Approach to the Sensory Examination
– Neurologic Examination > Sensory Examination > Chapter 28 –
Approach to the Sensory Examination
localize neurologic pathology by looking for characteristic
distributions of sensory loss.
pin and vibratory sensation, should be performed on any patient who
presents with sensory symptoms, such as numbness or tingling in a part
of the body or extremities. A detailed sensory examination should also
be performed on any patient with signs or symptoms of any focal
disorder of the central of peripheral nervous system, because the
finding of associated sensory loss may aid in localization.
significant focal neurologic symptoms or signs, however, the sensory
examination plays a limited role. In these patients, an assessment of
distal vibratory sensation usually suffices to confirm normal sensory
function.
begin in peripheral receptors, travel up the peripheral nerves to the
dorsal nerve roots, and then enter the spinal cord. In the spinal cord,
the sensory pathways ascend as the spinothalamic tract (mainly subserving pain and temperature sensation; see Chapter 29, Examination of Pinprick Sensation) and the posterior columns (mainly subserving vibration and proprioceptive sensation; see Chapter 30,
Examination of Vibration and Position Sensation). After ascending in
the spinal cord, these tracts synapse in the contralateral thalamus,
where the sensory information is then relayed to the cerebral cortex.
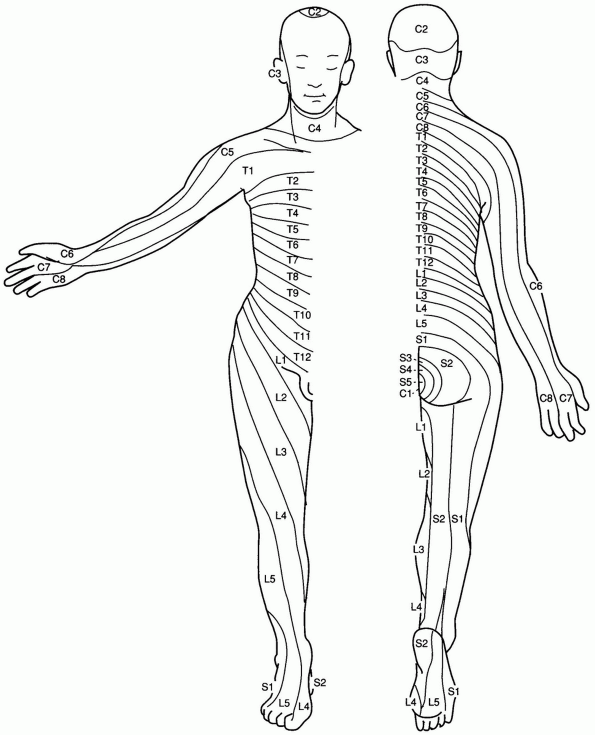
summarize the approximate cutaneous sensory territory of nerve root
innervation of the body and the extremities. These charts are helpful
in localizing patients’ sensory symptoms to the appropriate region when
those symptoms are due to a lesion of the nerve root or the spinal
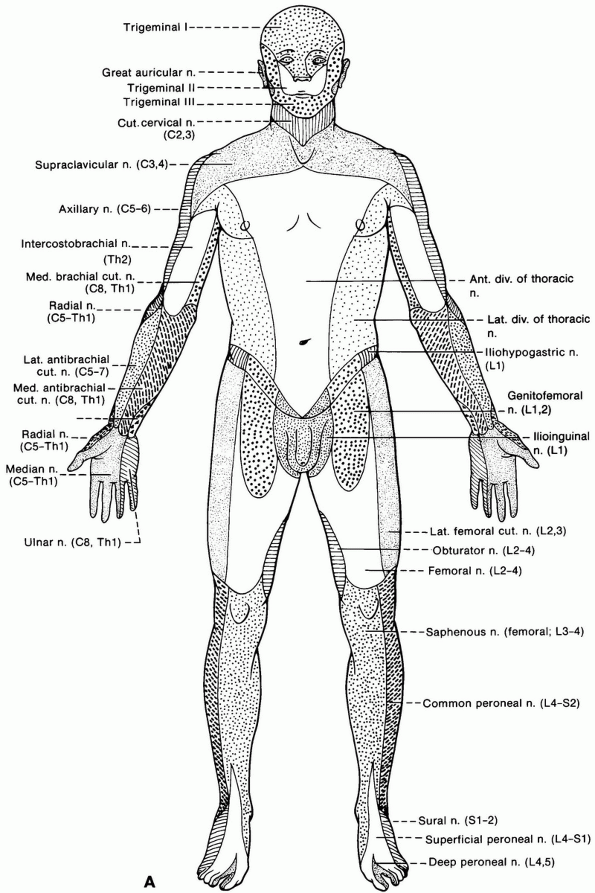
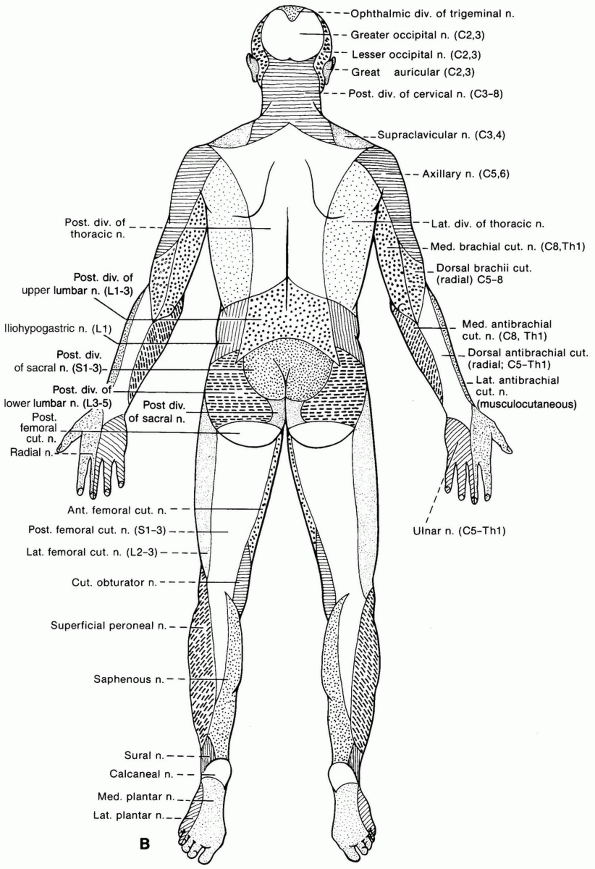
cord. The cutaneous distribution of the peripheral nerves themselves (Fig. 28-2)
can also be shown graphically and can aid in localization of patients’
sensory symptoms to a particular peripheral nerve lesion.
 |
|
Figure 28-1 Dermatome chart of the anterior and posterior body and extremities. (From Dudek RW. High-yield gross anatomy. Philadelphia: Williams & Wilkins, 1997.)
|
-
256-Hz tuning fork
-
Safety pin (see Chapter 29, Examination of Pinprick Sensation, for details on the use of a safety pin or appropriate alternative to test pin sensation)
Examination of Vibration and Position Sensation. In general, though,
the approach to performing the sensory examination should vary
depending on the clinical suspicion of lesion localization as your
thought process evolves during the history and examination.
-
If you suspect a brain, thalamic, or brainstem localization, concentrate on detecting side-to-side differences in sensation.
-
If you suspect a spinal cord localization
of the patient’s symptoms, concentrate on detecting a decrease in
sensation below a dermatomal level (see Chapter 51, Examination of the Patient with a Suspected Spinal Cord Problem). -
If you suspect a nerve root localization
of symptoms, concentrate on assessing sensation within the dermatome of
the nerve root of concern, comparing it to other nerve root
distributions on the same side and on the other side. -
If you suspect a lesion of a specific
nerve, concentrate on assessing sensation within the distribution of
that nerve, comparing it to the sensation within areas supplied by
other nerves on the same side and the other side. -
If you suspect a polyneuropathy,
concentrate on assessing the extremities for a change in sensation
distally compared to proximally.
equally on both sides of the body, within all cutaneous distributions,
and sensation should be the same distally, as well as proximally.
-
Any alteration in sensation is
potentially abnormal. Abnormal findings on sensory testing may include
loss of sensation or an abnormally painful sensation to the sensory
stimulus being tested. Table 28-1 summarizes some of the terminology used to describe sensory findings. -
Use the distribution of any sensory
abnormality you discover (and the distribution of the patient’s
subjective sensory symptoms) to help you determine the most likely
localization of your patient’s pathology. Table 28-2 summarizes the localizations suggested by different distributions of sensory signs and symptoms. -
Use the rest of the neurologic
examination (particularly the motor and reflex components) to look for
further evidence to support or refute your hypothesis obtained from
sensory testing regarding the localization of pathology.
-
The sensory examination is of limited
value in the absence of a sensory complaint, such as numbness or
tingling, or in the absence of a suspicion of a process that may cause
sensory findings. Abnormalities found on the sensory examination should
be interpreted within the clinical context. -
When comparing sensation in one area to
another, it is preferable to ask the patient if the sensation is “about
the same” in each area rather than asking the patient if there is a
“difference” in the sensation. When asked if there is a difference in
sensation, the suggestible patient may feel compelled to report
inadvertent minor differences in the pressure exerted by the physician,
instead of just reporting areas of truly diminished sensation.
 |
|
Figure 28-2 A,B:
The cutaneous distribution of the peripheral nerves. Ant., anterior; C, cervical; cut., cutaneous; div., division; L, lumbar; lat., lateral; med., medial; n., nerve; post., posterior; S, sacral; Th, thoracic. Continued. (From Haerer A. DeJong’s the neurologic examination. Philadelphia: JB Lippincott Co, 1992:56-57.) |
 |
|
Figure 28-2 Continued.
|
|
TABLE 28-1 Terminology Used to Describe Sensory Examination Findings
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
TABLE 28-2 Lesion Localization by Distribution of Sensory Examination Findings and Sensory Symptoms
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
