LEGG-CALVÉ-PERTHES DISEASE
avascular necrosis of the femoral head. Although the exact etiology of
the disorder is not known, the association of Legg-Calvé-Perthes
disease with delayed skeletal maturation suggests a systemic
susceptibility to the problem. Some children have abnormalities of
coagulation with decreases in the factors involved in thrombolysis,
which may predispose them to avascular necrosis.
difficult for the clinician to know for certain which patients need and
will benefit from treatment. Current use of the lateral pillar
radiographic classification has improved our ability to assess severity
and prognosis in an individual case. Children younger than 6 years of
age at onset usually have a benign course, and major treatment is not
often necessary because they have a longer growing time to remodel
abnormalities. Children between 6 and 9 years of age at onset have more
symptoms and often benefit from surgical treatment. Children older than
9 years of age have a more severe course, and their response to
treatment is less predictable. In the long run, 50% of patients have no
disability as adults and the other half develop degenerative hip
disease by the fifth or sixth decade of life.
which means positioning the femoral head within the acetabulum in such
a way as to reduce lateralization and collapse of the softened head. In
the past, this was done with braces, but at present, femoral or pelvic
osteotomies are preferred.
disease are well established. The femoral head becomes ischemic for
reasons unknown and for an unknown period of time. Several studies
suggest that at least two episodes of ischemia are necessary to produce
the typical changes of Legg-Calvé-Perthes disease (7,27). More recent studies have shown that a number of children have deficiencies of proteins S and C and hypofibrinolysis (8,9).
The original studies suggested that the majority of children were
deficient in these factors, but subsequent reports have found only a
small proportion patients with Legg-Calvé with these coagulopathies (14).
radiodense, then appears fragmented radiographically as dead bone is
resorbed, and finally reossifies with new bone formation. These
sequential phases have been classified by Waldenström (30)
as increased density, fragmentation, reossification, and residual
stages. No treatment to date has been shown to either accelerate or
delay the healing process, although it was initially thought that
femoral osteotomy resulted in more rapid healing. This was disproved in
studies by Clancy and Steel (4) and Kendig and Evans (15).
During the fragmentation phase in more severe disease, the head loses
height, enlarges, and may flatten. As the head enlarges, the anterior
and lateral portions of the head extrude from the acetabulum. Over
several years, the femoral head completely reossifies and may remain
round in mild cases, become ovoid in moderate cases, and become
flattened in severe cases. Stulberg and colleagues (29) classified these groups according to femoral head status as:
|
disease can be estimated to some degree. The most frequently reported
prognostic factor is the age of the child at the onset of the disease.
Most, but not all, children presenting at younger than 6 years of age
have a good prognosis, whereas those between 6 and 9 years of age have
a variable course. Children older than 9 years of age presenting with
Legg-Calvé-Perthes disease have a worse prognosis than those with an
earlier onset. Within these general guidelines, the disease is quite
variable, and individual prognostication is difficult.
Legg-Calvé-Perthes disease. The Catterall classification delineates
four groups based on areas of femoral head involvement (2):
|
(extrusion, Gage’s sign, lateral calcification, and a horizontal growth
plate) suggests a worse prognosis.
classification, a newer system—the lateral pillar classification—has
come into general use (Table 173.1 and Fig. 173.1, Fig. 173.2 and Fig. 173.3) (12).
In this scheme, the lateral portion of the femoral head is evaluated on
the anteroposterior (AP) radiograph in the early fragmentation stage of
the disease.
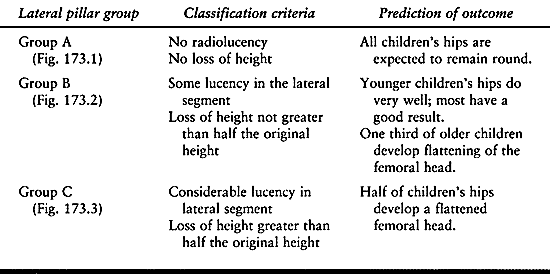 |
|
Table 173.1. Lateral Pillar Classification
|
 |
|
Figure 173.1.
Lateral pillar group A classification. AP radiograph of the left hip showing well-demarcated lateral pillar. There is no loss of height in the lateral segment of the femoral head in spite of some changes in radiodensity. |
 |
|
Figure 173.2. Lateral pillar group B classification.
|
 |
|
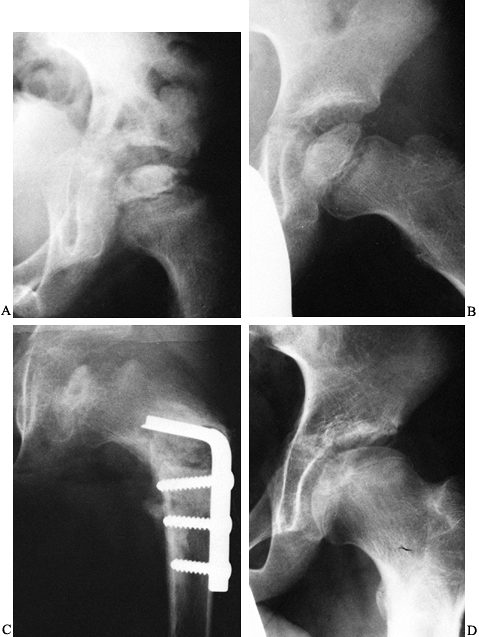
Figure 173.3.
Lateral pillar group C classification. AP radiograph of the pelvis of a boy who has had a varus osteotomy for Legg-Calvé-Perthes disease. A: The lateral portion of the femoral head is lucent and collapsed relative to the central portion. B: AP radiograph 9 months later showing further collapse of the lateral pillar. C: AP radiograph several years later showing flattening of the femoral head. |
been well studied, and all reports state that the majority of
individuals with the disorder do well through most of their adult lives
(6,10,23). McAndrew and Weinstein (17)
have shown that with follow-up studies of 48 years, about 50% of the
patients will develop severe enough hip disability to require a total
hip replacement by their fifth or sixth decade of life. In these
studies, those with onset of disease after 9 years of age had the
highest incidence of poor results. These studies demonstrate that
long-term prognosis is closely related to the roundness of the femoral
head and the congruity of the hip joint.
This was a natural evolution, because in those early days, the disorder
had just been distinguished from tuberculosis, and weight relief was
the mainstay of treatment for tuberculous hips. With time, the concept
of maintaining abduction along with bed rest became the basis for
containment therapy (20). Subsequent studies showed good results with weight-bearing abduction devices, and ambulatory containment was born (11,19).
necrosis in pigs and found that those animals whose hips were kept in
abduction had femoral heads that remained round, whereas the femoral
heads of the untreated animals flattened. Based on this work, surgical
containment, either with femoral or pelvic osteotomy, has been commonly
performed for Legg-Calvé-Perthes disease.
centers concerning indications for treatment of Legg-Calvé-Perthes
disease. Our current approach is based on preliminary data from a
long-term multicenter study that compared the treatment methods of
range of motion, bracing, femoral osteotomy, and Salter osteotomy.
-
Age at onset of disease between 6 and 10 years
-
Lateral pillar group B involvement with bone age at onset of more than 6 years
-
Lateral pillar group C involvement
-
Hips with a reasonable range of motion
-
All lateral pillar group A hips
-
Lateral pillar group B hips with a bone age at onset of 6 years or less
-
Any children younger than 6 years of age at the onset of the disease
activities when pain and limp worsen, and occasional periods of rest or
traction when necessary for loss of range of motion. Anti-inflammatory
medications are used when necessary. If persistent loss of motion
occurs, a period of a few months of ambulatory abduction bracing may
help the patient maintain range of motion.
onset is difficult. Many surgeons perform containment surgery, with the
caution that all may not go well. These children often lose range of
motion after surgery and may even need abduction casting or bracing
postoperatively. The combination of femoral and pelvic osteotomy may be
appropriate in this age group.
instituting containment treatment. In the child who has had recent
onset of Legg-Calvé-Perthes disease and presents in the early
radiographic stages, motion is usually relatively easily regained.
Often a few days of bed rest are sufficient to regain enough abduction
to “cover” the femoral head radiographically. If the hip is more
resistant to loosening up, then a program of night traction in
abduction may be helpful. After this, bracing or surgical containment
may be instituted.
has reached the fragmentation stage may require more vigorous methods
to regain motion. Try full-time traction and bed rest and, if these
measures are insufficient, institute a period in Petrie plasters. The
usual procedure is to evaluate the patient under anesthesia and perform
an arthrogram to assess femoral head flattening. If the hip can be
abducted sufficiently to cover the cartilaginous head, apply long-leg
plasters with an abduction bar. If the hip will not abduct, decide
whether “hinge abduction” is occurring. This is a condition in which
the head levers out of the acetabulum with abduction instead of moving
within the socket. If there is hinge abduction, containment surgical
procedures are contraindicated because severe hip stiffness may ensue.
If the head abducts but motion is limited by tight adductor muscles, an
adductor tenotomy may be helpful, followed by the Petrie casts.
motion to cover the hip before femoral osteotomy, but others perform
the procedure even when there is reduced motion (Fig. 173.4).
Because there is the occasional very stiff hip after the operation, I
recommend that the surgery be performed only in children with at least
30° of hip abduction. In those patients who lack this motion, I regain
range of motion by using Petrie casts for 6 weeks before performing
femoral osteotomy. If the patient has had Legg-Calvé-Perthes disease
for many months, there may be flattening of the femoral head, and thus
I perform an arthrogram before
osteotomy.
If the femoral head levers out of the joint with abduction (hinge
abduction), a varus osteotomy is contraindicated. Instead, a trial
period of Petrie casts may be instituted with repeat arthrogram to
determine if the hinge abduction has resolved, in which case the
osteotomy may be performed. Otherwise, other procedures such as valgus
osteotomy may be appropriate in these late cases.
 |
|
Figure 173.4. A 7 1/2-year-old boy with recent onset of symptoms. A:
An anteroposterior radiograph of the left hip showing the risk signs of lucency of the lateral portion of the femoral head, metaphyseal lucency, and lateral widening of the joint space. B: An abduction-internal rotation radiograph of the left hip. There is adequate coverage of the femoral head on this view. Note the subchondral lucency over two thirds of the femoral head, classifying this as a Salter-Thompson type B. There is also lateral calcification, another of Catterall’s risk signs. C: An AP radiograph following a varus proximal femoral osteotomy fixed with a blade plate. The neck-shaft angle is 118°. D: An AP radiograph 4 years after osteotomy showing satisfactory roundness of the femoral head. The blade plate was removed 1 year postoperative. |
subtrochanteric level. There are a variety of opinions as to how much
varus and derotation should be used. Some surgeons estimate the amount
of varus based on the amount of abduction required to cover the lateral
portion of the femoral head under the acetabulum. Most surgeons,
however, seek a certain neck-shaft angle regardless of the estimated
coverage. A commonly used angle is 115° to 120°. A greater amount of
varus will result in an abductor limp that may persist. Some remodeling
of the neck-shaft angle will occur in younger children with lesser
involvement, but older children and those with severe disease may not
have the growth capacity to remodel the neck-shaft angle. Rab (22)
has published a review of preoperative radiographic evaluation for
osteotomies about the hip, which is helpful in the planning stage.
concept that this will improve anterior coverage of the femoral head.
This may cause the patient to out-toe and probably should be done
minimally, if at all. Other surgeons perform a proximal osteotomy, and
extend or anteriorly angulate the osteotomy to improve anterior
coverage.
plates or screw plate devices specifically designed for children.
Immobilize in a cast those patients requiring muscle releases and those
who cannot cooperate with limited weight bearing. (Remember that these
children tend to be extremely active.) See Chapter 166 for more details on the operative technique.
with these active children. Malunion into varus is a serious problem,
which will result in a poor gait. Nonunion, however, is uncommon. The
more severely involved hips may become progressively stiffer following
the osteotomy. When this occurs, the varus of the osteotomy results in
adduction of the thigh. It may be necessary to return the patient to
the operating room for adductor muscle releases and placement of Petrie
casts for a period of time to restore hip range of motion. We have even
had to return patients to brace wear for 6 to 8 weeks to maintain
abduction postoperatively.
that time, if there is excessive varus (perhaps less than 110°
neck-shaft angle), an arrest of the greater trochanter may be
appropriate to keep the trochanter below the femoral head.
Occasionally, when excessive varus has been introduced, it may be
necessary to perform a valgus femoral osteotomy subsequently to restore
a normal gait.
Salter has recommended that a full range of motion be obtained and that
an arthrogram show no flattening of the femoral head as a prerequisite
to his operation (25,26).
In practice, many surgeons perform the procedure when an adequate range
of motion has been obtained and the flattening of the femoral head is
mild.
 |
|
Figure 173.5.
An 11-year-old boy with a history of 4 months of right hip discomfort and limp. Children of this age often have the poorest results regardless of treatment. A: Anabduction-internal rotation radiograph showing adequate coverage of the right femoral head. The head is in the phase of increased density, and risk factors have not yet appeared. B: An anteroposterior radiograph 3 months after Salter innominate osteotomy. The pins have been removed, and the osteotomy is healed. The femoral head is showing signs of flattening. C: An AP radiograph 20 months after osteotomy. The femoral head has healed and is reasonably round. D: An AP radiograph 6 years after osteotomy. The femoral head has further flattened over the intervening years. |
described. Salter has emphasized lengthening the iliopsoas to reduce
the pressure on the hip. Some surgeons prefer the Kalamchi modification
of the procedure, which moves the distal fragment of the osteotomy into
a notch in the posterior part of the pelvis (13).
The purpose of this technique is to avoid lengthening the pelvis and
increasing the pressure on the femoral head. Other surgeons add a shelf
of cancellous bone over the femoral head to add to coverage. Most
surgeons immobilize the hips in spica casts for 6 weeks, but some use
screw fixation for the osteotomy and allow partial weight bearing until
the osteotomy has healed. See Chapter 166 for details on operative technique.
stiffness, which at times can be severe. As with the femoral osteotomy,
it may be necessary to perform muscle releases and use Petrie casts and
braces postoperatively to regain range of motion. As with any
osteotomy, it is important to position the osteotomy fragments properly
and obtain secure internal fixation. If the fixation pins or screws are
improperly placed, the osteotomy will displace posteriorly and be
ineffective.
indicated for the patient who presents late with well-established head
deformity and hinge abduction (3,21).
The purpose of the osteotomy is to reduce the adduction of the thigh
and allow better weight-bearing alignment. At times, the femoral head
will remodel after this procedure. This should be considered a late,
reconstructive operation and is not appropriate as primary treatment.
See Chapter 29, Chapter 104, and Chapter 166 for details on the operation.
involved hips, especially in children older than 9 years of age at the
onset of the disease. The current reports of this approach suggest that
there is an improvement in outcome, but more evaluation is necessary
before this procedure should be done commonly (5,18).
will develop an osteochondritic lesion, usually many years after the
onset of the disorder. The symptoms of locking and popping suggest the
diagnosis, which then may be confirmed with arthrography or computed
tomography (CT) scanning. Arthroscopy may allow removal of either a
loose body or, more commonly, a softened area in the center of the
femoral head (1,28).
Sometimes an anterior arthrotomy to locate the loose body is
appropriate, but it may be necessary to dislocate the hip to find the
loose body.
Legg-Calvé-Perthes disease who presents when the disease is in the
phase of increased density or early fragmentation follows: For a child
whose bone age is six years or less, I institute conservative treatment
(rest, anti-inflammatory agents) until there is enough fragmentation to
determine lateral pillar classification. If the patient’s hip is
determined to be class A, I perform no further treatment. If the hip is
determined to be class B, I continue symptomatic treatment, and if it
is Class C, I prefer containment surgery, usually a Salter osteotomy.
clinical signs are minimal, I observe the patient until I am certain of
a significant degree of disease beyond class A. If significant clinical
signs are present, I allow the patient to regain range of motion
conservatively and consider containment surgery (I prefer Salter
osteotomy).
difficult. I consider containment surgery if the disease is in the
early phase. Usually a Salter osteotomy is performed, sometimes
combined with a proximal femoral varus osteotomy. In children in this
age group, one must recognize that the overall prognosis is poor.
scheme: *, classic article; #, review article; !, basic research
article; and + , clinical results/outcome study.
C, Crawford A, Roy D, et al. Association of Antithrombotic Factor
Deficiencies and Hypofibrinolysis with Legg-Perthes Disease. J Bone Joint Surg 1996;78A:3.
C, Glueck H, Greenfield D, et al. Protein C and S Deficiency,
Thromphilia, and Hypofibrinolysis: Pathophysiologic Causes of
Legg-Perthes Disease. Pediatr Res 1994;35:383.
MH, Menon MP. Legg-Calvé-Perthes Disease. The Value of Roentgenographic
Measurement in Clinical Practice with Special Reference to the
Broomstick Plaster Method. J Bone Joint Surg 1966;48A:1310.
JR, Hresko T, McDougall PA, et al. Prospective Re-evaluation of the
Association between Thrombotic Diathesis and Legg-Calvé-Perthes
Disease. Pediatric Orthopaedics Society of North America (POSNA) 1998 Annual Meeting. Cleveland, 1998, p 96.
M, Zahir A, Freeman MA. The Experimental Stimulation of Perthes Disease
by Consecutive Interruptions of the Blood Supply to the Capital Femoral
Epiphysis in the Puppy. J Bone Joint Surg 1973;55A:335.
A, Lechevallier J, Rao N, Bowen J. Diagnostic and Therapeutic
Arthroscopy of the Hip in Children and Adolescents: Evaluation of
Results. J Pediatr Orthop 1995;15:317.
