Ankle Fractures
Management of these fractures depends on careful identification of the
extent of bony injury as well as soft tissue and ligamentous damage.
This chapter will deal with rotational injuries that involve the
supramalleolar region of the distal tibia and fibula down to the talar
dome. Once defined, the key to successful outcome following rotational
ankle fracture is anatomic restoration and healing of the ankle mortise.95,177,178
In this chapter, we will discuss the pertinent anatomic and biomechanic
considerations and how they affect injury characteristics. Evaluation
of the suspected ankle fracture will include a detailed history,
physical examination, appropriate radiographic examination, and initial
treatment options. We will then discuss the management options based on
the classification systems of Lague-Hansen,111
whose sentinel work on the mechanistic classification of these injuries
remains the standard more than 50 years later, and the AO-Orthopaedic
Trauma Association (OTA) system based on the work of Weber and Danis.46,236
Operative treatment of these fractures will be discussed in a stepwise
manner, with alternate options proposed. New techniques and
technologies will be discussed as well as outcomes.
injuries involving a twisting mechanism. These injuries reflect the
relative strength of the ligamentous components of the ankle mortise
compared with the bone. Observational studies have demonstrated that
both the incidence and severity of ankle fractures in elderly patients
has significantly increased over the last 30 years. Currently in the
United States, ankle fractures have been reported to occur in as many
as 8.3 per 1000 Medicare recipients. Similarly, Kannus et al.96
reported that among Finnish patients older than 70 years, the number of
ankle fractures occurring between 1970 and 2000 increased three-fold.
The authors also showed an increase in the more unstable Lauge-Hansen
supination-external rotation stage IV fractures, compared
with more stable ankle fracture patterns in this elderly patient population.
with improved implants and fixation techniques have led to an increased
trend toward surgical fixation for most unstable ankle fracture
patterns despite patient age.
rotational mechanism. Patients may describe a twisting motion around a
planted foot or a sudden inversion type injury when landing from a
jump. The mechanism of the injury is similar to those sustained in
simple ankle sprains and in fact represents the continuum of this
injury. Although each ankle fracture has its own “personality,” the
vast majority of these injuries do not represent high-energy
mechanisms, although they can be sustained in falls from height and
motor vehicle accidents.
times difficult to diagnose. The most commonly missed injuries include
Achilles tendon ruptures, lateral process of the talus fractures,
metatarsal fractures, and anterior process of the calcaneus fractures.
provide a history of trauma. The mechanism of injury is often as benign
and low-energy as an awkward step off a curb but may also be associated
with a high-energy motor vehicle accident. No matter what the mechanism
of injury, a consistent and through history and physical examination is
required to fully characterize the injury and develop a treatment
algorithm.
 |
|
FIGURE 57-1 Example of severe fracture blisters associated with an unstable ankle fracture dislocation.
|
circumstance of the injury. Patients oftentimes are able to provide a
history of the mechanism of injury, although obtunded or
polytraumatized patients may not be able to give a reliable history.
Perhaps the most important aspect of the history is the status of the
ankle before the injury as this may affect both diagnosis and
treatment. A history of prior neuropathy, diabetes, congenital or
neurologic disorders, history of stroke, vascular insufficiency ulcers,
history of smoking, as well as a history of previous injuries to the
ankle must be elicited and documented in the patient’s chart. Other
crucial information is the chronicity of the injury to the time of
presentation at the emergency department, which may affect the urgency
toward surgical repair. As in any other injury, documentation of the
patient’s perceived mechanism of injury is critical for both medical
legal and clinical reasons. All these factors are taken together to
help target the physical examination and form a treatment plan.
conducted in a methodical and comprehensive fashion in every case to
avoid missing associated and occult injuries. Inspection begins with
observation of the soft tissue envelope. Attention should be noted to
the degree of swelling; presence of fracture blisters should be noted
as well as their nature (serous or blood filled) (Fig. 57-1).
Areas of ecchymosis can provide a good indication of the location of
injury. The location and size of any associated wounds should also be
noted as certain types of open wounds indicate a specific
fracture-dislocation pattern (open wound over medial malleolus
indicates a lateral ankle fracture dislocation). Tenting of the skin
associated with deformity is important to note preoperatively, and that
area should be monitored postoperatively for late ischemic changes.
the dorsalis pedis and posterior tibial pulses as this part of the
examination is often neglected. Palpation should then reveal the skin
temperature of the foot and ankle. Sensation should be tested
and
compared with the contralateral side if it is not injured. The
superficial peroneal nerve provides sensation to the dorsum of the foot
with the exception of the first web space, which is innervated by the
terminal branch of the deep peroneal nerve. Even minor ankle sprains
can be associated with superficial peroneal nerve injuries and a
careful examination is the best way to assess the status of the
peroneal nerve.186 The saphenous nerve supplies the medial side of the ankle.
|
TABLE 57-1 Ankle Joint Normal Range of Motion22,186
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
palpation along the shaft of the fibula where a fracture may be present
indicating a Maisonneuve type of injury. The “squeeze test” has been
described as a diagnostic test for syndesmosis injury and is performed
by squeezing the fibula towards the tibia in the proximal calf, which
causes separation at the distal tibial-fibular joint, and elicits pain
when the syndesmosis is disrupted.88,219,254
The external rotation test for syndesmosis stability may also be
performed at this time by assessing for pain over the syndesmosis while
externally rotating the foot and holding the knee in a 90-degree flexed
position.254 The Thompson test for
the assessment of the continuity of the Achilles tendon can be
performed at this time before proceeding to a direct examination of the
ankle. The Thompson test is a passive test performed by compression of
gastrocnemius muscle belly and assessing for plantarflexion of the
foot. Failure of plantarflexion of the foot indicates a ruptured
Achilles tendon.220
with a sequential assessment of the ankle ligaments with special
attention to tenderness over the deltoid ligament. The anterior drawer
test of the ankle is performed by stabilizing the tibia with one hand
while cupping the posterior calcaneus with the other and imparting an
anterior translational force. Laxity relative to the other ankle may
indicate an anterior talofibular ligament injury or an unstable
fracture pattern. The ability of the patient to weight bear should be
assessed. Other areas of associated injuries that should be palpated
are the base of the fifth metatarsal, the anterior process of the
calcaneus, lateral process of the calcaneus, as well as the Lisfranc
joint, all of which may be injured via the same mechanism causing the
ankle injury.
 |
|
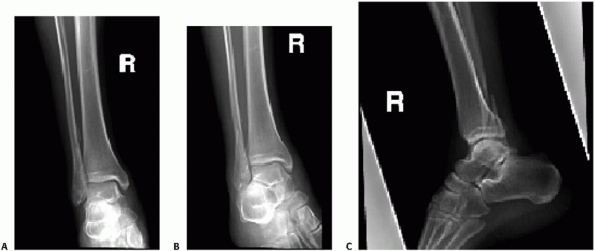
FIGURE 57-2 Example of standard ankle trauma series including AP (A), mortise (B), and lateral (C).
|
toe motion and ankle motion. It is imperative that a full motor and
sensory examination be completed before manipulation of the injured
ankle and the findings documented before and immediately following the
manipulation. Clearly, a dislocated ankle or a severe ankle injury
affords a limited ankle examination; however, any motor function that
can be examined should be documented. Normal range of motion of the
ankle joint is detailed in Table 57-1.
anteroposterior (AP), 15-degree internal rotation AP (mortise), and
lateral views (Fig. 57-2). Using these three
views is best for ensuring that the diagnosis of fracture instability
is made; however, AP and lateral views only can be sufficient and may
provide a great deal of information regarding the integrity of the
ankle.26 To manage the large volume
of ankle injuries of patients who present to emergency and subacute
settings, certain criteria have been established for requiring ankle
radiographs. Based on the Ottawa Ankle Rules, the patients who merit a
radiograph evaluation are listed in Table 57-2.
found to be both cost effective and reliable (up to 100% sensitivity),
their implementation has been inconsistent in general clinical practice.7,34,61
however, in the setting of significant ankle injuries such as
fracture-dislocations or fractures sustained via a high-energy
mechanism to obtain films of the foot as well as the knee to rule out
associated injuries for which the ankle injury serves as a distraction
and may lead to a missed diagnosis. A tibial-fibular radiograph is
indicated if physical examination points to tenderness over the shaft
of the fibula as this may represent a Maisonneuve pattern injury.
|
TABLE 57-2 Ottawa Ankle Rules205,206,207
|
|
|---|---|
|
identified in order to establish the integrity of the joint. An initial
evaluation of the radiographs should first focus on the tibiotalar
articulation and assess for fibular shortening, widening of the joint
space, malrotation of the fibula, and talar tilt. The specific anatomic
relationships that need to be established radiographically are listed
in Table 57-3.
the tibia and fibula on the mortise film, represented by differences in
measurements of the medial, superior, and lateral clear spaces, may
indicate ankle instability and subluxation. The degree to which an
asymmetry at the mortise is tolerable is controversial, although 1 mm
of tibiotalar displacement has been shown in a static cadaveric ankle
model to decrease the contact area by 42%.183
Dynamic cadaveric ankle models have disputed the existence of this
decrease in contact area; however, the current standard of care is to
achieve an anatomic reduction of the mortise on static
non-weight-bearing films.39
Therefore, after an initial cursory evaluation of radiographs is
completed as a screen for an osseous ankle injury, a more detailed
evaluation of each view should then be undertaken with quantification
of specific radiographic relationships.
|
TABLE
57-3 Radiographic Relationships Indicating Fibular Shortening, Syndesmosis Disruption, Medial Malleolar Fractures, Posterior Malleolar Fracture, and Deltoid Ligament Rupture |
||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
adequate reduction with the foot in neutral have been established and
validated.95,177
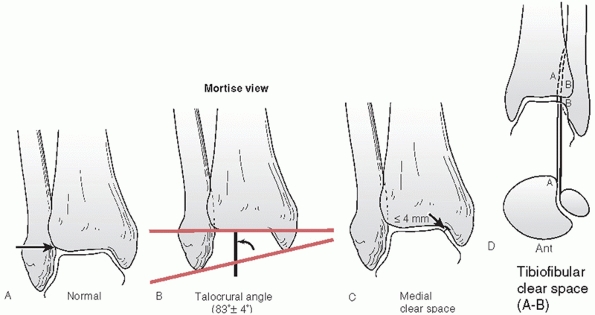
Parameters that suggest unstable fracture patterns include lateral
malleolar displacement greater than 2 mm with resultant talar shift on
the AP or lateral, significant medial malleolar displacement, deltoid
ligament disruption defined by greater than 5 mm medial clear space,
syndesmosis injury identified by tibial-fibular clear space greater
than 5 mm or tibial-fibular overlap of less than 10 mm (both on the
AP), or a tibial-fibular overlap of less than 1 mm on the mortise view (Fig. 57-3).
the talocrural angle and the “ball sign.” The talocrural angle is
measured between a line perpendicular to the tibial plafond and a line
connecting the tips of the medial and lateral malleoli. Normal range is
83 ± 4 degrees or a deviation from the talocrural angle measurement on
the contralateral side197 (see Fig. 57-3).
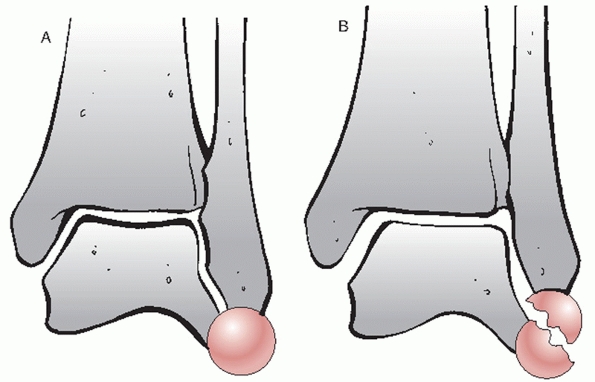
The “ball” or “dime sign” is described on the AP view as an unbroken
curve connecting the recess in the distal tip of the fibula and the
lateral process of the talus when the fibula is out to length (Fig. 57-4).240
bimalleolar ankle fractures; however, this is not the case when a
fibula fracture occurs in association with a medial-sided ligamentous
injury. Traditional teaching has in the past mandated that where the
physical examination points toward a medial-sided injury, a manual
stress view of the ankle should be performed.167,169,170,171
The purpose of the stress view is to identify deltoid ligament injury
by creating a widening of the medial clear space, which would be
indicative of potential instability. To obtain an accurate stress test,
the ankle must be stressed in dorsiflexion and external rotation.120,172 Although the validity of the stress view has been recently called into question, when positive stress
examinations have been elicited in fractures where no medial sided
symptoms existed, a stress view is still advocated at most centers.53,130,176
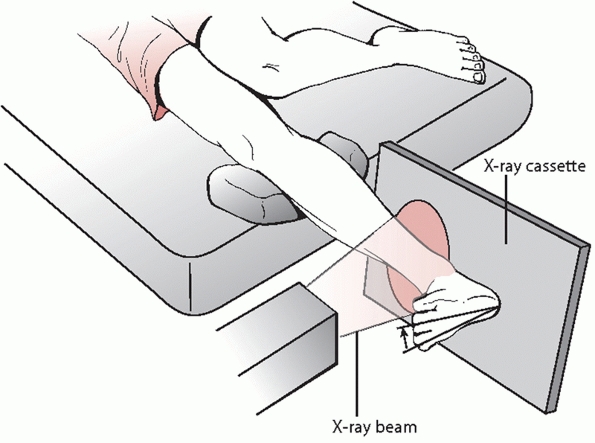
Another method for performing a stress test is the gravity stress view.
Advocated as a less painful stress view, it was originally described in
cadaveric specimens and later validated clinically.141,200
During the gravity stress view, the patient lies in the lateral
decubitus position on the side of the affected ankle with the distal
leg, ankle, and foot allowed to hang dependent off the end of the table
while a mortise view is obtained (Fig. 57-5).
This patient positioning, in effect, acts to impart an external
rotational force as in the manual stress view. Without
physician-assisted dorsiflexion of the ankle, however, a false widening
of the mortise may be seen as the talus is wider anteriorly than
posteriorly.
 |
|
FIGURE 57-3 Radiographic appearance of the normal ankle on mortise view. A. The condensed subchondral bone should form a continuous line around the talus. B.
Talocrural angle should be approximately 83 degrees. When the opposite side can be used as a control, the talocrural angle of the injured side should be within a few degrees of the noninjured side. C. The medial clear space should be equal to the superior clear space between the talus and the distal tibia and less than or equal to 4 mm on standard radiographs. D. The distance between the medial wall of the fibula and the incisural surface of the tibia, the tibiofibular clear space, should be less than 6 mm. |
 |
|
FIGURE 57-4 A.
The “ball” or “dime sign” is described on the AP view as an unbroken curve connecting the recess in the distal tip of the fibula and the lateral process of the talus when the fibula is out to length. B. Fibula malreduced in a shortened position, ball sign is absent. |
of ankle fractures is limited. The CT scan provides cross sectional
information, which clarifies the relationship of the tibia and fibula
at the mortise, the fit of the talus within the mortise, as well as
information regarding possible associated injuries to the peroneal or
posterior tibial tendons.191,192,193,217
The greatest asset of CT scans in the setting of ankle fractures is to
diagnose tibial plafond impaction injuries, posterior malleolar
fractures, and
associated injuries of the talus.123,147,148
The size of the posterior malleolar fragment, which determines
operative treatment, is notoriously poorly quantified on plain films
with low interobserver and intraobserver reliability. The CT scan is
clearly useful in cases where the size of the posterior malleolus is
questionable.60 Other uses for CT scans of the ankle are evaluation of chronic ankle sprains and subtalar injuries.136,137
 |
|
FIGURE 57-5
During the gravity stress view, the patient is made to lie in the lateral decubitus position on the side of the affected ankle with the distal leg, ankle, and foot allowed to hang dependent off the end of the table while a mortise view is obtained. This patient positioning, in effect, acts to impart an external rotational force as in the manual stress view. |
three-dimensional intraoperative imaging has become available and has
been found useful in ankle fracture surgery. Use of this machine allows
for images comparable to those obtained via a CT scanner to be obtained
intraoperatively and can help guide reductions, especially of
articulations that are difficult to assess with plain films such as the
syndesmosis.9,188 The major drawback of using this technology is its current high costs.
acute evaluation of ankle injuries is mainly used to evaluate the
tendinous structures. In patients presenting with chronic or
unresolving pain, MRI is useful in evaluation of chronic ligament
ruptures as well as evaluation of the articular cartilage and possible
osteochondral injuries impeding the recovery of the patient.35,120
represent the two most commonly used classification systems for ankle
fractures. The Lauge-Hansen classification system is a mechanism of
injury-based scheme that uses radiographic fracture patterns to
describe the mechanism of injury.111
The Danis-Weber classification became the basis of the AO-OTA
classification system, which is based on the location of fracture lines
and the location of the fibula fracture in relation to the level of the
syndesmosis. Although both classification systems address the osseous
and ligamentous injury patterns and lend information regarding the
severity of the architectural derangement of the ankle, none of these
classification systems address soft tissue issues such as open
fracture, blistering, or neurovascular compromise. It is important to
note and describe the fracture as well as the soft tissue envelope in
which the injury is contained to be able to provide the appropriate
treatment.
It is perhaps the recognition that the fracture pattern is associated
with a rotational injury, as opposed to an axial load type of injury,
which must be ascertained before assigning the injury a classification
system. The Lauge-Hansen classification system was developed from a
cadaveric experiment where the tibia was fixed and a rotational
deforming force was applied to the ankle in one of three different
directions. For a given foot position and deforming force at the ankle,
a consistently reproducible pattern of osseous and ligamentous injury
was described. The first part of the name in the classification system
describes the position of the foot at the time of injury, while the
second part of the name describes the direction of force applied to the
foot. Four injury patterns are described: supination-adduction (SA),
supination-external rotation (SER), pronation-adduction (PA), and
pronation-external rotation (PER).
supinated foot experiences a forceful adduction force without a
rotational moment (see Fig. 57-6). Here, the
first structure injured is either the lateral collateral ligament or
the fibula. A fibula fracture created by this mechanism appears as a
low transverse fracture line at a level below the syndesmosis. As the
severity of the adduction moment increases, the talus gets displaced
toward the medial malleolus and a vertical fracture line is created
extending from the medial axilla of the joint and proximally into the
metaphyseal cortex of the tibia. This tends to be a large shear
fragment and is rarely associated with comminution at the medial
malleolus. Frequently, the medial tibial plafond will present an
impaction injury, which is not always easily recognized on plain films
although CT scan will demonstrate this injury clearly.
 |
|
FIGURE 57-6 Schematic diagram and case examples of Lauge-Hansen SER and SA ankle fractures. A.
A supinated foot sustains either an external rotation or adduction force and creates the successive stages of injury shown in the diagram. The SER mechanism has four stages of injury, and the SA mechanism has two stages. (continued) |
 |
|
FIGURE 57-6 (continued) AP (B) and lateral (C)
radiographs show an unstable SER stage IV ankle fracture with the characteristic oblique distal fibula fracture and a medial side injury. D. An AP radiograph of a SA ankle fracture with a transverse fibula fracture and an impacted medial malleolar fracture. |
vertical shear pattern of the medial malleolus fracture is the sine que
non of this injury pattern and may be the only osseous injury with the
lateral-sided injury being purely ligamentous. The SA pattern
represents up to 20% of ankle fractures.76
Here, the foot is in a supinated position while an external rotation
force is imparted to the ankle relative to a fixed tibia. A shearing
force is therefore imparted to the fibula and the medial
osteoligamentous complex experiences an avulsion-type force.126
tibial-fibular ligament (ATFL) and, when present as an isolated injury,
represents an SER1 pattern. An SER2 injury is an oblique fracture line
of the fibula associated with either a midsubstance rupture of the ATFL
or an avulsion fracture of the ATFL insertion into the tibia (Chaput
tubercle) or its origin on the fibula (Wagstaffe tubercle). SER2 fibula
fractures share three common characteristics: minimal displacement,
fracture at the level of the syndesmosis but not affecting the
syndesmosis, and fracture line proceeding from distal anterior to
proximal posterior. SER3 injuries share all the characteristics of the
SER2 injuries with the addition of either a posterior tibial-fibular
ligament rupture or fracture of the posterior malleolus. In the SER4
pattern, the injury progresses to the medial-sided structures where the
medial malleolus osteoligamentous complex (MMOLC) is injured. The
injury may be an isolated medial malleolus fracture (an oblique
fracture line at the level of the axilla in the majority of cases), or
an isolated deltoid ligament injury (the deep and superficial portions
of the deltoid are ruptured) representing an SER4 “equivalent” lesion.
More recently, a combination of both a medial malleolus and deltoid
injury has been characterized (Fig. 57-7). In
this fracture pattern, the anterior colliculus of the medial malleolus
is fractured; while the posterior colliculus remains intact, the injury
passes through the deep fibers of the deltoid ligament that are
attached to the posterior colliculus of the medial malleolus.171,203,226
It has therefore been suggested that the size of the medial malleolar
fragment was the most important variable in predicting deltoid
competence. When the medial malleolus fragment is greater than 2.8 cm
wide (supracollicular fracture), the deltoid ligament is likely intact
and stress view is negative. When the fragment is less than 1.7 cm wide
(anterior collicular or intercollicular fracture), the deltoid may be
incompetent and the stress view should be performed. It is in the
situation where an SER4 equivalent lesion is suspected that a stress
view is advocated by some authors.167,169,170,171
As mentioned previously, the utility of the stress view has been called
into question by several authors who doubt its usefulness in
distinguishing ankle instability as widening has been found in ankles
without any medial symptoms and widening also was found in ankles with
negative MRIs of deltoid ligaments.103
 |
|
FIGURE 57-7
Combination of medial malleolus fracture and deltoid ligament disruption. The anterior colliculus of the medial malleolus is fractured, while the posterior colliculus remains intact. The injury passes through the deep fibers of the deltoid ligament that are attached to the posterior colliculus of the medial malleolus. (From Tornetta P 3rd. Competence of the deltoid ligament in bimalleolar ankle fractures after medial malleolar fixation. J Bone Joint Surg Am 2000;82A:843-848.) |
SER2 injury from an SER4 equivalent injury is evidence of anterior or
posterior subluxation of the talus, significant shortening (greater
than 2 mm) of the fibula, and mild lateral subluxation without any
stress. It is important to make the distinction between SER2 and SER4
injuries as the former have been shown to have a good outcome with
nonoperative treatment despite mild talar subluxation on stress views.15,37,106,232
The typical appearance is an avulsion-type medial malleolus fracture
while bending forces at the fibula create a relatively transverse
fracture or commonly have either lateral butterfly or comminution
related to the bending failure. The fibula usually fractures 5 to 7 cm
above the joint.117 As in most cases
of comminuted fractures, judging length and rotation is challenging,
making the operative fixation more difficult than the supination injury
patterns. As this injury represents the direct counterpart to the SA
injury that may present with a medial plafond impaction, an
anterolateral tibial plafond fracture may be present and may contribute
to residual talar tilt or subluxation.117,224
Stress radiographs are important to assess the integrity of the
syndesmosis and help differentiate direct blow injuries (stable) from
indirect injuries (unstable). Isolated medial malleolar fractures are
differentiated from higher-grade PA of PER injuries with the stress
radiograph as well. Intraoperatively, manual stress examination should
be performed following fibular fixation to assess integrity of the
syndesmosis.
occur when the pronated foot experiences an external rotator force and
account for up to 19% of all rotational ankle fractures.76
Here again, the medial osteoligamentous complex is the first injured
via either a direct deltoid ligament rupture or a transverse medial
malleolar fracture. The next structure injured is the anterior inferior
tibial-fibular ligament (AITFL), followed by a fibular fracture. The
characteristic fibular lesion is a fracture at a level above the
syndesmosis that is typically spiral in nature. The fibula fracture
progresses in a direction opposite from its SER4 counterpart as the
fracture line progresses from distal posterior to proximal and anterior.168
The last structure injured in this rotational mechanism is the
posterior tibial-fibular ligament or the posterior tubercle of the
distal tibia.111 Since the fibula
fracture is typically in the area proximal to the syndesmosis,
evaluation of the syndesmosis intraoperatively is critical since it may
be ruptured. The clinician should be aware that although the PER injury
is the most commonly seen injury that is associated with a syndesmosis
injury, SER and PA mechanisms can also be associated with a syndesmosis
disruption and should be evaluated accordingly.168
characterized by a proximal fibula shaft fracture. A Maisonneuve
fracture should always be suspected when an isolated medial malleolus
fracture is seen and is best screened for by palpation of the proximal
fibula and assessing for tenderness followed by a tibial-fibular
radiograph.
 |
|
FIGURE 57-8 Schematic diagram and case examples of Lauge-Hansen PER and PA ankle fractures. A.
A pronated foot sustains either an external rotation or abduction force and creates the successive stages of injury shown in the diagram. The PER mechanism has four stages of injury, and the PA mechanism has three stages. (continues) |
 |
|
FIGURE 57-8 (continued) An AP radiograph (B)
of the ankle and tibia and fibula demonstrate a high fibula fracture. External rotation stress shows lateral displacement of the talus and widening of the distal syndesmosis (C). These radiographs are characteristic of a PER rotation injury. D. An AP radiograph of a typical PA ankle fracture. The fibula is laterally comminuted. |
is based on the location of fracture lines and degree of comminution
and serves to describe the severity and degree of instability
associated with a particular fracture pattern.1,153
The AO-OTA classification expands on the Danis-Weber classification
scheme, which is still in use, is perhaps the most rudimentary of the
classification systems, and is based simply on the level of the fibula
fracture.47,239
A Weber type A has a fibula fracture below the level of the
syndesmosis. A Weber type B occurs at the level of the syndesmosis,
while a type C is above the level of the syndesmosis.
system to be inadequate as the level of the fibula fracture does not
consistently predict the degree of syndesmosis injury since both B and
C fractures may be stable after isolated fibular fixation. The Weber
classification also ignores the status of the medial-sided structures
and does not base treatment on the status of this vital
osteoligamentous structure.14,30,157
The AO-OTA classification uses the Weber classification as its basis
but has been expanded to include medial-sided injuries and ligamentous
avulsions from the distal tibia. Although more comprehensive, the
AO-OTA classification has also been found to have a limited
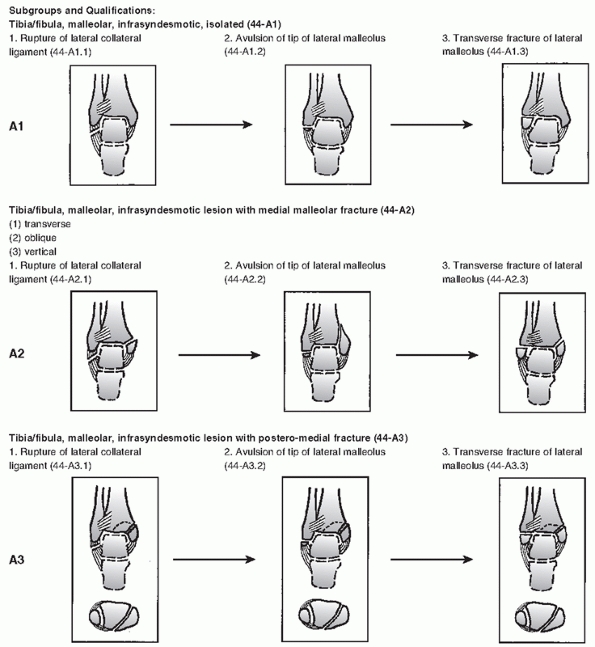
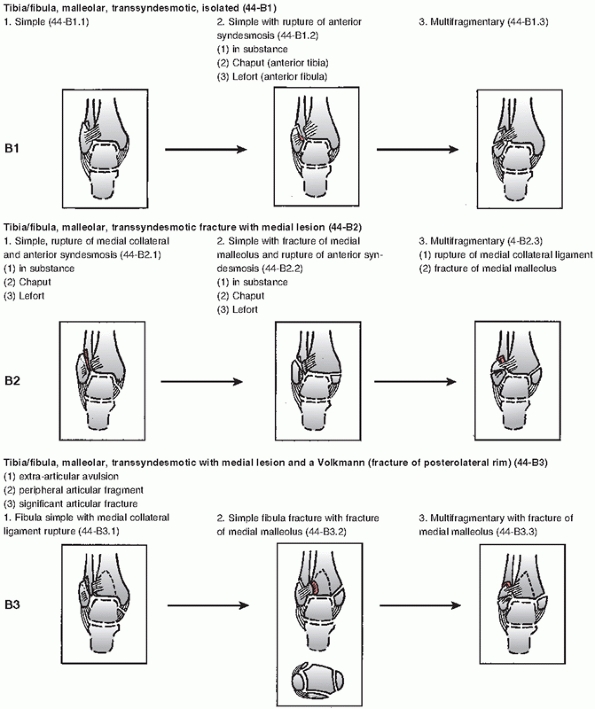
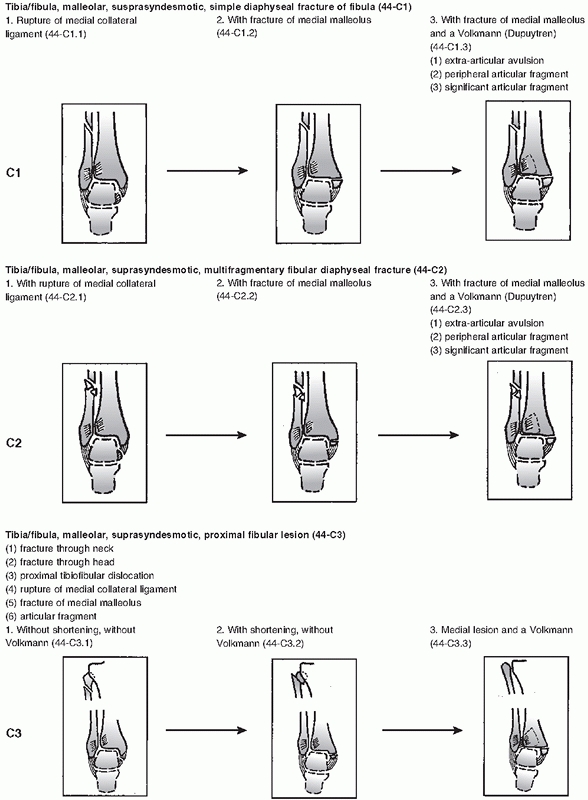
interobserver and intraobserver reliability.45,221 Details of the classification system are described in Figure 57-9.
 |
|
FIGURE 57-9
The AO-OTA classification. This classification system is based upon the location of fracture lines and degree of comminution and serves to describe the severity and degree of instability associated with a particular fracture pattern. The AO-OTA classification expands on the Danis-Weber classification scheme, which is still in use and is perhaps the most rudimentary of the classification systems and is based simply on the level of the fibula fracture. A. Basic fracture types. (continued) |
 |
|
FIGURE 57-9 (continued) B. Subtypes of “A-type” ankle fractures. (continued)
|
 |
|
FIGURE 57-9 (continued) C. Subtypes of “B-type” ankle fractures. (continued)
|
 |
|
FIGURE 57-9 (continued) D. Subtypes of “C-type” ankle fractures.
|
existing classification schemes are limited in their ability to fully
categorize many injuries. Two recent studies serve to underscore the
limitations of the current classification systems. A recent study that
attempted to correlate MRI findings with positive stress views has
found that there were no statistically significant correlations between
the medial clear space measurements and MRI documentation of complete
deltoid ligament rupture.103 Another
study comparing MRI findings to the Lauge-Hansen classification of a
particular fracture has found less than 50% correlation between the MRI
findings and the ligamentous injury predicted by the Lauge-Hansen
classification.68 As our
understanding of ankle fractures evolves, it is becoming clear that
treatment decisions should be based less rigidly on a classification
system, but rather that fracture classification serves as one data
point in the overall comprehensive evaluation of the fracture.
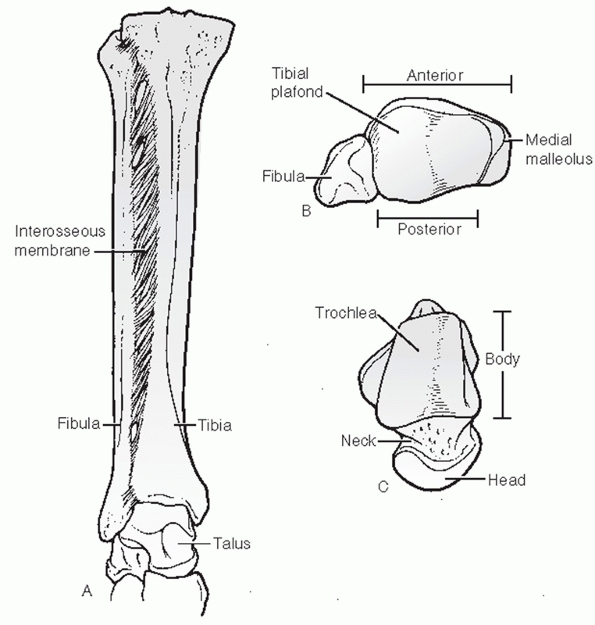
The ankle is a three-bone joint composed of the tibia, fibula, and
talus. The talus articulates with the tibial plafond superiorly, the
posterior malleolus of the tibia posteriorly, and the medial malleolus
medially. The lateral articulation of the talus is with the lateral
malleolus portion of the fibula. The joint is considered a saddle joint
with the talar dome being wider anteriorly then posteriorly. This
wedge-shaped footprint of the talar dome creates a situation whereby
the dorsiflexed position creates a stable bony articulation while the
plantarflexed position is more mobile and is stabilized by ligamentous
structures. As the ankle dorsiflexes, the wider anterior talus forces
the fibula to externally rotate through the syndesmosis (Fig. 57-10).
 |
|
FIGURE 57-10 Bony anatomy of the ankle. Mortise view (A), inferior-superior view of the tibiofibular side of the joint (B), and superior-inferior view of the talus (C).
The ankle joint is a threebone joint with a larger talar articular surface than matching tibiofibular articular surface. The lateral circumference of the talar dome is larger than the medial circumference. The dome is wider anteriorly than posteriorly. The syndesmotic ligaments allow widening of the joint with dorsiflexion of the ankle, into a stable, close-packed position. |
developed a static cadaveric biomechanical model and found that even a
1-mm lateral talar shift within the mortise decreases the joint contact
area by 42%. Further research has expanded on this finding. Clarke et
al.39 developed an axially loaded
cadaver ankle model testing tibiotalar stability in bimalleolar ankle
fractures. Their findings showed that with a 6-mm lateral displacement
of the lateral malleolus, there was no significant change on the
contact area of the ankle as long as it was axially loaded. However,
once the deltoid ligament was sectioned, all ankles showed a
significant decrease in tibiotalar contact area. This result was
consistent with the observation that the pattern of instability was not
a straight lateral translation but rather anterolateral rotation
underneath the tibial plafond. In a follow-up study, Michelson and
Waldman139 used a similar
unconstrained axially loaded cadaver model to assess instability in SER
fracture models. This study confirmed that in an axially loaded,
isolated lateral fibula fracture without medial malleolus or deltoid
ligament disruption, there was no appreciable loss of tibiotalar
contact and that the deltoid ligament, specifically
the deep portion, served as a main checkrein to anterolateral rotation of the ankle.136
applied their unconstrained axially loaded cadaver ankle model to show
that in the face of intact medial structures, even a syndesmotic injury
is not destabilizing. In this iteration of the cadaver experiment, when
the medial osteoligamentous structures were disrupted along with a high
fibular fracture and a disrupted syndesmosis, the talus dislocated from
the mortise. When the medial structures were intact, the talus remained
reduced. Solari et al. also demonstrated the importance of the medial
malleolus in the stability of Weber C fractures in a cadaver study
evaluating the need for syndesmotic screws.205
In this study, the rotational component of instability was assessed
specifically. A Weber C fracture pattern where the medial malleolus
alone was treated attained 56% of total rotational talar stability,
isolated lateral malleolus fixation attained 36% stability, and
fixation of the lateral malleolus and medial malleolus (without
syndesmotic fixation) attained 76% of total stability. Their conclusion
was that the medial malleolar osteoligamentous complex is the single
most important contributor to ankle stability in Weber C fracture
patterns.
of the medial malleolus to which the fibers of the deltoid ligament are
attached. When discussing the anatomy and function of the medial
malleolus, it is important to understand its close interrelationship to
the deltoid ligament, which originates from it. The most accurate
description of what we will refer to as the MMOLC was provided by
Pankovich et al. and Skie et al. in cadaveric studies.171,203
malleolus, which is composed of the anterior and posterior colliculi
separated by the intercollicular groove. The anterior colliculus is the
narrower and most distal portion of the medial malleolus and serves as
the origin of the superficial deltoid ligaments. The intercollicular
groove and the posterior colliculus, which is broader than the anterior
colliculus, provide the origin of the deep deltoid ligaments. The
insertions of the deltoid ligaments (medial tubercle of the talus,
navicular tuberosity, and the sustentaculum tali) can also be
considered part of the MMOLC.
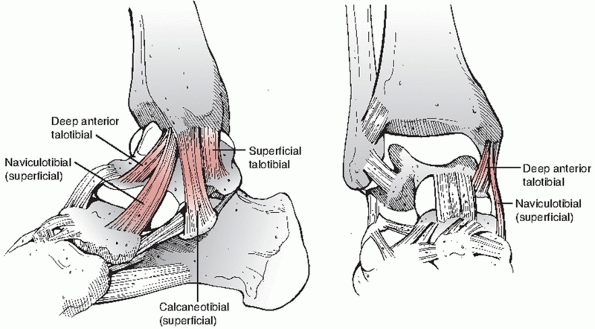 |
|
FIGURE 57-11 The deltoid ligament and its individual components.
|
and deep, comprises the rest of the MMOLC. The superficial deltoid,
originating from the anterior colliculus, has three main components.
The naviculotibial ligament is most anterior portion of the superficial
deltoid inserting on the dorsomedial navicular. The strongest portion
of the superficial deltoid is the calcaneotibial ligament, which
inserts at the sustentaculum tali. The most posterior structure of the
superficial deltoid is the superficial talotibial ligament, which
inserts at the medial talar tubercle.
anterior talotibial ligament, originating from the intercollicular
groove deep to the calcaneotibial ligament, inserts on the medial
talus. The deep posterior talotibial ligament originates from the
intra-articular aspect of the posterior colliculus and inserts on the
medial talus. This ligament is the strongest and thickest ligament of
the deltoid complex. This intra-articular ligament is not accessible
from outside the joint. Also important to consider is the close
approximation of the posterior tibial and flexor hallucis tendons to
the deltoid ligament as their tendon sheaths are essentially contiguous
with the insertions of the deltoid ligament complex (Fig. 57-11).
anterior and posterior tubercles. The anterior tubercle (Chaput
tubercle) is the origin of the AITFL, and the posterior tubercle is the
origin of the deep component of the posterior inferior tibiofibular
ligament (PITFL). The anterior tubercle overlaps the fibula, and this
relationship is the basis of the radiologic interpretation of the
status of the syndesmosis. The more superficial fibers of the posterior
tibiofibular ligaments are also attached to the posterior tubercle and
are typically not injured in trimalleolar fractures. This serves to
tether the posterior malleolus to the lateral malleolus and is the
basis for the observed indirect reduction
of the posterior malleolar fragment with restoration of fibular length.
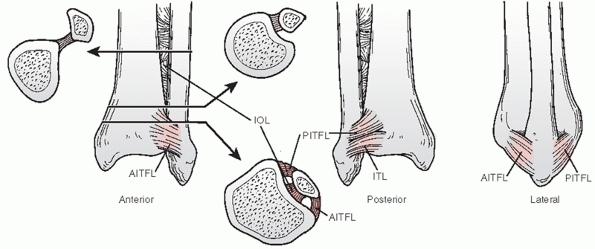 |
|
FIGURE 57-12
Three views of the tibiofibular syndesmotic ligaments. Anteriorly, the AITFL spans from the anterior tubercle and anterolateral surface of the tibia to the anterior fibula. Posteriorly, the tibiofibular ligament has two components: the superficial PITFL, which is attached from the fibula across to the posterior tibia, and the thick, strong ITL, which constitutes the posterior labrum of the ankle. Between the anterior and PITFLs resides the stout interosseous ligament (IOL). |
the tibial plafond. The posterior malleolus is important as it serves
as the point of origin of the posterior inferior tibiofibular ligaments
of the syndesmosis (Fig. 57-12). The degree of
articular involvement associated with a posterior malleolus fracture
helps to determine the stability of the ankle joint as it prevents
posterior translation.199 This fact,
however, was challenged by two cadaveric studies that demonstrated no
talar instability with posterior malleolus fractures involving up to
40% of the articular surface if there was no lateral-sided injury to
the fibula or posterior ankle ligaments.83,182
The posterior malleolus has also been noted to contribute significantly
to the weight-bearing surface with a loss of 35% of contact pressure
seen with a fracture involving half the joint surface.80,182
malleolus. The lateral malleolus extends distally farther than the
medial malleolus, a property that is used to assess length and forms
the basis of the talocrural angle described previously. The lateral
malleolus is secured to the talus as well as tibia via a multiple
ligamentous structures as described earlier. The main ligamentous
complex of the ankle is the syndesmosis, which secures the fibula to
the tibia. The four components of the syndesmosis include the AITFL,
which runs from Chaput tubercle on the tibia to Wagstaffe tubercle on
the fibula; the PITFL, which runs from Volkmann tubercle and attaches
to the posterolateral aspect of the fibula. Distal to the PITFL is the
inferior transverse tibiofibular ligament (ITL). The ITL is thick and
cartilaginous and forms a structure akin to a labrum in the posterior
ankle joint. The fourth component of the interosseous membrane is the
tibiofibular interosseous membrane, which thickens and becomes the
tibiofibular interosseous ligament (see Fig. 57-12).
largely covered by articular cartilage and has no musculotendinous
attachments. It has a limited blood supply, which will be discussed in
a later chapter. The medial and lateral facets, which articulate with
the medial malleolus and lateral malleolus respectively, are contiguous
with the articular surface of the dome. In general, the talar dome is
rarely injured during ankle fractures as its bone is considered more
dense than that of the tibial plafond bone. It is more typically
injured during an axial loading mechanism. The dome of the talus is
trapezoidal, being broader anteriorly and narrower posteriorly, and
this greatly affects ankle stability. In dorsiflexion, there is
significant stability from the bony conformity of the joint. In
plantarflexion, it is the ligamentous structures that help stabilize
the joint. The medial deltoid ligament fibers that attach to the talus
have been discussed. On the lateral side, it is the three lateral
collateral ligaments (LCLs) that help stabilize the
lateral
malleolus to the talus. The weakest of the LCLs is the ATFL, which is
essentially a thickening within the ankle capsule running from the
anterior-inferior portion of the lateral malleolus to the capsular
attachment on the talus. This ligament is highly susceptible in ankle
sprain injuries and is almost universally affected in this situation.
The calcaneofibular ligament (CFL) is stronger than the ATFL and
originates at the lower segment of the anterior border of the lateral
malleolus inserting on the calcaneus deep to the peroneal tendons. The
CFL resists ankle inversion in a dorsiflexed ankle. The posterior
talofibular ligament (PTFL) is the strongest of the three LCLs and
originates on the medial surface of the lateral malleolus extending
horizontally to the posterior surface of the talus. The PTFL functions
to prevent a posterior rotatory subluxation of the talus.
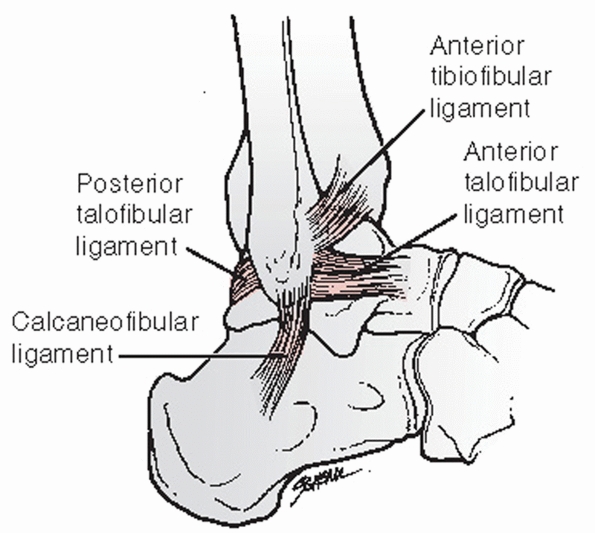 |
|
FIGURE 57-13 LCLs of the ankle and the anterior syndesmotic ligament.
|
 |
|
FIGURE 57-14 A. Structures crossing the medial ankle. B. Structures crossing the anterior ankle. C.
Structures crossing the lateral ankle. Small sensory branches are easily injured during surgical approaches to the ankle. Dissection at the subcutaneous level must be done with care to reduce the incidence of these injuries. |
posterior, medial, anterior, and lateral. The posterior and medial
tendon groups function to plantarflex and invert the ankle and are
innervated by the tibial nerve (Fig. 57-14).
The anterior and lateral tendons are primarily powered by the peroneal
nerve and work to dorsiflex and evert the ankle. The posterior group is
comprised of the Achilles and plantaris tendons. The medial tendon
group is composed of the tibialis posterior, flexor digitorum longus,
and flexor hallucis longus (FHL), and they are transmitted past the
ankle under the lacinate ligament, which forms the roof of the tarsal
tunnel.
lateral compartment and are transmitted past the ankle under the
superior peroneal retinaculum posterior to the fibula. At the level of
the lateral malleolus, the peroneus brevis is directly in contact with
the fibula and is therefore anterior and medial relative to the longus
tendon. Rupture of the superior peroneal retinaculum during ankle
injuries can cause a subluxation of the tendons that might not be
evident until stability has been re-established at the ankle joint. The
anterior tendons are transmitted under
the
extensor retinaculum proximal to the ankle and under the Y-shaped
inferior extensor retinaculum just distal to the ankle joint.
the ankle. Superficial to the anterior border of the medial malleolus
and the lacinate ligament lies the saphenous vein and nerve. These
structures are often injured with approaches to fixation of the medial
malleolus, and one should take care to avoid them, especially at the
proximal extent of the incision. The second neurovascular structure at
the medial side of the ankle is the posterior tibial artery and tibial
nerve, which passes under the laciniate ligament within the tarsal
tunnel and is consistently found between the flexor digitorum longus
and the flexor hallucis longus. The lateral side of the ankle transmits
the superficial peroneal nerve anteriorly at a point approximately 10
cm from the tip of the lateral malleolus 50% of the time and
approximately 5 cm from the tip 20% of the time; therefore, great care
must be taken to protect this superficial structure during approaches
to the lateral malleoleus.89 Also on
the lateral side, roughly located halfway between the lateral border of
the Achilles tendon and posterior border of the lateral malleolus lies
the sural nerve, which assumes a more anterior position within the 5 mm
of the posterior aspect of the lateral malleolus, at the tip.89
The anterior ankle contains the deep peroneal nerve and anterior tibial
arteries, which are transmitted under the superior and inferior
extensor retinaculum between the extensor hallucis longus and extensor
digitorum longus. A safe interval for an anterior approach to the ankle
is between tibialis anterior and the extensor hallucis longus with
medial retraction of the neurovascular bundle.
straightforward with several specific considerations to keep in mind.
The posterior location of the fibula relative to the tibia is easier to
approach when a small bump is placed underneath the operative side
buttock to internally rotate the lower extremity slightly. Also, a
sterile bump is useful to keep the ankle elevated and open up more
degrees of freedom for angling of the drill and screws. The level of
the fracture site is palpated or localized under fluoroscopy; this
determines the center of the incision and the approach. The superficial
peroneal nerve pierces the lateral peroneal fascia and traverses the
lateral compartment into the anterior compartment approximately 10 cm
proximal to the tip of the lateral malleolus, although it can be found
within 5 cm in 20% of ankles.89 A
relative safe zone is directly over the center of the fibula extending
to a distance of 5 cm from the tip of the lateral malleolus, above
which a more careful dissection is advised. Skin flaps should be kept
thick to prevent any undue trauma and decrease the risk of skin
breakdown. Distally, the incision can be angled slightly anteriorly to
allow visualization of the anterolateral joint and the AITFL. This
structure can be repaired through this approach, although it is rarely
indicated once fibular and syndesmotic fixation has been achieved.
Dissection should be kept to a minimum at the bone, and the periosteum
should be elevated only at the level of the fracture. Placement of
clamps may be facilitated by creating strategic perforations in the
anterior fascia over the anterior border of the fibula to allow entry
of the clamp medially without unnecessarily performing a wide
dissection of that area.
Here, the incision over the fibula is centered vertically over the
posterior border of the lateral malleolus. This approach takes the
surgeon away from the danger of damaging the superficial nerve;
however, the sural nerve becomes a more proximate structure that is at
risk of being damaged. This dissection also does not allow ready access
to the anterolateral joint if fixation of Chaput tubercle is desired, a
fact that must be recognized before selecting posterior plating. The
approach is taken down the posterior border of the fibula and outside
the peroneal tendon fascial envelope. Occasionally, through this
approach, a portion of the superior peroneal retinaculum is divided and
may be reapproximated at the end of the procedure. The plate is affixed
directly posteriorly and the screws are aimed anteriorly, providing for
bicortical purchase throughout the length of the plate without danger
of intra-articular penetration. A large sterile bump as well as
significant internal rotation of the lower extremity facilitates aiming
of the screws posterior to anterior.
For large laterallybased fragments where the posterior malleolus does
not extend to the medial malleolus, a direct posterior approach is
helpful. The patient is ideally placed in the prone position, and a
longitudinal incision is undertaken on the lateral side of the Achilles
tendon. Here, the sural nerve is at risk for injury as it passes
through the middle of the operative field. The sural nerve is located
subcutaneously in the areolar fat tissue and can be easily cut. Careful
dissection will mobilize the nerve laterally as the interval between
the peroneal tendons and the Achilles (superficially) and FHL tendon
(deep) is approached. The approach extends down to the posterior
malleolus on its lateral side and the posterior aspect of the
syndesmosis. Care must be taken to visualize and cauterize a branch of
the peroneal artery that lies on the posterior aspect of the
syndesmosis. Through this interval, both the fibula as well as
posterior malleolus can be instrumented and reduced. On the fibula, a
posterior plate is placed while the medial malleolus can be repaired
with either a plate or posterior to anterior directed lag screws. The
medial malleolus can be easily approached via a separate incision in
the prone position.
medial malleolar fractures and can also be used to approach
mediallybased posterior malleolus fragments. Two types of medial-sided
incisions are commonly used. A curvilinear incision (“hockey stick
incision”) can be made based over the anteromedial aspect of the medial
malleolus centered over the joint “axilla” and curving either
anteriorly or posteriorly around the tip of the medial malleolus. The
structures at risk with this approach are the saphenous vein and nerve
at the proximal incision and the posterior tibial tendon at the distal
extent of the incision. This incision is ideal for visualization of the
medial joint axilla and therefore allows fixation of medial impaction
fractures, medial comminution, and evaluation of osteochondral injuries
of the talus should they be present. The main limitation of this
incision
is
that it is not extensile distally. An alternative and commonly used
incision is a straight vertical incision over the midsubstance of the
medial malleolus. This incision, although extensile, is limited in its
ability to allow visualization of the medial joint axilla.
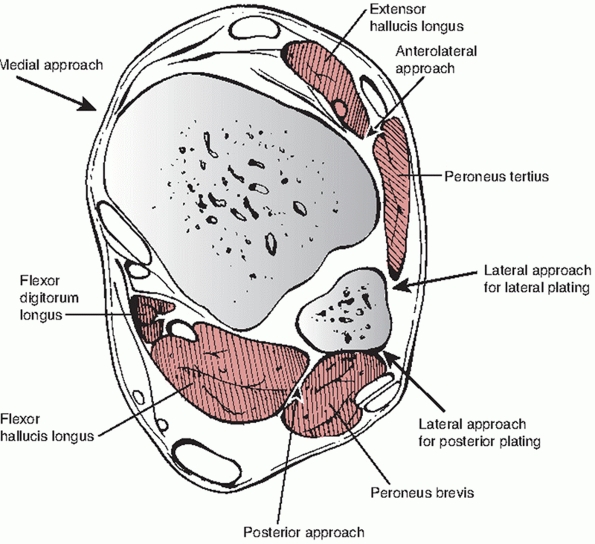 |
|
FIGURE 57-15 Cross section of ankle showing the intervals for the common surgical approaches.
|
ankle fractures, an anterior approach may sometimes be desirable
specifically in situations where a full posterior exposure of the
posterior malleolus is not advised (because of soft tissue
constraints). In this scenario, the posterior malleolus can be clamped
and lagged from anterior to posterior. The interval used here is
between the anterior tibialis tendon and the extensor hallucis longus
tendon (Fig. 57-15).
modification of the lateral approach for the purposes of minimally
invasive extraperiosteal plating of the lateral malleolus, which has
been specifically described for pronation abduction injuries but can be
applied to other fibula fractures.201,230 In this approach, the plate is used as a bridge-plate construct, avoiding direct reduction of the fracture fragments.
treatment of ankle fractures lie in an understanding of ankle
biomechanics and the evolution of this understanding. During the 1930s
and through the 1960s, the vast majority of ankle fractures were
treated nonoperatively. If surgery was indicated, the recognized
standard fixation technique for bimalleolar ankle fractures was an open
reduction of the medial malleolus and closed reduction of the lateral
malleolus. The teaching was that an anatomic reduction of the medial
malleolus was sufficient to reduce the talus and re-establish a stable
and congruent mortise and that the integrity of the medial malleolus
was considered to be the chief determinant of ankle stability. Several
outcome studies, however, indicated unsatisfactory long-term results
for surgically treated displaced ankle fractures. The poor long-term
outcome of ankle fractures prompted further critical analysis of the
approach to treatment of these fractures.46,90,190
stabilizer of the ankle joint was first challenged by Yablon et al.,
who conducted a combined anatomic and clinical study of unstable ankle
fractures.250 In the anatomic arm of
the study, cadaver ankles underwent stress testing after an isolated
deltoid ligament division, isolated medial malleolus fracture, isolated
division of the fibular collateral ligaments, and a short oblique
distal fibula osteotomy with all ligaments intact. Stress testing of
these sectioned specimens revealed that both an incompetent deltoid
ligament and a medial malleolar fracture contributed little to ankle
instability. Both of the lateral lesions of the ankle, however (lateral
malleolus fracture or ligament disruption), caused marked ankle
instability. In the clinical arm of the study, 42 patients with
bimalleolar ankle fractures and 11 patients with a lateral malleolus
fracture and tear of the deltoid ligament (indicated by talar shift)
were treated operatively. The 11 patients with a fibula fracture and
deltoid ligament tear were treated with isolated fibular plating and
all fractures were anatomically
reduced.
Of the 42 patients with bimalleolar fractures, the first 17 were fixed
with medial malleolar fixation only. Intraoperative radiographs
revealed inadequate talar reduction in 14 of these cases, at which
point all hardware was removed and the fibula alone was plated. All
patients achieved reduction of the talus after lateral malleolar
fixation. The authors concluded that the lateral malleolus is the
keystone for ankle stability after ankle fracture.
corroborated the poor results associated with isolated medial malleolar
fixation in bimalleolar ankle fractures. Twenty-nine patients with
either SER4 or PER3/PER4 fractures were treated with isolated medial
malleolar fixation and closed reduction of the lateral malleolus.
Sixteen of the 29 patients in this series had unsatisfactory results
with development of ankle arthritis within the 4.8-year average
follow-up period. They attributed the poor results to malunions of the
fibula and lack of talar reduction by medial malleolar fixation alone.
A total of 118 unstable ankle fractures were enrolled and all underwent
initial closed reduction. If closed reduction was judged inadequate,
open reduction was undertaken. Forty-six ankles underwent operative
fixation of the medial malleolus or suture repair of the deltoid
ligament without fibular fixation in any of the fractures. During a
follow-up period of 1 to 7.5 years, the authors looked at radiographic
criteria of reduction as well as subjective and objective evaluation of
function. In the 46 operatively treated fractures, 22 (46%) were
considered to have poor results, with similar results in the closed
treatment group. An analysis of the factors most predictive of a poor
result showed a correlation with degree of talar displacement, severity
of fracture, and presence of deltoid ligament ruptures. This study
concluded that isolated medial malleolar fixation and treatment of the
MMOLC was inadequate in restoring a normal tibiotalar relationship,
having results similar to nonoperative treatment.
would expand on our knowledge of ankle fractures. In this study, the
authors established radiographic criteria for evaluating the adequacy
of lateral malleolar reduction and syndesmotic disruption and then used
these criteria to assess ankle fractures treated by medial malleolar
fixation versus bimalleolar fixation. One hundred and forty-six
displaced ankle fractures were analyzed after they were treated closed,
treated with open bimalleolar fixation, or treated with medial
malleolar fixation alone. Analysis revealed that the overall result was
most affected by the degree of medial and lateral malleolar
displacement, integrity of the syndesmosis, and the patient’s age. They
concluded that the relative orders of importance for structures that
require restoration are the lateral malleolus, medial malleolus,
deltoid ligament, and finally the syndesmosis. Their analysis also
revealed that bimalleolar open reduction and internal fixation (ORIF)
of both SER4 and PER3/ PER4 fractures fared significantly better than
closed treatment and significantly better than reduction of the medial
malleolus alone. As a matter of fact, the data showed a trend toward a
worse outcome for isolated medial malleolar fixation compared with
closed treatment. Their conclusions were that anatomic reduction of
bimalleolar fractures correlated with superior outcome and that the
prognosis worsened as the number of deranged structures increased
following treatment.
reported a prospective study of 49 SER4 and PER4 ankle fractures with
an acceptable closed reduction who were randomized to operative
treatment or continuation of nonoperative treatment. A second arm of
the study assessed the treatment of 22 SER4 and PER4 ankle fractures
with unacceptable closed reductions randomized to bimalleolar or medial
malleolar fixation. Their conclusions stated that bimalleolar ORIF
provided far superior results than closed treatment of ankle fractures
and that patients with a medial malleolar fracture (as opposed to just
a deltoid ligament rupture) fared significantly worse when treated
closed. In the second arm of the study, bimalleolar fixation appeared
to have superior results to medial malleolar fixation alone; however,
this did not reach statistical significance.
most responsible for ankle stability comes from two case reports that
describe a traumatic extrusion and loss of the medial malleolar
fragment secondary to an open fracture. In both cases, an effort was
made to repair the deltoid ligament. Lindenbaum et al.118
reports follow-up of 3 years showing no evidence of arthritis, range of
motion 5 degrees less than the contralateral side, and stability under
a lateral stress radiograph. In a second case report by Hernigou et al.,85
20-year follow-up of a patient with similar absence of the medial
malleolus showed roughly equal range of motion in both ankles. This
patient’s radiographs, however, showed arthritic changes within the
joint. The hypothesis of the authors was that although ankle varus and
valgus stability is conferred by the lateral malleolus, the rotational
stability and articular congruency provided by the medial malleolus are
important for maintaining the ankle articulation and preventing
arthritis.
unstable ankle fractures changed during the 1970s and shifted attention
to an anatomic reduction of the fibula. As previously mentioned, much
of this shift was stimulated by the study of Yablon et al.250
and subsequent clinical studies. Several authors, however, have shown
that dorsiflexion and plantarflexion of the ankle is a complex motion
that involves some movements out of the plane of motion of the ankle
and therefore static models of ankle kinematics such as Yablon’s were
flawed. It has subsequently been suggested and shown that during axial
loading, the talus may seek its own position beneath the tibia, tending
to reduce the lateral subluxation force.132,173,235
It had also been shown that rotational stability of the talus within
the ankle is because of tension in the deltoid and lateral ligaments.
Excision of the lateral malleolus articular surface did not reduce
rotational stability, but division of the deltoid ligament caused a
twofold increase in rotational instability.151
developed an axially loaded cadaver ankle model testing tibiotalar
stability in bimalleolar ankle fractures. Their findings showed that
even with a 6-mm lateral displacement of the lateral malleolus, there
was no significant change on the contact area of the ankle as long as
it was axially loaded. However, once the deltoid ligament was
sectioned, all ankles showed a significant decrease in tibiotalar
contact area. This result was consistent with the observation that the
pattern of instability was not a straight lateral translation but
rather anterolateral rotation underneath the tibial plafond. In a
follow-up study, Michelson et al.138
used a similar unconstrained axially loaded cadaver model to assess
instability in SER fracture models. This study confirmed that in an
axially loaded ankle,
isolated
lateral fibula fracture without medial malleolus, or deltoid ligament
disruption, there was no appreciable loss of tibiotalar contact and
that the deltoid ligament, specifically the deep portion, served as a
main checkrein to anterolateral rotation of the ankle.
applied their unconstrained axially loaded cadaver ankle model to show
that in the face of an intact MMOLC even a syndesmotic injury is not
destabilizing. In this iteration of the cadaver experiment, when the
MMOLC was disrupted along with a high fibular fracture and a disrupted
syndesmosis, the talus dislocated from the mortise. When the MMOLC was
intact, the talus remained reduced. Solari et al.205
also demonstrated the importance of the medial malleolus in the
stability of Weber C fractures in a cadaver study evaluating the need
for syndesmotic screws. In this study, the rotational component of
instability was assessed specifically. A Weber C fracture pattern where
the medial malleolus alone was treated attained 56% of total rotational
talar stability, isolated lateral malleolus fixation attained 36%
stability, and fixation of the lateral malleolus and medial malleolus
(without syndesmotic fixation) attained 76% of total stability. Their
conclusion was that the MMOLC is the single most important contributor
to ankle stability in Weber C fracture patterns.
MMOLC is important for ankle fracture stability when considering the
ankle joint in a dynamic state. Clearly, all fracture patterns are
located on a continuum of severity and their treatment must be
individualized. It appears that although a near anatomic reduction of
lateral side of the ankle is important, it is only relevant when the
MMOLC is disrupted. Therefore, ankle injuries that do not present with
a medial-sided injury are likely stable and can be treated
nonoperatively. Displaced fibula fractures without any medial-sided
injury has been considered a possible indication for surgery, as it was
believed that the distal fibula is externally rotated. External
rotation of the distal fibula has been stated as a reason for ankle
symptoms and poor function after SER2 ankle fractures.251
Michelson et al. refuted this notion with a CT study that found the
proximal fibula internally rotates relative to the distal malleolus
fragment and the relationship of the lateral malleolus at the ankle is
maintained.140 This study provides evidence that ankle biomechanics are not altered in an SER2 type of injuries.
when an osseous injury is not present. Koval et al. studied 21 Weber B
type ankle fractures that had a positive stress test. All ankles
underwent MRI to evaluate for a deep deltoid rupture. The study
reported no statistically significant correlation between MRI findings
at the deltoid ligament and a positive stress test as 19 of the 21
patients had only a partial tear of the deltoid ligament. Only the
patients with a full rupture of the ligament on MRI underwent surgery,
and all patients in this group had excellent outcomes.103
Another study by Egol et al. found that the clinical signs of medial
tenderness and swelling were not sensitive for predicting medial
widening on stress views. Moreover, this study found that patients
without any medial signs of injury and a positive stress test who were
treated without surgery had good or excellent clinical results.53
Deangilis et al. lent further support to these data as they found no
statistically significant relationship between the presence of medial
tenderness and deep deltoid ligament incompetence. Medial tenderness
was determined to have a 57% sensitivity and 59% specificity for
predicting a deep deltoid injury.50
fractures may continue to evolve. At this point, however, the main
criteria for surgery are a widened mortise and obvious signs of
instability on radiograph such as dislocation, subluxation, syndesmosis
widening, or joint impaction. Other patient-specific indications must
obviously be taken into consideration such as age, functional level,
comorbidities, and soft tissue considerations.
have shown that isolated lateral injuries (SER2) are treated well
nonoperatively with excellent functional results.13,106,195,255
Long-term follow-ups of patients with SER2 fractures that were treated
nonoperatively have shown a near-complete recovery up to 20 and 30
years after the initial injury. Other studies where SER2 fractures were
treated operatively have shown equivalent results to nonoperative
treatment.252
closed injuries was detailed earlier. The practice of obtaining a
stress view has historical precedence for ruling out instability. Both
a manual stress view and a gravity stress examination have been
described as legitimate methods to stress the ankle mortise130,172,200; however, recent data have brought the utility of the stress view into question.53,68,103,157
Despite this, the practice of obtaining a stress view has become a
standard of care that should still be used but now should be
interpreted with greater caution.
in a supportive brace with weight bearing allowed as tolerated.
Favorable results have been described with treatment using high-top
shoes, elastic support brace, air cast stirrup brace, or a walking boot.29,195,255
Physical therapy can be instituted throughout the recovery period
encouraging range-of-motion exercises. The therapy can be advanced to
full weight-bearing strengthening and proprioception training for
several weeks with almost uniform excellent results. The complication
rate from nonoperative treatment in stable ankle fractures is
negligible despite reports of rare fibular nonunions.58,143,184
ankle fracture is identified, a closed reduction is indicated as the
first line of treatment. Clearly, ankle fracture-dislocations are a
sign of great instability and require more immediate attention and a
prompt closed reduction. Once a satisfactory closed reduction is
achieved, the patient should be given the option of proceeding with
operative or nonoperative treatment. The typical regimen of
nonoperative treatment is a long-leg cast, to neutralize rotational
forces at the ankle, for a period of 6 weeks and then advanced to
either a short-leg cast or walking boot.
anesthetic to facilitate relaxation of the limb and allow manipulation
as well as immobilization while maintaining optimal patient comfort.
Some advocate the use of anesthesia or a conscious sedation protocol to
achieve the reduction,194 although performing an intra-articular block or hematoma block may require less nursing and ancillary support.6,66,243
An intra-articular block is performed by placing the patient in a
supine position. The affected ankle is prepared with Betadine solution.
A 20-gauge needle is inserted into the medial aspect of the ankle
joint, medial to
the
tibialis anterior tendon. Once the joint is penetrated and hematoma is
aspirated, confirming appropriate placement of the needle, the joint
can be injected with 12 mL of 1% lidocaine without epinephrine. White
et al.243
compared an intra-articular hematoma block to conscious sedation in a
randomized prospective manner and reported a similar degree of
analgesia (Fig. 57-16).
appropriately relaxed, a reduction maneuver is performed. The classic
closed reduction maneuver was originally described by Quigley in 1959
and has since come to be known as “Quigley’s maneuver.”181
lies in external rotation. If the limb in this position is suspended by
the great toe, then the ankle and foot being of much less weight and
mass of the leg and thigh, fall into adduction, internal rotation and
supination.”
emergency department, allowing the physician to perform both the
reduction and casting with minimal assistance as the leg is hung from
an intravenous line pole while the reduction is performed and a
long-leg cast is applied. The mortise should be anatomically reduced;
otherwise, the reduction should be repeated (Fig. 57-17).
 |
|
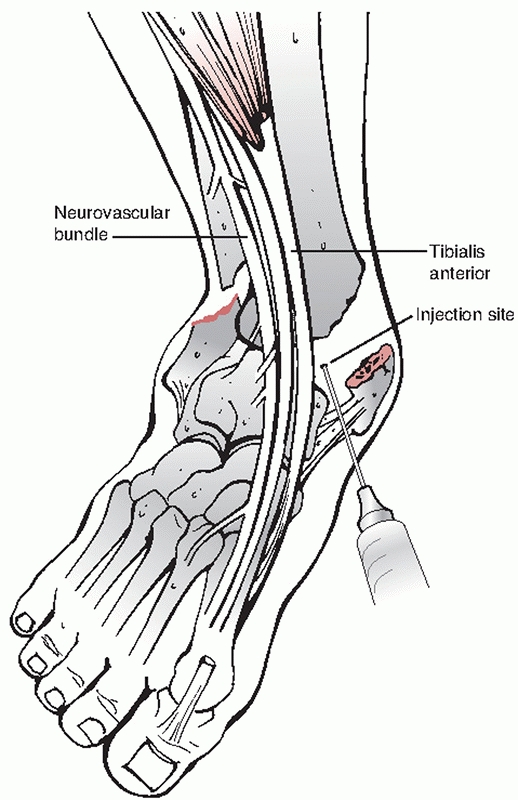
FIGURE 57-16
Intra-articular block for ankle fracture. An intra-articular block is performed by placing the patient in a supine position. The affected ankle is prepared with Betadine solution. A 20-gauge needle is inserted into the medial aspect of the ankle joint, medial to the tibialis anterior tendon. Once the joint is penetrated and hematoma is aspirated, confirming appropriate placement of the needle, the joint can be injected with 12 mL of 1% lidocaine without epinephrine. |
 |
|
FIGURE 57-17 The Quigley maneuver.
|
well known. Maintaining the reduction in a cast can be exceedingly
difficult despite an initial congruent reduction, with one study
showing 34% rate of anatomic reduction with up to 26% rate of loss of
reduction.57 Obstacles to
maintaining a reduction in a cast are body habitus, poor patient
tolerance of a long-leg cast, elderly and polytraumatized patients,
decreased swelling, and subsequent cast loosening. Closed treatment
requires close follow-up with nearly weekly radiologic examinations for
a period of 3 weeks. Quigley, in his original article, acknowledged
that certain fracture patterns such as those where the medial malleolar
fracture line is at the level of the plafond or above will have no
medial buttress and the talus will subluxe medially.181 The ideal treatment for unstable ankle fractures is arguably surgical.
to allow for optimal results. It is important to ensure that the cast
or splint is well contoured without any wrinkling of the cotton padding
that could exacerbate any soft tissue compromise that already exists.
The ankle must be kept in neutral and great care should be taken to
avoid an equinus posture. Certain fracture patterns are highly unstable
in neutral and can only be closed reduced in plantarflexion; this
should serve as an indication for operative fixation.
treatment of ankle fractures should be the degree of instability that
is present. As previously discussed, our understanding of what
constitutes ankle instability continues to evolve; however, obvious
instability should receive surgical treatment. Other indications for
operative treatment are failure to hold a reduction in a cast,
syndesmosis diastases, articular surface incongruity as
marginal
plafond impaction injuries, comminution at the medial axilla of the
joint, and large displaced medial malleolar fractures. Special
considerations are surgical timing, open fractures, elderly patients,
and diabetic patients.
consideration with regard to surgical timing of ankle surgery is
related to the status of the soft tissues. The ankle is essentially a
subcutaneous structure with no muscle bellies to provide an additional
layer of protection in cases of soft tissue compromise. High-energy
ankle fracture-dislocations in particular are at high risk of
developing skin complications, blistering, and breakdown. Elderly
patients, smokers, and diabetics have a further compromised circulatory
status, which can exacerbate the insult sustained by the soft tissue
envelope of the ankle. It is therefore important to evaluate each case
individually with regard to timing.
ankle is imperative to stabilize the soft tissues. Clinical experience
has shown that a reduced mortise will decrease articular damage as well
as facilitate decreased swelling of the ankle. Another modality to
decrease swelling around the ankle in the acute phase is with the use
of a intermittent pneumatic compression or continuous cryotherapy. Both
of these modalities were shown to significantly decrease swelling about
the ankle and were largely well tolerated by the patients.211,222
consideration of timing. Fracture blisters occur because of strain at
the dermal-epidermal junction secondary to fracture displacement at the
time of injury. A complete separation of the dermal-epidermal junction
(full thickness) presents as blood-filled blisters, whereas partial
separation (partial thickness) presents as serous-filled blisters.72,73
The presence of blisters directly over the area of planed incisions has
historically been a cause of surgical delay. A standardized protocol of
blister unroofing and application of Silvadene cream has been shown to
decrease soft tissue complications and promote re-epithelialization
allowing surgery to proceed after a delay of approximately 1 week.
Caution should be taken in diabetic patients who present with blisters
as the zone of injury is greater than the blister area making this
cohort of patients more likely to develop serious wound complications.213
surgery until swelling has decreased and the soft tissue envelope has
started to recover, there are clear disadvantages to surgical delay, as
shown in multiple studies. Carragee et al. recommended early operative
intervention for high-energy ankle fractures as a higher soft tissue
complication rate was seen even for a delay of greater than 24 hours.36 Fogel et al. showed a higher rate of malreduction when surgical delay exceeded 1 week for ankle fractures.64
Breederveld et al. and Koonrath et al. also evaluated the effect of
surgical delay and found no difference in outcome, although a prolonged
length of stay for the delayed group was cited.28,102
that each fracture be evaluated on a case-by-case basis. Significantly
traumatized, yet closed, soft tissue envelope should delay surgical
fixation until swelling has decreased and any blisters in the surgical
incision site are re-epithelialized. Diabetic patients should be even
more carefully scrutinized because of a higher rate of complications.
cites ankle fractures as among the most common orthopaedic injuries,
occurring in the elderly with an increasing rate of up to 8 per 1000
Medicare enrollees in certain regions of the country. An
epidemiological survey of ankle fractures in patients 60 years old or
older in Finland has identified a 317% increase in the incidence of
ankle fractures in the elderly between 1970 and 1995. Regression
analysis derived from these data have predicted a three-fold increase
in ankle fractures in the elderly by 2030.96
Furthermore, within the United States, a striking geographic
heterogeneity has been demonstrated with regard to surgical indications
in this population. Clearly, a consistent treatment algorithm does not
exist for ankle fractures in the elderly as it does for hip fractures.
Some of the indications cited by previous authors for surgical fixation
of ankle fractures in the elderly include the need for early
mobilization, prevention of posttraumatic arthritis, maintaining range
of motion at the ankle, and avoiding the soft tissue complications
associated with cast treatment. There are authors who have mentioned
that prevention of arthritis is not as important a surgical indication
in the elderly as it is in younger patients, and they state that the
main goals of surgery in the elderly should focus on providing a
functionally stable ankle joint.13
elderly with ankle fractures stems from reports in the past that have
shown poor to moderate results from such endeavors.16,121,196
An often-cited study by Beauchamp et al. reported on 126 patients older
than 50 years, of whom 55 were treated conservatively and 71 were
treated operatively. A 2-year follow-up completed for 86 of these
patients revealed little difference in function between the operative
and nonoperative group. This study also concluded that although
operative fixation provided a more anatomic result, the complication
rate was higher, especially in women. The reason cited for the
increased complication rate in women was marked osteoporosis.16
Salai et al. reported on their series of unstable ankle fractures in
patients 65 years old or older who were randomized to operative (49
patients) and nonoperative treatment (16 patients). Final analysis, at
a mean follow-up of 37.5 months, showed significantly higher American
Orthopaedic Foot and Ankle Society (AOFAS) scores as well as better
pain, function, and alignment scores in the nonoperative group.
Although there was no analysis of fracture severity in each group, the
authors concluded that close consideration should be made for
nonoperative treatment in the elderly with an unstable ankle fracture.196
elderly are also reported. Srinivasan et al. retrospectively reviewed
the treatment of 38 consecutive patients 70 years old or older who
underwent operative treatment after their unstable fractures were not
adequately reduced by closed means. The authors found that 84% of these
patients returned to preoperative function at an unspecified follow-up
time.206 Pagliaro et al. reviewed
their series of 23 patients, all of whom were 65 years old or older,
with unstable ankle fractures who were treated operatively. They
reported a 100% union rate and three minor wound complications as well
as one wound dehiscence and delayed union. No functional outcome scores
were obtained; however, the authors concluded that healing and
complication rates are similar to the general population norm.166
Makwana et al., in a prospective randomized trial, evaluated operative
versus nonoperative treatment of ankle fractures in 36 patients 55
years old or older. Their findings indicated that although more
complications were associated with the open treatment group, overall
function as assessed by the Olerud-Molander scale was improved in the operative group.125,162
More specifically, this study found that at the mean 27-month
follow-up, patients in the operative group had better function, less
swelling, and increased range of motion. Davidovitch et al. compared
the functional outcome after surgical fixation of ankle fractures in
patients older than 60 and younger than 60 years. The authors found
that although the older cohort recovered their preoperative functional
level at a slower rate than the younger cohort, the total AOFAS scores
were equal throughout the 1-year follow-up period. Based on these
findings, the authors concluded that surgical treatment of unstable
ankle fractures in patients older than 60 years provides a reasonable
functional result.48 Koval et al.
reported low complication rates in properly selected operatively and
nonoperatively treated elderly patients in an analysis of the Medicare
database.106
The use of locked plating in osteoporotic bone has been extensively
reported; however, several studies have focused on ankle fractures in
particular.146 Locked plating has
been found to be advantageous in ankle fractures, providing increased
fixation in the distal fracture fragment over conventional plating.101
Placing the fibular plate in the posterolateral antiglide position can
be advantageous in osteoporotic patients as it allows by cortical
purchase of the distal screws without risk of joint penetration.
Minihane et al. compared a laterally placed locked plate with a
conventional plate place in the posterolateral antiglide position and
reported increased biomechanical strength with the posterolateral plate.144
Koval et al. has also reported increased strength of fixation in
lateral plates augmented with intramedullary Kirschner wires (K-wires).104
include intramedullary rush rod fixation in select fractures, which
have been shown to provide satisfactory results.180
Other strategies may include the injection of calcium phosphate and
methylmethacrylate cement to increase screw purchase, although these
techniques have been largely replaced by the use of locked plates.92,109,114
with ankle fractures are a difficult subgroup of patients to treat. The
rate of complications in these patients has been reported to be high
with both operative and nonoperative treatment.22,43,64
The indications for surgery are similar to those for patients without
diabetes, and unstable ankle fractures should certainly be stabilized
surgically. The major issues with diabetics are impaired wound and
fracture healing and the development of a Charcot neuropathy. Costigan
et al. and Jones et al. identified neuropathy and hypertension as the
most important predictors of postoperative complications in diabetic
patients with ankle fractures.43,94
The risk of infection can be up to 60% of operatively treated ankle
fractures, although Jones et al. reported no increased complication
risk (including infections) in diabetics without other comorbidities.94,107,244
Blotter et al. retrospectively reviewed their experience with diabetic
ankle fractures and noted a significantly higher complication rate in
insulin-dependent compared with non-insulindependent diabetics. The
authors did note, however, that glycosylated hemoglobin levels are
likely more important than the presence or absence of insulin
dependency. The presence of vascular disease, neuropathy, and Charcot
neuropathy, however, has been widely accepted as the most important
predictors of complications in this patient population.248
in the decision for surgical timing as in all ankle fractures, but it
is even more important in the diabetic patient. The role of the
external fixator as a bridge to internal fixation in place of a splint
is likely more prominent as it allows a more rigid stabilization of the
fracture and soft tissues and it allows a closer surveillance of the
status of the soft tissues. Fracture fixation in diabetics also tends
to be more extensive, sometimes requiring syndesmotic fixation for
adjunctive stabilization. Other techniques used in osteoporotic bone
(discussed earlier) are recommended for many of these patients. A
prolonged period of immobilization and non-weight bearing is also
advisable with a rule of thumb of keeping the patient non-weight
bearing for twice as long as the nondiabetic patient (Fig. 57-18).
appropriately treated is generally good. Multiple studies have
established that the adequacy of reduction on radiographs correlates
well with overall outcome.62,95,149,177
As discussed, stable ankle fractures that are treated in a closed
fashion have good to excellent results at various follow-up times with
the only subjective long-term symptom being swelling.15,106
The outcomes of operatively treated unstable ankle fractures have also
been favorable as shown by multiple authors with up to 85% to 90%
excellent results.17,119
Although variability among postoperative weightbearing protocols exists
in the literature, outcomes seem to be favorable when an unstable
injury is identified and treated appropriately.54,74,112,202 Surgery for unstable ankle fractures has even been shown to be a cost-effective endeavor.18
fractures using validated outcome scores have been limited in the past.
In one study of 141 patients followed for 2 years after
operative
stabilization of an ankle fracture, 77% obtained a good or excellent
result, as measured with the Olerud-Molander score.110 Obremsky et al. have shown continued improvement in the SF-36 even 20 months after surgery.159
Day et al. showed only 52% good or excellent outcome after bimalleolar
ankle fracture fixation with a follow-up of 10 to 14 years using the
Phillips scoring system.49 With regard to driving, patients have been shown to return to baseline breaking function at 9 weeks status post ankle surgery.55
A more recent study from our institution was conducted to identify
demographic and patient factors that are associated with functional
recovery. In this prospectively followed cohort of patients, the AOFAS
and SMFA scores were used for evaluation. The patient factors most
predictive of functional recovery were found to be patient age, gender
(males with better outcomes), the presence of diabetes mellitus, and
the ASA classification. The same study found that at the 1-year
follow-up, patients had largely returned to their preoperative baseline
function and were experiencing little to no pain.56
Bhandari et al. found that modifiable social factors such as smoking
and alcohol consumption are important determinants of outcomes in
patients with operatively treated ankle fractures.19
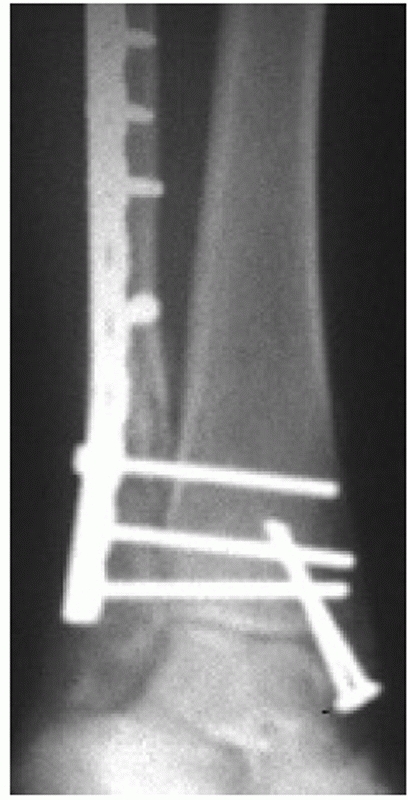 |
|
FIGURE 57-18 Enhanced fixation in diabetic. Note multiple syndesmotic screws gaining fixation in the tibia.
|
of the lateral malleolus. The approach used, as discussed previously,
is at the discretion of the surgeon and can lead to either lateral
fibular plating or posterior plating of the fibula. Other options
include intramedullary fixation as well as isolated lag screw fixation.
In general, however, an anatomic reduction at the level of the mortise
and syndesmosis is mandatory no matter what fixation method is used.
fibula are in fractures where the fibula fracture is at the proximal or
midshaft region. In those circumstances, it is the reduction of the
syndesmosis that can be relied on to reduce both the length of the
fibula and the syndesmosis. The exact level of the fibular shaft where
an anatomic fixation is no longer required has not been determined,
although some authors have stated that this technique is best suited to
fibula fractures in the proximal third.224,229
The approach to the fibular shaft should be undertaken with caution as
the peroneal muscle bellies as well as the peroneal nerve become more
prominent and require extensive mobilization and soft tissue disruption.
a decision that should ideally be made during preoperative templating.
The fracture is approached laterally in either case and must first be
cleaned at the fracture edges from overhanging periosteum and clot.
Reproducing the fracture mechanism (i.e., supination and external
rotation) redisplaces the fracture and allows a more complete
irrigation of clot and removal of interposed bone fragments and tissue
that may obstruct the reduction. A lion jaw-type clamp or pointed
reduction clamp can then be used to gently restore both the length and
rotation of the fracture and obtain compression at the fracture site.
On occasion, when the fracture presents to surgery in a delayed
fashion, length is difficult to restore with use of clamp alone and an
AO distractor is very helpful. An assistant should facilitate the
manual reduction via providing an indirect reduction force by pulling
traction and providing rotation at the foot.
fluoroscopically, the fibula can then be internally fixed. The typical
fixation method in noncomminuted fractures is placement of a lag screw
perpendicular to the fracture line, obtaining primary compression at
the fracture site. The rotational forces around the fracture line are
then neutralized by placement of a one-third tubular plate. The plate
can either be precontoured to the bone or contoured in situ with
progressive placement of screws, as it is a malleable implant. When the
plate is applied laterally, the distal most screws must be kept
unicortical to avoid penetration into the lateral gutter of the ankle
joint. These distal screws may be cancellous screws or unicortical
locked screws in a locking plate.
posteriorly. The advantages of the posterior plate are its antiglide
function and the ability to achieve bicortical screw purchase distally
without violating the ankle joint.164,246
In fractures that are not comminuted, the antiglide position of the
plate may allow for sufficient stabilization and the omission of distal
screw fixation in addition to the lag screw. The main disadvantage of
this approach is mobilization of the peroneal tendons and potential
irritation of the tendons, although one study reported less symptomatic
hardware after posterior compared with lateral plating. When comparing
the posterior plate to a laterally placed locked plate, Minihane et al.
found the posterior plate to provide improved biomechanical stability.144
comminuted fibula fractures in osteoporotic bone can be fixed via an
extraperiosteal technique which provides for a bridge-plate construct.
This technique has been previously described in the literature and
utilizes an indirect reduction technique.(201,230)
Although an open approach is performed, the periosteum at the fracture
site is not disturbed. The authors prefer a fully percutaneous approach
where a distal incision is made over the fibula and a one third tubular
locking plate is advanced extraperiosteally. A pointed reduction clamp
is used to obtain length and rotation of the distal fibula fragment. A
single screw is placed in the distal plate. The plate is then aligned
with the proximal shaft radiographically. A 3-cm incision made
proximally followed by blunt dissection down to the plate allows
placement of a single screw proximally fixing the length and rotation
of the fibula. Additional screws can be placed away from the fracture (Fig. 57-19).
also been successfully fixed with lag screws alone, foregoing the
neutralization plate.78,100,227
The advantages sited for the lag screw-only approach is decreased
dissection with the advent of primary compression of fracture fragments
and a decreased need for hardware removal. This approach is not ideal
in an osteoporotic patient, as screw fixation needs to be solid. Also,
additional immobilization is likely required.134
described in the past with the main indications being noncomminuted
fractures. Ideal fracture configurations are transverse. A long oblique
fracture line is likely inadequately treated with an intramedullary
device. The difficulty with intramedullary fixation is restoration of
length and rotation.11,180,185 The limitations associated with this fixation limit its applications.
are the PA type where the distal fragment is small and is often
associated with comminution proximally. Several fixation methods
are
available. A K-wire and tension band construct may be useful when there
is not a significant amount of comminution. In situations where there
is comminution, a combination of a lateral one third tubular plate
fashioned into a hook plate distally is first fixed to the proximal
shaft buttressing the distal fragment into alignment, while an
intramedullary screw is used for additional stabilization. In these
types of fractures, reducing and fixing the medial malleolus initially
may provide sufficient stability to allow for an easier fibular
reduction.
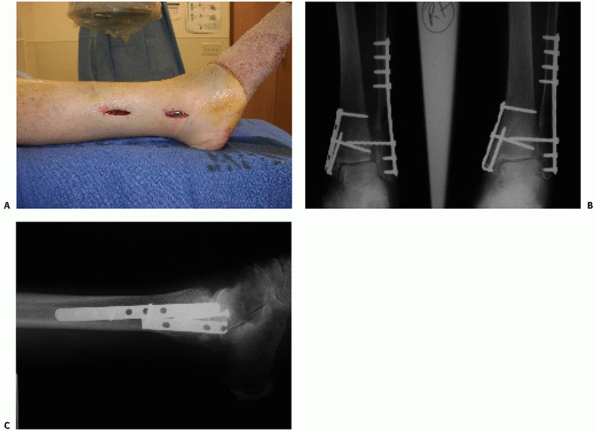 |
|
FIGURE 57-19 Extraperosteal plating. A. Surgical incisions. B, C. Patient 6 weeks status post surgery showing maintained alignment and callous formation.
|
ensure a delicate soft tissue dissection and be mindful to avoid
unnecessary periosteal stripping, which may contribute to nonunion. The
length and rotation of the fibula must be returned to an anatomic
relationship with the talus.
Although the posterior malleolus fracture may occur as part of any
rotational mechanism, the size of the fragment is variable. Large
fragments may often be associated with a posterior fracture-dislocation
of the ankle and can be difficult to hold in a reduced position unless
placed in extreme plantarflexion182 (Fig. 57-20).
The posterior malleolus is important in stabilizing against posterior
subluxation of the ankle; however, the primary restraint to a posterior
forces is the ATFL and the fibula. In general, however, most posterior
malleolar fractures tend to smaller, laterally based fragments, still
bearing the ligament of the PTFL.80
In these smaller fragments, obtaining length on the fibula is generally
sufficient in achieving a reduction of the posterior malleolus. The
surgeon should be mindful that a malreduced posterior malleolus may
indicate failure in restoring fibular length. The posterior malleolus
has also been recently shown to contribute to the stability of the
syndesmosis.67
large enough to warrant internal fixation is made with radiographic
studies. Plain films have been shown to be unreliable in determining
the size of the fragment as the tendency exists to overestimate the
size of the fragment using this modality.60
An external rotation lateral view may be useful in better quantifying
the size of the fragment; however, the study of choice when a large
fragment is suspected is a CT scan.52
The CT scan can provide information regarding the configuration of the
fracture fragment and assist in deciding on the optimal approach.
sparse, but evidence does exist that trimalleolar fractures carry a
worse prognosis than bimalleolar fractures.13 Several studies have shown that larger posterior malleolar fragments have led to worse results than smaller fragments.133,149 However, evidence does exist that even small posterior malleolar fragments may increase the risk of arthrosis.93
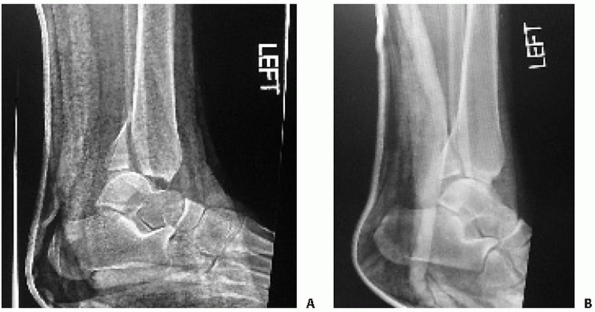 |
|
FIGURE 57-20 A. Failure to hold ankle reduction with large posterior malleolus on dorsiflexion. B. Splinting the ankle in plantarflexion reduced the posterior malleolus and stabilized the ankle.
|
In one technique, the fracture line is directly visualized and
instrumented, while in the other, an indirect reduction is performed.
The posterior malleolus can be approached from posteriorly as described
in the approach section of this chapter. The joint line is not directly
visualized, but the cortical fracture line, which is generally not
comminuted, can be directly visualized and reduced. Often, an antiglide
plate construct can be used and a fluoroscopic image is taken to ensure
that the articular surface is reduced (Fig. 57-21).
This approach requires extensive dissection. In the indirect approach,
a large pointed reduction clamp can be placed either percutaneously or
through the lateral or medial malleolar incisions. To obtain an
adequate reduction via this method, the fibula must first be fixed and
brought out to length, as this will also provisionally align the
posterior malleolus. Once the posterior malleolus has been brought down
by the fibula, it is compressed from anterior to posterior with a
clamp. Lag screws can then be placed through small stab incisions from
anterior to posterior to compress the posterior malleolus into position.
whether or how the posterior malleolus will be reduced. No matter what
approach is used, however, it is clear that the fibula must be reduced
out to length to ensure an adequate posterior malleolar reduction and
ankle stability.
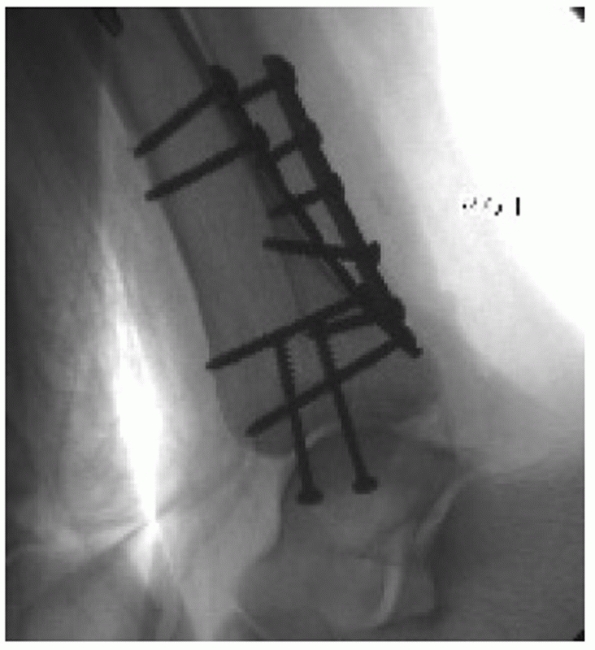 |
|
FIGURE 57-21 Antiglide plate used to reduce posterior malleolus fracture.
|
that articulation is a well-known feature of rotational ankle
fractures. Historically, it has been thought that the level of the
fibula fracture is related to the likelihood of syndesmosis injury, and
this serves as the basis of the Weber classification as previously
described in this chapter. However, it is known that a syndesmosis
injury can in fact occur in the absence of a fibula fracture or in the
presence of a fibula fracture at the level of the joint.50,68,83,204
The ability to predict that a syndesmosis disruption is present based
on current classification schemes is poor, and the surgeon must
carefully scrutinize the injury to ascertain a syndesmotic disruption.
Preoperative radiographs may sometimes demonstrate the injury, but an
occult injury should be assessed intraoperatively after bimalleolar
fixation has been achieved using either a manual stress test or a
“cotton test” (Fig. 57-22).
tied to the integrity of the MMOLC. Biomechanical studies have shown
that when the MMOLC is intact, disruption of the syndesmosis does not
lead to widening of the mortise.22,32
This implies that in cases when the medial malleolus is fixed,
syndesmotic fixation is not indicated. Solari et al. have shown that in
a Weber C fracture model with syndesmotic disruption, fixation of the
lateral and medial malleoli restored 73% of ankle stability. The
addition of syndesmotic fixation increased stability to 100%.205
Tornetta points out that in anterior collicular fractures of the medial
malleolus, internal fixation of the medial fracture fragment may not be
sufficient to stabilize the ankle since a deep deltoid transsection may
coexist, and a stress view is therefore recommended intraoperatively
for all such fractures.226
a large pointed clamp and is evaluated radiographically
intraoperatively. To achieve a reduction of the syndesmosis, the fibula
must be brought back out to length and its rotation must be corrected
to normal. It is desirable to avoid overcompression of the syndesmosis,
which theoretically can occur by application
of
the screw with the ankle in plantarflexion. As noted previously, the
talus is narrower posteriorly than anteriorly, and the plantarflexed
posture allows for increased compression across the syndesmosis. This
has been thought to cause overtightening of the mortise and loss of
motion at the joint.132,161
A cadaveric study by Tornetta et al., however, has shown that even in
plantarflexion, overcompression is not possible provided the
syndesmosis is accurately reduced.228
Unfortunately, our ability to judge an accurate syndesmotic reduction
intraoperatively is not as reliable as we once thought with a large
proportion of syndesmotic reductions shown to be inaccurate.69,242
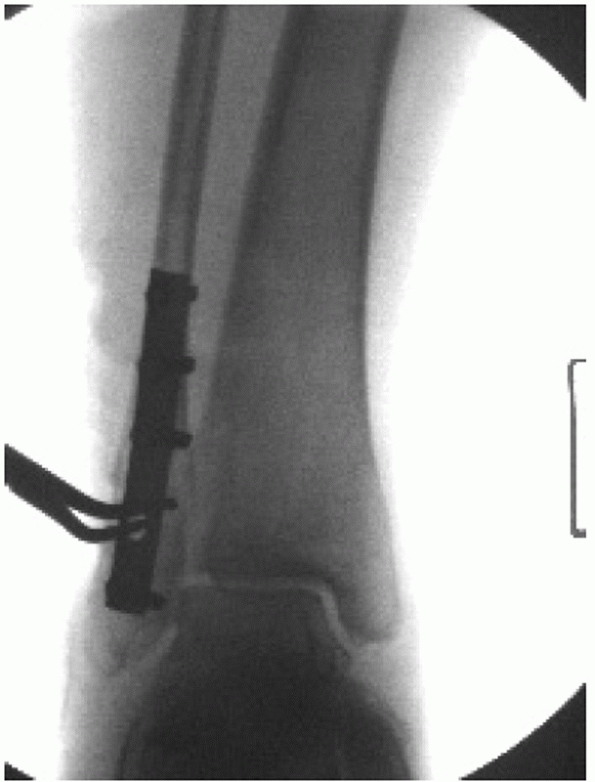 |
|
FIGURE 57-22 Cotton test. The clamp pulls laterally on the reduced fibula to test the integrity of the syndesmotic complex.
|
several options exist. The syndesmosis can be fixed using one or two
screws; the screws can be placed either tricortically or
tetracortically. The screws used can be either 3.5- or 4.5-mm screws.
Other options are bioabsorbable screws and a suture repair over a
button.65,223
Most surgeons use 3.5-mm cortical screws; however, 4.5-mm screws are
also used and are easier to localize and remove under local anesthesia
in the outpatient setting. The larger screw also is less likely to
break once the patient begins weight bearing on the leg. Tetracortical
fixation is stiffer and more secure, and therefore those screws are
more likely to break than to loosen compared with the 3.5-mm screws.98,150
One study has shown comparable stability between 3.5-mm screws and
obliquely oriented K-wires, but the latter is rarely used in clinical
practice.175
stability in the setting of a bimalleolar ankle fracture and especially
when associated with a syndesmotic injury. The indications for fixation
of an isolated medial malleolus fracture are less clear and include
joint incongruity in widely displaced fractures and prevention of a
painful nonunion. Herscovici et al. reported on a series of isolated
medial malleolus fractures treated nonoperatively in a cast with
excellent results.87 A variety of
fracture patterns exist at the medial malleolus, and therefore a large
variation of internal fixation techniques exists.
anteromedially placed incision that curves posteriorly. The structures
to avoid are the saphenous vein and nerve in the anterior aspect of the
incision and the posterior tibial tendon in the distal and inferior
aspect of the incision. This approach allows visualization of the
anteromedial articular surface of the ankle also known as the “axilla”
of the joint. Comminuted and loose osteochondral fragments can be
removed from the joint from this approach, and assessment of articular
damage is possible. Rarely, with severe ankle fracture-dislocations,
the posterior tibial tendon may subluxate into the fracture site.
comminution, fixation may be carried out with two 4.0-mm partially
threaded cancellous screws, a combination of a screw and K-wire, or a
tension band construct. A recent report even advocated the use of a
miniature intramedullary nail with multiple locking holes for medial
and lateral malleolar fixations; however, the relevance of this implant
is not yet established. Care must be taken when placing the medial
malleolar screws to avoid the posterior tibial tendon and not leave the
implants proud.59
various medial malleolar fracture fixation constructs on six cadaver
specimens. Each specimen was stressed in pronation first with K-wires
alone, then with the addition of the tension band, and finally the
tension band and K-wires were removed, and two 4.0-mm cancellous lag
screws were placed. Their results showed that tension band fixation
provided the greatest resistance to pronation forces. The tension band
was at least four times stiffer than the two screws, which were
significantly stiffer than the two K-wires alone. The authors followed
up their mechanical study with a clinical study, whereby 32 consecutive
patients with a medial malleolar fracture were treated with tension
band fixation and followed up to 1 year. There were no cases of
nonunion, one case of asymptomatic malunion, and two cases of
symptomatic hardware requiring removal165 (Fig. 57-23).
associated with SA fracture patterns may benefit from an antiglide type
of construct along with intrafragmentary screws. Because of the
direction of the fracture line, placement of screws from the tip of the
medial malleolus proximally would cause displacement at the fracture
site. In addition to an antiglide plate, screws oriented horizontally
along the joint line can provide adequate compression at the fracture
site at a line perpendicular to the fracture.225
collicular fractures or comminuted fractures of the medial malleolus
where a portion of the medial malleolus is fixed with a plate and
another portion is held with a K-wire (Fig. 57-24).
malleolus must be examined closely to avoid intra-articular
penetration. The mortise view that is often taken to assess implant
position within the medial malleolus gives an inaccurate assessment of
intra-articular penetration. The reason for this is the lack of
parallelism between the medial and lateral talomalleolar spaces caused
by the asymmetric shape of the talar dome (wider
anteriorly
than posteriorly). In a cadaveric study of 10 ankles, the authors
placed medial malleolar wires in parallel and performed 15- and
30-degree mortise views followed by an anatomic dissection. The study
showed that there was a false appearance of an intra-articular
posterior wire on four of the 15-degree mortise specimens and eight of
the 30-degree mortise views. It was the conclusion of this study that
the 15-degree internal rotation mortise view was best for assessing
lateral malleolar fixation and that the AP view is most accurate for
assessing the medial malleolar implants.75
 |
|
FIGURE 57-23 Medial malleolus tension band using fiber wire suture. A. Clinical photograph. B. Radiograph of medial malleolus tension band construct.
|
series: AP, lateral, and mortise views. Full-length tibial-fibular
radiographs should be obtained to assess for a proximal fibula fracture
in cases where there is a medial malleolus fracture alone or
medial-sided tenderness without evidence of distal fibular fracture.
Patients with isolated lateral malleolar fractures with clinical signs
of medial injury should undergo manual external rotation stress
radiography to determine instability.53,130,200
location and size of the medial malleolar fragment. Stability is
directly related to the size of the medial fragment. Anterior
collicular fragments will have only the superficial deltoid attached.170
In approximately 25% of SER4 injuries, there will be an associated deep
deltoid rupture. Thus, fixation of this fragment will not enhance
stability. The lateral radiograph is the key. If the fragment is
greater than 2.8 cm in width, the deep deltoid will be attached and
stability is restored. If the fragment is less than 1.7 cm in width,
then stability is not restored with fixation. For those fractures in
between, an intraoperative external rotation stress examination should
be performed following malleolar fixation.226
ankle fractures, CT may provide information not readily available on
plain radiographs.24,38,69,71,80,234
CT has completely replaced the use of standard radiographic tomography
because of its availability, quality, and ease of use. The use of
thin-section CT scanning allows for accurate two- and three-dimensional
reconstructions of the ankle mortise. CT scanning may be helpful in
assessing posterior malleolar fragment size in rotational ankle
fractures (Fig. 57-25). Information like this
may play a role in selection of surgical approach or implant choice and
is therefore of significant value when diagnoses are in question. CT
scanning may also allow for accurate assessment of articular impaction
that may be seen with SA fracture patterns. Postoperative CT scanning
may help identify cases in which a malreduction of the ankle mortise is
suspected (Fig. 57-26). Portable CT scanners
are currently in use and may be helpful intraoperatively to allow
assessment of syndesmotic reduction before the end of any surgical
intervention.
isolated lateral malleolus fracture with signs of medial injury and an
equivocal stress examination. To date, most studies using MRI have been
diagnostic.152,154,187 Most studies have used MRI to evaluate syndesmotic injury after ankle fracture.152,154
In a series of 73 ankle fractures that underwent MRI evaluation,
Nielson et al. reported that the level of fibula fracture did not
correlate with the integrity or extent of interosseous membrane tear.157
Similar to previous studies, use of MRI as part of our clinical
protocol often found associated injuries to the ankle not suspected
from the physical or radiographic examination; however, the clinical
implications of the common findings of associated bone bruise or
chondral injury remain unclear since most, if not all, of the patients
in our study were doing well at latest follow-up. MRI was used in one
study as a decision-making tool. Koval et al.
found
MRI was able to identify partially intact deltoid ligaments in patients
who had a mildly widened medial clear space on stress radiograph.103 These findings allowed for nonoperative treatment of the injuries in these patients.
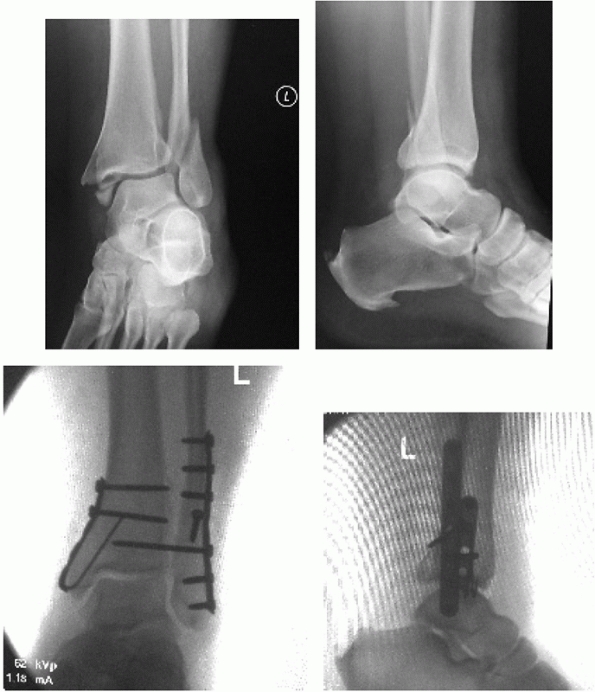 |
|
FIGURE 57-24 Anterior colliculus fracture shear fracture of posterior colliculus requiring hybrid fixation.
|
no role in displaced fractures about the ankle. They may be helpful in
identifying stress reactions or fractures about the ankle in cases of
longstanding pain, especially about the medial malleolus.115,129,155 This modality, however, has largely been replaced by MRI.128,158
despite the level of complexity. This exercise forces the surgeon to
understand the “personality” of the fracture and mentally prepare an
operative strategy. This concept applies to any attempted operative
treatment of a fracture. The surgeon should understand the exact nature
of the fracture before attempting any type of intervention. Radiographs
of the contralateral extremity may benefit by serving as templates. It
is often helpful to draw out the involved anatomy and plan a
reconstruction by overlying implant templates on tracing paper. Each
step of the operative tact is written out and includes positioning,
approach with all anatomic considerations, reduction techniques and
instruments used, implant type, size, and length, as well as steps for
intraoperative assessment of reduction. Furthermore, one must make sure
that all needed equipment is available. The instruments and implants
required for these surgeries include a tourniquet, a femoral
distractor, osteotomes, bone tamps, suture anchors,
bone
graft substitutes, small- and/or large-fragment standard or
periarticular plates and screws, or external fixation of choice.
 |
|
FIGURE 57-25 CT axial slice through the level of the syndesmosis and posterior malleolus defining the fracture.
|
operative fixation of any ankle fracture. Image intensifier machine
size is dependent on the preference of the operating surgeon. Small or
mini C-arm machines have the advantage operator independence and
minimal radiation exposure at the expense of image quality with respect
to fine detail. Larger image intensifiers often require a licensed
radiologic technician to be present and are associated with greater
radiation exposure. In either case, a radiolucent operating table
should be used. We prefer the use of a table that does not have a base
at the end to allow for surgeon positioning at the end of the affected
limb.
If a bimalleolar fracture is present, the bump should not be so large
as to limit access to the medial aspect of the ankle. In circumstances
where difficulty is encountered approaching the medial malleolus after
fibular fracture fixation has been accomplished, the bump can be
removed, which will allow external rotation of the limb and improved
access. A pneumatic tourniquet can be applied to the affected thigh if
desired for use during the surgical procedure. The affected limb is
prepped and draped free. In cases in which direct access to the
posterior malleolar fragment is required, a posterior approach may be
chosen. In this case, the patient may be placed in the prone position
to allow access to the posterior tibia via the posterolateral approach (Fig. 57-28).
When this approach is selected, care must be taken to ensure that all
bony prominences are well padded and that appropriate size chest rolls
allow for adequate expansion of the chest wall during respiration. A
lateral position is an alternate to the prone position in cases where
the posterolateral approach is required. Presence of a medial malleolar
fracture precludes this positioning for cases in which medial access is
needed.
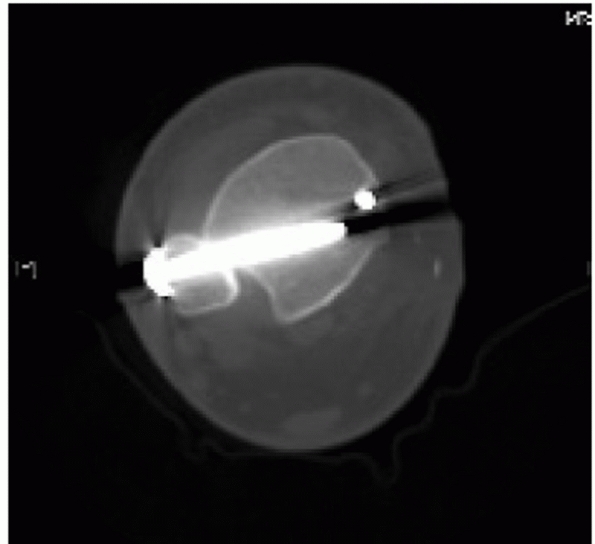 |
|
FIGURE 57-26 CT axial slice showing malreduced syndesmosis.
|
 |
|
FIGURE 57-27
Patient in a supine position with a bump under the ipsilateral buttock, neutralizing external rotation of the leg and allowing ready access to the surgical site. |
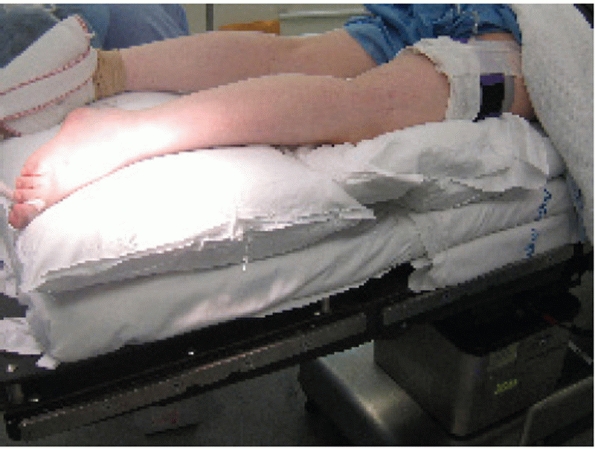 |
|
FIGURE 57-28 Patient in a prone position for a posterolateral approach to the posterior malleolus and fibula.
|
factors, including the fracture pattern (Lague-Hansen), the size of
fragments, and the condition of the soft tissues. The fibula is
approached via a direct lateral skin incision. The incision is kept
just off the posterior border of the fibula but may be adjusted
slightly based on soft tissue considerations. Deeper tissues are
incised in line with the skin incision. Care must be taken proximally
in the wound to avoid injury to the superficial peroneal nerve, which
crosses the field approximately 7 cm proximal to the distal tip of the
fibula. Next, the peroneal fascia is divided and the peroneal tendons
and musculature are retracted posteriorly. With gentle elevation of the
periostium about the fracture site, the fibula should be exposed. Care
should be taken to avoid excessive stripping of fracture fragments as
well as iatrogenic disruption of the syndesmotic ligaments as they
insert anteriorly on the fibula.
anteromedial incision. A concave anterior incision is parallel to the
saphenous vein. A concave posterior incision allows better
visualization of the anteromedial joint. Whichever skin incision is
chosen must take into account the need for joint visualization as well
as implant placement from distal (malleolar fragment) to proximal
(intact tibia). After the skin, the subcutaneous tissues should be
carefully dissected to prevent injury to the saphenous vein and nerve.
With the dissection carried down sharply to the bone, periosteum is
elevated for 1 mm proximally and distally. The fracture should be
booked open to allow for visual inspection of the talar dome for
chondral injury. The medial gutter should be irrigated for any loose
hematoma or debris that may impede reduction.
through the posterolateral approach to the fibula. Here, the skin
incision is moved posteriorly to lie between the fibula and lateral
edge of the Achilles tendon. The sural nerve may cross the wound in its
distal extent and must be protected. The lateral compartment fascia is
divided in line with the skin incision. The interval between the
Achilles tendon and the peroneal tendons is developed. The FHL is taken
off the fibula down to the interosseous membrane and then the rest of
the deep posterior compartment is taken off the posterior tibia bluntly
with an elevator. This will give direct visualization of the posterior
malleolar fracture spike.
fracture, the first step involves cleaning of the fracture site. This
step is critical to ensure an accurate fracture fragment reduction.
Periosteum is elevated approximately 1 to 2 mm from the fracture ends.
Hematoma is removed from the fracture site by light curettage and
gentle irrigation. This is followed by fracture reduction. Usually,
reduction is afforded by a small lion jaw clamp or pointed reduction
forceps. If reduction is difficult, manual traction with pronation and
external rotation will afford fracture alignment in SER patterns. Care
should be taken to avoid placement of clamps over fracture spikes to
prevent inadvertent comminution. If the clamps make it difficult to
place a lag screw or plate, a provisional K-wire may be inserted across
the fracture and the clamps removed. At this point, if a lateral plate
is chosen, the lag screw is placed in the anterior-to-posterior
direction, perpendicular to the fracture. In this case, the near cortex
is overdrilled with a 3.5-mm drill bit, followed by drilling of the far
cortex with a 2.5-mm drill bit. The length of the screw is then
measured with a depth gauge and the screw track is then tapped with a
3.5-mm tap, followed by screw placement with a 3.5-mm screw of
appropriate length. The tapping step may be skipped if a self-tapping
3.5-mm screw is chosen as the implant of choice. Next, a small-fragment
(usually one third tubular) plate is placed directly lateral on the
fibula to act as a neutralization device. The proximal screw holes are
filled with bicortical 3.5-mm screws after drilling with the 2.5-mm
drill bit. Distally unicortical cancellous screws are placed with care
not to penetrate the distal tibial-fibular joint.
surgical approach is similar to the lateral plating technique. When
application of a posterior or antiglide plate is chosen, placement of a
lag screw is optional.231,247
The authors’ preferred method is to apply the plate along the flat
posterior surface of the bone, using it as a reduction aid with a bone
reduction clamp. We prefer to place a posterior-to-anterior-directed
lag screw through the plate. It should be noted that because of the
biomechanical properties of this plate construct, this lag screw is
optional.81,246
Next, at least two or three bicortical screws are placed in the plate.
A bicortical screw placed posterior to anterior in the distal screw is
optional. If a posterior plate is applied, the proximal screws are
placed bicortically from posterior to anterior, both proximal and
distal to the fracture. This may be an advantage in osteoporotic bone (Fig. 57-29).
fracture patterns are amenable to intramedullary fixation of the
fibula. This can be achieved with several different implants. The
benefit of this technique is the relative sparing of the soft tissue
envelope associated with percutaneous placement. Under fluoroscopic
control, the tip of the lateral malleolus is identified on both the AP
and lateral views. We prefer the use of an intramedullary screw. A
small incision is made and either a guidewire or drill bit is used to
enter the distal fibular metaphysis. Once entry is confirmed, either
the wire is advanced up the canal across the fracture site or a
partially threaded screw of appropriate length is inserted retrograde
to gain purchase on the proximal intramedullary cortex (Fig. 57-30).
Alternatively, intramedullary nails specifically designed for the
fibula are available and may be inserted retrograde as well.
Large-diameter K-wires, Rush rods, and elastic titanium nails may be
used instead.
the medial malleolus should be booked open to allow visualization of
the medial aspect of the talar dome. Fracture hematoma and any loose
fragmentation of bone and cartilage should be copiously irrigated from
the joint. The periosteum should be elevated 1 to 2 mm from the
fracture edges to aid in anatomic reduction of the joint fragments. The
medial malleolar fragment (usually one large piece) can be reduced
with
the aid of a dental tool or small pointed reduction clamp. Sometimes,
it is necessary to drill a small pilot hole in the distal medial tibia
to anchor the clamp for reduction. The fragment can be provisionally
stabilized with small-diameter K-wires or guidewires placed in
parallel. Following radiographic documentation of the reduction and
wire placement, cannulated screws of appropriate length may be placed
over the wires after drilling of the out cortices with a cannulated
drill. Alternatively, noncannulated screws may be used independent of
the provisional stabilization. The majority of times, a 4.0-mm
partially threaded cancellous screw may be placed. However, if the
fragment is small, 3.5- or 3.0-mm cannulated screws are now available.
More recent studies have advocated for the use of two bicortical 2.7-mm
screws placed in lag mode. Two screws are recommended for rotational
control, but if the fragment is too small, one screw may suffice
because of the inherent stability of the undulating fracture line.
Countersinking the screw heads medially may help to alleviate painful
prominent hardware. Comminuted fractures that are not amenable to screw
fixation may benefit from a small buttress plate, or a “tension band”
technique with either suture or small-diameter wire may be chosen. This
technique uses the deltoid ligament for fixation distally and a screw
placed into the distal tibial metaphysis placed parallel to the
articular surface. Vertically oriented fractures of the medial
malleolus benefit from the use either a buttress plate or screws
inserted perpendicular to the fracture line.
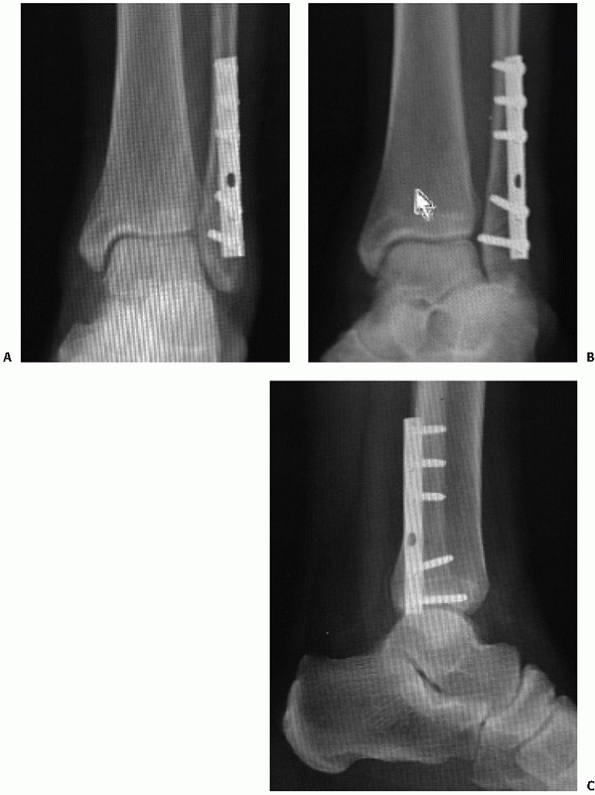 |
|
FIGURE 57-29 Posterior fibular plating. A. Anteroposterior. B. Mortise. C. Lateral.
|
may be stabilized with cannulated lag screws placed in the
anterior-to-posterior direction. If an open approach is used for
reduction, screws placed posterior to anterior may be placed across the
fracture site. If the fracture fragment is of sufficient size, an
antiglide plate (one third tubular) may be placed with undercontouring
of the plate to provide a satisfactory buttress effect (Fig. 57-31).
 |
|
FIGURE 57-30 Intramedullary fixation of the fibula.
|
 |
|
FIGURE 57-31 Posterior plating of the fibula, posterior malleolus, and antiglide fixation of medial malleolus. A. AP. B. Mortise. C. Lateral.
|
and lateral sides of the ankle, syndesmotic integrity should be
assessed. Cotton test involves providing a lateral force on the fibula
with a bone hook or bone clamp (see Fig. 57-23).
Lateral displacement, which allows more than a few millimeters of
tibial-fibular widening, is considered pathologic and an indication for
syndesmotic fixation. The lateral radiograph should be scrutinized to
assess the relationship of the fibula to the articular surface of the
ankle joint. In general, on a true lateral view of the ankle, the tip
of the fibula should be anterior to the posterior border of the
diaphyseal tibia, but comparisons to the contralateral ankle can be
assessed. With a bolster behind the ankle, a large tenaculum clamp is
placed across the tibial-fibular joint with one tine on the distal
tibia and the other on the fibula (Fig. 57-32).
Reduction is confirmed on the AP, mortise, and lateral radiographic
views. While dorsiflexion of the talus has been recommended in the past
to prevent overtightening of the syndesmosis, more recent studies have
shown it virtually impossible to overtighten an anatomically reduced
mortise. Fixation choices range from one or two screws, with three or
four cortices drilled and 3.5- or 4.5-mm screw diameters used. Although
the size and number of screws remain controversial, some parameters are
agreed on. The screw should be placed 1.5 to 2 cm proximal and parallel
to the joint. We prefer the use of a single 3.5-mm three-cortex screw.
This allows for toggle within the distal tibia when weight bearing is
resumed. The screw should not be placed in lag mode. If a lateral plate
was used, the screw is placed through one of the distal holes. If a
posterior plate was used, the syndesmosis screw will likely be placed
outside the plate on the lateral cortex. In cases in which only
syndesmosis fixation (high fibula fractures) is performed, we prefer
the use of two screws to counteract the forces acting over a greater
span.
 |
|
FIGURE 57-32
Syndesmosis reduction. A large tenaculum clamp is placed across the tibiofibular joint with one tine on the distal tibia and the other on the fibula. |
most common ankle fracture pattern encountered. It is identified by its
typical fibular fracture pattern. This injury is a fracture at the
level of the ankle mortise with its anteroinferior-toposterosuperior
fracture line seen on the lateral radiographic view. The posterior
malleolus may be involved to a varying degree and the medial injury may
be purely ligamentous, purely bony, or a combination of the two. The
syndesmosis may be disrupted in up to 50% of cases as well. SER2
injuries are treated nonoperatively with progressive weight bearing
with some type of functional bracing. Because of an intact medial
malleolar osteoligamentous complex, the ankle mortise is stable. Very
rarely, these injuries may be indicated for surgical repair if
significant displacement of the fracture with lateral clear space
widening is noted. When a SER fracture pattern is treated surgically,
we prefer a lateral approach to the fibula. Simple SER fracture
patterns are well suited for posterior plating of the fibula. In
contrast to historical teaching, medial arthrotomy to clear out the
medial gutter before fibular fixation is not warranted. Following
approach to the fibula, two options for fixation are available. The
first is an anterior-to-posterior-directed lag screw with a subsequent
laterally applied small-fragment neutralization plate. The second
option is the authors’ preferred technique. The small-fragment plate is
applied to the posterior surface of the fibula with at least three
screw holes proximal to the fracture apex. In this position, the plate
will act as an antiglide device.81 A
posterior-to-anterior-directed lag screw may be placed through the
plate at the surgeon’s discretion. Furthermore, the distal most screw
holes may be filled at the surgeon’s discretion. This is appealing in
the case of distal fractures and fractures associated with poor bone
quality as the screws are placed bicortically and extra-articularly.
the posterior malleolar fragments are usually reduced indirectly by
pull of the posteroinferior tibiofibular ligaments. If less than 25% of
the articular surface, fixation of these fragments is not performed. If
greater than 25% and fixation of this fragment is desired, one or two
anterior-to-posterior cannulated lag screws may be placed to prevent
displacement. If reduction is not achieved indirectly, the fragment may
be reduced with either a pointed clamp placed between the fragment and
the anterior cortex or a direct open approach between the peroneal and
FHL muscles. In the latter case, following direct reduction of the
fracture fragments, a posterior small-fragment plate may be applied in
an antiglide position (see Fig. 57-31).
Following stabilization of the lateral and posterior malleoli,
attention is turned medially. If the medial lesion is solely
ligamentous, no repair is necessary.4,10,82,214
Fixation choices depend on the size of the medial fragment. The
fracture pattern is usually a transverse fracture involving one or both
colliculi. It is the authors’ preferred option to use two partially
threaded lag screws placed across the fracture site. If the fragment is
too small to accept two 3.5- or 4.0-mm screws, then consideration is
given for screws of smaller diameter or use of a single screw with a
supplementary K-wire. In cases of fracture comminution, a tension band
technique may be used. In these cases, a heavy nonabsorbable suture or
small-diameter wire is placed through the deltoid ligament and
tensioned in a figure-of-eight manner about a screw head placed
proximal to the fracture line. Unlike tension bands placed about the
extensor mechanisms of the elbow and knee, this tension band has no
dynamic properties.
cotton test should be performed to assess the status of the
syndesmosis. If widening is suspected, syndesmotic fixation should be
performed. As mentioned previously, the authors prefer use of a single,
three-quarters cortex transsyndesmotic screw in cases in which fibular
fixation has been performed with a plate and screw construct (Fig. 57-33).
involve the fibula alone or occurs with the posterior and/or medial
malleolus as well. The rotational fibula fracture differs from the
supination variant in that it generally occurs at a higher level
(suprasyndesmotic) and is associated with syndesmotic disruption and
the fracture pattern on the lateral
radiograph
is anterosuperior to posteroinferior. Because the fibula fracture is
higher in these injuries, posterior plating may be more difficult as
the peroneal muscle bellies get in the way. Our preferred fixation
strategy is still a posterior plate, but we will use a lateral
small-fragment plate if needed. Often, these fractures are shortened
and may require use of fibular lengthening techniques (see Pearls).
Posterior malleolar fixation in these cases may preclude the need to
place independent syndesmotic fixation and should be considered on a
case-by-case basis. Medial fixation follows the tenants described of
SER fracture patterns.
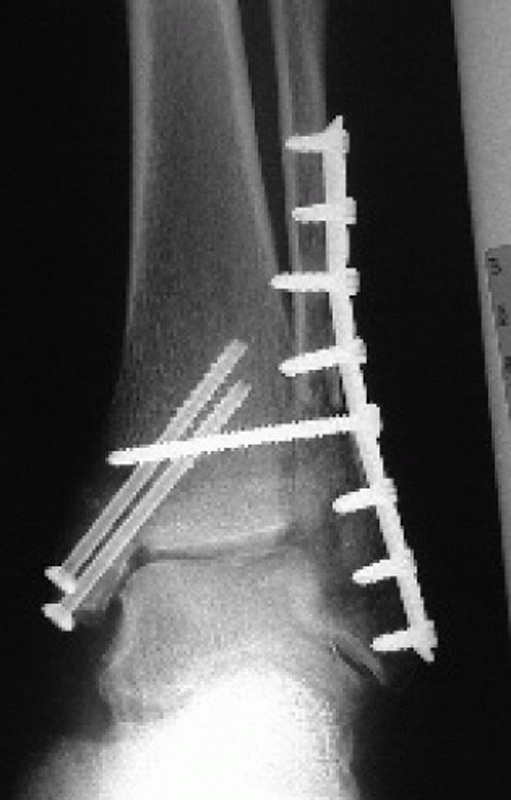 |
|
FIGURE 57-33 Tricortical 3.5-mm syndesmotic screw.
|
special PER situation. These fractures are associated with a transverse
medial malleolar fracture and a spiral proximal fibular fracture. The
syndesmosis and interosseous ligament are disrupted. Following fixation
of the medial injury, the syndesmosis is reduced and fixed. There is no
need to perform an ORIF on the proximal fibula because in these cases,
there is almost no shortening of the fibula. Following closed reduction
of the syndesmosis with a large tenaculum clamp, the reduction is
confirmed on AP, mortise, and lateral radiographs. Fixation is achieved
with two 3.5-mm transsyndesmotic screws placed parallel to the ankle
joint (Fig. 57-34). Our preference is to use a
three-cortex construct, rather than a four-cortex construct. A two-hole
small-fragment plate may be used as a washer in poor bone.
by a low transverse fracture of the fibula and a vertical fracture of
the medial malleolus. There is often articular impaction of the tibial
plafond at the shoulder of the medial joint. The fibula may be open
reduced and plated or fixed in a percutaneous manner with an
intramedullary implant. Our preferred technique is use of a cannulated
3.5- or 4.0-mm screw placed from the tip of the lateral malleolus up
the fibular shaft. The medial malleolus should be open reduced.
Inspection of the joint should be carried out. Any impacted articular
segments should be disimpacted and grafted. Fixation of the vertical
fracture is accomplished with at least two screws placed perpendicular
to the fracture line or with the use of a small-fragment plate and
screws placed in an antiglide position.
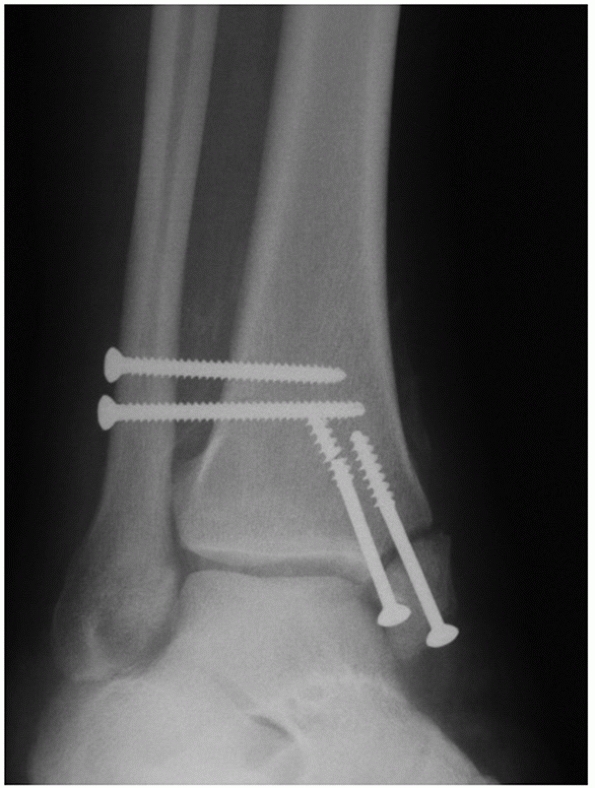 |
|
FIGURE 57-34 Tricortical 3.5-mm syndesmotic screw fixation in a Maisonneuve fracture pattern. Medial malleolus has gone to nonunion.
|
by an oblique medial-sided injury and a transverse or comminuted
fibular fracture secondary to varying degrees of bending. In these
cases, we begin fixation on the medial side of the injury and
accomplish stabilization with two screws as previously detailed. The
lateral fixation is always a laterally placed small-fragment plate to
counteract the deforming forces. Often, these fractures have a
shortened fibula and may require a “push-pull” technique or external
distractor application to regain fibular length. In cases of severe
comminution, consideration to acute bone grafting should be given.
Intraoperatively, manual stress examination should be performed
following fibular fixation to assess integrity of the syndesmosis.
fractures is indicated in patients whose fractures are not displaced or
minimally displaced, have poor soft tissue envelopes, have medical
contraindications for surgery, or refuse surgical intervention.
Indications for isolated medial malleolar fracture fixation are
inconsistent and vary according to author. We prefer to stabilize
displaced medial malleolar fractures with
displacement
of 2 mm or more in the absence of mortise instability. We prefer the
use of two screws placed in lag mode, by either design or technique.
This may be accomplished by using partially threaded screws or fully
threaded bicortical screws placed in lag mode.
splint for 7 to 10 days to allow for wound healing. Elevation is
maintained for the first 24 to 48 hours to minimize soft tissue
swelling. At first postoperative visit, the suture line is discontinued
and the patient is placed in a removable orthrosis. We have used an
ankle stirrup in the past54 but have
moved to a removable fracture boot. The boot allows for the prevention
of equinus during the rehabilitation period and allows the patient to
remove the orthrosis and begin active and active assisted range of
ankle motion exercises. We prefer to keep patients non-weight bearing
for a minimum of 6 weeks until there is radiographic evidence of
fracture healing. Patients who sustain syndesmotic injuries are delayed
up until 8 weeks to begin weight bearing. Diabetic and neuropathic
patients are restricted in weight bearing for 10 to 12 weeks. In all
cases, we believe that earlier motion protocols lead to improved early
functional outcomes.54
whether weight bearing is allowed immediately in a plaster cast or
patients are kept non-weight bearing.2,3,79
Since no benefits to early weight bearing have been shown, we prefer to
keep our patients non-weight bearing until signs of fracture union are
present. Hardware, including syndesmosis screws, is not removed
routinely. Patients are educated on the indications for hardware
removal and offered if symptomatic.
infection, and peroneal tendonitis with painful hardware. Major
complications include nonunion, hardware failure, deep infection, and
compartment syndrome. In a large review of over 30,000 Medicare
patients, Koval et al. found an overall medical and surgical
complication rate of 2% in surgically and non-surgically treated ankle
fractures.105
following surgical stabilization of unstable ankle fractures is
difficult to determine because of various definitions used in the
literature. Incidences between 1.8% and 11% have been reported for
superficial infection.91,119,124,178
Certain systemic conditions will predispose patients to development of
wound complications and include diabetes, venous insufficiency, older
patient age, and history of smoking. Superficial wound complications
following ankle fracture surgery are not uncommon36,112 (Fig. 57-36).
The occurrence of this may be related to patient factors such as poor
vascular flow or excessive surgical trauma in a compromised soft tissue
envelope. Most cases of superficial wound epidermolysis or edge
necrosis may be observed or treated with local wound care methods such
as wet-to-dry dressing changes. Deeper areas of skin slough may require
formal débridement of necrotic tissue and prompt a plastic surgical
consultation. Antibiotic therapy should be started for cultureproved
bacterial colonization. Implant exposure before healing may warrant
further methods to obtain a stable, closed soft tissue envelope.27,41
irrigation and débridements and culture-specific antibiotic
suppression. Close monitoring of laboratory serology will help gauge
medical response. Failure of treatment may require removal of implants
followed by repeated irrigation and débridement and antibiotic
treatment. Revision fixation should follow successful treatment of the
infection. Deeper infections may require significant bony débridement.
If ankle stability is compromised following bony resection, ankle
arthrodesis may be the only salvage operation available.20
compared with patients without diabetes mellitus. The incidence of this
complication in these patients may be 3 to 4 times that of nondiabetics.116 The associated peripheral neuropathy, peripheral vascular disease, and swelling from injury are contributing factors.
unstable fracture patterns that are treated nonoperatively. It may
occur early when associated with poor bone stock. This complication is
best avoided by recognizing situations in which augmentation strategies
may be used. Loss of reduction is more commonly associated with
nonoperative care of unstable fracture patterns.16
As swelling subsides, it is possible for fracture fragments to shift
and move, leading to loss of ankle mortise reduction. When attempting
to treat an unstable unimalleolar, bimalleolar, or trimalleolar ankle
fracture closed, frequent radiographic follow-up is critical to catch
any displacement early before malunion.
There are several case reports associated with this particular
complication. The deep posterior compartment is the most commonly
affected compartment in the leg. The key to prevention is recognition
of the elevation of intracompartmental pressure postinjury or
preoperatively and very close monitoring of the limb following casting
or after surgery. Any neurovascular change should be a trigger for the
treating physician to suspect an elevation in intracompartmental
pressures of the leg.
It is, however, likely that factors such as traumatic chondrocyte death
and unrecognized osteochondral injury contribute to posttraumatic
arthritis as well.163
It will usually take several years for the radiographic changes such as
subchondral sclerosis, joint space narrowing, and osteophyte formation
to develop.119 Stable patterns have
shown little tendency toward arthritic change up to 30 years
postinjury, while radiographic evidence of arthritis may be seen in
over 30% of more unstable patterns.15
|
TABLE 57-4 Pearls and Pitfalls
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
of fracture has been documented with arthroscopic evaluation at the
time of fracture fixation. Traumatic cartilage injuries generally
comprise three categories: microdamage or blunt trauma, chondral
fractures, and osteochondral fractures. Arthroscopy performed at the
time of ankle fracture fixation has identified several regions involved,5
and the number of lesions present following fracture seems to be
related to the severity of injury according to the Lague-Hansen
classification.5,111 Thus, despite
the surgeon’s best efforts at anatomic restoration of the ankle
mortise, the potential for postinjury degenerative changes persists.
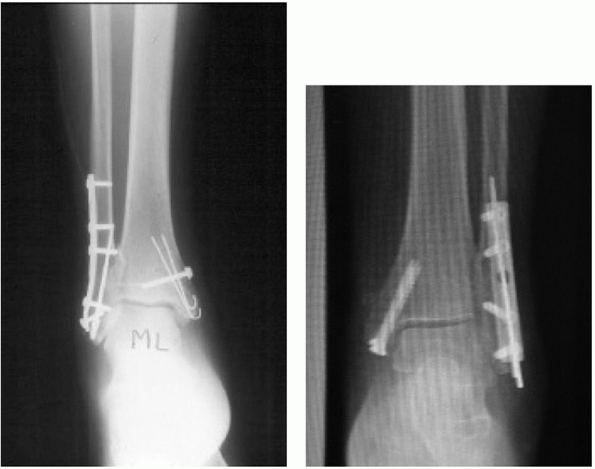 |
|
FIGURE 57-35 Examples of multiple intraosseous K-wires providing enhanced fixation stability in relatively osteopenic bone.
|
reduction or by loss of reduction of the mortise. It may occur with
either nonoperative or operative treatment but is certainly more common
with nonoperative care. If nonoperative treatment is chosen for an
unstable pattern, the treating surgeon must be compulsive about
checking the quality of mortise radiographs frequently during the
treatment period as minor shifts in the tibiotalar articulation may
have significant consequences.183
to failure to recognize an inadequate reduction intraoperatively or
loss of that reduction secondary to failure of bone or fixation method.
Inadequate reduction risk may be related to loss of normal landmarks
secondary to extensive comminution. Certain fracture patterns should
raise the suspicion of the surgeon as to associated injuries, such as
tibial marginal articular impaction in supination adduction injuries.131
Failure to recognize this aspect of the injury with subsequent failure
to reduce will lead to early arthritic change within the tibiotalar
joint.
 |
|
FIGURE 57-36 Postoperative wound breakdown.
|
Shortening of the fibula laterally with varying degrees of malrotation
will lead to characteristic medial widening, talar tilt, and varying
degrees of arthritic change.127,160,240,241,248,251 A fibular lengthening osteotomy with lateral reconstruction has been described as treatment for this problem.127,160,238,240,251
Patients may present late. In one series, patients with a fibular
malunion did not become symptomatic until 5 years after injury, on
average.251 Marti et al. reported on
31 patients who underwent fibular osteotomy and reconstruction. Six
patients had definite signs of arthritic change before surgery.
Following surgery, they found no progression of arthritic change in
these patients. Seventy-seven percent of the patients in this series
reported good to excellent results. Hughes89
reported on 28 patients treated with a similar protocol. In this
series, 71% of patients reported good to very good results
subjectively. Furthermore, time from injury to late reconstruction did
not seem to influence the development of a poor result.
radiographic evaluation, arthroscopy may have a role as part of the
procedure to evaluate the articular cartilage remaining on both the
tibial and talar sides of the joint.156 Ankle arthrodesis remains an option for the patients with a significant ankle fracture malunion and advanced arthrosis.218
Correction of malalignment, in conjunction with ankle arthrodesis, will
lead to better stance and muscle balance and should be performed.
obvious (widened tibial-fibular space) or subtle. Recent studies have
shown plain radiographic evaluation of malreduction of the syndesmosis
to be inaccurate. CT scanning of the distal tibial-fibular joint has
shown this to be of greater incidence.69
Three reasons why the syndesmosis may be malreduced are malreduction of
one or both malleoli, bony or soft tissue interposition, or
malreduction of the fibula within the incisura.86
Persistent malreduction of the syndesmosis will lead to restricted
ankle range of motion and arthrosis if not corrected. The best course
of action is to reconstruct as soon as this problem is identified.
well-known complication. This may be because of several factors,
including blood flow to the fragment, interposed soft tissue, or
effects of synovial fluid on the fracture hematoma.135
Presence of a nonunited medial malleolus does not necessarily mean a
symptomatic patient. A painless nonunion of the medial malleolus may be
followed and treated conservatively. Nonunion of the medial malleolus
following surgical repair can occur as well (see Fig. 57-34).
This may be related to a residual fracture gap left, excessive
stripping, or an infection. A nonunion of the fibula, likewise, that
results in a pain-free, reduced mortise may also be treated
nonoperatively. The presence of a nonunion may rarely occur in the
fibula following rotational fracture. These metaphyseal fractures
usually have a good blood supply and failure to unite may be diagnosed
based on persistent symptoms with the presence of a radiographic line
or on CT scan in the absence of plain radiographic findings.236
Diaphyseal fibular nonunions may be more common, secondary to the
poorer blood supply to this region of the bone and the higherenergy
fracture patterns associated with pronation-type fibular fractures (Fig. 57-37). The inherent soft tissue stripping present following a pronation-abduction injury may be compounded by attempts at ORIF.
 |
|
FIGURE 57-37 CT scan cuts demonstrating a fibular nonunion following fixation of a pronation-abduction-type fracture.
|
Sneppen in which 119 patients with a nonunited medial malleolar
fracture were followed. Forty-five percent of these patients developed
evidence of posttraumatic osteoarthritis.204
A more recent prospective study showed a diminished incidence of medial
malleolar nonunion with nonoperative care and no evidence of arthritic
change.87 A symptomatic nonunion of
the medial malleolus may be treated with formal takedown, compression
screw placement, and grafting with either autogenous graft or
application of bone morphogenic protein.
fibular nonunion include persistent pain or gait abnormality in
conjunction with CT evidence of bony nonunion.236
Fibular atrophic nonunions require plating and bone graft application,
while hypertrophic nonunions require only stabilization with internal
fixation.
is frequently associated with irritation because of its subcutaneous
location or the associated tendonitis that comes with the peroneal
tendons rubbing over the implants. Persistent pain in the region of
implanted orthopaedic hardware after radiographic evidence of fracture
union commonly leads to implant removal.25,31,33 The treating physician must consider whether the patient may reliably expect pain relief after hardware removal.
ankle, the results are somewhat better than for other locations in the
body. Jacobsen et al. reported on 66 patients who underwent hardware
removal following malleolar fracture as part of their
standard
treatment protocol. The authors found improvement in pain complaints
following hardware removal. In a prospective study, Minkowitz et al.145
evaluated 60 patients undergoing removal of symptomatic hardware
following successful fracture union. These patients were worked up and
considered to have painful retained hardware. Twenty-two of these
patients had malleolar implants that were removed. The authors obtained
preoperative and postoperative functional evaluations and pain scores.
Patients had a 43% improvement in function, a 10% improvement in the
mental component of the SF-36, and a 78% reduction in pain. Mean pain
scores went from 5.5 to 1.3 on average. Finally, 100% of patients were
satisfied with the procedure and would do it again.145
distally to the fibula but may be injured upon a posterolateral
approach to the fibula and tibia. The superficial peroneal nerve
crosses from the lateral to the anterior compartment approximately 7 cm
proximal to the fibular tip. Most SER ankle fractures are therefore
safe when approaching the fibula. When a higher fibular fracture is
operated on, we recommend identification and protection of the nerve
throughout the surgical procedure and closure to prevent damage to the
nerve. Painful neuromas about the ankle are difficult problems to treat
and will degrade otherwise good clinical results. The best treatment is
to prevent this complication.
the development of deep venous thrombosis, including fractures of the
ankle, and ranges from 3% to 21%.70,108,174 Several studies have looked
at development of deep venous thrombosis in patients treated
nonoperatively for ankle fractures.108
In one study, the use of low-molecular-weight heparin was able to
reduce the risk of deep venous thrombosis from 19% to 9%. A second
study looked at the use of low-molecular-weight heparin for either 1 or
6 weeks and found a diminished incidence of deep venous thrombosis with
extended therapy regardless of whether cast immobilization or removable
orthrosis was used.108 There is some
debate as to whether closed fractures treated with immobilization
should undergo prophylaxis as there as complications associated with
the use of chemical venous thromboembolism prophylaxis. The American
College of Chest Surgeons has recommended against the routine use of
isolated lower extremity trauma.70
chemoprophylaxis following surgical intervention for unstable ankle
fractures. Development of a postoperative deep venous thrombosis is
usually asymptomatic but may be the source of persistent calf and foot
swelling. Case reports of pulmonary emboli following ankle fracture
treatment are cause for concern for the treating physician.237
It is incumbent on the treating surgeon to determine whether associated
risk factors are present that would lead toward the use of
chemoprophylaxis in these patients.
performed a randomized clinical trial to assess the optimal treatment
methods for displaced, unstable ankle fractures. A total of 71 patients
were followed for an average 3.5 years. Forty-nine of these patients
underwent a satisfactory closed reduction and were randomized into cast
treatment versus operative treatment. Those in whom an acceptable
closed reduction could not be attained (29 patients) were randomized as
well; however, these patients were randomized into operative treatment
with medial-sided fixation alone versus standard fixation of all
displaced components of the fracture. Functional outcome scores were
greater in the patients treated operatively compared with those treated
in plaster, but the differences were not significant. Radiographically,
mild and moderate arthritic changes were similar between groups. There
was a 23% incidence of arthritic severe arthritic change in those
treated nonoperatively, compared with 0% in those treated with surgery,
at latest follow-up.
looked at in more detail in recent years. The SF-36 questionnaire has
been used to look at physical and mental health following treatment.
Several studies have shown patient physical function to improve over
time following ankle fracture surgery when validated outcome measures
are used.19,56,110,159 Despite these improvements, many patients report residual functional limitations and pain from 1 to 2 years following injury.
Weber B type ankle fracture. These authors looked at what patient-,
injury-, and surgery-related factors predicted outcome based on the
SF-36.19 Patients’ physical and
mental health improved over time following surgical treatment of their
injuries, but the physical function domain of the SF-36 scores never
returned to population normative values. Overall, patient reported pain
improved over time. Smoking was found to be associated poorer physical
function at 2 years and with reporting of higher pain scores at latest
follow-up.19
These authors used the SF-36 as well as the Olerud-Molander score to
assess postoperative function at 2 years. Thirty-six percent of
patients reported fully recovery. Forty-four percent of patients had
some limitations with work-related tasks and 61% of patients had some
difficulty with sports-related performance. B3 type fractures were
associated with lower Olerud-Molander scores.179
patients who had been treated for an stable and unstable fracture of
the ankle.110 Weber A fractures
fared better than types B and C, as would be expected with the mean
Olerud-Molander score of 90 for that cohort. These authors found
functional difficulties in patients treated surgically for an unstable
ankle fracture at 2 years postinjury.
These authors used the SMFA and AOFAS ankle and hindfoot score to
assess functional outcome at points during recovery and compared them
with baseline. Patients were followed at 3, 6, and 12 months clinically
and radiographically. Ninety percent of patients achieved 90%
functional recovery by 1 year. Predictors of recovery included younger
age (<40 years), female sex, healthier patients (ASA Class 1 and 2),
and absence of diabetes mellitus.
poorer outcomes following unstable ankle fracture. Older patient groups
have been found to fail to return to baseline following
ankle fracture surgery.56 Other studies have shown geriatric patients are able to obtain the same good clinical results seen in younger patients.166
These series have had relatively high superficial wound complication
rates, however. Morbidly obese patients have also been at risk for the
development of complications and poor outcomes with regard to fracture
treatments.99 This, however, has not been the case with ankle fracture patients. Body mass index greater than 30 kg/m2
was not associated with an increase in either postoperative
complications or poorer physical function following operative
stabilization in one large series.209
and dislocation compendium. Orthopaedic Trauma Association Committee
for Coding and Classification. J Orthop Trauma 1996;10(suppl 1):v-ix,
1-154.
T, Dalen N, Lundberg A, et al. Early mobilization of operated on ankle
fractures. Prospective, controlled study of 40 bimalleolar cases. Acta
Orthop Scand 1993;64: 95-99.
T, Dalen N, Selvik G. Ankle fractures. A clinical and roentgenographic
stereophotogrammetric study. Clin Orthop Relat Res 1989:246-255.
S, Kocaoglo B, Gereli A, et al. Incidence of chondral lesions of talar
dome in ankle fracture types. Foot Ankle Int 2008;29(3):287-292.
RJ, Furia JP, Marquardt JD. Hematoma block for ankle fractures: a safe
and efficacious technique for manipulations. J Orthop Trauma
1995;9:113-116.
K, Finkelstein J, Khoury A, et al. The use of intraoperative
three-dimensional imaging (ISO-C-3D) in fixation of intraarticular
fractures. Injury 2007;38:1163-1169.
RA, Jackson ST. Fractures of the distal part of the fibula with
associated disruption of the deltoid ligament. Treatment without repair
of the deltoid ligament. J Bone Joint Surg Am 1987;69A:1346-1352.
AB, Anderson LD, Nimityongskul P. Intramedullary screw fixation of
lateral malleolus fractures. Foot Ankle Int 1994;15:599-607.
M, Bengner U, Johnell O, et al. Supination-eversion fractures of the
ankle joint: changes in incidence over 30 years. Foot Ankle
1987;8:26-28.
M, Bergstrom B, Hemborg A, et al. Malleolar fractures: nonoperative
versus operative treatment. A controlled study. Clin Orthop Relat Res
1985:17-27.
CG, Clay NR, Thexton PW. Displaced ankle fractures in patients over 50
years of age. J Bone Joint Surg Br 1983;65B:329-332.
AE, Kabbani KT, Xenakis TA, et al. Surgical treatment of malleolar
fractures. A review of 144 patients. Clin Orthop Relat Res 1997:90-98.
M, Sprague S, Ayeni OR, et al. A prospective cost analysis following
operative treatment of unstable ankle fractures: 30 patients followed
for 1 year. Acta Orthop Scand 2004;75:100-105.
M, Sprague S, Hanson B, et al. Health-related quality of life following
operative treatment of unstable ankle fractures: a prospective
observational study. J Orthop Trauma 2004;18:338-345.
AT, Wood MB, Sheetz KK. Arthrodesis of the ankle with a free
vascularized autogenous bone graft. Reconstruction of segmental loss of
bone secondary to osteomyelitis, tumor, or trauma. J Bone Joint Surg Am
1995;77A:1867-1875.
RH, Connolly E, Wasan A, et al. Acute complications in the operative
treatment of isolated ankle fractures in patients with diabetes
mellitus. Foot Ankle Int 1999;20: 687-694.
SD, Labropoulos PA, McCowin P, et al. Mechanical considerations for the
syndesmosis screw. A cadaver study. J Bone Joint Surg Am
1989;71A:1548-1555.
S, Gardner MJ, Helfet DL, et al. High association of posterior
malleolus fractures with spiral distal tibial fractures. Clin Orthop
Relat Res 2008.
O, Pihlajamaki H. Routine implant removal after fracture surgery: a
potentially reducible consumer of hospital resources in trauma units. J
Trauma 1996;41:846-849.
EA BK, Dorfmann D, et al. Evaluation of ankle fractures: two-view
versus three view radiographic series and comparison of two-view
combinations. AJR Am J Roentgenol 1999.
TJ, Endicott M, Capra SE. Treatment of open ankle fractures. Immediate
internal fixation versus closed immobilization and delayed fixation.
Clin Orthop Relat Res 1989: 47-52.
RS, van Straaten J, Patka P, et al. Immediate or delayed operative
treatment of fractures of the ankle. Injury 1988;19:436-438.
O, Staunstrup H, Sommer J. Stable lateral malleolar fractures treated
with aircast ankle brace and DonJoy R.O.M.-Walker brace: a prospective
randomized study. Foot Ankle Int 1996;17:679-684.
PL, Bisschop AP. Operative treatment of ankle fractures in adults:
correlation between types of fracture and final results. Injury
1991;22:403-406.
RM, Wheelwright EF, Chalmers J. Removal of metal implants after
fracture surgery: indications and complications. J R Coll Surg Edinb
1993;38:96-100.
WC 2nd, Prakash K, Adelaar R, et al. Tibiotalar joint dynamics:
indications for the syndesmotic screw: a cadaver study. Foot Ankle
1993;14:153-158.
C NC. No impact from active dissemination of the Ottawa Ankle Rules:
further evidence of the need for further implementation of practice
guidelines. CMAJ 1999;160:1165-1168.
EJ, Csongradi JJ, Bleck EE. Early complications in the operative
treatment of ankle fractures. Influence of delay before operation. J
Bone Joint Surg Br 1991;73B: 79-82.
RH, Buckwalter KA, Rydberg J, et al. CT with 3D rendering of the
tendons of the foot and ankle: technique, normal anatomy, and disease.
Radiographics 2004; 24:343-356.
HJ, Michelson JD, Cox QG, et al. Tibio-talar stability in bimalleolar
ankle fractures: a dynamic in vitro contact area study. Foot Ankle
1991;11:222-227.
JF, Csencsitz TA. Limb threatening neuropathic complications from ankle
fractures in patients with diabetes. Clin Orthop Relat Res 1998:212-219.
W, Thordarson DB, Debnath UK. Operative management of ankle fractures
in patients with diabetes mellitus. Foot Ankle Int 2007;28:32-37.
WL 3rd, Dirschl DR. Effects of binary decision making on the
classification of fractures of the ankle. J Orthop Trauma
1998;12:280-283.
RI, Tejwani NC, Koval KJ, et al. Functional outcome after surgically
treated ankle fractures; does age matter? Annual Meeting of the
American Academy of Orthopaedic Surgeons, Chicago, IL, 2006.
GA, Swanson CE, Hulcombe BG. Operative treatment of ankle fractures: a
minimum ten-year follow-up. Foot Ankle Int 2001;22:102-106.
NA, Eskander MS, French BG. Does medial tenderness predict deep deltoid
ligament incompetence in supination-external rotation type ankle
fractures? J Orthop Trauma 2007;21:244-247.
NA, Elgafy H, Padanilam T. Syndesmotic disruption in low fibular
fractures associated with deltoid ligament injury. Clin Orthop Relat
Res 2003:260-267.
NA, Wong FY. External rotation views in the diagnosis of posterior
colliculus fracture of the medial malleolus. Am J Orthop
1996;25:380-382.
KA, Amirtharajah M, Tejwani NC, et al. Ankle stress test for predicting
the need for surgical fixation of isolated fibular fractures. J Bone
Joint Surg Am 2004;86A: 2393-2398.
KA, Dolan R, Koval KJ. Functional outcome of surgery for fractures of
the ankle. A prospective, randomised comparison of management in a cast
or a functional brace. J Bone Joint Surg Br 2000;82B:246-249.
KA, Sheikhazadeh A, Mogatederi S, et al. Lower-extremity function for
driving an automobile after operative treatment of ankle fracture. J
Bone Joint Surg Am 2003; 85A:1185-1189.
KA, Tejwani NC, Walsh MG, et al. Predictors of short-term functional
outcome following ankle fracture surgery. J Bone Joint Surg Am
2006;88A:974-979.
JE, Gruber BF, Karunakar MA. Safe zone for the placement of medial
malleolar screws. J Bone Joint Surg Am 2007;89A:133-138.
JS, DeCoster TA, Firoozbakhsh KK, et al. Plain radiographic
interpretation in trimalleolar ankle fractures poorly assesses
posterior fragment size. J Orthop Trauma 1994;8:328-331.
R, Funk L, Pinzur MS, et al. Health related quality of life in patients
with supination-external rotation stage IV ankle fractures. Foot Ankle
Int 2005;26: 1038-1041.
K, Freedman KB, Stover MD, et al. Comparison of a novel
FiberWire-button construct versus metallic screw fixation in a
syndesmotic injury model. Foot Ankle Int 2008;29:49-54.
JP, Alioto RJ, Marquardt JD. The efficacy and safety of the hematoma
block for fracture reduction in closed, isolated fractures. Orthopedics
1997;20:423-426.
MJ, Brodsky A, Briggs SM, et al. Fixation of posterior malleolar
fractures provides greater syndesmotic stability. Clin Orthop Relat Res
2006;447:165-171.
MJ, Demetrakopoulos D, Briggs SM, et al. The ability of the
Lauge-Hansen classification to predict ligament injury and mechanism in
ankle fractures: an MRI study. J Orthop Trauma 2006;20:267-272.
MJ, Demetrakopoulos D, Briggs SM, et al. Malreduction of the
tibiofibular syndesmosis in ankle fractures. Foot Ankle Int
2006;27:788-792.
M, El-Khoury GY. MDCT in the evaluation of skeletal trauma: principles,
protocols, and clinical applications. Emerg Radiol 2006;13:7-18.
SP, Trakru S, Kefer G, et al. A comparative study of early motion and
immediate plaster splintage after internal fixation of unstable
fractures of the ankle. Injury 1993; 24:529-530.
PV, Knuth AE, Nuber GF. Radiographic evaluation of the position of
implants in the medial malleolus in relation to the ankle joint space:
anteroposterior compared with mortise radiographs. J Bone Joint Surg Am
1999;81A:364-369.
K, Hviid K, Jensen CM, et al. Successful immediate weight-bearing of
internal fixated ankle fractures in a general population. J Orthop Sci
2000;5:552-554.
N, Haruyama H, Toga H, et al. Pathoanatomy of posterior malleolar
fractures of the ankle. J Bone Joint Surg Am 2006;88A:1085-1092.
MC. The antiglide plate for distal fibular fixation. A biomechanical
comparison with fixation with a lateral plate. J Bone Joint Surg Am
1988;70A:149-150.
P, Goutallier D. Absence of the medial malleolus. A case report with a
20-year follow-up study. Clin Orthop Relat Res 1991:141-142.
D Jr, Anglen JO, Archdeacon M, et al. Avoiding complications in the
treatment of pronation-external rotation ankle fractures, syndesmotic
injuries, and talar neck fractures. J Bone Joint Surg Am
2008;90A:898-908.
D Jr, Scaduto JM, Infante A. Conservative treatment of isolated
fractures of the medial malleolus. J Bone Joint Surg Br 2007;89B:89-93.
DB, Bunnell WP. Operative anatomy of nerves encountered in the lateral
approach to the distal part of the fibula. J Bone Joint Surg Am
1995;77A:1021-1024.
JL, Weber H, Willenegger H, et al. Evaluation of ankle fractures:
non-operative and operative treatment. Clin Orthop Relat Res
1979:111-119.
GS, Griffon DJ, Siegel AM, et al. Evaluation of an osteoconductive
resorbable calcium phosphate cement and polymethylmethacrylate for
augmentation of orthopedic screws in the pelvis of canine cadavers. Am
J Vet Res 2005;66:1954-1960.
RA, Ittner G, Schedl R. Fractures of the posterior tibial margin: their
role in the prognosis of malleolar fractures. J Trauma
1989;29:1565-1570.
KB, Maiers-Yelden KA, Marsh JL, et al. Ankle fractures in patients with
diabetes mellitus. J Bone Joint Surg Br 2005;87B:489-495.
G, Patzakis MJ, Harvey JP Jr. Precise evaluation of the reduction of
severe ankle fractures. J Bone Joint Surg Am 1974;56A:979-993.
P, Palvanen M, Niemi S, et al. Increasing number and incidence of
low-trauma ankle fractures in elderly people: Finnish statistics during
1970-2000 and projections for the future. Bone 2002;31:430-433.
P, Parkkari J, Niemi S, et al. Epidemiology of osteoporotic ankle
fractures in elderly persons in Finland. Ann Intern Med
1996;125:975-978.
H, Kalenderer O, Karapinar L, et al. Effects of three- or four-cortex
syndesmotic fixation in ankle fractures. J Am Podiatr Med Assoc
2007;97:457-459.
MA, Shah SN, Jerabek S. Body mass index as a predictor of complications
after operative treatment of acetabular fractures. J Bone Joint Surg Am
2005;87A: 1498-1502.
T, Ayturk UM, Haskell A, et al. Fixation of osteoporotic distal fibula
fractures: A biomechanical comparison of locking versus conventional
plates. J Foot Ankle Surg 2007;46:2-6.
G, Karges D, Watson JT, et al. Early versus delayed treatment of severe
ankle fractures: a comparison of results. J Orthop Trauma
1995;9:377-380.
KJ, Egol KA, Cheung Y, et al. Does a positive ankle stress test
indicate the need for operative treatment after lateral malleolus
fracture? A preliminary report. J Orthop Trauma 2007;21:449-455.
KJ, Petraco DM, Kummer FJ, et al. A new technique for complex fibula
fracture fixation in the elderly: a clinical and biomechanical
evaluation. J Orthop Trauma 1997; 11:28-33.
KD, Hansen T. Closed treatment of ankle fractures. Stage II
supination-eversion fractures followed for 20 years. Acta Orthop Scand
1985;56:107-109.
B. Results of surgical treatment of malleolar fractures in patients
with diabetes mellitus. Dan Med Bull 1983;30:272-274.
LJ, Ponzer S, Elvin A, et al. Prolonged thromboprophylaxis with
Dalteparin during immobilization after ankle fracture surgery: a
randomized placebo-controlled, double-blind study. Acta Orthop
2007;78:528-535.
S, Bauer TW. Use of injectable calcium phosphate cement for fracture
fixation: a review. Clin Orthop Relat Res 2002:23-32.
N, Horne G, Fielden J, Devane P. Ankle fractures: functional and
lifestyle outcomes at 2 years. Aust N Z J Surg 2002;72:724-730.
N. Fractures of the ankle. II. Combined experimental-surgical and
experimental-roentgenologic investigations. Arch Surg 1950;60:957-985.
H, Jarvinen TL, Honkonen S, et al. Use of a cast compared with a
functional ankle brace after operative treatment of an ankle fracture.
A prospective, randomized study. J Bone Joint Surg Am 2003;85A:205-211.
N, Hinojosa L, Panchbhavi VK. Arthroscopically detected intraarticular
lesions associated with acute ankle fractures. J Bone Joint Surg AM
2009;91(2)333-339.
KS, Siu WS, Li SF, et al. An in vitro optimized injectable calcium
phosphate cement for augmenting screw fixation in osteopenic goats. J
Biomed Mater Res B Appl Biomater 2006;78:153-160.
M, Torres R, Guillen P. Complications of open reduction and internal
fixation of ankle fractures. Foot Ankle Clin 2003;8:131-147, ix.
U. Operative treatment of ankle fracture-dislocations. A follow-up
study of 306/321 consecutive cases. Clin Orthop Relat Res 1985:28-38.
VW, Matthews LS, Zwirkoski P, et al. The joint-contact area of the
ankle. The contribution of the posterior malleolus. J Bone Joint Surg
Am 1991;73A:347-351.
D, Michelson JD, Ney DR, et al. ankle fractures: comparison of plain
films and interactive two- and three-dimensional CT scans. AJR Am J
Roentgenol 1990;154: 1017-1023.
NK, Bhowal B, Harper WM, et al. Conservative versus operative treatment
for displaced ankle fractures in patients over 55 years of age. A
prospective, randomised study. J Bone Joint Surg Br 2001;83B:525-529.
KL, Schmalzried TP, Ferkel RD. Torsional strength of the ankle in
vitro. The supination-external-rotation injury. Clin Orthop Relat Res
1989:266-272.
RK, Raaymakers EL, Nolte PA. Malunited ankle fractures. The late
results of reconstruction. J Bone Joint Surg Br 1990;72B:709-713.
S, Fiori R, Marinetti A, et al. Imaging the ankle and foot and using
magnetic resonance imaging. Int J Low Extrem Wounds 2003;2:217-232.
T, Creevy W, Tornetta P 3rd. Stress examination of supination external
rotation-type fibular fractures. J Bone Joint Surg Am
2004;86A:2171-2178.
T, Tornetta P 3rd. Marginal plafond impaction in association with
supination-adduction ankle fractures: a report of eight cases. J Orthop
Trauma 2001;15: 447-449.
CJ, Burge PD. Rotatory stability of the load-bearing ankle. An
experimental study. J Bone Joint Surg Br 1980;62B:460-464.
JM, Hoffmeyer P, Savoy X. High resolution computed tomography in the
chronically painful ankle sprain. Foot Ankle 1988;8:291-296.
JD, Ahn UM, Helgemo SL. Motion of the ankle in a simulated
supination-external rotation fracture model. J Bone Joint Surg Am
1996;78A:1024-1031.
JD, Varner KE, Checcone M. Diagnosing deltoid injury in ankle
fractures: the gravity stress view. Clin Orthop Relat Res 2001:178-182.
JD, Waldman B. An axially loaded model of the ankle after pronation
external rotation injury. Clin Orthop Relat Res 1996:285-293.
KP, Lee C, Ahn C, et al. Comparison of lateral locking plate and
antiglide plate for fixation of distal fibular fractures in
osteoporotic bone: a biomechanical study. J Orthop Trauma
2006;20:562-566.
RB, Bhadsavle S, Walsh M, et al. Removal of painful orthopaedic
implants after fracture union. J Bone Joint Surg Am 2007;89A:1906-1912.
MJ, Ho C, Howard BA, et al. Diagnostic imaging of trauma to the ankle
and foot: I. Fractures about the ankle. J Foot Surg 1989;28:174-179.
MA, Sedlin ED, Weiner LS, Miller AR. Postoperative radiographs as
predictors of clinical outcome in unstable ankle fractures. J Orthop
Trauma 1992;6:352-357.
JA Jr, Shank JR, Morgan SJ, Smith WR. Syndesmosis fixation: a
comparison of three and four cortices of screw fixation without
hardware removal. Foot Ankle Int 2006;27:567-572.
JR, Lee J, Thordarson D, et al. Magnetic resonance imaging of acute
Maisonneuve fractures. Foot Ankle Int 1996;17:259-263.
HH, Bicimoglu A, Celebi L, et al. Magnetic resonance arthrographic
evaluation of syndesmotic diastasis in ankle fractures. Arch Orthop
Trauma Surg 2005;125: 222-227.
T, Butt SH, Cassar-Pullicino VN. Stress fractures and related disorders
in foot and ankle: plain films, scintigraphy, CT, and MR Imaging. Semin
Musculoskelet Radiol 2005;9:210-226.
JH, Gardner MJ, Peterson MG, et al. Radiographic measurements do not
predict syndesmotic injury in ankle fractures: an MRI study. Clin
Orthop Relat Res 2005: 216-221.
MH, Sormaala MJ, Kiuru MJ, et al. Bone stress injuries of the ankle and
foot: an 86-month magnetic resonance imaging-based study of physically
active young adults. Am J Sports Med 2007;35:643-649.
WT, Dirschl DR, Crowther JD, et al. Change over time of SF-36
functional outcomes for operatively treated unstable ankle fractures. J
Orthop Trauma 2002;16: 30-33.
CM, Graham JD, Hall JH, et al. Late revision of fibular malunion in
ankle fractures. Clin Orthop Relat Res 1982:145-149.
C. The effect of the syndesmotic screw on the extension capacity of the
ankle joint. Arch Orthop Trauma Surg 1985;104:299-302.
A, Nishikawa S, Nagao A, et al. Arthroscopically assisted treatment of
ankle fractures: arthroscopic findings and surgical outcomes.
Arthroscopy 2004;20:627-631.
AJ, Michelson JD, Mizel MS. Results of operative fixation of unstable
ankle fractures in geriatric patients. Foot Ankle Int 2001;22:399-402.
AM. Trauma to the ankle. In MH Jhass, ed. Disorders of the Foot and
Ankle: Medical and Surgical Management. 2nd ed. Philadelphia: WB
Saunders, 1991: 2361-2414.
AM, Shivaram MS. Anatomical basis of variability in injuries of the
medial malleolus and the deltoid ligament. I. Anatomical studies. Acta
Orthop Scand 1979; 50:217-223.
AM, Shivaram MS. Anatomical basis of variability in injuries of the
medial malleolus and the deltoid ligament. II. Clinical studies. Acta
Orthop Scand 1979;50: 225-336.
SS, Kubiak EN, Egol KA, et al. Stress radiographs after ankle fracture:
the effect of ankle position and deltoid ligament status on medial
clear space measurements. J Orthop Trauma 2006;20:11-18.
R, Shoji H, D’Ambrosia RD. Effects of ligamentous injury on ankle and
subtalar joints: a kinematic study. Clin Orthop Relat Res 1979:266-272.
S, Gandhi J, Curzon I, et al. Incidence of deep-vein thrombosis in
patients with fractures of the ankle treated in a plaster cast. J Bone
Joint Surg Br 2007;89B: 1340-1343.
RE, Harrington RM, Henley MB, et al. Biomechanical effects of internal
fixation of the distal tibiofibular syndesmotic joint: comparison of
two fixation techniques. J Orthop Trauma 1994;8:215-219.
FA, Gail M, Pee D, et al. Quantitative criteria for prediction of the
results after displaced fracture of the ankle. J Bone Joint Surg Am
1983;65A:667-677.
WA, Schwartz HS, Keller CS, et al. A prospective, randomized study of
the management of severe ankle fractures. J Bone Joint Surg Am
1985;67A:67-78.
S, Nasell H, Bergman B, et al. Functional outcome and quality of life
in patients with type B ankle fractures: a two-year follow-up study. J
Orthop Trauma 199913: 363-368.
WG, Larkin JJ, Draganich LF. Assessment of the posterior malleolus as a
restraint to posterior subluxation of the ankle. J Bone Joint Surg Am
1992;74A:1201-1206.
PL, Hamilton W. Changes in tibiotalar area of contact caused by lateral
talar shift. J Bone Joint Surg Am 1976;58A:356-357.
N, Mosheiff R, Liebergall M. Nonunion of a fracture of the lateral
malleolus: a case report and review of the literature. Foot Ankle Int
1997;18:50-52.
TD, Nimityongskul P, Anderson LD. Percutaneous intramedullary fixation
of lateral malleolus fractures: technique and report of early results.
J Trauma 1994;36:669-675.
DJ, Sauve PS, Sakellariou A. Investigation of incidence of superficial
peroneal nerve injury following ankle fracture. Foot Ankle Int
2003;24:771-774.
P, Stabler A, Merl T, et al. Diagnosis of acute fractures of the
extremities: comparison of low-field MRI and conventional radiography.
Eur Radiol 2004;14: 625-630.
M, Geerling J, Zech S, et al. Intraoperative three-dimensional imaging
with a motorized mobile C-arm (SIREMOBIL ISO-C-3D) in foot and ankle
trauma care: a preliminary report. J Orthop Trauma 2005;19:259-266.
A, Andersson GB. Normal range of motion of the hip, knee and ankle
joints in male subjects, 30-40 years of age. Acta Orthop Scand
1982;53:205-208.
ZS, Cheung Y, Jahss MH, et al. Rupture of posterior tibial tendon: CT
and MR imaging with surgical correlation. Radiology 1988;169:229-235.
ZS, Jahss MH, Noto AM, et al. Rupture of the posterior tibial tendon:
CT and surgical findings. Radiology 1988;167:489-493.
DI, Norris SH, Duckworth T. A prospective trial comparing operative and
manipulative treatment of ankle fractures. J Bone Joint Surg Br
1986;68B:610-613.
L, Bengtsson S. Isolated fracture of the lateral malleolus requires no
treatment: 49 prospective cases of supination-eversion type II ankle
fractures. Acta Orthop Scand 1992;63:443-446.
M, Dudkiewicz I, Novikov I, et al. The epidemic of ankle fractures in
the elderly: is surgical treatment warranted? Arch Orthop Trauma Surg
2000;120:511-513.
JS, Cody GW. Closed treatment of ankle fractures: a new criterion for
evaluation: a review of 250 cases. J Trauma 1976;16:323-326.
KB, Stiehl JB, Skrade DA, et al. Posterior malleolar ankle fractures:
an in vitro biomechanical analysis of stability in the loaded and
unloaded states. J Orthop Trauma 1992;6:96-101.
HJ, Pinzur M, Manion L, et al. The use of gravity or manual-stress
radiographs in the assessment of supination-external rotation fractures
of the ankle. J Bone Joint Surg Br 2007;89B:1055-1059.
J, Tornetta P 3rd. Extraperiosteal plating of pronation-abduction ankle
fractures. Surgical technique. J Bone Joint Surg Am 2008;90(suppl
2)A:135-144.
CJ, Maegele MG, Lefering R, et al. Functional treatment and early
weightbearing after an ankle fracture: a prospective study. J Orthop
Trauma 2006;20:108-114.
J, Benjamin J, Wilson J, et al. Ankle mortise stability in Weber C
fractures: indications for syndesmotic fixation. J Orthop Trauma
1991;5:190-195.
E, Tornetta P 3rd, Creevy WR. Syndesmotic instability in Weber B ankle
fractures: a clinical evaluation. J Orthop Trauma 2007;21:643-646.
IG, Greenberg GH, McKnight RD, et al. Decision rules for the use of
radiography in acute ankle injuries. Refinement and prospective
evaluation. JAMA 1993;269: 1127-1132.
IG, Wells G, Laupacis A, et al. Multicentre trial to introduce the
Ottawa Ankle Rules for use in radiography of acute ankle injuries.
Multicentre Ankle Rules Study Group. Br Med J 1995;311:594-597.
U, Hoffmann R, Schutz M, et al. Fastest reduction of posttraumatic
edema: continuous cryotherapy or intermittent impulse compression? Foot
Ankle Int 1997; 18:432-438.
EJ, Frank JB, Walsh M, et al. Does obesity influence the outcome after
the operative treatment of ankle fractures? J Bone Joint Surg Br
2007;89B:794-798.
EJ, Petrucelli G, Bong M, et al. Blisters associated with
lower-extremity fracture: results of a prospective treatment protocol.
J Orthop Trauma 2006;20:618-622.
K, Hoqevold HE, Skjeldal S, et al. The repair of a ruptured deltoid
ligament is not necessary in ankle fractures. J Bone Joint Surg Br
1995;77B:920-921.
H, Bremersko V, Baekgaard N. Ankle fractures treated by fixation of the
medial malleolus alone. Acta Orthop Scand 1978;49:211-214.
MD, Roberts JB. Compartment syndrome after Bosworth
fracture-dislocation of the ankle: a case report. J Orthop Trauma
2001;15:301-303.
M Jr, St Pierre RK, Fleming LL, et al. Computerized tomography in the
evaluation of peroneal tendon dislocation. A report of two cases. Am J
Sports Med 1983;11:444-447.
Y, Tanaka Y, Sugimoto K, et al. Long-term results of arthrodesis for
osteoarthritis of the ankle. Clin Orthop Relat Res 1999:178-185.
CC, Harrington RM. A biochemical analysis of the squeeze test for
sprains of the syndesmotic ligaments of the ankle. Foot Ankle Int
1998;19:489-492.
NO, Overgaard S, Olsen LH, et al. Observer variation in the
radiographic classification of ankle fractures. J Bone Joint Surg Br
1991;73B:676-678.
DB, Ghalambor N, Perlman M. Intermittent pneumatic pedal compression
and edema resolution after acute ankle fracture: a prospective,
randomized study. Foot Ankle Int 1997;18:347-350.
DB, Hedman TP, Gross D, et al. Biomechanical evaluation of polylactide
absorbable screws used for syndesmosis injury repair. Foot Ankle Int
1997;18: 622-627.
BC, Koval KJ, Kummer FJ, et al. Vertical shear fractures of the medial
malleolus: a biomechanical study of five internal fixation techniques.
Foot Ankle Int 1994;15: 483-489.
P 3rd. Competence of the deltoid ligament in bimalleolar ankle
fractures after medial malleolar fixation. J Bone Joint Surg Am
2000;82A:843-848.
P 3rd, Spoo JE, Reynolds FA, et al. Overtightening of the ankle
syndesmosis: is it really possible? J Bone Joint Surg Am
2001;83A:489-942.
P. Fractures and soft tissue injuries of the ankle. In: Staff W, ed.
Skeletal Trauma. Philadelphia: WB Saunders, 1992:1871-1956.
PG, DiGiovanni CW. Malleolar fractures: open reduction internal
fixation. In D W, ed. Master Techniques in Orthopaedic Surgery;
Fractures. Philadelphia: Lippincott-Raven, 1998:485-504.
JR, Fallat LM. The antiglide plate for the Danis-Weber type-B fibular
fracture: a review of 71 cases. J Foot Ankle Surg 1993;32:573-579.
den Hoogenband CR, van Moppes FI, Stapert JW, et al. Clinical
diagnosis, arthrography, stress examination and surgical findings after
inversion trauma of the ankle. Arch Orthop Trauma Surg 1984;103:115-119.
der Werken C, Oostvogel HJ. The dorsal approach for internal fixation
of fractures of the lateral malleolus. Neth J Surg 1986;38:85-86.
A, Lubitz J, Gierer P, et al. Detection of fibular torsional
deformities after surgery for ankle fractures with a novel CT method.
Foot Ankle Int 2006;27: 1115-1121.
F, Wera G, Knoblich GO, et al. Pulmonary embolism following operative
treatment of ankle fractures: a report of three cases and review of the
literature. Foot Ankle Int 2002;23:406-410.
AJ, Ackroyd CE, Baker AS. Late lengthening of the fibula for malaligned
ankle fractures. J Bone Joint Surg Br 1990;72B:714-717.
D, Friederich NF, Muller W. Lengthening osteotomy of the fibula for
posttraumatic malunion. Indications, technique and results. Int Orthop
1998;22:149-152.
B, Bhandari M. Predictors of functional outcome following
transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma
2005;19:102-108.
BJ, Walsh M, Egol KA, et al. Intra-articular block compared with
conscious sedation for closed reduction of ankle fracture-dislocations.
A prospective randomized trial. J Bone Joint Surg Am 2008;90A:731-734.
B, Weber BG, Simpson LA. The dorsal antiglide plate in the treatment of
Danis-Weber type-B fractures of the distal fibula. Clin Orthop Relat
Res 1990:204-209.
JC, van Laarhoven CJ, van der Werken C. The posterior antiglide plate
for fixation of fractures of the lateral malleolus. Injury
1992;23:94-96.
IG, Heller FG, Shouse L. The key role of the lateral malleolus in
displaced fractures of the ankle. J Bone Joint Surg Am 1977;59A:169-173.
J, Kristensen KD. Ankle fractures. Supination-eversion fractures stage
II. Primary and late results of operative and non-operative treatment.
Acta Orthop Scand 1980; 51:695-702.
S, Taylor L, Kealey D. Isolated lateral compartment syndrome after
Weber C fracture dislocation of the ankle: a case report and literature
review. Injury 2005; 36:345-346.
