Sternoclavicular Joint Injuries
injuries are discussed as injuries that can essentially be managed with
a sling and swathe.41 The first case reports of sc injury are attributed to Rodrigues166
who described a patient with posterior dislocation presenting with
signs of suffocation following a compression injury between a wall and
a cart. Isolated nineteenth century reports in Europe were followed by
those of American authors in the 1920s and 1930s.55,118
SC joint injuries are uncommon and are usually relatively benign
injuries. However, the more severe posterior injury patterns can
represent true medical emergencies and require the orthopaedic surgeon
to be knowledgeable regarding the proper steps in diagnosis and
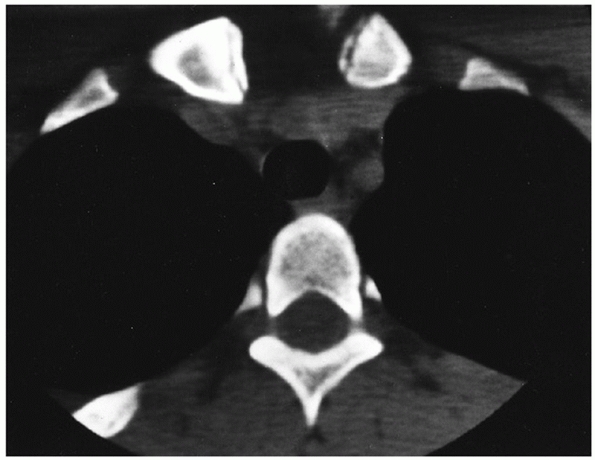
treatment. Computed tomography (CT) scan remains the imaging modality
of choice. Early and prompt reduction is indicated for posterior
dislocations and posterior physeal injuries. A variety of
reconstructive techniques are available if needed, but are rarely
required.
dislocation of the SC joint. Because the SC joint is subject to
practically every motion of the upper extremity and because the joint
is small and incongruous, one would think that it would be the most
commonly dislocated joint in the body. However, the ligamentous
supporting structure is strong and so designed that it is, in fact, one
of the least commonly dislocated joints. A traumatic dislocation of the
SC joint usually occurs only after tremendous forces, either direct or
indirect, have been applied to the shoulder.
 |
|
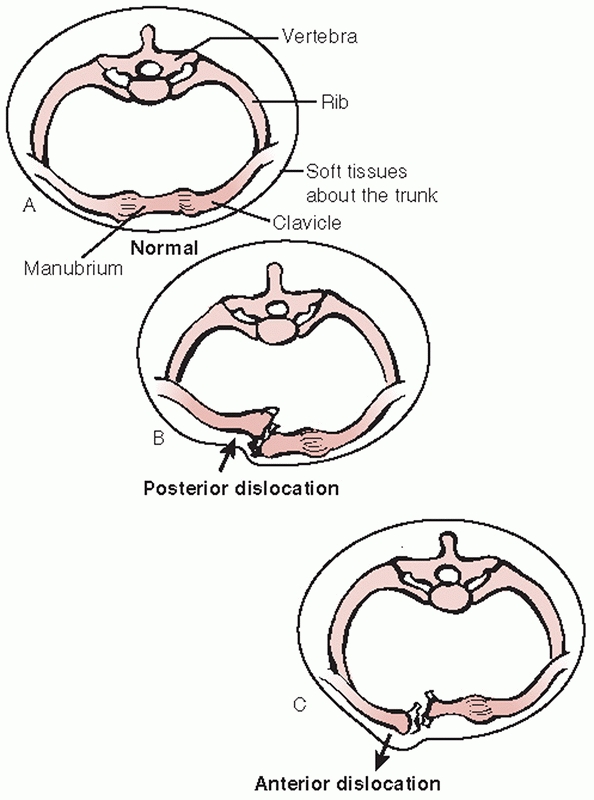
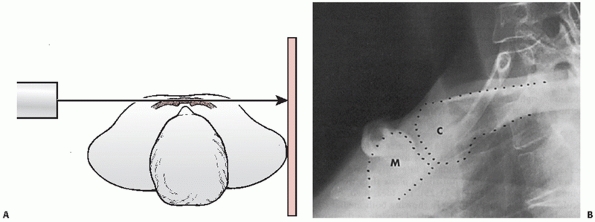
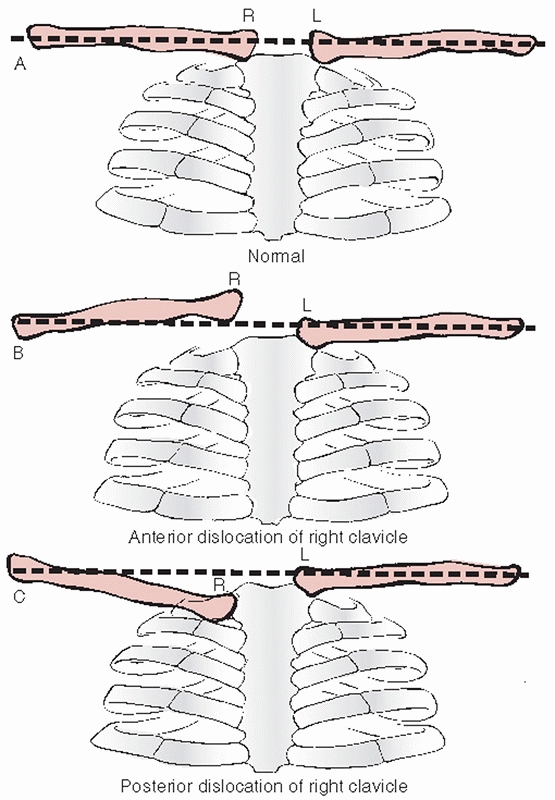
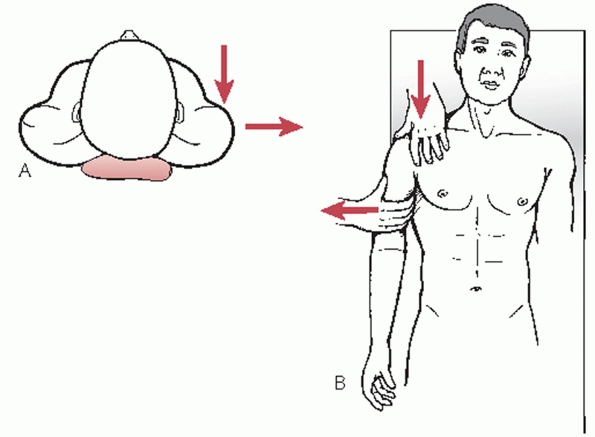
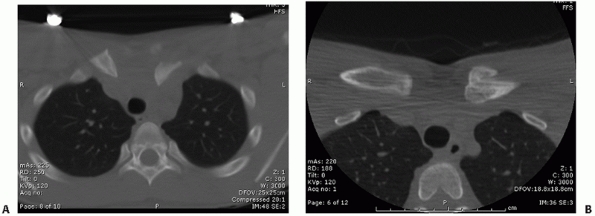
FIGURE 40-1 Cross sections through the thorax at the level of the SC joint. A. Normal anatomic relations. B. Posterior dislocation of the SC joint. C. Anterior dislocation of the SC joint.
|
aspect of the clavicle, the clavicle is pushed posteriorly behind the
sternum and into the mediastinum (Fig. 40-1).
This may occur in a variety of ways: an athlete lying on his back on
the ground is jumped on and the knee of the jumper lands directly on
the medial end of the clavicle, a kick is delivered to the front of the
medial clavicle, a person lying supine is run over by a vehicle, or a
person is pinned between a vehicle and a wall (Fig. 40-2). Anatomically, it is essentially impossible for a direct force to produce an anterior SC dislocation.
 |
|
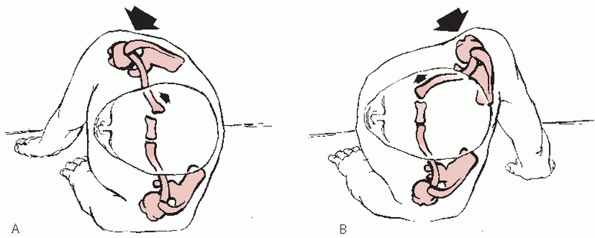
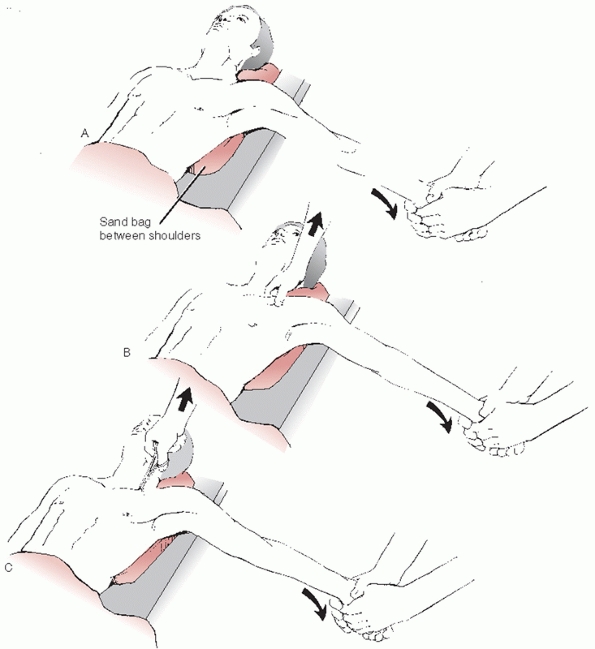
FIGURE 40-3 Mechanisms that produce anterior or posterior dislocation of the SC joint. A.
If the patient is lying on the ground and a compression force is applied to the posterolateral aspect of the shoulder, the medial end of the clavicle will be displaced posteriorly. B. When the lateral compression force is directed from the anterior position, the medial end of the clavicle is dislocated anteriorly. |
 |
|
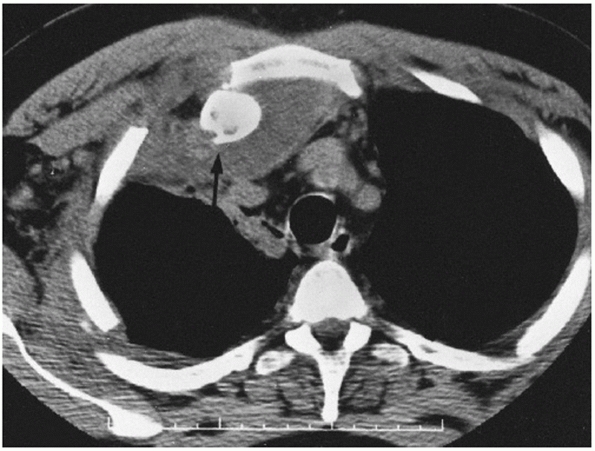
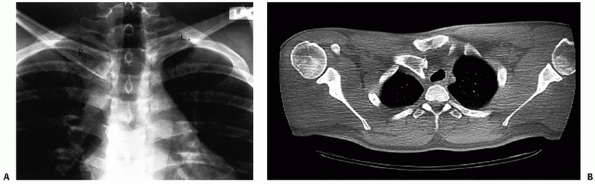
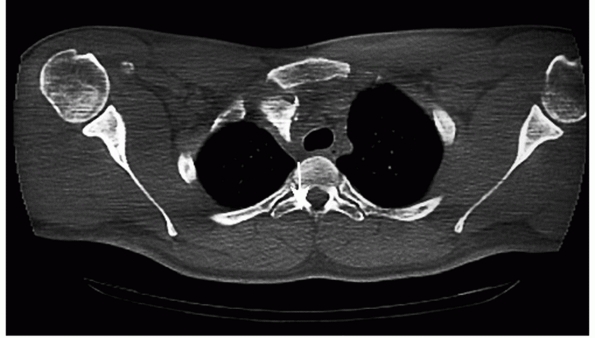
FIGURE 40-2
Computed axial tomogram of a posterior SC joint dislocation that occurred when the driver’s chest impacted the steering wheel during a motor vehicle accident. The steering wheel was fractured from the driving column and the vehicle was totally destroyed. |
the anterolateral or posterolateral aspects of the shoulder. This is
the most common mechanism of injury to the sternoclavicular joint.
Mehta and coworkers131 reported that three of four posterior SC dislocations were produced by indirect force, and Heinig86
reported that indirect force was responsible for eight of nine cases of
posterior SC dislocations. If the shoulder is compressed and rolled
forward, an ipsilateral posterior dislocation results; if the shoulder
is compressed and rolled backward, an ipsilateral anterior dislocation
results (Fig. 40-3).
vehicular accidents; the second is an injury sustained during
participation
in sports.139,143,195 Omer,143
in his review of patients from 14 military hospitals, found 82 cases of
SC joint dislocations. He reported that almost 80% of these occurred as
the result of vehicular accidents (47%) or in athletics (31%).
is 3%. (Specific incidences in the study were glenohumeral dislocations
at 85%, acromioclavicular injuries 12%, and SC injuries 3%.) In the
series by Cave et al.,38 and in our experience, dislocation of the SC joint is not as rare as posterior dislocation of the glenohumeral joint.
showed that injuries involving the shoulder complex accounted for 39.1%
of upper extremity injuries and 11.4% of all alpine skiing injuries. Of
the 393 injuries involving the shoulder complex, SC separations
accounted for 0.5%.
reviewed 18 cases of SC dislocations, none of which were posterior.
However, in our series of 185 traumatic SC injuries, there were 135
patients with anterior dislocation and 50 patients with a posterior
dislocation.
the critical surrounding structures in the neck and thorax and/or by
other musculoskeletal injuries. Significant concomitant injuries of the
mediastinum must be considered to avoid catastrophic outcomes. These
injuries almost always occur in the setting of posterior SC fractures
and dislocations and include:
-
Tracheal compression: from the initial case report of Rodriques166
to multiple case reports in recent articles, the trachea can be
displaced by the posteriorly displaced medial aspect of the clavicle.
Acute airway compromise or subacute dyspnea are key symptoms.121,137 -
Pneumothorax: pleural violation by the
clavicle has been noted with SC dislocation and should be especially
considered in high-energy direct trauma.147 -
Laceration of the great vessels: the
great vessels of the mediastinum can be directly transected and case
reports have included the pulmonary artery,204 brachiocephalic vein,42 and superior vena cava.147 Compression of any of the great vessels without frank laceration can also occur as a complication of injury.140,144 -
Esophageal perforation/rupture: cases of esophageal rupture are often described in relation to local sequelae. Howard90 reported a case of rupture complicated by osteomyelitis of the clavicle. Wasylenko196 reported on a fatal tracheoesophageal fistula.
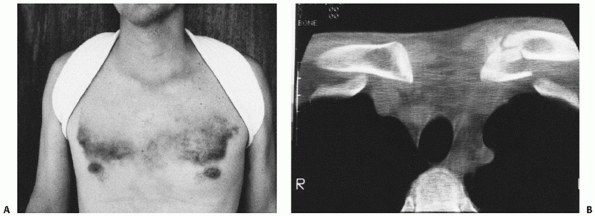
reported a bilateral traumatic dislocation of the SC joint. The senior
author has treated four cases of bilateral SC dislocation. Bilateral
subluxation has also been reported.77
reported a single case and reviewed 15 cases that had been previously
reported. With the exception of this patient, all patients had been
treated conservatively with acceptable function. Dieme et al.53 reported three cases of “floating clavicle.” In 1990, Sanders et al.170
reported 6 patients who had a dislocation of both ends of the clavicle.
Two patients who had fewer demands on the shoulder did well with only
minor symptoms after nonoperative management. The other 4 patients had
persistent symptoms that were localized to the acromioclavicular (AC)
joint. Each of these patients had a reconstruction of the AC joint,
which resulted in a painless, full range of motion and a return to
normal activity (Fig. 40-4). AC dislocation can also accompany medial clavicle epiphyseal fracture/dislocation.75 Wade et al.194
reported a trapped posterior inferior AC dislocation associated with a
medial epiphyseal fracture which required open reduction of the AC
joint and exploration of the SC injury with a good result.
anterior or posterior dislocation of the SC joint has been noted. It is
important to assess the AC joint and the SC joint in the face of the
more obvious midshaft clavicle fracture to avoid a delay in diagnosis.
Tanlin,183 Arenas et al.,4 Friedl and Fritz,70 and Thomas184 have all reported patients who had an anterior dislocation of the SC joint and a fracture of the midclavicle. Allen et al.,3 Nakazato,138 and Mounasamy136
each reported on a skeletally immature patient who had an ipsilateral
clavicle fracture and a posterior dislocation of the SC joint. Velutini
and Tarazona192 reported a bizarre
case of posterior dislocation of the left medial clavicle, the first
rib, and a section of the manubrium. Elliott58
reported on a tripartite injury about the clavicle region in which the
patient had an anterior subluxation of the right SC joint, a type II
injury to the right AC joint, and a fracture of the right midclavicle.
Pearsall and Russell149 reported a
patient who had an ipsilateral clavicle fracture, an anterior SC joint
subluxation, and a long thoracic nerve injury. All of these injuries
involving the SC joint and the clavicle were associated with severe
trauma to the shoulder region.
reported a patient with SC dislocation associated with scapulothoracic
dissociation. This patient had also sustained a transection of the
axillary artery and an avulsion of the median nerve. Following a
vascular repair and an above the elbow amputation, this patient was
left with a complete brachial plexopathy.
for treatment of each individual dislocation separately. When patients
have dislocations of both ends of the clavicle, we recommend
stabilization of the AC joint with appropriate surgical techniques for
type III, IV, V, and VI separations. The SC dislocation is generally
treated nonoperatively with the exception of the
unreduced
posterior dislocation which is treated following the guidelines
outlined later in this chapter. When the clavicle is fractured with an
SC dislocation, the clavicle should be stabilized with internal
fixation for posterior injuries and treated as appropriate for an
isolated clavicle fracture when the SC dislocation is anterior. In the
rare case of a scapulothoracic disassociation and SC dislocation, only
the exclusive criteria for SC management can be applied in isolation.
 |
|
FIGURE 40-4 Dislocation of both ends of the clavicle. A. Clinical view demonstrating anterior dislocation of the right SC joint. B. The axillary radiograph reveals posterior dislocation of the AC joint. C. These injuries are generally treated by AC joint repair/reconstruction with return of near normal function.
|
initial treating physician to associated injuries and to the direction
of dislocation. The patient should be questioned about pain in the
adjacent ACjoint and glenohumeral joint. The patient with a posterior
dislocation has more pain than a patient with an anterior dislocation,
and the anterosuperior fullness of the chest produced by the clavicle
is less prominent and visible when compared with the normal side. The
usually palpable medial end of the clavicle is displaced posteriorly.
The corner of the sternum is easily palpated as compared with the
normal SC joint. Venous congestion may be present in the neck or in the
upper extremity.80 Symptoms may also include a dry irritating cough and hoarseness.59,150
Breathing difficulties, shortness of breath, or a choking sensation may
be noted. Circulation to the ipsilateral arm may be decreased, although
the presence of pulses does not exclude vessel injury. The patient may
complain of difficulty in swallowing or a tight feeling in the throat
or may be in a state of complete shock or possibly have a pneumothorax.
The distal neurologic exam may reveal diminished sensation or weakness
secondary to brachial plexus compression. Complete nerve deficits
suggest more severe injury patterns. The exam should include assessment
of the Wynne-Davies signs205 of
generalized ligamentous laxity as these patients are predisposed to
atraumatic anterior SC joint subluxation. We have seen a number of
patients who clinically appeared to have an anterior dislocation of the
SC joint but on x-ray studies were shown to have complete posterior
dislocation. The point is that
one
cannot always rely on the clinical findings of observing and palpating
the joint to make a distinction between anterior and posterior
dislocations.
 |
|
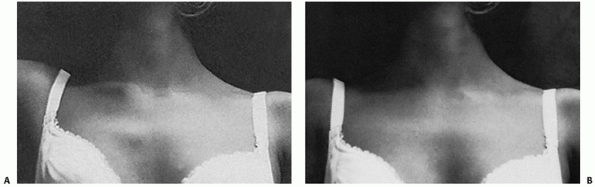
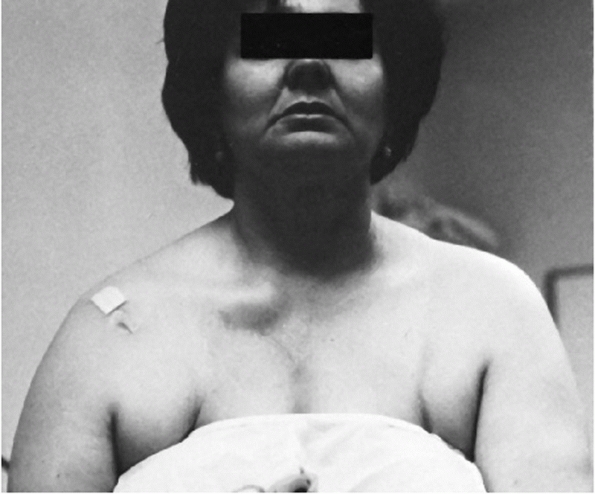
FIGURE 40-5 A.
A 34-year-old patient was involved in a motorcycle accident and sustained an anterior blow to the chest. Note the symmetric anterior chest wall ecchymosis. B. CT reveals a left medial clavicle fracture without disruption of the SC joint. |
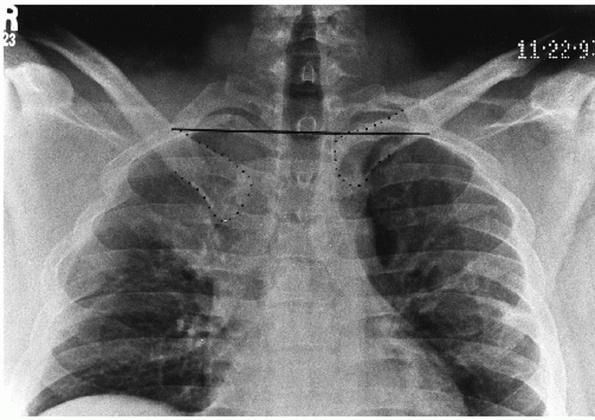
posteroanterior radiographs of the chest or SC joint suggest something
is wrong with one of the clavicles, because it appears to be displaced
as compared with the normal side. McCulloch et al.128
reported that on nonrotated frontal radiographs, a difference in the
relative craniocaudal positions of the medial clavicles of greater than
50% of the width of the heads of the clavicles suggests dislocation. It
would be ideal to take a view at right angles to the anteroposterior
plane, but because of the anatomy, it is impossible to obtain a true
90-degree cephalic-to-caudal lateral view. Lateral radiographs of the
chest are at right angles to the anteroposterior plane, but they cannot
be interpreted because of the density of the chest and the overlap of
the medial clavicles with the first rib and the sternum. Regardless of
a clinical impression that suggests an anterior or posterior
dislocation, radiographs and preferably a CT scan must be obtained to
confirm one’s suspicions (Fig. 40-5).
 |
|
FIGURE 40-6 Heinig view. A. Positioning of the patient for x-ray evaluation of the SC joint, as described by Heinig. B. Heinig view demonstrating a normal relationship between the medial end of the clavicle (C) and the manubrium (M).
|
While the serendipity view is frequently obtained as a front line image
for evaluation of the SC joint, the Heinig and Hobbs views are rarely
obtained if CT is available. However, the Heinig and Hobbs views can be
useful when suspicion is high on clinical exam and confirmation is
needed before referral for CT, especially in the outpatient setting
when delayed presentation often leads to misdiagnosis.
x-ray tube is placed approximately 30 inches from the involved SC joint
and the central ray beam is directed tangential to the joint and
parallel to the opposite clavicle. The cassette is placed against the
opposite shoulder and centered on the manubrium (Fig. 40-6).
 |
|
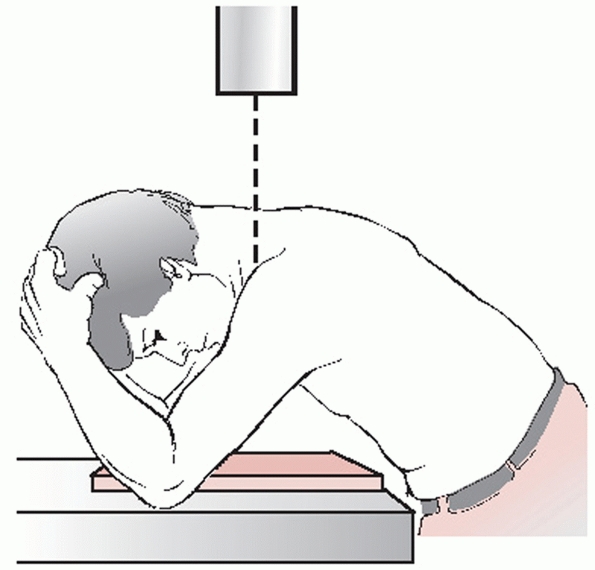
FIGURE 40-7
Hobbs view. Positioning of the patient for x-ray evaluation of the SC joint, as recommended by Hobbs. (From Hobbs DW. Sternoclavicular joint: a new axial radiographic view. Radiology 1968;90:801-802.) |
the x-ray table, high enough to lean forward over the table. The
cassette is placed on the table, and the lower anterior rib cage is
against the cassette (Fig. 40-7). The patient
leans forward so that the nape of his flexed neck is almost parallel to
the table. The flexed elbows straddle the cassette and support the head
and neck. The x-ray source is above the nape of the neck, and the beam
passes through the cervical spine to project the sternoclavicular
joints onto the cassette.
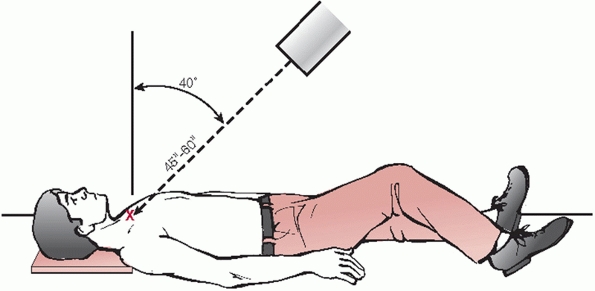
named because that is the way it was developed. The senior author
accidentally noted that the next best thing to having a true
cephalocaudal lateral view of the SC joint was a 40-degree cephalic
tilt view. The patient is positioned on his back squarely and in the
center of the x-ray table. The tube is tilted at a 40-degree angle off
the vertical and is centered directly on the sternum (Figs. 40-8, 40-9, 40-10 and 40-11).
A nongrid 11- × 14-inch cassette is placed squarely on the table and
under the patient’s upper shoulders and neck so that the beam aimed at
the sternum will project both clavicles onto the film.
 |
|
FIGURE 40-8
Serendipity view. Positioning of the patient to take the “serendipity” view of the SC joints. The x-ray tube is tilted 40 degrees from the vertical position and aimed directly at the manubrium. The nongrid cassette should be large enough to receive the projected images of the medial halves of both clavicles. In children, the tube distance from the patient should be 45 inches; in thicker-chested adults, the distance should be 60 inches. |
 |
|
FIGURE 40-9 When viewed from around the level of the patient’s knees, it is apparent that the left clavicle is dislocated anteriorly.
|
 |
|
FIGURE 40-10
Posterior dislocation of the right medial clavicle as seen on 40-degree cephalic tilt serendipity radiograph. The right clavicle is inferiorly displaced as compared to the normal left clavicle. |
 |
|
FIGURE 40-11 Interpretation of the cephalic tilt (serendipity view) x-ray films of the SC joints. A. In the normal person, both clavicles appear on the same imaginary line drawn horizontally across the film. B.
In a patient with an anterior dislocation of the right SC joint, the medial half of the right clavicle is projected above the imaginary line drawn through the level of the normal left clavicle. C. If the patient has a posterior dislocation of the right SC joint, the medial half of the right clavicle is displaced below the imaginary line drawn through the normal left clavicle. |
 |
|
FIGURE 40-12 A. Routine anteroposterior radiograph of posteriorly dislocated right SC joint. B.
The anteroposterior view is suggestive of a posterior dislocation. However, the CT scan clearly demonstrates the posteriorly displaced right medial clavicle. Note the displacement of the trachea. |
distinguishing between a SC dislocation and a fracture of the medial
clavicle. They are also helpful in questionable anterior and posterior
injuries of the SC joint to distinguish fractures from dislocations and
to evaluate arthritic changes.
recommended the use of tomography and said it was far more valuable
than routine radiographs and the fingertips of the examining physician.
In 1975, Morag and Shahin135
reported on the value of tomography, which they used in a series of 20
patients, and recommended that it be used routinely to evaluate
problems of the SC joint. From a study of normal SC joints, they
pointed out the variation in the x-ray appearance in different age
groups.
It clearly distinguishes injuries of the joint from fractures of the
medial clavicle and defines minor subluxations of the joint. One must
remember to request CT scans of both SC joints and the medial half of both clavicles
so the injured side can be compared with the normal side. Numerous
authors have reported on the value of using a CT scan as the method of
choice for radiographic evaluation of the SC joint.30,43,44,51,52,54,111,114,120 Lucet et al.120
used CT scans to evaluate the SC joints in 60 healthy subjects
homogeneously distributed by sex and decade of life from 20 to 80 years
old. They reported that 98% of the subjects had at least one sign of
various abnormalities, such as sclerosis, osteophytes, erosion, cysts,
and joint narrowing. The number of signs increased with age and the
number of clavicular signs was greater than those in the sternum.
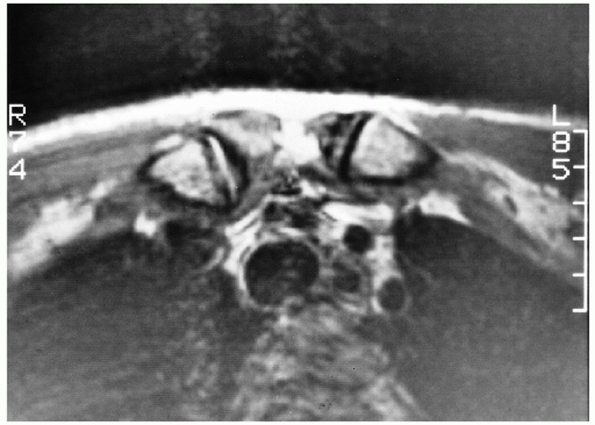
correlated magnetic resonance imaging (MRI) scans with anatomic
sections in 14 SC joints from elderly cadavers. They concluded that MRI
did depict the anatomy of the SC joint and surrounding soft tissues (Fig. 40-13).
T2-weighted images were superior to T1-weighted images in depicting the
intra-articular disk. Magnetic resonance arthrography allowed the
delineation of perforations in the intra-articular disk. In children
and young adults when there are questions of diagnosis between
dislocation and
SC
joint or physeal injury, the MRI scan can be used to determine if the
epiphysis has displaced with the clavicle or is still adjacent to the
manubrium. Benitez et al.15
evaluated 41 patients with SC trauma at an average of 9 months
postinjury and found an 80% incidence of articular disk injury and a
59% incidence of subluxation. MRI may be useful in this light to better
understand the in vivo mechanisms of injury of the SC joint and to
elucidate causes of pain well after the traumatic event.16
 |
|
FIGURE 40-13 MRI of the SC joint. The epiphysis on both medial clavicles is clearly visible.
|
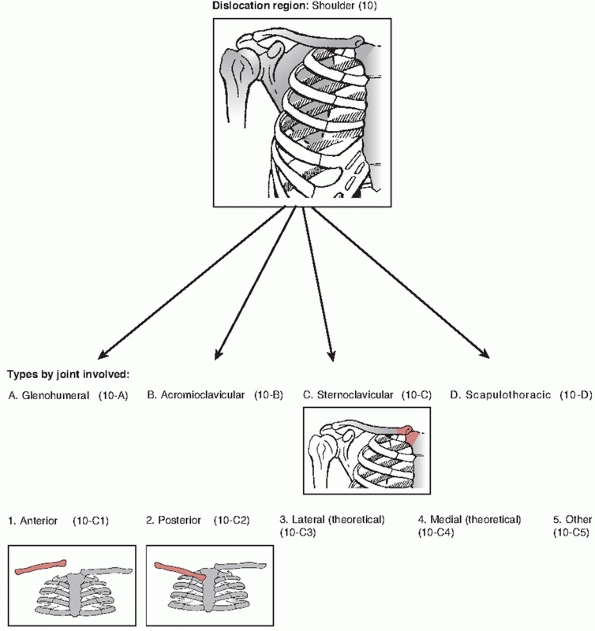
subluxations and dislocations: the anatomic position of the injury and
the etiology of the problem. The Orthopaedic Trauma Association
Classification is simply based on the direction of the dislocation and
not on etiology.
described. A recent case report confirms the possibility of a superior
dislocation which occurred after and indirect force mechanism. The
authors noted that only the interclavicular and intra-articular disc
ligaments were ruptured (Fig. 40-14).115
dislocations are the most common. The medial end of the clavicle is
displaced anteriorly or anterosuperiorly to the anterior margin of the
sternum.
uncommon. The medial end of the clavicle is displaced posteriorly or
posterosuperiorly with respect to the posterior margin of the sternum
(see Fig. 40-19A,B).
sprain, all the ligaments are intact and the joint is stable. There may
be local damage to the capsule and the joint may develop an effusion,
but there is no translation of the clavicle or loss of congruity.
In a moderate sprain, there is subluxation of the SC joint. The
capsular ligaments, the intra-articular disk, and costoclavicular
ligaments may be partially disrupted. The subluxation is usually
anterior but posterior subluxation can occur.
dislocated SC joint, the capsular and intra-articular ligaments are
ruptured. Occasionally, the costoclavicular ligament is intact but
stretched out enough to allow dislocation of the joint.
the initial acute traumatic dislocation does not heal, mild to moderate
forces may produce recurrent dislocations; this is rare.
original dislocation may go unrecognized, it may be irreducible, or the
physician may decide not to reduce certain dislocations.
It usually occurs in patients who have generalized ligament laxity of
other joints. In middle-aged women, spontaneous anterior or
anterior/superior subluxation can occur and may be in association with
condensing osteitis of the clavicle.191
In some patients, the atraumatic anterior dislocation of the SC joint
is painful and is associated with a snap or pop as the arm is elevated
overhead, and another snap occurs when the arm is returned to the
patient’s side. Atraumatic posterior dislocation126 and subluxation have been reported.127
important to consider other pathologies particular to the SC joint
during the diagnostic process. Infection may mimic trauma and should
especially be considered in patients with history of intravenous drug
abuse, immunocompromise, or indwelling subclavian catheters. SC
hyperostosis is an inflammatory condition of the SC joint and medial
ribs which results in new bone formation and even ankylosis of the SC
joint. It is associated with Japanese ethnicity and dermatologic
lesions in the palms and plantar regions. Three conditions which
predominate in women are condensing osteitis, Friedreich disease, and
osteoarthritis.201 Condensing
osteitis of the medial clavicle typically occurs in women of late
child-bearing age and presents as a painful joint with sclerosis on
radiographs, similar to condensing osteitis of the ilium and pubis seen
in the same demographic group. Friedreich’s disease is osteonecrosis of
the medial clavicle. Osteoarthritis typically manifests in the
postmenopausal years and can appear as a pseudosubluxation anteriorly.23
 |
|
FIGURE 40-14
Orthopaedic Trauma Association classification of SC injuries. (From Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium-2007: Orthopaedic Trauma Association classification, database, and outcomes committee. J Orthop Trauma. 2007;21(10 Suppl):S104-107, with permission.) |
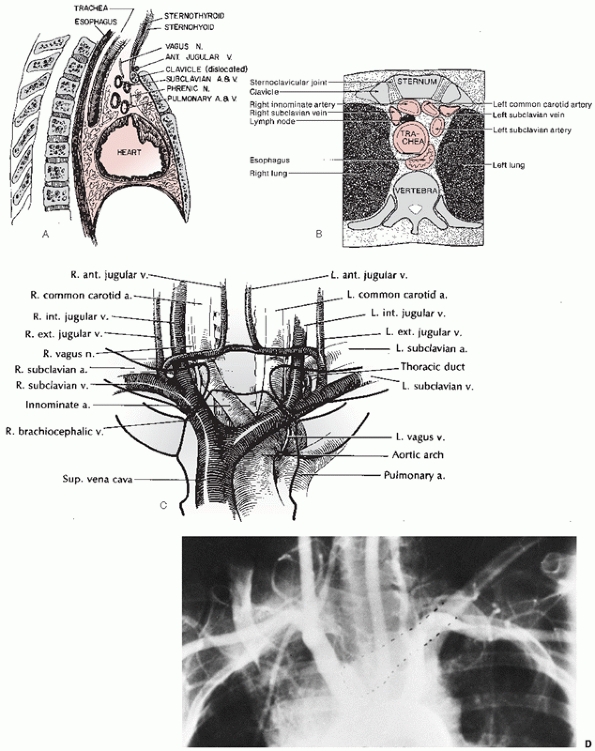
near the SC joint should be completely knowledgeable about the vast
array of anatomic structures immediately posterior to the SC joint.
There is a “curtain” of muscles (the sternohyoid, sternothyroid, and
scaleni) posterior to the SC joint and the inner third of the clavicle,
and this curtain blocks the view of the vital structures. Some of these
vital structures include the innominate artery, innominate vein, vagus
nerve, phrenic nerve, internal jugular vein, trachea, and esophagus (Fig. 40-16).
It is important to remember that the arch of the aorta, the superior
vena cava, and the right pulmonary artery are also very close to the SC
joint. Another structure to be aware of is the anterior jugular vein,
which is between the clavicle and the curtain of muscles.
true articulation between the upper extremity and the axial skeleton.
The articular surface of the clavicle is much larger than that of the
sternum, and both are covered with hyaline cartilage. The enlarged
bulbous medial end of the clavicle is concave front to back and convex
vertically and therefore creates a saddle-type joint with the
clavicular notch of the sternum.81,164 The clavicular notch of the sternum is curved, and the joint surfaces are not congruent. Cave37 demonstrated that in 2.5% of patients,
there is a small facet on the inferior aspect of the medial clavicle,
which articulates with the superior aspect of the first rib at its
synchondral junction with the sternum.
 |
|
FIGURE 40-15 Spontaneous anterior subluxation of the SC joint. A.
With the arm in the overhead position, the medial end of the right clavicle spontaneously subluxates anteriorly without any trauma. B. When the arm is brought back down to the side, the medial end of the clavicle spontaneously reduces. Usually this is not associated with significant discomfort. (From Rockwood CA, Matsen F III, eds. The Shoulder. Philadelphia: WB Saunders, 1990, with permission.) |
articulates with the upper angle of the sternum, the SC joint has the
distinction of having the least amount of bony stability of the major
joints of the body.
the SC joint has to come from its surrounding ligaments: the
intra-articular disk ligament, the extra-articular costoclavicular
ligament (rhomboid ligament), the capsular ligament, and the
interclavicular ligament.
ligament is a very dense, fibrous structure that arises from the
synchondral junction of the first rib and the sternum and passes
through the SC joint. It divides the joint into two separate spaces.81,164 The upper attachment is on the superior and posterior aspects of the medial clavicle. DePalma48
has shown that the disk is perforated only rarely; the perforation
allows a free communication between the two joint compartments.
Anteriorly and posteriorly, the disk blends into the fibers of the
capsular ligament. The disk acts as a checkrein against medial
displacement of the inner clavicle.
also called the rhomboid ligament, is short and strong and consists of
an anterior and a posterior fasciculus.14,36,81 Cave36 reported that the average length is 1.3 cm, the maximum width is 1.9 cm, and the average thickness is 1.3 cm. Bearn14
has shown that there is always a bursa between the two components of
the ligament. Because of the two different parts of the ligament, it
has a twisted appearance.81 The
costoclavicular ligament attaches below to the upper surface of the
first rib and at the adjacent part of its synchondral junction with the
sternum. It attaches above to the margins of the impression on the
inferior surface of the medial end of the clavicle, sometimes known as
the rhomboid fossa.81,164 Cave36
has shown, in a study of 153 clavicles, that the attachment point of
the costoclavicular ligament to the clavicle can be one of three types:
(i) a depression, the rhomboid fossa (30%), (ii) flat (60%), or (iii)
an elevation (10%).
anteromedial surface of the first rib and are directed upward and
laterally. The fibers of the posterior fasciculus are shorter and rise
lateral to the anterior fibers on the rib and are directed upward and
medially. The fibers of the anterior and posterior components cross and
allow for stability of the joint during rotation and elevation of the
clavicle. The two-part costoclavicular ligament is in many ways similar
to the two-part configuration of the coracoclavicular ligament on the
outer end of the clavicle.
experimentally that the anterior fibers resist excessive upward
rotation of the clavicle and that the posterior fibers resist excessive
downward rotation. Specifically, the anterior fibers also resist
lateral displacement, and the posterior fibers resist medial
displacement.
connects the superomedial aspects of each clavicle with the capsular
ligaments and the upper sternum. According to Grant,79
this band may be comparable to the wishbone of birds. This ligament
helps the capsular ligaments to produce “shoulder poise,” that is, to
hold up the shoulder. This can be tested by putting a finger in the
superior sternal notch; with elevation of the arm, the ligament is
quite lax, but as soon as both arms hang at the sides, the ligament
becomes tight.
have shown experimentally that the costoclavicular and interclavicular
ligaments have little effect on anterior or posterior translation of
the SC joint. In an anatomic study, Tubbs et al.189
found that the interclavicular ligament prevented superior displacement
of the clavicle with shoulder adduction and depression and failure
occurred at 53.7N.
anterosuperior and posterior aspects of the joint and represents
thickenings of the joint capsule. The anterior portion of the capsular
ligament is heavier and stronger than the posterior portion.
 |
|
FIGURE 40-16 Applied anatomy of the vital structures posterior to the SC joint. Sagittal (A) and transverse (B) views in cross section demonstrating the structures posterior to the SC joint. C. A diagram demonstrating the close proximity of the major vessels posterior to the SC joint. D. An aortogram showing the relationship of the medial end of the clavicle to the major vessels in the mediastinum.
|
this may be the strongest ligament of the SC joint, and it is the first
line of defense against the upward displacement of the inner clavicle
caused by a downward force on its distal end. The clavicular attachment
of the ligament is primarily onto the epiphysis of the medial clavicle,
with some secondary blending of the fibers into the metaphysis. The
senior author has demonstrated this, as have Poland,152 Denham and Dingley,47 and Brooks and Henning.25
Although some authors report that the intra-articular disk ligament
greatly assists the costoclavicular ligament in preventing upward
displacement of the medial clavicle, Bearn14
has shown that the capsular ligament is the most important structure in
preventing upward displacement of the medial clavicle. In experimental
postmortem studies, he determined, after
cutting
the costoclavicular, intra-articular disk, and interclavicular
ligaments, that they had no effect on clavicle poise. However, the
division of the capsular ligament alone resulted in a downward
depression on the distal end of the clavicle. Bearn’s14 findings have many clinical implications for the mechanisms of injury of the SC joint.
 |
|
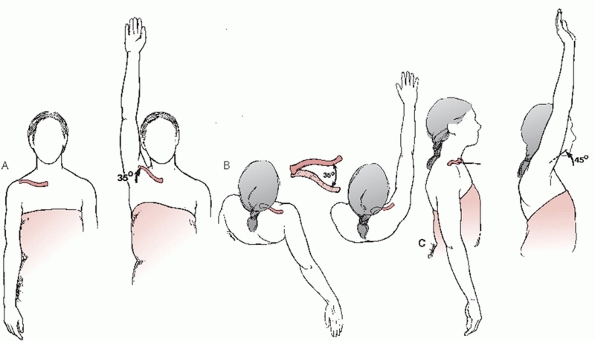
FIGURE 40-17 Motions of the clavicle at the SC joint. A. With full overhead elevation, the clavicle elevates 35 degrees. B. With adduction and extension, the clavicle displaces anteriorly and posteriorly 35 degrees. C. The clavicle rotates on its long axis 45 degrees, as the arm is elevated to the full overhead position.
|
measured anterior and posterior translation of the SC joint. Anterior
and posterior translation were measured in intact specimens and
following transection of randomly chosen ligaments about the SC joint.
Cutting the posterior capsule resulted in significant increases in
anterior and posterior translation. Cutting the anterior capsule
produced significant increases in anterior translation. This study
demonstrated that the posterior SC joint capsule is the most important
structure for preventing both anterior and posterior translation of the
SC joint, with the anterior capsule acting as an important secondary
stabilizer.
studied the function of the subclavius muscle and found that the basic
function of the subclavius was to stabilize the SC joint. They also
stated that the subclavius could act as a substitute for the ligaments
of the SC joint. We believe that this is an important study as it might
explain why some people, after loss of the medial clavicle and the SC
ligament, do not have instability of the medial end of the clavicle. It
also gives a reason for leaving the subclavius muscle intact during
operations on the SC joint.
a ball-and-socket joint with motion in almost all planes, including
rotation.19,119
In normal shoulder motion the clavicle, via motion through the SC
joint, is capable of 30 to 35 degrees of upward elevation, 35 degrees
of combined forward and backward movement, and 45 to 50 degrees of
rotation around its long axis (Fig. 40-17). It
is likely the most frequently moved joint of the long bones in the
body, because almost any motion of the upper extremity is transferred
proximally to the SC joint.
to ossify (during the fifth intrauterine week), the epiphysis at the
medial end of the clavicle is the last of the long bones in the body to
appear and the last physis to close (Fig. 40-18). The medial clavicular epiphysis does not ossify until the 18th to 20th year,
and it fuses with the shaft of the clavicle around the 23rd to 25th year.79,81,152 Webb and Suchey,198
in an extensive study of the physis of the medial clavicle in 605 males
and 254 females at autopsy, reported that complete union may not be
present until 31 years of age. This knowledge of the epiphysis is
important, because many of the SC dislocations in adults are injuries
through the physeal plate.
 |
|
FIGURE 40-18 CT scan demonstrating the thin, wafer-like disk of the epiphysis of the medial clavicle.
|
successfully managed by nonoperative measures (observation or closed
reduction). This includes most of the acute and chronic anterior
subluxations and dislocations, the acute traumatic posterior
subluxations and dislocations, and, remembering that the physis of the
medial clavicle does not close until the 23rd to 25th year, the acute
traumatic anterior and posterior physeal injuries of the medial
clavicle.
irreducible posterior dislocation that may require a surgical
procedure. Some authors also recommend the open reduction and internal
fixation of acute and chronic anterior dislocations.
Application of ice is recommended for the first 12 hours, followed by
heat for the next 24 to 48 hours. The joint may be subluxated
anteriorly or posteriorly, which may be reduced by drawing the
shoulders backward as if reducing and holding a fracture of the
clavicle. For both anterior and posterior subluxations that are stable,
a clavicle strap can be used to hold the reduction. A sling and swath
can also be used to hold up the shoulder and to prevent motion of the
arm. The patient should be protected from further injury for 4 to 6
weeks. Immobilization can be accomplished with a soft figure-of-eight
bandage with a sling for temporary support.
of acute anterior dislocation of the SC joint. A large series of SC
injuries was published in 1988 by Fery and Sommelet.67
They reported on 40 anterior dislocations, 8 posterior dislocations,
and 1 unstable SC joint. They ended up treating 15 injuries closed, but
because of problems, had to operate on 17 patients; 17 patients were
not treated. They had good and excellent results with both the closed
and operative treatment, but recommended that closed reduction should
be initially undertaken. In 1990, de Jong and Sukul46
reported long-term follow-up results in 10 patients with traumatic
anterior SC dislocations. All patients were treated nonoperatively with
analgesics and immobilization. The results of treatment were good in 7
patients, fair in 2 patients, and poor in 1 patient at an average
follow-up of 5 years. Most acute anterior dislocations are unstable
following reduction, and many operative procedures have been described
to repair or reconstruct the joint. At this time, the mixed results of
these procedures have not clearly advanced a case for their use instead
of observation.
dislocation of the SC joint may be accomplished with local or general
anesthesia or, in stoic patients, without anesthesia. Most authors
recommend the use of narcotics or muscle relaxants. The patient is
placed supine on the table, lying on a 3- to 4-inch-thick pad placed
between the shoulders. In this position, the joint may reduce with
direct gentle pressure over the anteriorly displaced clavicle. However,
when the pressure is released, the clavicle usually dislocates again.
Occasionally, the clavicle will remain reduced. Sometimes, the
physician will need to push both of the patient’s shoulders back to the
table while an assistant applies pressure to the anteriorly displaced
clavicle.
healing, the shoulders should be held back for 4 to 6 weeks with a
figure-of-eight dressing or one of the commercially available
figure-of-eight straps used to treat fractures of the clavicle.
of anterior dislocations of the SC joint, we believe that the operative
complications are too great and the end results are too unsatisfactory
to consider an open procedure.
patient complains of moderate discomfort. The joint may be swollen and
tender to palpation. Care must be taken to rule out the more
significant posterior dislocation, which may have initially occurred
and spontaneously reduced. When in doubt, it is best to protect the SC
joint with a figure-of-eight bandage for 2 to 6 weeks. As with all
injuries to the SC joint, it must be carefully evaluated by CT scan.
the SC joint is suspected, the physician must perform a very careful
examination of the patient to rule out damage to the structures
posterior to the joint such as the trachea, esophagus, the brachial
plexus, the great vessels, and the lungs. Not only is a careful
physical examination important, but special radiographs must be
obtained. A CT scan of both medial clavicles allows the physician to
compare the injured side with the normal side, and this is the
recommended imaging study. Occasionally, when vascular injuries are
suspected, the CT scan will need to be combined with an arteriogram of
the great vessels.
whom many if not most of the injuries are physeal fractures, a
nonoperative approach of closed reduction should be strongly considered.
a posterior dislocation of the SC joint because the patient has pain
and muscle spasms. However, for the stoic patient, some authors have
performed the reduction under intravenous narcotics and muscle
relaxants.
that the treatment of choice for posterior SC dislocation was
operative. However, since the 1950s, the treatment of choice has been
closed reduction.33,40,44,65,83,86,129,130,134,148,169,181
dislocations are successfully reduced closed if accomplished within 48
hours of injury. A variety of techniques have been described.
the patient is placed on his or her back with the dislocated shoulder
near the edge of the table. A 3- to 4-inch-thick sandbag is placed
between the shoulders (Fig. 40-19). Lateral
traction is applied to the abducted arm, which is then gradually
brought back into extension. This may be all that is necessary to
accomplish the reduction. The clavicle usually reduces with an audible
snap or pop, and it is almost always stable. Too much extension can
bind the anterior surface of the dislocated medial clavicle on the back
of the manubrium. Occasionally, it may be necessary to grasp the medial
clavicle with one’s fingers to dislodge it from behind the sternum. If
this fails, the skin is prepared, and a sterile towel clip is used to
grasp the medial clavicle to apply lateral and anterior traction (Fig. 40-20).
 |
|
FIGURE 40-19 Technique for closed reduction of the SC joint. A.
The patient is positioned supine with a sandbag placed between the two shoulders. Traction is then applied to the arm against countertraction in an abducted and slightly extended position. In anterior dislocations, direct pressure over the medial end of the clavicle may reduce the joint. B. In addition to the traction, it may be necessary to manipulate the medial end of the clavicle with the fingers to dislodge the clavicle from behind the manubrium. C. In stubborn posterior dislocations, it may be necessary to sterilely prepare the medial end of the clavicle and use a towel clip to grasp around the medial clavicle to lift it back into position. |
the patient is supine on the table with a 3- to 4-inch bolster between
the shoulders. Traction is then applied to the arm in adduction, while
a downward pressure is exerted on the shoulder (Fig. 40-21). The clavicle is levered over the first rib into its normal position. Buckerfield and Castle29 reported that this technique was successful in 7 patients when the abduction traction technique had failed.
 |
|
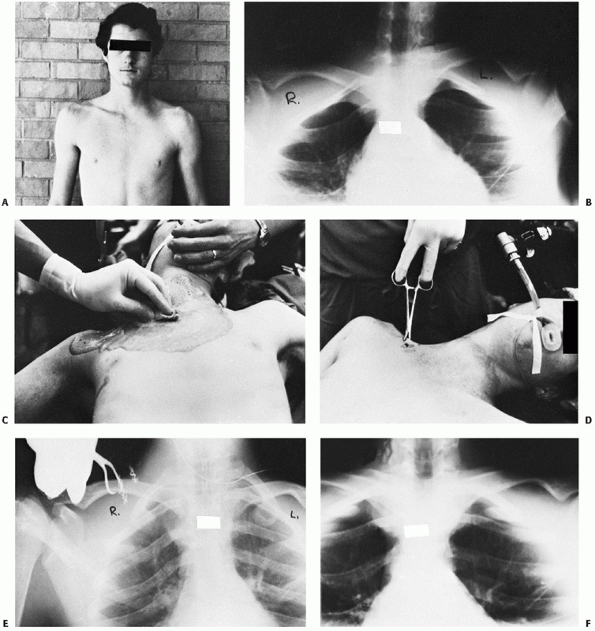
FIGURE 40-20 Posterior dislocation of the right SC joint. A.
A 16-year-old boy has a 48-hour-old posterior dislocation of the right medial clavicle that occurred from a direct blow to the anterior right clavicle. He noted immediate onset of difficulty in swallowing and some hoarseness in his voice. B. A 40-degree cephalic tilt radiograph confirmed the posterior displacement of the right medial clavicle as compared with the left clavicle. Because of the patient’s age, this was considered most likely to be a physeal injury of the right medial clavicle. C. Because the injury was 48 hours old, we were unable to reduce the dislocation with simple traction on the arm. The right shoulder was surgically cleansed so that a sterile towel clip could be used. D. With the towel clip placed securely around the clavicle and with continued lateral traction, a visible and audible reduction occurred. E. Postreduction radiographs showed that the medial clavicle had been restored to its normal position. The reduction was quite stable, and the patient’s shoulders were held back with a figure-of-eight strap. F. The right clavicle has remained reduced. Note the periosteal new bone formation along the superior and inferior borders of the right clavicle. This is the result of a physeal injury, whereby the epiphysis remains adjacent to the manubrium while the clavicle is displaced out of a split in the periosteal tube. |
 |
|
FIGURE 40-21 The Buckerfield-Castle technique. A,B.
The patient is lying on the table with a bolster between the shoulders. Traction is applied to the arm in adduction while a downward force is applied on the shoulder. |
healing, the shoulders should be held back for 4 to 6 weeks with a
figure-of-eight dressing or one of the commercially available
figure-of-eight straps used to treat fractures of the clavicle.
maintaining stability of the posterior dislocation of the SC joint. A
delay in reduction of 48 hours may make closed reduction impossible,
reinforcing the importance of early diagnosis.35
In these situations, open reduction and acute repair of the soft
tissues is warranted. The first option is direct repair of the anterior
and posterior capsule, intra-articular disk ligament, and
costoclavicular ligament. The surgeon can also employ one of the
various techniques that are available for ligament reconstruction for
an unreduced or chronic dislocation, especially if additional stability
is required due to the disruption of native tissues.
reconstructed, but do not generally require such procedures.
Occasionally, following conservative treatment of a subluxation of the
SC joint, the pain lingers on and the symptoms of popping and grating
persist. Joint exploration may be required as several authors have
reported symptom relief following joint exploration, removal of the
torn or degenerated intra-articular disk, along with a capsulorraphy.6,12,55
Many authors have included chronic or unreduced anterior dislocations
with posterior dislocations in their series of operative patients. This
makes it difficult to understand the true benefits of surgery in this
situation. Postoperatively, recurrent instability,67 limitations of activity,7 and pain61
often occur, and patient expectations should be adjusted accordingly.
While most chronic posterior SC fracture-dislocations require open
procedures, a singular exception is young adults who may have no
symptoms, and the physician can wait to see if the physeal plate
remodeling process removes the posteriorly displaced bone.163
displacement of the medial clavicle in the adult, an operative
procedure should be performed, because most adult patients cannot
tolerate posterior displacement of the clavicle into the mediastinum.
Complications accompanying unreduced posterior dislocations include
late thoracic outlet syndrome, late and significant vascular problems,
respiratory compromise, and dyspnea on exertion.24,73,117,186
We have treated patients with a medial clavicle resection and
reconstruction who have had complaints of swelling and arm
discoloration, in addition to signs and symptoms of effort thrombosis
and dysphagia secondary to a posteriorly displaced medial clavicle.
from the pressure of the posteriorly displaced clavicle into the
mediastinum and closed reduction is unsuccessful, an operative
procedure should be performed. If the patient is under 25 and without
symptoms after the initial obligatory attempt at closed reduction, then
close observation is acceptable as remodeling potential still exists.
Much like the AC joint, the recent literature has focused on case
reports of technique descriptions and modifications of existing
surgeries. Given the rarity of the injury and even rarer necessity for
surgery, there is no large experience with any of the techniques.
Nonetheless, certain basic principles should be adhered to in the midst
of this creative atmosphere.
that disturbs as few of the anterior ligament structures as possible.
If the procedure can be performed with the anterior ligaments intact,
then, with the shoulders held back in a figure-of-eight dressing, the
reduction may be stable. If all the ligaments are disrupted, a decision
has to be made whether to try to stabilize the SC joint or to resect
the medial 1 to 1.5 inches of the medial clavicle and anatomically
stabilize the remaining clavicle to the first rib. Resection alone
cannot be performed in the setting of disrupted ligaments and may
worsen the instability of the residual medial clavicle, requiring even
greater attention to the need for ligament reconstruction in such a
scenario.17
has to embrace a surgical strategy from the existing armamentarium.
Procedures can be viewed from two different perspectives: tissue and
stabilization. With regards to tissue, options are: (a) local ligaments
and capsule, (b) tendon transfers (subclavius or sternocleidomastoid),
or (c) grafts. With regards to stabilization, options are: (a)
stabilize to first rib, (b) stabilize to manubrium, or (c) stabilize to
the first rib and the manubrium. Fixation is generally provided by soft
tissue tensioning and suture, although augmenting with pins, plates, or
screws have all been proposed.
(i) intramedullary ligament transfer, (ii) costoclavicular ligament
reconstruction, and (iii) SC ligament reconstruction. Spencer and Kuhn,179
through a biomechanic analysis, evaluated the three different
reconstruction techniques in a cadaver model. The intramedullary
ligament,164 the
subclavius tendon transfer,32
and a semitendinosus graft placed in a figure-of-eight fashion through
drill-holes in the clavicle and manubrium were used to reconstruct the
SC joint. Each of the three reconstruction methods was subjected to
anterior or posterior translation to failure, and the changes in
stiffness compared with the intact state were analyzed statistically.
The figure-of-eight semitendinosus reconstruction showed superior
initial mechanical properties to the other two techniques. The authors
believed that this method reconstructs both the anterior and posterior
joint capsules providing an initial stiffness that is closer to that of
the intact sternoclavicular joint (Figs. 40-22 and 40-23). This technique has now been described with some success in young adults with refractory anterior instability.7,34,157
A plethora of other techniques abound in the literature. Some of the
literature from the 1960s and 1970s recommended stabilization of the SC
joint with Kirschner wires (K-wires) or Steinmann pins.25,28,47,49,59
These techniques have become largely historical due to their high
complication rate as will be discussed later. Other authors recommended
the use of various types of suture wires across the joint,9,31,70,84,98,142,151,156,181,182 reconstruction using local tendons,10,19,122,124 or the use of a special plate.85
Fascia lata, suture, screw fixation across the joint, subclavius
tendons, osteotomy of the medial clavicle, and resection of the medial
end of the clavicle have also been advocated.2,9,10,27,32,81,102,118,122,133,143,164,177
|
TABLE 40-1 Surgical Techniques for Sternoclavicular Reconstruction
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
used the clavicular head of the sternocleidomastoid as an anterior
sling across the SC joint augmented with pins. Armstrong et al.5
modified the use of the sternocleidomastoid by using only a slip of the
sternal head and passing it through a medial clavicle bone tunnel. The
graft is sutured to itself to recreate the anterior SC ligament without exposure of the first rib.
 |
|
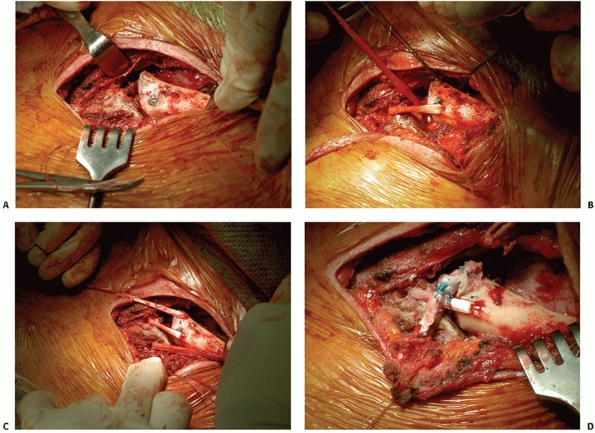
FIGURE 40-22 Semitendinosus figure-of-eight reconstruction. A. Drill holes are passed from anterior to posterior through the medial part of the clavicle and the manubrium. B.
A free semitendinosus tendon graft is woven through the drill holes such that the tendon strands are parallel to each other posterior to the joint and cross each other anterior to the joint. C. The tendon ends are tied in a square knot and secured with suture. (From Spencer EE, Kuhn JE. Biomechanical analysis of reconstructions for sternoclavicular joint instability. J Bone Joint Surg 2004;86A(1):98-105.) |
 |
|
FIGURE 40-23 Semitendinous figure-of-eight reconstruction A. Reduction of the SC joint. B. Passing the tendon graft through bone tunnels with suture passer. C. Tensioning of the graft. D. Completed figure-of-eight construct. (Courtesy of Charles E. Rosipal, MD, and T. Kevin O’Malley, MD.)
|
reported a safe surgical technique for stabilization of the SC joint
with the use of suture material. Their technique involved tying the
suture material on the superficial aspects of the medial clavicle and
manubrium. This avoids the exposure of the first rib and avoids
drilling through the inner cortex of the clavicle and manubrium.
Recently Abiddin1 has described a
similar technique with the use of suture anchors in the manubrium and
drill holes in the clavicle. While smooth pin and wire fixation is now
taboo, fixation of the SC joint with other metal implants is still
considered a valid option, although the implants do require removal.
Franck et al.69 reported an
alternative therapy for traumatic SC instability using a plate for
stabilization. A Balser plate was contoured to match the shape of the
clavicle and the hook of the plate was used for sternal fixation. A
retrosternal hook position was used for seven anterior dislocations and
an intrasternal position was used for three posterior dislocations. For
each patient, the plate was attached to the clavicle with screws and
the torn ligaments were repaired. All plates were removed by 3 months.
At 1-year follow-up, 9 of 10 patients had excellent results with no
cases of redislocation. One patient developed a postoperative seroma
that required surgical drainage, and one patient developed arthrosis (Fig 40-24). In 1997, Brinker et al.24
described another technique of hardware fixation across the joint. The
authors used two 75-mm cannulated screws to stabilize an unstable
posterior dislocation of the SC joint. The screws were removed at 3
months, and at 10 months the patient had full range of motion without
pain and returned to college level football.
presented three cases of an Achilles tendon allograft and bone plug
used to treat anterior instability in 2 patients and a medial clavicle
fracture nonunion in one. The graft was fixed to a trough in the medial
clavicle resection with screws, passed through bone tunnels in the
manubrium and sutured upon itself.23 Meis et al.132
reported using an intramedullary transfer of the sternocleidomastoid as
an interposition for degenerative SC joint pain after resection.
reduction and internal fixation for acute injuries, as well as for
chronic problems. In 1982, Pfister and associates150,151 recommended open reduction and repair of the ligaments over nonoperative treatment. In 1988, Fery and Sommelet67 reported 49 cases of dislocations of the SC joint. In these patients, if closed reduction
was not successful, they performed open reduction. In symptomatic
chronic unreduced dislocations, they either performed a myoplasty or
excised the medial end of the clavicle if the articular surfaces were
damaged. They were able to follow 55% of their patients for an average
of more than 6 years. They had 42% excellent results among the
operative cases. Of those patients who were treated with closed
reduction, 58% were satisfied. Ferrandez and colleagues64
reported 18 subluxations and dislocations of the SC joint. Seven had
moderate sprains and 11 had dislocations. Of the 3 patients with a
posterior dislocation, all had symptoms of dysphagia. All of the
subluxations were treated nonoperatively with excellent results. The
remaining 10 patients with dislocations were treated with surgery
(i.e., open reduction with suture of the ligaments and K-wires placed
across the clavicle and the sternum). The wires were removed 3 to 4
weeks following surgery. At 1- to 4-years follow-up, most of the
operative cases had a slight deformity. In 2 patients, migration of the
K-wires was noted but was without clinical significance.
 |
|
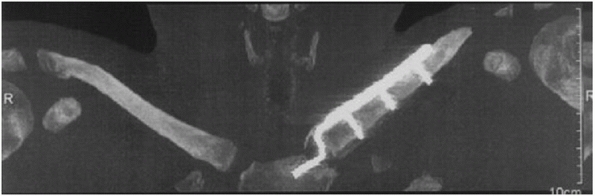
FIGURE 40-24
CT scan of manubrium showing intrasternal plate insertion. (From Franck WM, Jannasch O, Siassi M, et al. Balser plate stabilization: an alternate therapy for traumatic sternoclavicular instability. J Shoulder Elbow Surg 2003;12(3):276-281.) |
strongly urged operative repair of dislocations of the SC joint. In
1989, they reported on 12 patients treated for painful SC joints. The
average time from injury was 1.5 years, and the average follow-up after
surgery was 4.7 years. In 5 patients, the SC joint was stabilized with
a palmaris longus or plantaris tendon graft placed between the first
rib and the manubrium; in 4 patients, the medial 2.5 cm of the clavicle
was resected without any type of stabilization; and in 3 patients, the
clavicle was fixed to the first rib with a fascia lata graft. They
reported good results in four patients, three treated with tendon
grafts and one with a fascia lata graft. They had four fair results and
four poor results in those patients who had only resection of the
medial clavicle. There was little discussion of the patients’
preoperative symptoms, work habits, or range of motion, or the degree
of joint reduction following the surgery. In 1990, Tricoire and
colleagues186 reported six
retrosternal dislocations of the medial end of the clavicle. They
recommended reduction of these injuries to avoid the possible
complications arising from protrusion of the clavicle into the
mediastinum. SC capsulorrhaphy was performed in 2 patients and a
subclavius tenodesis was used in the remaining 4 patients. All joints
were temporarily stabilized with SC pins for 6 weeks. Results were
satisfactory in all cases at a mean follow-up of 27 months.
have all recommended excision of the medial clavicle when degenerative
changes are noted in the joint. If the medial end of the clavicle is to
be removed because of degenerative changes, the surgeon should be
careful not to damage the costoclavicular ligament (Fig. 40-25).
recommended a safe resection length that would result in no or minimal
disruption of the costoclavicular ligament of 1.0 cm in men, and 0.9 cm
in women.
be done because it prevents the previously described normal elevation,
depression, and rotation of the clavicle. The end result would be a
severe restriction of shoulder movement (Fig. 40-26).
figure-of-eight bandage for 4 to 6 weeks. When K-wires or Steinmann
pins are used, the patient should avoid vigorous activities until the
pins are removed. The pins should be carefully monitored with
radiographs until they are removed.
are not dislocations but physeal injuries. Most of these injuries will
heal without surgical intervention. In time, the remodeling process
eliminates
any bone deformity or displacement. Anterior physeal injuries can
certainly be left alone without problem. Posterior physeal injuries
should be reduced. If the posterior dislocation cannot be reduced by
closed means and the patient is having no significant symptoms, the displacement can be observed while remodeling occurs (Fig. 40-27).
It is only in this regard that posterior physeal injuries differ from
posterior SC dislocations in adults. If the posterior displacement is
symptomatic and cannot be reduced closed, the displacement must be
reduced surgically as is required for posterior SC dislocations in
adults (Fig. 40-28).
 |
|
FIGURE 40-25 Resection of the medial end of the clavicle, retaining the costoclavicular ligament.
|
 |
|
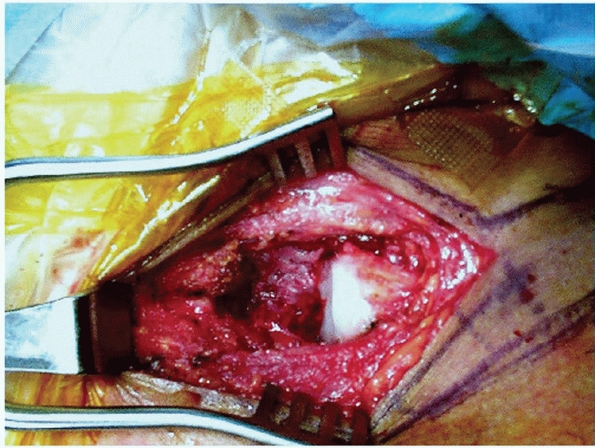
FIGURE 40-26 The effect of an arthrodesis of the SC joint on shoulder function. A.
As a result of a military gunshot wound to the left SC joint, this patient had a massive bony union of the left medial clavicle to the sternum and the upper three ribs. B. Shoulder motion was limited to 90-degrees of flexion and abduction. C. Radiograph after resection of the bony mass and freeing up the medial clavicle. D. The motion of the left shoulder was essentially normal after the elimination of the SC arthrodesis. |
 |
|
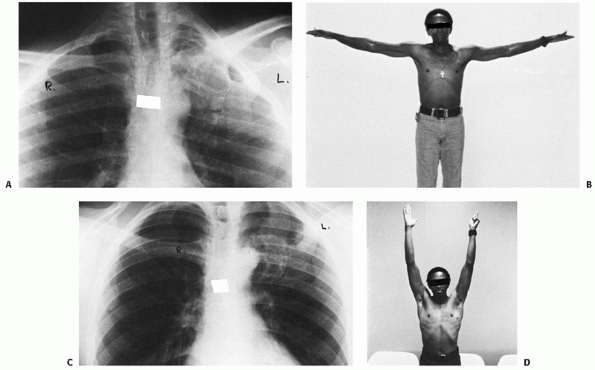
FIGURE 40-27 A 17-year-old man with a posterior SC physeal injury. A.
The initial injury CT scan displays a physeal fracture-dislocation. The patient had no symptoms of mediastinal compression and was treated with observation after initial attempts at closed reduction were unsuccessful. B. Six months after injury, the CT scan shows healing with remodeling and a reduced SC joint. The patient remained asymptomatic and returned to normal activities. |
is significant and may extend until the 23rd to 25th year. The senior author162
has demonstrated a similar mechanism to support conservative treatment
of adolescent AC joint injuries or “pseudodislocations,” in which there
is a partial tear of the periosteal tube containing the distal
clavicle. The coracoclavicular ligaments remain secured to the
periosteal tube. Because of its high osteogenic potential, spontaneous
healing and remodeling to the preinjury “reduced” position occur within
this periosteal conduit. Waters et al.197
reported successful operative treatment of 13 traumatic posterior SC
fracture-dislocations in children and adolescents, and other authors
have reported the successful treatment of posteriorly displaced medial
clavicle physeal injuries in adolescents.91,206,207
 |
|
FIGURE 40-28
CT scan of a 19-year-old patient who was involved in a motor vehicle accident and presented with complaints of chest pain and a “choking sensation” that was exacerbated by lying supine. Note the physeal injury of the medial clavicle and compression of the trachea. |
patient is younger than 25 years, closed reduction, as described for
anterior dislocation of the SC joint, should be performed. The
shoulders should be held back in a clavicular strap or figure-of-eight
dressing for 3 to 4 weeks, even if the reduction is stable. Healing is
prompt, and remodeling will occur at the site of the deformity.
medial clavicle should be performed in the manner described for
posterior dislocation of the SC joint. The reduction is usually stable
with the shoulders held back in a figure-of-eight dressing or strap.
Immobilization should continue for 3 to 4 weeks. If the posterior
physeal injury cannot be reduced, the patient is not having symptoms,
and the patient is younger than 23 years, the physician can wait to see
if remodeling eliminates the posterior displacement of the clavicle.
instability, the importance of distinguishing between traumatic and
atraumatic instability of the SC joint must be recognized if
complications are to be avoided. C. R. Rowe (personal communication,
1988) described several patients who had undergone one or more
unsuccessful attempts to stabilize the SC joint. In all cases, the
patient was able to voluntarily dislocate the clavicle after surgery.
Rockwood and Odor’s165 study of 29
patients with spontaneous subluxation treated nonoperatively with no
failures further reflects the appeal of avoiding surgery in this
population.
reported a case of spontaneous atraumatic anterior dislocation
secondary to pseudoarthrosis of the first and second ribs. Despite a
6-month course of conservative treatment, this 14-year-old girl was
still painful. A CT scan of the chest with three-dimensional
reconstruction was performed. The scan revealed a pseudoarthrosis
anteriorly between the first and second ribs underlying the medial part
of the clavicle. Resection of the anterior portions of the first and
second ribs containing the pseudoarthrosis relieved her symptoms and
allowed the patient to return to her normal activities. The authors
recommended chest radiographs and a possible CT scan with
three-dimensional reconstruction to completely evaluate an underlying
congenital condition if the subluxation is rigid and unresponsive to
nonoperative care.
described a case of spontaneous atraumatic posterior dislocation of the
SC joint. This occurred in a 50-year-old previously healthy woman who
awoke one morning with a painful SC joint. A CT scan confirmed the
posterior dislocation. She later developed dysphagia, and a closed
reduction was unsuccessful. At 1 year without any other treatment, she
was back to playing golf and was asymptomatic. More recently, Martinez
et al.127 reported on the operative
treatment of a 19-year-old woman with a symptomatic spontaneous
posterior subluxation. The posteriorly displaced medial clavicle was
stabilized with a figure-of-eight suture technique with the use of a
gracilis autograft. At follow-up the patient was pain free; however, a
repeat CT scan demonstrated posterior subluxation of the medial
clavicle with erosion of the clavicle and manubrium. In light of the
recurrence of subluxation after reconstruction, the authors recommended
conservative treatment of atraumatic posterior subluxation of the SC
joint.
cold packs for the first 12 to 24 hours and a sling to rest the joint.
Ordinarily, after 5 to 7 days, the patient can use the arm for everyday
activities.
use a soft, padded figure-of-eight clavicle strap to gently hold the
shoulders back to allow the SC joint to rest. The harness can be
removed after a week or so. Then the arm is placed in a sling for about
another week, or the patient is allowed to return gradually to everyday
activities.
of the SC joint in adults by either a closed reduction or by “skillful
neglect.” Most of the anterior dislocations are unstable, but we accept
the deformity since we believe it is less of a problem than the
potential problems of operative repair and internal fixation.
instances, even knowing that the anterior dislocation will be unstable,
we still try to reduce the anterior displacement. Muscle relaxants and
narcotics are administered intravenously, and the patient is placed
supine on a table with a stack of three or four towels between the
shoulder blades. While an assistant gently applies downward pressure on
the anterior aspect of both of the patient’s shoulders, the medial end
of the clavicle is pushed backward where it belongs. On some occasions,
rare as they may be, the medial clavicle may stay adjacent to the
sternum. However, in most cases, either with the shoulders still held
back or when they are relaxed, the anterior displacement promptly
recurs. We explain to the patient that the joint is unstable and that
the hazards of internal fixation are too great, and we prescribe a
sling for a couple of weeks and allow the patient to begin using the
arm as soon as the discomfort is gone.
patients up to 25 years of age are not dislocations of the SC joint.
Rather, they are type I or II physeal injuries, which heal and remodel
without operative treatment. Patients older than 25 years with anterior
dislocations of the SC joint do have persistent prominence of the
anterior clavicle. However, this does not seem to interfere with usual
activities and, in some cases, has not even interfered with heavy
manual labor.
reduction is stable, we place the patient in either a figure-of-eight
dressing or in whatever device or position the clavicle is most stable.
If the reduction is unstable, the arm is placed into a sling for a week
or so, and then the patient can begin to use the arm for gentle
everyday activities.
and perform a careful physical examination in the patient with a
posterior SC dislocation (Table 40-2). For
every patient, the physician should obtain radiographs and/or a CT
scan. If the patient has distention of the neck vessels, swelling of
the arm, a bluish discoloration of the arm, or difficulty swallowing or
breathing, then the patient should be evaluated by using a CT scan with
contrast of the vascular structures. It is also important to determine
if the patient has a feeling of choking or hoarseness. If any of these
symptoms are present, indicating pressure on the mediastinal
structures, the appropriate cardiovascular or thoracic specialist
should be consulted.
|
TABLE 40-2 Keys to the Diagnosis of Posterior Sternoclavicular Dislocation
|
|
|---|---|
|
required to reduce acute posterior SC joint dislocations. Furthermore,
once the joint has been reduced by closed means, it is usually stable.
anterior or posterior injury of the SC joint could always be made on
physical examination, one cannot rely on the anterior swelling and
firmness as being diagnostic of an anterior injury as the posterior
injuries may create a significant anterior fullness. Therefore, we
recommend that the clinical impression always be documented with
appropriate imaging studies, preferably a CT scan, before a decision to
treat or not to treat is made.
The patient is placed in the supine position with a 3- to 4-inch-thick
sandbag or three to four folded towels placed between the scapulas to
extend the shoulders. The dislocated shoulder should be near the edge
of the table so that the arm and shoulder can be abducted and extended.
If the patient is having extreme pain and muscle spasm and is quite
anxious, we use general anesthesia; otherwise, narcotics, muscle
relaxants, or tranquilizers are given through an established
intravenous route in the normal arm. First, gentle traction is applied
on the abducted arm in line with the clavicle while countertraction is
applied by an assistant who steadies the patient on the table. The
traction on the abducted arm is gradually increased while the arm is
brought into extension (see Fig. 40-19). If
reduction cannot be accomplished with the patient’s arm in abduction,
then we will use the adduction technique of Buckerfield and Castle29 that is described above (see Fig. 40-21).
pop or snap and the relocation can be noted visibly and by palpation.
If the traction techniques are not successful, an assistant grasps or
pushes down on the clavicle in an effort to dislodge it from behind the
sternum. Occasionally, in a stubborn case, especially in a
thick-chested person or a patient with extensive swelling, it is
impossible to obtain a secure grasp on the clavicle with the fingers
alone. The skin should then be surgically prepared and a sterile towel
clip used to gain purchase on the medial clavicle percutaneously (see Fig. 40-20).
The towel clip should encircle the shaft of the clavicle as the dense
cortical bone prevents the purchase of the towel clip into the
clavicle. Then the combined traction through the arm plus the anterior
lifting force on the towel clip will reduce the dislocation. Following
the reduction, the SC joint is usually stable, even with the patient’s
arms at the side. However, we always hold the shoulders back in a
wellpadded figure-of-eight clavicle strap for 3 to 4 weeks to allow for
soft tissue and ligamentous healing.
and erosion of the medial clavicle into any of the vital structures
that lie posterior to the SC joint. Therefore, in adults over the age
of 23, if closed reduction fails, an open reduction should be
performed. It is critical that a thoracic surgeon is immediately
available when the patient is taken to the operating room to intervene
if needed.
evaluate the residual stability of the medial clavicle. It is the same
analogy as used when resecting the distal clavicle for an old AC joint
problem. If the coracoclavicular ligaments are intact, an excision of
the distal clavicle is indicated. If the coracoclavicular ligaments are
gone, then, in addition to excision of the distal clavicle, one must
reconstruct the coracoclavicular ligaments with a SC injury. If the
costoclavicular ligaments are intact, the clavicle medial to the
ligaments should be resected and beveled smooth. If the ligaments are
torn, the clavicle must be stabilized to the first rib. If too much
clavicle is resected, or if the clavicle is not stabilized to the first
rib, an increase in symptoms can result (Fig. 40-29).
four towels or a sandbag should be placed between the scapulae. The
upper extremity should be draped out free so that lateral traction can
be applied during the open reduction. In addition, a folded sheet
around the patient’s thorax should be left in place so that it can be
used for countertraction when traction is applied to the involved
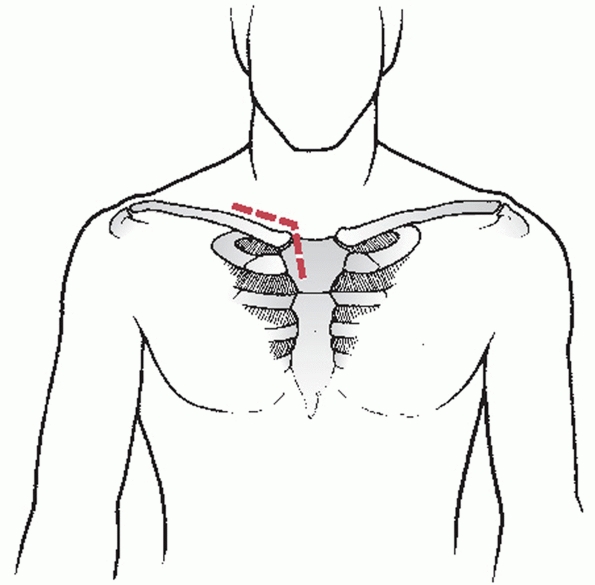
extremity. An anterior incision is used that parallels the superior
border of the medial 3 to 4 inches of the clavicle and then extends
downward over the sternum just medial to the involved SC joint (Fig. 40-30).
The trick is to try to remove sufficient soft tissues to expose the
joint but to leave the anterior capsular ligament intact. The reduction
can usually be accomplished with traction and countertraction while
lifting up anteriorly on a clamp placed around the medial clavicle.
Along with the traction and countertraction, it may be necessary to use
an elevator to pry the clavicle back to its articulation with the
manubrium.
 |
|
FIGURE 40-29
This postmenopausal, right-handed woman had a resection of the right medial clavicle because of a preoperative diagnosis of “possible tumor.” The postoperative microscopic diagnosis was degenerative arthritis of the right medial clavicle. After surgery, the patient complained of pain and discomfort, marked prominence, and gross instability of the right medial clavicle. |
 |
|
FIGURE 40-30 The proposed skin incision used for open reduction of a posterior SC dislocation.
|
held back, the reduction will be stable if the anterior capsule has
been left intact. If the anterior capsule is damaged or is insufficient
to prevent anterior displacement of the medial end of the clavicle, we
recommend excision of the medial 1 to 1.5 inches of the clavicle and
securing the residual clavicle anatomically to the first rib with 1-mm
polyester fiber tape. The medial clavicle is exposed by careful
subperiosteal dissection (Fig. 40-31). When
possible, any remnant of the capsular or intra-articular disk ligaments
should be identified and preserved as these structures can be used to
help stabilize the medial clavicle. The capsular ligament covers the
anterosuperior and posterior aspects of the joint and represents
thickenings
of the joint capsule. This ligament is primarily attached to the
epiphysis of the medial clavicle and is usually avulsed from this
structure with posterior SC dislocations. The intra-articular disk
ligament is a very dense, fibrous structure and may be intact. It
arises from the synchondral junction of the first rib and sternum and
is usually avulsed from its attachment site on the medial clavicle. If
the sternal attachment sites of the intra-articular or capsular
ligaments are intact, a nonabsorbable no. 1 cottony polyester fiber
suture is woven back and forth through the ligament so that the ends of
the suture exit through the avulsed free end of the tissue. The medial
1- to 1.5-inch end of the clavicle is resected, being careful to
protect the underlying vascular structures, and being careful not to
damage any of the residual costoclavicular (rhomboid) ligament. The
vital vascular structures are protected by passing a curved Crego
elevator or ribbon retractor around the posterior aspect of the medial
clavicle to isolate them from the operative field during the bony
resection.
 |
|
FIGURE 40-31 Subperiosteal exposure of the medial clavicle. Note the posteriorly displaced medial end of the clavicle.
|
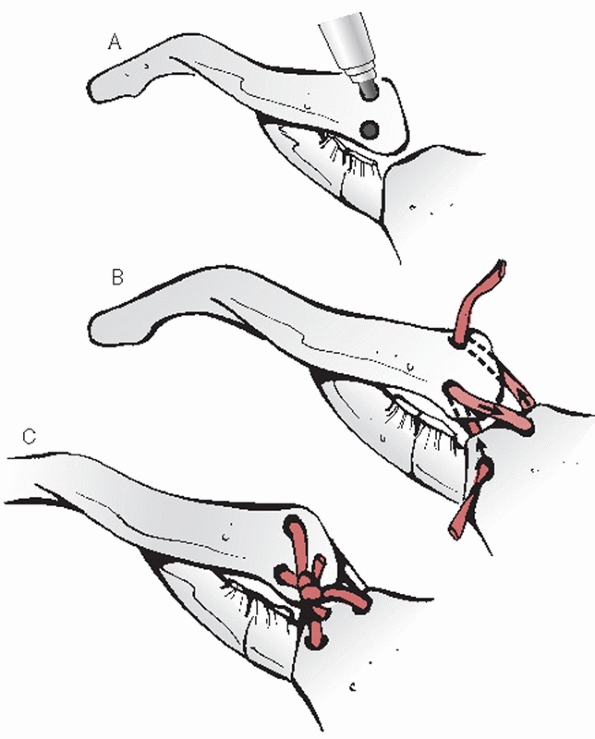
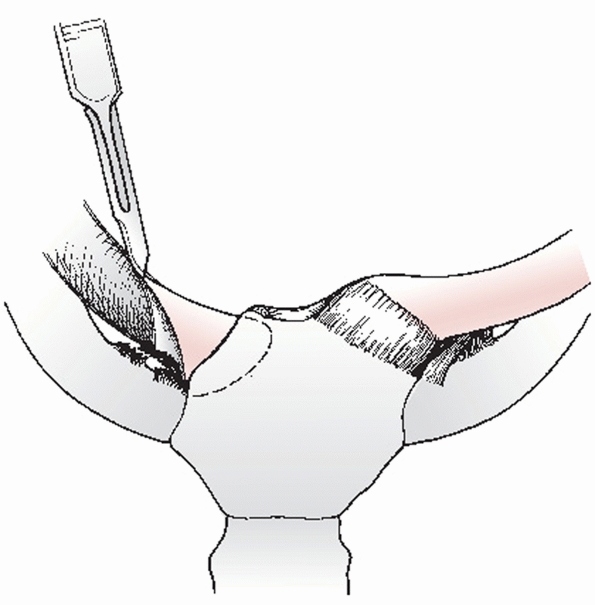
creating drill holes through both cortices of the clavicle at the
intended site of clavicular osteotomy. Following this step, an air
drill with a side-cutting burr is used to complete the osteotomy (Fig. 40-32).
The anterior and superior corners of the clavicle are beveled smooth
with an air burr for cosmetic purposes. The medullary canal of the
medial clavicle is drilled and curetted to receive the transferred
intra-articular disk ligament (Fig. 40-33). Two
small drill holes are then placed in the superior cortex of the medial
clavicle, approximately 1 cm lateral to the site of resection (Fig. 40-34).
These holes communicate with the medullary canal and will be used to
secure the suture in the transferred ligament. The free ends of the
suture are passed into the medullary canal of the medial clavicle and
out the two small drill holes in the superior cortex of the clavicle (Fig. 40-35).
While the clavicle is held in a reduced anteroposterior position in
relationship to the first rib and sternum, the sutures are used to pull
the ligament tightly into the medullary canal of the clavicle (Fig 40-36). The suture is tied, thus securing the
transferred ligament into the clavicle (Fig. 40-37).
The stabilization procedure is completed by passing multiple (five or
six) 1-mm cottony polyester fiber sutures around the reflected
periosteal tube, the clavicle, and any of the residual underlying
costoclavicular ligament and periosteum on the dorsal surface of the
first rib (Figs. 40-38, 40-39 and 40-40).
The intent of the sutures passed around the periosteal tube and
clavicle and through he costoclavicular ligament and periosteum of the
first rib is to anatomically restore the normal space between the
clavicle and the rib. To place sutures around the clavicle and the
first rib and pull them tight would decrease the space and could lead
to pain. We usually detach the clavicular head of the
sternocleidomastoid, which temporarily eliminates the superior pull of
the muscle on the medial clavicle. Postoperatively, the shoulders
should be held back in a figure-of-eight dressing for 4 to 6 weeks to
allow for healing of the soft tissues.
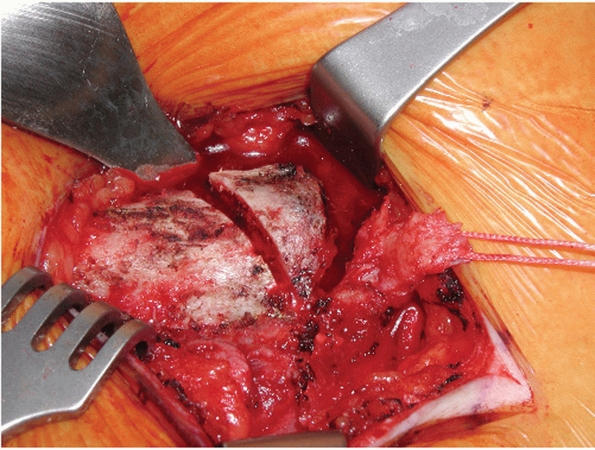 |
|
FIGURE 40-32
Resection of the medial clavicle and identification of the intra-articular ligament tagged with a suture. (Courtesy of Charles E. Rosipal, MD, and R. Michael Gross, MD.) |
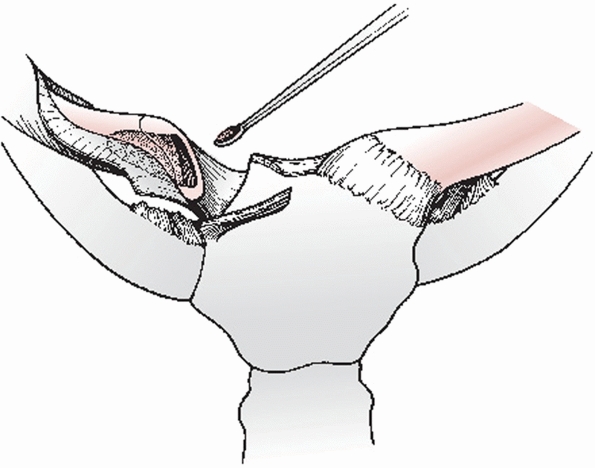 |
|
FIGURE 40-33 The medullary canal of the medial clavicle is curetted in preparation for receiving the transferred intra-articular ligament.
|
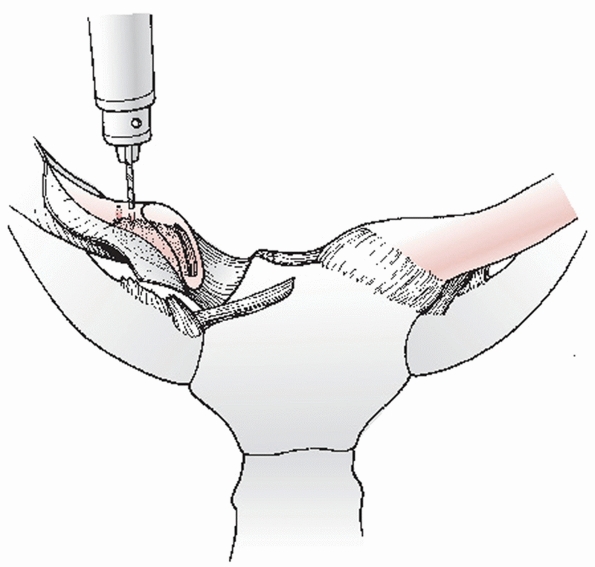 |
|
FIGURE 40-34 Drill holes are placed in the superior cortex of the clavicle, approximately 1 cm lateral to the osteotomy site.
|
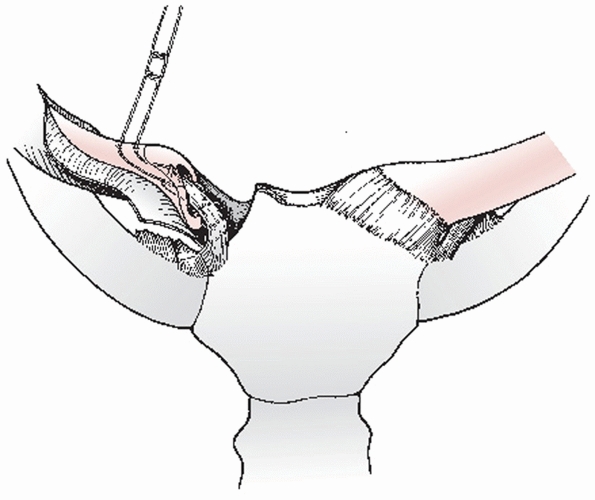 |
|
FIGURE 40-35 The free ends of the suture are passed into the medullary canal and out the two holes in the superior cortex.
|
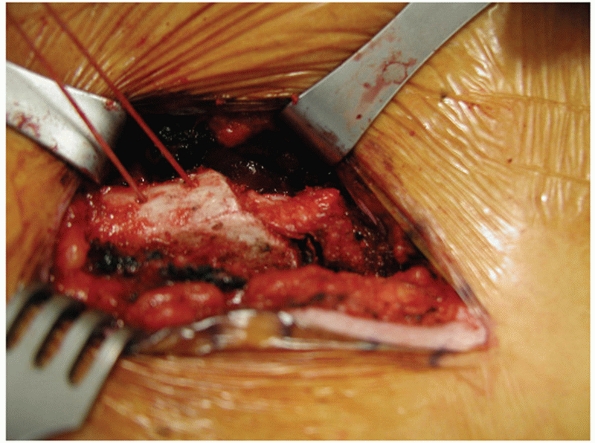 |
|
FIGURE 40-36
Passage of the intra-articular disc ligament into the medullary canal. (Courtesy of Charles E. Rosipal, MD, and R. Michael Gross, MD.) |
or any other type of metallic pins to stabilize the SC joint. The
complications
can be very serious and are discussed in the section on complications.
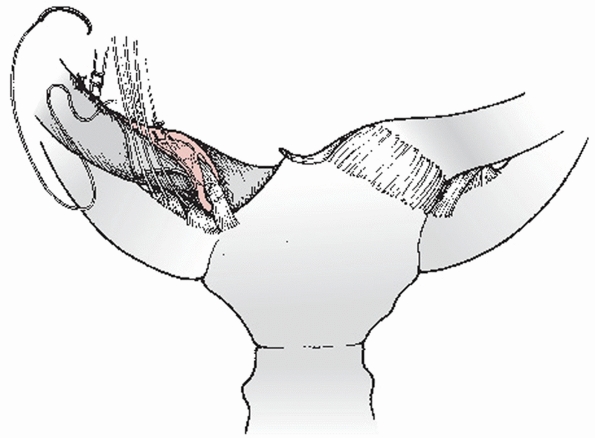 |
|
FIGURE 40-37
The transferred ligament is secured into the medial clavicle by tying the sutures exiting from the superior cortex of the clavicle. |
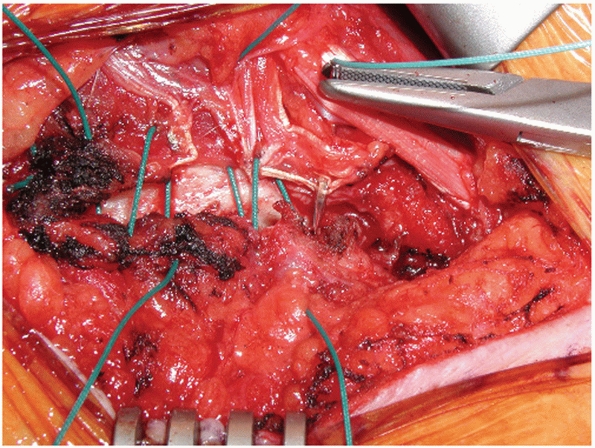 |
|
FIGURE 40-38
Passage of sutures through the clavicle and sutures through the periosteal sleeve. (Courtesy of Charles E. Rosipal, MD, and R. Michael Gross, MD.) |
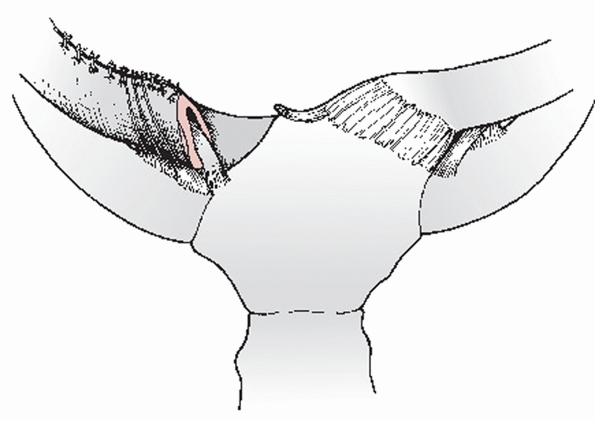 |
|
FIGURE 40-39
Closure of the periosteal sleeve around the medial clavicle and secure fixation of these structures to the costoclavicular ligament. |
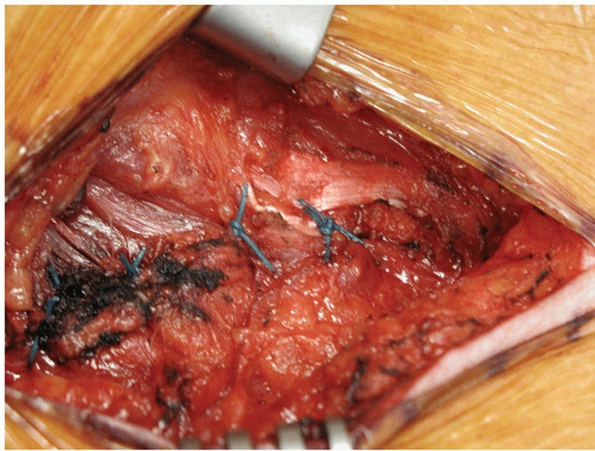 |
|
FIGURE 40-40
Intraoperative photograph showing polyester fiber sutures around the reflected periosteal tube, the clavicle, and the residual underlying costoclavicular ligament and periosteum on the dorsal surface of the first rib. (Courtesy of Charles E. Rosipal, MD, and R. Michael Gross, MD.) |
reported on a series of 23 patients who had undergone a resection of
the medial end of the clavicle. The patients were divided into two
groups: group I, those who underwent resection of the medial end of the
clavicle with maintenance or reconstruction of the costoclavicular
ligament; and group II, those who had a resection without maintaining
or reconstructing the costoclavicular ligament. The outcome in all but
1 of the 7 patients in group II was poor, with persistence or worsening
of preoperative symptoms. The only patient of this group with a
successful result had a posterior epiphyseal separation in which the
costoclavicular ligament remained attached to the periosteum, thus
preventing instability. All of the 8 patients in group I who had a
primary surgical resection of the medial end of the clavicle with
maintenance of the costoclavicular ligaments had an excellent result.
When the operation was performed as a revision of a previous procedure
with reconstruction of the costoclavicular ligament, the results were
less successful, but only 1 patient of 7 was not satisfied with the
outcome of treatment.
If open reduction is required, a figure-of-eight dressing is used for 6
weeks and this is followed by a sling for another 6 weeks. During this
time, the patient is instructed to avoid using the arm for any and all
strenuous activities of pushing, pulling, or lifting. They should not
elevate or abduct the arm more than 60 degrees during the 12-week
period. They can use the involved arm to care for bodily needs (i.e.,
eating, drinking, dressing, and toilet care). This prolonged
immobilization will allow the soft tissues a chance to consolidate and
stabilize the medial clavicle to the first rib. After 12 weeks, the
patient is allowed to gradually use the arm for usual daily living
activities, including over the head activities. However,
we do not recommend that the patients, after resection of the medial
clavicle and ligament reconstruction, return to heavy laboring
activities.
perform the closed reduction maneuvers as described above for a
suspected anterior or posterior injury. Open reduction of the physeal
injury is seldom indicated, except for an irreducible posterior
dislocation in a patient with significant symptoms of compression of
the vital structures in the mediastinum. After reduction, the shoulders
are held back with a figure-of-eight strap or dressing for 3 to 4 weeks.
cannot be sure whether a displacement about the SC joint is a
dislocation of the SC joint or a fracture through the physeal plate.
Despite the fact that there is significant displacement of the shaft
with either a type I or type II physeal fracture, the periosteal tube
remains in its anatomic position and the attaching ligaments are intact
to the periosteum (i.e., the costoclavicular ligament inferiorly and
the capsular and intra-articular disk ligaments medially) (Fig. 40-41).
patients with an unreduced and permanent anterior dislocation of the SC
joint are not very symptomatic, have almost a complete range of motion,
and can work and even perform manual labor without many problems.
Because the joint is so small and incongruous and because the results
in patients who have had the attempted reconstructions are so
inconsistent, we recommend a plan of “skillful neglect.”
arthritis for 6 to 12 months following a dislocation or a previous
arthroplasty, and if the symptoms can be completely relieved by
injection of local anesthesia into the SC joint region, we perform an
arthroplasty of the SC joint (Fig. 40-42).
potential problems that can be associated with the clavicle remaining
displaced posteriorly into the mediastinum, an arthroplasty is
performed as previously described (Fig. 40-43).
subluxation or dislocation of the SC joint. About the only symptom they
have is that the medial end of the clavicle subluxates or dislocates
anteriorly when they raise their arms over their head (see Fig. 40-15).165
This occurs without any history of trauma. Many of these patients have
the characteristic finding of generalized ligamentous laxity (i.e.,
hyperextension of the elbows, knees, and fingers as well as
hypermobility of the glenohumeral joints) (Fig. 40-44).
We have never seen a spontaneous posterior subluxation of the SC joint.
Only occasionally does the patient with atraumatic anterior
displacement complain of pain during the displacement. Because it is
difficult to stabilize the joint and prevent the subluxation or
dislocation and end up with a pain-free range of motion, we manage the
problem with skillful neglect.
of 37 patients with spontaneous atraumatic subluxation, 29 were managed
without surgery and 8 were treated (elsewhere) with surgical
reconstruction. With an average follow-up of more than 8 years, all 29
patients treated nonoperatively were doing fine without limitations of
activity or lifestyle. The 8 patients treated with surgery had
increased pain, limitation of activity, alteration of lifestyle,
persistent instability, and significant scars. In many instances,
before reconstruction or resection, these patients had minimal
discomfort, excellent range of motion, and only complained of a “bump”
that slipped in and out of place with certain motions. Postoperatively,
these patients still had the bump, along with scars and painful range
of motion (Fig. 40-45).
injuries (see Fig. 40-45). Many complications have been reported secondary to the retrosternal dislocation: right pulmonary artery laceration204; transected internal mammary artery and lacerated brachiocephalic vein42; pneumothorax and laceration of the superior vena cava147; tracheal stenosis and respiratory distress137,186; venous congestion in the neck, rupture of the esophagus with abscess and osteomyelitis of the clavicle20; pressure on the subclavian artery in an untreated patient90,140,180; occlusion of the subclavian artery late in a patient who was not treated180; obstruction of the subclavian vein caused by an unreduced type II Salter-Harris injury of the medial clavicular physis60; compression and thrombosis of the brachiocephalic vein103; myocardial conduction abnormalities186; compression of the right common carotid artery by a fracture-dislocation of the SC joint90; pseudoaneurysm of the right subclavian artery (Fig. 40-46); brachial plexus compression129 and hoarseness of the voice, onset of snoring, and voice changes from normal to falsetto with movement of the arm20,98,134,169,190; fatal tracheoesophageal fistula196; mediastinal compression95; and severe thoracic outlet syndrome with swelling and cyanosis of the upper extremity.73,92
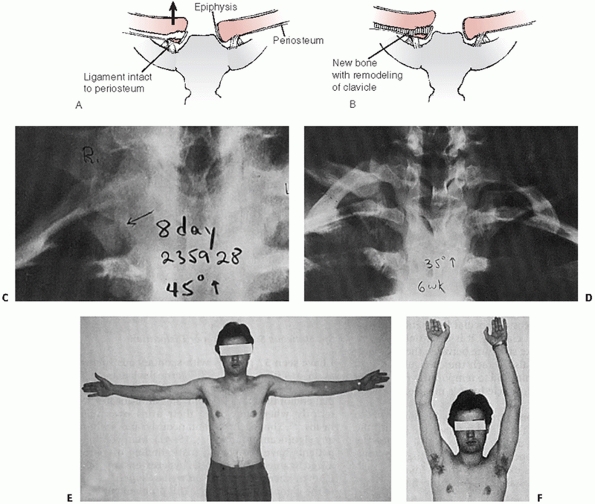 |
|
FIGURE 40-41 A.
A schematic of the healing process with a type II physeal injury of the medial clavicle. The medial clavicle splits out of the periosteal tube, leaving a small fragment (Thurstan Holland sign) behind. The costoclavicular ligament is intact to the inferior periosteal tube. B. Through remodeling from the retained epiphysis and the periosteal tube, the fracture heals. C. A radiograph at 8 days reveals that the right medial clavicle is displaced superiorly from the left clavicle. The inferior medial corner of the clavicle is still located in its normal position adjacent to the epiphysis. D. A radiograph at 6 weeks reveals new bone formation along the inferior periosteal tube. Note the thin epiphyseal plate of the normal left medial clavicle. E,F. Clinically, at 8 weeks the physeal injury has healed and the patient has a full range of motion. (From Rockwood CA, Matsen F III, eds. The Shoulder. Philadelphia: WB Saunders, 1990, with permission.) |
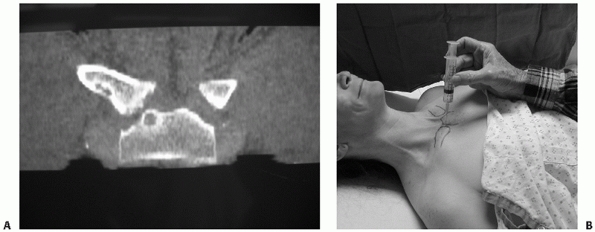 |
|
FIGURE 40-42 A.
CT scan of the SC joint. This 42-year-old patient had a symptomatic chronic anterior SC joint dislocation. Note joint space narrowing, medial clavicle osteophytes, and manubrial cysts. B. This patient’s symptoms were completely relieved by injection of local anesthesia into the SC joint. |
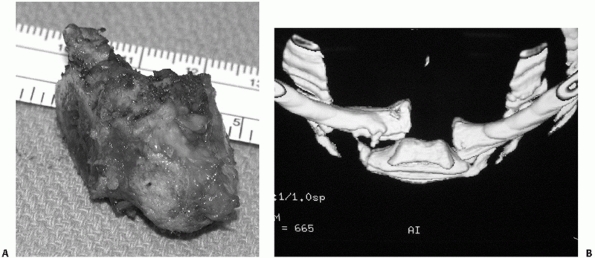 |
|
FIGURE 40-43 Chronic posterior SC joint dislocation. A. An osteophyte projecting from medial clavicle corresponds to the area of capsular injury. B. Three-dimensional reconstruction CT scan demonstrating the osteophyte.
|
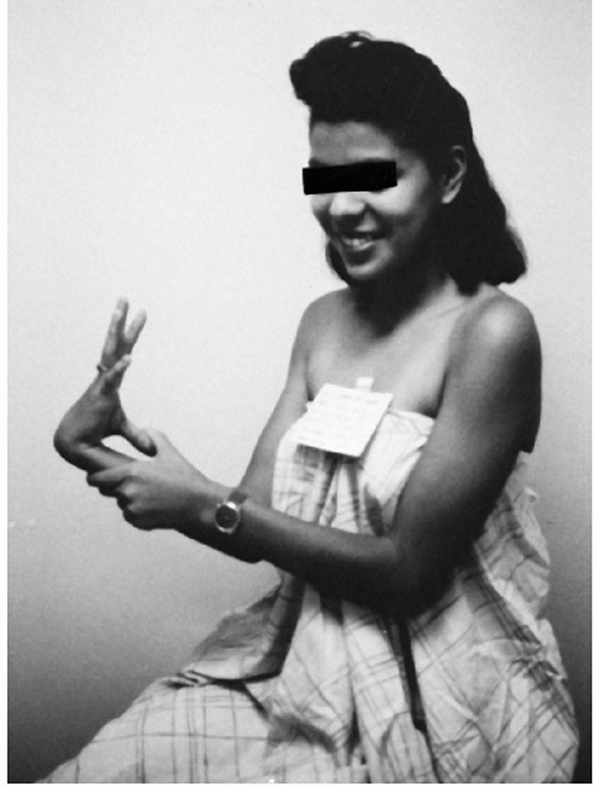 |
|
FIGURE 40-44
This patient has developed spontaneous subluxation of her SC joint. She also has generalized ligamentous laxity of the wrists, fingers, and elbows. |
in their excellent review of the complications associated with
posterior dislocations of the SC joint, reported that 16 of 60 patients
reviewed from the literature had suffered complications of the trachea,
esophagus, or great vessels.82,98,152
neardeaths from migrations of intact or broken K-wires or Steinmann
pins into the heart, pulmonary artery, or the aorta.* Numerous other authors have reported complications from pin migration into the pulmonary artery,27,113,115 aorta,141 heart,57,94,167,171 subclavian artery,174 mediastinum,64,78,109,193 and breast.77
published data on the migration of pins from the SC joint in 21
patients. They reported that pins from the SC joint had migrated into
the chest, heart, mediastinum, subclavian vein, and lung. They
recommended that large, small, smooth, threaded, bent, or straight pins
not be used for fixation of the SC joint
because of their potential to migrate into vital structures and even
cause death. Further, they recommended that any time pins were used to
manage any problems about the shoulder (i.e., clavicle fractures or
injuries to the AC joint), the pins be monitored very closely with radiographs and that they should always be removed (Fig. 40-47).
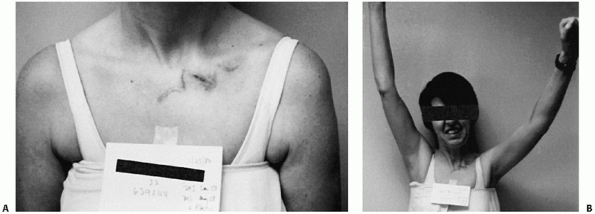 |
|
FIGURE 40-45
Patients treated with surgery for spontaneous, atraumatic subluxation of the SC joint often have increased pain, limitation of activity, alteration of lifestyle, persistent instability of the joint, and a significant scar. A,B. Not only was the cosmetic scarring a problem, but motion and pain were worse than before the reconstruction. (From Rockwood CA, Matsen F III, eds. The Shoulder. Philadelphia: WB Saunders, 1990, with permission.) |
some increased laxity which should normalize with time. A case report
of anterior subluxation after closed reduction of a posterior
dislocation noted that the residual anterior instability resolved with
observation.199 Even with
reconstructive procedures, the joint may remain subluxed or
subjectively unstable with motion. This is particularly true of
patients who were treated surgically for atraumatic instability.
Excessive resection of the medial clavicle without successful
stabilization can create a challenging instability of the residual
medial clavicle for which few options exist (Fig. 40-48). In such cases, total claviculectomy may be the only option.108
An islandized hemipectoralis muscle flap has been also suggested as a
means for filling a large medial clavicular defect and may prove useful
in these cases.173
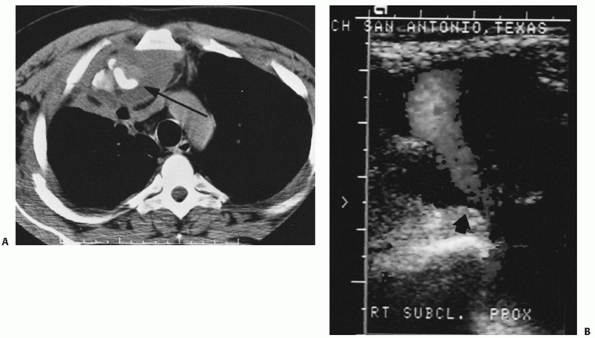 |
|
FIGURE 40-46 A.
CT scan revealing a posterior fracture-dislocation of the SC joint with significant soft tissue swelling and compromise of the hilar structures. B. Duplex ultrasound study revealing a large pseudoaneurysm of the right subclavian artery. Note the large neck of the pseudoaneurysm, which measured approximately 1 cm in diameter (arrow). |
unrecognized or are treated inappropriately. Only an occasional
publication cites the SC joint and because of the rarity of the
problem, it can almost be called the “forgotten joint.” It is one of
the strongest and most stable joints, and when it dislocates it is
difficult to stabilize. If more orthopaedic surgeons would write up
their treatment of this rare condition, there would be more data for
orthopaedic surgeons to review and to help understand the problem.
After years of experience in publications, we still have not read of
the ultimate stabilizing procedure for dislocations of the SC joint.
Most surgeons leave anterior dislocations of the joint alone as
patients can function nicely after despite some instability. The
question is: why shouldn’t we be able to reduce it and hold it and keep
it in place until the ligaments are healed? One thing that is for
certain in the twenty-first century is that we understand that the SC
dislocation should not be stabilized with K-wires, Steinmann pins, or
similar devices. Simple pinning of the joint with or without repairing
the ligaments usually results in pin migration to the chest,
mediastinum, abdominal organs, and even to the spinal canal. Many
deaths have been reported from intracardiac penetration of migrating
pins. Recently, the use of a combination clavicle plate with
intrasternal hook has been reported but long-term results are needed
before this is a commonly accepted procedure.
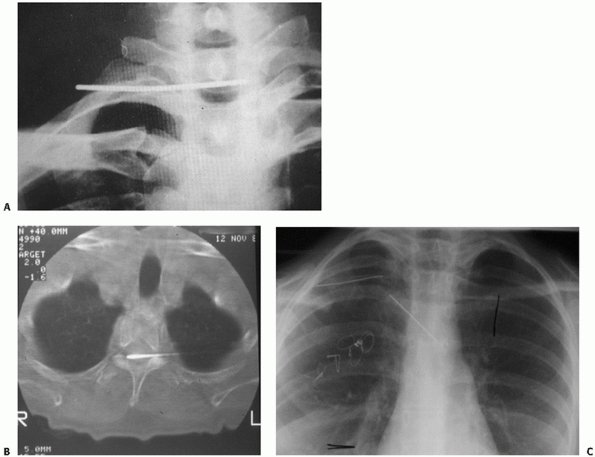 |
|
FIGURE 40-47 Migration of pins from the SC joint. A,B. Migration of Steinmann pin into the spinal canal. C. Migration of Steinmann pin into the mediastinum.
|
 |
|
FIGURE 40-48 Excessive resection of the medial clavicle resulting in residual instability of the medial clavicle with adduction.
|
a challenge. Certainly, we must recognize the condition in adults
because the continued displacement of the clavicle can cause erosion
into the great vessels and mediastinum and can produce severe
complications. If the clavicle is removed from the mediastinum, the
question is what to do next? Does one try to stabilize it, pin it,
plate it, or does one resect the medial 2 cm and then stabilize the
residual clavicle down to the first rib to prevent anterior/superior
and/or continued posterior displacement?
with anterior/posterior spontaneous subluxation of the SC joint. Does
one stabilize it, excise the medial clavicle, or continue to observe
the patient? So far, the literature reflects that this condition occurs
in young people and the symptoms gradually disappear with aging. Again,
if there were more publications on this complex problem, then more
orthopaedists would understand it.
treatment of traumatic and atraumatic conditions of the SC joint? The
use of SC pin fixation should be of historical interest only and we can
hope that some type of safe anterior or posterior stabilization
procedure can be developed for the unstable joint. Hopefully, we will
see more and more publications in the orthopaedic literature that will
educate orthopaedic surgeons in the management of problems of the SC
joint.
Z, Sinopidis C, Grocock CJ, et al. Suture anchors for treatment of
sternoclavicular joint instability. J Shoulder Elbow Surg 2006;15:315-8.
BF, Zielinski CJ. Posterior fracture through the sternoclavicular
physis associated with a clavicle fracture: A case report and
literarture review. AJ Ortho 1999;28(10): 598-600.
AL, Dias JJ. Reconstruction for instability of the sternoclavicular
joint using the tendon of the sternocleidomastoid muscle. J Bone Joint
Surg Br 2008;90:610-3.
DS, Kocher MS, Waters PM, Micheli LM, Griffery M, Dichtel L. Chronic
recurrent anterior sternoclavicular joint instability: results of
surgical management. J Pediatr Orthop. 2006;26:71-4.
TC, Pannunzio ME, Abhinav CB, et al. Interposition arthroplasty with
bone-tendon allograft: A technique for treatment of the unstable
sternoclavicular joint. J Orthop Tr 2005;19:124-129.
JD. Direct observation on the function of the capsule of the
sternoclavicular joint in clavicular support. J Anat 1967;101:159-180.
LJ, Dauphin N, Marzo JM. A safe zone for resection of the medial end of
the clavicle. J Shoulder Elbow Surg 2003;12(6):592-594.
B, Charow A, Cook W, et al. An unusual football injury (posterior
dislocation of the sternoclavicular joint). Arch Otolaryngol
1972;95:185-187.
E. Traumatic posterior displacement of the left clavicular head causing
chronic extrinsic compression of the subclavian artery. Physician
Sports Med 1987;15:87-89.
MR, Bartz RL, Reardon PR, et al. A method for open reduction and
internal fixation of the unstable posterior sternoclavicular joint
dislocation. J Orthop Trauma 1997;11:378-381.
J, Stabler A, Preidler KW, et al. Sternoclavicular joint: MR imaging—
anatomic correlation. Radiology 1996;198(1):193-198.
MI, Pozniak MA. Computed tomography with stress maneuver to demonstrate
sternoclavicular joint disease. J Comput Assist Tomogr
1990;14(1):159-160.
C, Neugebauer R. Carbon fiber replacement of the ligaments of the
shoulder girdle and the treatment of lateral instability of the ankle
joint. Clin Orthop 1985;196: 112-117.
HF. Tenodesis of subclavius in the treatment of recurrent dislocation
of the sternoclavicular joint. J Bone Joint Surg 1951;33B:240-243.
W, Ramadan LB, Bitar AC, et al. Sternoclavicular
dislocation-reconstruction with semitendinosus tendon autograft: a case
report. Knee Surg Sports Traumatol Arthrosc 2008;17.
KD, Longo A, Lick S, et al. Posterior sternoclavicular epiphyseal
fracture-dislocation with delayed diagnosis. Skeletal Radiol
2006;35:608-12.
RL, Milgram JW, Yawn DH. Fatal aortic perforation and cardiac tamponade
due to a Kirschner wire migrating from the right sternoclavicular
joint. South Med J 1974; 67:316-318.
AP. The Lectures of Sir Astley Cooper on the Principles and Practices
of Surgery. Philadelphia: E.L. Carey & A. Hart, 1935:559.
GJ, Stubbs D, Waller DA, et al. Posterior sternoclavicular dislocation:
a novel method of external fixation. Injury 1992;23:565-567.
R, Riddervold HO. Posterior dislocation of the sternoclavicular joint:
report on two cases, with emphasis on radiologic management and early
diagnosis. Skeletal Radiol 1988;17:247-250.
LA, Rubino LJ. Subluxation of the sternoclavicular joint secondary to
pseudoarthrosis of the first and second ribs. J Bone Joint Surg
2002;84A(4):623-626.
JM, Gilula LA, Murphy WA, et al. Computed tomography of the
sternoclavicular joint and sternum. Radiology 1981;138:123-129.
AL, Rexnick D, Mink JH. Computed tomography of the glenohumeral and
sternoclavicular joints. Orthop Clin North Am 1985;16(3):497-511.
C, Bousso A, Sane A, Sané JC, Niane M, Ndiaye A, Sy MH, Seye S. Bipolar
dislocation of the clavicle or floating clavicle. A report of 3 cases.
Chir Main 2007;26: 113-6.
K, Tropp H, Asberg B. Case report: retrosternal clavicular dislocation
in the sternoclavicular joint. Clin Radiol 1998;53:75-76.
R, Vojácek J, Lischke R, et al. Kirschner wire migration from the right
sternoclavicular joint to the heart: a case report. Heart Surg Forum
2006;9:E840-2
PS, Michaelson JE. Adolescent butterfly swimmer with bilateral
subluxing sternoclavicular joints. Br J Sports Med 2006;40:e12.
NW, Morris AD, Kaye JC, et al. Subclavian vein obstruction caused by an
unreduced type II Salter Harris injury of the medial clavicular physis.
J Shoulder Elbow Surg 2002;11(3):271-273.
L, Yubero J, Usabiaga J, et al. Sternoclavicular dislocation,
treatment, and complications. Ital J Orthop Traumatol 1988;14:349-355.
A, Leonard A. Transsternal sternoclavicular projection: diagnostic
value in sternoclavicular dislocations. J Radiol 1981;62:167-170.
WM, Jannasch O, Siassi M, et al. Balser plate stabilization: an
alternate therapy for traumatic sternoclavicular instability. J
Shoulder Elbow Surg 2003;12(3):276-281.
W, Fritz T. Die PDS-Kordefixation der Sternockavikularen Luxation und
Paraartikularen Klavikulafrankturen. Unfallchirurg 1994;97:263-265.
DW, Dunn ID, McPherson S, et al. Retrosternal dislocation of the
clavicle: the “stealth” dislocation: a case report. Injury
1992;23:563-564.
RB III, Williams GR Jr. Clinical evaluation of injuries to the
acromioclavicular and sternoclavicular joints. Clin Sports Med
2003;22:239-254.
D, Wemhoner SR, Ogbuihi S. On two cases of fatal heart tamponade due to
migration of fracture nails from the sternoclavicular joint. Z
Rechtsmed 1984;93: 53-60.
BA. Bilateral, spontaneous, anterior subluxation of the
sternoclavicular joint: a case report and literature review. Mil Med
2006;171:790-2.
R. Unusual dislocation of a fragment of Kirschner wire after fixation
of the sternoclavicular joint. Wiad Lek 1987;40:630-632.
Von H, Klammer NI. Komplihationem durch Drahtvenderungen nach
Kirschnerdracht-Sprakungen on der Klavikula. Fortschr Geb Rontgenstr
Nuklearmed Erganzungsband 1978;128:591-594.
H, Hertz H. [Origin, diagnosis and treatment of sternoclavicular joint
dislocation.] Aktuelle Traumatol 1987;17(1):23-28.
W. Retention Einer Seltenen Sternoclavicular Lluxationsfrktur Mittels
Modifizierter Y-platte der AO. Aktuel Traumatol 1986;16:39-40.
CF. Retrosternal dislocation of the clavicle: early recognition, x-ray
diagnosis, and management. J Bone Joint Surg 1968;50A:830(abst).
FM, Shafer SJ. Injuries to the clavicle with neurovascular
complications: a study of fourteen cases. J Bone Joint Surg
1965;47A:1335-1346.
HC, Wu JJ, Lo WH, et al. Epiphyseal fracture—retrosternal dislocation
of the medial end of the clavicle: a case report. Chin Med J
1993;52:198-202.
S, Monbaliu D, Thompson JF. Thoracic outlet syndrome caused by chronic
retrosternal dislocation of the clavicle. J Bone Joint Surg [Br]
2002;84B:116-118.
de Varebeke B, Van Osselaer G. Migration of Kirschner pin from the
right sternoclavicular joint resulting in perforation of the pulmonary
artery main trunk. Acta Chir Belg 1993;93:287-291.
V, Knoll D, Klinke F, et al. [Penetrating injuries of the heart and
intrapericardial blood vessels caused by migration of a Kirschner pin
after osteosynthesis.] Acta Chirg Iugosl 1982;29:274-276.
JB, Denis JL, Dromer CEH. Posterior dislocation of the sternoclavicular
joint leading to mediastinal compression. Ann Thoacic Surg
1996;61:711-713.
R, Frese J. Intrathoracic dislocation of a metal-piece after the use of
wires in bone-surgery. Unfallchirurgie 1980;6(1):56-61.
MA, Spreitzerm AM, Miro PA, et al. MR imaging of the abnormal
sternoclavicular joint—a pictorial essay. Clin Imaging 1997;21:138-143.
B, Cherkes-Zade D. Case of injury to the aorta by a Kirschner pin
during osteosynthesis of the sternoclavicular joint. Ortop Travmatol
Protez 1972;33:73-74.
V, Glauser F. Unusual sequela following pinning of medial clavicular
fracture. AJR Radium Ther Nucl Med 1956;76:1066-1069, 1956.
SG, Schiffern SC, Pennington SD, et al. Functional outcomes after total
claviculectomy as a salvage procedure. A series of six cases. J Bone
Joint Surg Am 2007; 89:1215-9.
CT, Senatus P, Patti J, et al. Dislocation of the sternoclavicular
joint. Evaluation using paraxial computed tomographic reconstruction.
Orthop Rev 1993;22(1): 101-103.
L, Rosman M. Sternoclavicular epiphyseal separation with adjacent
clavicular fracture: a case report. J Pediatr Orthop 1984;4:118-120.
EM, Bunnell WP, Yuan HA. Computed tomography in the diagnosis of
dislocations of the sternoclavicular joint. Clin Orthop 1979;140:12-6.
NJ, Bismil Q, Chipperfield A, et al. Superior dislocation of the
sternoclavicular joint. J Shoulder Elbow Surg 2008;17:e22-3.
HP, Chang CH, Lin PJ, et al. Migration of Kirschner wire for the right
sternoclavicular joint into the main pulmonary artery: a case report.
Chang Keng I Hsueh 1992; 15(1):49-53.
JA. Posterior dislocation of the sternoclavicular joint associated with
major spinal injury: a case report. S Afr Med J 1987;71:791-792.
JD, Bassett GS. Posterior sternoclavicular epiphyseal separation
presenting with hoarseness: A case report and discussion. Ped Emerg
Care 1998;14:130-132.
PA, Chapman KW, Frankel VH. Surgical treatment of chronic dislocation
of the sternoclavicular joint. J Bone Joint Surg 1975;57B:193-196.
F, Rockwood CA Jr. Current concepts review. Migration of pins used in
operations of the shoulder. J Bone Joint Surg 1990;72A:1262-1267.
WB. Safe and simple method of repair of recurrent dislocation of the
sternoclavicular joint. J Bone Joint Surg 1986;68B:332(abst).
A, Rodriguez A, Gonzalez G, et al. Atraumatic spontaneous posterior
subluxation of the sternoclavicular joint. Arch Orthop Trauma Surg
1999;119:344-346.
P, Henley BM, Linnau KF. Radiographic clues for high-energy trauma:
Three cases of sternoclavicular dislocation. AJR 2001;176:1534.
RC, Love RB, Keene JS, Orwin JF. Operative treatment of the painful
sternoclavicular joint: a new technique using interpositional
arthroplasty.J Shoulder Elbow Surg 2006;15:60-66.
E, Tanaka T, Noguchi T, et al. Tracheal stenosis caused by retrosternal
dislocation of the right clavicle. Ann Thorac Surg 2007;83:685-7.
T, Wada I, Tsuchiya D, et al. Clavicle fracture and posterior
sternoclavicular dislocation in a newborn. Ortho 2001;24(12):1169-1170.
M, Shiraishi H, Mizuno K. Chronic posterior sternoclavicular
dislocation causing compression of a subclavian artery. J Shoulder
Elbow Surg 1997;6(6):564-569.
K, Inagawa H, Kiyota K, et al. Posterior dislocation of the
sternoclavicular joint with obstruction of the innominate vein: case
report. J Trauma 1998;44(2):381-383.
JW, Wilhite J. Migration of a foreign body from the sternoclavicular
joint to the heart: a case report. Am Surg 1969;35:448-449.
AW, Russell GV. Ipsilateral clavicle fracture, sternoclavicular joint
subluxation, and long thoracic nerve injury: an unusual constellation
of injuries sustained during wrestling. AJ Sports Med 200;28(6):904-908.
RC, Bankes MJK, Emery RJH. Diagnosis of retrosternal dislocation of the
clavicle with ultrasound. Injury 1996;27(9):670-671.
SA Shah AK, Pruzansky ME. Using the semitendinosus tendon to stabilize
sternoclavicular joints in a patient with Ehlers-Danlos syndrome: a
case report. Am J Orthop 2005;34:315-8.
CA Jr. Dislocation of the sternoclavicular joint. In: Rockwood CA Jr,
Green DP, eds. Fractures, 1st ed, vol 1. Philadelphia: JB Lippincott,
1975:756-787.
CA Jr. Injuries to the Sternoclavicular Joint. In: Rockwood CA Jr,
Green DP, eds. Fractures. 2nd ed, vol 1. Philadelphia: JB Lippincott,
1984:910-948.
CA Jr, Groh GI, Wirth MA, et al. Resection arthroplasty of the
sternoclavicular joint. J Bone Joint Surg 1997;79(3):387-393.
CA Jr, Odor JM. Spontaneous atraumatic anterior subluxation of the
sternoclavicular joint. J Bone Joint Surg 1989;71A:1280-1288.
ZR, Moray B, Itzchak Y. Percutaneous removal of intravascular foreign
bodies. Cardiovasc Intervent Radiol 1982;5:64-68.
JO, Lyons FA, Rockwood CA Jr. Management of dislocations of both ends
of the clavicle. J Bone Joint Surg 1990;72A:399-402.
MR, Parsons BO, Lin H, et al. Islandized hemipectoralis muscle flap for
sternoclavicular defect. J Shoulder Elbow Surg 2007;16:e31-4.
FM, Hofer PH, Pinter H, et al. Intracardiac malpositioning of a
sternoclavicular fixation wire. J Orthop Trauma 1992;6:102-105.
EE, Kuhn JE. Biomechanical analysis of reconstructions for
sternoclavicular joint instability. J Bone Joint Surg
2004;86A(1):98-105.
EE, Kuhn JE, Huston LJ, et al. Ligamentous restraints to anterior and
posterior translation of the sternoclavicular joint. J Shoulder Elbow
Surg 2002;11(1):43-47
DP, Williams PR, Hoddinott HC. A “safe” surgical technique for
stabilization of the sternoclavicular joint: a cadaveric and clinical
study. Ann R Coll Surg Engl 2000; 82:432-435.
JL, Colombier JA, Choiron P, et al. Retrosternal dislocation of the
clavicle: a report of six cases. Fr J Orthop Surg 1990;1:107-112.
RS, Loukas M, Slappey JB, et al. Surgical and clinical anatomy of the
interclavicular ligament. Surg Radiol Anat 2007;29:357-60.
Holsbeeck M, van Melkebeke J, Dequeker J, et al. Radiographic findings
of spontaneous subluxation of the sternoclavicular joint. Clin
Rheumatol 1992;11:376-81.
J, Tarazona P. Fracture of the minubrium with posterior displacement of
the clavicle and first rib. Int Orthop 1998;22:269-271.
MJ, Busse EF. Posterior dislocation of the clavicle causing fatal
tracheoesophageal fistula. Can J Surg 1981;24:626-627.
PM, Bae DS, Kadiyala RK. Short-term outcomes after surgical treatment
of traumatic posterior sternoclavicular fracture-dislocations in
children and adolescents. J Pediatr Orthop 2003;23(4) ;464-469.
PA, Suchey JMM. Epiphyseal union of the anterior iliac crest and medial
clavicle in a modern multiracial sample of American males and females.
Am J Phys Anthropol 1985;68:457-466.
M, Borens O, Garofalo R, et al. Anterior subluxation after reduction of
a posterior traumatic sterno-clavicular dislocation: a case report and
a review of the literature. Knee Surg Sports Traumatol Arthrosc
2004;12:453-6.
J, Sterner S, Maurer D, et al. Retrosternal epiphyseal disruption of
medial clavicle: case and review in children. J Emerg Med 1989;7:9-13.
MA, Rockwood CA. Chronic conditions of the acromioclavicular and
sternoclavicular joints. In: Chapman MW, ed. Operative Orthopaedics,
part XI. 2nd ed. Philadelphia: JB Lippincott, 1992:1683-1693.
MA, Rockwood CA. Complications following repair of the sternoclavicular
joint. In: Bigliani LU, ed. Complications of the shoulder. Baltimore:
Williams & Wilkins, 1993:139-153.
MA, Rockwood CA. Complications of treatment of injuries to the
shoulder. In: Epps CH, ed. Complications in Orthopaedic Surgery. 3rd
ed. Philadelphia: JB Lippincott, 1994:229-253.
J, Al-Etani H, Letts M. Diagnosis and treatment of posterior
sternoclavicular joint dislocation in children. AJ Ortho
1996;25(8):565-569.
KR, Ray S, Neer CS. Conservative management of a displaced medial
clavicular physeal injury in an adolescent athlete. Am J Sports Med
1989;17(6):833-836.
