Fractures of the Distal Radius and Ulna
These fractures have been reported to be three times more common in
boys; however, the increased participation in athletics by girls at a
young age may be changing this ratio. Although these fractures occur at
any age, they are most frequent during the adolescent growth spurt.10,103
The fractures are described by location, metaphyseal or physeal, and by
severity of displacement. The pediatric Galeazzi injury usually
involves a distal radial metaphyseal fracture and a distal ulnar
physeal fracture that result in a displaced distal radioulnar joint.
These injuries are rare, but need to be identified acutely for proper
management. The specifics of fracture patterns for individual fracture
types are discussed in separate sections of this chapter. Most of these
injuries have traditionally been treated with closed reduction and cast
immobilization. Indications for percutaneous pinning and open reduction
in pediatric patients are evolving and are discussed in each section.
sufficient. Usually, this is secondary to a sporting event.
Snowboarding, skateboarding, soccer goal-keeping, and horseback riding
have been shown to be high-risk sports,19,114,116,138,187,196,197,231
but a severe enough fall in any recreational activity can lead to a
fracture. There is seasonal variation, with an increase in both
incidence and severity of fractures in summer.234
Children who are overweight have poor postural balance, ligamentous
laxity, or less bone mineralization, and are at increased risk for
distal radial fractures.58,82,83,84,131,155,176,204
The fractures generally occur with an extension deformity because of
the mechanism of a fall on an outstretched hand. Occasionally, a direct
blow or a fall onto a flexed wrist and hand causes volar displacement
or angulation of the distal fragment. In either case, there may be a
rotational component to the fracture pattern. Repetitive loading of the
wrist can lead to physeal stress injuries of the distal radius and,
less commonly, the ulna. These injuries are rare and occur most
frequently in gymnasts.5,23,43,51,141,191,223
Any patient with chronic physeal region wrist pain who participates in
an activity with repetitive axial loading of the wrist, such as
gymnastics or break dancing,79 should be examined for a stress injury.
the distal forearm, tenderness directly over the fracture site, and
limited motion of the forearm, wrist, and hand. Deformity depends on
the degree of fracture displacement. Fractures with marked extension
displacement can lead to a silver fork deformity similar to an adult
Colles fracture. Standard anteroposterior (AP) and lateral radiographs
are diagnostic of fracture type and displacement. Metaphyseal fractures
are most common, followed by physeal fractures74,146,222;
the distal fragment in either usually is extended. Neurovascular
examination should be performed before treatment to assess for median
or ulnar neuropathy or the rare compartment syndrome. Hand and elbow
regions need to be examined clinically and, if appropriate,
radiographically for associated injuries.
rare but need to be assessed because their presence implies more severe
trauma. The risk of a compartment syndrome is higher with a “floating
elbow” combination of radial, ulnar, and elbow fractures.185
With marked radial or ulnar fracture displacement, neurovascular
compromise can occur. Median neuropathy results from contusion at the
time of fracture displacement, persistent direct pressure from an
unreduced fracture, or an acute compartment syndrome.239
Ulnar neuropathy has been described with similar mechanisms as well as
entrapment. Wrist ligamentous and articular cartilage injuries have
been described in association with distal radial and ulnar fractures in
adults and less commonly in children.49,221 Concomitant scaphoid fractures have occurred.206
Associated wrist injuries need to be treated both in the acute setting
and in the patient with persistent pain after fracture healing. Some
patients with distal radial and ulnar fractures are multitrauma
victims. Their systemic care modifies their distal forearm fracture
care.
anatomic relationship to the physis. Transphyseal injuries are
classified by the widely accepted Salter-Harris system.194
Metaphyseal injuries may be torus or buckle fractures, greenstick or
incomplete fractures, or complete injuries. Pediatric equivalents of
adult Galeazzi fracture-dislocations involve a distal radial fracture
and either a soft tissue disruption of the distal radioulnar joint
(DRUJ) or a transphyseal fracture of the ulna (Table 9-1).
In contrast to adults, skeletally immature patients rarely sustain
intra-articular fractures of the distal radius. On occasion, a
Salter-Harris type III fracture, a triplane fracture,20 or an adolescent intra-articular Colles fracture occurs.
|
TABLE 9-1 Distal Forearm Fractures: General Classification
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||
than in children. At present, an unstable fracture in a child is often
defined as one in which closed reduction cannot be maintained.
Pediatric classification systems have yet to more precisely define
fracture stability, but this issue is critical in determining proper
treatment management. Distal radial metaphyseal fractures have been
shown to have a high degree of recurrent displacement and, therefore,
inherent instability.6,80,136,177,238,248,254
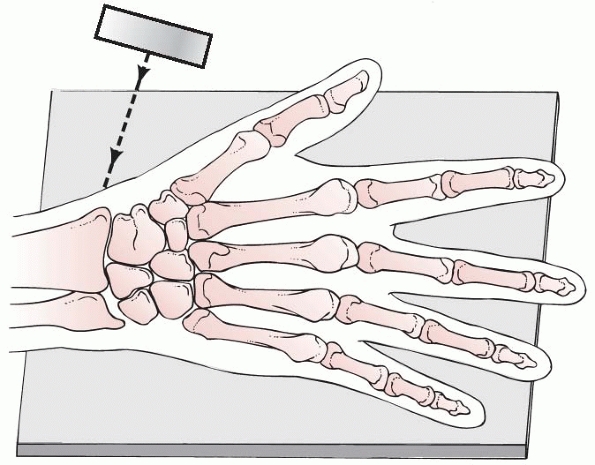
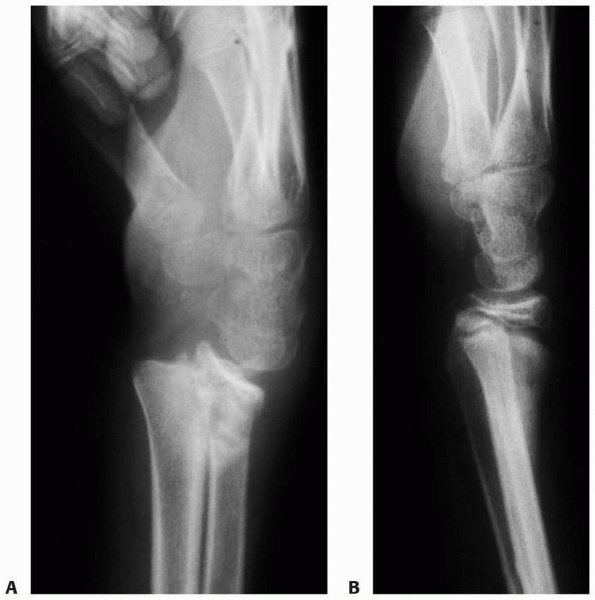
and angulation. Static AP and lateral radiographs can be diagnostic of
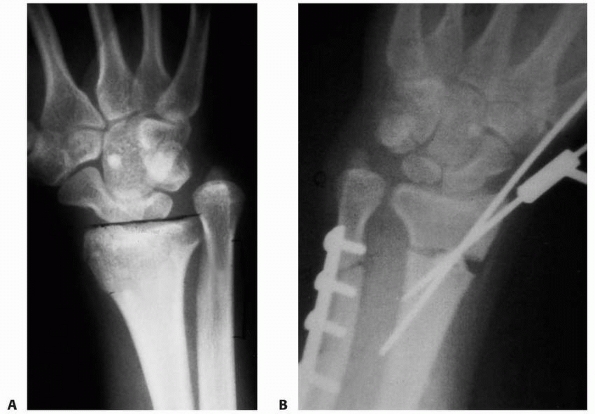
the fracture type and degree of deformity (Fig. 9-1). In adults,
the distal radial articular alignment averages 22 degrees on the AP view and 11 degrees on the lateral view.98,145,150,203,228
Radial inclination is a goniometric measurement of the angle between
the distal radial articular surface and a line perpendicular to the
radial shaft on the AP radiograph. Palmar tilt is measured by a line
across the distal articular surface and a line perpendicular to the
radial shaft on the lateral view. Pediatric values for radial
inclination tend to be less, depending on the degree of skeletal
maturity of the patient. Palmar tilt tends to be more consistent
regardless of the age of the patient.
 |
|
FIGURE 9-1
Angulation of the x-ray beam tangential to the articular surface, providing the optimal lateral view of the distal radius. The wrist is positioned as for the standard lateral radiograph, but the x-ray beam is directed 15 degrees cephalad. (Redrawn from Johnson PG, Szabo RM. Angle measurements of the distal radius: a cadaver study. Skel Radiol 1993;22:243, with permission.) |
intra-articular involvement or displacement. This can be by AP and
lateral tomograms, computerized tomographic (CT) scans, or magnetic
resonance imaging (MRI). Dynamic motion studies with fluoroscopy can
provide important information on fracture stability and the success of
various treatment options. Dynamic fluoroscopy requires adequate pain
relief and has been used more often in adult patients with distal
radial fractures. Ultrasound has been used to diagnose fractures in
some centers.52,97
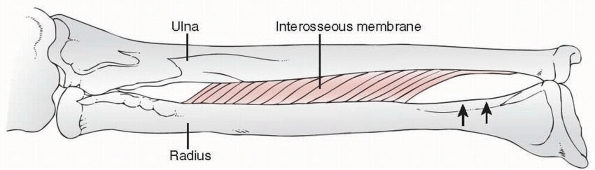
Initially transverse in appearance, it rapidly becomes more adultlike
with its triangular shape. The contour of the radial styloid
progressively elongates with advancing skeletal maturity. The secondary
center of ossification for the distal ulna appears at about age 7.
Similar to the radius, the ulnar styloid appears with the adolescent
growth spurt. It also becomes more elongated and adultlike until
physeal closure. On average, the ulnar physis closes at age 16 in girls
and age 17 in boys, whereas the radial physis closes on average 6
months later than the ulnar physis.86,145
The distal radial and ulnar physes contribute approximately 75% to 80%
of the growth of the forearm and 40% of the growth of the upper
extremity (Fig. 9-2).158
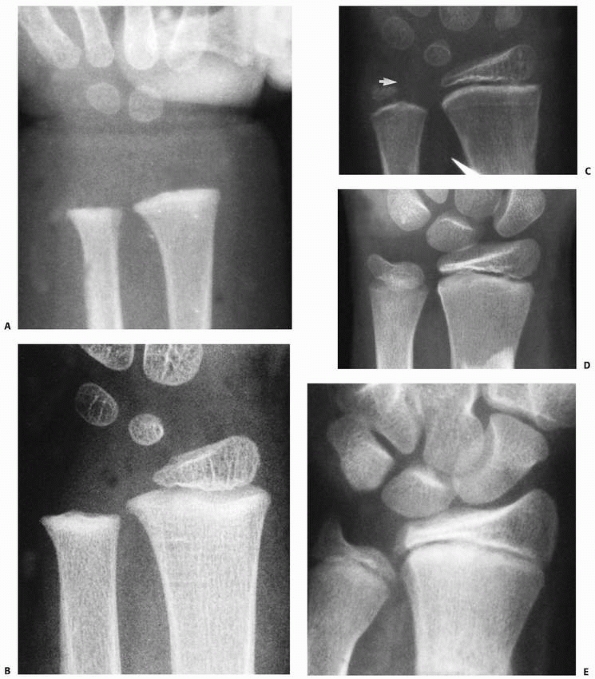
the DRUJ. Both the radius and ulna articulate with the carpus, serving
as the support for the hand. The radial joint surface has three
concavities for its articulations: the scaphoid and lunate fossa for
the carpus and the sigmoid notch for the ulnar head (Fig. 9-3).
These joints are stabilized by a complex series of volar and dorsal
radiocarpal, ulnocarpal, and radioulnar ligaments. The volar ligaments
are the major stabilizers. Starting radially at the radial styloid, the
radial collateral, radioscaphocapitate, radiolunotriquetral (long
radiolunate), and radioscapholunate (short radiolunate) ligaments
volarly stabilize the radiocarpal joint. The dorsal radioscaphoid and
radial triquetral ligaments are less important stabilizers.
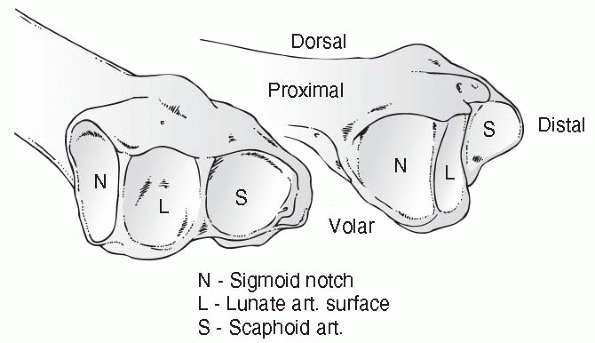
primary stabilizer of the ulnocarpal and radioulnar articulations. It
extends from the sigmoid notch of the radius across the DRUJ and
inserts into the base of the ulnar styloid. It also extends distally as
the ulnolunate, ulnotriquetral, and ulnar collateral ligaments and
inserts into the ulnar carpus and base of the fifth metacarpal.60 The interosseous ligament of the forearm (Fig. 9-4)
helps stabilize the radius and ulna more proximally in the diaphysis of
the forearm. The ulna remains relatively immobile as the radius rotates
around it. The complex structure of ligaments stabilize the radius,
ulna, and carpus through the normal wrist motion of 120 degrees of
flexion and extension, 50 degrees of radial and ulnar deviation, and
150 degrees of forearm rotation.60
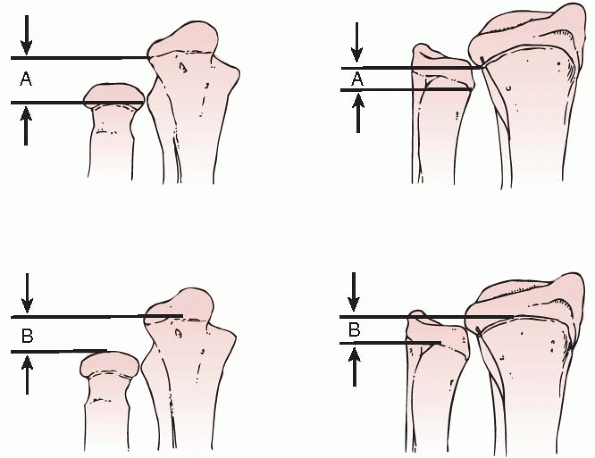
ulna is defined as ulnar variance. In adults, this is measured by the
relationship of the radial corner of the distal ulnar articular surface
to the ulnar corner of the radial articular surface.99 However, measurement of ulnar variance in children requires modifications of this technique. Hafner90
described measuring from the ulnar metaphysis to the radial metaphysis
to lessen the measurement inaccuracies related to epiphyseal size and
shape (Fig. 9-5). If the ulna and radius are of
equal lengths, there is a neutral variance. If the ulna is longer,
there is a positive variance. If the ulna is shorter, there is a
negative variance. Variance measurement is usually made in millimeters.
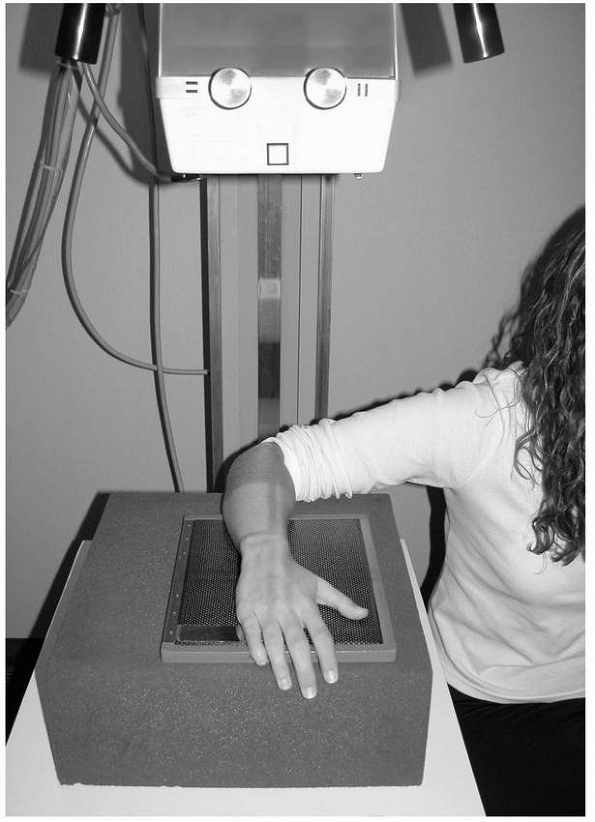
Radiographs of the wrist to determine ulnar variance should be
standardized with the hand and wrist pronated on the cassette, the
elbow flexed 90 degrees, and the shoulder abducted 90 degrees (Fig. 9-6).
The importance of ulnar variance relates to the force transmission
across the wrist with axial loading. Normally, the radiocarpal joint
bears approximately 80% of the axial load and the ulnocarpal joint
bears 20%. Changes in the length relationship of the radius and ulna
alter respective load bearing. Biomechanical and clinical studies have
shown that this load distribution is important in fractures, TFCC tears
(positive ulnar variance), and Kienböck disease (negative ulnar
variance).51,78,162
concluded from his observations at the Boston City Hospital outpatient
clinic that permanent deformity was rare. Instead, he emphasized the
remodeling potential of distal radial physeal fractures, even when not
reduced. The observations of Aitken have been confirmed throughout the
twentieth century (Fig. 9-7). Most researchers
agree that as long as there is sufficient growth remaining, a distal
radial extension deformity from a fracture malunited in extension has
the potential to remodel. Permanent deformity, however, can occur in
malunited fractures near the end of growth, with rotational deformity,
or fractures that cause distal radial growth arrest.
More than 50% of distal radial physeal fractures have an associated
ulnar fracture. This usually is an ulnar styloid fracture but can be a
distal ulnar plastic deformation, greenstick, or complete fracture.8,124,125
The mechanism of injury generally is a fall on an outstretched hand and
wrist. Many of the injuries are nondisplaced and present only with pain
at the physis.151,166
With displaced fractures, the distal fragment usually moves dorsally,
creating an extension deformity that is usually clinically apparent.
Patients
have pain and tenderness at the fracture site, and the range of motion
at the wrist and hand usually is limited by pain. Neurovascular
compromise is uncommon but can occur.239
When present, it usually consists of median nerve irritability or
dysfunction caused by direct trauma to the nerve at the time of injury
or ongoing ischemic compression from the displaced fracture. Thenar
muscle function and discriminatory sensibility (two-point
discrimination) should be tested before reduction in the emergency
setting. Acute carpal tunnel syndrome or forearm compartment syndrome
can occur, but more often is caused by marked volar forearm and wrist
swelling that occurs after reduction and application of a well-molded,
tight cast.34,195,239 Open physeal fractures are rare, but the local skin should be examined closely for penetration.
 |
|
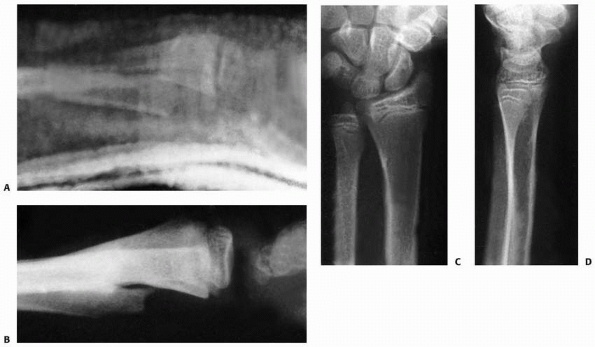
FIGURE 9-2 Ossification of the distal radius. A. Preossification distal radius with transverse ossification in a 15-month-old boy. B. The triangular secondary ossification center of the distal radius in a 2-year-old girl. C. The initial ossification center of the styloid in this 7-year-old girl progresses radially (arrow). D. Extension of the ulnar ossification center into the styloid process of an 11-year-old. E. The styloid is fully ossified and the epiphyses have capped their relative metaphyses in this 13-year-old boy.
|
 |
|
FIGURE 9-3
Articulations of the distal radioulnar joint. (Redrawn from Bowers WH. Green’s Operative Hand Surgery. New York: Churchill-Livingstone, 1993:988.) |
fracture type and deformity. The Salter-Harris system is the basis for
classification of physeal fractures.194
Most are Salter-Harris type II fractures. The dorsal displacement of
the distal fragment of the epiphysis and dorsal Thurston-Holland
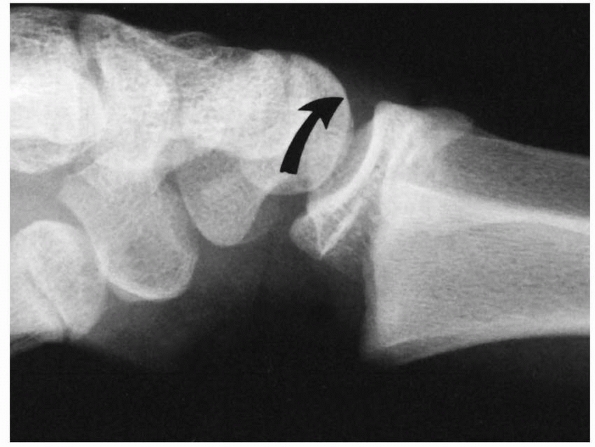
metaphyseal fragment is evident on the lateral view (Fig. 9-8).
Salter-Harris type I fractures also usually displace dorsally. Volar
displacement of either a Salter-Harris type I or II fracture is less
common (Fig. 9-9). Nondisplaced Salter-Harris type I fractures may be indicated only by a displaced pronator fat pad sign (Fig. 9-10)198,253 or tenderness over the involved physis.8,181 A scaphoid fat pad sign may indicate a scaphoid fracture (Fig. 9-11). If the acute fracture is unrecognized, a late-appearing periosteal reaction may indicate the fracture.
caused by a compression injury or an avulsion of the radial origin of
the volar radiocarpal ligaments (Fig. 9-12).7,124 Triplane equivalent fractures,169,170,171
a combination of Salter-Harris type II and III fractures in different
planes, are rare. CT scans may be necessary to define the fracture
pattern and degree of intra-articular displacement. Stress injuries to
the physis occur most commonly in competitive gymnasts (Fig. 9-13).
 |
|
FIGURE 9-4
The attachment and the fibers of the interosseous membrane are such that there is no attachment to the distal radius. (Redrawn from Kraus B, Horne G. Galeazzi fractures. J Trauma 1985;25:1094, with permission.) |
 |
|
FIGURE 9-5 Hafner’s technique to measure ulnar variance. A. The distance from the most proximal point of the ulnar metaphysis to the most proximal point of the radial metaphysis. B.
The distance from the most distal point of the ulnar metaphysis to the most distal point of the radial metaphysis. (From Hafner R, Poznanski AK, Donovan JM. Ulnar variance in children. Standard measurements for evaluation of ulnar shortening in childhood. Skel Radiol 1989;18:514, with permission.) |
and cast immobilization, closed reduction and pin fixation, and open
reduction. Nondisplaced fractures are immobilized until appropriate
healing and pain resolution have been achieved.8,191
If there is a question of fracture stability, these fractures should be
treated with a well-molded cast and monitored closely during the first
3 weeks of healing to be certain that there is no loss of alignment.
Most acute displaced Salter-Harris type I and II fractures can be
treated successfully with gentle closed reduction and cast
immobilization. There are advocates for both long-arm and short-arm
treatment methods.28,29,31,89,95,121,212
Closed reduction and percutaneous pin fixation are performed in
patients with neurovascular compromise and displaced physeal fractures239
to lessen the risk of development of a compartment syndrome in the
carpal tunnel or forearm. Open reduction is indicated for irreducible
fractures,
open
fractures, displaced Salter-Harris type III and IV fractures, and
triplane equivalent fractures. Irreducible fractures usually are due to
an entrapped periosteum or pronator quadratus.137
Internal fixation usually is with smooth, small-diameter pins to lessen
the risk of growth arrest. Plates and screws rarely are used unless the
patient is near skeletal maturity because of concerns about further
physeal injury. In the rare displaced intra-articular Salter-Harris
type III or IV fracture, internal fixation can be intraepiphyseal
without violating the physis. If it is necessary to cross the physis,
then smooth, small diameter pins should be used to lessen the risk of
iatrogenic physeal injury. Extra-articular external fixation also can
be used to stabilize and align the fracture.
 |
|
FIGURE 9-6
Technique for neutral rotation radiograph with wrist neutral, forearm pronated, elbow flexed 90 degrees, and shoulder abducted 90 degrees. |
 |
|
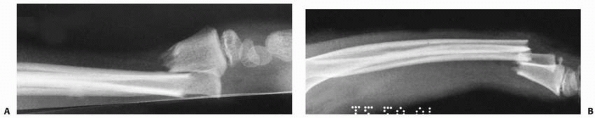
FIGURE 9-7 A.
A 13-year-old boy presented 1 month after injury with a displaced and healed Salter-Harris type II distal radial fracture with obvious clinical deformity. B. Over the next 6 months, the patient grew 4 inches and the deformity remodeled without intervention. |
 |
|
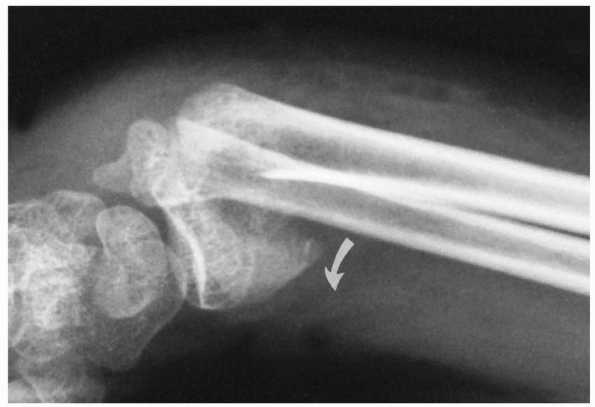
FIGURE 9-8 Dorsally displaced physeal fracture (type A). The distal epiphysis with a small metaphyseal fragment is displaced dorsally (curved arrow) in relation to the proximal metaphyseal fragment.
|
treated with closed reduction and cast stabilization. Closed
manipulation of the displaced fracture is performed with appropriate
conscious
sedation, analgesia, or, rarely, anesthesia to achieve pain relief and an atraumatic reduction.8,108,191
Most of these fractures involve dorsal and proximal displacement of the
epiphysis with an apex-volar extension deformity. Manipulative
reduction is by gentle distraction and flexion of the distal epiphysis,
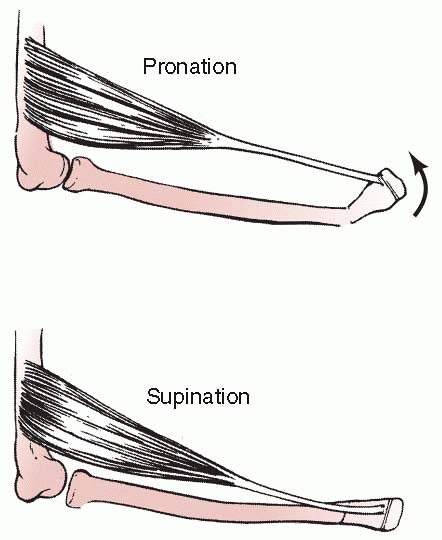
carpus, and hand over the proximal metaphysis (Figs. 9-14 and 9-15).
The intact dorsal periosteum is used as a tension band to aid in
reduction and stabilization of the fracture. Unlike similar fractures
in adults, finger trap distraction with pulley weights is often
counterproductive. However, finger traps can help stabilize the hand,
wrist, and arm for manipulative reduction and casting by applying a few
pounds of weight for balance. Otherwise, an assistant is helpful to
support the extremity in the proper position for casting.
 |
|
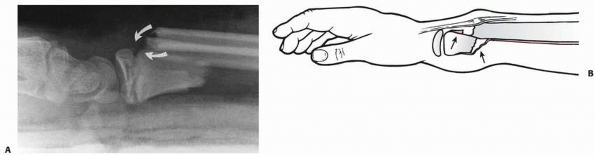
FIGURE 9-9
Volarly displaced physeal fracture (type B). Distal epiphysis with a large volar metaphyseal fragment is displaced in a volar direction (curved arrow). (Reprinted from Wilkins KE, ed. Operative Management of Upper Extremity Fractures in Children. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1994:21, with permission.) |
 |
|
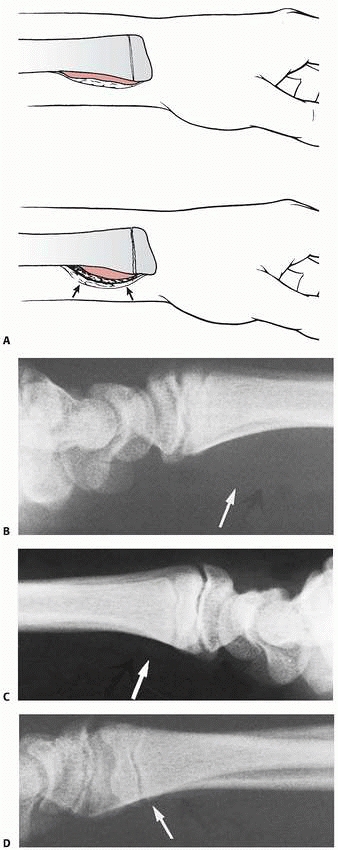
FIGURE 9-10 A.
Subperiosteal hemorrhage from an occult fracture of the distal radius causes an anterior displacement of the normal pronator quadratus fat pad (arrows). B. A 13-year-old girl with tenderness over the distal radius after a fall. The only radiographic finding is an anterior displacement of the normal pronator quadratus fat pad (arrow). C. The opposite normal side (arrow indicates normal fat pad). D. Two weeks later, there is a small area of periosteal new bone formation (arrow) anteriorly, substantiating that bony injury has occurred. |
 |
|
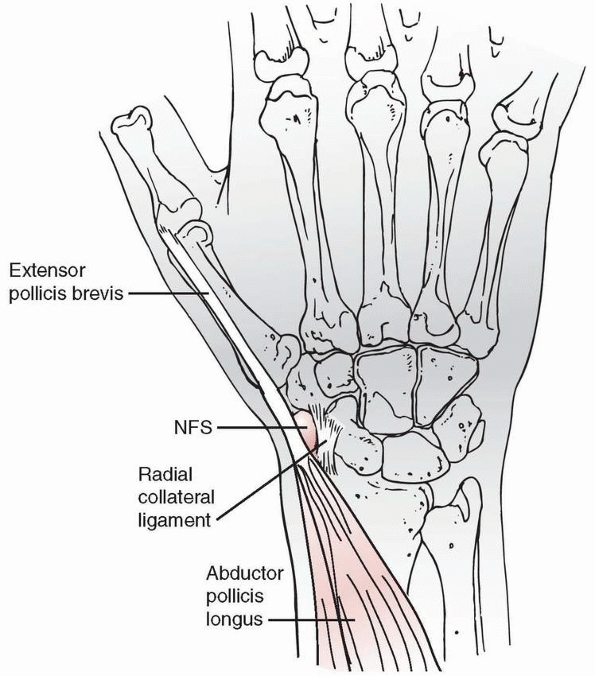
FIGURE 9-11
Anatomic relationships of the navicular fat stripe (NFS). The NFS, shaded black, is located between the combined tendons of the abductor pollicis longus and extensor pollicis brevis, and the lateral surface of the carpal navicular. (Reprinted from Terry DW, Ramen JE. The navicular fat stripe. Ham J Roent Rad Ther Nucl Med 1975;124: 25, with permission.) |
 |
|
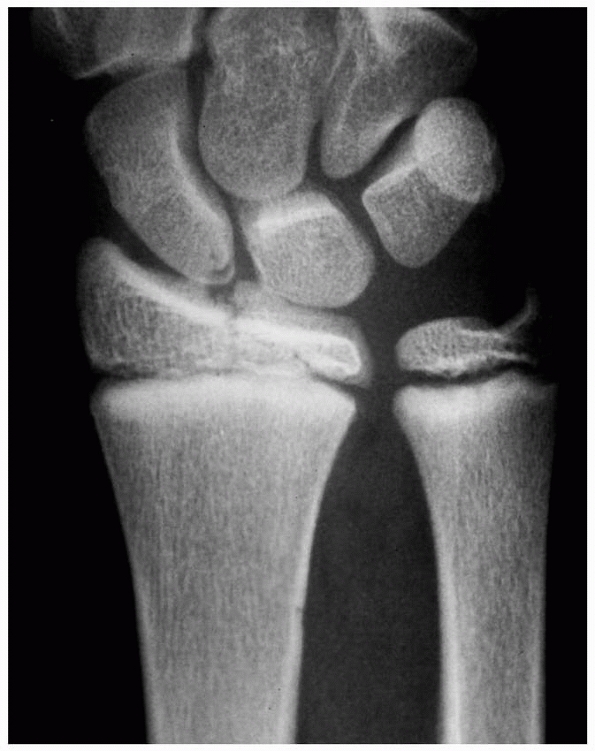
FIGURE 9-12 AP radiograph of Salter-Harris type III fracture of the distal radius.
|
 |
|
FIGURE 9-13 Stress changes in a female gymnast with widening of the distal radial physis from long-standing high-level performance.
|
 |
|
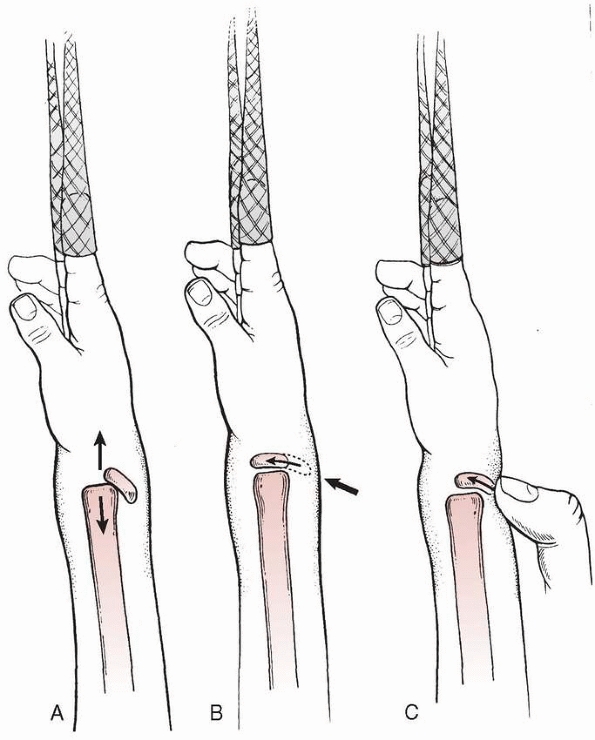
FIGURE 9-14 Acceptable method of closed reduction of distal physeal fractures of the radius. A. Position of the fracture fragments as finger trap traction with countertraction is applied (arrows). B. With traction alone, the fracture will often reduce without external pressure (arrows). C.
If the reduction is incomplete, simply applying direct pressure over the fracture site in a distal and volar direction with the thumb often completes the reduction while maintaining traction. This technique theoretically decreases the shear forces across the physis during the reduction process. |
 |
|
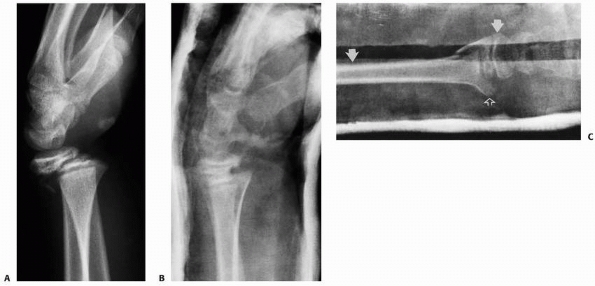
FIGURE 9-15 A. Lateral radiograph of dorsally displaced Salter-Harris type II fracture. B. Lateral radiograph after closed reduction and cast application. C.
Reduction of the volar displaced fracture shown in Figure 9-9. The forearm was in supination with three-point molding anterior over the distal epiphysis and proximal shaft (white arrows). The third point is placed dorsally over the distal metaphysis (open arrow). (The dorsal surface of the cast is oriented toward the bottom of this figure.) (Reprinted from Wilkins KE, ed. Operative Management of Upper Extremity Fractures in Children. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1994:17, with permission.) |
radiographic assessment of the reduction is obtained. Otherwise, a
well-molded cast is applied and AP and lateral radiographs are obtained
to assess the reduction. The cast should provide three-point
molding
over the distal radius to lessen the risk of fracture displacement and
should follow the contour of the normal forearm. The distal dorsal mold
should not impair venous outflow from the hand, which can occur if the
mold is placed too distal and too deep so as to obstruct the dorsal
veins. Advocates of short-arm casting28,29
indicate at least equivalent results with proper casting techniques and
more comfort during immobilization due to free elbow mobility.
Instructions for elevation and close monitoring of swelling and the
neurovascular status of the extremity are critical.
serial radiographs for the first 3 weeks to be certain that there is no
loss of anatomic alignment (Fig. 9-16).
Generally, these fractures are stable after closed reduction and cast
immobilization. If there is loss of reduction after 7 days, the surgeon
should be wary of repeat reduction because of the risk of physeal
arrest.8,194
Fortunately, remodeling of an extension deformity with growth is common
if the patient has more than 2 years of growth remaining and the
deformity is less than 20 degrees.
 |
|
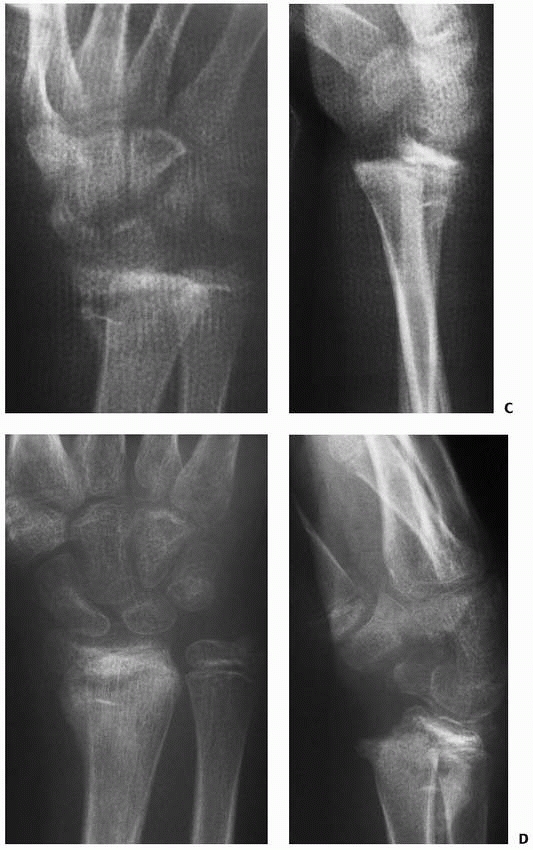
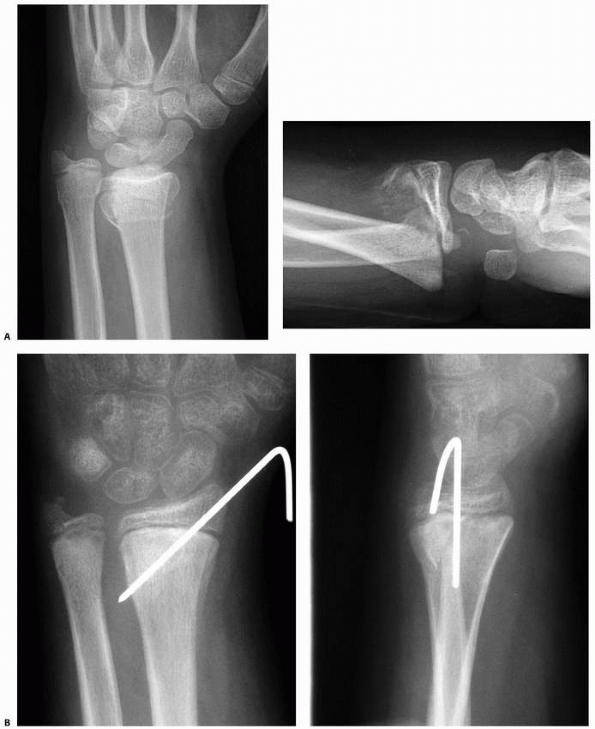
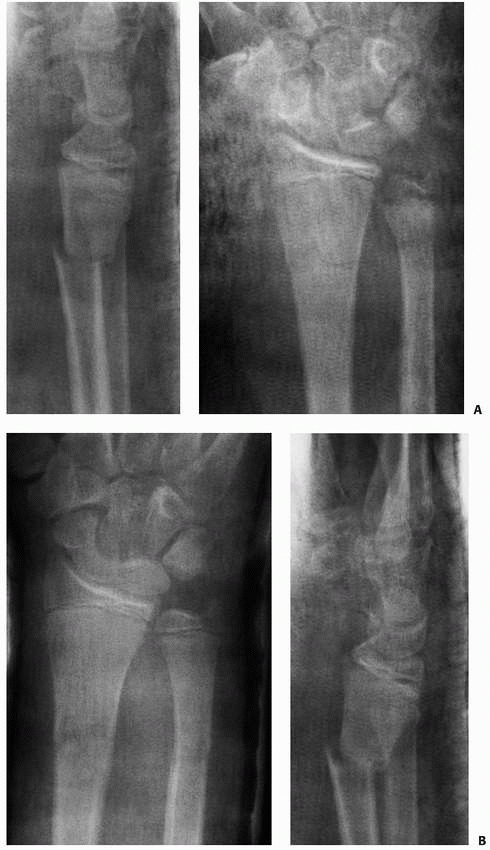
FIGURE 9-16 A. AP and lateral radiographs of severely displaced Salter-Harris type II fracture of the distal radius. B. Closed reduction shows marked improvement but not anatomic reduction. The cast had to be bivalved due to excessive swelling. (continues)
|
radial physeal fractures are still controversial. The best indication
is a displaced radial physeal fracture with median neuropathy and
significant volar soft tissue swelling (Fig. 9-17).239
These patients are at risk for development of an acute carpal tunnel
syndrome or forearm compartment syndrome with closed reduction and
well-molded cast immobilization.34,91,195,239
The torn periosteum volarly allows the fracture bleeding to dissect
into the volar forearm compartments and carpal tunnel. If a tight cast
is applied with a volar mold over that area, compartment pressures can
increase dangerously. Percutaneous pin fixation allows the application
of a loose dressing, splint, or cast without the risk of loss of
fracture reduction.
Fluoroscopy is used to guide proper fracture reduction and pin
placement. Anesthesia is used for adequate pain relief and to lessen
the risk of further physeal injury. The fracture is manipulated into
anatomic alignment and the initial, and often only, pin
is
placed from the distal epiphysis of the radial styloid obliquely across
the physis into the more proximal ulnar aspect of the radial metaphysis
(Fig. 9-19).
Alternatively, smooth pins may be placed such that they avoid crossing
the distal radial physis, theoretically decreasing the risk of physeal
disturbance, though this has not been well demonstrated in the
published literature.252 A
sufficient skin incision should be made with pin placement to be
certain there is no iatrogenic injury to the radial sensory nerve or
extensor tendons. Stability of the fracture should be evaluated with
flexion and extension and rotatory stress under fluoroscopy. Often in
children and adolescents, a single pin and the reduced periosteum
provide sufficient stability to prevent redisplacement of the fracture.
If fracture stability is questionable with a single pin, a second pin
should be placed. The second pin can either parallel the first pin or,
to create cross-pin stability, can be placed distally from the ulnar
corner of the radial epiphysis between the fourth and fifth dorsal
compartments and passed obliquely to the proximal radial portion of the
metaphysis. Again, the skin incisions for pin placement should be
sufficient to avoid iatrogenic injury to the extensor tendons.
 |
|
FIGURE 9-16 (continued) C. Unfortunately, the patient lost reduction after a new fiberglass cast was applied. D. Out-of cast-radiographs show a healed malunion in a similar position to the prereduction radiographs.
|
with a sterile dressing. Splint or cast immobilization is used but does
not need to be tight because fracture stability is provided by the
pins. The pins are left in until there is adequate fracture healing
(usually 4 weeks). The pins can be removed in the office without
sedation or anesthesia.
The risk of physeal arrest is more from the displaced fracture than
from a short-term, smooth pin. As a precaution, smooth, small-diameter
pins should be used, insertion should be as atraumatic as possible, and
removal should be done as soon as there is sufficient fracture healing
for fracture stability in a cast or splint alone.
 |
|
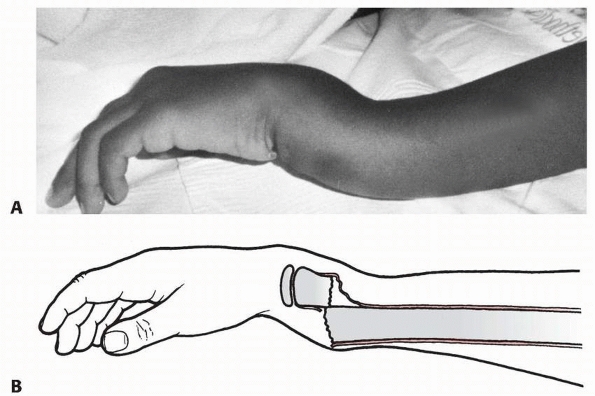
FIGURE 9-17 A.
Clinical photograph of patient with a displaced Salter-Harris type II fracture of the distal radius. The patient has marked swelling volarly with hematoma and fracture displacement. The patient had a median neuropathy upon presentation. B. Lateral radiograph of the displaced fracture. C. Lateral radiograph following closed reduction and cast application. Excessive flexion has been utilized to maintain fracture reduction, resulting in persistent median neuropathy and increasing pain. D. Radiographs following urgent closed reduction and percutaneous pinning. E. Follow-up radiograph depicting distal radial physeal arrest and increased ulnar variance. |
 |
|
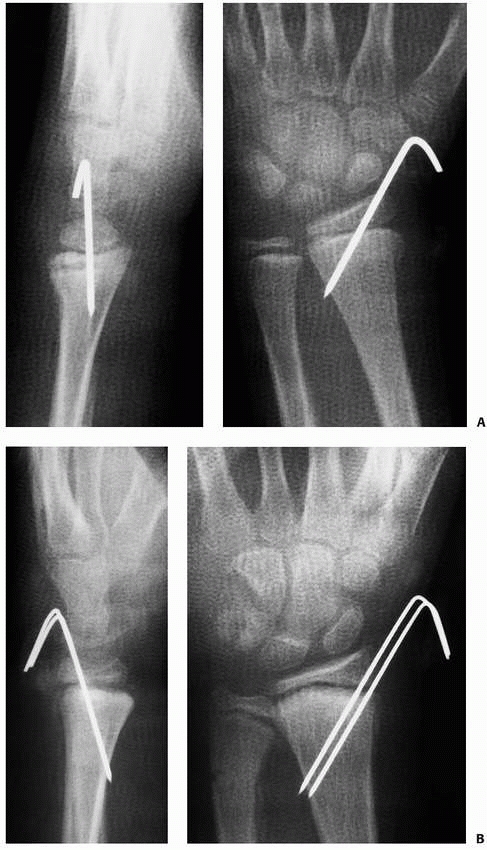
FIGURE 9-18 A. AP and lateral radiographs of displaced Salter-Harris type II fracture pinned with a single pin. B. After reduction and pinning with parallel pins.
|
distal radial Salter-Harris type II physeal fracture is irreducibility.
Most often this is caused by interposed periosteum or, less likely,
pronator quadratus.107,137,250
Open reduction is done through a volar approach to the distal radial
physis. The interval between the radial artery and the flexor carpi
radialis is used. This dissection also can proceed directly through the
flexor carpi radialis sheath to protect the artery. The pronator
quadratus is isolated and elevated from radial to ulnar. Although this
muscle can be interposed in the fracture site, the volar periosteum is
more commonly interposed. This is evident only after elevation of the
pronator quadratus. The periosteum is extracted from the physis with
care to minimize further injury to the physis. The fracture can then be
easily reduced. Usually, a percutaneous smooth pin is used for
stabilization of the reduction. The method of pin insertion is the same
as after closed reduction.
and débridement. Care should be taken with mechanical débridement of
the physeal cartilage to avoid further risk of growth arrest. Cultures
should be taken at the time of operative débridement, and appropriate
antibiotics are used to lessen the risk of deep space infection.
may require open reduction if the joint or physis cannot be
anatomically reduced closed. The articular and physeal alignment can be
evaluated by radiographic tomograms (trispiral or
CT),
MRI scans, or wrist arthroscopy. If anatomic alignment of the physis
and articular surface is not present, the risk of growth arrest,
long-term deformity, or limited function is great (Fig. 9-20).
Even minimal displacement (more than 1 mm) should not be accepted in
this situation. Arthroscopically assisted reduction is helpful to align
and stabilize these rare physeal fractures.48,76
Although it is an equipment intensive operation with arthroscopy,
external fixation, transphyseal and transepiphyseal pin or screw
fixation, and fluoroscopy, anatomic reduction, and stabilization of the
physis and articular surface can be achieved (Fig. 9-21).
 |
|
FIGURE 9-19 A. AP and lateral views of a displaced Salter-Harris type II distal radial fracture. B. AP and lateral views 1 month after simple pin fixation.
|
 |
|
FIGURE 9-20 A. A markedly displaced Salter-Harris type IV fracture of the distal radius in an 11-year-old boy who fell from a horse. B. Radiograph taken 3 weeks after closed reduction demonstrates displacement of the comminuted fragments. C.
Eighteen months after injury, there was 15 mm of radial shortening, and the patient had a pronounced radial deviation deformity of the wrist. |
closed under conscious sedation with the assistance of portable
fluoroscopy. A long-arm cast with appropriate three-point molding is
applied. This is changed to a short-arm cast when there is sufficient
healing for fracture stability, usually after 3 to 4 weeks. Cast
immobilization is discontinued when there is clinical and radiographic
evidence of fracture healing, generally 4 to 6 weeks after fracture.
Range-of-motion and strengthening exercises are begun with a home
program. When the child achieves full motion and strength, he or she
can return to full activity, including competitive sports. As the risk
of posttraumatic physeal disturbance is approximately 4% to 5%,
follow-up radiographs are obtained at 6 to 12 months after fracture to
be certain there is no growth arrest.9,24
physeal fracture associated with significant volar soft tissue
swelling, median neuropathy, or ipsilateral elbow and radial fractures
(“floating elbow”) is treated with closed reduction and percutaneous
pinning (Fig. 9-22). This avoids the increased
risk of compartment syndrome in the carpal canal or volar forearm that
is present if a well-molded, tight cast is applied. In addition, acute
percutaneous pinning of the fracture prevents increased swelling, cast
splitting, loss of reduction, and concerns about malunion or growth
arrest with repeat reduction. Acute pinning of the fracture with one or
two smooth pins through the radial epiphysis provides fracture
stability without a compressive cast. The risk of growth arrest from a
narrow-diameter, smooth pin left in place for 3 to 4 weeks is
exceedingly small.252
acute carpal tunnel or forearm compartment syndrome, displaced (more
than 1 mm) Salter-Harris type III or IV fractures, or triplane
equivalent fractures. For an irreducible Salter-Harris type I or II
fracture, exposure is from the side of the torn periosteum. Because
these fractures usually are displaced dorsally, a volar exposure is
used. Smooth pins are used for stabilization and are left in for 3 to 4
weeks. Open fractures are exposed through the open wound with proximal
and distal extension for adequate débridement. All open débridements
are performed in the operating room under general anesthesia. Acute
compartment syndromes are treated with immediate release of the
transverse carpal ligament or forearm fascia. The transverse carpal
ligament is released in a Z-plasty fashion to lengthen the ligament and
prevent volar bow-stringing and scarring of the median nerve against
the palmar skin. Displaced intra-articular fractures are best treated
with arthroscopically assisted reduction and fixation. Distraction
across the joint can be achieved with application of an external
fixator or wrist arthroscopy traction devices and finger traps.
Standard dorsal portals (3/4 and 4/5) are used for viewing the
intra-articular aspect of the fracture and alignment of the reduction66,76 In addition, direct observation through the arthroscope can aid in safe placement of the intraepiphyseal pins.48,129
Fluoroscopy is used to evaluate the extra-articular aspects of the
fracture (triplane equivalent and type IV fractures), the reduction,
and placement of fixation pins.
 |
|
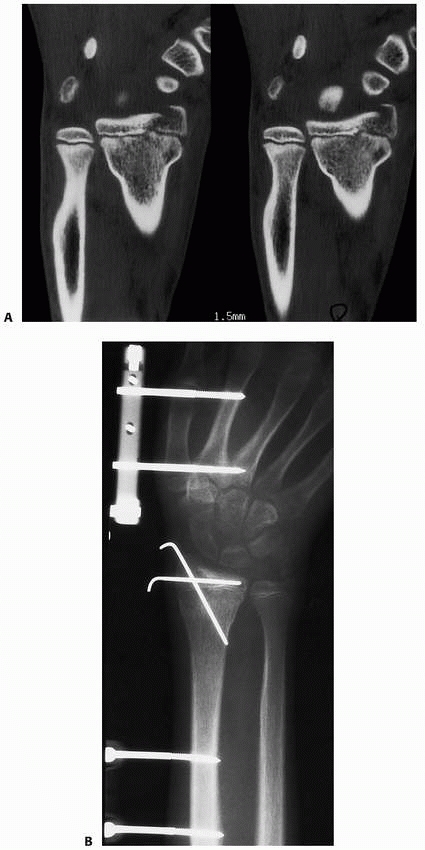
FIGURE 9-21 A. CT scan of displaced Salter-Harris type IV fracture. B. Surgical correction included external fixation distraction, arthroscopically assisted reduction, and smooth pin fixation.
|
 |
|
FIGURE 9-22 A.
Ipsilateral distal radial physeal and supracondylar fractures. This 6-year-old sustained both a dorsally displaced distal radial physeal fracture (closed arrow) and a type II displaced supracondylar fracture of the humerus (open arrows). B. Similar case treated with percutaneous pinning of radial physeal fracture and supracondylar humeral fracture. |
fractures often occur in children with significant growth remaining.
The deformity from a Salter-Harris type I or II fracture is in the
plane of motion of the wrist joint and, therefore, will remodel with
ensuing growth (Fig. 9-23).8,108,181
Repeat reduction should not be done more than 7 days after fracture
because of the risk of growth arrest. The malunited fracture should be
monitored over the next 6 to 12 months for remodeling. If the fracture
does not remodel, persistent extension deformity of the distal radial
articular surface puts the patient at risk for developing midcarpal
instability217 or degenerative
arthritis of the wrist, though a recent report has raised the question
of whether imperfect final radiographic alignment necessarily leads to
symptomatic arthrosis.64 For
malunion correction, an opening-wedge dorsal osteotomy is made, iliac
crest bone of appropriate trapezoidal shape to correct the deformity is
inserted, and either a plate or external fixator is used to maintain
correction until healing.62
 |
|
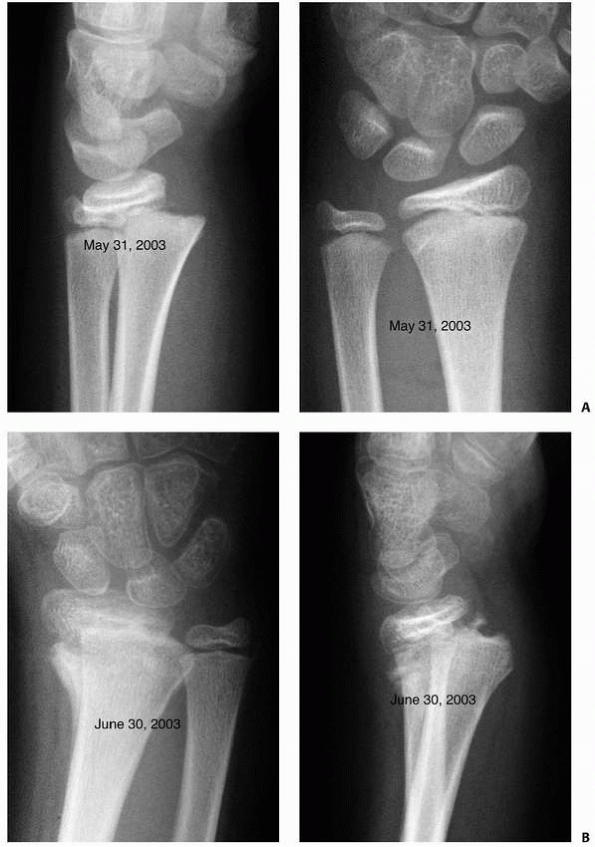
FIGURE 9-23 A. AP and lateral views of displaced radial physeal fracture. B. Healed malunion 1 month after radial physeal fracture. (continues)
|
the risk of development of degenerative arthritis if the articular
stepoff is more than 2 mm.113 MRI or
CT scans can be useful in preoperative evaluations. Arthroscopy allows
direct examination of the deformity and areas of impingement or
potential degeneration. Intra-articular osteotomy with bone grafting in
the metaphysis to support the reconstructed articular surface is
controversial and risky; however, it has the potential to restore
anatomic alignment to the joint and prevent serious long-term
complications. This problem fortunately is uncommon in children because
of the rarity of the injury and this type of malunion.
 |
|
FIGURE 9-23 (continued) C. Significant remodeling at 5 months after fracture. D. Anatomic remodeling with no physeal arrest.
|
or late (more than 7 days) reduction of a displaced fracture. The
incidence of radial growth arrest has been shown to be 4% to 5% of all
displaced radial physeal fractures.9,24,124
The trauma to the physeal cartilage from displacement and compression
is a significant risk factor for growth arrest. However, a correlation
between the risk of growth arrest and the degree of displacement, type
of fracture, or type of reduction has yet to be defined. Similarly, the
risk of further compromising the physis with late reduction at various
time intervals is still unclear. The current recommendation is for an
atraumatic reduction of a displaced physeal fracture less than 7 days
after injury.
on the severity of the arrest and the amount of growth remaining. A
complete arrest of the distal radial physis in a skeletally immature
patient can be a serious problem. The continued growth of the ulna with
cessation of radial growth can lead to incongruity of the DRUJ,
ulnocarpal impaction, and development of a TFCC tear (Fig. 9-25).9,236
The radial deviation deformity at the wrist can be severe enough to
cause limitation of wrist and forearm motion. Pain and clicking can
develop at the ulnocarpal or radioulnar joints, indicative of
ulnocarpal impaction or a TFCC tear. The deformity will progress until
the end of growth. Pain and limited motion and function will be present
until forearm length is rebalanced, until the radiocarpal, ulnocarpal,
and radioulnar joints are restored, and until the TFCC tear and areas
of chondromalacia are repaired or débrided.161,221,236
Radiographic screening 6 to 12 months after injury can identify the
early arrest. A small area of growth arrest in a patient near skeletal
maturity may be clinically inconsequential. However, a large area of
arrest in a patient with marked growth remaining can lead to ulnocarpal
impaction and forearm deformity if intervention is delayed. MRI can map
the area of arrest.168 If it is less than 45% of the physis, a bar resection with fat interposition can be attempted.120,121 This may restore radial growth and prevent future problems (Fig. 9-26). If the bar is larger than 45% of the physis, bar resection is unlikely to be successful.
An early ulnar epiphysiodesis will prevent growth imbalance of the forearm.236
The growth discrepancy between forearms in most patients is minor and
does not require treatment. However, this is not the case for a patient
with an arrest at a very young age, for whom complicated decisions
regarding forearm lengthening need to occur.
 |
|
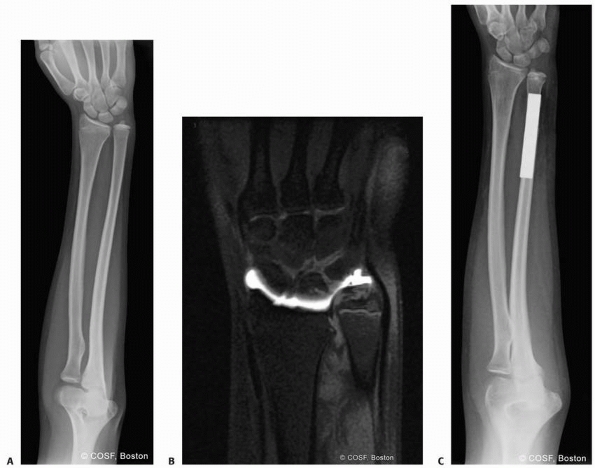
FIGURE 9-24 A. AP radiograph of growth arrest with open ulnar physis. B.
MRI scan of large area of growth arrest that was not deemed resectable by mapping. Note is made of impaction of the distal ulna against the triquetrum and a secondary peripheral TFCC tear. C. Radiograph after ulnar shortening osteotomy, restoring neutral ulnar variance. |
 |
|
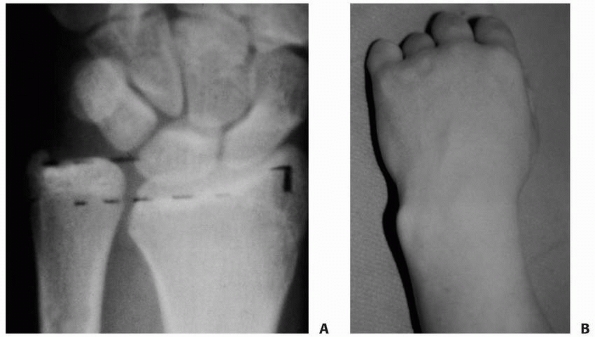
FIGURE 9-25 A.
AP radiograph of radial growth arrest and ulnar overgrowth after physeal fracture. Patient complained of ulnar-sided wrist pain and clicking. B. Clinical photograph of ulnar overgrowth and radial deviation deformity. |
 |
|
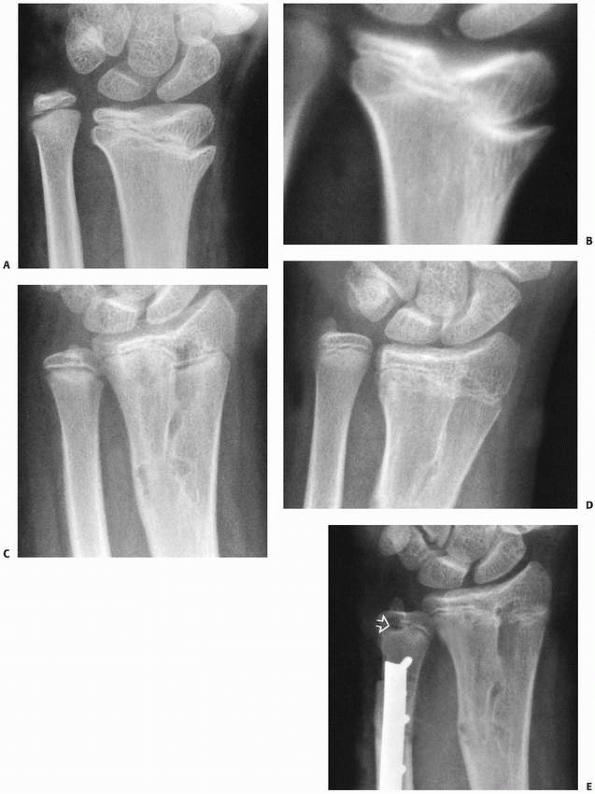
FIGURE 9-26 Osseous bridge resection. A.
This 10-year-old had sustained a distal radial physeal injury 3 years previously and now complained of prominence of the distal ulna with decreased supination and pronation. B. Polytomes revealed a well-defined central osseous bridge involving about 25% of the total diameter of the physis. C. The bridge was resected, and autogenous fat was inserted into the defect. Growth resumed with resumption of the normal ulnar variance. Epiphysiodesis of the distal ulna was postponed for 6 months. D. Unfortunately, the radius slowed its growth, and a symptomatic positive ulnar variance developed. E. This was treated with an epiphysiodesis (open arrow) and surgical shortening of the ulna. The clinical appearance and range of motion of the forearm returned to essentially normal. |
between the radius and ulna can lead to relative radial shortening and
ulnar overgrowth. The distal ulna can impinge on the lunate and
triquetrum and cause pain with ulnar deviation, extension, and
compression activities.12 This is particularly true in repetitive wrist loading sports such as field hockey, lacrosse, and gymnastics.45
Physical examination loading the ulnocarpal joint in ulnar deviation
and compression will recreate the pain. Radiographs show the radial
arrest, ulnar overgrowth, and distal ulnocarpal impingement. The
ulnocarpal impaction also may be caused by a hypertrophic ulnar styloid
fracture union
(Fig. 9-27) or an ulnar styloid nonunion.22,133
MRI may reveal chondromalacia of the lunate or triquetrum, a tear of
the TFCC, and the extent of the distal radial physeal arrest.
 |
|
FIGURE 9-27 AP radiograph revealing hypertrophic ulnar styloid healing as the source of the ulnar carpal impaction pain in this patient.
|
The ulnar overgrowth is corrected by either an ulnar shortening
osteotomy or radial lengthening. Most often, a marked degree of
positive ulnar variance requires ulnar shortening to neutral or
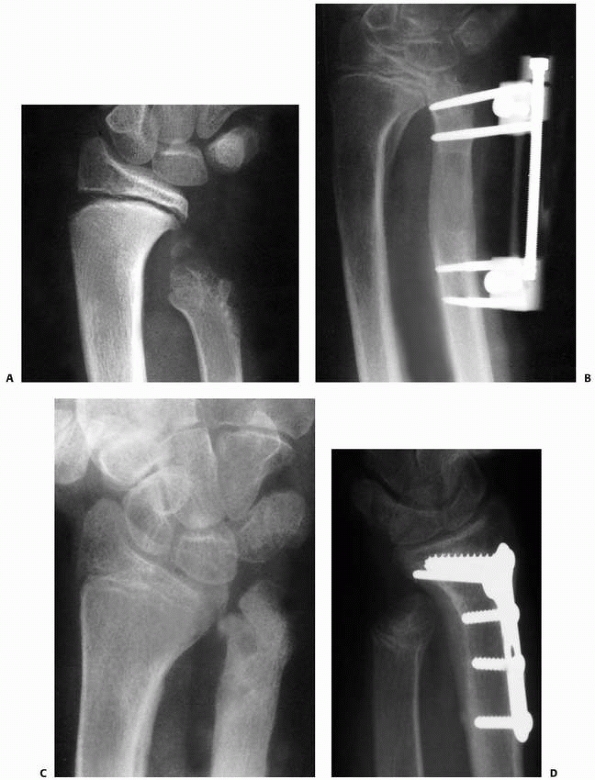
negative variance (Fig. 9-28). If the ulnar
physis is still open, a simultaneous arrest should be done to prevent
recurrent deformity. If the degree of radial deformity is marked, this
should be corrected by a realignment or lengthening osteotomy. Criteria
for radial correction is debatable, but we have used radial inclination
of less than 11 degrees on the AP radiograph as an indication for
correction (Fig. 9-29).236
In the rare case of complete arrest in a very young patient, radial
lengthening is preferable to ulnar shortening to rebalance the forearm.
 |
|
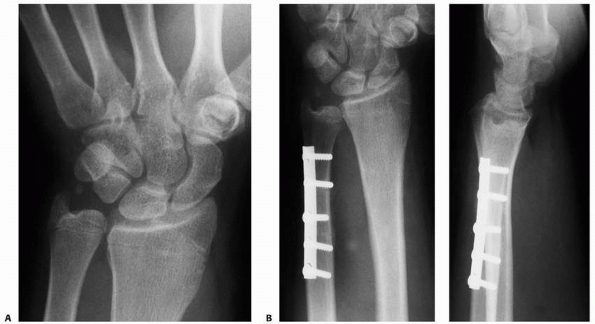
FIGURE 9-28 A.
AP radiogaph of distal radial growth arrest, ulnar overgrowth, and an ulnar styloid nonunion. Wrist arthroscopy revealed an intact triangular fibrocartilage complex. B. AP and lateral radiographs after ulnar shortening osteotomy. |
traumatic TFCC tears should be repaired. The presence of an ulnar
styloid nonunion at the base often is indicative of an associated
peripheral tear of the TFCC.1,161,221,236 The symptomatic ulnar styloid nonunion is excised22,133,159
and any TFCC tear is repaired. If physical examination or preoperative
MRI indicates a TFCC tear in the absence of an ulnar styloid nonunion,
an initial arthroscopic examination can define the lesion and
appropriate treatment. Peripheral tears are the most common TFCC tears
in children and adolescents and can be repaired arthroscopically by an
outside-in suture technique. Tears off the sigmoid notch are the next
most common in adolescents and can be repaired with
arthroscopic-assisted, transradial sutures. Central tears are rare in
children and, as opposed to adults with degenerative central tears,
arthroscopic débridement usually does not result in pain relief in
children. Distal volar tears also are rare and are repaired open, at
times with ligament reconstruction.221
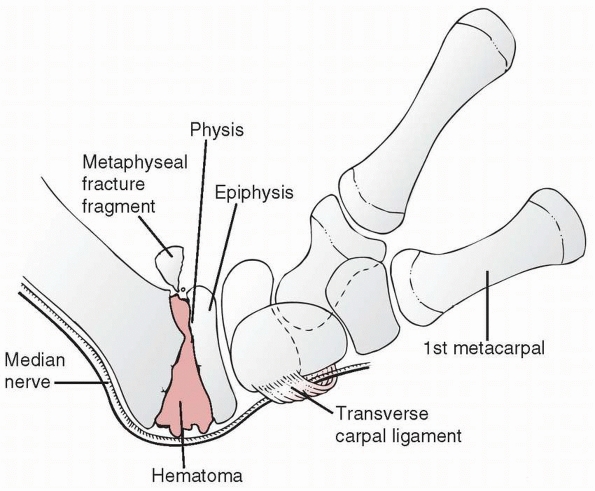
trauma from the initial displacement of the fracture, traction ischemia
from a persistently displaced fracture, or the development of a
compartment syndrome in the carpal canal or volar forear (Fig. 9-30).239 All patients with displaced distal radial fracturesm
should undergo a careful motor-sensory examination upon presentation to
an acute care facility. The flexor pollicis longus, index flexor
digitorum profundus, and abductor pollicis brevis muscles should be
tested. Light-touch and two-point discrimination sensibility of the
thumb and index finger should be tested in any child over 5 years of
age with a displaced Salter-Harris type I or II fracture. Median
neuropathy and marked volar soft tissue swelling are indications for
percutaneous pin stabilization of the fracture to lessen the risk of
compartment syndrome in a cast.
 |
|
FIGURE 9-29 A. More severe ulnar overgrowth with dislocation of the distal radioulnar joint and flattening of the radial articular surface. B. Intraoperative fluoroscopic view of ulnar shortening and radial osteotomy to corrective deformities.
|
ischemia generally resolves after fracture reduction. The degree of
neural injury determines the length of time to recovery. Recovery can
be monitored with an advancing Tinel sign along the median nerve.
Motor-sensory testing can define progressive return of neural function.
carpal tunnel syndrome will not recover until the carpal tunnel is
decompressed. After anatomic fracture reduction and pin stabilization,
volar forearm and carpal tunnel pressures are measured. Gelberman77
recommended waiting 20 minutes or more to allow for pressure-volume
equilibration before measuring pressures. If the pressures are elevated
beyond 40 mm Hg or the difference between the diastolic pressure and
the compartment pressure is less than 30 mm Hg,108
an immediate release of the affected compartments should be performed.
The carpal tunnel is released through a palmar incision in line with
the fourth ray, with care to avoid injuring the palmar vascular arch
and the ulnar nerves exiting the Guyon canal. The transverse carpal
ligament is released with a Z-plasty closure of the ligament to prevent
late bow-stringing of the nerve against the palmar skin. The volar
forearm fascia is released in the standard fashion.
 |
|
FIGURE 9-30
Volar forearm anatomy outlining the potential compression of the median nerve between the metaphysis of the radius and dorsally displaced physeal fracture. The taut volar transverse carpal ligament and fracture hematoma also are contributing factors. (Redrawn from Waters PM, Kolettis GJ, Schwend R. Acute median neuropathy following physeal fractures of the distal radius. J Pediatr Orthop 1994;14:173-177, with permission.) |
Competitive gymnastics is by far the most common cause.23,43,47,135,192,223 Other activities reported to cause radial physeal stress fractures include break dancing, wrestling, and cheerleading.79
Factors that predispose to this injury include excessive training, poor
techniques, and attempts to advance too quickly in competitive level.
Proper coaching is important in preventing these injuries.
recurring, activity-related wrist pain, usually aching and diffuse, in
the region of the distal radial metaphysis and physis. Extremes of
dorsiflexion and palmar flexion reproduce the pain. There is local
tenderness over the dorsal, distal radial physis. Resistive contracture
strength testing of the wrist dorsiflexors often reproduces the pain.
There may be fusiform swelling about the wrist if there is reactive
bone formation. The differential diagnosis includes physeal stress
injury, ganglion, ligamentous or TFCC injury, tendonitis or
muscle-tendon tear, fracture such as a scaphoid fracture, and
osteonecrosis of the scaphoid (Preiser disease) or lunate (Kienböck
disease). Radiographs may be diagnostic. Physeal widening and reactive
bone formation are indicative of chronic physeal stress fracture.
Premature physeal closure indicates long-standing stress.191,249
In this situation, continued ulnar growth leads to an ulnar positive
variance and pain from ulnocarpal impaction or a TFCC tear.5,45,223
Normal radiographs may not show an early physeal stress fracture. If
the diagnosis is suggested clinically, bone scanning or MRI is
indicated. Bone scanning is sensitive but nonspecific; MRI usually is
diagnostic.
difficult depending on the skill level of the athlete and the desires
of the child, coach, and parents to maintain constant training.
Education regarding the long-term consequences of a growth arrest is
important in this emotionally charged situation. Short-arm cast
immobilization for several weeks may be the only way to restrict stress
to the radial physis in some patients. Splint protection is appropriate
in cooperative patients. Protection should continue until there is
resolution of pain with examination and activity. The athlete can
maintain cardiovascular fitness, strength, and flexibility while
protecting the injured wrist. Once the acute physeal injury has healed,
return to weight-bearing activities should be gradual. This requires
the cooperation of the coach and parents. Adjustment of techniques and
training methods often is necessary to prevent recurrence. The major
concern is development of a radial growth arrest in a skeletally
immature patient. This is an avoidable complication.
presentation, treatment depends on the degree of deformity and the
patient’s symptoms. Physeal bar resection often is not possible because
the arrest is usually too diffuse in stress injuries. If there is no
significant ulnar overgrowth, a distal ulnar epiphysiodesis will
prevent the development of an ulnocarpal impaction syndrome. For ulnar
overgrowth and ulnocarpal pain, an ulnar shortening osteotomy is
indicated. Techniques include transverse, oblique, and Z-shortening
osteotomies. Transverse osteotomy has a higher risk of nonunion than
either oblique or Z-shortening and should be avoided. Even when oblique
or Z-shortenings are used, making the osteotomy more distally in the
metaphyseal region will lessen the risk of nonunion, owing to the more
robust vascularity of the distal ulna. The status of the TFCC also
should be evaluated by MRI or wrist arthroscopy. If there is an
associated TFCC tear, it should be repaired as appropriate.
ulnar physeal fractures occur in association with radial metaphyseal or
physeal fractures. Physeal separations are classified by the standard
Salter-Harris criteria. The rare pediatric Galeazzi injury usually
involves an ulnar physeal fracture rather than a soft tissue disruption
of the distal radioulnar joint. Another ulnar physeal fracture is an
avulsion fracture off the distal aspect of the ulnar styloid.1,211
Although an ulnar styloid injury is an epiphyseal avulsion, it can be
associated with soft tissue injuries of the TFCC and ulnocarpal joint
but does not cause growth-related complications.
occurring in 10% to 55% of patients. It is unclear why the distal ulna
has a higher incidence of growth arrest after fracture than does the
radius. Ulnar growth arrest in a young child leads to relative radial
overgrowth and bowing.
physeal fractures: immobilization alone, closed reduction and cast
immobilization, closed reduction and percutaneous pinning, and open
reduction. Often, these fractures are minimally displaced or
nondisplaced. Immobilization until fracture healing at 3 to 6 weeks is
standard treatment. Closed reduction is indicated for displaced
fractures with more than 50% translation or 20 degrees of angulation.
Most ulnar physeal fractures reduce to a near anatomic alignment with
reduction of the radial fracture due to the attachments of the distal
radioulnar joint ligaments and TFCC. Failure to obtain a reduction of
the ulnar fracture may indicate that there is soft tissue interposed in
the fracture site. This is an indication for open reduction. Exposure
should be from the side of the torn periosteum, typically opposite the
Thurston-Holland fragment or direction of displacement. The interposed
soft tissue (periosteum, extensor tendons, abductor digiti quinti, or
flexor tendons) must be extracted from the fracture site.55,117,157
If reduction is not stable, a small-diameter smooth pin can be used to
maintain alignment until healing at 3 to 4 weeks. Further injury to the
physis should be avoided during operative exposure and reduction
because of the high risk of growth arrest.
and represent a soft tissue avulsion of the attachment of the TFCC or
ulnocarpal ligaments. Treatment consists of immobilization and
monitoring of long-term outcome, and most heal without sequelae.119 However, an acute displaced fracture of the base of the styloid represents a disruption of the TFCC.1
Most of these injuries are caused by high-velocity trauma in
adolescents at or near skeletal maturity. Treatment should be open
reduction with tension band fixation
of the styloid to the metaphysis and repair of the TFCC. The tension band wire is removed at 3 to 6 weeks.
 |
|
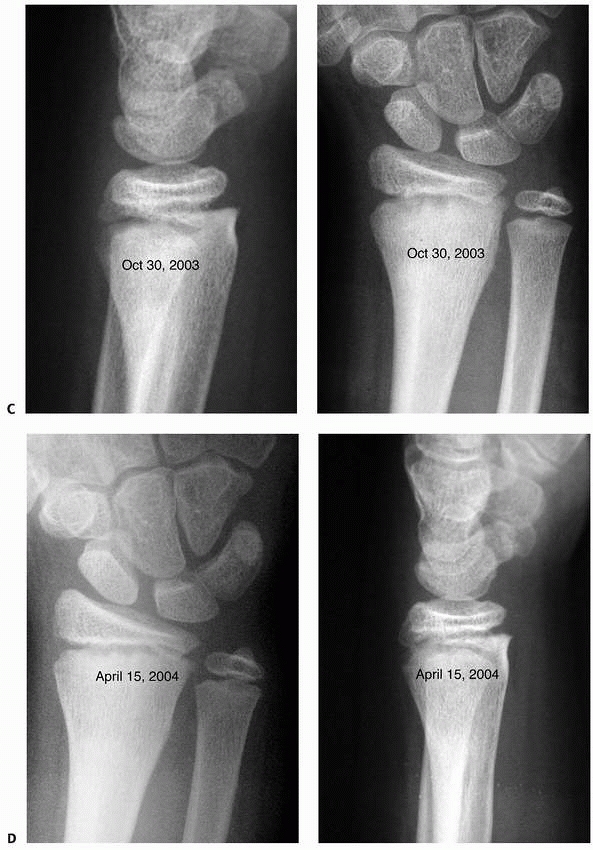
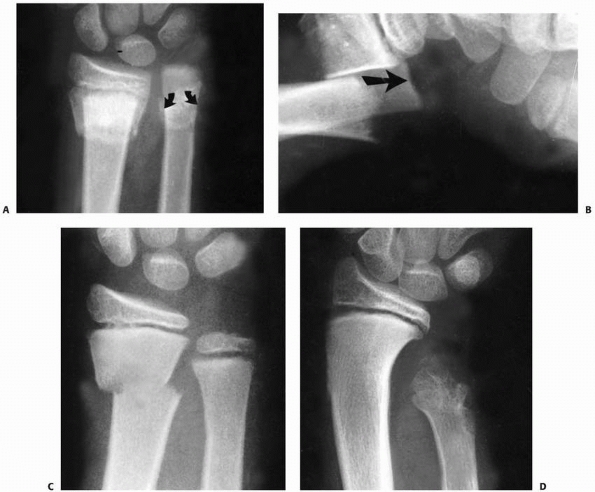
FIGURE 9-31 A,B. A 10-year-old boy sustained a closed Salter-Harris type I separation of the distal ulnar physis (arrows) combined with a fracture of the distal radial metaphysis. C. An excellent closed reduction was achieved atraumatically. D. Long-term growth arrest of the distal ulna occurred.
|
Nonunion may be associated with TFCC tears or ulnocarpal impaction. The
hypertrophic healing represents a pseudoulnar positive variance with
resultant ulnocarpal impaction. Both cause ulnar-sided wrist pain.
Compression of the lunate or triquetrum on the distal ulna reproduces
the pain. Clicking with ulnocarpal compression or forearm rotation
represents either a TFCC tear or chondromalacia of the lunate or
triquetrum. Surgical excision of the nonunion or hypertrophic union
with repair of the TFCC to the base of the styloid is the treatment of
choice. Postoperative immobilization for 4 weeks in a long-arm cast
followed by 2 weeks in a short-arm cast protects the TFCC repair.
described 18 such fractures, with growth arrest in 10%. If the patient
is young enough, continued growth of the radius will lead to deformity
and dysfunction. The distal ulnar aspect of the radial physis and
epiphysis appears to be tethered by the foreshortened ulna (Fig. 9-32).
The radial articular surface develops increased inclination toward the
foreshortened ulna. This is similar to the deformity Peinado164
created experimentally with arrest of the distal ulna in rabbits’
forelimbs. The distal ulna loses its normal articulation in the sigmoid
notch of the distal radius. The metaphyseal-diaphyseal region of the
radius often becomes notched from its articulation with the distal ulna
during forearm rotation. Frequently, these patients have pain and
limitation of motion with pronation and supination.12
development of marked ulnar foreshortening and subsequent radial
deformity. Because it is well known that distal ulnar physeal fractures
have a high incidence of growth arrest, these patients should have
serial radiographs at 6 to 12 months after fracture for early
identification. Unfortunately, in the distal ulnar physis, physeal bar
resection generally is unsuccessful. Surgical arrest of the radial
physis can prevent radial deformity. Usually, this occurs toward the
end of growth so that the forearm length discrepancy is not a problem.
 |
|
FIGURE 9-32 A. The appearance of the distal ulna in the patient seen in Figure 9-21,
3 years after injury, demonstrating premature fusion of the distal ulnar physis with 3.2 cm of shortening. The distal radius is secondarily deformed, with tilting and translocation toward the ulna. B. In the patient in Figure 9-21 with distal ulnar physeal arrest, a lengthening of the distal ulna was performed using a small unipolar distracting device. The ulna was slightly overlengthened to compensate for some subsequent growth of the distal radius. C. Six months after the lengthening osteotomy, there is some deformity of the distal ulna, but good restoration of length has been achieved. The distal radial epiphyseal tilt has corrected somewhat, and the patient has asymptomatic supination and pronation to 75 degrees. D. Similar case to Figure 9-32A-C, but with more progressive distal radial deformity treated with corrective osteotomy and epiphysiodesis of the distal radius. |
deformity. Treatment involves rebalancing the length of the radius and
ulna. The options include hemiphyseal arrest of the radius, corrective
radial closing wedge osteotomy, and ulnar lengthening (Fig. 9-32),12,81,152
or a combination of these procedures. The painful impingement of the
radius and ulna with forearm rotation can be corrected with
reconstitution of the distal radioulnar joint. If the radial physis has
significant growth remaining, a radial physeal arrest should be done at
the same time as the surgical rebalancing of the radius and ulna.154 Treatment is individualized depending on the age of the patient, degree of deformity, and level of pain and dysfunction.
 |
|
FIGURE 9-33 Metaphyseal biomechanical patterns. A. Torus fracture. Simple bulging of the thin cortex (arrow). B. Compression greenstick fracture. Angulation of the dorsal cortex (large curved arrow). The volar cortex is intact but slightly plastically deformed (small white arrows). C. Tension failure greenstick fracture. The dorsal cortex is plastically deformed (white arrow), and the volar cortex is complete and separated (black arrows). D.
Complete length maintained. Both cortices are completely fractured, but the length of the radius has been maintained. (Reprinted from Wilkins KE, ed. Operative Management of Upper Extremity Fractures in Children. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1994:24, with permission.) |
These fractures have a peak incidence during the adolescent growth
spurt, which in girls is age 11 to 12 years and in boys is 12 to 13
years.10 During this time of
extensive bone remodeling, there is relative osteoporosis of the distal
radial metaphysis, which makes this area more susceptible to fracture
with a fall.
 |
|
FIGURE 9-34 Complete fractures; bayonet apposition. A. Dorsal bayonet. B. Volar bayonet.
|
 |
|
FIGURE 9-35
A 10-year-old girl with an innocuous-appearing distal radial fracture associated with an ipsilateral angulated radial neck fracture (arrows). |
 |
|
FIGURE 9-36 Reverse bayonet. A. Typical volar bayonet fracture. Often the distal end of the proximal fragment is buttonholed through the extensor tendons (arrows).
(Reprinted from Wilkins KE, ed. Operative Management of Upper Extremity Fractures in Children. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1994:27, with permission.) B. Intact volar periosteum and disrupted dorsal periosteum (arrows). The extensor tendons are displaced to either side of the proximal fragment. |
outstretched hand. The usual dorsiflexion position of the wrist leads
to tension failure on the volar side. Fracture type and degree of
displacement depend on the height and velocity of the fall.205
These fractures can be nondisplaced torus or buckle injuries (common in
younger children with a minimal fall) or dorsally displaced fractures
with apex volar angulation (more common in older children with higher
velocity injuries) (Fig. 9-33). Displacement may be severe enough to cause foreshortening and bayonet apposition (Fig. 9-34).
Rarely, a mechanism such as a fall from a height can cause a distal
radial fracture associated with a more proximal fracture of the forearm
or elbow (Fig. 9-35).163,210,241 These “floating elbow” situations are indicative of higher-velocity trauma and risk of compartment syndrome.185 In addition, a fall with a palmar flexed wrist can produce a volarly displaced fracture with apex dorsal angulation (Fig. 9-36).
The incidence of wrist and forearm fractures was roughly half (5.7/1000
per year) in the three winter months in Wales compared with the rest of
the year (10.7/1000 per year). In addition, the nonwinter month
fractures were more severe in terms of requiring reduction and
hospitalization in this longitudinal study. Certain sports, such as
snowboarding, soccer goal-keeping, and horseback riding, have been
shown to have an increased risk of distal radial fracture.104,116,138,187,197,215
Protective wrist guards have been shown to decrease the injury rate in
snowboarders, especially beginners and persons with rental equipment.187
 |
|
FIGURE 9-37 Dorsal bayonet deformity. A. Typical distal metaphyseal fracture with dorsal bayonet showing a dorsal angulation of the distal forearm. B. Usually, the periosteum is intact on the dorsal side and disrupted on the volar side.
|
The clinical signs depend on the degree of fracture displacement. With
a nondisplaced torus fracture in a young child, medical attention may
not be sought until several days after injury, because the intact
periosteum is protective in this situation, lessening pain and the
child’s restriction of activities. Most children with distal radial
fractures, however, present acutely after the fall with an obvious
deformity. Physical examination is limited by the patient’s pain and
anxiety, but it is imperative to obtain an accurate examination of the
motor and sensory components of the radial, median, and ulnar nerves
before treatment. Median nerve motor function is evaluated by testing
the abductor pollicis brevis (intrinsic) and flexor pollicis longus
(extrinsic) muscles. Ulnar nerve motor evaluation includes testing the
first dorsal interosseous (intrinsic), abductor digit quinti
(intrinsic), and flexor digitorum profundus to the small finger
(extrinsic) muscles. Radial nerve evaluation involves testing the
common digital extensors for metacarpophalangeal joint extension.
Sensibility to light touch and two-point discrimination should be
tested. Normal two-point discrimination is less than 5 mm but is not
present until age 5 to 7 years. Pin-prick sensibility testing will only
hurt and scare the already anxious child and should be avoided. A
prospective study indicated an 8% incidence of nerve injury in children
with distal radial fractures.246
degree of displacement. Standard AP and lateral radiographs usually are
sufficient. Complete wrist, forearm, and elbow views are necessary for
high-velocity injuries or when there is clinical tenderness. More
extensive radiographic studies (CT scan, tomography) usually are not
necessary unless there is intra-articular extension of the metaphyseal
fracture in a skeletally mature adolescent.
of associated ulnar fracture, and direction of displacement. Fracture
displacement is broadly classified as dorsal or volar. Most distal
radial metaphyseal fractures are displaced dorsally with apex volar
angulation.222 Volar displacement with apex dorsal angulation can occur with palmar flexion injuries.
These injuries are stable because of the intact periosteum. Rarely,
they may extend into the physis, putting them at risk for growth
impairment.168,169
Incomplete or greenstick fractures occur with a combination of
compressive and rotatory forces, generally a dorsiflexion force and
supination deforming force. This leads to a volar tension side failure
and a dorsal compression injury. The degree of force determines the
amount of plastic deformation, dorsal comminution, and fracture
angulation and rotation. If the force is sufficient, a complete
fracture occurs with disruption of both the volar and dorsal cortices.
Length may be maintained with apposition of the proximal and distal
fragments. Frequently, the distal fragment lies proximal and dorsal to
the proximal fragment in bayonet apposition (Table 9-2).
metaphyseal fracture can be metaphyseal or physeal or an ulnar styloid
avulsion. Similar to radial metaphyseal fractures, the ulnar fracture
can be complete or incomplete.
The combination of a displaced supracondylar distal humeral fracture
and a displaced distal radial metaphyseal fracture has been called the
pediatric floating elbow. This injury combination is unstable and has
an increased risk for malunion and neurovascular compromise.
classified by degree of instability. Unstable fractures have been
predominately defined by the failure to maintain a successful closed
reduction
(Fig. 9-38). This occurs in approximately 30% of complete distal radial metaphyseal fractures.136,177,244
This high percentage of loss of alignment has been tolerated because of
the remodeling potential of the distal radius. Anatomic remodeling is
possible because the extension deformity is in the plane of motion of
the wrist joint, the metaphyseal fracture is juxtaphyseal, and most of
these fractures occur while there is still significant growth
remaining. However, concern has increased about the high failure rate
of closed reduction to maintain anatomic alignment of these fractures.
Factors that have been identified as increasing the risk of loss of
reduction with closed manipulation and casting include poor casting,
bayonet apposition, translation of more than 50% the diameter of the
radius, apex volar angulation of more than 30 degrees, isolated radial
fractures, and radial and ulnar metaphyseal fractures at the same level.6,136,177,244,254
|
TABLE 9-2 Classification: Distal Metaphyseal Fractures
|
||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||
 |
|
FIGURE 9-38 A. Serial radiographs at 3 days and 10 days (B) revealing slow loss of reduction that is common after closed reduction of distal radial metaphyseal fractures.
|
physeal fractures: immobilization alone, closed reduction and cast
immobilization, closed reduction and percutaneous pinning, and open
reduction. The fracture type, degree of fracture instability,
associated soft tissue or skeletal trauma, and the age of the patient
all influence choice of treatment.
|
TABLE 9-3 Acceptable Angular Corrections in Degrees
|
||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||
cortical disruption. As failure occurs in compression, by definition
these are inherently stable injuries. Treatment should consist of
protected immobilization to prevent further injury and relieve pain.39,109,156,173,208,215,243
Once the patient is comfortable, range-of-motion exercises and
nontraumatic activities can begin. Fracture healing usually occurs in 2
to 4 weeks.8,123,133,157 Simple torus fractures usually heal without long-term sequelae.
indicates a more severe injury than a stable torus fracture. Splint or
limited immobilization in this situation puts the child at risk for
displacement. More prolonged, long-arm cast protection in a young
patient who can wiggle out of a short-arm cast and closer follow-up
generally are recommended to lessen the risk of malunion. These
fractures generally heal in 3 to 6 weeks.
 |
|
FIGURE 9-39 Bayonet remodeling. A.
After numerous attempts at closed reduction, the best alignment that could be obtained was dorsal bayonet apposition in this 8-year-old. B. Three months after fracture, there is good healing and early remodeling. C,D. Five years after the injury (age 13), remodeling was complete and the patient had normal appearance and forearm motion. |
radial and ulnar fractures depends on the age of the patient, the
degree and direction of fracture displacement and angulation, the
surgeon’s biases regarding remodeling, and the surgeon’s and
community’s biases regarding deformity. In younger patients, the
remodeling potential of an acute distal radial malunion is extremely
high. Acceptable sagittal plane angulation of an acute distal radial
metaphyseal fracture has been reported to be from 10 to 35 degrees in
patients under 5 years of age.16,32,132,157,175,202,246 Similarly, in patients under 10 years of age, the degree of acceptable angulation has ranged from 10 to 25 degrees.16,32,132,157,175,202,246
In patients over 10 years of age, acceptable alignment has ranged from
5 to 20 degrees depending on the skeletal maturity of the patient (Table 9-3).16,32,41,132,157,175,202,244,246
metaphyseal malunion has led some clinicians to recommend
immobilization alone.46 As mentioned, the range of accepted sagittal malalignment has been broad and is age and clinician dependent (Figs. 9-39 and 9-40).
uniform. The fracture tends to displace radially with an apex ulnar
angulation. This does have the potential to remodel,165
but less so than sagittal plane deformity. Most researchers agree that
only 10 degrees or less of acute malalignment in the frontal plane
should be accepted. More malalignment than this may not remodel and may
result in loss of forearm rotation because of the loss of interosseous
space between the radius and ulna (see Table 9-3).245
 |
|
FIGURE 9-40 Extensive remodeling. A. Injury film of a 7-year-old with a tension failure greenstick fracture. B,C.
Lateral and AP views of the same patient taken 1 month later showing development of 45-degree angulation in the sagittal plane and 40 degrees in the coronal plane. D,E. True appearance taken 4 years later shows only residual angulation of 10 degrees in the sagittal plane and full correction of radial angulation in the coronal plane. The patient had a range of forearm motion equal to that of the opposite extremity and was asymptomatic. |
incomplete fractures should be reduced closed. The areas of controversy
are the degree of acceptable deformity, whether the intact cortex
should be fractured, and the position and type of immobilization.
fracture after closed reduction involve the same differences discussed
in the immobilization section. As mentioned, more malalignment can be
accepted in younger patients, in those with sagittal plane deformity,
and in those without marked cosmetic deformity. Malaligned apex volar
incomplete fractures are less obvious than the less common apex dorsal
fractures.
emphasized, incomplete forearm fractures have a rotatory component to
their malalignment. The more common apex volar fractures represent a
supination deformity, whereas the less common apex dorsal fractures are
malrotated in pronation. Correction of the malrotation is necessary to
achieve anatomic alignment. Controversy exists regarding completion of
greenstick fractures.40,61,102,181,199
Although some researchers advocate completion of the fracture to reduce
the risk of subsequent loss of reduction from the intact periosteum and
concave deformity acting as a tension band214,246 to redisplace the fracture, completing the fracture increases the risk of instability and malunion.
also have been controversial. Recommendations for the position of
postreduction immobilization include supination, neutral, and
pronation. The rationale for immobilization in pronation is that
reduction of the more common apex volar fractures requires correction
of the supination deformity.56 Following this rationale, apex dorsal fractures should be reduced and immobilized in supination. Pollen175 believed that the brachioradialis was a deforming force in pronation and was relaxed in supination (Fig. 9-41) and advocated immobilization in supination for all displaced distal radial fractures. Kasser108
recommended immobilization in slight supination to allow better molding
of the volar distal radius. Some researchers advocate immobilization in
a neutral position, believing this is best at maintaining the
interosseous space and has the least risk of disabling loss of forearm
rotation in the long term.44,132,216 Davis and Green40 and Ogden157 advocated that each fracture seek its own preferred position of stability. Gupta and Danielsson89
randomized immobilization of distal radial metaphyseal greenstick
fractures in neutral, supination, or pronation to try to determine the
best position of immobilization. Their study showed a statistical
improvement in final healing with immobilization in supination. More
recently, Boyer et al.21
prospectively randomized 109 distal third forearm fractures into
long-arm casts with the forearm in neutral rotation, supination, or
pronation following closed reduction. No significant differences in
final radiographic position were noted among the differing positions of
forearm rotation.
 |
|
FIGURE 9-41
The brachioradialis is relaxed in supination but may become a deforming force in pronation. (Reprinted from Pollen AG. Fractures and Dislocations in Children. Baltimore: Williams & Wilkins, 1973, with permission.) |
short-arm cast immobilization is better. Historically, most
publications on pediatric distal radial fracture treatment advocated
long-arm cast treatment for the first 3 to 4 weeks of healing.8,16,108,123,157,216
The rationale is that elbow flexion reduces the muscle forces acting to
displace the fracture. In addition, a long-arm cast may further
restrict the child’s activity and therefore decrease the risk of
displacement. However, Chess et al.28,29
reported redisplacement and reduction rates with well-molded short-arm
casts similar to those with long-arm casts. They used a cast index
(sagittal diameter divided by coronal diameter at the fracture site) of
0.7 or less to indicate a well-molded cast. Wilkins246
achieved similar results with short-arm cast treatment. The short-arm
cast offers the advantage of elbow mobility and better patient
acceptance of casting. Despite these data, historically most centers
continue to use long-arm cast immobilization.8,16,108,123,216
compared the efficacy of short- and long-arm cast immobilization
following closed reduction for pediatric distal radial fractures.17,240 Bohm et al.17
randomized 102 patients over the age of 4 years to either short- or
long-arm casts following closed reduction of displaced distal radial
metaphyseal fractures. No statistically significant difference was seen
in loss of reduction rate between the two treatment groups. Webb et al.240
similarly randomized 103 patients to short- or long-arm casts after
reduction of distal radial fractures. No significant difference in rate
of lost reduction was seen between the two cohorts. Patients in
short-arm casts, however, missed fewer days of school and required less
assistance with activities of daily living than those with long-arm
casts. In both of these studies, quality of fracture reduction and cast
mold were influential factors in loss of reduction rates. These studies
have challenged the traditional teaching regarding the need for elbow
immobilization to control distal radial fracture alignment.
a number of other radiographic parameters have been proposed to
quantify the quality of reduction and cast molding. These include the
gap index, the three-point index, and axis deviation.6,134,251 Three-point index was the most sensitive, specific, and predictive in a study by Ameldaroglu et al.6
an associated displaced ulnar fracture, are unstable fractures.
Generally,
these
fractures are displaced dorsally, tearing the volar periosteum and soft
tissues. The distal fragment of epiphysis and metaphysis often is in
bayonet apposition with the proximal fragment. Concomitant radial and
ulnar fractures at the same level may be more unstable than isolated
fractures.244 However, Gibbons et al.80
reported loss of reduction in 91% of isolated radial fractures after
closed reduction. Although a rare fracture with bayonet apposition in a
very young patient may remodel,246
the standard treatment for completely displaced fractures is reduction
and stabilization. The current controversy is whether cast
immobilization alone is adequate stabilization or whether percutaneous
pin fixation is more appropriate for displaced, complete, distal radial
metaphyseal fractures.25,74,140
expressed concern about the success of finger trap distraction because
the intact dorsal periosteum will not stretch adequately to allow
reduction. They advocated sequential reduction maneuvers: initial
manipulation of the distal fragment dorsally to accentuate the
deformity (Fig. 9-42), thumb pressure on the
relaxed dorsal edge of the distal fragment to correct the overriding,
and reduction of the fracture by application of distal and volar
pressure (Fig. 9-43). Anatomic reduction may
require repetitive “toggling” of the distal fragment volarly. Reduction
is then assessed with fluoroscopic imaging (Fig. 9-44).
This is clearly age dependent, because the younger the patient, the
greater the potential for remodeling. Volar-dorsal malalignment has the
greatest potential for remodeling because this is in the plane of
predominant motion of the joint. Marked radioulnar malalignment is less
likely to remodel. Malrotation will not remodel. The ranges for
acceptable reduction according to age are given in the immobilization
section on incomplete fractures and apply to complete fractures as well.
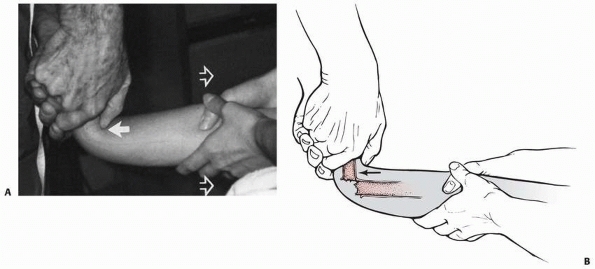 |
|
FIGURE 9-42 A,B. Use of the thumb to push the distal fragment hyperdorsiflexed 90 degrees (solid arrow) until length is re-established. Countertraction is applied in the opposite direction (open arrows).
|
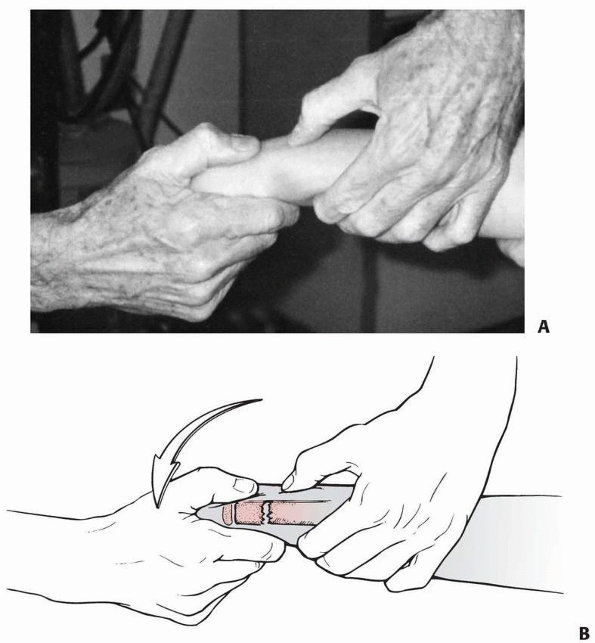 |
|
FIGURE 9-43 A,B.
Once length has been re-established, the distal fragment is flexed into the correct position. Alignment is checked by determining the position of the fragments with the thumb and forefingers of each hand. |
After reduction of a dorsally displaced fracture, three-point fixation
is used with dorsal pressure proximal and distal to the fracture site
and volar pressure over the reduced fracture (Fig. 9-46). The cast should be molded to the normal contour of the forearm. An extension
long-arm cast can be used in younger children to better maintain
reduction of the ulnar bow. A thumb spica component with felt over the
dorsum of the thumb and wrist prevents distal migration of cast and
skin irritation. Excessive swelling should be monitored due to
dependency of the hand. If there is any concern regarding impending
compartment syndrome, the cast and Webril (Kendall, Mansfield, MA)
should be immediately bivalved and the patient’s clinical status
monitored closely. In general, closed reduction and well-molded casting
will result in successful healing of the fracture in desired alignment (Fig. 9-47).
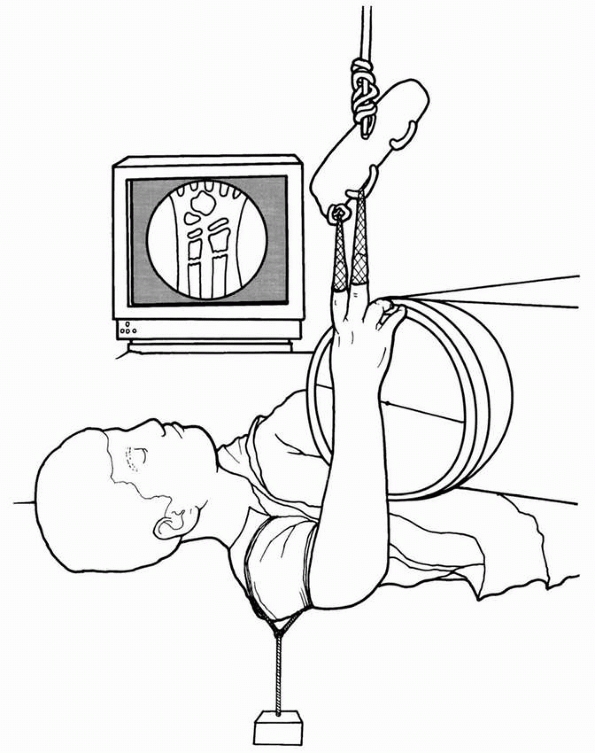 |
|
FIGURE 9-44
Once reduced, the fracture is maintained with finger trap traction and countertraction on the arm. The quality of reduction is assessed quickly with the image intensifier. |
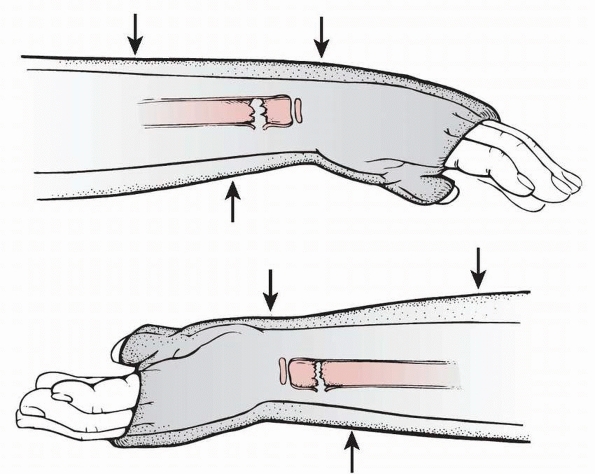 |
|
FIGURE 9-45 Three-point molding. Top:
Three-point molding for dorsally angulated (apex volar) fractures, with the proximal and distal points on the dorsal aspect of the cast and the middle point on the volar aspect just proximal to the fracture site. Bottom: For volar angulated fractures, where the periosteum is intact volarly and disrupted on the dorsal surface, three-point molding is performed with the proximal and distal points on the volar surface of the cast and the middle point just proximal to the fracture site on the dorsal aspect of the cast. |
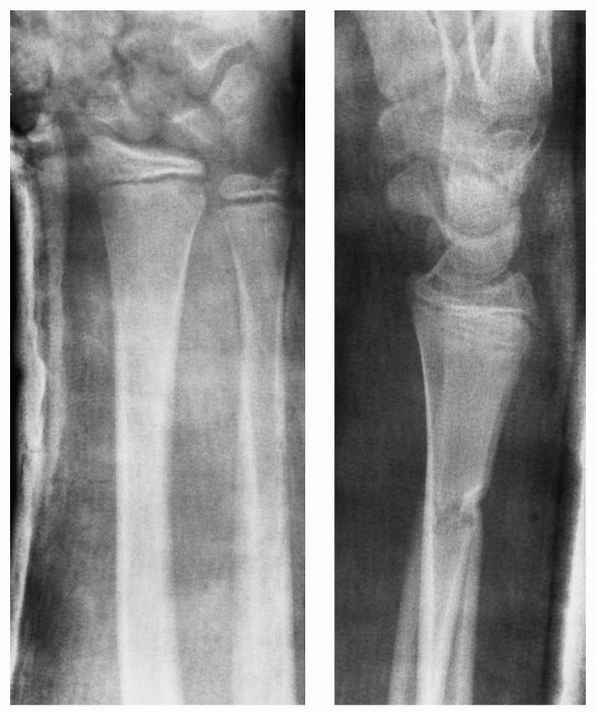 |
|
FIGURE 9-46 AP and lateral radiographs of anatomic alignment with closed reduction of a distal radial metaphyseal fracture.
|
concluded that initial displacement of the radial shaft of over 50% was
the single most reliable predictor of failure of reduction. Proctor et
al.177 found that complete initial
displacement resulted in a 52% incidence of redisplacement of distal
radial fractures in children. Gibbons et al.80
noted that completely displaced distal radial fractures with intact
ulnas had a remanipulation rate of 91% after closed reduction and cast
immobilization alone compared to a 0% rate of remanipulation when the
same fractures were treated with closed reduction, Kirschner wire
fixation, and cast immobilization. All three studies strongly advocated
percutaneous pinning of distal radial fractures at risk of
redisplacement. Two prospective studies confirmed the risk of loss of
reduction with cast immobilization. Miller et al.144
reported a study of distal radial metaphyseal fractures treated by
either closed reduction and cast immobilization or closed reduction and
percutaneous pinning. Selection criteria were a closed metaphyseal
fracture angulated more than 30 degrees in a skeletally immature
patient over 10 years of age. To maximize the outcome of the cast
immobilization group, these patients were treated by a member of the
Pediatric Orthopedic Society of North America with expertise in trauma
care.
General anesthesia, fluoroscopic control, and well-molded cast
immobilization were used. Despite these optimal conditions, 30% of the
patients in the cast immobilization group lost reduction and required
remanipulation. These findings were similar to the prospective study of
pinning and cast treatment of distal radial metaphyseal fractures.140
Again, closed reduction and cast immobilization had a loss of reduction
rate of 21%, whereas pinning maintained reduction. The authors of these
prospective, randomized studies concluded that pinning is a safe,
effective means of treating distal radial metaphyseal fractures;
however, in both prospective studies, results of casting and pinning
were equivalent after 2 years postfracture.140,144
 |
|
FIGURE 9-47 A. Lateral radiograph of displaced metaphyseal radial and ulnar fractures. B. AP and lateral radiographs show anatomic alignment after closed reduction.
|
 |
|
FIGURE 9-48 Results of angulation. A. Significant apex volar angulation of the distal fragment. B.
The appearance was not as apparent cosmetically as in another patient with less angulation that was directed apex dorsally. (Reprinted from Wilkins KE, ed. Operative Management of Upper Extremity Fractures in Children. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1994:27, with permission.) C. Radial deviation constricts the interosseous space, which may decrease forearm rotation. (Reprinted from Wilkins KE, ed. Operative Management of Upper Extremity Fractures in Children. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1994:28, with permission.) |
radial metaphyseal fractures with initial displacement of more than 30
degrees are inherently unstable. Loss of reduction is common, with the
risk in the 20%-to-60% range. Incomplete reduction136,177 and poor casting techniques28,29,246
increase the risk of loss of reduction. In addition, the risk of loss
of reduction increases with the age of the patient and the degree of
initial displacement. Bayonet apposition in a child older than 10 years
is the highest risk.
a malunion. Although the rate of malunion is frequent after these
fractures,8,28,29,34,35,40,91,108,125,195,232 because of the potential for remodeling in skeletally immature patients it has not been considered a serious problem (Fig. 9-49).3,4,16,67,68,71,98
Distal radial fractures are juxtaphyseal, the malunion often is in the
plane of motion of the wrist joint (dorsal displacement with apex volar
angulation), and the distal radius accounts for 60% to 80% of the
growth of the radius. All these factors favor remodeling of a malunion.
reported that of 602 distal radial fractures, 14% had an initial
malunion of more than 5 degrees. Of these, 78% corrected the frontal
plane deformity, and only 53% remodeled completely in the sagittal
plane. In addition, 37% had loss of forearm rotation. Do et al.46
came to similar conclusions in their analysis of 34 pediatric distal
radial metaphyseal fractures that lost reduction and healed with
angulation and/or shortening. Alemdaroglu et al.6
determined that initial complete displacement and initial fracture
obliquity of more than 30 degrees were the greatest risk factors for
redisplacement after closed reduction.
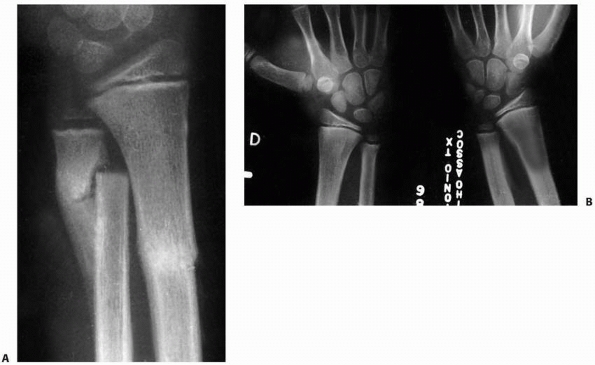 |
|
FIGURE 9-49 A.
Appearance 6 weeks after closed reduction of a distal forearm fracture in an 8½-year-old boy. The radius was reduced, and the ulnar fracture remained overriding. B. Eighteen months after injury, the ulnar fracture had remodeled completely with symmetric distal radioulnar joints. |
percutaneous pinning have become more common as the primary treatment
of distal radial metaphyseal fractures in children and adolescents.88,136,177,238,244 The indications cited include fracture instability and high risk of loss of reduction,88,136,177 excessive local swelling that increases the risk of neurovascular compromise,238,239,246 ipsilateral fractures of the distal radius and elbow region (floating elbow) that increase the risk of compartment syndrome,210,245 and the likelihood that remanipulation will be required.244,246
In addition, surgeon’s preference for pinning in a busy office practice
has been considered an acceptable indication because of similar
complication rates and long-term outcomes with pinning and casting140,144 and the avoidance of remanipulation because alignment is secure.
fluoroscopic guidance. When possible, the physis is avoided. Adequate
exposure through a small incision over the radial styloid should be
obtained to avoid radial sensory nerve or extensor tendon injury.
Smooth Kirschner or C-wires are used. In younger patients, a single pin
with supplemental cast immobilization may be adequate fixation (Fig 9-50). Crossed pins are more stable provided they do not cross at the fracture site (Fig. 9-51).
The first pin, or single pin, enters from the radial side distal to the
fracture and passes obliquely to the ulnar aspect of the radius
proximal to the fracture. The second pin enters the radius distal to
the fracture between the fourth and fifth compartments and passes
obliquely across the fracture into the proximal radial side of the
radius. The pins are left out through
the
skin to allow easy removal. Another technique of pinning is intrafocal
placement of multiple pins into the fracture site to lever the distal
fragment into anatomic reduction (Kapandji technique, Fig. 9-52). The pins are then passed through the opposing cortex for stability.130,224
A supplemental, loose-fitting cast is applied. The advantage of pin
fixation is that a tight, well-molded cast is not necessary to maintain
reduction. This lessens the risk of neurovascular compromise with
associated excessive swelling or ipsilateral fractures. Obviously, pin
fixation avoids the risk of loss of reduction in an unstable fracture.
Pinning does have the risk of infection and concerns regarding growth
injury.
 |
|
FIGURE 9-50 Severe swelling. A,B. Complete displacement and bayonet apposition of a distal radial fracture associated severe swelling from a high-energy injury. C.
Once reduced, the fragment was secured with an oblique percutaneous pin across the fracture site, sparing the distal radial physis. |
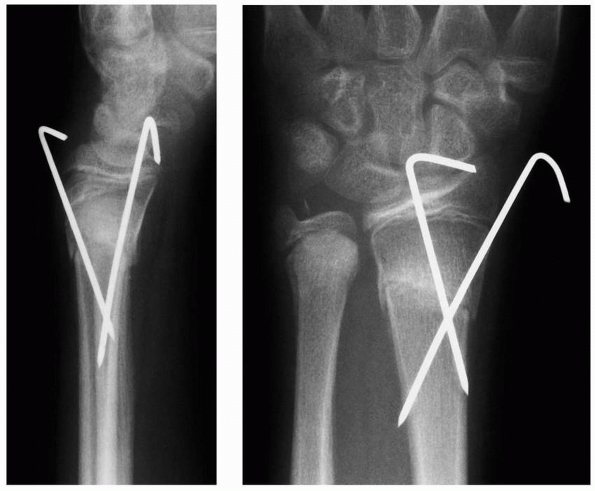 |
|
FIGURE 9-51 Crossed-pin technique for stabilization of distal radial metaphyseal fracture in a skeletally immature patient.
|
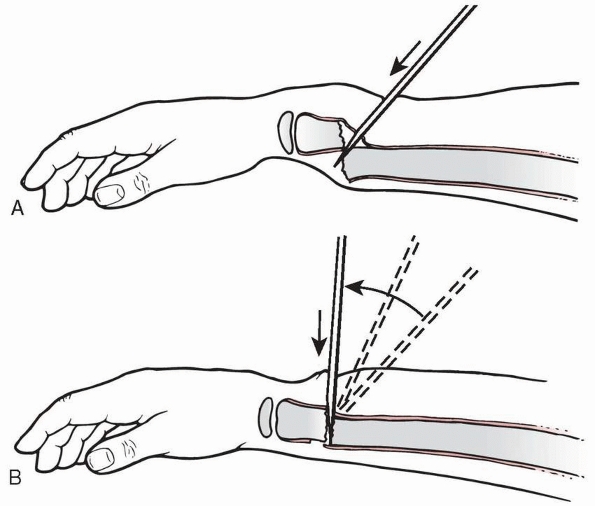 |
|
FIGURE 9-52 Pin leverage. A.
If a bayonet is irreducible, after sterile preparation, a chisel-point Steinmann pin can be inserted between the fracture fragments from a dorsal approach. Care must be taken not to penetrate too deeply past the dorsal cortex of the proximal fragment. B. Once the chisel is across the fracture site, it is levered into position and supplementary pressure is placed on the dorsum of the distal fragment (arrow) to slide it down the skid into place. This procedure is usually performed with an image intensifier. |
fixation rarely is indicated for similar fractures in skeletally
immature patients. Although it can be used successfully,201,232
the success rates of both closed reduction and percutaneous pinning
techniques make it unnecessary for uncomplicated distal radial
fractures in children. The best indication is severe associated soft
tissue injuries. A severe crush injury, open fracture, or replantation
after amputation that requires extensive soft tissue care and surgery
are all indications for the use of external fixation. Supplemental
external fixation also may be necessary for severely comminuted
fractures to maintain length and provide additional stability to pin
fixation. Standard application of the specific fixator chosen is done
with care to avoid injury to the adjacent sensory nerves and extensor
tendons.
fractures. Open fractures constitute approximately 1% of all distal
radial metaphyseal fractures. All open fractures, regardless of grade
of soft tissue injury, should be irrigated and débrided in the
operating room (Fig. 9-53). The open wound
should be enlarged adequately to débride the contaminated and nonviable
tissues and protect the adjacent neurovascular structures. After
thorough irrigation and débridement, the fracture should be
anatomically reduced and stabilized, usually with two smooth pins. If
the soft tissue injury is severe, supplemental external fixation allows
observation and treatment of the wound without jeopardizing the
fracture reduction. The original open wound should not be closed
primarily. Appropriate prophylactic antibiotics should be used
depending on the severity of the open fracture.
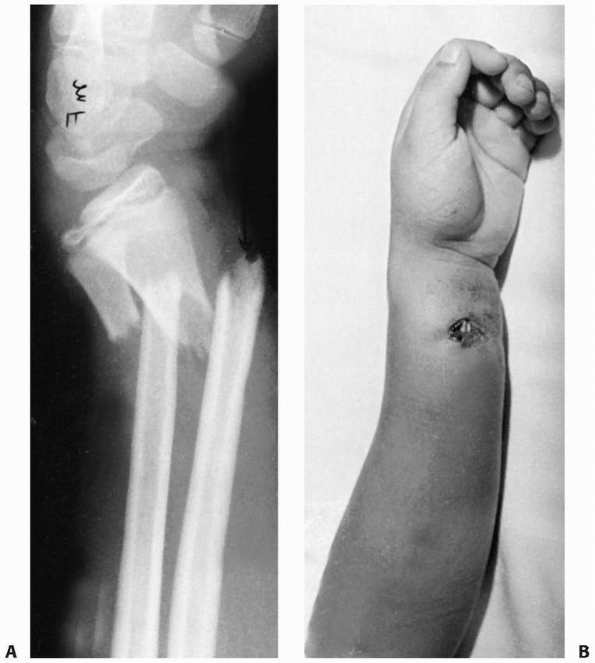 |
|
FIGURE 9-53 Open fractures. Radiograph (A) and clinical photo (B) of an open fracture of the distal radius. This patient needs formal irrigation and débridement in the operating room.
|
fractures, the interposed structure usually is the volar periosteum or pronator quadratus93
and rarely the flexor tendons or neurovascular structures. In volarly
displaced fractures, the periosteum or extensor tendons may be
interposed. The fracture should be approached in a standard fashion
opposite the side of displacement (i.e., volar approach for an
irreducible dorsal fracture). The adjacent neurovascular and tendinous
structures are protected and the offending soft tissue is extracted
from the fracture site. Pin stabilization is recommended to prevent
problems with postoperative swelling or loss of reduction in cast.
 |
|
FIGURE 9-54
A 10-year-old girl with a markedly displaced closed fracture of the distal radius with an angulated ulnar fracture. Note the wide separation between the radial fragments. Dimpling of the skin was noted when longitudinal traction was applied, and reduction was impossible. At open reduction, the proximal fragment was buttonholed through the forearm fascia and located between the median nerve and finger flexor tendons. The pronator quadratus muscle was also interposed between the two fragments. |
soft tissue. Occasionally, however, multiple attempts at reduction of a
bayonet apposition fracture can lead to significant swelling that makes
closed reduction impossible. If the patient is too old to remodel
bayonet apposition, open reduction is appropriate. Pin fixation without
violating the physis is recommended.
adolescents. Low profile, fragment specific fixation methods and
locking plates also are now commonly used for internal fixation of
distal radial fractures in adults. The utility of these anatomically
contoured locking plates in children and skeletally immature
adolescents is unknown, as is the deleterious effect, if any, on growth
potential. Furthermore, the advantage of these more rigid constructs in
younger patients in whom adequate stability may be achieved with pins
is unclear, particularly given the reports of late tendon rupture and
other soft tissue complications associated with fixed-angle volar
plates,36,112,180
Indications for skeletally mature adolescents are the same as for
adults. Articular malalignment and comminution are assessed by CT
preoperatively, and fracture-specific fixation is used as appropriate.
including torus and unicortical compression greenstick fractures, are
inherently stable. Immobilization is used until resolution of pain
(generally about 3 weeks). Depending on the activity level of the
patient, a volar wrist splint or a short-arm cast can be used.
Immobilization provides comfort from pain during healing and protects
against displacement with secondary injury. It is important that an
unstable bicortical fracture be recognized on radiograph. Bicortical
fractures need more protection, longer restriction of activity, and
closer follow-up to avoid displacement and malunion. A well-molded
short- or long-arm cast, depending on the age of the patient, is
applied and radiographs obtained every 7 to 10 days until evidence of
early healing is seen. A short-arm cast is then worn until clinical and
radiographic healing is complete. Any loss of reduction is treated with
repeat reduction. Return to contact sports is restricted until the
patient regains full motion and strength.
risk for redisplacement. If left unreduced or poorly immobilized, a
mild deformity can become severe during the course of healing.
Therefore, closed anatomic reduction is indicated in all bicortical
fractures with more than 10 degrees of malalignment. Generally, these
fractures have apex volar angulation and dorsal displacement. Conscious
sedation is used with portable fluoroscopy in the emergency care
setting. The distal fragment and hand are distracted and then reduced
volarly. With isolated distal radial fractures, it is imperative to
reduce the DRUJ with appropriate forearm rotation. For apex volar
fractures, this usually is with pronation. If the fracture is apex
dorsal with volar displacement, the reduction forces are the opposite.
A long-arm cast with three-point molding is used for 3 to 4 weeks.
Radiographs are obtained every 7 to 10 days until there is sufficient
callus formation. A short-arm cast or volar wrist splint is used until
full healing, generally at 4 to 6 weeks after fracture reduction. The
patient is then restricted from contact sports until full motion and
strength are regained, which may take up to 3 weeks after cast removal.
Formal therapy rarely is required. The patient and parents should be
warned at the start of treatment of the risk of redisplacement of the
fracture.
fractures usually results in foreshortening and dorsal overlap of the
distal fragment on the proximal fragment. This often is associated with
a same-level ulnar metaphyseal fracture, similarly in bayonet
apposition. Rarely, the distal fragment is in volar bayonet apposition.
Both of these situations require more skill of reduction and complete
analgesia at the fracture site. At our institution, we reduce this
fracture in the emergency room with conscious sedation and supplemental
local hematoma block or in the operating room with general anesthesia.
In either situation, portable fluoroscopy is used. The fracture usually
is reduced in the emergency room in young patients with minimal
swelling and no neurovascular compromise and in whom cast treatment
will be sufficient. Reduction with general anesthesia is preferred for
older patients and for those with marked displacement, swelling, or
associated neurovascular compromise in whom percutaneous pin treatment
is chosen.
anesthesia type or stabilization method. As opposed to a Colles
fracture in an adult, traction alone will not reduce the fracture
because the dorsal periosteum acts as a tension band that does not
respond to increasing linear traction with weights. Finger traps with
minimal weight (less than 10 lb) can be used to balance the hand and
help with rotational alignment (the “steel resident”) (see Fig. 9-14). However, applying progressive weight will only distract the carpus and will not alter the fracture alignment.
light-weight finger traps or hand traction, a hyperdorsiflexion
maneuver is performed. The initial deformity is accentuated and the
distal fragment is brought into marked dorsiflexion. The dorsum of the
hand should be brought more than 90 degrees and at times parallel to
the dorsum of the forearm to lessen the tension on the dorsal forearm.
Thumb pressure is used on the distal fragment while still in this
deformed position to restore length by bringing the distal fragment
beyond the proximal fragment. Reduction is then obtained by flexing the
distal fragment while maintaining length.
Often,
this initial reduction maneuver restores length and alignment, but
translational reduction is incomplete. The fracture should be
completely reduced by toggling the distal fragment all the way volarly
by repetitive slight dorsiflexion positioning of the distal fragment
followed by volar pressure with the thumbs. It is important to
anatomically reduce the fracture. Loss of reduction with cast
immobilization is more likely if the fracture remains translated or
malaligned.
the reduction is difficult, it is useful to try to lever the proximal
fragment distally with percutaneous smooth wire(s). This may prevent an
unnecessary open reduction. Percutaneous pin fixation is used after
reduction, either by standard pinning or intrafocal techniques.
prereduction signs or symptoms of neurovascular impairment, or has
minimal swelling, then cast immobilization is used. The cast is applied
with the aid either of an assistant or finger traps and balancing
counterweights on the upper arm. The advantage of the finger-trap steel
resident is that there is no risk of muscle fatigue, mental
distraction, or failure to maintain elbow flexion at 90 degrees that
can occur with a human assistant. A long-arm cast is applied with the
elbow flexed 90 degrees, the wrist in slight palmar flexion, and the
forearm in the desired rotation for stability and alignment. Rotational
positioning and short- versus long-arm casting varies with each
fracture and each surgeon. Our preference is neutral forearm rotation
unless the fracture dictates differently. This allows excellent molding
against the volar aspect of the distal radius at the fracture site.
casting for a forearm fracture is the application of the Webril
(Kendall, Mansfield, MA). The Webril should be applied in a continuous
roll with overlap of one third to one half its width. Extra padding is
applied over the olecranon when a long-arm cast is used, along the
volar and dorsal forearm where the cast may have to be split, and at
the ends of the cast to prevent irritation from fraying. Plaster of
Paris can be used for the cast to obtain the best mold possible.
Initially, a single layer is applied, followed by splints five layers
thick along the volar and dorsal forearm and the extension region of
the elbow. This lessens the bulk of the cast and still allows deep
molds. The cast is completed with plaster of Paris rolls over the
splints. A three-point mold is applied at the fracture site as the cast
hardens. In addition, molds are applied to maintain a straight ulnar
border, the interosseous space, and straight posterior humeral line.
This creates the classic “box” long-arm cast rather than the all too
frequent “banana” cast that allows displacement. Final radiographs are
obtained, and if the reduction is anatomic, the cast is overwrapped
with fiberglass to lessen the weight, increase patient satisfaction,
and prevent cast breakdown that could lead to loss of reduction.
hospital depending on the degree of concern regarding risk of excessive
swelling, neurovascular compromise, and patient and parental
reliability. If there is any doubt, the patient is admitted for
observation. The cast is split anytime there are signs of neurovascular
compromise or excessive swelling. The patient is instructed to maintain
elevation for at least 48 to 72 hours after discharge and return
immediately if excessive swelling or neurovascular compromise occurs.
The patient and family are warned of the risk of loss of reduction and
the need for close follow-up. We inform our patients and parents that
the risk of return to the day surgery unit for repeat reduction or
pinning is approximately 20% to 30% during the first 3 weeks.
every 7 to 10 days for 3 weeks. If there is loss of reduction, we
individualize treatment depending on the patient’s age, degree of
deformity, time since fracture, and remodeling potential. If
restoration of alignment with growth occurs, we reassure the family
that the child should achieve anatomic alignment over time with growth.
If the child is older, there is risk of further displacement, or the
deformity is marked, repeat reduction is done in the day surgery unit
with fluoroscopy. Most often, a percutaneous pin is used for the second
reduction (Fig. 9-55). Occasionally, in pure bending injuries, loss of reduction can be corrected with cast wedging.
molded cast is changed at 3 to 4 weeks. With clinical and radiograph
healing, a protective volar splint is used and activities are
restricted until the patient regains full motion and strength, usually
in 1 to 3 weeks after cast removal. As with other distal radial
fractures, formal physical therapy rarely is required.
fractures is most often used in patients with excessive swelling or
signs of neurologic injury. In these situations, the patient is at risk
for development of a forearm or carpal tunnel compartment syndrome with
a well-molded, tight-fitting cast. Similarly, concurrent displaced
supracondylar and distal radial fractures are treated with percutaneous
fixation of both fractures to lessen the risk of neurovascular
compromise (Fig. 9-56). Older patients near the
end of growth with bayonet apposition fractures also are treated with
percutaneous pin fixation because they have less ability to remodel and
their fractures are very unstable with a high risk of displacement.
Finally, open fractures usually are treated with pin fixation.
radial-sided pin or crossed radial- and ulnar-sided pins. Fixation of
the ulna rarely is necessary. Stability with a single pin is checked
with fluoroscopy, and if further fixation is needed, a second pin is
added. The physis is avoided if possible. Intrafocal pins are used if
reduction is not possible without levering the distal fragment into a
reduced position. A small incision is made for the insertion of each
pin to protect the radial sensory nerve and adjacent extensor tendons.
Smooth pins are used and are removed in the office as soon as there is
sufficient healing to make the fracture stable in a cast or splint
(usually at 4 weeks). Rehabilitation is similar to that for
cast-treated fractures.
an irreducible fracture. All open fractures are irrigated and débrided
in the operating room. The initial open wound is extended adequately to
inspect and cleanse the open fracture site. After thorough irrigation
and débridement, the fracture is reduced and stabilized. A cast rarely
is applied in this situation because of concern about fracture
stability, soft tissue care, and excessive swelling. Crossed-pin
fixation often is used with Gustilo grade 1 or 2 open fractures. More
severe soft tissue injuries usually require external fixation with a
unilateral frame, with care taken to avoid soft tissue impingement
during pin placement. If flap coverage is necessary for the soft tissue
wounds, the fixator pins should be placed in consultation with the
microvascular surgeon planning the soft tissue coverage.
 |
|
FIGURE 9-55 Remanipulation. A,B.
Two weeks after what initially appeared to be an undisplaced greenstick fracture, a 14-year-old boy was found to have developed late angulation of 30 degrees in both the coronal and sagittal planes. C. Because this was beyond the limits of remodeling, a remanipulation was performed. To prevent reangulation, the fracture was secured with a pin placed percutaneously obliquely through the dorsal cortex. |
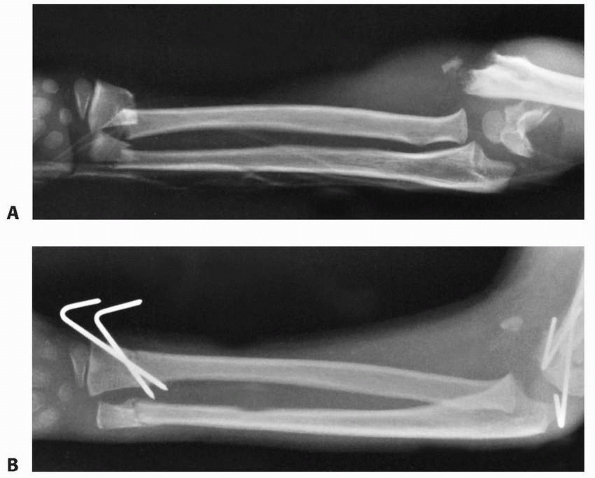 |
|
FIGURE 9-56 Ipsilateral fractures. A. Markedly displaced ipsilateral distal radial and supracondylar fractures. B.
Both fractures were reduced and stabilized with pins placed percutaneously. (Wilkins KE, ed. Operative Management of Upper Extremity Fractures in Children. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1994:29, with permission.) |
tissue entrapment. With dorsal displacement, this is most often either
the volar periosteum or pronator quadratus, and open reduction through
a volar approach is necessary to extract the interposed soft tissues
and reduce the fracture (Fig. 9-57).
Percutaneous pin fixation usually is used to stabilize the fracture in
patients with open physes. If plate fixation is used, it should avoid
violation of the physis (Fig. 9-58). Displaced
intra-articular injuries in skeletally immature adolescents are
adultlike and require standard treatment, such as open reduction and
internal fixation (Fig. 9-59). Lower profile and locking plates have been used more recently (Fig. 9-60).
similar to physeal fractures but with different frequencies. Loss of
reduction and malunion are the most common problems, and growth-related
complications are infrequent. Neurovascular compromise does occur and
should be considered in the acute management of this fracture.
this complication occurs in at least 30% of bayonet apposition fractures,80,136,177,234,244
many surgeons treat this fracture primarily with pin fixation to avoid
the problems that can occur with malunion. Otherwise, it is clear that
patients treated with cast immobilization need to be monitored closely.251
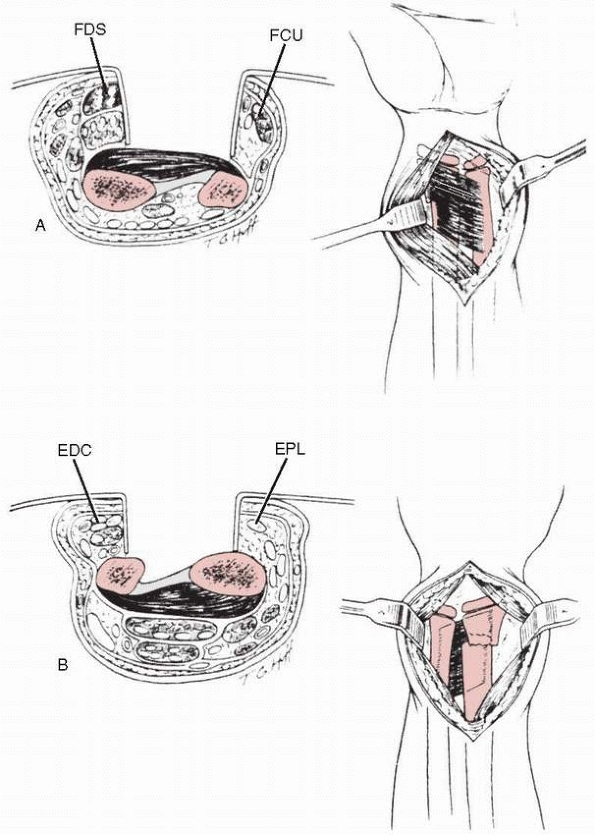 |
|
FIGURE 9-57 A.
Volar approach through the interval between the digital flexors and ulnar neurovascular bundle. FCU, flexor carpi ulnaris; FDS, flexor digitorum superficialis. B. Dorsal approach between the third and fourth dorsal compartments. EDC, extensor digitorum communis; EPL, extensor pollicis longus. (Reprinted from Holmes JR, Luis DS. Entrapment of pronator quadratus in pediatric distal-radius fractures: recognition and treatment. J Pediatr Orthop 1994, 14:498-500, with permission.) |
The younger the patient, the less the deformity, and the closer the
fracture is to the physis, the greater the potential for remodeling. It
is unclear whether there is any capacity for rotational malunion
remodeling.71,193
Angular and rotational malunion that does not remodel can lead to loss
of motion. The degree and plane of loss of motion, as well as the
individual affected, determine if this is functionally significant.251 In cadaver studies, malangulation of more than 20 degrees of the radius or ulna caused loss of forearm rotation,139,216,219
whereas less than 10 degrees of malangulation did not alter forearm
rotation significantly. Distal third malunion affected rotation less
than middle or proximal third malunion. Radioulnar malunion affected
forearm rotation more than volar-dorsal malunion. Excessive angulation
may lead to a loss of rotation at a 1:2 degree ratio, whereas
malrotation may lead to rotational loss at only a 1:1 degree loss.181
The functional loss associated with rotational motion loss is difficult
to predict. This has led some clinicians to recommend no treatment,38,40 arguing that most of these fractures will remodel, and those that do not remodel will not cause a functional problem.101 However, a significant functional problem is present if shoulder motion cannot compensate for loss of supination.
alignment as possible. No element of malrotation is accepted in the
reduction. As indicated in the treatment sections, fractures at high
risk of loss of reduction and malunion are treated with anatomic
reduction and pin or, rarely, plate fixation. Fractures treated in a
cast are followed closely and rereduced for any loss of alignment of
more than 10 degrees. Although loss of forearm rotation can occur with
anatomic healing,153,222,246 it is less likely than with malunions.
midcarpal instability217
and long-term arthrosis. A distal radial malunion in a skeletally
mature adolescent should be treated with an opening wedge osteotomy,
bone graft, and internal fixation (Fig. 9-61).62,142,178
 |
|
FIGURE 9-58 A. Radiograph of an open humeral diaphyseal fracture in the setting of a “floating elbow injury.” B. Radiograph depicting a displaced distal radial metaphyseal fracture. C. Plate fixation following irrigation and débridement of the humerus fracture. D,E. Radiographs following open reduction and plate fixation of the radius fracture, sparing the distal radial physis.
|
 |
|
FIGURE 9-59 A,B. AP and lateral radiographs of a 14-year-old skeletally mature female with a displaced extra-articular fracture. C,D.
This fracture was treated with a fixed-angle volar locking plate, with distal screws crossing the physis. The long-term effects of this type of fixation are unknown. |
 |
|
FIGURE 9-60 A. CT scan of a displaced intra-articular fracture of a nearly skeletally mature adolescent. B. Dorsal plating with a low profile system to achieve anatomic reduction and stable fixation.
|
In children, nonunion has been universally related to a pathologic
condition of the bone or vascularity.246 Congenital pseudarthrosis or neurofibromatosis (Fig. 9-62) should be suspected in a patient with a nonunion after a benign fracture.105
This occurs most often after an isolated ulnar fracture. The distal
bone is often narrowed, sclerotic, and plastically deformed. These
fractures rarely heal with immobilization. Vascularized fibular bone
grafting usually is necessary for healing of a nonunion associated with
neurofibromatosis or congenital pseudarthrosis. If the patient is very
young, this may include a vascularized epiphyseal transfer to restore
distal growth.
radial nonunion has been reported in a child with an ipsilateral
supracondylar fracture with brachial artery occlusion.
Revascularization of the limb led to eventual union of the fracture.
Nonunion also can occur with osteomyelitis and bone loss.22 Débridement of the necrotic bone and either traditional bone grafting, osteoclasis
lengthening, vascularized bone grafting, or creation of a single-bone
forearm are surgical options. The choice depends on the individual
patient.
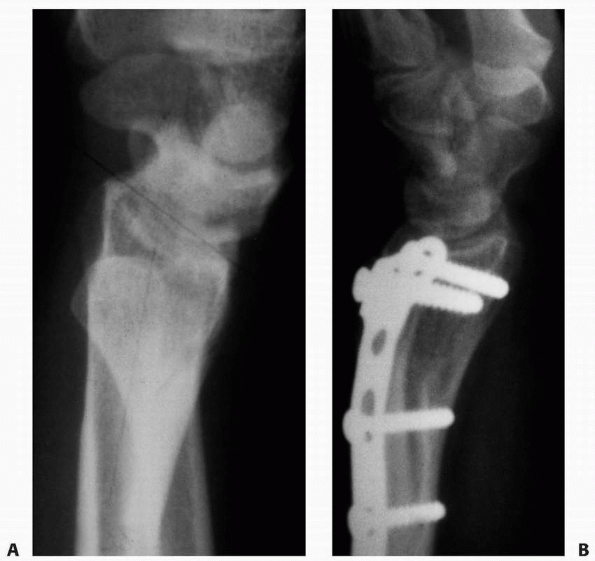 |
|
FIGURE 9-61 A. Radial metaphyseal fracture that did not remodel in a now 16-year-old skeletally mature boy. B. Corrective osteotomy with iliac crest bone graft and internal fixation was performed.
|
 |
|
FIGURE 9-62
This 3-year-old presented to the emergency room with pain after an acute fall on his arm. The ulna is clearly pathologic with thinning and deformity before this injury. This represents neurofibromatosis. |
radial and ulnar fractures. It has been described after high-energy
trauma and internal fixation.230 A single-pin crossing both bones increases the risk of cross-union.230
Synostosis take-down can be performed, but the results usually are less
than full restoration of motion. It is important to determine if there
is an element of rotational malunion with the cross-union because this
will affect the surgical outcome.
fractures are rare and much less common than after diaphyseal level
radial and ulnar fractures. Most commonly, refracture occurs with
premature discontinuation of immobilization or early return to
potentially traumatic activities. It is advisable to protectively
immobilize the wrist until full radiograph and clinical healing
(usually 6 weeks) and to restrict activities until full motion and
strength are regained (usually an additional 1 to 6 weeks). Individuals
involved in high-risk activities, such as downhill ski racing,
snowboarding, or skateboarding, should be protected with a splint
during those activities for much longer.
each reported one patient with physeal arrest after nondisplaced torus
fractures. Two additional patients were reported in a series of 150
distal radial metaphyseal fractures.63 Wilkins and O’Brien246
proposed that these arrests may be in fractures that extend from the
metaphysis to the physis. This coincides with a Peterson type I
fracture (Fig. 9-63)169,170 and in essence is a physeal fracture. These fractures should be monitored for growth arrest.
The average difference in growth was 3 mm, with a range of -5 to +10 mm
of growth disturbance compared with the contralateral radius. Maximal
overgrowth occurred in the 9- to 12-year-old age group. As long as the
patient is asymptomatic, under- or overgrowth is not a problem. If
ulnocarpal impaction or DRUJ disruption occurs, then surgical
rebalancing of the radius and ulna may be necessary.
nerves are less commonly injured in metaphyseal fractures than in
physeal fractures. The mechanisms of neural injury in a metaphyseal
fracture include direct contusion from the displaced fragment, traction
ischemia from tenting of the nerve over the proximal fragment,11,165 entrapment of the nerve in the fracture site,8,247 rare laceration of the nerve (Fig. 9-64),
and the development of an acute compartment syndrome. If signs or
symptoms of neuropathy are present, a prompt closed reduction should be
performed. Extreme
positions
of immobilization should be avoided because this can lead to persistent
traction or compression ischemia and increase the risk of compartment
syndrome. If there is marked swelling, it is better to percutaneously
pin the fracture than to apply a constrictive cast. If there is concern
about compartment syndrome, the forearm and carpal canal pressures
should be measured immediately. If pressures are markedly elevated,
appropriate fasciotomies and compartment releases should be performed
immediately. Finally, if the nerve was intact before reduction and is
out after reduction, neural entrapment should be considered, and
surgical exploration and decompression may be required. Fortunately,
most median and ulnar nerve injuries recover after anatomic reduction
of the fracture.
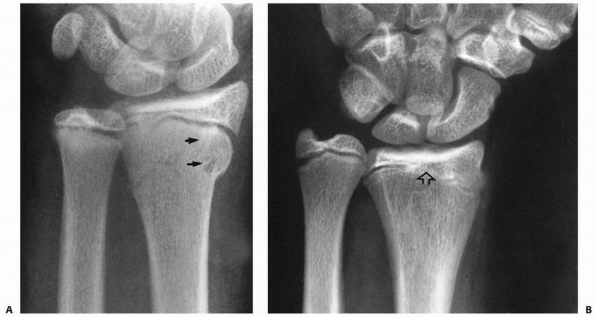 |
|
FIGURE 9-63 Physeal arrest in a Peterson type I fracture. A. Injury film showing what appears to be a benign metaphyseal fracture. Fracture line extends into the physis (arrows). B. Two years postinjury, a central arrest (open arrow)
has developed, with resultant shortening of the radius. (Reprinted from Wilkins KE, ed. Operative Management of Upper Extremity Fractures in Children. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1994:21, with permission.) |
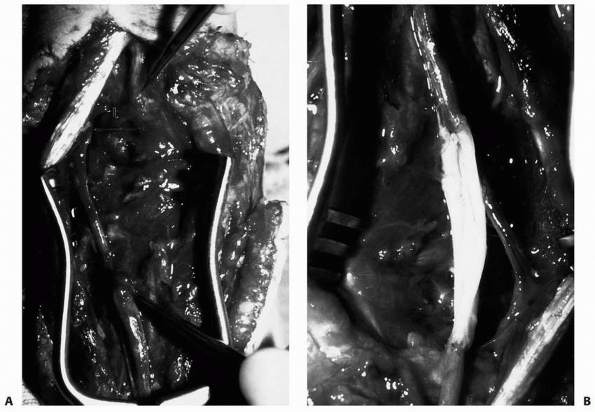 |
|
FIGURE 9-64
A grade III open fracture of the radius resulted in complete disruption of the ulnar nerve. Intraoperative photographs of the nerve deficit between the operative jeweler’s forceps (A) and sural nerve grafting (B) after the wound was clean enough to allow for nerve reconstruction. |
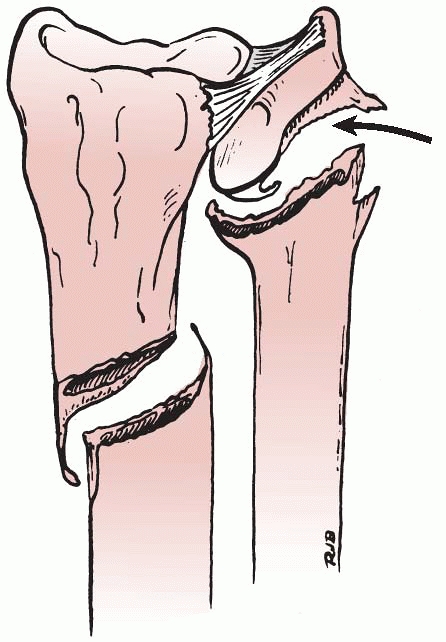 |
|
FIGURE 9-65 Galeazzi fracture-dislocation variant. Interposed periosteum can block reduction of the distal ulnar physis (arrow).
This destabilizes the distal radial metaphyseal fracture. (Reprinted from Lanfried MJ, Stenclik M, Susi JG. Variant of Galeazzi fracture-dislocation in children. J Pediatr Orthop 1991;11:333, with permission.) |
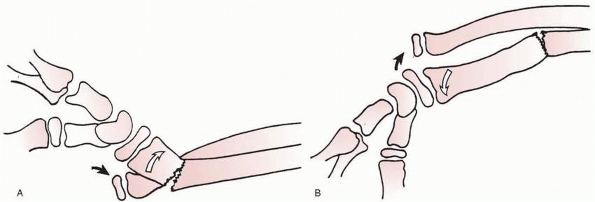 |
|
FIGURE 9-66 Walsh classification. A. The most common pattern, in which there is dorsal displacement with supination of the distal radius (open arrow). The distal ulna (black arrow) lies volar to the dorsally displaced distal radius. B. The least common pronation pattern. There is volar or anterior displacement of the distal radius (open arrow), and the distal ulna lies dorsal (black arrow).
(Reprinted from Walsh HPJ, McLaren CANP. Galeazzi fractures in children. J Bone Joint Surg Br 1987;69:730-733, with permission.) |
described the development of gas gangrene in four children after minor
puncture wounds or lacerations associated with distal radial fractures.
Treatment involved only local cleansing of the wound in all four and
wound closure in one. All four developed life-threatening clostridial
infections. Three of the four required upper limb amputations, and the
fourth underwent multiple soft tissue and bony procedures for coverage
and treatment of osteomyelitis.
rare. Superficial pin site infections can occur and should be treated
with pin removal and antibiotics. Deep-space infection from
percutaneous pinning of the radius has not been described.
disruption have been called Galeazzi fracture-dislocations. Although
Sir Ashley Cooper is credited with the first description of this injury
in 1824, Riccardo Galeazzi72,183
gave this fracture-dislocation its name with his 1934 report of 18 such
injuries. In children, this injury may involve either disruption of the
DRUJ ligaments or, more commonly, a distal ulnar physeal fracture (Fig. 9-65).1,15,117,127,182,183 Galeazzi fracture-dislocations are relatively rare injuries in children. Walsh and McLaren233 cited an occurrence of 3% of pediatric distal radial fractures in their study. Eberl et al.50
reported 26 cases in a series of 198 forearm fractures (13%). Most
series of Galeazzi fractures contain a relatively small number of
pediatric patients.127,143,170,233
In adults, the mechanism of injury usually is an axially loading fall
with hyperpronation. This results in a distal radial fracture with a
dorsal
ulnar dislocation. However, in children, both supination (apex volar)
and pronation (apex dorsal) deforming forces have been described.126,182,233
The mechanism of injury is most obvious when the radial fracture is an
incomplete fracture. With an apex volar (supination) radial fracture,
the distal ulna is displaced volarly, whereas with an apex dorsal
(pronation) radial fracture, the distal ulna is displaced dorsally (Fig. 9-67).
This is evident both on clinical and radiographic examinations. In
addition, the radius is foreshortened in a complete fracture, causing
more radial deviation of the hand and wrist (Fig. 9-68).
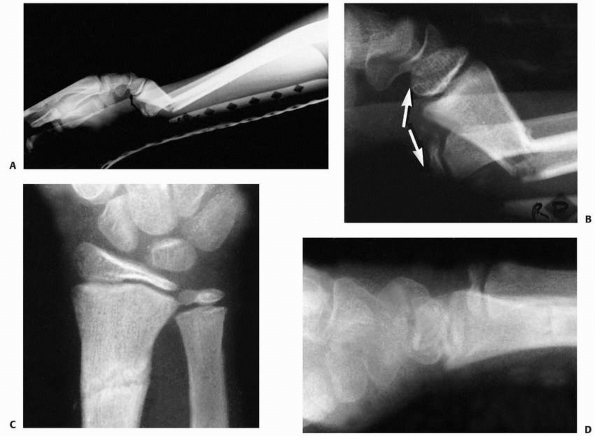 |
|
FIGURE 9-67 Supination-type Galeazzi fracture. A. View of the entire forearm of an 11-year-old boy with a Galeazzi fracture-dislocation. B. Close-up of the distal forearm shows that there has been disruption of the distal radioulnar joint (arrows).
The distal radial fragment is dorsally displaced (apex volar), making this a supination type of mechanism. Note that the distal ulna is volar to the distal radius. C,D. The fracture was reduced by pronating the distal fragment. Because the distal radius was partially intact by its greenstick nature, the length was easily maintained, re-establishing the congruity of the distal radioulnar joint. The patient was immobilized in supination for 6 weeks, after which full forearm rotation and function returned. |
of forearm rotation and wrist flexion and extension. Neurovascular
impairment is rare. The radial deformity usually is clinically evident.
The DRUJ disruption may be obvious by the prominence of the ulnar head.
A subtle ligament disruption may be evident only by local tenderness
and instability to testing on the DRUJ.
concurrent injuries to the ulna or DRUJ should be identified. A true
lateral view is necessary to identify the direction of displacement,
which is imperative to determine the method of reduction. Rarely are
special radiographs, such as a CT scan, necessary.
described by direction of displacement of either the distal ulnar
dislocation or the radial fracture. Letts126,127 preferred to describe the direction of the ulna: volar or dorsal. Walsh and McLaren233
classified pediatric Galeazzi injuries by the direction of displacement
of the distal radial fracture. Dorsal displacement (apex volar)
fractures were more common than volar displacement (apex dorsal)
fractures in their series. Wilkins and O’Brien246
modified the Walsh and McLaren method by classifying radial fractures
as incomplete and complete fractures and ulnar injuries as true
dislocations and physeal fractures (Table 9-4). DRUJ dislocations are called true Galeazzi lesions and distal ulnar physeal fractures are called Galeazzi equivalent lesions.94,117,126,127
stationary ulna. The two bones of the forearm articulate at the
proximal
and
distal radioulnar joints. In addition, proximally the radius and ulna
articulate with the distal humerus and distally with the carpus. These
articulations are necessary for forearm pronation and supination. At
the DRUJ, the concave sigmoid notch of the radius incompletely matches
the convex, asymmetric, semicylindrical shape of the distal ulnar head.18
This allows some translation at the DRUJ with rotatory movements. The
ligamentous structures are critical in stabilizing the radius as it
rotates about the ulna (Fig. 9-69).
 |
|
FIGURE 9-68 Pronation Galeazzi. This 8-year-old sustained a pronation Galeazzi fracture. A. The AP view shows some shortening of the distal radius (arrow) in relation to the distal ulna, which has a small greenstick component. B. The pronation component (arrow) is better appreciated on this lateral view. The distal ulna lies dorsal to the distal radius (open arrow).
|
|
TABLE 9-4 Classification: Galeazzi Fractures in Children
|
||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||
most important of which is the TFCC. The TFCC includes the volar and
dorsal ligamentous attachments of the distal ulna to the radial sigmoid
notch, as well as the distal extension to the ulnar styloid, carpus,
and base of the fifth metacarpal. The volar ulnocarpal ligaments (V
ligament) from the ulna to the lunate and triquetrum are important
ulnocarpal stabilizers.18,200,242 The central portion of the TFCC is the articular disk (Fig. 9-70).
The interaction between the bony articulation and the soft tissue
attachments accounts for stability of the DRUJ during pronation and
supination. At the extremes of rotation, the joint is most stable. The
compression loads between the radius and ulna are aided by the tensile
loads of the TFCC to maintain stability throughout rotation.
connects the radius to the ulna. It passes obliquely from the proximal
radius to the distal ulna. However, the interosseous ligament is not
present in the distal radius. Moore et al.149
found that injuries to the TFCC and interosseous ligament were
responsible for progressive shortening of the radius with fracture in a
cadaveric study. The soft tissue component to the injury is a major
factor in the deformity and instability in a Galeazzi
fracture-dislocation.
adults, it is imperative to anatomically reduce and internally fix the distal radial fracture.115,143,147,148,182
Generally, the DRUJ is reduced with reduction and fixation of the
radius. In pediatric patients, the distal radial fracture often is a
greenstick type that is stable after reduction; cast immobilization is
sufficient.143,233 Adolescents with complete fractures should be treated with internal fixation similar to adults.
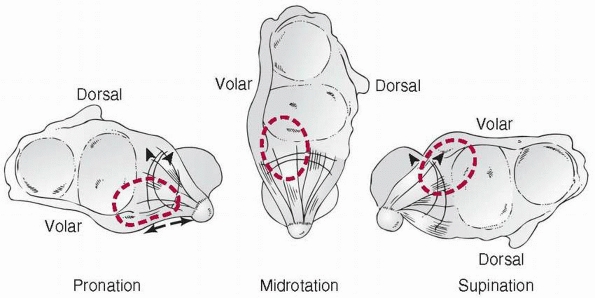 |
|
FIGURE 9-69 Distal radioulnar joint stability in pronation (left) is dependent on (a) tension developed in the volar margin of the triangular fibrocartilage (TFCC, small arrows)
and (b) compression between the contact areas of the radius and ulna (volar surface of ulnar articular head and dorsal margin of the sigmoid notch, large arrows). Disruption of the volar TFCC would therefore allow dorsal displacement of the ulna in pronation. The reverse is true in supination, where disruption of the dorsal margin of the TFCC would allow volar displacement of the ulna relative to the radius as this rotational extreme is reached. The dark area of the TFCC emphasizes the portion of the TFCC that is not supported by the ulnar dome. The dotted circle is the arc of load transmission (lunate to TFCC) in that position. (Redrawn from Bowers WH. Green’s Operative Hand Surgery. New York: Churchill-Livingstone, 1993.) |
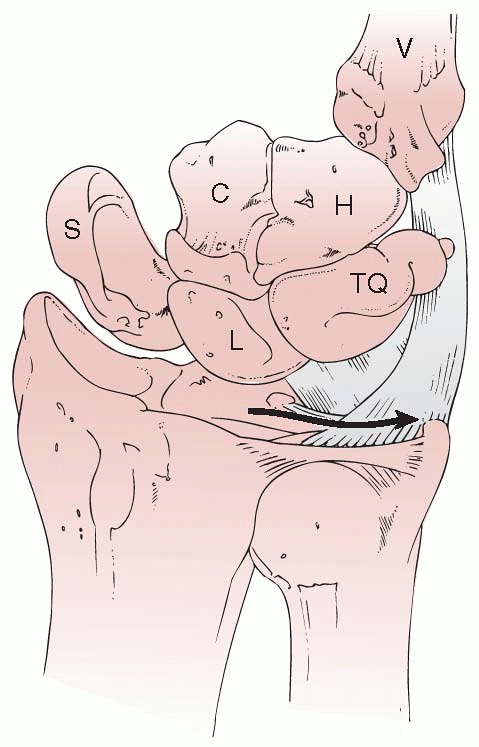 |
|
FIGURE 9-70
Diagrammatic drawing of the TFCC and the prestyloid recess. The meniscal reflection runs from the dorsoulnar radius to the ulnovolar carpus. The arrow denotes access under the reflection to the tip of the styloid—the so-called prestyloid recess. (Redrawn from Bowers WH. Green’s Operative Hand Surgery. New York: Churchill-Livingstone, 1993.) |
depends on the type of displacement. With apex volar dorsally displaced
fractures of the radius, the rotatory deformity is supination.
Pronating the radius and applying a dorsal-to-volar reduction force
should align the fracture and reduce the DRUJ. Similarly, if the
incomplete radial fracture is an apex dorsal volar displaced fracture,
the rotatory deformity is pronation. Supinating the forearm and
applying a volar-to-dorsal force should reduce the incomplete fracture
of the radius and the DRUJ dislocation.126,127,144,246
In both these situations, portable fluoroscopy can be used to evaluate
the fracture-dislocation reduction and to test the stability of the
distal ulna. If anatomically reduced and stable, a long-arm cast is
applied with appropriate rotation and three-point molds. The cast is
left in place for 6 weeks to allow the soft tissue injuries to heal.
and an ulnar physeal fracture, both bones should be reduced. Usually,
this can be accomplished with the same methods of reduction as when the
radial fracture is incomplete. The distal ulnar physis can remodel a
nonanatomic reduction if there is sufficient growth remaining and the
ulnar physis continues to grow normally. Unfortunately, the risk of
ulnar growth arrest after a Galeazzi equivalent has been reported to be
as high as 55%.81
rate of loss of reduction after closed treatment than do incomplete
fractures (Fig. 9-71).246
If not monitored closely and rereduced if necessary, loss of reduction
can lead to malunion with loss of motion and function. These injuries
may be best treated with open reduction as in adults.
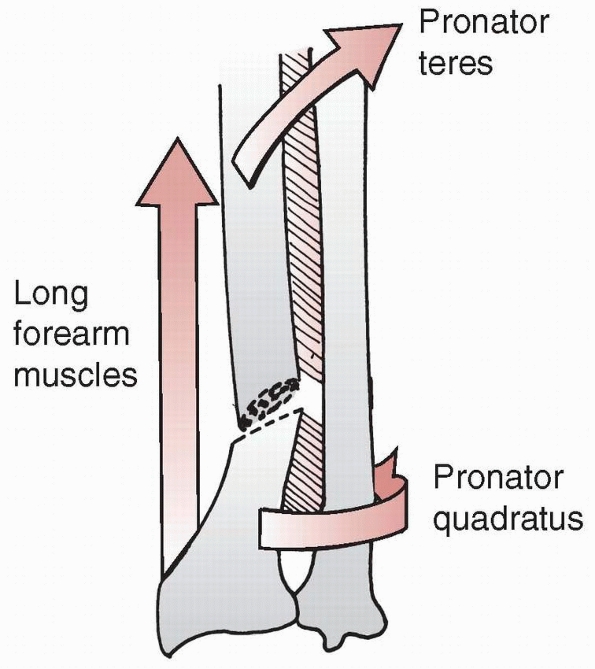 |
|
FIGURE 9-71
Fractures of the distal radius are angulated toward the ulna due to the pull of the long forearm muscles and the pronator quadratus. (Redrawn from Cruess RL. The management of forearm injuries. Orthop Clin North Am 1973;4:969-982, with permission.) |
is failure to obtain or maintain fracture reduction. This most often
occurs with unstable complete fractures. Open reduction and internal
fixation of the radius are done through an anterior approach. Standard
compression plating is preferred to intramedullary or cross-pinning
techniques (Fig. 9-72). Stable, anatomic
reduction of the radius almost always leads to stable reduction of the
DRUJ dislocation. A long-arm cast is used for 6 weeks to allow fracture
and soft tissue healing.
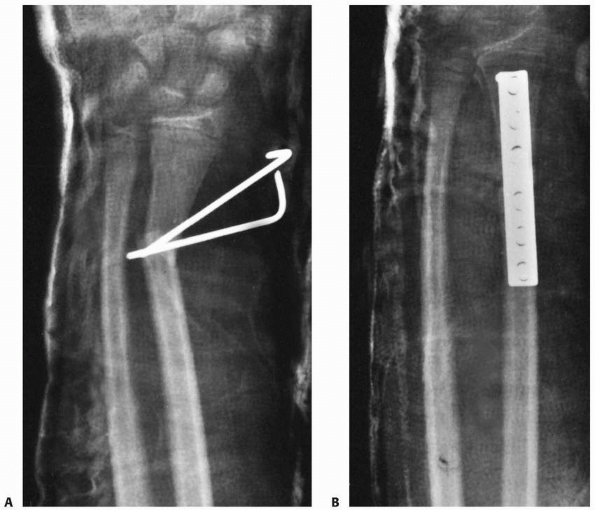 |
|
FIGURE 9-72 A. The patient with the pronation injury shown in Figure 9-68
had a closed reduction and attempted fixation with pins placed percutaneously across the fracture site. However, this was inadequate in maintaining the alignment and length of the fracture of the distal radius. B. The length of the radius and the distal radioulnar relationship were best re-established after internal fixation of the distal radius with a plate placed on the volar surface. The true amount of shortening present on the original injury film (see Fig. 9-68A) is not really appreciated until the fracture of the distal radius is fully reduced. (Reprinted from Wilkins KE, ed. Operative Management of Upper Extremity Fractures in Children. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1994:34, with permission.) |
because of interposed soft tissues, most commonly the periosteum,
extensor tendons (extensor carpi ulnaris, extensor digit quinti), TFCC,
or other ligamentous structures.14,26,100,127
The easiest approach for open reduction of the DRUJ is an extended
ulnar approach. Care should be taken to avoid injury to the ulnar
sensory nerve. This approach allows exposure both volarly and dorsally
to extract the interposed soft tissues and repair the torn structures.
Alternatively, a Bowers approach to the distal radioulnar joint may be
used, providing the advantage of more direct visualization and
extraction of interposed soft tissues in irreducible cases. Smooth pin
fixation of the DRUJ can be used to maintain reduction and allow
application of a loose-fitting cast. The pin is removed in the office
at 4 weeks with continuation of the cast for 6 weeks.
in a Galeazzi equivalent injury. This also has been reported to be
secondary to interposed periosteum,117,182 extensor tendons,160 or joint capsule.53 Open reduction must be executed with care to avoid further violating the physis.
true dislocation of the DRUJ or an ulnar physeal fracture are treated
with closed reduction and long-arm cast immobilization. This can be
done in the emergency room with conscious sedation or in the operating
room with general anesthesia. Portable fluoroscopy is used. If the
fracture is apex volar with dorsal displacement of the radius and volar
dislocation of the DRUJ, then
pronation
and volar-to-dorsal force on the radial fracture is used for reduction.
If the fracture is apex dorsal with volar displacement of the radius
and dorsal dislocation of the DRUJ, then supination and dorsal-to-volar
force is applied to the distal radius for reduction. The reduction and
stability of the fracture and DRUJ dislocation are checked on dynamic
fluoroscopy before long-arm cast immobilization. If both are
anatomically reduced and stable, the cast is used for 6 weeks to allow
soft tissue and fracture healing. In a Galeazzi equivalent injury,
there is potential for remodeling of the physeal fracture if sufficient
growth remains. As long as the DRUJ is reduced, malalignment of less
than 10 degrees can remodel in a young child. The risk of physeal
growth arrest is high with this physeal injury, and operative exposure
may increase the risk of growth impairment. If the fracture is severely
malaligned, the DRUJ cannot be reduced, or the patient is older and
remodeling is unlikely, open reduction and smooth pin fixation are
indicated.246
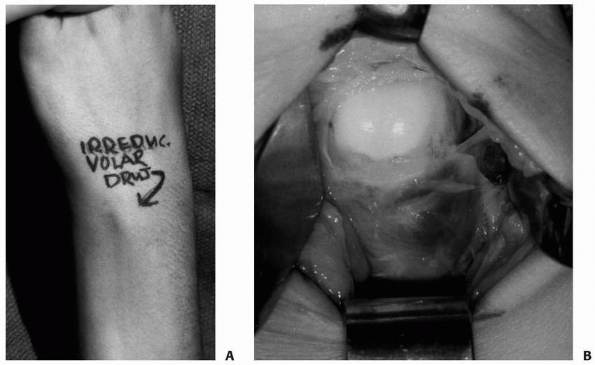 |
|
FIGURE 9-73 An adolescent girl presented 4 weeks after injury with a painful, stiff wrist. A.
By examination, she was noted to have a volar distal radioulnar dislocation that was irreducible even under general anesthesia. B. At the time of surgery, the distal ulna was found to have buttonholed out of the capsule, and there was entrapped triangular fibrocartilage and periosteum in the joint. |
plate and screws are used for complete Galeazzi fractures of the
radius. The DRUJ usually reduces anatomically and is stable with
reduction and fixation of the radius. The patient is immobilized in a
long-arm cast for 4 weeks and a short-arm cast for 2 more weeks. Return
to unrestricted activities and sports depends on restoration of full
motion and strength.
reduction. Extensile exposure is necessary to define the pathologic
anatomy and carefully reduce the DRUJ. The interposed soft tissues are
extracted and repaired. Depending on the stability of the reduction and
repair, a supplemental smooth pin may be used across the DRUJ for 4
weeks to maintain the joint reduction. This is particularly true if the
patient presents late.
DRUJ, limited forearm rotation, and pain, usually secondary to
persistent shortening and malrotation of the radial fracture. Most
often, this occurs when complete fractures are treated with closed
reduction and there is failure to either obtain or maintain reduction
of the radial fracture. The ulna remains subluxed and heals with an
incongruent joint. Treatment of this requires proper recognition and
corrective osteotomy. If physical examination is not definitive for
diagnosis, then a CT scan in pronation, neutral rotation, or supination
may be helpful. MRI or wrist arthroscopy will aid in the diagnosis and
management of associated ligamentous, chondral, or TFCC injuries that
will benefit from débridement or repair. It is important to understand
that if the DRUJ subluxation is caused by a radial malunion, a soft
tissue reconstruction of the DRUJ alone will fail.18
In the true soft tissue disruption, repair of the TFCC will often
stabilize the DRUJ. If there is no TFCC tear, soft tissue
reconstruction of the DRUJ ligaments with extensor retinaculum or local
tendon is appropriate.
ulnar physeal arrest in 55% of Galeazzi equivalent fractures. If the
patient is young enough, this ulnar growth arrest in the presence of
ongoing radial growth will lead to deformity. Initially, there will be
ulnar shortening. Over time, the foreshortened ulna can act as a
tether, causing asymmetric growth of the radius. There will be
increased radial articular inclination on the AP radiograph and
subluxation of the DRUJ. Operative choices include ulnar lengthening,
radial closing wedge osteotomy, radial epiphysiodesis, and a
combination of the above procedures that is appropriate for the
individual patient’s age, deformity, and disability.
described an 8% rate of injury to the radial nerve with operative
exposure of the radius for internal fixation in their series. Careful
surgical exposure, dissection, and retraction can decrease this risk.
A, Accadbled F, Kany J, et al. Ulnar styloid fracture in children: a
retrospective study of 46 cases. J Pediatr Orthop B 2008;17:15-19.
LJ, Thompson GH. Deformity after premature closure of the distal radial
physis following a torus fracture with a physeal compression injury.
Report of a case. J Bone Joint Surg Am 1987;69:1450-1453.
SA, Palmer AK, Kerr DR, et al. Wrist pain and distal growthplate
closure of the radius in gymnasts. J Pediatr Orthop 1989;9:23-28.
KB, Iltar S, Cimen O, et al. Risk factors in redisplacement of distal
radial fractures in children. J Bone Joint Surg Am 2008;90:1224-1230.
P, Joughlin J, Clarke H. Pediatric fractures of the forearm, wrist, and
hand in skeletal trauma in children. In: Green N, Swiontkowski M, eds.
Skeletal Trauma in Children. Philadelphia: WB Saunders, 1994:161-257.
DA, Wedge JH, McCulloch RG, et al. Epidemiology of fractures of the
distal end of the radius in children as associated with growth. J Bone
Joint Surg Am 1989; 71:1225-1231.
MP, Dalldorf PG, Marquardt JD. Skateboard and in-line skate fractures:
a report of one summer’s experience. J Orthop Trauma 1992;6:301-305.
A. Ipsilateral Monteggia equivalent injury and distal radial and ulnar
fracture in a child. J Orthop Trauma 1994;8:431-433.
ER, Bubbar V, Yong Hing K, et al. Above and below-the-elbow plaster
casts for distal forearm fractures in children. A randomized controlled
trial. J Bone Joint Surg Am 2006;88:1-8.
W. The distal radioulnar joint. In: Green D, Hotchkiss R, Pederson W,
ed. Green’s Operative Hand Surgery. New York: Churchill-Livingstone,
1999:986-1032.
KT, Brownson P, Hunter JB. Distal radial fractures in young
goalkeepers: a case for an appropriately sized soccer ball. Br J Sports
Med 2001;35:409-411.
EM, Peterson HA. Partial premature closure of the distal radial physis
associated with Kirschner wire fixation. Orthopedics 1991;14:585-588.
BA, Overton B, Schrader W, et al. Position of immobilization for
pediatric forearm fractures. J Pediatr Orthop 2002;22:185-187.
D, Roy S, Singer KM, et al. Stress changes of the distal radial growth
plate. A radiographic survey and review of the literature. Am J Sports
Med 1992;20:290-298.
G, DeMaio F, Mancini F, et al. Physeal fractures of the distal radius
and ulna: long-term prognosis. J Orthop Trauma 2003; 17:172-179.
C, Williams P. Management of completely displaced metaphyseal fractures
of the distal radius in children. J Bone Joint Surg Br 2003;85:933.
JC, Shen WY. Limb fracture pattern in different pediatric age groups: a
study of 3350 children. J Orthop Trauma 1993;7(1):15-22.
DG, Hyndman JC, Leahey JL, et al. Short-arm plaster cast for distal
pediatric forearm fractures. J Pediatr Orthop 1994;14:211-213.
AC, Spencer RF. Ulnar nerve palsy following fractures of the distal
radius: clinical and anatomical studies. J Hand Surg Br 1991;16:438-440.
JP. Transcarpal injuries associated with distal radial fractures in
children: a series of three cases. J Hand Surg Br 1992;17:311-314.
C, Zaleske DJ, Ehrlich MG. Analyzing forearm fractures in children. The
more subtle signs of impending problems. Clin Orthop Relat Res
1984;188:40-53.
AW, Schmidt CC. Flexor tendon injuries following locked volar plating
of distal radius fractures. J Hand Surg Am 2008;33:164-167.
JS. A study of radioulnar movements following fractures of the forearm
in children. Clin Orthop Relat Res 1979;139:114-120.
JS, Brown DJ, Barnes SN, et al. Simple treatment for torus fractures of
the distal radius. J Bone Joint Surg Br 2001;83:1173-1175.
Courtivron B. Spontaneous correction of the distal forearm fractures in
children. Presented at the European Pediatric Orthopaedic Society
Annual Meeting; Brussels, Belgium, 1995.
Pablos J, Franzreb M, Barrios C. Longitudinal growth pattern of the
radius after forearm fractures conservatively treated in children. J
Pediatr Orthop 1994;14: 492-495.
Smet L, Claessens A, Lefevre J, et al. Gymnast wrist: an epidemiologic
survey of ulnar variance and stress changes of the radial physis in
elite female gymnasts. Am J Sports Med 1994;22:846-850.
JP, Puffer JC, Aish B, et al. Wrist pain, distal radial physeal injury,
and ulnar variance in young gymnasts: does a relationship exist? Am J
Sports Med 2002;30: 879-885.
TT, Strub WM, Foad SL, et al. Reduction versus remodeling in pediatric
distal forearm fractures: a preliminary cost analysis. J Pediatr Orthop
Br 2003;12:109-115.
K, Hattori Y, Otsuka K, et al. Intra-articular fractures of the distal
aspect of the radius: arthroscopically assisted reduction compared with
open reduction and internal fixation. J Bone Joint Surg Am
1999;81:1093-1110.
BE, Waters PW, Wyzokowski RJ. Arthroscopic treatment of partial
scapholunate tears in children with chronic wrist pain. J Bone Joint
Surg Am 2006;88(11): 2448-2455.
WD, Keene JS. Irreducible fracture-separation of the distal ulnar
epiphysis. Report of a case. J Bone Joint Surg Am 1985;67:1130-1132.
RA, Bowers WH, Guilford WB. Ulnar variance—the effect of wrist
positioning and roentgen filming technique. J Hand Surg Am
1982;7:298-305.
DL, Stauber M, Frykman GK. Irreducible epiphyseal plate fracture of the
distal ulna due to interposition of the extensor carpi ulnaris tendon.
A case report. 1990; 251:162-165.
JF, Mosher JF. An unusual complication of fracture of both bones of the
forearm in a child. A case report. J Bone Joint Surg Am 1986;68:451-453.
RA, Davison KS, Bailey DA, et al. Size-corrected BMD decreases during
peak linear growth: implications for fracture incidence during
adolescence. J Bone Miner Res 2006;21(12):1864-1870.
NF, Dobranski A, Bisla RS. Gas gangrene complicating open forearm
fractures. Report of five cases. J Bone Joint Surg Am 1977;59:135-138.
DL, Palmer AK. Fractures of the distal radius. In: Green D, Hotchkiss
R, Pederson W, eds. Green’s Operative Hand Surgery. New York:
Churchill-Livingstone, 1999:929-985.
DL. Conservative treatment of forearm fractures in children. In:
Chapchal G, ed. Fractures in Children. New York: Thieme-Stratton, 1981.
DL. Correction of posttraumatic wrist deformity in adults by osteotomy,
bone-grafting, and internal fixation. J Bone Joint Surg Am
1982;64;1164-1178.
DI. A study of wrist injuries in children: the incidence of various
injuries and of premature closure of the distal radial growth plate.
Arch Emerg Med 1992;9:9-13.
DP, Davis TRC, Sithole JS. Do young patients with malunited fractures
of the distal radius inevitably develop symptomatic posttraumatic
osteoarthritis? J Bone Joint Surg Br 2008;90:629-637.
JV, Kassab MT. Displaced supracondylar fractures of the elbow in
children. A report on the fixation of extension and flexion fractures
by two lateral percutaneous pins. J Bone Joint Surg Br 1974;56B:490-500.
KS. Remodelling after distal forearm fractures in children. I. The
effect of residual angulation on the spatial orientation of the
epiphyseal plates. Acta Orthop Scand 1979;50:537-546.
KS. Remodelling after distal forearm fractures in children. II. The
final orientation of the distal and proximal epiphyseal plates of the
radius. Acta Orthop Scand 1979;50:731-739.
KS. Remodelling after distal forearm fractures in children. III.
Correction of residual angulation in fractures of the radius. Acta
Orthop Scand 1979;50:741-749.
AK, Fischer J, Waseem M. Management of completely displaced metaphyseal
fractures of the distal radius in children. J Bone Joint Surg Br
2003;85:463.
RK, Wilson P, Mason Brown JJ, et al. Spontaneous correction of
deformity following fractures of the forearm in children. Br J Surg
1962;50:5-10.
SM, Rohmann CG, Silverman FN. Radiographic standards for postnatal
ossification and tooth calcification. Med Radiogr Photogr 1967;43:45-66.
W, Freeland A, Weiss AP, et al. Techniques of wrist arthroscopy.
Instructional course lecture. J Bone Joint Surg Am 1999;81:1184-1197.
RH. Acute carpal tunnel syndrome. In: Gelbern AN, ed. Operative Nerve
Repair and Reconstruction. Philadelphia: JB Lippincott, 1991:937-948.
CL, Woods DA, Pailthorpe C, et al. The management of isolated distal
radius fractures in children. J Pediatr Orthop 1994;14:207-210.
A, Jones IE, Taylor RW, et al. Bone mineral density and body
composition in boys with distal forearm fractures: a dual-energy x-ray
absorptiometry study. J Pediatr 2001;139:509-515.
A, Jones IE, Taylor RW, et al. Dynamic and static tests of balance and
postural sway in boys: effects of previous wrist bone fractures and
high adiposity. Gait Posture 2003;17:136-141.
A, Jones IE, Taylor RW, et al. More broken bones: a 4-year double
cohort study of young girls with and without distal forearm fractures.
J Bone Miner Res 2000; 15:2011-2018.
W, Pyle SI. Radiographic atlas of skeletal development of the hand and
wrist. Stanford: Stanford University Press; 1959.
S. Fractures and epiphyseal fracture separation of the distal bones of
the forearm in children. In: Saffar P, Cooney WP, eds. Fractures of the
Distal Radius. Philadelphia: JB Lippincott, 1995.
RP, Danielsson LG. Dorsally angulated solitary metaphyseal greenstick
fractures in the distal radius: results after immobilization in
pronated, neutral, and supinated position. J Pediatr Orthop
1990;10:90-92.
R, Poznanski AK, Donovan JM. Ulnar variance in children-standard
measurements for evaluation of ulnar shortening in juvenile rheumatoid
arthritis, hereditary multiple exostosis and other bone or joint
disorders in childhood. Skeletal Radiol1989; 18:513-516.
J Jr, Peterson HA. Fracture of the distal radial physis complicated by
compartment syndrome and premature physeal closure. J Pediatr Orthop
1986;6:627-630.
H, Nilsson BE, Willner S. Correction with growth following diaphyseal
forearm fracture. Acta Orthop Scand 1976;47:229-303.
JR, Louis DS. Entrapment of pronator quadratus in pediatric
distal-radius fractures: recognition and treatment. J Pediatr Orthop
1994;14:498-500.
J, Smith JA. Fracture of the lower end of the radius associated with
fracture or dislocation of the lower end of the ulna. Boston Med Surg J
1922;187:401-407.
U, Schlicht W, Outzen S, et al. Ultrasound in the diagnosis of
fractures in children. J Bone Joint Surg Br 2000;82:1170-1173.
Y, Horiuchi Y, Takahashi M, et al. Extensor tendon involvement in
Smith’s and Galeazzi’s fractures. J Hand Surg Am 1987;12:535-540.
IE, Cannan R, Goulding A. Distal forearm fractures in New Zealand
children: annual rates in a geographically defined area. N Z Med J
2000;113:443-445.
IE, Williams SM, Dow N, et al. How many children remain fracture-free
during growth? A longitudinal study of children and adolescents
participating in the Dunedin Multidisciplinary Health and Development
Study. Osteoporos Int 2002;13:990-995.
O, Ogawa R. Pseudarthrosis of the radius associated with
neurofibromatosis: report of a case and review of the literature. J
Pediatr Orthop 1990;10:128-131.
EO, Ryöppy SA, Mäkinen RJ. Remodelling by asymmetrical epiphysial
growth. An experimental study in dogs. J Bone Joint Surg Br
1976;58:122-126.
J, Appelqvist R. Irreducible fracture of the wrist in a child.
Entrapment of the extensor tendons. Acta Orthop Scand 1987;58:280-281.
JR. Forearm fractures. In: MacEwen GD, Kasser JR, Heinrich SD, eds.
Pediatric Fractures: A Practical Approach to Assessment and Treatment.
Baltimore: Williams & Wilkins, 1993:165-190.
KS, Grufferty A, Gallagher O, et al. A randomized trial of “soft cast”
for distal radius buckle fractures in children. Acta Orthop Belg
2007;73:594-597.
S, Melton LJ 3rd, Dekutoski MB, et al. Incidence of childhood distal
forearm fractures over 30 years: a population based study. JAMA
2003;290:1479-1485.
RA, Press CM, Gonzalez MH. Rupture of the flexor pollicis longus tendon
after volar fixed-angle plating of a distal radius fracture: a case
report. J Hand Surg Am 2007;32:984-988.
JL, Jupiter JB. Intra-articular fractures of the distal end of the
radius in young adults. J Bone Joint Surg Am 1986;68:647-659.
SB, Nance ML, Rutherford GW Jr, et al. Skateboard-associated injuries:
participation-based estimates and injury characteristics. J Trauma
2002;53:686-690.
LA. Fracture patterns in children. Analysis of 8682 fractures with
special reference to incidence, etiology and secular changes in a
Swedish urban population 1950-1979. Acta Orthop Scand Suppl
1983;202:1-109.
R. Fracture of the ulnar styloid process. Effect on wrist function in
the presence of distal radius fracture [in German]. Zentralbl Chir
1989;114:1006-1011.
A, Osterman K. Surgical treatment of partial closure of the epiphysial
plate. Reconstr Surg Traumatol 1979;17:48-64.
E, Vittas D, Torp-Pedersen S. Remodeling of angulated distal forearm
fractures in children. Clin Orthop Relat Res 1988;237:190-195.
L. Fractures of the distal radius and ulna in management of pediatric
fractures. In: Letts M, ed. Management of Pediatric Fractures. New
York: Churchill-Livingstone, 1994:345-368.
BS, Esterhai JL Jr, Das M. Fracture of the distal radial epiphysis.
Characteristics and surgical treatment of premature, posttraumatic
epiphyseal closure. Clin Orthop Relat Res 1984;(185):90-96.
PD, Georgis T, Slabaugh P. Irreducible Salter-Harris type II fracture
of the distal radial epiphysis. J Pediatr Orthop 1987;7:719-721.
RM. Monteggia and Galeazzi fractures. In: Letts RM, ed. Management of
Pediatric Fractures. New York: Churchill-Livingstone, 1994:313-321.
CK, Liau KH, Chew WY. Results of distal radial fractures treated by
intrafocal pin fixation. Ann Acad Med Singapore 2001;30:573-576.
D, Jones G. The association between bone mineral density, metacarpal
morphometry, and upper limb fractures in children: a population-based
case-control study. J Clin Endocrinol Metab 2003;88:1486-1491.
A, Tsintzas D, Mahawar K, et al. Gap index: a good predictor of failure
of plaster cast in distal third radius fractures. J Pediatr Orthop Br
2007;16:48-52.
BR, Bartolozzi AR, Davis CA, et al. Wrist pain syndrome in the gymnast.
Pathogenetic, diagnostic, and therapeutic considerations. Am J Sports
Med 1989;17: 305-317.
GV, Hui PW, Cheng JC. Translation of the radius as a predictor of
outcome in distal radial fractures of children. J Bone Joint Surg Br
1993;75:808-811.
K, Sumi H, Sumi Y, et al. Wrist fractures from snowboarding: a
prospective study for 3 seasons from 1998 to 2001. Clin J Sport Med
2004;14:64-71.
LS, Kaufer H, Garver DF, et al. The effect on supination-pronation of
angular malalignment of fractures of both bones of the forearm. J Bone
Joint Surg Am 1982; 64:14-17.
GJ, Cowan B, Annan IH, et al. Management of completely displaced
metaphyseal fractures of the distal radius in children. A prospective,
randomized controlled trial. J Bone Joint Surg Br 2002;84:413-417.
R, Prommersberger KJ, van Griensven M, et al. Surgical correction of
deformities of the distal radius due to fractures in pediatric
patients. Arch Orthop Trauma Surg 2004;124:1-9.
BS, Taylor B, Widmann RF, et al. Cast immobilization versus
percutaneous pin fixation of displaced distal radius fractures in
children: a prospective, randomized study. J Pediatr Orthop
2005;25(4):490-494.
DE, Palmer AK, Levinsohn EM. Radiography and computerized tomography in
the diagnosis of incongruity of the distal radioulnar joint. A
prospective study. J Bone Joint Surg Am 1985;67:247-252.
T, Benson WM, Foster BK, et al. Statistical analysis of the incidence
of physeal injuries. J Pediatr Orthop 1987;7:518-523.
TM, Lester DK, Sarmiento A. The stabilizing effect of soft-tissue
constraints in artificial Galeazzi fractures. Clin Orthop Relat Res
1985;194:189-194.
TM, Klein JP, Patzakis MJ, et al. Results of compression-plating of
closed Galeazzi fractures. J Bone Joint Surg Am 1985;67:1015-1021
RS, Macari G. Salter-Harris I fractures of the distal radius
misdiagnosed as wrist sprain. J Emerg Med 2000;19:265-270.
BE, Obrant K. The range of motion following fracture of the shaft of
the forearm in children. Acta Orthop Scand 1977;48;600-602.
KJ. Ulnar growth arrest after distal radius and ulna fracture. In Price
CT ed. Complications in Orthopaedics. Pediatric upper extremity
fractures. Rosemont, IL. American Academy of Orthopaedic Surgeons;
2004:12-20.
SE, Hennrikus WL, Loncarich DP, et al. Relationship between ligamentous
laxity and the site of upper extremity fractures in children: extension
supracondylar fracture versus distal forearm fracture. J Pediatr Orthop
B 1999;8:90-92.
EA, Ooi KS, Barnett PL. A randomized controlled trial of two methods of
immobilizing torus fractures of the distal forearm. Pediatr Emerg Care
2008;24:65-70.
JA, Beall JK, Conlogue GJ, et al. Radiology of postnatal skeletal
development. IV. Distal radius and ulna. Skeletal Radiol 1981;6:255-266.
LH, Toh CL. Galeazzi-equivalent fracture in children associated with
tendon entrapment—report of two cases. Ann Acad Med Singapore
2001;30:51-54.
AK, Glisson RR, Werner FW. Relationship between ulnar variance and
triangular fibrocartilage complex thickness. J Hand Surg Am
1984;9:681-682.
J, Monroe K, King W, et al. Can clinical parameters predict fractures
in acute pediatric wrist injuries? Acad Emerg Med 2000;7:1152-1155.
HA, Madhok R, Benson JT, et al. Physeal fractures: Part 1. Epidemiology
in Olmsted County, Minnesota, 1979-1988. J Pediatr Orthop
1994;14:423-430.
AC, Perry JJ, Correll R, et al. A randomized, controlled trial of
removable splinting versus casting for wrist buckle fractures in
children. Pediatrics 2006;117:691-697.
D, Diamond G, Kattan A, et al. The effect of calcium intake and
physical activity on bone quantitative ultrasound measurements in
children: a pilot study. J Bone Miner Metab 2008;26:248-253.
MT, Moore DJ, Paterson JM. Redisplacement after manipulation of distal
radial fractures in children. J Bone Joint Surg Br 1993;75:453-454.
KJ, Van Schoonhoven J, Lanz UB. Outcome after corrective osteotomy for
malunited fractures of the distal end of the radius. J Hand Surg Br
2002;27:55-60.
FW, Cordell LD. Unstable fracture-dislocations of the forearm. The
Monteggia and Galeazzi lesions. Arch Surg 1968;96:999-1007.
R, Rønning I, Gerner T, et al. The efficacy of wrist protectors in
preventing snowboarding injuries. Am J Sports Med 2001;29:581-585.
A, Reis M, Molina M, et al. Supracondylar fractures of the humerus
associated with ipsilateral forearm fractures in children. J Pediatr
Orthop 2001;21:307-312.
AP. Anterior dislocation of the ulna at the inferior radioulnar joint.
Case report, with a discussion of the anatomy of rotation of the
forearm. J Bone Joint Surg Br 1960;42-B:515-521.
S, Caine D, Singer KM. Stress changes of the distal radial epiphysis in
young gymnasts. A report of 21 cases and a review of the literature. Am
J Sports Med 1985; 13:301-308.
S, Karaharju EO. Alteration of epiphyseal growth by an experimentally
produced angular deformity. Acta Orthop Scand 1974;45:490-498.
V, Mara J. Compartmental syndrome complicating Salter-Harris type II
distal radius fracture. Clin Orthop Relat Res 1988;226-229.
K, Takagi M, Kiyoshige Y, et al. Snowboarder’s wrist: its severity
compared with Alpine skiing. J Trauma 1999;46:1059-1061.
Y, Sugioka Y. The pronator quadratus sign: its classification and
diagnostic usefulness for injury and inflammation of the wrist. J Hand
Surg Br 1989;14:80-83.
PJ, Fagg PS. Undisplaced fractures of the distal third of the radius in
children: an innocent fracture? Injury 1992;23:165-167.
F, Cooney WP 3rd, Burny F, et al. Small external fixation devices for
the hand and wrist. Clin Orthop Relat Res 1993;293;77-82.
DL, Loro ML, Pitukcheewanont P, et al. Increased body weight and
decreased radial cross-sectional dimensions in girls with forearm
fractures. J Bone Miner Res 2001;16:1337-1342.
PG. Complete fracture of the lower third of the radius in childhood,
with greenstick fracture of the ulna. Ann Surg 1915;61:209-225.
M, et al. Combined fracture of the distal radius and scaphoid in
children. Report of two cases. Acta Orthop Belg 2003;69:79-81.
GA, Chrisman OD, Wilson TC, et al. Subluxation of the distal radioulnar
joint by hyperpronation. J Bone Joint Surg Am 1969;51:1315-1323.
S, Freiman S, Volpin G. Anterior interosseous nerve palsy associated
with Galeazzi fracture. J Pediatr Orthop B 2000;9:45-46.
CL, Micheli LJ. Simultaneous ipsilateral fractures of the arm and
forearm in children. Clin Orthop Relat Res 1980;218-222.
SD, Swischuk LE, Swischuk JL, et al. Significance of ulnar styloid
fractures in childhood. Pediatr Emerg Care 1990;6:99-103.
AH Jr, Katz SF. Stabilization of comminuted fractures of the distal
inch of the radius: percutaneous pinning. Clin Orthop Relat Res
1975;174-181.
KG. Fractures of the distal forearm. In: Weber BG, Burner C, Freuler F,
eds. Treatment of Fractures in Children and Adolescents. New York:
Springer-Verlag, 1980: 203-217.
S, Rowsell M, Bhowal B, et al. Hospital versus home management of
children withbuckle fractures of the distal radius. A prospective,
randomised trial. J Bone Joint Surg Br 2001;83:556-560.
J, Watson HK. Midcarpal instability caused by malunited fracture of the
distal radius. J Hand Surg Am 1984;9(3):350-357.
CW, Kay RM, Skaggs DL. Growth arrest of the distal radius following a
metaphyseal fracture: case report and review of the literature. J
Pediatr Orthop B 2002;11: 89-92.
RR, Garfinkel AI, Sarmiento A. The effects of angular and rotational
deformities of bothbones of the forearm. An in vitro study. J Bone
Joint Surg Am 1984;66:65-70.
PA, Graham HK. The “floating elbow” in children. Simultaneous
supracondylar fractures of the humerus and of the forearm in the same
upper limb. J Bone Joint Surg Br 1995;77:791-796.
AR, Sanderson PL, De Smet L, et al. The gymnast’s wrist: acquired
positive ulnar variance following chronic epiphyseal injury. J Hand
Surg Br 1992;17:678-681.
TE, Wagner W, Hanel DP, et al. Intrafocal (Kapandji) pinning of distal
radius fractures withand without external fixation. J Hand Surg Am
1998;23:381-394.
V, Westerlund M. Fracture of the carpal scaphoid in children. A
clinical and roentgenological study of 108 cases. Acta Orthop Scand
1980;51:909-913.
JA, Albiñana J, Certucha JA. Early posttraumatic physeal arrest in
distal radius after a compression injury. J Pediatr Orthop B
1996;5:57-60.
der Linden W, Ericson R. Colles’ fracture. How should its displacement
be measured and how should it be immobilized? J Bone Joint Surg Am
1981;63:1285-1288.
M, Sheehan E, Glynn A, et al. Heelys and street gliders injuries: a new
type of pediatric injury. Pediatrics 2007;119:e1294-e1298.
SJ, Weiner DS, Leighley B. Redisplacement after closed reduction of
forearm fractures in children. J Pediatr Orthop 1990;10:79-84.
K, Johansen A, Stone MD, et al. Seasonal variation in the incidence of
wrist and forearm fractures, and its consequences. Injury
2003;34:219-222.
PM, Bae DS, Montgomery KD. Surgical management of posttraumatic distal
radial growth arrest in adolescents. J Pediatr Orthop 2002;22:717-724.
PM, et al. Prospective study of displaced radius fractures in
adolescents treated with casting vs. percutaneous pinning. 2000.
PM, Kolettis GJ, Schwend R. Acute median neuropathy following physeal
fractures of the distal radius. J Pediatr Orthop 1994;14:173-177.
GR, Galpin RD, Armstrong DG. Comparison of short- and long-arm plaster
casts for displaced fractures in the distal third of the forearm in
children. J Bone Joint Surg Am 2006;88:9-17.
FW, Palmer AK, Fortino MD, et al. Force transmission through the distal
ulna: effect of ulnar variance, lunate fossa angulation, and radial and
palmar tilt of the distal radius. J Hand Surg Am 1992;17:423-428.
S, Andrews J, Bebbington A, et al. Buckle fractures of the distal
radius are safely treated in a soft bandage: a randomized prospective
trail of bandage versus plaster cast. J Pediatr Orthop 2005;25:322-325.
R, Waters PM, Reeves S. Complications of closed treatment of distal
radius fractures in children. Presented at the POSNA annual meeting,
Miami, 1995.
KE. Operative Management of Upper Extremity Fractures in Children.
American Academy of Orthopaedic Surgeons. Chicago, IL: Rosemont, 1994.
KE, O’Brien E. Distal radius and ulnar fractures. In: Bucholz RW,
Heckman JD, eds. Rockwood and Green’s Fractures in Adults.
Philadelphia: Lippincott Williams & Wilkins, 2002.
JS, Eyring EJ. Median-nerve entrapment within a greenstick fracture; a
case report. J Bone Joint Surg Am 1974;56:1270-1272.
K, Wedge JH, Bowen CV. Chronic injury to the distal ulnar and radial
growthplates in an adolescent gymnast. A case report. J Bone Joint Surg
Am 1988;70: 1087-1089.
TB. Irreducible displacement of the distal radial epiphysis
complicating a fracture of the lower radius and ulna. Injury
1984;16:166-168.
AS, Tredwell SJ, Mackenzie WG, et al. Accurate prediction of the
outcome after pediatric forearm fracture. J Pediatr Orthop
1994;14:200-206.
PS, Lam CY, Ng BK, et al. Percutaneous transphyseal intramedullary
Kirschner wire pinning: a safe and effective procedure for treatment of
displaced diaphyseal forearm fracture in children. J Pediatr Orthop
2004;24:7-12.
MM, Khoshhal KI. Displaced fracture of the distal radius in children:
factors responsible for redisplacement after closed reduction. J Bone
Joint Surg Br 2005;87: 841-843.
