatic tears and in those knees undergoing concomitant anterior cruciate ligament (ACL) reconstruction. Tears that are stable with less than 3 mm of displacement with probing and that are less than 1 cm in length can be left unrepaired with predictable results.
Relative contraindications to an all-inside repair are tears that occur at the meniscocapsular junction and tears that extend to the anterior horn. There must be a meniscal rim intact for the anchoring mechanisms of these devices to work appropriately. The anterior horn is difficult to access through anterior portals with any of the available all-inside devices. These situations may be better served with a suture technique, such as the inside-out or outside-in technique.
For knee arthroscopy with meniscal repair, one may use a lateral post or a leg holder. The patient is placed supine. A tourniquet of the appropriate size is placed high on the thigh. When a lateral post is to be used, the leg of the bed need not be broken, although it may improve posterior access. With a leg holder, it is important to position the patient far enough down the bed to allow adequate knee flexion for the operation.
After standard arthroscopic portals are established, a complete diagnostic knee arthroscopy is performed. Meniscal disease is identified, and if it is amenable to repair, the meniscus is prepared with standard techniques as appropriate, such as gentle rasping of the torn surfaces and more aggressive rasping of the adjacent synovium to stimulate proliferation. For isolated meniscal repair, one may consider biologic augmentation with a fibrin clot. Delivery to the tear can be facilitated by use of an absorbable suture. When an ACL reconstruction is performed simultaneously, fibrin clot occurs naturally.
The portal that affords the most perpendicular approach to the tear should be used to place the device. Typically, this will be the contralateral portal (i.e., introduce the device through the lateral portal for placement in the medial meniscal body). It is common to change portals for optimal access as devices are placed around the meniscal rim. If possible, leave sutures attached until all implants are placed so that they can be tensioned again for optimal compression.
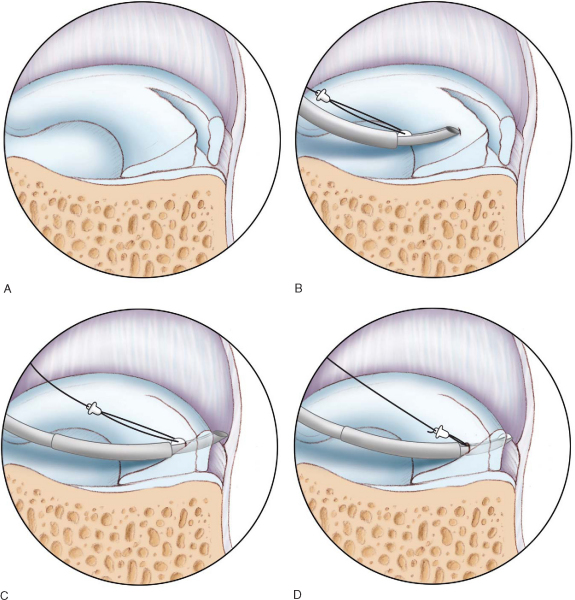
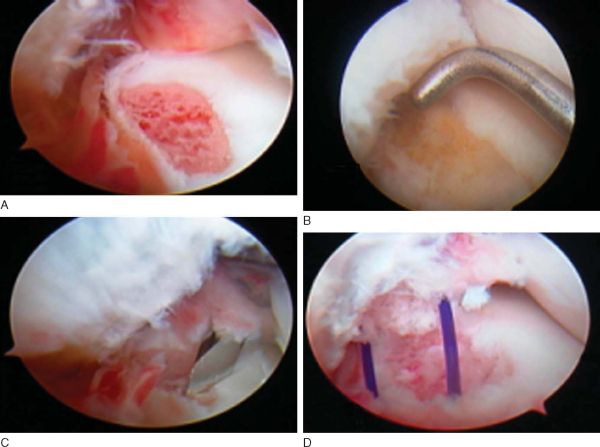
Meniscal tear repair by the RapidLoc system is illustrated in
Figure 46-1
.
|
|
|
|
Figure 46-1 |
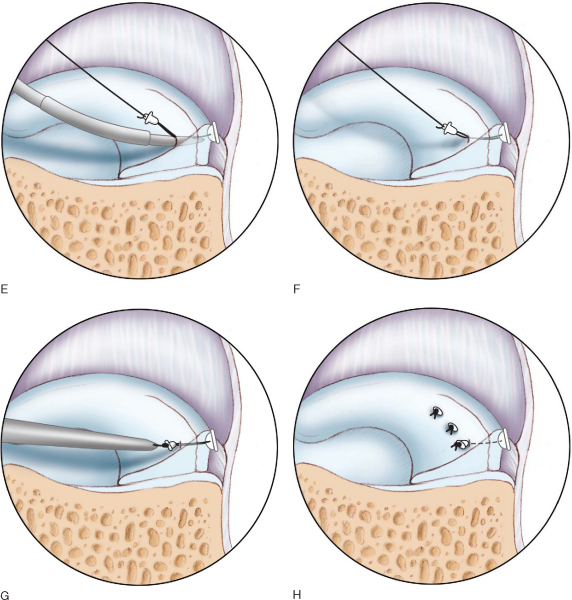
Meniscal tear repair by the FasT-Fix system is illustrated in
Figure 46-2
.
|
|
|
|
Figure 46-2 |
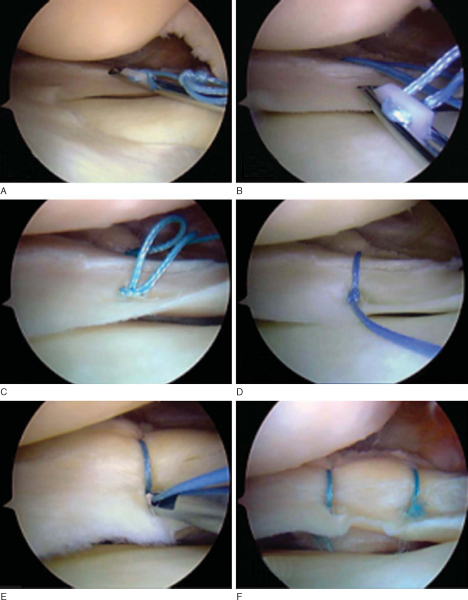
Meniscus Arrow and Other Barbed Implants
The implant is introduced into the joint with either a hand inserter or a gun (
Fig. 46-3
). The tip of the implant is used to reduce the meniscus, and the arrow is placed across the tear by hand or gun. It is nearly impossible to re-tension after the implant is placed.
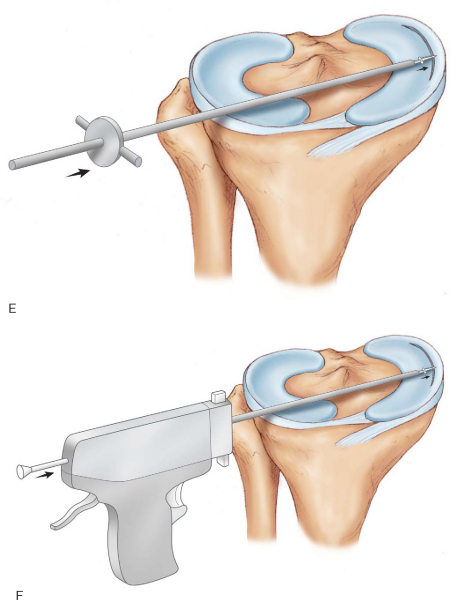
Meniscal Root or Ossicle Repair
The meniscal ossicle is seen as calcification within the meniscus. Most often, it is found within the posterior root of the medial meniscus. Some believe these represent vestigial structures, whereas others believe that they are secondary to trauma. The same technique may be used for acute avulsion of the meniscal root with or without the presence of an ossicle.
The technique for repair of a meniscal root tear is illustrated in
Figure 46-4
.
|
|
|
|
Figure 46-4 |
Originally described in 1991, the first generation of all-inside meniscal repair used curved suture hooks to pass suture across tears from the back of the knee through additional portals, allowing retrieval of the suture followed by knot tying. Technical challenges associated with this technique along with potential risk to the neurovascular structures led to second-generation implants.
Second-generation repairs began the evolution of placing devices across the tear by use of standard arthroscopic portals. The T-Fix (Smith & Nephew, Inc., Andover, Mass) had sutures connected to a polyethylene bar that was deployed through a needle to capture the peripheral meniscus or capsule. Pairs of sutures could be tied with a square knot that was pushed onto the meniscal surface, which presented a technical challenge to some. The inability to tension the knot provided another technical drawback. The preliminary results were encouraging with short-term success rates of 80% to 90%. [3] [5] [10] The T-Fix taught surgeons that an all-inside device could be safely delivered through anterior portals without undue neurovascular risk. However, the desire for a simpler device with more compression across the repair led to the development of third-generation devices.
Many absorbable repair devices, including arrows, screws, darts, and staples, then became available. These capture the torn meniscus and anchor it to its peripheral portion or capsule. Common features of these devices include long-term absorbable material, such as polylactic acid, and a rigid design. The meniscal arrow (Linvatec, Largo, Fla) has achieved popularity secondary to its ease of use and early success rates. Our early experience with the arrow showed a 90.6% success rate with average 2-year followup in a population undergoing concurrent ACL reconstruction with the arrow.[12] However, when the same group was observed to 6.6 years, our success rate dropped to 71.4%.[17] This observation suggests that some tears partially heal and become symptomatic as the polylactic acid device dissolves at 2 to 3 years. In addition, longer followup may be needed to better determine true outcomes. We have since abandoned the use of the arrow.
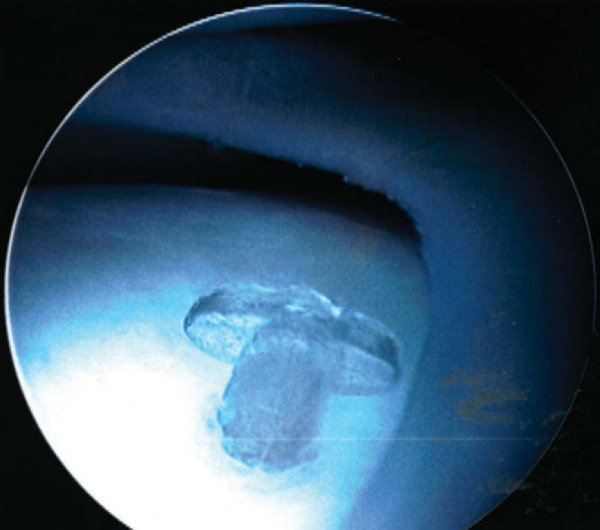
Complications reported with these devices, especially the arrow, have included transient synovitis, inflammatory reaction, migration of devices, chondral damage, cyst formation, and device failure (
Fig. 46-5
). [2] [7] [14] [19] [21] [22] [24] [25] [26] A study with a 2-year minimum followup had a clinical failure rate of only 7% but had a local soft tissue complication rate of 31.6% with two devices that migrated through the skin.[15]
|
|
|
|
Figure 46-5 |
In a prospective randomized study of 68 patients, a comparison of the arrow and a horizontal mattress suture technique was evaluated. Unique to this study was that a second-look arthroscopy was performed in 96% of the participants at 3 to 4 months. The investigators reported 91% and 75% healing rates for the arrow versus suture, respectively. The operative time for arrow insertion was half that of the suture technique. No complications were reported for either group.[1] However, another study comparing suture, arrows, and the T-Fix showed success rates of 78.6%, 56.5%, and 57.1%, respectively.[27] Laprell et al[16] reported on the Mitek meniscal repair system in 2002 in 37 menisci. They found a success rate of 86% at 1 year. In addition, 17 patients underwent second-look arthroscopy at 6 to 8 weeks, and there were five patients with a residual cleft and one with a chondral abrasion. However, all 17 menisci were still reduced. The findings of the long-term arrow study help point out the need for followup beyond the point at which these devices dissolve.
Some of these techniques remain popular when they are used in a hybrid fashion with a combination of suture in the body and anterior horn and third-generation implants for the posterior portion of tears. Placement of inside-out suture across the extreme posterior horn can be the most technically demanding and pose the greatest risk to the neurovascular structures. Use of one or two all-inside devices at the extreme posterior horn helps improve these issues.
The majority of the third-generation devices are rigid, increasing the potential for articular cartilage injury. In addition, the native meniscus moves and changes shape with activity. This may be impaired with the use of such rigid devices. Furthermore, once these devices are placed, it is nearly impossible to modify the position if more compression is needed across the tear or if the top of the implant is proud relative to the meniscal surface. The chondral risk and lack of adjustability have led to the fourth-generation devices.
The fourth-generation devices are flexible and suture based and allow variable compression across the meniscal tear. Two systems are currently available, the FasT-Fix and the RapidLoc meniscal repair device. The FasT-Fix has an inserter with two implants loaded. Each implant consists of 5-mm suture bar anchors and braided No. 0 polyester suture. A needle inserter with an implant loaded at its tip is advanced across the tear, and the anchor is deployed. The needle inserter is withdrawn from the meniscal tissue while it remains within the joint. A button on the handle of the inserter is advanced to allow the second implant to be loaded at the tip of the needle inserter. This can then be advanced through the meniscus in a different location, leaving a suture bridge in either a horizontal or vertical mattress fashion across the tear. A pre-tied slip knot is then advanced to apply variable compression across the tear by use of the knot pusher or suture-cutting device (see
Fig. 46-2
).
In a prospective case study of 42 meniscal tears treated with the FasT-Fix with an average 2-year followup, the group with concurrent ACL reconstruction had a reported success rate of 91%; with isolated repair, that dropped to 80%. No complications were noted, including no chondral abrasion in eight followup arthroscopies. In fact, the authors stated that the healing response around the sutures made them barely visible or completely incorporated into the meniscus.[13]
The RapidLoc device is an absorbable anchor and suture device with a pre-tied slip knot to compress an absorbable top hat on the surface of the meniscus (see
Fig. 46-1
). The top hat is made from either PDS or polylactic acid; the suture options include Ethibond and slowly resorbing Panacryl. A single case applier is introduced with a 0-, 12, or 27-degree needle with the device loaded. The needle is advanced across the tear, as perpendicular as possible, to its silicone hub, limiting insertion depth to 13 mm. The handle on the applier is fired, which advances and deploys the backstop. The applier is removed. A knot pusher advances the pre-tied slip knot with top hat to the meniscus surface and allows variable tensioning across the tear.
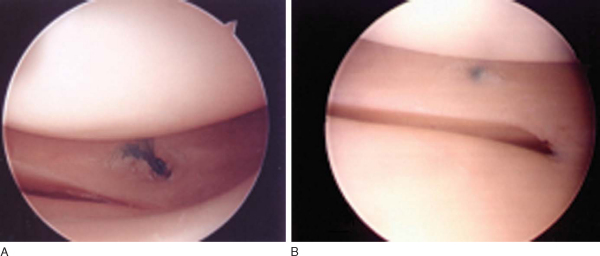
In a study of the RapidLoc, we reviewed 75 meniscal repairs in patients who had undergone concomitant ACL reconstruction with a mean followup of 35 months. There was a 90.7% clinical success rate, similar to the equivalent group in the FasT-Fix study. Univariate analysis suggested that negative prognostic factors included a bucket-handle configuration, multiplanar morphologic features, tear length greater than 2 cm, and more than 3 months from tear to repair. Second-look arthroscopy in a small group showed healing and incorporation of the top hat into the meniscal tissue and no chondral abrasion, similar to the FasT-Fix study (
Fig. 46-6
).[23]
|
|
|
|
Figure 46-6 |
Cadaveric studies of both the RapidLoc and FasT-Fix have been performed. Of the 48 RapidLoc anchors placed by two experienced surgeons, popliteus tendon and superficial medial collateral ligament entrapments by the backstops were the only potential complications encountered, an outcome common with suture techniques and of doubtful clinical importance. More than 80% were placed correctly, and no cartilage injury or vessel entrapment was noted.[20]
In a similar study of the FasT-Fix, 45 anchors were placed. Only 27 were thought to be in the correct position. The original 22-mm preset length was too long and led to penetration of the collateral ligaments, iliotibial tract, and skin. There was difficulty with suture tensioning and early deployment of the anchors. Since the time of this study, modifications to the system have been made, including a shorter insertion device and improvements in its tensioning and deployment characteristics. It is recommended that the optional depth limiter be trimmed to no longer than 15 mm to help avoid potential entrapments and neurovascular injury.
Biomechanical characteristics are shown in
Table 46-1
.
| Author | Vertical FasT-Fix | Horizontal FasT-Fix | Arrow | RapidLoc | Vertical Suture | Horizontal Suture | |
|---|---|---|---|---|---|---|---|
| Barber et al[4] (2004) | Load to failure (N) | 70.9 | 72.1 | 43.28 | 80.43 | 55.9 | |
| Fisher et al[11] (2002) | Load to failure (N) | 45.89 | 107.65 | ||||
| Durselen et al[9] (2003) | Load to failure (N) | 52 | 103 | ||||
| Load to failure after cyclic load (N) | 48 | 82 | |||||
| McDermott et al[18] (2003) | Load to failure (N) | 49.1 | 34.2 | 72.7 | |||
| Gap after cycling (mm) | 3.47 | 2.18 | 3.29 | ||||
| Dervin et al[8] (1997) | Load to failure (N) | 29.6 | 58.3 | ||||
| Zantop et al[28] (2005) | Load to failure (N) | 94.1 | 80.8 | 30.3 | 71.3 | 50.2 | |
| Gap after cycling (mm) | 5.34 | 6.23 | 6.84 | 5.61 | 6.03 | ||
| Borden et al[6] (2003) | Load to failure (N) | 104 | 49 | 102 | |||
| Gap after cycling (mm) | 5.1 | NA | 6 | ||||
| Stiffness | 7.7 | 6.1 | 7.7 |
| • | 10 to 14 days for suture removal and wound check | |
| • | 6-week followup and progress check |
For meniscal repair in conjunction with ACL reconstruction, the standard ACL protocol is used with the addition of the following:
| • | Postoperative hinged ACL brace for 6 weeks, 0 to 90 degrees of motion | |
| • | 50% weight bearing for 6 weeks |
For isolated meniscal repair without ACL reconstruction, return to sports is permitted at 5 months.
Most complications are the same as in other types of meniscal repair. The complications specific to all-inside techniques are listed in
Box 46-1
.
| Complications Specific to All-Inside Techniques | |||||||||||||||||||||||||||
|
Third-generation rigid devices
|
All-inside meniscal repair is an attractive option for surgeons. It is easier and can be done with fewer assistants than inside-out and outside-in techniques. Longer followup with third-generation rigid devices, such as the meniscal arrow, has shown decreased success rates from originally reported promising midterm results with various complications, including chondral abrasion. The newer fourth-generation devices are promising in that they are flexible and allow variable tensioning across the repair, characteristics that are more similar to the inside-out technique. The early 2- to 3-year followup studies of both the FasT-Fix and RapidLoc are promising, particularly in those patients with smaller tears undergoing concomitant ACL reconstruction, in which greater than 90% success rates have been seen. Second-look arthroscopies with both implants are promising in that there have been no reports of chondral abrasion, and it appears that the meniscal tissue can grow over these devices.
Currently, we recommend use of these devices for meniscal repairs in conjunction with an ACL repair. On the basis of a critical analysis of our RapidLoc data, we think that to achieve results similar to those of the inside-out techniques, the optimal tear configuration for an all-inside repair includes tears less than 2 cm in length, acute tears (less than 3 months from injury), and those that are in a vertical, non–bucket-handle configuration (cannot be displaced into the notch).[23] It is important that a peripheral rim of meniscal tissue be present. Inside-out techniques should be used for meniscocapsular junction tears. Isolated tears without ACL reconstruction may be best repaired with inside-out or hybrid techniques (all-inside device posteriorly, inside-out suture for remaining posterior horn and body) until long-term followup studies are available for these new devices. Inside-out suture remains the “gold standard” against which all new devices must be measured.
Results of studies of all-inside techniques are listed in
Table 46-2
.
| Third-Generation Devices | ||||
|---|---|---|---|---|
| Author | Device | Followup | Success Rate | Notes |
| Gill and Diduch[12] (2002) | Arrow | 2 years (average) | 90.6% | |
| Lee and Diduch[17] (2005) | Arrow | 6.6 years (average) | 71.4% | Same population with longer followup |
| Albrecht-Olsen et al[1] (1999) | Arrow | 3–4 months | 91% | Second-look arthroscopy |
| Suture | 75% | |||
| Venkatachalam et al[27] (2001) | Arrow | 78.6% | ||
| Suture | 56.5% | |||
| FasT-Fix | 57.1% | |||
| Laprell et al[16] (2002) | Mitek repair system | 1 year | 86% | 1/17 patients with second-look arthroscopy with chondral injury |
| Fourth-Generation Devices | ||||
|---|---|---|---|---|
| Author | Device | Followup | Success Rate | Notes |
| Hass et al[13] (2005) | FasT-Fix | 2 years | 91% | With ACL reconstruction |
| 80% | Isolated repair, no ACL | |||
| Quinby et al[23] (2005) | RapidLoc | 35 months | 90.7% | With ACL reconstruction |