Rotator Cuff Tear Arthropathy
III – Shoulder Reconstruction > Part B – Evaluation and Treatment of
Shoulder Disorders > 45 – Rotator Cuff Tear Arthropathy
disease are a treatment challenge. Most patients will present primarily
because of shoulder pain. Shoulder function can be variable even with
significant chronic rotator cuff deficiency. The arthritic condition of
the shoulder owing to a chronic rotator cuff tear has been termed “cuff
tear arthropathy.” This is characterized clinically by pain and poor
active motion but with near-normal passive motion. It is most common in
women older than the age of 62 years. Many patients are unaware of the
condition until the onset of pain. Operative intervention presents a
challenge because of the lack of rotator cuff and the degenerative
changes present.
Rotator cuff fiber failure occurs as a result of degenerative
processes. This occurs over a period of time. The body adapts as the
humeral head elevates through the defect in the rotator cuff and
contacts the acromion. The coracoacromial (CA) arch becomes the new
fulcrum for the humeral head. Osseous adaptive changes on the humeral
head occur with rounding off of the greater tuberosity. The acromion
becomes concave, and a new acromiohumeral articulation forms. The
patient may have surprisingly little pain, good function, and not know
of the condition. The nonphysiologic contact of the humeral head on the
acromion and superior glenoid can lead to repeated cartilage and
osseous wear with fluid production. Pain and crepitus and loss of
function can occur. With further bony erosion and progressive cuff
damage, shoulder function may deteriorate.
shoulder. Extension of the pre-existing rotator cuff tear can disrupt
the balance of the shoulder that has developed. This can lead to
significant pain and loss of function. The degenerative condition was
present, but the trauma exposed the vulnerability of the shoulder.
progress into cuff deficiency and arthropathy. MRI, ultrasound, and
cadaver studies have reported rotator cuff tears in the elderly
population to be more prevalent with each decade. Some report the
presence of rotator cuff tears in 50% of the population older than 70
years of age. Most of these are asymptomatic. There are some estimates
that 4% to 5% of patients with rotator cuff tears may progress to a
symptomatic CTA from a degenerative cuff tear that is irreparable.
Certainly most rotator cuff tears will not progress to a CTA clinical
picture. In most series most patients with CTA are women older than 62
years of age. Thus it is a disease that is most prevalent in the
seventh and eighth decade of life.
of the humeral head, and loss of cuff function, there is a progressive
degeneration of both rotator cuff substance and bone structure from the
humeral head and acromion. The acromion becomes sclerotic and concave.
The greater tuberosity becomes rounded off. There is an
“acetabularization” of the acromion and a “femoralization” of the
humeral head. The superior glenoid also is subjected to increased force
from the elevated humeral head. The subacromial bursa becomes thickened
and fibrotic. The arthropathic process creates an environment of fluid
production, enzyme production, and further degenerative changes.
the severity of the functional loss, pain, or radiographic changes.
There are no studies to correlate the severity of radiographic changes
with shoulder function or pain. This
makes it difficult to communicate about disease severity, treatment options, and success or failure.
surgery around the shoulder, especially earlier attempts at rotator
cuff repair with coracoacromial arch violation, is important to know. A
history of trauma such as previous falls, dislocations, or fractures
needs to be known. History of inflammatory arthritis, previous
infections, gout, and the number of previous steroid injections is
important to document. Also the type of medication the patient is on,
especially antimetabolites or corticosteroids, is extremely important
to document.
of motion and strength, with increasing pain. Night pain is common. The
ability to use the hand away from the body can be compromised. The
patient will have an internal rotation drop sign as the forearm falls
into internal rotation when trying to reach or hold out in a
handshake-type position. The other presentation will be a minor trauma
that results in a significant amount of pain and shoulder dysfunction.
The relatively small insult exposes the vulnerability of the affected
shoulder.
Visual inspection from behind the patient will reveal degrees of
atrophy of the supraspinatus and infraspinatus. There may be a
fluid-filled appearance under the deltoid owing to excessive fluid
production. Strength testing will elicit weakness in external rotation.
Crepitus with both active and passive motion may be noted. All of these
findings may be seen with surprisingly little pain. The patients who
have very poor active elevation ability (<45 degrees), using mostly
a shoulder shrug, and very little if any pain, are termed
“pseudoparalytic.” This is a functionally disabling condition. Anterior
superior instability with the humeral head riding out from underneath
the coracoacromial arch with attempted elevation is important to note.
In patients without advanced osseous changes, a CT scan or MRI scan can
be considered. This will give a quantitative and qualitative impression
of the size and location of the rotator cuff tear and, more important,
the status of the rotator cuff muscle bellies. These studies can
provide the surgeon with an assessment for the reparability of a
rotator cuff tear. They can also provide qualitative information about
the status of the muscle bellies of the cuff muscles. Most patients
with advanced rotator cuff tear arthropathy with adaptive and
degenerative changes seen on plain films will not require advanced
imaging studies such as CT scan or MRI, however.
|
TABLE 45-1 Clinical Features of Cuff Tear Arthropathy
|
|||||
|---|---|---|---|---|---|
|
 |
|
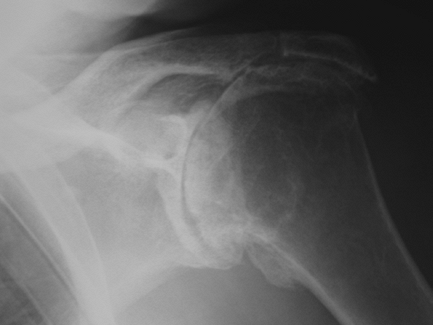
Figure 45-1
Anteroposterior radiograph of a left shoulder with characteristic cuff tear arthropathy changes: humeral head elevation, adaptive changes on the acromion, and greater tuberosity. There are degenerative joint changes in the glenohumeral joint. |
superior wear with significant adaptive changes and concavity of the
acromion. There can be more of a centralized wear pattern between the
humeral head and significant loss of glenoid bone stock. There can also
be seen a more massive destructive arthropathy between the humeral
head, glenoid, and acromion. It is unclear if these are three different
points on the time line of degeneration, or if the shoulder responds
differently with differing degenerative patterns to the chronic cuff
deficiency. There has been no validated staging or classification of
these radiographic changes or of clinical function. To make matters
more confusing, not every shoulder with an irreparable rotator cuff
tear goes on to painful, symptomatic cuff tear arthropathy.
|
TABLE 45-2 Radiographic Features of Cuff Tear Arthropathy
|
|||||
|---|---|---|---|---|---|
|
 |
|
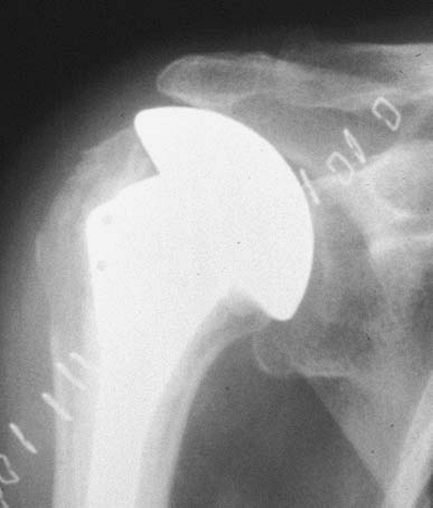
Figure 45-2
This patient exhibits anterosuperior instability with attempted active elevation. There was previous rotator cuff repair failure with coracoacromial arch violation. Hemiarthroplasty will not correct the anterosuperior instability. A reverse shoulder replacement is a better option. |
not hard to make the diagnosis based on history, physical exam, and
radiologic findings. Other conditions also need to be considered. The
cause of the rotator cuff deficiency leading to the arthritis and
shoulder dysfunction is important to know. Other diagnostic
possibilities include rheumatoid arthritis, neuropathic arthropathy,
septic arthritis, and failed rotator cuff repair with loss of
coracoacromial arch containment. Rheumatoid arthritis will usually have
multiple joint involvement. Neuropathic arthropathy is most commonly
caused by syringomyelia. An MRI of the cervical spine will aid in the
diagnosis. Rotator cuff repair failure with anterosuperior instability
will be apparent by history of previous surgery, physical exam, and
MRI. The patients with multiple failed rotator cuff repair will
manifest anterosuperior instability with attempted elevation (Fig. 45-2).
The degenerative changes on the humerus, acromion, and glenoid will not
be as advanced as those seen with CTA. Function is poor and pain is
significant in this population with cuff deficiency and joint injury.
involves history, physical examination, standard radiographs, blood
work to rule out infection or rheumatoid arthritis, and routine blood
work. Joint aspiration is rarely indicated unless septic arthritis is
suspected.
injection to decrease the inflammation and fluid production and to
control the pain and allow the patient to rehabilitate. Physical
therapy should focus on the structures that are left, which are
typically some of the external rotators, some of the internal rotators,
and the anterior deltoid. These exercises can be done at home. They
should be done without pain, and isometrics and closed chain technique
is easiest in the elderly population. This can help patients gain
another 5, 10, or 15 degrees of motion and stability. This can be a
significant gain for these patients with regard to using the hand away
from the body. If pain relief can be maintained, patients can be quite
satisfied with these gains. Realistic expectations for active motion,
strength, and function should be emphasized to the patient.
relief. As stated earlier, the active forward elevation and shoulder
function ability of patients in this disease process can be somewhat
variable. Some patients have almost no pain but extremely poor function
with the inability to actively elevate above the horizontal or even use
the hand away from the body at waist height. This patient is much more
of a challenge because they have a painless pseudoparalysis of the
shoulder. Hemiarthroplasty will not restore active elevation ability in
a patient who has pseudoparalysis. Any surgery on cuff tear arthropathy
is a limited-goals procedure for pain relief and improved function of
the shoulder for activities of daily living. The ability to actively
elevate above the horizontal will be unpredictable.
conservative management and has had no previous coracoacromial arch
surgery, and who has active elevation ability of 60 degrees or better,
the best treatment option for rotator cuff tear arthropathy seems to be
hemiarthroplasty. There is no advantage to total shoulder arthroplasty
with resurfacing of the glenoid in an unconstrained shoulder design.
Bipolar shoulder hemiarthroplasty has poorer active elevation ability
than hemiarthroplasty. Arthrodesis is poorly tolerated in the elderly
population and is not recommended.
relieve pain in cuff tear arthropathy. Functional ability, specifically
active elevation, has been less predictable, however. At best, patients
and surgeons should expect active elevation on the average to be
approximately 90 degrees. With longer follow-up, hemiarthroplasty has
shown progressive bone changes in the acromion and glenoid. These
changes have correlated with increasing pain and decreasing function.
It is unclear why some patients do better than others with regard to
active elevation and shoulder function. No prognostic factor has been
identified to correlate with a better functional result. However, it is
quite clear that poorer results are associated with those patients who
had prior rotator cuff surgery and coracoacromial arch violation. If
there has been coracoacromial arch violation, hemiarthroplasty is not
indicated, as anterosuperior instability will result.
the United States in 2004. It had been used in Europe for >8 years.
The reverse shoulder arthroplasty is indicated for cuff deficiency and
joint injury when no other satisfactory option is available (Table 45-3). Specific indications
include CTA with a pseudoparalysis clinical picture. If there is
extremely poor active elevation, hemiarthroplasty will not predictably
restore elevation ability. If there has been previous coracoacromial
arch violation or there is anterosuperior instability of the humeral
head, then reverse is a better option. If there is a failed
hemiarthroplasty for CTA or fracture, then reverse is a better option.
In age-matched populations with CTA and no previous surgery, the
reverse arthroplasty achieved an average of 40 degrees greater active
forward elevation compared with hemiarthroplasty. The reverse provides
for the potential for better active elevation ability. However, both
internal and external rotation can be limited owing to the constraint
of the reverse design.
|
TABLE 45-3 Indication for Reverse Shoulder Arthroplasty
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
patients who have had multiple failed rotator cuff repair attempts with
violation of the coracoacromial arch and present with pain, poor
function, and anterior superior instability. It should also be
considered in those patients with pseudoparalysis and extremely poor
active motion. Those patients with an extremely thin acromion or an
acromial insufficiency fracture should also be considered candidates
for reverse shoulder arthroplasty.
arthropathy begins with a thorough preoperative evaluation. The vast
majorities of these patients are elderly, older than 62 years of age,
and have comorbidities. Positioning is important. The patient should be
moved to the lateral edge of the operating room table. The operative
arm should be able to be brought off the side of the table for gentle
extension, external rotation, and adduction to dislocate the humeral
head forward. The head and neck need to be supported. The shoulder and
arm are draped free for maximum flexibility and position.
the anterior deltoid. The cephalic vein can be taken laterally with the
deltoid or medially with the pectoralis major according to the
surgeon’s preference. Extensive bursal material will be encountered
under the deltoid and under the clavipectoral fascia lateral to the
strap muscles off the coracoid. This material should be debrided. The
subscapularis should be incised off the lesser tuberosity. The
subscapularis should be tagged with sutures and reflected medially.
dislocated. These patients are typically females older than 65 years of
age with osteopenic bone. Great care should be taken to gently distract
the arm and put a flat retractor behind the humeral head; with
extension, adduction, and external rotation the humeral head is brought
forward. The humeral head should be osteotomized with an oscillating
saw. Careful reaming of the humeral canal should be performed owing to
osteopenic bone. In the vast majority of these cases, the humeral stem
is cemented into place. Also, cement will stabilize the proximal aspect
of the humerus and support sutures that are placed through the anterior
anatomic neck for subscapularis reattachment.
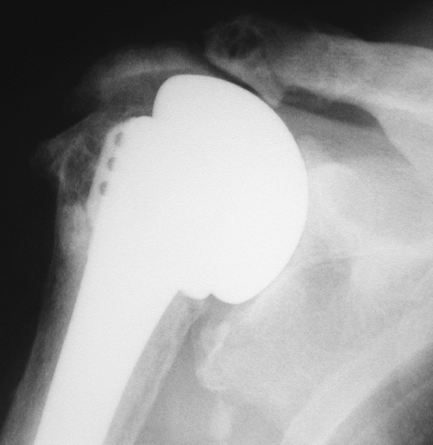
General guidelines can be thought of as choosing a humeral head size
that will fill the existing coracoacromial arch (Fig. 45-3).
It is helpful to have a prosthetic head that allows approximately 50%
of posterior translation on the glenoid. With the arm in approximately
70 degrees of abduction, at least 40 degrees of internal rotation of
the arm should occur.
after relocation of the new prosthesis in the joint. A drain may or may
not be used underneath the deltoid. In many patients, because of the
amount of bursal material and fluid production that needed to be
debrided, there can be significant dead space. A drain for 24 hours may
prevent a collection of a hematoma. The deltopectoral interval is then
tacked
closed with absorbable sutures. The subcutaneous tissue is closed with
absorbable sutures and then the skin closed by surgeon preference. A
supportive sling and swathe device can be applied.
 |
|
Figure 45-3
Hemiarthroplasty for cuff tear arthropathy. Note that the prosthetic head size fills the arch of the upper glenoid and coracoacromial arch without overstuffing the joint. |
arthropathy should be supported in a sling. Passive range of motion
should begin on the first postoperative day with pendulum exercises.
Passive external rotation with a limit of 30 degrees, passive forward
elevation with a limit of approximately 90 degrees, and pulley
exercises should be instituted. The patient is encouraged to use the
hand, wrist, and elbow for activities of daily living within the sling.
After 1 month, the sling can be discontinued and active assisted range
of motion can begin. Isometric strengthening for the muscle groups that
are still workable are instituted. These include the external rotators,
all three heads of the deltoid, and the scapular rotators. At the end
of 2 months, light resistive exercises with resistive exercise bands
should be instituted for the external rotators, the internal rotators,
and all three heads of the deltoid. Patients should be informed both
preoperatively and postoperatively that this will be a prolonged and
slow rehabilitation. They will not reach their best or maximum
potential for approximately 6 months after the operation.
relief that hemiarthroplasty can provide to patients who have
unremitting pain from the degenerative changes of arthritis with cuff
deficiency. This has also been shown to be the most consistent when
there have not been previous attempts at rotator cuff repair or
acromioplasty/coracoacromial arch violation type surgery. The average
active forward elevation that patients can expect from a
hemiarthroplasty for cuff tear arthropathy is approximately 90 degrees.
Most studies have 2-year follow-up, but longer-term follow-up studies
are being reported. These studies show that there is progressive bony
erosion of the acromion and superior glenoid and that these erosions
correlate with pain and decreasing function over the longer periods of
time.
arthroplasty is through the deltopectoral approach. It has also been
described through the superior approach by incising the deltoid off the
anterior acromion and repairing the deltoid. The technical
considerations are to obtain exposure to the glenoid that is not needed
in hemiarthroplasty. The humeral head is resected, and the glenoid
component is placed in the inferior aspect of the glenoid. The inferior
capsule needs to be elevated off the glenoid rim and the glenoid
component placed inferiorly. The component should be placed at neutral
or at best a slight inferior tilt. These technical tips can avoid
scapular notching inferiorly. The humeral component is placed in
approximately 10 degrees of retroversion. The myofascial sleeve tension
should allow the humeral component to reduce under the glenoid with a
1- to 2-mm push-pull action. The strap muscles will be under tension.
The humerus should be cemented.
hemiarthroplasty; however, the author rarely has patients do formal
therapy after a reverse shoulder arthroplasty. A sling is used for 3 to
4 weeks. Patients are allowed to do activities of daily living in the
sling immediately. Closed chain exercises for the anterior deltoid and
isometrics for external and internal rotation are begun. The reverse
will allow the scapula to function more efficiently, and patients
progress very well on their own with surgeon direction.
follow-up, patients with no prior shoulder surgery and CTA were treated
either with hemiarthroplasty or reverse shoulder arthroplasty. The
patients with reverse shoulder arthroplasty had 40 degrees greater
active forward elevation for an average of 138 degrees, and the
Constant score was 20 points higher than for those patients with
hemiarthroplasty. There were no cases of glenoid loosening requiring
revision. The hemiarthroplasties had more than one third of the cases
with progressive bone erosion in the superior glenoid and acromion with
increasing pain.
comorbidities. Medical problems can be exacerbated by surgery in the
elderly. The unpredictable function results, especially with regard to
strength and active forward elevation, make it imperative that a
discussion occurs with the patient to avoid unrealistic expectations.
One of the complications that has recently been seen after 4- to 5-year
follow-up is the bone erosion that is progressive at the superior
glenoid and the undersurface of the acromion that correlates with
increasing pain and decreasing function (Fig. 45-4).
 |
|
Figure 45-4 Hemiarthroplasty with progressive superior glenoid erosion. Increasing pain and decreasing function were noted by the patient.
|
dislocation, hematoma formation, infection, implant failure, and
scapular notching inferior to the glenoid component. The complication
rate is higher than with hemiarthroplasty, but these complications do
not seem to affect the results of the operation. Glenoid loosening has
been rare, but is a concern with longer-term follow-up.
shoulder found in elderly patients. It is variable in its presentation
with regard to the extent of degenerative osseous change in the
glenoid, humeral head, and acromion. It is variable in its presentation
with regard to preoperative active elevation ability and pain level.
The overriding indication for operative intervention in cuff tear
arthropathy is pain relief.
A, Edwards TB, Walch G, et al. Early results of a reverse design
prosthesis in the treatment of arthritis of the shoulder in elderly
patients with a large rotator cuff tear. Orthopedics. 2002; 25:129-133.
L, Lautmann S, Sirveaux F, et al. Hemiarthroplasty versus reverse
arthroplasty in the treatment of osteoarthritis with massive rotator
cuff tear. In: Walch G, Boileau P, Mole D, eds. 2000 Shoulder Prostheses. … Two to Ten Year Follow-up. Montpelier, France: Sauramps Medical; 2001:261-268.
J, Cofield RH, Rowland CM. Shoulder hemiarthroplasty for glenohumeral
arthritis associated with severe rotator cuff deficiency. J Bone Joint Surg. 2001; 83A:1814-1822.
CML, Steinmann PA, Gilbart M, et al. Treatment of painful pseudoparesis
due to irreparable rotator cuff dysfunction with the Delta III
reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg. 2005; 87A:1776-1786.
