Fractures and Dislocations of the Foot
The dogma existed that the bones of the foot were predominantly
cartilaginous and would remodel as the child matures. Few, if any,
long-term studies exist to measure the outcomes of these treatments.
greater physical intensity that lead to more complex fractures and
dislocations.4,38,41,130 It is not uncommon for young children to be competing in motocross, extreme skiing, and rock-climbing.4,157
Professional sport has brought about more intense training and greater
expectations from the child, the parent, and the coach. Injuries need
to be treated “quicker” and rehabilitation time decreased to allow
early return to the sport. These expectations should not get in the way
of treating the child’s foot injury in the best possible way.
cartilaginous foot becomes ossified and fracture and dislocation
patterns change. Ogden118 showed
that the cartilaginous bones were elastic and absorbed the energy from
the trauma and dissipated it differently from the adult foot. This
resulted in different fracture patterns.118
The management algorithms for the adolescent foot are therefore quite
different from the infant’s foot; however, the exact age at which this
occurs needs to be individualized for each patient. The amount of
fracture angulation and joint line displacement to accept is one of the
real challenges in treating the skeletally immature foot. Some complex
fractures of the talus and calcaneus in adolescents are in fact best
internally fixed according to the priniciples used to treat adult
trauma.
is helpful as the variable ossification centers, apophyses, and growth
plates makes fracture recognition difficult. Most of the papers quoted
in this chapter are level IV (uncontrolled case series) or level V
(expert consensus). One of the problems with pediatric foot and ankle
research is that long follow-up intervals are necessary to validate
treatments. There are no pediatric outcome scores for children’s foot
trauma, so prediction of outcome is dependent on orthopaedic first
principles of anatomic reduction, union, and effective rehabilitation.
Long-term retrospective studies also have the difficulty of locating
children treated decades earlier and, therefore, the follow-up rate is
low.
the bones are largely cartilaginous until adolescence. Although the
mechanisms of injury are similar, the resulting fracture is usually
less severe in the child as the energy of the injury is dissipated by
the elasticity of the cartilage. The cartilage also makes
interpretation of imaging more difficult and fractures may not be
appreciated on plain radiograph. Computed tomography (CT) and magnetic
resonance imaging (MRI) scans assist in clarification of anatomy and
identification of fractures. The remodeling potential of cartilage
allows some displacement and angulation of fractures to be accepted in
children, whereas in adults it may be unacceptable.
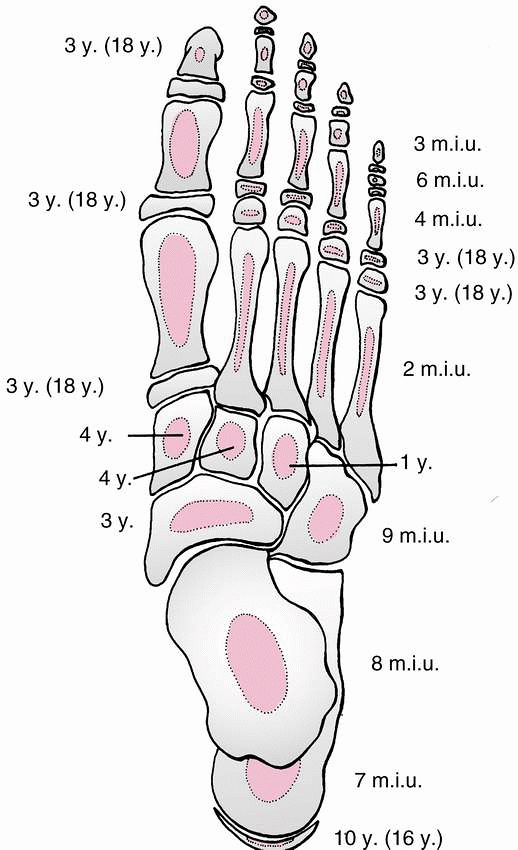
growth plates also make fracture recognition more difficult. The
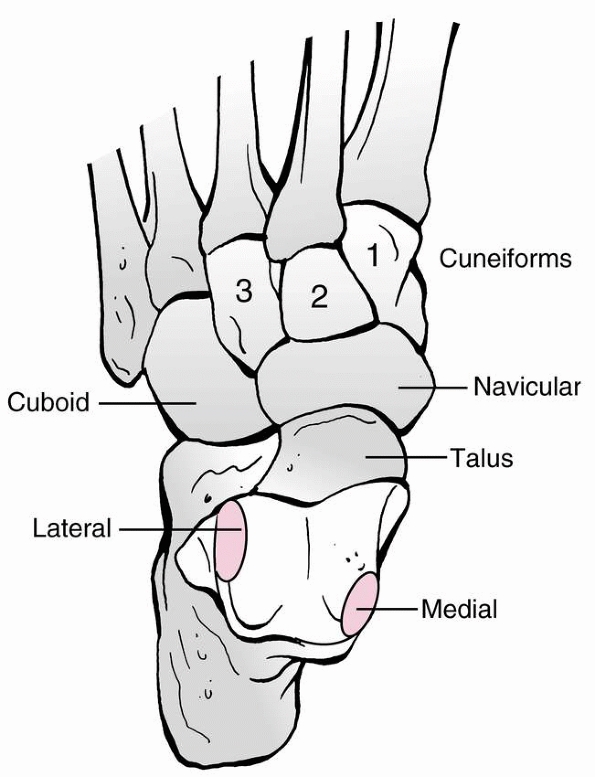
appearance of the ossification centers are summarized in Figure 27-1.5
The calcaneus and talus are usually ossified at birth and the cuboid
ossification center usually becomes evident shortly after. The
navicular does not develop its primary ossification center until the
child is around 3 years of age. Figure 27-2
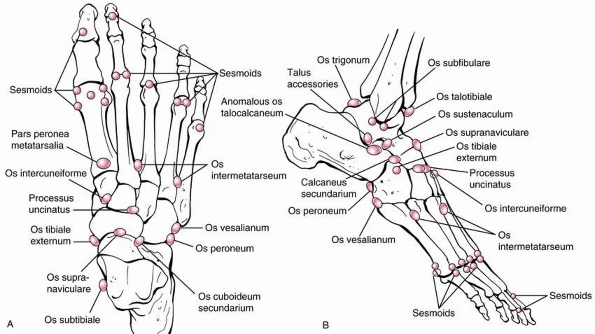
shows the accessory ossicles and sesamoid bones in the foot which can
also be confused with fractures especially if they are bipartite or if
the accessory bones are closely adhered. It is useful clinically to
radiograph the opposite foot if any doubt exists as to what may be
normal or pathologic.
 |
|
FIGURE 27-1
Appearance and fusion times of foot ossification centers, with figures in parentheses indicating the time of fusion of the primary and secondary ossification centers (y, years; m.i.u., months in utero). (From Aitken JT, Joseph J, Causey G, et al. A Manual of Human Anatomy. 2nd ed. London: E & S Livingstone, 1966:80, with permission). |
however, every attempt should be made to ascertain the mechanism of
injury. Often, other children or adults who witnessed the accident can
give a more accurate account than the patient. The degree of force, the
speed and height of the fall, and the way the foot is twisted all help
predict the degree of displacement or severity of the injury. In more
subtle injuries, the ability to weight bear, degree of instability, and
the location of the pain are vital parts of the history.
to the site of injury. The child often complains of the whole foot
“hurting”; however, systematic palpation helps localize the most
painful site. Appropriate radiographs can then be taken. Bruising
and
swelling will also help predict the injury pattern. Isolated bruising
on the sole of the midfoot often overlies a subtle Lisfranc injury
whereas excessive dorsal swelling may predict a more severe fracture
dislocation.139 In a soft tissue injury such as a crush injury, the possibility of increase compartment pressures should be considered.
 |
|
FIGURE 27-2
Diagrammatic representation of accessory ossicles and sesamoid bones about the foot and ankle. Note that the sesamoid bones can be bipartite and that accessory ossicles can be multicentric. (From Traughber PD. Imaging of the foot and ankle. In Coughlin MJ, Mann RA. Surgery of the Foot and Ankle. 7th ed. St. Louis: Mosby, 1999.) |
secondary survey should be undertaken to exclude other injuries. For
example, bilateral calcaneus fractures following a fall may be
associated with a tibial fracture or spinal column injury.
Talus fractures most commonly occur through the neck and occasionally
the body. Although rare, talus fractures are important to recognize due
to the possible complication of avascular necrosis (AVN). This can
occur due to the precarious blood supply and fracture patterns. In
children, AVN seems more prevalent in innocuous fractures when compared
to adults with similar injuries.134
The majority of talus fractures in children can be treated with cast
immobilization whereas displaced fractures in adolescents need to be
treated operatively similar to an adult fracture.
The foot is forcibly dorsiflexed and the neck of the talus impinges
against the anterior lip of the distal tibia. This shear force usually
results in a vertical or slightly oblique fracture line at the junction
of the body and neck of the talus. When the dorsiflexion is combined
with supination of the foot, the impingement occurs more medially and
the medial malleolus may be fractured as well. With displaced
fractures, the subtalar joint may become subluxed. The force required
to fracture a child’s talus is almost twice that required to fracture
the other ankle and tarsal bones.125
One must be thorough in looking for other injuries that may coexist as
a result of the severe trauma. The talus can also be fractured with
crushing injuries, and compound fractures are well described in
lawnmower accidents.118 Fractures of
the lateral process of the talus have been described recently in
snowboarding accidents where the mechanism appears to be forced
dorsiflexion and inversion of the ankle.89
especially associated with a fall from a height should lead to a
suspicion of a talus fracture. The same mechanism of injury can cause
other foot fractures and dislocations as well. The ankle and foot are
extremely swollen and the foot is usually held plantarflexed. Due to
this soft tissue swelling, the foot needs to be examined closely for
increased compartment pressure. As with all fractures, the soft tissues
need to be inspected for any puncture wounds, abrasions, or fracture
blisters as these are important in determining the management of the
patient.
A number of studies have found fractures of the calcaneus, malleoli,
tibia, and lumbar spine in the presence of a talus fracture.20,26,61,121,122 Hawkins,61 in his study, on adult talus fractures found 64% of the patients had an associated musculoskeletal injury.
have described a pronated oblique view of the talus which may
demonstrate the fracture more clearly. The fractures are not always
easy to see in young children, as the talus is largely cartilaginous
until the second decade.105 The
cartilage anlage often leads to an underestimation of fracture
displacement. Some authors have even suggested the use of MRI to show
the morphology better in children less than 10 years old.118,166
assessing the fracture plane, communition, degree of displacement, and
any other associated foot or ankle fractures. This is particularly
useful preoperatively when pain prohibits the full range of radiographs
mentioned above to be taken. If an open reduction is planned, the CT
scan will also aid in the preoperative planning of the size and
placement of the screws. Hawkins61
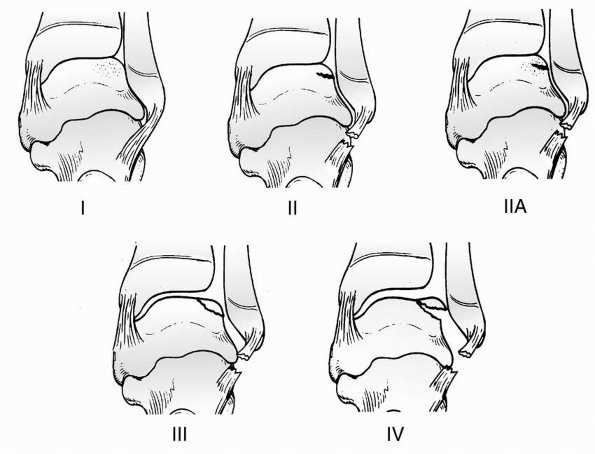
described an x-ray classification to define the different types of
fractures of the talar neck and used it to predict the risk of AVN (Fig. 27-3):
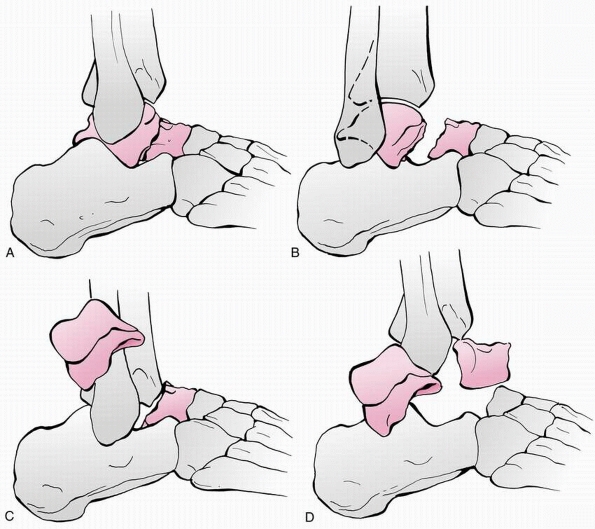 |
|
FIGURE 27-3 Hawkins classification of talar neck fractures (see text for details). A. Type I, nondisplaced fracture of the talar neck. B. Type II, displaced talar neck fracture with subluxation or dislocation of the subtalar joint. C.
Type III, displaced talar neck fracture with associated dislocation of the talar body from both the subtalar and tibiotalar joints. D. Type IV, as suggested by Canale and Kelly, displaced talar neck fracture with an associated dislocation of the talar body from subtalar and tibiotalar joints and dislocation of the head and neck fragment from the talonavicular joint. (From Canale ST, Kelly FB Jr. Fractures of the neck of the talus: long-term evaluation of seventy-one cases. J Bone Joint Surg Am 1978; 60:143-156.) |
described a subchondral lucent line, the “Hawkins sign,” that indicates
normal bloodflow to the talar body. The absence of this lucency may
indicate the development of osteonecrosis (see complications of talar
fractures).
either in the body or the neck. Some authors suggest classifying talar
fractures based on the age of the patient as children less than 6 years
of age generally have a better prognosis.105
has classified these into three different types depending on whether
the fracture is displaced and the degree of subluxation of the subtalar
and ankle joints (see Fig. 27-3). This
classification was developed so it could be used to predict if the
talus would become avascular due to the disruption of the tenuous blood
supply. Canale and Kelly26 later modified the classification (see Fig. 27-3)
to include a type IV injury in which there is subluxation or
dislocation of the ankle, subtalar, and talonavicular joints. In the
adult literature, the majority of talar fractures are type II and III.26,61 This classification of talus fractures
can help predict the type of treatment required and the outcome one can expect (Table 27-1).
|
TABLE 27-1 Hawkins Classification of Talar Neck Fractures
|
|||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||
severity of the fracture and the age of the child. The Hawkins
classification system is useful in directing the treatment. In a child
less than 8 years of age, a less than perfect reduction of the fracture
can be accepted due to the remodeling potential.74,92,105 Adolescent fractures should be treated the same way as an adult injury.
for 6 to 8 weeks nonweight bearing in a below-knee cast. The child can
then start taking full weight if the fracture has healed
radiographically. Canale and Kelly26 accepted 5 mm of displacement and 5 degrees of angulation of the talar neck in their series.
usually presents with significant soft tissue swelling and pain. This
makes management more difficult than type I injuries. Achieving
adequate radiographs to assess the degree of displacement is difficult
without sedation. The distal fragment of the neck is usually displaced
dorsally and medially.
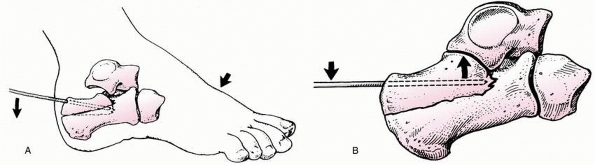
should be reduced under general anesthesia, most often by gentle
plantarflexion and pronation of the foot. If a stable reduction is
achieved, a well molded below-knee cast can be applied with the foot in
plantarflexion. This initial cast is changed to a more neutral position
at 4 weeks and then removed 8 weeks following fracture reduction.
Postoperative serial radiographs or a CT scan should be performed as
the fracture position may be lost when the soft tissue swelling
subsides. If the fracture is unstable after reduction, percutaneous
Kirschner wire (K-wire) fixation is useful to hold the fracture. Two
K-wires can be passed through a small dorsomedial incision and across
the fracture. The incision should be on the medial side of extensor
hallucis longus to avoid damage to the tibial vessels. Although the
amount of residual displacement or angulation acceptable is not clearly
defined, it may be better to accept a few millimeters of offset and up
to 10 degrees of angulation rather than perform an open reduction and
risk devascularising the talus further.
-
Posterolateral
-
Anteromedial
-
Anterolateral
the soft tissues and the familiarity of the approach by the surgeon.
Occasionally, more than one approach is required if adequate reduction
cannot be achieved. It is preferable to use the posterolateral approach
as this causes less potential disruption to the blood supply; however,
direct visualization of the talar neck is not possible.The timing of
the open reduction of these fractures is somewhat controversial. With
such a tenuous blood supply, one would think that urgent reduction and
internal fixation is indicated. Lindvall et al.96
compared the results of surgery within 6 hours to delayed surgery in 26
fractures of the talus in adult patients and found no significant
difference in outcome. Kellam et al.,79
in another similar study, concluded that the severity of the injury,
the quality of the reduction, and the surgical outcomes had a bigger
influence on long-term outcome than if the surgery was fixed emergently
or delayed (greater than 12 hours).
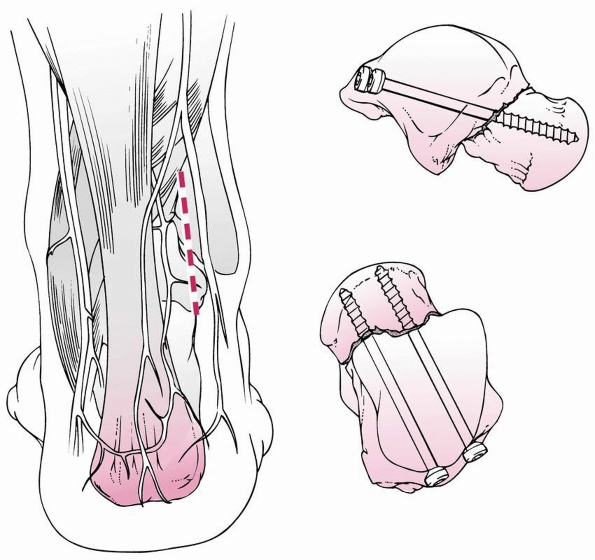
to internally fix fractures of the talar neck once it has been reduced.
The patient is positioned supine so the other approaches can
be
utilized if necessary. The incision is made just lateral to the
tendoachilles. Blunt dissection is then carried out down to the joint
capsule avoiding damage to the sural nerve. The posterior joint capsule
can then be opened if not already torn by the injury and the posterior
process of the talus can be identified. If possible, two partially
threaded cannulated 4.5- or 6.5-mm screws can be used to provide
compression across the fracture. It is preferable to use titanium
screws which are MRI compatible to allow investigation of AVN during
fracture healing if necessary. If only one screw is used, a separate
K-wire should also be passed across the fracture for rotational
stability. These posterior screws are more stable biomechanically than
anterior screws (Fig. 27-4).159
visualize the talar neck and directly reduce the fracture. Often, there
is communition of the medial wall of the neck which makes restoring
length difficult. With the patient supine, the incision is made from
just anterior to the medial malleolus and directly distally down the
midfoot. Deeper dissection is carried out medial to the tibialis
anterior and the extensor hallucis longus tendon. The dissection down
to the capsule is in the interval between the tibialis anterior and
tibialis posterior tendons. This approach avoids damage to the deltoid
branch of the posterior tibial artery and the medial branches of the
anterior tibial artery. This approach is potentially less harmful to
the blood supply of the talus when compared to the anterolateral
approach.3
is that it permits excellent exposure of the lateral talar neck which
is not usually comminuted allowing anatomic reduction. The approach
also gives good access to the subtalar joint. The disadvantage to this
approach is that it may disrupt the blood supply more than the other
approaches. The incision starts at the tip of the lateral malleolus and
extends to the base of the fourth metatarsal. Care must be taken to
avoid damaging the sural nerve with deeper dissection. In the base of
the incision is the artery of the sinus tarsi which should be
visualized if possible.
 |
|
FIGURE 27-4
Posterolateral approach to the talus. Incision is based lateral to the Achilles tendon. The Achilles tendon and flexor hallucis longus are reflected medially. The posterolateral talar tubercle is the starting point for the guide pin. Right: Screws are directed in line with the long axis of the neck of the talus in a plantar-medial direction such that the distal threads of the screw are all in the distal fragment (talar head), beyond the fracture line to allow for compression. Combinations of two screws or one screw and one smooth pin are determined by size and anatomy. (From Adelarr RS. Complex fractures of the talus. Instr Course Lect 1997; 46:328, with permission.) |
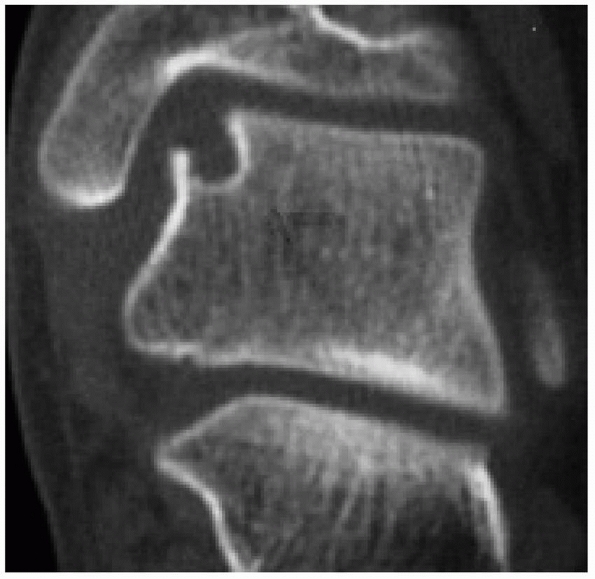
neck fractures, the foot is placed in a non-weight-bearing below-knee
cast for 6 to 8 weeks. Radiographs are then taken to assess fracture
healing and the presence or absence of the Hawkins sign. If the
subchondral lucent line is present, one can assume there is adequate
blood supply to the body of the talus and osteonecrosis is unlikely to
occur. If the fracture has also healed, the child can start progressive
weight bearing as tolerated. The absence of a subchondral lucency
during healing should alert the surgeon to the possible development of
osteonecrosis (Fig 27-5). The patient should
continue to be nonweight bearing until the lucency is present. If it is
still not present 3 months postinjury, an MRI scan should be performed
which will assess the vascularity more accurately.63
The use of titanium screws in the open reduction makes this possible.
The decision on the amount of weight bearing in the presence of altered
blood supply to the talus is not clear. AVN of the talus often takes 18
months to 2 years to revascularise so it would be impractical, if not
impossible, to keep a child non-weight bearing for this period in the
hope it will prevent premature collapse of the body.
head. Ossification starts from one center that appears in the sixth
intrauterine month. The talus ossification process starts in the head
and neck and proceeds in a retrograde direction towards the subchondral
bone of the body. Approximately two thirds
of
the talar body is articular cartilage with just a small area of bare
bone on the neck where the bone receives its nutrient blood supply.
There are no tendon insertions into the talus. The stability is
provided by the capsular and ligamentous attachments to the surrounding
bones.
 |
|
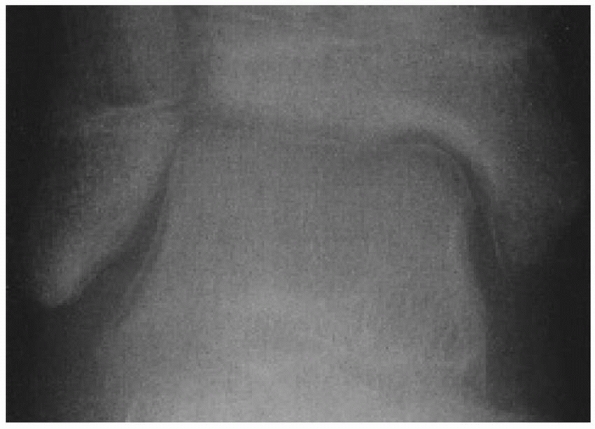
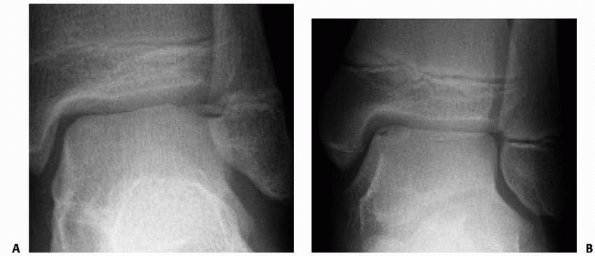
FIGURE 27-5
A 14-year-old girl with a talar neck fracture and a positive Hawkins sign. Disuse osteoporosis leads to halolike image of the talus on the AP view denoting adequate talar dome vascularization; if there had been no blood supply, there would be no bloodflow to loose calcium. If this happens, the dome of the talus would become denser and more radio-opaque than the surrounding bones that are undergoing diffuse osterporosis. |
anteriorly than it is posteriorly. Traditional teaching suggests the
foot should generally be immobilized in neutral dorsiflexion so this
widest part of the talus is engaged in the ankle mortise to help
prevent an equinus contracture. This is of less importance in younger
children who are less likely to develop equinus contractures. The
lateral wall of the superior articular surface curves posteriorly
whereas the medial wall is straight. The two walls converge posteriorly
to form the posterior tubercle of the talus. Often, there is a separate
ossification centre (os trigonum) that appears here on radiographs at
11 to 13 years of age in boys and 8 to 10 years of age in girls. It
usually fuses to the talus 1 year after it appears (Fig. 27-6).107
approximately 10 to 44 degrees and plantarflexed between 5 and 50
degrees in relation to the axis of the body.52
Beneath the talar neck is the tarsal canal, a funnel shaped area that
contains the anastomotic ring formed between the artery of the tarsal
canal and the artery of the tarsal sinus.112 The broad interosseous ligament joining the calcaneus and talus is also within the canal.
posteromedial (apex) to anterolateral where the base of the cone is
known as the sinus tarsi (Fig. 27-7).
 |
|
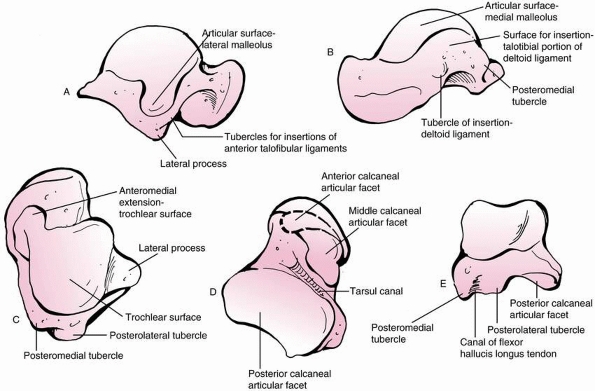
FIGURE 27-6
Anatomic details of the talus are important when correlating high-definition imaging, such as CT scans, with normal anatomy for the purposes of fracture management decision making. |
wedged-shaped process that is covered in articular cartilage. It
articulates with the fibular superiorly and laterally and with the
subtalar joint inferiorly. The lateral talocalcaneal ligament is
attached to the most distal part of the process.60,62
and articulates with the concave surface of the navicular. The
undersurface of the talus is comprised of three articulating surfaces
for the calcaneus: the posterior, middle, and anterior facet. Between
the posterior and middle facets is a transverse groove which forms the
roof of the tarsal canal.
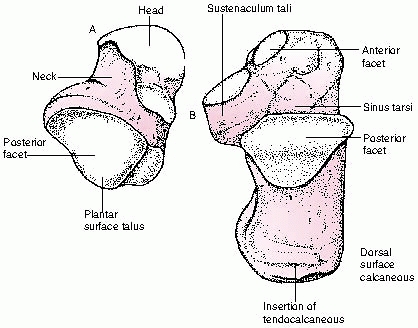
The nutrient arteries are derived from the three major vessels that
cross the ankle joint: posterior tibial artery, tibialis anterior
artery, and peroneal artery (Fig. 27 -8).
Branches of these three vessels perforate circumferentially the short
talar neck which is the only part of the talus denude of articular
cartilage. A fracture in this area can disrupt this intricate
anastamosis of vessels and lead to AVN of the body of the talus.
of the tarsal canal. This artery branches off the posterior tibial
artery approximately 1 cm proximal to the origin of the medial and
lateral plantar arteries. It passes between flexor digitorum
longus
and flexor hallucis longus before entering the tarsal canal where it
anastamoses with the artery of the tarsal sinus. Before entering the
canal, the artery of the tarsal canal gives off a deltoid branch that
penetrates the deltoid ligament and supplies the medial third of the
talar body.53 A dorsal vessel of the deltoid branch anastamoses with the medial branch of the dorsalis pedis artery to enter the talar neck.
 |
|
FIGURE 27-7 Subtalar joint opened such that the medial borders of the joint face each other. A.
Plantar surface of the talus, which articulates with the dorsal surface of the calcaneus. Note the extensive area of the talus that is articular cartilage. B. Dorsal surface of the calcaneus with the articular facets occupying the anterior half of the calcaneus. (From Sammarco GJ. Anatomy. In: Helal B, Rowley D, Cracchiolo AC, et al, eds. Surgery of Disorders of the Foot and Ankle. Philadelphia: Lippincott-Raven, 1996.) |
tibial artery and its terminal extension, the dorsalis pedis artery.
Multiple vessels from these arteries penetrate the dorsal neck of the
talus. The third source of blood supply is from the peroneal artery.
Small branches supply the posterior process of the talus and a larger
branch forms the artery of the sinus tarsi to supply the lateral aspect
of the talus.
found only 4 (29%) were fractures through the body. Undisplaced
fractures can be treated in a nonweight bearing below-knee cast for 6
to 8 weeks until the fracture is healed and the outcome is excellent.
Undisplaced intra-articular fractures can be treated in the same way;
however, serial radiographs must be taken to confirm displacement does
not occur. Anatomic reduction of displaced fractures has been
recommended because residual displacement of the articular surfaces
leads to degenerative osteoarthritis.91
in adults and children, and a high level of suspicion is required if
the diagnosis is to be made. The lateral process is a wedged-shaped
prominence that forms almost the whole lateral wall of the talus. It is
covered entirely in articular cartilage and is the articulating surface
of the talus with the fibular. The talocalcaneal ligament inserts into
the tip of the lateral process. The mechanism of injury is a forced
dorsiflexion injury with inversion of the foot.60 The talocalcaneal ligament may avulse the lateral process.
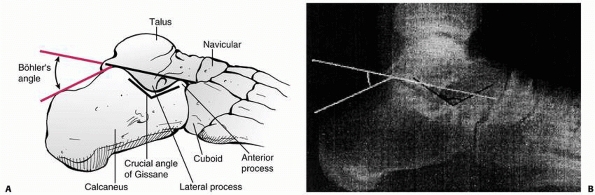
suggest this may occur in 46% of the cases. The lateral process is best
visualized on the mortise view so the fibula is not overlying it. On
the lateral radiograph, the lateral process is seen just superior to
the angle of Gissane.62 This is the
angle between a line drawn along the lateral border of posterior facet
and a line drawn along the anterior process (Fig 27-9).
If there is persistent pain laterally around the ankle following an
inversion ankle injury, one should have a high suspicion for a lateral
process fracture or an osteochondral injury. If not clearly seen on the
plain films, a CT scan should be performed to assess the talus and rule
out any other coexisting fractures.81,117
reviewed 3213 snowboarding injuries and found an unusually high
incidence of lateral process fractures. They comprised of all ankle
fractures.81
process is with a nonweight-bearing cast for 6 to 8 weeks. Displaced
fractures are best treated with open reduction and internal fixation;
however, the degree of displacement that is acceptable in a child is
not clearly defined. What may be more important is the congruity of the
joint surface of the talus. A step or gap in the articular surface of
more than 2 to 3 mm may be useful criteria
as
to when to open reduce the fracture. The fracture can be held with one
3.5-mm partially threaded cancellous screw inserted from lateral to
medial perpendicular to the fracture line. A below-knee cast is then
applied for 6 weeks.60,62,89,165
 |
|
FIGURE 27-8 Arterial blood supply to the talus. Medial blood supply (A) and lateral blood supply (B). Dorsal view with sagittal cut through length (a) of talus and transverse cut through neck of talus (b). (From Gelberman RH, Mortensen WW. The arterial anatomy of the talus. Foot Ankle 1983;4:64-72.)
|
|
TABLE 27-2 Sneppen Classification System of Talar Body Fractures
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
caused by direct trauma or may be due to an underlying osteochondal
lesion (osteochondritis dissecans [OCD]) that may have been present for
some time and has been made symptomatic by the injury. The pathogenesis
and etiology of OCD is controversial; however, most authors report
preceding trauma as a cause of the defects (Canale and Bedding25 80%, Letts et al.91 79%, Higuera et al.65 63%, and Perumal et al.123 47%). The medial
lesion is usually deeper and cup shaped compared to the thinner “wafer”
type lateral lesion. The lateral lesion is more often associated with
trauma and more symptomatic than the medial lesions. It is postulated
that the medial lesions may be due to more repetitive microtrauma.25,26 Berndt and Harty,12
in 1959, used freshly amputated legs to biomechanically reproduce
injuries to the ankle and observe the injuries inflicted. They showed
that the anterolateral talus hits the medial aspect of the fibula with
dorsiflexion and inversion and that plantarflexion and inversion caused
posteromedial osteochondral lesions (Fig. 27-10).
 |
|
FIGURE 27-9 Diagrammatic depictions of the crucial angle of Gissane (A) and the Böhler angle (B).
The Böhler angle is more frequently used for decision making regarding fracture management. For measuring the Böhler angle, the landmarks on the lateral radiograph of the calcaneus are the anterior and posterior facets and the superior margin of the calcaneal tuberosity. |
 |
|
FIGURE 27-10 Typical positions of osteochondral lesions of the talus. Berndt et al.48
found that of 201 osteochondral lesions in adults 56% were on the medial side and 44% on the lateral side. Letts et al. found medial lesions in 79% of 24 children, lateral lesions in 21%, and central lesions in 1%. (From Letts M, Davidson D, Ahmer A. Osteochondritis dissecans of the talus in children. J Pediatr Orthop 2003;23:617-625, with permission.) |
child should be closely assessed for an osteochondral injury. If pain
and swelling persist for over 2 months after an “ankle sprain,” then
further investigations should be carried out to look for an
osteochondral lesion. This will initially be a further radiograph
series; however, an MRI scan is often more useful at this stage to look
for an osteochondral lesion as a small percentage are purely
cartilaginous. Some consider an MRI arthrogram useful in further
determining whether the fragment is detached or not as occasionally the
arthrographic contrast can be seen deep to the osteochondral lesion.
The bone scan has largely been superseded by the MRI scan in the
diagnosis and assessment of these lesions. The bone scan is useful,
however, when it is not clear if the pain in the child’s ankle is
coming from the osteochondral lesion or some other pathology. A normal
bone scan in the presence of a stage I or II osteochondral lesion may
indicate a soft tissue lesion as being a source of the pain.
common as one would think but can occur with these lesions if the loose
fragment becomes trapped within the joint. The pain seems to be related
to the synovitis and effusion that develops secondary to the uneven
articular surface. On examination, the ankle is slightly swollen and
can be painful on passive movement as the loose fragment passes under
the tibia. With planterflexion of the foot, the anterolateral talus can
be palpated directly and a lesion here can be painful on direct
pressure.
modified this classification after correlating clinical findings with
radiographs and MRI scans. They described the stage I lesion as not
visible on plain radiographs
but
visible on an MRI scan. They also introduced a stage IIa lesion, which
is an undisplaced osteochondral lesion with a subchondral cyst adjacent
to the floor of the lesion. Anderson and his colleagues8 felt a atage IIa lesion should be treated surgically whereas a atage II lesion can initially be treated nonoperatively (Fig. 27-12).
 |
|
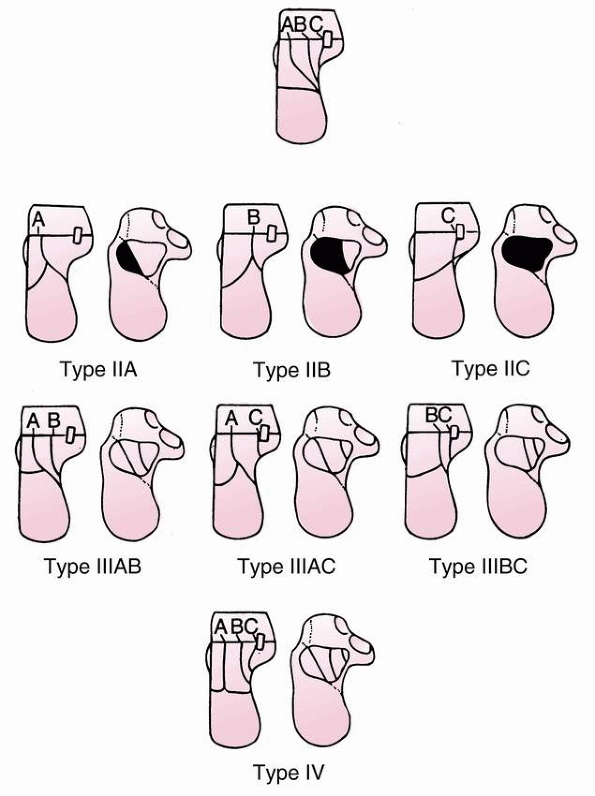
FIGURE 27-11 Adaptation of the Berndt and Hardy12 (1951) classification of osteochondral injuries of the talus by Anderson et al.8
Stage 1 is identified only by MRI scanning, which demonstrates trabecular compression of subchondral bone; stage 2 lesions have incomplete separation of the osteochondral fragment from the talus. If a subchondral cyst also is present, the lesion is designated stage 2a. Stage 3 lesions occur when the fragment is no longer attached to the talus but is undisplaced. Stage 4 indicates both complete detachment and displacement. (From Alexander IF, Chrichton KI, Grattan-Smith Y, et al. Osteochondral fractures of the dome of the talus. J Bone Joint Surg Am 1989;71:1143, with permission.) |
in 1986 based on the arthroscopic appearance of the articular cartilage
at the time of surgery. The quality of the articular cartilage was
placed into one of three grades:
 |
|
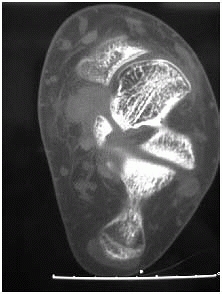
FIGURE 27-12
This CT scan clearly shows a well circumscribed cyst at the base of a stage II osteochondral lesion. This would be classified by Anderson et al.8 as a stage IIa lesion. |
should be treated with activity modification (grade I), who should have
arthroscopic drilling (grade II), and finally which patients require
arthroscopic curettage and microfracture (grade III).
children is challenging. Only a few papers purely address this
condition in children,65,91,123
and the rest of the literature is a combination of adult and childhood
lesions. It is important to distinguish between an acute osteochondral
fracture and a chronic osteochondral lesion as the two may require
different treatment strategies.
followed up for a minimum of 2 years as it takes this long for the
lesion to become radiographically healed despite the child often being
clinically normal.123
This usually relieves the acute symptoms; over the next 6 weeks, the
patient has activity modification maintaining a pain-free range of
movement. This allows the fracture to heal before returning to active
sport. Higuera et al.65 treated their stage 3 lesions nonoperatively as well and all 7 patients had good outcomes.
the talus are controversial. It is hard to compare results between
authors as they have often used different outcome measures. Some
authors use pain as their primary outcome91
whereas others also consider radiologic healing. The long term outcome
of an asymptomatic subchondral lucency in the talar body is unknown. In
some series, the patients have had arthrotomies91 while others had arthroscopic débridement.123 The staging of the lesions are also subject to interobserver variability.91 Letts et al.89
performed surgery in 24 patients with osteochondral lesions. They used
arthroscopy in three patients only and two of those patients required
arthrotomy as well.89 With modern
ankle arthroscopy equipment and newer surgical techniques, ankle
arthroscopy has become the primary surgical treatment for both medial
and lateral lesions of the talar dome. The anterolateral lesions are
more accessible; however, with good ankle distraction and different
portal placement posteromedial lesions are accessible.
reviewed 31 patients with juvenile OCD with a minimum of 6-months
follow-up. They recommended nonoperative treatment with an ankle brace
and activity modification in most cases for 6 months. Only 16% of the
lesions healed radiographically in that timeframe. If pain continues
after this time and the lesion is still present, further immobilization
and activity modification is recommended. They recommend arthroscopic
surgery for patients with type II lesions who are not prepared to
modify their activities longer than 6 months and patients with type III
lateral lesions and all stage IV lesions. Thirteen of the 31 patients
were treated surgically.
 |
|
FIGURE 27-13 A. Anterolateral stage III osteochondral lesion that was treated by arthroscopic excision and microfracture. B. Posteromedial stage II osteochondral lesion that was treated successfully nonoperatively.
|
-
Drilling the lesion (antegrade or retrograde)
-
Curettage and microfracture
-
Internal fixation with bioabsorbable nails
-
Bone grafting and internal fixation
showed excellent results drilling through the lesion into the
subchondral bone. They also found that in skeletally immature patients,
there may be an increased tendency for the lesion to heal when compared
to the adult patients. Retrograde drilling can be performed using
specific tip directed instrumentation.161
This avoids damage to the articular cartilage and may prevent
fragmentation of a small lesion. Access to a posteromedial lesion can
be difficult. One approach is to use a transmalleolar portal after
drilling a 3.5-mm drill through the medial malleolus or to use a
posteromedial portal taking care to avoid damaging the neurovascular
bundle.
relatively straightforward procedure. It is particularly useful in
small stage III and stage IV lesions where the fragment is too small to
internally fix or there is no subchondral bone on the lesion for
healing. The articular cartilage is débrided back to stable tissue and
the subchondral bone is curettaged until bleeding occurs. Either a
microfracture pick or 2-mm drill is then used in the subchondral bone.
Anderson et al.8 would suggest this treatment for all stage IIa lesions where a subchondral cyst is present.
difficult procedure for the inexperienced arthroscopist. It is
preferable to use absorbable pegs or nails rather than metallic
implants. In large stage III and IV acute osteochondral lesions, this
is probably the treatment of choice rather than excising the fragment.
anatomically reduced especially if they are intra-articular and there
is 2 to 3 mm of incongruity in the joint surface. A lateral approach is
used and a single compression screw inserted across the fracture. The
foot is immobilized in a below-knee cast for 6 weeks.
soon as possible. If the fracture can be reduced closed, the author
prefers a posterolateral approach to insert the compression screws as
this helps preserve the tenuous blood supply (see Fig. 27-4).
These screws are best inserted through this open approach so an
accurate starting point can be found and neurovascular structures
protected. The author has no hesitation to use an anteromedial approach
as well to help with fracture reduction before inserting the screws.
Through this approach, the neck fragment can be stabilized while the
screws are being compressed and anatomic fracture reduction can be
seen. Usually, two 4.5-mm partially threaded titanium screws are used
depending on the size of the talus and degree of fragmentation. The
titanium screws allows MRI postoperatively if osteonecrosis is
suspected.
distinguished from OCD lesions. Acute lesions should be repaired after
assessing the amount of bone present on the lesion. This can be
initially assessed arthrocopically but is repaired through an
arthrotomy depending on the position on the talus. The author prefers
to repair the lesion with dissolvable nails.
nonoperatively for 6 months. Initially, the child or adolescent wears a
Cam walker for 4 to 6 weeks to help the symptoms settle and then an
elastic ankle support and activity modification. If symptoms persist,
the author performs a repeat MRI scan and, if the staging has worsened,
proceeds to an arthroscopic débridement and microfracture or
stabilization. For patients with displaced fragments on presentation
(stage IV), the author recommends arthroscopic removal and
microfracture or repair if possible.
complication of talus fractures. This has been reported in a number of
large series of predominantly adult patients.26,61
Osteonecrosis of the body of the talus occurs when the blood supply has
been disrupted by a fracture of the talar neck. The result is necrosis
of
the
talar dome and possible collapse of the articular surface. It appears
that this process of necrosis can start as early as the first month
following the fracture. Hawkins61
described the presence of a subchondral lucent line, the “Hawkins
sign,” as prognostic of a good outcome as it indicates adequate blood
flow to the talar body. The absence of the sign on a 6 to 8 week
radiograph implies there is inadequate blood supply and osteonecrosis
may evolve.
related to the degree of displacement of the femoral neck fracture.
Hawkins61 showed that type I
fractures had a 0% to 10% AVN rate, type II fractures a 20% to 50% AVN
rate, type III an 80% to 100% AVN rate, and all type IV fractures
develop AVN. Canale and Kelly26 had similar long-term results.
fractures; however, it does not seem to be as predictable as the adult
literature suggests. The Hawkins sign was described in adults, and Ogden118 suggests this sign may not be as reliable in the cartilaginous talar dome of a child. Mazel et al.105
reported on seven complete fractures of the talar neck in children over
6 years of age and two developed AVN. Similarly, Letts and Gibeault92
had 3 children with AVN after talus fractures. Interestingly, 2 of
these patients had undisplaced fractures of the talus at the time of
their injury that were not initially picked up. Subsequent radiographs
revealed the AVN.92 Rammelt and colleagues134
also reported on a 5-year-old whose undisplaced talar neck fracture was
missed who went on to develop AVN. In a literature search, they found a
16% incidence of AVN of the talus in undisplaced talar fractures in
children. They suggest that the pediatric talus is more susceptible to
AVN than the adult counterpart.134 Jensen et al.,74 on the other hand, had no cases of AVN in 14 children with talus fractures.
the patient regarding weight bearing when the Hawkins sign is not
present by 8 weeks. Some of the above series report AVN occurring 6
months after the injury and not resolving for many years. There does
not appear to be any series comparing outcomes in patients who bear
weight over this period and those who do not. If the Hawkins sign is
not present, it is advisable to perform an MRI scan at 3 months to
establish if AVN is present or not.63,163
If present, it may be advisable to encourage the child to avoid impact
activities to prevent collapse rather than have a prolonged period of
non-weight bearing.
The treatment of these fractures has historically been nonoperative,
relying on the largely cartilaginous bone to remodel with time. The
majority of fractures in children less than 14 years old are
extra-articular whereas in older children the fracture pattern
resembles those in adults. Children appear to have more coexisting
lower limb fractures than adults but fewer fractures of the axial
skeleton.150
or are diagnosed late on radiographs or bone scan when the child is
still limping long after the injury. At the other end of the spectrum,
the adolescent patient has often had a major fall and has a displaced
intra-articular fracture. This older age group should be treated like
the adult population with open reduction and internal fixation
restoring the joint congruity and calcaneal height and width. The
challenge for the surgeon is at what age and what degree of
displacement is this more aggressive treatment indicated in a group of
patients traditionally treated nonoperatively.
height. This axial load drives the talus into the calcaneus resulting
in the fracture. The degree of communition appears to be less in
children even though they often fall from greater heights than adults.20 Wiley and Profitt174
found that in young children, the fall was usually less than 4 feet and
in children older than 10 years the fall was greater than 14 feet. They
noted that the minor falls in the younger children often resulted in
undisplaced fractures that were diagnosed late.
reviewed 56 children with calcaneal fractures of which 25 (45%) were
due to a fall from a height. They also found that children less than 14
years of age predominantly had extra-articular fractures, hypothesizing
that the calcaneus in this age bracket absorbs the compression force
rather than dissipating it through the joint.
injuries when compartment syndrome may coexist and open fractures are
common in lawnmower injuries.
their feet should be examined carefully for a calcaneal fracture.
Associated injuries should also be evaluated with a thorough secondary
survey, especially of the lower limbs and spine.
around the heel and dorsum of the foot. Symptoms and signs of
compartment syndrome, including excessive pain, pallor, parasthesia,
and pulselessness should be assessed. In more subtle injuries, careful
palpation is necessary to elucidate areas of pain which may disclose an
underlying undisplaced fracture.
missed and diagnosed late. Often, the fracture line is not evident on
the initial radiographs. Inokuchi et al.71 reported that 44% of fractures in their series were initially missed, as were 55% of those reported by Schantz and Rasmussen148 and 44% of those reported by Wiley and Profitt.174
causes of heel pain in a child. These include Sever disease,
osteomyelitis, a unicameral bone cyst, or a stress fracture.
reviewed 59 children with 62 calcaneal fractures and found a number of
associated injuries. These included fractures of the lumbar spine,
lower limb fractures, a pelvic fracture, and upper extremity fractures.
These other skeletal
injuries
were more frequent in children over 13 years of age. Associated lower
limb fractures occurred twice as frequently as in adults; however,
injuries to the axial skeleton occurred half as often as in adults.
Wiley and Profitt,174 however, only had 2 patients with accompanying significant injuries in their series of 32 pediatric calcaneal fractures.
Subsequent radiographs at 10 to 14 days often show the fracture line.
The majority of these missed fractures are extra-articular.150
are posteroanterior, lateral, and axial views. The posteroanterior view
shows the calcaneocuboid and talonavicular joints well. The lateral
view is excellent at showing the congruity of the posterior articular
facet and allows calculation of Böhler’s angle (see Fig. 27-9).
The axial view demonstrates the tuberosity, the body, the sustenaculum
tali, and the posterior facet of the calcaneus.. Oblique views are also
useful and will show a fracture of the anterior process more clearly (Fig. 27-14).136
The oblique views also define the subtalar joint well so are very
useful in intra-articular fractures. Broden views can also be taken
that look at the posterior facet of the calcaneus. These are taken with
the leg internally rotated 40 degrees and the x-ray beam angled between
15 to 40 degrees toward the head.18
This is a difficult radiograph for the technicians to master and almost
the same information can be achieved by ordering a mortise view of the
ankle and looking at the posterior facet of the subtalar joint.
 |
|
FIGURE 27-14 Fracture of the anterior process of the talus.
|
angle. This is the angle between a line drawn from the highest point of
the anterior process to the highest point of the posterior facet and a
line drawn tangential to the highest point of the calcaneal tuberosity.
The normal value in an adult is between 20 and 40 degrees. In a child,
the angle is slightly less than in an adult and may be due to the
incomplete ossification of the calcaneus. It is advisable to perform a
lateral radiograph of the contralateral calcaneus to use as a
comparison rather than accept the absolute value of Böhler’s angle. The
child’s calcaneus does not resemble that of an adult until after 10
years of age.67,69,118,166
Another angle which is not so easy to measure is “the crucial angle of
Gissane”. This is the angle formed by two strong cortical struts seen
on the lateral radiograph. One runs along the lateral margin of the
posterior facet and the other runs up to the anterior process of the
calcaneus. The angle between them ranges from 95 to 105 degrees (see Fig. 27-9).47
always important to be cognizant of the normally appearing ossification
centers and accessory bones about the growing foot, which often are
confused with fractures (see Figs. 27-1 and 27-2).27
The os calcis is the earliest tarsal bone to ossify with the primary
ossification center appearing in the third intrauterine month. The
secondary ossification center appears around 6 to 8 years and is the
crescentic epiphysis seen posteriorly that gives rise to Sever’s
disease. This epiphysis fuses to the body of the calcaneus when the
adolescent is 14 to 16 years old.
calcaneal fractures is uncommon with the ready availability of MRI
scans. The bone scan is useful in evaluating a nonlocalized painful
limp in a toddler and in this setting a calcaneal fracture may be
diagnosed. Laliotis et al.83 used
bone scans and identified five calcaneal fractures in 7 toddlers less
than 36 months of age who had no history of significant injury. Bone
scanning is sensitive for bone pathology but not specific and will be
positive when other conditions are present like infection, Sever
disease, juvenile arthritis, and some neoplasms. A CT scan is a useful
investigation to evaluate the positive bone scan.
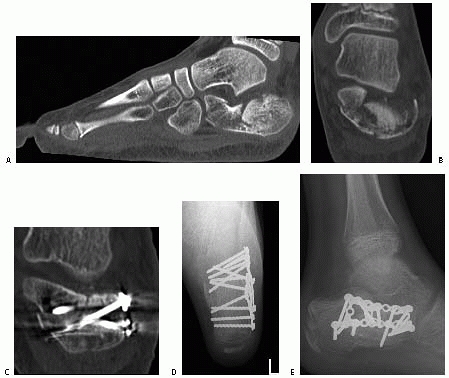
the fractured calcaneus. Not only does it clearly show the fracture
lines and altered anatomy, but also reveals injuries to adjacent bones.
Sanders et al.146 have used CT scans
to develop a classification system that is particularly useful in the
preoperative planning of open reduction of these fractures. The primary
and secondary fracture lines are identified and the degree of
communition and position of the fragments is more accurately seen than
in the radiographs. The primary fracture line usually runs obliquely
from plantar-medial to dorsolateral exiting the posterior facet.
Secondary fracture lines that develop off this primary line are also
seen and their pattern determines the classification of the fracture (Fig. 27-15).
The CT scan also allows a three-dimensional reconstruction to be made
which again is useful in visualizing the fracture lines for possible
internal fixation.
reviewed 9 patients with 10 calcaneal fractures and performed CT scans
on all of them. They found the fracture patterns in these adolescents
(average 13.4 years old) to be very similar to those found in adults.
They did find less communition in children than in adults, even though
the children reportedly had fallen from greater heights.
 |
|
FIGURE 27-15
Sanders CT-based classification of intra-articular fractures of the calcaneus in adults. (From Sanders R. Intraarticular fractures of the calcaneus: present state of the art. J Orthop Trauma 1992;6:254, with permission.) |
 |
|
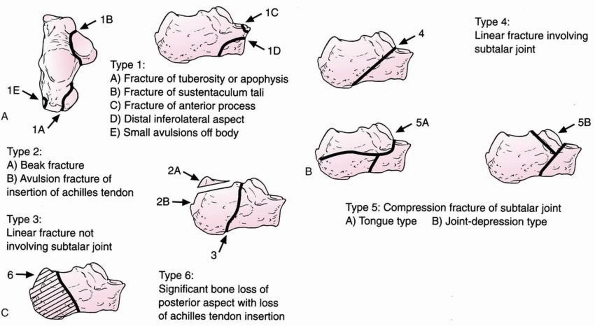
FIGURE 27-16 Schmidt classification of calcaneal fracture patterns in children. A. Extra-articular fractures. B. Intra-articular fractures. C.
Type 6 fracture pattern with significant bone loss, soft tissue injury, and loss of Achilles tendon insertion. (From Schmidt TL, Weiner DS. Calcaneus fractures in children: an evaluation of the nature of injury in 56 children. Clin Orthop Relat Res 1982;171:150, with permission.) |
majority of calcaneal fractures. They can be useful in young children
when the calcaneus is still largely cartilaginous and a fracture is not
seen on plain films or CT.
and added a new fracture type (type VI) to develop a classification for
pediatric calcaneal fractures which is in routine use today (Fig. 27-16).
This is an adult classification system that was developed after
reviewing the CT scans on 120 cases preoperatively and at minimum
1-year follow-up. The follow up CT scans were correlated with the
clinical outcome scores to help validate the classification system used.
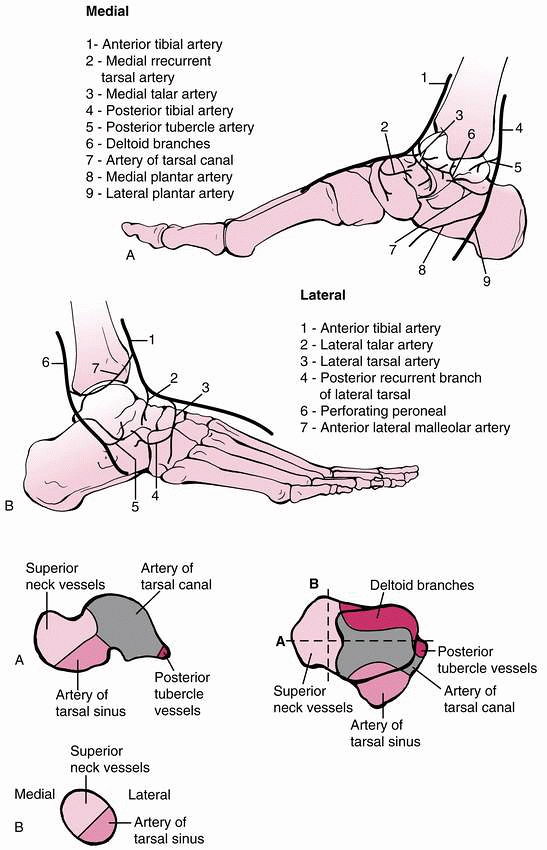
an unusual shape. It has three articular facets (anterior, middle, and
posterior) on the superior surface where it articulates with the talus
to form the subtalar joint (see Fig. 27-7) and
anteriorly there is a saddle-shaped articular surface for the cuboid.
The posterior facet is the largest facet and is slightly convex. The
middle facet is anterior and medial to the posterior facet lying on the
sustenaculum tali. It is concave like the anterior facet with which it
is often contiguous. Between the middle and posterior facets lies the
calcaneal groove, which forms the inferior wall of the sinus
tarsi.
Posteriorly, the tendoachilles inserts into the tuberosity of the
calcaneus which is the whole area behind the posterior facet. On the
lateral surface of the calcaneus are two shallow grooves with a small
ridge in between (the peroneal trochlea). The peroneus longus and
brevis run either side of this trochlea. The medial side is concave and
is structurally stronger than the lateral side. The sustentaculum tali
projects from the medial wall and supports the middle articular facet
on its surface. The tendon of flexor hallucis longus runs on the
undersurface of the sustenaculum. On the plantar surface are the medial
and lateral processes for the origin of the abductor hallucis and
abductor digiti minimi muscles, respectively (Fig. 24-17).
between the ages of 6 and 10 years. Inflammation in the apophysis
around this age causes heel pain and is referred to as Sever’s disease.
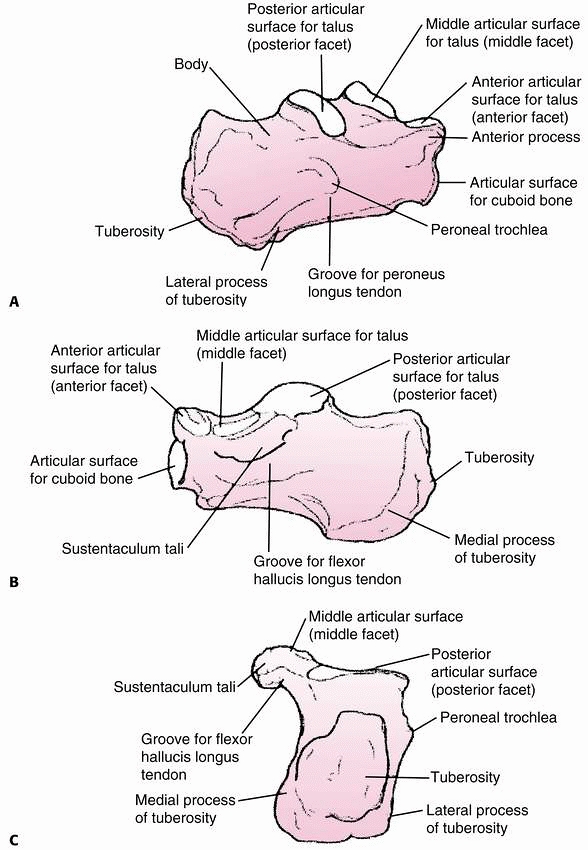
the calcaneus to help make treatment decisions. The coronal views show
the important posterior facet and the sustenaculum tali and the height
and width of the heel. The position of the peroneal tendons and flexor
hallucis tendon can also be seen. The sagittal views provide additional
information about the posterior facet and also show the anterior
process well. The axial views visualize the calcaneocuboid joint well,
the anteriorinferior aspect of the posterior facet, and the
sustenaculum tali. This information can then be used in planning the
reconstruction of the calcaneus.144,145
 |
|
FIGURE 27-17 Anatomic details of various angles of the calcaneus including lateral (A), medial (B), and coronal (C)
views through the level of the sustentaculum tali, which correlate with the CT scan view important in reconstruction of the posterior facet. |
severe than in the adult population and often do well without operative
intervention. The adolescent, on the other hand, often has fracture
patterns similar to adults and requires open reduction and internal
fixation. The challenge to the orthopaedic surgeon is to recognize the
patient that requires this form of surgery. There is a degree of
remodeling that will take place in the child and hence the amount of
growth remaining, degree of ossification,
and difference in morphology from the contralateral side all need to be considered in making the treatment decisions.
by cast immobilization for 6 weeks. The child can start weight bearing
in this cast when comfortable and can be changed to a Cam walker for
the final few weeks if necessary.19,71
the posterior gap is less than 1 cm and the Achilles tendon has not
been significantly shortened by bringing the fragment up proximally.
Occasionally, the technique described by Essex-Lopresti47 for percutaneous reduction of tongue-type fractures (Fig. 27-18) is useful.
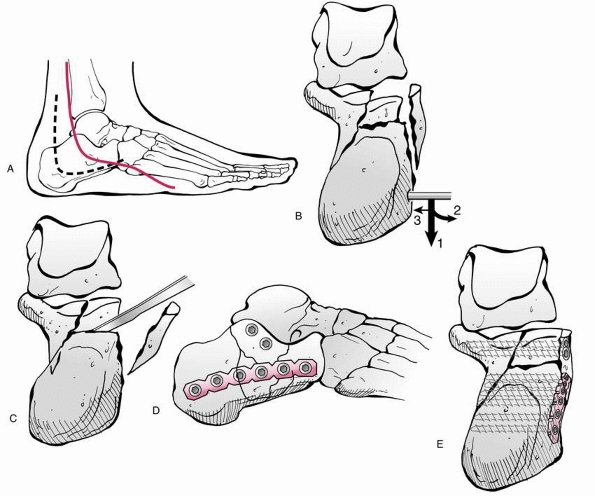
severe intra-articular fractures with displacement of the fragments and
depression of the joint surfaces. These fractures occur almost
exclusively in the adolescent patient where the ossification process is
complete. The adult literature abounds with indications for internal
fixation, surgical approaches, rehabilitation, complications, and
outcome measures (Fig. 27-19).10,126,143,144,145,146
These series only have a few adolescent fractures among them, and
therefore it is difficult to draw any conclusions specifically about
children’s calcaneal fractures. The literature on the management of
displaced intra-articular fractures in children is somewhat conflicting
in the indications for surgery. Schantz and Rasmussen148
reported on the outcome of displaced intra-articular fractures in
children less than 15 years old treated nonoperatively. The majority of
the patients had a good outcome; however, 4 complained of pain an
average of 12 years after injury.148,162 Brunet19
believes the outcome does not correlate to the severity of the
fracture. This is most likely due to the remodeling potential of the
calcaneus in this age group. This concept also was supported by Mora et
al.,111 who concluded that open
reduction may be suitable only for severely displaced fractures in
adolescents. The difficulty is defining the age or maturity of the
patient that may predict a poor outcome if the fracture is left
unreduced. Using validated quality-of-life scales 2 to 8 years after
surgery, Buckley et al.21 found that
younger patients (adults under the age of 30 years) who had operative
treatment had better gait satisfaction scores than those who did not
have surgery. Allmacher et al.6
questioned whether short-term or intermediate results of displaced
intra-articular calcaneal fractures can predict long-term functional
outcome. Using validated outcome instruments, they studied adult
patients treated nonoperatively and found that nonoperative treatment
often led to pain and loss of function, which increased in the second
decade after injury.
 |
|
FIGURE 27-18 Percutaneous reduction technique for tongue-type fractures of the calcaneus, as described by Essex-Lopresti.47
This technique remains an alternative to conservative treatment and open reduction with internal fixation of displaced, tongue-type fractures. A. A pin is inserted into the tongue fragment and used as a joystick to manipulate the fragment into better position, usually with a downward force on the pin and the forefoot (plantarflexion). B. After reduction, the pin is driven across the fracture to maintain reduction. (From Tornetta a III. The Essex-Lopresti reduction for calcaneal fractures revisited. J Orthop Trauma 1998;12: 471, with permission.) |
reviewed the results of open reduction with internal fixation of
displaced intra-articular calcaneal fractures in 6 adolescent patients
(average age, 13 years) and found good short-term results at an average
of 30 months after injury. None of the 6 patients (seven calcaneal
fractures) developed any of the serious complications reported in
adults. Four of the seven feet were completely pain-free, and three had
some minor pain with sports or hard floors. Ceccarelli28
found that adolescents with displaced intra-articular fractures had
better clinical and radiologic outcomes if treated by open reduction
rather than nonoperatively. Buckingham et al.20
reviewed 10 adolescent patients and reported good or excellent outcomes
in 8 patients. They had no wound complications and the range in motion
was hardly affected in 7 patients. They recommended the routine removal
of the screws and plates after fracture healing as this had improved
the symptoms in 6 of 8 patients.20
demanding, and if the treating surgeon is not experienced with the
approach, the child is best referred to a colleague who is.
fractures is which ones require surgical intervention and which ones
can be treated in a cast. Almost all closed fractures in children less
than 10 years of age can be treated nonoperatively due to the
remodeling potential. This includes intra-articular fractures that are
displaced.
treated by nonoperative means with a below-knee cast for 6 weeks.
Weight bearing in the cast can start after 2 to 3 weeks as the patient
becomes more comfortable.
 |
|
FIGURE 27-19 A. Lateral L-shaped approach to displaced intra-articular calcaneal fractures. The incision (dashed line)
is laterally based, with the proximal arm approximately half the distance from the fibula to the posterior border of the foot and the distal arm halfway from the tip of the fibula to the sole of the foot. The sural nerve is illustrated. A full-thickness, subperiosteal flap exposes the entire lateral calcaneus. B. Reduction maneuvers 1, 2, and 3 (densest arrow indicates greatest displacement) with a Schantz screw are used to pull the tuberosity down and allow access to disimpact the posterior facet (C) after the lateral wall of the calcaneus is levered open. The posterior facet is then reduced anatomically, held provisionally with K-wires, and then fixed with two partially threaded cancellous screws (outside of plate) into the sustentaculum tali. Lateral view (D) of reduced calcaneus and axial view (E) of reduced fracture with hardware. (From Benirschke SK, Sangeorzan BJ. Extraarticular fractures of the foot: surgical management of calcaneal fractures [Review]. Clin Orthop Relat Res 1993;292:128-134; with permission.) |
treated in a below-knee cast. In this group of patients, it is
advisable for them to be nonweight bearing for 6 weeks or until the
fracture is healed to prevent further displacement.
Before embarking on this surgery, a thorough assessment of the skin
needs to be performed. Surgery should be delayed to allow swelling to
subside and fracture blisters to resolve. This will decrease some of
the wound complications commonly seen after open fixation of adult
calcaneal fractures. The key point in performing this surgery is to
maintain thick skin flaps, restore joint congruity, use specialized
calcaneal plates, and be prepared to bone graft the defect. An outline
of the surgical technique is in Table 27-3.
had no wound problems in the six adolescents (age range 11 to 16 years)
they treated with open reduction and internal fixation. All the
patients were treated with an extensile lateral approach an average of
10.5 days from the time of injury. The lower incidence in children
reflects fewer risk factors in this group when compared to the adult
population. Smoking, obesity, and diabetes all contribute to wound
problems.
of the incision. In adults, it has been shown that a two layer closure
is preferable to a single layer of sutures.1,51 Wound
dehiscence can occur from days to weeks after the surgery. The best
initial treatment is immobilization of the foot and ankle to decrease
any tension on the wound edges. This is best accomplished in a
below-knee cast with a large window cut around the entire incision.
This allows space for wound dressing changes and débridements as
necessary. Oral antibiotics may be required if superficial infection is
also present. Once the wound is healed, gradual mobilization can be
reinstated.
 |
|
FIGURE 27-20 Intra-articular depressed fracture of the calcaneus in a 13-year-old boy. A. Preoperative sagittal CT shows the depression of the posterior facet into the body of the calcaneus. B. Coronal CT shows the displacement of the frature fragments. C. Postoperative CT scans are useful at checking the fracture reduction and length and position of the screws. D,E. Postoperative radiographs confirm restoration of the Böhler angle.
|
require rehospitalization, repeat surgical débridements, and
intravenous antibiotics. Often, the use of a suction dressing
(Vacuum-Assisted Closure [VAC], KCI, Inc., San Antonio, TX) is
advisable in recalcitrant wounds. This VAC device has been shown to be
safe and effective by Mooney et al.110
for traumatic wounds in pediatric patients of all ages. Skin closure is
usually not possible following such radical débridement. It is very
helpful to consult with plastic surgeons early in the course of
treatment as the patient often requires tissue transfer to cover the
exposed metalware.
dystrophy (RSD), is a devastating painful disorder that can occur
following operative or nonoperative management of a calcaneal fractures
or other trauma about the foot. The condition is usually diagnosed when
there is severe pain present out of proportion to the severity of the
injury following the acute phase of healing. The pain is difficult to
control even with oral narcotics. The child will not bear weight or
even allow the foot to be examined. Light touch even by water may
stimulate an unusual pain response. The foot clinically demonstrates
the signs of autonomic dysfunction. There is often a greyish
discoloration, cold clammy skin, and decreased hair growth. Through
disuse of the foot, the calf will atrophy. If radiographss are taken,
the bones of the foot will show patchy disuse osteopenia.
reviewed 70 children (average age, 12.5 years) with RSD and 87% had
injuries to the lower limb. Eighty-four percent of their patients were
girls, and on average the time from injury to a diagnosis of RSD was 12
months. Despite multidisciplinary treatments, 54% of patients still had
persistent symptoms of RSD at 3 years after diagnosis. They emphasized
that complex regional pain syndrome (CRPS) has a different disease
course in children when compared with
adults
and needs to be treated appropriately. CRPS occurs most commonly in
girls with the incidence peaking at or just before puberty.170
|
TABLE 27-3 Operative Planning for Open Reduction and Internal Fixation of Intra-articular Calcaneal Fractures in Adolescents
|
||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||
multidisciplinary pain teams that treat CRPS. These comprise a
physician (anesthetist or pediatrician), a psychiatrist or clinical
psychologist, a physiotherapist, and sometimes an occupational
therapist. The child initially undergoes a multidisciplinary assessment
that involves both schooling and social circumstances. The
physiotherapist carries out a thorough functional assessment.
therefore extensive physiotherapy is performed initially. Analgesics
need to be used to facilitate this and include anti-inflammatory drugs,
amitriptyline, and gabapentin. In severe cases, regional blocks
occasionally need to be used to control the pain. Children appear to
respond to physiotherapy better than adults and they
require
less medication and invasive procedures. On the other hand, the
recurrence rate of CRPS is higher in children; however, they respond
well to the reinitiation of treatment.170
nonoperated foot. Pain in the peroneal tendons on movement or direct
palpation may indicate prominent underlying metalware. Simply removing
the offending screw or plate may help. Buckingham et al.20
recommended the routine removal of metalware in their series of
adolescent calcaneal fractures as this resulted in resolution of pain
in their patients.
prevented the peroneal tendon subluxation that used to occur with the
Kocher incision. Care has to be taken at the proximal and distal ends
of this incision as the sural nerve can be damaged and a painful
neuroma develop.
nonoperatively, a displaced lateral wall can sublux or even dislocate
the peroneal tendons. Lateral impingement pain can also result from the
fragment coming in direct contact with the fibula.
in differentiating the cause of pain in the adult foot but its use in
children is limited. It should, however, be considered in adolescents
who are willing to cooperate.
infrequently and are particularly uncommon in children. They occur most
often in young adult males. There are no series published on this
condition in children; however, Dimentberg and Rosman41 reported on five talonavicular dislocations.
results from a forced inversion injury to the foot. The talonavicular
and talocalcaneal ligaments rupture while the calcaneonavicular
ligament stays intact. The result is that all the bones of the foot
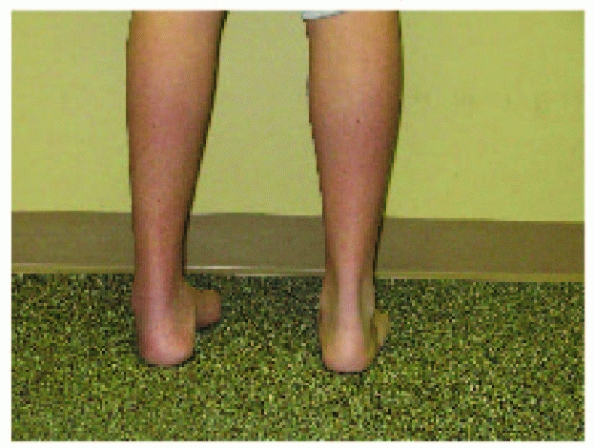
dislocate medially while the talus remains in the ankle mortise (Fig. 27-21).
The foot looks markedly deformed and the talar head can be palpated
laterally. A lateral dislocation is caused by a forced eversion injury
and results in a laterally displaced “flatfoot.”
 |
|
FIGURE 27-21 Posterior view demonstrating cavovarus deformity of the left foot. (Courtesy of Dr. Thomas Lee, MD.)
|
 |
|
FIGURE 27-22
Lateral view showing subluxation of the subtalar joint. There is incongruity of the calcaneocuboid joint. (Courtesy of Dr. Thomas Lee, MD.) |
The key is to look for the “empty navicular” where the talar head no
longer articulates with it. A CT scan is useful to look for any
associated fractures or osteochondral damage; however, it is probably
more useful to perform this after a closed reduction to confirm
anatomic alignment as well (Fig. 27-24).
reduction under general anesthetic. The knee should be flexed to relax
the tendoachilles and then the deformity accentuated before a
reduction
is carried out by relocating the deformed foot. Usually, the reduction
is stable and anatomic reduction can be confirmed by radiographs and CT
scan. The foot is immobilized until the child is comfortable enough to
start gentle mobilizations. K-wire stabilization and 6 weeks of
immobilization are necessary for unstable dislocations.
 |
|
FIGURE 27-23 AP view demonstrating translation of the transverse tarsal joint. (Courtesy of Dr. Thomas Lee, MD.)
|
 |
|
FIGURE 27-24
CT scan axial view shows marked talar head uncoverage (“ball is not in cup”). There is also significant incongruity of the subtalar joint. (Courtesy of Dr. Thomas Lee, MD.) |
closed means and has to be opened through an anteromedial approach. The
bone or soft tissue (often the tibialis posterior tendon) is removed
from the joint and the foot reduced.
cuneiforms are rare pediatric foot injuries. The midtarsal region
extends from the calcaneocuboid and talonavicular joints (Chopart’s
joint) to the metatarsals. It includes the cuboid, navicular, and three
cuneiform bones. These bones are interlinked by extremely strong
ligaments especially on the plantar surface. The lateral side of the
midfoot is more stable than the medial side. The shape of these small
bones and strength of their ligaments help maintain the longitudinal
and transverse arch of the foot. Disruption of this rigid anatomy
therefore requires a large force especially in the cartilaginous bones
of a child’s foot. Isolated injuries to this area are rare and one
needs to look for other associated fractures and dislocations.
This classification uses five broad categories based on the direction
of the force causing the injury and the direction that the fragment is
displaced. In parentheses are the percentages of this type of injury in
Main and Jowett’s100 review of 71 midtarsal injuries.
reviewed four cases of midtarsal dislocations in children, and this is
the only report in the literature of this injury in the pediatric age
group. The children had an average age of 9.5 years, and the mechanism
of injury was forced supination in 3 of the patients. They all had
associated midtarsal injuries and presented with significant swelling.
The key to making the diagnosis, which was delayed in 3 of the
patients, was subluxation or dislocation of the calcaneocuboid joint on
the lateral radiograph. The AP view only showed the dislocation in 2
patients and the oblique view showed it in only 1 patient.
with percutaneous K-wires. If an anatomic reduction is not possible
closed, then one must proceed to an open reduction.
associated injuries to both the midtarsal bones and rest of the foot.
One of the patients in Hosking and Hoffman’s66
series had an ipsilateral tibial fracture so associated injuries may be
present due to the amount of force required to cause a midfoot
disruption in a child.
navicular, cuboid, and cuneiforms are usually fractured in association
with a Chopart joint (talonavicular and calcaneocuboid) dislocation or
a serious Lisfranc injury. The navicular has a number of conditions
that can mimic a fracture. Between the ages of 2 and 5 years, the
navicular can become avascular (Kohler disease) and cause pain and limp
while the changes seen on radiograph can look similar to a fracture (Fig. 27-25). Likewise, an
accessory navicular may be present that may mimic an avulsion fracture
of the navicular tuberosity. These can be differentiated from a
fracture as they have smooth, rounded edges and are usually symmetrical
when a radiograph is taken of the other foot. Stress fractures of the
navicular are also becoming an increasingly common problem as children
and adolescents train more aggressively for competitions (see stress
fractures of the foot). These stress fractures usually run in the
sagittal plane in the middle third of the bone. They are often
difficult to see on plain radiographs but are more easily seen on bone
scans, CT, and MRI.
 |
|
FIGURE 27-25 Kohler disease of the navicular that can occasionally be confused with a stress fracture.
|
children and were usually associated with other foot fractures. Recent
literature, however, reveals that this fracture may occur more often
than we thought and commonly in isolation. Senaran et al.152
reported on 28 consecutive cuboid fractures in preschool children from
1998 to 2004. They found most patients had an avoidance gait pattern
and walked on the outside of their foot. They used the “nutcracker”
maneuver to help diagnose the fracture. To perform this test, the heel
is stabilized by the examiner and the forefoot is abducted. Pain in the
lateral aspect of the foot usually confirms a fracture of the cuboid.
The diagnosis was then confirmed on initial or subsequent radiographs.
A below-knee cast or Cam walker was used for 2 to 3 weeks and all
fractures healed without complications. Six patients had ipsilateral
fractures in the tibia or foot. Interestingly, 8 patients had an
associated genetic or systemic abnormality.152 Cuboid fractures have been classified by Weber and Locher169 into distal impaction shear-type fractures (type 1) and burst fractures (type 2).
reported on 4 female teenagers who had equestrian injuries and cuboid
fractures. The mechanism of the injury in all cases was a crush to the
foot when the horse fell and abduction of the forefoot while it was
still in the stirrup. All four cuboid fractures were associated with
multiple midfoot fractures and the authors recommend CT scans in all
patients in this age group with a cuboid fracture. Two patients
required surgical reconstruction. This was performed through a lateral
incision from the tip of the fibula to the base of the fifth
metatarsal. The interval is then developed between the peroneal tendons
and the extensor digitorum brevis. The lateral column length of is then
restored using an allograft block.30
to as a Lisfranc injury, are more common in adults than they are in
children.175 The degree of injury
varies from a subtle disruption of the Lisfranc ligament to an
extensive fracture-dislocation of the forefoot. Subtle injury can be
difficult to diagnose especially if it is not thought about and if left
untreated can develop into a painful chronic problem.
foot, usually secondary to a falling object, or indirect, where there
is forced plantarflexion of the forefoot combined with a rotational
force (Fig. 27-26 ).172,173
indirect injury where a load is applied to the foot while it is in the
tiptoe position. A common example of this injury is jumping to the
ground and landing awkwardly on the toes, producing acute
plantarflexion at the TMT joint. The result is a TMT joint dislocation
and usually a fracture at the base of the second metatarsal. Another
example would be by putting the foot down suddenly to reduce speed
while riding a bike.
is in a kneeling position when the impact load strikes the heel. This
is an example of a direct compression type injury and usually results
in lateral dislocation of the lesser metatarsals and fracture of the
base of the second metatarsal.
falls backward while the forefoot is fixed to the ground by a heavy
weight. An example would be a fall backwards while the foot was pinned
under the wheel of a car. The patient’s heel, which is resting on the
ground, becomes the fulcrum for the forefoot injury.
of 18 patients with TMT joint injuries, 10 (56%) were a fall from a
height in the “tiptoe” position, 3 (18%) suffered “heel to toe”
compression, and 4 (22%) sustained a fall backwards while their
forefoot was pinned to the ground. One patient could not recall their
mechanism of injury following a motorbike collision.
in miniscooter injuries where the foot is planted to break speed. The
resulting dorsiflexion, axial loading, and abduction cause the
metatarsals to be impacted laterally. The result is a fracture of the
base of the second metatarsal and a crush fracture of the cuboid.13
Some of the injuries are subtle and will present with minor pain and
swelling at the base of the first and second metatarsals. This can be
accompanied by ecchymosis on the plantar aspect of the midfoot where
the TMT ligaments have been torn (Fig. 27-27).139 This can be confirmed by gently abducting and pronating the forefoot while the hindfoot is held fixed with the other hand,114
though this would be quite painful acutely. Alternatively, the child
can be asked to try and perform a single limb heel lift. Pain in the
midfoot often implies a TMT joint injury. With significant trauma,
there is greater ligamentous injury and the resulting swelling makes it
difficult to recognize
any
bony anatomy. It is important to assess the foot for a compartment
syndrome in such circumstances, particularly when the foot has been
crushed as part of the mechanism of injury.
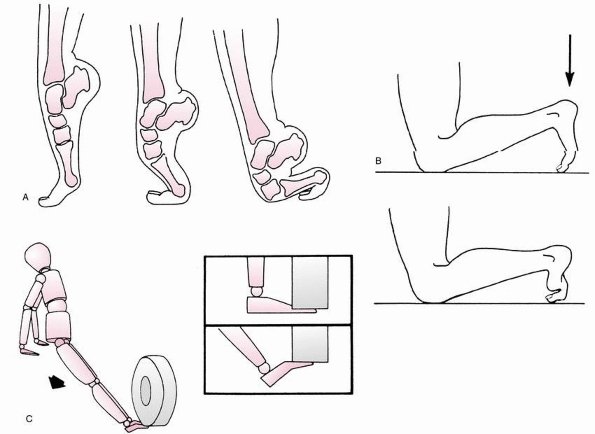 |
|
FIGURE 27-26 Mechanism of Lisfranc injuries. A. The most common mechanism of injury: progression from the “tiptoe” position to complete collapse of the TMT joint. B. Plantarflexion injury: direct heel-to-toe compression produces acute plantar flexion of the TMT joint. C. Backward fall with the forefoot pinned.
|
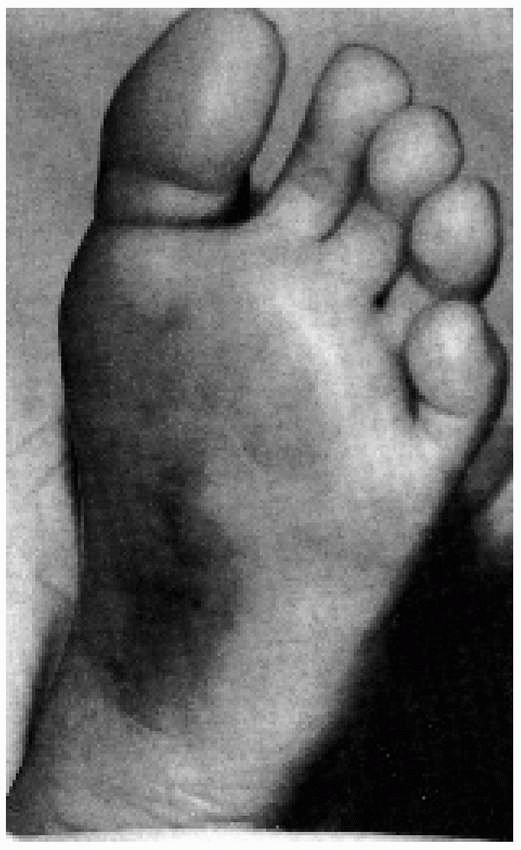 |
|
FIGURE 27-27
Plantar ecchymosis sign. Ecchymosis along the plantar aspect of the midfoot is an important clinical finding in subtle Lisfranc TMT injuries. (From Ross G, Cronin R, Hauzenblas J, et al. Plantar ecchymosis sign: a clinical aid to diagnosis of occult Lisfranc tarsometatarsal injuries. J Orthop Trauma 1996;10:120.) |
to have a high level of suspicion for a Lisfranc injury as they are
uncommon and difficult to diagnose but have a poor prognosis if left
untreated.
the entire metatarsal joint in a single plane. This can be either
coronal or sagittal or combined.
the joint is seen involving either medial displacement of the first
metatarsal or lateral displacement to the four lateral metatarsals. The
medial dislocation involves displacement of the first metatarsal from
the first cuneiform because of disruption of the Lisfranc ligament or
fracture at the base of the metatarsal, which remains attached to the
ligament.
be displaced laterally. This is associated with partial or total incongruity.
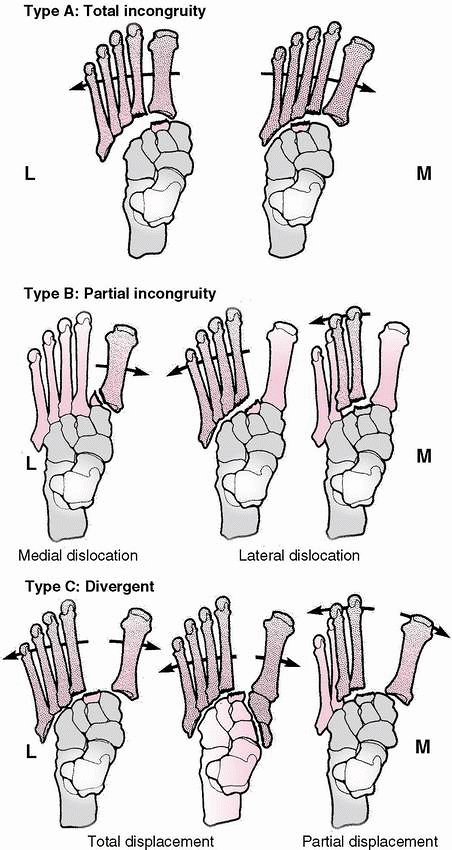 |
|
FIGURE 27-28 Classification of TMT dislocations. L, lateral; M,
medial. (From DeLee JC. Fractures and dislocations of the foot. In: Mann RA, Coughlin MJ. Surgery of the Foot and Ankle. 6th ed. St. Louis: Mosby, 1993:1465-1703, with permission; From Hardcastle PH, Reschauer R, Kutscha-Lissberg E, et al. Injuries to the tarsometatarsal joint: incidence, classification, and treatment. J Bone Joint Surg Br 1982;64:349-356.) |
oblique views of the foot. These should be performed weight bearing if
possible to stress the joint complex.
metatarsal should be in line with the lateral border of the medial
cuneiform and the medial border of the second metatarsal should line up
with the medial border of the middle cuneiform. On the oblique
radiograph, the medial border of the fourth metatarsal should be in
line with the medial border of the cuboid. The examiner looks for a
disruption in these lines or diastases of greater than 2 mm between the
base of the first and second metatarsals. It is very useful to obtain a
weight-bearing radiograph of the opposite foot for comparison (Fig. 27-29).
When the radiographs appear normal or minimally displaced and a
Lisfranc injury is still suspected, alternative imaging with CT or MRI
scans is strongly recommended. The CT scan will often show a small
avulsion fracture of the first TMT ligament and will show any other
associated fractures in the foot.55,87,99 The MRI scan can accurately visualize a partial tear or complete rupture of the first TMT ligament.128
alert the examiner to the possibility of a TMT dislocation because
these injuries can spontaneously reduce. Likewise, a cuboid fracture in
combination with a fracture of the base of the second metatarsal is
highly suspicious for a Lisfranc injury (Fig. 27-30).
abduction stress view can be obtained; however, in children these are
difficult to obtain without general anesthesia. Bone scans may be
helpful in the diagnosis of this injury when radiographs are normal,
although they are not specific for the severity of the injury57 and less useful than MRI or CT.
the apex of the longitudinal and transverse arches of the foot and
therefore its structural integrity is crucial in maintaining normal
foot function. At the same time, there needs to be enough motion
between the joints to allow the transfer of weight evenly from the
hindfoot to the forefoot during the walking cycle. This intricate
relationship is achieved by the anatomy of the tarsal and metatarsal
bones and the arrangement of the ligaments. These midfoot bones are
trapezoidal in cross section with their base dorsal. This creates a
“Roman arch” effect, which is structurally very strong and helps
maintain the transverse arch in the midfoot. The TMT joint complex can
be divided up into a medial column and a lateral column. The medial
column is a continuation of the talus and navicular and includes the
cuneiforms and the medial three metatarsals. The lateral column is a
continuation of the calcaneus and comprises the cuboid and the fourth
and fifth metatarsals which articulate with it. The medial column has
far less mobility than the lateral column, reflecting the increased
need for stability on the medial side of the foot to maintain the
longitudinal arch. This stability is also provided by the second
metatarsal which is “keyed” into the step formed by the cuneiforms.
This explains why the second metatarsal is usually fractured when a
dislocation occurs across the TMT joint. The ligaments also play a big
role in maintaining stability medially and movement laterally. The
plantar ligaments are extremely strong compared to the weaker dorsal
ligaments. The intermetatarsal ligaments help bind the lateral four
metatarsals together but are absent between the first and second
metatarsals. Instead, the second metatarsal is connected to the medial
cuneiform by Lisfranc’s ligament (medial interosseous ligament) and an
avulsion fracture of this strong ligament can sometimes be seen on
radiograph (Fig. 27-31).173
 |
|
FIGURE 27-29
Weight-bearing radiographs show a subtle Lisfranc injury to the right foot. Weight-bearing radiographss are essential for diagnosis; using the opposite foot for comparison is also helpful. |
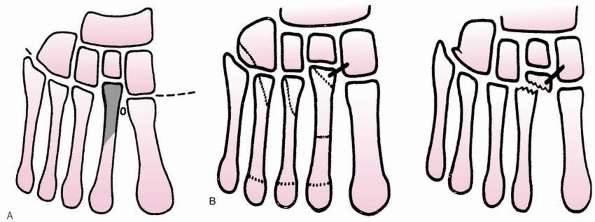 |
|
FIGURE 27-30 A. Second metatarsal is the “keystone” of the locking mechanism. B. Fractures of the cuboid and second metatarsal are pathognomonic signs of disruption of the TMT joints.
|
it courses between the first and second metatarsals to form the plantar
arterial branch. The deep peroneal nerve travels beside the artery but
continues on to supply sensation to the first web space. This
neurovascular bundle can be damaged by the injury and care must be
taken protect these structures when internally fixing these
fracture-dislocations. The tibialis anterior tendon inserts into the
base of the first metatarsal and medial cuneiform. The peroneous longus
tendon inserts into the plantar surface of the base of the first
metatarsal and acts as a flexor of this bone. Together, these two
muscles and their tendon insertions give added stability to the medial
column of the foot.
the extent of the injury and the degree of instability. Once this is
established, the appropriate treatment can be instigated. In all these
injuries, a weight-bearing radiograph at the end of treatment should
confirm anatomic congruency of the TMT joint complex.
foot should be immobilized in a below-knee cast for 6 weeks. The MRI
scan may confirm a partial tear of the first TMT ligament, but
regardless this painful injury takes time to heal and immobilization is
the best treatment. In young adult athletes, these injuries can take a
long time to heal.108 When there is
complete intraligamentous rupture or an avulsion fracture of the first
TMT ligament and no displacement of the joint surfaces, a below-knee
cast for 6 weeks is advised. Whether the patient should be weight bearing or not for the entire 6 weeks is debatable. Wiley173 treated the children with undisplaced TMT joint injuries in his series with 3 to 4 weeks of immobilization with good results.
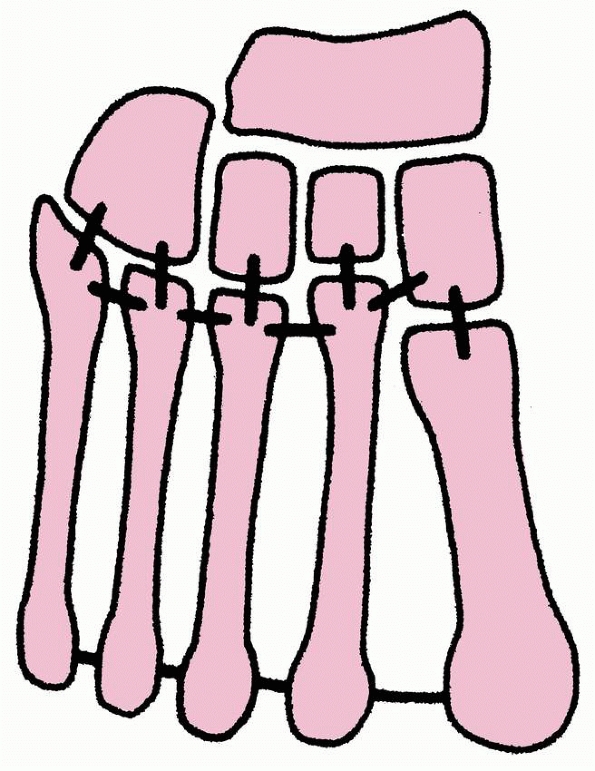 |
|
FIGURE 27-31
The ligamentous attachments at the TMT joints. There is only a flimsy connection between the bases of the first and second metatarsals (not illustrated). The second metatarsal is recessed and firmly anchored. (From Wiley JJ. The mechanism of tarsometatarsal joint injuries. J Bone Joint Surg Br 1971;53:474, with permission.) |
found that following a closed reduction greater than 2-mm displacement
or a talometatarsal angle of greater than 15 degrees would lead to a
poor outcome. A closed reduction is best carried out under a general
anesthetic when the acute swelling has subsided. “Finger traps” can
help with traction on the toes while the displaced metatarsals are
manipulated into place. If a stable anatomic reduction is achieved
clinically and this is confirmed radiologically, a well molded
below-knee cast can be applied. Radiographs in the cast should also be
taken while the patient is under anesthesia to confirm the reduction
has been held. The nonweight-bearing cast is worn for 6 weeks with
radiographs taken at 1 and 2 weeks to confirm the fracture-dislocation
has remained reduced.
but the fragments are unstable, then K-wire fixation is used to hold
the alignment of the foot. Stout 0.062 in smooth K-wires should be
used. Their placement is determined by the direction of displacement of
the metatarsals and how many are involved. The most important wire is
used to stabilize the second metatarsal to the medial cuneiform.
Additional wires can be used between the first metatarsal and the
medial cuneiform, and between the lesser metatarsals and their
corresponding tarsal bones. A useful wire can also be passed form the
first metatarsal to the second metatarsal. These K-wires are left bent
over outside of the skin and are removed at 4 to 6 weeks when
mobilization is initiated if the radiographs confirm healing. Again,
full weight-bearing radiographs are necessary when comfort allows and
after K-wire removal to confirm adequate stability. Wiley173
used K-wire fixation in 4 patients. He removed these at 3 to 4 weeks
and the alignment was maintained in all the children. There were some
joint incongruities from intra-articular fractures that were not
surgically addressed but they did not seem to alter the clinical
outcome.
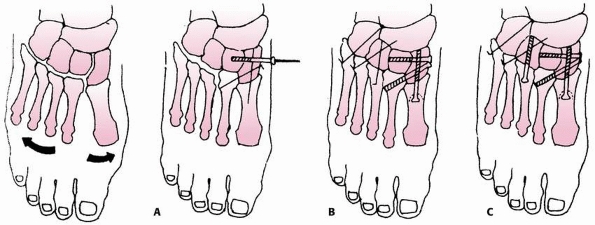 |
|
FIGURE 27-32 Sequence of repair for reduction and stabilization of TMT fracture dislocations. A. Stabilization of the first ray by alignment of the metatarsal, medial cuneiform, and navicular. B.
Stabilization of the Lisfranc ligament by accurate alignment of the second metatarsal to the medial cuneiform, as well as the medial and middle cuneiforms. C. Alignment and stabilization of the third through fifth metatarsal rays. Cannulated screws can be used instead of pins as needed for stability and compression. (From Trevino SG, Kodros S. Controversies in tarsometatarsal injuries. Orthop Clin North Am 1995;26:229-238, with permission.) |
for these fractures. It is indicated if there is greater than 1 to 2 mm
of joint displacement. The impediments to reduction are
-
Tibialis anterior tendon
-
Interposition of fracture fragments in the second metatarsalmiddle cuneiform joint.
-
Incongruity of the first metatarsal-medial cuneiform articulation15
One is made over the first-second metatarsal space and the second in
line with the fourth metatarsal. The medial incision allows
identification of the neurovascular bundle and access to the first and
second metatarsalcuneiform joints. The lateral incision allows the
joints of the lesser TMT joints to be clearly seen. After anatomic
reduction, the joints can held reduced with K-wires or internally fixed
with 3.5 mm screws (Fig. 27-32). Small chondral
defects can be excised and larger ones repaired. Care must be taken to
avoid the proximal growth plate of the first metatarsal if screw
fixation is used. The adult literature supports the use of K-wire
stabilization of the lesser metatarsals rather than screws as it is
important to maintain the mobility in these joints long-term.43
Debate exists as to when to remove the screws across these
weightbearing joints. In a child, it would seem appropriate to remove
the screws once pain free weight bearing is established as the
ligaments and bone would have healed by this stage and further
displacement is unlikely. Leaving the screws in longer than 3 months
risks damage to the joint and possible screw breakage.
these patients is confirming this diagnosis accurately and treating
them until the joint is stable. If any doubt in the diagnosis exists,
the author takes a comparable radiograph of the other foot. The author
routinely orders a CT scan of the midfoot to assess the extent of the
injury and to look for any associated injuries.
treated in a below-knee nonweight-bearing cast for 6 weeks.
Weightbearing radiographs are taken on removal of the cast to assess
stability. These radiographs are repeated 6 weeks later once pain free
weight bearing is achieved to confirm no further displacement.
then the author performs a closed reduction and routinely uses
percutaneous K-wire fixation with image intensifier control. Although
these injuries can be held with cast immobilization, the author prefers
the assurance of knowing the fracture-dislocation is being held
internally. This is especially useful when the foot is very swollen and
repeated assessments are necessary to rule out compartment syndrome. In
the rare circumstance of an open reduction, the author prefers to use
temporary screw fixation. These injuries are usually far more severe
than a type B dislocation and the TMT joints are very unstable. After
open reduction through two longitudinal incisions, 3.5-mm cortical
screws are used to hold the reduction taking care to avoid the proximal
growth plate of the first metatarsal. These screws are removed usually
within a month of cast removal.
treated, all these patients must be investigated at outpatient
appointments with weight-bearing radiographs to confirm that the
ligaments have healed and there is no residual subluxation.
posttraumatic arthritis. This can often occur because the injury is
“missed” and the subtle fracture-dislocation remains displaced. Another
cause is a loss of reduction. Lastly, the trauma itself can damage the
articular cartilage and, despite an anatomic reduction, arthritis can
develop.
found similar results in athletes who had a delayed diagnosis. This
reinforces the importance of making the diagnosis early and treating
appropriately.
injuries in a significant percentage of adults, and this is best
prevented by achieving an anatomic reduction.114 Wiss et al.176
performed gait analysis on 11 adult patients with TMT joint
fracture-dislocations and found that no patient walked normally after a
displaced TMT fracture-dislocation. In Wiley’s173
series of 18 children, none of whom required open reduction, 14
patients were asymptomatic 3 to 8 months postinjury. Four patients had
persisting pain of minor severity at the TMT joint 1 year following
injury. Two of these patients had residual angulation at the injury
site. One patient had an unrecognized dislocation and had not been
treated; the other had not had an anatomic reduction due to extensive
intra-articular fractures. One 16-year-old patient developed
asymptomatic osteonecrosis of the second metatarsal head, and this was
attributed to a possible compromise of the blood supply at the time of
injury as the nutrient vessel to this area is a terminal branch of the
dorsalis pedis. Buoncristiani et al.22
followed 8 children (3 to 10 years old) with indirect TMT joint
injuries treated in a below-knee cast and found 7 were asymptomatic at
an average follow-up of 32 months. The one patient who had midfoot pain
had developed early degenerative changes on the plain radiographs.
arthrodesis if conservative care has failed. In children this would be
extremely unusual. An arthrodesis often requires extensive soft tissue
release to allow anatomic reduction of the joint and then rigid
internal fixation with screws. It is important not to fuse the lesser
TMT joints as mobility here is important for the long-term function of
the foot.
fractures of the foot in children, accounting for up to 60% of all
pediatric foot fractures.35,36,119,155 Owen et al.119
showed in an epidemiologic study that in children younger than 5 years
of age, 73% of metatarsal fractures involve the first metatarsal,
whereas in children older than 10 years these fractures accounted for
only 12%. The most common metatarsal fracture for all 60 patients was a
fracture of the fifth metatarsal (45%). Six and a half percent of all
the fractures and 20% of first metatarsal fractures were not diagnosed
at the initial consultation in their series.
indirect injury. Direct injuries are usually caused by a heavy load
falling on the forefoot or a crush injury (i.e., the foot being run
over by a car). The metatarsals can be fractured anywhere along the
shaft but typically they are fractured middiaphyseal. Indirect injuries
are caused by axial loading or torsional forces and usually produce
spiral fractures of the proximal shaft or neck of the metatarsal.
Singer et al.155 found in a recent
study of 125 children that if the patient was less than 5 years of age,
the primary mechanism was a fall from a height and this usually
occurred within the home. In children older than 5 years of age, most
injuries occurred while playing sport and occurred on a level playing
surface.
bruising of the foot due to the extensive soft tissue injury as well as
the metatarsal fractures. Careful evaluation of a compartment syndrome
should take place. An indirect injury usually has more subtle clinical
findings and careful palpation will usually locate the site of the
fracture. The infant with a metatarsal fracture due to an unwitnessed
injury may present with minimal swelling but an inability to bear
weight.
associated with tarsal fractures or fracture-dislocations, and this
should be evaluated
further
with a CT scan. A fracture of the second metatarsal and a cuboid
fracture is highly suggestive of a TMT joint dislocation rather than
two isolated fractures. Singer et al.155
found that the first and fifth metatarsals were usually isolated
fractures, whereas if multiple metatarsals were fractured, they were
always contiguous bones and involved the second, third, and fourth
metatarsals.
and oblique views of the whole foot. The AP view often gives the
impression that the fractures are minimally displaced; however, the
lateral view often shows significant plantar or dorsal displacement.
Other associated fractures may be apparent on the plain radiographs and
if any doubt exists, especially if there has been significant trauma, a
CT scan is advised. In a young child, if a fractured metatarsal is
suspected but not visible on the initial radiograph, a repeat film can
be taken 10 to 14 days later that often shows the fracture line or
early callus.
first through fourth metatarsals. Fractures of the fifth metatarsal are
classified according to their location along the bone (see section on
treatment of the fifth metatarsal below).
treated nonoperatively in a below-knee cast. The child with a displaced
fracture often needs to be admitted overnight in the hospital for pain
relief and observation for compartment syndrome.The initial treatment
includes elevation for the severe swelling that coexists with the
fractures. Immobilization may be performed by a well padded cast,
splint, or a Cam walker.. Once the swelling subsides, a molded
below-knee cast can be applied. Weight bearing can be initiated when
pain allows, and the cast can usually be removed at 3 to 4 weeks at
which time the patient can be transitioned to a Cam walker.
child has not been determined. A closed reduction of the central
metatarsals is indicated in an adult if there is more than 10 degrees
angulation in the dorsal plain or more than 4 mm of translation in any
plane.153 These criteria may be
appropriate for an older adolescent whose growth plates had closed but
are far too stringent for a skeletally immature patient. If there is
severe dorsal angulation of greater than 20 degrees or “tenting” of the
skin and shortening of greater than 5 mm, then a closed reduction is
indicated. This is best performed under a general anesthetic when the
swelling has subsided. Finger traps have been advocated by some
surgeons to help with traction while the metatarsals are manipulated. A
below-knee cast can be molded with pressure applied to both the dorsal
and plantar aspects of the foot; however, the need to allow for
swelling suggests implants should be used to hold fracture reduction
rather than molding of a cast. To accomodate the swelling and to relax
the plantar fascia, the cast can be applied with the ankle in slight
equinus and when it is changed 2 weeks later, it can be bought up into
a neutral position.
especially in the adolescent patient. The first ray is important in
maintaining the longitudinal arch of the foot and the position of the
first metatarsal head in relation to the lesser metatarsal heads is
also vitally important. A closed reduction should be considered if
there is greater than 10 degrees of dorsal angulation or any shortening
of the first metatarsal. It is unusual to have angulation in the
coronal plane if the second metatarsal is intact and transverse
displacement is acceptable if there is no shortening.
at times required. Intramedullary placement is difficult to perform
without opening the fracture and passing the wires under direct vision.
Small, dorsal, longitudinal incisions are made over the fracture sites
and dissection is carefully carried out down to the fracture. The wire
is drilled down the distal fragment to exit the plantar skin. The wire
is then withdrawn enough to allow the fracture to be reduced, then the
wire is driven retrograde across the fracture site and sufficiently far
enough into the proximal fragment. Another technique is to hold
fracture reduction by placing K-wires across the fractured metatarsal
to an adjacent nonfractured metatarsal both proximal and distal to the
fracture. The K-wire is cut and bent outside the skin to facilitate
removal in the outpatient clinic in 3 to 4 weeks when the patient can
be placed in a walking cast for 2 further weeks to allow fracture
consolidation. This is the same technique that can be used on the rare
occurrence an open reduction is required for an irreducible fracture or
when the fracture is open.
metatarsal fracture in children, comprising almost 50% of all
metatarsal fractures in some series.64,119,155
Traditionally, treatment has been based on treatment algorithms from
the adult literature. Fractures of the base of the fifth metatarsal are
discussed separately from the other metatarsal fractures as the
anatomy, fracture patterns, and treatment indications are quite
different.
insertions at its base. The peroneus brevis tendon inserts on the
dorsal aspect of the tubercle and the peroneus tertius attaches on the
dorsal aspect of the fifth metatarsal at the metaphyseal-diaphyseal
junction. The strong plantar aponeurosis inserts into the plantar
aspect of the tubercle at the base.
metatarsal medially at the junction of the proximal and middle thirds
of the diaphysis and sends intraosseous branches proximally and
distally (Fig. 27-33). Proximally within the bone are the metaphyseal
vessels, and the small area where these overlap with the proximal
vessels from the nutrient artery is known as the watershed area. This
region corresponds with Zone 2 and fractures in this area have a higher
rate delayed of union or nonunion in those close to maturity The
proximal apophyseal growth center of the fifth metatarsal can often be
confused for a fracture. The apophyseal growth center (os vesalianum)
has a longitudinal orientation roughly parallel to the metarsal shaft
and generally has smooth contours which distinguish it from a
transverse orientated fracture (Fig. 27-34). The os vesalianum usually appears by the age of 9 years and unites with the metaphysis between the ages of 12 and 15 years (Fig. 27-35).
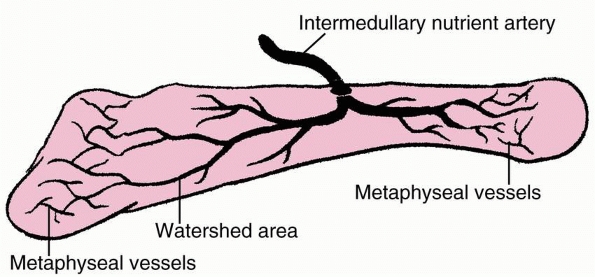 |
|
FIGURE 27-33 Blood supply of the proximal fifth metatarsal.
|
 |
|
FIGURE 27-34 A. A normal apophysis of the base of the fifth metatarsal at the attachment of the peroneus brevis (arrow) in a 10-year-old girl. B. The thicker arrow points to the normal apophysis, which is roughly parallel to the metatarsal. The thinner arrow points towards a fracture, which is roughly perpendicular to metatarsal.
|
 |
|
FIGURE 27-35
This 11-year-old girl had pain in her proximal fifth metatarsal after twisting her foot during physical education at school. No fracture was visible; however, her secondary ossification center is clearly seen running parallel to the shaft of the metatarsal. |
Zone 1 is the cancellous tuberosity, which includes the insertion of
the peroneus brevis tendon, the abductor digiti minimi tendon, and the
strong calcaneometatarsal ligament of the plantar fascia. Zone 2 is the
distal aspect of the tuberosity where the dorsal and plantar
ligamentous attachments to the fourth metatarsal attach to insert. Zone
3 is the region that extends from distal to these ligamentous
attachments to approximately the middiaphyseal area. Herrera-Soto et al.64 tried to define this classification further in their recent review of 103 children with fifth
metatarsal fractures. They define a type I fracture as a “fleck”
injury. A type II fracture is a tubercle fracture with an
intra-articular extension, and a type III fracture represents a
fracture at the proximal diaphyseal region (Jones fracture).
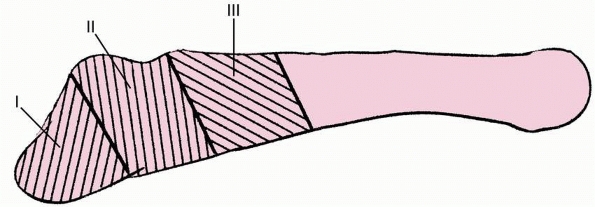 |
|
FIGURE 27-36 The three anatomic zones of the proximal fifth metatarsal.
|
algorithms from the adult literature. Treatment of fractures of the
base of the fifth metatarsal in children is determined primarily by the
zone of the fracture, and somewhat by age.
traction-type injuries where the force from the peroneus brevis tendon
and the pull from the plantar aponeurosis result in an avulsion
fracture of the fifth metatarsal. Some authors suggest the fracture may
be an avulsion at the origin of abductor digiti minimi.78,137 Treatment involves a weight-bearing below-knee walking cast for 3 to 6 weeks. Herrera-Soto et al.64
found all 30 of their children with an extra-articular type 1 fracture
treated in this way healed with good outcomes even if they were
displaced. Undisplaced intra-articular tuberosity fractures also healed
well in the series64; however,
displaced (>2 mm) intra-articular fractures took significantly
longer to heal. Radiographic union usually lags behind resolution of
symptoms, and most patients are asymptomatic after 3 weeks.64
This delay in radiographic union should not prevent the child returning
to full activities as symptoms allow. Treatment with a Cam walker
rather than a cast may be considered. Nonunion can occur but usually is
asymptomatic.37 Although operative
fixation of acute tuberosity avulsions rarely is indicated, it may be
considered for significant displacement (more than 3-mm) in young
active patients who want to return to competitive sports sooner (Fig. 27-37).
 |
|
FIGURE 27-37 A. A 12-year-old boy who is a professional snowboarder with a displaced, intra-articular fifth metatarsal fracture. B. This was reduced open and internally fixed, which allowed him to compete 8 weeks after surgery.
|
fracture. This is an oblique fracture in the watershed area at the
proximal metaphyseal-diaphyseal junction. It typically occurs in
adolescents and is thought to be caused by a combination of vertical
loading and coronal shear forces at the junction of the stable proximal
metaphysis and the mobile fifth metatarsal diaphysis. Frequently, these
fractures are stress injuries, usually involving athletic adolescents
who present with a traumatic event superimposed on prior symptoms.24,34,76,77,86,142
A good history is important to determine the duration of symptoms
because chronic injuries are unlikely to respond to nonoperative
treatment
as well as acute fractures. Critical radiographic analysis will also show cortical sclerosis in the chronic injuries.
non-weight-bearing cast for 6 weeks. Serial radiographs and
examinations are necessary to determine adequate healing, and further
non-weight-bearing immobilization may be necessary if the fracture has
not healed clinically and radiographically at 6 weeks. With evidence of
callus and diminished tenderness, the patient can begin protected
weight bearing in a hard-soled shoe or Cam walker for an additional 4
weeks. This protected weight bearing may prevent refracture.64 In a series of adults, Torg et al.164
reported successful healing in 14 of 15 patients treated with
non-weight-bearing casts, whereas only 4 of 10 who were allowed to bear
weight went on to union. Herrera-Soto et al.64
reported 15 fractures in this zone (type III) and found a higher rate
of delayed union and refracture in patients over 13 years of age. They
feel that primary internal fixation in this age group may be indicated.
been present for more than 3 months, nonoperative management is
unlikely to be successful. Nonetheless, it is worthwhile initially
trying 6 weeks immobilization in a non-weight-bearing below-knee cast
or brace. If this fails, then internal fixation is required. A useful
technique is to insert an intramedullary screw from proximal to distal
which stabilizes the fracture site. A 4-mm cancellous screw is usually
sufficient; however, in an older adolescent with a capacious
intramedullary canal, a 6.5-mm cancellous screw may give better
fixation and compression. It is beneficial to curette the
intramedullary canal and use cancellous bone graft, which can be
harvested from the distal tibia (Fig. 27-38).88
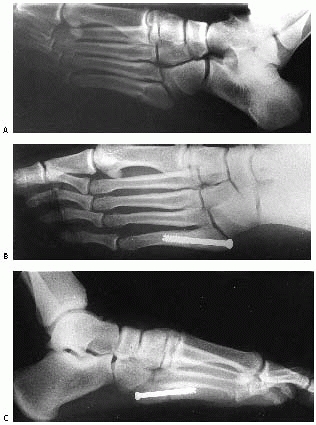 |
|
FIGURE 27-38
This 15-year-old high-level basketball player sustained a proximal fifth metatarsal fracture at the metaphyseal-diaphyseal junction. The patient chose intramedullary screw fixation because of his desire to return to sport as promptly as possible, lessen his time in immobilization, and lessen the risk of delayed union or nonunion. A. Radiograph at time of injury. B,C. After intramedullary screw fixation. (Courtesy of Keith S. Hechtman, MD.) |
fractures in active athletes. Acute fractures in this zone with no
prodromal symptoms can be treated with a below-knee non-weight-bearing
cast for 6 weeks followed by protective weight bearing for 4 weeks. In
the more common scenario, where the patient complains of pain with
activity for several months, this period of casting is often
unsuccessful but worth trying in the first instance. The stress
fracture may heal clinically with 6 to 12 weeks of immobilization and
radiographs will confirm the reconstitution of the medullary canal and
less sclerosis at the fracture site. Electrical stimulation may be
used. If the chronic stress fracture does not heal, then surgical
intervention is required
similar
to that in a zone 2 fracture outlined above. Some authors advocate a
more aggressive open débridement of the fracture site with bone
grafting before introducing the intramedullary screw.131,164
the proximal fifth metatarsal is a painful nonunion. This is more
common in zone 2 and zone 3 fractures and rarely occurs in zone 1.
Herrera-Soto et al.64 concluded that
pediatric fifth metatarsal fractures behaved similarly to adult
fractures and can be treated the same. If a symptomatic nonunion
develops and surgery is indicated, a thorough débridement of the
sclerotic medullary canal should be undertaken, the area bone grafted,
and strong compression achieved across the fracture site with the
appropriate size intramedullary screw.54
nonoperatively in a below-knee walking cast for 3 to 4 weeks. Grossly
displaced fractures in older children with greater than 20 degrees of
dorsiflexion or more than 5 mm of shortening are treated with closed
reduction under a general anesthetic and a well molded below-knee cast.
If the reduction is difficult, percutaneous K-wires are used for
supplementary support. Except for open injuries, rarely is an open
reduction through longitudinal incisions required.
fifth metatarsal is treated by closed reduction and crossed K-wire
fixation.
challenging problem. Treatment is determined by the location of the
fracture in the bone and the age and activity level of the child. If
inadequately treated, they can go on to a delayed or nonunion. For zone
1 fractures that are intra-articular and displaced greater than 3 to 4
mm, the author recommends open reduction and internal fixation with a
3.5-mm partially threaded screw, especially if the child is involved in
competitive sports, as this will allow an earlier return to sport. This
fixation is perpendicular to the fracture line and gives maximum
compression. The screw is inserted through a direct lateral approach.
Care must be taken to identify and protect the sural nerve which is
usually directly under the incision. The peroneous brevis and peroneous
tertius tendons are identified, and the area between them at their
insertion into the proximal fifth metatarsal is a good starting point
for the screw. The author prefers to insert a bicortical cannulated
compression screw, and this can either be a partially threaded
cancellous screw or a fully threaded cortical screw. The fracture can
usually be indirectly reduced and held with a K-wire. In difficult
fracture patterns or in delayed presentations, the fracture line needs
to be clearly seen and can be held reduced with a compression clamp.
the patient in a nonweight-bearing cast for 6 weeks and then protected
weight bearing in a moon-boot for 2 to 4 weeks as comfort allows. The
recent study by Herrera-Soto et al.64
showing poor results with this treatment in patients over 13 years old
may make primary internal fixation a better option in this age group.
internal fixation. The author prefers to perform this with an
intramedullary screw which compresses the fracture site. If a 3.5-mm
cancellous screw does not achieve adequate internal fixation in the
medullary canal, the author increases the diameter of the screw until
it does. Often, a 4.0-mm malleolar screw is used. A small curette is
used down the medullary canal to help remove the sclerotic bone. If
this is not possible, the fracture site should be débrided open with
small osteotomes and rongeurs. Bone grafting is required for these
chronic injuries and can be harvested from the distal tibia.
are treated with closed reduction and cast immobilization for 6 weeks.
Occasionally, crossed K-wires are required.
Most toe injuries are treated by primary care physicians, so
orthopaedic surgeons only see the more severe fractures. Phalangeal
fractures are the result of direct trauma by a falling object or
indirect trauma when the unprotected toe is struck against a hard
object (so-called “stubbing”). The proximal phalanx is more commonly
injured than the distal phalanges.
skin especially at the base of the nail as this may indicate an open
Salter-Harris fracture with an associated nailbed injury. These
compound injuries require a thorough débridement, repair of the
nailbed, and often a single longitudinal K-wire to stabilize the
fracture (Fig. 27-39). IV antibiotics should be
given for 24 hours followed by 7 days of oral antibiotics. Nailbed
injuries should be repaired as meticulously as in the hand. A poorly
repaired germinal matrix will cause abnormal nail growth and difficulty
with shoewear long after the fracture has healed.
reduction and can be treated by simple “buddy strapping” to the
adjacent toe and immediate mobilization. A hard sole shoe or Cam walker
may help; however, crowding in the toe box may make this more
uncomfortable than bare feet. An angulated toe in both the coronal and
sagittal plane usually remodels well if the growth plate is still open.
In adolescents, a percutaneous K-wire can be used if the fracture is
grossly unstable and unable to be held reduced by strapping alone. This
wire can be passed longitudinally through the tip of the affected toe
or obliquely across the fracture. It is extremely unusual to get any
growth disturbance from a smooth wire crossing the growth plate in the
phalanges. These pins can be removed in clinic 4 to 6 weeks later.
Laterally angulated fractures of the little toe sometimes need closed
reduction before strapping them to the fourth toe.
lesser toes. Standard AP and lateral radiographs are taken; however, it
is useful to have the patient hold the lesser toes dorsiflexed with a
small towel to maximize visualization on the lateral view.
Intra-articular fractures of the proximal phalanx are more common in
the great toe than the other toes. They are usually Salter-Harris type
III or IV fractures (Fig. 27-40). Most of these fractures
can be managed with “buddy-strapping” to the second toe; however, if
greater than 25% of the joint surface is involved and there is
displacement of more than 2 to 3 mm of the joint surface, reduction
should be performed. Fracture reduction may be held by strapping to the
second toe or a percutaneous K-wire. In the rare occasion that this is
not successful, an open reduction can be performed either through a
midlateral or dorsal incision. With diaphyseal fractures, axial
alignment and rotation both need to be addressed with the closed
reduction. Often, the clinical appearance of the toe following the
reduction is more useful than the postreduction radiograph as the toe
usually looks “fine” even though the radiograph shows malalignment.
 |
|
FIGURE 27-39 A.
This 7-year-old boy “stubbed” his toe barefoot on his bike and sustained a compound fracture of the tuft of the distal phalanx and associated laceration of the germinal matrix. B. Preoperative radiograph shows the small tuft fracture. C,D. The wound was thoroughly débrided, germinal matrix repaired, and a K-wire passed across the fracture to hold the fragment and soft tissues reduced. |
 |
|
FIGURE 27-40 A.
An 11-year-old boy with an intra-articular fracture of the proximal phalanx of the great toe. Successful treatment was achieved with simple buddy strapping. B. A lateral radiograph of the great toe is best taken with the lesser toes held flexed with a bandage. |
in the United States affecting children 20 years or younger with an
average age of 10.7 years. This incidence has not changed in 15 years,
indicating that new safety regulations have been ineffective.167
These accidents occur with all types of lawnmowers; however, the most
severe injuries are a result of a child being run over by a
riding-mower.97,168 Seventy-two percent of children who have severe lawnmower injuries are bystanders.42,168 Ross et al.,140
however, had a higher number of children in their series who fell off
the riding-mowers and were run over. Seventy-eight percent of all
lawnmower accidents occur in boys.167 Loder and colleagues97
reviewed 235 children who had a traumatic amputation and found that
these injuries are more common in the spring and summer. Children under
the age of 14 years are most susceptible to injury with those under the
age of 6 years having the greatest risk of death.115 The most common body region injured is the hand (34.6%), followed by the leg (18.9%) and the foot (17.7%) (Fig. 27-41).167
assessment of the injuries suffered and appropriate resuscitation.
Often, a large volume of blood has been lost from the time of the
accident to arriving in the emergency department. Once the child is
stabilized, a secondary survey can be conducted to assess the extent of
the injury to each limb. With regard to the foot, these injuries are
mutilating and heavily contaminated with soil and grass. After
inspection, the wound should be dressed and a firm bandage applied to
prevent further bleeding. Antibiotics need to be administered as soon
as possible and include a cephalosporin, aminoglycoside, and
penicillin. The patient’s tetanus status should be ascertained and
tetanus prophylaxis administered if unknown.
operating room for the initial débridement. Considerable time should be
spent removing the foreign material as meticulously as possible. A
water jet lavage system can be useful, but should be used with care as
it can force debris further in to the soft tissue envelopes.
Devitilized tissue should be débrided; however, questionable tissue
should be left as there will be multiple return trips to the operating
room when further débridements can take place. It is useful to involve
a plastic surgeon even at this initial surgery so they can see the
extent of the damage and start planning for definitive coverage. The
child will generally need at least three trips to the operating room
and some cases many more.42 These return trips should be every 24 to 48 hours depending
on the state of the wound. Each débridement is important and should not
be left to the most junior member of the surgical team to perform.
Every piece of viable skin is vital and may be the difference between a
primary closure over an amputation stump or a skin graft or tissue
transfer. There is no hurry to close the wound until the soft tissue
and bone is completely free of foreign material and the tissues are
well perfused. Shilt and colleagues154
have found the use of VAC safe and effective in managing these types of
lawnmower injuries. Fractures need to be stabilized and initially
external fixation is useful. This allows plenty of room for further
débridements and does not compromise later internal fixation once the
soft tissue coverage has been determined.
 |
|
FIGURE 27-41
A 4-year-old boy with a severe lawnmower accident after being run over by the driver. There was extensive soft tissue loss and compound fractures to the foot. Despite multiple débridements, the leg was amputated below the knee. |
When the soft tissue defect is large or there is exposed bone that
would be better to preserve than excise, a free tissue transfer is
helpful.46,94 Lin et al.95
recently reviewed 93 microsurgical reconstructions of soft tissue
defects of the pediatric foot. They reported excellent results with
free musculocutaneous flaps or skin grafted muscle flaps. For plantar
foot reconstructions, the musculocutaneous flaps had better results
with fewer tropic ulcers and fewer resurfacing procedures. They also
found that reconstruction of the tendons in the immediate setting led
to fewer subsequent operations than staged tendon reconstructions.95
treating these severe injuries is whether to salvage the affected part
of the limb or amputate the questionable part. This decision is largely
based on what the functional outcome will be with either treatment and
what effect prolonged treatments and hospitalizations will have on the
child. Amputation rates vary between 16% and 78% in the literature.7,42,168 A mangled extremity severity score (MESS) has been developed in adults to help surgeons make these decisions.75. The MESS score was validated in children by Fagelman and coworkers48;
however, they did not include fractures below the ankle. It is useful
to ask for a colleague’s advice when contemplating an amputation so the
advantages and disadvantages can be freely debated. If an amputation is
performed, as much length of the bone should be preserved as possible,
and transdiaphyseal amputation should generally be avoided to prevent
problems with stump overgrowth.2,98
reviewed the functional outcome of 21 children with lawnmower accidents
and found that patients who had their injury confined to the forefoot
had 88% of normal function compared to 72% of normal function in
patients who had sustained injuries to the posterior and plantar
aspects of their foot.
with severe soft tissue injuries in the presence or absence of
associated fractures. Most commonly, it occurs with severe crush
injuries of the forefoot where there are multiple fractures and
dislocations; however, it can occur without any fracture, such as the
case of a car running over a foot causing crush and shear injury to
soft tissue. The symptoms are not as obvious as they are in compartment
syndrome of the forearm or leg, and increased pain with passive motion
of the toes is not always present. There is significant pain from the
injury itself, which often requires considerable amounts of pain
relief. Pallor, pain on passive extension, parasthesia, and a dorsalis
pedis pulse that is difficult to palpate likewise can all be clinical
signs in a large number of foot injuries. The clinician needs to have a
high index of suspicion for a compartment syndrome and if any doubt
exists, the compartment pressures should be measured or the child taken
urgently to the operating room for a decompression of the foot.
perform with invasive catheterization in an awake child with trauma to
the foot. Often, the compartments need to be measured under a general
anesthetic, so the child and parents need to be warned that the surgeon
may proceed to a decompression. There are nine compartments in the
foot, and it is difficult to confirm exact compartment location. It is
important, however, to measure the pressure in the calcaneal
compartment because it appears to be the most sensitive.103 When a pressure of greater than 30 mm Hg is measured in any compartment, a fasciotomy should be performed.103,113
It may be more accurate to use a measurement that takes into account
the patient’s blood pressure. In adults, the threshold is a measured
pressure that is less than 30 mm Hg below the patient’s diastolic blood
pressure.102
contain the intrinsic muscles and short plantar flexors. When a
decompression is carried out, all the compartments should be released
regardless of the clinical findings or compartment measurements. The
most thorough way to achieve this is by using
the three incision technique described by Myerson113 (Fig. 27-42).
Two dorsal longitudinal incisions are made in line with the second and
fourth metatarsals. Dissection is then carried out through the
interosseous compartments and fascia to enable decompression of the
deep plantar compartments. Puncturing the fascia and spreading with a
hemostat is an effective and safe technique. The lateral compartment is
decompressed through the incision over the fourth metatarsal by
dissecting deep to the fifth metatarsal. A medial incision is made
along the arch of the foot as far posterior as the medial malleolus.
This incision allows decompression of the medial compartment and a more
thorough decompression of the deep compartments. It also allows
decompression of the tarsal tunnel. Dissection is carried out on both
the dorsal and plantar surfaces of the abductor hallucis muscle,
freeing it from both the plantar fascia and bony attachments. Care must
be taken to avoid damaging the lateral plantar nerve and vessels which
lie on the quadrates plantae muscle. The deep compartments can now be
easily released under direct vision. These three incisions are usually
well placed to help with fracture reduction and K-wiring to stabilize
the foot at the same time as the decompression. The wounds should be
left open initially and closed 5 to 7 days later. Often, one of the
wounds will require split-skin grafting.
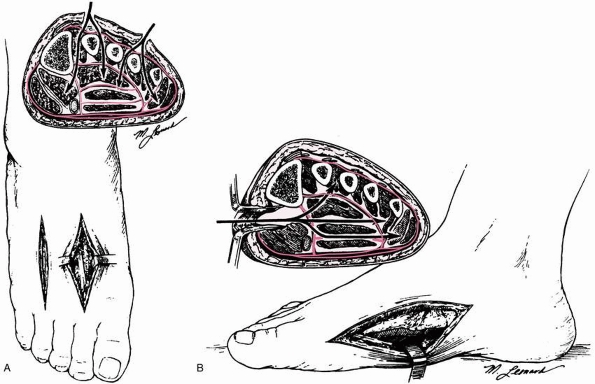 |
|
FIGURE 27-42 Surgical approaches for fasciotomy of the foot. A.
The dorsal approach is made through an incision over the second and fourth metatarsal shafts and is more suitable for injuries of the forefoot or midfoot. B. The medial approach is more suitable for injuries of the hindfoot, with the incision extending from the base of the first metatarsal to the medial malleolus. A tarsal tunnel release can be done through this incision. (From Myerson MS. Experimental decompression of the fascial compartments of the foot: the basis for fasciotomy in acute compartment syndromes. Foot Ankle 1988;8:308-314, with permission.) |
compartment syndrome can lead to disability including clawtoe
deformity, paresthesia, cavus deformity, stiffness, and residual pain.14,160
children and frequently treated by primary care physicians or in the
emergency department. Most injuries can be treated by simply removing
the offending foreign body, irrigating the entry site, giving tetanus
prophylaxis if required, and a short course of oral antibiotics. It is
important to carefully assess the foreign body that is removed to make
sure a small part of it has not been retained in the foot. Often, the
patient will bring the offending foreign body with them if it broke off
or came out spontaneously. The depth of penetration should also be
assessed by looking at the length of the foreign object as well as the
point of entry. This may help predict if a joint or tendon sheath has
been penetrated. The amount of contamination can also help determine if
an open débridement is necessary and the length of administration of
antibiotics.
wounds as occasionally a foreign body will be seen. If the foreign body
has punctured a joint, air may be seen as well. When a retained foreign
body is still suspected but not seen on radiograph, an ultrasound scan
can be useful to identify its location. An MRI scan is even more useful
at identifying foreign bodies and has the added advantage of showing
secondary changes of septic arthritis or osteomyelitis if the puncture
wound is more chronic (Fig. 27-43).
improve clinically, further investigation is required to rule out a
retained foreign body, deep soft tissue infection, septic arthritis, or
osteomyelitis. Eidelman et al.44
recommend that patients who have an established infection 24 to 36
hours after a puncture wound should be admitted to hospital for IV
antibiotics. In their series of 80 children with puncture wounds, a
delay in diagnosis or presentation was associated with deep infection.44 The most common organism causing deep infections in their study was Staphylococcus aureus and Group A Streptococcus.
A complete blood count, erythrocyte sedimentation rate, and C-reactive
protein should be performed, and an MRI scan is the most accurate
radiologic investigation.70,84 The patient can then be treated accordingly with IV antibiotics and open débridement of the entry site and deeper tissues.
 |
|
FIGURE 27-43
MRI scans are useful following penetrating foot injuries as the extent of the soft tissue or joint involment can be clearly seen. This 6-year-old boy had pain 4 days after standing on a nail in barefeet, and despite oral antibiotics he had developed a septic arthritis. |
a child presents with foot pain and swelling following a puncture wound
to the foot with a nail while wearing sneakers. Pseudomonas
osteochondritis is thought to occur when the cartilage is damaged at
the initial injury.50 The source of the pseudomonas is debatable; however, some authors have postulated that it is from the sneakers.49,85
The patient should be admitted to hospital and a thorough débridement
of the affected soft tissues, cartilage, and bone should be carried
out. IV antibiotics are administered often for 5 to 7 days or until the
infection has clearly resolved.72,73
The long-term sequelae of pain, growth arrests, chronic osteomyelitis,
and recurrence make this an important infection to identify early and
treat aggressively.
due to overtraining in youth athletics and year-round participation in
sports.31 The tibia, fibula, femur,
and pars interarticularis are the areas most commonly affected;
however, stress fractures in the foot can also occur.33,40,56,177
and this usually coincides with the beginning of an intense period of
training. The repetitive training results in bone fatigue and eventual
partial or complete fracture. The normal cortical bone remodeling is
accelerated and resorption occurs at a faster rate than the reparative
process resulting in weakening of the bone and inevitable
microfracture. Treatment, therefore, is aimed at breaking this cycle by
activity modification and protected weight bearing to prevent further
fracture and allow the reparative process to “catch up.”
pain on weight bearing and often no history of any particular injury
that may have been the cause. A thorough history of their training
regimen is essential, particularly any increases or changes in
technique playing surface or footwear. On examination, there is point
tenderness but minimal swelling. Radiographs taken early in the process
are often normal but later show periosteal layering of new bone on the
cortex and osteolysis at the fracture site. Bone scans are often more
sensitive initially and a threephase technetium bone scan is helpful
when the radiographs are normal in the first 2 to 3 weeks after the
onset of symptoms.45 MRI has been
shown to identify stress fractures before radiographic changes are
evident, and in a prospective study of collegiate basketball players,
MRI demonstrated marrow edema even before stress fractures were
clinically evident.101
patient should be assessed for any conditions that could predispose
them to stress fractures. These conditions include metabolic bone
diseases, amenorrhea, eating disorders, and incorrect training
techniques. There may have been as simple a cause as a change in
footwear that has lead to increased stress in a particular bone in the
foot.
foot to get a stress fracture. This usually occurs at the neck of the
metatarsal at the junction of the mobile shaft and rigid metaphysis.
Treatment involves rest and partial weight bearing in a moonboot for
4-6 weeks. It is best to avoid a cast as during this time the athlete
can maintain physical fitness with swimming, deep water running, and
exercycling. A gradual return to activity can be restarted when
radiographs confirm adequate healing and the symptoms have abated which
often takes 8 to 12 weeks. Stress fractures of the navicular are
disabling and difficult to treat. They occur most commonly in
basketball players, hurdlers, and runners.109 Bennell and Bruckner11
reviewed 18 large studies of stress fractures and found that the
incidence of navicular stress fractures can range between 0% and 28.6%
of injuries among track and field athletes. These fractures are thought
to arise due to overuse and the reduced vascularity that can exist in
the central third of the navicular. They are difficult to diagnose and
one needs to have a high level of suspicion as with any other stress
fracture. The fracture is often diagnosed by technetium bone scan, and
if this is positive in the region of the navicular, a CT scan is very
helpful in delineating the stress response from an acute injury. The
fracture line on CT, and if present on radiograph, is vertically
orientated in the middle third of the bone. Most of these fractures
heal with rest and protective weight bearing; however, some do go on to
delayed
or nonunion. The treatment for a painful nonunion is open reduction and internal fixation with autogenous bone grafting.127 The average time for the return to activity following a navicular stress fracture in athletes is 5.6 months.80
Stress fractures of the base of the fifth metatarsal usually occur in
zone 2 or 3 and their treatment is discussed earlier in the chapter
under the section sactures of the fifth metatarsal base.
NA, Dhawan S, Gruen GS, et al. Wound-healing risk factors after open
reduction and internal fixation of calcaneal fractures. Foot Ankle Int
1998;19(12):856-861.
DH, Galles KS, Marsh JL. Intra-articular calcaneal fractures treated
nonoperatively and followed sequentially for 2 decades. J Orthop Trauma
2006;20(7):464-469.
IF, Crichton KJ, Grattan-Smith T, et al. Osteochondral fractures of the
dome of the talus. J Bone Joint Surg Am 1989;71(8):1143-1152.
MD, Aquino L, Aquino JM. Talar neck fractures: a review of vascular
supply and classification. J Foot Surg 1986;25(3):188-193.
C, Lin SS, Cunningham FJ. Acute traumatic compartment syndrome of the
foot in children. Pediatr Emerg Care 2000;16(4):244-248.
W. Injuries of the foot. In: Beaty JH, Kasser JR, eds. Fractures in
Children. Philadelphia: Williams and Wilkins, 1955:195-196.
F, Barthelemy M. Injuries of Lisfranc’s joint: severe sprains,
dislocations, fractures. Study of 39 personal cases and biomechanical
classification. J Chir (Paris) 1976; 111(5-6):573-592.
R, Jackson M, Atkins R. Calcaneal fractures in adolescents. CT
classification and results of operative treatment. Injury
2003;34(6):454-459.
R, O’Brien J, McCormack R. Personal gait satisfaction of patients with
displaced intraarticular calcaneal fractures: a 2- to 8-year follow-up.
Poster Presentation 2770 in Orthopaedic Trauma Association Annual
Meeting: Salt Lake City, Utah; October, 2003.
AM, Manos RE, Mills WJ. Plantar-flexion tarsometatarsal joint injuries
in children. J Pediatr Orthop 2001;21(3):324-327.
KE, Reimer CD, Fields KB. Lisfranc injury of the foot: a commonly
missed diagnosis. Am Fam Physician 1998;58(1):118-124.
ST, Kelly FB Jr. Fractures of the neck of the talus. Long-term
evaluation of 71 cases. J Bone Joint Surg Am 1978;60(2):143-156.
N. Fractures and dislocations of the tarsal bones. In: Letts RM, ed.
Management of Pediatric Fractures. New York: Churchill Livingstone,
1994.
F, Faldini C, Piras F, et al. Surgical versus nonsurgical treatment of
calcaneal fractures in children: a long-term results comparative study.
Foot Ankle Int 2000; 21(10):825-832.
J. Fractures of the tarsal bones, metatarsals, and toes. In: Weber B,
Brunner C, Freuler F, eds. Treatment of Fractures in Children and
Adolescents. New York: Springer-Verlag, 1980.
D, De Rosa V, De Coulon G, et al. Cuboid nutcracker fracture due to
horseback riding in children: case series and review of the literature.
J Pediatr Orthop 2007;27(5): 557-561.
MA, Clarke NM. Bilateral “Jones” fractures of the fifth metatarsal
following relapse of talipes equinovarus. Injury 1996;27(8):599-601.
A. Fractures and dislocations of the foot and ankle. In: Green NE, ed.
Skeletal Trauma in Children. Philadelphia: WB Saunders; 1994 :449-516.
TB Jr. Fractures of the proximal fifth metatarsal: selecting the best
treatment option. J Am Acad Orthop Surg 1995;3(2):110-114.
JP, Azzoni M, Davidsion RS, et al. Major lower extremity lawn mower
injuries in children. J Pediatr Orthop 1995;15(1):78-82.
J. In: Rockwood CA, Green DP, Bucholz RW, et al, eds. Rockwood and
Green’s Fractures in Adults. Philadelphia: Lippincott Williams &
Wilkins, 2006:2337-2400.
M, Bialik V Miller Y, et al. Plantar puncture wounds in children:
analysis of 80 hospitalized patients and late sequelae. Isr Med Assoc J
2003;5(4):268-271.
EE, Gelfand MJ, Paltiel HJ. Bone scintigraphy in preschool children
with lower extremity pain of unknown origin. J Nucl Med
1992;33(3):351-354.
D, Lee B, Roberts CD, et al. Management of lawnmower injuries to the
lower extremity in children and adolescents. Ann Plast Surg
2000;45(6):595-600.
JW, Starr AJ, Early JS. Early wound complications of operative
treatment of calcaneus fractures: analysis of 190 fractures. J Orthop
Trauma 1999;13(5):369-372.
MT, Naranja RJ Jr, Glasgow SG, et al. Analysis of failed surgical
management of fractures of the base of the fifth metatarsal distal to
the tuberosity: the Jones fracture. Foot Ankle Int 1996;17(8):449-457.
RC, Connell DG, Nichols DM. CT evaluation of tarsometatarsal
fracture-dislocation injuries. AJR Am J Roentgenol 1985;144(5):985-990.
LY. Common sports injuries of the foot and ankle seen in children and
adolescents. Orthop Clin North Am 1994;25(1):83-93.
D, Alperson M, Mendes DG, et al. Bone scintigraphy findings in Lisfranc
joint injury. Foot Ankle Int 1995;16(11):710-711.
RA, Sullivan CR, Kelly PJ, et al. The extraosseous and intraosseous
blood supply of the talus. J Bone Joint Surg Am 1958;40-A(5):1115-1120.
PH, Reschauer R, Kutshca-Lissberg E, et al. Injuries to the
tarsometatarsal joint. Incidence, classification, and treatment. J Bone
Joint Surg Br 1982;64(3): 349-356.
RC. Posttraumatic necrosis of the talus: the Hawkins sign versus
magnetic resonance imaging. J Orthop Trauma 1991;5(1):96-99.
JA, Scherb M, Duffy MF, et al. Fractures of the fifth metatarsal in
children and adolescents. J Pediatr Orthop 2007;27(4):427-431.
J, Laguna R, Peral M, et al. Osteochondritis dissecans of the talus
during childhood and adolescence. J Pediatr Orthop 1998;18(3):328-332.
CB, Benson MK. The ossific nuclei and the cartilage anlage of the talus
and calcaneum. J Bone Joint Surg Br 1992;74(4):620-623.
JL, Buckley R, McCormack R, et al. Complications following management
of displaced intra-articular calcaneal fractures: a prospective
randomized trial comparing open reduction internal fixation with
nonoperative management. J Orthop Trauma 2003;17(4):241-249.
AM, Meyer JS, Davidson RS, et al. Relationship between the ossification
center and cartilaginous anlage in the normal hindfoot in children:
study with MR imaging. AJR Am J Roentgenol 1993;161(4):849-853.
RF, McCarthy RE, Elser JM. Pseudomonas osteochondritis complicating
puncture wounds of the foot in children: a 10-year evaluation. J Infect
Dis 1989;160(4): 657-661.
I, Wester JU, Rasmussen F, et al. Prognosis of fracture of the talus in
children. 21 (7- to 34-)-year follow-up of 14 cases. Acta Orthop Scand
1994;65(4):398-400.
K, Daines M, Howey T, et al. Objective criteria accurately predict
amputation following lower extremity trauma. J Trauma
1990;30(5):568-572; discussion 572-573.
PO, Karlsson M, Redlund-Johnell I, et al. Closed treatment of Jones
fracture. Good results in 40 cases after 11-26 years. Acta Orthop Scand
1994;65(5):545-547.
PO, Karlsson M, Redlund-Johnell I, et al. Jones fracture. Surgical
versus nonsurgical treatment. Clin Orthop Relat Res 1994;299:252-255.
J, Bosse M, Obremskey W. Timing of surgical fixation of talar neck
fractures. Paper 2745. Presented at: Orthopedic Trauma Association
Annual General Meeting. Salt Lake City, Utah; October 9-11, 2003.
KM, Fuller PJ, Brukner PD, et al. Outcome of conservative and surgical
management of navicular stress fracture in athletes. Eighty-six cases
proven with computerized tomography. Am J Sports Med 1992;20(6):657-666.
T, Takakura Y, Higashiyama I, et al. Arthroscopic drilling for the
treatment of osteochondral lesions of the talus. J Bone Joint Surg Am
1999;81(9):1229-1235.
TJ, Armstrong DG, Caporusso J, et al. Soft tissue and bone infections
from puncture wounds in children. West J Med 1997;166(2):126-128.
LP, van der Werken C. Fracture-dislocations of the tarsometatarsal
joint, a combined anatomical and computed tomographic study. Injury
1992;23(1):51-55.
RC, Torg JS, Pavlov H, et al. Fractures of the base of the fifth
metatarsal distal to the tuberosity: a review. Foot Ankle
1987;7(4):245-252.
ED, Simanovsky N, Abu-Sneinah K, et al. Fractures of the lateral
process of the talus in children. J Pediatr Orthop B 2001;10(1):68-72.
LS, Nunley JA. The management of soft-tissue problems associated with
calcaneal fractures. Clin Orthop Relat Res 1993;290:151-156.
CH, Mardini S, Wei FC, et al. Free flap reconstruction of foot and
ankle defects in pediatric patients: long-term outcome in 91 cases.
Plast Reconstr Surg 2006;117(7): 2478-2487.
E, Haidukewych G, DiPasquale T, et al. Open reduction and stable
fixation of isolated, displaced talar neck and body fractures. J Bone
Joint Surg Am 2004;86-A(10):2229-2234.
RT. Demographics of traumatic amputations in children. Implications for
prevention strategies. J Bone Joint Surg Am 2004;86-A(5):923-928.
J, Ebraheim NA, Skie M, et al. Radiographic and computed tomographic
evaluation of Lisfranc dislocation: a cadaver study. Foot Ankle Int
1997;18(6):351-355.
NM. Role of MRI in prevention of metatarsal stress fractures in
collegiate basketball players. AJR Am J Roentgenol 2006;186(1):255-258.
RE, Frymoyer JW. Fracture of the calcaneus in young children. Report of
three cases. J Bone Joint Surg Am 1973;55(5):1091-1094.
C, Rigault P, Padovani JP, et al. [Fractures of the talus in children.
Apropos of 23 cases]. Rev Chir Orthop Reparatrice Appar Mot
1986;72(3):183-195.
P, Bladin C. Fractures of the lateral process of the talus: a clinical
review. “Snowboarder’s ankle.” Clin J Sport Med 1996;6(2):124-128.
JF 3rd, Argenta LC, Marks MW, et al. Treatment of soft tissue defects
in pediatric patients using the V.A.C. system. Clin Orthop Relat Res
2000;376:26-31.
MS. Experimental decompression of the fascial compartments of the
foot—the basis for fasciotomy in acute compartment syndromes. Foot
Ankle 1988;8(6):308-314.
MS, Fisher RT, Burgess AR, et al. Fracture dislocations of the
tarsometatarsal joints: end results correlated with pathology and
treatment. Foot Ankle 1986;6(5): 225-242.
R, Hadley J, Paul C, et al. “Snowboarder’s fracture”: fracture of the
lateral process of the talus. J Am Board Fam Pract 1994;7(2):130-133.
J, Royle SG. Fracture of the lateral process of the talus: computed
tomographic scan diagnosis. Br J Sports Med 1992;26(4):245-246.
L, Goldie IF. The arterial supply of the talus. A study on the
relationship to experimental talar fractures. Acta Orthop Scand
1975;46(6):1026-1034.
A, Benaroch TE, Guy P, et al. Clinical outcome of pediatric calcaneal
fractures treated with open reduction and internal fixation. J Pediatr
Orthop 2004;24(2): 178-180.
D, Hallivis R, Dollard MD. Sports injuries in the pediatric and
adolescent foot and ankle: common overuse and acute presentations. Clin
Podiatr Med Surg 2006; 23(1):209-231, x.
HG, Deland JT, Gusmar PB, et al. Magnetic resonance imaging of the
Lisfranc ligament of the foot. Foot Ankle Int 1998;19(7):438-446.
M, Horoshovski H, Farine I. Arthroscopic treatment of osteochondral
lesions of the talus. J Bone Joint Surg Am 1986;68(6):862-865.
E, Küss G. Étude sur les luxations du metataese (luxations
métatarsotariennes) du diastasis entre le 1er et la 2e metatarsien. Rev
Chir Orthop Reparatrice Appar Mot 1909;39:281-336.
S, Zwipp H, Gavlik JM. Avascular necrosis after minimally displaced
talus fracture in a child. Foot Ankle Int 2000;21(12):1030-1036.
F, Schantz K. Radiologic aspects of calcaneal fractures in childhood
and adolescence. Acta Radiol Diagn (Stockh) 1986;27(5):575-580.
WR, Rosenthal DI. Avulsion fracture of the fifth metatarsal:
experimental study of pathomechanics. AJR Am J Roentgenol
1984;143(4):889-891.
G, Cronin R, Hauzenblas J, et al. Plantar ecchymosis sign: a clinical
aid to diagnosis of occult Lisfranc tarsometatarsal injuries. J Orthop
Trauma 1996;10(2):119-122.
R. Fractures and fracture-dislocations of the calcaneus. In: Coughlin
M, Mann R, eds. Surgery of the Foot and Ankle. 7th ed. St. Louis:
Mosby, 1999.
R, Fortin P, DiPasquale T, et al. Operative treatment in 120 displaced
intra-articular calcaneal fractures. Results using a prognostic
computed tomography scan. Clin Orthop Relat Res 1993;290:87-95.
RC Jr, Heckman JD. Fractures and dislocations of the forefoot:
operative and nonoperative treatment. J Am Acad Orthop Surg
1995;3(2):70-78.
TL, Weiner DS. Calcaneal fractures in children. An evaluation of the
nature of the injury in 56 children. Clin Orthop Relat Res
1982;171:150-155.
C, Coin C. Effect of weight-bearing on the appearance and development
of the secondary calcaneal epiphysis. Radiology 1968;86:201-206.
JS, Yoder JS, Manuck TA, et al. Role of vacuum-assisted closure in the
treatment of pediatric lawnmower injuries. J Pediatr Orthop
2004;24(5):482-487.
TV, Bray TJ, Holmes GB Jr. Fractures of the talar neck. A mechanical
study of fixation. J Bone Joint Surg Am 1992;74(4):544-551.
B, Scola E, Zwipp H. [Surgical treatment and late results of foot
compartment syndrome]. Unfallchirurg 1991;94(5):262-266.
WS, Bisignani GA, Towers JD, et al. Retrograde drilling of
osteochondral lesions of the medial talar dome. Foot Ankle Int
1999;20(8):474-480.
DB, Triffon MJ, Terk MR. Magnetic resonance imaging to detect avascular
necrosis after open reduction and internal fixation of talar neck
fractures. Foot Ankle Int 1996;17(12):742-747.
JS, Balduini FC, Zelko RR, et al. Fractures of the base of the fifth
metatarsal distal to the tuberosity. Classification and guidelines for
nonsurgical and surgical management. J Bone Joint Surg Am
1984;66(2):209-214.
DJ, Feder JM, Boylan JP. Fractures of the lateral process of the talus:
two case reports and a comprehensive literature review. Foot Ankle Int
1998;19(9):641-646.
R, Staheli LT, Chew DE, et al. Measurements on radiographs of the foot
in normal infants and children. J Bone Joint Surg Am 1988;70(3):407-415.
D, Smith GA. Epidemiology of lawnmower-related injuries to children in
the United States, 1990-2004. Pediatrics 2006;118(2):e273-278.
CL, Gruel CR, Herndon WA, et al. Lawnmower injuries of the pediatric
foot and ankle: observations on prevention and management. J Pediatr
Orthop 1995;15(4): 504-509.
M, Locher S. Reconstruction of the cuboid in compression fractures:
short to midterm results in 12 patients. Foot Ankle Int
2002;23(11):1008-1013.
RT, Berde CB, Wolohan M, et al. Reflex sympathetic dystrophy in
children. Clinical characteristics and follow-up of 70 patients. J Bone
Joint Surg Am 1992;74(6): 910-919.
DW. Injuries of the tarsometatarsal joints. Etiology, classification,
and results of treatment. J Bone Joint Surg Br 1972;54(4):677-686.
DA, Kull DM, Perry J. Lisfranc fracture-dislocations of the foot: a
clinical-kinesiological study. J Orthop Trauma 1987;1(4):267-274.
D. Stress fractures in the pediatric athlete. In: Sullivan J, Grana W,
eds. The Pediatric Athlete. Park Ridge, IL: American Academy of
Orthopaedic Surgeons, 1990: 235-240.
