Subtrochanteric Fractures
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > IV – Lower Extremity Fractures and Dislocations > 31 – Subtrochanteric Fractures
31
Subtrochanteric Fractures
ANATOMY
-
A subtrochanteric femur fracture is a fracture between the lesser trochanter and a point 5 cm distal to the lesser trochanter.
-
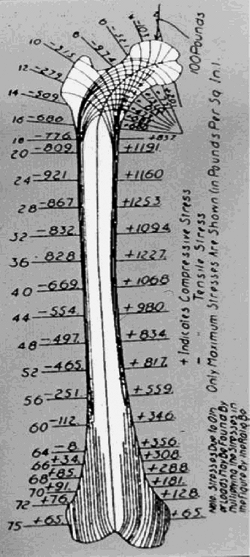
The subtrochanteric segment of the femur
is the site of very high biomechanical stresses. The medial and
posteromedial cortices are the sites of high compressive forces,
whereas the lateral cortex experiences high tensile forces (Fig. 31.1). -
The subtrochanteric area of the femur is
composed mainly of cortical bone. Therefore, there is less vascularity
in this region, and the potential for healing is diminished as compared
with intertrochanteric fractures. -
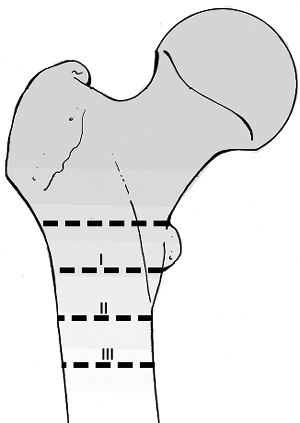
The deforming muscle forces on the
proximal fragment include abduction by the gluteus, external rotation
by the short rotators, and flexion by the psoas. The distal fragment is
pulled proximally and into varus by the adductors (Fig. 31.2).
MECHANISM OF INJURY
-
Low-energy mechanisms: Elderly individuals sustain a minor fall in which the fracture occurs through weakened bone.
-
High-energy mechanisms: Younger adults
with normal bone sustain injuries related to motor vehicle accidents,
gunshot wounds, or falls from a height. -
Pathologic fracture: The subtrochanteric
region is also a frequent site for pathologic fractures, accounting for
17% to 35% of all subtrochanteric fractures. -
Ten percent of high-energy subtrochanteric fractures result from gunshot injuries.
CLINICAL EVALUATION
-
Patients involved in high-energy trauma should receive full trauma evaluation.
-
Patients typically are unable to walk and have varying degrees of gross deformity of the lower extremity.
-
Hip motion is painful, with tenderness to palpation and swelling of the proximal thigh.
-
Because substantial forces are required
to produce this fracture pattern in younger patients, associated
injuries should be expected and carefully evaluated. -
Field dressings or splints should be
completely removed, with the injury site examined for evidence of soft
tissue compromise or open injury. -
The thigh represents a compartment into
which volume loss from hemorrhage may be significant; monitoring for
hypovolemic shock should thus be undertaken, with invasive monitoring
as necessary. -
Provisional splinting (i.e., traction
pin) until definitive fixation should be performed to limit further
soft tissue damage and hemorrhage. -
A careful neurovascular examination is
important to rule out associated injuries, although neurovascular
compromise related to the subtrochanteric fracture is uncommon.
P.339
 |
|
Figure
31.1. Koch’s diagram showing the compression stress on the medial side and the tension stress on the lateral side of the proximal femur. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
RADIOGRAPHIC EVALUATION
-
An anteroposterior (AP) view of the pelvis and AP and lateral views of the hip and femur should be obtained.
-
One should assess the entire femur including the knee.
-
Associated injuries should be evaluated, and if suspected, appropriate radiographic studies ordered.
-
A contralateral scanogram is helpful to determine femoral length in highly comminuted fractures.
CLASSIFICATION
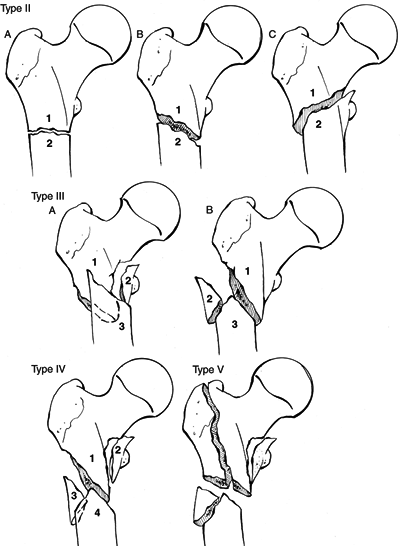
Fielding (Fig. 31.3)
This is based on the location of the primary fracture line in relation to the lesser trochanter.
| Type I: | At the level of the lesser trochanter |
| Type II: | <2.5 cm below the lesser trochanter |
| Type III: | 2.5 to 5 cm below the lesser trochanter |
 |
|
Figure
31.2. The deforming force by the unopposed pull of the iliopsoas causes the proximal femur in flexion and external rotation. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
 |
|
Figure 31.3. Fielding classification of subtrochanteric fractures.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
P.340
P.341
Seinsheimer (Fig. 31.4)
 |
|
Figure 31.4. Seinsheimer classification of subtrochanteric fractures.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
This is based on the number of major bone fragments and the location and shape of the fracture lines.
| Type I: | Nondisplaced fracture or any fracture with <2 mm of displacement of the fracture fragments, regardless of pattern |
| Type II: | Two-part fractures |
| IIA: | Two-part transverse femoral fracture |
| IIB: | Two-part spiral fracture with the lesser trochanter attached to the proximal fragment |
| IIC: | Two-part spiral fracture with the lesser trochanter attached to the distal fragment (reverse obliquity pattern) |
| Type III: | Three-part fractures |
| IIIA: | Three-part spiral fracture in which the lesser trochanter is part of the third fragment, which has an inferior spike of cortex of varying length |
| IIIB: | Three-part spiral fracture of the proximal third of the femur, with the third part a butterfly fragment |
| Type IV: | Comminuted fracture with four or more fragments |
| Type V: | Subtrochanteric-intertrochanteric fracture, including any subtrochanteric fracture with extension through the greater trochanter |
P.342
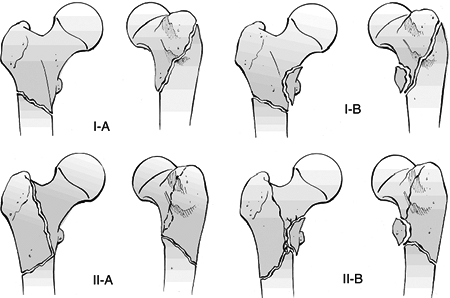
Russell-Taylor (Fig. 31.5)
 |
|
Figure 31.5. Russell-Taylor classification of subtrochanteric fractures.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
This was created in response to the development of first- and second-generation interlocked nails.
| Type I: | Fractures with an intact piriformis fossa in which: |
| IIA: | The lesser trochanter is attached to the proximal fragment. |
| IIB: | The lesser trochanter is detached from the proximal fragment. |
| Type II: | Fractures that extend into the piriformis fossa and: |
| IIA: | Have a stable medial construct (posteromedial cortex). |
| IIB: | Have comminution of the piriformis fossa and lesser trochanter, associated with varying degrees of femoral shaft comminution. |
P.343
OTA Classification of Subtrochanteric Fractures
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
TREATMENT
Nonoperative
-
This involves skeletal traction in the 90/90-degree position followed by spica casting or cast bracing.
-
This is reserved only for those elderly individuals who are not operative candidates and for children.
-
Nonoperative treatment generally results
in increased morbidity and mortality in adults, as well as in nonunion,
delayed union, and malunion with varus angulation, rotational
deformity, and shortening.
Operative
-
Operative treatment is indicated in most subtrochanteric fractures
Implants
INTERLOCKING NAIL
-
First-generation (centromedullary) nails are indicated for subtrochanteric fractures with both trochanters intact.
-
Second-generation cephalomedullary (i.e.,
reconstruction) nails are indicated for fractures with loss of the
posteromedial cortex. -
Second-generation nails can also be used
for fractures extending into the piriformis fossae, but they are
technically more difficult to insert. -
Nails that utilize either a piriformis or greater trochanteric starting point can be used.
-
With use of an intramedullary nail, one
must monitor for the nail exiting posteriorly out of the proximal
fragment. One must also monitor for the common malalignment of varus
and flexion of the proximal fragment.
NINETY-FIVE-DEGREE FIXED ANGLE DEVICE
-
The 95-degree fixed angle plates are best
suited for fractures involving both trochanters; an accessory screw can
be inserted beneath the fixed angle blade or screw into the calcar to
increase proximal fixation (Fig. 31.6). -
These devices function as a tension band when the posteromedial cortex is restored.
-
A dynamic condylar screw is technically easier to insert than a blade plate.
-
One must take care not to devitalize the fracture fragments during fracture reduction and fixation.
SLIDING HIP SCREW
-
This is generally not indicated for subtrochanteric fractures except those with intertrochanteric extension.
P.344
Bone Grafting
 |
|
Figure 31.6. A subtrochanteric fracture fixed with a fixed angle blade plate and bone graft on the posteromedial cortex.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Closed reduction techniques have
decreased the need for bone grafting, because fracture fragments are
not devascularized to the same extent as in open reduction. -
If needed, it should be inserted through the fracture site, usually before plate application.
Open Subtrochanteric Fractures
-
These are rare, almost always associated
with either penetrating injury or high-energy trauma from a motor
vehicle accident or a fall from a height. -
Treatment consists of immediate surgical debridement and osseous stabilization.
COMPLICATIONS
Loss of Fixation
-
With plate and screw devices, implant
failure usually occurs secondary to screw cutout from the femoral head
and neck in patients with osteopenic bone or plate breakage. -
With interlocked nails, loss of fixation
is commonly related to failure to lock the device statically,
comminution of the entry portal, or use of smaller-diameter nails. -
Fixation failure involves removal of
hardware, revision internal fixation with either plate and screws or an
interlocked nail, and bone grafting.
P.345
Nonunion
-
This may be evident by a patient’s inability to resume full weight bearing within 4 to 6 months.
-
Symptoms are pain about the proximal thigh and pain on attempted weight bearing.
-
Nonunion usually occurs in the femoral shaft portion of the fracture.
-
Nonunions that develop following
intramedullary nailing can be treated by implant removal followed by
repeat reaming and placement of a larger-diameter intramedullary nail.
Malunion
-
The patient may complain of a limp, leg length discrepancy, or rotational deformity.
-
Coxa varus is mainly the result of the uncorrected abduction deformity of the proximal segment caused by the hip abductors.
-
A valgus osteotomy and revision internal fixation with bone grafting are the usual treatment for a varus malreduction.
-
Leg length discrepancy is a complex
problem that is more likely to occur following a fracture with
extensive femoral shaft comminution stabilized with a dynamically
locked rather than a statically locked nail. -
Malrotation may occur with use of plate
and screws or an intramedullary nail if the surgeon is not alert to
this potential complication.
