Sciatica
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Sciatica
Sciatica
Philip R. Neubauer MD
Damien Doute MD
Description
-
Sciatica is pain referred down the leg in a distribution of the sciatic nerve, which courses from the lumbosacral plexus L2–S3.
-
5 different areas of pain may be noted:
-
Back: Midline lumbosacral, radicular radiation pattern
-
Buttocks: Deep-seated, “crampy” pain
-
Posterior or lateral thigh (L5, S1)
-
On occasion, both posterior and lateral thigh
-
Anterior thigh (high lumbar root L2, L3, L4)
-
Epidemiology
Incidence
2% of the general population, with lifetime incidence near 40% (1)
Etiology
Most sciatica is from the intervertebral disc (most commonly, L4–L5) and mechanical compression of the lumbosacral nerve roots.
Signs and Symptoms
-
Back:
-
Most patients have previous back pain, and 50% of those have a history of trauma (1).
-
Pain lateralizes to the hip or leg, gradually or suddenly.
-
A precipitating event may occur, such as bending over or straining.
-
-
Leg:
-
Pain can be more debilitating than back pain.
-
L5–S1 root compression: Cramp or a viselike feeling in the gastrocnemius or peroneal muscle belly
-
L4: Medial shin or lateral thigh
-
L5: Lateral calf
-
S1: Back of calf
-
L1: Groin
-
L2: Medial thigh
-
L3: Anterior thigh
-
Most adults have pain below the knee.
-
-
Foot:
-
The most common symptom is paresthesia.
-
L5: Foot dorsum
-
S1: Lateral foot
-
Actual foot pain is unusual.
-
-
Rarely, motor symptoms predominate; if they do, consider spinal tumor or peripheral neuropathy.
-
Aggravating or relieving factors:
-
Bending, stooping, lifting, coughing, sneezing, straining, and sitting worsen pain.
-
Standing, walking, and resting are more tolerable.
-
Lying with the knee or hip flexed and sleeping with a pillow under the knees give some relief.
-
Physical Exam
-
Spine:
-
Variable examination: Most physical findings are in the legs, not the back.
-
Lumbar spine flattened and flexed
-
Limited spine extension, forward flexion, and lateral flexion toward affected side
-
“Sciatic scoliosis”: Patient leans away from side of pain
-
-
Extremities:
-
Test all muscle groups and make a chart to document baseline:
-
Flexion/extension/adduction/abduction for the hip
-
Flexion/extension of the knee
-
Dorsiflexion/plantarflexion/eversion/inversion/ flexion of the ankle
-
Flexion/extension of the 1st toe
-
-
Test sensation with pinprick in all dermatomes and compare with those in the contralateral limb.
-
Test reflexes
-
Trendelenburg sign: A lurch or pelvic
tilt is noted with ambulation, as is weakness of the hip adductors
(gluteus medius and minimus). -
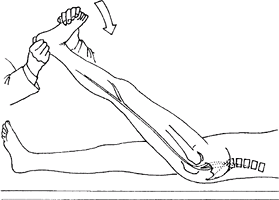
Root tension sign: A limited straight-leg
raise (with a small amount of hip internal rotation and adduction,
slowly raise leg) reproduces leg pain at <60° of flexion (Fig. 1). -
Contralateral straight-leg raise: When
the unaffected leg is lifted, the opposite symptomatic side has a
painful axilla or midline disc. -
Lasègue sign: Pain is increased on forced
dorsiflexion of the ankle with straight-leg raising and is relieved
with hip or knee flexion (Fig. 2). -
Bowstring sign:
-
Perform straight-leg raise to the point of sciatica.
-
Allow the knee to flex.
-
Apply pressure to the hamstring insertion at the knee, which stretches the nerve to reproduce leg pain.
-
-
Femoral nerve stretch test: Unilateral thigh pain is produced by knee flexion, tension on the 2nd to the 4th roots.
-
-
The diagnosis also is suggested by motor weakness or by sensory or reflex changes.
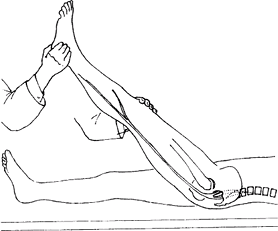 Fig. 1. The straight-leg-raise test is used to detect nerve root stretch. The knee is kept straight while the hip is flexed.
Fig. 1. The straight-leg-raise test is used to detect nerve root stretch. The knee is kept straight while the hip is flexed. -
Muscle wasting:
-
Rare unless the lesion is present for >3 weeks
-
Marked wasting suggests a tumor.
-
Tests
Lab
In patients >50 years old, one should exclude the
diagnosis of multiple myeloma with a complete blood count, ESR, and
serum protein electrophoresis.
diagnosis of multiple myeloma with a complete blood count, ESR, and
serum protein electrophoresis.
Imaging
-
Conventional radiography:
-
AP view of the lumbosacral spine
-
AP view of the pelvis
-
-
Screening radiography:
-
Compression fractures (lateral view)
-
Spondylolisthesis (lateral view)
-
Pedicle destruction in metastatic bone disease (AP view)
-
Scoliosis (AP view)
-
Tumors of the pelvis (AP view of the pelvis)
-
-
MRI is procedure of choice for detecting and defining anatomy of:
-
Herniated discs
-
Compression from vertebral body fractures
-
Marrow involvement from neoplastic processes, spinal cord tumors
-
-
CT is effective and used primarily for patients:
-
Who cannot undergo MRI
-
With previous surgery who have metal implants
-
Pathological Findings
Nuclear pulposus extruded through a weakened annular fibrosis
Differential Diagnosis
-
Diabetic neuropathy
-
Disc space infection or epidural abscess
-
Spondylogenic: Disc rupture, spinal stenosis, muscle sprain
-
Psychogenic: Vague and stocking–glove type pain
-
Neurogenic: Spinal cord tumor or cysts
![]() Fig. 2. The Lasègue maneuver confirms nerve tension, with increased pain as the ankle is dorsiflexed.
Fig. 2. The Lasègue maneuver confirms nerve tension, with increased pain as the ankle is dorsiflexed.
P.371
General Measures
-
A systematic approach is necessary to identify the correct diagnosis and minimize disability.
-
Noninvasive treatment:
-
Highly successful
-
Patient education:
-
Limit bending, heavy lifting
-
Teach and encourage back strengthening and cardiovascular fitness.
-
-
Limited bed rest (1–3 days), then gradual increase in activity
-
-
Invasive treatment:
-
Epidural steroids may provide relief of variable duration.
-
Special Therapy
Physical Therapy
Physical therapy can be useful for back exercises, healthy-back educational programs, and aerobic conditioning.
Medication
First Line
-
Muscle relaxants
-
NSAIDs
-
Avoid narcotics.
Surgery
-
If nonoperative treatment fails after 6 weeks
-
If neurologic deficit, cauda equina
-
Microdiscectomy
-
Current standard is laminotomy and discectomy.
-
Minimally invasive microdiscectomy is performed with greater frequency through various tubular and expandable retractor systems.
-
The procedure may result in less tissue damage than current procedures.
-
Prospective studies comparing this technique to conventional microdiscectomy are underway.
-
Prognosis
Good; most patients recover spontaneously with some reports of a >70% rate of recovery with nonoperative treatment (2,3).
Complications
-
Cauda equina syndrome: Large central disc herniation causing bowel/bladder symptoms and findings
-
Persistent pain
-
Progressive spondylosis (disc degeneration)
Patient Monitoring
The patient should be seen at 2–4-week intervals to document strength and recovery.
References
1. Frymoyer JW. Back pain and sciatica. N Engl J Med 1988;318:291–300.
2. Awad JN, Moskovich R. Lumbar disc herniations: surgical versus nonsurgical treatment. Clin Orthop Relat Res 2006;443:183–197.
3. Weber H. The natural history of disc herniation and the influence of intervention. Spine 1994;19: 2234–2238.
Additional Reading
McCulloch J, Transfeldt E. Disc degeneration with root irritation: disc ruptures. In: MacNab’s Backache, 3rd ed. Baltimore: Williams & Wilkins, 1997:500–568.
Codes
ICD9-CM
722.10 Displacement of herniated disc
Patient Teaching
Patients are instructed on care of the back, to minimize disability.
FAQ
Q: What are the symptoms of sciatica?
A:
Sciatica is a symptom itself. The patient may experience burning, pain,
or a tingling sensation in the back and legs as a result of pressure on
the sciatic nerve.
Sciatica is a symptom itself. The patient may experience burning, pain,
or a tingling sensation in the back and legs as a result of pressure on
the sciatic nerve.
Q: What are the main causes of sciatica?
A: The most common cause of sciatica is a herniated intervertebral disc.
Q: What are the treatment options for patients with sciatica?
A:
Physical therapy, exercise, and anti- inflammatory medications should
be tried 1st, followed by spinal injections and surgery.
Physical therapy, exercise, and anti- inflammatory medications should
be tried 1st, followed by spinal injections and surgery.