EXTENSOR TENDON INJURIES: ACUTE REPAIR AND LATE RECONSTRUCTION
III – THE HAND > Conditions of Tendons > CHAPTER 49 – EXTENSOR
TENDON INJURIES: ACUTE REPAIR AND LATE RECONSTRUCTION
Buffalo School of Medicine and Biomedical Sciences, State University of
New York; Millard Fillmore Health System, Buffalo, New York, 14209.
machinery of much refinement and tissues of great delicacy and
specialization” (8). The extensor mechanism is
a prime example of the “machinery” Bunnell was describing. Because of
its subcutaneous vulnerability, it is one of the most frequently
injured structures in the hand.
extensor mechanism, among them Albinus, who presented the first
detailed structural description in 1734 (46).
Reconstructive surgeons who attempt surgical correction of hand
dysfunction resulting from extensor tendon injury or imbalance quickly
gain respect for the structure.
the diagnosis of most extensor lesions (acute and chronic) is
relatively simple. Likewise, the surgical exercise of tendon suture is
not as technically demanding as it is for flexor tendons, because the
extensors are primarily extrasynovial. The thin nature of the extensors
within the digits, however, as well as the intimate proximity of the
extensor mechanism to periosteum and bone (to which it readily adheres)
and the influence of the digital extensors on the critical function of
the interphalangeal joints (49,58), all contribute to potentially poor functional results following surgical treatment of extensor tendon injuries (19,20,22,23,25,36,45,51,74).
lack of or excess of extension in either joint reciprocally affects the
other. The swan-neck or boutonnière positions are the classic examples
of this interphalangeal reciprocity (see Fig. 49.10).
The entire extensor mechanism, the total digital deformity, and the
lack of motion or presence of abnormal motion at each joint must be
considered in planning reconstruction (13).
Eaton has aptly described the extensor mechanism as a “sleeping giant
which is not appreciated until it becomes disorderly or out of balance.
When out of control it can create great disturbances” (17).
 |
|
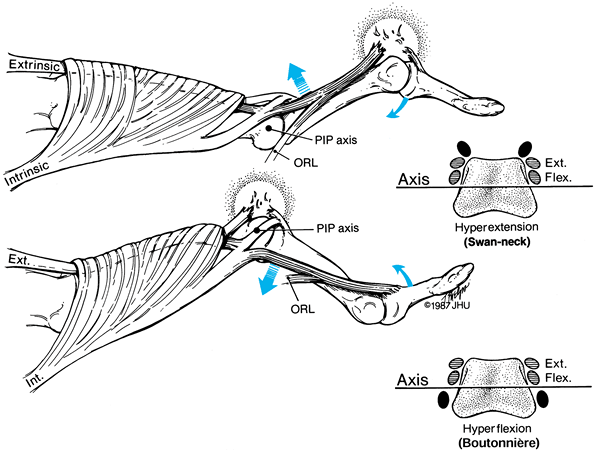
Figure 49.10.
The dorsopalmar translation of the conjoined lateral bands is demonstrated in the two classic reciprocal digital deformities: swan-neck (top) and boutonnière (bottom). The insets are transaxial representations of the condyles of the proximal phalanx, showing the normal positions of the conjoined lateral bands in extension and flexion of the PIP joint. The abnormal positions of the conjoined lateral bands in each deformity are represented in black. |
be more difficult than reconstructing a flexor system. A surgeon
contemplating such a restorative attempt must approach the problem with
complete understanding and great care. Failure to comprehend the
diverse and complex structure’s functional anatomy and to appreciate
the need for proper dressing and appropriate rehabilitation may
contribute to poor results in extensor reconstruction, regardless of
the anatomic level or the mechanism of injury (22).
procedures but rather a description of principles and concepts useful
for devising appropriate management for each case. The primary focus of
the chapter is the finger extensor mechanism; the thumb extensor system
and the wrist extensor will be discussed briefly. Table 49.1 lists abbreviations and terminology that will be used.
 |
|
Table 49.1. Abbreviations and Terminology
|
formed by the interlinkage of two separate and neurologically
independent components: tendons of the extrinsic,
radial-nerve-innervated muscle and tendons of the intrinsic,
ulnar/median-nerve-innervated muscles.
 |
|
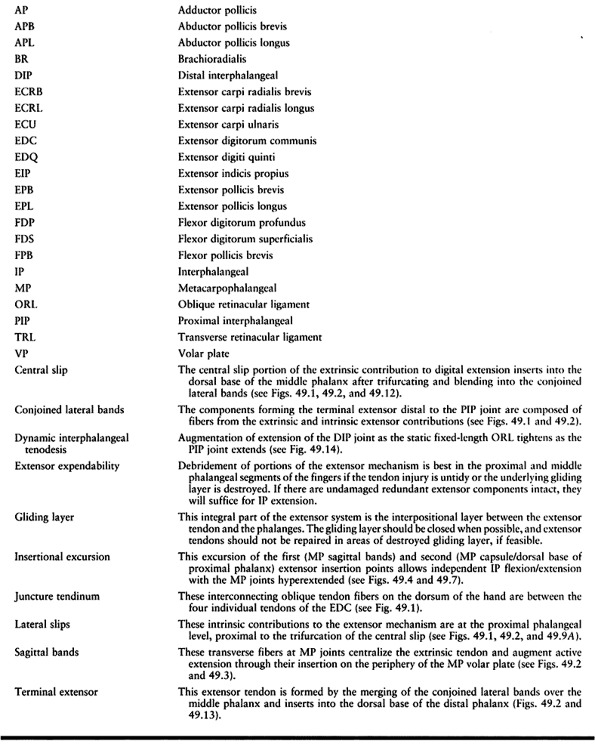
Figure 49.1. The extensor mechanism of the wrist and dorsum of the hand. The six extensor compartments at the wrist contain (1) the abductor pollicis longus (APL) and extensor pollicis brevis (EPB); (2) the extensor carpi radialis longus (ECRL) and brevis (ECRB); (3) the extensor pollicis longus (EPL); (4) the extensor digitorum communis (EDC) II–V and extensor indicis proprius (EIP); (5) the extensor digiti quinti (EDQ); and (6) the extensor carpi ulnaris (ECU).
An important anatomic detail is the presence of a synovial sheath around each tendon unit within each fibro-osseous canal. These sheaths are often involved in rheumatoid disease. |
 |
|
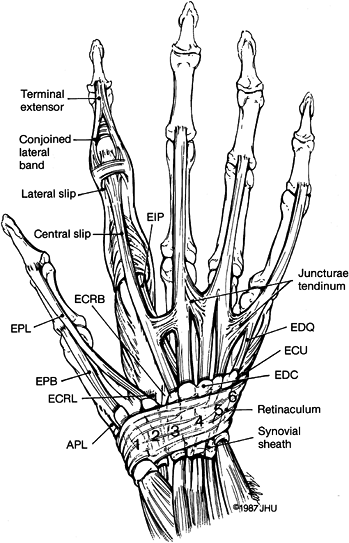
Figure 49.2. Digital extensor mechanism. A: Dorsal view. B: Lateral view.
|
to the extensor mechanism, and their fingers of action, are the
extensor digiti communis (EDC) (all fingers), the extensor indicis
propius (EIP) (index), and the extensor digiti quinti (EDQ) (little
finger) (Fig. 49.1). While this arrangement is considered normal, subtle variations in extrinsic extensor tendon anatomy are fairly common (2,15,27,67,77,79,83), especially the presence or absence of a discrete separate EDC tendon to the little finger (60). After passing beneath the extensor retinaculum (69)
(through synovial sheaths within each extensor compartment), the
extrinsic extensor tendons are interconnected by juncturae tendinum on
the dorsum of the hand (66,78,80).
Laceration of individual extrinsic extensor tendons proximal to the
juncturae may be masked by partial metacarpophalangeal (MP) extension
transmitted through the juncturae by the adjacent tendons (15,66,78,80). The juncturae tendinum may act as force vectors in the dynamic stabilization of the MP joints during flexion (1).
 |
|
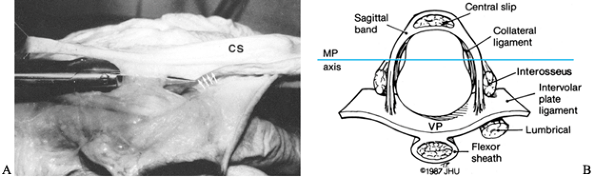
Figure 49.3. A:
Radial sagittal band of the middle finger. There is a natural cleavage plane (through which the scissors penetrate) between the transverse fibers of the sagittal band and the oblique fibers from the lateral slip (arrows) to the central slip (CS). B: Transaxial view at the MP level of the sagittal bands and their insertion into the periphery of the volar plate (VP) and intervolar plate ligament. Note the relationship of the interossei and lumbrical to the MP axis of rotation and intervolar plate ligament. |
 |
|
Figure 49.4.
Hand of a 39-year-old woman with systemic lupus erythematosus, treated for 20 years with oral steroids. All five extensor tendons subluxate with digital flexion. With extension, marked MP hyperextension/dorsal prolapse of the EDC tendons is present due to incompetence of the MP sagittal bands. |
band may allow subluxation of the extensor tendon into the ulnar
intermetacarpal sulcus with MP flexion (36). If
this subluxation is reducible, the physical finding may simply be
painful snapping as the tendon moves to and fro with MP flexion or
extension (Fig. 49.5) (30,33,34,58,59).
If, however, the extensor tendon becomes permanently fixed palmar to
the MP axis of rotation in the ulnar intermetacarpal sulcus (frequently
seen in rheumatoid disease; see Chapter 70), it becomes a strong MP flexor and contributes significantly to ulnar deviation of the fingers (56).
 |
|
Figure 49.5. A: Ulnar subluxation of the EDC of the middle finger (arrow) with finger flexion in an elderly patient with extremely atrophic skin. B: Reduction of the subluxation occurs with finger extension.
|
of the intrinsic and extrinsic contributions to the digital extensor
mechanism, these two separate and distinct systems act as antagonists
at this level. The intrinsics, being palmar to the MP rotational axis,
act as MP flexors; the extrinsics, being dorsal, are MP extensors (Fig. 49.2B).
This paradox of action at the MP joint is a primary factor contributing
to difficulty in understanding the digital extensor mechanism (17,43).
 |
|
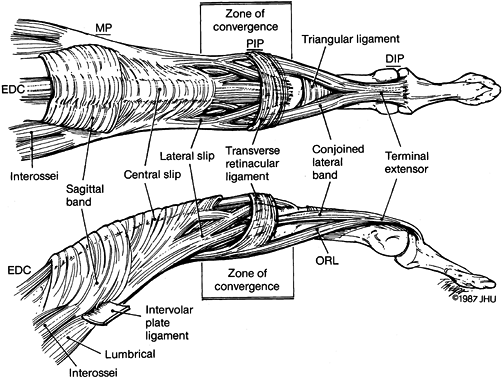
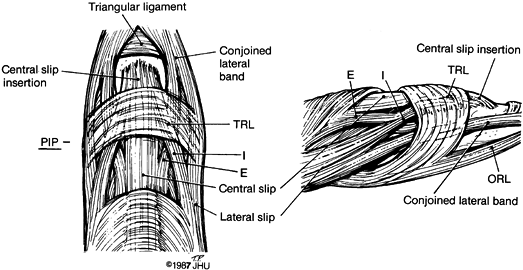
Figure 49.6.
The zone of convergence of the digital extensor mechanism, which begins at about the midportion of the proximal phalanx and ends at the level of the central slip insertion into the dorsal base of the middle phalanx. Proximal to the zone of convergence, the extrinsic and intrinsic components of the extensor mechanism are separate: The central slip is extrinsic, while the lateral slips are intrinsic. Within the zone of convergence there is complete reciprocal crossover of fibers from the central slip and lateral slips. The products of the completed convergence are the central slip insertion and the conjoined lateral bands, both of which have dual muscular activity (intrinsic and extrinsic) for extension of both interphalangeal joints. PIP, proximal interphalangeal joint; TRL, transverse retinacular ligament; ORL, oblique retinacular ligament; E, extrinsic contribution to conjoined lateral bands; I, intrinsic contribution to central slip insertion. |
it is consistently present and represents the second of the insertion
points of the extensor system, the first being the sagittal bands (Fig. 49.3) (75).
These two insertion points are not firmly fixed bony insertions in the
pure sense, as are those at the dorsal base of the middle and distal
phalanges. In fact, these insertions have an excursion approximately
equal to the excursion of the central slip at the PIP joint (Table 49.2) and therefore become taut only when the PIP joint is in full extension (18).
 |
|
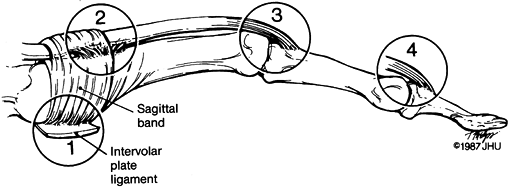
Figure 49.7. Lateral aspect of a finger demonstrating the four insertion points of the extensor mechanism. (1) Insertion through the sagittal bands into the volar plate and intervolar plate ligament. (2)
Extensor insertion into the dorsal MP joint capsule and base of the proximal phalanx. This is a loose or indifferent insertion. (3) Central slip insertion into dorsal base of middle phalanx. (4) Terminal extensor insertion into dorsal base of distal phalanx. |
 |
|
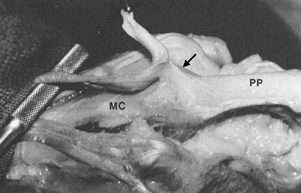
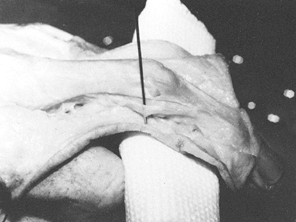
Figure 49.8. Extensor insertion into the dorsal MP capsule and dorsal base of the proximal phalanx (arrow).
This insertion is filmy and loose and has an excursion equal to the extensor amplitude at the PIP joint. This “insertional excursion” allows PIP and DIP flexion while the MP joint is in maximum hyperextension. With PIP extension, however, this insertion becomes taut and assists extension of the proximal phalanx (PP). MC, metacarpal. |
 |
|
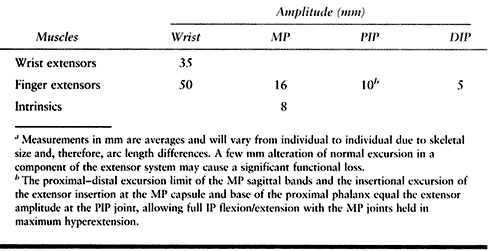
Table 49.2. Extensor Tendon Excursiona
|
finger by maintaining the MP joint in maximum hyperextension and
actively flexing and extending the interphalangeal (IP) joints. A fixed
insertion of the extrinsic extensor at the MP level would obviate the
possibility of this maneuver. If the entire extensor mechanism is
lacerated at the proximal phalangeal level (rarely the case in isolated
laceration of the tendon, because of its broad convex shape, but
frequently seen in dorsal guillotine-type injuries with transection of
the bone), the extensor mechanism retracts only a distance equal to or
less than the available insertional excursion.
mechanism is composed of the interossei (all ulnar-innervated), the
fourth and fifth lumbricals (ulnar-innervated), and the second and
third lumbricals (median-innervated). Along the proximal phalangeal
segment, the fibers of the intrinsic tendons (lateral slips) merge,
winglike, into the central slip (Fig. 49.9A). This configuration explains the necessity of the triangular (wing) excision (Fig. 49.9B) in cases of intrinsic muscle contracture proposed by Littler for complete intrinsic release (41).
A smaller excision or simple lateral slip tenotomy will not completely
eliminate the influence of abnormal intrinsic muscle tension on the
central slip and its attendant limitation of IP flexion.
 |
|
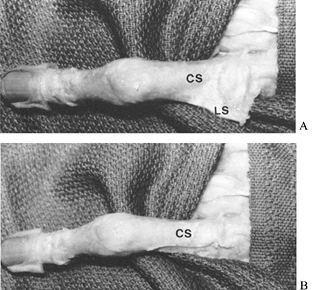
Figure 49.9. A: Anatomic preparation demonstrating winglike configuration of intrinsic contribution to the digital extensor mechanism. B:
The wing excision of Littler that is necessary for complete elimination of intrinsic influence on the digital extensor mechanism. CS, central slip; LS, lateral slip. |
central slip begins its trifurcation. Distal to this level of
trifurcation, there is free exchange of fibers from the central slip to
the lateral slips and from the lateral slips to the central slip (Fig. 49.6).
Distal to the anatomic zone of convergence, the central slip and
conjoined lateral bands are truly a dual extensor mechanism with both
intrinsic and extrinsic contributions, either (or both) of which is
capable of powering active IP extension.
Even Bunnell had held a different functional view of the extensor
mechanism before Fowler’s observations (D. C. Riordan, personal
communication, 1987) (8,46). This duality of extensor motor power at the IP joint (29,54),
plus the mechanical concept of a dynamic IP tenodesis [the oblique
retinacular ligament (ORL)], forms the basis for many procedures
involving redistribution of forces in IP joint extensor dysfunction (42,47,73,76).
(TRL) act to gently maintain the conjoined lateral bands within certain
limits of dorsopalmar excursion (Fig. 49.2B). This dorsopalmar translation of the conjoined lateral
bands (Fig. 49.10) was presented in 1923 by Hauck (31).
Palmar displacement of the conjoined lateral bands occurs normally with
PIP flexion, allowing synchronized distal interphalangeal (DIP) flexion
(62). Smooth, unrestricted DIP flexion depends
on normal PIP flexion, which allows relaxation of the conjoined lateral
bands and oblique retinacular ligament.
flexion while the PIP joint is maintained in extension (usually slight
hypertension). This maneuver is possible only in people with PIP-VP
laxity and normal supple intrinsic muscles. Repeating this “trick” may
result in further VP laxity, stretching of the TRL, allowing further
dorsal migration of the conjoined lateral bands and development of
painful locking of the PIP joint in hyperextension, a dynamic swan-neck
deformity (Fig. 49.10, Fig. 49.11).
 |
|
Figure 49.11. Dynamic swan-neck deformity in a professional musician with PIP volar plate laxity. The conjoined lateral bands (arrows) bowstring dorsally as the transverse retinacular ligament stretches (see Fig. 49.10).
The finger is locked in extension at the PIP joint, causing occupational disability. Successful surgical treatment was flexor superficialis tenodesis of the PIP joint blocking PIP hyperextension; this allowed complete DIP extension. |
the static VP in the normal and abnormal dynamics of extension. Littler
has emphasized the importance of the VP as an adjunct to the dynamic
process of normal digital extension (49). VP
stretching or contracture also contributes to the fixed reciprocal
deformities, including the swan-neck deformity (PIP hyperextension and
DIP flexion) and the boutonnière deformity (PIP flexion and DIP
hyperextension).
The triangular ligament is composed of transverse fibers between the
conjoined lateral bands distal to the central slip insertion and
proximal to the merging of the bands (Fig. 49.6) (37).
 |
|
Figure 49.12. Broad insertion of central slip (CS)
into the dorsal base of the middle phalanx. The glistening, gliding layer is seen covering the dorsal aspect of the proximal phalanx. |
 |
|
Figure 49.13. Bony insertion of the terminal extensor (TE) into the dorsal base of the distal phalanx. The proximal ends of the conjoined lateral bands (arrows) are visible at the PIP joint level.
|
extensor system. The existence and biomechanical significance of the
ORL in normal digits is controversial (53,55,65). Weitbrecht illustrated this structure in 1742 and named it the retinaculum tendini longi (82). The ORL
(Fig. 49.14)
originates palmar to the PIP axis of rotation from the periosteum of
the proximal phalanx and flexor sheath and passes dorsally and distally
to join the terminal extensor tendon (63). Walsh clearly demonstrated the ORL in a prize-winning monograph in 1897 (81).
Landsmeer subjected the ligament to a sophisticated dynamic analysis,
and the soundness of the mechanical basis of a “dynamic interphalangeal
tenodesis” concept has induced procedures designed to augment DIP
extension based on active PIP extension (38,39 and 40,42,73).
ORL tightness may also contribute to pathologic conditions such as
fixed DIP hyperextension in the boutonnière deformity and DIP extension
contracture in digital Dupuytren’s disease (see Chapter 62).
 |
|
Figure 49.14.
The oblique retinacular ligament, elevated by the probe, originates along the proximal phalangeal periosteum and flexor sheath, passes volar to the PIP axis of rotation, and joins the terminal extensor tendon. The principle of “dynamic interphalangeal tenodesis” is based on the biomechanical fact that a structure of fixed length extending from the proximal phalanx to the distal phalanx, palmar to the PIP axis, and dorsal to the DIP axis will relax with PIP flexion and tighten with PIP extension. |
elusive, but functional understanding requires only time and
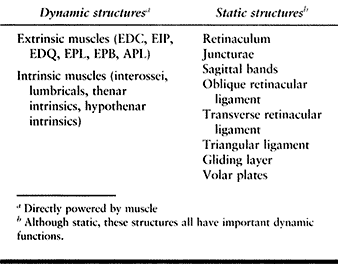
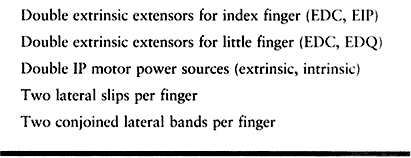
assimilation of many small bits of information. The complete mechanism (Table 49.3)—extrinsic
and intrinsic motors, merging tendons, dynamic and static retaining
ligaments, and other contributing components—when functioning normally
has been described as a “fugue of motion” (J. W. Littler, personal
communication, 1987).
 |
|
Table 49.3. Components of the Digital Extensor System
|
dorsal base and into the fascia of the thenar intrinsic muscles
provides extension and abduction of the first metacarpal (Fig. 49.1). The multiple slips of this muscle–tendon unit make it very useful in reconstructive procedures at the base of the thumb (70).
the dorsoradial base of the proximal phalanx and the extensor pollicis
longus (EPL) into the dorsal base of the distal phalanx (Fig. 49.1).
These two muscle–tendon units exert extensor influence on multiple
joints: the EPB on the trapeziometacarpal joint (extension/abduction)
and MP joint (extension); and the EPL on the trapeziometacarpal
joint (extension/abduction), MP joint (extension), and IP joint (extension).
(APB), flexor pollicis brevis (FPB), and adductor pollicis (AP)]
contribute to IP extension through the extensor hood at the MP joint
and frequently confuse the inexperienced examiner in cases of suspected
EPL laceration (48). The intact thenar
intrinsics will extend the IP joint to a near-neutral position, but the
diagnosis of EPL rupture or laceration is obvious if the entire thumb
ray is compared with that of the uninjured thumb.
in flexion) at the site of extensor muscle tendon action is the simple
sign of complete extensor functional deficit (43).
An MP drop is seen with extrinsic extensor laceration or rupture, a PIP
drop with complete central slip laceration or rupture, and a DIP drop
(mallet) with terminal extensor tendon laceration or rupture.
extensor compartment (EPB, APL) will present as flexion/adduction of
the first metacarpal and a lag in full extension of the MP joint. The
EPL functions as both MP and IP extensor in this situation. Isolated
laceration of the EPB is rare, and repair of this tendon is optional,
depending on the functional deficit at the MP joint. This lesion is
frequently undiagnosed in the emergency situation because of the
presence of MP extension through the intact EPL. EPL extension of the
MP joint, however, will usually be incomplete when compared with that
of the opposite, uninjured side. The magnitude of the MP extensor lag
secondary to EPB laceration is variable, and this factor determines
whether EPB repair is warranted.
presentation depends on whether the laceration site is proximal or
distal to the MP joint. Proximal to the MP joint, the entire thumb ray
is affected and demonstrates metacarpal adduction, incomplete MP
extension, and IP extension lag (some IP extension remains, by virtue
of intact thumb intrinsics). The EPL retracts significantly when
lacerated proximal to the MP extensor hood, and retrieval from the
synovial extensor compartment or the distal forearm may be difficult
and may require a proximal counterincision.
joint is simpler, easily diagnosed by consideration of the injury
location and loss of IP hyperextension. The tendon cannot retract more
than a few millimeters because of its attachment to the MP extensor
hood. It should be repaired and treated as a sharply lacerated terminal
extensor tendon of a finger (discussed later).
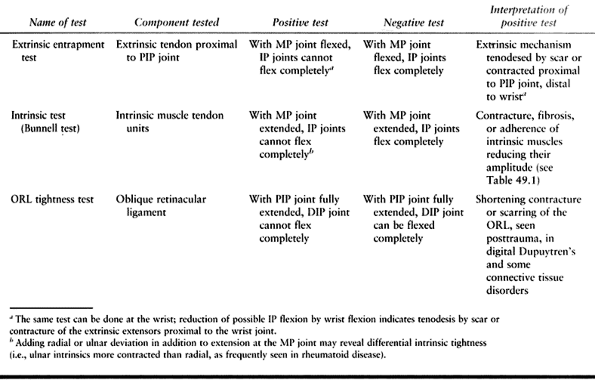
restriction of gliding (tenodesis) of the extrinsics or
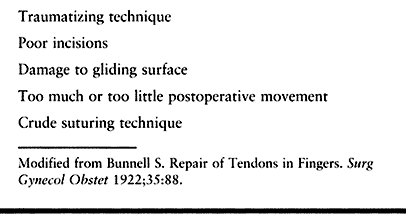
contracture/fibrosis of the intrinsic components (Table 49.4).
The level of extrinsic tenodesis is frequently made obvious by scars.
Intrinsic contracture and contracture of the ORL, however, cannot be
appreciated without the use of clinical tests (43).
 |
|
Table 49.4. Clinical Tests for Tightness or Entrapment of Extensor Mechanism Components
|
 |
|
Table 49.5. Reasons for Poor Results after Extensor Tendon Surgery
|
mechanism and the phalanges is important. This layer is often described
as periosteum, and indeed the deep portion of the layer is phalangeal
periosteum. The superficial cellular components of the gliding layer,
however, are more areolar in nature and cannot be distinguished from
paratenon. Absence of the gliding layer makes adherence to bone much
more likely. Repair of a cleanly lacerated gliding layer, when
possible, improves chances for more normal extensor excursion.
Preserving the gliding layer in
the exposure for reconstruction of phalangeal fractures improves the postoperative range of motion (14,58).
Careful preservation of the gliding layer improves results after other
elective procedures, and this specialized tissue should be considered
an integral part of the extensor mechanism (71).
tendon and gliding layer are unnecessary and should not be used. They
do not facilitate bone reduction but rather create severe extensor
mechanism trauma, resulting in adherence and loss of tendon amplitude.
Incisions preserving the entire extensor mechanism allow access and
reduction of all phalangeal fractures (14,52).
decision making in both acute repairs and late reconstructions. A
common power-saw injury, for instance, results in an untidy laceration
of a lateral slip and portion of the central slip over the proximal
phalangeal segment with destruction of the underlying gliding layer and
abrasion or cortical chipping of the phalanx. Such an injury is best
treated by debridement of the shredded tendon followed by early
initiation of motion.
 |
|
Table 49.6. Extensor System Dualities
|
done when the surgeon does not realize that there is enough undamaged
extensor mechanism to perform IP extension. Adequacy of the mechanism
can be checked easily after digital anesthesia by asking the patient to
straighten the finger. Recognizing the redundancy of the extensor
mechanism, and therefore the expendability of certain elements, should
prevent one of the complications of extensor repairs seen by hand
surgeons—unnecessary suture of partial lacerations resulting in digits
stiffly fixated in extension.
wrist extensor tendons, and the subject deserves mention. The wrist
extensors maintain balanced alignment of the hand and provide
stabilization of the hand during grip. They should be repaired when
possible. Isolated laceration of a wrist extensor is rare, because of
the intimate anatomic arrangement of the extensor complex in the
forearm and wrist. Wrist extensor tendon lacerations are therefore
usually associated with laceration of one or more of the digital
extensors.
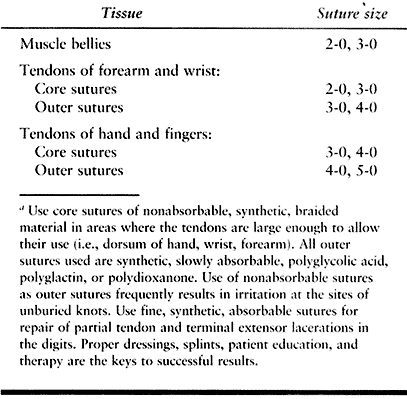
neurovascular injuries is mandatory (stab wounds in the forearm with
small entry wounds may be very misleading), followed by complete
surgical exploration and repair. Dorsal laceration in the proximal
forearm frequently involves branches of the radial nerve. Explore and
repair them if feasible. Muscle bellies of the extensor muscles can be
opposed with nonabsorbable or synthetic absorbable sutures (Table 49.7).
 |
|
Table 49.7. Suture Materials for Extensor Tendon Repaira
|
identifiable, afford the most secure purchase for suture placement.
Synthetic, slowly absorbed sutures are now preferred for peripheral
sutures of muscle and tendon. The details of extensor
repair—positioning after surgery, proper dressings and splints, patient
education, and appropriate type and timing of therapy—are more
important than the type of suture material used (72).
longus (ECRL), extensor carpi radialis brevis (ECRB), EDC, and EDQ have
their origins from the lateral epicondyle, elbow flexion (in addition
to wrist extension) facilitates repair (15).
After surgery, use a long-arm dressing with elbow at 90° flexion, the
forearm in neutral rotation, the wrist extended 45°, and the MP joints
flexed about 15°. Allow the IP joints full, unrestricted motion
throughout treatment of the injury. Allow active motion of the MP
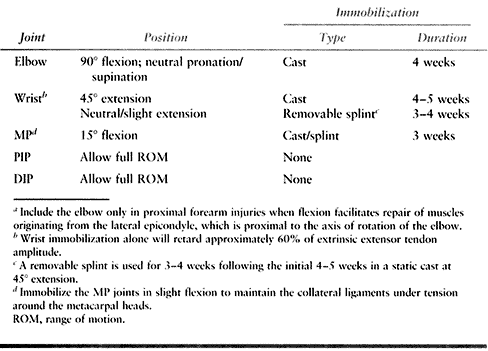
joints at 3 weeks, and of the elbow at 4 weeks (Table 49.8).
At 5 weeks, gently institute wrist motion under the guidance of a hand
therapist. Use a removable splint that maintains the neutral or
slightly extended position between exercise sessions and at night for
an additional 3 to 4 weeks. The development of sufficient tensile
strength to allow application of significant stress across the repair
requires at least 5 weeks (50). However, some motion at the juncture site is beneficial for the return of maximum postoperative tendon excursion.
 |
|
Table 49.8. Postoperative Management of Extensor Tendon Repairs in the Forearm and Wrista
|
that is adequate for the specific repair and some motion that is prompt
enough to achieve early tendon gliding. The surgeon determines the
immobilization method and mobilization sequence. Observe the juncture
directly before wound closure and assess the effects of passive MP and
IP flexion. Because about 60% of the digital extensor amplitude occurs
at the wrist, immobilization of the wrist in extension affords
significant protection for extensor repairs (45).
Graduated institution of range of motion for each of the joints
possibly affected by extensor injuries, rather than prolonged
immobilization of all joints, contributes to improved results (6,21).
by juncturae tendini pull-through. Laceration of the EIP and EDQ
results in loss of independent MP extension of the index or little
finger. Repair all of these tendons (3) using appropriate core and outer sutures (Table 49.7).
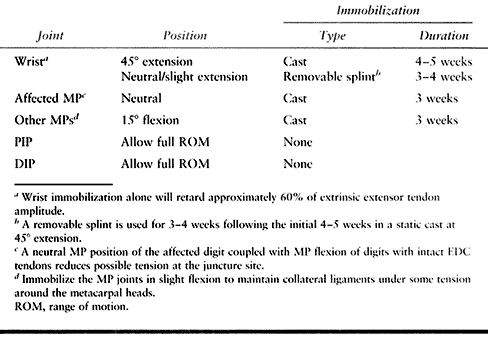
is similar to that for lacerations in the forearm and wrist.
Involvement of the EDC tendons necessitates inclusion of all fingers in
the dressings and splints, but isolated lacerations of the EIP and EDQ
may be treated with immobilization of only the involved digit and the
wrist.
 |
|
Table 49.9. Postoperative Management of Extensor Tendon Repairs in the Dorsum of the Hand
|
joint capsule is prudent. The rationale for wound irrigation,
inspection, open wound treatment, splinting, and delayed repair after 5
to 10 days of antibiotic treatment is to minimize the risk of infection
from human bites, which is increased by primary closure (16). Primary closure, an inappropriate treatment for a human bite, frequently leads to septic destruction of the MP joint (see Chapter 73).
Perform primary closure of lacerations of the extensor tendon and MP
joint only if you are confident of the history, and if the wound
appears compatible with that history. The methods and duration of
immobilization are the same as those described for extensor lacerations
on the dorsum of the hand (Table 49.8).
Repair acute sharp injuries to the radial sagittal band of the MP joint
to prevent ulnar extensor tendon subluxation. Chronic subluxation that
does not respond to MP extension splinting requires surgical treatment.
Release the ulnar sagittal band and, if possible, reef the radial
sagittal band. If adequate substance for repair is not present in the
radial sagittal band, several surgical reconstructions have been
described using juncturae or strips of the tendon secured to soft
tissue on the radial side of the joint to prevent the ulnar subluxation
(10).
digit. Therefore, lacerations over the proximal phalanx are usually
partial and affect only the tendon over the convex portion of the
phalanx. These tendon injuries do not retract significantly, do not
result in loss of extension at the IP joints, and are usually diagnosed
only through direct visual inspection of the wound.
slip repair, especially if the gliding layer is disrupted, is optional.
Treat untidy injuries of a single lateral slip with debridement of the
crushed tendon ends. Initiate motion after 10 days of splinting.
Remember the dualities of the system and the concept of expendability
in crushing and abrading injuries. Fine, synthetic, slowly absorbable
sutures are preferable for repair of the central slip.
ask the patient to actively flex and extend the MP and PIP joints. This
exercise provides some indication of whether early motion will
jeopardize the repair. If no tension on the repair is demonstrated with
active flexion/extension of the MP or PIP joints, consider early
motion. If there is significant tension on the repair, follow the
postoperative regimen for laceration of the extensor tendon at the PIP
joint (Table 49.10).
 |
|
Table 49.10. Postoperative Management of Extensor Tendon Repairs of the PIP Joint (Acute Boutonnière Deformity)
|
joint allows development of the buttonhole (boutonnière) deformity. The
inevitable flexion of the middle phalangeal segment due to unopposed
FDS pull encourages herniation of the proximal phalangeal condyles
through the central slip defect. As the PIP flexion deformity
progresses, the conjoined lateral bands slide palmar to the PIP axis,
maintaining and increasing PIP flexion and tightening the terminal
extensor, which produces DIP hyperextension (Fig. 49.10).
The boutonnière deformity, when allowed to progress, is one of the most
difficult reconstructive challenges to confront a hand surgeon (9,47,61,76).
exploration of all wounds over the PIP dorsum and extensor tendon
repair. If there is a complete PIP extension deficit, the PIP joint
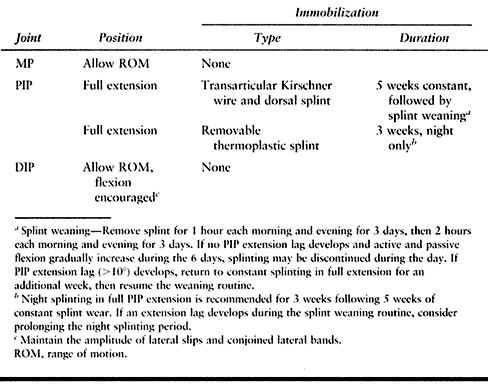
should be maintained in full extension with a transarticular Kirschner
wire before tendon repair. If the PIP extension deficit is not severe
(less than 30° to 40°), tendon repair and external splinting will
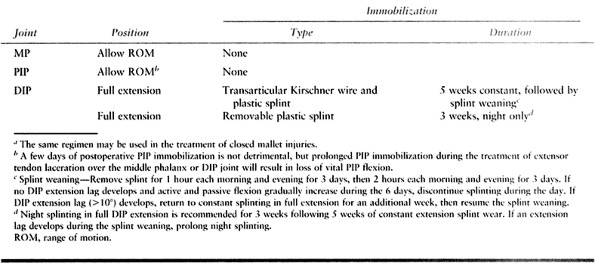
usually suffice. Careful postoperative management (Table 49.10) is necessary for optimum results.
many late-presenting, difficult, fixed boutonnière deformities.
Prevention in these cases is simply based on an awareness of the
potential problem and a high index of suspicion. Immobilize the PIP
joint in extension and observe it with careful follow-up examinations.
Unrestricted finger flexion after blunt trauma to the dorsum of the PIP
region with central slip contusion/rupture may lead to severe
deformity. PIP flexion, therefore, should be instituted gradually
and
only after follow up examinations reveal full active PIP extension. If
there is significant periarticular swelling and pain with attempted
flexion, a prudent assumption is that the injury is a closed
boutonnière deformity until proven otherwise; adherence to the regimen
presented in Table 49.10 is indicated.
-
Closed rupture of the terminal extensor tendon
-
Intraarticular avulsion fracture of the
terminal extensor insertion (dorsal base of the distal phalanx) without
palmar DIP subluxation -
Intraarticular avulsion fracture of the
terminal extensor insertion (dorsal base of the distal phalanx) with
palmar DIP subluxation -
Open laceration of the terminal extensor at the middle phalanx or DIP level
-
Dorsal abrasion/degloving-type composite tissue injury with loss of tendon substance
-
Extraarticular fracture at the base of the distal phalanx in adults with marked palmar angulation
-
Transepiphyseal fracture of the distal phalanx in children with marked palmar angulation
it is these that are the basis for discussion of mallet fingers in this
chapter. Fortunately, injuries in the fifth group are relatively rare;
they often require flap or graft coverage (see Chapter 8, Chapter 38)
before extensor tendon reconstruction can be considered. The last two
groups of fractures, because of marked palmar angulation at the
fracture site, are usually associated with nail-root avulsions and are
treated relatively easily (see Chapter 38, Chapter 40).
contact with the distal phalanx (groups 1 through 5) may present with
PIP recurvatum (swan-neck deformity), the magnitude of which depends on
the ability of the PIP VP to resist the increased extensor force
(central slip plus conjoined lateral bands) on the middle phalanx.
In group 2, the area of articular surface on the fracture fragment of
the distal phalanx is not critical, as long as the DIP joint is not
palmarly subluxated (11). Even though anatomic reduction may be impossible in a splint, results are good if joint alignment is maintained (11).
indicates that enough of the DIP collateral ligament insertion is
present on the fracture fragment to allow the unopposed FDP insertion
to palmarly displace the distal phalanx. This circumstance usually does
not occur until 50% or more of the articular surface of the distal
phalanx is present on the fracture fragment (11).
treat the injury surgically with reduction of the DIP joint,
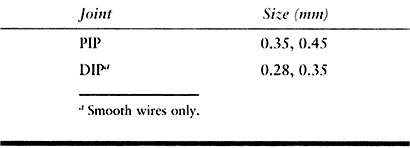
transarticular Kirschner wire fixation (Table 49.11),
and open reduction of the fracture fragment. Methods for fragment
fixation are diverse, and none have a clear advantage. The clear
disadvantage of open treatment of any mallet deformity is loss of DIP
flexion. A certain amount of flexion loss is the cost of accurate joint
and fracture reduction in group 3 mallet deformities and tendon repair
in group 4 mallet deformities. A patient who is advised about this
problem in advance of surgery is usually satisfied with the surgeon’s
efforts, while the unprepared patient is often disappointed.
 |
|
Table 49.11. Transarticular Kirschner Wire Sizesa
|
Place fine, synthetic, absorbable sutures in the tendon after the DIP
joint has been fixed in neutral extension with a transarticular
Kirschner wire.
 |
|
Table
49.12. Postoperative Management of Extensor Tendon Repair Over the Middle Phalanx or at the DIP Joint (Acute Mallet Deformity)a |
many procedures have been described. The following are a few simple
guidelines divided into general anatomic levels for the management of
chronic extensor deficits.
accompanying disruption of wrist extensors and extrinsic digital
extensors. Without wrist extensors, the grasp function of the hand is
disabled. Loss of MP extension eliminates the placement arc of the
fingers, while digital encompassment (IP flexion through FDP/FDS, and
IP extension through intact intrinsic musculature) is maintained (49). Loss of
either wrist extension or MP extension results in marked disability.
Tenodesis and stiffened joints may also contribute to the clinical
presentation.
extension using a technique that provides satisfactory power and
amplitude to meet functional requirements. Normal amplitude is rarely
achieved, but adequate power for extensor function is a reasonable
goal, since normal digital extensor strength is 10% of that of all the
muscles below the elbow, and digital extensor work capacity is less
than one third of that of the digital flexors (5).
Indeed, according to Brand, the FDS and FDP of the middle finger alone
are as strong as the extensors of all the other fingers (5).
extrinsic wrist and digital extensor loss are attempted delayed repair,
interpositional tendon graft, and redistribution of power through
tendon transfer. In general, tendon transfers are the most successful.
Delayed repair and interpositional tendon graft suffer in comparison
because the lacerated muscle–tendon unit is usually compromised by
retraction, adherence, and weakness. There are multiple options for
tendon transfers to restore wrist and MP extension; these methods are
most fully described in treatises dealing with reconstruction following
radial nerve palsy (see Chapter 55) (64).
If composite tissue loss on the dorsum of the hand or forearm
necessitates flap coverage, the use of silicone rods beneath the flap
will facilitate later tendon transfer (61).
metacarpals and phalanges is a relatively common clinical problem,
presenting after extensor tendon injuries with or without fractures.
The gliding layer has been disrupted in these cases and dense adhesions
are present between the bone and extensor tendon. Extensor tenolysis in
the hand or digit with or without use of synthetic interpositional
material (silicone sheets, which eventually require removal) is a
worthy surgical attempt to improve functional range of motion. The
long-term results, however, are highly variable.
some patients and dismally poor in others. Adhesions may extend far
beyond the level of injury; other factors, both objective (e.g.,
stiffened MP or IP joints, loss of muscle amplitude, altered tendon
nutrition) and subjective (e.g., pain perception and tolerance, patient
understanding and motivation), are as important as simply lysing tendon
from bone. The gains in flexion will be more significant than the
reduction in extensor lag, and the necessity for joint capsulotomy will
decrease the overall benefit of extensor tenolysis (12).
If the joints are supple, however, and a well-motivated patient
understands the rigors of maintaining postoperative tendon excursion,
tenolysis is an acceptable surgical option.
interphalangeal encompassment, is most affected by extensor tenodesis
of the central slip over the proximal phalanx (48,49).
Consider the feasibility of separation of the extrinsic and intrinsic
contributions to the extensor mechanism at the proximal phalangeal
level. The extrinsics would then be isolated as MP extensors. Excise
the area of tenodesis to eliminate the extensor tether of the PIP
joint. If the lateral slips are normal and the area of tenodesis is
proximal to the zone of convergence (Fig. 49.6), the intrinsic muscles then become the sole IP extensors. When possible, this solution to the problem can be very successful (44,45).
extensor injury followed by tenodesis over the middle phalanx, even
though DIP flexion is uniformly decreased after such injuries.
Tenolysis at the middle phalangeal level could be considered in a
patient with unique occupational demands (e.g., a professional
musician, requiring maximum DIP range of motion).
not easily accomplished and often frustrates the most experienced hand
surgeons. The fixed or flexible nature of the PIP flexion deformity is
extremely important in operative planning. All reconstructions in late
boutonnière deformities depend on attainment of maximum passive PIP
extension followed by appropriate distribution of the available
extensor power (9,13,45,58,61,68,76).
proposed and used in restoration of swan-neck deformity. If the DIP
joint assumes the extended position when PIP hyperextension is blocked
at neutral or slight flexion, direct treatment simply at limiting PIP
extension to a neutral or slightly flexed position.
of the terminal extensor in patients with lax PIP volar plates. The
increased extensor pull on the middle phalanx (Fig. 49.10)
causes progressive PIP hyperextension. In these cases, surgical
management can be divided into two basic categories: procedures
designed to shift extensor pull from the middle to the distal phalanx,
and procedures using the dynamic interphalangeal tenodesis concept to
limit PIP hyperextension and augment DIP extension.
allows proximal shift of the conjoined lateral bands, increasing DIP
extensor tone. This procedure is simple and is usually effective in
improving DIP extension and reducing PIP hyperextension. DIP extension
will not be complete in most cases, however, and PIP extension lag is a
potential problem following central slip tenotomy (71).
Use this procedure exclusively in swan-neck deformities resulting from
rupture and separation of the terminal extensor tendon.
strong oblique retinacular ligament homologue; they have been reported
to be effective (30,42,43,73). These procedures provide predictable methods for correcting loss of DIP extension and PIP hyperextension.
finger) with no tendency toward PIP hyperextension, direct treatment
toward reconstituting the terminal extensor tendon by excision of
interposed scar and secondary repair, tendon graft, or tendodermadesis (34).
than in the fingers because of the thumb’s recessed and palmar abducted
position, which provides relative protection from longitudinal dorsal
trauma. The thumb of the nondominant glove hand in baseball and
softball is an exception to this rule, but athletes tend to sustain
fractures and ligament injuries rather than extensor tendon deficits
after thumb trauma.
to the deformities of rheumatoid disease or attritional rupture of the
EPL following a distal radial fracture. Reconstruction of the
rheumatoid thumb is discussed in Chapter 70. Tendon transfer, especially EIP, provides the most satisfactory solution to late EPL deficit, if the joints are supple (70). All procedures discussed in this chapter regarding late mallet deformities are applicable, but rarely applied, to the thumb.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
J, Gudera M. The Functional Significance of the Juncturae Tendinae in
Dynamic Stabilization of the Metacarpophalangeal Joints of the Fingers.
J Hand Surg 1980;5:288.
G. Die Ruptur der Dorsal Aponeuroe am ersten Interphalangeal Gelenk,
zugleich eim Beitrag zur Anatomie and Physiologie der Dorsal
Aponeurose. Arch Klin Chir 1923;123:197.
JW. Restoration of the Oblique Retinacular Ligament for Correcting
Hyperextension Deformity of the Proximal Interphalangeal Joint. Groupe
d’Éaatudes de la Main L’Expansion Editeur. 1966;1:39.
GD, Wood MB, Engber WD. Nonoperative Treatment of Traumatic
Dislocations of the Extensor Digitorum Tendons in Patients Without
Rheumatoid Disorders. J Hand Surg 1985;10A:714.
MM, Johnson RK. A Systematic Study of the Oblique Retinacular Ligament
of the Human Finger: Its Structure and Function. J Hand Surg 1977;2:194.
