The Elbow: Physeal Fractures, Apophyseal Injuries of the Distal Humerus, Osteonecrosis of the Trochlea, and T-Condylar Fractures
Two – Upper Extremity > 15 – The Elbow: Physeal Fractures,
Apophyseal Injuries of the Distal Humerus, Osteonecrosis of the
Trochlea, and T-Condylar Fractures
injury, each with a distinct fracture pattern. The vulnerability of the
various physes to injury is altered by age and injury mechanism. Next
to those of the distal radius, injuries to the distal humeral physes
are the most common physeal injuries. In general, the physes of the
major long bones are most vulnerable to fracture just before puberty,
when the perichondral ring is weakest.142
Fractures involving the medial epicondylar apophysis are most common in
preadolescents (peak ages: 11 to 15 years), probably because many
avulsions of this apophysis are associated with posterolateral
dislocations, which are also common in this age group. Fractures
involving the lateral condylar physis occur early, with the average age
around 6 years.59,73,83,98,142 Fractures concerning the medial condylar physis are rare and occur most often in children 8 to 12 years of age.59,83,98 Fractures
involving the total distal humeral physis may occur in neonates or within the first 2 to 3 years of life.40,127
of injury are discussed in detail in the following sections dealing
with these specific fractures.
immature skeleton either cross the physis or follow it for a short
distance into the trochlea. Fractures of the lateral condylar physis
constitute 16.9% of distal humeral fractures.
Within the elbow region, the associated injuries that can occur with
this fracture include dislocation of the elbow (which may be a result
of the injury to the lateral condylar physis rather than a separate
injury), radial head fractures, and fractures of the olecranon, which
are often greenstick fractures. Acute fractures involving only the
anatomic capitellum are rare in the immature skeleton.
be less obvious both clinically and on radiograph than that of
supracondylar fractures, especially if the fracture is minimally
displaced. Functional loss of range of motion in the elbow is much more
frequent with lateral condylar physis fractures because the fracture
line often extends into the articular surface. Malunion of a
supracondylar fracture that results in cubitus varus is likely to
result in a surgically correctable cosmetic deformity with an
essentially normal range of motion in the elbow. A poorly treated
lateral condylar physeal injury, however, is likely to result in a
significant loss of range of motion that is not as responsive to
surgical correction. The complications of supracondylar fractures are
usually evident in the immediate post-injury period. The poor outcome
of a lateral condylar physeal fracture may not be obvious until months
or even years later.84,172,179 Ippolito et al.84
evaluated 49 individuals with humeral condylar fractures 18 to 45 years
after the injury. Twenty fractures with displacement of 2 mm to 10 mm
with no tilting of the osteochondral fragment had been treated without
reduction, and 16 fractures with marked displacement and fragment
tilting had been treated surgically; all 36 had good results. All 13
patients treated operatively or nonoperatively for old, displaced
fractures had poor results. Nonunion developed in four patients, and
osteonecrosis occurred in six. Arthrosis of the elbow was found in
fractures complicated by osteonecrosis and nonunion and in old
fractures when the humeral condyle was resected, but it was not
observed in uncomplicated fractures.
fractures that exited through the trochleocapitellar groove as type I
and those that exited through the trochlea as type II. Around the same
time, Cotton35 described more
details of the various subluxations of both the fragment and elbow
joint that occurred with this type of fracture. He noted that because
the fragment was usually still attached to the proximal radius, both
the radius and ulna were subluxed. The most common displacement was
“outward and backward”; “inward and forward” displacement was rare.
Cotton35 also noted that the main
pathology was associated with condylar fragment rotation. He observed
that this fracture often resulted in limited extension, had some local
lateral outgrowth at the fracture site, and rarely resulted in axial
deviation of the elbow unless there was a resultant nonunion. More
recent investigators have added little to his description of this
lesion’s pathology.
either the fracture line’s anatomic location or by the stage of
displacement, as described by Wilkins.199
classified lateral condylar physeal injuries as type IV injuries in
their classification of physeal fractures. A true Salter-Harris type IV
injury through the ossific nucleus of the lateral condyle is rare.
Although lateral condylar fractures are similar to Salter-Harris type
II and IV fractures, treatment guidelines follow those of a type IV
injury: open reduction and internal fixation of displaced
intra-articular fractures, with the potential for mild growth
disturbance of the distal humeral physis. There is no contact between
the trochlea’s ossification center and the exposed bone in the
metaphyseal fragment.
then courses along the physeal cartilage, it has some of the
characteristics of both type II and IV injuries according to the
Salter-Harris classification. This fracture classification is
debatable, because the fracture exits the joint in the not-yet-ossified
cartilage of the trochlea.
compared intraoperative findings to preoperative radiographic
classification in 25 displaced fractures of the lateral condyle and
found that in 13 (52%), the Milch classification did not correlate with
intraoperative findings. Eight of 17 fractures (47%) classified
preoperatively as Milch type I fractures (Fig. 15-1) were unstable, and five of eight fractures classified preoperatively as Milch type II fractures (Fig. 15-2) were extra-articular, extending across the distal humeral physis medially. Mirsky et al.122
identified three distinct fracture patterns: nine fractures exited the
distal humeral epiphysis just medial to the capitellum, 11 exited
through the trochlear epiphysis, and five extended across the physis
medially. No fracture appeared to traverse the ossified portion of the
capitellum (Milch type I).
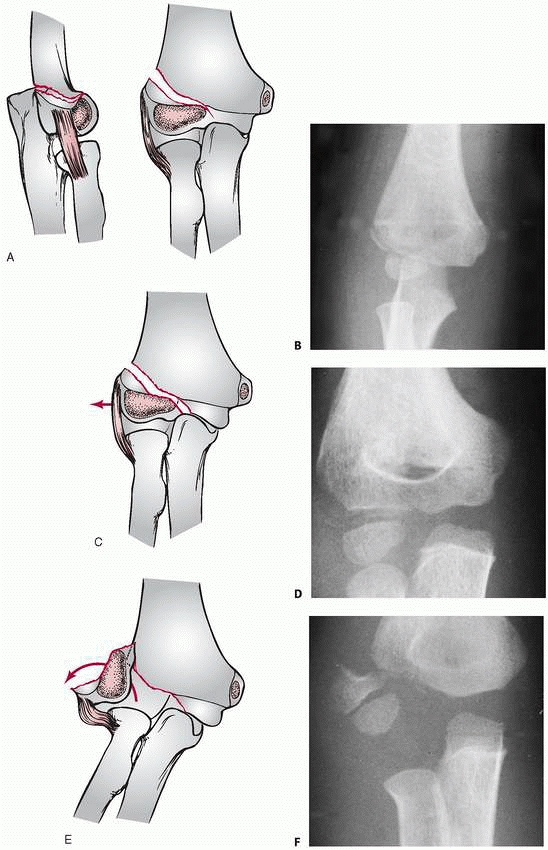
This allows the proximal fragment to become more displaced and can
allow lateral displacement of the olecranon. In the third stage, the
condylar fragment is rotated and totally displaced laterally and
proximally, which allows translocation of both the olecranon and the
radial head (Fig. 15-3E,F).
modified the description of stage I displacement to include fractures
with less than 2 mm of displacement seen on the anteroposterior (AP) or
lateral radiograph only or seen on both views.
metaphysis, with a soft tissue tear in the area between the origins of
the
extensor
carpi radialis longus and the brachioradialis muscle. The extensor
carpi radialis longus and brevis muscles remain attached to the free
distal fragment, along with the lateral collateral ligaments of the
elbow. If there is much displacement, both the anterior and posterior
aspects of the elbow capsule are usually torn. This soft tissue injury,
however, is usually localized to the lateral side and may help identify
a minimally displaced fracture. More extensive soft tissue swelling at
the fracture site may indicate more severe soft tissue injury,106,143 which may indicate that the fracture is prone to late displacement.
 |
|
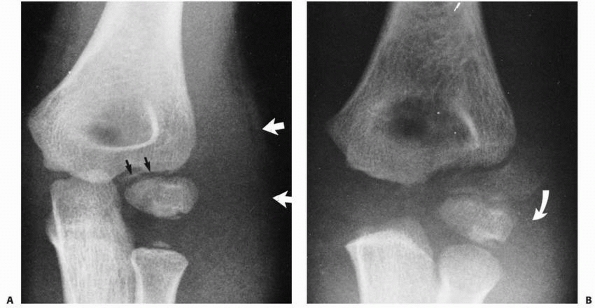
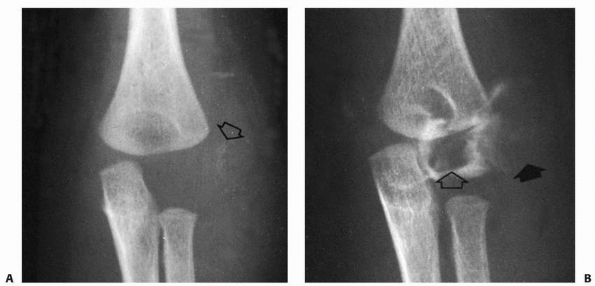
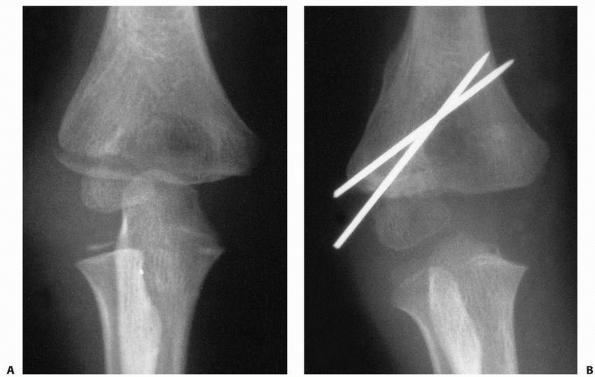
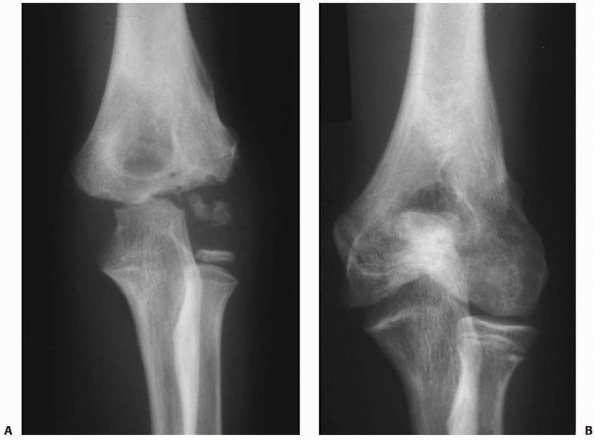
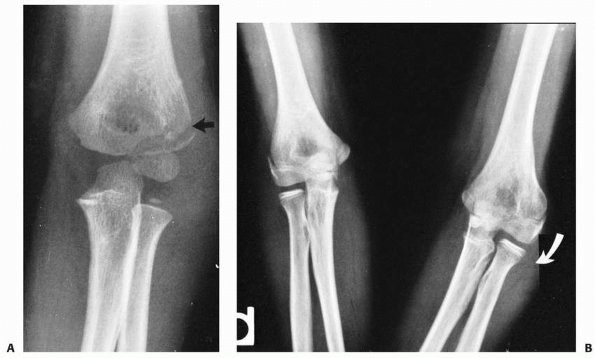
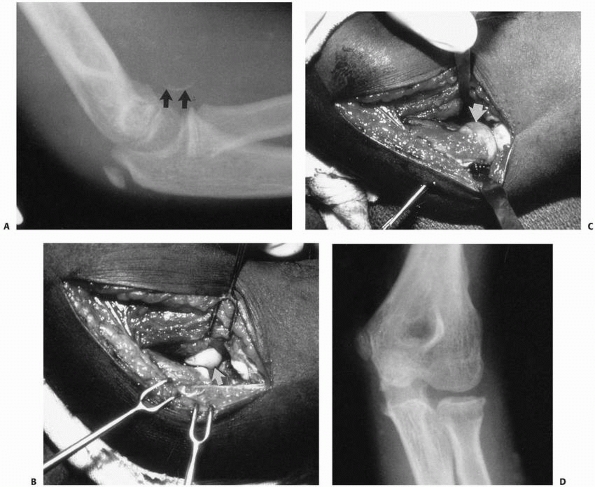
FIGURE 15-1 A. Injury film of a 7-year-old with an undisplaced fracture of the lateral condyle (small arrows). Attention was drawn to the location of the fracture because of extensive soft tissue swelling on the lateral aspect (white arrows). B.
Because of the extensive soft tissue injury, there was little intrinsic stability, allowing the fracture to become displaced at 7 days (arrow). |
of displacement varies according to the magnitude of the force applied
and whether the cartilaginous hinge of the articular surface remains
intact. If the articular surface is intact, the resultant displacement
of the condylar fragment is simply a lateral tilt hinging on the intact
medial articular surface. Horn et al.82
studied 16 lateral humeral condylar fractures with radiographs and
magnetic resonance imaging (MRI) and determined that all fractures
unstable on radiograph had disruption of the cartilage hinge on MRI,
confirming the relation of the cartilage hinge on fracture stability.
If the fracture is complete, the fragment can be rotated and displaced
varying degrees; in the most severe fractures, rotation is almost the
full 180 degrees, so that the lateral condylar articular surface
opposes the denuded metaphyseal fracture surface. Wilson203
showed that in addition to this coronal rotation of the distal
fragment, rotation can also occur in the horizontal plane. The lateral
margin is carried posteriorly, and the medial portion of the distal
fragment rotates anteriorly.
 |
|
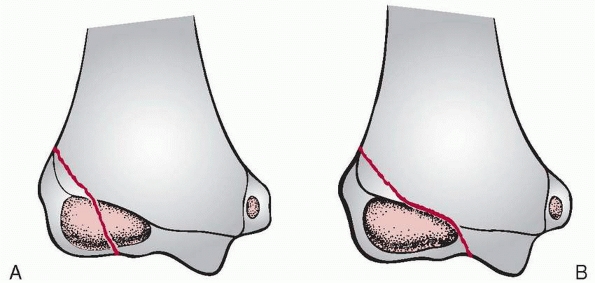
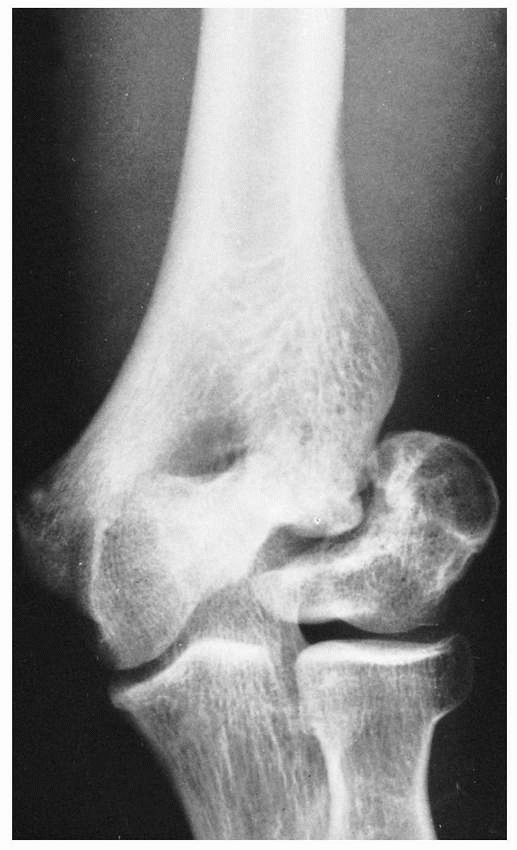
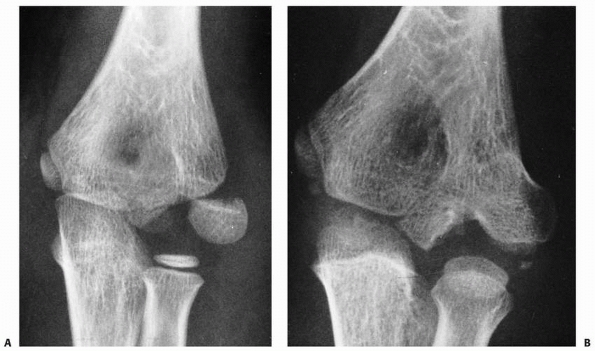
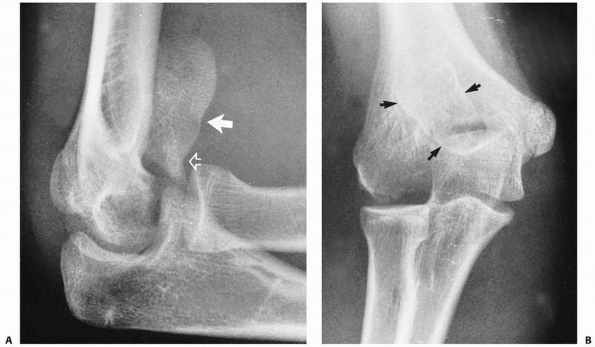
FIGURE 15-2 Physeal fractures of the lateral condyle. A. Physeal injury (Milch type II) through the nonossified trochlea. B.
Physeal injury (Milch type I) through the ossific nucleus of the lateral condyle. (Adapted and reprinted with permission from Milch HE. Fractures and fracture-dislocations of the humeral condyles. J Trauma 1964;4:592-607.) |
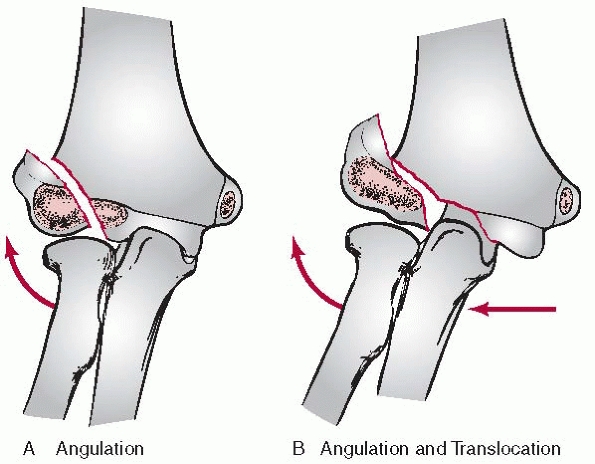
crista of the trochlea, the elbow joint is unstable, creating the
possibility of posterolateral subluxation of the proximal radius and
ulna. Thus, the forearm rotates along the coronal plane into valgus,
and there may also be lateral translocation of the lateral condyle with
the radius and ulna (Fig. 15-4). This concept of lateral translocation is important in the late reconstruction of untreated fractures.
the lateral condylar epiphysis, the elbow remains reasonably stable
because the trochlea remains intact. Total coronal rotation of the
condylar fragment can occur with this injury. The axial deformity that
results is pure valgus without translocation (see Fig. 15-4).
condylar physeal injury has led to the mistaken concept that this
injury is associated with a primary dislocation of the elbow,32 which is rarely the case. The posterolateral instability of the elbow is usually a result of the injury, not a cause of it.156
injury is rare in adults. Two mechanisms have been suggested:
“push-off” and “pull-off.” The pull-off or avulsion theory has more
advocates than the push-off mechanism.85,181 In early studies,181
this injury was consistently produced in young cadavers by adducting
the forearm with the elbow extended and the forearm supinated. The work
of Jakob and Fowles85 confirmed the results of these studies. Some of Stimson’s181
work strengthens the push-off theory. In his cadaver studies, he
produced the injury by applying a sharp blow to the palm when the elbow
was flexed35; other investigators
have speculated that because the forearm goes into valgus when
extended, the radial head can push off the lateral condyle or that the
injury can result from a direct blow to the olecranon.
 |
|
FIGURE 15-3 Stages of displacement. A,B. Stage I displacement-articular surface intact. C,D. Stage II displacement-articular surface disrupted. E,F.
Stage III displacement-fragment rotated. (A, C, and E: Reprinted with permission from Jakob R, Fowles JV, Rang M, et al. Observations concerning fractures of the lateral humeral condyle in children. J Bone Joint Surg Br 1975;57:430-436.) |
injury. The more common type of fracture, which extends to the apex of
the trochlea, is probably a result of avulsion forces on the condyle,
with the olecranon’s sharp articular surface serving to direct the
force along the physeal line into the trochlea. When a child falls
forward on his or her palm with the elbow flexed, the radial head is
forced against the capitellum and may cause
the less common Milch type I physeal fracture that courses through the ossific nucleus of the capitellum.
 |
|
FIGURE 15-4 Angular deformities. A. Milch type I fractures tend only to angulate. B.
Milch type II fractures are unstable with lateral translocation in addition to angulation. (Adapted and reprinted with permission from Milch HE. Fractures and fracture-dislocations of the humeral condyles. J Trauma 1964;4:592-607.) |
of the elbow that occurs with displaced supracondylar fractures, little
distortion of the elbow, other than that produced by the fracture
hematoma, may be present with lateral condylar fractures. The key to
the clinical evaluation of this fracture is the location of soft tissue
swelling concentrated over the lateral aspect of the distal humerus.106
Stage I displacement may produce only local tenderness at the condylar
fracture site, which may be increased by forcibly flexing the wrist.
Stage II or III displacement may result in some local crepitus with
motion of the lateral condylar fragment. The benign appearance of the
elbow with some stage I and II displacements may account for the delay
of parents seeking treatment for a child with a minimally displaced
fracture.
varies according to the fracture line’s anatomic location and the
displacement stage. In the AP view, the metaphyseal flake may be small
and seemingly minimally displaced. The degree of displacement can often
be better appreciated on the true lateral view. In determining whether
the articular hinge is intact (i.e., stage I vs. stage II), the
relationship of the proximal ulna to the distal humerus is evaluated
for the presence of lateral translocation. Oblique views are especially
helpful in patients in whom a stage I displacement is suspected.
and minimally displaced fractures of the lateral condyle, Finnbogason
et al.54 identified three groups of
fractures: stable fractures, fractures with an undefinable risk, and
fractures with a high risk of later displacement. Stable fractures had
no gap or a small gap and did not extend all the way to the epiphyseal
cartilage; most of these 65 fractures were in younger children and none
had later displacement. Fractures with undefinable risk of displacement
were the same type as stable fractures, but the fracture could be
clearly observed extending all the way to the epiphyseal cartilage;
displacement occurred in 6 (17%) of these 35 fractures. High-risk
fractures had a gap that was as wide or almost as wide laterally as
medially; displacement occurred in five of 12 (42%) of these fractures.
reported that MRI evaluation of 12 minimally displaced (less than 2 mm
on radiograph) lateral condylar fractures identified five fractures
that crossed the physis into the joint space and were unstable
fractures. One of five fractures with 1-mm displacement was unstable,
and four fractures of seven with 2-mm displacement were unstable. These
investigators suggested that MRI evaluation might prevent late
displacement or delayed union by identifying those minimally displaced
fractures that required percutaneous pin fixation rather than cast
immobilization.
in the radiographic evaluation of nondisplaced or minimally displaced
lateral condylar fractures, Song et al.177
compared the oblique view to standard anteroposterior views in 54
children. They found that 38 fractures (70%) had different amounts of
displacement on the two views; 30 of these had more displacement on the
oblique view than on the AP view and eight had more displacement on the
AP view. Fracture patterns differed between the two views in 75%. These
authors recommended routine use of an internal oblique view if a
lateral condylar fracture is suspected to evaluate the amount of
fracture displacement and to assess stability.
this fracture from a fracture of the entire distal humeral physis. In a
young child in whom the condyle is unossified, an arthrogram or MRI may
be helpful (Figs. 15-5, 15-6, and 15-7).67 Potter31
recommended MRI with thin (1.5-mm to 2-mm) sections and appropriate
pulse sequencing to provide differential contrast between subchondral
bone, cartilage, and joint fluid. Chapman et al.29
recommended multidetector computed tomography (MDCT) for the evaluation
of pediatric lateral condylar fractures because it is painless and
fast, usually requiring no sedation even in very young children, and is
highly reproducible. They compared MDCT to standard radiographs in 10
children with lateral condylar fractures and found that interobserver
agreement was better with MDCT than with radiographs regarding fracture
displacement and fracture classification. Based on MDCT, fracture
management was altered in two patients with displacement near the
surgical threshold of 2 mm. Their study also suggested that cartilage
integrity can be assessed on MDCT in patients with fracture
displacement of more than 2 mm. Because of its relatively high cost
compared to standard radiographs, MDCT probably should be reserved for
evaluation of fractures in which displacement is near 2 mm so that
appropriate surgical or conservative treatment can be chosen.
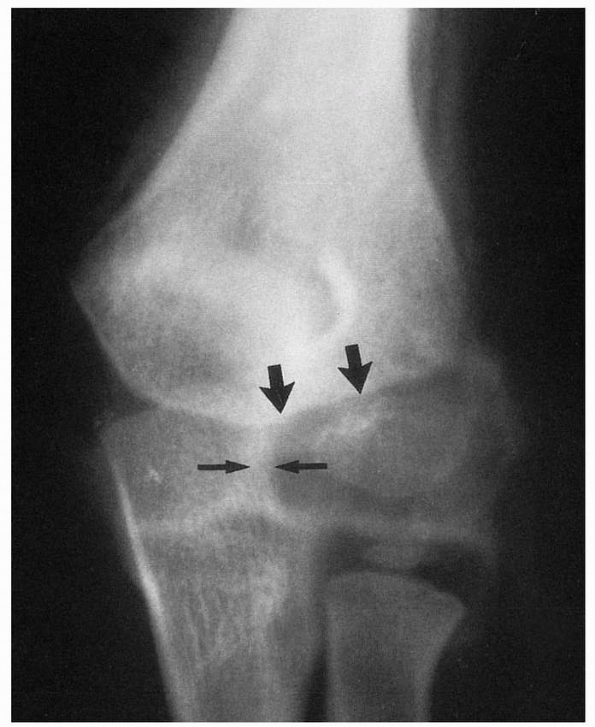
The relationship of the lateral condylar ossification center to the
proximal radius remains intact. In true fractures involving only the
lateral condylar physis, the relationship of the condylar ossification
center to the proximal radius is lost (Fig. 15-8B).
ulna is more likely to be lateral due to the loss of stability provided
by the lateral crista of the distal humerus. Treatment Methods.
Fractures involving the lateral condylar physis can be treated with
simple immobilization alone,
closed reduction and percutaneous pinning, or open surgical reduction.
 |
|
FIGURE 15-5 Unossified lateral condyle. A. AP view. A small ossific nucleus can barely be seen (arrow) in the swollen lateral soft tissues. B. An arthrogram shows the defect left by the displaced lateral condyle (open arrow). The displaced condyle is outlined in the soft tissues (solid arrow).
|
considerable intrinsic soft tissue attachments that prevent
displacement of the distal fragment. About 40% of lateral condylar
physeal fractures are sufficiently undisplaced so that they can be
treated by simple immobilization without surgical intervention.85
If the fracture line is barely perceptible on the original radiograph
(stage I displacement), the degree of displacement is usually minimal
and the chance for subsequent displacement is low. Radiographs should
be obtained weekly for the first 3 weeks after injury to ensure that
late displacement does not occur.
reported uniformly excellent results both anatomically and functionally
in patients with undisplaced fractures, none of whom had any
abnormalities of growth or premature physeal fusion. Simple
immobilization of nondisplaced or minimally displaced (less than 2 mm)
fractures in a sling, collar and cuff, or posterior splint appears
adequate.8,10,11,20,178 Close follow-up and repeat radiographs to detect any late displacement are mandatory if this method is used.
 |
|
FIGURE 15-6 Arthrogram of stage I fracture of the lateral condyle (large arrows). Articular surface is intact with no displacement (small arrows).
|
determined that only fractures with type I displacement (i.e., the
fracture line is seen on only one radiographic view) can be safely
treated nonoperatively. In their experience, any fracture with
displacement, even of less than 2 mm, can displace later in the cast or
splint. In a review of 57 fractures of the lateral condyle, Beaty and
Wood11 found that two of 24 fractures with stage I displacement displaced late. Bast, Hoffer, and Aval10
reported a union rate of 98% after nonoperative treatment of 95
nondisplaced or minimally displaced fractures of the lateral humeral
condyle. Their criteria for nonoperative treatment were acute fracture
(less than 24 hours at initial evaluation) and displacement of less
than 2 mm in three radiographic planes (AP, lateral, and internal
oblique). Two fractures that displaced 6 and 9 days after closed
reduction required open reduction and internal fixation before they
united without complications.
which fractures will displace later. The potential to displace often
depends more on the degree of associated soft tissue injury and whether
the articular cartilage of the trochlea is intact, rather than on the
amount of initial displacement. Considerable soft tissue swelling on
the lateral aspect of the distal humerus, which can be appreciated both
clinically and on radiographs, should alert the physician to the fact
that the fracture may be unstable and has the potential to displace. If
crepitus between the fragments is detected with motion of the forearm
or elbow, significant loss of soft tissue attachments and a potentially
unstable fracture should be suspected.35
 |
|
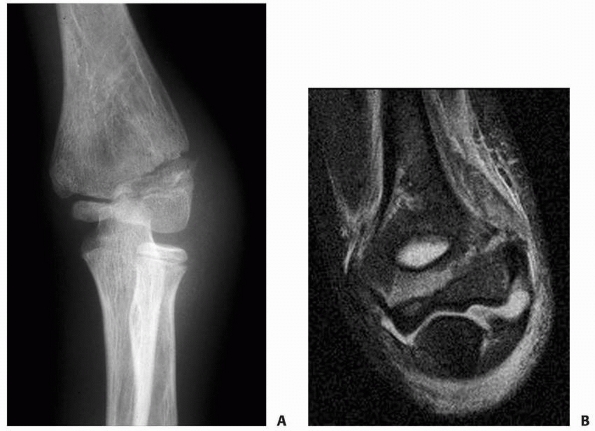
FIGURE 15-7 A. Radiograph of a stable type II fracture of the lateral condyle in a 10-year-old child. B. Gradient-echo MRI clearly differentiates this fracture from a fracture of the entire distal humeral physis.
|
reduction, with the recommended elbow position ranging from
hyperflexion to full extension; however, it appears from clinical
experience and experimental studies that reduction is best achieved
with the forearm supinated and the elbow extended. Placing a varus
stress on the extended elbow allows further room for manipulation of
the fragment. Unfortunately, it is difficult to maintain reduction of a
displaced lateral condylar fracture with closed techniques, and closed
reduction is not recommended for treating stage III displaced lateral
condylar fractures. Minimally displaced fractures can be stabilized
with percutaneous pins across the fracture. In lateral condylar physeal
fractures with moderate displacement, confirmation of fracture
stability by stress testing and arthrography may precede percutaneous
pin fixation. Mintzer et al.121
reported good results after percutaneous pin fixation of 12 lateral
condylar fractures with displacement of more than 2 mm. They believed
this method is
appropriate
for selected fractures with 2 mm to 4 mm of displacement and an
arthrographically demonstrated congruent joint surface. If a
satisfactory reduction cannot be obtained, then reduction should be
achieved and maintained by open reduction and internal fixation.
 |
|
FIGURE 15-8 A. Total distal humeral physeal fracture in a 2-year-old. The lateral condyle (closed arrow) has remained in line with the proximal radius. The proximal radius, ulna, and lateral condyle have all shifted medially (open arrow). B. Displaced fracture of the lateral condyle in a 2-year-old. The relationship of the lateral condyle (closed arrow) to the proximal radius is lost. Both the proximal radius and ulna (open arrow) have shifted slightly laterally.
|
reported good results in 46 (73%) of 63 unstable lateral condylar
fractures, 53 of which were treated with closed reduction and
percutaneous pinning. They formulated a treatment algorithm based on a
five-stage classification system that considered degree of displacement
and fracture pattern. Closed reduction was attempted in all fractures,
regardless of the amount of displacement. If closed reduction up to 2
mm failed, open reduction and internal fixation were performed. These
authors suggested that open reduction is not necessary for all lateral
condylar fractures with no less than 2 mm of displacement and rotation
of the fragment (stage V in their classification), noting excellent
results in three such fractures treated with closed reduction and
pinning. They listed three elements as essential to obtaining good
results with this treatment protocol: (i) accurate interpretation of
the direction of fracture displacement (mainly posterolaterally, not
purely laterally) and the amount of displacement of the fracture
fragment, (ii) routine intraoperative confirmation of the reduction on
both anteroposterior and internal oblique radiographs, and (iii)
maintenance of the reduction with two parallel percutaneous Kirschner
wires (K-wires).
Pinning. To avoid the dissection required for open reduction and
anatomic reduction, arthroscopic techniques have been used to reduce
the lateral condylar fracture before the insertion of percutaneous pins.26,76 Micheli et al.,118
in an earlier study, established the safety and efficacy of elbow
arthroscopy in pediatric and adolescent patients with osteochondrosis
dissecans, arthrofibrosis, synovitis, acute trauma, and posterior
olecranon impingement syndrome. None of their 47 patients had nerve
injury, infection, or loss of elbow motion after arthroscopy. Hausman
et al.76 reported arthroscopic
reduction and percutaneous pinning of six fractures of the lateral
humeral condyle in patients ranging from 2 to 6 years old. All
fractures healed within 4 weeks, and all patients had full active and
passive ranges of motion and were pain-free at latest evaluation
(average 8 months). These authors76
cited as advantages to the arthroscopic technique improved
visualization of the fracture reduction over uniplanar arthrography,
the ability to remove fragments from the fracture site, more direct
assistance in fracture reduction than that provided by closed
reduction, and less dissection than with open reduction. Standard
anterolateral and anteromedial arthroscopic portals are used, and
K-wires are used as joysticks to reduce the fracture. A 2.5-mm wrist
arthroscope may be needed in small patients (usually younger than 3
years), but in older children and adolescents, a standard 4.5-mm
arthroscope can be used.
cosmetic results with closed reduction methods, open reduction has
become the most widely advocated method for unstable fractures with
stage II displacement and fractures with stage III displacement.6,19,20,32,73,85,87,113,125,174,193,201,208 In a study of 97 children with minimally displaced lateral condylar fractures, Launay et al.99
found that immobilization alone resulted in additional displacement and
more nonunions than did operative treatment. About 60% of all fractures
involving the lateral condylar physis require open reduction and
internal fixation.85 There is
uniform agreement regarding the need for open reduction of displaced
fractures of the lateral condylar physis. Most investigators recommend
fixation with smooth K-wires in children or screws in adolescents
nearing skeletal maturity. Parent et al.,139
in a biomechanical study, compared compression and stability in
simulated lateral condylar fractures fixed with a tension band
technique using wire or bioabsorbable sutures. Although the suture
tension bands had lower ultimate failure loads and less compression at
the fracture site, the authors suggested that fixation with
bioabsorbable sutures might be appropriate for small children to avoid
the need for surgery to remove fixation materials.139
believed that at least two pins were necessary to prevent rotation. The
passage of a smooth wire through the physis does not result in any
growth disturbance,51,105
which is of note because only 20% of the humerus’ growth occurs through
the distal humeral physis. It also appears that the wires can be placed
either parallel or crossed in the distal fragments.
fragment. They should cross at the lateral aspect of the metaphysis and
diverge as much as possible to enhance the stability of fixation. If
there is only a small metaphyseal fragment, the pins can be placed
across the physis without concern.
carried out early (i.e., within the first few days after the injury),
the results are uniformly good. The key, however, is to be sure that
the reduction is adequate. Hardacre et al.73
found that poor results after open reduction occurred when the
reduction was incomplete. Surgery alone does not ensure a good result
unless the reduction is nearly anatomic and the fixation is secure.
organization of the clot with early fibrin development makes it
difficult to achieve a reduction without extensive soft tissue
dissection in fractures that are treated late. The pins can be buried
or left protruding through the skin with a low incidence of infection.
Leaving pins buried requires a second operative procedure, even though
it usually can be accomplished with a local anesthetic. The fracture
generally is sufficiently stable to allow pin removal by 3 to 4 weeks
and to allow the patient to begin protected active range of elbow
motion at 2 to 3 weeks.
reported painless, full range of elbow motion in 36 of 37 children who
had displaced (more than 2 mm in any direction) lateral condylar
fractures fixed with partially threaded 4-mm AO cancellous screws. One
patient had delayed union, with loss of 10 degrees of elbow motion.
fragment on AP and lateral views) and the clinical signs also indicate
there is reasonable soft tissue integrity, we simply immobilize the
elbow in a long-arm cast with the forearm in neutral rotation and the
elbow flexed 60 to 90 degrees. Radiographs are taken within the first 3
to 5 days after the fracture with the cast removed and the elbow
comfortably extended. If there is no displacement, the radiographs are
repeated in another 3 to 5 days. If the radiographs again show no
displacement, then another long-arm cast is applied and is worn for
about 3 to 5 weeks, or until fracture union is apparent.
displacement (type II injury), the fracture pattern is such that the
articular cartilage appears intact. If there is any question about the
stability at the time of the fracture, MRI can be obtained or the
extremity can be examined with the patient under general anesthesia.
Gentle varus stress views with the forearm supinated and the elbow
extended should be taken to determine if the fracture displaces
significantly. Preoperative MRI or intraoperative arthrography can be
used to determine the stability of the nonossified articular cartilage
of the trochlea.
varus stress views should be obtained and arthrography should be done
with the patient under anesthesia. If the fracture is stable,
percutaneous pinning is indicated (Fig. 15-9).
internal fixation are indicated. We prefer open reduction and internal
fixation of all fractures with stage III displacement. It is important
that open reduction is performed as soon as possible after the injury.
The standard lateral Kocher approach provides sufficient exposure of
the fragment. Often, a tear in the aponeurosis of the brachioradialis
muscle laterally leads directly to the fracture site. Extreme care must
be taken to avoid dissecting near the posterior portion of the fragment
because this is the entrance of the blood supply of the lateral
condylar epiphysis.
 |
|
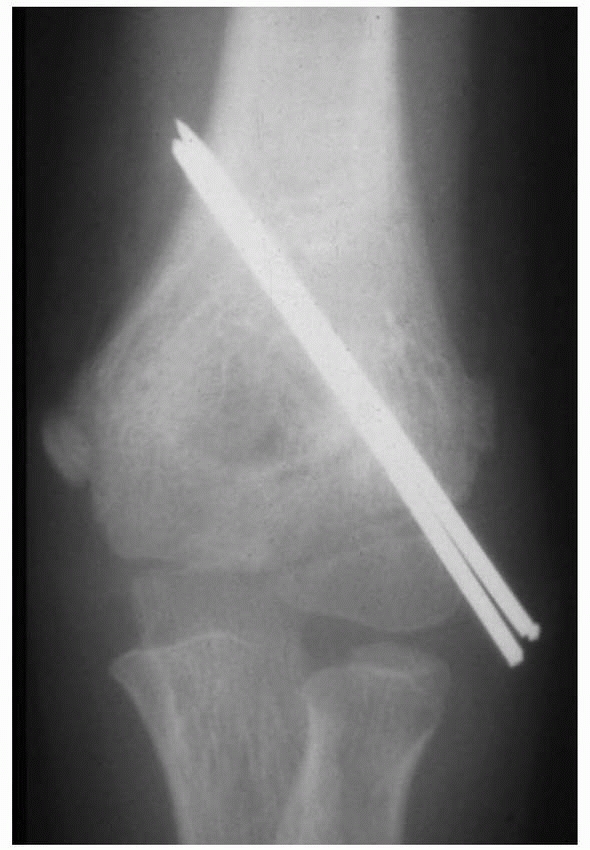
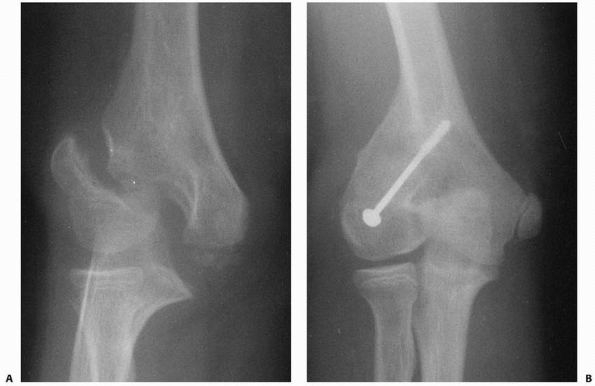
FIGURE 15-9 Stage II fracture of the lateral condyle. A.
AP radiograph shows 4 mm of displacement of the metaphyseal segment; however, the fracture was stable by stress examination and arthrography. B. Four weeks after percutaneous pinning, the fracture is healed. |
recommended a posterolateral approach because of the excellent exposure
it provides with minimal dissection. Another suggested advantage is the
improved cosmetic results by more posterior placement of the surgical
scar. Mohan et al.124 reported no complications in 20 patients in whom this approach was used.
the fracture line along the anterior aspect of the articular surfaces.
This usually can be determined either by direct vision or by digital
palpation. We prefer to use smooth K-wires that cross just medial to
the condylar fragment to maintain the reduction (Fig. 15-10).
The wires penetrate the skin through a separate stab incision posterior
to the main incision. A long-arm cast is applied with the elbow flexed
60 to 90 degrees and the forearm in neutral or slight pronation. The
cast and pins are removed in 3 weeks if there is adequate healing on
radiographs. Early active motion is started at that time. If necessary,
pin removal can be delayed 1 to 2 weeks to allow further healing in
older children.
third distal (Fig. 15-11).
In the interval between the brachioradialis and the triceps, the
dissection is carried down to the lateral humeral condyle. The joint’s
anterior surfaces are exposed by separating the fibers of the common
extensor muscle mass. Soft tissue detachment is limited to only that
necessary to expose the fragment, the fracture, and the joint; the
posterior soft tissues are left intact. Retracting the antecubital
structures exposes the anterior joint surface. The trochlea and the
more medial entry point of the condylar fracture are inspected. The
displacement and the size of the fragment are always greater than is
apparent on the radiographs because much of the fragment is
cartilaginous. The fragment usually is rotated as well as displaced.
The joint is irrigated to remove blood clots and debris, the articular
surface and the metaphyseal fragment are reduced accurately, and the
reduction is confirmed by observing the articular surface, particularly
at the trochlea. The position is held with a small tenaculum, bone
holder, or towel clip. When a large metaphyseal fragment is present,
two smooth K-wires are inserted across it into the medial portion of
the metaphysis. When the epiphyseal portion is small, as is more
common, two smooth K-wires are inserted through the condyle, across the
physis, and into the humeral metaphysis, penetrating the medial cortex
of the humerus. The wires are directed 45 to 60 degrees; the reduction
and the position of the internal fixation are checked by AP and lateral
radiographs before closing the wound. The ends of the wires are cut off
beneath the skin but are left long enough to allow easy removal. The
arm is placed in a posterior plaster splint with the elbow flexed 60 to
90 degrees.
 |
|
FIGURE 15-10 Fixation of lateral condylar fracture with two smooth K-wires, crossing just medial to the condylar fragment.
|
 |
|
FIGURE 15-11
Lateral approach for open reduction and internal fixation of a lateral humeral condylar fracture of the left elbow. The approach is made through the brachioradialis-triceps interval; an anterior retractor is used to expose the joint surfaces, and the fracture is reduced and pinned percutaneously posterior to the incision. |
pins can be removed at 3 weeks if union is progressing. Gentle active
motion of the elbow is then usually resumed and continued until full
range of motion returns.
these fractures may go untreated or unrecognized for a prolonged
period. Even in modern medical settings, elbow injuries may be treated
as “sprains,” and the diagnosis of a displaced lateral condylar
fracture is not made. Thus, patients often present months or even years
later with a nonunited or malunited fracture fragment.
malunion, occurs in a fracture in which the fracture fragments are in
satisfactory position but union of the lateral condylar fragment to the
metaphysis is delayed. Various reasons have been suggested for delayed
union of lateral condylar fractures. Flynn and Richards56 speculated that it was caused by poor circulation to the metaphyseal fragment. Hardacre et al.73
believed that bathing the fracture site by articular fluid inhibited
fibrin formation and subsequent callus formation. It is most likely
that a combination of these two factors, in addition to the constant
tension forces exerted by the muscle arising from the condylar
fragment, is responsible for delayed union.
nonoperatively. The symptoms and clinical examination determine the
aggressiveness of treatment. The fragment is usually stable during
clinical examination, the elbow is nontender, and the range of elbow
motion increases progressively. On radiographs, the position of the
fragment remains unchanged. With time, these fractures usually heal (Fig. 15-12).
Lateral spur formation or cubitus varus is relatively common with these
fractures. The need for further treatment depends on the presence of
significant symptoms or further displacement that may disrupt the joint
surface and cause functional impairment. If neither of these conditions
is present, the radiographic persistence of the fracture line requires
only follow-up observation. If there is any question as to the
integrity of the joint surface, an MRI may
help determine any loss of continuity and the need for surgical treatment as a nonunion rather than a simple delayed union.
 |
|
FIGURE 15-12 Delayed union and cubitus varus. A. Stage III lateral condylar fracture in a 7-year-old boy was treated in a cast. B. Seven months later, delayed union with malunion of the fracture and cubitus varus deformity was present.
|
recommended long-term immobilization for minimally displaced fractures
with delayed union. They found that 70% of minimally displaced
fractures had united by 12 weeks. Jeffrey87 recommended screw fixation with bone grafting. Hardacre et al.,73
however, found that minimally displaced fractures with delayed union
ultimately united if there was no significant displacement of the
condylar fragment.
improved by a late open reduction and internal fixation of the fracture
fragment. Delayed open reduction has been complicated by osteonecrosis
and further loss of elbow motion. Speed and Macey178
were among the first investigators to question whether patients treated
with late surgery did better than those not treated. In patients with
malunion who were treated late, they found a high incidence of poor
results due to “epiphyseal changes” that probably represented
osteonecrosis. There have been many subsequent reports of osteonecrosis
occurring after late open reduction. The high incidence of
osteonecrosis of the fragment is believed to be due to the extensive
soft tissue dissection necessary to replace the fragment (Fig. 15-13). Böhler,20
on the other hand, had good results in his patients with delayed
treatment. He avoided extensive soft tissue dissection by approaching
the fragment transarticularly after performing an osteotomy of the
olecranon. Yang et al.205 used
Böhler’s technique in six children with Milch type II lateral condylar
fractures with displacement of more than 10 mm, rotation of the
fragments, and abundant callus formation. The delay from injury to
surgery averaged 4 months and ranged from 2 to 5 months. All fractures
and osteotomies united within 3 months of surgery. Four children had
excellent functional results and two had good results; all were
pain-free.
course of the blood supply to the lateral condyle. Only a small portion
of the condyle is extra-articular. In his studies, Haraldsson71
found that the vessels that supply the lateral condylar epiphysis
penetrate the condyle in a small posterior nonarticular area (Fig. 15-14).
reported that patients treated later than 3 weeks after the fracture
did no better than those who received no treatment at all. They found
that early callus and fibrous tissue made it extremely difficult to
obtain a satisfactory open reduction without performing considerable
soft tissue dissection. All their patients treated after 3 weeks lost
range of motion (at least 34 degrees on average), and osteonecrosis,
premature physeal closure, as well as valgus deformity were common. In
patients who received no treatment, valgus deformity due to nonunion
and malunion was frequent, but no osteonecrosis of the lateral condylar
epiphysis occurred. These investigators recommended that no open
reduction should be performed for fractures older than 3 weeks, but
that early ulnar nerve transposition should be performed to eliminate
the possibility of late ulnar nerve symptoms that occur with cubitus
valgus deformity after nonunion. Dhillon et al.41 and Zionts and Stolz211 also reported that osteonecrosis was frequent after late open reduction and recommended no treatment for these fractures.
drew attention to the development of nonunion after lateral humeral
condylar fractures when he described his findings in two cadaver
specimens. He pointed out that there was absolutely no bony continuity
between the distal humerus and the condylar fragment. True nonunion
with significant deformity is rare because it usually is the result of
a nontreated displaced fracture of the lateral condylar physis.19,113
displacement of the fragment. The mobile fragment can be palpated, or
the patient has weakness or pain in the elbow. According to the
criteria of Flynn et al.,55 if the fracture has not united by 12 weeks, it is classified as a nonunion.
 |
|
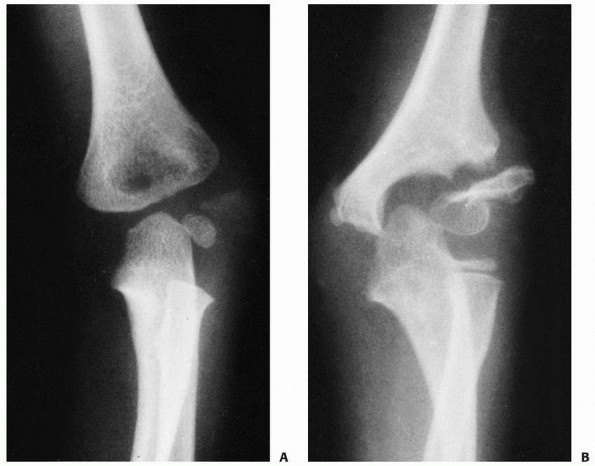
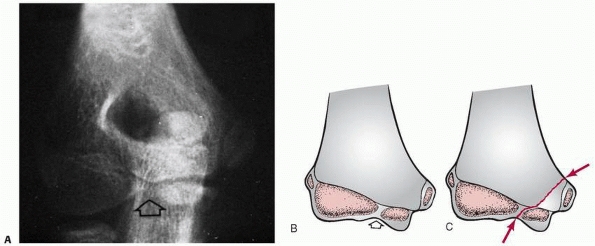
FIGURE 15-13 Osteonecrosis of the lateral condyle after lateral condylar fracture in a 10-year-old boy. AP (A) and lateral (B) radiographs.
|
 |
|
FIGURE 15-14
Asymptomatic nonunion of a lateral condyle in a 19-year-old military recruit. Because the patient had a completely normal and asymptomatic range of motion in his nondominant extremity, operative stabilization was not thought to be necessary. |
Many patients with nonunions and minimal fragment displacement have no
angulation and remain relatively asymptomatic for normal activities
(see Fig. 15-14). Others have weakness or
symptoms when the arm is used for high-performance activities. Because
they are not significantly displaced, these fractures can often be
stabilized with minimal extra-articular dissection using a combination
of screw fixation and a laterally placed bone graft.
common after unstable fractures with stage II and III displacement. If
the fragment becomes free, it tends to migrate proximally with a
subsequent valgus elbow deformity. Nonunion can lead to a cubitus
valgus deformity, which in turn, is associated with the development of
a tardy ulnar nerve palsy.
displaced enough to allow the condylar fragment’s cartilaginous
articular surface to oppose the bony surface of the humeral metaphysis.
In such a situation, union is impossible. Flynn and Richards55
reported successful treatment of nonunion 9 months to 3 years after
fracture and strongly advised early surgery for established nonunion
when the condylar fragment is in “good position” in a child with open
physes. Papandrea and Waters133
recommended stable internal fixation with percutaneously placed pins or
cannulated screws for early (less than 12 weeks), minimally displaced
nonunions. For late displaced nonunions, they recommended staged
procedures: ulnar nerve transposition and bone grafting and fixation in
situ of the lateral condyle followed by osteotomy to correct angulation
once the nonunion is healed and elbow range of motion is regained.
The fragment migrates both proximally and laterally, giving not only an
angular deformity but also lateral translocation of the proximal radius
and ulna (Fig. 15-15). Milch119
noted that lateral translocation is not as likely to develop in the
more lateral type of these fractures (Milch type I) because the lateral
crista of the trochlea is intact (Fig. 15-16).
 |
|
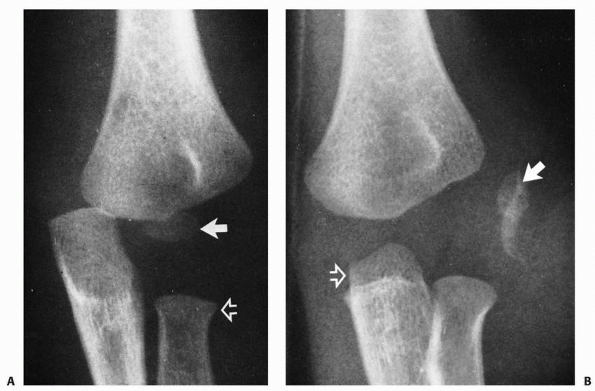
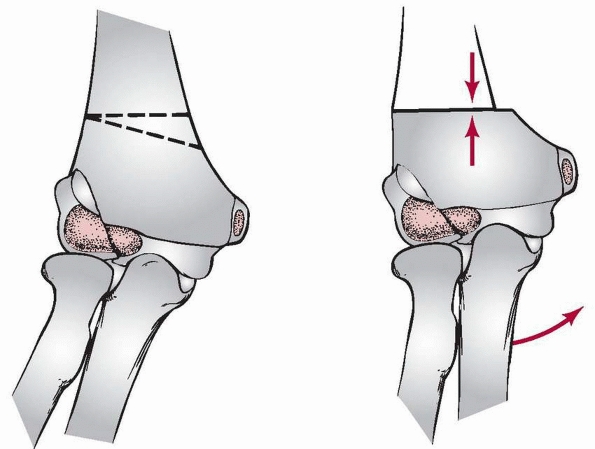
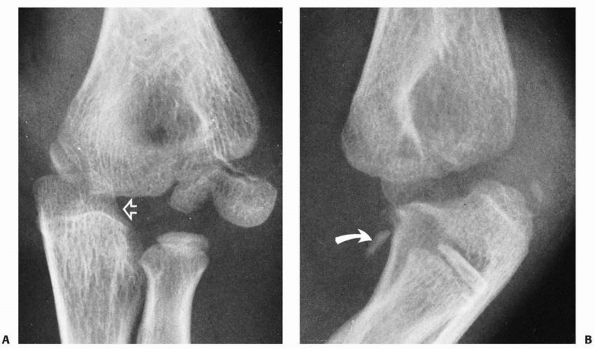
FIGURE 15-15 A. A 10-year-old boy with cubitus valgus resulting from a fracture of the lateral condylar physis with nonunion. B.
Nonunion with cubitus valgus. Radiograph showing both angulation and translocation secondary to nonunion of the condylar fragment. |
 |
|
FIGURE 15-16
Nonunion without translocation. Milch type I fracture pattern. Despite nonunion, elbow stability was maintained because the lateral crista of the trochlea had remained intact (arrow). Valgus angulation also developed. |
lateral condylar fragment is difficult and requires correcting two
problems. First, articular cartilage may be opposing the distal humeral
metaphysis, and union seldom can be obtained without mobilizing the
fragments and applying an internal compressive device. The second
problem is correcting the angular deformity (Fig. 15-17).
reported excellent or good results in 15 of 16 patients at an average
follow-up of 11 years after osteosynthesis for nonunion of fractures of
the lateral humeral condyle. The one patient with a poor result had
evidence of osteonecrosis
of
the fragment. The average interval between injury and osteosynthesis
was 5 years (range, 5 months to 10 years). To prevent progression of
cubitus valgus deformity and subsequent ulnar nerve dysfunction,
Shimada et al.166
recommended osteosynthesis for nonunion of lateral humeral condylar
fractures in children because union is easily achieved, the range of
motion is maintained, ulnar nerve function usually returns, and
remodeling of the articular surfaces can be expected. They noted that
bone grafting is essential to bridge the defect, to obtain congruity of
the joint, and to promote union; damage to the blood supply should be
avoided to prevent osteonecrosis. Wattenbarger et al.196
described late (>3 weeks) open reduction and internal fixation of
lateral condylar fractures in 11 children, 10 of whom had nonunions and
one a malunion. Of the nine children available for follow-up, seven had
good results and two had fair results. To avoid the development of
osteonecrosis, the authors accepted malreduction rather than stripping
the soft tissue off the lateral condylar fragment to achieve a more
anatomic reduction. For fractures with more than 1 cm of displacement,
the position of the fragment often was improved very little by surgery,
but all fractures united, alignment of the arm was good, and no child
had developed osteonecrosis at an average 6-year follow-up.
 |
|
FIGURE 15-17
In the Milch type I fracture pattern, there is only an angular deformity that can be easily corrected with a closing wedge osteotomy. (Adapted and reprinted with permission from Milch HE. Fractures and fracture-dislocations of the humeral condyles. J Trauma 1964;4: 592-607.) |
described a technique that includes in situ compression fixation of the
lateral condylar nonunion and a dome-shaped supracondylar osteotomy of
the distal humerus through a single posterior incision. In their eight
patients (average age: 8.6 years), the average interval between
fracture and surgery was 5 years. All eight nonunions healed within 3
months, as did all of the supracondylar dome osteotomies. At 4.5-year
follow-up, results were excellent in two patients, good in four, and
fair in two. The authors recommended this procedure for minimally
displaced, established lateral condylar nonunions with a cubitus valgus
deformity of 20 degrees or more, especially when the deformity is
progressing or is complicated by a concurrent ulnar neuropathy or is in
patients with elbow instability or elbow pain during sports activities.
They listed as a contraindication to the procedure a lateral condylar
nonunion associated with radiographic evidence of prominent
displacement and rotation. In situ fixation of the nonunion is
recommended because the extensive soft tissue stripping required for
mobilization and reduction of the fracture fragments results in
devascularization of the fragment, which can cause osteonecrosis, loss
of motion, and persistent nonunion.
to 14 days after injury) and established nonunions (usually from 3
months to several years after injury). If we believe that we can obtain
fracture union without loss of elbow motion and avoid osteonecrosis of
the lateral condyle, then we recommend surgery for selected patients.
condylar fracture poses a difficult dilemma. If no treatment is
rendered, a progressive cubitus valgus deformity may occur with growth.
Patients are usually asymptomatic except for those with high-demand
athletic or labor activities. A mild flexion contracture of the elbow
is present, but the cubitus valgus deformity is more cosmetic than
functional. The danger in this approach is failure to recognize and
treat early a tardy ulnar nerve palsy. If surgery is performed for an
established nonunion, the potential risks of osteonecrosis and loss of
elbow motion must be carefully considered.
-
A large metaphyseal fragment
-
Displacement of less than 1 cm from the joint surface
-
An open, viable lateral condylar physis
clinical situations. First, for an established nonunion with a large
metaphyseal fragment, minimal migration, and an open lateral condylar
physis, we recommend modified open reduction, screw fixation, and a
lateral extra-articular iliac crest bone graft. This technique is
markedly different from the surgical treatment of an acute lateral
condylar fracture. The metaphyseal fragment of the lateral condyle and
the distal humeral metaphysis are exposed, but no attempt is made to
realign the articular surface. Intra-articular dissection should be
avoided to help prevent any further loss of elbow motion. The
metaphyseal fragments are débrided by gently removing any interposed
fibrous tissue. The lateral condylar fragment can usually be moved
distally a small distance. The metaphyseal fragments are firmly
apposed, and a cancellous or cortical screw is used to fix the
fragments with interfragmentary compression. Iliac crest bone graft can
be placed between the metaphyseal fragments and laterally. The elbow is
immobilized in 80 to 90 degrees of flexion for 3 to 4 weeks (Fig. 15-18).
concerns but no functional complaints, treatment is similar to that for
cubitus varus deformity after a supracondylar humeral fracture. If the
patient and family desire, a supracondylar osteotomy can be performed.110
Rigid internal fixation should be used to allow early motion. Late
osteosynthesis of the lateral condyle is rarely indicated in an
adolescent or young adult with high functional demands and symptoms of
instability.
valgus deformity, and symptomatic tardy ulnar nerve palsy should be
treated with anterior transposition of the ulnar nerve.
maintained with solid fixation, results are uniformly good. In
supracondylar fractures, an incomplete reduction may result in a
cosmetic deformity, but functional results are generally good. In
displaced fractures of the lateral condylar physis, a marginal
reduction can result in both cosmetic deformities and functional loss
of motion.179 The complications that
affect the outcome can be classified as either biologic or technical.
Biologic problems occur as a result of the healing process, even if a
perfect reduction is obtained. These problems include spur formation
with pseudocubitus varus or a true cubitus varus. The technical
problems usually arise from management errors and result in nonunion or
malunion with or without valgus angulation and osteonecrosis.
Other technical problems can arise from the injury itself, including neurologic injuries and myositis ossificans.
 |
|
FIGURE 15-18 A. Established nonunion with a large metaphyseal fragment. B. After fixation with a cancellous screw and bone grafting of the metaphyseal fragment.
|
is one of the most common deformities after a fracture involving the
lateral condylar physis. Cotton35
believed that it is caused by coronal rotation of the distal fragment,
which tends to displace the flap of periosteum associated with the
distal fragment laterally. This periosteum then produces new bone
formation in the form of a spur.
treatment. After nonoperative treatment, it results from the minimal
displacement of the metaphyseal fragment and usually has a smooth
outline. In patients with no real change in carrying angle, the lateral
prominence of the spur may produce an appearance of mild cubitus varus
(pseudovarus). In patients in whom a true cubitus varus develops, the
presence of the lateral spur accentuates the varus alignment (Fig. 15-19A,B).
The spur that occurs after operative treatment has a more irregular
outline and is usually the result of hypertrophic bone formation from
extensive dissection at the time of open reduction and internal
fixation. During open reduction, care should be taken to limit the
aggressiveness of the dissection and to carefully replace the lateral
periosteal flap of the metaphyseal fragment.
parents may be told that either lateral overgrowth with mild cubitus
varus or lateral spur may develop, regardless of the treatment method.
They should be told that this mild deformity is usually not of cosmetic
or functional significance.
show that a surprising number heal with some residual cubitus varus
angulation.58,78,113,126,158,171,175,191 In some series, the incidence of cubitus varus is as high as 40%,58,175 and the deformity seems to be as frequent after operative treatment as after nonoperative treatment.158,175 Skak et al.171
reported visible varus deformities in six and valgus deformities in
three of 28 children with displaced lateral condylar fractures. All
patients with a valgus tilt of the joint surface were younger than 9
years of age at the time of injury. These investigators concluded that
reduced growth potential at the trochlear groove is a regular
complication of Milch type III fractures. The exact cause is not
completely understood. In some instances, it is probably a combination
of both an inadequate reduction and growth stimulation of the lateral
condylar physis from the fracture insult (Fig. 15-20).175
cause concern or require further treatment. This is probably because it
is a pure coronal varus angulation and does not have the horizontal
anterior rotation of the lateral condyle along with the sagittal
extension that makes the cubitus varus that occurs after supracondylar
fractures such an unacceptable deformity. Some investigators have noted
that children with cubitus varus deformities have pain, decreased range
of motion, epicondylitis, and problems with sports such as sidearm
pitching, swimming, judo, and pushups. Davids et al.37
reported lateral condylar fractures in six children with pre-existing
cubitus varus deformities from previous elbow fractures, usually
supracondylar humeral fractures. They concluded that posttraumatic
cubitus varus deformity may predispose a child to subsequent lateral
condylar fracture and should be viewed as more than just a cosmetic
deformity. They recommended valgus supracondylar osteotomy of the
distal humerus.
been reported to result from premature epiphysiodesis of the lateral condylar physis.193 As with cubitus varus, it is usually minimal and is rarely of clinical or functional significance. Piskin et al.,145
however, described cubitus valgus deformity after lateral condylar
fractures in eight adolescent patients who were treated with osteotomy
and gradual distraction using the Ilizarov method. They cited as
advantages to this method an ability to adjust the position of the
distal fragment in all planes, immediate mobilization, which prevents
elbow stiffness, and avoidance of an unsightly scar. Two patients with
tardy ulnar nerve palsies did not have anterior nerve transposition
before frame application and the ulnar nerve palsy persisted despite
correction of the deformity, leading the authors to recommend routine
nerve transposition before frame application.
 |
|
FIGURE 15-19 Spur formation. A.
Follow-up radiograph of a boy whose lateral condylar fracture was treated nonoperatively. The periosteal flap produced a spur on the lateral aspect of the metaphysis (arrow). This fracture healed with a mild varus angulation as well. B. Clinically, the spur accentuated the lateral prominence (arrow) of the elbow, which in turn accentuated the mild valgus angulation. C. Considerable soft tissue dissection was performed in the process of open reduction of this lateral condylar fracture. D. At 2 months postsurgery, there is a large irregular spur formation secondary to periosteal new bone formation from the extensive dissection. (From Wilkins KE. Residuals of elbow fractures. Orthop Clin N Am 1990;21:289-312, with permission.) |
 |
|
FIGURE 15-20 True varus. A. The injury film with a minimally displaced fracture (arrow). This 5-year-old child was treated with simple immobilization until the fracture was healed. B. Five years later, the patient had a persistent cubitus varus (arrow)
that remained clinically apparent. The carrying angle of the uninjured right elbow measured 5 degrees of valgus; the injured elbow had 10 degrees of varus. (From Wilkins KE. Residuals of elbow trauma in children. Orthop Clin N Am 1990;21:289-312, with permission.) |
“fishtail deformity” of the distal humerus may occur. The first, a
sharpangled wedge, commonly occurs after fractures of the lateral
condyle (Fig. 15-21). It is believed that this
type of malformation is caused by persistence of a gap between the
lateral condylar physis ossification center and the medial ossification
of the trochlea.193,201
Because of this gap, the lateral crista of the trochlea may be
underdeveloped, which may represent a small “bony bar” in the distal
humeral physis.78 Despite some reports of loss of elbow motion with this type of fishtail deformity,193 most investigators8,11,41,58 have not found this type of radiographic deformity to produce any functional deficiency. Nwakama et al.130
reported four patients (average age: 5 years) with fishtail deformities
accompanied by premature closure of a portion of the distal humeral
physis with resultant deformity, length retardation, decreased elbow
motion, and functional impairment. Kim et al.95
reviewed the records of 18 children in whom trochlear deformities
developed after distal humeral fractures (12 transcondylar or
transphyseal, five supracondylar, one lateral condylar) and found that
17 of the 18 had cubitus varus deformities (varus angulation from 2 to
18 degrees). Bony defects in the medial and central trochlea were
evident on radiographs as early as 1 month after injury (average: 3.4
months). At intermediate follow-up, eight of 10 patients evaluated had
no progression of their deformities, and none of the five patients seen
at long-term follow-up (more than 10 years) had progression.
smooth curve. It is usually believed to be associated with
osteonecrosis of the lateral part of the medial crista of the trochlea.126 The mechanisms of the development of this type of deformity are discussed in the section on osteonecrosis of the trochlea.
neuropathy involving the ulnar nerve (the so-called tardy ulnar nerve palsy).
 |
|
FIGURE 15-21
An angular “fishtail” deformity that persisted in this 14-year-old boy after operative treatment of a lateral condylar fracture, which occured 6 years previously. |
reported two patients with posterior interosseous nerve injury after
open reductions of the lateral condylar fragment, both of whom
recovered spontaneously. McDonnell and Wilson113 reported a case of transient radial nerve paralysis after an acute injury.
reported a delayed radial nerve laceration from the tip of the screw
that was used to stabilize a lateral condylar fracture 26 years
earlier. This occurred when the patient sustained a hyperextension
injury to the elbow.
Tardy ulnar nerve palsy as a late complication of fractures of the
lateral condylar physis is well known, especially after the development
of cubitus valgus from malunion or nonunion of fractures of the lateral
condylar physis.65 The symptoms are usually gradual in onset. Motor loss occurs first, with sensory changes developing somewhat later.65 In Gay and Love’s65 series of 100 patients, the average interval of onset was 22 years.
from anterior transposition of the ulnar nerve (originally the most
commonly used procedure) to simple relief of the cubital tunnel. We
prefer simple subcutaneous anterior transposition of the nerve.
fusion of the various secondary ossification centers to each other,
with little or no deformity. Such a situation occurs much later than
the original fracture. This phenomenon probably occurs because the
fracture stimulates the ossification centers to grow more rapidly, and
thus they reach maturity sooner; it is rarely caused by inadvertent
dissection in the lateral condylar physis. Because only 20% of humeral
growth occurs in the distal physis, physeal arrest seldom causes any
significant angular or length deformities.
 |
|
FIGURE 15-22 A.
Injury film of a 7-year-old who sustained a Milch type I lateral condylar fracture. This patient was treated with cast immobilization alone. B. Radiograph taken 2 years later showed complete fusion of the condylar epiphysis to the metaphysis, with the development of a “bifid” condyle. |
Cubitus valgus has been reported to occur as a result of malunion of
the fracture fragments.193 Malunion of a Milch type I fracture pattern can result in the development of a bifid lateral condyle (Fig. 15-22).
No reliable operative treatment has been described to re-establish the
congruity of the articular surfaces in condylar malunions, and they are
probably best left untreated. We have seen several patients with
malunions in which the lateral condyle rotates in the coronal plane,
with subsequent cubitus varus deformity.
and is most commonly associated with the extensive dissection necessary
to effect a late reduction or from loss of the blood supply at the time
of injury.73,85,113 Wilson,201
however, described partial osteonecrosis in an essentially nondisplaced
fracture of the lateral condylar physis that had a radiographic
appearance and clinical course similar to those of osteochondritis
dissecans. Osteonecrosis is rare in fractures of the lateral condylar
physis that receive little or no initial treatment and result in
nonunion.85,203
much like Legg-Calveé-Perthes disease in the hip. Any residual deformity is usually related to loss of motion.
 |
|
FIGURE 15-23
Osteonecrosis and nonunion developed in this child after extensive dissection and difficulty in obtaining a primary open reduction. A. Injury film. B. Two years later, there was extensive bone loss in the metaphysis and a nonunion of the condyle. |
and fractures of the medial epicondyle. Often, an elbow dislocation is
misdiagnosed in a patient with a lateral condylar fracture. Loss of the
lateral crista can make the elbow unstable and allow the proximal
radius or ulna to translocate laterally. This is a part of a normal
pathologic condition associated with completely displaced lateral
condylar fractures. In a true elbow dislocation, the proximal radius
and ulna are displaced not only medially or laterally but also
proximally (Fig. 15-24).
 |
|
FIGURE 15-24 Ipsilateral injury. A. AP radiograph of an 8-year-old boy with a true posteromedial elbow dislocation (open arrow) and a Milch type I lateral condylar fracture. B. A small fracture of the coronoid process of the ulna (closed arrow) confirms the primary nature of the elbow dislocation on the lateral radiograph.
|
articular surface of the lateral condyle. This includes, in some
instances, the
articular
surface of the lateral crista of the trochlea. Generally, this fragment
comes from the anterior portion of the distal articular surface. In
adults, these fractures are not uncommon, but they are rare in
children. In their review of 2000 elbow fractures in children, Marion
and Faysse108 found only one fracture of the capitellum. Since then, this fracture has been frequently reported in older adolescents.60,88,105,108,132 Marion and Faysse108
pointed out that verified fractures of the capitellum have not been
described in children under 12 years of age. There have been two
reports,3,46 however, of so-called anterior sleeve fractures of the lateral condyles, both in 8-year-olds (Fig. 15-25).
These fractures involved a good portion of the anterior articular
surface, although technically they could not be classified as pure
capitellar fractures because they contained nonarticular epicondylar
and metaphyseal portions in the fragment. Sodl et al.176 described an acute osteochondral shear fracture (Kocher-Lorenz) of the capitellum in a 12-year-old boy.
 |
|
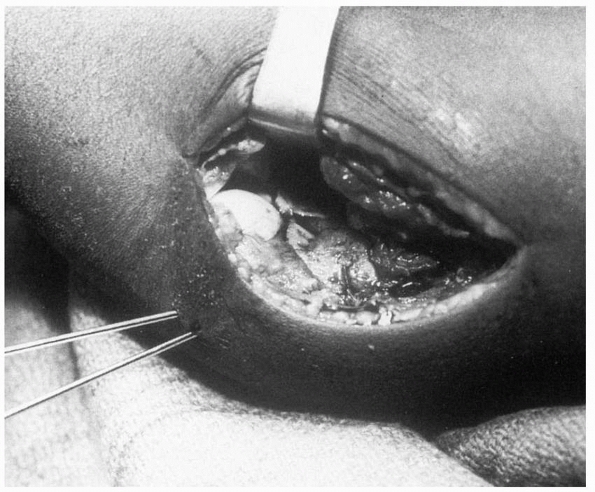
FIGURE 15-25 Fracture of the capitellum. A. Osteochondral fracture of the capitellum in an 8-year-old girl. Note the small fleck of bone (arrow), which indicates possible osteochondral fragment. B. Intraoperative photograph shows the size and origin of the fracture fragment from the lateral humeral epiphysis. C. Intraoperative photograph after fragment reduction into the bed of the capitellum. D.
Healed fracture with articular congruity, restoration of cartilage space, and no osteonecrosis. (From Drvaric DM, Rooks MD. Case report. Anterior sleeve fracture of the capitellum. J Orthop Trauma 1990;4:188, with permission.) |
there is little ossified tissue. It is composed mainly of pure
articular surface from the capitellum and essentially nonossified
cartilage from the secondary ossification center of the lateral condyle.
which usually contains a rather large portion of cancellous bone of the
lateral condyle. The lateral crista of the trochlea is often also
included (Fig. 15-26). The second, or
Kocher-Lorenz, type is more of a pure articular fracture with little if
any subchondral bone attached and may represent a piece of articular
cartilage from an underlying
osteochondritis dissecans. This type of fracture is rare in children.3,176
 |
|
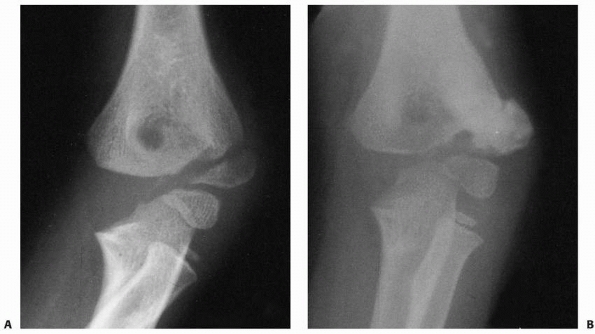
FIGURE 15-26 Fracture of the capitellum in a 13-year-old girl. A.
Injury film, lateral view, shows the large capitellar fragment lying anterior and proximal to the distal humerus. Both the radiocapitellar (solid arrow) and trochlear grooves (open arrow) are seen in the fragment. B. In the AP view, only a faint outline of the fragment is seen (arrows). |
anterior articular surface of the lateral condyle is sheared off by the
radial head.60 The presence of cubitus recurvatum or cubitus valgus seems to predispose the elbow to this fracture pattern.
fragment restricts flexion. If the fragment is large, it may be readily
apparent on a lateral radiograph (Fig. 15-27). On an AP radiograph, however, the fragment may be obliterated by the overlying distal metaphysis (see Fig. 15-26).
If the fragment is small, oblique views may be necessary to show the
fragment. In younger children, arthrography or MRI may be required to
diagnose this rare fracture. Letts et al.102 recommended computed tomography to help delineate the fracture type.
of the capitellum by the radial head, it stands to reason that there
may be an associated radial head or neck fracture.88 In Palmer’s132 large series, including both children and adults, 31 % had associated injuries of the proximal radius.
reattachment are the two most common forms of treatment. Closed
reduction is not likely to be successful.
reported good results after excision and noted that the earlier the
fragment was excised, the better the results were. Even when large
fragments were excised, joint instability did not appear to be a
problem. In patients in whom treatment is delayed, although the results
are not as good as when treatment is provided immediately after injury,
improvement in function can be expected, even with late excision.
reattached, the stability of the fracture is provided by wires or
screws inserted through the posterior surface of the lateral condyle.
The major problems with reattachment are associated with osteonecrosis
of the reattached fragment. Letts et al.102
reported satisfactory results with fixation of five capitellar
fractures using K-wires (three fractures), Herbert screws (one
fracture), and a cannulated screw (one fracture). In a biomechanical
cadaver study, Elkowitz et al.48
demonstrated that Acutrak compression screws (Acromed, Hillsboro, OR)
provided more stable fixation of simulated capitellar fractures than
did Herbert screws. In an earlier study,49
they determined that fixation with posteroanteriorly directed
cancellous lag screws was significantly more stable than fixation with
anteroposteriorly directed lag screws; however, anteroposteriorly
directed Acutrak compression screws provided significantly more stable
fixation than the posteroanteriorly directed lag screws. An advantage
of screw fixation is that it may not require later removal. Sodl et al.176
described suture fixation of an acute osteochondral (Kocher-Lorenz)
shear fracture of the capitellum in a 12-year-old boy. Two horizontal
mattress
sutures placed across the fracture fragment in an X-configuration
achieved both stable fixation and compression of the frature fragment.
Advantages cited for this technique include a low risk of growth
arrest, sufficient stability to allow immediate postoperative motion,
avoidance of implant removal, and facilitation of the acquisition of
high-quality postoperative MR images to evaluate healing.
 |
|
FIGURE 15-27 A,B. Fracture of the capitellum in a 14-year-old boy. C,D. After open reduction and fixation with two small cannulated screws through a lateral approach.
|
if an anatomic reduction can be achieved with a minimum of open
manipulation or dissection, then we prefer to reattach it with two
small cannulated screws inserted from posterior to anterior through a
lateral approach. Enough bone must be present in the capitellar
fragment to engage the screw threads, and if possible, countersink the
heads of the screws (see Fig. 15-27). If the
fracture is old, if there is any comminution of the fragment, or if
there is little bone in which to engage the screw threads, we believe
the appropriate treatment is to simply excise the fragment and start
early motion.
This, of course, occurs only in fractures in which the capitellar
fragment is retained. Posttraumatic degenerative arthritis can occur
whether the fragments are excised or retained. Many patients who are
treated either operatively or nonoperatively can expect to lose some
range of motion, but this loss is not always of functional or cosmetic
significance. It is important to emphasize to the parents before the
onset of treatment that complications can occur regardless of the
treatment method.
components. The intra-articular component involves, in some manner, the
trochlear articular surface. The extra-articular portion includes the
medial metaphysis and medial epicondyle. Because the fracture line
extends into the articular surface of the trochlea,
these often are called trochlear fractures. For purposes of description in this chapter, fractures of the trochlea are those that include only the articular surface.
in skeletally immature children, accounting for less than 1 % of
fractures involving the distal humerus.40
literature and early fracture texts do not mention these fractures as a
separate entity. Blount18 described only one such fracture in his classic text. In Faysse and Marion’s53
review of more than 2000 fractures of the distal humerus in children,
only 10 fractures involved the medial condylar physis. Although it has
been reported in a child as young as 2 years of age,7 this fracture pattern is generally considered to occur during later childhood.
in which the specific ages were given showed that 37 patients were in
the age range of 8 to 14 years. Thus, this fracture seems to occur
after the ossification centers of the medial condylar epiphysis begin
to appear. This fracture can occur as early as 6 months of age,
however, before any ossification of the distal humerus has appeared,14,38 making the diagnosis extremely difficult.
intra- and extra-articular components. They behave as Salter-Harris
type IV physeal injuries, but not enough fractures have been described
to show whether the fracture line courses through the secondary
ossification center of the medial condylar epiphysis or whether it
enters the common physeal line separating the lateral condylar
ossification center from the medial condylar ossification center. This
common physeal line terminates in the notch of the trochlea. The
trochlea’s lateral crista is ossified from the lateral condylar
epiphysis. Only the medial crista is ossified by the secondary
ossification centers of the medial condylar epiphysis. We believe that
this fracture is a “mirror image” of the lateral condylar physeal
injury and thus has characteristics of Salter-Harris type IV physeal
injuries (Fig. 15-28). The deformity that
develops if the fracture is untreated is nonunion, similar to that
after lateral condylar physeal fracture, rather than physeal fusion, as
occurs after a typical Salter-Harris type IV injury. The resultant
deformity is cubitus varus instead of the cubitus valgus deformity that
occurs with nonunion of the lateral condyle.
 |
|
FIGURE 15-28 A. The AP radiograph of a 9-year-old boy demonstrates the location of the ossification centers. A common physeal line (arrow) separates the medial and lateral condylar physes. B. Relationship of the ossification centers to the articular surface. The common physis terminates in the trochlear notch (arrow). C. Location of the usual fracture line involving the medial condylar physis (arrows).
|
 |
|
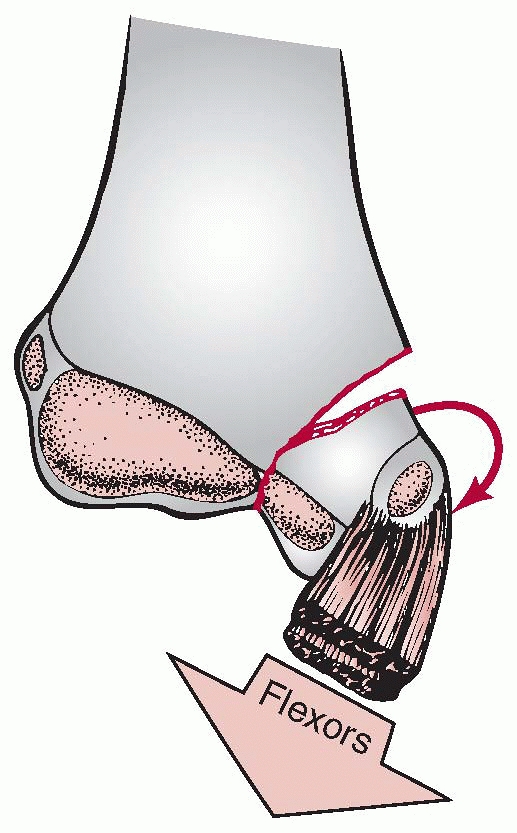
FIGURE 15-29
Displacement of the medial condyle. The pull of the forearm flexor muscles rotates the fragment so that the fracture surface is facing anteromedially and the articular surface is posterolateral. (Adapted and reprinted with permission from Chacha PB. Fractures of the medial condyle of the humerus with rotational displacement. J Bone Joint Surg Am 1970;52:1453-1458.) |
the intact medial epicondyle along with the common flexor origin of the
muscles of the forearm. These flexor muscles cause the loosened
fragment to rotate so that the fracture surface is facing anteriorly
and medially and the articular surface is facing posteriorly and
laterally (Fig. 15-29).7,28 Rotation of the fragment is especially accentuated when the elbow is extended. Chacha28
also noted that often the lateral aspect of the common flexor origin
and the anterior capsule of the joint were torn and the fracture
surface could usually be reached through this anterior opening into the
joint.
metaphysis courses extra-articularly along with the medial flexor
muscle groups. The blood supply to the lateral ossification center of
the medial crista of the trochlea, however, must traverse the surface
of the medial condylar physis. If the fracture line disrupts these
small intra-articular vessels, disruption and subsequent circulation
loss to the lateral portion of the medial crista can result, leading to
the development of a fishtail deformity.
many patients sustained this injury when they fell on their
outstretched arms. The theory is that this is an avulsion injury caused
by a valgus strain at the elbow (Fig. 15-30B). Fowles and Kassab59
reported a patient with a concomitant valgus greenstick fracture of the
olecranon associated with a fracture of the medial condylar physis.
They believed this fracture provided further evidence that this was a
valgus avulsion type of injury. Once the fragment becomes disassociated
from
the distal humerus, the forearm flexor muscles produce a sagittal anterior rotation of the fragment.
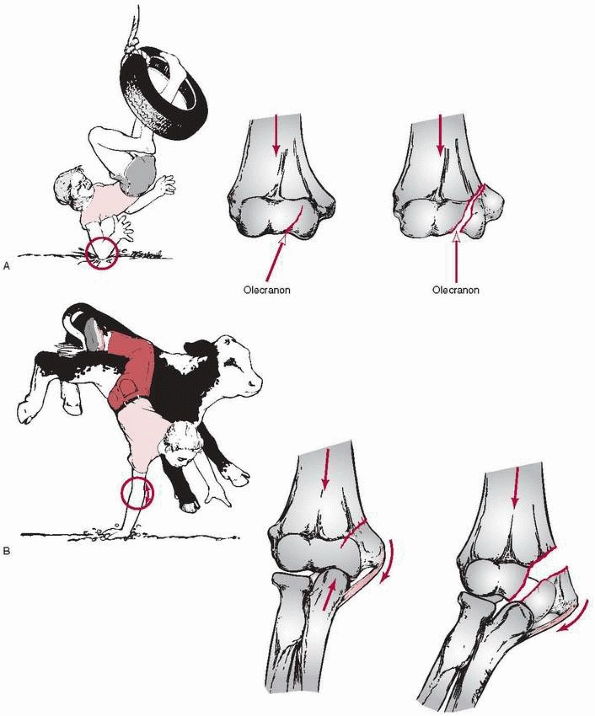 |
|
FIGURE 15-30
Medial condylar fracture mechanisms of injury. A. A direct force applied to the posterior aspect of the elbow causes the sharp articular margin of the olecranon to wedge the medial condyle from the distal humerus. B. Falling on the outstretched arm with the elbow extended and the wrist dorsiflexed causes the medial condyle to be avulsed by both ligamentous and muscular forces. |
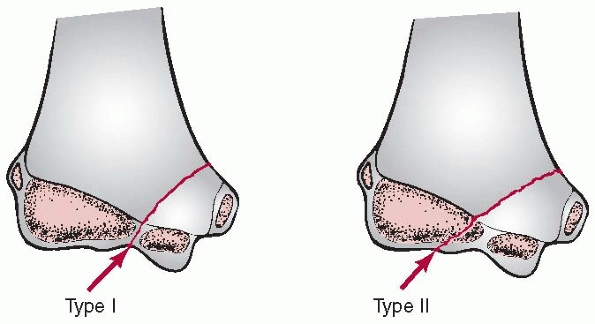 |
|
FIGURE 15-31 Medial condylar fracture patterns. In the Milch type I injury, the fracture line terminates in the trochlear notch (left, arrow). In the Milch type II injury, the fracture line terminates more laterally in the capitulotrochlear groove (right, arrow).
(Adapted and reprinted with permission from Milch H. Fractures and fracture-dislocations of the humeral condyles. J Trauma 1964;4:592-607.) |
condylar physis, is based on the fracture line’s location and the
degree of the fracture’s displacement. Location of the Fracture Line.
Milch119 classified fractures of the
medial condylar physis in adults into two types. In type I fractures,
the fracture line traverses the apex of the trochlea. In type II
fractures, it traverses the capitulotrochlear groove. He believed that
the origin of the fracture line depended on whether the radial head, as
in type II, or the semilunar notch of the olecranon, as in type I,
served as the impinging force for the abduction injury. Both fracture
patterns occur in children (Fig. 15-31), but
type I fractures seem to be more common because the common physeal
line, which serves as a point of weakness, ends in the apex of the
trochlea.
In type I, the fracture line in the medial condylar metaphysis extends
down to the physis. He noted that some of these might represent
incomplete supracondylar fractures. Unless there is a greenstick
crushing of the medial supracondylar column, these fractures are
usually of no clinical significance. In type II, the fracture line
extends into the medial condylar physis. The intra-articular portion,
as it is in preosseous cartilage, is often not recognized. In this
second type, the medial condylar fragment usually remains undisplaced.
In type III, the condylar fragment is both rotated and displaced.
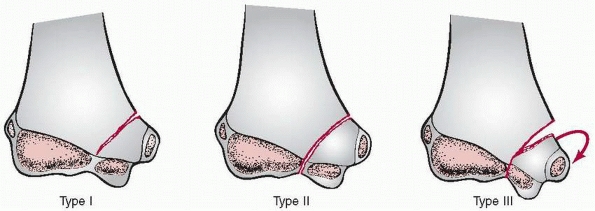 |
|
FIGURE 15-32
Kilfoyle classification of displacement patterns. (Adapted and reprinted with permission from Kilfoyle RM. Fractures of the medial condyle and epicondyle of the elbow in children. Clin Orthop 1965;41: 43-50.) |
found that type III displacement fractures, which accounted for only
25%, were more likely to occur in older adolescents, and type I
fractures were more common in younger children. These studies also
confirmed the correlation between the type of displacement and the
treatment method.
association with greenstick fractures of the olecranon and with true
posterolateral elbow dislocations (Fig. 15-33).14,162 Some investigators14,38 found that child abuse was more common in their younger patients with these fractures than with other elbow fractures.
condylar physis is most often confused with a fracture of the medial
epicondyle.100 In both types of
intra- and extra-articular fractures, swelling is concentrated
medially, and there may be valgus instability of the elbow joint. In a
true intra-articular fracture, however, there is varus instability as
well. Such is usually not the case with an isolated extra-articular
fracture of the medial epicondyle. Ulnar nerve paresthesia may be
present with both types of fractures.
involvement of the entire condyle is usually obvious on radiographs; in
younger children, in whom only the epicondyle is ossified, fracture of
the medial condylar physis may be erroneously diagnosed as an isolated
fracture of the medial epicondyle (Fig. 15-34)34,51,59
remember that medial epicondylar fractures are often associated with
elbow dislocations, usually posterolateral, and that elbow dislocations
are rare before ossification of the medial condylar epiphysis begins.
With medial condylar physeal fractures, the
elbow tends to subluxate posteromedially34 due to the loss of trochlear stability.
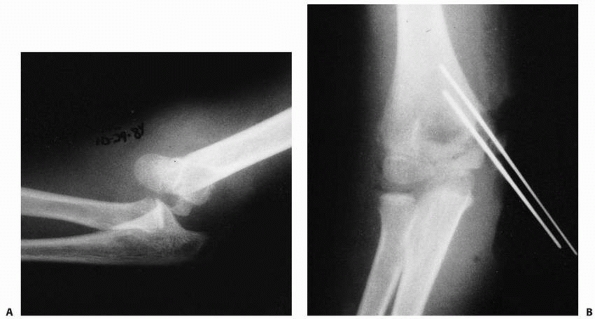 |
|
FIGURE 15-33 A.
Injury film of a 10-year-old girl who sustained a type III displaced fracture of the medial condyle associated with a posterolateral elbow dislocation. B. After open reduction and K-wire fixation through an anteromedial approach. (Courtesy of Elizabeth A. Szalay, MD.) |
fragment suggests the presence of an intra-articular fracture of the
medial condyle and is an indication for further evaluation. Often, the
medial condyle and the medial epicondyle are markedly displaced as a
unit. A positive fat pad sign indicates that the injury has entered the
elbow joint and a fracture of the medial condyle is likely.74,170 Isolated fractures of the medial epicondyle are extra-articular and usually do not have positive fat pad signs.
questionable in a child younger than 8 to 10 years of age with
significant medial elbow ecchymosis, arthrography or MRI of the elbow
should be performed.
The fracture fragment can be approached by a posteromedial incision
that allows good exposure of both the fracture site and the ulnar
nerve. Fixation is easily achieved with smooth K-wires (see Fig. 15-33)
or with screws in older adolescents. Two wires are necessary because of
the sagittal rotation forces exerted on the fracture fragment by the
common flexor muscles. El Ghawabi47 reported frequent delayed union and nonunion in fractures that were not rigidly stabilized.
patterns, enough residual internal stability is usually present to
allow the fracture to be simply immobilized in a cast or posterior
splint.14,47,53,94,137
As with fractures of the lateral condylar physis, union may be slow. In
fractures treated promptly, results have been satisfactory.28,51,59
Because there usually is more displacement in older children, the
results in this age group are not as satisfactory as those in younger
children, who tend to have relatively nondisplaced fractures.14
simple observation and a posterior splint. Follow-up radiographs at
weekly intervals are taken to ensure there is no late displacement.
When there is good callus at the metaphyseal portion of the fracture
line by 3 to 4 weeks, the splint is removed and early active motion is
initiated. We continue to follow the patient until there is a full
range of motion and obliteration of the fracture line.
stabilized. This is usually difficult to do by closed methods because
the swelling associated with this injury makes it hard to accurately
identify the landmarks for pin placement. We proceed with an open
reduction through a medial approach with identification and protection
of the ulnar nerve. The posterior surface of the condylar fragment and
the medial aspect of the medial crista of the trochlea should be
avoided in the dissection because these are the blood supply sources to
the ossific nuclei of the trochlea. Fixation with two parallel pins
should be in the metaphyseal segment if possible (Fig. 15-35). Cannulated screw fixation can be used in adolescents near skeletal maturity.
diagnosis. This is especially true in younger children, in whom a
medial condylar fracture can be confused with a displaced fracture of
the medial epicondyle (see Fig. 15-34). When
the diagnosis is a real possibility, especially in a child with no
ossification of the trochlea, examination with anesthesia,
arthrography, or MRI may be helpful. Leet, Young, and Hoffer101 reported complications
after 33% of 21 medial condylar fractures, including osteonecrosis of
the trochlea, nonunion, and loss of reduction. Untreated displaced
fractures usually result in nonunion with cubitus varus deformity (Fig. 15-36).59,192 Ryu et al.159
described a painful nonunion of the medial condyle in an adolescent
that apparently resulted from a fracture when he was 3 years old. An
osteotomy was made to remove the ununited section of bone, and an iliac
bone graft was inserted and fixed with two malleolar screws. Union was
obtained, and the patient was able to participate in sports without
pain. We have seen one nonunion after a fracture of the medial condyle.
Delayed union has been reported in patients treated with insecure
fixation or simply placed in a cast.47,94
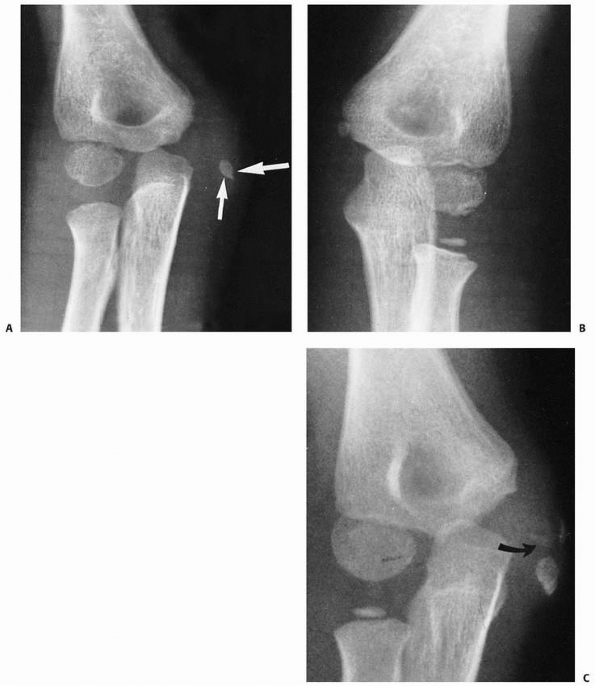 |
|
FIGURE 15-34 Missed medial condylar fracture. A. Initial film of a 6-year-old who was originally diagnosed as having a displaced fracture of the medial epicondyle (arrows). B. Normal side for comparison. C. Three months later, the patient continued to have a painful elbow, and there was ossification of the metaphysis (arrow) adjacent to the epicondyle.
|
condylar fragment may occur during open reduction and internal fixation
or at the time of initial injury. Several investigators have reported
subsequent avascular changes in the medial crista of the trochlea.47,59,94,137 Hanspal70 reviewed Cothay’s original patient34
18 years after delayed open reduction and found that despite some
minimal loss of motion, the patient was asymptomatic. Radiographs,
however, showed changes compatible with osteonecrosis of the medial
condyle.
reported in patients whose fractures united uneventfully. The valgus
deformity appears to be caused by secondary stimulation or overgrowth
of the medial condylar fragment. Some simple stimulation of the medial
epicondyle’s prominence may also produce the false appearance of a
cubitus valgus deformity. Cubitus varus appears to result from
decreased growth of the trochlea, possibly caused by a vascular insult.
Principles for
treating nonunion of lateral condylar fractures are generally applicable to nonunions of the medial condyle (Fig. 15-37).
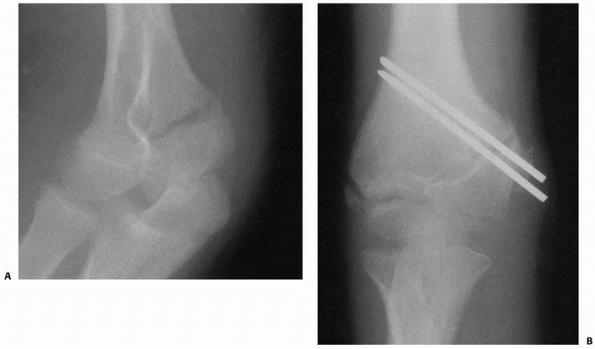 |
|
FIGURE 15-35 A. Stage II fracture of the medial condyle in a 10-year-old girl. B. After open reduction and K-wire fixation through a medial approach
|
 |
|
FIGURE 15-36 Nonunion in addition to cubitus varus deformity. A. Original film of a 5-year-old girl who sustained an injury 1 year previously. The metaphyseal fragment (arrow) is attached to the medial epicondyle. B. Film taken 2 years later. Some ossification has developed in the medial condylar epiphysis (arrow). (Courtesy of Roy N. Davis, MD.)
|
 |
|
FIGURE 15-37 Nonunion of a medial condylar fracture in a 10-year-old girl. Note medial subluxation of the radius and ulna.
|
described one partial ulnar neuropathy occurring after this type of
injury. The neuropathy almost completely recovered after anterior
transposition of the ulnar nerve.
portion of the trochlea are extremely rare in skeletally immature
children. Grant and Miller66
reported a 13-year-old boy who had a posterolateral dislocation of the
elbow with marked valgus instability and fractures of the medial
epicondyle and radial neck. When the elbow was explored to secure the
epicondyle, a large osteochondral fragment from the medial crista of
the trochlea was found lying between the two articular surfaces. The
fragment was replaced and fixed, and a satisfactory result was
obtained, although the presence of the fragment was not detected
preoperatively.
described osteochondritis dissecans (OCD) in two patients (three
elbows) aged 12 and 14 years. In one patient, open biopsy was done
because the osteochondral lesion was thought to be a neoplastic lesion.
The other patient with bilateral lesions was treated conservatively
with good results. Matsuura et al.111
evaluated 1802 young baseball players, 717 (40%) of whom had elbow
pain. Of the 150 who had bilateral elbow radiographic examination,
osteochondral lesions of the elbow were identified in 121 (81%);
trochlear lesions accounted for 0.5% of these. More recently, Marshall
et al.109 reported osteochondral
lesions of the trochlea in 18 young athletes ranging in age from 6 to
17 years; 10 of the 18 were throwing athletes and two were gymnasts.
Based on MRI and MR arthrogram findings, injuries were classified as
chondral/osteochondral injury/OCD lesions (13 patients) or trochlear
osteonecrosis (five patients). Ten of the 13 osteochondral lesions
involved the lateral trochlea and were described as classic OCD; the
three medial trochlear lesions were small (<6 mm) and were located
on the posterior articular surface of the medial trochlea. Trochlear
osteonecrosis in five patients was characterized by growth disturbance
involving the ossification centers of the trochlea. The affected
trochleas were misshapen and underdeveloped, and radiographs showed the
secondary ossification centers to be fragmented, small, and sclerotic,
or absent entirely. All five of the patients with osteonecrosis had
histories of distal humeral fractures treated with K-wire fixation
earlier in childhood (two lateral condylar fractures and one each
supracondylar, medial epicondylar, and medial condylar fracture). The
authors suggested that the athletic demands placed on the adolescent
elbow revealed osteonecrosis from these earlier fractures.109
The OCD lesions consistently occurred in the posteroinferior aspect of
the lateral trochlea corresponding to a watershed zone of diminished
vascularity, and the authors hypothesized that the lesions were caused
by repeated forced elbow extension/hyperextension that led to
impingement of the normal blood supply.109
Small osteochondral lesions on the posteromedial trochlea were
suggested to result from olecranon abutment occurring in an elbow with
collateral ligament laxity or insufficiency.
in whom there is some widening of the joint after reduction, an
intra-articular fracture of the trochlea or capitellum should be
suspected. Arthrography, MRI, or computed tomographyarthrography,
should be used for confirmation.
Once the presence of this injury became recognized, larger series
appeared. Seven separate series reported a total of 45 fractures,4,39,40,81,114,123,141 and Abe et al.1
reported a series of 21 fractures. Originally thought to be a rare
injury, it appears that fractures involving the entire distal humeral
physis occur frequently in children. The major problem is the initial
recognition of this injury.
the secondary ossification of the medial epicondyle until about 6 to 7
years of age in girls and 8 to 9 years in boys. Thus, fractures
involving the entire physeal line include the medial epicondyle up to
this age. In older children, only the lateral and medial condylar
physeal lines are included.
physis occur before the age of 6 or 7. The younger the child is, the
greater the volume of the distal humerus that is occupied by the distal
epiphysis will be. As the humerus matures, the physeal line progresses
more distally, with a central V forming between the medial and lateral
condylar physes (Fig. 15-38). Ashhurst7
believed that this V-shaped configuration of the physeal line helps
protect the more mature distal humerus from physeal fractures.
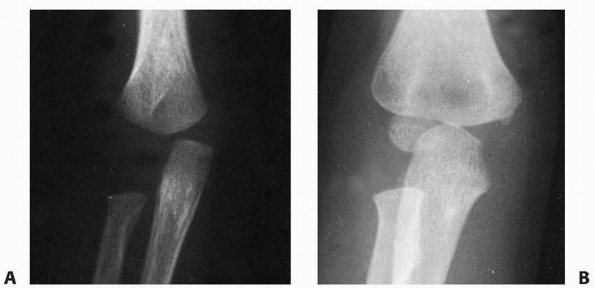 |
|
FIGURE 15-38 A. At 5 months of age, the metaphysis has advanced only to the supracondylar ridges. B. By 4 years of age, the edge of the metaphysis has advanced well into the area of the epicondyles
|
physis traverse the anatomic centers of the condyles, they are the
pediatric counterparts of the adult bicondylar fracture. Because the
fracture is distal, the fracture surfaces are broader than those
proximally through the supracondylar fractures. This broader surface
area of the fracture line may help prevent tilting of the distal
fragment. Because the fracture lines do not involve the articular
surface, development of joint incongruity with resultant loss of elbow
motion is unlikely if malunion occurs.
of the trochlea courses directly through the physis. The blood supply
to this area is vulnerable to injury, which may cause osteonecrosis in
this part of the trochlea.
A hyperextension injury in this age group is more likely to result in a
physeal separation than a bony supracondylar fracture.36
probably varies with the age group involved. A few consistent factors
are evident.
noted that the clinical appearance of these injured elbows at the time
of delivery was not especially impressive. There was only moderate
swelling and some crepitus.
a physis is more likely to fail with rotary shear forces than with pure
bending or tension forces. Young infants have some residual flexion
contractures of the elbow from intrauterine positioning; this prevents
the hyperextension injury that results in supracondylar elbow fractures
in older children. Rotary forces on the elbow, which can be caused by
child abuse or birth trauma in young infants, are probably more
responsible for this injury than hyperextension or varus or valgus
forces, which produce other fracture patterns in older children.
21 children, ranging in age from 1 to 11 years (average: 5 years), with
fracture separations of the distal humeral epiphysis, all of which were
sustained in falls.
classified fractures of the entire distal humeral physis into three
groups based on the degree of ossification of the lateral condylar
epiphysis (Fig. 15-39). Group A fractures occur
in infants up to 12 months of age, before the secondary ossification
center of the lateral condylar epiphysis appears (Fig. 15-39A,B).
They are usually Salter-Harris type I physeal injuries. This injury is
often not diagnosed due to the lack of an ossification center in the
lateral condylar epiphysis. Group B fractures occur most often in
children 12 months to 3 years of age in whom there is definite
ossification of the lateral condylar epiphysis (Fig. 15-39C).
Although there may be a small flake of metaphyseal bone, this is also
essentially a type I Salter-Harris physeal injury. Group C fractures
occur in older children, from 3 to 7 years of age and result in a large
metaphyseal fragment that is most commonly lateral but can be medial or
posterior (Fig. 15-39D,E).
injuries with the distal epiphyseal fragment posterior to the
metaphysis. A rare flexion type of injury can occur in which the
epiphyseal fragment is displaced anteriorly.15 Stricker et al.183
reported a coronal plane transcondylar (Salter-Harris type IV) fracture
in a 3-year-old child that was initially diagnosed as a fracture of the
lateral humeral condyle. No growth disturbance was evident 3 years
after open reduction and pin fixation.
swollen secondary to trauma or suspected trauma, a fracture involving
the entire distal humeral physis should be considered. In a young
infant or newborn, swelling may be minimal with little crepitus. Poland146
described the crepitus as “muffled” crepitus because the fracture ends
are covered with softer cartilage than the firm osseous tissue in other
fractures about the elbow. The relationship between the epicondyles and
the olecranon is maintained. Because of the large, wide fracture
surfaces, there are fewer tendencies for tilting with distal fragment
rotation, and the angular deformity is less severe than that with
supracondylar fractures. In older children, the elbow is often so
swollen that a clinical assessment of the bony landmarks is impossible,
and radiographic evaluation must provide confirmation of the diagnosis
(see Fig. 15-39A,B).
the ossification center of the lateral condyle is not visible in an
infant. The only relationship that can be determined is that of the
primary ossification centers of the distal humerus to the proximal
radius and ulna. The proximal radius and ulna maintain an anatomic
relationship to each other but are displaced posteriorly and medially
in relation to the distal humerus. This posteromedial relationship is
diagnostic. Although theoretically, the distal fragment can be
displaced in any direction, with rare exceptions15
most fractures reported have been displaced posteromedially. Comparison
views of the opposite uninjured elbow may be helpful to determine the
presence of posteromedial displacement (see Fig. 15-39A,B).
displacement of the entire distal epiphysis is much more obvious. The
anatomic relationship of the lateral condylar epiphysis with the radial
head is maintained, even though the distal humeral
epiphysis is displaced posterior and medial in relation to the metaphysis of the humerus (see Fig. 15-39C,D).
 |
|
FIGURE 15-39 A.
Group A—AP view of a small infant who had a swollen left elbow after a difficult delivery. The displacement medially of the proximal radius and ulna (arrows) helps to make the diagnosis of a displaced total distal humeral physis. B. Normal elbow for comparison. C. Group B—AP view showing the posteromedial displacement of the distal fragment (arrows). The relationship between the ossification center of the lateral condyle and the proximal radius has been maintained. D. Group C—AP view with marked medial displacement of the distal fragment. E. Group C—lateral view of the same patient showing posterior displacement of the distal fragment. There is also a large metaphyseal fragment associated with the distal fragment (arrow). |
fractures may be confused with either a low supracondylar fracture or a
fracture of the lateral condylar physis. The key diagnostic point is
the smooth outline of the distal metaphysis in fractures involving the
total distal physis. With supracondylar fractures, the distal portion
of the distal fragment has a more irregular border.
physis and the rare elbow dislocation in an infant can be made on
radiograph. With a displaced fracture of the lateral condylar physis,
the relationship between the lateral condylar epiphysis and the
proximal radius is usually disrupted (see Fig. 15-8B). If the lateral crista of the trochlea is involved, the proximal radius and ulna may be displaced posterolaterally.
fractures of the entire distal humeral physis. With elbow dislocations,
the displacement of the proximal radius and ulna is almost always
posterolateral, and the relationship between the proximal radius and
lateral condylar epiphysis is disrupted.
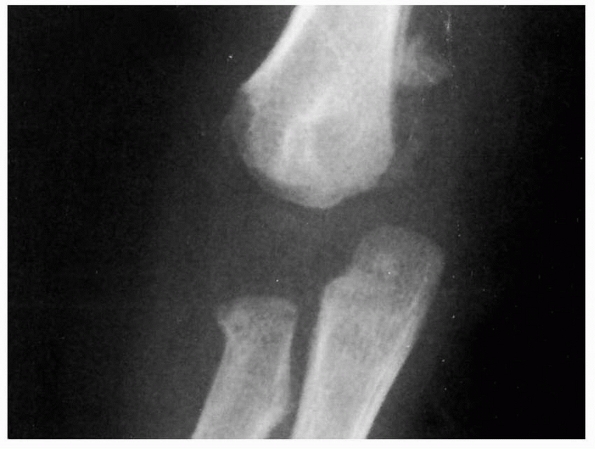 |
|
FIGURE 15-40
The true nature of this injury as involving the entire distal humeral physis was not appreciated until periosteal new bone became visible 3 weeks after injury. |
around the distal humerus, and the whole epiphysis may remain displaced
posteriorly and medially (Fig. 15-40).
recognition. Because this damage may be associated with child abuse,
the parents may delay seeking treatment.
reported 12 fracture separations of the distal humeral epiphysis, three
of which were initially diagnosed as fractures of the lateral condyle
and one as an elbow dislocation. Due to the frequency of cubitus varus
after this injury in young children, they recommended closed reduction
and percutaneous pinning in children younger than 2 years of age so
that the carrying angle can be evaluated immediately after reduction
and corrected if necessary.
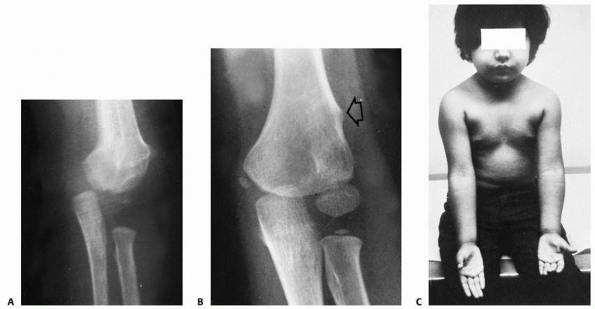 |
|
FIGURE 15-41 Remodeling of untreated fractures. A.
AP view of a 2-year-old who had an unrecognized and untreated fracture of the distal humeral physis. The medial translocation is apparent. There was no varus or valgus tilting. B. Four years later, there had been almost complete remodeling of the distal humerus. A small supracondylar prominence (arrow) remains as a scar from the original injury. C. Clinical appearance 4 years after injury shows no difference in elbow alignment. |
usually performed owing to misdiagnosis as a displaced fracture of the
lateral humeral condyle.4,81,154,200 Mizuno et al.,123
however, recommended primary open reduction because of his poor results
with closed reduction. They approached the fracture posteriorly by
removing the triceps insertion from the olecranon with a small piece of
cartilage. If the fracture is old (more than 5 to 6 days) and the
epiphysis is no longer mobile, manipulation should not be attempted,
and the elbow should be splinted for comfort. Many essentially
untreated fractures remodel completely without any residual deformity
if the distal fragment is only medially translocated and not tilted (Fig. 15-41).
of fresh fractures. The elbow is initially manipulated into extension
to correct the medial displacement, and then the fragment is stabilized
by flexing the elbow and pronating the forearm. The distal epiphysis is
more securely held with the elbow flexed and the forearm pronated. When
the forearm is supinated with the elbow flexed, the distal fragment
tends to displace medially. This displacement is usually a pure medial
horizontal translocation without mediolateral coronal tilting.
anesthesia or percutaneous pin fixation may be difficult, we typically
simply immobilize the extremity in 90 degrees of flexion
with the forearm pronated. The extremity is then externally stabilized with a figure-of-eight splint.
immobilization is usually not dependable in maintaining the reduction.
As a rule, in these patients, we perform the manipulation with the
patient under general anesthesia and secure the fragment with two
lateral pins (Fig. 15-42). Due to the swelling
and immaturity of the distal humerus, the medial epicondyle is
difficult to define as a distinct landmark, making it risky to attempt
the percutaneous placement of a medial pin. If a medial pin is
necessary for stable fracture fixation, a small medial incision can be
made to allow direct observation of the medial epicondyle. In small
infants and young children with minimal ossification of the epiphyseal
fragment, an intraoperative arthrogram may be obtained to help
determine the quality of the reduction.
allow active elbow motion to resume. The patient is then followed until
full motion is regained and until there is radiographic evidence of
normal physeal and epiphyseal growth. Usually, 3 weeks of
immobilization is sufficient.
epiphysis is not freely movable, the elbow is simply immobilized in a
splint or cast. It is probably better to treat any resulting deformity
later with a supracondylar osteotomy rather than risk the complication
of physeal injury or osteonecrosis of the epiphysis by performing a
delayed open reduction. Only occasionally does an untreated patient
have a deformity severe enough to require surgical correction at a
later date. Because the articular surface is intact, complete
functional recovery can usually be expected.
 |
|
FIGURE 15-42 A. Injury film of a 20-month-old showing medial displacement of the distal fragment. B,C. The medial and posterior displacement of the condylar fragment (arrow) is better defined after an arthrogram. D. Fixation is achieved by two lateral pins placed percutaneously
|
this injury, especially a type A fracture pattern, unless it occurs at
birth. A young infant is unlikely to incur this type of injury
spontaneously from the usual falls that occur during the first year of
life. Of the 16 fractures reported by DeLee et al.,40 six resulted from documented or highly suspected child abuse, all in children younger than 2 years of age.
transient or permanent, are rare with this fracture, probably because
the fracture fragments are covered with physeal cartilage and do not
have sharp edges as do other fractures in this area. In addition, the
fracture fragments are usually not markedly displaced. Nonunion. Only
one nonunion after this fracture has been reported; it occurred in a
patient seen 3 months after the initial injury.123
Because of the extreme vascularity and propensity for osteogenesis in
this area, union is rapid even in patients who receive essentially no
treatment.
 |
|
FIGURE 15-43
An AP view of a residual cubitus varus in a 2-year-old 6 months after physeal fracture of the distal humerus. This patient was treated initially with simple immobilization. |
Because the fracture surfaces are wider with this injury than with
supracondylar fractures, the distal fragment tends to tilt less, which
seems to account for the lower incidence of cubitus varus after this
injury than after untreated supracondylar fractures (see Fig. 15-43); however, reduction and percutaneous pinning are recommended for acute fractures with displacement.
lateral condyle or the trochlear epiphysis has rarely been reported
after fractures of the entire distal humeral physis. Yoo et al.207
reported eight patients with osteonecrosis of the trochlea after
fracture separations of the distal end of the humerus. Six of the eight
fractures were diagnosed initially as medial condylar fractures,
lateral condylar fractures, or traumatic elbow dislocation. All eight
patients had rapid dissolution of the trochlea within 3 to 6 weeks
after injury, followed by the development of a medial or central
condylar fishtail defect. We have noted osteonecrosis of the trochlea
after three fractures of the entire humeral physis, two of which were
inadequately reduced and one of which was anatomically reduced by
closed methods (Fig. 15-44). All three had
marked displacement of the distal epiphyseal fragment. In one, the
osteonecrosis of the trochlea produced a secondary cubitus varus
deformity that continued to progress with growth and a significant loss
of elbow motion. The etiology of this complication was discussed in the
section on osteonecrosis of the trochlea.
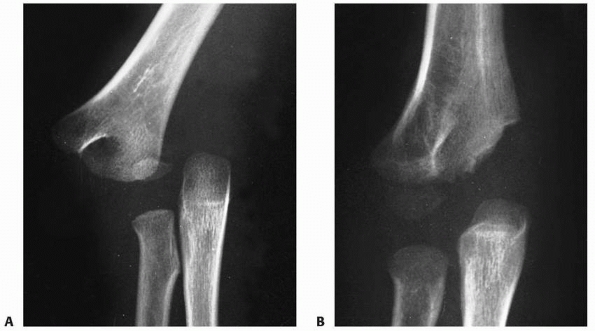 |
|
FIGURE 15-44
Osteonecrosis. A. Injury film in a 5-year-old with marked displacement of the distal epiphysis. Closed reduction was followed by lateral pin fixation. B. Nevertheless, radiographs taken 14 months later showed early evidence of osteonecrosis of the medial condyle. (Courtesy of Salvador J. Mendez, MD.) |
was often associated with elbow dislocation and the apophyseal fragment
could become entrapped within the joint.194
Much of the discussion during that era centered on the manipulative
techniques used to extract the fragment from the joint. In recent
years, the proponents of uniform nonoperative management89,134,202 have outnumbered the proponents of uniform operative management.80
In the interval since the third edition of this volume, little has been
written about the treatment of this injury; most of the focus has been
on the increased recognition of this injury occurring during sports.103,104,131
constitute approximately 14.1% of fractures involving the distal
humerus and 11.5% of all fractures in the elbow region.12,16,31
later peak age, similar to fractures involving the medial condylar
physis. The youngest reported patient with this injury was 3.9 years.31 In the large series of fractures of the medial epicondylar
apophysis, most occurred between ages 9 and 14, and the peak age incidence was 11 to 12 years.12,62,80,94,129,134,173,202
Fractures of the epicondylar apophysis affect boys by a ratio of almost
4 to 1. In six large series in the literature, boys constituted 79% of
the patients.62,63,107,155,194,202
|
TABLE 15-1 Fractures of the Medial Epicondylar Apophysis: Incidence
|
||||
|---|---|---|---|---|
|
of the elbow has varied from as low as 30% to as high as 55% in many of
the reported series.12,202 Two bilateral injuries associated with bilateral elbow dislocations have been reported.16,52 Both patients sustained their injuries while participating in gymnastics.
epicondylar apophysis is 9 to 12 years. The injury occurs in boys four
times more often than in girls. About 50% of such injuries are
associated with elbow dislocations. In at least 15% to 18% of patients,
the fragment is incarcerated in the joint (Table 15-1).
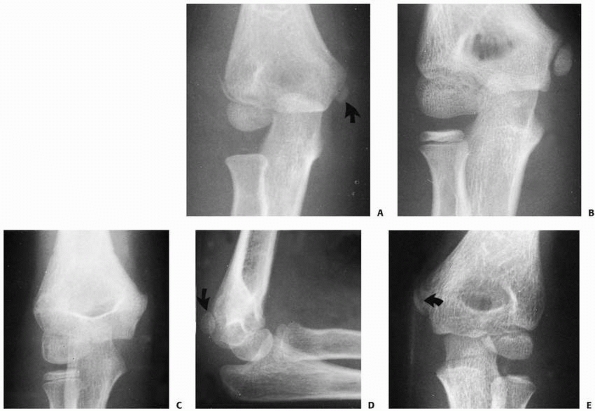 |
|
FIGURE 15-45 Ossification of the medial epicondyle. A. The concentric oval nucleus of ossification of the medial epicondylar apophysis (arrow). B. As ossification progresses, parallel smooth sclerotic margins develop in each side of the physis. C.
Because it is somewhat posterior, on a slightly oblique anteroposterior view the apophysis may be hidden behind the distal metaphysis. D. The posterior location of the apophysis (arrow) is appreciated on this slightly oblique lateral view. E. On the anteroposterior view, the line created by the overlapping of the metaphysis (arrow) can be misinterpreted as a fracture line (pseudofracture). |
is used throughout the description of this injury. The forces across
its physis are tension rather than the compressive forces present
across the condylar physes of the distal humerus. Because it is an
apophysis, it does not contribute to the overall length of the distal
humerus.
epicondylar apophysis is part of the entire distal humeral epiphysis.
With growth and maturity, it becomes separated from the entire distal
humeral epiphysis by intervening metaphyseal bone. In younger children,
when there is a separation of the distal humeral epiphysis, the medial
epicondylar apophysis is included as part of the distal fragment.
the posterior surface of the medial distal humeral metaphysis. As was
mentioned in Chapter 14, this posterior
location is important when percutaneous pin fixation is used. Likewise,
this posterior position affects the image of the apophysis on
radiographs (Fig. 15-45).
described various unique aspects of the ossification process of the
medial epicondylar apophysis. The following discussion is paraphrased
from their work.
occurring at about 15 years of age. It is the last secondary
ossification center to fuse with the distal humeral metaphysis. The
ossification center starts as a small eccentric oval nucleus (Fig. 15-45A). As it matures, parallel sclerotic margins develop along both sides of the physis (Fig. 15-45B).
There may be some irregularity of the ossification process, which gives
the ossific nucleus a fragmented appearance. This fragmentation may be
falsely interpreted as a fracture.
center may be difficult to see on an AP radiograph, especially if the
elbow is slightly oblique (Fig. 15-45C). The
posterior position of the apophysis is best appreciated on a lateral
radiograph. If the elbow is slightly oblique, the outline of the
epicondyle may be better appreciated (Fig. 15-45D).
Because of this posterior location on AP radiographs, the distal medial
metaphyseal border may overlap the ossific nucleus of the apophysis.
This overlapping may appear as a lucent line that can be misinterpreted
as a fracture (Fig. 15-45E).
of the flexor carpi radialis, flexor carpi ulnaris, flexor digitorum
superficialis, palmaris longus, and part of the pronator teres,
originates from the anterior aspect of the apophysis (Fig. 15-46).169 Part of the flexor carpi ulnaris also originates on the posterior aspect of the epicondyle.
origin extends up to the physeal line of the epicondyle. In older
children and adolescents, as the epicondyle migrates more proximally,
the capsule is attached only to the medial crista of the trochlea.7
Thus, in younger children, a fracture line involving the medial
epicondylar apophysis can enter the joint because part of the capsule
is attached to the epicondylar fragment. In older children, however, if
there is a pure avulsion force on the epicondyle, the capsule may
remain attached to the trochlea’s outer border. In this age group, the
fracture may be totally extra-articular.
ligaments originate from this apophysis. The ulnar collateral ligament
is composed of three separate bands (Fig. 15-47).204 Woods and Tullos204
pointed out that the major stabilizing ligamentous structure in the
elbow is the anterior band of the ulnar collateral ligament. The band’s
anterior portion is taut in extension, and the posterior fibers are
taut in flexion. The fibers of the posterior band of the ulnar
collateral ligament are relaxed in extension and are taut in flexion
(see Fig. 15-47). Thus, this posterior band
provides stability only in flexion. Because the radial collateral
ligaments do not attach directly to the ulna or radius, but instead
attach to the orbicular ligament, they provide only minimal stability
to the elbow joint.
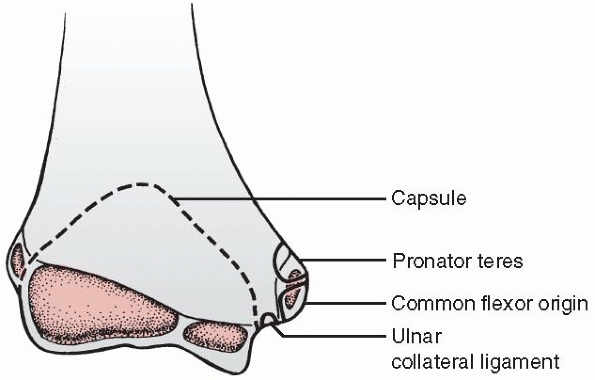 |
|
FIGURE 15-46
Soft tissue attachments. The AP view of the distal humerus demonstrates the relationship of the apophysis to the origins of the medial forearm muscles. The origin of the ulnar collateral ligament lies outside the elbow capsule. The margin of the capsule is outlined by the dotted line. |
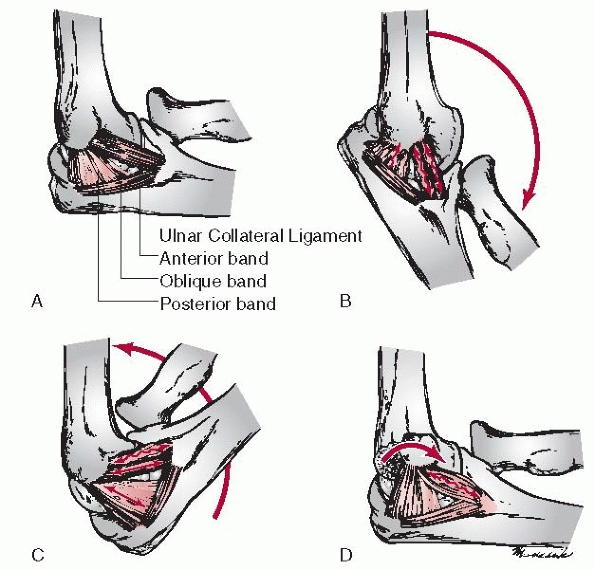 |
|
FIGURE 15-47 Ligamentous structures. A. The ulnar collateral ligament is divided into anterior, posterior, and oblique bands. B.
On extension, the anterior fibers of the anterior band are taut. The posterior fibers of the anterior band and the entire posterior band are loose in this position. C. In flexion, the posterior fibers of the anterior bands and posterior band become taut. The anterior fibers of the anterior band become loose. D. When the epicondyle is rotated anteriorly, the entire anterior band can become loose. (From Woods WG, Tullos HS. Elbow instability and medial epicondyle fractures. Am J Sports Med 1977;5:23-30, with permission.) |
commonly occur as acute injuries in which a distinct event produces a
partial or a complete separation of the apophyseal fragment. Three
theories have been proposed about the mechanism of acute medial
epicondylar apophyseal injuries: a direct blow, avulsion mechanisms,
and association with elbow dislocation (Table 15-2).
speculated that this type of injury could occur as a result of a direct
blow on the posterior aspect of the epicondyle. Among more recent
investigators, however, only Watson-Jones195
described this injury as being associated with a direct blow to the
posterior medial aspect of the elbow. In rare patients in whom the
fragment is produced by a direct blow to the medial aspect of the
joint, the medial epicondylar fragment is often fragmented (Fig. 15-48). In these injuries, there may also be more superficial ecchymosis in the skin.
epicondyle by the flexor muscles of the forearm.94,140
This muscle avulsion force can occur in combination with a valgus
stress in which the elbow is locked in extension, or as a pure
musculature contraction that may occur with the elbow partially flexed.
|
TABLE 15-2 Fractures of Medial Condylar Apophysis: Mechanism of Injury
|
|||||||
|---|---|---|---|---|---|---|---|
|
proposed that when a child falls on his outstretched upper extremity
with the elbow in extension, the wrist and fingers are often
hyperextended as well, placing an added tension force on the epicondyle
by the forearm flexor muscles (Fig. 15-49). The
normal valgus carrying angle tends to accentuate these avulsion forces
when the elbow is in extension. Many proponents of this theory point to
the other associated elbow fractures that have been seen with this
injury as evidence to confirm that a valgus force is applied across the
elbow at the time of the injury. These associated injuries include
radial neck fractures with valgus angulation and greenstick valgus
fractures of the olecranon.94
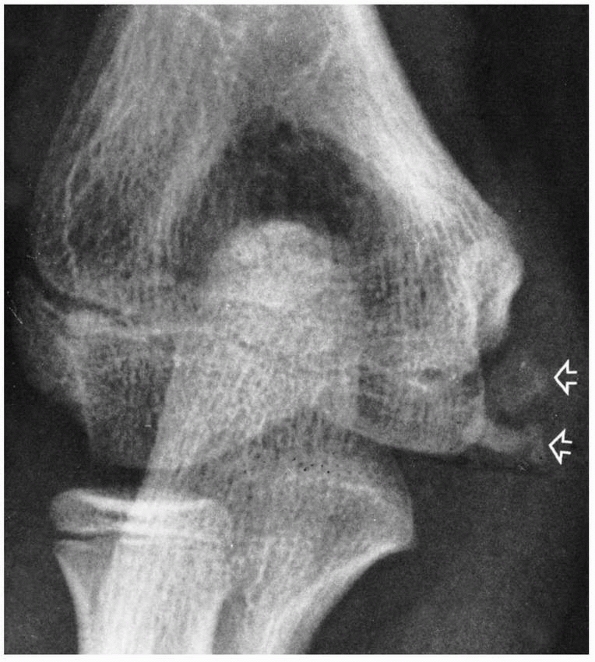 |
|
FIGURE 15-48 Direct fragmentation. The fragmented appearance of the medial epicondyle (arrows)
in a 13-year-old who sustained a direct blow to the medial aspect of the elbow. (From Wilkins KE. Fractures of the medial epicondyle in children. Instr Course Lect 1991;40:1-8, with permission.) |
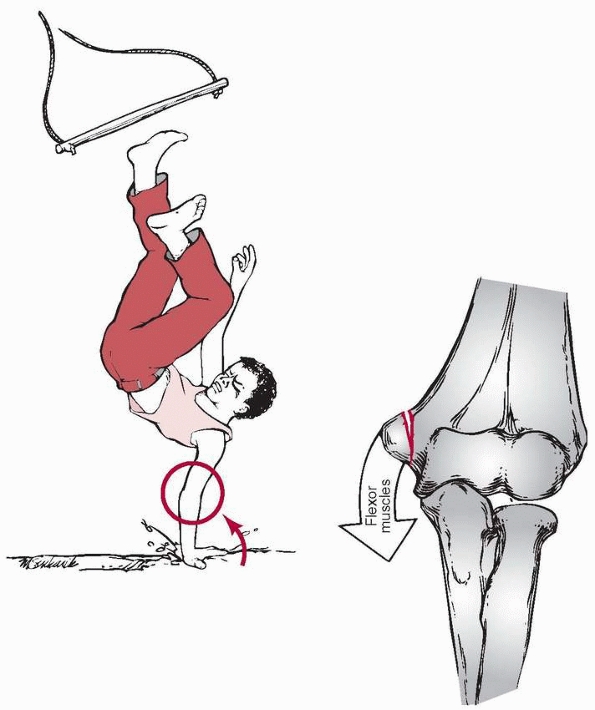 |
|
FIGURE 15-49
Hyperextension forces. When a person falls on the outstretched upper extremity, the wrist and fingers are forced into hyperextension (solid arrow), which places tension on the forearm flexor muscles. This sudden tension along with the normal valgus carrying angle tends to place a strong avulsion force on the medial epicondyle (open arrow). |
Isolated avulsion can also occur in adolescents with the simple act of
throwing a baseball. In this instance, the sudden contracture of the
forearm flexor muscles may be sufficient to cause the epicondyle to
fail (Fig. 15-50). The literature has reflected a high incidence of medial epicondylar
apophyseal avulsions occurring with arm wrestling in patients near skeletal maturity.104,131 The largest series, reported by Nyska et al.131 from Israel, involved eight boys 13 to 15 years of age, all of whom were treated conservatively with good results.
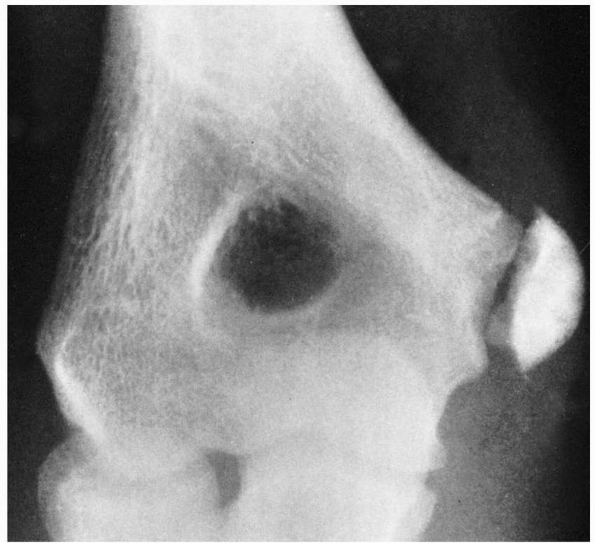 |
|
FIGURE 15-50
Muscle avulsion. Isolated avulsion of the medial epicondyle occurred suddenly in this 14-year-old Little League pitcher after throwing a curve ball. (From Wilkins KE. Fracture of the medial epicondyle in children. Instr Course Lect 1991;40:1-8, with permission.) |
proposed is that this injury is associated with elbow dislocation in
which the ulnar collateral ligament provides the avulsion force. If the
elbow is dislocated when the patient is initially seen, there is no
doubt that this is a major factor in the cause of this fracture. The
question of whether this fracture is caused by an occult or partial
elbow dislocation that has reduced spontaneously is often raised. Some
investigators12,16,62
have noticed calcification development in the lateral collateral
ligaments and adjacent lateral periosteum after fracture. They believed
this calcification was evidence that this ligament had been stretched
during the process of elbow dislocation. Marion and Faysse107
found that most elbow dislocations associated with this injury were
posterolateral, but some pure lateral, posterior, and posteromedial
dislocations were also observed.
epicondylar fragment into the joint can occur without a dislocation.
Patrick140 believed that when an
extreme valgus stress was applied to the joint, a vacuum was created
within the joint that “sucked in” the avulsed epicondylar fragment.
acute apophyseal injury of the distal humerus. The direct blow
mechanism appears to occur only rarely. Many of these injuries may be
associated with an elbow dislocation that may or may not have reduced
spontaneously.
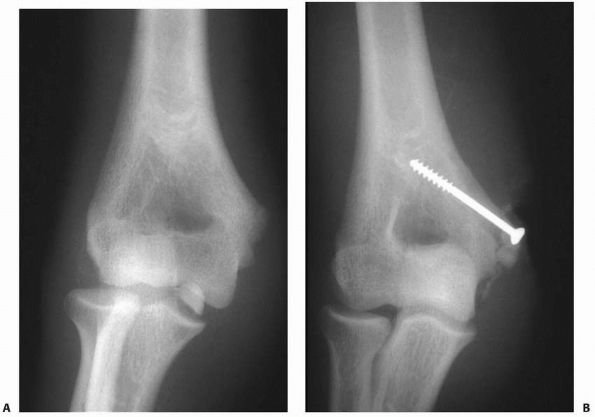 |
|
FIGURE 15-51 A. Entrapment of fracture fragment in medial epicondylar fracture with posterolateral elbow dislocation. B. After fragment extraction, open reduction, and screw fixation.
|
distally. Avulsion generally involves only the apophysis, but a small
flake of metaphyseal bone is occasionally attached to the apophyseal
fragment. The fracture line rarely passes through the apophysis, and
only part of the apophysis is avulsed.169
Although these partial avulsions may appear as only minor injuries, the
partial fragment can be incarcerated within the joint just as easily as
the full apophysis (Fig. 15-51).
incarcerated into the joint, the raw bone surface may become adherent
to the coronoid process of the ulna.155
In late cases, the union of the fragment to the coronoid process may
make extraction difficult. A universal finding when the fragment is
incarcerated within the joint is a thick fascial band that binds the
ulnar nerve to the underlying muscle.7,140
The constriction that this band creates is believed to be responsible
for either the immediate or late dysfunction of the ulnar nerve.
associated with this injury include fracture of the radial neck,
olecranon, or coronoid process. If the epicondyle fragment is only
rotated on its axis, the anterior band of the ulnar collateral ligament
can become lax. This laxity can produce some medial elbow instability
during extension.204
that can be useful in determining the proper treatment method. In the
discussion of this classification, the clinical and radiographic
findings are delineated for each type
of
fracture pattern. Initially, we have separated these injuries into two
primary categories based on whether the injuries are acute or chronic.
|
TABLE 15-3 Fractures of the Medial Epicondyle Apophysis: Classification
|
||||||
|---|---|---|---|---|---|---|
|
In undisplaced fractures, the physeal line remains intact. The clinical
manifestations usually consist only of swelling and local tenderness
over the medial epicondyle. Crepitus and motion of the epicondyle are
usually not present. On radiograph, the smoothness of the edge of the
physeal line remains intact. Although there may be some loss of soft
tissue planes medially on the radiograph, displacement of the elbow fat
pads may not be present because the pathology is extra-articular.74
stronger avulsion force, so there is often more soft tissue swelling.
Palpating the fragment may elicit crepitus because the increased
displacement allows motion of the fragment. On radiograph, there is a
loss of parallelism of the smooth sclerotic margins of the physis (Fig. 15-52).169 The radiolucency in the area of the apophyseal line is usually increased in width.
In significantly displaced fractures, there is no question as to
whether the fragment is displaced, as it may be palpable and freely
movable. Because it is displaced a considerable distance from the
distal humerus, crepitus between the fragments may not be present.
There may have been an elbow dislocation that reduced spontaneously or
by manipulation. On the other hand, there may have been no
documentation of the original dislocation. On radiograph, the long axis
of the epicondylar epiphysis is rotated medially (Fig. 15-53).
The displacement usually exceeds 5 mm, but the fragment remains
proximal to the true joint surface. This fragment may contain a
metaphyseal fragment.
In many instances, the elbow appears reduced. The key clinical finding
is a block to motion, especially extension. The epicondylar fragment is
usually between the joint surfaces of the trochlea and the semilunar
notch of the olecranon. On radiograph, any time the fragment appears at
the level of the joint, it must be considered to be totally or
partially within the elbow joint until proven otherwise.140
If the radiograph is examined carefully, the elbow is usually still
found to be incompletely reduced. Due to an impingement of the fragment
within the joint, a good AP view may be difficult to obtain because of
the inability to extend the elbow fully. If the fracture is old and if
the fragment is fused to the coronoid process, widening of the medial
joint space may be the only clue that the fragment is lying in the
joint. The epicondylar ossification center may become fragmented and
mistaken for the fragmented appearance of the medial crista of the
trochlea.31,155 Absence of the apophyseal center on radiograph may be further
confirmatory evidence that the fragment is within the joint. Comparison
radiographs of the opposite elbow may be necessary to delineate the
true pathology.
 |
|
FIGURE 15-52 AP radiograph shows loss of normal smooth margins of the physis after type II medial epicondylar fracture.
|
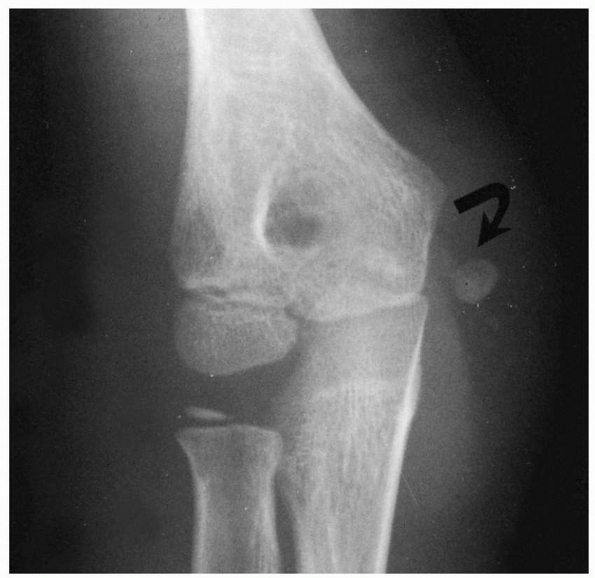 |
|
FIGURE 15-53 Type III displaced medial epicondylar fracture. AP view of an elbow in which the epicondyle (arrow) is significantly displaced both distally and medially. In addition, the fragment is rotated medially.
|
if the elbow is dislocated, the fragment can still lie within the joint
and prevent reduction. Recognition of this fragment as being within the
joint before a manipulation should alert the physician of the possible
need for open reduction. There should be adequate relaxation during the
manipulative process. An initial manipulation to extract the fragment
from the elbow joint may need to be accomplished before a satisfactory
closed reduction of the elbow joint can be obtained (Fig. 15-54).
from either a direct blow or avulsion of only part of the apophysis. In
either case, the fragments may or may not be displaced. The normal
lucent line formed by the overlying metaphyseal border should not be
confused with this injury. Although described by Silberstein et al.,169 this intrafragment fracture is a rare presentation.
diagnostic points have been discussed in the previous section on the
classification of this injury, much of the emphasis in this section is
on the determination of elbow instability. Because the anterior oblique
band of the ulnar collateral ligament may be attached to the medial
epicondylar apophysis, the elbow may exhibit some instability after
injury. To evaluate the medial stability of the elbow, Woods and Tullos204 and Schwab et al.164
advocated a simple valgus stress test. This test is performed with the
patient supine and the arm abducted 90 degrees. The shoulder and arm
are externally rotated 90 degrees. The elbow must be flexed at least 15
degrees to eliminate the stabilizing force of the olecranon. If the
elbow is unstable, simple gravity forces will open the medial side. A
small additional weight or sedation may be necessary to acquire an
accurate assessment of the medial stability with this test.
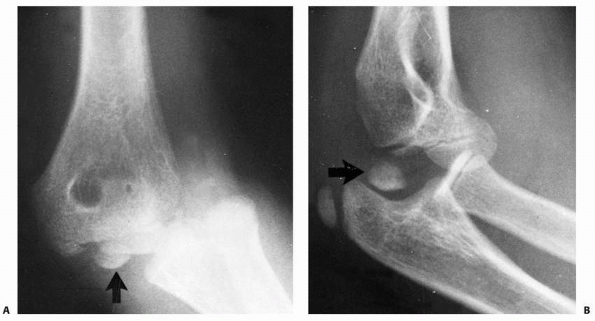 |
|
FIGURE 15-54 Dislocation with incarceration. A. AP view showing a posterolateral elbow dislocation. The presence of the medial epicondyle within the elbow joint (arrow) prevented a closed reduction. B. The lateral view of the same elbow demonstrates the fragment (arrow) between the humerus and olecranon.
|
nerve must be carefully assessed. It is especially wise to document the
presence or absence of an ulnar nerve injury before instituting therapy.
the only clue in fractures that are only slightly displaced or
nondisplaced. If the fragment is significantly displaced, the
radiographic diagnosis is usually obvious. If the fragment is totally
incarcerated in the joint, however, it may be hidden by the overlying
ulnar or distal humerus. The clue here is the total absence of the
epicondyle from its normal position just medial and posterior to the
medial metaphysis.
that properly performed MRI might disclose acute or chronic injury to
the medial epicondylar apophysis. Recommended pulse sequences for
evaluating the apophysis include fat-suppressed gradient echo imaging.
On MRI, increased signal intensity and abnormal widening of the medial
epicondylar physis are seen, typically with surrounding soft tissue
edema.
If the fracture is only minimally displaced and if it is the result of
an avulsion injury, there may be no effusion because all the injured
tissues remain extra-articular. In fractures associated with elbow
dislocation, there is rupture of the capsule, so its ability to confine
the hemarthrosis is lost. In minimally displaced fractures of the
medial
epicondyle
with significant hemarthrosis, the evaluation must be especially
thorough to ensure that an unrecognized fracture involving the medial
condylar physis or an associated elbow dislocation is not present.
condylar physis. This is especially true if the secondary ossification
centers are not present (see “Fractures Involving the Medial Condylar
Physis”). If there is a significant hemarthrosis or a significant piece
of metaphyseal bone accompanying the medial epicondylar fragment,
arthrography or MRI may be indicated to determine if there is an
intra-articular component to the fracture (Fig. 15-55).
agreement as to the proper method of treating fractures that are
undisplaced or only minimally displaced. These first two types are
easily treated with simple immobilization for comfort. Some
investigators have recommended initiation of motion early to prevent
stiffness, which is the most common complication of this injury.16,173
Likewise, if the fragment is incarcerated in the joint, the accepted
treatment is to extract the fragment from the joint by manipulation or
surgical intervention.
treatment method for patients with significant displacement (fragment
displacement more than 5 mm).
reports in which only one method (i.e., operative or nonoperative) of
treatment of all displaced fractures was used, results tend to support
that method. The best argument for surgical management comes from Hines
et al.80 whose practice was to
surgically repair all fractures displaced more than 2 mm. They found
that 96% of their patients had good to excellent results. Bad results
were attributed mainly to technical errors. Josefsson and Danielsson89
obtained equal results and treated all of these injuries
nonoperatively. Although more than 60% of their patients demonstrated
nonunion on radiograph, these investigators had an equal number of good
results at a mean follow-up of 11 years. Other reports in the literature5,134,202 also demonstrated the overall good results with nonoperative management.
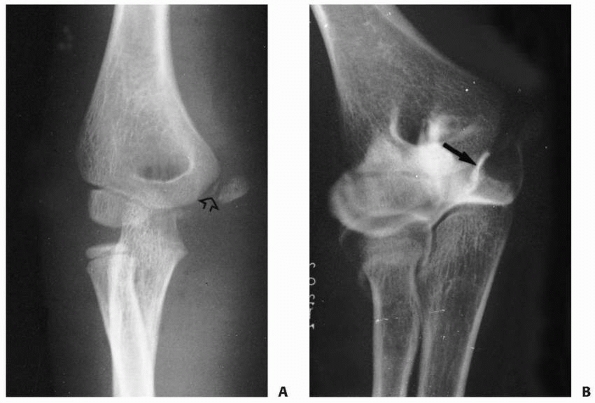 |
|
FIGURE 15-55 Intra-articular extension. A.
Injury film in a 7-year-old girl who was initially suspected of having only a fracture of the medial epicondyle. In addition to moderate displacement, there was a significant metaphyseal fragment (arrow). B. An arthrogram revealed intra-articular components (arrow), which defined this injury instead as a fracture involving the medial condylar physis. (Courtesy of Carl McGarey, MD.) |
treatment results comes from reports in which both methods were used in
the same institution. Bede et al.12
had superior results in patients treated nonoperatively compared with
those treated operatively. This same superiority of nonoperative
management has been found in subsequent reports as well.16,62,202
reported that surgical intervention only added to the original trauma
produced by the dislocation, increasing the residual loss of motion.
The indications for operative intervention in acute injuries are
divided into two categories: absolute and relative. The single absolute
indication is incarceration of the epicondylar fragment within the
joint. The relative indications include ulnar nerve dysfunction and a
need for elbow stability.
If the fragment is found in the joint acutely, it must be removed.
There are proponents and techniques of both nonoperative and operative
extraction of the fragment.
methods of extracting the fragment by nonoperative methods have been
proposed. The success rate of extracting the fragment successfully from
the joint by manipulation alone is only about 40%.140 All the nonoperative methods require either heavy sedation or light general anesthesia.
It involves placing a valgus stress on the elbow while supinating the
forearm and simultaneously dorsiflexing the wrist and fingers to place
the forearm muscles on stretch; theoretically, this maneuver should
extract the fragment from the
joint. To be effective, this procedure should be carried out within the first 24 hours after injury.
to extract the fragment by manipulative techniques is an indication to
proceed with open surgical extraction. Once open extraction and
reduction have been performed, many methods have been advocated to
stabilize the fragment, including screw fixation or sutures in the
comminuted fracture. Excision has also been advocated, especially if
the fragment is comminuted.
challenged the opinion that surgery is detrimental in patients with
late incarceration, and the idea remains controversial. In their
patients in whom the fragment was surgically extracted an average of 14
weeks after injury, 80% more elbow motion was regained. In addition,
the patients’ preoperative pain was relieved, and the ulnar dysfunction
resolved. On a long-term basis, intra-articular retention of the
fragment may not be all that disabling. Rosendahl155
reported an 8-year follow-up of a fragment retained within the joint.
The epicondyle had fused to the semilunar surface of the ulna,
producing a large bony prominence clinically. There was only minor loss
of elbow motion, with little functional disability.
Ulnar nerve dysfunction is a relative indication for operative
intervention. If there are mild-to-moderate ulnar nerve symptoms at the
time of the injury, there is usually no need to explore the nerve,
because most of these mild symptoms resolve spontaneously.16,42
If the dysfunction is complete, then the ulnar nerve is probably
wrapped around the fragment and should be explored surgically. One of
the original fears was that the raw surface of the fracture fragment
would create scar tissue around or adjacent to the nerve and cause
continued dysfunction. Thus, it was originally recommended that the
ulnar nerve should be transposed at the time of open reduction.195 Subsequent reports have not found this step to be necessary.186
symptoms can even occur after fractures of the epicondyle that are not
associated with elbow dislocation. In a review of more than 100
patients with uncomplicated fractures involving the medial epicondylar
apophysis, Patrick140 could not find
any instance in which a delayed ulnar neuritis developed. He found some
patients with late ulnar neuritis after fractures that were associated
with elbow dislocation. Bernstein et al.16
found that their patients with initial ulnar nerve symptoms all did
well when treated nonoperatively. Thus, the original fear of delayed
ulnar nerve dysfunction has been dispelled.
suggested that even minor forms of valgus instability after elbow
injuries involving the medial epicondylar apophysis can cause
significant disability in athletes. This condition is especially true
in athletes who must have a stable upper extremity, such as baseball
pitchers, gymnasts, or wrestlers. In younger adolescents (younger than
14 years of age), the anterior band of the ulnar collateral ligament
often displaces with the apophyseal fragment. In older individuals (15
years or older), large fragments may be avulsed without a ligamentous
injury. Rather than depending on arbitrary measurements of fracture
displacement, Woods and Tullos204
recommended using the gravity valgus stress test to determine the
presence or absence of valgus instability. They believed that
demonstration of a significant valgus instability, using this simple
gravity test, was an indication for surgical intervention in patients
who require a stable elbow for their athletic activities. Pimpalnerkar
et al.144 also suggested that
clinical evidence of instability, as shown by gravity valgus stress
testing, is an indication for operative fixation.
as a rough guide to treatment. We also strongly consider the expected
activity of the involved extremity in deciding on nonoperative or
operative treatment (Table 15-4).
including fractures associated with elbow dislocations. The parents are
warned that no matter which type of treatment is provided, some loss of
elbow extension may occur. They should be reassured, however, that this
loss of motion, if it does occur, is not usually of any functional or
cosmetic significance. The elbow is immobilized initially with a
removable posterior splint, used mainly for comfort and some support.
this injury, we promote early active motion. The patient is encouraged
to remove the splint and start active motion as soon as 3 to 4 days
after injury. The splint is exchanged for a sling as soon as the
patient feels he or she no longer needs it for support. The same
instructions apply to the sling: it is also discarded when it is no
longer needed. This regimen of early motion is also used in fractures
associated with a documented dislocation. Redislocation after elbow
dislocation is rare, but elbow stiffness is common, so it is more
important to initiate motion as soon as possible after reduction of the
elbow. Due to the greater amount of soft tissue injury associated with
an elbow dislocation, the patient may not feel comfortable initiating
early motion until about 5 to 7 days after reduction. Physical therapy
should be used only if voluntary active motion is difficult to obtain.
The therapist should emphasize modalities designed to decrease swelling
and pain and re-establish strength. Range of motion should be achieved
only by active means, not by passive stretching.
cannot be extracted by manipulative means from within the elbow joint.
Second, we stabilize the epicondyles operatively in patients whose
expected high-level physical activity requires a stable elbow. We
realize, however, that it is difficult to predict the athletic
potential of a young child.
|
TABLE 15-4 Authors’ Preferred Treatment
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||
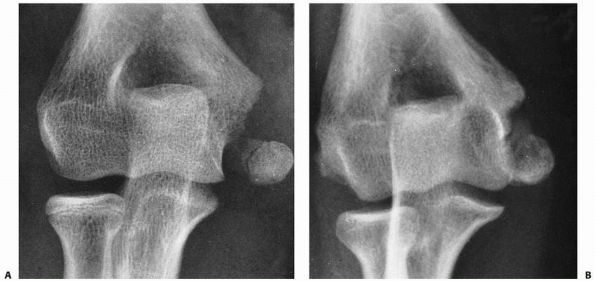 |
|
FIGURE 15-56 Nonoperative management. A.
Postreduction film of a 13-year-old girl who sustained a displaced medial epicondyle following an acute elbow dislocation in her nondominant extremity. She was treated nonoperatively. B. One year later, the fragment has remained distally displaced with an apparent fibrous union. The patient, however, had a full painless range of elbow motion. (From Wilkins KE. Fractures of the medial epicondyle in children. Instr Course Lect 1991;40:1-8, with permission.) |
to attempt to extract the fragment before reduction. If this technique
fails to remove the fragment or if there is any ulnar nerve
dysfunction, we proceed directly with an open procedure. The fragment
is then extracted under direct vision just before reducing the elbow
dislocation. If the elbow is reduced and if the fragment is
incarcerated, we avoid the initial manipulation and proceed directly
with an open extraction. We usually stabilize these fractures with a
single cannulated screw, which allows almost immediate motion, rather
than wires or pins.
intervention is to ensure a stable elbow in patients participating in
high-demand activities with their upper extremity (Fig. 15-57).
This usually involves the dominant extremity of baseball pitchers,
tennis players, or football quarterbacks. In wrestlers and gymnasts,
the stability of the nondominant extremity also must be considered,
which is best achieved with operative fixation.
in deciding on the need for operative stabilization of an athlete’s
medial epicondyle. Almost all of these patients with any significant
displacement have a positive valgus stress test. Our decision is based
primarily on the patient’s need to have a very stable elbow for his or
her athletic or work activity.
Pins provide stability but do not allow early motion. Fortunately, most
patients are mature enough so that the fragment can be secured with a
cannulated screw.
approach to the fracture site. We make a longitudinal incision just
anterior to the medial epicondyle. The fragment is usually displaced
distally and anteriorly. The periosteum is removed from the fracture
site, and the clot is extracted by irrigation. It is important to
identify and protect the ulnar nerve, but a complete dissection of the
nerve is usually unnecessary. A small towel clip is used to reduce the
fracture while the elbow is flexed and the forearm is pronated. Again,
the medial epicondyle is normally situated posteriorly. The fragment is
reduced and stabilized temporarily with one or two small K-wires. The
final fixation is achieved using a screw, either partially threaded and
overdrilled, in the epicondylar fragment to compress it against the
metaphysis or a cannulated 4.0-mm screw. After removal of the K-wires,
the elbow is checked to ensure valgus stability and re-establishment of
a full range of motion. After the surgical incision is closed, the
extremity is placed in a long-arm cast, which is bivalved at 5 to 10
days, and active motion is initiated.
to achieve elbow stability, an American Society for Internal Fixation
spiked washer can be used to secure the multiple pieces to the
metaphysis. If the washer is used, a second procedure may be necessary
to
remove the spike washer once the epicondyle is securely united to the
metaphysis. If removal is impossible, we simply excise the fragments
and reattach the ligament to the bone and periosteum at the base of the
epicondylar defect.
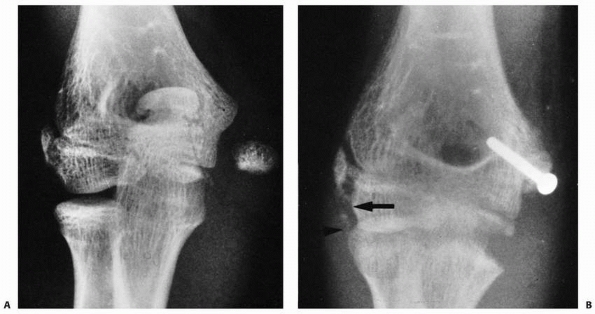 |
|
FIGURE 15-57 Operative stabilization. A.
Injury film in a 12-year-old gymnast. Although this was a nondominant extremity, it was thought that both elbows needed stability. B. Radiographs taken 4 weeks postoperatively show stabilization of the fragment with a single screw. There was also calcification of the lateral ligaments (arrows), confirming that the elbow was probably originally dislocated as well. (From Wilkins KE. Fractures of the medial epicondyle in children. Instr Course Lect 1991;40:1-8, with permission.) |
the medial epicondylar apophysis, few complications are attributed to
the fracture itself. The major complications that result in loss of
function are failure to recognize incarceration in the joint and ulnar
or medial nerve dysfunction. Most of the other complications are minor
and result in only minimal functional or cosmetic sequelae (Table 15-5).
|
TABLE 15-5 Fractures of the Medial Epicondylar Apophysis: Complications
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Failure to recognize incarceration of the epicondylar fragment into the
joint can result in significant loss of elbow motion, especially if it
remains incarcerated for any length of time. The management for late
incarceration was detailed in the previous section on treatment.
other major complication associated with this injury is the development
of ulnar nerve dysfunction. The incidence of ulnar nerve dysfunction
varies from 10% to 16%.12,107 If the fragment is entrapped in the joint, the incidence of ulnar nerve dysfunction may be as high as 50%.12,52
More profound ulnar nerve injury has been reported after manipulative
procedures.140 Thus, in patients
with fragments incarcerated in the joint, manipulation may not be the
procedure of choice if a primary ulnar nerve dysfunction is present.
Patients in whom the fragment was left incarcerated in the joint for a
significant time have experienced poor recovery of the primary ulnar
nerve injury.107
ulnar nerve is the major nerve injured, the median nerve may be trapped
between a bony fragment and the distal humerus.133
It is speculated that the nerve can be entrapped between the apophyseal
fragment and the distal humerus at the time of the original injury.
This type of injury is described in greater detail in the section on
complications of elbow dislocations.
complications are minimal. Nonunion of the fragment with the distal
metaphysis occurs in up to 50% of fractures with significant
displacement.12 This appears to be more of a radiographic problem than a functional problem.
elbow extension. A loss of 5% to 10% can be expected to develop in
about 20% of these fractures. Little functional deficit is attributed
to this loss of elbow dysfunction. Prolonged immobilization seems to be
the key factor in loss of elbow extension. Again, it is important to
emphasize before treatment is begun that loss of motion is common after
this injury, regardless of the treatment method used.
vigorous and repeated manipulation to extract the fragment from the
joint. As with many other elbow injuries, myositis may be a result of
the treatment rather than the injury itself. Myositis ossificans must
be differentiated from ectopic calcification of the collateral
ligaments, which involves only the ligamentous structures. This
condition may occur after repeated injuries to the epicondyle and
ligamentous structures (Fig. 15-58). Often,
this calcified ligament is asymptomatic and does not seem to create
functional disability. The cosmetic effects are minimal. In some
patients, an accentuation of the medial prominence of the epicondyle
creates a false appearance of an increased carrying angle of the elbow.
In his extensive review, Smith173 recognized only a slight decrease in the carrying angle in two patients.
to treat. One of the authors has treated a high-performance adolescent
baseball pitcher who had to stop pitching after nonoperative management
of a medial epicondylar fracture. The patient had developed a fibrous
nonunion (Fig. 15-59). Attempts to establish
union surgically were unsuccessful. The patient continued playing
baseball, but had to change to another position.
injury, with only a few isolated injuries described, mostly in
textbooks.
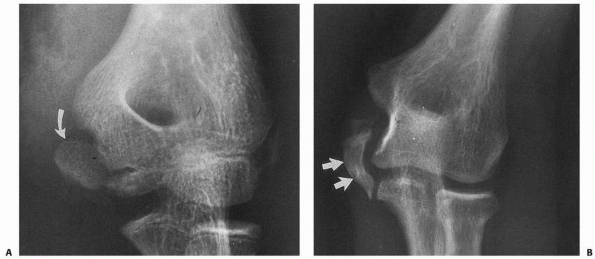 |
|
FIGURE 15-58 Heterotopic calcification. A. Injury to an 11 -year-old who had moderate displacement of the medial epicondyle (arrow). B. One year later, she had considerable calcification of the ulnar collateral ligament (arrows).
Other than mild instability with valgus stress, the patient had full range of motion and was asymptomatic. (Courtesy of Mark R. Christofersen, MD.) |
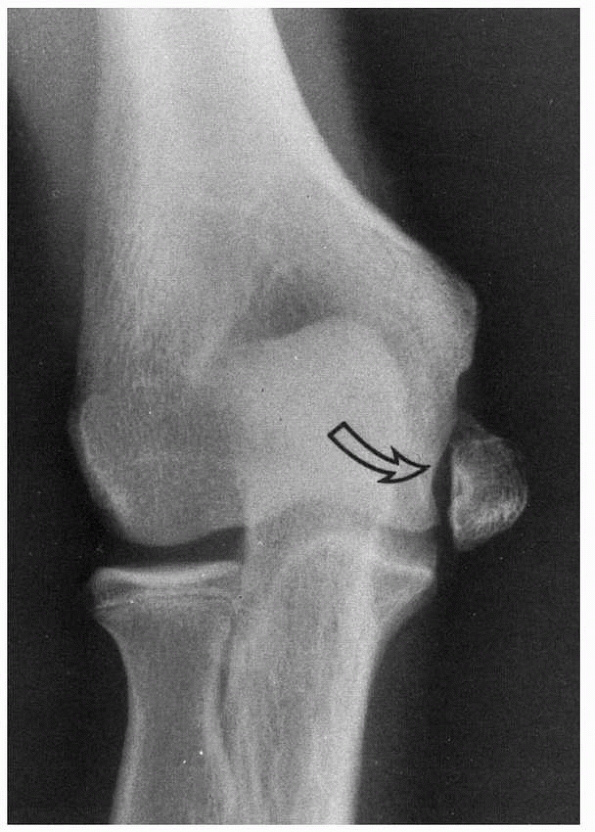 |
|
FIGURE 15-59
Nonunion in an athlete. This 15-year-old baseball pitcher had an untreated medial epicondyle fracture 1 year before this radiograph He developed a fibrous union, but the epicondyle was shifted distally (arrow). His elbow was unstable enough to prevent him from pitching. |
misinterpreted as a small chip fracture, a thorough understanding of
the anatomy and ossification process is essential for evaluating
injuries in this area.
present for a considerable period but does not become ossified until
the second decade. The best discussion of the anatomy of the
ossification process is in a report by Silberstein et al.,168 and much of the following discussion is paraphrased from their
work. Just before ossification of the apophysis, the ossification
margin of the lateral supracondylar ridge of the distal metaphysis
curves abruptly medially toward the lateral condylar physis (Fig. 15-60).
This process causes the osseous borders on the lateral aspect of the
distal humerus to take the shape of the number 3. The central wedge of
this defect contains the cartilaginous lateral epicondylar apophysis,
which begins to ossify around 10 to 11 years of age. Ossification
begins at the level of the lateral condylar physeal line and proceeds
proximally and distally to form a triangle, with the apex directed
toward the physeal line. The shape of the epicondylar apophyseal
ossification center may also be in the form of a long sliver of bone
with an irregular ossification pattern. Silberstein et al.168
noted that the fracture line involving the lateral condylar physis
often involves the proximal physeal line of the lateral epicondylar
apophysis. Thus, this apophysis is almost always included with the
lateral condylar fragment.
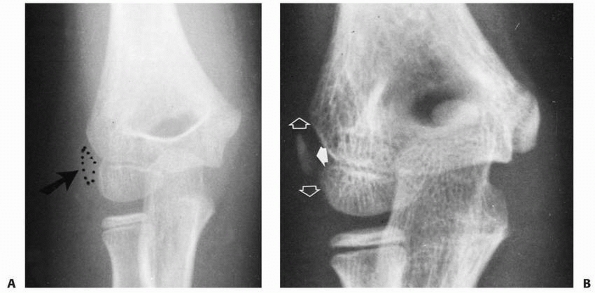 |
|
FIGURE 15-60 Lateral epicondylar apophysis. A. The cartilaginous apophysis occupies the wedge-shaped defect at the margin of the lateral condyle and metaphysis (arrow). The dotted line shows the margin of the cartilaginous apophysis. B. Ossification of the apophysis begins at the central portion of the wedge defect (solid arrow) and progresses both proximally and distally (open arrows) to form a triangular center.
|
blow to the lateral side of the elbow. In children, because the forearm
extensor muscles originate from this area, it is believed that avulsion
forces from these muscles can be responsible for some of these
injuries. Hasner and Husby75
suggested that the location of the fracture line in relation to the
origins of the various extensor muscles determines the degree of
displacement that can occur (Fig. 15-61). If
the proximal part of the fracture line lies between the origin of the
common extensors and the extensor carpi radialis longus, there is
usually little displacement. If the fracture lines enter the area of
origin of the extensor carpi radialis longus, then considerable
displacement can occur.
surface of the apophysis and proceeds centrally, the ossification
center often appears separated from the lateral metaphysis and lateral
condylar epiphysis. This natural separation can be confused with an
avulsion fracture. The key to determining true separation is looking
beyond the osseous tissues for the presence of associated soft tissue
swelling (Fig. 15-62). If the ossification
center lies distal to the osteochondral border of the lateral condylar
epiphysis, it should be considered displaced (Fig. 15-63).
treatment usually consists of simple immobilization for comfort.
Although nonunion of the fragment can occur, this radiographic finding
usually does not affect elbow function.
fractures involving the lateral epicondylar apophysis: entrapment of
the fragment, either within the elbow joint115 or between the capitellum and the radial head.59
the elbow flexed.210
This injury is rare in normal children because an avulsion force
generated through the expansion of the triceps tendon inserting on the
metaphysis distal to the physis usually results in a fracture through
the more distal metaphysis. Carney et al.25 described a healthy 11-year-old boy who sustained a displaced apophyseal olecranon fracture in a fall. Bracq21
noted that fractures of the olecranon apophysis appeared to occur more
often in children with osteogenesis imperfecta (OI), and several
reports since that time have confirmed his observation.44,68,97,182,210 Why children with OI may be predisposed to this injury is unknown. Zionts and Moon210
suggested that a combination of weakness of the subchondral bone
adjacent to the physis of the proximal olecranon and increased laxity
of the triceps expansion might make the olecranon apophysis more
vulnerable to injury in children with OI. Because OI was not recognized
in half of their patients, they suggested that OI should be considered
in any child who has an isolated, displaced fracture of the olecranon
apophysis, especially when the injury results from relatively minor
trauma.210
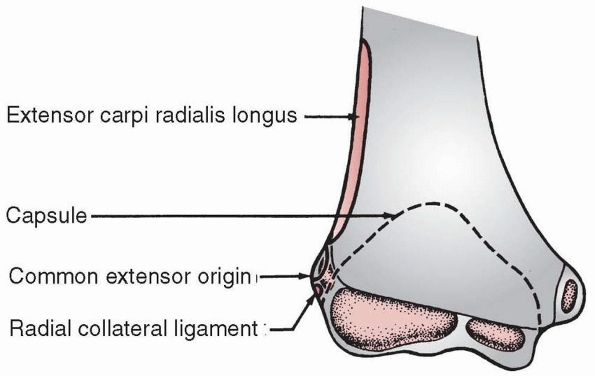 |
|
FIGURE 15-61
Soft tissue attachments. The origins of the forearm and wrist extensor muscles, radial collateral ligament, and outline of the capsule are shown in relation to the lateral epicondylar apophysis. (From Hasner E, Husby J. Fracture of the epicondyle and condyle of humerus. Acta Chir Scand 1951;101:195-202, with permission.) |
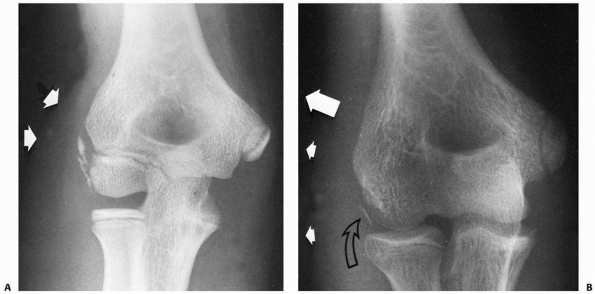 |
|
FIGURE 15-62 Lateral swelling. A. Soft tissue swelling in the area of the lateral epicondylar apophysis (arrows)
suggests an undisplaced fracture involving the apophysis. The fragmentation of the apophysis is caused by irregular ossification. B. A small avulsion of the lateral epicondyle (open arrow) in an adolescent who is almost skeletally mature. There was considerable soft tissue swelling in this area (solid arrows). |
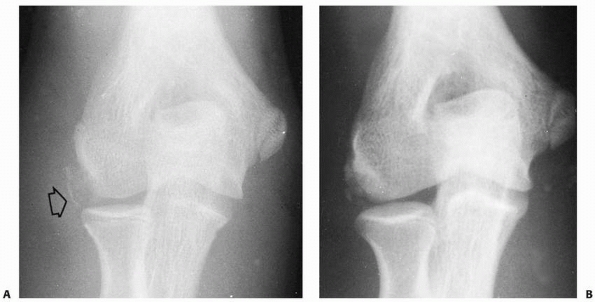 |
|
FIGURE 15-63 Avulsion injury. A. Avulsion of a portion of the lateral epicondyle in an adolescent (arrow). The fragment is at the level of the joint. Most of the epicondyle has fused to the condyle. B. The appearance 9 months later shows fragmentation and partial union of the fragment. (Courtesy of R. Chandrasekharan, MD.)
|
immobilization. Operative treatment is usually recommended for
displaced fractures of the olecranon apophysis in all children,
although the amount of “acceptable” displacement ranges from 3 to 5 mm.
Fixation is with two smooth intramedullary K-wires and
a
tension band of either stainless-steel wire or absorbable suture.
Problems with the K-wires backing out and refracture after hardware
removal have been reported in children with OI50,68,128,210; Gwynne-Jones68 suggested that retaining the hardware or using nonabsorbable sutures might decrease the risk of refracture.
70% of children with OI who sustain an olecranon apophyseal fracture
later have a fracture of the contralateral olecranon apophysis; the
mean time to second fracture reported by Gwynne-Jones68 and by Zionts and Moon210 was 7 months. Parents should be advised of this possibility, and the child’s high-risk activities should be avoided.
reported 5 adolescent baseball pitchers with chronic elbow pain and
radiographic evidence of olecranon nonunions; the patients ranged in
age from 13 to 17 years (average age: 15 years) and had symptoms for 1
week to 18 months before operative treatment. All five had open
reduction and internal fixation with cannulated compression screws, and
four had additional figure-of-eight tension band wiring. Bone grafting
was done in four, using cancellous bone from the starting hole of the
cannulated screw. All returned to their previous activity levels at an
average of 30 weeks.
demonstrated that the radiographic changes were due to excessive
throwing and emphasized the need for preventive programs. This injury
is thought to be due to excessive tension on the medial epicondyle with
secondary tendinitis. There can also be a repeated compression on the
lateral condyle, producing an osteochondritis.
the Little League are followed (i.e., pitch counts of 50 to 75 pitches
per game depending on age), the incidence of these chronic tension
stress injuries is fairly low.63
Most of the problems arise when overzealous parents and coaches require
excessive pitching preseason and at home between practices. Albright5
found a greater incidence in pitchers who had improper pitching
techniques. The spectrum of these chronic injuries is outlined in Table 15-6.
|
TABLE 15-6 Spectrum of Chronic Tension Stress Injuries of Medial Epicondylar Apophysis
|
|||||
|---|---|---|---|---|---|
|
Syndrome), the history is usually quite characteristic. It is found in
young baseball pitchers who are throwing an excessive number of pitches
or who are just starting to throw curve pitches.63
Clinically, this syndrome is manifested by a decrease in elbow
extension. Medial epicondylar pain is accentuated by a valgus stress to
the elbow in extension. There is usually significant local tenderness
and swelling over the medial epicondyle.
humerus is increased due to the chronicity of the stress. The physeal
line is irregular and widened. If the stress has been going on for a
prolonged period, there may be hypertrophy of the distal humerus with
accelerated bone growth. The bone age of the elbow is greater than the
patient’s chronologic age (Fig. 15-64).
the parents, coaches, and player. Once symptoms develop, all pitching
activity must cease until the epicondyle and adjacent flexor muscle
origins become nontender. In addition, local and systemic measures to
decrease the inflammatory response are used. Once the initial pain and
inflammation have decreased, a program of forearm and arm muscle
strengthening is initiated. The pitching technique is also examined to
see if any corrections need to be made. Once strength has been
re-established in the muscles in the upper extremity and motion has
been fully reestablished, the patient is gradually returned to pitching
with careful monitoring of the number of innings and pitches within a
specified time period.
posttraumatic changes that occur in the distal humerus after fractures
in the vicinity of the trochlea: malunion, partial growth arrest, and
vascular injury. The most common form follows some type of elbow
trauma. In some cases, the trauma is occult or poorly defined.17,85,113,116,126,207
This form results in a spectrum from simply a small defect of the
trochlea (fishtail deformity) to complete destruction of the medial
aspect of the distal humerus with a progressive varus deformity,
decreased range of motion, and associated instability of the elbow.
Because it is seldom reported in the literature, the exact incidence is
unknown. Toniolo and Wilkins188
reported a series of 30 cases collected over the past 20 years from
various sources and suggested that osteonecrosis of the trochlea is
probably one of the most unrecognized sequela of injuries to the distal
humerus.
of the blood supply of the distal humerus, it was demonstrated that the
medial crista of the trochlea had two separate blood supply sources (Fig. 15-65).
Neither has anastomoses with each other or with the other metaphyseal
vessels. In the young infant, the vessels are small and lie on the
surface of the perichondrium.
the lateral aspect of the medial crista. These vessels cross the physis
to enter the posterior aspect of the lateral trochlear ossification
center. Their terminal branches lie just under the articular surface.
Thus, they are particularly vulnerable to injury when the fracture line
occurs through this area, as is typical in fractures of the medial
condylar physis, lateral condyle, or a T-condylar
fracture.
By the same token, a fracture in the supracondylar area in which the
fracture line is very distal or a total distal humeral physeal
displacement can also disrupt the lateral trochlear epiphyseal vessels
as they course along the surface of the metaphysis or at their entrance
into the physeal plate.
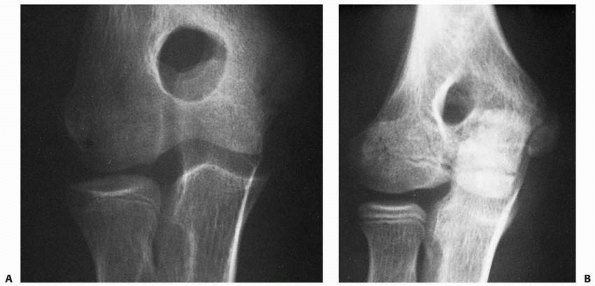 |
|
FIGURE 15-64 Chronic tension stress. A. AP view of a 13-year-old pitcher with chronic pain and significant loss of elbow motion. The bone age is around 15 years. B. Same view of the opposite elbow with a bone age of 13 years.
|
nonarticulating surface of the trochlea. This set of vessels supplies
the most medial aspect of the medial crista or the medial portion of
the trochlear epiphysis. As shown in Haraldsson’s71,72 studies, there appear to be no anastomoses between the two sets of vessels supplying the trochlear epiphysis.
appearance and development. Before these centers appear, the vessels
are more superficial and less well defined. It is speculated that a
lesion in these immature vessels in children leads only to a delay in
the appearance of the centers. In older children, where there is
already a well-defined ossification center, disruption produces a true
bony osteonecrosis of one or both of the trochlea’s ossification
centers. This can result in a partial or total absence of further
epiphyseal ossification, leading to hypoplasia of the central or whole
medial aspect of the trochlea.
central defect (type A) or total hypoplasia manifest by complete
absence of the trochlea (type B), depending on the extent of the
vascular injury.
medial crista or apex of the trochlea becomes involved in the necrotic
process, which produces the typical fishtail deformity (Fig. 15-66).
This more common pattern of necrosis seems to occur with very distal
supracondylar fractures or with fractures involving the lateral
condylar physis.
This type of necrosis has occurred as a sequela of fractures involving
the entire distal humeral physis or fractures of the medial condylar
physis192 and can lead to a cubitus varus deformity in which the angulation progresses as the child matures.
between the two patterns of necrosis. Patients who have the type A or
fishtail deformity usually do not develop any angular deformities. The
severity of the fishtail deformity is related to the degree of necrosis
and seems to dictate the severity of the symptoms. In children who have
a pattern of total osteonecrosis of the trochlea, including part of the
nonarticular surface, a progressive varus deformity usually develops.
Because the total medial trochlear surface is disrupted, significant
loss of range of motion also develops. These deformities usually worsen
cosmetically and functionally as the child matures. Early degenerative
joint disease with a loss of range of motion is the most common sequela
in severe cases.
thought to be due to a multiplicity of factors, including joint
malalignment, abnormal position of the ulnar nerve and triceps tendon,
loss of protection by a deep ulnar groove, and the acute angle of
entrance of the two heads of the flexor carpi ulnaris.
consequence of trauma to the vessels at the time of injury, there is no
effective prevention or treatment of the primary necrosis. Treatment is
aimed at only the sequelae of the osteonecrosis of the trochlea. If a
loss of range of motion is due to a significant disruption of the
articular surface itself, there does not appear to be any good
operative or nonoperative method that significantly improves elbow
function. If the osteonecrosis of the trochlea has resulted in a varus
deformity of the elbow, this deformity can be corrected by a
supracondylar osteotomy with ulnar nerve transposition. The correction
of the carrying angle is mostly cosmetic, with little functional
improvement. Surgical treatment carries the risk of increased stiffness
to the already limited elbow.
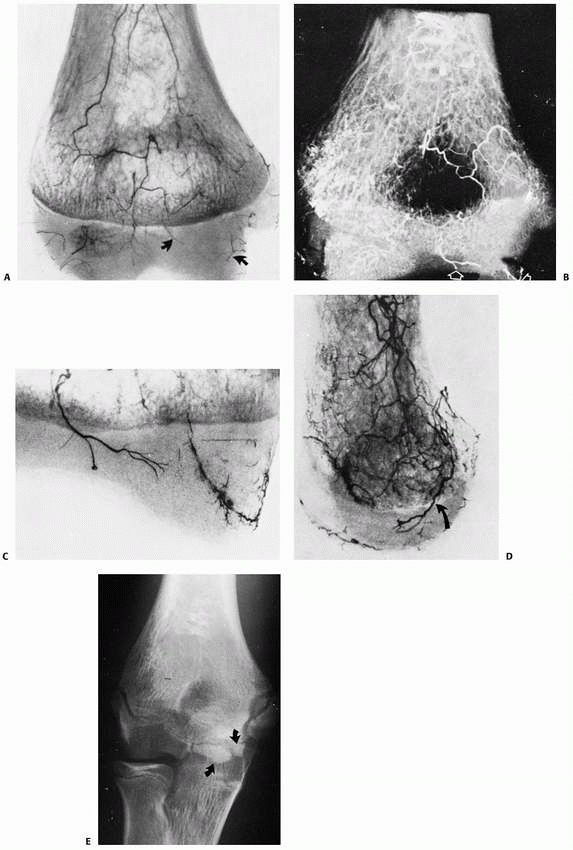 |
|
FIGURE 15-65
Blood supply of the trochlea. A. Intraosseus vasculature in a 3-year-old boy. Only two small vessels supply the medial crista of the trochlea (arrows). The central portion of the crista appears avascular. B. In the lateral view through the medial crista of the trochlea, note that the vessels penetrate the physis posteriorly (arrow) to enter the epiphyseal cartilage. C. Close-up view showing the extent of the vascular supply of the trochlea. Note that no anastamoses are seen between these medial and lateral vessels. D. Lateral view through the medial crista of the trochlea. Note that the vessels penetrate the physis posteriorly (arrow) to enter the epiphyseal cartilage. (A-D: reprinted from Haraldsson S. On osteochondritis deformans juvenilis capituli humeri including investigation of intraosseous vasculature in distal humerus. Acta Orthop Scand Suppl 1959;38:1-232, with permission.) E. Radiograph of a 12-year-old boy. The persistence of the two separate ossification centers (arrows) of the media crista is seen. The area supplied by the lateral vessel is larger than that supplied by the medial vessel. |
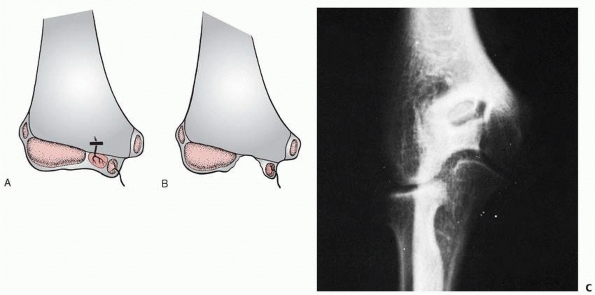 |
|
FIGURE 15-66
Fishtail deformity. A,B. Type A deformity. Osteonecrosis of only the lateral ossification center creates a defect in the apex of the trochlear groove. C. The typical fishtail deformity is seen in a radiograph of a 14-year-old boy who sustained an undisplaced distal supracondylar fracture 5 years previously. |
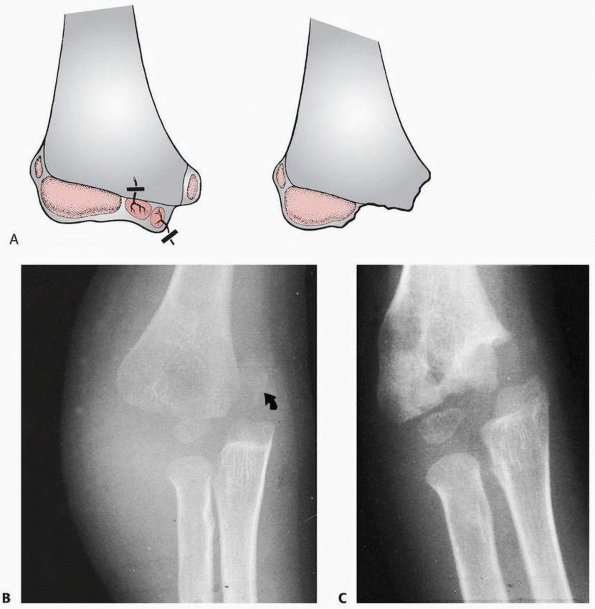 |
|
FIGURE 15-67 Osteonecrosis of the entire trochlea. A.
In this type B deformity, loss of blood supply from both the medial and lateral vessels results in osteonecrosis of the entire medial crista along with a portion of the metaphysis. B. Radiograph of a 4-year-old boy who sustained a type II physeal fracture involving the entire distal humeral physis. In this injury film, there is a large metaphyseal fragment on the medial side (arrow). C. As shown by the appearance 5 months later, a mild varus deformity present is due to an incomplete reduction. The ossification in the medial metaphyseal fragment has disappeared. |
the central groove of the trochlea and courses proximal to the
olecranon and the coronoid fossae, where it divides and separates the
medial and lateral bony columns of the distal humerus. If the proximal
fracture lines are oblique, the fracture may be termed Y-condylar. This injury is rare in skeletally immature children.
who reported 6 patients near skeletal maturity, were accurate when they
said, “the fractures [T-condylar] take on the characteristics of an
adult fracture and should be treated as such.”
low, but it may be underdiagnosed because it is often confused with
other fractures, such as those involving the lateral condylar physis or
total distal physis. Special imaging studies such as arthrograms or MRI
may be necessary to demonstrate the intracondylar aspect in young
children. The combination of an increased awareness of the possibility
of this injury and a more aggressive diagnostic approach may result in
more cases being uncovered in this younger age group.
effect of the articular surface of the olecranon on the distal end of
the humerus. The sharp edge of the semilunar notch or coronoid process
acts as a wedge to break the trochlea and split the condyles, which in
turn separates the two columns of the distal humerus. Flexion and
extension types of injuries have been described.
a direct blow to the posterior aspect of the elbow, usually when the
child falls directly on the flexed elbow. This flexion mechanism in
young children contributes to its rarity because most upper-extremity
injuries in children have a component of elbow hyperextension. In these
flexion injuries, the wedge effect is produced at the apex of the
trochlea by the central portion of the trochlear notch. The condylar
fragments usually lie anterior to the shaft in these flexion injuries (Fig. 15-68A,B).
outstretched arm with the elbow in only slight flexion. This extension
mechanism has been suggested by patients in their description of the
dynamics of the fall and indirectly by the position of the distal
fragments in relation to the diaphyses of the humerus—in other words,
lying posterior (Fig. 15-68C,D). In the extension type of injury, the coronoid portion of the semilunar notch produces the wedge effect.
flexor and extensor muscles may play a role in the displacement pattern
of this fracture. Because of their origins on the epicondyles, they
accentuate both the separation in the coronal plane and the forward
displacement in the sagittal plane. This displacement pattern is often
evident on the injury films (see Fig. 15-68C,D).
in adults. The condylar fragments are often separated, with the
articular surface completely disrupted. In addition to separation of
the condylar fragments by the force of the original injury, the muscles
that originate on these condylar fragments rotate them in both the
coronal and sagittal planes (see Fig. 15-68C,D).
In the sagittal plane, the position of the condylar fragments in
relation to the humeral shaft and metaphysis can either be anterior
(flexor mechanism; see Fig. 15-68B) or posterior (extension mechanism; see Fig. 15-68D).
the condylar fragments are usually separated, but the articular surface
may remain intact because of its large cartilage component (Fig. 15-69).136
Thus, the disruption and displacement are primarily in the osseous
supracondylar area. The elasticity of the cartilage of the distal end
of the humerus often protects the articular surface from being
completely disrupted.
for adult T-condylar fractures have been proposed, but there are
problems with applying these classifications to children’s injuries.
For example, the number of children with this fracture is so small that
no clinician can include all types of fracture patterns in his or her
own experience. In addition, there is no useful classification for
younger patients, in whom the unossified intact articular cartilage is
not visible on radiograph. Toniolo and Wilkins189
proposed a simple classification based on the degree of displacement
and comminution of the fracture fragments. Type I fractures are
minimally displaced (Fig. 15-70A,B). Type II fractures are displaced but do not have comminution of the metaphyseal fragments (Fig. 15-70C). Type III fractures are displaced fractures with comminution of the metaphyseal fragments (Fig. 15-70D,E).
be difficult to determine without using arthrography or MRI. Because
the initial integrity of the articular surface may not be that
important to the prognosis, this factor was not believed to
significantly contribute to a general classification scheme.
extension-type supracondylar fractures. The extended position of the
elbow, along with the massive swelling, is almost identical to that of
the displaced extension type of supracondylar fracture.
In older children, the differentiation must be made from that of a
comminuted supracondylar fracture. Sometimes, the diagnosis is not
obvious until the fragments have been partially reduced, which allows
the vertical fracture lines splitting the trochlea to become more
evident. In younger children, the diagnosis is much more difficult
because the articular surface is not visible. In addition, because of
its rarity, the possibility of a T-condylar fracture may not be
considered in this age group.
either the isolated lateral or medial condyles and complete separation
of the distal humeral physis. In these latter fractures, an important
sign is the presence of a medial or lateral Thurstan-Holland fragment
in the metaphysis.13 The key
differential for the T-condylar fracture is the presence of a vertical
fracture line extending down to the apex of the trochlea.
 |
|
FIGURE 15-68 Mechanism patterns. A,B. The more common flexion pattern in which the condylar fragments are situated anterior to the distal shaft. C,D.
An extensor pattern in which the condylar fragments are situated posterior to the distal shaft. The muscle origins on the respective condyles cause them to diverge in the coronal plane (arrows) and flex in the sagittal plane. |
of the static radiographs, it can be confirmed with varus or valgus
stress films made while the patient is under general anesthesia.13 The use of contrast medium in the form of an arthrogram also is helpful.
recommendations cannot be based on multiple case experiences. Most of
the experience has been based on isolated cases or small series.13,86,93,136 Regardless of the treatment method, certain basic principles must be considered in dealing with these fractures.
fracture and the surgeon’s level of expertise and experience. The
following principles must be considered in planning a treatment method:
-
Elbow articular mobility depends on
articular congruity, correct alignment of the axis of motion, and
debris- and bonefree fossae. -
The stability depends on the integrity of the lateral and medial supracondylar columns.
-
The T-condylar fracture is an articular fracture, so the first goal is to restore and stabilize the joint surface.
-
Closed methods alone usually cannot produce an acceptable result because of the muscle forces applied to the fragments.
-
Most patients are adolescents with minimal potential for bone remodeling.
-
Although surgical reduction may produce
an acceptable reduction on radiograph, it may add to the already
extensive damage to soft tissues; this in turn can contribute to
postoperative stiffness.
 |
|
FIGURE 15-69
Intact articular surface. In this T-condylar fracture in a 7-year-old boy, the thick articular cartilage remains essentially intact, preventing separation of the condylar fragments. This fracture was secured with simple percutaneous pins. |
advocated establishing an anatomic reduction with internal fixation so
that early motion could facilitate a more rapid rehabilitation. In the
two young children described by Beghin et al.,13 operative intervention was necessary to achieve a satisfactory reduction. A review of three series86,93,136
supports surgical management: 29 of the 31 elbows in these combined
series were treated operatively. The investigators of these series
maintained that open reduction and internal fixation was the best way
to restore the integrity of the articular surface and stabilize the
fracture sufficiently to allow early mobilization. All but one of the
patients in this combined series who were treated surgically had good
or very good results at follow-up.
described closed reduction of the intra-articular component, with
fixation by partially threaded pins for interfragmentary compression.
Two elastic titanium intramedullary nails were used for stabilizing the
supracondylar component. T-condylar fractures in two adolescents healed
without complications after using this technique. Both patients
returned to sports with full elbow range of motion at 6 weeks after
surgery.
posterior longitudinal splitting of the triceps without an osteotomy of
the olecranon. This approach gives adequate exposure of the fracture
and the articular surface and does not seem to produce any loss of
strength from splitting the triceps.93 Although one reported patient had radiographic evidence of osteonecrosis of the trochlea,136 another had a nonunion,93
and many had some loss of range of motion, none of these surgically
treated patients demonstrated any significant loss of elbow function or
discomfort.
described a triceps-sparing approach in which the extensor mechanism is
reflected laterally, exposing the whole distal humerus. Remia et al.150
evaluated triceps function and elbow motion in nine patients with
T-condylar fractures treated with open reduction through a
triceps-sparing approach and compared them to those reported after a
tricepssplitting approach. No statistically significant differences
were found in function or range or motion.
standard recommended treatment. Our suggestions are based on a
combination of our clinical experience and the experience of others in
a few series.86,93,136
Our first consideration in these fractures is to re-establish the
integrity of the articular surface to maintain the congruity of the
joint. Usually, this cannot be achieved adequately by closed methods,
so we proceed with an open surgical technique. We have found the simple
classification into three types based on the degree of displacement or
comminution to be helpful in guiding the aggressiveness of our
treatment.
bony supracondylar columns. In children, the periosteum is often intact
and can provide some intrinsic stability. In addition, the thicker
articular and epiphyseal cartilage in skeletally immature children may
still be intact, even if the bony epiphysis appears severed by a
vertical fracture line. Because of this condition, we have found two
methods to be successful for these types of fractures.
general anesthesia and radiographic control to re-establish the
supracondylar columns. If there is anterior or posterior rotation in
the sagittal plane of the metaphyseal portion of the column, a pin
placed into that column can be used as a “joystick” to manipulate the
fragment into a satisfactory position. Once a satisfactory reduction is
achieved, the pin can then be advanced across the fracture site for
fixation. These fractures usually require multiple pins placed
percutaneously, such as those used in comminuted supracondylar
fractures (Fig. 15-71). Because of the rapid healing, the pins can be removed at 3 weeks to allow early active motion.
hinge with traction. The rotational displacement of the condyles
created by the origins of the forearm muscles can be neutralized with
olecranon traction, in which the elbow is suspended at 90 degrees of
flexion. There is usually adequate stability from the callus around the
fracture site at 2 to 3 weeks to discontinue the traction. The elbow is
then immobilized in a hinged cast brace for an additional 2 to 3 weeks.
This immobilization allows the initiation of protected active motion.
With the present emphasis on short hospitalization, however, we find
that skeletal traction is less acceptable for both social and financial
reasons. Skeletal traction may be the only acceptable method of
treatment in patients seen on a delayed basis with extensive skin
abrasions, severe soft
tissue
injury, or gross comminution, in which cast application or other
operative interventions might carry a high risk of infection.
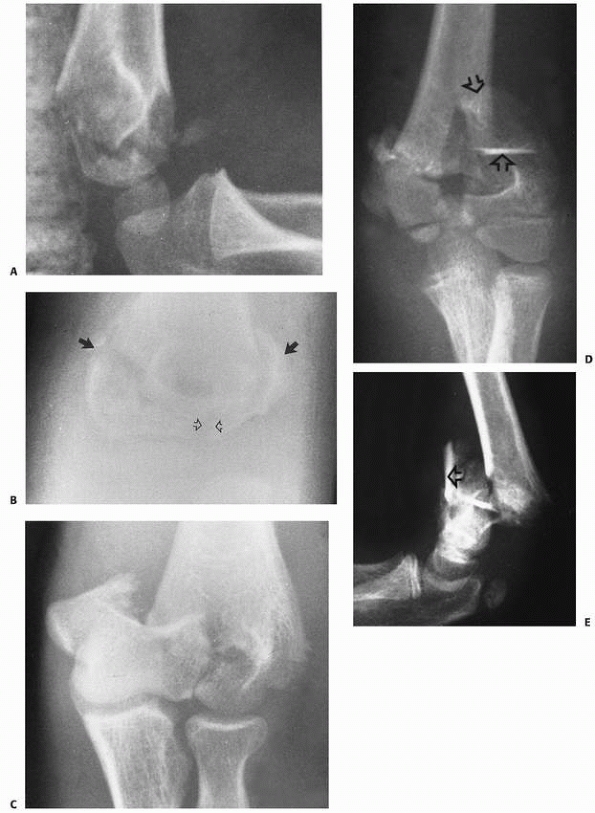 |
|
FIGURE 15-70 Types of T-condylar fractures. A. Type I—Lateral view of undisplaced T-condylar fracture in a 6-year-old. B. The T-condylar fracture line (open arrows) was not appreciated until it healed. There are both medial and lateral Thurstan-Holland fragments (solid arrows). (Courtesy of Ruben D. Pechero, MD.) C. Type II—a displaced T-condylar fracture with very little metaphyseal comminution. D,E. Type III—two views of a markedly comminuted T-condylar fracture with multiple displaced fragments (arrows) in a 12-year-old.
|
with marked disruption of the articular surface, stability and
articular congruity can be established only with an open surgical
procedure. We prefer the Bryan-Morrey posterior triceps-sparing
approach.24 The patient is placed
prone on the operating table with the arm supported on a pillow and the
forearm hanging down off the edge of the operating table. This position
provides the best approach for direct observation of the posterior
surface of the distal humerus. Olecranon osteotomy is reserved for
severely comminuted articular fractures in adolescents.
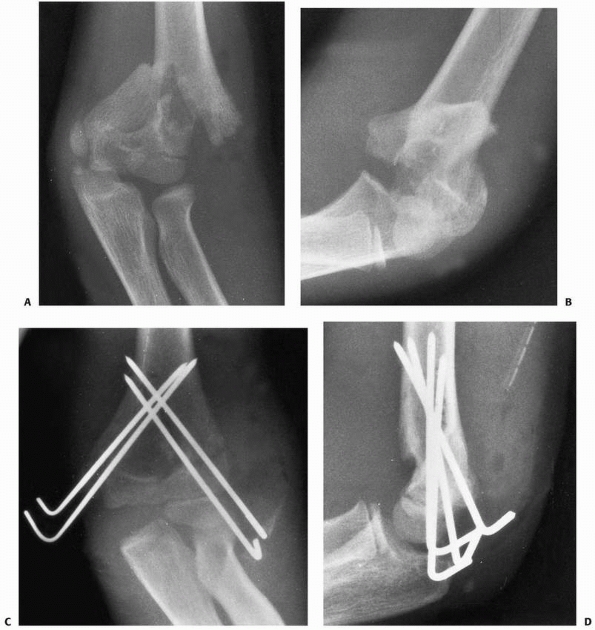 |
|
FIGURE 15-71 Closed reduction and pin fixation. A,B. Two views of a type II T-condylar fracture in a 15-year-old. C,D.
Because an anatomic reduction was achieved by manipulative closed reduction, it was secured with simple multiple pin fixation placed percutaneously. The articular surface was minimally displaced. The pins were removed at 3 weeks. At this age, healing was rapid enough to pull the pins at 3 weeks to allow active motion. Ultimately, the patient was deficient only 10 degrees from achieving full extension. |
the articular fragments—in other words, to convert it to a
supracondylar fracture (Fig. 15-72A-C). The
olecranon and coronoid fossae must be cleared of bony fragments or
debris to eliminate the chance of bony impingement with their
respective processes. The best way to stabilize the condyles is with a
screw passed transversely through the center of the axis of rotation in
such a manner as to apply transverse compression. This stabilization
method may require a small temporary secondary transverse pin proximal
to the screw to prevent rotation of the fragments as the guide hole is
drilled or when the compression screw is being applied. This pin can be
removed after the fragments are secured.
re-established, the distal fragments must be secured to the proximal
fragment by stabilizing the supracondylar fragment columns. The
decision here is how important it is to initiate early motion. In a
younger child with rapid bony healing, pin fixation is often
satisfactory; the pins can be removed after 3 weeks in order to start
protected motion. In an older adolescent nearer to skeletal maturity,
we prefer fixation—
usually plates or screws—that allows early motion (Figs. 15-72E,F and 15-73). Before applying the plates, the supracondylar columns can be stabilized temporarily with pin fixation (Fig. 15-73D).
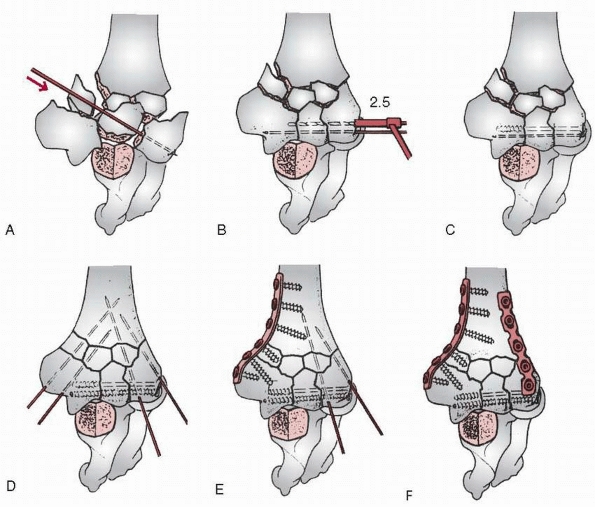 |
|
FIGURE 15-72 Sequence of distal humerus reconstruction. A-C. First, the articular portions are reassembled with provisional K-wire fixation, followed by screw fixation. D. K-wires can then also be used to provide temporary fixation of the distal humerus. E. A one-third tubular plate is attached to the medial side. F.
A 3.5 pelvic reconstruction plate was attached to the posterolateral border. (From Heim U, Pfeiffer KM. Internal Fixation of Small Fractures. 3rd ed. Berlin: Springer-Verlag, 1988, with permission.) |
The reinforced malleable reconstructive type of plates used for
fixation of pelvic fractures provide very secure fixation. A J-type of
plate can also provide rigid fixation when used to stabilize the
lateral column.163 It is best to place the plates at 90 degrees to each other, which provides for a more stable construct.77,96,161
supporting posterior splint for 5 to 7 days to allow the soft tissue
swelling to decrease and the incisions to heal. At this time, active
flexion and extension are initiated and the arm is protected with a
removable cast brace.
to allow adequate fixation. In such cases, we have found that the best
initial treatment method in children involves reestablishing the
articular surface and joint congruity with a limited open reduction.
The separated condyles are secured with a transverse screw providing
compression through the axis of rotation. This procedure can usually be
done with minimal soft tissue dissection. Once this is stabilized, the
supracondylar columns are then re-established by placing the extremity
in olecranon traction and allowing them to reconstitute with callus
formation. Traction must be maintained until there appears to be good
osseous tissue formed in the supracondylar areas. While in traction,
motion can be initiated. This technique can also be used in patients
seen late with contaminated soft tissue abrasions or severe soft tissue
problems. In selected patients, such as an adolescent with severe bone
loss, plating followed by bone grafting may be indicated.
that this is a serious fracture. Because of the considerable soft
tissue injury and the involvement of the articular surface of the
distal humerus, stiffness and loss of motion of the elbow can be
expected regardless of the treatment mode.86,112,136
In adolescents, failure to provide solid internal fixation that
facilitates early motion (i.e., using only pin fixation) can result in
a satisfactory radiographic appearance but considerable dysfunction due
to residual loss of elbow motion.
mentioned in the few cases reported in the literature, the incidence is
probably about equal to that of supracondylar fractures. Because these
fractures occur late in the growth process, partial or total growth
arrest due to internal fixation is not thought to be a major
complication. Likewise, because these are older children, little
remodeling can be expected. Nonunion,93 osteonecrosis of the trochlea,136 and failure of internal fixation have also been reported as complications.
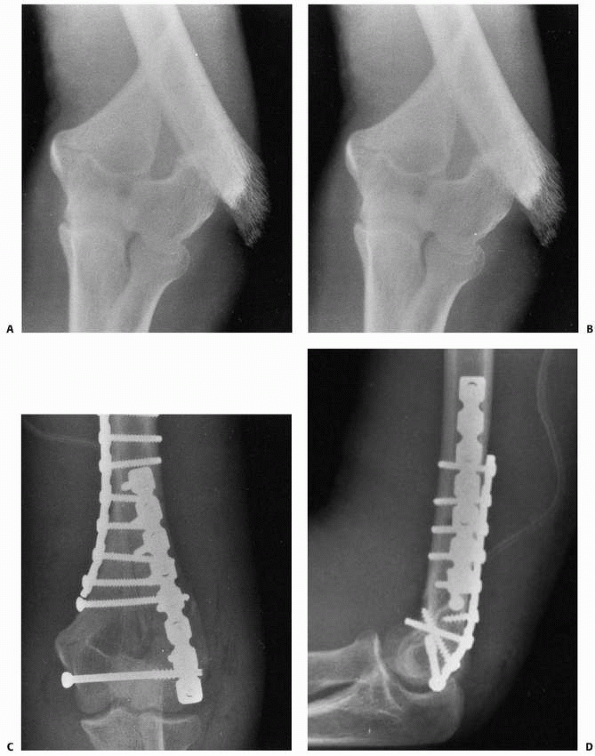 |
|
FIGURE 15-73 T-condylar numeral fractures with plate and screw fixation. A,B. Injury films of a type II flexion pattern in a 16-year-old boy. C,D.
Articular integrity was first restored with a transcondylar compression screw. The condyles were secured to the metaphysis and distal shaft using pelvic reconstruction plates placed at 90 degrees to each other. |
M, Ishizu T, Nagaoka T, et al. Epiphyseal separation of the distal end
of the humeral epiphysis: a follow up note. J Pediatr Orthop
1995;15:426-434.
JE. Injury to the throwing arm. A study of traumatic changes in the
elbow joints of boy baseball players. Calif Med 1965;102:127-132.
HJ, Marcus NW. Articular cartilage sleeve fracture of the lateral
humeral condyle capitellum: a previously undescribed entity. J Pediatr
Orthop 1984;4:620-622.
BA, Silberstein MJ, Rende RJ, et al. Arthrography in the diagnosis of
fractures of the distal end of the humerus in infants. J Bone Joint
Surg Am 1986;68:599-602.
JA, Jokl P, Shaw R, et al. Clinical studies of baseball players:
correlation of injury to throwing arm with method of delivery. Am J
Sports Med 1978;6:15-21.
APC. An Anatomical and Surgical Study of Fractures of the Lower End of
the Humerus. Philadelphia: Lea & Febiger, 1910.
O, Bensahel H, Mazda K, et al. Lateral humeral condylar fractures in
children: a report of 47 cases. J Pediatr Orthop 1988;8:31-34.
WP, Almquist EA, Staheli LT. Fracture separation of the distal humeral
physis in the newborn. J Pediatr Orthop 1984;4:617-619.
SC, Hoffer MM, Aval S. Nonoperative treatment for minimally and
nondisplaced lateral humeral condyle fractures in children. J Pediatr
Orthop 1998;18:448-450.
JH, Wood AB. Fractures of the lateral humeral condyle in children.
Paper presented at the annual meeting of the American Academy of
Orthopedic Surgeons, January 18, 1985; Las Vegas, NV.
JL, Bucholz RW, Wenger DR. Intercondylar fractures of the humerus in
young children. J Bone Joint Surg Am 1982;64A:1083-1087.
H, Csukonyi Z, Badelon O, et al. Fractures of the medial condyle of the
humerus in children. J Pediatr Orthop 1986;6:430-433.
JM, Weiner DS. Neonatal fracture separation of the distal humeral
chondroepiphysis: a case report. Orthopedics 1980;3:875-879.
WF, Heppt P, Glückert K, et al. Aseptic osteonecrosis of the humeral
trochlea (Hegemann’s disease). Arch Orthop Trauma Surg 1990;110:45-48.
RW, Burstein AH, Elmore SM. Epiphyseal-plate cartilage. A biomechanical
and histological analysis of failure modes. J Bone Joint Surg Am
1974;56:688-703.
RS, Morrey BF. Extensive posterior exposure of the elbow. A triceps
sparing approach. Clin Orthop Relat Res 1982;166:188-192.
LP, Golano P, Vega J. Arthroscopic-assisted reduction and percutaneous
external fixation of lateral condyle fractures of the humerus.
Arthroscopy 2007;23:1131-1134.
SL, Hennrikus WL. Surgical treatment of displaced medial epicondyle
fractures in adolescent athletes. Am J Sports Med 1997;25:682-686.
VM, Grottkau BE, Albright M, et al. Multidector computed tomography of
pediatric lateral condylar fractures. Comput Assist Tomogr
2005;29:842-846.
WP, Chandler RW. Persistence of the olecranon physis in baseball
players: results following operative management. J Shoulder Elbow Surg
2003;12:59-62.
JW, Rogers LF, White H, et al. Injuries of the medial epicondyle
ossification center of the humerus. AJR Am J Roentgenol 1977;129:49-55.
DM. Injury to the lower medial epiphysis of the humerus before
development of the ossific centre. Report of a case. J Bone Joint Surg
Br 1967;49:766-767.
FJ. Elbow fractures in children. Fractures of the lower end of the
humerus; lesions and end results, and their bearing upon treatment. Ann
Surg 1902;35:75-104.
JR, Maguire MF, Mubarak SJ, et al. Lateral condylar fracture of the
humerus following posttraumatic cubitus varus. J Pediatr Orthop
1994;14:466-470.
KS, Sengupta S, Singh BJ. Delayed management of fracture of the lateral
humeral condyle in children. Acta Orthop Scand 1988;59:419-424.
JJ, Johnson GV, Hoskinson J, et al. Management of severely displaced
medial epicondyle fractures. J Orthop Trauma 1987;1:59-62.
JJ, Lamont AC, Jones JM. Ultrasonic diagnosis of neonatal separation of
the distal humeral epiphysis. J Bone Joint Surg Br 1988;70:825-828.
PE, Sew-Hoy A, Krom W. Bilateral isolated fractures in an infant as
presentation of osteogenesis imperfecta. Orthopedics 1992;15:741-743.
DM, Wirth CR. Fracture of the distal humeral chondroepiphysis in the
neonate. A case report. Clin Orthop Relat Res 1982;169:155-158.
SJ, Kubiak EN, Polatsch D, et al. Comparison of two headless screw
designs for fixation of capitellum fractures. Bull Hosp Jt Dis
2003;61:123-126.
SJ, Polatsch DB, Egol KA, et al. Capitellum fractures: a biomechanical
evaluation of three fixation methods. J Orthop Trauma 2002;16:503-506.
J, De Smet L, Fabry G. Consequences of a fracture through a minimally
ossified apophysis of the olecranon. J Pediatr Orthop B 2000;9:212-214.
JJ, O’Brien ET. Fracture-separation of the medial humeral condyle in a
child confused with fracture of the medial epicondyle. J Bone Joint
Surg Am 1971;53: 1102-1104.
T, Karlsson G, Lindberg L, et al. Nondisplaced and minimally displaced
fractures of the lateral humeral condyle in children: a prospective
radiographic investigation of fracture stability. J Pediatr Orthop
1995;15:422-425.
JC, Richards JF Jr. Nonunion of minimally displaced fractures of the
lateral condyle of humerus in children. J Bone Joint Surg Am
1971;53:1096-1101.
JC, Richards JF Jr, Saltzman RI. Prevention and treatment of nonunion
of slightly displaced fractures of the lateral humeral condyle in
children. J Bone Joint Surg Am 1975;57:1087-1092.
P, Mackenzie DA, Rosman M. Missed, maluniting, and malunited fractures
of the lateral humeral condyle in children. J Trauma 1978;18:329-335.
JV, Kassab MT, Moula T. Untreated intra-articular entrapment of the
medial humeral epicondyle. J Bone Joint Surg Br 1984;60:562-565.
JV, Slimane N, Kassab MT. Elbow dislocation with avulsion of the medial
humeral epicondyle. J Bone Joint Surg Br 1990;72B:102-104.
RJ, Smith RJ. Radial nerve laceration 26 years after screw fixation of
a humeral fracture. J Bone Joint Surg Am 1984;66:959-960.
IR, Miller JH. Osteochondral fracture of the trochlea associated with
fracture-dislocation of the elbow. Injury 1975;6:257-260.
JF, Roebuck DJ, Cheng JC, et al. Acute elbow trauma in children:
spectrum of injury revealed by MR imaging not apparent on radiographs.
AJR Am J Roentgenol 2001;176:53-60.
DP. Displaced olecranon apophyseal fractures in children with
osteogenesis imperfecta. J Pediatr Orthop 2005;25:154-157.
PE, Barnes DA, Tullos HS. Case report—arthrographic diagnosis of an
injury pattern in the distal humerus of an infant. J Pediatr Orthop
1982;2:569-572.
RS. Injury to the medial humeral condyle in a child reviewed after 18
years. Report of a case. J Bone Joint Surg Br 1985;67:638-639.
S. Osteochondrosis deformans juvenilis capituli humeri including
investigation of intra osseous vasculature in distal humerus. Acta
Orthop Scand Suppl 1959; 38:1-232.
S. The interosseous vasculature of the distal end of the humerus with
special reference to capitulum. Acta Orthop Scand 1957;27:81-93.
JA, Nahigian SH, Froimson AI, et al. Fracture of the lateral condyle of
humerus in children. J Bone Joint Surg Am 1971;53:1083-1095.
RB, Keats TE, Frankel CJ, et al. Radiographic clues to fractures of the
unossified medial humeral condyle in young children. Skeletal Radiol
1984;11:209-212.
MR, Qureshi S, Goldstein R, et al. Arthroscopically-assisted treatment
of pediatric lateral humeral condyle fractures. J Pediatr Orthop
2007;27:739-742.
DL, Hotchkiss RN. Internal fixation of the humerus: a biomechanical
comparison of methods. J Orthop Trauma 1990;4:260-264.
RF, Herndon WA, Evans JP. Operative treatment of medial epicondyle
fractures in children. Clin Orthop Relat Res 1987;221:170-174.
ME, Manoli A II, LaMont RL. Epiphyseal separation of the distal end of
the humerus with medial displacement. J Bone Joint Surg Am
1980;62:52-57.
BD, Herman MJ, Crisci K, et al. Fractures of the lateral humeral
condyle: role of the cartilage hinge in fracture stability. J Pediatr
Orthop 2002;22:8-11.
S, Mehdi B, Larsen MS. The epidemiology of elbow fracture in children:
analysis of 355 fractures, with special reference to supracondylar
humerus fractures. J Orthop Sci 2001;6:312-315.
E, Tudisco C, Farsetti P, et al. Fracture of the humeral condyles in
children: 49 cases evaluated after 18 to 45 years. Acta Orthop Scand
1996;67:173-178.
R, Fowles JV, Rang M, et al. Observations concerning fractures of the
lateral humeral condyles in children. J Bone Joint Surg Br
1975;57(4):430-436.
J, Rosman M. Fracture of the capitulum humeri in children: a rare
injury, often misdiagnosed. Clin Orthop Relat Res 1980;146:157-160.
PO, Danielsson LG. Epicondylar elbow fracture in children: 35-year
followup of 56 unreduced cases. Acta Orthop Scand 1986;57:313-315.
M, Shinohara Y, Kurokawa M, et al. Assessment of stability in
children’s minimally displaced lateral humeral condyle fracture by
magnetic resonance imaging. J Pediatr Orthop 1999;19:570-572.
AD, Yiannakopoulos CK. Closed reduction and percutaneous stabilization
of pediatric T-condylar fractures of the humerus. J Pediatr Orthop
2004;24:13-16.
SS, Reckling FW. Fracture separation of lower humeral epiphysis with
medial displacement. J Bone Joint Surg 1971;53:1105-1108.
JR, Richards K, Millis M. The triceps dividing approach to open
reduction of complex distal humerus fractures in adolescents: a cybex
evaluation of triceps function and motion. J Pediatr Orthop
1990;10:93-96.
HT, Song MB, Conjares JN, et al. Trochlear deformity occurring after
distal humeral fractures: magnetic resonance imagines and its natural
progression. J Pediatr Orthop 2002;22:188-193.
P, Goulet JA, Freiberg A, et al. A biomechanical evaluation of fixation
methods for fractures of the distal humerus. Orthop Trans 1990;14:674.
LA, Danielsson LG. Elbow fractures in children. An epidemiological
analysis of 589 cases. Acta Orthop Scand 1986;57:309-312.
F, Leet AI, Jacopin S, et al. Lateral humeral condyle fractures in
children: a comparison of two approaches to treatment. J Pediatr Orthop
2004;24:385-391.
HH, Shen HC, Chang JH, et al. Operative treatment of displaced medial
epicondyle fractures in children and adolescents. J Shoulder Elbow Surg
2005;14:178-185.
F, Velkes S, Engel J. Avulsion of the medial epicondyle of the humerus
in arm wrestlers: a report of five cases and a review of the
literature. Injury 1991;22:69-70.
YZ, Zheng CB, Zhou TL, et al. Percutaneous probe reduction of frontal
fractures of the humeral capitellum. Clin Orthop Relat Res
1984;183:17-21.
NM, Crawford ST. Elbow effusions in trauma in adults and children: is
there an occult fracture? AJR Am J Roentgenol 2002;178:413-418.
KW, Marshall DL, Busch MT, Williams JP. Osteochondral lesions of the
humeral trochlea in the young athlete. Skeletal Radiol 2009;38:479-491.
K, Kawai H, Kawabata H, et al. Osteosynthesis for old, established
nonunion of the lateral condyle of the humerus. J Bone Joint Surg (Am)
1990;72:32-40.
T, Kashiwaguchi S, Iwase T, et al. Epidemiology of elbow osteochondral
lesions in young baseball players. Presented at the 75th Annual Meeting
of the American Academy of Orthopaedic Surgeons, San Francisco,
California, February, 2008.
GG, Gray AJ, Turner MS. Elbow dislocation with intra articular
entrapment of the lateral epicondyle. J R Coll Surg Edinb
1993;38:112-113.
A, Sugawara J. Humeral trochlear hypoplasia secondary to epiphyseal
injuries as a cause of ulnar nerve palsy. Clin Orthop Relat Res
1988;221:225-230.
CM, Water PM, Brown DJ, et al. Percutaneous pinning in the treatment of
displaced lateral condyle fractures. J Pediatr Orthop 1994;14:462-465.
EC, Karas EH, Weiner LS. Lateral condyle fractures in children:
evaluation of classification and treatment. J Orthop Trauma
1997;11:117-120.
K, Hirohata K, Kashiwagi D. Fracture-separation of distal humeral
epiphysis in young children. J Bone Joint Surg 1979;61:570-573.
N, Hunter JB, Colton CL. The posterolateral approach to the distal
humerus for open reduction and internal fixation of fractures of the
lateral condyle in children. J Bone Joint Surg Br 2000;82:643-645.
B, Fassier F, Poitras B, et al. Results of early surgical treatment of
fractures of the lateral humeral condyle in children. Rev Chir Orthop
Reparatrice Appar Mot 1988; 74:129-131.
Y, Komiyama Y. Hypoplasia of the trochlea and the medial epicondyle of
the humerus associated with ulnar neuropathy—report of two cases. J
Bone Joint Surg Br 1978;60:225-227.
AC, Peterson HA, Shaughnessy WJ. Fishtail deformity following fracture
of the distal humerus in children: historical review, case
presentations, discussion of etiology, and thoughts on treatment. J
Pediatr Orthop B 2000;9:309-318.
M, Peiser J, Lukiec F, et al. Avulsion fracture of the medial
epicondyle caused by arm wrestling. Am J Sports Med 1992;20:347-350.
R, Waters PM. Posttraumatic reconstruction of the elbow in the
pediatric patient. Clin Orthop Relat Res 2000;370:115-126.
VA. Fracture-separation of the medial epicondylar epiphysis of the
elbow joint. Clin Orthop Relat Res 1982;171:172-174.
VA, Beslikas TA. Fractures of the lateral humeral condyle in
children—an analysis of 39 cases. Injury 1985;16:364-366.
VA, Beslikas TA. T-condylar fractures of the distal humeral condyles
during childhood: an analysis of six cases. J Pediatr Orthop
1986;6:302-305.
VA, Nenopoulos S, Venturis T. Fractures of the medial condyle of the
humerus in childhood. J Pediatr Orthop 1987;7:421-423.
S, Wedemeyer M, Mahar AT, et al. Displaced olecranon fractures in
children: a biomechanical analysis of fixation methods. J Pediatr
Orthop 2008;28:147-151.
N, Weiner SD. Osteochondritis dissecans involving the trochlea: report
of two patients (three elbows) and review of the literature. J Pediatr
Orthop 2002;22:48-51.
A, Mut T, Aracil J, et al. Fracture-separation of the lower humeral
epiphysis in young children. Acta Orthop Scand 1981;52:295-298.
P, Sapin C, Henry G, et al. Rate of abnormal osteoarticular
radiographic findings in pediatric patients. Am J Roentgenol
2001;176:987-990.
AL, Balasubramaniam G, Young SK, et al. Type four fractures of the
medial epicondyle: a true indication for surgical intervention. Injury
1998;29:751-756.
A, Tomak Y, Sen C, Tomak L. The management of cubitus varus and valgus
using the Ilizarov method. J Bone Joint Surg Br 2007;89:1615-1619.
FA. Lateral condylar fracture and ipsilateral ulnar shaft fracture:
Monteggia equivalent lesions? J Pediatr Orthop 1985;5:364-366.
LF, Richards K, Waters PM. The Bryan-Morrey triceps-sparing approach to
open reduction of T-condylar humeral fractures in adolescents: cybex
evaluation of triceps function and elbow motion. J Pediatr Orthop
2004;24:615-619.
AC, Wurth TR, Mieling P. Nonunion of olecranon stress fractures in
adolescent baseball pitchers. A case series of 5 athletes. Am J Sports
Med 2006;34:653-656.
EJ, Radin EL. Intercondylar T fracture of the humerus in the adult. A
comparison of operative and nonoperative treatment in 29 cases. J Bone
Joint Surg Am 1969;51A:130-141.
B. Displacement of the medial epicondyle into the elbow joint: the
final result in a case where the fragment has not been removed. Acta
Orthop Scand 1959; 28:212-219.
D, Ferguson C, Younis A, et al. Pediatric elbow dislocations associated
with a Milch type I lateral condyle fracture of the humerus. J Orthop
Trauma 1999;13: 458-460.
K, Nagaoka M, Ryu J. Osteosynthesis for nonunion of the medial humeral
condyle in an adolescent: a case report. J Shoulder Elbow Surg
2007;26:e8-el2.
RA, Raney EM, Pipkin S. Operative treatment of bicondylar
intraarticular fractures of the distal humerus, original research.
Orthopedics 1992;15:159-163.
SK, Tuli SM. Concomitant medial condyle fracture of the humerus in a
childhood posterolateral dislocation of the elbow. J Orthop Trauma
1989;3:352-354.
EH, Tencer AF, Henley MB. Biomechanical evaluation of methods of
internal fixation of the distal humerus. J Orthop Trauma 1994;8:468-475.
GH, Bennett JB, Woods GW, et al. Biomechanics of elbow instability: the
role of the medial collateral ligament. Clin Orthop Relat Res
1980;146:42-52.
JC, Arora A, Mathur NC, et al. Lateral condylar fractures of the
humerus in children: fixation with partially threaded 4.0-mm AO
cancellous screws. J Trauma 1995;39:1129-1133.
K, Masada K, Tada K, et al. Osteosynthesis for the treatment of
nonunion of the lateral humeral condyle in children. J Bone Joint Surg
Am 1997;79:234-240.
DL, Mirzayan R. The posterior fat pad sign in association with occult
fracture of the elbow in children. J Bone Joint Surg Am
1999;81:1429-1433.
SV, Olsen SD, Smaabrekke A. Deformity after fracture of the lateral
humeral condyle in children. J Pediatr Orthop B 2001;10:142-152.
FM. An 84-year follow-up on a patient with ununited fracture of the
lateral condyle of humerus. A case report. J Bone Joint Surg Am
1973;55:378-380.
YC, Fang D, Orth MC, et al. Varus deformity following lateral humeral
condylar fracture in children. J Pediatr Orthop 1985;5:569-572.
JF, Ricchetti ET, Huffman GR. Acute osteochondral shear fracture of the
capitellum in a twelve-year-old patient. A case report. J Bone Joint
Surg Am 2008;90:629-633.
KS, Kang CH, Min BW, et al. Closed reduction and internal fixation of
displaced unstable lateral condylar fracture of the humerus. J Bone
Joint Surg Am 2008;90: 2673-2681.
AA, Maritz NG, O’Driscoll SW, et al. Operative treatment of elbow
contracture in patients 21 years of age or younger. J Bone Joint Surg
Am 2002;84A:382-387.
NS, Zionts LE. Displaced fractures of the apophysis of the olecranon in
children who have osteogenesis imperfecta. J Bone Joint Surg Am
1993;75:1026-1033.
SJ, Thomson JD, Kelly RA. Coronal plane transcondylar fracture of the
humerus in a child. Clin Orthop Relat Res 1993;292:308-311.
S, Yamauchi T, Fukushima M. Hypoplasia of the trochlea of the humerus
as a cause of ulnar nerve palsy. Report of two cases. J Bone Joint Surg
Am 1985;67: 151-154.
AA, Shively RA. Bilateral elbow dislocations with intra articular
displacement of medial epicondyles. J Trauma 1980;20:332-335.
YC, Chen JC, Fu YC, et al. Supracondylar dome osteotomy for cubitus
valgus deformity associated with a lateral condylar nonunion in
children. Surgical technique. J Bone Joint Surg Am 2006;88 Suppl 1 Pt
2:191-201.
RM, Wilkins KE. Avascular necrosis of the trochlea. Paper presented at
the 15th Annual Meeting of European Orthopaedic Society, April 13,
1996; Prague, Czech Republic.
RM, Wilkins KE. Part VI: T-condylar fractures. Fractures and
dislocations of the elbow region. In: Rockwood CAJr, Wilkins KE, Beaty
JH, eds. Fractures in Children. 4th ed. Philadelphia: Lippincott-Raven,
1996.
JS, Moyer RA. Nonunion of a stress fracture through the olecranon
epiphyseal plate observed in an adolescent baseball pitcher. J Bone
Joint Surg Am 1977;59:264-265.
Vugt AB, Severijnen RV, Festern C. Fractures of the lateral humeral
condyle in children: late results. Arch Orthop Trauma Surg
1988;107:206-209.
BP, Srivastava TP. Fractures of the medial condyle of the humerus in
children: a report of four cases including the late sequelae. Injury
1972;4:171-174.
HB. A case of dislocation of the elbow with separation of the internal
epicondyle and displacement of the latter into the joint. Br J Surg
1928;15:667-679.
JM, Gerardi J, Johnson CE. Late open reduction internal fixation of
lateral condyle fractures. J Pediatr Orthop 2002;22:394-398.
R, Mahring M, Hofer HP. Supraintercondylar fractures of the distal
humerus: results of internal fixation. Review of two consecutive
series. J Orthop Trauma 1991;5:301-307.
RD, Johns JC. Nonunion of an olecranon stress fracture in an adolescent
gymnast: a case report. Am J Sports Med 1990;18:432-434.
KE. Fractures and dislocation of the elbow region. In: Rockwood CAJr,
Wilkins KE, King RE, editors: Fractures in Children, 3rd edition.
Philadelphia, JB Lippincott. 1991:509-828.
B, Stuyck J, Hoogmartens M, et al. Fracture-separation of the distal
humeral epiphysis. Acta Orthop Belg 1987;53:109-111.
NIL, Ingran R, Rymaszewski L, et al. Treatment of fractures of the
medial epicondyle of the humerus. Injury 1988;19:342-344.
WE, Shih CH, Lee ZL, et al. Anatomic reduction of old displaced lateral
condylar fractures of the humerus in children via a posterior approach
with olecranon osteotomy. J Trauma 2008;64:1281-1289.
CI, Suh JT, Suh KT, et al. Avascular necrosis after fracture-separation
of the distal end of the humerus in children. Orthopedics
1992;15:959-963.
H. Fractures of the elbow. In: Weber BG, Brunner C, Freuler F, eds.
Treatment of fractures in children and adolescents. New York:
Springer-Verlag, 1980.
LE, Moon CN. Olecranon apophysis fractures in children with
osteogenesis imperfecta revisited. J Pediatr Orthop 2002;22:745-750.
