Fractures and Dislocations of The Hand and Carpus In Children
Two – Upper Extremity > 8 – Fractures and Dislocations of The Hand
and Carpus In Children
reasons. Usage pattern of the exposed hand and the child’s curiosity
about the surrounding world are prime factors. Youngsters often are
unaware of dangers and place their hands in vulnerable situations.14,84,196,209,210 Hand and wrist injuries account for up to 25% of pediatric fractures (Table 8-1).70,84 The annual incidence is approximately 26.4 fractures per 10,000 children.209
age groups: the toddler and the adolescent. In the toddler age group,
the injury usually is secondary to a crush,10,56,108,196 often involving a finger caught in a closing door. In the adolescent
age group, the injury is most commonly from participation in sports.29,59,66,118,158,204,212 Football and skiing are prime examples of sports prone to athletic hand injuries.15,27,59
|
TABLE 8-1 Incidence of Pediatric Hand Injuries
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||
In addition, overweight adolescents have poorer balance than those of
healthy weight, which may explain their propensity for fracture.69 Hand fractures in children peak around age 13, which coincides with active participation in organized contact sports.
injuries and Salter-Harris (S-H) II fractures of the proximal
phalangeal base.70,84,117,152,209,210 The border digits (index and small fingers) are the most commonly injured rays.14,84,117,152,209,210
Dislocations of the pediatric hand are relatively uncommon injuries.
The metacarpophalangeal (MCP) joint is the most commonly dislocated
joint in the immature hand.38,65,110 The proximal interphalangeal (PIP) joint is the most commonly injured joint from volar plate tears or avulsion fractures.
injury because of different usage patterns and differences in
underlying skeletal and soft tissue composition. Knowledge of the
architecture of the physis, the soft tissue origins and insertions, and
the surrounding periosteum is useful for recognition and treatment of
children’s hand fractures.
distal ends of all the tubular hand bones. Secondary ossification
centers, however, develop only at the distal ends of the metacarpals of
the index, long, ring, and small rays, and at the proximal end of the
thumb. Conversely, the secondary centers of ossification are present
only at the proximal ends of the phalanges in all digits.75,118
 |
|
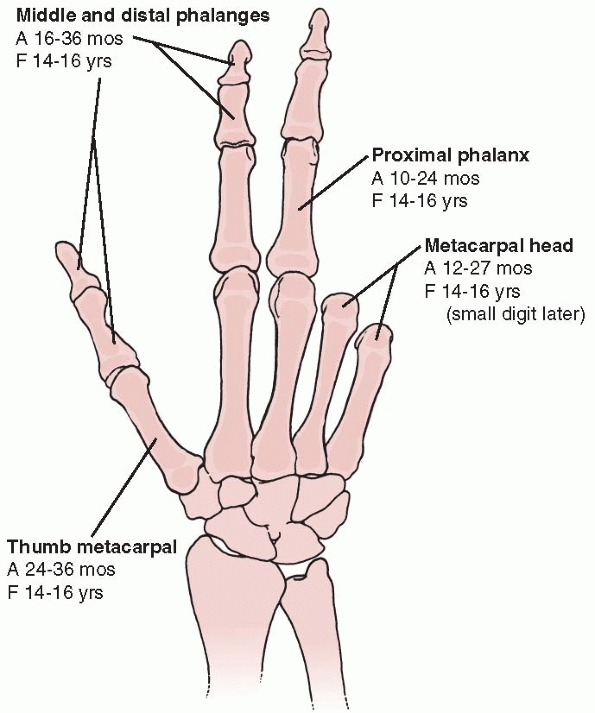
FIGURE 8-1 Appearance of secondary ossification centers (A). Fusion of secondary centers to the primary centers (F).
|
proximal phalanges appear at 15 to 24 months and fuse at bone age of 16
years (Fig. 8-1).75,188
In girls, the appearance and fusion occur earlier, at 10 to 15 months
and bone age of 14 years, respectively. The appearance of the secondary
ossification centers of the middle and distal phalanges is later than
the proximal phalanx, usually by 6 to 8 months. Fusion of the secondary
ossification centers, however, occurs from distal to proximal.
centers appear at 18 to 27 months in boys and at 12 to 17 months in
girls. The proximal thumb metacarpal secondary ossification center
appears 6 to 12 months after the fingers. The secondary centers within
the metacarpals fuse between 14 to 16 years of age in girls and boys.
The physis is divided into four distinct zones: germinal,
proliferative, hypertrophic, and provisional calcification. The zone of
chondrocyte hypertrophy (zone III) is the least resistant to mechanical
stresses. This zone is devoid of the collagen that provides inherent
stabilizing properties. The collagen is present in germinal and
proliferative (zones I and II), and the calcium present in provisional
calcification (zone IV) provides similar structural strength.70,194 Therefore, the fracture often propagates
through the zone of chondrocyte hypertrophy (zone III) as the path of
least resistance. However, high-energy injuries may undulate through
all four zones of the physis.133,176
Thus, a fracture line may be transmitted through several zones. This
variable path through irregular topography may contribute to partial
growth arrest after adolescent fractures that involve the physis.176
This change in irregularity also explains the differing patterns of
physeal injuries dependent on age: S-H I and II fractures tend to occur
in younger patients compared to S-H III or IV fractures, which are more
prevalent in children close to skeletal maturity.
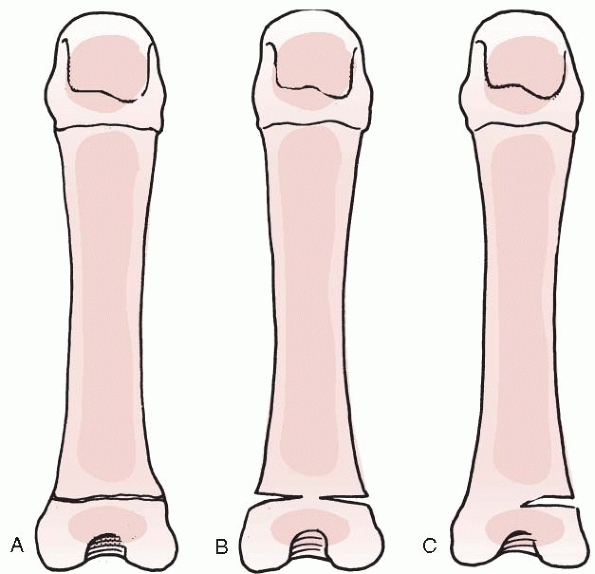
The pseudoepiphysis appears earlier than the proximal epiphysis and
fuses rapidly. By the sixth or seventh year, the pseudoepiphysis is
incorporated within the metacarpal and is inconspicuous.
Pseudoepiphyses also have been noted at the proximal ends of the finger
metacarpals, usually of the index ray. The only clinical significance
is differentiation from an acute fracture (Fig. 8-2).
but these anomalies are more common in the metacarpals of the index
finger and thumb. There are variable expressions of double epiphyses,
but the true entity is considered only when a fully developed growth
mechanism is present on both ends of a tubular bone. Double epiphyses
usually are seen in children with other congenital anomalies, but their
presence does not appear to influence overall bone growth. When
fractures occur in bones with double epiphyses, growth of the involved
bone appears to be accelerated.208
Periphyseal notching can be confused with trauma or double epiphyses.
The location of the notches can coincide with the physis or may be
slightly more distant from the epiphysis. Notching is a benign
condition that does not influence the structural properties of the bone.208
 |
|
FIGURE 8-2 Abnormal epiphyseal appearance. A. Double epiphysis. B. Pseudoepiphysis. C. Notched epiphysis.
|
terminal tendon of the digital extensor mechanism and the extensor
pollicis longus insert on the epiphyses of the distal phalanx. The
central slip of the extensor mechanism inserts onto the epiphysis of
the middle phalanx. The extensor pollicis brevis inserts onto the
epiphysis of the proximal phalanx. The abductor pollicis longus has a
broad-based insertion onto both the epiphysis and metaphysis of the
thumb metacarpal. The extensor digitorum communis connects into the
sagittal band at the MCP joint, which in turn lifts the proximal
phalanx into extension by its insertion along the volar plate.
long digital flexor tendons (the flexor digitorum profundus and the
flexor pollicis longus) insert into the metadiaphyseal region of their
respective terminal phalanges.82 The flexor digitorum superficialis inserts onto the central three fifths of the middle phalanx.
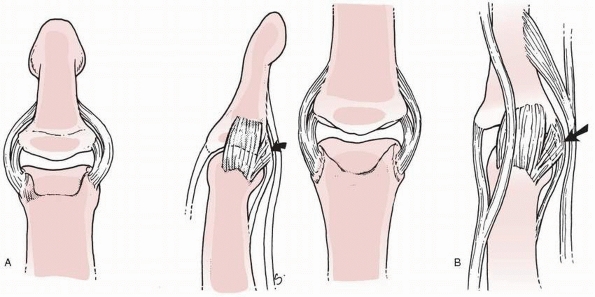
originate from the collateral recesses of the phalangeal head, span the
physis, and insert onto both the metaphysis and epiphysis of the middle
and distal phalanges (Fig. 8-3). The
collaterals also insert onto the volar plate to create a three-sided
box that protects the physes and epiphyses of the interphalangeal
joints from laterally directed forces.38,82 This configuration explains the rarity of S-H III injuries at the interphalangeal joints.
joints originate from the metacarpal epiphysis and insert almost
exclusively onto the epiphysis of the proximal phalanx (Fig. 8-4).
This anatomic arrangement accounts for the frequency of S-H III
injuries at the MCP joint level. The ligamentous anatomy about the
thumb MCP joint more closely resembles that of the PIP joints, which
mirrors the arrangement of the adjacent physes.
interphalangeal joint and MCP joints and resists hyperextension forces.
The volar plate originates from the metaphysis of the respective
proximal digital segment and inserts onto the epiphysis of the distal
segment (Fig. 8-3B). The plate receives
insertional fibers from the accessory collateral ligaments to create a
three-sided box that protects the joint.
as a considerable asset or liability in fracture management. The
periosteal sleeve can minimize fracture displacement, aid in fracture
reduction, or interpose between displaced fracture fragments and
prevent reduction.
 |
|
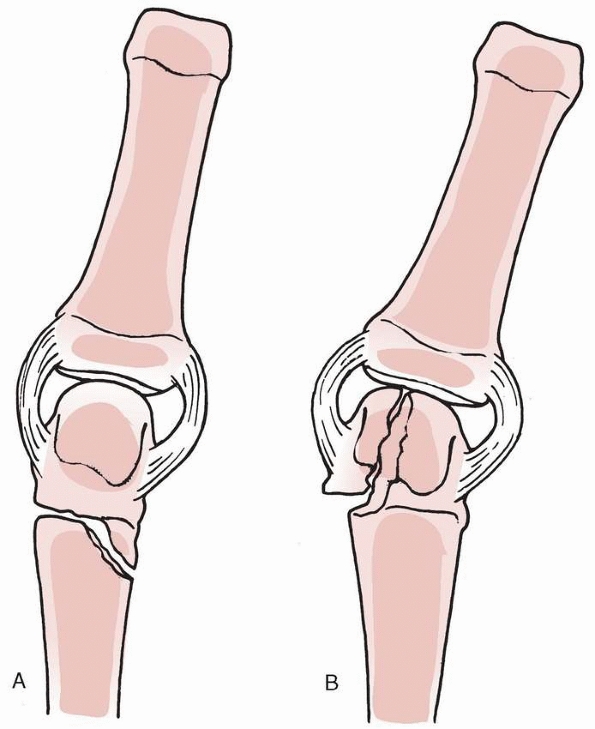
FIGURE 8-3 Anatomy of the collateral ligaments at the distal (A) and proximal (B)
interphalangeal joints. The collateral ligaments at the interphalangeal joints originate in the collateral recesses and insert into both the metaphyses and epiphyses of their respective middle and distal phalanges. Additional insertion into the volar plane (arrows) is seen at the interphalangeal joints. |
 |
|
FIGURE 8-4
The collateral ligaments at the MCP joint both originate and insert almost exclusively on the epiphyseal regions of the metacarpal and the proximal phalanx. |
fracture management. Factors that influence remodeling include the
patient’s age, the proximity of the fracture to the physis, the plane
of motion of the adjacent joint, and the plane of malalignment.17 The remodeling capacity is greater in younger children, fractures near a physis, and deformity in the plane of motion.70,71,130,153
Several clinicians have observed remodeling between 20 to 30 degrees in
the sagittal plane in children under 10 years of age and about 10 to 20
degrees in older children.36,130
Remodeling in the coronal or adduction-abduction plane is considerably
reduced compared to the sagittal plane. The amount is rarely quantified
but is probably 50% or less than remodeling in the sagittal plane.
Rotational remodeling does not occur.
toddlers, is more difficult than an adult. The child frequently is
noncompliant, unable to understand instructions, and fearful of the
physician. The physician must be patient and engage the child.
Observation and play are the mainstays of the examination. The child’s
hand posture and movements provide clues about the location and
severity of the injury as the child interacts with toys, parents, and
the environment in the examining area. Fracture is diagnosed by
swelling, ecchymosis, deformity, or limited movement. Fracture
malrotation is noted by digital scissoring during active grasp or
passive tenodesis. Tendon integrity is observed by digital posture at
rest and during active grasp around objects of varying size. Comparison
to the uninjured hand is invaluable. A hurried exam or a frightened
child can lead an erroneous or missed diagnosis. Passive wrist exam
with
finger flexion tenodesis is a critical part of the exam to accurately diagnose fracture malrotation.
areas of tenderness and move injured joints to assess their integrity.
Stress testing should be gentle, and joint stability should be recorded
in the anteroposterior and lateral directions. Neurologic injuries are
especially difficult to detect in a young child. The proper digital
artery is dorsal to the proper digital nerve within the finger.
Therefore, there is a high concordance between pulsatile bleeding
indicative of a digital artery injury and laceration of the digital
nerve.
in a young child. Normal discriminatory sensibility does not occur
until 5 to 7 years of age. Therefore, meaningful objective data are
difficult to obtain. A clinical clue is that children often bypass an
anesthetic digit during grasp and pinch. A helpful examination maneuver
is the wrinkle test. Immersion of an innervated digit in warm water for
5 minutes usually results in corrugation or wrinkling of the volar skin
of the tuft. Wrinkling is often absent in a denervated digit. If there
is doubt about the integrity of the nerve, operative exploration is
appropriate.
conducting a proper radiographic examination. Localization of areas of
tenderness or deformity directs a thorough radiographic assessment.
Several pediatric imaging factors complicate interpretation of plain
radiographs, including lack of bony detail and normal variations. The
normal ossification pattern of the immature hand creates problems with
the detection of fractures and also promotes false interpretation of
ligamentous injuries. Uncertain interpretation requires comparison to
the uninjured hand or consultation with a pediatric atlas of child
development and normal radiographic variants.75,188
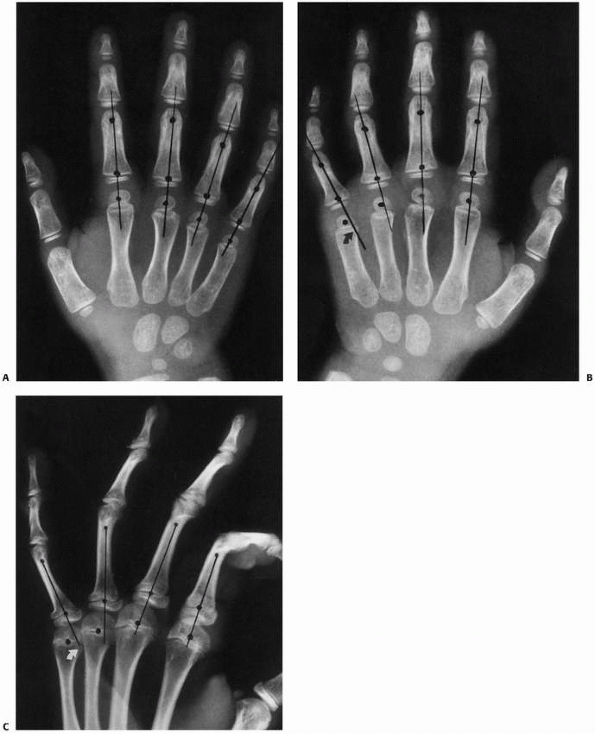
for complete evaluation of the injured hand or digit. The phalangeal
line test is useful in recognizing displaced fractures and joint
malalignment. If a line is drawn from the center of the phalangeal neck
through the center of the phalangeal metaphysis at the level of the
physis, it should pass through the exact center of the metacarpal or
phalangeal head in a normal finger, regardless of joint flexion (Fig. 8-5).26
Oblique views are particularly useful for assessing displacement and
intra-articular extension. A common radiograph pitfall is failure to
obtain a true lateral radiograph of the injured digit. Isolation of the
affected digit on the film or splaying of the fingers projects a true
lateral view. Stress views are rarely used for fracture evaluation.
Minifluoroscopy units are invaluable and allow a real-time assessment
of articular congruity and joint stability. These units have
considerable advantages, including the ability to obtain multiple views
and stress views with low-radiation exposure for the patient and
physician.
entities that may be interpreted as acute injuries. These diagnoses are
uncommon but may cause swelling, deformity, or decreased motion.
terminal phalanx of the small digit distal phalanx. This deformity
occurs spontaneously between the ages of 8 and 14 years and may be
confused with an acute fracture or epiphyseal separation (Fig. 8-6).101 A Kirner deformity, however, usually is bilateral and not associated with trauma.49
A trigger thumb in a young child sometimes is mistaken for an
interphalangeal joint dislocation because of the fixed flexion posture
and near equivalent clinical feel of “joint reduction” with
manipulative digital extension and triggering of the nodule through the
A1 pulley. The key diagnostic feature of a trigger thumb is the
palpable nodule over the A1 pulley.
burns from flame or radiation) may cause bizarre deformities from
altered appositional and interstitial bone growth. An ischemic necrosis
of the physes and epiphyses may result (Fig. 8-7).
The clinical result may yield altered bone width, length, or angulation
secondary to the unpredictable effect on the growing elements that make
interpretation of subsequent trauma difficult.79,138
epiphyseal narrowing and fragmentation, which are characteristic of
Thiemann disease. This hereditary entity usually involves the middle
and distal phalanges and typically resolves without treatment, although
some permanent joint deformity has been reported.40,165
bone or confused with fracture secondary to swelling and pain. An
enchondroma of the proximal phalanx is the classic benign tumor that
may fracture after trivial trauma (Fig. 8-8).
The malignant bone, cartilage, or muscle tumors are rare. Radiographs
reveal intrinsic destructive bony changes in an osteogenic sarcoma or
extrinsic compression with adjacent periosteal reaction secondary to an
adjacent rhabdomyosarcoma.
traumatic injury. The affected digit(s) present(s) with fusiform
swelling and decreased motion. The medical history usually is positive
for sickle cell disease. The inflammatory arthropathies (e.g., juvenile
rheumatoid arthritis, psoriatic arthritis, scleroderma, systemic lupus)
may be confused with trauma. A joint effusion and tenosynovitis are
common findings that require further diagnostic evaluation. Aside from
standard laboratory testing, magnetic resonance imaging (MRI) is
important for diagnosis of an inflammatory synovitis or tenosynovitis.
An infectious process often can be mistaken for injury, although local
and systemic evaluation usually ascertains this diagnosis.
malalignment in the coronal and sagittal planes. In contrast, children
cannot remodel malrotation, which requires reduction and stabilization
to prevent malunion and digital scissoring. It is essential that the
clinician properly diagnose and adequately treat problematic fractures.
Anesthesia is required for fracture reduction. A digital block may be
used for finger fracture reduction in adolescents. Conscious sedation,
regional anesthesia, and general anesthesia are alternatives. Rapid
fracture manipulation without anesthesia should be avoided.
Immobilization is best applied immediately after reduction. The choice
of a splint or cast depends on the degree of swelling, the difficulty
of reduction, and the age of the patient. The amount of padding is an
important consideration during cast application. Too much padding
renders the cast ineffective in maintaining the reduction.
In
contrast, too little padding may cause skin compromise from thermal
injury or direct pressure. The use of rigid materials other than
accepted casting materials (e.g., tongue blades, arm boards, metal
rods) should be discouraged. Immobilization of a solitary digit in a
child should be avoided because it is ineffective.
 |
|
FIGURE 8-5
The straight-method of assessing alignment about the MCP joint. The long axes of the metacarpal and proximal phalanx should align, as they do in this normal hand (A). If there is a fracture in the proximal phalanx, as in this patient’s opposite or injured hand (B,C), the axes will not be colinear (arrows). (Courtesy of Robert M. Campbell, Jr., MD.) |
 |
|
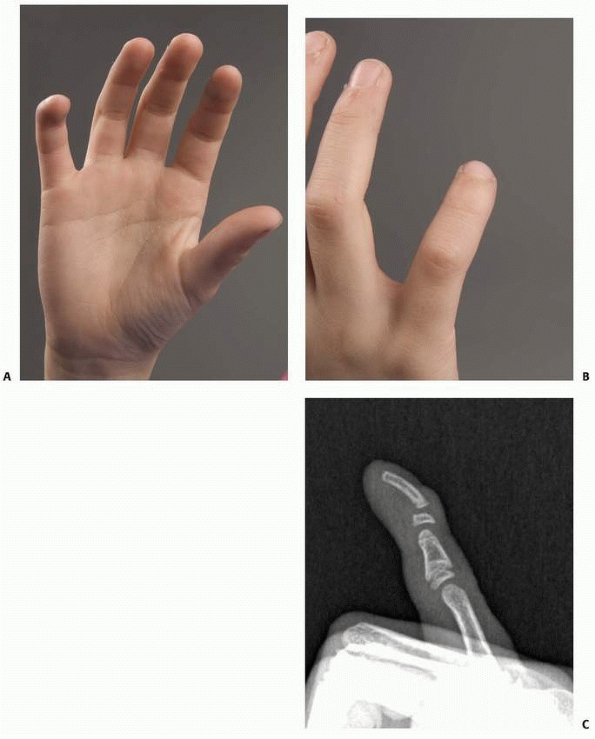
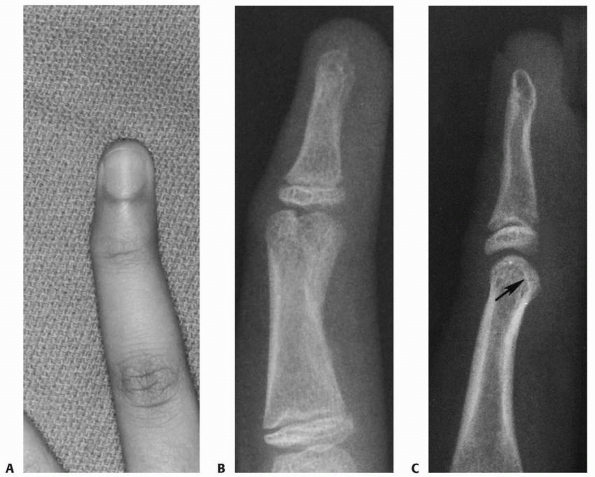
FIGURE 8-6 A-C.
A 9-year-old girl with incurving of the tip of the right small finger. Similar findings are noted in family members. The anteroposterior and lateral radiograph shows radial and palmar incurving of the distal phalanx, characteristic of Kirner deformity. |
immobilization of the injured digit with at least one of the adjacent
digits. Similar to the adult hand, the child’s hand is best immobilized
in the “safe position” with the MCP joints in flexion and the
interphalangeal joints in extension. Short-arm immobilization usually
is adequate for hand fractures, provided cooperation is reasonable.
Fractures in infants and toddlers require long-arm immobilization to
encircle the elbow and decrease the chances of escaping from the cast.
immobilization and re-evaluation in 3 to 4 weeks for cast or splint
removal. Fractures that required reduction necessitate weekly
evaluation to ensure maintenance of alignment. The first evaluation
should be within a week to allow detection of recurrent displacement
and provide ample time to perform repeat reduction before the rapid
healing process that occurs in children. To assess for malrotation, it
is necessary to remove the immobilization and check alignment by active
motion and passive tenodesis because radiographs can be misleading
regarding rotational alignment. An unstable malaligned fracture should
be treated with pin fixation to avoid malunion.
heal. Therefore, delayed union and nonunion are uncommon problems
except after open fractures or open surgery that disrupts the inherent
blood supply. A frequent concern is growth arrest following a physeal
injury. The arrest usually is secondary to
the initial injury, although repeated manipulations impart additional trauma to the damaged physis and should be avoided.
 |
|
FIGURE 8-7
An 11-year-old girl sustained a frostbite injury to the right hand. Radiograph reveals premature fusion of the physis of the distal and proximal phalanges with irregularity of the bases of the shortened phalanges. |
There are inherent differences in anatomy that require special
consideration. The periosteum is thick and periosteal flaps can be
created and later approximated to enhance healing and remodeling. The
periosteal layer also provides excellent coverage for implants and a
good sliding surface for tendons.
dissection around the physis should be minimized to avoid injury.
Fixation across a physis requires thoughtful consideration concerning
growth arrest. When fixation is necessary, the smallest diameter smooth
wire that effectively holds the fracture fragments should be used.
Implants, such as plates, should also avoid the physis.
necessary. Simple liberation from immobilization and instructions to
the patient and parents regarding range of motion, strengthening, and
activity return usually are sufficient. In uncommon circumstances
(e.g., complicated fractures or multiple trauma), formal hand therapy
is indicated.
 |
|
FIGURE 8-8 A,B.
A 14-year-old girl with multiple enchondromas (Ollier disease), which weaken the bone and increase the susceptibility to fracture. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.) |
relatively uncommon. However, the physician should avoid being
nonchalant in thinking that the pediatric hand is forgiving in its
ability to remodel and regain motion. Recognition of the potential
pitfalls is important, as is the development of a systematic plan for
rectifying complications.
is failure to diagnose the fracture or an underappreciation of the
extent of injury. Anteroposterior, lateral, and oblique radiographs are
needed for complete evaluation of the injured hand or digit. Imaging of
the contralateral hand for comparison and consultation with a pediatric
atlas of child development and normal radiographic variants should be
done whenever the diagnosis is in question.75,188
treatment is instituted to ensure anatomic healing and return of normal
function. Displacement or rotation at the fracture site may be subtle
on radiographs. Inspection of the radiographs and a meticulous
examination are necessary. Finger fractures must be scrutinized for
evidence of malrotation by evaluating the plane of the fingernails with
the fingers semiflexed by tenodesis or active motion. A malrotated or
markedly displaced fracture requires reduction under anesthesia to
regain bony alignment. The degree of reduction required depends on the
configuration, location, and extent of the fracture as well as the age
of the child. Although sagittal and coronal remodeling can occur in the
immature skeleton, rotational malalignment will not remodel.140
Pin stabilization may be required to maintain reduction. Open reduction
and internal fixation may be necessary for displaced intra-articular
fractures (i.e., S-H III thumb proximal phalanx fractures).
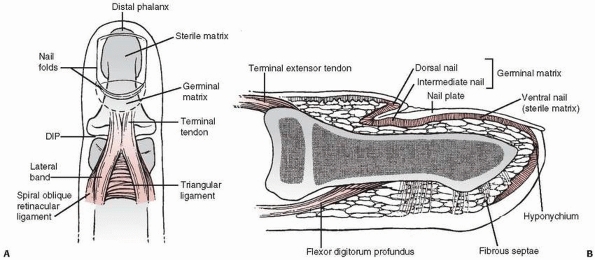
The dorsal periosteum of the distal phalanx is the underlying
nutritional and structural support for the sterile matrix and nail bed.
The germinal matrix is responsible for generating the nail plate. The
volar aspect of the distal phalanx anchors the pulp through tough,
fibrous septae that stabilize the skin against shear forces. The
terminal extensor tendon inserts onto the epiphysis of the distal
phalanx. The flexor digitorum profundus bypasses the physis to insert
onto the metadiaphysis of the distal phalanx.
 |
|
FIGURE 8-9 Anatomy about the distal phalanx. A.
The skin, nail, and extensor apparatus share a close relationship with the bone of the distal phalanx. Specific anatomic structures at the terminal aspect of the digit are labeled. B. This lateral view of the nail demonstrates the tendon insertions and the anatomy of the specialized nail tissues. |
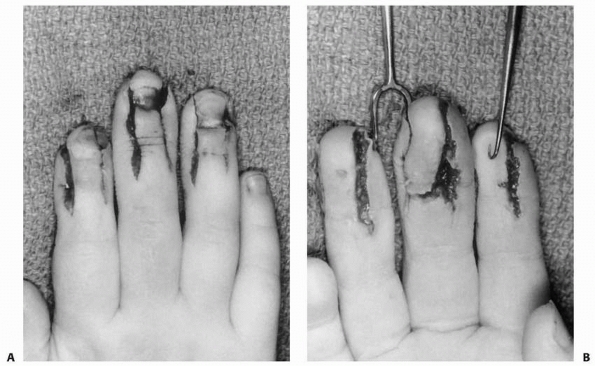
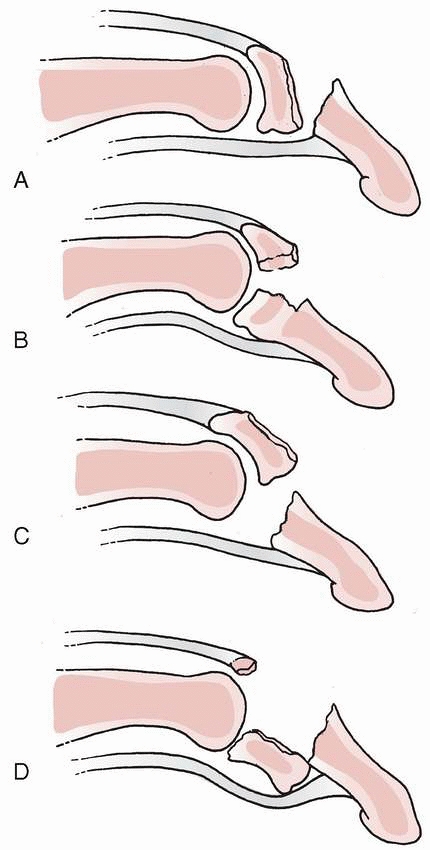
hyperflexion, and hyperextension. A crush injury creates a spectrum of
injury from minor tissue disruption with little need for intervention
to severe tissue trauma that requires bony fixation, meticulous nail
bed repair, and skin coverage (Fig. 8-10). A
flexion force applied to the extended tip of the finger results in a
mallet injury to the terminal tendon insertion or physeal separation
with nail bed injury (Seymour fracture). The distal interphalangeal
(DIP) joint rests in flexion and active extension is impossible in both
cases. A hyperextension force can produce a bony avulsion injury of the
flexor digitorum profundus tendon (pediatric jersey finger).
Extraphyseal fractures are common and range from a simple distal tuft
fracture to an unstable diaphyseal fracture underlying a nail bed
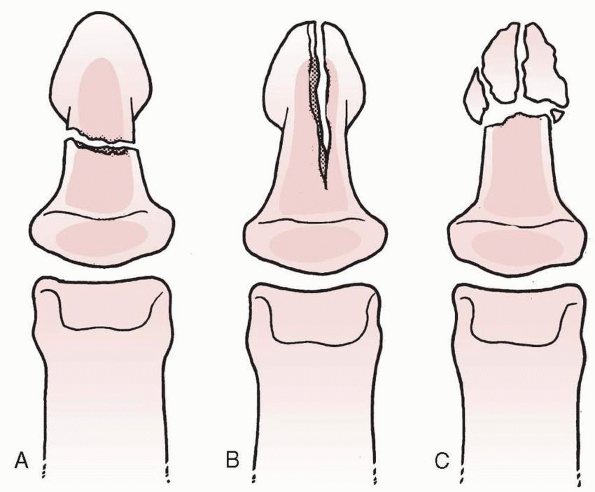
laceration. The fracture pattern can be divided into three types (Fig. 8-11). A transverse fracture (Fig. 8-11A)
may occur either at the distal extent of the terminal phalanx or
through the diaphysis. Displaced transverse fractures through the
diaphysis are almost always associated with a considerable nail bed
injury that requires repair. A longitudinal splitting type fracture is
much less common (Fig. 8-11B). This pattern is
the result of excessive hoop stress within the tubular distal phalanx
at the time of a crush injury. The “cloven-hoof” appearance of the
fracture is characteristic (Fig. 8-12). The fracture may be contained within
the shaft or can propagate through the physis and even into the joint.10 A comminuted fracture of the distal diaphysis also can occur and usually is accompanied by extensive soft tissue injury (Figs. 8-11C).
 |
|
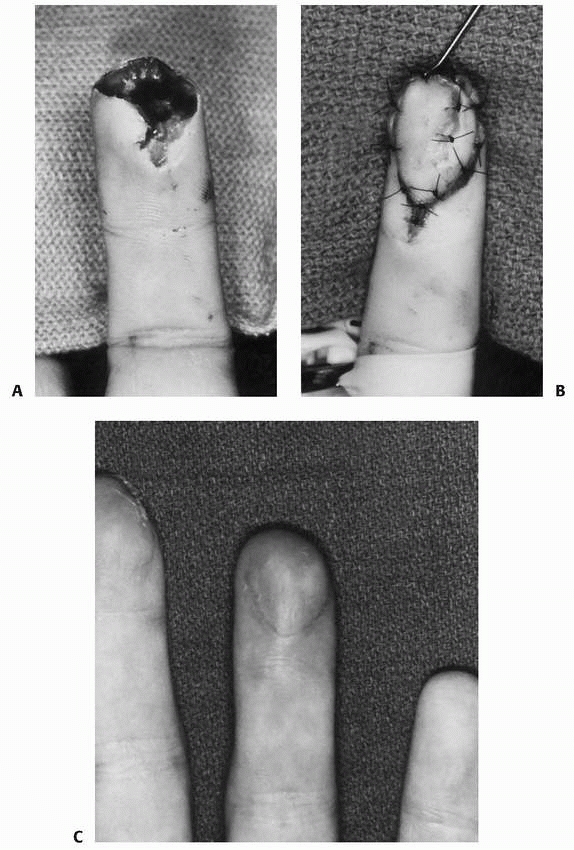
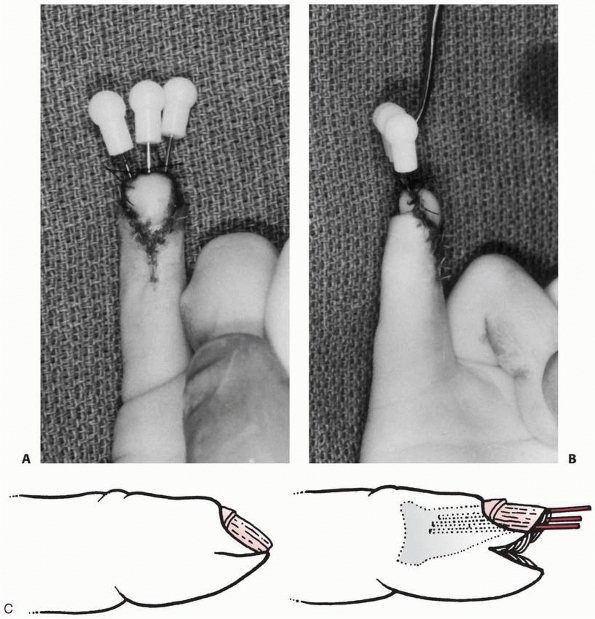
FIGURE 8-10 A,B. Crush injury to the fingers of a 4-year-old with nail bed laceration requiring meticulous repair with absorbable suture.
|
|
TABLE 8-2 Classification of Distal Phalangeal Fractures
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||
 |
|
FIGURE 8-11 Three types of extraepiphyseal fractures of the distal phalanx. A. Transverse diaphyseal fracture. B. Cloven-hoof longitudinal splitting fracture. C. Comminuted distal tuft fracture with radial fracture lines.
|
 |
|
FIGURE 8-12
Extraepiphyseal fracture of the distal phalanx: the cloven-hoof longitudinal splitting fracture. In this patient, the fracture line (arrow) does not appear to extend across the physis. |
 |
|
FIGURE 8-13
Flexor digitorum profundus avulsion fracture of the distal phalanx (jersey finger). This bony avulsion is apparent on radiographs, indicating the extent of proximal migration. |
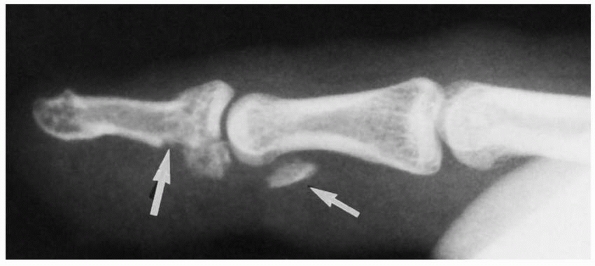
forced extension of the flexed DIP joint. This mechanism can result in
either a bony avulsion injury or a soft tissue disruption of the flexor
digitorum profundus (jersey finger) (Fig. 8-13).106,205
An avulsion fracture often limits flexor digitorum profundus retraction
in the pulley system by tethering of the bone fragment on the A5 or A4
pulley. The radiographic location of the bony fragment identifies the
level of tendon retraction. In contrast, soft tissue disruption of the
flexor digitorum profundus frequently retracts into the palm. Diagnosis
of this injury is often missed in the acute setting.
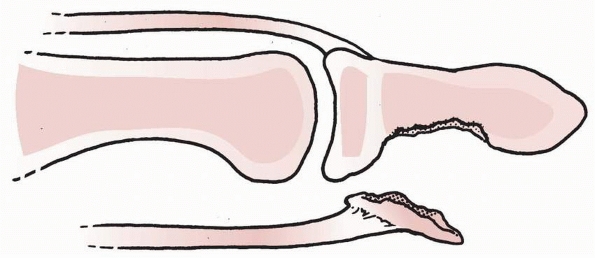
There are four basic fracture patterns and all result in a flexed
posture of the DIP joint (Fig. 8-14). A S-H I
or II fracture with flexion of the distal fragment occurs predominantly
in young patients less than 12 years of age. The unopposed flexor
digitorum profundus flexes the distal fragment. The injury often is
open and associated with a nail bed injury. There is a high risk for
incarceration of the germinal or sterile matrix in the fracture site,
known as a Seymour fracture.169
Closed reduction may be blocked by interposition of the nail bed in the
dorsal physis deep to the nail plate. Rarely, a S-H I or II fracture
causes extrusion of the epiphyseal fragment.125,199
This “epiphyseal dislocation” is challenging to diagnose with an
unossified epiphysis because the remaining distal phalanx remains
colinear with the axis of the digit, whereas the displaced unossified
epiphysis is dorsally dislocated by traction produced by the extensor
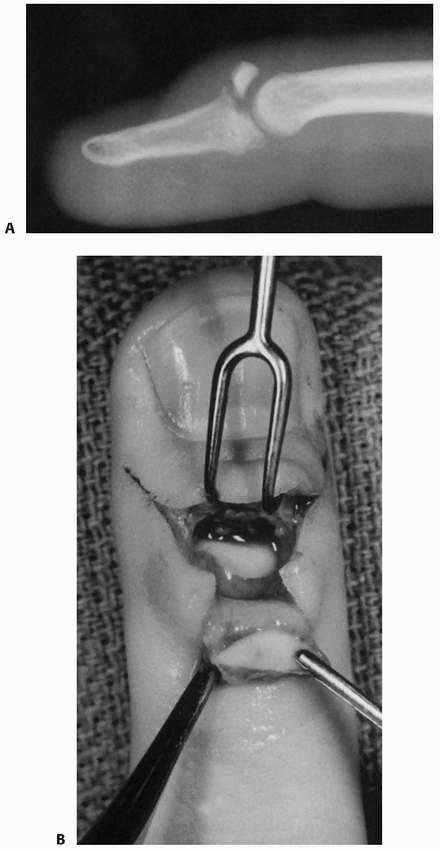
tendon. A dorsal S-H III fracture of the distal phalanx occurs in
teenagers and results in an extension lag at the DIP joint. Rarely, the
epiphysis also may separate from the terminal extensor tendon.164
 |
|
FIGURE 8-14 A-D. Mallet-equivalent fracture types.
|
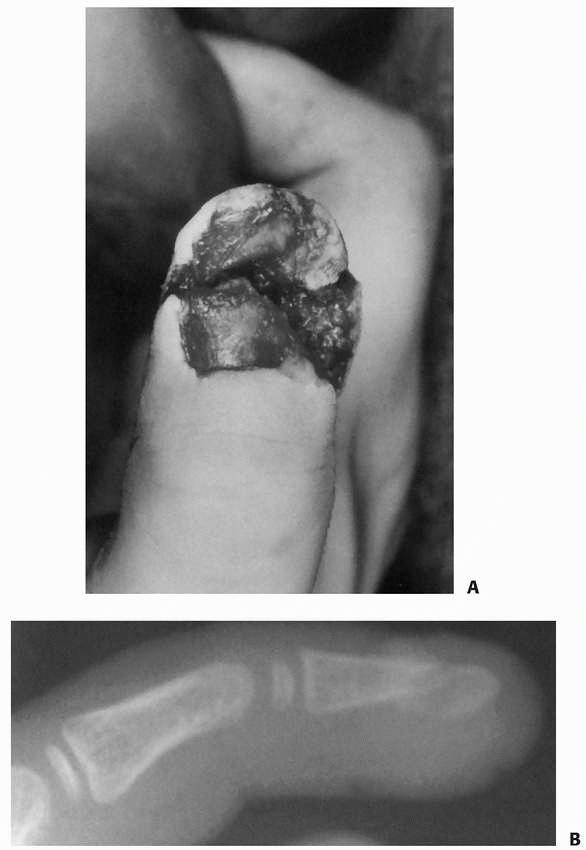
straightforward. The history and physical examination are consistent
with a distal phalanx fracture. A nail bed injury or a subungual
hematoma greater than 50% creates a high index of suspicion for bony
injury and displaced nail bed laceration (Fig. 8-15).213 Radiographs are confirmatory and detail the fracture pattern. Anteroposterior
and lateral views of the distal phalanx are necessary to ascertain fracture configuration.
 |
|
FIGURE 8-15 A. A crush injury to the thumb of a 4-year-old with a stellate nail bed laceration and fracture of the tuft. B. Radiograph reveals a comminuted tuft fracture.
|
attention to the soft tissue and bony injuries. The soft tissue repair
is as critical to outcome as the bony treatment. Any substantial nail
bed laceration requires repair. The distal phalangeal fracture is
assessed for alignment and stability. An unstable fracture that cannot
support the nail bed necessitates stabilization.
fractures can be treated with nonoperative measures using a splint or
cast. Mild and moderate displacement of extraphyseal fractures will
heal without difficulty. Even physeal injuries with mild displacement
of the dorsal epiphyseal fragment have favorable results with splinting.
evacuation include subungual hematoma involving more than 50% of the
nail plate or painful pressure under the nail.42
Decompression can be done with a hypodermic needle that penetrates the
nail plate. A heated paper clip or cautery tip may also be used, but
the heat can cause further nail bed injury if penetration is too deep.
nail bed lacerations and potentially for subungual hematomas that
involve more than 50% of the nail plate. A blunt freer elevator is used
to remove the nail plate to avoid additional nail bed injury. Partial
nail removal is rarely indicated for nail bed repair in children.
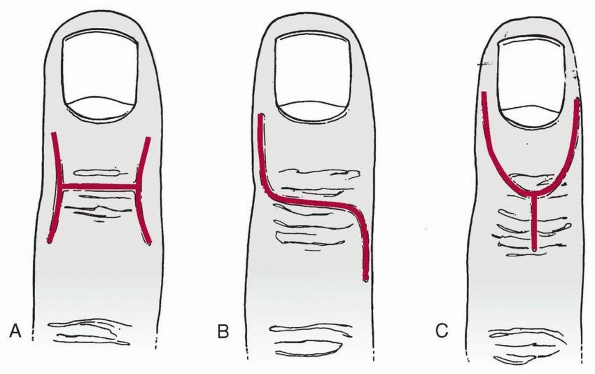
Proximal exposure of the germinal matrix requires incisions along the
eponychial folds and proximal retraction of the eponychial flap. The
nail bed is repaired with interrupted 6-0 or 7-0 absorbable sutures
under loupe magnification. Following repair, the nail bed is supported
using the nail plate or another substitute, such as the foil from the
suture pack.54,163,213
fractures with wide displacement may require stabilization. Usually a
smooth Kirschner wire can be inserted across the fracture through the
tip of the finger. A hypodermic needle can be used as a substitute for
the smooth wires.124 Physeal
fractures with a dorsal fragment larger than 50% of the epiphysis or
considerable DIP joint subluxation may require operative intervention.38,80 Closed manipulation and percutaneous Kirschner-wire fixation usually is sufficient.
The Seymour fracture represents an irreducible fracture that requires
open reduction. The sterile matrix must be extricated from the fracture
site and repaired beneath the eponychium. Epiphyseal dislocations also
require operative intervention to both restore joint congruity and
reestablish extensor tendon continuity.
indication for open repair. Surgery should be done as soon as possible
to limit tendon ischemia and shortening. The profundus tendon is
identified at the level of retraction and repaired to the distal
phalanx (Fig. 8-17). Too often, this diagnosis is made late.
small portion of the collateral ligaments may be recessed to enhance
exposure; however, soft tissue dissection should be limited to prevent
osteonecrosis of small bony fragments. Fracture fixation can be
accomplished with a smooth wire, pullout wire, tension band, or heavy
suture.70,80,84,102,140
Fixation across the DIP joint with a small diameter, smooth wire
usually is necessary to maintain joint and physeal congruity. A volar
approach is used for avulsion of the flexor digitorum profundus tendon.
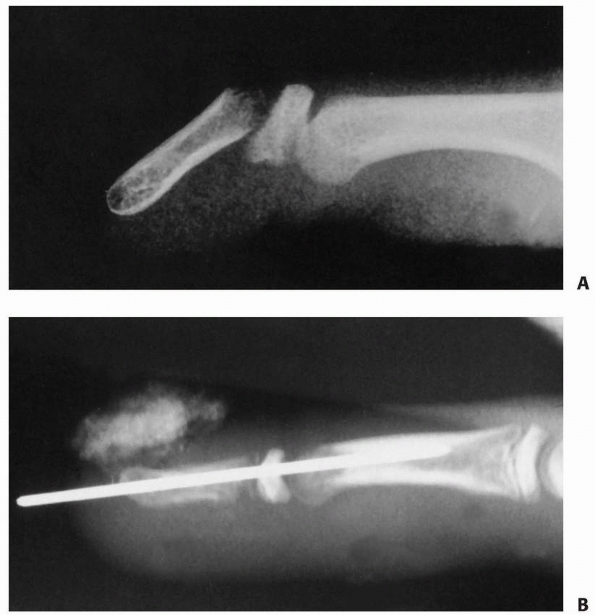 |
|
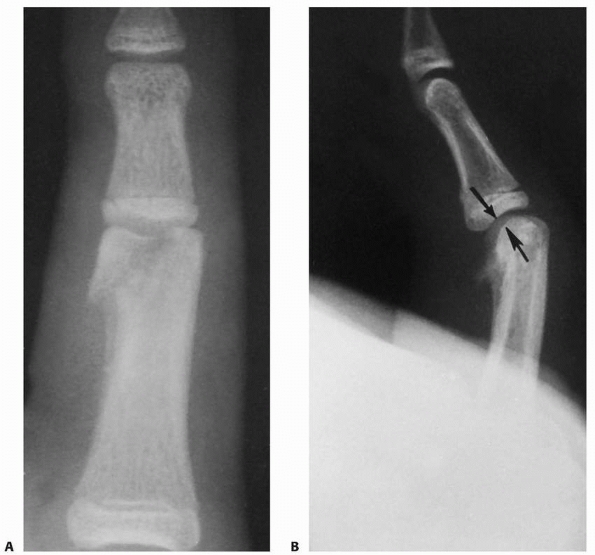
FIGURE 8-16 A. An irreducible distal phalangeal fracture that required extrication of the nail bed from within the fracture site. B. Stabilization of the fracture fragments with a longitudinal Kirschner wire across the DIP joint.
|
 |
|
FIGURE 8-17
A 17-year-old athlete with an avulsion fracture from the flexor digitorum profundus tendon. The fracture extends through the epiphysis and into the joint (large arrow). The flexor digitorum profundus tendon with its attached bony fragment has retracted to the level of the A4 pulley (small arrow). |
 |
|
FIGURE 8-18 Exposures to the DIP joint. A. H-type flap with the transverse limb over the DIP joint. B. S-shaped exposure of the DIP joint. C.
An extended exposure of the DIP joint. All exposures must avoid injury to the germinal matrix, which is located just proximal to the nail fold. |
 |
|
FIGURE 8-19 A. Displaced mallet fracture with considerable articular involvement and dorsal prominence. B. Open reduction through a dorsal approach reveals the articular fragment attached to the terminal tendon.
|
distal phalangeal fractures. The injury may involve skin, nail tissue,
and bone. Support for nail growth is a primary consideration. Minimal
loss of tissue can be treated with local wound care and healing through
secondary intention. A small amount of exposed bone does not preclude
spontaneous healing in children. The likelihood of nail deformity
(hooked or “parrot’s beak”) is high for amputations that involve more
than 50% of the distal phalanx.
coverage varies depending on the degree of tissue loss and direction of
injury. Simple healing by primary closure is preferred for most volar
oblique fingertip amputations. Dorsal oblique amputations are
complicated by nail bed injury and are more difficult to cover.
Composite grafts of skin and subcutaneous tissue from the amputated
part have been used in young children with variable results. Local
flaps are another option for coverage of large volar or dorsal oblique
amputations. Options include a variety of flaps, such as a V-Y volar
advancement, a thenar flap, a cross-finger flap, a pedicled flap, or a
neurovascular island flap (Figs. 8-20 and 8-21).7,98
Fortunately, coverage issues are rare in children. An amputation of the
distal thumb also can be covered with a bipedicle (Moberg volar
advancement flap) or unipedicle neurovascular flap.132 The choice of coverage depends
on the degree and direction of soft tissue loss, age of the patient, and preference of the surgeon.
 |
|
FIGURE 8-20 Volar V-Y advancement flap for coverage. A. A volar oblique tissue loss of the ring finger with intact nail bed. B.
Flap designed with apex at the DIP joint and mobilized to cover the fingertip. The defect is closed proximal to the flap creating the Y. C. Satisfactory result with good durability and sensibility. |
 |
|
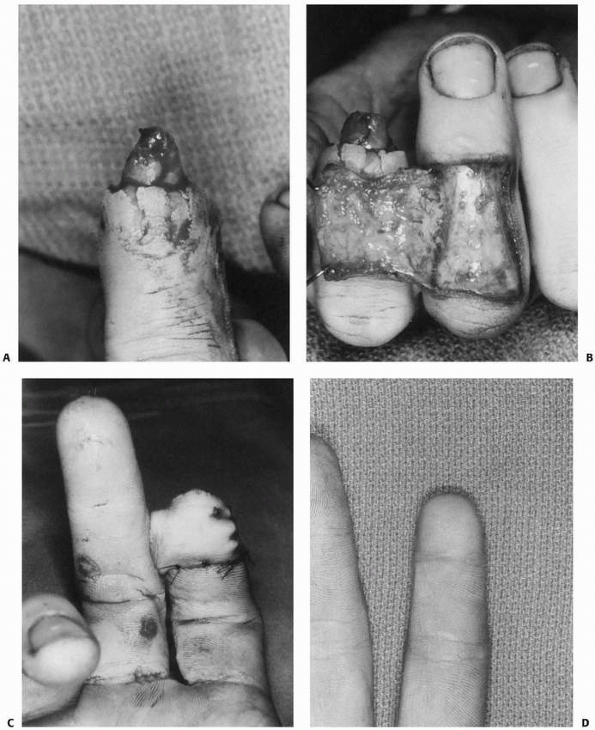
FIGURE 8-21 Cross-finger flap in a 17-year-old male with open distal phalangeal injury and tissue loss. A. Extensive volar and distal soft tissue loss with preservation of the bone and nail bed. B.
A cross-finger flap of skin and subcutaneous tissue is elevated from the dorsal aspect of the adjacent donor digit based on the side of the index finger. C. The vascular epitenon is preserved on the donor digit to support a skin graft. The flap is transferred to the volar aspect of the index finger to recreate the tuft. D. Satisfactory coverage and functional result. |
long arm mitten casts. As the child ages, the degree of immobilization
is decreased. An adolescent with a simple distal phalangeal fracture or
nail bed repair usually can be treated similar to an adult with only
DIP joint immobilization. Percutaneous fixation is removed in the
office 4 to 6 weeks after surgery. Formal hand therapy usually is not
required, although an instructed home program with emphasis on DIP
joint motion is useful. DIP blocking exercises are particularly helpful
to regain full joint movement. Formal therapy is reserved for patients
who fail to regain motion and strength after 3 to 4 weeks on a home
program.
fractures are favorable. A small loss of motion has little functional
impact. A small extensor lag or minor longitudinal nail ridge is well
tolerated by most patients. Considerable nail irregularity or deformity
is a frequent source of dissatisfaction.
immobilization. Immobilization for 3 to 4 weeks allows clinical union,
which proceeds complete radiographic healing by about 1 month.
Uncommonly, an unstable distal phalangeal fracture requires
percutaneous pinning with a small Kirschner wire. The DIP joint usually
is transfixed to provide additional stability. The pin is removed
approximately 4 weeks after injury.
anesthesia, removal of the nail plate, and nail bed repair. The parents
and patient are told that it takes several cycles of nail growth (3 to
6 months) before the final morphology of the nail is known.
Fortunately, in properly treated nail bed injuries, chronic deformity
is rare.
reduction and splinting. Placement of the DIP joint into extension
reduces most fractures. A splint is applied and radiographs are taken
to assess the degree of reduction. Adequate alignment requires
full-time splinting for 4 to 6 weeks depending on the age of the child,
size of the fracture fragment, and amount of bony apposition. The DIP
joint is positioned in neutral to 15 degrees of extension. Extreme
hyperextension is contraindicated because dorsal skin hypoperfusion and
necrosis may result.155 Careful
instructions regarding skin monitoring are given to parents and
patients to avoid splint pressure necrosis. Radiographs are taken
weekly for the first 2 weeks and then every 2 weeks thereafter to
monitor for loss of reduction or volar joint subluxation.
grossly unstable, irreducible, or have unacceptable alignment. Closed
reduction and percutaneous fixation is preferred unless the fracture is
irreducible. Additional fixation of the dorsal fragment can be
accomplished with a 0.028-inch smooth Kirschner wire placed parallel to
the epiphysis. An irreducible fracture requires open reduction.
Fixation techniques vary depending on the age of the child and the
fracture configuration. Smooth wires, however, are the principle means
of fixation.
matrix (Seymour fractures) require nail plate removal, extrication of
the nail bed, and repair. Axial alignment after nail bed repair is
maintained with a splint or longitudinal fixation for 4 weeks (Fig. 8-22).
tendon disruption are treated similarly to adults with 4 to 6 weeks of
dorsal DIP joint splint immobilization. Operative repair of soft tissue
or bony mallet fingers rarely is indicated, even for chronic injuries.
Most chronic mallet injuries will heal with splint immobilization. The
loss of digital flexion associated with surgery can be more disabling
than a minor extension lag after an untreated injury.
 |
|
FIGURE 8-22 A. A 13-year-old boy sustained an open S-H type II fracture. B. The wound was cleansed, and acceptable alignment was obtained with closed reduction.
|
Too often, this injury is missed in the acute setting. Specific
examination for profundus function is necessary for diagnosis.
Bone-to-bone fixation is preferred using wires or suture. Fragments
that are too small for fixation require bone removal and repair of the
tendon directly to the fracture bed. This usually requires transosseous
sutures from volar to dorsal, avoiding injury to the germinal nail bed.
Repair of long-standing profundus avulsions is controversial and is
usually not recommended with an intact and functioning flexor digitorum
superficialis tendon.
bone is best treated by wound cleansing, dressing changes, and healing
by secondary intention. Acceptable functional and cosmetic results are
uniform. Skin or composite grafts are rarely necessary for coverage in
children and are associated with donor site morbidity,
hyperpigmentation, and lack of sensibility. Extensive soft tissue loss
with exposed bone requires more innovative coverage. A volar oblique
injury usually can be treated with a variety of local flaps, including
a V-Y advancement flap, cross finger flap, or thenar flap (see Figs. 8-20 and 8-21).
nail bed injury adds additional complexity. Mild loss can be treated by
local wound care. Moderate to severe loss may require a reverse
cross-finger flap or a more distant flap. Unfortunately, nail bed
replacement techniques often result in considerable nail deformity.
fractures are uncommon. Potential problems include nonunion, malunion,
and osteomyelitis. Nonunion and malunion are exceedingly rare, except
in open injuries that result in avascular
fracture
fragments or untreated widely displaced fractures. Osteomyelitis can
result from open fractures and requires application of the basic tenets
for the treatment of infected bone. Débridement, removal of any
sequestrum, and intravenous antibiotics are required to resolve the
infection. Additional tissue coverage is necessary in digits with a
marginal soft tissue envelope. These infections are rare due to the
robust vascularity of a child’s hand.
prevalent than bony problems. Difficulties may involve the skin,
subcutaneous tissue, nail, and tendons. An inadequate soft tissue
envelope can be reconstructed with replacement using a variety of local
flaps.
bed injury. Damage to the germinal matrix produces deficient nail
growth and nail ridging. Injury to the sterile matrix causes poor nail
adherence or nail ridging. Treatment options are limited and usually
involve resection of the damaged segment and replacement with a
full-thickness or split-thickness skin graft.31,170,214
Adjacent digits or toes are potential sources of nail bed transfers.
The results in children have been superior to those in adults.103,170,171,214
The hook-nail or “parrot’s beak” nail is a nail plate complication
related to the underlying bony deficit and volar, distal soft tissue
contracture. The nail plate curves over the abbreviated end of the
distal phalanx (Fig. 8-23). Treatment requires
restoring length to the shortened distal phalanx and creation of an
adequate soft tissue envelope to support the nail plate (Fig. 8-24).7 Usually, a thenar flap or composite graft is used to provide improved support for the nail bed in these situations.
pediatric mallet fracture treatment. No further treatment is warranted.
Severe DIP joint deformities are uncommon but may result in swan-neck
positioning of the finger. Reconstruction options are similar to
methods used in adults, such as a spiral oblique retinacular ligament
reconstruction or central slip tenotomy.192
In a young child, untreated lacerations proximal to the terminal tendon
insertion may result in an extensor lag that can be repaired
successfully with a dermodesis repair.43,99
 |
|
FIGURE 8-23 A hook-nail deformity of the small finger after a distal fingertip amputation.
|
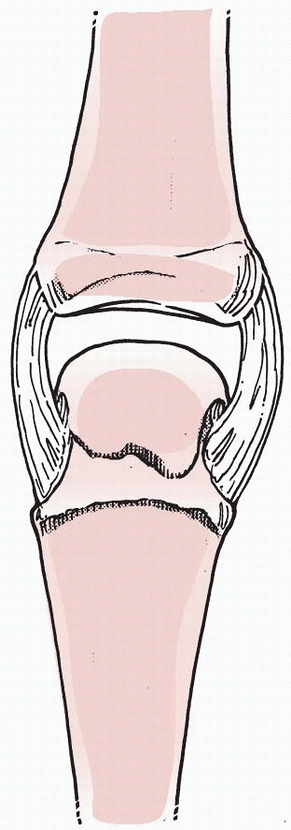
phalanges. The physis of the thumb metacarpal is also located in the
proximal portion, whereas the physes of the finger metacarpals are
located in the distal segment (see Fig. 8-1).
The collateral ligaments at the PIP and DIP joints originate from the
collateral recesses of the proximal bone and insert into both the
epiphysis and metaphysis of the distal bone (see Fig. 8-3).
The thumb MCP collateral ligaments resemble those of the
interphalangeal joints, having epiphyseal and metaphyseal insertions
(see Fig. 8-4). The collateral ligaments at
the MCP joints of the fingers originate and insert almost exclusively
onto the epiphyses of the opposing bones.
the epiphysis of the middle and distal phalanges. The flexor digitorum
superficialis inserts over about two thirds of the central portion of
the middle phalanx. The flexor digitorum profundus has a metaphyseal
insertion onto the distal phalanx.
result from some form of axial load combined with a torsional or
angular force, such as catching a ball or collision in sports. An
isolated lateral force across the PIP or MCP joint can lead to a
lateral fracture-dislocation. Crush injuries are less common in the
proximal and middle phalanges than in the distal phalanx.
amount of force incurred. There are four locations: the physis, the
shaft, the neck, and the condylar area (Table 8-3).
Extra-articular S-H II fractures are most prevalent, and
intra-articular S-H III and IV fractures are less common. Physeal
fractures about the middle phalanx can involve the lateral, dorsal, or
volar aspects of the physis. A lateral force across the PIP joint may
cause a S-H III or IV fracture. Similarly, a flexion force may produce
a dorsal S-H III fracture indicative of a central slip avulsion
fracture (pediatric boutonniere injury). A hyperextension injury
produces small avulsion fragments from the middle phalangeal epiphysis
associated with a volar plate injury.
to injury. An ulnar collateral ligament avulsion injury at the base of
the thumb proximal phalanx is similar to the adult gamekeeper’s or
skier’s thumb. The fracture pattern usually is a S-H III injury. The
ligament usually remains attached to the epiphyseal fracture fragment.
Fracture displacement with articular incongruity and joint instability
is common.183 Displaced injuries require open reduction and internal fixation to restore articular alignment and joint stability.
 |
|
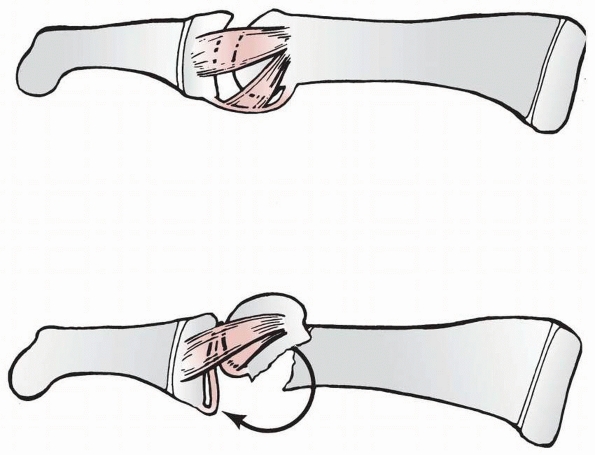
FIGURE 8-24 A,B.
Postoperative photographs of the patient shown in Figure 8-25 after the antenna procedure. The procedure involved a volar V-Y advancement flap to cover the distal tip, elevation of the sterile matrix, and the nail supported using three Kirschner-wires. C. Line drawings demonstrating technique of elevation and support of the sterile matrix with wires. (A,B. Courtesy of William B. Kleinman, MD. C. Reprinted from Atasoy E, Godfrey A, Kalisman M. The “antenna” procedure for the “hook-nail” deformity. J Hand Surg [Am] 1983;8:55, with permission.) |
fracture of the PIP joint, considered “pilon” fractures or
fracture-dislocations.184 These
injuries can occur in adolescent athletes and result from an axial load
sustained while catching a ball or contacting an opponent. Fracture
lines often propagate into the physis. The fracture fragment from the
volar side may have the volar plate attached, while the dorsal fragment
is likely to have the central slip attached. The central aspect of the
joint may be depressed and comminuted. The joint can be unstable and
incongruent, requiring careful treatment.
|
TABLE 8-3 Classification of Proximal and Middle Phalangeal Fractures
|
||||
|---|---|---|---|---|
|
fractures in children are less common. The fracture configuration may
be transverse, spiral, or spiral oblique. The fracture may be
comminuted. Proximal phalangeal fractures usually are angulated in an
apex volar pattern because the distal fragment is extended by the
central slip and lateral band and the proximal fragment is flexed by
the intrinsic musculature (Fig. 8-25). Oblique
fractures often rotate and shorten. Careful clinical evaluation of
rotational alignment is critical. Comminution is secondary to a
high-energy injury or direct trauma to the phalanx (Fig. 8-26).
fractures of the phalanx are problematic with regards to treatment and
functional outcome. Displaced neck fractures also are referred to as
subcondylar fractures and often occur in young children as a result of
finger entrapment in a closing door. The head fragment remains attached
to the collateral ligaments and tends to rotate into extension.46
This displacement disrupts the architecture of the subcondylar fossa,
which normally accommodates the volar plate and base of the phalanx
during interphalangeal joint flexion. Malunited neck fractures,
therefore, result in a mechanical block to interphalangeal
joint
flexion. Frequently, these fractures are inadequately imaged,
underappreciated, or misinterpreted as trivial and referred late for
care.
 |
|
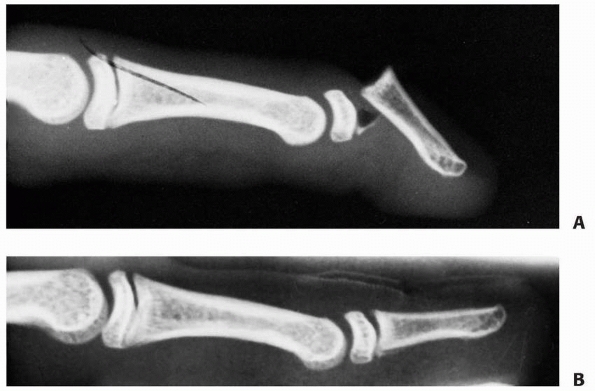
FIGURE 8-25 A,B.
Lateral and oblique radiographs of a transverse proximal phalangeal fracture that demonstrates the characteristic apex volar deformity. |
Condylar fractures involve the joint and represent a constellation of
fracture patterns, including small lateral avulsion fractures,
unicondylar or intracondylar fractures, bicondylar or transcondylar
fractures, and a rare shearing injury of the entire articular surface
and its underlying subchondral bone from the distal aspect of the
phalanx (Fig. 8-27). Condylar fractures can be
associated with subluxations or dislocations of the joint. Many of
these fractures are initially misdiagnosed as sprains.84,108 Restoration of articular alignment and joint stability is critical to a successful outcome.
phalangeal fractures begins with a high index of suspicion based on the
history and physical examination. Swelling and ecchymosis are the
clinical clues to an underlying fracture. The child usually refuses to
move the digit and resists passive motion. Mild fractures may not be
clinically apparent, and radiographs should be routinely obtained.
Every fracture must be carefully examined for malrotation and
rotational deformity regardless of radiographic appearance. Active or
passive movement can be used to detect malrotation of the fracture (see
Fig. 8-27). Active finger flexion will produce
deviation of the plane of the nails or overt digital scissoring.
Passive wrist extension will cause long finger flexor tenodesis, and
malrotation is evident by an abnormal digital cascade.
views are mandatory. Oblique radiographs are often helpful to determine
fracture configuration and alignment. Failure to recognize the extent
of injury is an ongoing problem, especially with unicondylar and
bicondylar fractures. These fractures may appear fairly normal on the
anteroposterior view, but a slight overlap of the subchondral surfaces
usually is present on the true lateral projection. This “double
density” shadow is made by the offset of the displaced condyle and
should not be regarded as a normal finding (Fig. 8-28).
Questionable radiographic findings can be further evaluated by
additional views, tomograms, or fluoroscopy. Phalangeal neck fractures
are too often interpreted as benign injuries.
fractures varies greatly with the location of injury. Nonoperative
treatment is predictable management for most physeal and shaft
fractures. Operative treatment is common for neck and condylar
fractures, especially fractures that are displaced or unstable.
proximal and middle phalanges can be managed by simple immobilization.
Displaced fractures often require closed reduction. A common fracture
pattern is a S-H II fracture along the ulnar aspect of
the
proximal phalanx of the small digit. The small digit is angulated in an
ulnar direction. This fracture has been termed the “extra-octave
fracture” to denote its potential benefit to the span of a pianist’s
hand (Fig. 8-29).153
Minimal displacement is treated with splinting in the safe position for
3 weeks. Moderate displacement requires closed reduction with local
anesthesia or conscious sedation. Placing the MCP joint into flexion to
tighten the collateral ligaments and angulating the digit into radial
deviation reduces the fracture. Placing a pencil or digit in the web
space and using it as a fulcrum to assist reduction has been
recommended.207 Minimal force is necessary to restore alignment.5,51 Buddy taping and cast immobilization will maintain alignment until healing.
 |
|
FIGURE 8-26 Comminuted fractures secondary to a crush injury with longitudinal splitting into the physis.
|
 |
|
FIGURE 8-27 A.
Anteroposterior radiograph of a S-H II fracture at the long finger proximal phalanx. The radiogaph reveals slight angulation and can appear benign. Clinical examination must be done to assess the digital cascade for malrotation. B. Tenodesis of the wrist with passive extension reveals unacceptable malrotation as evident by the degree of overlap of the middle finger on the ring finger. |
A variety of tissues, including periosteum and tendons, may prevent
reduction. Open treatment with removal of the impeding tissue and
fracture reduction is required for these rare injuries (Fig. 8-30).
In addition, some S-H II fractures may be reducible but unstable after
reduction. These fractures tend to be higher-energy injuries with more
disruption of the supporting soft tissues. Insertion of a smooth
Kirschner wire after reduction is required to maintain fracture
alignment.83,167
Another indication for operative management is a displaced S-H III
fracture of the proximal phalangeal base with a sizable (more than 25%)
epiphyseal fragment. Closed or open reduction may be required to
restore articular congruity.84,167 Small Kirschner wires can be inserted parallel to the joint surface, avoiding the physis. Tension-band wiring179
techniques can be used for S-H III and IV fractures. Operative exposure
and fixation techniques are challenging with nonborder digit proximal
phalangeal S-H III fractures.
 |
|
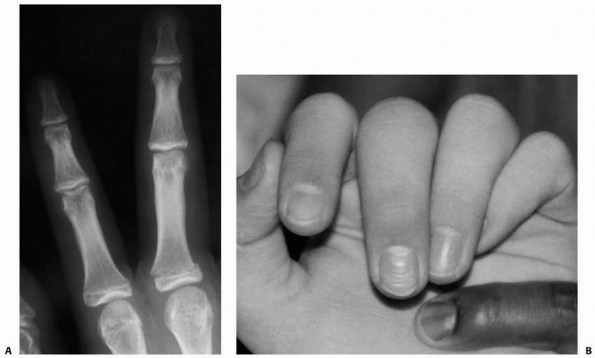
FIGURE 8-28 A. Anteroposterior radiograph reveals intra-articular fracture of the small finger. B. Lateral view demonstrates double density sign indicative of displacement (arrows).
|
 |
|
FIGURE 8-29 A. An extra-octave fracture in a 12-year-old girl. B. The fracture was reduced with the MCP joint in full flexion.
|
 |
|
FIGURE 8-30
Displaced S-H II fracture of the proximal phalanx that was irreducible. The distal fragment was herniated through a rent in the periosteum and extensor mechanism that prohibited reduction. |
and stable can be treated with simple immobilization. Safe position
splinting for 3 to 4 weeks should be adequate for clinical union.
Displaced or angulated fractures require closed reduction. The amount
of acceptable angulation in the plane of motion is controversial.172
In children less than 10 years of age, 20 to 30 degrees may be
acceptable. In children older than 10 years, 10 to 20 degrees
angulation is acceptable. Less angulation is acceptable in the coronal
plane. Malrotation is unacceptable.
irreducible by closed methods require operative intervention. A shaft
fracture that is unstable after reduction is managed by Kirschner-wire
fixation.181 Open reduction is
indicated for fractures that cannot be reduced. A dorsal approach
usually is used for exposure. The extensor tendon is split for proximal
phalangeal fractures and elevated for middle phalangeal fractures. The
choice of implant depends on the age of the patient and the fracture
configuration. Smooth wires or screws are preferable to plates to avoid
extensor mechanism adherence.90 Bone grafting alone has been described to provide rigid fixation to proximal phalangeal base fractures.186 All malrotated fractures require reduction and fixation.
of the phalangeal neck is difficult because these fractures often are
unstable (Fig. 8-31). Closed manipulation is
done with digital distraction, a volar-directed pressure on the distal
fragment, and hyperflexion of the PIP joint. Percutaneous pinning
usually is necessary to maintain the reduced position.46
Under fluoroscopy, Kirschner wires are inserted through the collateral
recesses and across the fracture. These wires should engage the
contralateral cortex proximal to the fracture site. An alternative
technique with a small distal fragment is to insert the pins through
the articular surface of the phalanx in a longitudinal fashion,
crossing the fracture to engage the proximal fragment.
 |
|
FIGURE 8-31
Phalangeal neck fractures often are unstable and rotated. These fractures are difficult to reduce and control by closed means because of the forces imparted by the volar plate and ligaments. (Reprinted from Wood BE. Fractures of the hand in children. Orthop Clin North Am 1976;7:527-534, with permission.) |
treated by immobilization. Weekly radiographs are necessary to ensure
maintenance of reduction. Displaced intra-articular fractures require
closed or open reduction.167 Closed
or percutaneous reduction can be accomplished with traction and use of
a percutaneous towel clip or reduction clamp to obtain provisional
fracture reduction. Percutaneous fixation is used for definitive
fracture fixation. Fractures not appropriate for closed manipulation
require open reduction and internal fixation (Fig. 8-32).
A dorsal, lateral, or even volar incision is used for direct inspection
of the fracture and articular surface. Care is taken to preserve the
blood supply of the fracture fragments entering through the collateral
ligaments. Fracture stabilization is by either Kirschner wires or
miniscrews.
difficult to treat. Shear fractures and osteochondral slice fractures
are difficult to recognize. Treatment is open reduction and smooth wire
fixation. Osteonecrosis, especially of small fragments, is a concern.
Some of these fractures require a volar surgical approach. Avoidance of
extensive soft tissue dissection lessens the risk of osteonecrosis.
are uncommon in children. Operative intervention is usually required to
restore articular congruity. Anatomic reduction is preferred whenever
possible (Fig. 8-33).185
Bone grafting may be necessary for stable reduction. Extreme joint
comminution may preclude anatomic reduction, and alternative treatment
options, such as dynamic traction, may be necessary.2,166
structures, and bone may all be injured in the same digit (Fig. 8-34).
Open fracture care is mandatory, followed by establishment of a stable
bony foundation. Markedly comminuted fractures or injuries with bone
loss may require external fixation followed by delayed bony
reconstruction. Neurovascular and tendon reconstruction in children
follows the same principles as for adults. Rehabilitation of complex
injuries in children can be complicated by a lack of cooperation.
Vascular injuries can affect subsequent growth.
 |
|
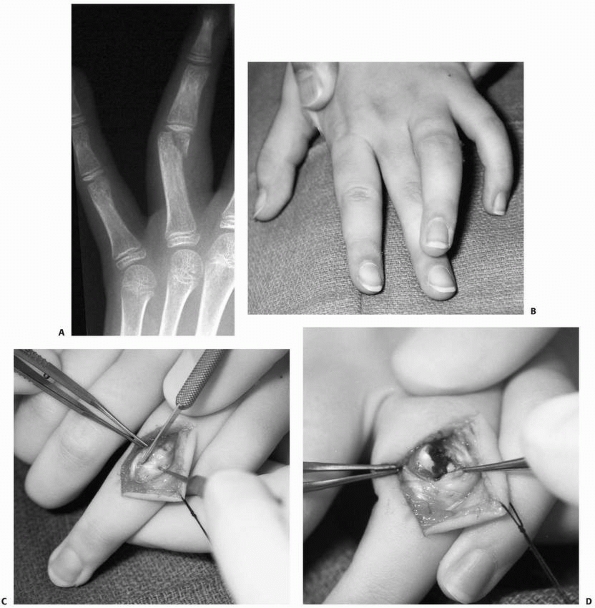
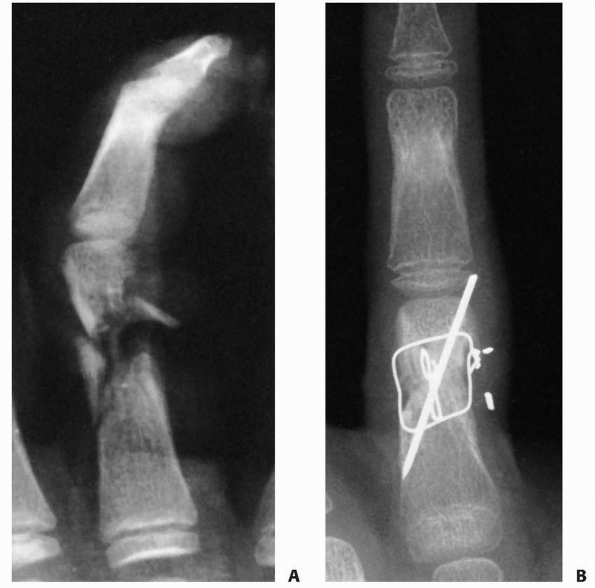
FIGURE 8-32 A. A 10-year-old girl with a displaced unicondylar fracture of the ring finger proximal phalanx. B. Clinical examination reveals malrotation of the digit. C. Dorsal exposure with incision between lateral band and central slip. D. Exposure of displaced fracture fragment. (continues)
|
 |
|
FIGURE 8-32 (continued) E. Fracture reduced with Kirschner-wire fixation. F.
Postoperative radiograph shows restoration of articular surface. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.) |
 |
|
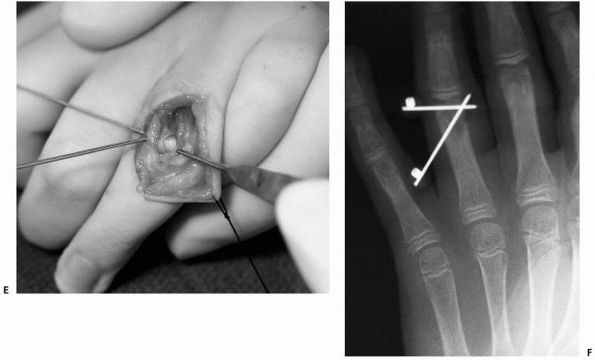
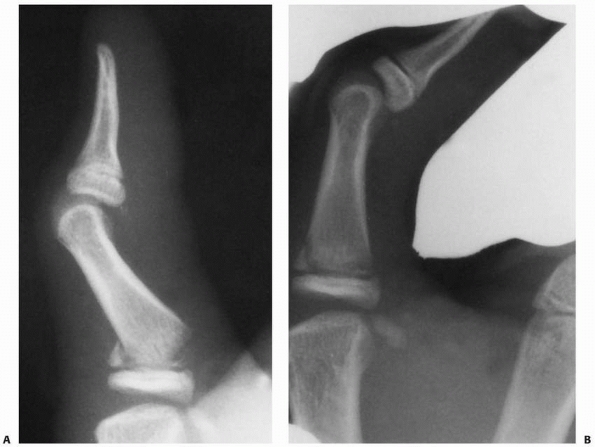
FIGURE 8-33 A. A 16-year-old girl with a severe intra-articular pilon fracture of the small finger PIP joint. B. Traction radiograph helps define fracture components. (continues)
|
 |
|
FIGURE 8-33 (continued) C. Dorsal exposure revealed ulnar condyle outside of joint requiring incision of extensor tendon for reduction. D. Reduction of joint surface and Kirschner-wire fixation. E. Postoperative anteroposterior radiograph shows restoration of articular surface. F. Lateral radiograph shows sagittal alignment of condyles. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.)
|
immobilization for 3 weeks. Most displaced S-H I and II fractures can
be treated with closed reduction (Fig. 8-35).
Alignment and rotation is verified clinically and reduction is assessed
with radiographs. The hand is immobilized in a safe-position splint,
and a radiograph is obtained 5 to 7 days later to ensure maintenance of
reduction. When there is doubt about anatomic alignment, the cast is
removed for more thorough clinical and radiographic examinations.
Immobilization is continued for 3 to 4 weeks. Physeal fractures that
are unstable after closed reduction require percutaneous pin fixation.
Small smooth wires are used to secure the reduction. Irreducible
fractures require open reduction, removal of any interposed tissue, and
fixation.
proximal phalanges are difficult to reduce and maintain by closed
methods. Dorsal S-H III or IV fractures of the middle phalangeal base
often require open reduction and fixation to avoid
the development of a boutonniere deformity (Fig. 8-36).
A dorsal approach, with an incision between the central tendon and the
lateral band, is preferred. The PIP joint may require supplemental pin
fixation for 3 weeks to permit healing. Lateral S-H III fractures that
are displaced more than 1.5 mm or involve more than 25% of the
articular surface also may require open reduction and internal
fixation. This fracture pattern is especially common in the proximal
phalanx of the thumb.
 |
|
FIGURE 8-34 A. A 14-year-old boy sustained a near-amputation of his ring digit with severe soft tissue injury. B. 90-90 intraosseous wiring supplemented with Kirschner-wire fixation to provide a stable base for soft tissue repair.
|
 |
|
FIGURE 8-35 A. A S-H II fracture of the proximal phalanx of the thumb. B. Gentle closed reduction under fluoroscopic control obtained an anatomic reduction.
|
 |
|
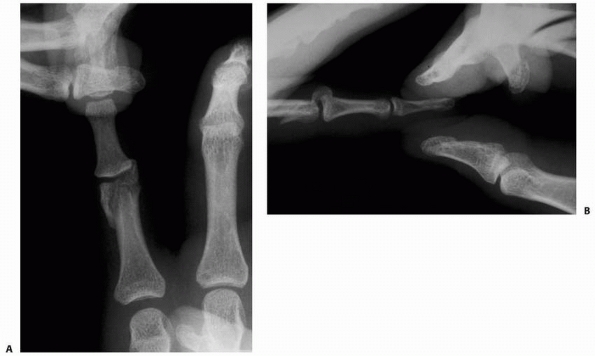
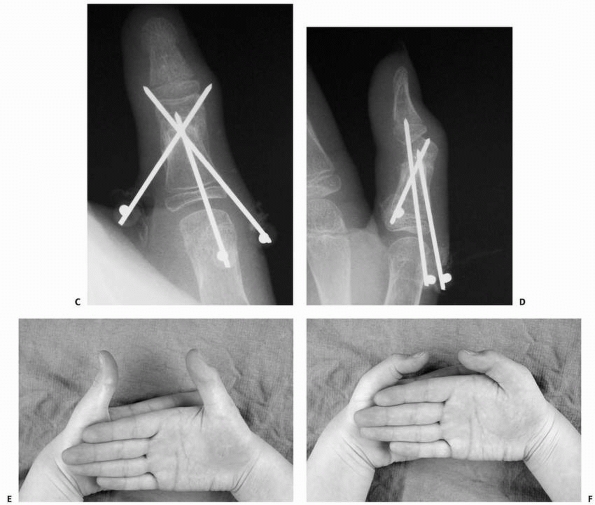
FIGURE 8-36 A,B. A 16-year-old male sustained a dorsal S-H IV fracture of the middle phalanx. C,D.
Open reduction and internal screw fixation were accomplished through a dorsal approach. Radiographs show reduction of joint subluxation and fixation of fracture fragment. E,F. Postoperative extension and flexion with near normal motion. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.) |
for 3 to 4 weeks. Displaced fractures are treated with closed reduction
and percutaneous pin fixation.72
Reduction is accomplished with longitudinal traction and rotation of
the distal fragment to approximate the proximal fragment. For a
proximal phalangeal fracture, the MCP joint is flexed to relax the
intrinsic muscle pull and to stabilize the proximal fragment. The
fracture orientation dictates the angle of pin
insertion.
Optimal pin placement is perpendicular to the fracture line. Placement
of the pins in the midaxial line prevents iatrogenic injury of the
neurovascular structures or entrapment of the extensor mechanism by the
pin. Open reduction is reserved for irreducible fractures.
If closed reduction is obtainable, then percutaneous pin fixation is
performed. The pins are placed through the collateral recesses to
engage the proximal fragment in a crossed fashion. If closed reduction
is unsuccessful, open reduction with preservation of the collateral
ligaments and similar percutaneous pinning are indicated. However, open
reduction should be avoided whenever possible to decrease the chances
of osteonecrosis.
consideration of the time from injury and fracture displacement.
Considerable displacement requires treatment to regain joint flexion (Fig. 8-37).
If the fracture line is still visible, a percutaneous pin osteoclasis
may be possible. Under fluoroscopy, one or two smooth Kirschner wires
are inserted into the fracture site to break up any callus. These
Kirschner wires are used to “joystick” the distal fragment into a
reduced position.201 The fracture is
then stabilized with additional percutaneous pins. This approach may
decrease the risk of osteonecrosis associated with late open reduction.
A nascent or established malunion that cannot be reduced by osteoclasis
can be treated by late open reduction (Fig. 8-38).
The callus is gently removed and the fracture aligned. The risks of
osteonecrosis must be weighed against acceptance of the malunion. Mild
loss of the condylar recess can be treated with recession of the
prominent volar bone rather than risk osteonecrosis associated with
extensive fracture mobilization.173,189
In addition, slow remodeling is feasible in very young children without
rotational malalignment and with a family that is willing to wait up to
2 years for remodeling.36,85
 |
|
FIGURE 8-37
Displaced phalangeal neck fracture of the proximal phalanx revealing loss of subchondral fossa at the PIP joint. If this is not corrected to anatomic alignment, there will be a mechanical block to flexion. |
 |
|
FIGURE 8-38 A. A 14-year-old girl with incipient malunion of right thumb proximal phalanx neck fractures that impede flexion. B. Lateral radiograph reveals loss of the subchondral fossa. (continues)
|
 |
|
FIGURE 8-38 (continued) C. Anteroposterior view after open reduction and Kirschner-wire fixation. D. Oblique view reveals restoration of subchondral fossa. E,F.
Postoperative flexion and extension compared to the other side. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.) |
require percutaneous or open reduction. Unicondylar fractures that are
mildly displaced can be treated with closed reduction and percutaneous
pinning. Widely displaced unicondylar and bicondylar fractures require
open reduction (see Fig. 8-32). A dorsal
approach is preferred. Fixation usually is obtained with smooth wires.
The placement and direction are dictated by the fracture configuration.
Rotational control of the fragment may require multiple wires. The
fixation device must avoid tethering of the collateral ligament, which
will limit motion. Usually, a pin is placed parallel to the joint to
maintain articular alignment, followed by oblique pins to stabilize the
articular fragment(s) to the shaft. In adolescents, miniscrew fixation
can be used. These screws must avoid impingement of the collateral
ligaments, which will impede flexion.
Open reduction is worthwhile when the fragments are large and the joint
surface can be reconstructed. Bone grafting may be necessary for stable
reduction. Severe articular damage and comminution are treated with
dynamic traction.
intervention for phalangeal fractures is usually 3 to 4 weeks.
Percutaneous pins are removed at that time and motion instituted.
Formal hand therapy usually is not required, although the child must be
encouraged to re-establish a normal usage pattern to improve motion and
flexibility. Periarticular fractures are monitored closely for
persistent loss of motion that would benefit from formal hand therapy.
Patients with complex fractures or replantations are more prone to
develop stiffness. In these instances, therapy is routinely prescribed
to regain motion. Therapy is directed at both flexion and extension of
the injured
digit.
Static or dynamic splinting may be required after fracture healing.
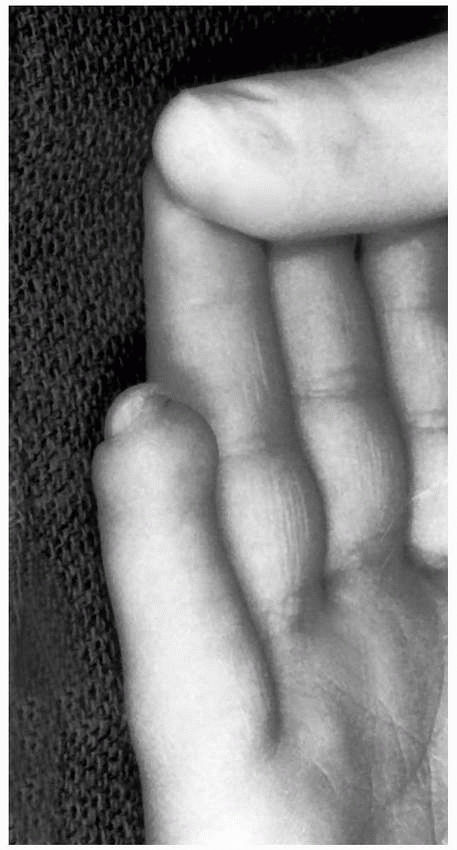
Persistent stiffness may require tenolysis and joint release to regain
motion (Fig. 8-39).
phalangeal fractures are positive. Considering the frequency of these
fractures, the occurrence of complications and functional impairment is
low. Despite appropriate treatment, however, some children have
permanent loss of motion, malunion, or growth disturbance. The major
concern is to avoid rotational, articular, or periarticular malunion
due to inappropriate diagnosis or treatment.
 |
|
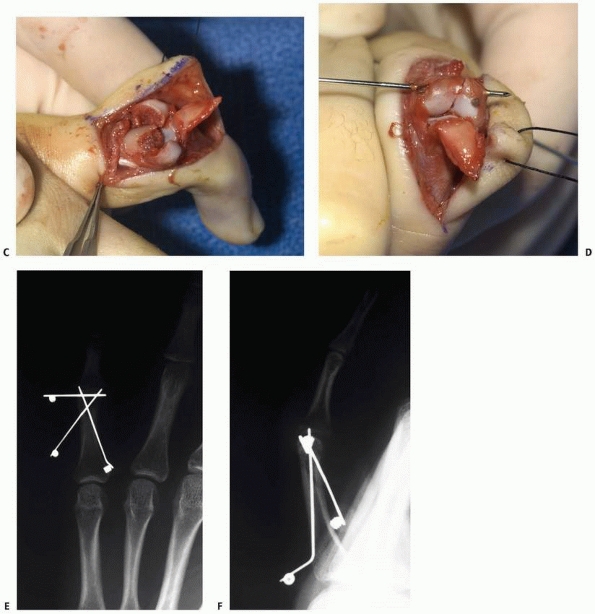
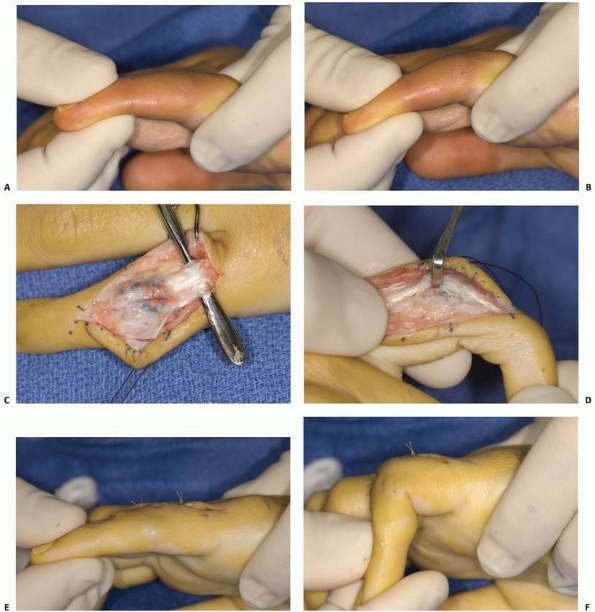
FIGURE 8-39
A 16-year-old girl with a severe intra-articular pilon fracture of the small finger PIP joint depicted in Figure 8-33 with healed fracture, but limited motion after therapy. A. Passive extension B. Passive flexion. C. Dorsal exposure and tenolysis under local anesthesia with sedation. D. Joint release. E. Passive extension. F. Passive flexion. (continues) |
correctly and scrutinized for subtle abnormalities. Questionable
findings warrant additional views or advanced imaging studies. A common
misdiagnosis is failure to recognize a displaced phalangeal neck
fracture because of inadequate lateral radiographs of the fracture.
 |
|
FIGURE 8-39 (continued) G. Active flexion. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.)
|
 |
|
FIGURE 8-40 A.
A 3-year-old girl sustained a fracture of the neck of the proximal phalanx of the index and middle fingers. The displaced fracture in the middle finger appears similar to an epiphysis at the distal end of the phalanx. B. No true lateral radiograph of the injured finger was obtained. Close scrutiny of this lateral view shows a dorsally displaced neck fracture, rotated almost 90 degrees (arrow). C. Eighteen months later, lateral radiograph reveals malunion with hyperextension of the PIP joint and loss of flexion. |
“nondisplaced” fracture that is malrotated. All children with
phalangeal fractures require careful examination for rotational
alignment. The clinical examination is the mainstay for determining
fracture rotation. Digital scissoring is indicative of fracture
malrotation and requires reduction. Regardless of radiographic
appearance, rotational alignment should be evaluated by active finger
flexion and passive tenodesis.
satisfactory alignment after closed reduction. Certain fractures,
however, have a propensity for redisplacement (Fig. 8-41).
Oblique shaft fractures, unicondylar articular fractures, and neck
fractures are prime examples. Early follow-up to ensure maintenance of
reduction is paramount if closed treatment is chosen. Displacement
requires repeat manipulation and pin fixation. When in doubt, the digit
should be examined carefully for malalignment and blocks to motion due
to fracture displacement. Most of these fractures do best with pin
fixation after acceptable reduction.
osteonecrosis, growth disturbance, and arthritis. Nonunion is rare
except in combined injuries with devascularization of the fracture
fragments.
Bone grafting is usually successful. Malunion can result in angulation
or limited motion. Extra-articular malunion can cause angulation or
rotational abnormalities. The treatment depends on the child’s age and
ability to remodel according to fracture location, plane of malunion,
and degree of deformity (Fig. 8-42). Considerable deformity may require osteotomy to realign the bone.67
A subcondylar or intra-articular malunion is particularly difficult to
treat. Early diagnosis within the first month offers the possibility of
fracture realignment through the site of deformity. Treatment of a late
diagnosis must include consideration of the risks and benefits
associated with extensive surgery.
 |
|
FIGURE 8-41 A,B. An 8-year-old girl with a mildly displaced fracture of the neck of the middle phalanx. C. Closed reduction was successful on the day of injury and a plaster splint was applied. D. Two weeks later, the fracture had markedly redisplaced.
|
comminution, soft tissue injury, or surgical dissection of an
intra-articular fracture. In severe cases, reconstruction is limited to
some form of joint transfer. Growth disturbance can result from any
injury that involves the physis. A shortened or angulated digit may
result. It is fortunate that this complication is rare because
reconstruction options for growth are limited. Malangulation is
corrected by osteotomy.
children, but intra-articular injury and sepsis may result in
arthrosis. Treatment is directed toward the child’s symptoms and not
the radiographic findings. Minimal pain and excellent function often
accompany considerable arthritic changes on radiographs and warrant no
treatment. Pain and functional limitations require treatment; options
include a vascularized joint transfer, interposition or distraction
arthroplasty, prosthetic joint replacement, and arthrodesis.174
relatively protected within the hand. Considerable variation exists in
the relative mobility of the metacarpals through the carpometacarpal
(CMC) joints. The index and long rays have minimal CMC joint motion (10
to 20 degrees). In contrast, the ring and small rays possess more
motion (30 to 40 degrees), and the thumb CMC joint has universal motion.
The metacarpal geometry and composition predispose the metacarpal neck
to injury. The distal metacarpal angles as it approaches the MCP joint,
and the cortical bone within the subcondylar fossa is relatively thin,
which creates a vulnerable area susceptible to injury.
all cause fractures of the metacarpal. Contact sports or striking an
object are the most common mechanisms.
 |
|
FIGURE 8-42 A. A 13-year-old boy with malunion of the ring finger middle phalanx articular surface. B,C.
Radiographs reveal slight malunion of the radial condyle with mild intra-articular incongruity. The lateral view suggests a double density shadow (arrow). The flexion and extension motion of the digit was normal, and reconstruction was not recommended. |
fractures of the metacarpal head are rare but occur most often in the
small ray.11,26,84,111 S-H II fractures of the small metacarpal are most common among patients 12 to 16 years of age.111,122,140
Intra-articular, head-splitting fractures at the metacarpal epiphysis
and physis consistent with S-H III and IV patterns seldom occur at the
metacarpal level but are problematic when displaced (Fig. 8-43).
most frequent site of metacarpal fractures in children. Neck fractures
in children are analogous to boxer’s fractures in adults (Fig. 8-44).
Neck fractures are more common in the small and ring fingers.
Fortunately, these injuries are juxtaphyseal and have considerable
remodeling potential.
are relatively common. Torsional forces cause oblique and spiral
fractures while direct trauma produces transverse fractures. An
isolated shaft fracture of a central ray is suspended by the
intermetacarpal ligaments, which limit displacement and shortening. In
contrast, the border digits (index and small) displace more readily.
|
TABLE 8-4 Classification of Finger Metacarpal Fractures
|
||||
|---|---|---|---|---|
|
 |
|
FIGURE 8-43 A. S-H type II fracture of the metacarpal head. B. Head-splitting fracture of the metacarpal epiphysis.
|
 |
|
FIGURE 8-44 A. A true boxer’s fracture of the metacarpal neck of the fifth ray. B. This fracture is more in the diaphysis and should not be considered a boxer’s fracture.
|
uncommon in children. The base is protected from injury by its proximal
location in the hand and the stability afforded by the bony congruence
and soft tissue restraints. The small finger CMC joint is the most
prone to injury. Fracture-dislocations of the small finger CMC joint
are often unstable because of the proximal pull of the extensor carpi
ulnaris (reverse Bennett fracture).
is based on the history and physical examination. Deformity and
swelling may be hidden in the dorsal hand. The child usually avoids
active movement and resists passive motion. Every metacarpal fracture
must be examined for malrotation. Malrotation will result in digital
scissoring during active flexion or an abnormal digital cascade with
passive tenodesis.
readily visible on radiographs. Anteroposterior and lateral views may
be supplemented by an oblique view to assess fracture configuration. A
metacarpal head splitting fracture may be difficult to detect and
requires special views. The Brewerton view is helpful and is made with
the dorsum of the hand against the cassette and the MCP joints flexed
about 65 degrees. The central beam is angled 15 degrees to the ulnar
side of the hand.104 This projection
focuses on the metacarpal heads and may highlight subtle bony
abnormalities. MRI scans to assess articular alignment are diagnostic
in complex injuries.
location, extent, and configuration of the fracture. Nonoperative or
closed treatment is the primary mode of management for most fractures.
Operative intervention is used for multiple metacarpal fractures,
extensive soft tissue injury, intra-articular head splitting fractures,
malrotated fractures, and irreducible fractures.
the amount of displacement and fracture stability. Many of these
fractures can be treated by closed methods. Gentle reduction under
metacarpal or wrist block anesthesia is followed by application of a
splint in the safe position. If the fracture is reducible but unstable,
percutaneous pin fixation is recommended. If the Thurston-Holland
fragment is large enough, the wire can secure the metaphyseal piece and
avoid the physis. Otherwise, the wire must cross the physis to obtain
stability. A small-diameter smooth wire is advocated, and multiple
passes should be avoided.
require open reduction and internal fixation to restore articular
congruity. Many of these fractures have unrecognized comminution that
complicates internal fixation. Wire or screw fixation is used,
depending on the age of the patient and size of the fragments.
Transosseous suture repair may be necessary. Bone grafting may be
necessary for stable reduction. The primary goal of surgical treatment
is anatomic reduction of the joint. A secondary goal is stable fixation
to allow early motion.
is controversial. Greater angulation is allowable in the mobile ring
and small rays compared to the index and long. Another consideration is
the effect of remodeling over time, which is dependent on the age of
the child. In general, 10 to 30 degrees of angulation greater than the
corresponding CMC joint motion is acceptable.
reduction with local anesthesia or conscious sedation and splint or
cast application. The Jahss maneuver is commonly recommended and
involves initial flexion of the MCP joint to 90 degrees to relax the
deforming force of the intrinsic muscles and tighten the collateral
ligaments.93 Subsequently, upward
pressure is applied along the proximal phalanx to push the metacarpal
head in a dorsal direction while counterpressure is applied along the
dorsal aspect of the proximal metacarpal fracture. Jahss93
suggested immobilization with the MCP and PIP joints flexed, but this
type of immobilization is no longer advocated for fear of stiffness and
skin breakdown. Immobilization in the intrinsic plus or safe position
is the appropriate position. A well-molded splint or cast is necessary.
Three-point modeling over the volar metacarpal head and proximal dorsal
shaft is recommended. The PIP joints may or may not be included in the
immobilization depending on the status of the reduction and reliability
of the patient.
 |
|
FIGURE 8-45 A,B. A 14-year-old boy with a dorsally angulated fracture of the second metacarpal. C.
Closed reduction was unstable, and percutaneous Kirschner-wire fixation was performed. (Reprinted from O’Brien ET. Fractures of the hand. In: Green DP, ed. Operative Hand Surgery. 2nd ed. New York: Churchill Livingstone, 1988: 715-716, with permission.) |
Pins can be inserted in a variety of configurations. Extramedullary
techniques include crossed pinning or pinning to the adjacent stable
metacarpal. Intramedullary techniques also can be used, similar to
those used for metacarpal shaft and neck fractures in adults.57,68
Intramedullary techniques are reserved for patients near physeal
closure. Prebent Kirschner wires or commercially available implants are
inserted through the metacarpal base in an antegrade fashion. The wires
can be used to assist in fracture reduction. Stability is obtained by
stacking several wires within the canal and across the fracture site.
required in children and is reserved for irreducible fractures,
unstable fractures in skeletally mature children, multiple metacarpal
fractures, and combination injuries that require a stable bony platform.
fracture is often minimally displaced because the metacarpals are
suspended by the intermetacarpal ligaments. Immobilization for 4 weeks
is usually all that is necessary. In contrast, the index and small
digits may require additional treatment, such as closed reduction and
immobilization. Percutaneous pinning is reserved for unstable shaft
fractures (Fig. 8-46). Pins can be inserted
with extramedullary or intramedullary techniques. Diaphyseal fractures
are slower to heal and more prone to malunion than neck fractures.
shaft fracture are rarely indicated in children unless there are
multiple fractures or extensive soft-tissue damage or the child is
skeletally mature. However, a long spiral-oblique fracture with
substantial malrotation and shortening may require miniscrew fixation
to re-establish alignment.
 |
|
FIGURE 8-46 A 14 year-old boy with a reducible, but unstable, ring finger metacarpal shaft fracture. A. Anteroposterior radiograph appears reduced. B. Lateral radiograph with persistent apex dorsal angulation. C. Anteroposterior radiograph after closed reduction and percutaneous pinning. D. Lateral radiograph with anatomic alignment. (continues)
|
base or fracture-dislocations at the CMC joint are usually high-energy
injuries with substantial tissue disruption. Assessment for signs of
compartment syndrome and careful neurovascular assessment are
mandatory. Isolated fracture-dislocations of the small ray CMC joint
are the most common metacarpal base fractures. CT scans may better
define articular congruity and comminution. Closed reduction and
percutaneous pinning are usually sufficient to restore alignment and to
resist the deforming force of the extensor carpi ulnaris.162 The pins can be placed transversely between the small and ring metacarpals and/or across the CMC joint.
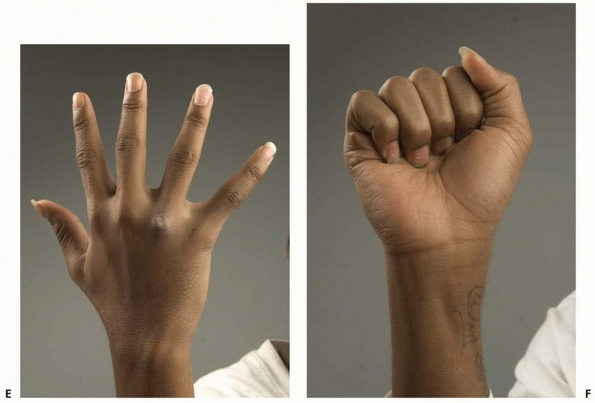 |
|
FIGURE 8-46 (continued) E. Full extension after pin removal and home therapy. F. Full flexion with normal digital cascade. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.)
|
ensure stable fixation in high-energy injuries. A transverse or
longitudinal incision can be used for exposure. Longitudinal incisions
are recommended in patients with concomitant compartment syndrome to
allow for simultaneous decompression. Fixation options are numerous,
depending on the fracture configuration. Supplemental bone graft may be
necessary for substantial comminution. Late presentation is especially
difficult. Treatment often requires open reduction or CMC arthrodesis (Fig. 8-47).
immobilization. S-H II metacarpal neck fractures seldom require
reduction. These fractures typically occur in adolescents who possess
enough remodeling to accept 30 to 35 degrees of sagittal angulation as
long as rotation is acceptable and there is sufficient growth
remaining. A widely displaced fracture that is reducible requires
percutaneous pinning to maintain the reduction. Displaced epiphyseal
fractures with considerable intra-articular displacement require open
reduction and internal fixation through a dorsal approach and splitting
of the extensor apparatus over the MCP joint. Anatomic reduction of the
articular surface is the objective, and fixation devices vary according
to the patient and fracture configuration.
treatment. Considerable sagittal angulation is acceptable, especially
in the ring and small digits. Small finger angulation up to 30 degrees
usually does not necessitate closed reduction as long as there is no
malrotation and there is sufficient growth remaining. Greater
angulations are treated with closed reduction and cast application.
Index and ring finger angulations of more than 20 degrees are treated
by closed reduction. Pin fixation is used for unstable fractures that
have a tendency to redisplace. Open reduction rarely is necessary.
metacarpal shaft fracture(s) dictate treatment. Isolated fractures that
are minimally displaced require only immobilization. Isolated fractures
that are displaced or malrotated require closed reduction and
percutaneous fixation. Rotation is carefully assessed to ensure
adequate reduction. An irreducible fracture or multiple fractures
usually require open reduction (see Fig. 8-46).
The fixation technique varies according to the age of the child and
fracture pattern. If open fixation is necessary, stable fixation is the
goal. Miniplate and screw fixation is preferred to restore alignment
and to allow early mobilization of tendons and soft tissue. The physis
should be avoided during plate application to prevent growth
disturbance. The operative approach and internal fixation principles
are similar in children and adults. Long oblique fractures are managed
with interfragmentary screw fixation. Short oblique and transverse
fractures require a neutralization plate with purchase of four cortices
proximal and distal to the fracture.
unstable. Extra-articular fractures can be treated by closed reduction
with or without percutaneous pinning. Intra-articular
fracture-dislocations
are
more challenging. Percutaneous pinning is often required to stabilize
the fracture and to reduce CMC joint subluxation. The wires are placed
between the bases of the adjacent metacarpals or across the CMC joint
in isolated injuries. Irreducible or multiple fracture-dislocations
require open reduction. Late presentation with symptomatic degenerative
changes requires CMC arthrodesis (see Fig. 8-47).
 |
|
FIGURE 8-47
A 15-year-old boy with crush injury of the right hand requiring compartment release. He presented 6 weeks later with persistent pain and limited motion. A. Anteroposterior radiograph with overlapping long, ring, and small CMC joints B. Lateral radiographs show fracture-dislocations of long, ring, and small CMC joints. C. Postoperative anteroposterior radiograph after reduction and CMC fusion using mini-plates. D. Lateral radiograph after reduction and CMC fusion. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.) |
are immobilized for 4 weeks. Subsequently, a home program of
range-of-motion exercises is started and formal therapy is not needed.
In active children and young athletes, a light splint can be worn for
protection and as a peer warning signal for an additional few weeks. If
percutaneous pin fixation is used, the wires are removed in the office
4 weeks after surgery.
of the fixation and the dependability of the patient. Older and
reliable patients with stable internal fixation are mobilized earlier,
usually 5 to 7 days after surgery. A removable splint for protection
between exercise sessions is used for 4 to 6 weeks.
sequelae. Mild deformity in the plane of motion is tolerated and may
correct with remodeling. Considerable angulation or rotation creates a
functional impairment that requires treatment.
Even a small amount (less than 10 degrees) of rotational malalignment
may create overlap of the digits during flexion and a functional
disturbance (Fig. 8-48). Corrective osteotomy
to realign the digit is often necessary. The osteotomy for rotational
correction can be made at the site of fracture or anywhere along the
metacarpal. The proximal shaft or base has certain advantages. This
area provides ample bone for healing and offers the opportunity for
internal fixation using wires or a plate. Diaphyseal malunions with
symptomatic flexion deformity into the palm require a dorsal wedge
osteotomy and internal fixation.
intra-articular fracture. Factors include the degree of injury and the
intracapsular pressure caused by the hemarthrosis.39,122,151
Theoretically, early joint aspiration may diminish the intra-articular
pressure. Fortunately, partial osteonecrosis in a growing child incites
remarkable remodeling of the adjacent articular surface and often
results in a functional joint. Part-time splint protection during the
remodeling phase is recommended. Considerable joint incongruity is
rare, and reconstruction options are limited.174
thenar muscles play a role in fracture mechanics and can displace
metacarpal fractures. Their directions of pull dictate the direction of
fracture displacement and deformity. The adductor pollicis inserts onto
the proximal phalanx and into the extensor apparatus through the
adductor aponeurosis. Epiphyseal fragments of the proximal phalanx base
with the attached ulnar collateral ligament (UCL) can displace outside
the adductor aponeurosis.183 This
pediatric “Stener lesion” prohibits healing and requires open
reduction. The abductor pollicis longus inserts onto the metacarpal
base and is the primary deforming force in most fracture-dislocations
about the thumb CMC joint (Bennett fractures or pediatric equivalents).
|
TABLE 8-5 Adverse Factors for Finger Metacarpal Fractures
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
all cause thumb metacarpal fractures. Sporting endeavors are the prime
events causing fractures. A valgus force to the MCP joint usually
produces an epiphyseal fracture. Skiing and extreme biking are specific
activities that place the thumb MCP joint and metacarpal shaft in a
vulnerable position. Adduction forces, such as direct trauma to a
soccer goalie or basketball player during a fall or ball injury, place
the thumb CMC joint and base of thumb metacarpal at risk.
epiphysis, physis, neck, shaft, or base. Fractures of the neck and
shaft and their treatment principles are similar to those of the
fingers (Table 8-6). Thumb metacarpal base fractures that involve the physis or epiphysis require particular mention (Fig. 8-49).
of the thumb metacarpal are subdivided according to their location.
Type A fractures occur between the physis and the junction of the
proximal and middle thirds of the bone. They often are transverse or
slightly oblique. There often is an element of medial impaction, and
the fracture is angulated in an apex lateral direction (Fig. 8-50).
metacarpal base. Most patterns have the metaphyseal fragment on the
medial side (type B) (see Fig. 8-49). The
shaft fragment is adducted by the pull of the adductor pollicis and
shifted in a proximal direction by the pull of the abductor pollicis
longus. Although this pattern resembles a Bennett fracture with respect
to the deforming forces, there is no intra-articular extension.13
Type C fractures are the least common and have the reverse pattern,
with the metaphyseal fragment on the lateral side and the proximal
shaft displacement in a medial direction. This pattern often results
from more substantial trauma and does not lend itself to closed
treatment.
fracture usually is straightforward. Swelling and ecchymosis are
obvious signs of injury. Most of the swelling appears about the thenar
eminence and at times can be marked. Active thumb motion is limited,
and passive thumb movement is painful. The thumb may appear angulated
or rotated. However, thumb motion is oriented differently than finger
movement, which makes angulation and malrotation more difficult to
judge.
the fingers are required. Biplanar radiographs ensure adequate
evaluation of fracture position. A hyperpronated view of the thumb
accentuates the view of the CMC joint.
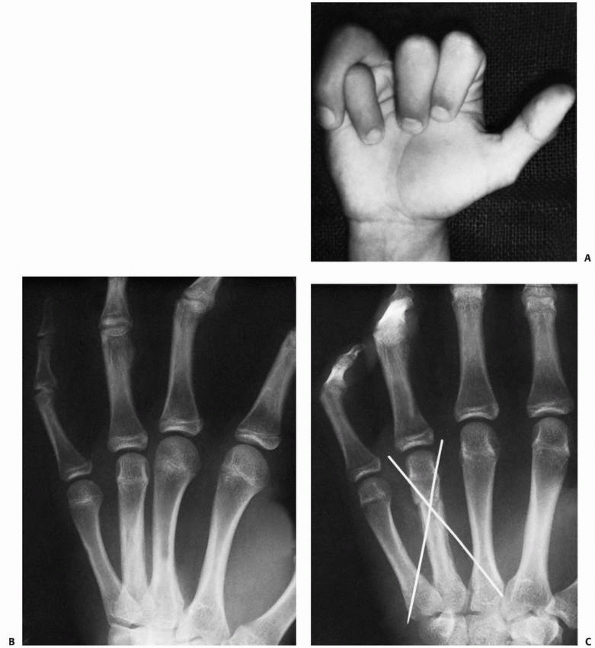 |
|
FIGURE 8-48 A,B.
A 15-year-old boy with severe overlapping of the ring finger on the little finger secondary to rotatory malunion of a spiral fracture of the ring metacarpal. C. Distal osteotomy through the deformity stabilized with pin fixation to correct the malrotation. (Reprinted from O’Brien ET. Fractures of the hand. In: Green DP, ed. Operative Hand Surgery. 2nd ed. New York: Churchill Livingstone, 1988:731, with permission.) |
|
TABLE 8-6 Classification of Thumb Metacarpal Fractures
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||
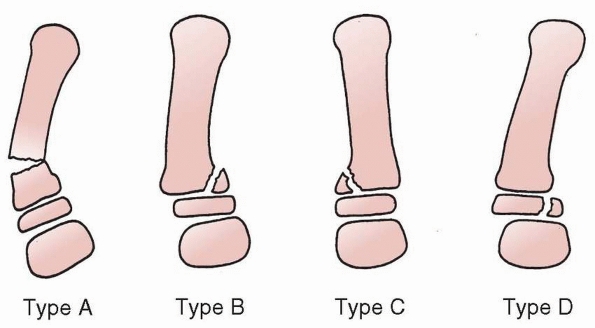 |
|
FIGURE 8-49
Classification of thumb metacarpal fractures. Type A: Metaphyseal fracture. Types B and C: S-H type II physeal fractures with lateral or medial angulation. Type D: S-H type III fracture (pediatric Bennett fracture). |
 |
|
FIGURE 8-50
Metaphyseal thumb metacarpal fracture that does not involve the physis. Treatment consisted of closed reduction and cast immobilization. |
 |
|
FIGURE 8-51 A 13-year-old boy fell down stairs and injured his right thumb A. Anteroposterior radiograph with displaced fracture base of the thumb metacarpal B. Lateral radiograph shows considerable angulation. (continues)
|
usually can be treated by closed methods. Although swelling about the
thenar eminence limits manipulation of the fracture and diminishes the
effectiveness of immobilization, most fractures can still be treated
successfully by closed reduction and immobilization. The CMC joint has
near universal motion, and the physis is proximal in the metacarpal, so
remodeling is extensive in young patients. If reduction is attempted,
pressure is applied to the apex of the fracture to affect reduction.
Anatomic reduction is not required because remodeling is plentiful.102,140 Unstable fractures with marked displacement require percutaneous pin fixation to maintain alignment (Fig. 8-51).
reduction is more difficult for type B and C fractures. The mobility of
the metacarpal base and the swelling make closed reduction difficult.
Comminution, soft tissue interposition, or transperiosteal
“buttonholing” in type C fractures may further complicate reduction.207
If closed reduction is accomplished and stable, then short-arm thumb
spica splint or cast immobilization is possible. Repeat radiographic
evaluation should be obtained 5 to 7 days later to ensure maintenance
of reduction.11
There are multiple options for pin configuration including direct
fixation across the fracture, pinning across the reduced CMC joint, and
pinning between the first and second metacarpals. Open reduction is
indicated for irreducible fractures. Type C fractures may
require open reduction to remove any interposed periosteum that blocks reduction (Fig. 8-53).25,207
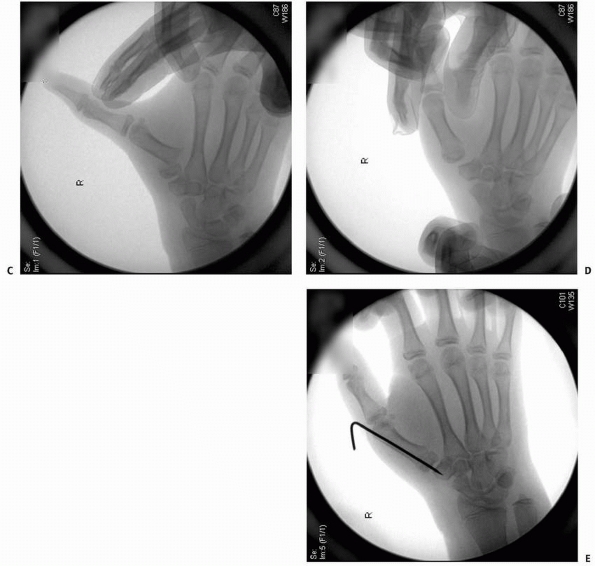 |
|
FIGURE 8-51 (continued) C. At time of reduction, fracture was very unstable. D. Closed reduction under fluoroscopy E. Percutaneous pin fixation to maintain alignment. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.)
|
An acceptable closed reduction is maintained by percutaneous pin
fixation. An unacceptable closed reduction is rare but requires open
reduction and fixation.167 The
choice of implant must be individualized, although smooth wires are
favored to minimize potential injury to the physis and articular
cartilage (Fig. 8-54).70,167 Skeletal traction is an alternative treatment for complex injuries with severe bony or soft tissue damage.23,178
reduction and cast application. Residual angulation between 20 to 30
degrees is acceptable depending on the age of the child and clinical
appearance of the thumb. The multiplanar motion of the CMC joint
combined with the potential for remodeling makes this degree of
angulation inconsequential. Fractures that are reducible, but unstable,
require percutaneous pinning (see Fig. 8-51).
degree of periosteal disruption. Mild angulation requires only cast
application without reduction. Moderate angulation is treated with
closed reduction and immobilization. Severe angulation usually is
combined with displacement and requires reduction. A successful closed
reduction is often augmented with percutaneous pin fixation due to
fracture instability. An unsuccessful closed reduction requires open
reduction and fixation.
alignment of the joint and physis. If an open reduction is required,
the preferred approach is through a gently curved incision overlying
the CMC joint along the glabrous border of the skin. The cutaneous
nerves are protected. The origins of the thenar eminence muscles are
reflected. A CMC joint arthrotomy is made and the articular surface is
exposed. The fracture joint surface is reduced and fixed with pins or
miniscrews. Additional percutaneous pin fixation of the first to second
metacarpal is used to protect the fracture fixation.
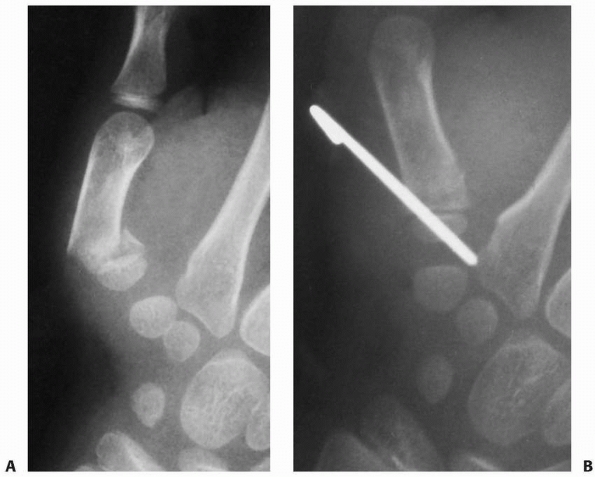 |
|
FIGURE 8-52 A. An 8-year-old boy with reducible, but unstable, fracture. B. A single percutaneous pin was placed to maintain alignment.
|
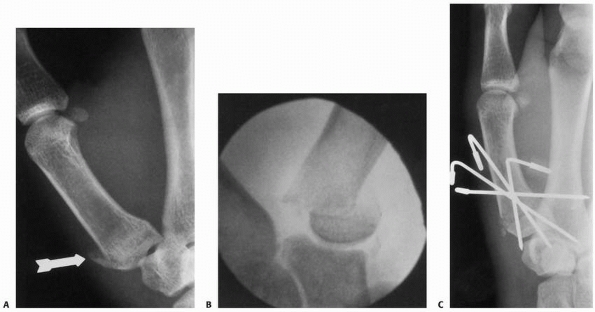 |
|
FIGURE 8-53 A. Fracture of the thumb metacarpal base with small lateral metaphyseal flag that appears innocuous on radiograph (arrow). B. However, additional images revealed marked displacement of the distal fragment. C.
Closed reduction was unsuccessful, because of interposed tissue. After open reduction, Kirschner wires were used to stabilize the fracture. |
 |
|
FIGURE 8-54 A.
A 14-year-old boy sustained a S-H type III fracture of the proximal thumb metacarpal with lateral subluxation of the carpometacarpal joint. B. Open reduction and Kirschner-wire fixation to restore joint alignment and congruity. (Reprinted from O’Brien ET. Fractures of the hand. In: Green DP, ed. Operative Hand Surgery. 2nd ed. New York: Churchill Livingstone, 1988:769, with permission.) |
weeks, depending on the fracture severity and degree of soft tissue
damage. A home program for range of motion is started thereafter.
Formal therapy is not instituted unless considerable soft tissue injury
occurred. In active children and young athletes, a light splint may be
worn for protection for an additional few weeks.
fixation and the reliability of the patient. Young children or marginal
fixations require 4 to 6 weeks of immobilization. Fracture union with
mild stiffness takes precedence over fracture nonunion with excessive
motion. Adolescents with stable fixation can be mobilized earlier,
usually 5 to 7 days after surgery, provided they are trustworthy in
terms of activity restrictions. A removable splint is used for
protection between exercise sessions until union.
hand function. The remodeling capabilities of fractures near or
involving the physis are extensive. The basilar thumb joint also allows
multiplanar motion and can accommodate moderate fracture malunion.
Residual deformity along the thumb metacarpal can be concealed through
CMC joint motion, and the thumb tolerates malrotation better than the
fingers (Fig.8-55).
Intra-articular incongruity may occur after incomplete reduction of
intra-articular fractures or inadequate fixation after satisfactory
reduction. Sequelae include pain, diminished motion, and arthrosis.
Fortunately, the occurrence of articular malunion and the development
of symptoms are uncommon. Available treatment options are limited and
include fusion or interposition arthroplasty.
The detection of injuries to the immature carpus is problematic because
of the difficulties in examining an injured child and the limited
ability of radiographs to detail the immature skeleton.11,136,159
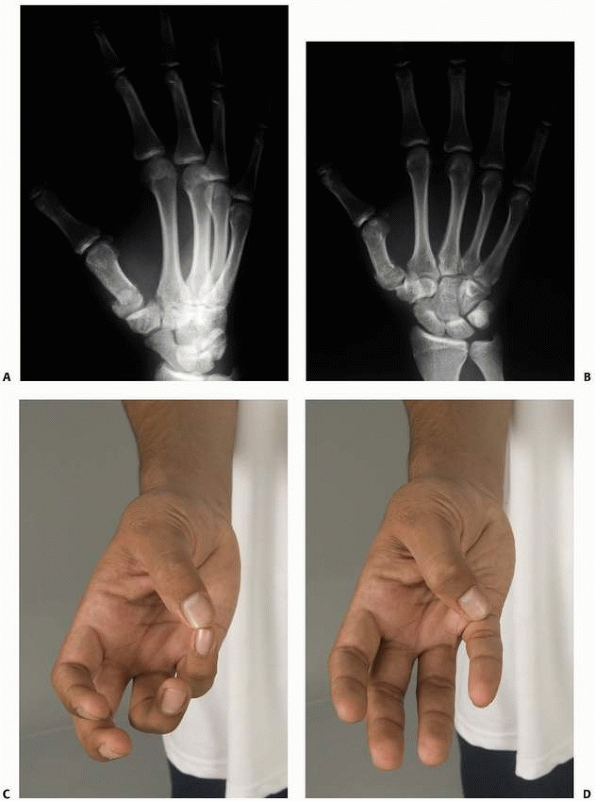 |
|
FIGURE 8-55 A 14-year-old boy presents 3 weeks after injury with mild pain and deformity base of right thumb A. Anteroposterior radiograph shows moderately displaced fracture base of the thumb metacarpal B. Lateral radiograph shows mild angulation. C. Follow-up motion after splinting for an additional 2 weeks, and home therapy reveals excellent opposition. D. Thumb able to touch base of small finger. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.)
|
By the tenth week of gestation, the carpus transforms into eight
distinct entities with definable intercarpal separations. Although
there are some minor changes in contour, these precursors greatly
resemble the individual carpal bones in their mature form.109
The capitate is the first bone to ossify, usually within the first few
months of life. The pattern of ossification proceeds in a clockwise
fashion. The hamate appears next, usually at about 4 months of age. The
triquetrum appears during the second year, and the lunate begins
ossification around the fourth year. The scaphoid begins to ossify in
the fifth year, usually slightly predating the appearance of the trapezium.105 Scaphoid ossification begins at the distal aspect and progresses proximally.140
The trapezium and trapezoid ossify in the fifth year, with the
trapezoid lagging slightly behind. The ossification pattern usually
concludes with the pisiform in the ninth or tenth year. The scaphoid,
trapezoid, lunate, trapezium, and pisiform may demonstrate multiple
centers of ossification.114,140 Although these variations are well recognized, they may be confused with acute trauma by the uninitiated observer.
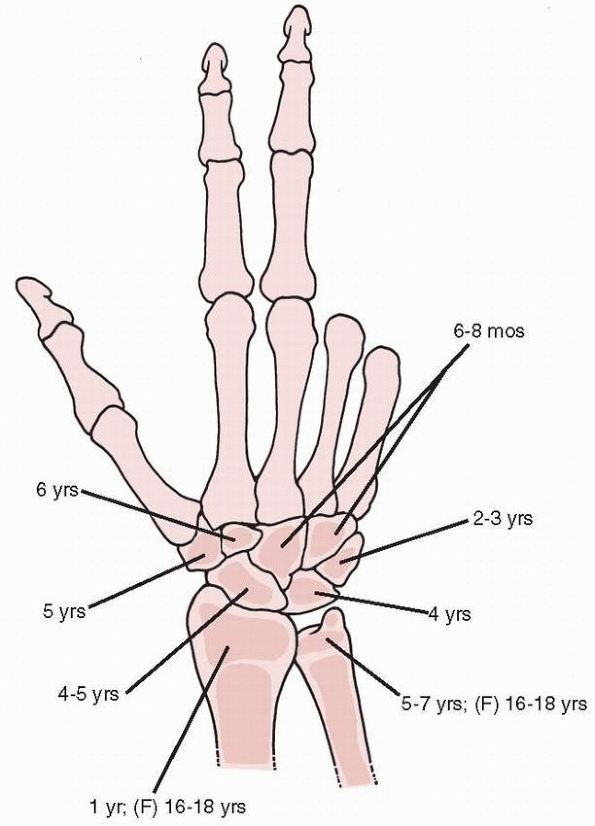 |
|
FIGURE 8-56
The age at the time of appearance of the ossific nucleus of the carpal bones and distal radius and ulna. The ossific nucleus of the pisiform (not shown) appears at about 6 to 8 years of age. |
during development. This arrangement is thought to provide a unique
shelter from injury.11,70
This observation is supported by epidemiologic studies of scaphoid
fractures that highlight the infrequent incidence in children younger
than 7 years of age and the marked increase in teenagers.74,105
most likely related to the thick peripheral cartilage that covers and
protects the ossification center. Therefore, fracture requires a
considerable force to disrupt this cartilaginous shell and injure the
underlying bone.41 The pattern of
pediatric scaphoid injury differs from that of adults because of the
evolving changes in the ossification center.52 During early stages of ossification, the scaphoid is more susceptible to avulsion fractures about the distal pole fracture.180,195 As the ossification progresses from distal to proximal, the fracture pattern mirrors the adult forms by early adolescence (Fig. 8-57).
scaphoid have traditionally been the most common injury pattern and
often result from direct trauma.16,41,195
However, scaphoid waist fractures are increasing in frequency in
younger children as participation in contact athletics begins earlier.
Proximal pole fractures are rare in children and often represent an
avulsion fracture of the scapholunate ligament. These fractures are at
higher risk for nonunion and osteonecrosis. The scaphoid also can be
fractured as a component of a greater arc perilunate injury.52
and 8-59).33,195
The fracture line and size of the avulsion fragment vary from an
isolated chondral injury that is barely visible on radiograph to a
large osteochondral fragment.
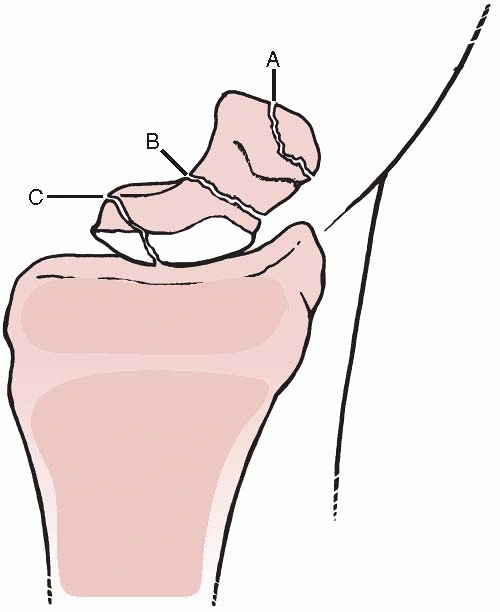 |
|
FIGURE 8-57 Three types of scaphoid fractures. A. Distal third. B. Middle third. C. Proximal pole.
|
 |
|
FIGURE 8-58
A 12-year-old boy fell on his right wrist and was tender over scaphoid tubercle. Radiograph reveals small avulsion fracture of distal scaphoid that can easily be overlooked. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.) |
fractures do occur in skeletally immature patients. The mechanism of
injury usually is a fall onto the outstretched hand and pronated
forearm, which exerts tensile forces acting across the volar portion of
the scaphoid as the wrist extends.32,52,203 Bony comminution may be present (Fig. 8-60). A careful scrutiny for other injuries about the carpus is mandatory.3,30
fractures are rare in children but have been reported in competitive
adolescent athletes. The mechanism often is unclear and can be
atypical, such as punching game machines or fighting.193
A proximal pole fracture may propagate through the interface between
newly ossified tissue and the cartilaginous anlage, or the injury may
be strictly through the cartilage. Proximal fractures may cause
destabilization of the scapholunate joint, as the scapholunate
interosseous ligament remains attached to the avulsed fragment (Fig. 8-61).
The most important prognostic factor is the presence or absence of
joint involvement. Extra-articular fractures may be either volar or
dorsal avulsions (see Fig. 8-58). A volar
pattern is more common and is attributed to the stout scaphotrapezial
ligaments. A dorsal fracture configuration is less common and is
attributed to the dorsal intercarpal ligament. The fragments vary in
size, and the radiographic appearance is age dependent.
 |
|
FIGURE 8-59
A 12-year-old boy fell playing ice hockey and complained of right wrist pain. Radiograph reveals a distal pole scaphoid fracture with slight comminution. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.) |
bone into thirds or delineating the area bounded by the
radioscaphocapitate ligament defines the waist of the scaphoid. Waist
fractures occur in many forms. Pediatric fractures are incomplete,
minimally displaced, or complete with or without displacement.
Comminuted fractures are rare and are associated with higher energy
(see Fig. 8-60).
diagnostic and therapeutic dilemmas. The proximal pole is the last to
ossify, which further complicates diagnosis. The tenuous blood supply
of this region presents the same problems in children as adults in
terms of nonunion and osteonecrosis risks.
Criteria that must be met to diagnose a congenital bipartite scaphoid
include: (a) similar bilateral appearance, (b) absence of historical or
clinical evidence of antecedent trauma,
(c)
equal size and uniform density of each component, (d) absence of
degenerative change between the scaphoid components or elsewhere in the
carpus, and (e) smooth, rounded architecture of each scaphoid
component. A unilateral “bipartite scaphoid” should be viewed as a
posttraumatic scaphoid nonunion.
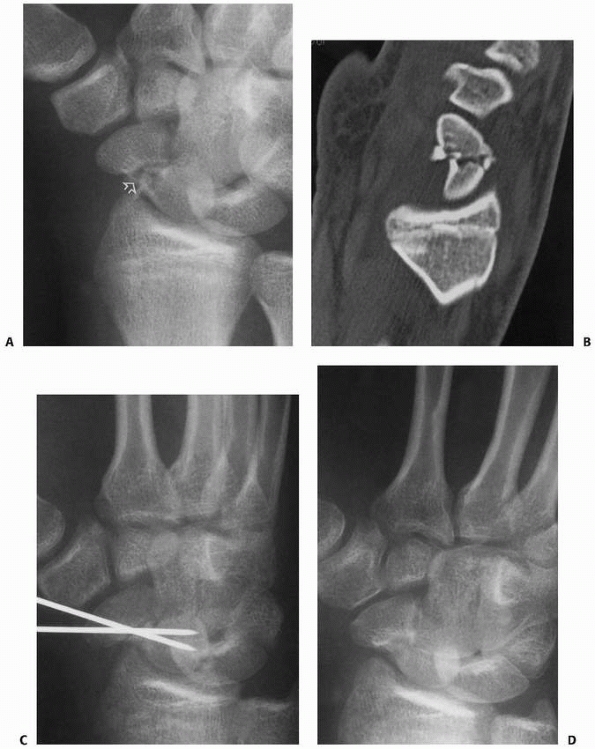 |
|
FIGURE 8-60 A. A displaced midwaist scaphoid fracture with comminution, including a butterfly fragment from the volar radial aspect (arrow). B. CT scan demonstrates the comminution. C. Open reduction with internal fixation was performed with two smooth wires and bone graft from the distal radius. D. Healing of fracture after pin removal.
|
 |
|
FIGURE 8-61
Anteroposterior radiograph of a 16-year-old male hockey player with a proximal one-third scaphoid fracture. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.) |
and clinical suspicion are the essential elements to diagnosis of a
scaphoid fracture.148 While the
findings are similar in adults and children, they are more difficult to
elicit in children. The relative infrequency of this injury and the
difficulty in interpreting radiographs of the immature wrist increase
the rate of missing a pediatric scaphoid fracture. A distal pole
fracture presents with swelling or tenderness over the scaphoid
tuberosity. A scaphoid waist fracture presents with pain to palpation
within the anatomic snuffbox, scaphoid tubercle, and/or with axial
compression of the thumb ray.
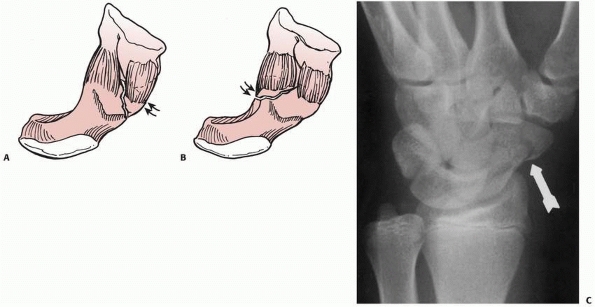 |
|
FIGURE 8-62 Two variations of an A2 intra-articular fracture of the scaphoid distal pole. A.
The more prevalent type is on the radial aspect of the volar distal scaphoid. This fragment is attached to the radial portion of the scaphotrapezial ligament (arrows). B. The less common type is on the ulnar aspect of the volar distal scaphoid. This fragment is attached to the ulnar portion of the scaphotrapezial ligament (arrows). C. Radiograph of an intra-articular distal pole scaphoid fracture. |
|
TABLE 8-7 Classification of Scaphoid Fractures
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||
scaphoid views in ulnar deviation of the wrist are routine. Middle
third fractures may or may not be evident on initial radiographs.
Distal pole fractures are best seen on the lateral view. A pronated
oblique view further highlights the CMC joint and distal pole fracture
pattern. A scaphoid view places the scaphoid parallel to the film and
reveals the scaphoid in its full size. One must be aware of the
pseudo-Terry Thomas sign.107 The
scaphoid ossifies from distal to proximal, which changes the distance
between the ossified lunate and scaphoid as the child approaches
adolescence. This produces an increased distance between the scaphoid
and lunate in the immature patient, which
ranges from 9 mm in a 7-year-old to 3 mm in a 15-year-old.96,107
Failure to appreciate these normal radiographic variants may lead to an
erroneous diagnosis of scapholunate dissociation when the apparent gap
is filled with normal cartilage and unossified bone. Comparison to
contralateral wrist radiographs is extremely useful in distinguishing
abnormal from normal patterns; however, one must keep in mind that
carpal ossification is not always symmetric. MRI or CT scans are
usually diagnostic.
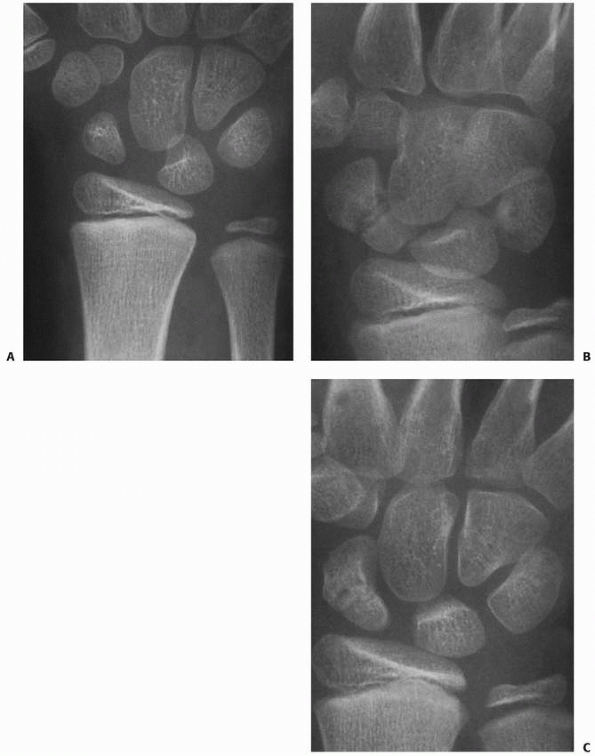 |
|
FIGURE 8-63 A.
A 9-year-old boy who fell on an outstretched wrist and had radial-sided pain and tenderness; original radiographs failed to reveal any bony abnormalities. B. About 1.5 years later, he had persistent radial-sided wrist pain, and radiographs revealed a midwaist scaphoid nonunion. This would not be considered a bipartite scaphoid, but instead an injury that was sustained when the cartilaginous anlage was present. C. After 2 months of casting, early fracture union is present. |
fracture but the radiographs are negative, the patient should be
immobilized. The child should either be instructed to return in 2 weeks
for repeat exam and radiographs, or advanced images studies may be
ordered. MRI is a useful modality to detect scaphoid fractures that are
not visualized on the initial radiographs.22,35,48,94,116 Johnson et al.94
evaluated 56 children (57 injuries) with MRI within 10 days of injury.
All children had a suspected scaphoid injury but negative radiographs.
In 33 (58%) of the 57 injuries, the MRI was normal and the patients
were discharged from care. In 16 cases (28%), a fractured scaphoid was
diagnosed, and treatment was initiated. MRI does require sedation in
the young child and may be overly sensitive in identifying bone edema
that never develops into a fracture.
scaphoid fracture (Fig. 8-64).52
The role of bone scan has been nearly supplanted by MRI. CT scans are
most valuable in the assessment of scaphoid fracture displacement for
operative indications and in the determination of scaphoid union. The
CT images must be made along the longitudinal axis of the scaphoid,
which is different than CT imaging of the wrist.161
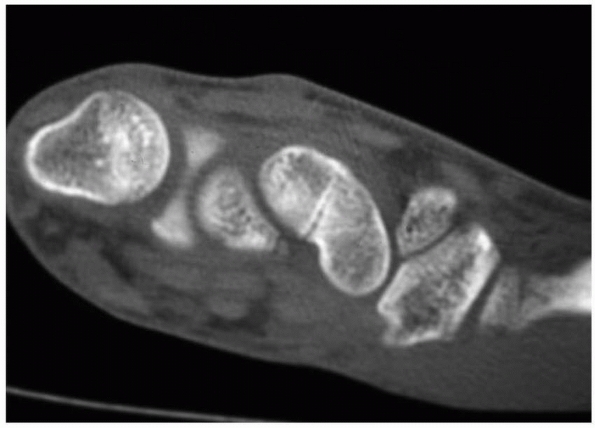 |
|
FIGURE 8-64
CT scan of 16-year-old male with negative radiographs but persistent pain. Sagittal image reveals waist fracture without displacement. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.) |
the presence of a scaphoid fracture. Clinical suspicion in the presence
of normal radiographs warrants immobilization and reevaluation in 2
weeks.30 The cast is removed, the
wrist is examined, and radiographs are obtained. Pain resolution and
negative radiographs warrant discontinuation of immobilization and
return to normal activities. Persistent pain with normal radiographs
requires continued immobilization and advanced imaging studies. MRI
scans have been shown to be diagnostically useful in this clinical
setting to avoid both misdiagnosis and overtreatment.22,35,48,94,116 However, MRI may be overly sensitive in identifying bone edema that fails to develop into a fracture.
immediate treatment is required. Most pediatric scaphoid fractures can
be treated with cast immobilization because children possess a great
ability to heal and remodel. In addition, most scaphoid fractures in
children are either incomplete (disrupting only a single cortex) or
nondisplaced. This principle is especially true for the distal pole,
which is a frequent site of scaphoid fracture (Fig. 8-65).52
Therefore, cast immobilization is the standard of treatment for most
nondisplaced or minimally displaced pediatric scaphoid fractures. For
avulsion and incomplete fractures, a short thumb spica cast for 4 to 6
weeks is recommended. In the young child, a long arm cast is
appropriate to prevent the cast from sliding off the arm. For complete
distal third and waist fractures, immobilization is recommended until
healing or 6 to 8 weeks of casting.
recommended for proximal pole fractures, delayed diagnosis, or
fractures with apparent bony resorption.52
Immobilization usually begins with 4 to 6 weeks of a long thumb spica
cast, followed by up to 6 weeks of a short thumb spica cast. The exact
cast position and the joints immobilized are a matter of individual
preference.24,62,81 Most authors favor a long arm thumb spica cast that permits thumb interphalangeal joint motion.62
 |
|
FIGURE 8-65 A 12-year-old boy depicted in Figure 8-59 after 8 weeks of casting. A. Scaphoid view demonstrates healing of the fracture. B. Pronated oblique radiograph further confirms fracture union. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.)
|
open reduction and internal fixation is a more reliable method for restoring alignment and obtaining union.
However, the fracture must be reduced at the time of screw fixation.
Fracture reduction can be accomplished with manipulation, joysticks, or
arthroscopic assistance. This technique can be applied to adolescent
patients with displaced scaphoid fractures. Screws can be placed under
fluoroscopic control either volarly (distal to proximal) or dorsally
(proximal to distal) depending on fracture patterns and surgeon
preference (Fig. 8-66).20,175 This procedure is challenging in displaced scaphoid fractures.
Displacement of more than 1 mm or intrascaphoid angulation of more than
10 degrees on any image warrants open reduction and internal fixation.
The implant choice is individualized according to the fracture and
patient. Scaphoid screws are the primary fixation techniques, although
Kirschner wires can be used.127
with cast immobilization. Indications for open reduction are fractures
with more than 1 mm of displacement or an angular deformity of more
than 10 degrees. Transscaphoid perilunate injuries also require
operative management.
cast for the initial 4 to 6 weeks, followed by a short arm cast until
clinical and radiographic union. Radiographs are obtained in the first
7 to 10 days to ensure alignment and then monthly until union. If in
doubt regarding anatomic alignment or union, a CT scan is obtained.
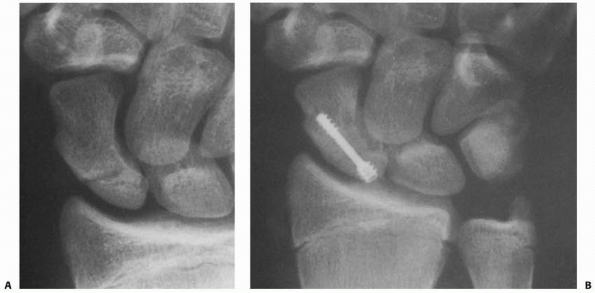 |
|
FIGURE 8-66 A. Nondisplaced proximal pole scaphoid fracture in a skeletally mature adolescent athlete. B. Treatment by percutaneous screw fixation led to healing.
|
osteonecrosis and nonunion. These injuries are unstable with motion due
to the scapholunate ligament insertions. Percutaneous screw fixation
stabilizes the fracture fractures without further disruption of the
precarious blood supply by operative exposure. Although technically
exacting, percutaneous screw fixation of these fractures with protected
immobilization until sufficient healing may lessen the risk of
osteonecrosis, nonunion, and degenerative changes.
Fractures of the middle and distal thirds are exposed through a volar
approach. Proximal third fractures are exposed through a dorsal
approach.156 The implant depends on
the fracture configuration and age of the child. Smooth wires may be
necessary in young children. Wires are buried beneath the skin and
removed after union. Scaphoid screw fixation is preferred in
adolescents.86,87,129,134 Comminution is treated with bone graft obtained from the metaphysis of the distal radius or iliac crest.
until union. After the cast is removed, a home therapy program is
started. Formal therapy usually is not necessary. Displaced fractures
treated with open reduction and internal fixation require variable
periods of immobilization. Fixation with
Kirschner
wires requires prolonged immobilization and may require formal therapy
to recover motion. Stable screw fixation allows early motion 10 to 14
days after surgery with a short arm thumb spica splint worn for
protection during vigorous activity until union. However, many
adolescents will not wear the splint dependably and require longer
periods of immobilization to prevent loss of screw fixation and
nonunion.
Nondisplaced pediatric scaphoid fractures have a greater than 95%
healing rate. A delay in treatment impedes healing and increases the
possibility of displacement.74,167,195 Displaced fractures require recognition and open reduction because adequate reduction and fixation result in predictable union.
and late presentation. Scaphoid nonunions do occur in children,
although the incidence is low.30,44,55,113,120,141,177
There are numerous reasons for late presentation, including a
reluctance for children to tell their parents about their mechanism of
injury, moderate symptoms that were not severe enough to seek medical
attention, and a fear of losing their position on a sporting team.89 Open reduction, bone grafting, and internal fixation are the standard procedures for treatment of scaphoid nonunions (Fig. 8-67).55,89,129,193
The approach varies according to the location of fracture and
vascularity of the fracture fragments. The principles of operative
scaphoid nonunion treatment in children are similar to those in adults.
Persistent scaphoid nonunion results in altered kinematics within the
wrist and produces degenerative changes over time.115,202 The goal is to obtain union to prevent long-term arthrosis.
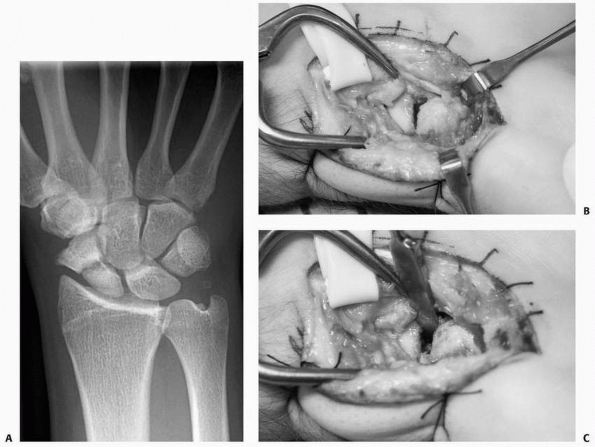 |
|
FIGURE 8-67 A. A 16-year-old male with a right scaphoid nonunion with resorption at the fracture site. B. Volar approach and exposure of the fracture site. C. The fracture site was débrided of fibrous material, and the hump back deformity was corrected. (continues)
|
proximal fragment is more prone to avascular changes. Avascular changes
within the proximal fragment do not preclude union after internal
fixation. The size of the fragment and the extent of avascularity
dictate management. The treatment principles are similar in adults and
children. Options to obtain union include conventional or vascularized
bone grafting.200 With nonunion and osteonecrosis of the proximal pole, vascularized bone grafting from the distal radius has been successful.182,200
completely around the lunate and cause a perilunate or lunate dislocation.30,34,146 The injury also can halt within the capitate and produce a scaphocapitate syndrome.6,197
 |
|
FIGURE 8-67 (continued) D. The fracture site was packed with bone graft and a guide wire was placed for screw fixation. E. The screw was inserted over the guide wire. F,G.
Anteroposterior and lateral radiographs after fracture reduction, bone grafting, and screw placement. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.) |
mechanism. The waist of the capitate abuts against the lunate or dorsal
aspect of the radius. The fracture occurs through the waist with
variable displacement.
swollen and painful to palpation. The clinical presentation varies with
the associated carpal injuries. Median nerve paresthesias may be
present secondary to swelling within the carpal tunnel.
or the proximal capitate fragment can rotate 180 degrees. Either
scenario can create a confusing image that often results in
misinterpretation. Incomplete ossification further complicates
radiographic diagnosis and degree of displacement. Small osteochondral
fragments in the midcarpal region may indicate a greater arc injury or
isolated capitate fracture. In these cases, advanced imaging studies,
such as MRI or CT, may be useful (Fig. 8-70).
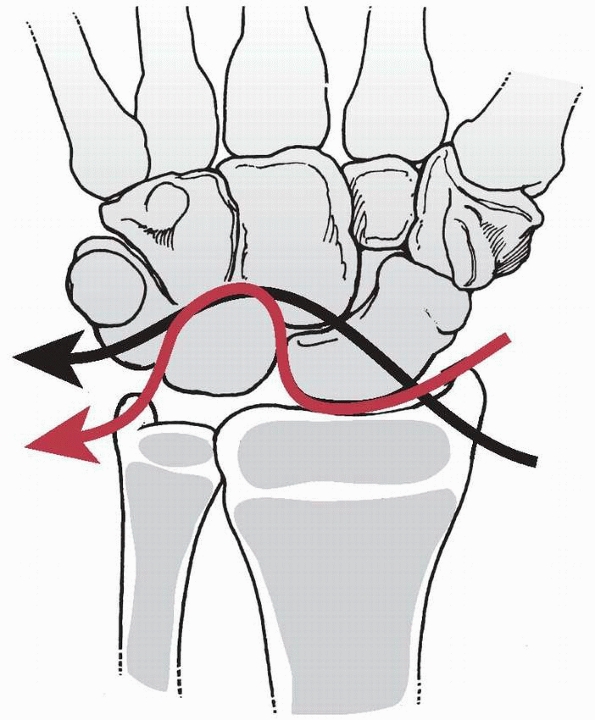 |
|
FIGURE 8-68 Progressive perilunar instability. The greater arc (black arrow)
is associated with fractures of the carpal bones, which may include the scaphoid, lunate, capitate, hamate, and triquetrum. The red arrow depicts the lesser arc, in which forces are transmitted only through soft tissue structures. (Reprinted from Mayfield JK, Johnson RP, Kilcoyn RK. Carpal dislocations: pathomechanics and progressive perilunar instability. J Bone Joint Surg Am 1980;5:226-241, with permission.) |
displacement, and associated injuries. Distraction radiographs, MRI, or
CT scans may be necessary to determine the exact pattern of injury.
 |
|
FIGURE 8-69
A 12-year-old boy sustained multiple carpal fractures attributed to a crushing injury. Sixteen months later, an established nonunion of the capitate is present that required bone grafting to obtain union. (Courtesy of James H. Dobyns, MD.) |
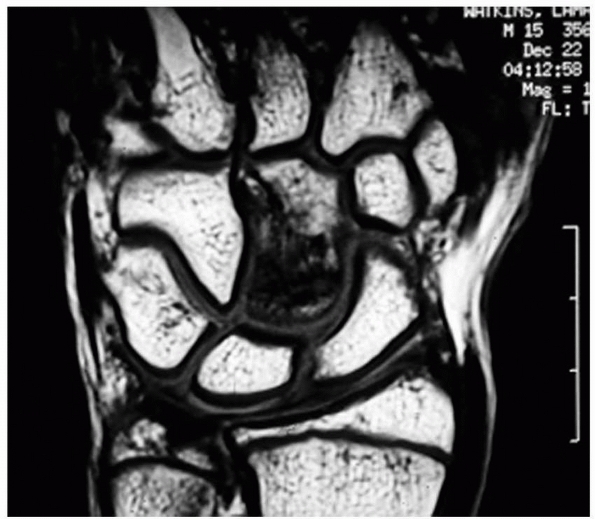 |
|
FIGURE 8-70
A 13-year-old boy with persistent midcarpal pain after a fall. MRI shows a capitate fracture. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.) |
capitate and/or scaphoid can be treated with a long arm cast for 6 to 8
weeks. Closed reduction of displaced fractures is not feasible.34
reduction, especially the rotated proximal capitate pole. Associated
perilunar injuries also require internal fixation and ligamentous
repair. The anatomic relationships within the carpus must be restored.
Wire or osseous screw fixation is appropriate stabilization after open
reduction. Suture repair of ligamentous injuries is performed.
generalizations. Early recognition and appropriate treatment lead to an
acceptable outcome. Nonunion is rare and requires bone grafting (see Fig. 8-69).126 Despite the considerable rotation of the proximal pole, osteonecrosis of the capitate is rare.
adults than in children. The injury may occur in adolescents as carpal
ossification nears completion. A fracture through the body of the
triquetrum is rare and may occur with a perilunar injury as the path of
the greater arc injury passes through the triquetrum.121
probable mechanism for a dorsal triquetrum fracture is a pulling force
through the dorsal ligaments or abutment of the ulnar styloid.
painful to palpation directly over the dorsal triquetrum. The clinical
presentation is more severe with associated carpal injuries.
may not show the avulsion fracture. A pronated oblique view highlights
the dorsum of the triquetrum and may reveal the avulsed fragment. At
times, CT scans are necessary for accurate diagnosis (Fig. 8-71).
immobilization (3 to 6 weeks) followed by motion and return to
activities. A fracture through the body of the triquetrum with a
perilunar injury requires open reduction and internal fixation.
Treatment results in prompt and complete recovery. Body fractures
associated with perilunar injures have a guarded prognosis, depending
on the extent of concomitant injuries and treatment provided.
trapezium are rare. Hook of the hamate fractures usually occur in
adults but may occur in adolescents with traumatic falls. A CT scan may
be necessary for diagnosis if the fracture is not visible on the carpal
tunnel view. Pisiform fractures are the result of direct trauma. Lunate
fractures are associated with Kienböck disease,154 which is relatively uncommon in children. Trapezium fractures can occur with CMC joint injuries about the thumb.
 |
|
FIGURE 8-71 A minimally displaced dorsal triquetral avulsion fracture (arrow) that was treated with short-term immobilization.
|
Motor vehicle accidents and sports-related injuries are potential
causes of the rare fracture-dislocation. However, recurrent or chronic
wrist pain is not uncommon in adolescents. Most recurrent ligamentous
pain results from hypermobility and overuse during the adolescent
growth spurt. This mechanism may result in joint subluxation, chondral
impingement, or ligamentous tears similar to patellofemoral injuries in
adolescents.
with an acute traumatic injury avoids use of the wrist and hand. The
wrist is swollen and painful to palpation, making isolation of the
injured segment difficult except in extremely cooperative children.
Provocative maneuvers for carpal instability usually are not possible
because of pain in the injured wrist.
overuse, and relative muscular weakness. These children complain of
diffuse pain, generalized tenderness, and limited strength on
examination. Diagnosis is difficult particularly because of concerns
regarding emotional overlay.
 |
|
FIGURE 8-72 Anteroposterior (A) and lateral (B) radiographs of a dorsal perilunar dislocation in a 6-year-old boy. (Courtesy of William F. Benson, MD.)
|
Anteroposterior and lateral views are routine. The incomplete
ossification complicates radiographic interpretation, especially the
assessment of carpal widening. Detection of slight widening or
malalignment within the carpus often is difficult. Contralateral views
are useful to compare ossification and carpal spacing.96
Suspicion of a fracture warrants advanced imaging studies, such as
arthrography, stress radiograph, fluoroscopy, and MRI. MRI scans are
used for diagnosis of ligamentous injuries.
traumatic dislocation injuries are difficult. Decisive factors include
the age of child, degree of clinical suspicion, and extent of injury.
Minor injuries are treated with immobilization for 3 to 6 weeks and
re-examination. Resolution of symptoms and signs allows return to
normal activities. Persistent pain warrants further clinical and
radiographic evaluation. Overt ligamentous injuries with static
instability and malalignment require accurate diagnosis and appropriate
treatment. A complete ligament tear (e.g., an adolescent with a
scapholunate injury) is treated with principles similar to those for
adults. Open reduction, anatomic reduction, and ligament repair are the
basic tenets of treatment.
persistent activity-related pain is especially difficult to treat.
Discerning focal from nonfocal wrist pathology is imperative.
Radiographs and MRI scans often are normal. Most of these children
respond to therapeutic strengthening. Protective sport-specific wrist
protectors or taping may be appropriate (Fig. 8-73).
A small subset of children have unresolved pain caused by chondral
injuries or ligamentous tears that require arthroscopic treatment.50
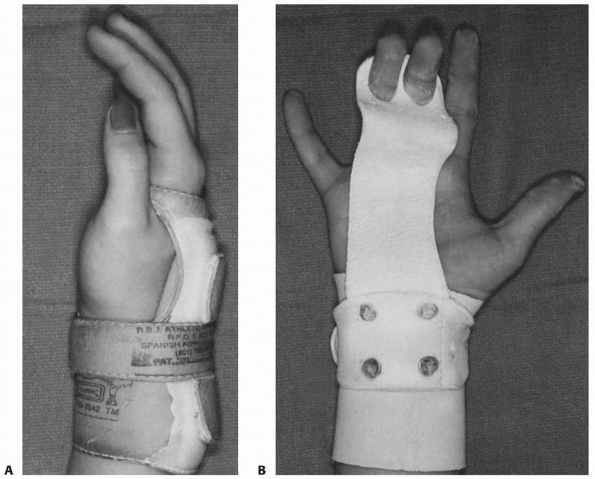 |
|
FIGURE 8-73 Wrist guards for gymnastics. A. The “lion’s paw” protector used mainly for vault. B. Hand and wrist protectors used primarily for the uneven parallel bars.
|
These tears most often are associated with distal radial fractures,
radial growth arrest, ulnar overgrowth, and ulnar carpal impaction.
Most often these children present late after acute trauma with
activity-related pain.
and the volar ulnocarpal ligaments. The TFC spans the sigmoid notch of
the radius to the fovea at the base of the ulnar styloid and provides
stability to the distal radioulnar and ulnocarpal joints.
the TFCC. In children with a positive ulnar variance, the TFC is
thinner and more susceptible to injury. Similarly, ulnar styloid
hypertrophic unions and nonunions increase the risk of TFCC injuries
with ulnocarpal impaction.
Peripheral tears (type B) are most common in adolescents. Tears from
the radial insertion (type D) are next in frequency, while central
(type A) and volar (type C) tears are rare.142,144
region. Forearm rotation may be limited and usually reproduces the
pain, particularly at the extremes of supination and/or pronation.
Compression and ulnar deviation of the carpus against the ulna may
reproduce the pain with crepitus. The stability of the distal
radioulnar should be compared to the contralateral side.137,190
An acute displaced fracture at the base of the styloid suggests the
likelihood of a TFCC tear. Arthrograms and MRI scans may help in the
diagnosis.28,77
pain without instability incorporates rest until symptoms subside
followed by a strengthening program. If pain persists after regaining
symmetric pinch and grip strength, then further evaluation is
appropriate. If clinical examination is consistent with a TFCC tear or
ulnar-carpal impaction, MRI and/or arthroscopy is appropriate. Partial
TFCC tears or carpal chondromalacia is treated with arthroscopic
débridement. Full thickness tears from the fovea (1B) require
peripheral repair, usually arthroscopically, to restore stability.
Tears from the radial insertion (1D) require a trans-radial repair.
interphalangeal joints are stronger than the physis, which explains the
propensity for fracture rather than dislocation. Occasionally,
dislocations and fracture-dislocations occur about the interphalangeal
and metacarpophalangeal joints (Fig. 8-74).
or lateral DIP joint dislocation. The collateral ligaments and volar
plate typically detach from the middle phalanx. Most dislocations can
be reduced by longitudinal traction, recreation of the dislocation
force, and reduction of the distal phalanx. The DIP joint reduction and
congruity are confirmed by clinical motion and radiographs. Two to 3
weeks of DIP joint splinting is sufficient, followed by a home program
that focuses on DIP joint motion.
Open reduction through a dorsal approach is required for removal of the
interposed tissue. The volar plate often is the offending agent,
although the collateral ligaments and the flexor digitorum profundus
can block reduction.143,150
A stable DIP joint is treated with DIP joint splinting for 3 to 4
weeks. An unstable DIP joint requires pin fixation for 3 to 4 weeks.
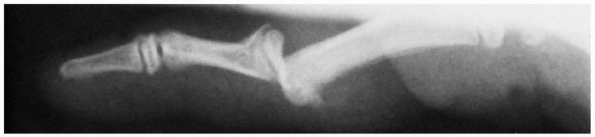 |
|
FIGURE 8-74 A dorsal dislocation of the PIP joint with a S-H type II fracture of the middle phalanx in a 15-year-old boy.
|
directions. Dorsal dislocations are the most common, although lateral
and volar dislocations also occur. The differential diagnosis includes
adjacent bony and tendon injuries.53
Radiographs are required to assess the physis and to confirm joint
alignment. The postreduction lateral radiograph must confirm concentric
joint reduction. Subtle joint subluxation is detected by a slight
offset between the proximal and middle phalanges along with a dorsal V
space instead of smooth articular congruity.
displaced dorsal to the proximal phalanx. The collateral ligaments and
volar plate are disrupted. Many dorsal dislocations probably are joint
subluxations that retain some of the collateral ligament or volar plate
integrity. Some subluxations are reduced by the patient or trainer and
never receive medical evaluation.
deformity. If necessary, anesthesia usually can be accomplished with a
digital block. The dislocation is reduced with longitudinal traction,
hyperextension, and palmar translation of the middle phalanx onto the
proximal phalanx. The quality of the reduction and the stability of the
joint must be assessed. Asking the patient to flex and extend the digit
evaluates active motion. Most dislocations are stable throughout the
normal range of motion, and radiographs confirm a concentric reduction.
A stable joint requires a brief period (3 to 5 days) of splinting for
comfort, followed by range of motion and buddy taping. Immediate motion
may be started, although pain often prohibits movement. Prolonged
immobilization leads to PIP joint stiffness.
during PIP joint extension. The radiographs must be scrutinized for
subtle dorsal subluxation and concomitant fracture of the middle
phalangeal base. Unstable PIP joint dislocations, with or without small
fractures of the middle phalangeal base, have a stable arc of motion
that must be defined. This stable arc is typically from full flexion to
about 30 degrees of flexion. This arc is used to determine the confines
of extension-block splinting.122 A
short arm cast is applied with an aluminum outrigger that positions the
MCP joint in flexion and the PIP joint in 10 degrees less than the
maximal extension that leads to joint subluxation. Reduction is
verified by lateral radiographs. The aluminum splint is modified every
7 to 10 days to increase PIP joint extension 10 degrees. A lateral view
or dynamic fluoroscopy is used to confirm concentric reduction. This
process
is continued over 4 to 5 weeks. The cast and splint are then discontinued and a home therapy program is instituted.
30 degrees of flexion almost always involve considerable fracture of
the middle phalanx. These injuries are regarded as pilon fractures or
intra-articular fracture-dislocations. Treatment presents a management
dilemma as discussed earlier.185 Options range from open reduction to dynamic traction. Long-term subluxation, stiffness, and arthrosis are concerns.
The proximal phalangeal head may herniate between the lateral band and
the central tendon. In contrast to dorsal dislocations, long-term
results often are suboptimal. This outcome may be related to a delay in
treatment or the degree of soft tissue involvement, especially the
central slip.
Reducible dislocations are treated with 4 weeks of full-time PIP joint
extension splinting to promote healing of the central slip.191
Radiographs are necessary to confirm concentric reduction. An unstable
reduction may require temporary pin fixation across the PIP joint.
Irreducible dislocations require open reduction through a dorsal
approach to extricate any interposed tissue. The central slip can be
repaired to the middle phalanx. Postoperative immobilization consists
of 4 weeks of full-time PIP joint extension splinting.
dislocations are uncommon, although dorsal dislocations may have a
lateral component.60 An isolated
lateral dislocation represents severe disruption of the collateral
ligament complex. The injury is a spectrum of injury, beginning with
damage to the proper and accessory collateral ligaments and culminating
in volar plate disruption.100 Bony avulsion fragments may accompany the ligamentous failure.37
Closed reduction is uniformly successful. A brief period (5 to 7 days)
of immobilization followed by buddy taping to protect the healing
collateral ligament complex is the customary treatment.
dislocations include the extent and anatomic location of soft tissue
disruption, presence or absence of fracture, reducibility, and
stability after reduction. The initial treatment of almost all PIP
dislocations is an attempt at closed reduction followed by a stability
assessment. Early mobilization is important to prevent PIP joint
stiffness.
followed by early motion. Coban-wrap (3M, St. Paul, Minnesota) buddy
taping is used until full stable motion is achieved. Sports are
restricted until the patient gains joint stability and full motion. An
unstable reduction that can be held reduced in more than 30 to 40
degrees of flexion is treated with extension block splinting. Extremely
unstable fracture-dislocations require open treatment, external
fixation, or dynamic traction depending on the size of the fracture
fragments.
weeks with the PIP joint in extension. Unstable reductions are treated
with percutaneous pin fixation to maintain a concentric reduction.
Irreducible dislocations require open reduction with repair of the
central slip.
usually is obtainable, followed by a brief period of immobilization.
Irreducible dislocations require open reduction with or without
collateral ligament repair.
The dislocation may involve a finger or thumb. The gamekeeper’s or
skier’s thumb can be considered a subset of subluxation or dislocation.
which results from a hyperextension force that ruptures the volar
plate. The proximal phalanx is displaced dorsal to the metacarpal head.
The diagnosis is readily apparent because the digit is shortened,
supinated, and deviated in an ulnar direction. The interphalangeal
joints are slightly flexed due to digital flexor tendon tension. The
volar skin is tense over the prominent metacarpal head.
complex. Complex dislocations are irreducible because of volar plate
interposition in the joint. The injury can be open with the metacarpal
head penetrating the palmar skin (Fig. 8-76).
Simple dislocations are in a position of hyperextension on radiographs.
Irreducible dislocations have bayonet apposition of the proximal
phalanx dorsal to the metacarpal head. The sesamoid bone(s) of the
index or thumb may be seen within the joint. The position of the
sesamoid bones is indicative of the site of the volar plate.26,157 The most common irreducible dislocation is at the index MCP joint. Additional structures may impede reduction.97
The metacarpal head becomes “picture-framed” by the flexor tendon on
the ulnar side and the lumbrical on the radial side. The superficial
transverse metacarpal ligament and the natatory ligaments also can
entrap the metacarpal neck. The collar of retraining tissue is
tightened by longitudinal traction, and this reduction maneuver may
convert a dislocation from reducible to irreducible.
and volar manipulation of the proximal phalanx over the metacarpal
head. Avoidance of hyperextension during reduction is important to
prevent conversion of a simple to a complex dislocation. These
reductions are usually stable. Reduction of a complex dislocation is
problematic. The maneuver involves further hyperextension
of
the joint and palmar translation of the proximal phalanx. The goal is
to extricate the volar plate with the proximal phalanx during palmar
translation. Intra-articular infiltration of anesthetic fluid may
assist reduction through joint distention and “floating” of the volar
plate from its displaced position. The success rate for conversion of
an irreducible dislocation to a reducible dislocation is low; open
reduction is necessary in almost all patients.
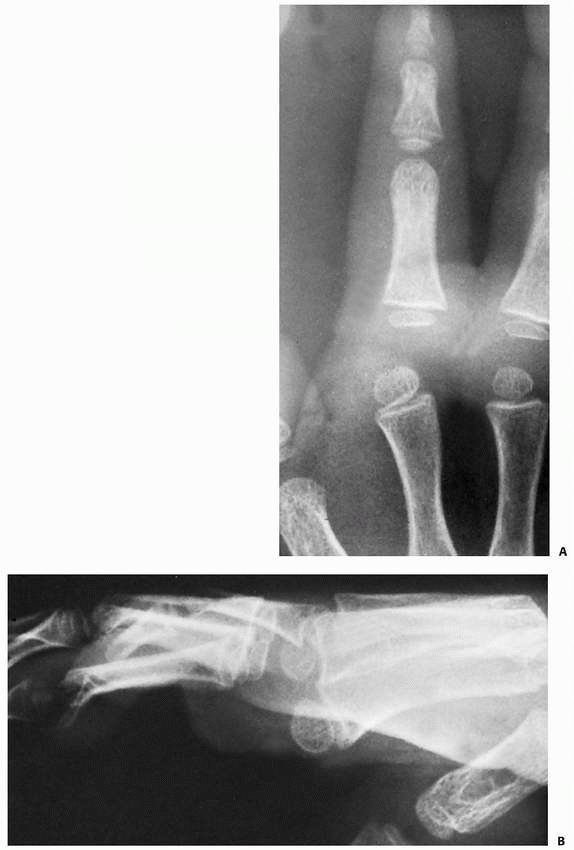 |
|
FIGURE 8-75 A. A 3-year-old boy with a complete complex dislocation of the index finger metacarpal joint. B. Note the parallelism in this lateral view. Open reduction was done through a volar approach.
|
dorsal approach. The volar approach provides excellent exposure of the
metacarpal head and the incarcerated structures.9,12,65,73,97,110,123
However, the digital nerves are draped over the articular surface of
the metacarpal head and precariously close to the skin. A deep skin
incision can cut these nerves. The skin is gently incised and soft
tissue is dissected. The first annular pulley is incised. The
metacarpal head is extricated from between the flexor tendon and the
lumbrical. The joint is evaluated for interposed structures, such as
the volar plate, and then reduced under direct observation.
joint. A transverse or longitudinal capsulotomy is made if the injury
has not torn the capsule. A Freer elevator is placed within the joint
to clear it of any interposed tissue. Often, the interposed volar plate
needs to be split longitudinally to reduce the joint. If the flexor
tendon is wrapped around the metacarpal, the Freer is used to extricate
the metacarpal head.
 |
|
FIGURE 8-76
A 17-year-old male after fall from height with open index and middle finger dorsal dislocations. (Courtesy of Joshua Ratner, MD.) |
The postoperative regimen is a 3 to 5 day immobilization period,
followed by active motion. Rarely, a dorsal blocking splint is needed
to prevent hyperextension that may foster repeat dislocation.
but delay of a few months may still result in an acceptable outcome. A
delay of more than 6 months is associated with joint degeneration and a
less predictable result. Late reduction may require a combined dorsal
and volar approach for adequate exposure.9,112,135 Collateral ligament resection and temporary MCP joint pin fixation may be necessary.
fingers, and hyperextension is the common mechanism. Thumb dislocations
are classified according to the integrity and position of the volar
plate, the status of the collateral ligaments, and the relative
position of the metacarpal and proximal phalanx. The components of the
classification are incomplete dislocation, simple complete dislocation,
and complex complete dislocation (Fig. 8-79).
An incomplete dislocation implies rupture of the volar plate with
partial preservation of the collateral ligament integrity. The proximal
phalanx perches on the dorsum of the metacarpal. Closed reduction is
easily accomplished, and a 3-week course of immobilization is adequate.
Return to sports requires protection for an additional 3 weeks.
 |
|
FIGURE 8-77
A rare dorsal dislocation of the long finger that was irreducible by closed means. A dorsal approach permitted inspection of the joint and extrication of the volar plate. |
simple, complete dislocation implies volar plate and collateral
ligament disruption. The proximal phalanx is displaced in a dorsal
direction and is angulated 90 degrees to the long axis of the thumb
metacarpal. Many of these dislocations can be reduced by closed means,
although unnecessary longitudinal traction may convert a reducible
condition into an irreducible situation (Fig. 8-80).73,123
A successful reduction requires thumb spica immobilization for 3 to 4
weeks to allow healing of the volar plate and collateral ligaments.
Dislocation. A complete or irreducible dislocation is the most severe
type of injury. The long axes of both the proximal phalanx and
metacarpal often are parallel. Open reduction is usually required to
extricate the volar plate from within the joint (Fig. 8-81).19 A dorsal or volar approach is suitable, with concerns similar to those for irreducible index MCP joint dislocations.184
types of injury: (i) a simple sprain of the UCL, (ii) a rupture or
avulsion of the insertion or origin of the ligament, (iii) a simple S-H
I or II fracture of the proximal physis, or (iv) a S-H III avulsion
fracture that involves one fourth to one third of the epiphysis of the
proximal phalanx (Figs. 8-82 and 8-83).128,206
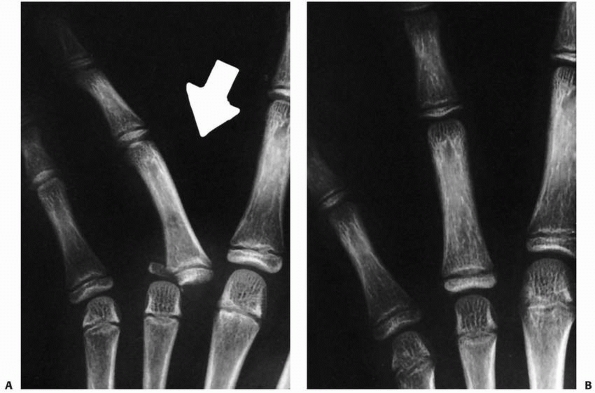 |
|
FIGURE 8-78 A. A 9-year-old girl sustained this radial fracture-dislocation of the middle fingers. B. Closed reduction restored joint and fracture alignment.
|
adolescents. A history of trauma is customary, especially involving
sports. The thumb is swollen about the MCP joint with ecchymosis, and
tenderness to palpation is well localized over the UCL. Pain is
exacerbated by abduction stress. A complete rupture or displaced
fracture lacks a discrete endpoint. Anteroposterior and lateral
radiographs are used to diagnosis and delineate fracture configuration.
Stress views may be needed if the diagnosis is questionable. MRI can be
used to evaluate ligament disruption in complicated injuries.
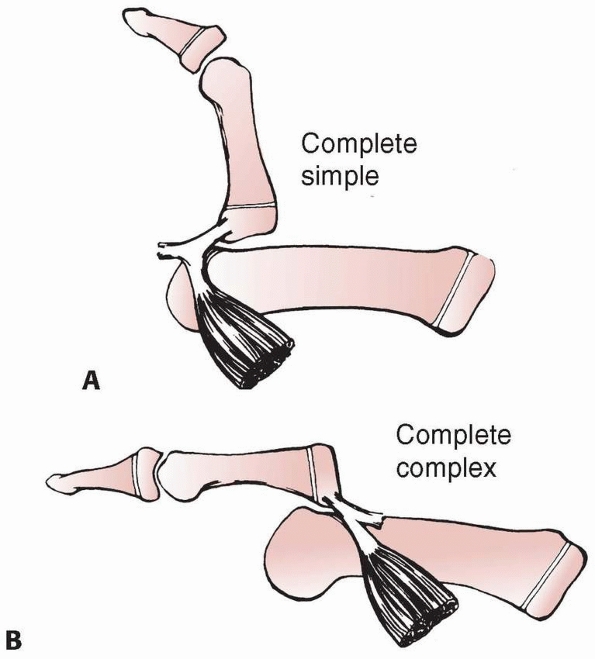 |
|
FIGURE 8-79 Simple and complex dorsal dislocations of the thumb MCP joint. Simple dislocations (A) are in extension and reducible. Complex dislocations (B) are in bayonet apposition and are irreducible because of the interposed volar plate.
|
simple sprains, incomplete injuries, and nondisplaced fractures.
Complete ruptures or displaced fractures usually require operative
intervention. A major concern is displacement of
the ligament or fracture fragment behind the adductor aponeurosis, which prohibits healing.183,184
A S-H III fracture of the ulnar corner of the epiphysis of the proximal
phalanx is the most common childhood gamekeeper’s injury. A displaced
fracture (fragment rotated or displaced more than 1.5 mm) requires open
reduction and internal fixation to restore the integrity of the UCL and
to obtain a congruous joint surface (Fig. 8-84).
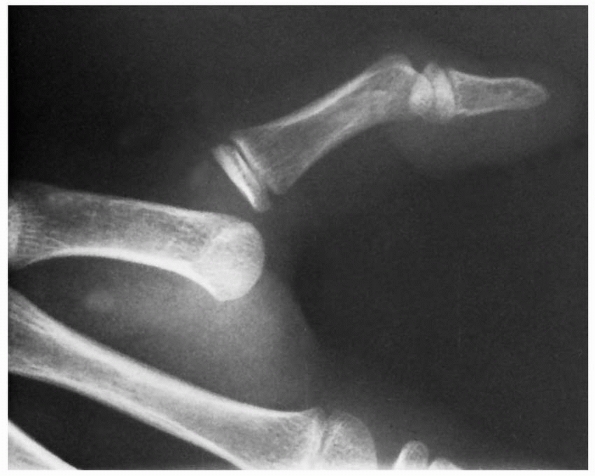 |
|
FIGURE 8-80 A 9-year-old boy with a complete simple dorsal dislocation of the thumb MCP joint.
|
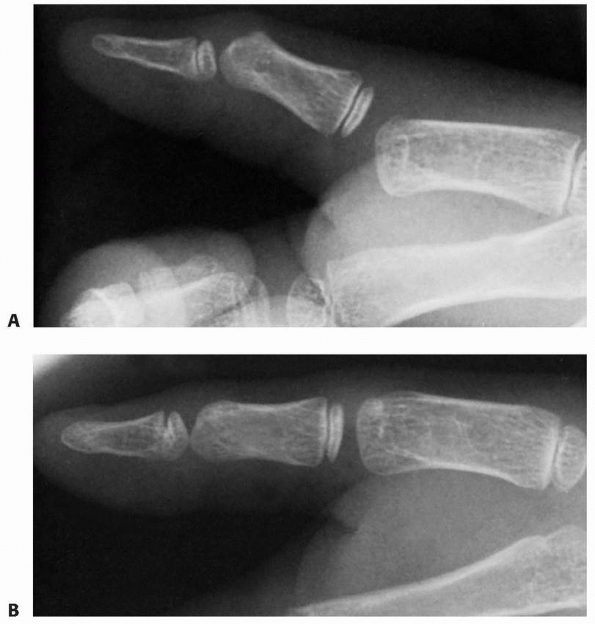 |
|
FIGURE 8-81 A. Irreducible dorsal MCP dislocation in a 7-year-old boy. B. After open reduction through a volar incision.
|
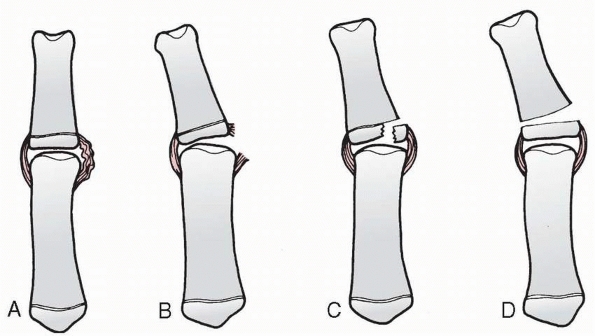 |
|
FIGURE 8-82 Ulnar instability of the thumb metacarpal joint. A. Simple sprain. B. Rupture of the ligament. C. Avulsion fracture (S-H type III). D. Pseudogamekeeper’s injury resulting from a S-H type I or II fracture of the proximal phalanx.
|
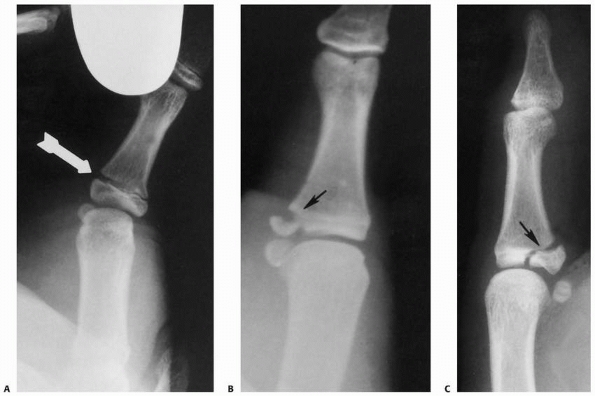 |
|
FIGURE 8-83 Spectrum of ulnar collateral ligament injuries of the thumb. A,B. On stress examination, a widening of the physis is seen. Varying sizes of fragments (B,C) may be associated with ulnar collateral ligament avulsion fractures (arrows). The size of the fragment is important with respect to the congruity of the MCP joint.
|
depends on the length of time since original injury, age of the
patient, and current level of function. Options range from
reconstruction to fusion.174
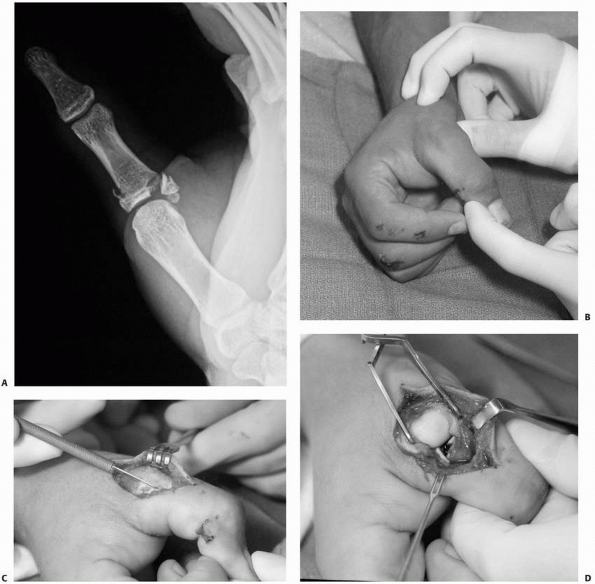 |
|
FIGURE 8-84 A. A 13-year-old boy with a displaced S-H III fracture of the right thumb proximal phalanx. B. Valgus instability on stress testing. C. Exposure through an incision of adductor aponeurosis. D. Fracture fragment exposed revealing rotation and displacement. (continues)
|
fingers and thumb should be stepwise and logical. The initial treatment
for simple dislocations is usually closed reduction. This requires
local anesthesia or conscious sedation to ensure comfort and eliminate
resistance. Irreducible dislocations require open reduction. It is
important to avoid multiple attempts at closed reduction of an
irreducible dislocation. A dorsal or volar approach is used with
removal of any interposed structure(s). The volar approach must respect
the taut digital nerves overlying the prominent metacarpal head.
Postoperative immobilization is used for 7 to 10 days, followed by
active motion with splint-protection; athletic activities are
restricted until healing is complete.
injuries or minimally displaced fractures are treated with cast
immobilization. Unstable ligamentous injuries or displaced fractures
are treated with open reduction.
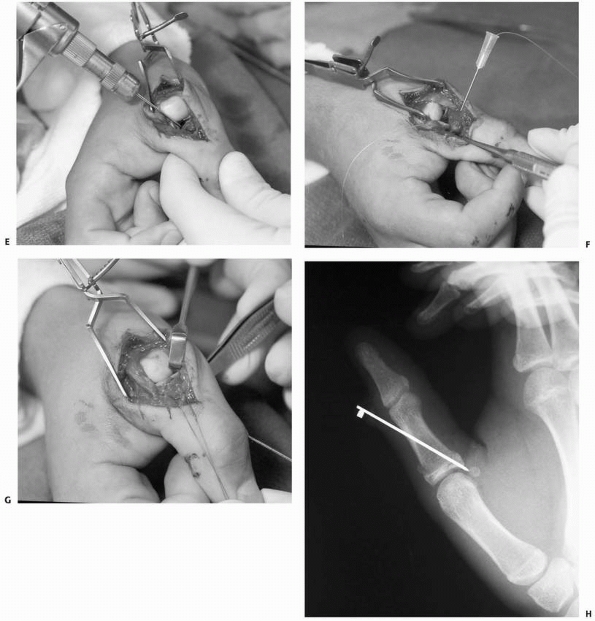 |
|
FIGURE 8-84 (continued) E. Antegrade Kirschner wire through fracture site. F. Thumb is placed into pronation and suture is passed for tension band fixation. G. Fracture reduced, Kirschner wire advanced, and suture tied in a figure-eight fashion. H.
After tension band fixation with restoration of joint and fracture alignment. (Courtesy of Shriners Hospitals for Children, Philadelphia, PA.) |
L, Lindau T, Arner M. Acutrak screw fixation versus cast immobilisation
for undisplaced scaphoid waist fractures. J Hand Surg Br
2001;26:192-195.
JM. Unstable fracture dislocations of the proximal interphalangeal
joint of the fingers: a preliminary report of a new treatment
technique. J Hand Surg Am 1978;3: 386-389.
MM. Extra-articular transverse fractures of the base of the distal
phalanx (Seymour’s fracture) in children and adults. J Hand Surg Br
2001;26:201-206.
MM. Juxta-epiphyseal fractures of the base of the proximal phalanx of
the fingers in children and adolescents. J Hand Surg Br 2002;27:24-30.
E, Ioakimidis E, Kasdan ML, et al. Reconstruction of the amputated
finger tip with a triangular volar flap. A new surgical procedure. J
Bone Joint Surg Am 1970; 52(5):921-926.
LW, Miller DL, Lockhart LD, et al. Metacarpophalangeal-joint
dislocations of the fingers. J Bone Joint Surg Am 1967;49(8):1587-1590.
PA, Weseley MS. Dorsal dislocation of the metacarpophalangeal joint of
the index finger treated by late open reduction. A case report. J Bone
Joint Surg Am 1972; 54-A: 1311-1313.
JL, Christian JD Jr, Goodwin HN, et al. A simplified technique for
treating the complex dislocation of the index metacarpophalangeal
joint. J Bone Joint Surg Am 1975;57(5):698-700.
MS, Dandrea LA, Davis HW. Hand injuries in children presenting to a
pediatric emergency department. Ann Emerg Med 1993;22:1519-1523.
GP. A morphologic study of the relationship of collateral ligaments to
growth plates in the digits. J Hand Surg Am 1983;8:74-79.
PG, Gelberman RH, Vandell RF, et al. Complex dislocations of the
metacarpophalangeal joint. Clin Orthop Relat Res 1982(164):208-210.
CD, Shin AY, McBride MT, et al. Percutaneous screw fixation or cast
immobilization for nondisplaced scaphoid fractures. J Bone Joint Surg
Am 2001;83-A(4):483-488.
U, McCollam SM, Oppikofer C. Comminuted fractures of the basilar joint
of the thumb: combined treatment by external fixation, limited internal
fixation, and bone grafting. J Hand Surg Am 1991;16(556-560).
RM Jr. Operative treatment of fractures and dislocations of the hand
and wrist region in children. Orthop Clin North Am 1990;21:217-243.
L, del Pinal F, Abascal F, et al. Imaging findings in ulnar-sided wrist
impaction syndromes. Radiographics 2002;22(1):105-121.
RB. Orthopaedic injuries in athletes (ages 6 to 17). Comparison of
injuries occurring in six sports. Am J Sports Med 1979;7:195-197.
RH, Wood MB, Cooney WP III. Nail bed repair and reconstruction by
reverse dermal grafts. J Hand Surg Am 1983;8:594-598.
JP. Transcarpal injuries associated with distal radial fractures in
children: a series of three cases. J Hand Surg Br 1992;17:311-314.
PA, Yu JS, Wiand W, et al. Suspected scaphoid fractures in skeletally
immature patients: application of MRI. J Comput Assist Tomogr
1997;21(4):511-515.
R, Waters PM. Remodeling of phalangeal neck fracture malunions in
children: case report. J Hand Surg Am 2004;29:458-461.
NJ, Kranik AD. An irreducible juxta-epiphyseal fracture of the proximal
phalanx. Report of a case. Clin Orthop Relat Res 1975(110):42-44.
HV, Chari PR, Crock MC. The blood supply of the wrist and hand bones in
man. In: Tubiana R, ed. The Hand. Philadelphia: W.B. Saunders, 1981,
335-347.
JC. Thiemann disease. Osteochondrosis juvenilis of the basal epiphyses
of the phalanges of the hand. Report of two cases. J Bone Joint Surg Br
1970;52:532-534.
Boeck H, Jaeken R. Treatment of chronic mallet finger deformity in
children by tenodermodesis. J Pediatr Orthop 1992;12:351-354.
Boeck H, Van Wellen P, Haentjens P. Nonunion of a carpal scaphoid
fracture in a child. A case report. J Orthop Trauma 1991;5:370-372.
Iturriza JR, Tanner JM. Cone-shaped epiphyses and other minor anomalies
in the hands of normal British children. J Pediatr 1969;75:265-272.
GL Jr, Moon NF. Rotational supracondylar fractures of the proximal
phalanx in children. Clin Orthop Relat Res 1972;83:151-156.
TA, Major NM, Helms CA. Cost-effectiveness of immediate MR imaging
versus traditional follow-up for revealing radiographically occult
scaphoid fractures. AJR Am J Roentgenol 2001;177:1257-1263.
BE, Waters PM, Wyzykowski RJ. Arthroscopic treatment of partial
scapholunate ligament tears in children with chronic wrist pain. J Bone
Joint Surg Am 2006;88(11): 2448-2455.
T, Roesch M, Wachter N, et al. Functional treatment of physeal and
periphyseal injuries of the metacarpal and proximal phalangeal bones. J
Pediatr Surg 2001;36(4): 611-615.
BT, Shin AY, Kozin SH. Scaphoid fractures in children. In: Shin AY, ed.
Scaphoid Fractures. Rosemont, IL: American Academy of Orthopaedic
Surgeons Monograph Series; 2007:85-95.
RA. Rupture of the central slip of the extensor hood of the finger. A
test for early diagnosis. J Bone Joint Surg Br 1986;68:229-231.
O, De Boeck H, Haentjens P. Fractures and nonunions of the carpal
scaphoid in children. Acta Orthop Belg 2001;67(2):121-125.
MD, McElfresh EC. Physeal and periphyseal injuries of the hand.
Patterns of injury and results of treatment. Hand Clin 1994;10:287-301.
RY, Hurst LC, Leppard J, et al. Complex dislocations of the PIP joint.
A pathoanatomic classification of the injury. Orthop Rev 1984;13:21-28.
H, Caputo RJ, Carter V, et al. Comparison of short and long thumb-spica
casts for nondisplaced fractures of the carpal scaphoid. J Bone Joint
Surg Am 1989; 71(3):354-357.
GE, Shaw DG. Lunate subluxation associated with a Salter-Harris type 2
fracture of the distal radius. J Hand Surg Br 1994;19:193-194.
A, Jones IE, Taylor RW, et al. Dynamic and static tests of balance and
postural sway in boys: effects of previous wrist bone fractures and
high adiposity. Gait Posture 2003;17(2):136-141.
DP, Anderson JR. Closed reduction and percutaneous pin fixation of
fractured phalanges. J Bone Joint Surg Am 1973;55(8):1651-1654.
DP, Terry GC. Complex dislocation of the metacarpophalangeal joint.
Correlative pathological anatomy. J Bone Joint Surg Am
1973;55:1480-1486.
WW, Pyle SI. Radiographic Atlas of Skeletal Development of the Hand and
Wrist. Stanford, CA: Stanford University Press; 1959.
AH, Schweitzer ME, Morrison WB, et al. Limitations of MR imaging in the
diagnosis of peripheral tears of the triangular fibrocartilage of the
wrist. AJR Am J Roentgenol 2002;178(2):419-422.
RW. Cold-induced digital epiphyseal necrosis in childhood (symmetric
focal ischemic necrosis). Can J Surg 1972;15:168-178.
RS, Horrell ED, Pierret GP. Treatment of mallet finger due to
intra-articular fracture of the distal phalanx. J Hand Surg Am
1978;3:361-363.
JE, Desai VV, Schranz PJ, et al. Acute fractures of the scaphoid.
Treatment by cast immobilisation with the wrist in flexion or
extension? J Bone Joint Surg Br 1999;81(1):91-92.
FM, Janda DH. Tendon and ligament attachments in relationship to growth
plate in a child’s hand. J Hand Surg Br 1989;14:315-318.
DT II, Jordan TF III. Physeal phalangeal fracture with flexor tendon
entrapment. A case report and review of the literature. Clin Orthop
Relat Res 1990;250: 194-196.
WL, Cohen MR. Complete remodeling of displaced fractures of the neck of
the phalanx. J Bone Joint Surg Br 2003;85:273-274.
KA, Ross DC, Patterson SD, et al. Dorsal perilunate dislocations and
fracture-dislocations: questionnaire, clinical, and radiographic
evaluation. J Hand Surg Am 2000;25(6):1069-1079.
TC, Hatton M, Davis TR. A prospective, randomized controlled study of
fixation of long oblique and spiral shaft fractures of the proximal
phalanx: closed reduction and percutaneous Kirschner-wiring versus open
reduction and lag screw fixation. J Hand Surg Br 2003;28:5-9.
JC, Watts HB, Glasgow JD. Dorsal dislocation of the metacarpophalangeal
joint of the index finger with particular reference to open
dislocation. J Bone Joint Surg Am 1967;49(8): 1572-1578.
ML, Taleisnik J. Nonunion of metacarpal extraarticular fractures in
children: report of two cases and review of the literature. J Pediatr
Orthop 1986;6(3):352-355.
KJ, Haigh SF, Symonds KE. MRI in the management of scaphoid fractures
in skeletally immature patients. Pediatr Radiol 2000;30(10):685-688.
NF, Jupiter JB. Irreducible palmar dislocation of the proximal
interphalangeal joint associated with an epiphyseal fracture of the
middle phalanx. J Hand Surg Am 1985;10:261-264.
W, Ecklund K, Di Canzio J, et al. Normal ranges of scapholunate
distance in children 6 to 14 years old. J Pediatr Orthop
2001;21(4):464-467.
T, Bae DS, Waters PM. The results of tenodermodesis for severe chronic
mallet finger deformity in children. J Pediatr Orthop 2008;28(1):81-85.
J. Doppelseitige verdrummung des kleinfingr-grundgleides als
selbstandiges krankheitsbild. Fortschr Geb Rontgenstr 1927;36:804.
WB, Bowers WH. Fractures and ligamentous injuries to the hand. In: Bora
FW Jr, ed. The Pediatric Upper Extremity: Diagnosis and management.
Philadelphia, PA: W.B. Saunders, 1988.
PR, Janes JM. Twenty-year follow-up of an unreduced dislocation of the
first metacarpophalangeal joint in a child. Report of a case. J Bone
Joint Surg Am 1969; 51(6):1216-1218.
WG, Friedman RL, Urbaniak JR. Bilateral nonunion of the carpal scaphoid
in a child. A case report. J Bone Joint Surg Am 1995;77(1):124-126.
K, Sumi H, Sumi Y, et al. Wrist fractures from snowboarding: a
prospective study for three seasons from 1998 to 2001. Clin J Sport Med
2004;14(2):64-71.
JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and
progressive perilunar instability. J Hand Surg Am 1980;5:226-241.
CM, Waters PM. Late presentation of a ligamentous ulnar collateral
ligament injury in a child. J Hand Surg Am 1994;19:1048-1049.
T, Benson WM, Foster BK, et al. Statistical analysis of the incidence
of physeal injuries. J Pediatr Orthop 1987;7(5):518-523.
K, Doi K, Kuwata N, et al. Scaphoid fracture in the young
athlete—therapeutic outcome of internal fixation using the Herbert
screw. Arch Orthop Trauma Surg 2002;122(9-10):510-513.
AF, Stark HH. Closed dislocation of the metacarpophalangeal joint of
the index finger. J Bone Joint Surg Am 1967;49(8):1579-1586.
T, Ogino T. Epiphyseal destruction of children’s hands after frostbite:
a report of two cases. J Hand Surg Am 1986;11:289-292.
R, Sadler AH. An isolated, closed, complex dislocation of the
metacarpophalangeal joint of the long finger: a unique case. J Hand
Surg Am 1986;11:558-561.
AK, Linscheid RL. Irreducible dorsal dislocation of the distal
interphalangeal joint of the finger. J Hand Surg Am 1977;2:406-408.
A, Martos F, Mut T, et al. Transscaphoid perilunate dislocation in a
child. A case report. Acta Orthop Scand 1981;52(1):31-34.
DR, Braunstein EM, Shirazi KK. Carpal ligamentous laxity with bilateral
perilunate dislocation in Marfan syndrome. Skeletal Radiol
1985;13:62-64.
RY, Segal D. Carpal scaphoid fracture and nonunion in an 8-year-old
child. Report of a case. J Bone Joint Surg Am 1983;65(8):1188-1189.
A, Basu AK, Vaidhyanath R, et al. Hand fractures: a study of their site
and type in childhood. Clin Radiol 2001;56(8):667-669.
GM, Mullins PT. Skin necrosis complicating mallet finger splinting and
vascularity of the distal interphalangeal joint overlying skin. J Hand
Surg Am 1987;12:548-552.
ME, Raskin KB. Retrograde compression screw fixation of acute proximal
pole scaphoid fractures. J Hand Surg Am 1999;24:1206-1210.
S, Caine D, Singer KM. Stress changes of the distal radial epiphysis in
young gymnasts. A report of 21 cases and a review of the literature. Am
J Sports Med 1985; 13:301-308.
PB, Gelberman RH. Irreducible dislocation of the interphalangeal joint
of the thumb. J Bone Joint Surg Am 1978;60(3):400-401.
WE. Evaluation of the humpback scaphoid by computed tomography in the
longitudinal axial plane of the scaphoid. J Hand Surg Am
1988;13:182-187.
RR. Dynamic traction and early passive movement for fractures of the
proximal interphalangeal joint. J Hand Surg Am 1986;11:850-858.
G, Schonenberger F. Treatment of fractures in children and adolescents.
In: Weber BG, Brunner C, Freuler F, eds. Fracture of the Hand. New
York: Springer-Verlag, 1980:218-225.
M, Seki T, Yoshizu T, et al. Microsurgical toenail transfer to the
hand. Plast Reconstr Surg 1991;88(1):102-109; discussion 110.
BP, Peters TT. Subcondylar fossa reconstruction for malunion of
fractures of the proximal phalanx in children. J Hand Surg Am
1987;12(6):1079-1082.
JF III, Geissler WB, Gutow AP, et al. Percutaneous internal fixation of
selected scaphoid nonunions with an arthroscopically assisted dorsal
approach. J Bone Joint Surg Am 2003;85-A(Suppl 4):20-32.
DG, Geist RW, Cooperman DR. Microscopic examination of a naturally
occurring epiphyseal plate fracture. J Pediatr Orthop 1985;5(3):306-308.
S, Jupiter JB. Salter-Harris type II and IV epiphyseal fractures in the
hand treated with tension-band wiring. J Pediatr Orthop 1999;19:233-235.
SP, Bishop AT, Berger RA. Use of the 1, 2 intercompartmental
supraretinacular artery as a vascularized pedicle bone graft for
difficult scaphoid nonunion. J Hand Surg Am 2002;27:391-401.
B. Displacement of the ruptured ulnar collateral ligament of the MCP
joint of the thumb. A clinical and anatomical study. J Bone Joint Surg
Br 1962;44:869-879.
B. Hyperextension injuries to the metacarpophalangeal joint of the
thumb: rupture of ligaments, fracture of sesamoid bones, rupture of
flexor pollicis brevis. An anatomical and clinical study. Acta Chir
Scand 1963;125:275-293.
PJ, Roman RJ, Kiefhaber TR, et al. Pilon fractures of the proximal
interphalangeal joint. J Hand Surg Am 1991;16(5):844-850.
M, Nagy L, Buchler U. Rigid internal fixation of basilar fractures of
the proximal phalanges by cancellous bone grafting only. J Hand Surg Br
2001;26:455-458.
WD. Displaced intra-articular osteochondral fracture. Cause for
irreducible dislocation of the distal interphalangeal joint. J Hand
Surg Am 1982;7:77-78.
HC, Pyle SI, Cornoni J, et al. Onsets, completions, and spans of
ossification in the 29 bonegrowth centers of the hand and wrist.
Pediatrics 1962;29:237-249.
LC, Yong FC, Chong KC. Condylar advancement osteotomy for correcting
condylar malunion of the finger. J Hand Surg Br 2002;27:31-35.
V, Westerlund M. Fracture of the carpal scaphoid in children. A
clinical and roentgenological study of 108 cases. Acta Orthop Scand
1980;51(6):909-913.
RM, Gelberman RH, Evans EF. Scaphocapitate fractures. Patterns of
dislocation, mechanisms of injury, and preliminary results of
treatment. J Bone Joint Surg Am 1980;62(2):271-276.
PM, Stewart SL. Surgical treatment of nonunion and avascular necrosis
of the proximal part of the scaphoid in adolescents. J Bone Joint Surg
Am 2002;84-A(6): 915-920.
PM, Taylor BA, Kuo AY. Percutaneous reduction of incipient malunion of
phalangeal neck fractures in children. J Hand Surg Am 2004;29:707-711.
HK, Ballet FL. The SLAC wrist: scapholunate advanced collapse pattern
of degenerative arthritis. J Hand Surg Am 1984;9:358-365.
HS, Wu WC, Chang RY, et al. Percutaneous cannulated screw fixation of
acute scaphoid waist fracture. J Hand Surg Br 2002;27(1):42-46.
