INTRINSIC MUSCLE CONTRACTURES
III – THE HAND > Reconstructive Procedures > CHAPTER 63 –
INTRINSIC MUSCLE CONTRACTURES
Departments of Orthopaedic Surgery and Anatomic Sciences, University at
Buffalo School of Medicine and Biomedical Sciences, State University of
New York; Department of Hand and Microsurgery, Millard Fillmore Health
System; and The Hand Center, University of Buffalo, Buffalo, New York,
14209.
If an injury or pathologic condition affects one set of these muscles,
the hand may become dysfunctional. Intrinsic muscle imbalance may be
attributable to weakness, paralysis, loss of compliance, stiffness, or
contracture (18,36,39).
Contracture or stiffness of the hypothenar, lumbrical, or interosseous
muscles leads to digital imbalance that disables the hand. This chapter
focuses on the correction of hand problems caused by contracture of the
intrinsic muscles. An understanding of the anatomy, as well as of the
specific pathophysiology, is essential if the operating surgeon is to
correct these problems (1,13,28).
Although the causes of intrinsic contractures may vary, there are a
number of typical pathologic patterns based on the common mechanisms of
trauma, spasticity, and connective tissue diseases.
defined as the central axis of the third metacarpal. The dorsal
interosseous muscles abduct the fingers from this axis, whereas the
palmar interosseous muscles adduct them. There are four dorsal and
three palmar interosseous muscles. In addition, there are three
hypothenar muscles
that
function like dorsal interosseous muscles. Dorsal interosseous muscles
arise from the metacarpal shafts and insert so as to achieve digital
abduction; the designation of first dorsal interosseous muscle thus
belongs to that muscle on the radial side of the index finger, and so
on, in an ulnar direction. The little finger is actually abducted by
the abductor digiti quinti; the middle finger is abducted in both a
radial and an ulnar direction and, therefore, has two dorsal
interosseous muscles (2,3,6,15,20).
have two muscle bellies and therefore two (tendon) insertions—one into
the base of the proximal phalanx and the other via the dorsal (tendon)
mechanism (Fig. 63.1). The bony insertion
deviates the digit and has a mild effect on proximal phalangeal
[metacarpophalangeal (MP) joint] flexion. The tendon insertion produces
MP joint flexion via the transverse fibers over the dorsum of the
proximal phalanx. The tendon insertion also assists with proximal
interphalangeal (PIP) and distal interphalangeal (DIP) extension via
the oblique fibers that continue distally to join the lateral slips of
the extensor tendon, forming the conjoined lateral band. The (radial
and ulnar) lateral bands unite over the dorsum of the middle phalanx to
become the terminal tendon. The abductor digiti quinti inserts into
bone on the ulnar side of the proximal phalanx of the little finger,
and the flexor digiti quinti brevis forms the ulnar lateral band in the
little finger. The palmar interosseous muscles also arise from the
metacarpal shafts, but each has only one muscle belly. None has a bone
insertion into the proximal phalanx, but each functions as do the
lateral bands from the dorsal interossei (via the transverse fibers,
conjoined lateral band, and terminal tendon). The opponens digiti
quinti, the most dorsal of the three hypothenar muscles, has an unusual
insertion into the ulnopalmar shaft of the fifth metacarpal, producing
carpometacarpal flexion and supination when it contracts.
 |
|
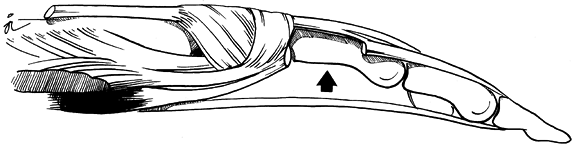
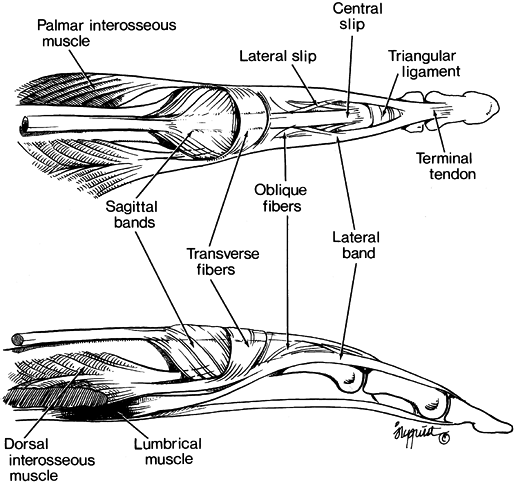
Figure 63.1.
Dorsal view of the anatomy of the interosseous muscles. Except for the third, all dorsal interossei have two muscle bellies and two tendon insertions. The dorsal interossei act as digital abductors. The hypothenar muscles function as dorsal interossei. Without exception, the palmar interosseous muscles, which have only one muscle belly, insert into the lateral band and oblique fibers. |
assist in flexing the MP joints. The lumbricals are unique in that they
arise on their antagonist, originating from the tendons of the flexor
digitorum profundus in the mid palm (Fig. 63.2).
Lumbricals of the index and middle fingers originate from the radial
side of the respective flexor digitorum profundus tendons. Lumbricals
of the ring and little fingers originate from bipennate muscle bellies
on the adjacent surfaces of the flexor digitorum profundus tendons.
Lumbrical tendons course distally palmar to the deep transverse
intermetacarpal ligaments, becoming part of the radial lateral bands at
the midportion of the proximal phalanges. When the lumbrical muscles
contract, they pull the flexor digitorum profundus tendon distally,
decreasing its flexion effect (relaxing the antagonist), as well as
pulling proximally on the lateral band and terminal tendon, thereby
extending the PIP and DIP joints.
 |
|
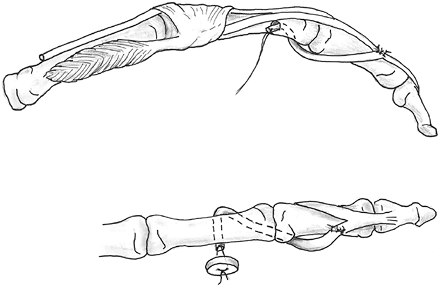
Figure 63.2.
Lumbrical anatomy. The lumbrical is unique in that it both arises from and inserts into a tendon, relaxing its antagonist when functioning. Normal lumbrical contraction tightens the lateral band (interphalangeal extensor fibers); it also pulls the flexor digitorum profundus tendon distally, diminishing flexor tone. |
the proximal phalanges (MP joints), lying in the dorsal midline and
inserting via the sagittal bands (Fig. 63.3).
These aponeuroses pass in a palmar direction, attaching into the palmar
plate and base of the proximal phalanges. The sagittal bands (extrinsic
extensor fibers) are proximal and medial to the transverse fibers
(intrinsic flexor fibers). It is important not to confuse the sagittal
bands with the transverse fibers, since the sagittal bands arise from
the extensor tendon, pass in a palmar direction, and extend the finger,
whereas the more distal transverse fibers arise from the lateral band
and pass dorsally, insert into the dorsal tendon mechanism (not bone),
and flex the proximal phalanx (Fig. 63.4) (9,18,20,31,36).
 |
|
Figure 63.3.
Anatomy of the extrinsic extensor tendons. The dorsal tendon mechanism at the metacarpophalangeal (MP) and proximal interphalangeal joint is composed of MP joint extensor fibers from the sagittal bands and intrinsic flexor fibers via the transverse fibers. More distally, the interphalangeal extensor tendons are formed from both the intrinsic and extrinsic tendons. |
 |
|
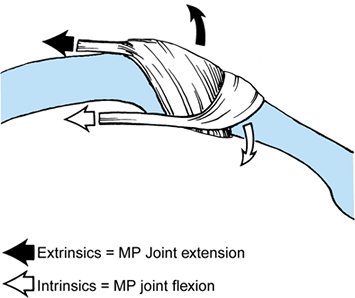
Figure 63.4.
Functional slings. At the metacarpophalangeal (MP) joint, the more proximal extrinsic extensor tendon extends the joint via the sagittal fibers, which course distally and in a palmar direction to insert on the palmar plate and flexor sheath. The intrinsic tendons act as flexors via the transverse fibers, coursing distally and dorsally over the base of the proximal phalanx. (From Smith RJ. Intrinsic Muscles of the Fingers: Function, Dysfunction and Surgical Reconstruction. Instr Course Lect 1975;24:200, with permission.) |
interphalangeal joints, and deviate the fingers. Therefore, intrinsic
contractures, with concomitant loss of compliance or elasticity, would
be expected to interfere with interphalangeal joint flexion and MP
joint extension. Less severe contractures tend to affect the
interphalangeal joints, whereas more severe contractures produce
deformity at both levels.
A simple physical test will usually confirm the diagnosis. Passive PIP
flexion is tested by the examiner while the MP joint is held flexed; it
is then tested again while the MP joint is held extended. A test of
intrinsic tightness is positive if there is significantly less passive
PIP flexion with the MP joint extended than with it flexed. Many
authors have described this test, and it is often (confusingly)
recorded eponymically (7,10,30,34).
In contrast, extrinsic tightness (contracture of the extensor tendons)
is present if passive PIP flexion is more limited when the MP joint is
flexed than when it is held in extension. It may be impossible to
perform these tests effectively if there are contractures in the MP or
PIP joints, or if a joint is dislocated. If there are both intrinsic
and extrinsic contractures simultaneously, one may obscure the other.
 |
|
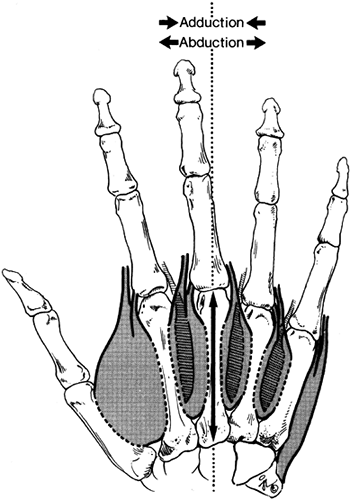
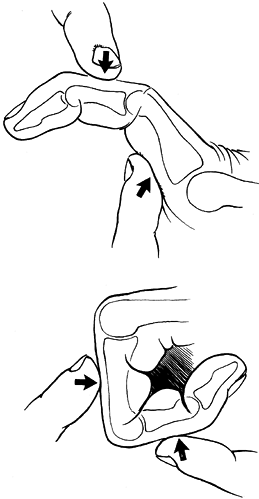
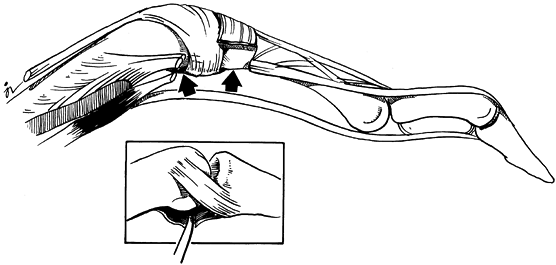
Figure 63.5.
Intrinsic muscle tightness is tested by passively flexing the proximal interphalangeal joint while the metacarpophalangeal (MP) joint is held flexed; it is then tested again while the MP joint is held extended. The intrinsic tightness test is positive if there is significantly less passive proximal interphalangeal flexion with the MP joint extended than with it flexed. |
significant intrinsic contracture follows trauma, probably caused by
muscle changes as a consequence of edema, anoxia, and immobilization.
For example, a patient may complain that she cannot grasp objects;
sometimes patients report weakness. A careful history and examination
will reveal the intrinsic muscle pathology. When examined in the
office, the patient may be almost able or fully able to make a fist
with unrestricted simultaneous MP and PIP flexion. In attempting to
grasp a hammer, however, the flexion of the MP joints is blocked by the
hammer, and active flexion of the PIP joints is decreased. This
activity is a functional test of intrinsic tightness.
contracture is made soon after injury (after a Colles’ fracture, for
example), significant dysfunction may be avoided. Treat to reduce
swelling, mobilize the intrinsic tendons, and stretch the muscle
bellies. Institute elevation, fluid-flushing massage,
and
intrinsic muscle-stretching exercises. Stretch the intrinsic muscles by
gradually and repetitively performing an intrinsic tightness test,
which involves simultaneous passive extension of the MP joints and
passive flexion of the PIP joints. This home and supervised outpatient
therapy program must be continued for several weeks to be fully
effective.
severely swollen, measure the pressure of the intrinsic muscle
compartments. (See Chapter 13 and Chapter 65
for information on compartment syndromes.) In acute cases, surgical
release of the fascial envelope about the intrinsic muscles, in
addition to the adductor pollicis, and release of the carpal tunnel may
be required (23,29).
-
After applying a tourniquet, approach the
intrinsic compartments of the swollen hand through longitudinal
incisions about 5 cm long, centered over the mid shafts of the second
and fourth metacarpals. Avoid injury to the dorsal veins and sensory
nerves. -
Retract the extensor tendons and incise
the interosseous fascia longitudinally at each intermetacarpal space.
If the second metacarpal incision does not afford adequate access to
the adductor pollicis in the first web, once the first dorsal
interosseous muscle fascia has been released, make an additional 3 cm
longitudinal incision just ulnar to the thumb MP joint, extending it
proximally. Incise the fascia dorsal and palmar to the adductor. -
In severe injuries, it may be necessary
to perform decompression of the hypothenar muscle via a longitudinal 3
cm incision at the ulnopalmar aspect of the hand and another incision
over the thenar muscles, as well as carpal tunnel release. -
Pin the MP joints of severely swollen
hands at about 70° of flexion with smooth 0.045 Kirschner wires
(K-wires); pin the thumb metacarpal in wide palmar abduction and
pronation. Do not close these longitudinal wounds while the hand
remains swollen; they may be closed secondarily after several days, or
by skin grafting. -
Keep the hand elevated and closely
observe circulation. Begin hand therapy with bedside visits to
encourage tendon gliding and small joint motion, except in those joints
that are transfixed. Continue active exercises during the period of
healing and maturation of skin grafts, if grafting has been required.
Dynamic splints and closely supervised active exercises may be
necessary. Remove the transfixion K-wires when the swelling has
subsided adequately; in any event, remove wires within 21 to 28 days
following insertion.
develop intrinsic tightness that affects the PIP joints exclusively.
When the hand is unprotected and swollen, MP joint flexion also becomes
difficult. The intrinsic muscles, however, can achieve relatively
unresisted PIP extension because the capsule and collateral ligaments
are initially more lax in that position. Continued PIP extension via
tight intrinsic muscles results in limited PIP flexion; in severe
cases, it may also be associated with actual capsular tightness at the
PIP level. The intrinsic tightness test is positive in such cases.
intrinsic stretching exercises has failed—a distal intrinsic release is
needed. The entire intrinsic mechanism need not be sacrificed, since
only PIP flexion is impaired. This release of the oblique fibers of the
lateral bands is known as a distal intrinsic release (i.e., it is
distal to the transverse fibers) (2,3,10,18,36).
-
Approach the lateral bands in the
affected fingers through a dorsal, longitudinal incision 2–3 cm long
over the middle third of the proximal phalanx. Carry the incision down
to the dorsal mechanism, then elevate the skin flaps, first to the
radial side and then to the ulnar side, exposing the lateral bands, the
oblique fibers, and the central and lateral slips of the tendon
mechanism. -
Divide the lateral bands and their
oblique fibers near the distal edge of the wound as they insert into
the central slip of the extensor mechanism (Fig. 63.6). Do not
P.1754P.1755
divide the lateral slip or the central slip of the extensor tendon;
preserve the transverse fibers of the intrinsic tendon as well. Resect
a 1 cm piece of the lateral band and its oblique fibers to correct the
contracture completely.![]() Figure 63.6.
Figure 63.6.
Distal intrinsic release. For moderate intrinsic contracture that
limits proximal interphalangeal flexion, resection of the oblique
fibers and contiguous lateral bands is performed on both the radial and
ulnar sides of the finger through a dorsal incision. -
Repeat the intrinsic tightness test after
both radial and ulnar lateral bands have been resected to verify the
completeness of the procedure (Fig. 63.7). Close the wounds and splint the MP joints in extension, taping the PIP joints into flexion.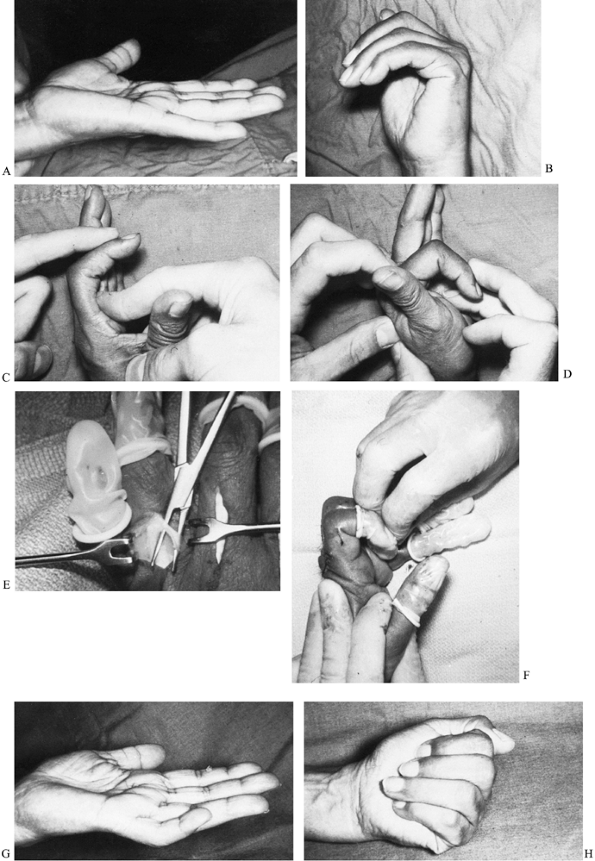 Figure 63.7. A,B: A 56-year-old woman had limited active proximal interphalangeal flexion 6 months after a Colles’ wrist fracture. C,D: The intrinsic tightness test was positive. E: A distal intrinsic release was performed. F: Immediately after the surgical release of the intrinsic, the tightness test was negative. G,H:
Figure 63.7. A,B: A 56-year-old woman had limited active proximal interphalangeal flexion 6 months after a Colles’ wrist fracture. C,D: The intrinsic tightness test was positive. E: A distal intrinsic release was performed. F: Immediately after the surgical release of the intrinsic, the tightness test was negative. G,H:
At 2 years after surgery, marked improvement in active proximal
interphalangeal flexion continues, although motion is still imperfect. -
Begin active and passive PIP flexion
exercises within a day or two of surgery. The MP flexion-block splint
can generally be discontinued after 14 days, although intrinsic
stretching and exercises should be continued for several weeks.
prolonged elevated compartment pressure will produce intrinsic
myonecrosis with secondary fibrosis, causing deformities at both the MP
and the interphalangeal joints (2,3,18,19,34,36).
These MP flexion contractures result only from marked and severe
intrinsic fibrosis, as evidenced by the fact that most significant
posttraumatic MP joint deformities are extension contractures resulting
from tight collateral ligaments and secondary capsular scarring. The
swollen MP joints strongly resist being flexed, and only in the
presence of marked intrinsic muscle scarring will a contracture be
severe enough to force the already tight, extended MP joints into a
flexed position. Severe PIP extension or hyperextension may also be a
part of this often static deformity. Secondary changes at both joints,
with pericapsular fibrosis in the deformed position, are not uncommon.
Often the first web is also limited because of contracture of the
adductor pollicis and the first dorsal interosseous muscles. A
significant degree of hand dysfunction results from these contractures.
only the distal intrinsic fibers, but also the transverse fibers of the
dorsal tendon mechanism that normally flex the MP joints (Fig. 63.8).
It is unlikely that these scarred intrinsic muscles will be functional
to any extent; therefore, they are best handled by removing the tendons
altogether, thus eliminating the deforming force. Overcorrection is
rarely a problem, even with an aggressive and complete release. Indeed,
full correction may be difficult to achieve.
 |
|
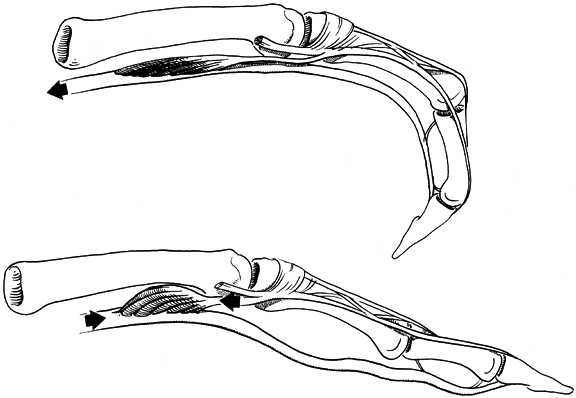
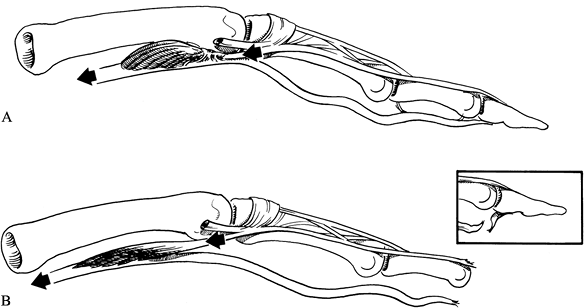
Figure 63.8.
Proximal intrinsic release. For severe intrinsic contracture causing fixed metacarpophalangeal (MP) flexion and proximal interphalangeal extension deformities, transverse fibers of the dorsal mechanism, intrinsic insertions into bone, and contiguous oblique fibers are resected on both sides of the affected digits. MP joint release may also be needed. |
-
Make a dorsal transverse incision that
extends from the radial mid-axis of the second metacarpal to the ulnar
mid-axis of the fifth, just proximal to the MP joints at the
metaphyseal flare of the metacarpals. -
Divide the tendons of all interossei and
of the abductor digiti quinti muscles at the MP joints. If MP flexion
persists even after the tendons have been removed, free the accessory
collateral ligaments and palmar plate from their attachments to the
base of the proximal phalanx, and with a dental probe release any
scarring between the plate and the metacarpal head. -
Verify relief of the combined MP flexion and PIP extension contractures by repeating the intrinsic tightness test.
-
When residual capsular inelasticity
hinders positioning of the MP joints in extension, it may be necessary
to pin them in that position with obliquely placed, smooth K-wires for
about 2 weeks. To correct PIP extension, it may also be necessary to
release the lateral bands separately—in much the same manner as the
distal intrinsic release was performed—at the time of the proximal
intrinsic release. In such cases, individual dorsal
P.1756
incisions may also be required to relieve the PIP contractures completely. -
Postoperative care is essentially the same as it is for a distal intrinsic release, as described earlier.
Since the skin is often tight, I have found that the most dependable
way to relieve the first web contracture is by approaching the adductor
via a standard Z-plasty or a Wolff four-flap Z-plasty in which the
dorsal longitudinal limb can be extended as far proximally as necessary
(6). The dorsal approach prevents injury to the palmar neurovascular and tendon structures.
-
Use a small chisel or elevator to free the adductor from its third metacarpal origin.
-
If necessary, pin the first metacarpal in
wide palmar abduction and pronation for up to 3 weeks, depending on the
ease of maintaining the corrected position with splints and dressings
alone.
in patients with cerebral palsy; it may also occur following
cerebrovascular accidents, and it may also affect patients with central
nervous system diseases (11,19,24,26,27,33).
At times, the intrinsic spasticity is not clinically evident until
after the tighter and stronger finger and wrist flexors have been
released surgically. Weeks or months after a flexor release or slide,
the previously corrected digits may begin to assume an intrinsic-plus
posture, with combined MP flexion and PIP extension or hyperextension,
often appearing unexpectedly. Although this deformity is similar to
that associated with severe posttraumatic contracture, the cause and
treatment are different. This condition is attributable to overactive
muscles, not scarred and necrotic tissue. The purpose of a surgical
release is ideally to decrease the spasticity, and to lengthen the
intrinsic muscle–tendon unit to correct the deformity and preserve
function. Strictly speaking, the intrinsic muscle cannot be lengthened;
however, such an effect is attainable via a muscle slide (31,32).
-
Make dorsal longitudinal incisions.
Generally, incisions over the second and fourth metacarpals are
sufficient. Avoid injury to sensory nerves, dorsal veins, and extensor
tendons. -
After incising the interosseous fascia
longitudinally, completely release the metacarpal origins of the
interossei subperiosteally with an elevator. Place the fingers in the
intrinsic-minus (claw) position, and slide the released muscles
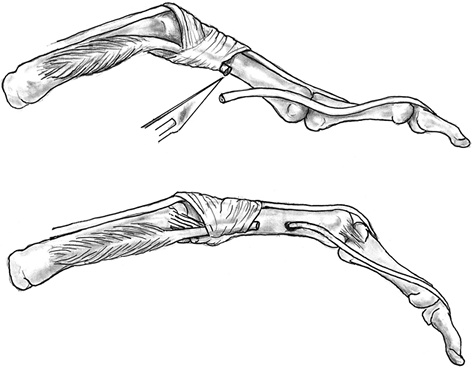
distally (Fig. 63.9).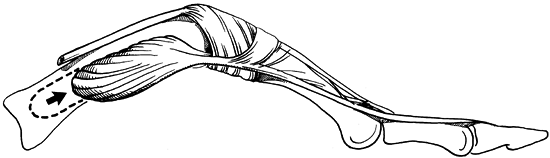 Figure 63.9.
Figure 63.9.
Intrinsic muscle slide. The metacarpal origins of the interossei are
completely released subperiosteally with an elevator. Placing the
fingers in an intrinsic-minus (claw) position causes the released
muscles to slide distally. -
Make separate incisions over the ulnar
portion of the first metacarpal for the superficial head of the first
dorsal interosseus, avoiding trauma to the princeps pollicis artery,
and at the ulnar aspect of the little-finger MP joint to transect the
tendons of the flexor digiti quinti. -
Transection of the abductor digiti quinti
may also be necessary. In this situation, maintain splinting in the
intrinsic-minus (claw) position of combined MP extension and PIP
flexion for 2–3 weeks before initiating therapy and exercises, so as to
encourage the released muscles to reattach more distally.
by intrinsic muscle slide is precluded. Patients with such deformities
may have associated capsular contractures and PIP hyperextension. The
best operation in these cases is an ulnar motor neurectomy.
-
Make a curvilinear, longitudinal,
ulnopalmar incision extending distally from a point just proximal and
radial to the pisiform, to a position distal and radial to the hamulus
(hook) of the hamate. -
Identify the deep motor branch of the
ulnar nerve as it courses dorsally and in a radial direction around
(distal to) the hamulus. Excise a 1 cm segment of nerve. Do not cut the
sensory branches of the nerve. Contractures, if present, may be
addressed appropriately at the same time.
reconstruction or replacement may occur in the chronically spastic
hand. For a discussion of the sublimis tenodesis and other similar
procedures, see Chapter 68.
the proximal part of the terminal tendon and contiguous conjoined
lateral bands retract proximally, unbalancing the extensor forces at
the PIP joint. A hyperextension deformity of the PIP joint may
gradually develop, or the joint may merely become more difficult to
flex actively (14,27). The intrinsic tightness test is typically positive.
stretching exercises may be required to correct this problem. Digital
rebalancing may have to be undertaken in resistant cases. The need for
tendon transfer release or capsulodesis is determined by a careful
assessment of the combined effects of the intrinsic and extrinsic
tendon contributions to the PIP overpull.
and inserts into a tendon, relaxing its antagonist when functioning.
Normal PIP flexion depends on balanced flexor digitorum profundus
contraction and lumbrical relaxation. Lumbrical scarring (shortening)
and loss of elasticity cause transmission of flexor digitorum profundus
traction into the lumbrical tendon, to which it has become tethered,
rather than through the more distal portion of the flexor digitorum
profundus tendon (Fig. 63.10A). Active pull on the flexor digitorum profundus tendon then causes PIP and DIP extension via the contracted lumbrical,
rather than flexion, a situation Parkes termed the “paradoxical lumbrical-plus finger” (25).
 |
|
Figure 63.10. Lumbrical contracture. A:
Lumbrical scarring to the flexor digitorum profundus causes transmission of flexor force into the lumbrical tendon rather than through the more distal portion of the flexor digitorum profundus tendon. B: When the normal flexor digitorum profundus insertion is lost (as in an untreated flexor digitorum profundus laceration or a distal joint amputation), contraction of the flexor digitorum profundus muscle is transmitted distally only via the intact lumbrical, thereby producing a paradoxical extensor effect. |
also be seen when the normal flexor digitorum profundus insertion is
lost, as may occur in untreated distal tendon lacerations or distal
joint amputations (Fig. 63.10B). The then-lax
profundus tendon retracts proximally, and contraction of the flexor
digitorum profundus muscle is transmitted to the dorsum of the PIP
joint via the lumbrical tendon, producing paradoxical extension or
limited active flexion. A loosely inserted tendon graft would have the
same effect. The intrinsic tightness test is positive in such cases.
problem. Indeed, I am careful to test patients with DIP amputations for
intrinsic tightness, and I often perform an acute radial lateral band
release. Intrinsic stretching exercises become a regular part of the
rehabilitation program.
rheumatoid arthritis. Unlike posttraumatic deformities, contracture may
be associated with painful synovitis, ulnar digital drift, joint
subluxation, and joint destruction. Secondary deformities are common
and may require a combination of joint and tendon reconstruction and
releases (5,8,35,37).
It is beyond the scope of this chapter to discuss correction of
rheumatoid ulnar drift, intrinsic tenodesis, and spiral oblique
retinacular ligament reconstruction (see Chapter 70).
hand but may develop after trauma, with severe intrinsic tightness. In
general, there must be a physiologic predisposition to (passive) PIP
joint hyperextension (present in many patients with connective tissue
inflammatory diseases). In addition, intrinsic tightness, whether
clinical or subclinical, is a requirement for this deformity,
characterized by the combination of PIP joint hyperextension and DIP
joint flexion. At the PIP joint, there is (secondary) laxity of the
volar plate, dorsal subluxation of the lateral bands, and contracture
of the collateral ligaments, which makes it difficult for the patient
to initiate PIP flexion, at first. With time, the deformities may
become fixed.
other causes of swan-neck deformity in patients with systemic
arthritis. Extrinsic tightness in a patient with palmar subluxation of
the proximal phalanx but no ulnar drift increases tension in the
extrinsic extensor central slip, producing PIP hyperextension. In such
a case, the intrinsic tightness test will be negative, but the
extrinsic tightness test is positive. Further, there are patients who
have coexisting intrinsic and extrinsic tightness. Such individuals
demonstrate marked resistance or inhibition of passive PIP joint
flexion at the extremes of both the intrinsic and extrinsic tightness
tests. In these, the PIP joint is “least tight” when the MP joint is
held at about 30° to 40° of flexion; and it is “most tight” at maximal
MP flexion and also at maximal MP extension. Flexor tendon rupture
(especially of the flexor superficialis), PIP joint volar plate laxity,
and DIP joint destruction resulting in terminal extensor tendon rupture
all may produce swan-neck deformities. In such problems, testing for
intrinsic and extrinsic tightness will not necessarily limit passive
PIP joint flexion until and unless the PIP deformity becomes fixed.
contracture of the PIP joint collateral ligaments and fixed dorsal
luxation of the lateral bands. Release of the intrinsics alone will not
restore normal balance and physiologic tendon function. Such fingers
need intrinsic release (proximal or distal release, as appropriate),
restoration of DIP joint extension—or tenodesis in an extended
position—and correction of the volar plate–ligament incompetence at the
PIP joint. If the PIP joint extension contracture is fixed, perform
dorsal capsulectomy and serial sectioning of some, or the majority, of
the collateral ligaments. To achieve treatment goals, combine the PIP
joint and intrinsic releases with an intrinsic tenodesis (Fig. 63.11).
 |
|
Figure 63.11.
Intrinsic tenodesis is performed when tightness is associated with proximal interphalangeal (PIP) joint palmar plate laxity. Proximal intrinsic release is done on one side of the finger (typically the ulnar side). The other intrinsic tendon is detached proximally, but its lateral band is kept attached to its normal distal phalangeal insertion and then passed proximally, palmar to Cleland’s ligament. The tendon is inserted into bone by suture or anchor with the PIP joint held flexed about 30° to 40°. (From Peimer CA. Intrinsic Muscle Dysfunction and Contractures. In: Surgery of the Hand and Upper Extremity. Peimer CA, ed. New York: McGraw-Hill, 1996:1559, with permission.) |
-
Approach fingers dorsally, through a
curvilinear longitudinal incision centered at the PIP joint, producing
the releasing incision described earlier. -
Divide the ulnar lateral band as for a
standard (proximal or distal) intrinsic release. Then detach the radial
lateral band proximally, and dissect distally over the middle phalanx,
carefully separating it from the intact central slip, and continuing
dissection to the middle third of the middle phalanx. Keep the terminal
tendon attached distally. -
Pass the dissected tendon slip in a
proximal direction, keeping it palmar to the axis of the PIP joint
motion and palmar to Cleland’s ligament, with gentle dissection via a
small curved clamp. -
In the majority, anchor the tendon into bone with the PIP joint flexed about 30°; the joint may be pinned temporarily.
the PIP joint, creates a volar check-rein (ligament) at the PIP joint,
and increases extensor tenodesis in the terminal tendon to improve DIP
joint extension.
preference) may dictate using the ulnar lateral band rather than the
radial one, and there is not a significant technical difference. The
goal of the operation is to tenodese the PIP joint in about 30°
flexion. Postoperative dressings protect this position.
operation—this is critical to prevent fixed PIP joint contracture and
tendon adhesions. Hand therapists can fabricate a custom digital
extension-block splint that allows active PIP flexion and extension to
about 30° to 35° during active and passive exercises. Beginning at
about 4–5 weeks after surgery, allow active PIP joint extension out of the splint, but continue splint protection for 6–8 weeks after surgery.
a spiral oblique retinacular ligament (SORL), but this requires a free
tendon graft.
-
Suture the graft into the normal
insertion of the terminal extensor tendon at the distal phalanx, and
then pass proximally, but diagonally, across the palmar surface of the
fibro-osseous canal, staying dorsal to the neurovascular bundles. -
Suture it into the proximal phalanx, volar and proximal to the PIP joint (Fig. 63.12).
![]() Figure 63.12.
Figure 63.12.
Spiral oblique retinacular ligament (SORL) reconstruction follows the
principles of intrinsic tenodesis but is utilized when Cleland’s
ligament is inadequate or the dorsal tendons unsuitable. A tendon graft
is needed and is passed from distal to proximal across the
fibro-osseous canal, but dorsal to the neurovascular bundles. It is
inserted into bone with the PIP joint flexed 30° to 40°. (From Peimer
CA. Intrinsic Muscle Dysfunction and Contractures. In: Surgery of the Hand and Upper Extremity. Peimer CA, ed. New York: McGraw-Hill, 1996:1559, with permission.)
than intrinsic tenodesis, in addition to the need for a tendon graft,
and probably should be reserved for patients who do not otherwise have
adequate stability of Cleland’s ligament to act as a check to retain an
intrinsic tendon palmar to the axis of PIP motion. Alternatively, one
can
reasonably
consider passing the native intrinsic tendon, if available (as
described earlier), across the flexor surface, as with the SORL, to
avoid tendon graft where dorsal tissues allow native correction but
Cleland’s ligament still does not provide a useful check-rein.
and contractures is failure to recognize the underlying cause of
limited PIP motion following injury. Intrinsic contractures are far
more common than generally appreciated. Adequate correction requires
accurate diagnosis. When active PIP flexion is limited as a result of
posttraumatic hand edema, suspect intrinsic tightness and impending
contractures and perform an intrinsic tightness test. Prompt
institution of intrinsic muscle-stretching exercises and regular
supervised therapy will often prevent the development of deformity and
fixed contractures.
required, should not be considered an end in itself, but rather a means
to an end—a second chance at therapy. Intrinsic contracture destroys
the delicate balance of the hand. Intrinsic release will not achieve
functional improvement unless these very demanding and unforgiving
small joints and tendons are made to glide in order to regain the full
range of motion in the postoperative interval. Select patients
carefully, and make every effort to help them understand the crucial
role they will play in their own recovery. Patients who are not
intellectually and emotionally committed to a recovery that requires
tediously repetitive therapeutic exercises, including frequent hand
therapy and office visits, should not undergo the procedure.
illustrations in this chapter, and Frances S. Sherwin for editorial
assistance.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
JW, Schreuders TA, Birke JA, et al. Manual Muscle Strength Testing:
Intraobserver and Interobserver Reliabilities for the Intrinsic Muscles
of the Hand. J Hand Ther 1995;8A:185.
VC, Wren C, Elliot D. Internal Splints for Prevention of First Web
Contracture Following Severe Disruption of the First Web Space. J Hand Surg 1994;19:560.
MW, Toth N, Schick K, et al. EMG Study of Hand Muscle Recruitment
during Hard Hammer Percussion Manufacture of Oldowan Tools. Am J Anthropol 1998;105:315.
AY, Chambers H, Wilkins KE, Bucknell A. Suction Injuries in Children
Leading to Acute Compartment Syndrome of the Interosseous Muscles of
the Hand: Case Reports. J Hand Surg 1996;21:675.
RJ, Kaplan EB. Rheumatoid Deformities at the Metacarpophalangeal Joints
of the Fingers: A Correlated Study of Anatomy and Pathology. J Bone Joint Surg Am 1967;49:31.
Schroeder HP, Botte MJ. Definitions and Terminology of Compartment
Syndrome and Volkmann’s Ischemic Contracture of the Upper Extremity. Hand Clin 1998;14:331.