HIP Dislocations, Femoral Head Fractures, and Acetabular Fractures
fracture, is a major injury. The forces needed to cause hip dislocation
are considerable, and, in addition to the disruption noted on
roentgenography, soft-tissue injury is significant. Occasionally, small
osseous or cartilaginous fragments remain in the hip joint. The injury
is most frequently caused by an automobile or automobile-pedestrian
accident, so significant injury elsewhere in the body is likely. A
fracture or fracture-dislocation at the hip can easily be missed when
associated with an ipsilateral extremity injury. Such an injury
emphasizes the rule: always visualize the joint above and the joint
below the diaphyseal fracture. Because injuries about the pelvis can be
missed in a seriously traumatized patient, most authorities advocate a
routine pelvic roentgenogram for all patients involved in severe blunt
trauma. The condition is viewed as an orthopaedic emergency. In
general, the sooner the reduction is achieved, the better is the end
result (1,2).
-
Anterior dislocations
-
Obturator
-
Iliac
-
Pubic
-
Associated femoral head fractures (see V)
-
-
Posterior dislocations
-
Without fracture
-
With posterior wall fracture (see IV)
-
With femoral head fracture (see V)
-
-
This injury usually occurs in an automobile accident, in a severe fall, or from a blow to the back while squatting. The mechanism of injury
is forced abduction. The neck of the femur or trochanter impinges on
the rim of the acetabulum and levers the femoral head out through a
tear in the anterior capsule. If in relative extension, an iliac or
pubic dislocation occurs; if the hip is in flexion, an obturator
dislocation occurs. In many instances, there is an associated impaction
or shear fracture of the femoral head as the head passes superiorly
over the anteroinferior rim of the acetabulum. These injuries are
associated with poor long-term results (3,4). -
On examination with an obturator dislocation, the hip is abducted, externally rotated, and flexed, but in the iliac or pubic dislocation,
the hip may be extended. The femoral head can usually be palpated near
the anterior iliac spine in an iliac dislocation or in the groin in a
pubic dislocation. In all patients, carefully assess the circulatory
and neurologic status before attempting a reduction. The diagnosis is
readily apparent on roentgenogram, which shows the femoral head out of
the acetabulum in an inferior and medial position. -
Treatment (2,3).
Early closed reduction is the treatment of choice, but open reduction
may be necessary. Reduction is optimally attempted under spinal or
general anesthesia, which ensures complete muscle relaxation. In the
multiply injured patient, reduction may be attempted in the emergency
department with sedation or pharmacologic paralysis after the airway is
controlled. Initiate strong but gentle traction along the axis of the
femur while an assistant applies stabilization of the pelvis by
pressure on the anterior iliac crests. For the obturator dislocation, the
P.308
traction is continued while the hip is gently flexed, and the reduction
is accomplished usually by gentle internal rotation. A final maneuver
of adduction completes the reduction but should not be attempted until
the head has cleared the rim of the acetabulum with traction in the
flexed position. For the iliac or pubic dislocation,
the head should be pulled distal to the acetabulum. The hip is gently
flexed and internally rotated. No adduction is necessary. If the hip
does not reduce easily, forceful attempts are not indicated. Failure to
obtain easy reduction with the above maneuvers usually indicates that
traction is increasing the tension on the iliopsoas or closing a rent
in the anterior capsule, producing a “buttonhole” effect. Forced
maneuvers only increase the damage. Because the closed reduction may
fail, the patient is initially prepared for an open procedure. The open
reduction can be accomplished through a muscle-splitting incision,
using the lower portion of the standard anterior Smith-Peterson
approach. The structures preventing the reduction are released. The
postreduction treatment is the same as for a posterior dislocation of
the hip, except it is important to avoid excessive abduction and
external rotation. -
Prognosis and complications.
Excellent reviews of hip dislocations have been published; anterior
dislocations occur in approximately 13% of some 1,000 hip dislocations.
Early reduction is necessary if a satisfactory result is to be
obtained, and although the end result is frequently excellent in the
child, traumatic arthrosis and, occasionally, avascular necrosis make
the prognosis guarded in the adult. Recurrent dislocation is rare in an
adult (1,2,3).
-
The mechanism of injury
is usually a force applied against the flexed knee with the hip in
flexion, as occurs most commonly when the knee strikes the dashboard of
an automobile during a head-on impact. If the hip is in neutral or
adduction at the time of impact, a simple dislocation is likely, but if
the hip is in slight abduction, an associated fracture of the posterior
or posterosuperior acetabulum can result. As the degree of hip flexion
increases, it is more probable that a simple dislocation is produced. -
Physical examination
reveals that the leg is shortened, internally rotated, and adducted. A
careful physical examination should be carried out before reduction
including sensory exam and muscle group motor strength grading. Sciatic
nerve injury is associated with 10% to 13% of these injuries (5).
Associated bony or ligamentous injury to the ipsilateral knee, femoral
head, or femoral shaft is not uncommon. When associated with a femoral
shaft fracture, a dislocation may go unrecognized because the classic
position of flexion, internal rotation, and adduction is not apparent.
In this situation, the diagnosis is confirmed by a single
anteroposterior roentgenogram of the pelvis as part of the initial
trauma roentgenographic series. This single examination does not allow
adequate assessment of any associated acetabular fracture (6,7,8),
however, so more roentgenograms are needed for treatment planning
before carrying out a reduction if an acetabular fracture is
identified. The patient, not the x-ray beam, is moved to obtain the
following films: the anteroposterior obturator oblique and the iliac
oblique views (6,9).
This is best accomplished by keeping the patient on a backboard and
using foam blocks to support the oblique position of the board (Fig. 22-1).
If necessary, computed tomography (CT) scanning can also be performed;
optimally, this is done after the closed reduction of the hip joint to
reestablish femoral head circulation. Although some authors question
its routine use after uneventful closed reduction, others report a 50%
incidence of bony fragments being identified with CT (9,10,11,12). -
Treatment
-
Posterior dislocation without fracture.
This dislocation is reduced as soon as possible and always within 8 to
12 hours when possible. Reduction is accomplished with the Allis
maneuver under spinal or general anesthesia to overcome the significant
muscle spasm. The essential step in a reduction is traction in the line
of the deformity, followed by gentle flexion of the hip to 90 degrees
while an assistant stabilizes the pelvis with pressure on the iliac
spine. With continued traction, the hip then is gently rotated into
internal
P.309
and
external rotation, which usually brings about a prompt restoration of
position. Because considerable traction is required, even with good
muscle relaxation, the alternative method of Stimson may be attempted.
The patient is placed prone with the hip flexed over the end of the
table, and an assistant fixes the pelvis by extending the opposite leg.
The same traction maneuvers described earlier are completed, but the
pull is toward the floor with pressure behind the flexed knee. Although
considerable traction is necessary, under no circumstances should rough
or sudden manipulative movement be attempted. Postreduction stability
should be confirmed on physical examination and by a roentgenogram
obtained in the operating room to be sure there are no fractures around
the femoral head or neck.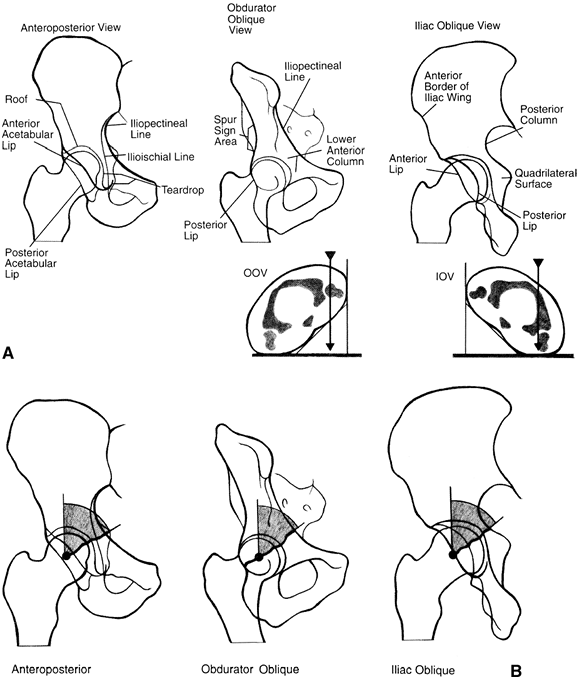 Figure 22-1. Radiographic assessment of acetabular fractures. A: The anteroposterior, obturator oblique, and iliac views are essential for the definition of the fracture. B:
Figure 22-1. Radiographic assessment of acetabular fractures. A: The anteroposterior, obturator oblique, and iliac views are essential for the definition of the fracture. B:
The “roof arc” measurement is made between a vertical line and the
angle of the fracture. Angles greater than 40 degrees on all three
views indicate a fracture which may be treated nonoperatively. (From
Hansen ST, Swiontkowski MF. Orthopaedic trauma protocols. New York: Raven, 1993:249.)P.310-
Postreduction treatment.
Isometric exercises for the hip musculature are instituted as soon as
pain subsides sufficiently. Continuous passive motion (CPM) may be
useful to maintain joint motion but is not essential. There is no
consensus in the literature as to the length of time the patient should
be restricted from weight bearing. The authors favor bed rest until the
patient is pain free and has established near-normal abduction and
extension muscle power. The patient then is allowed to move around,
using crutches for protective weight bearing until it is determined
that he or she can ambulate without pain or an antalgic limp; this
generally takes 3 to 6 weeks. At that time, full weight bearing is
permitted. -
Prognosis and complications
-
Sciatic nerve injuries are discussed in IV.2.c and e.
-
Avascular necrosis of the femoral head
is the most feared delayed complication from a simple posterior
dislocation of the hip. It occurs late, but various authors have noted
an average time of 17 to 24 months from injury to time of diagnosis.
Rates of approximately 6% to 27% are variously reported, and figures
show an incidence of 15.5% for early closed reductions, increasing to
48% if reduction is delayed. There were no good results if reduction
was delayed more than 48 hours. In Epstein’s classic study of 426
cases, better results were obtained with open reduction and internal
fixation in patients who had associated fractures (see Selected Historical Readings).
The overall rate of avascular necrosis was 13.4% with a higher rate of
18% in patients with associated fractures. For fracture-dislocations
treated by open means, the avascular necrosis rate was only 5.5%.
Treatment of avascular necrosis is discussed in Chap. 23, I.I.2. -
Epstein also reported an overall rate of traumatic osteoarthritis
of 23% following posterior hip dislocations, with a rate of 35% in
dislocations treated by closed means and a rate of 17% in those treated
by open means. In another series, after 12 to 14 years of follow-up,
16% of patients had posttraumatic arthritis, and arthritis developed in
an additional 8% as a result of avascular necrosis (2). Similar results have been reported from other centers (1,2).
-
-
-
Posterior dislocation with associated acetabular fracture
-
As previously noted, the dislocation is reduced as soon as possible considering the patient’s other injuries.
If the patient needs to undergo a lengthy trauma evaluation, then an
attempt can be made in the emergency department to reduce the hip with
sedation. In the patient who has been intubated for airway control,
chemical paralysis totally eliminates muscle spasm. If reduction
attempts fail, then the urgency for hip reduction must be transmitted
to the trauma team leader so the patient can be brought to the
operating room earlier in the evaluation phase. An alternative to
standard closed reduction maneuvers involves inserting a 5-mm Schanz
pin into the ipsilateral proximal femur at the level of the lesser
trochanter. This allows more focused lateral and distal traction by a
second assistant to accompany the reduction maneuver. If this maneuver
fails, then open reduction is preferred via a posterior approach. A
posterior wall fracture is internally fixed with lag screws and a
neutralization plate after joint lavage. If a more complex acetabular
fracture is present, then an experienced acetabular and pelvic surgeon
should be consulted (13). If the basic
posterior acetabular anatomy appears intact and the joint debridement
is complete, then a CT scan should be obtained to check on the adequacy
of debridement and to evaluate for associated fractures (4,11). -
Postoperative treatment.
Historically, traction has been used postoperatively, but this is no
longer recommended. With stable internal fixation, early motion is
advised starting with CPM. Flexion is generally limited to 60 degrees
for the first 6 weeks postoperatively for large posterior wall
fractures (13). Weight bearing is limited and crutches are used for 12 weeks (6,7,8,9). -
Sciatic nerve injury.
Direct contusion, partial laceration by bone fragments, a traction
injury, or occasionally an iatrogenic injury resulting from
malplacement of retractors during open reduction can cause this injury.
Nerve injury should be evaluated early by a careful motor and sensory
examination before reduction. If the nerve function is normal before
reduction and is abnormal after reduction, then this may represent
sciatic nerve entrapment in a fracture line. Emergent open reduction
and nerve exploration are indicated (6,7,8,9).
The peroneal portion of the sciatic nerve is most commonly injured
because it lies against the bone in the sciatic notch. When the entire
distal sciatic nerve function is abnormal, the tibial portion of
function returns nearly 100% of the time. The peroneal portion of
function is regained in 60% to 70% of cases: The more dense the motor
injury, the less likely is the return of good function (5).
The postinjury foot drop is generally easily managed by a plastic
ankle-foot orthotic. Tendon transfers at a later date remain an option. -
Prognosis and complications. Late traumatic arthritis and femoral head avascular necrosis can result in 20% to 30% of cases (6,7,8,9,13).
Of all acetabular fractures, the posterior wall injury, despite its
being the simplest pattern, has the worst prognosis with regard to
these complications (14,15,16).
Total hip arthroplasty is the most acceptable reconstruction option
when these complications occur; long-term results in this situation are
not as predictable as with total hip arthroplasty for arthritis (2,15).
Rarely total hip arthroplasty is indicated as the initial surgical
therapy in elderly patients with complex fracture patterns (17).
Most patients who sustain these injuries are younger than 50 years of
age, so loosening of the components over the patient’s lifetime is a
real concern (16).
P.311 -
-
-
Diagnosis.
Fractures of the femoral head generally occur with an associated hip
dislocation. They are seen as abrasion or indentation fractures of the
superior aspect of the head in association with an anterior dislocation
or as shear fractures of the inferior aspect of the head in association
with a posterior dislocation. Comminuted head fractures occasionally
occur with severe trauma. Femoral neck or acetabular fractures may be
involved. The diagnosis is established by roentgenograms and CT scan. -
Treatment
-
Emergent.
Early treatment must focus on reducing the hip dislocation and
diagnosing the fracture pattern. Diagnosis, made by clinical
examination, is confirmed by the admission anteroposterior pelvic
roentgenogram. Great care should be given in evaluating the
roentgenograms before reducing the hip because nondisplaced associated
femoral neck fractures may be displaced with the reduction maneuver. If
these are noted, the reduction should be performed in the operating
room under fluoroscopy so that, if the femoral neck fracture appears
unstable with the reduction maneuver, the surgeon can proceed with an
open reduction. If the closed reduction is successful, a repeat
roentgenogram is obtained to confirm the reduction and a CT scan should
be obtained for treatment planning. -
Definitive.
If the femoral head fracture is an indentation fracture associated with
an anterior dislocation, early CPM and mobilization with crutches
(partial weight bearing) are indicated. The prognosis regarding
degenerative joint disease is poor, however (3,4,18).-
If the femoral head fracture is a shear fracture associated with a posterior dislocation and is of small size (Pipkin type I, infrafoveal),
the treatment can involve a brief period of traction for comfort
followed by mobilization with a restriction of flexion to less than 60
degrees for 6 weeks. Indications for surgery include a restriction of
hip motion resulting from an incarcerated fragment and multiple
associated injuries. The fracture should be approached anteriorly for
best visualization (18). -
If the fracture is of larger size (Pipkin type II, suprafoveal),
the reduction should be anatomic or within 1 mm on the postreduction CT
to proceed with conservative treatment as outlined earlier. If it is
displaced,
P.312
open reduction and internal fixation with well-recessed (countersink) screws using an anterior approach is indicated (18). -
If the fracture is associated with a femoral neck fracture (Pipkin type III),
both fractures should be internally fixed via an anterior approach, and
early motion with CPM should be initiated. The prognosis for this
combination injury is not as favorable as with isolated femoral head
fractures because of the higher incidence of posttraumatic
osteonecrosis associated with the neck fracture. -
Femoral head fractures associated with acetabular fractures (Pipkin type IV)
should be managed in tandem with the acetabular fracture. Generally
this is accomplished operatively by an experienced pelvic surgeon (6,7,8).
-
-
-
Mechanism of injury.
These fractures result from a blow on the greater trochanter or with
axial loading of the thigh with the limb in an abducted position. -
Physical examination. These patients often have multiple injuries, so the management of the patient is the same as outlined in Chap. 1.
A careful examination of the sciatic nerve function must be conducted
with detailed sensory exam to light touch and motor grading of all
distal muscle groups. The muscles innervated by the femoral and
obturator nerves must also be examined because they can occasionally be
injured with complex anterior column fractures. The anteroposterior
pelvis admission trauma film and the two 45-degree pelvic oblique views
described by Judet (see Selected Historical Readings) (Fig. 22-1), as well as a CT scan of the pelvis (6,7,8,9),
are used to evaluate the fracture pattern. The scan is helpful in
determining the presence of intraarticular bone fragments, femoral head
fractures, and displacement in the weight-bearing region of the
acetabulum (12). Roof arc measurements are useful for treatment planning (Fig. 22-1). -
Treatment
-
Nonoperative. Traction was once the recommended definitive treatment for all acetabular fractures (19).
With modern techniques, nearly all significantly displaced acetabular
fractures can be fixed safely and effectively, even in elderly
individuals (20,13,6,7,8,9).
As definitive therapy, traction is not currently generally recommended,
with the exception of elderly patients with multiple medical
comorbidities. It is generally reserved for temporary treatment of
displaced transverse acetabular fractures in which the femoral head is
articulating on the ridge of the fracture edge on the lateral portion
of the joint. Traction prevents further cartilage injury and femoral
head indentation; however, it must be heavy (35–50 lb) and with a
distal femoral pin. Trochanteric pins to provide a lateral traction
vector should never be used if open reduction is an option at any time
in the patient’s management. If nonoperative management is selected,
then bed-to-chair mobilization for 6 to 8 weeks is the best option,
followed by gradual return to weight bearing. Total hip arthroplasty is
an effective salvage technique as long as the acetabular anatomy is not
too distorted (15,16). -
Operative. In
young patients, displacement of 2 to 3 mm in the major weight-bearing
portions of the acetabulum is an indication for open reduction (6,7,8,9).
Numerous surgical approaches to reduction are available, including the
Kocher-Langenbach posterolateral approach, the ilioinguinal, the
extended iliofemoral, and combined approaches. These procedures should
be undertaken by experienced acetabular surgeons because the techniques
for reduction and fixation are numerous and require much special
equipment; inferior results are documented by surgeons who are
inexperienced (13). Postoperatively, CPM is
occasionally used; patients are mobilized with 12 weeks of “touch down”
weight bearing with crutches. If posterior wall involvement is
significant, then flexion is restricted to 60 degrees for the first 6
weeks. Complications include infection (1%–2%), heterotopic
ossification (4%–6% functionally limiting), avascular necrosis (5%),
deep venous thrombosis (10%–20%), pulmonary embolus (1% fatal),
degenerative arthritis (20%–30%, generally associated with posterior
wall fractures), and sciatic nerve injury (2%–5%) (13,14,20,21,22,23). Occasionally, acute hip replacement is indicated in older patients with complex fractures.P.313Heterotopic ossification is most commonly associated
with extended posterior (the extended iliofemoral) and combined
approaches (21). All of these complications
occur more often when surgeons are inexperienced. Effective prophylaxis
includes indomethacin, 25 mg t.i.d for 6 weeks, and low-dose
irradiation (800–1,000 R) in the first week postoperatively (13,22). The use and relative benefits of radiation therapy and indomethacin remain controversial.
-
should be dealt with by internal fixation; then the acetabular injury
should be treated as outlined previously (6,7,8,9). Attempts at treating both injuries by traction have not been satisfactory.
Classic balanced traction with a half or a full ring Thomas splint is
not only cumbersome but also restricts the use of the hip in the muscle
rehabilitation program. A hip exerciser such as that described by Fry
should be considered. These techniques must be learned because they are
occasionally needed in treating problems associated with severe
preexisting systemic disease or local skin problems.
-
Immediate reduction is essential. Delaying reduction for more than 24 hours increases the incidence of avascular necrosis.
-
Weight bearing should be prohibited for 3 months
(a spica cast is recommended for children younger than 8 years of age),
at which time it usually is possible to determine the degree of
avascular necrosis, although a 3-year follow-up period is necessary to
assess this complication fully. Institution of prompt treatment and
protected weight bearing as for Legg-Calvé-Perthes disease probably is
indicated. Recurrent dislocation can occur in children who are not
immobilized. -
When reduction is achieved rapidly with no gross associated trauma, the results are usually satisfactory,
especially in patients younger than 6 years old. The incidence of
avascular necrosis, however, has been reported to be approximately 5%
to 10%.
pelvic radiograph and physical examination. Leg is shortened and
internally rotated for posterior dislocation and flexed and externally
rotated for anterior dislocation. Judet views and CT scan are obtained
after redcuction.
pelvis radiograph and physical examination these nearly always
accompany a hip dislocation, 90% of which are posterior dislocations
of hip (see previous discussion) followed by CT scan to assess size and
reduction of fragment. If reduction is anatomic, limited weight bearing
with crutches for 6 weeks
Surgical approach of ilioinguinal, Kocher-Langenbach or extended
approach based on fracture pattern and experience of surgeon; fixation
with lag screws and reconstruction plates; limited weight bearing for
12 weeks
SS, Moulton A, Srikrishnamurthy K. An analysis of the late effects of
traumatic posterior dislocation of the hip without fractures. J Bone Joint Surg (Br) 1983;65:150–152.
JM. Fractures of the acetabulum: accuracy of reduction and clinical
results in patients managed operatively within three weeks after the
injury. J Bone Joint Surg (Am) 1996;78:1632–1645.
Pierre RK, Oliver T, Somoygi J, et al. Computerized tomography in the
evaluation and classification of fractures of the acetabulum. Clin Orthop 1984;188:234–237.
FA, Bone LB, Border JR. Open reduction and internal fixation of
acetabular fractures: heterotopic ossification and other complications
of treatment. J Orthop Trauma 1991;5:439–445.
BR, Willson Carr SE, Gruson KI, et al. Computed tomographic assessment
of fractures of the posterior wall of the acetabulum after operative
treatment. J Bone Joint Surg (Am) 2003;85:512–522.
MF, Thorpe M, Seiler JG, et al. Operative management of displaced
femoral head fractures: case matched comparison of anterior versus
posterior approaches for Pipkin I and Pipkin II fractures. J Orthop Trauma 1992;6:437–442.
N, Matta JM, Bernstein L. Heterotopic ossification following operative
treatment of acetabular fracture. An analysis of risk factors. Clin Orthop 1994;305:96–105.
LX, Rush PT, Fuller SB, et al. Greenfield filter prophylaxis of
pulmonary embolism in patients undergoing surgery for acetabular
fracture. J Orthop Trauma 1992;6:139–145.
