Acetabular Fractures: Ilioinguinal Approach
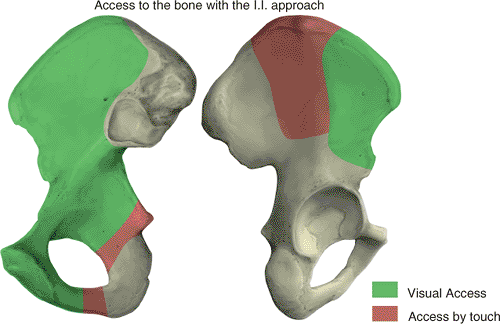
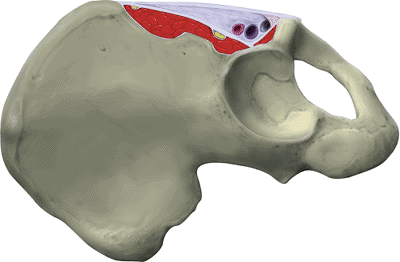
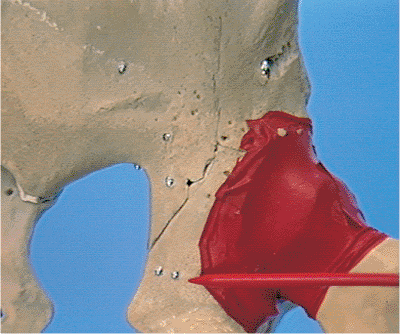
an approach to the anterior column of the acetabulum and the inner
aspect of the innominate bone. It allows exposure of the entire,
internal, iliac fossa and pelvic brim from the anterior aspect of the
sacroiliac joint to the pubic symphysis. The quadrilateral surface of
the innominate bone and the superior and inferior rami are also
accessible. Access to a portion of the external aspect of the ilium
also is possible (Fig. 42.1).
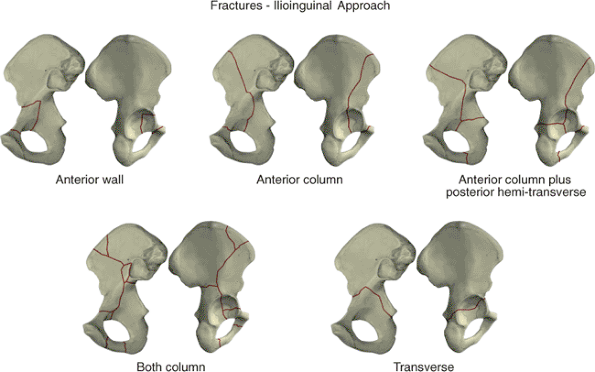
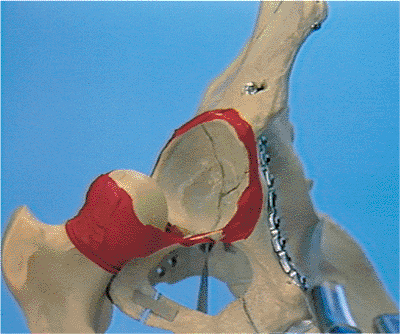
fractures of the anterior wall and column. The majority of acute,
associated, anterior-plus-posterior, hemitransverse fractures may also
be managed with the ilioinguinal approach. If the fracture is older
than 15 days, the ilioinguinal may still be used unless the posterior
component of the fracture is significantly displaced. In this
circumstance, an extended iliofemoral approach is more applicable.
of associated both-column fractures. The presence of a fracture
involving the posterior wall does not necessarily preclude the use of
this approach. If the posterior-wall fragment contains a spike of
ilium, the reduction may be possible through the exposure of the
lateral ilium. The ilioinguinal approach is not recommended for an
associated both-column fracture with small or comminuted posterior-wall
fragments or those with fracture involvement of the sacroiliac joint.
the ilioinguinal approach. Specifically, fractures with significant
displacement at the pelvic brim but slight or no displacement
posteriorly may be addressed in this manner. In addition, the
ilioinguinal may be used as a subsequent approach when incomplete
reduction of the anterior column portion of a T-shaped fracture has
been obtained through a prior Kocher-Langenbeck approach (Fig. 42.2).
 |
|
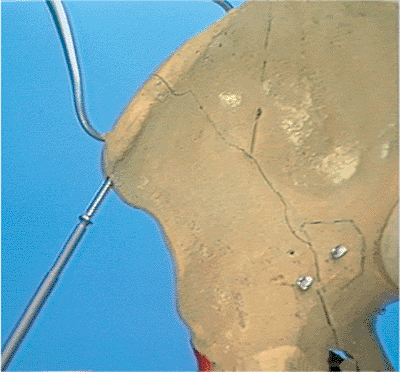
Figure 42.1. Access to the innominate bone with the ilioinguinal approach. (Redrawn with permission from
J. M. Matta, Surgical Approaches to Fractures of the Acetabulum and Pelvis. Copyright © J. M. Matta, 1996.
) |
 |
|
Figure 42.2. Fractures addressed through the ilioinguinal approach. (Redrawn with permission from
J. M. Matta, Surgical Approaches to Fractures of the Acetabulum and Pelvis. Copyright © J. M. Matta, 1996.
) |
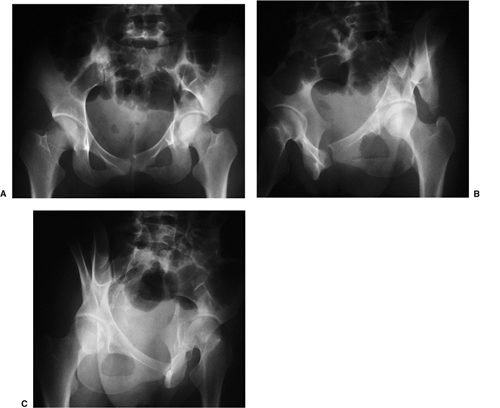
acetabulum fracture should include an anteroposterior (AP) pelvic
radiograph and 45-degree oblique views of the pelvis. Although
obtaining these views may be initially uncomfortable for the patient,
they are vital to fully understand the fracture pattern. Adequate
analgesia should be provided, and the physician may need to be on-site
to ensure proper positioning. These films should be obtained in the
radiology department rather than as portable radiographs and with the
patient out of traction. A careful evaluation of the radiographs allows
the fracture to be classified properly by determination of the exact
fracture pattern.
information regarding the fracture configuration and presence of
incarcerated or impacted fragments within the acetabulum.
Three-dimensional CT reconstructions also can assist in providing a
better understanding of complicated fracture patterns. Drawing the
fracture on a dry bone or pelvic model (or drawing the innominate bone)
helps ensure that the surgeon understands the fracture configuration
before embarking on surgical intervention.
areas infrequently used by most orthopedic surgeons. In addition,
reduction of the fracture and proper placement of fixation require a
thorough understanding of the fracture pattern and the normal
acetabular anatomy. Before undertaking the approach, the surgeon is
strongly advised to practice on a cadaver and to assist a surgeon who
is familiar with the exposure, reduction, and fixation of these
difficult injuries.
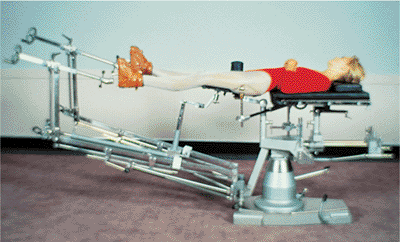
The affected leg is positioned with the hip slightly flexed to relax
the iliopsoas muscle, femoral nerve, and external iliac vessels. If
required during the surgery, a lateral traction device may be used
through a traction screw placed into the greater trochanter. Before
surgery, a Foley catheter is introduced into the bladder.
 |
|
Figure 42.3.
Patient positioned on the Judet–Tasserit fracture table. The hip is flexed to relax the iliopsoas and external iliac vessels. The lateral traction device is demonstrated. (Redrawn with permission from J. M. Matta, Surgical Approaches to Fractures of the Acetabulum and Pelvis. Copyright © J. M. Matta, 1996.
) |
 |
|
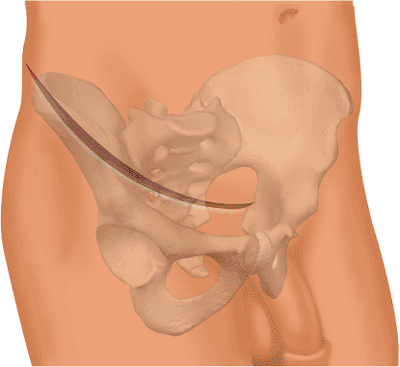
Figure 42.4.
Skin incision for the ilioinguinal approach. The incision begins 3 to 4 cm above the symphysis pubis and must extend beyond the most convex portion of the ilium. (Redrawn with permission from J. M. Matta, Surgical Approaches to Fractures of the Acetabulum and Pelvis. Copyright © J. M. Matta, 1996.
) |
 |
|
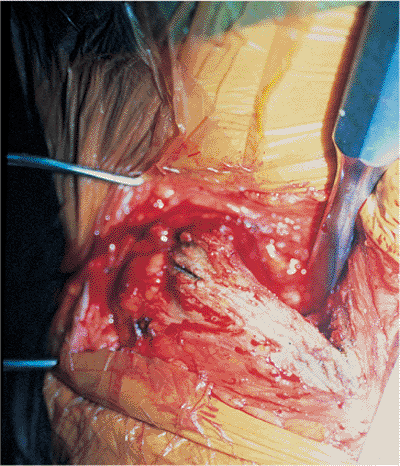
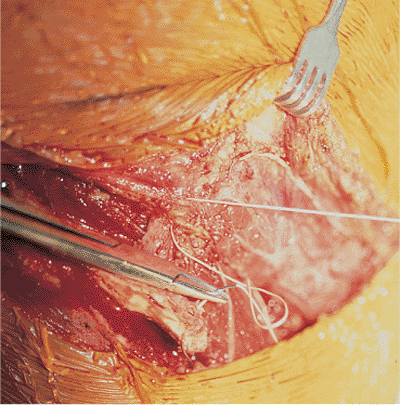
Figure 42.5. Release of the insertion of the abdominal muscles and subperiosteal dissection of the internal iliac fossa.
|
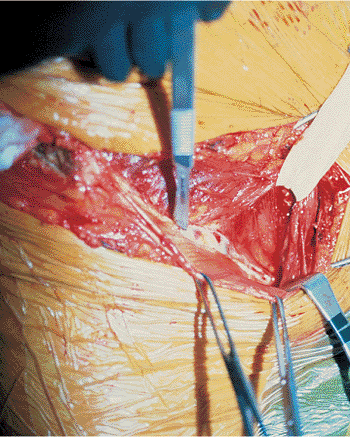
to the symphysis pubis. It proceeds laterally to the anterior,
superior, iliac spine and then along the anterior two thirds of the
iliac crest. The incision must extend beyond the most convex portion of
the ilium (Fig. 42.4). The periosteum is
incised along the iliac crest, and the attachment of the abdominal
muscles and the origin of the iliacus are released. By subperiosteal
dissection, the iliacus is elevated from the internal iliac fossa as
far posterior as the sacroiliac joint and medially to the pelvic brim (Fig. 42.5).
The internal iliac fossa is then packed for hemostasis. Through the
lower portion of the incision, the aponeurosis of the external oblique
muscle and the external rectus abdominis fascia are exposed. These
structures are sharply incised in line with the cutaneous incision at
least 1 cm proximal to the external inguinal ring. The aponeurosis of
the external oblique muscle is then reflected distally. This unroofs
the inguinal canal and exposes the inguinal ligament. The spermatic
cord or round ligament is visualized at the medial aspect of the
incision. A Penrose drain is then placed around the spermatic cord or
round ligament and the adjacent ilioinguinal nerve. It may be used to
facilitate retraction during the procedure (Fig. 42.6).
2-mm cuff of the ligament remains with the common origin of the
internal oblique and transversus abdominis muscles and the
transversalis fascia (Fig. 42.7). Great care
must be taken to avoid injuring the underlying neurovascular
structures. Immediately beneath the inguinal ligament, the lateral
femoral-cutaneous nerve exits into the thigh. This nerve may be found
adjacent to or up to 3 cm medial to the anterior, superior, iliac
spine. It must be identified and protected throughout the operation.
Directly beneath the midportion of the incision lie the external iliac
vessels (Fig. 42.8). Medial to these vessels,
the insertion of the conjoined tendon onto the pubis is incised. It may
be necessary to incise a portion of the rectus abdominis tendon as
well; it is incised just above its insertion onto the pubis. The
retropubic space of Retzius is now accessible and is packed with moist
sponges after evacuation of the fracture hematoma.
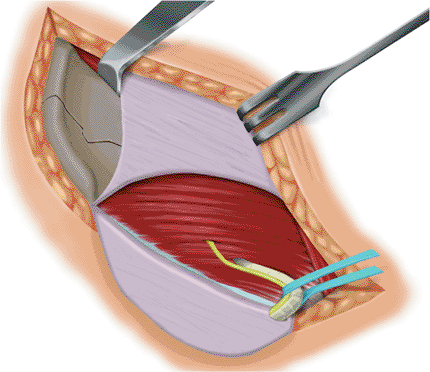
vessels and the surrounding lymphatics are exposed in the midportion of
the incision within the lacuna vasorum. The more laterally situated
lacuna musculorum contains the iliopsoas, the femoral nerve, and the
lateral
femoral cutaneous nerve. The iliopsoas sheath, or iliopectineal fascia, separates the two lacunae (Fig. 42.9).
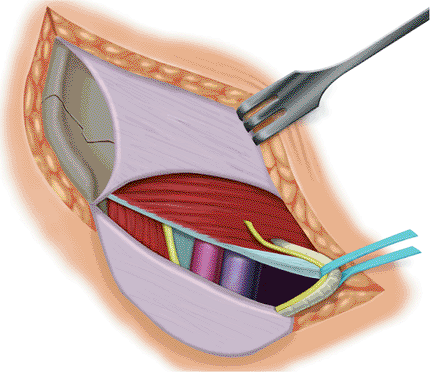
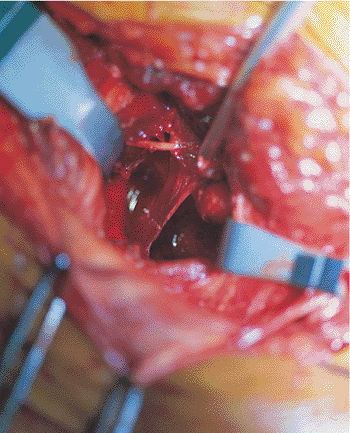
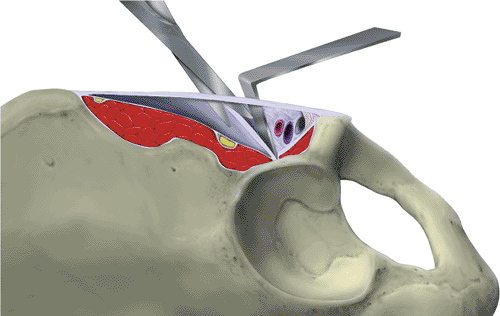
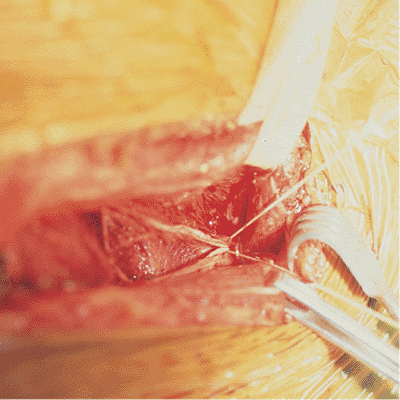
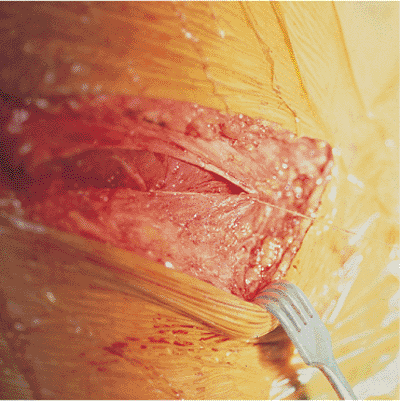
The vessels and lymphatics are carefully dissected away and retracted
from the medial aspect of the fascia, and the iliopsoas muscle and
femoral nerve are retracted from the lateral aspect (Figs. 42.10 and 42.11). The iliopectineal fascia is sharply incised to the pectineal eminence (Fig. 42.12).
The pulse of the external iliac artery should be palpated before this
step to ensure that the vascular bundle is protected from injury. The
iliopectineal fascia is sharply detached from the pelvic brim (Fig. 42.13).
In certain individuals, this occasionally may be performed with finger
dissection. Detaching the iliopsoas fascia allows access to the true
pelvis and subsequently the quadrilateral surface and the posterior
column. A second Penrose drain is placed around the iliopsoas; femoral
nerve;
and
lateral, femoral, cutaneous nerve for retraction purposes. A third
Penrose is placed around the femoral vessels and lymphatics. Care
should be taken to leave undisturbed the fatty areolar tissue
surrounding the vessels, as this contains the lymphatic vessels.
Disrupting the lymphatics may result in impaired postoperative
lymphatic drainage and edema.
 |
|
Figure 42.6.
Inguinal canal has been unroofed, and the external oblique aponeurosis is reflected inferiorly. The ilioinguinal nerve and the spermatic cord are protected by a Penrose drain. The inguinal ligament is identified. (Redrawn with permission from J. M. Matta, Surgical Approaches to Fractures of the Acetabulum and Pelvis. Copyright © J. M. Matta, 1996.
) |
 |
|
Figure 42.7.
Abdominal muscles and transversalis fascia have been detached from the inguinal ligament. A 1-mm cuff of ligament remains for closure. (Redrawn with permission from J. M. Matta, Surgical Approaches to Fractures of the Acetabulum and Pelvis. Copyright © J. M. Matta, 1996.
) |
 |
|
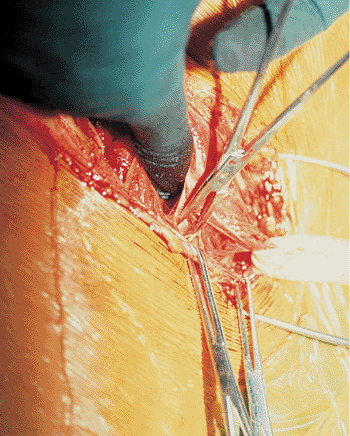
Figure 42.8.
Directly beneath the inguinal ligament lie the external iliac vessels. Note how superficial the external iliac artery and vein may lie beneath the ligament. |
 |
|
Figure 42.9.
In this oblique section at the level of the inguinal ligament, the iliopectineal fascia separates the lacuna musculorum and the lacuna vasorum. (Redrawn with permission from J. M. Matta, Surgical Approaches to Fractures of the Acetabulum and Pelvis. Copyright © J. M. Matta, 1996.
) |
 |
|
Figure 42.10.
External iliac vessels and lymphatics are dissected away from the medial aspect of the iliopectineal fascia. The iliopsoas and femoral nerve have already been dissected away from the lateral aspect of the fascia and are retracted by the surgeon’s finger. |
 |
|
Figure 42.11.
The iliopsoas and femoral nerve are retracted laterally, and the external iliac vessels are retracted medially, exposing the iliopectineal fascia. |
 |
|
Figure 42.12.
This oblique section demonstrates the division of the iliopectineal fascia from the inguinal ligament to the pectineal eminence. (Redrawn with permission from J. M. Matta, Surgical Approaches to Fractures of the Acetabulum and Pelvis. Copyright © J. M. Matta, 1996.
) |
 |
|
Figure 42.13. Iliopectineal fascia is dissected free from its attachment to the pelvic brim. (Redrawn with permission from
J. M. Matta, Surgical Approaches to Fractures of the Acetabulum and Pelvis. Copyright © J. M. Matta, 1996.
) |
iliopectineal nerve and artery should be identified posteromedial to
the vessels. A search is made for an anomalous origin of the obturator
artery from the inferior epigastric artery or the presence of an
anastomosis between the obturator and the external iliac vessels.
Whereas the presence of a venous anastomosis is relatively common, an
arterial anastomosis is rare. If either of these is present, the artery
or vein or both should be clamped, ligated, and divided to prevent
intraoperative avulsion of the vessel and hemorrhage, which may be
difficult to control.
brim and superior pubic ramus. The periosteum also may be elevated from
the quadrilateral surface. Care should be taken when placing retractors
near the greater sciatic notch to avoid injury to the superior gluteal
vein or branches of the internal iliac artery. The reduction and
fixation of the fracture may now be completed by working back and forth
in the three visualization windows.
allows visualization of the entire internal iliac fossa, the sacroiliac
joint, and the pelvic brim via the first window (Fig. 42.14).
Lateral retraction of the iliopsoas and femoral nerve, combined with
medial retraction of the external iliac vessels, opens the second
window (Fig. 42.15). This window gives access
to the pelvic brim, from the sacroiliac joint to the pectineal
eminence, as well as access to the quadrilateral surface for reduction
of posterior column fractures. The pulse of the external iliac artery
should be frequently checked when working within this window. Medial
retraction of the vessels gives access to the superior pubic ramus and
the symphysis pubis if required (Fig. 42.16). The spermatic cord or round ligament is retracted medially or laterally as needed.
may be obtained by detaching the sartorius and the inguinal ligament
from the anterior, superior, iliac spine and elevating the
tensor
fascia-lata muscle from the ilium. This often facilitates placement of
reduction clamps across the anterior innominate bone.
 |
|
Figure 42.14.
First window of the ilioinguinal approach. The internal iliac fossa is visualized. A Hohmann retractor is placed on the anterior sacroiliac joint. (Redrawn with permission from J. M. Matta, Surgical Approaches to Fractures of the Acetabulum and Pelvis. Copyright © J. M. Matta, 1996.
) |
 |
|
Figure 42.15. Second window of the ilioinguinal approach. The pelvic brim and quadrilateral surface are visualized.
|
 |
|
Figure 42.16.
Third window of the ilioinguinal approach. The symphysis pubis and retropubic space of Retzius are exposed. The spermatic cord or round ligament may be retracted medially or laterally as needed. (Redrawn with permission from J. M. Matta, Surgical Approaches to Fractures of the Acetabulum and Pelvis. Copyright © J. M. Matta, 1996.
) |
are placed in the retropubic space of Retzius as well as along the
quadrilateral surface and internal iliac fossa. The external aspect of
the bone should also be drained if it has been exposed. The abdominal
fascia is sewn to the fascia lata with heavy suture. If the sartorius
has been detached, it is repaired through a drill hole in the anterior,
superior, iliac spine (Fig. 42.17). Muscular
relaxation should be used during closure, and continuous traction is
required to prevent the abdominal fascia from retracting proximally and
posteriorly. If the abdominal muscles are not anatomically repaired, a
sound repair of the floor and roof of the inguinal canal is not
possible. The tendon of the rectus abdominis is repaired, and the
transversalis fascia and the conjoined tendon of the internal oblique
and transversus abdominis muscles are reattached to the inguinal
ligament (Fig. 42.18). The roof of the inguinal canal is repaired by closure of the aponeurosis of the external oblique (Fig. 42.19). The iliopectineal fascia is not repaired.
 |
|
Figure 42.17.
Origins of the sartorius muscle and the abdominal muscles are secured through a drill hole in the anterior, superior, iliac spine. |
 |
|
Figure 42.18.
Inguinal ligament is repaired. Superior are the transversalis fascia and the conjoined tendon of the internal oblique and transversus abdominis muscles. Inferior is the inguinal ligament. |
 |
|
Figure 42.19. Aponeurosis of the external oblique is repaired, closing the roof of the inguinal canal.
|
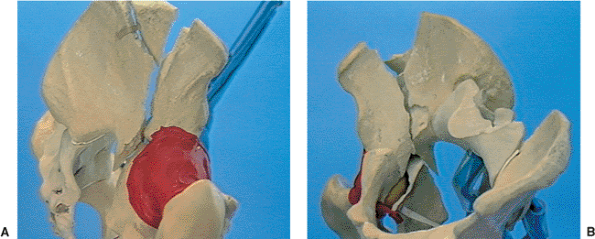
both-column injury is anatomically to reduce the fracture of the
anterior column. The iliac crest and wing are reduced first. The
reduction of fracture lines in the ilium must be perfect if the
articular surface is to be reduced. It is important to restore the
normal concavity to the internal iliac fossa, which is frequently
greater than imagined. Often traction must be applied through the
fracture table to allow disimpaction of the iliac wing. Frequently the
iliac wing fracture bifurcates to reach the iliac crest at two points,
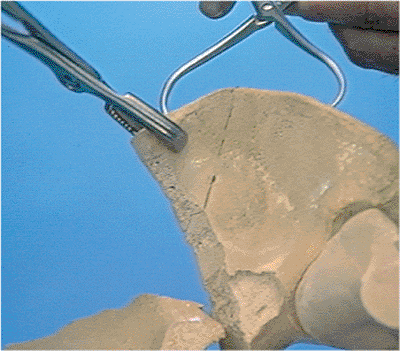
creating a free triangular fragment of the wing (Fig. 42.20).
Because it facilitates the accurate reduction of the anterior column,
this fracture fragment should be anatomically reduced and fixed first. (Fig. 42.21).
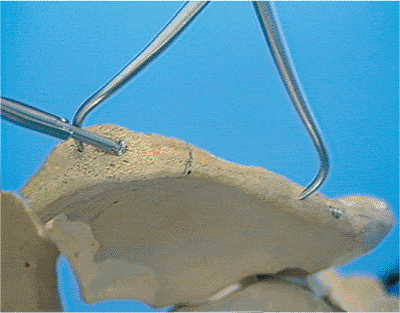
At the level of the iliac crest, a 3.5- or 4.5-mm screw may be inserted
between the tables of the ilium, which will fix the vertical or
triangular fractures (Fig. 42.22). Care must be taken when inserting these screws so reduction is not lost during the
final tightening. Alternatively, a 3.5-mm pelvic plate applied to the
iliac crest may provide more reliable fixation. This implant may be
placed either in the internal iliac fossa just below the crest, or it
may be located directly on the iliac crest. Plates applied directly to
the iliac crest allow the placement of long screws between the two
tables of the iliac wing. However, screws and plates in this location
are often a source of irritation, and this may necessitate their
removal.
 |
|
Figure 42.20. A. Associated both-column fracture of the right acetabulum. View of the lateral aspect of the ilium. B.
Associated both-column fracture of the right acetabulum. Note the free triangular-fracture fragment at the iliac crest. There is also a free fracture fragment at the pelvic brim. (Reprinted with permission from AO/ASIF, Both Column Fracture Through the Ilioinguinal Approach [Video]. Copyright © AO/ASIF Video, 1991.
) |
 |
|
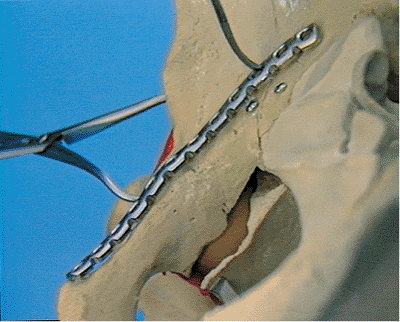
Figure 42.21.
Farabeuf and Weber clamps are used in the reduction of the triangular iliac-crest fracture fragment. (Reprinted with permission from AO/ASIF, Both Column Fracture Through the Ilioinguinal Approach [Video]. Copyright © AO/ASIF Video, 1991.
) |
 |
|
Figure 42.22.
Screw is inserted between the tables of the ilium parallel to the iliac crest while the Weber clamp maintains the reduction. (Reprinted with permission from AO/ASIF, Both Column Fracture Through the Ilioinguinal Approach [Video]. Copyright © AO/ASIF Video, 1991.
) |
pelvic brim is common. Although these free cortical fragments are
extra-articular, it is imperative that they be reduced anatomically and
fixed: The reduction of the anterior column is impossible to judge
without these pieces.
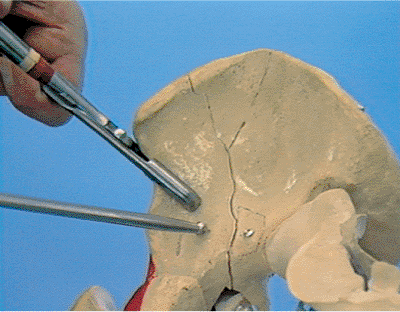
reduction maneuver may be accomplished with the use of the Farabeuf
clamp and ball spike (Fig. 42.23).
Occasionally, clamps placed across the anterior border of the bone may
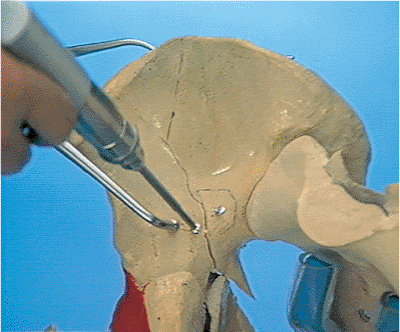
be useful. A screw placed from just lateral to the pelvic brim and
directed toward the sciatic notch will hold the reduction (Fig. 42.24). In addition, a screw may be placed between the tables of the ilium at the level of the iliac crest (Fig. 42.25). A long curved plate is then contoured to the superior aspect
of the pelvic brim. Specialized, precurved, pelvic plates are available
with curvature radii of 88 and 108 degrees. These are designed to fit
the curvature of the typical male and female pelvic brims. This plate
may extend anterior from the front of the sacroiliac joint to the body
of the pubis. The plate has a typical contour, which includes a
concavity for the body of the pubis, a convexity over the pectineal
eminence, and a concavity for the internal iliac fossa (Fig. 24.26). In
addition, the plate must be twisted to match appropriately the contour
of the ilium. Contouring of the plate is frequently time-consuming. It
is important that the plate fit the bone as perfectly as possible to
avoid loss of fracture reduction.
 |
|
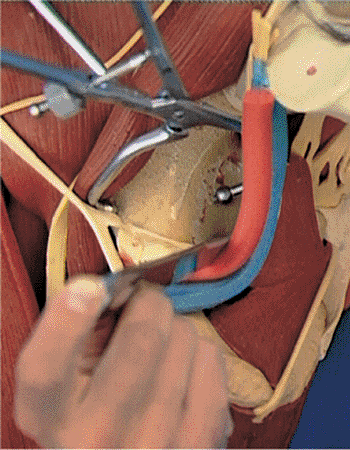
Figure 42.23.
Farabeuf and Weber clamps are used to reduce the anterior column fracture. Note that the fracture fragment from the pelvic brim has been reduced and fixed with a single screw. The accurate reduction of the anterior column is not possible unless the two extra-articular fracture fragments are accurately reduced and stabilized. (Reprinted with permission from AO/ASIF, Both Column Fracture Through the Ilioinguinal Approach [Video]. Copyright © AO/ASIF Video, 1991.
) |
 |
|
Figure 42.24.
Anterior column reduction is held with a screw placed from just lateral to the pelvic brim and directed toward the sciatic notch. (Reprinted with permission from AO/ASIF, Both Column Fracture Through the Ilioinguinal Approach [Video]. Copyright © AO/ASIF Video, 1991.
) |
 |
|
Figure 42.25.
Additional 3.5-mm screw is placed between the tables of the ilium at the level of the iliac crest. (Reprinted with permission from AO/ASIF, Both Column Fracture Through the Ilioinguinal Approach [Video]. Copyright © AO/ASIF Video, 1991.
) |
angled reduction clamp, restoring the profile of the greater sciatic
notch. The reduction clamp is usually placed entirely within the second
window of the approach (Fig. 42.27), but
occasionally a large clamp placed across the anterior border of the
bone is helpful. In most cases, the quadrilateral surface is attached
to the posterior column, and the accuracy of the posterior column
reduction may be assessed by inspecting the reduction of the
quadrilateral surface to the anterior
column. The posterior column fixation is achieved by screws placed parallel to the quadrilateral surface (Fig. 42.28).
These screws may be placed either inside or separate from the
pelvic-brim plate and used to achieve fixation in the retroacetabular
surface (Fig. 42.29). In addition, a screw
started on the anterior pillar of the lateral surface of the ilium and
directed obliquely toward the quadrilateral surface may be used. This
screw may also be used in situations in which a separate fragment of
the quadrilateral surface requires fixation. Comminuted fragments of
the quadrilateral surface are frequently encountered, but these pieces
usually
make up a portion of the cotyloid fossa and do not contribute to the
direct articular portion of the joint or to hip stability. Plates
contoured over the pelvic brim and onto the quadrilateral surface are
not routinely used.
 |
|
Figure 42.26.
Curved pelvic plate is contoured to the innominate bone. Shown is the concavity at the superior ramus, the convexity at the pectineal eminence, and the concavity of the internal iliac fossa. (Reprinted with permission from AO/ASIF, Both Column Fracture Through the Ilioinguinal Approach [Video]. Copyright © AO/ASIF Video, 1991.
) |
 |
|
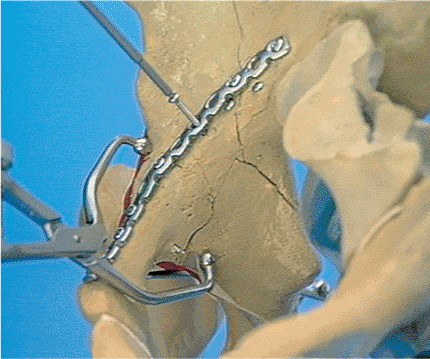
Figure 42.27.
Posterior column fracture is reduced with the use of an angled reduction clamp placed entirely within the second window of the approach. The iliopsoas and femoral nerve are retracted laterally, the external iliac vessels are retracted laterally, and the external iliac vessels are retracted medially. One point of the reduction clamp is on the anterior wall and the other is on the quadrilateral surface. (Reprinted with permission from AO/ASIF, Both Column Fracture Through the Ilioinguinal Approach [Video]. Copyright © AO/ASIF Video, 1991.
) |
 |
|
Figure 42.28.
Posterior column is held reduced with an angled reduction clamp. The screw is placed through the plate and parallel with the quadrilateral surface. (Reprinted with permission from AO/ASIF, Both Column Fracture Through the Ilioinguinal Approach [Video]. Copyright © AO/ASIF Video, 1991.
) |
 |
|
Figure 42.29.
Posterior column fixation achieves purchase in the retroacetabular surface of the ilium. Tips of the two screws inserted through the pelvic brim plate (red pointer). (Reprinted with permission from AO/ASIF, Both Column Fracture Through the Ilioinguinal Approach [Video]. Copyright © AO/ASIF Video, 1991.
) |
addressed by developing the exposure to the lateral surface of the
ilium. A large reduction clamp placed across the anterior innominate
bone can be used to reduce the posterior wall. This fracture can be
fixed with obliquely oriented screws placed from just lateral to the
pelvic brim and directed posteriorly toward the superior extension of
the ilium. However, it is imperative to use the image intensifier to
confirm an extra-articular screw location.
encountered, especially with medial displacement of the femoral head.
The lateral traction device on the Judet–Tasserit table may be used to
position the femoral head beneath the intact segment of articular
surface. The femoral head may then be used as a mold for the reduction
of the impacted segments. The disimpaction of such fragments is
performed through the anterior column or quadrilateral surface fracture
lines.
acetabulum cannot be directly visualized but is assumed to be correct
after anatomic restoration of the internal contour of the innominate
bone (Fig. 42.30). The image intensifier is a
valuable adjunct to ensure both the proper orientation of screws near
the acetabulum and the perfect reduction of the articular surface. An
AP pelvis radiograph should be obtained in the operating suite to
confirm the adequacy of reduction. Before the patient is discharged
from the hospital, AP and 45-degree oblique views of the pelvis are
obtained to document reduction and fixation. If there is any suspicion
that hardware may be intra-articular, fluoroscopic examination can be a
valuable tool. The x-ray beam may be directed exactly parallel to any
screw to document its location. Occasionally a postoperative CT scan
may give additional information regarding the fracture reduction or
hardware placement, but this is not routinely performed.
cephalosporin and gentamicin is continued for 72 hours after surgery.
The suction drains are generally removed at 48 hours
or when drainage has ceased.
 |
|
Figure 42.30. Reduction of the articular surface is never directly visualized. (Reprinted with permission from
AO/ASIF, Both Column Fracture Through the Ilioinguinal Approach [Video]. Copyright ©AO/ASIF Video, 1991.
) |
All patients are screened with Doppler ultrasound for possible deep
venous thrombosis (DVT) at the time of admission. Those positive for
DVT receive a caval filter. If no DVT is present, mechanical
sequential-compression devices are applied preoperatively and left
continually throughout the patient’s hospital course. An adjusted-dose
warfarin (Coumadin) regimen is begun on the 2nd postoperative day and
continued for 6 weeks.
weight bearing is limited to 30 pounds until 8 weeks after the
operation. Standing active-motion exercises of the hip are encouraged
during this time. At 8 weeks after surgery, weight bearing is advanced
to full, and active-motion exercises against resistance are begun. An
emphasis is placed on strengthening the hip flexors and abductors. No
heterotopic bone prophylaxis is necessary.
weeks, 3 months, 6 months, 1 year, and yearly thereafter. An AP pelvis
radiograph is obtained at each visit. If loss of reduction or early
posttraumatic arthritis is suspected, then Judet obliques may be
obtained as well.
months; if heavy labor is involved, they may return to work in 6
months. They usually return to recreational activities by 6 months and
to vigorous athletics by 1 year. Although the majority of patients with
acetabular fractures will report that their hip never feels entirely
normal, 70% are eventually able to return to their previous levels of
function.
primarily neurovascular injuries. The lateral, femoral, cutaneous nerve
is the most frequently injured nerve, resulting in lateral thigh
paresthesia or numbness. Injuries to the femoral nerve are usually
stretch injuries, attributable to vigorous retraction of the iliopsoas
and femoral nerve. Sciatic nerve injuries are due either to placement
of retractors in the sciatic notch or to direct nerve injury by a
drill. Lymphatic complications and postoperative thigh edema are
avoidable if the perivascular tissue surrounding the external iliac
vessels is left undisturbed. The potential exists for direct laceration
of the external iliac artery or vein. In addition, overzealous
retraction of the vessels may produce an intimal injury of the external
iliac artery and subsequent arterial thrombosis. Careful palpation of
the arterial pulse throughout the surgery is critical. Postoperatively,
the peripheral pulses should be monitored for 24 hours to identify any
evolving vascular compromise.
found a 30% incidence of surgical wound infections. With the routine
use of prophylactic antibiotics and closed suction drainage of the
space of Retzius, however, surgical infection rates have significantly
decreased (5,6). With
restoration of the internal contours of the innominate bone, the hip
joint is not immediately in direct connection with the infection.
Routine exploration of the hip joint is not performed unless clinical
signs and symptoms lead one to suspect an intra-articular infection.
Deep wound infection, when encountered, is managed by repeated
exploration of the wound, irrigation, debridement, and closure over
drains. Appropriate broad-spectrum antibiotic coverage is used until
culture results are obtained and directed coverage is possible.
or inadequate repair of the inguinal canal. Careful dissection of the
floor of the inguinal canal during exposure should leave sufficient
tissue for a sound repair. Letournel reported significant
abdominal-wall hernias in only 1.1% of their patients.
accident, sustaining an associated both-column fracture of the
acetabulum. AP pelvis and 45-degree oblique radiographs are shown in Figure 42.31.
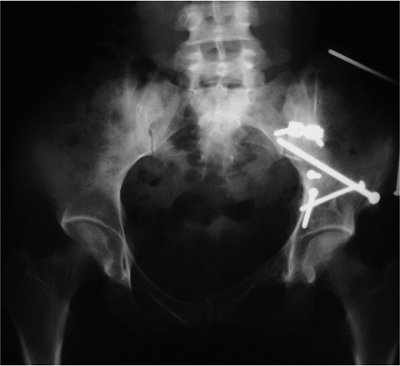
The patient underwent open reduction and internal fixation (ORIF) of
her fracture through the ilioinguinal approach. An AP radiograph at the
4-year follow-up showed that the fracture healed with maintenance of
the hip joint (Fig. 42.32). Her hip function was normal.
 |
|
Figure 42.31. A. AP pelvis, (B) obturator oblique, and (C) iliac oblique radiographs of an associated both-column acetabulum fracture.
|
 |
|
Figure 42.32.
AP pelvis radiograph at 4-year follow-up. The fracture is healed, and the hip joint is rated excellent based on both radiographic and clinic examination. |
JM. Fracture of the acetabulum: accuracy of reduction and clinical
results in patients managed operatively within three weeks after the
injury. J Bone Joint Surg Am 1996:78:1632.
Al, Greeno RA, Brooks LR, et al. Prevention of deep venous thrombosis
and pulmonary embolism in acetabulum and pelvic fracture surgery. Clin Orthop 1994;305:10–19.
