Infection Associated with Neuropathy
Editors: Tornetta, Paul; Einhorn, Thomas A.; Damron, Timothy A.
Title: Oncology and Basic Science, 7th Edition
Copyright ©2008 Lippincott Williams & Wilkins
> Table of Contents > Section
IV – Basic Science > 27 – Infectious Disorders of Bone and Joint
> 27.3 – Infection Associated with Neuropathy
IV – Basic Science > 27 – Infectious Disorders of Bone and Joint
> 27.3 – Infection Associated with Neuropathy
27.3
Infection Associated with Neuropathy
Charcot Arthropathy
A wide spectrum of neurologic disorders are associated with the late development of neuropathic joint:
-
Spinal cord level or higher
-
Syphilis (tabes dorsalis)
-
Syringomyelia
-
Meningomyelocele
-
Cerebral palsy
-
-
Peripheral neuropathy
-
Diabetes
-
Leprosy
-
Alcohol abuse
-
Any other cause of peripheral neuropathy
-
Neuropathic joint (Charcot arthropathy) is defined as a
progressive disease of bone and joints characterized by painless bone
and joint destruction arising in limbs that have lost sensory and
autonomic innervation.
progressive disease of bone and joints characterized by painless bone
and joint destruction arising in limbs that have lost sensory and
autonomic innervation.
Pathophysiology
The fundamental first step leading to joint and
periarticular destruction is a profound regional osteopenia arising as
a result of a loss of vasomotor control. A sustained regional
hypervascular flush (active hyperemia) is associated with marked
osteoclast activity. There is a loss of important structural
subchondral bone with collapse under physiologic load of the affected
joint. The loss of sensation to the region allows little perception of
what is, in essence, a stress fracture situation. Normal weight bearing
continues with mechanical displacement of shards of shredded and
displaced articular cartilage, evoking a foreign body granulomatous
response in the periarticular soft tissues. Once destruction has
occurred, the biology of fracture healing occurs, modulated by the
abnormal biomechanics of the region and ongoing abnormal
vasore-gulation. Over months to years the region may develop bony and
soft tissue stability or may require surgery or external bracing to
provide this.
periarticular destruction is a profound regional osteopenia arising as
a result of a loss of vasomotor control. A sustained regional
hypervascular flush (active hyperemia) is associated with marked
osteoclast activity. There is a loss of important structural
subchondral bone with collapse under physiologic load of the affected
joint. The loss of sensation to the region allows little perception of
what is, in essence, a stress fracture situation. Normal weight bearing
continues with mechanical displacement of shards of shredded and
displaced articular cartilage, evoking a foreign body granulomatous
response in the periarticular soft tissues. Once destruction has
occurred, the biology of fracture healing occurs, modulated by the
abnormal biomechanics of the region and ongoing abnormal
vasore-gulation. Over months to years the region may develop bony and
soft tissue stability or may require surgery or external bracing to
provide this.
Classification
A modified Eichenholtz classification is given in Table 27.3-1.
Diagnosis
Clinical Presentation
Acute
-
The manifestations begin with synovitis
and progressively involve instability, subluxation, dislocation, and
complete destruction of the joint. -
The first manifestation of Charcot arthropathy can be swelling, erythema, warmth, and pain.
-
Infection can be considered in the
differential diagnosis for this presentation but is less likely the
cause because the pain is not severe. -
Gout, inflammatory arthritis, and trauma are also considered in the differential.
Chronic
-
The acute presentation may be missed or not perceived, and the patient may present with an established deformity.
Radiologic Findings
-
Plain films (Fig. 21-17)
can show an alarming degree of regional osteopenia and destruction of
joint and periarticular structures. The destructive process can happen
over a very short period (weeks). -
Once destruction has occurred, the radiographs will demonstrate the evolution over time of fracture healing in this region.
Diagnostic Work-up
-
Recognition of the underlying neurological condition
-
Cultures are negative in the acute presentation without skin breakdown.
-
With an ulcer the issue becomes whether
the ulcer is superficial or deep and involving bone, as per the Wagner
ulcer classification (Table 27.3-2).P.522Table 27.3-1 Modified Eichenholz Classification of Charcot ArthropathyStage Stage Name Description 0 Clinical Erythema, edema, increased temperature to foot 1 Fragmentation Periarticular fractures, joint dislocation, instability, deformed foot 2 Coalescence Reabsorption of bone debris, evolution of fracture healing process 3 Reparative Stable foot, osseous healing complete -
Biopsy will show shards of cartilage that
characteristically evoke a marked foreign body granulomatous response
in the adjacent periarticular soft tissues.
Treatment
-
Principles of management
-
Relief of pain
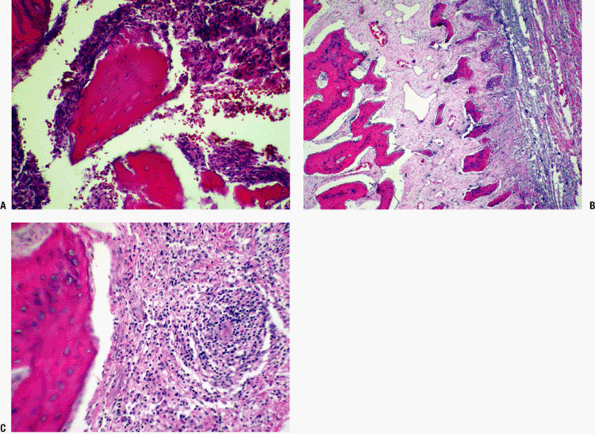 Figure 27.3-1
Figure 27.3-1
Congenital syphilis (severe periostitis). Three photos illustrate the
severe inflammatory process produced by this infection. Marked chronic
inflammation (lymphocytes and plasma cells with fewer histiocytes and a
few multinucleated giant cells are seen in A, with an extensive
periosteal new bone formation evident in B). The immature cortex has a
cancellized look and is associated with marked chronic periostitis,
gaping thin-walled blood vessels, vascular congestion, and thick-walled
small blood vessels with endothelial hyperplasia (endarteritis
obliterans can occur when the infection is severe). (C)
Heavy perivascular plasma cell infiltration with vascular obliteration
is a strong clue to rule out the possibility of syphilis (the Warthin
Starry silver stain is helpful to look for the spirochetal organisms).
-
-
Treat any associated infection: rest,
elevation, antibiotics (usually broad-spectrum), surgery as indicated
by the clinical situation and investigations -
Maintenance of stability
-
External supports (bracing must be judiciously applied and carefully monitored and adjusted to avoid skin problems)
-
Surgical procedures to return and maintain the
P.523
affected joint to physiologic alignment (osteotomy, arthrodesis)Table 27.3-2 Wagner Ulcer Classification for Diabetic FeetGrade Description 1 Superficial diabetic ulcer 2 Ulcer extension to ligament, tendon, joint capsule, or deep fascia without abscess or osteomyelitis 3 Deep ulcer with abscess or osteomyelitis 4 Gangrene to portion of forefoot 5 Extensive gangrenous involvement of the foot
-
Diabetic Feet
This condition, a unique form of Charcot arthropathy,
represents a significant burden on the health care system.
Diabetes-related foot problems are the most common cause of
hospitalization in patients with diabetes.
represents a significant burden on the health care system.
Diabetes-related foot problems are the most common cause of
hospitalization in patients with diabetes.
Etiology
The patient, systemically impaired, often presents with
a benign indifference to a potentially catastrophic local problem. The
sensory neuropathy plays a pivotal role: most ulcers and infection are
the result of a break in the skin caused by unrecognized or unperceived
pressure. With altered local mechanics (increased pressure over bony
prominence) secondary to the process of neuropathic joint breakdown, a
portal of entry is created and infection occurs. The following factors
interact in the diabetic patient.
a benign indifference to a potentially catastrophic local problem. The
sensory neuropathy plays a pivotal role: most ulcers and infection are
the result of a break in the skin caused by unrecognized or unperceived
pressure. With altered local mechanics (increased pressure over bony
prominence) secondary to the process of neuropathic joint breakdown, a
portal of entry is created and infection occurs. The following factors
interact in the diabetic patient.
Angiopathy
-
Combination of large vessel
(atherosclerosis) and micro-vascular lesions is more severe and more
prevalent and occurs at an earlier age than in the nondiabetic. -
Below the popliteal trifurcation the
distal lesions of the arteries involve all three vessels in a ragged
and widespread luminal narrowing that is more diffuse than the limited,
discrete lesions of normal atherosclerosis.-
Histologically lesions are in different layers: media in diabetics, intima in nondiabetics.
-
Explains the calcified, stovepipe appearance of vessels on plain film radiography
-
-
There is no known anatomic lesion demonstrated to explain a “small vessel disease” in diabetics.
Neuropathy
-
Typically distal and symmetric (glove-and-stocking)
-
Reduced protective sensation, loss of
proprioception, autonomic neuropathy, and motor neuropathy lead to
altered skeletal structure, calluses, nail deformity, and skin
breakdown.-
Sensory neuropathy: the most important
contributing factor to neuropathic fractures, skin breakdown, and
ulceration; early identification of the sensory deficit is clinically
important for all further management of the potential Charcot process -
Autonomic neuropathy: Loss of regulation
of skin temperature and sweating leads to dry, scaly, stiff skin that
cracks easily, opening the portal for infection; loss of vessel
autoregulation sets up the uncontrolled hyperemia that induces bone
loss and subsequent fractures. -
Motor neuropathy: leads to muscle
imbalance, contractures, and subsequent prominences that become the
sites of increased pressure and potential skin breakdown
-
Immunopathy
-
Occurs at the cellular level, likely worsened by hyperglycemia
-
Decreased chemotaxis, impaired intracellular killing
-
Impaired lymphocyte transformation
Systemic Abnormalities
-
Delayed wound healing secondary to malnutrition and to lack of control of hyperglycemia
-
Indices that indicate whether the patient has adequate nutrition for wound healing:
-
Total lymphocyte count >1,500/mL
-
Total protein >6.2 g/dL
-
Albumin >3.5 g/dL
-
Dementia
-
Often poor compliance
Suggested Reading
Brodsky
JW. Evaluation of the diabetic foot. In Zuckerman JD, ed. AAOS
Instructional Course Lectures 48. Rosemont, IL: American Academy of
Orthopaedic Surgeons, 1999; Chapter 36, pp. 289-303.
JW. Evaluation of the diabetic foot. In Zuckerman JD, ed. AAOS
Instructional Course Lectures 48. Rosemont, IL: American Academy of
Orthopaedic Surgeons, 1999; Chapter 36, pp. 289-303.
Hill SL, Holtzman GI, Buse R. The effects of peripheral vascular disease with osteomyelitis in the diabetic foot. Am J Surg 1999;177(4): 282-286.
