Knee Osteotomy
unicompartmental arthrosis of the knee. Alignment correction procedures
about the knee have been used since their introduction by Langenbeck in
the 19th century and were popularized by Jackson, Coventry, and Maquet.
Paramount to success is understanding the biomechanics and
pathophysiology, as well as proper patient selection and surgical
execution. In this chapter the pathogenesis, diagnosis, surgical
indications, surgical technique, results, and potential complications
will be discussed.
including genetic factors, major trauma or trauma from overload
secondary to obesity, and/or mechanical malalignment. A concentration
of force greater than that which the articular cartilage and
subchondral bone can tolerate is a common theme leading to secondary
knee osteoarthritis. Malalignment of the limb in excessive varus or
valgus will overload the medial or lateral compartments, respectively,
and is an important factor in the development of unicompartmental
arthritis of the knee. The rationale for realignment osteotomy is to
correct the malalignment at the knee by decreasing the excessive load
across the affected compartment.
activity-related knee pain, which is typically located in the affected
compartment. Examination should focus on knee range of motion,
ligamentous stability, and excluding extra-articular causes of pain
(hip, back, vascular, and soft tissue problems). Proper imaging
includes radiographs of the knee in three planes and a flexed
posterior-anterior weight-bearing view. A long-leg weight-bearing
radiograph is essential for preoperative planning. In selected
situations, MRI or bone scan may be used to study the status of the
noninvolved compartment and meniscus and to look for associated
chondral lesions. In most cases prior to considering surgery, patients
should have pain sufficient to justify an operation and have failed a
structured nonoperative treatment program including appropriate
activity modification, weight reduction, use of nonsteroidal
anti-inflammatory agents, bracing, and shoe wedges.
indication for osteotomy is unicompartmental osteoarthritis with a
secondary varus or valgus malalignment. Osteotomy also has been used
for patients with localized avascular necrosis, cartilage defects, and
concurrently with osteochondral allografts although little is known
about the long-term results of the procedure in these conditions.
Ligamentous stability is necessary, although cruciate instability is
not an absolute contraindication as ligament reconstruction can be done
at the same time or staged with the osteotomy. A reasonable range of
motion is necessary with at least 110 degrees of flexion and no more
than 10 degrees loss of extension. Age over 60 to 65 years is a
relative contraindication, but physiologic age and activity are more
important considerations. Inflammatory arthritis, diffuse
osteoarthritis, and marked femoral-tibial subluxation are absolute
contraindications. Obesity, osteoporosis, chondrocalcinosis, and marked
malalignment (>20 degrees) are not strict contraindications, but the
success rate and prognosis are compromised.
corrected on the tibial side of the joint and those with valgus
malalignment are best dealt with on the femoral side to minimize
postoperative joint line obliquity. Patients with severe malalignment
occasionally should be corrected on both sides of the joint to minimize
joint line obliquity. This chapter will focus on the correction of the
more commonly seen varus-malaligned limb.
the decision of whether to do a closing wedge versus an opening wedge
needs to be made. Both have advantages and disadvantages (Table 23-1).
postoperative mechanical axis. There are multiple ways to plan for an
osteotomy, and below is one such technique.
|
TABLE 23-1 Advantages and Disadvantages of A Closing Wedge Versus an Opening Wedge
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||
draw the contours of the whole limb. One should take into account
instability of the lateral collateral ligament to avoid overcorrection
with the osteotomy. If there is marked lateral collateral ligament
instability, stress views can facilitate how much deformity is
corrected by the instability versus bony deformity and help determine
the proper correction. Depending on the severity of the medial
cartilage loss, the new axis is planned to be located 10% to 40% into
the lateral compartment. With increasing severity of medial compartment
arthritis, the amount of correction is increased.
 |
|
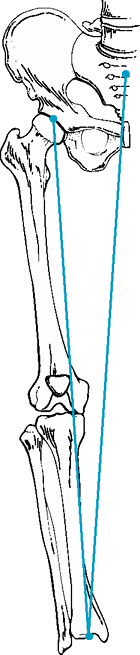
Figure 23-1 Drawing with present mechanical axis placed from center of femoral head to center of ankle.
|
 |
|
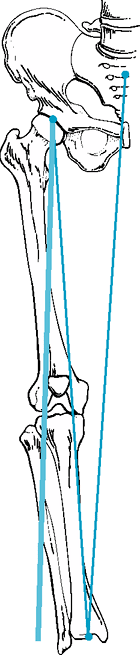
Figure 23-2 Drawing with planned mechanical axis from center of head through lateral compartment.
|
head through the desired point in the lateral compartment (10% to 40%)
to the ankle (Fig. 23-2).
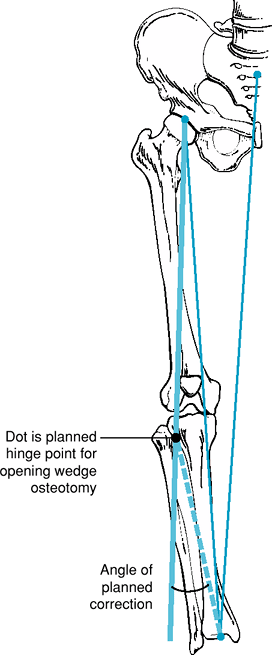
distally to the new and old center of the ankle. This gives the angle
of desired correction (Fig. 23-3).
anterolateral tibia is exposed to the fibula head. If a major
correction is planned (>10 to 12 degrees) resection of the
tibia-fibular joint can be performed with an osteotome and/or rongeur.
Osteotomy of the tibia is then performed under fluoroscopic control. A
K-wire is placed parallel to the joint line, approximately 2.5 cm
distal to the joint line. A second K-wire is placed distally, creating
a closing wedge at an angle that equals the desired amount of
correction. Fluoroscopy can confirm correct size angle of the wedge.
The osteotomies are then performed, protecting the posterior structures
and patellar tendon. It is important to maintain the integrity of the
medial cortex as this serves as a tension band when the osteotomy is
closed. The bony wedge is removed, and the osteotomy is closed and
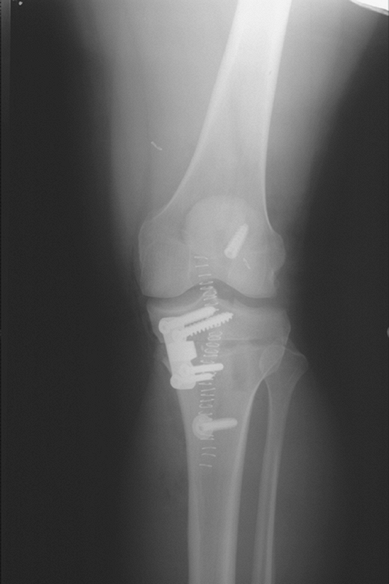
fixed with staples or a small laterally based L-plate (Fig. 23-4). Prior to fixation, with the osteotomy closed, it is important to check for overall
alignment using fluoroscopy. An electrocautery cord or a long metal rod
may be superimposed over the center of the hip and center of the ankle
to ensure correct placement of the restored mechanical axis into the
lateral compartment.
 |
|
Figure 23-3 Hinge point identified and planned correction angle generated from hinge point to old and new ankle center.
|
anterior-medial incision. A 2-mm K-wire is drilled parallel to the
joint line, 3.5 to 4.5 cm distal to the joint line, engaging the
opposite cortex. Proper position is confirmed with fluoroscopy. The
osteotomy is performed distal to the K-wire to prevent intra-articular
fracture into the lateral compartment. The osteotomy is performed
proximal to the tibial tuberosity. The posterior structures are
protected, and the osteotomy is performed leaving the lateral cortex
intact, provided that no sagittal correction is needed. The posterior
soft tissues are released to avoid increasing the posterior slope when
the osteotomy is opened. The osteotomy is opened slowly using stacked
osteotomes or a manufactured wedge to the desired correction. Proper
correction is confirmed using intraoperative fluoroscopy with a long
rod or a electrocautery cord.
Small corrections (<10 degrees) can be left alone, but most surgeons
favor using allograft bone or bone graft substitute to fill the defect.
The plate is placed distally under the pes anserine tendons. Closure is
routine over drains.
 |
|
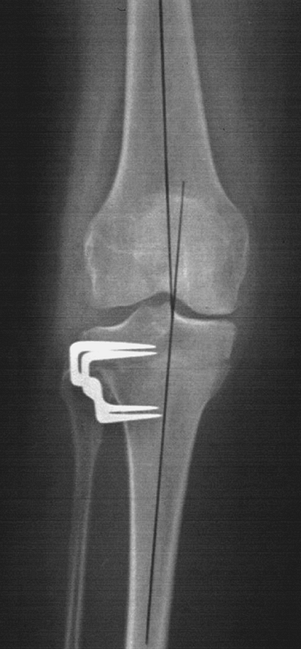
Figure 23-4 Ten-year postoperative radiograph after closing wedge osteotomy fixed with two staples.
|
 |
|
Figure 23-5 Postoperative radiograph after opening wedge osteotomy with simultaneous ligament reconstruction.
|
after closing or opening wedge procedures. Neurovascular problems can
be avoided by proper technique and careful retraction. Fracture into
the joint is probably more common with the open wedge technique and can
be avoided by making sure one has osteotomized at least 90% to 95%
across the proximal tibia and gradual opening of the osteotomy.
Fracture of the lateral cortex or medial cortex may occur, especially
in young patients with hard bone. If this occurs, making sure one
obtains stable fixation will minimize the risk of this becoming
problematic. Poor correction can be avoided by careful technique and
the use of intraoperative fluoroscopy, but this is a relatively crude
technique. Inadvertent changing of the tibial slope is more difficult
to monitor. Making sure that the osteotomy is done properly in the
sagittal plane and that distraction or closure of the wedge is done
properly can minimize this problem. One may want
to
alter the slope intentionally in three situations: (i) In patients with
extension lags, decreasing the posterior tibial slope will improve
extension; (ii) in patients with hyperextension, increasing the
posterior tibial slope will help limit overextension; (iii) in patients
with posterior knee instability, increasing the slope will improve
stability in extension as the femur slides posteriorly and the tibia
anteriorly in this position. Delayed or nonunions can be avoided by
maximizing bony apposition and obtaining proper stability. DVT,
infection, hematoma, and compartment syndrome have been described.
removed on the second postoperative day. Mobilization and partial
weight bearing (approximately 15 to 20 kg) are begun immediately. With
closing wedge osteotomy and good fixation, range of motion is begun at
4 or 5 days with or without a removable splint. Patients with closing
wedge osteotomy fixed with staples may be immobilized in a cast for 4
to 6 weeks. If at 6 weeks radiographs show consolidation, progressive
weight bearing is allowed. Opening wedge osteotomy patients can begin
range of motion immediately and weight bearing after 6 to 8 weeks.
in patients treated with a closing wedge technique. Multiple authors
have shown that clinical results deteriorate with time. Insall showed
that at 2-year follow-up, 97% of patients had a good or excellent
result. The outcome deteriorates to 85% at 5 years and 59% at 9 years.
Multiple authors have also reported successful outcome, although with
shorter follow-up, with an opening wedge technique. Hernigou has
reported on 93 knees treated with opening wedge technique with 90%
having a good result at 5 years. Success depends on multiple factors
including proper correction, preoperative condition of the noninvolved
compartment meniscus, and severity of obesity.
osteoarthritis secondary to limb malalignment is a reliable and
somewhat durable procedure. Proper patient selection and surgical
execution will help optimize outcome.
P, Medevielle D, Debeyre J, et al. Proximal tibial osteotomy for
osteoarthritis with varus deformity. A ten to thirteen-year follow-up
study. J Bone Joint Surg 1987;69A:332–354.
