EQUIPMENT
questions need to be considered when writing the prescription for a
child who will need to use a wheelchair:
-
How long will the child be in the chair each day?
-
Will this be the child’s primary means of mobility?
-
Are there any fixed deformities of the trunk or lower extremities?
-
Does the child have head and trunk control?
-
What are the child’s activities?
-
What are the environmental requirements?
therapist is essential. Include diagnosis, duration of need, and
justification for type of chair, and each component or accessory. Table 22-1 details the many variables of wheelchairs.
-
Type: frame and weight
-
Back
-
□ Height: need to support mid-back
-
□ Fixed/reclining
-
-
Components and accessories
-
□ Foot rests
-
□ Seat/cushion: abduction wedge; air, gel, or foam
-
□ Trochanter pads/hip guides
-
□ Scoliosis pads
-
-
Control straps
-
□ Seat belt
-
□ “H” straps: kyphosis
-
□ Pelvic belt: controls sacral sitting
-
-
Tray
and swing phase of gait, enhance balance, and decrease the
weightbearing load.
-
Crutches
-
□ Axillary
-
□ Forearm (Lofstrand/Canadian)
-
□ Platform
-
-
Canes
-
□ C-handle
-
□ Four-pronged base
-
□ Hemiwalker
-
-
Walkers
-
□ Standard
-
□ Folding: portable
-
□ Reciprocating: articulated, each arm can move independently
-
□ Rolling: wheeled—front, back, both
-
□ Platform: forearm support
-
□ Posterior: positioned behind the patient; promotes erect posture (sometimes called a Kaye walker)
-
challenging given the dynamics of growth, activity level, and variable
motor coordination.
-
Provide components appropriate to the child’s age and level of gross and fine motor function.
-
Function should be a priority over cosmesis.
-
Initial lower limb prosthesis fitted when starting to pull to stand (7 to 9 months)
-
Initial upper limb prosthesis fitted when starting twohanded activities (6 to 9 months)
-
Suspension: belt versus socket
-
Activity level: influences suspension, structural strength needed
-
Structure
|
TABLE 22-1 WHEELCHAIR VARIABLES
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
-
Birth to 6 months: usually not fitted
-
7 to 14 months
-
□ Foot: foam filling in shoe
-
□ Solid tube connecting foot to socket
-
□ Hip joint for sitting if needed
-
□ Omit knee joint
-
-
15 to 36 months
-
□ Consider articulated knee
-
□ Tube extension for growth
-
-
37 to 72 months: add solid ankle cushion heel (SACH) foot or articulated knee
-
7 to 12 years
-
□ Consider hydraulic polycentric knee
-
□ Depends on height and weight and muscle control
-
-
12 years to adulthood: transition to adult prosthesis
-
Hip disarticulation
-
□ Socket
-
□ Extends to waist
-
□ Enclose contralateral side for suspension
-
□ Single-axis hip joint
-
□ Endoskeletal structure
-
□ Knee locked initially
-
-
-
Transfemoral
-
□ Socket
-
□ Ischial containment variations
-
□ Adducts femur and locks ischial tuberosity
-
-
-
Suspension
-
□ Silesian belt initially
-
□ Silicone socket at 2 to 3 years
-
□ Suction socket at maturity
-
-
Transtibial
-
□ Socket
-
□ Patellar tendon bearing (PTB)
-
□ Supracondylar suprapatellar (SCSP)
-
□ Supracondylar (SC): patella-free
-
-
□ Suspension
-
□ SC cuff
-
□ Silicone suspension liners
-
-
-
Ankle disarticulation (Symes)
-
□ Socket: extends to patellar tendon
-
□ Obturator (medial opening) design
-
□ Silicone bladder prosthesis
-
-
-
Partial foot
-
□ Lange silicone partial foot prosthesis
-
□ Cosmetic foot shell
-
□ Silicone-laminated socket
-
□ Posterior zipper
-
-
-
Prosthetic feet
-
Body powered
-
□ Shoulder movement activates terminal device
-
□ Grip strength from rubber bands
-
□ Bulky harness
-
□ Terminal device: hand or hook
-
-
Externally powered
-
□ Switch or myoelectric control
-
□ No harness
-
□ Muscle in limb controls terminal device
-
□ Heavy; difficult to use in children under 2 years
-
□ Grip strength built into system
-
□ Terminal device: hand only
-
|
TABLE 22-2 ACRONYMS USED: ORTHOTIC AND PROSTHETIC PRESCRIPTIONS
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
-
Hands and hooks
-
□ Body or external power
-
□ Voluntary open and closing
-
-
Most common congenital upper extremity deficiency
-
Most ideal for prosthetic fitting
-
□ Initial fit at 6 to 15 months: passive hand
-
□ 15 to 18 months reaching begins: start body- or external-powered prostheses.
-
the elements that must be included in a prescription for an orthosis.
|
TABLE 22-3 JOINT MOTION CONTROL OPTIONS
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
-
Postoperative shoes
-
□ Hard sole (wooden)
-
□ Velcro closure
-
□ Open toe
-
-
Extra-depth shoes
-
□ 1/3-inch longer, ½-inch wider than standard size shoe
-
□ Removable inner sole to accommodate orthosis
-
-
Custom-molded shoes
-
□ Made from cast of foot
-
□ Accommodates severe rigid deformity
-
-
Corrective shoes
-
□ Reverse last open-toe prewalker shoes—forefoot abducted
-
□ Reverse last closed-toe shoes (ambulatory)—forefoot abducted
-
□ Straight last open-toe prewalker shoes—forefoot neutral
-
□ Straight last closed-toe shoes (ambulatory)—forefoot neutral
-
-
Shoe modifications
-
□ Heel
-
□ Thomas heel: additional medial support to control pronation
-
□ Medial wedge: controls midfoot and hindfoot pronation
-
□ Lateral wedge: controls midfoot and hindfoot supination
-
-
□ Sole
-
□ Medial sole wedge: controls forefoot eversion
-
□ Lateral sole wedge: controls forefoot inversion
-
□ Metatarsal bar: decreases pressure on metatarsal heads
-
-
-
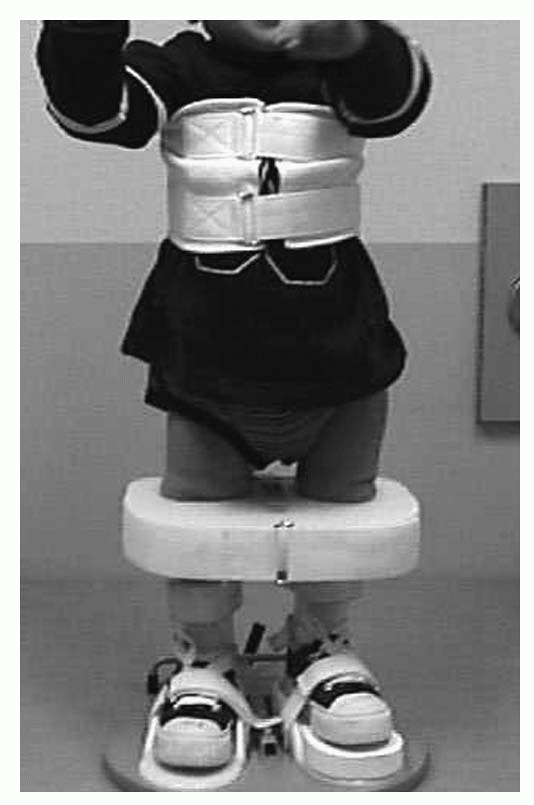
Denis Browne bar (foot abduction bar) (Fig. 22-1)
-
□ Attaches to reverse last or straight last shoes
-
□ Positions feet in adjustable amounts of external rotation
-
□ Able to set separate amounts of external rotation for unilateral applications
-
□ Width of bar should equal width of child’s shoulders
-
-
Date
-
Institution or office or origination
-
Patient’s name, age, gender, address, telephone number
-
Diagnosis: status post is not sufficient; condition for which the surgery was done is also required
-
Description of the orthosis and orthotic goal
-
Acronym for orthosis and description of the motion control of each joint
-
If shoes to be attached to or fit over the orthosis, include modifications
-
Justification for orthosis (letter of medical necessity)
-
Inclusion of office note may be sufficient
 |
|
Figure 22-1 Denis Browne bar (attached to reverse-last shoes)
|
-
Accommodative
-
□ Soft materials
-
□ Custom molded or off-the-shelf (OTS)
-
-
Semi-rigid
-
□ Multidensity layered materials
-
□ Custom molded or OTS
-
-
Corrective
-
□ Rigid materials
-
□ Used for flexible deformities
-
□ Custom molded or OTS
-
-
Medial wedge: controls pronation and heel valgus
-
Lateral wedge: controls supination and heel varus
-
Longitudinal arch support: controls pronation and heel valgus
-
Metatarsal pad: pressure relieves metatarsal head, placed proximal to metatarsal heads
-
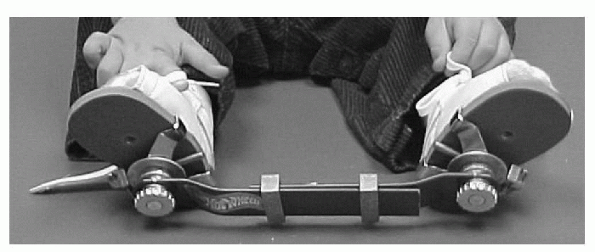
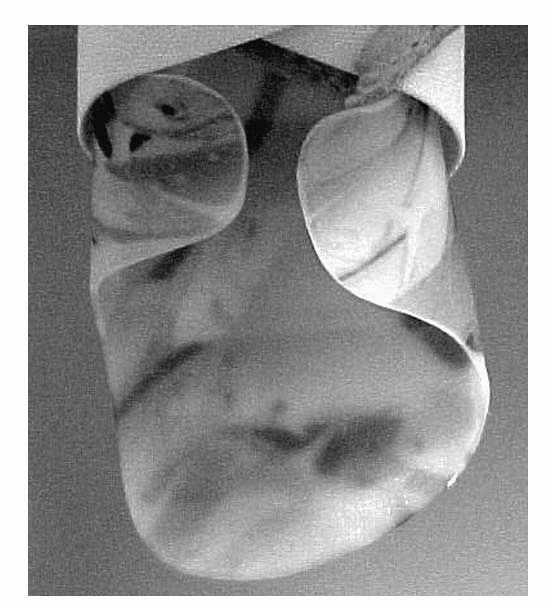
Plastic molded insert named for origin of development (UCBL)
-
Controls flexible hindfoot deformity
-
Accommodates rigid deformity and prevents progression of deformity
-
Extended medial wall to control forefoot adduction
-
Extended lateral wall to control forefoot abduction
 |
|
Figure 22-2 University of California, Berkeley, Laboratory (UCBL) orthosis.
|
-
Canvas orthosis with lace-up anterior support and medial and lateral corrective straps to control inversion, eversion, or both
-
Fits in athletic shoe
-
Restricts inversion and eversion (coronal plane motion)
-
Allows free dorsiflexion and plantarflexion (sagittal plane motion)
-
Fits in athletic shoe
-
Prefabricated ankle immobilizer
-
Immobilizes ankle but allows knee flexion
-
Smallest size: accommodates 6-inch foot length
-
Molded or prefabricated plastic orthosis that extends above malleoli
-
Allows limited plantarflexion and dorsiflexion, restricts inversion and eversion
-
Controls pronation and supination, forefoot motion
-
AFOs can be custom molded or fit from prefabricated design components.
-
Solid ankle (Fig. 22-4): restricts sagittal and coronal plane motion
-
Articulated ankle
-
□ Provides controlled motion at the ankle
-
□ Limited or assisted motion (plantarflexion and dorsiflexion)
-
□ Dorsiflexion stop: check strap or pin in anterior channel of metal joint
-
□ Plantarflexion stop: plastic stop or pin in posterior channel of metal joint
-
□ Dorsiflexion assist: assist joint or spring in metal joint
-
□ Plantarflexion assist: assist joint or spring in metal joint
-
□ Free motion: free dorsiflexion and plantarflexion with restricted subtalar motion
-
-
Dorsiflexion assist
-
□ Nonarticulated
-
□ Posterior leaf spring design
-
□ Plastic trimmed posterior to malleoli
-
□ Low-profile design
-
□ Restricts plantarflexion and allows limited dorsiflexion
-
-
□ Articulated (Fig. 22-5)
-
□ Jointed with dorsiflexion spring assist
-
□ Limits inversion and eversion
-
□ Resists plantarflexion but allows range of motion
-
□ Allows free assisted dorsiflexion
-
-
-
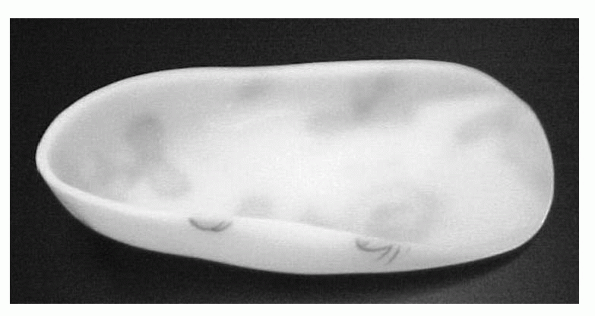
Patellar tendon bearing (Fig. 22-6)
-
□ Modifications done to positive cast to lessen weight on lower extremity
-
□ May include solid or articulated ankle
-
-
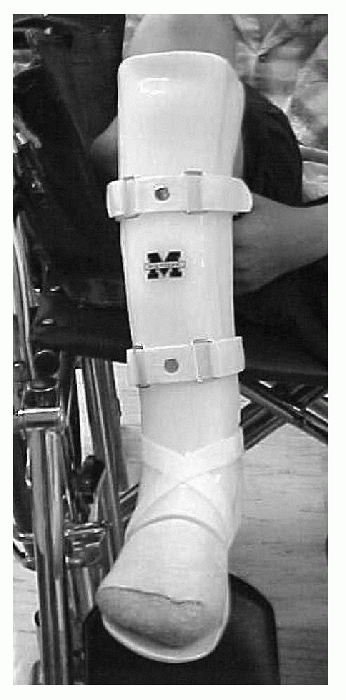
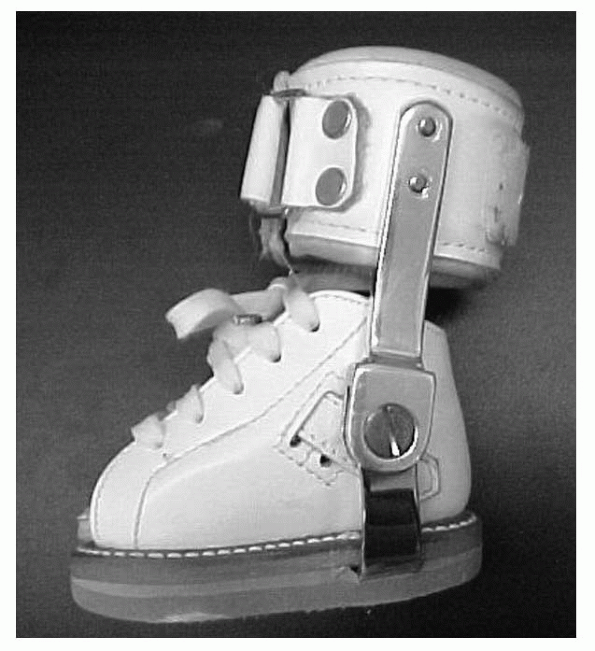
Conventional metal (Fig. 22-7)
-
□ Can be rigidly attached to shoe with metal stirrup
-
□ Can be fit inside shoe with plastic insert attached to metal stirrup
-
□ Double upright: increased stability and rigidity, heavier person, more adjustability
-
□ Single upright: smaller lever arm (shorter leg), less rigidity
-
□ Single-action adjustable joint (SAAJ): dorsiflexion assist or stop
-
□ Double-action adjustable joint (DAAJ): dorsiflexion and plantarflexion assist and stop
-
-
Extended medial wall to control forefoot adduction
-
Extended lateral wall to control forefoot abduction (Fig. 22-8)
-
Toe sulcus length footplate to allow metatarsal phalangeal (MTP) extension
-
Full-length footplate to protect toes and allow for growth
-
Tone-reducing footplate to apply contact and stimulation to decrease hypertonicity or spasticity
-
Total contact: includes anterior shell (clamshell design)
-
Sustentacular tali or longitudinal arch pads to control pronation
-
Eversion and inversion control straps
-
Lateral flanges to control supination and inversion
-
Medial flanges to control pronation and eversion
 |
|
Figure 22-3 Supramalleolar orthosis.
|
 |
|
Figure 22-4 Solid ankle-foot orthosis.
|
 |
|
Figure 22-5 Articulated ankle-foot orthosis.
|
 |
|
Figure 22-6 Patellar tendon-bearing orthosis.
|
 |
|
Figure 22-7 Conventional metal ankle-foot orthosis.
|
 |
|
Figure 22-8 Extended lateral wall-forefoot abduction control.
|
prefabricated components based on a series of measurements. Support is
provided to the knee, ankle, and foot. Parameters for control needed at
each joint must be provided on the prescription.
-
Foot control options
-
□ Full-length footplate
-
□ Sulcus-length footplate
-
□ Tone-reducing footplate
-
□ See additional foot orthosis prescription criteria based on individual control requirements (described earlier).
-
-
Ankle control options
-
Solid ankle
-
Articulated ankle
-
□ Dorsiflexion or plantarflexion assist
-
□ Dorsiflexion or plantarflexion stop
-
□ Free motion
-
-
Conventional metal
-
See additional AFO prescription criteria based on individual control requirements (described earlier)
-
-
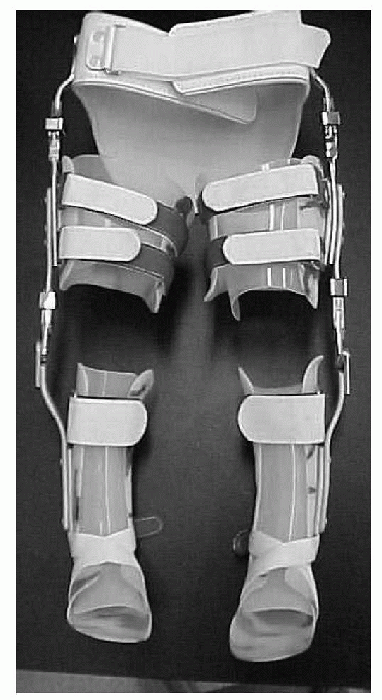
Knee control options
-
Drop lock
-
Engaged locks in full extension
-
Disengaged allows free flexion
-
-
Adjustable extension
-
Allows knee to lock in position other than full extension
-
Combined with drop lock will allow full flexion when lock disengaged
-
-
Posterior offset: allows extension movement to prevent knee flexion (buckling) without need for manual drop lock
-
Bail lock
-
Locks in full extension
-
Releases into flexion with lever located behind the knee
-
-
Static progressive
-
Allows incremental increases in range of motion
-
No motion, locks at position set, used for stretching or contracture management
-
-
Single upright (Fig. 22-9) or double upright (Fig. 22-10)
P.246 -
 |
|
Figure 22-9 Single metal upright ankle-foot orthosis.
|
and foot. They are generally custom molded but can be assembled from
measurements using prefabricated components. Parameters for control
required or range of motion to be limited/allowed must be specified on
the completed prescription for each joint included. They may be
unilateral or bilateral.
 |
|
Figure 22-10 Double metal upright knee-ankle-foot orthosis.
|
 |
|
Figure 22-11 Hip-knee-ankle-foot orthosis.
|
-
For foot, ankle, and knee options, see previous section on knee-ankle-foot orthosis.
-
Hip control options
-
□ Drop locks
-
□ Lock in full extension
-
□ Free flexion when unlocked
-
-
□ Adjustable extension
-
□ Lock in set amount of flexion or extension
-
□ Used with drop lock generally
-
-
□ External and internal rotation control: twister cable from knee to hip joint or offset in metal upright
-
□ Abduction and adduction control: allows range of motion between set parameters or locked at abducted position
-
□ Hip control provided with pelvic band
(molded or prefabricated) or extended thoracic support (molded or
prefabricated) for additional trunk control
-
-
Adds component of thoracic stability to HKAFO
-
Can be used with or without HKAFO system
-
Some models flex at knee, allow swivel walking (limited mobility)
-
Custom molded (Fig. 22-13)
-
□ May include anterior shell for total contact
-
□ Impact protection for postfracture healing
-
□ Allows metacarpal phalangeal (MP) flexion to 90 degrees, should not extend past palmar crease
-
□ Allows elbow flexion, should end distal to bicipital crease
-
□ May include thumb spica
-
-
Prefabricated
-
□ Elastic or neoprene
-
□ Aluminum palmar or dorsal support (aluminum stay)
-
□ Limited motion control and impact protection
-
□ May include thumb spica
-
 |
|
Figure 22-13 Molded wrist-hand orthosis.
|
-
Ventilated neoprene material
-
Measured or used prefabricated
-
Used to maintain wrist in extension or thumb abducted
-
Provides varus and valgus control at elbow
-
Usually custom molded
-
Provides total contact, free or limited range of motion at elbow
-
Sarmiento design for fracture management of distal humeral fractures
-
Fracture management of proximal-third humeral fracture
-
Includes thoracic stability strap to decrease rotation of orthosis
-
Trimmed distally to allow elbow flexion
-
Midshaft humeral fractures: total contact design
-
Can be custom molded or prefabricated (smaller patients custom molded)
-
Controls and limits shoulder motion: abduction and adduction, flexion and extension, internal and external rotation
-
Generally custom molded for small children
-
Prefabricated options for adolescent or larger children
-
Immobilizes arm in shoulder adduction and internal rotation, with elbow flexed
-
Pediatric sizes available with smaller envelopes to free fingers
-
Sling combined with rotation-control thoracic strap
-
Further immobilizes the shoulder and prevents abduction and flexion
 |
|
Figure 22-14 Elbow-wrist-hand orthosis.
|
-
Prevents scapular protraction and encourages scapular retraction
-
Postural correction, clavicle fracture management
-
Can be added to spinal orthosis for kyphosis correction
-
Soft collar
-
□ Support for cervical muscle spasms or minor ligamentous injuries
-
□ Serves simply as kinesthetic reminder, provides soft tissue warmth
-
-
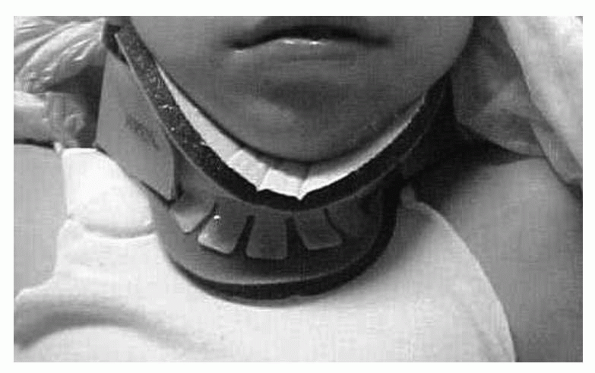
Hard collar
-
□ Limits sagittal motion better than the soft collar
-
□ Support for muscle spasms and atlantoaxial rotary subluxation
-
□ Many types: Philadelphia, Aspen (Fig. 22-15), Miami J
-
-
Increases stability of cervical orthosis alone by extending inferiorly over thoracic region
-
Addresses C1 fractures without subluxation, stable hangman fracture, and flexion injuries of C3-C5
-
Minerva
-
□ Plastic with removable liner
-
□ Good flexion control
-
-
SOMI: sternal occipital mandibular immobilizer
-
□ Can be easily applied in a supine position
-
□ Good flexion control, limited extension control
-
-
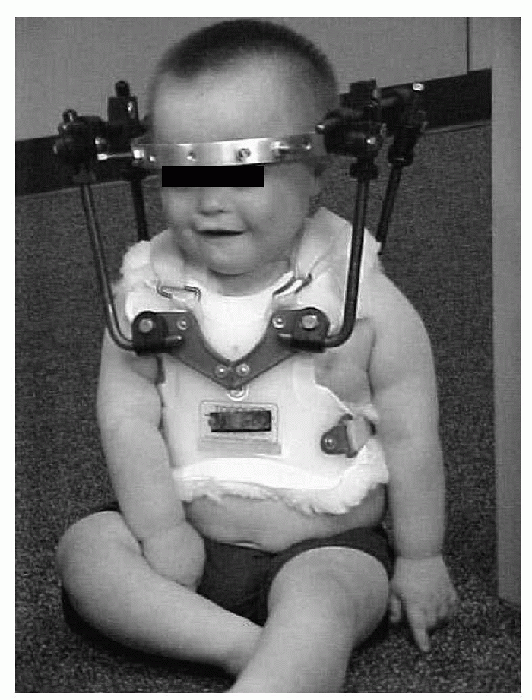
Halo (Fig. 22-16)
-
□ Addresses unstable cervical injuries
-
□ Most rigid control through skeletal fixation
-
□ Excellent flexion, extension, and rotation control
-
-
Addresses acute or chronic low back pain, acute low back and leg pain, sacroiliac disorders
-
Support from L1 to L5
-
Provides varying degrees of abdominal support, motion control, and pain relief
-
Nonoperative and operative types
-
□ Corset or elastic wraparound styles sized (OTS)
-
□ Rigid plastic LSO (custom molded)
-
 |
|
Figure 22-15 Aspen cervical collar.
|
 |
|
Figure 22-16 Halo.
|
congenital malformation, neurologic disease with muscle paralysis,
spondylolisthesis, disc herniation, stenosis
-
Hyperextension TLSO (Jewett, CASH): addresses anterior compression fracture and prevents flexion
-
Knight-Taylor TLSO
-
□ Fabricated from measurements only
-
□ Applicable for obese patients
-
□ Easily accommodates weight fluctuations
-
□ Provides good ventilation
-
-
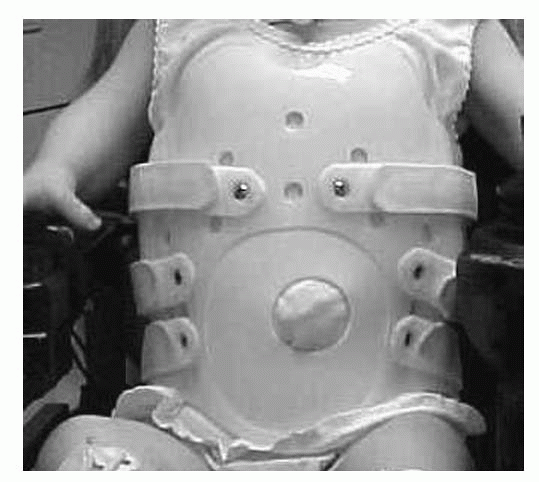
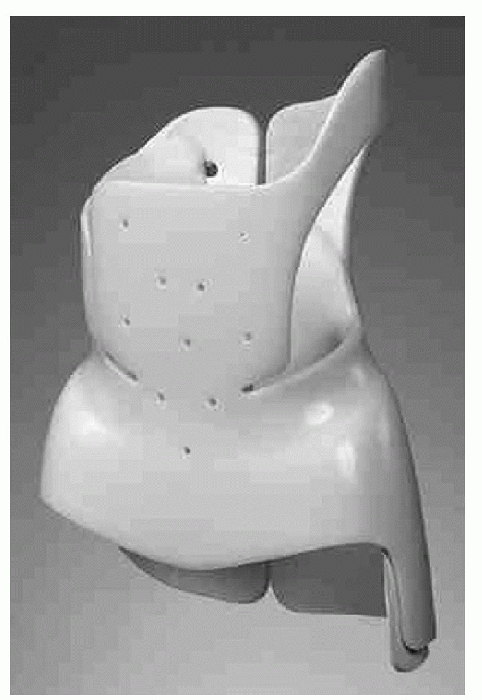
Custom-molded TLSO
-
□ Provides intimate fit and maximum control of flexion, extension, lateral flexion, and rotation
-
□ Can be molded in desired position (Fig. 22-17)
-
-
TLSO with thigh extension: used to control motion at L5-S1 level
-
Scoliosis—TLSO
-
□ Used to manage idiopathic (not neuromuscular) scoliotic curves from 25 to 40 degrees
-
□ Uses specific trim lines to a module with interior pads to apply counteractive forces
-
□ Boston brace: worn up to 23 hours a day (Fig. 22-18)
-
□ Charleston bending brace (overcorrection): molded in bent position to reverse scoliotic curve; nighttime use only
-
□ Wilmington, Lyon, Milwaukee: used to address higher thoracic curves
-
 |
|
Figure 22-17 Molded thoracolumbosacral orthosis.
|
 |
|
Figure 22-18 Scoliosis—thoracolumbosacral orthosis.
|
-
Cervical extension added to TLSO to address multiple spinal injuries
-
Halo, Minerva, or SOMI extension may be added to TLSO depending on stability needed
-
Milwaukee CTLSO
-
□ Addresses kyphosis or high scoliotic curves
-
□ Very low compliance because of metal extensions in cervical region
-
JG, Carter PR, Cummings DB, et al. Limb deficiencies. In: Herring JA,
ed. Tachdjian’s pediatric orthopaedics, 3rd ed. Philadelphia: WB
Saunders, 2002:1745-1810.
JH, Michael JW, eds. Atlas of limb prosthetics: surgical, prosthetic,
and rehabilitation principles, 2nd ed. St. Louis: Mosby-Year Book, 1992.
RT, Giavedoni B, Coulter-O’Berry C. The limb-deficient child. In:
Morrissy RT, Weinstein SL, eds. Pediatric orthopaedics, 5th ed.
Philadelphia: Lippincott Williams & Wilkins, 2001: 1217-1272.