Sciatic Nerve Blocks
II – Single-Injection Peripheral Blocks > B – Lower Extremity >
12 – Sciatic Nerve Blocks
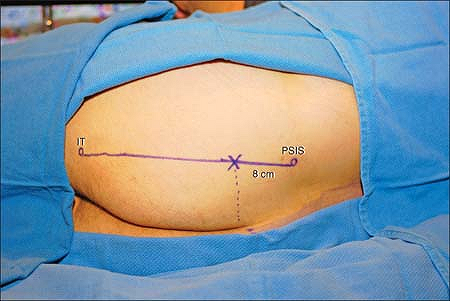
The ischial tuberosity and the posterior superior iliac spine (PSIS)
are major surface landmarks for this block. The sciatic nerve is
comprised of L4 through S3 ventral rami and exits the pelvis through
the inferior portion of the greater sciatic foramen, deep (anterior) to
the piriformis muscle. It lies deep to the gluteus maximus muscle and
medial to both the gluteus medius and gluteus minimus. It is the most
lateral of all structures passing inferior to the piriformis muscle.
Medial to it lies the internal pudendal and inferior gluteal vessels
and nerves. Occasionally the sciatic nerve divides prior to entering
the gluteal region, with the common fibular nerve passing superior to,
or through the piriformis muscle.
The needle insertion lies along this line, slightly caudal to the
superior aspect of the gluteal cleft, or approximately 6–8 cm caudal to
the PSIS. The needle is connected to a nerve stimulator (2 Hz, 1.5 mA,
0.1 ms) and advanced in a parasagittal plane. If the sacrum is
contacted, the needle is withdrawn and redirected slightly laterally,
walking off the border of the sacrum into the greater sciatic foramen.
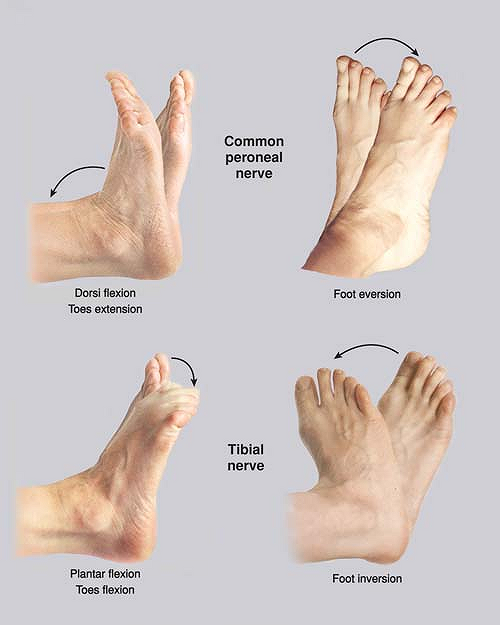
The endpoint of needle advancement is a sustained sciatic stimulation
eliciting foot plantar flexion/inversion (tibial nerve) or
dorsiflexion/eversion (common fibular nerve) motor
response with a current less than 0.5 mA (Fig. 12-2). Following negative aspiration for blood, local anesthetic is slowly injected in 5-mL increments, with intermittent aspiration.
 |
|
Figure 12-1. The PSIS and the inferior aspect of the ischial tuberosity are palpated and marked, and a line drawn between the two points.
|
-
The posterior femoral cutaneous nerve
accompanies the sciatic nerve medially along with the inferior gluteal
artery, and is reliably blocked using this approach. -
This block is commonly performed in
combination with a lumbar plexus block for hip procedures. The depth at
which the sciatic nerve is often located is often the same as the one
of the femoral nerve. Consequently, we first perform the lumbar plexus
block. -
The sciatic nerve usually innervates no
muscles in the gluteal region. Direct gluteal stimulation on
advancement of the needle indicates that the sciatic nerve is still
deep to the needle tip. -
Pelvic splanchnic and distal sympathetic
block are possible given their close proximity to the block site
leading to possible urinary retention. -
In morbidly obese patients it is sometime
necessary to use a 15-cm needle. However, we recommend to first start
with a 10-cm needle, unless there is clear evidence that a 15-cm is
required. -
Close pudendal nerve proximity may lead
to genital tingling during needle positioning, and anesthesia following
the block. If genital tingling is elicited during needle placement, the
needle should be repositioned more laterally and superficially. -
This approach is useful for hip
procedures as it allows for the concurrent block of additional sacral
branches involved in hip joint innervation. Two of these nerves that
exit through the greater sciatic foramen are the superior gluteal nerve
(L4-S1, coursing superior to the piriformis muscle) and the nerve to
the quadratus femoris muscle (L4-S1, coursing anterior to the sciatic
nerve). -
Weakness in leg adduction with this block
is due to block of the sciatic branch to the hamstring portion of the
adductor magnus rather than obturator block. -
Limit advance of the needle to 2 cm beyond the border of the sacrum to minimize the chance of pelvic organ damage.
 |
|
Figure 12-2.
The endpoint of needle advancement is a sustained sciatic stimulation eliciting foot plantar flexion/inversion (tibial nerve) or dorsiflexion/eversion (common fibular nerve) motor response with a current less than 0.5 mA. |
NY, Bennetts FE. An observational study of combined continuous lumbar
plexus and single shot sciatic nerve blocks for post–knee surgery
analgesia. Reg Anesth 1996;21:287–291.
Anesthesia and immediate postoperative analgesia for surgery at and
below the knee or requiring the use of a thigh tourniquet for more than
30 minutes.
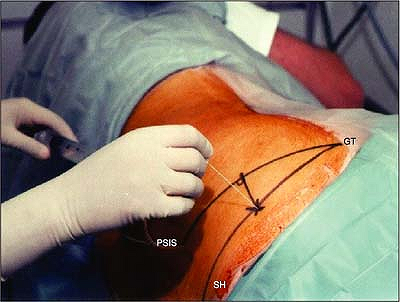
The center of the greater trochanter and the posterior iliac spine are
identified and marked, and a line is drawn between these two points.
Next, the sacral hiatus is identified and marked. Another line is drawn
from the greater trochanter to the sacral hiatus. A perpendicular line
is drawn to the midpoint of the greater trochanter–posterior iliac
spine line. The intersection between this line and the greater
trochanter–sacral hiatus line represents the point of insertion of the
needle. The insulated needle connected to a nerve stimulator (1.5 mA, 2
Hz, 0.1 ms) is introduced perpendicular to the skin (Fig. 12-3). The stimulation of the sciatic nerve produces a flexion of the
foot and toes or an inversion of the foot (tibial nerve) or a
dorsiflexion of the foot and extension of the toes or an eversion of
the foot (common peroneal nerve). The needle is positioned to maintain
the same motor response with a current of less than 0.5 mA. After
negative aspiration for blood, the local anesthetic is injected slowly,
with repeated aspiration for blood every 5 mL.
 |
|
Figure 12-3. The insulated needle connected to a nerve stimulator is introduced perpendicular to the skin.
|
-
A pillow may be placed between the legs at the level of the knee.
-
Appropriate positioning is critical to establish the proper site for the introduction of the needle.
-
Already at this level, the sciatic nerve
is separated into the common peroneal and the tibial nerves, and the
posterior femoral cutaneous nerve of the thigh has branched. -
The stimulation of the sciatic nerve is almost always preceded by the stimulation of the gluteus maximus.
-
A bone contact usually indicates that the needle is too lateral.
-
Stimulation of the piriformis muscle indicates that the needle is too cephalad.
-
A motor response at the level of the toes increases the likelihood of success.
-
When patients complain of pelvic
discomfort, it suggests that the needle is too anterior and is going
through the greater sciatic notch. -
Because the sciatic nerve is found at a
depth of 8 to 13 cm, no redirection of the needle should be attempted
after it passes the skin to avoid bending the needle. -
This approach can be uncomfortable for
the patient and therefore requires appropriate local anesthesia with a
38-mm needle and an appropriate sedation. -
This approach is not recommended in anticoagulated patients.
-
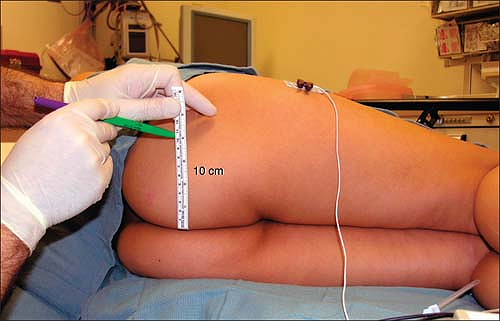
A new posterior approach has been
described in adults: The patient is positioned either prone or in the
lateral position. The site of introduction of the needle is 10 cm
lateral from the midpoint of the intergluteal sulcus.
The patient is placed in the lateral decubitus position with the side
to be blocked up. Both lower extremities are flexed slightly at the
hips and knees with the buttocks forming a 90° angle with the bed.
Anesthesia and postoperative analgesia for any surgical procedure in
the lower extremity involving the posterior thigh and any area distal
to the knee excluding the medial side of the leg, which is innervated
by the saphenous nerve, a branch of the femoral nerve.
This simple approach is based on the fact that the sciatic nerve runs
parallel to and about 10 cm from the midline (intergluteal sulcus) in
all adults regardless of gender and body habitus. Thus, the block can
be performed at 10 cm from the midline at about any point in the
gluteal area including the subgluteal fold. In the gluteal area it is
usually performed lateral to the midpoint of the intergluteal sulcus
only because this point is easy to visualize and teach. The 10-cm
measurement must be linear as shown in Figure 12-4, disregarding any individual contour on the patient’s buttocks.
This linear distance reflects the distance between the midline and the
area immediately lateral to the ischial tuberosity where the nerve runs.
 |
|
Figure 12-4.
With the patient in true lateral position the needle insertion point is easily found by measuring 10 linear cm from the midline (intergluteal sulcus). No other landmarks are identified. |
 |
|
Figure 12-5. The needle is advanced parallel to the patient’s midline at 10 cm from it without the need to find any additional landmarks.
|
insulated needle connected to a nerve stimulator (around 1.5 mA, 1 Hz,
0.1 ms) is then slowly advanced parallel to the midline (parallel to
the bed) as shown in Figure 12-5.
Usually a motor twitch of the gluteus maximus can be easily seen as the
needle passes through this muscle and continues to be visible until the
needle reaches the deep surface of the gluteus maximus. The needle then
needs to traverse the small amount of connective tissue deep to this
muscle before reaching the sciatic nerve. The tip of the needle is then
carefully manipulated until a response is still visible at 0.5 mA. The
injection of local anesthetic is given slowly with frequent aspirations.
the reposition is easy since the nerve could only be either lateral or
medial to the needle. The needle is withdrawn completely and a very
small (10°) correction is made to the angle of insertion, first lateral
and then if necessary medial.
-
Positioning of the patient is important,
as with any regional anesthesia technique. The patient is placed in
true lateral position (not Sim’s). Both hips and knees remain slightly
flexed and the buttocks are at a right angle with the bed. This
position aligns the midline of the patient with the horizontal plane of
the bed making it easier to judge the angle of insertion of the needle. -
The prone position can be used but it is usually unnecessary and more time consuming.
-
The sciatic nerve enters the upper
gluteal area describing a downward curve from medial to lateral before
running down parallel to the midline. Thus, it is recommended to
attempt the block in the lower three-fourths of the buttocks because in
the upper fourth the nerve is located less than 10 cm from the midline. -
The differences between male and female
pelvises lie in the shape and diameters of the inner pelvis and not in
the total width (bicrestal diameter), which is virtually the same in
both sexes. The female inner pelvis is wider while the male bones are
thicker. In fact, different hormone-dependent patterns of fat
deposition in both sexes explain the perceived differences in pelvis
width. -
Deposition of fat in the buttocks does
not affect the position of the sciatic nerve with respect to the
midline but it does affect its depth and its relative position with
respect to the lateral side of the body. In other words, the nerve’s
relative position in the buttocks changes, but not its absolute
position with respect to the midline, which remains fixed at 10 cm. -
The gluteus maximus muscle is the only
muscle that covers the sciatic nerve superficially in most of the
gluteal region. In the uppermost area of the buttocks the small
piriformis muscle is also superficial to the nerve. -
In our experience any response that can
be elicited from stimulation of the sciatic nerve (e.g., dorsal or
plantar flexion, eversion and inversion) provides a similar success
rate provided the response is obtained at low output. -
When reposition of the needle is
necessary it is important to realize that small changes in the angle of
insertion of the needle have a profound impact in the position of the
tip of the needle when dealing with deep structures like the sciatic
nerve. A modest 10° correction angle for example has been calculated to
move the tip of the needle approximately 1.6 cm at a depth of 9 cm.
Anesthesia and immediate postoperative analgesia for major surgery at
and below the knee, including the foot and ankle, especially when
tourniquet use is anticipated.
At this level the sciatic nerve is covered by the gluteus maximus
muscle only. A groove may be palpated between the lateral border of
quadriceps femoris (vastus lateralis) and biceps femoris (Fig. 12-7).
At the level of the thigh, the sciatic nerve runs toward the popliteal
fossa (sciatic line), lying on the posterior surface of the adductor
magnus, within the posterior medial compartment of the thigh. The
septum intermusculare femoralis mediale and a reinforcement of the
posterior fascia of the adductor magnus muscle limit this compartment.
 |
|
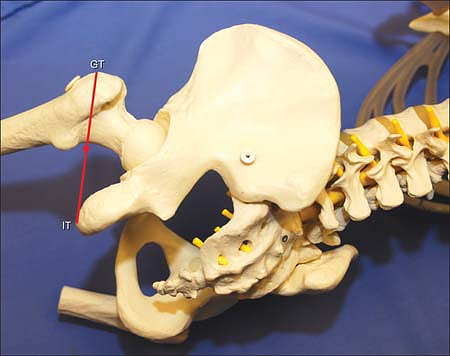
Figure 12-6. Anatomic landmarks. GT, greater trochanter; IT, ischial tuberosity.
|
 |
|
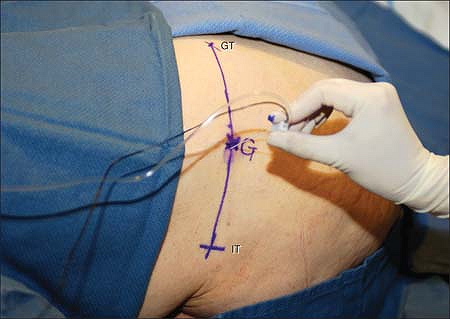
Figure 12-7. Anatomic landmarks. GT, greater trochanter; IT, ischial tuberosity; G, gluteal approach; SG, subgluteal approach.
|
The greater trochanter (GT) and the ischial tuberosity (IT) are
identified and marked, and a line is drawn between these two points.
Midpoint of this line is the site of the introduction of the needle
(G). At this level, a skin depression can be palpated, representing the
groove between the biceps femoris and vastus lateralis (Fig. 12-7).
After proper local skin infiltration, the insulated needle connected to
a nerve stimulator (1.5 mA, 2 Hz, 0.1 ms) is introduced perpendicular
to the skin. The needle is advanced until the sciatic nerve is
stimulated—inversion/plantar flexion of the foot and toes (tibial
nerve) or eversion/dorsiflexion of the foot and extension of the toes
(common peroneal nerve). The needle is adjusted to maintain the same
motor response with a current at or below 0.5 mA. After a negative
aspiration for blood, planned volume of local anesthetic solution is
slowly injected, with repeat aspiration every 5 ml (Fig. 12-8).
 |
|
Figure 12-8.
After a negative aspiration for blood, planned volume of local anesthetic solution is slowly injected, with repeat aspiration every 5 ml. |
-
The gluteal approach as compared with
other sciatic approaches (classic, high lateral) reduces the risk of
misplacements or dislocation of the catheter after surgery and reduces
the risk of vascular puncture. -
This block is usually performed in combination with a single or continuous lumbar plexus or femoral block.
-
A variant of the gluteal approach is the
subgluteal approach (SG). A line is drawn perpendicularly and extending
caudally for 4 cm in the middle of the ischial tuberosity–greater
trochanter line. The end of this line represents the site of
introduction of the needle (SG) (Fig. 12-7). -
Gluteal or subgluteal approach is preferred in obese patients, because at this level the sciatic nerve is the most superficial.
-
Compared with the classic posterior
approach of Labat, this approach, as well as subgluteal, is less
painful because the needle is introduced in the groove between the
biceps femoris and lateral border of quadriceps femoris muscles. -
If the femur is contacted, the needle needs to be withdrawn and redirected medially (toward sacrum).
-
If direct stimulation of gluteus maximus
muscle is noticed (too shallow), needle should be advanced a few
millimeters until distal response with foot movement is recorded. -
Hamstring contraction represents either a
direct muscle contraction or the stimulation of tibial nerve, except
the short head of biceps femoris, which is innervated by common
peroneal nerve (and not considered part of the hamstring muscles). This
response is not reliable for the block below the knee. The needle
should be readjusted to elicit a distal (toes) response. -
If patient reports painful paresthesia
along the leg, the needle should be withdrawn and redirected to achieve
painless stimulation with movement of the toes with a current of or
below 0.5 mA.
Benedetto P, Bertini L, Casati A, et al. A new posterior approach to
the sciatic nerve block: a prospective, randomized comparison with the
classical posterior approach. Anesth Analg 2001;93:1040–1044.
Benedetto P, Casati A, Bertini L. Continuous subgluteus sciatic nerve
block after orthopedic foot and ankle surgery: comparison of two
infusion techniques. Reg Anesth Pain Med 2002;27:168–172.
Benedetto P, Casati A, Bertini L, et al. Postoperative analgesia with
continuous sciatic nerve block after foot surgery: a prospective,
randomized comparison between the popliteal and subgluteal approaches. Anesth Analg 2002;94:996–1000.
Anesthesia and immediate postoperative analgesia for surgery of the
knee and below. Analgesia prior to surgery following a leg trauma.
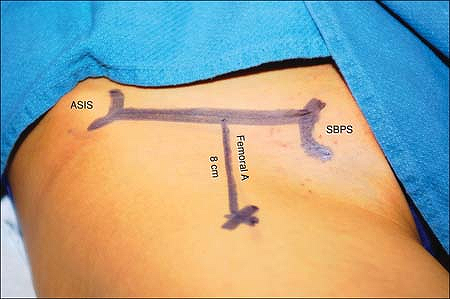
A line is drawn between the anterior iliac spine and the superior angle
of the pubic tubercle. At its midpoint, a perpendicular line is drawn.
The site of introduction of the needle is 8 cm distally (Fig. 12-9). The 150-mm insulated needle connected to a nerve stimulator (1.5 mA, 2 Hz, 0.1 ms) is introduced vertically (Fig. 12-10).
Within 3 to 5 cm, movements of the patella are elicited, indicating the
proximity of the femoral nerve. The current is then reduced to 0.5 mA
and the motor response disappears. The current is increased 2 cm deeper
to 5 mA. If the femur is contacted, the needle is removed and
introduced 1.5 to 2.0 cm medially, and all steps are repeated.
Stimulation of the sciatic nerve is usually obtained at a depth of 10
to 12 cm and produces a dorsiflexion of the foot and extension of toes,
or an eversion of the foot (common peroneal nerve stimulation) or a
flexion of the foot and toes, or an inversion of the foot (tibial nerve
stimulation) (see Fig. 12-2). The needle is positioned to maintain the same motor
response with a current of less than 0.6 mA. After negative aspiration
for blood, the local anesthetic solution is slowly injected with
repeated aspiration every 5 mL.
 |
|
Figure 12-9.
At its midpoint, a perpendicular line is drawn. The site of introduction of the needle is 8 cm distally. Anterior superior iliac spine (ASIS). Superior border of pubis tubercle (SBPS). |
 |
|
Figure 12-10. The insulated needle connected to a nerve stimulator is introduced vertically.
|
-
In this approach, the nerve stimulator
has a dual function. First, it helps prevent damage to the femoral
nerve during the first 3 to 5 cm of needle introduction, and second, it
helps to localize the sciatic nerve. If, during the introduction of the
needle, it is found that the needle is directly on the femoral nerve
(presence of movement of the patella with a current of 0.5 mA), the
needle is directed slightly medially before continuing with any further
advancement (Fig. 12-11). -
Except for morbidly obese patients
(>100 kg), it is rarely necessary to introduce the 150-mm needle. In
most cases, the nerve is found at an approximate depth of 10 to 12 cm. -
Introduction of an insulated needle
through the quadriceps is easy. However, if at a depth of 10 to 12 cm,
the introduction of the needle becomes more difficult, this is a sign
that the needle is very close to the femur. In such cases, it should be
withdrawn to the skin and redirected slightly more medially. -
The onset time for a sciatic nerve block
is usually longer than other blocks. It usually requires 20 to 30
minutes or even longer. -
Using the anterior sciatic approach also
allows one to block the femoral nerve through the same skin
introduction point. However, to avoid any risk of injury of the femoral
nerve by the insulated needle on its way to the sciatic nerve, it is
recommended to first block the sciatic nerve and then proceed to block
the femoral nerve while retrieving the needle. This technique offers
the advantage of only one stick. However, with such a distal approach
to the femoral nerve, it is not possible to also block the femoral
cutaneous nerve or the obturator (three-in-one block). -
Beck first described an anterior
approach. The Chelly and Delaunay approach and the Beck approach use
different anatomic landmarks, but both lead to the same site (Fig. 12-12) and both approach the sciatic nerve above the lesser trochanter.P.125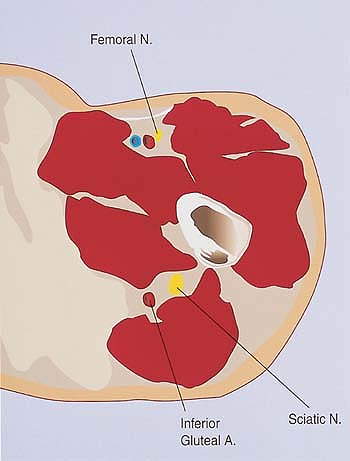 Figure 12-11. Femoral nerve.
Figure 12-11. Femoral nerve. -
Van Elstraete et al. described new
landmarks (2.5 cm medial from the femoral artery and 2.5 cm distal from
the inguinal crease). In this case the 150-mm insulated needle
connected to a nerve stimulator is introduced at a 10° to 15° angle
relative to the vertical plane. This latter approach offers the
advantage of being based only on a landmark
P.126
found below the femoral crease. Van Elstraete appears to approach the sciatic nerve below the lesser trochanter.![]() Figure 12-12. Anatomic landmarks.
Figure 12-12. Anatomic landmarks. Figure 12-13. The needle is introduced perpendicular to the skin, and stimulation of the sciatic nerve is produced between 4 to 12 cm.
Figure 12-13. The needle is introduced perpendicular to the skin, and stimulation of the sciatic nerve is produced between 4 to 12 cm. -
Anterior approach to the sciatic nerve is
especially interesting in morbidly obese and trauma patients who cannot
be moved. However, in patients weighing over 100 kg, the 150-mm needle
may be too short. In these cases, it is possible to approach the
sciatic nerve using the lithotomy approach described by Raj, with the
patient supine and the hip and the knee flexed. This gluteal approach
is based on the identification of the ischial tuberosity and greater
trochanter. The middle of the ischial tuberosity–greater trochanter
line represents the site of introduction of the needle. The needle is
introduced perpendicular to the skin, and stimulation of the sciatic
nerve is produced within 4 to 12 cm (depending on the size of the
thigh) (Fig. 12-13).
Elstraete AC, Poey C, Lebrun T, et al. New landmarks for the anterior
approach to the sciatic nerve block: imaging and clinical study. Anesth Analg 2002;95:214–218.
Anesthesia and immediate postoperative analgesia for surgery at and
below the knee. This block is usually combined with the femoral or
saphenous nerve block to obtain complete anesthesia.
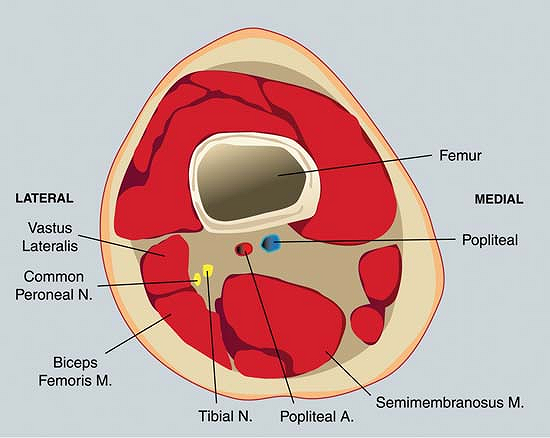
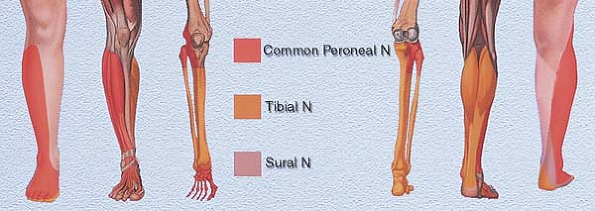
The popliteal crease, the lateral border of the biceps femoris, and the
medial border of the semi-membranous/semi-tendinous tendons (Fig. 12-14). The innervation of the sciatic nerve below the knee is presented in Figure 12-15.
The lateral border of the biceps femoris and the medial border of the
semi-membranous/semi-tendinous tendons are identified and marked at the
level of the popliteal crease. At the level of the popliteal crease, a
perpendicular line is drawn in the middle and extended cephalad. The
site of introduction of the needle is 1 cm lateral to the 5 cm mark (Fig. 12-16).
The 25-mm, b-beveled insulated needle connected to a nerve stimulator
(1.5 mA, 2 Hz, 0.1 ms) is introduced perpendicular to the skin and
slowly advanced until a branch of the sciatic nerve (either the common
peroneal nerve [dorsiflexion of the foot and extension of toes or
eversion] or the tibial nerve [flexion of the foot and toes or
inversion] [see Fig. 12-2])
is stimulated (at a depth of 1.5 to 2.5 cm). The position of the needle
is adjusted to maintain the same motor response with a current less
than 0.5 mA. After negative aspiration for blood, the local anesthetic
solution is injected 5 mL at a time with multiple aspirations for blood
in between.
 |
|
Figure 12-14. Anatomic landmarks.
|
 |
|
Figure 12-15. The innervation of the sciatic nerve below the knee.
|
-
This is one of the easier blocks to perform.
-
This block can also be performed with a 50-mm needle with the patient placed in the lateral position.
-
The anatomic landmarks can be easily identified by asking the patient to perform an active flexion of the leg.P.129
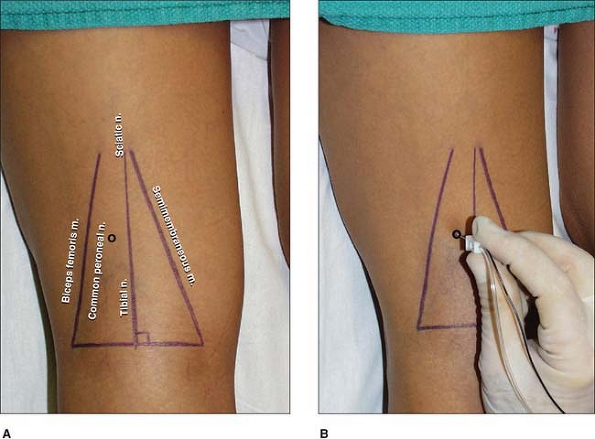 Figure 12-16.
Figure 12-16.
The site of the introduction of the needle is 1 cm lateral to the 5 cm
mark. The insulated needle connected to a nerve stimulator is
introduced perpendicular to the skin and slowly advanced until a branch
of the sciatic nerve or the tibial nerve is stimulated. -
The best positioning of the leg and foot
can be achieved by either positioning the patient with the foot outside
of the stretcher or placing a pillow under the leg. -
Minimal discomfort should be experienced
by the patient because only interstitial fat lies between the skin and
the nerve. If the patient complains of pain, this suggests that the
needle is going through the semi-tendinous/semi-membranous tendons
rather than being medial to them. -
It is possible to perform the same block using the lithotomy approach.
-
For surgery performed at the level of the
knee, especially with the use of a tourniquet placed at the thigh, a
femoral or a lumbar plexus block is required to complete the
anesthesia. For surgery below the knee, especially when a tourniquet is
placed at the level of the calf or below, a saphenous nerve block is
sufficient. -
There are at least three techniques that
can be used to perform a saphenous nerve block at the level of the knee
and with the patient in the supine position. First, a 22-gauge, 38-mm
blunt needle mounted on a 10-mL syringe (containing 10 mL of local
anesthetic solution) is introduced perpendicular to the skin and
through the sartorius muscle, 3 to 4 cm cephalad from the medial
femoral condyle. Within 3 cm, a loss of resistance is felt. After
negative aspiration for blood, 10 mL of local anesthetic is injected
slowly, with aspiration for blood after 5 mL. Second, a 50-mm insulated
needle connected to a nerve stimulator (2 mA, 2 Hz, 0.1 ms) is
introduced perpendicular to the skin, 3 cm distally to the medial
femoral epicondyle. Within 2 to 3 cm, the patient should report an
electrical paresthesia in the medial aspect of the leg. The needle
position is adjusted to maintain the paresthesia with a current of less
than 0.4 mA. After negative aspiration for blood, 6 to 8 mL of local
anesthetic is injected slowly. Third, a 25-gauge, 38-mm needle is
introduced 3 cm below the tibial plateau and directed from the middle
to the medial border of the leg. Ten milliliters of local anesthetic
solution is then injected subcutaneously. -
This block can be performed at any level
of the popliteal fossa. However, the more cephalad from the popliteal
crease, the closer are the common peroneal and tibial nerves.
Conversely, the more distal, the more separated the nerves become.
Indeed, the tibial nerve runs in the middle of the popliteal fossa
while the common peroneal nerve runs in a lateral direction toward the
head of the fibula. -
Variants of the proposed technique
include using the perpendicular line in the middle of the popliteal
crease as a starting point. If no motor response is elicited, the
needle is directed more laterally. -
The deep femoral vessels become the
popliteal vessels after passing through the adductor hiatus. The
popliteal vessels, which are initially medial and anterior and
separated from the sciatic nerve, run medial and anterior to the tibial
nerve at the lower part of the popliteal fossa. Consequently, the risk
of vessel puncture is minimal if the needle is kept in the lateral
upper quadrant of the popliteal fossa or if the needle is introduced
above the adductor hiatus (above the popliteal fossa). However, this
latter approach requires a 100-mm needle to be introduced deeper and
through the hamstring muscles, which is more painful to patients.
JD, Hadzic A, Kitain E. Anatomic considerations for sciatic nerve block
in the popliteal fossa through the lateral approach. Reg Anesth 1996;21:414–418.
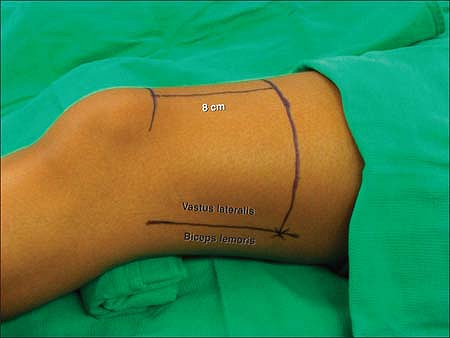
The groove between the biceps femoris muscle and the vastus lateralis
muscle is palpated and marked. A circumferential line is drawn on the
thigh 8 to 10 cm proximal from the top of the patella. The point of
needle entry is marked by the intersection of this line with the groove
between the biceps femoris muscle and vastus lateralis muscle (Fig. 12-17).
After disinfection and local infiltration with 1% lidocaine, a 100-mm
insulated needle connected to a nerve stimulator (1.5 mA, 2 Hz, 0.1 ms)
is inserted perpendicular to the skin (Fig. 12-18)
in search of either the common peroneal or tibial nerve. After
adjusting the needle position to maintain a motor response at a current
below 0.5 mA and negative aspiration for blood, the volume is injected
slowly (10 mL/min) and in 5 mL increments. If a sciatic
nerve
response cannot be obtained with the described change in needle angle
the needle is withdrawn until the local biceps femoris muscle
reappears. The needle is then reinserted in 10° increments first more
posterior than the initial angle, or in 10° increments more anterior.
 |
|
Figure 12-17.
The point of needle entry is marked by the intersection of this line with the groove between the biceps femoris muscle and vastus lateralis muscle. |
 |
|
Figure 12-18. An insulated needle connected to a nerve stimulator is inserted perpendicular to the skin.
|
-
If the medial aspects of the lower leg
and ankle are involved in the surgery, the addition of a saphenous
nerve block will be necessary to provide complete anesthesia. This can
be achieved by blocking the saphenous nerve selectively above or below
the knee or by performing a femoral nerve block. The latter is
especially recommended if thigh coverage will be used during surgery. -
In most individuals the division of the
sciatic nerve into the common peroneal nerve and the tibial nerve
occurs below the suggested level of needle insertion. However, if this
block is performed closer to the knee, a double stimulation and
injection technique accounting separately for both branches may be
necessary to achieve a complete block in the sciatic nerve territory of
the lower leg. -
If the local biceps femoris muscle twitch
cannot be elicited, the needle can be inserted in a perpendicular
direction until the femur is contacted. Then the needle is withdrawn
and reinserted in 10° to 15° increments posterior to the horizontal
plane until a sciatic nerve response is obtained. -
Plantar flexion (tibial nerve response)
as the elicited motor response may yield a more complete block and a
faster onset time than dorsiflexion (peroneal nerve response). -
This approach is a great alternative to
the posterior popliteal and the classic approaches to the sciatic nerve
if the patient cannot be positioned in prone or lateral decubitus
position. -
Slightly supporting the knee by placing a small towel under the popliteal fossa allows for easier needle operation.
A, Vloka JD. A comparison of the posterior versus the lateral
approaches to the block of the sciatic nerve in the popliteal fossa. Anesthesiology 1998;88:1480–1486.
DH, Wong DH, Vaghadia H, et al. Lateral popliteal sciatic nerve block
compared with ankle block for analgesia following foot surgery. Can J Anaesth 1995;42:765–769.
Muniz M, Alvarez J, Cortes J, et al. Lateral approach to the sciatic
nerve block in the popliteal fossa: correlation between evoked motor
response and sensory block. Reg Anesth Pain Med 2003;28:450–455.
JD, Hadzic A, Kitain E, et al. Anatomic considerations for sciatic
nerve block in the popliteal fossa through the lateral approach. Reg Anesth 1996;21:14–41.

