De Quervain’s Release
initially described by de Quervain in 1895. The abductor pollicis
longus (APL) and the extensor pollicis brevis (EPB) are inflamed as
they pass under the extensor retinaculum of the first dorsal
compartment. Localized tenderness and swelling in this region with a
positive Finkelstein test confirm the diagnosis of de Quervain’s
tenosynovitis. Initial nonoperative treatment consists of splinting and
local cortisone injection. If conservative modalities fail to relieve
the symptoms, surgical decompression of the first compartment is
indicated.
The first extensor compartment, which is the most radial compartment,
contains the tendons of the APL and the EPB. The extensor retinaculum
covers the tendons in the first compartment and holds them adjacent to
the radial styloid. Proximal to the wrist, these tendons cross
superficial to the radial wrist extensors in the second dorsal
compartment, and they then form the palmar border of the anatomic snuff
box. The APL originates from the posterior surface of the radius and
ulna and inserts onto the base of the thumb metacarpal. The APL is an
abductor and extensor of the thumb and is innervated by the posterior
interosseous nerve. The EPB originates from the posterior surface of
the radius and interosseous membrane and inserts onto the dorsal base
of the thumb proximal phalanx. The EPB extends the thumb proximal
phalanx and is also innervated by the posterior interosseous nerve.
deep from the volar forearm into the interosseous space between the
thumb and index finger metacarpals. The radial sensory nerve branches
superficial to the first compartment tendons, as it innervates the skin
over the dorsum of the thumb and fingers.
been described, and these must be known before surgical treatment is
performed to ensure complete release of both the APL and EPB. These
include multiple slips of the APL, variable insertions of the APL, and
separate compartments for the APL and EPB tendons. Failure to recognize
these variations and subsequent incomplete release of the APL or EPB
will result in persistence of symptoms after surgical decompression of
the first dorsal compartment.
consists of splinting with a thumb spica splint to immobilize the
involved tendons. Corticosteroid is also injected into the first
compartment. Oral nonsteroidal antiinflammatory medication can be
helpful in mild cases in conjunction with splinting. If the patient
fails to respond adequately to these modalities, surgical release of
the first dorsal compartment is indicated.
table, with the upper extremity on an arm board or hand table. A
pneumatic tourniquet is placed on the proximal aspect of the upper
extremity, over a layer of padding, and is preset to 250 mm Hg (Fig. 14-2).
The surgeon sits within the corner made by the arm board and the
operating room table. The skin and subcutaneous tissue just proximal to
the radial styloid is infiltrated with 2% lidocaine without
epinephrine, and the extremity is then prepped and draped in the usual
sterile fashion.
palpated, and the skin incision is marked with a sterile marking pen or
methylene blue. A variety of skin incisions have been described for
exposure and release of the first compartment. The skin incision must
provide adequate exposure to identify and protect the radial sensory
nerve branches that lie superficial to the extensor retinaculum
covering the first dorsal compartment.
This incision allows for exposure and safe retraction of the radial
sensory nerve branches before incision of the retinaculum. Other
potential incisions include a short oblique incision, zigzag incision,
and a chevron incision, with the apex volarly to allow for retraction
of a dorsal flap of skin and subcutaneous tissue. A
transverse incision proximal to the radial styloid in a natural skin
crease provides adequate exposure and heals well. A longitudinal skin
incision is more likely to result in an unsightly painful hypertrophic
scar.
 |
|
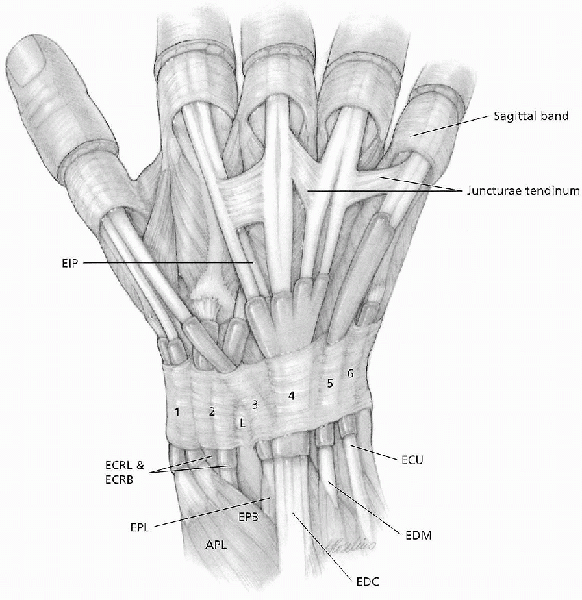
FIGURE 14-1.
The wrist extensor retinaculum and the most common arrangement of the extensor tendons and juncturae. The wrist, thumb, and finger extensors gain entrance to the hand beneath the extensor retinaculum through a series of six tunnels, and at this level are covered with a synovial sheath. (From Doyle JR. Hand. In: Doyle JR, Botte MB, eds. Surgical anatomy of the hand and upper extremity. Philadelphia: Lippincott Williams & Wilkins, 2003:532-666, with permission.) |
 |
|
FIGURE 14-2. Patient position.
|

is exsanguinated, and the tourniquet is inflated to 250 mm Hg. The skin
is sharply incised with a no. 15 scalpel along the marked incision
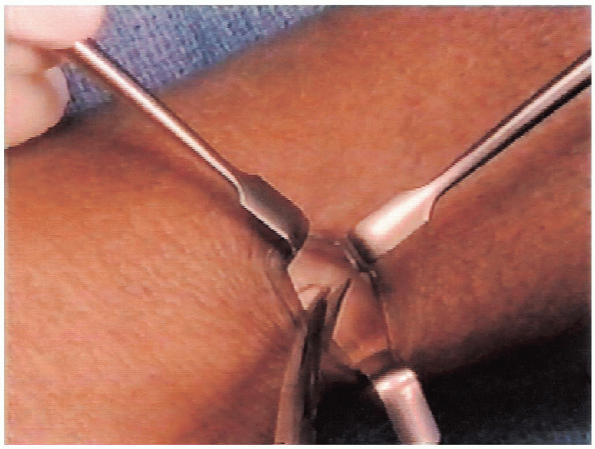
line. After sharply incising the skin (Fig. 14-4),
the subcutaneous dissection is performed with a blunt-tipped scissors
to the level of the extensor retinaculum over the first dorsal
compartment. The branches of the radial sensory nerve are identified
and carefully retracted dorsally and volarly to expose the extensor
retinaculum (Fig. 14-5).
problem for the patient than was the
first-compartment tenosynovitis. The radial sensory nerve and its
branches are superficial and are prone to injury with a deep skin
incision. After sharply incising the skin, the subcutaneous tissue
should be bluntly dissected off the retinaculum and retracted, before
the retinaculum is divided. It is not necessary to identify and dissect
all of the branches of the radial sensory nerve; this will result in
symptomatic neuropraxia and possibly loss of sensation over the dorsal
aspect of the thumb and index finger.
 |
|
FIGURE 14-3. Transverse skin incision marked 1 cm proximal to radial styloid.
|
 |
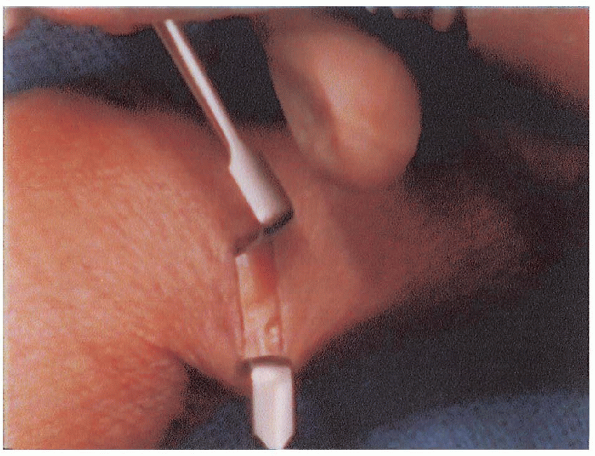
|
FIGURE 14-4. Skin incision completed, before subcutaneous dissection and identification of radial sensory nerve.
|
 |
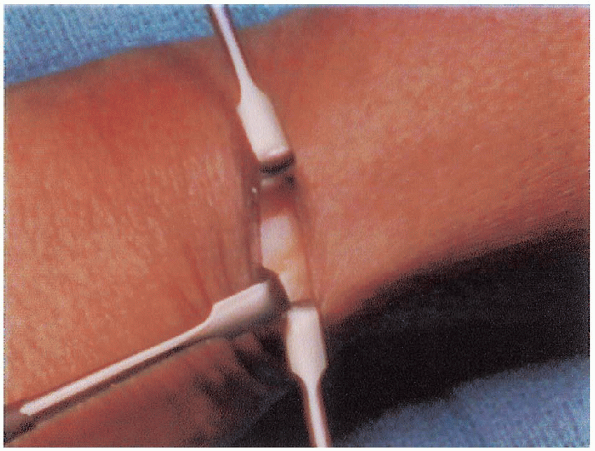
|
FIGURE 14-5. Identification of radial sensory nerve branches.
|
 |
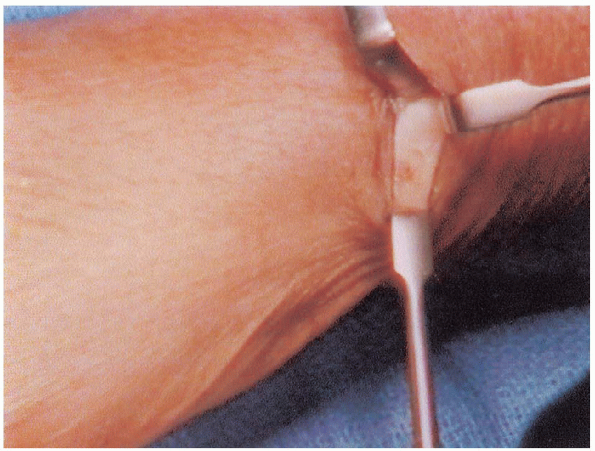
|
FIGURE 14-6. Proximal extent of the extensor retinaculum.
|
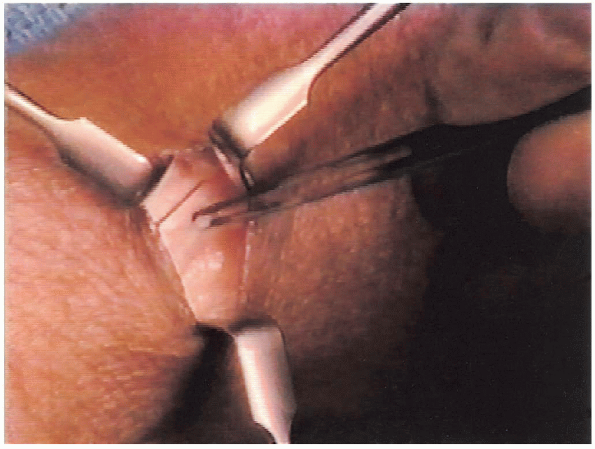
retinaculum can be identified by careful distal and then proximal
retraction of the skin (Figs. 14-6 and 14-7).
Again, the branches of the radial sensory nerve are carefully
retracted. With a scalpel, the extensor retinaculum is then incised
longitudinally along the length of the first compartment, in the dorsal
aspect of the retinaculum (Fig. 14-8). By incising the
extensor retinaculum in this fashion, a palmar-based flap of
retinaculum remains to prevent volar subluxation of the tendons of the
first compartment.
 |
|
FIGURE 14-7. Distal extent of the extensor retinaculum.
|
 |
|
FIGURE 14-8. Incision in the dorsal aspect of the extensor retinaculum.
|
 |
|
FIGURE 14-9. Palmar-based flap of extensor retinaculum pre-
|
 |
|
FIGURE 14-10. The decompressed tendons of the dorsal compartment.
|
 |
|
FIGURE 14-11. Traction on the decompressed extensor pollicis brevis tendon.
|
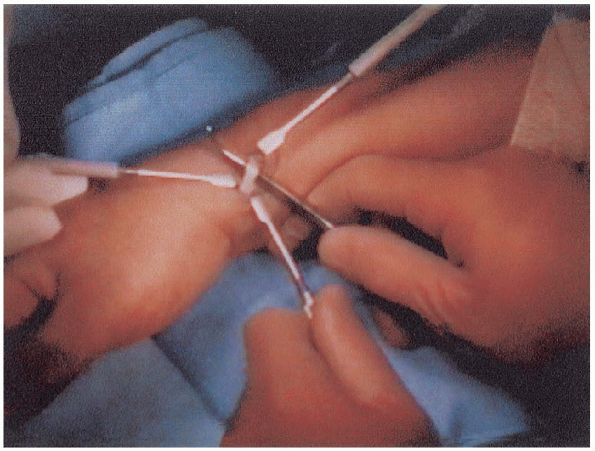
dorsal aspect with preservation of a palmar-based flap minimizes
potential volar subluxation of the extensors that can occur with wrist
flexion (Fig. 14-9). Postoperative splinting with the wrist in extension may also limit this complication.
The EPB lies dorsal in the first compartment and typically has a more
distal muscle belly. The APL is more volar in the first compartment and
typically has multiple slips. The tendons may be housed in two separate
compartments within the first compartment, and if there is a septum
dividing the first compartment, both tendons must be relieved of
constriction.
anomalous insertions of the tendons, and the
presence of a septum within the first compartment separating the APL
and EPB. Inadequate operative release of the retinaculum can be avoided
by careful identification and decompression of both the APL and EPB
during the surgical procedure.
 |
|
FIGURE 14-12. Traction on the released abductor pollicis longus tendon.
|
 |
|
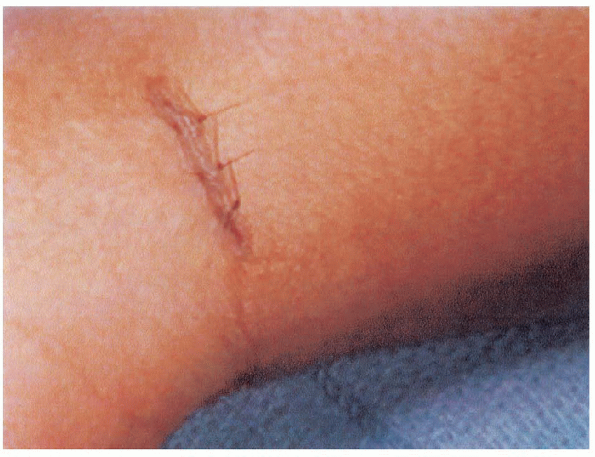
FIGURE 14-13. Skin closure.
|
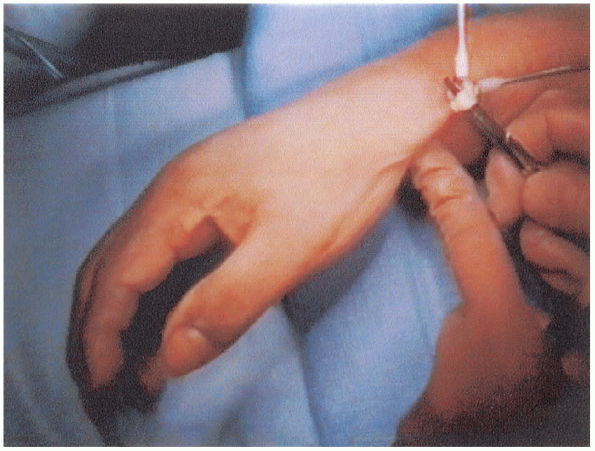
hemostat to verify their release. Traction on the EPB tendon extends
the metacarpophalangeal joint (Fig. 14-11), and tension on the APL abducts and extends the thumb metacarpal shaft (Fig. 14-12). Release of both tendons must be completed before wound closure.
is deflated. Hemostasis is obtained with electrocautery. The wound is
irrigated and closed with 5-0 nylon suture (Fig. 14-13).
A bulky hand dressing is then applied, with a thumb spica plaster
splint in wrist extension. The patient is transferred to the recovery
room to be discharged later in the day. The patient is given a
prescription for analgesia and is instructed on strict elevation of the
hand for several days.
surgical procedure. The dressing and the sutures are removed. A
removable thumb spica splint is provided and used intermittently for 2
weeks, with the patient gradually weaning from the splint as the
discomfort resolves.
