Femoral Neck Fractures
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > IV – Lower Extremity Fractures and Dislocations > 29 – Femoral Neck Fractures
29
Femoral Neck Fractures
EPIDEMIOLOGY
-
More than 250,000 hip fractures occur in
the United States each year (50% involve the femoral neck), and this
number is projected to double by the year 2040. -
The average age of occurrence is 77 years for women and 72 years for men.
-
80% occur in women, and the incidence doubles every 5 to 6 years in women age >30 years.
-
The incidence in younger patients is very low and is associated mainly with high-energy trauma.
-
Risk factors include female sex, white
race, increasing age, poor health, tobacco and alcohol use, previous
fracture, fall history, and low estrogen level.
ANATOMY
-
The upper femoral epiphysis closes by age 16 years.
-
Neck-shaft angle: 130±7 degrees
-
Femoral anteversion: 10±7 degrees
-
There is minimal periosteum about the femoral neck; thus, any callus that forms must do so by endosteal proliferation.
-
Calcar femorale: This is a vertically
oriented plate from the posteromedial portion of the femoral shaft
radiating superiorly toward the greater trochanter (Fig. 29.1). -
The capsule is attached anteriorly to the
intertrochanteric line and posteriorly 1 to 1.5 cm proximal to the
intertrochanteric line. -
Three ligaments attach in this region:
-
Iliofemoral: Y-ligament of Bigelow (anterior)
-
Pubofemoral: anterior
-
Ischiofemoral: posterior
-
-
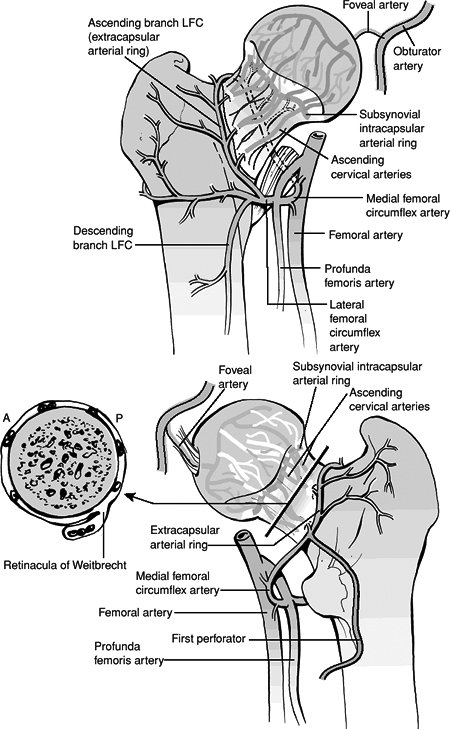
Vascular supply (Fig. 29.2):
-
Base of the femoral neck: An
extracapsular ring is formed anteriorly by the ascending branch of the
lateral femoral circumflex artery and posteriorly by the medial femoral
circumflex artery. -
The ascending cervical branches from this
ring pierce the hip capsule near its distal insertion, becoming the
retinacular arteries coursing along the femoral neck. Most supplying
the femoral head are posterosuperior in location. -
A subsynovial intracapsular arterial ring
is formed by these retinacular arteries at the base of the femoral
head. As they enter the femoral head, they unite to form the lateral
epiphyseal arteries. -
The lateral epiphyseal arteries that
arise from the posterosuperior ascending cervical branches supply the
majority of the femoral head. -
The artery of the ligamentum teres, usually a branch of the obturator, offers a small supplemental contribution to the
P.319
femoral head and is limited to the area around the fovea capitis.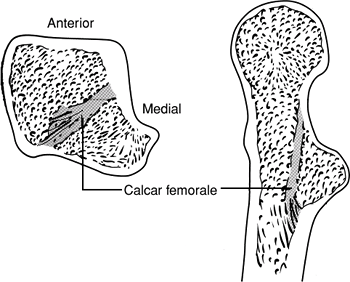 Figure
Figure
29.1. Left: The calcar femorale is a vertical plate of bone that
originates in the posteromedial portion of the femoral shaft under the
lesser trochanter and radiates laterally toward the posterior aspect of
the greater trochanter. Right: The calcar femorale fuses with the
posterior aspect of the femoral neck superiorly and extends distally
anterior to the lesser trochanter and fuses with the posteromedial
aspect of the femoral diaphysis.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
-
-
Forces acting across the hip joint:
-
Straight leg raise: 1.5 × body weight
-
One-legged stance: 2.5 × body weight
-
Two-legged stance: 0.5 × body weight
-
Running: 5.0 × body weight
-
-
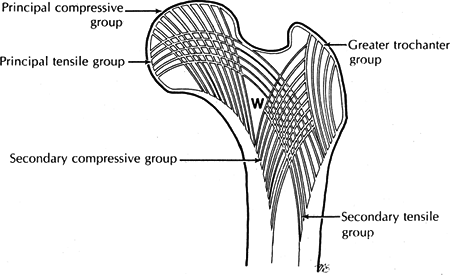
Internal anatomy: The direction of the
trabeculae parallels the direction of compressive forces. The bony
trabeculae are laid down along the lines of internal stress. A set of
vertically oriented trabeculae results from the weight-bearing forces
across the femoral head, and a set of horizontally oriented trabeculae
results from the force of the abductor muscles. These two trabeculae
systems cross each other at right angles (Fig. 29.3).
MECHANISM OF INJURY
-
Low-energy trauma; most common in older patients:
-
Direct: A fall onto the greater
trochanter (valgus impaction) or forced external rotation of the lower
extremity impinges an osteoporotic neck onto the posterior lip of the
acetabulum (resulting in posterior comminution). -
Indirect: Muscle forces overwhelm the strength of the femoral neck.
-
-
High-energy trauma: This accounts for
femoral neck fractures in both younger and older patients, such as
motor-vehicle accident or fall from a significant height. -
Cyclical loading-stress fractures: These
are seen in athletes, military recruits, ballet dancers; patients with
osteoporosis and osteopenia are at particular risk.
 |
|
Figure
29.2. Vascular anatomy of the femoral head and neck. Top: Anterior aspect. Bottom: Posterior aspect. LFC, lateral femoral circumflex artery. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
 |
|
Figure
29.3. Anatomy of the bony trabeculae in the proximal end of the femur. In a nonosteoporotic femur, all five groups of bony trabeculae are readily evident on x-ray. The Ward triangle (W) is a small area in the neck of the femur that contains thing and loosely arranged trabeculae only. (From Rockwood CA Jr, Green DP, Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 4th ed, vol. 2. Philadelphia: Lippincott-Raven, 1996:1667.)
|
P.320
P.321
CLINICAL EVALUATION
-
Patients with displaced femoral neck
fractures typically are nonambulatory on presentation, with shortening
and external rotation of the lower extremity. Patients with impacted or
stress fractures may however demonstrate subtle findings, such as
anterior capsular tenderness, pain with axial compression, lack of
deformity, and they may be able to bear weight. -
Pain is evident on range of hip motion, with possible pain on axial compression and tenderness to palpation of the groin.
-
An accurate history is important in the
low-energy fracture that usually occurs in older individuals. Obtaining
a history of loss of consciousness, prior syncopal episodes, medical
history, chest pain, prior hip pain (pathologic fracture), and
preinjury ambulatory status is essential and critical in determining
optimal treatment and disposition. -
One should assess the wrist and shoulders in elderly individuals because 10% have associated upper extremity injuries.
RADIOGRAPHIC EVALUATION
-
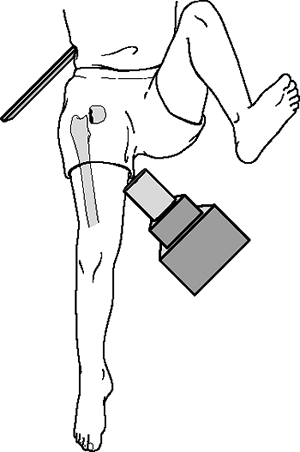
An anteroposterior (AP) view of the
pelvis and an AP and a cross-table lateral view of the involved
proximal femur are indicated (Fig. 29.4). -
An internal rotation view of the injured hip may be helpful to further clarify the fracture pattern.
-
Technetium bone scan or preferably
magnetic resonance imaging may be of clinical utility in delineating
nondisplaced or occult fractures that are not apparent on plain
radiographs.
 |
|
Figure
29.4. A cross-table lateral view of the affected hip is obtained by flexing the uninjured hip and knee 90 degrees and aiming the beam into the groin, parallel to the floor and perpendicular to the femoral neck (not the shaft). This allows orthogonal assessment of the femoral neck without the painful and possible injurious manipulation of the effected hip required for a “frog-leg” lateral view. (From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)
|
P.322
CLASSIFICATION
Anatomic Location
-
Subcapital
-
Transcervical
-
Basicervical
Pauwel
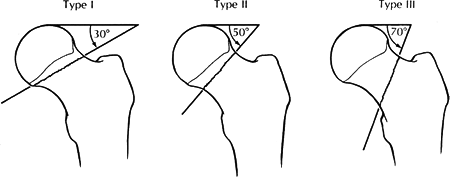
This is based on the angle of fracture from the horizontal (Fig. 29.5).
| Type I: | 30 degrees |
| Type II: | 50 degrees |
| Type III: | 70 degrees |
Increasing shear forces with increasing angle lead to more fracture instability.
Garden
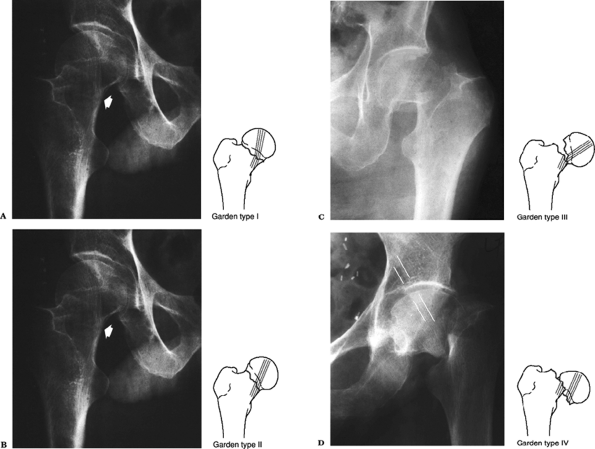
This is based on the degree of valgus displacement (Fig. 29.6).
| Type I: | Incomplete/valgus impacted |
| Type II: | Complete and nondisplaced on AP and lateral views |
| Type III: | Complete with partial displacement; trabecular pattern of the femoral head does not line up with that of the acetabulum |
| Type IV: | Completely displaced; trabecular pattern of the head assumes a parallel orientation with that of the acetabulum |
P.323
OTA Classification of Femoral Neck Fractures
 |
|
Figure
29.5. The Pauwel classification of femoral neck fractures is based on the angle the fracture forms with the horizontal plane. As a fracture progresses from Type I to Type III, the obliquity of the fracture line increases, and, theoretically, the shear forces at the fracture site also increase. (From Rockwood CA Jr, Green DP, Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 4th ed, vol. 2. Philadelphia: Lippincott-Raven, 1996:1670.)
|
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
Because of too poor intraobserver and interobserver
reliability in using the various classifications, femoral neck
fractures are commonly described as either:
reliability in using the various classifications, femoral neck
fractures are commonly described as either:
-
Nondisplaced: impacted valgus femoral neck fractures/stress fractures: This is a much better prognostic situation.
-
Displaced: Characterized by any detectable fracture displacement.
TREATMENT
-
Goals of treatment are to minimize
patient discomfort, restore hip function, and allow rapid mobilization
by obtaining early anatomic reduction and stable internal fixation or
prosthetic replacement. -
Nonoperative treatment for traumatic
fractures is indicated only for patients who are at extreme medical
risk for surgery; it may also be considered for demented nonambulators
who have minimal hip pain. -
Early bed to chair mobilization is
essential to avoid increased risks and complications of prolonged
recumbency, including poor pulmonary toilet, atelectasis, venous
stasis, and pressure ulceration.
 |
|
Figure
29.6. The Garden classification of femoral neck fractures. Type I fractures can be incomplete, but much more typically they are impacted into valgus and retroversion (A). Type II fractures are complete, but undisplaced. These rare fractures have a break in the trabeculations, but no shift in alignment (B). Type III fractures have marked angulation, but usually minimal to no proximal translation of the shaft (C). In the Garden Type IV fracture, there is complete displacement between fragments, and the shaft translates proximally (D). The head is free to realign itself within the acetabulum, and the primary compressive trabeculae of the head and acetabulum realign (white lines). (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Baltimore: Lippincott Williams & Wilkins, 2005.)
|
P.324
P.325
P.326
Fatigue/Stress Fractures
-
Tension-sided stress fractures (seen at
the superior lateral neck on an internally rotated AP view): These are
at significant risk for displacement; in situ screw fixation is
recommended. -
Compression-sided stress fractures (seen
as a haze of callus at the inferior neck): These are at minimal risk
for displacement without additional trauma; protective crutch
ambulation is recommended until asymptomatic.
Impacted/Nondisplaced Fractures
-
Approximately 8% to 33% of “impacted”
fractures will displace without internal stabilization, decreasing to
<5% with internal fixation. -
Less than 10% develop osteonecrosis
secondary to kinking of the lateral epiphyseal vessels and tethering of
the medial vessels in a valgus position or intracapsular hypertension. -
In situ fixation with three cancellous
screws is indicated; exceptions are pathologic fractures, severe
osteoarthritis/rheumatoid arthritis, Paget disease, and other metabolic
conditions, which require prosthetic replacement.
Displaced Fractures
-
Young patient with high-energy injury and
normal bone: Urgent closed/open reduction with internal fixation and
capsulotomy is performed. -
Elderly patients: Treatment is controversial:
-
High functional demands and good bone density: Use closed/open reduction and internal fixation versus total hip replacement.
-
Normal to intermediate longevity but poor
bone density, chronic illness, and lower functional demands: Perform
modular unipolar or bipolar hemiarthroplasty. -
Low demand and poor bone quality: Perform hemiarthroplasty using a one-piece unipolar prosthesis.
-
Severely ill, demented, bedridden patients: Consider nonoperative treatment or prosthetic replacement for intolerable pain.
-
Operative Treatment Principles
-
Fracture reduction should be achieved in
a timely fashion. Risk of osteonecrosis may increase with increasing
time to fracture reduction. Furthermore, the quality of fracture
reduction is believed to be the most predictive factor under the
surgeon’s control for loss of fixation.-
Fracture reduction maneuver: Perform hip
flexion with gentle traction and external rotation to disengage the
fragments, then slow extension and internal rotation to achieve
reduction. Reduction must be confirmed on the AP and lateral images. -
Guidelines for acceptable reduction: On
the AP view, valgus or anatomic alignment is seen; on the lateral view,
maintain anteversion while avoiding any posterior translation of the
fracture surfaces. -
Posterior comminution must be assessed.
-
-
Internal fixation
-
Multiple screw fixation: This is the most
accepted method of fixation. Threads should cross the fracture site to
allow for compression. -
Three parallel screws are the usual
number for fixation. Additional screws add no additional stability and
increase the chances of penetrating the joint. The screws should be in
an inverted triangular configuration with one screw adjacent to the
inferior femoral neck and one adjacent to the posterior femoral neck. -
Avoid screw insertion distal to the
lesser trochanter secondary to a stress riser effect and risk of
subsequent subtrochanteric fracture.
-
-
Sliding-screw sideplate devices: If they
are used, a second pin or screw should be inserted superiorly to
control rotation during screw insertion. -
Prosthetic replacement
-
Hemiarthroplasty:
-
Advantages over open reduction and internal fixation:
-
It may allow faster full weight bearing.
-
It eliminates nonunion, osteonecrosis,
failure of fixation risks (>20% to 30% of cases with open reduction
and internal fixation require secondary surgery).
-
-
Disadvantages:
-
It is a more extensive procedure with greater blood loss.
-
A risk of acetabular erosion exists in active individuals.
-
-
-
Indications for hemiarthroplasty:
-
Comminuted, displaced femoral neck fracture in the elderly
-
Pathologic fracture
-
Poor medical condition
-
Poorer ambulatory status before fracture
-
Neurologic condition (dementia, ataxia, hemiplegia, parkinsonism)
-
-
Contraindications:
-
Active sepsis
-
Active young person
-
Preexisting acetabular disease (e.g., rheumatoid arthritis)
-
-
Bipolar versus Unipolar implants:
-
Bipolar theoretically reduces the risk of acetabular erosion.
-
Bipolar has a lower risk of postoperative dislocation.
-
It is very hard to close reduce a dislocated bipolar prosthesis.
-
Bipolar introduces the risk of polyethylene debris.
-
Over time, the bipolar may lose motion at its inner bearing and functionally become unipolar.
-
Unipolar is a less expensive implant.
-
-
Cement versus noncemented:
-
Better functional results with use of cement
-
Risk of intraoperative hypotension and death with use of cement
-
-
Primary total hip replacement:
-
Recent enthusiasm has been reported with
the use of total hip replacement for acute treatment of displaced
femoral neck fractures. -
Studies have reported better functional results compared with hemiarthroplasty.
-
It eliminates the potential for acetabular erosion.
-
Disadvantages over hemiarthroplasty
include a more extensive surgical procedure, increased implant cost,
and a higher risk of prosthetic dislocation. -
Indications include:
-
Preexisting ipsilateral degenerative disease.
-
Active elderly individual with a displaced femoral neck fracture.
-
Preexisting ipsilateral acetabular metastatic disease.
-
P.328 -
-
P.327
COMPLICATIONS
-
Nonunion: This is usually apparent by 12
months as groin or buttock pain, pain on hip extension, or pain with
weight bearing. It may complicate up to 5% of nondisplaced fractures
and up to 25% of displaced fractures. Elderly individuals presenting
with nonunion may be adequately treated with arthroplasty, whereas
younger patients may benefit from cancellous bone grafting, proximal
femoral osteotomy, or muscle pedicle graft. -
Osteonecrosis: This may present as groin,
buttock or proximal thigh pain; it complicates up to 10% of
nondisplaced fractures and up to 27% of displaced fractures. Not all
cases develop evidence of radiographic collapse. Treatment is guided by
symptoms.-
Early without x-ray changes: Protected weight bearing or possible core decompression.
-
Late with x-ray changes: Elderly
individuals may be treated with arthroplasty, whereas younger patients
may be treated with osteotomy, arthrodesis, or arthroplasty.
-
-
Fixation failure: This is usually related
to osteoporotic bone or technical problems (malreduction, poor implant
insertion). It may be treated with attempted repeat open reduction and
internal fixation or prosthetic replacement. -
Prominent hardware may occur secondary to fracture collapse and screw backout.
