Entrapment Neuropathies of the Upper Extremity
-
Muscle weakness, with or without associated sensory loss
-
Sharp burning pain and paresthesia along the distribution of the affected nerve (Fig. 12.1)
-
Muscle atrophy and vegetative disturbances in advanced cases
 |
|
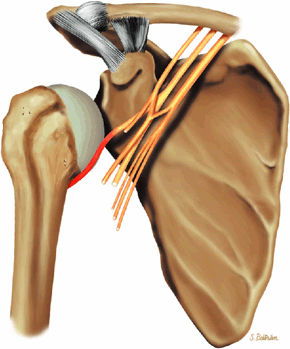
FIGURE 12.1 ● (A) Upper extremity volar sensory innervation. (B) Upper extremity dorsal sensory innervation.
|
-
Confirmation of the presence of nerve compression or entrapment
-
Determination of the presence of mechanical compression (e.g., soft-tissue mass)
-
Determination of the nature, site, and extent of the nerve compression
-
Exclusion of other lesions that can cause similar signs and symptoms (e.g., rotator cuff tear)
-
Neuropraxia is a first-degree nerve injury with temporary loss of nerve conduction.
-
Axonotmesis is a second-degree nerve injury characterized by interruption of the axon with intact connective tissue structures surrounding the axon and Schwann cells.
-
Neurotmesis is complete disruption of the nerve and supporting connective tissue structures.
-
Neuropraxia, or first-degree nerve injury, is the least severe nerve injury with the greatest capability for recovery. There is a temporary loss of nerve conduction secondary to distortion of the myelin near the nodes of Ranvier due to ischemia, mechanical compression, or electrolyte imbalance. Also, there is a segmental block of conduction without Wallerian degeneration. Complete recovery is expected within 2 to 3 months.
-
Axonotmesis, or second-degree nerve injury, implies a more extensive injury due to interruption of the axon with secondary Wallerian degeneration distal to the site of injury. There is, however, preservation of all the supporting connective tissue structures that surround the axon and Schwann cells. The recovery period, ranging from weeks to months, depends on the distance between the site of injury and the end organs. The prognosis is relatively good, dependent on sprouting and re-innervation.
-
Neurotmesis refers to the most severe degree of injury, with no chance of regeneration. It is caused by complete disruption of the nerve and its supporting structures.
-
Third-degree nerve injury, in which the endoneurium is disrupted with intact perineurium and epineurium
-
Fourth-degree nerve injury, in which all neural elements are disrupted except the epineurium
-
Fifth-degree nerve injury, in which the nerve is transected, resulting in complete discontinuity of the nerve
-
STIR or FS PD FSE images are more sensitive than T2 FSE images in the detection of denervated muscle.
-
Exclude focal mass lesions or external compression
-
Identify signs of neuritis/neuropathy
-
Visualize denervation muscle injury
seen as early as 24 hours after complete transection of the sciatic nerve in rats and precede muscle atrophy.9 MR imaging has also been successfully used experimentally as an indicator of nerve healing and re-innervation following transection and repair of the posterior tibial nerve in rats. Changes in T2 relaxation, noted in the first 4 weeks following surgical intervention, completely returned to normal at 6 weeks of follow-up.10
-
Suprascapular nerve syndrome
-
Proximal entrapment associated with supraspinatus and infraspinatus muscle denervation
-
Distal entrapment associated with infraspinatus muscle denervation
-
T1- or PD-weighted images are required to assess fatty atrophy.
-
FS PD FSE images are sensitive to muscle denervation.
-
-
Axillary neuropathy includes quadrilateral space syndrome and posttraumatic injury to the axillary nerve.
-
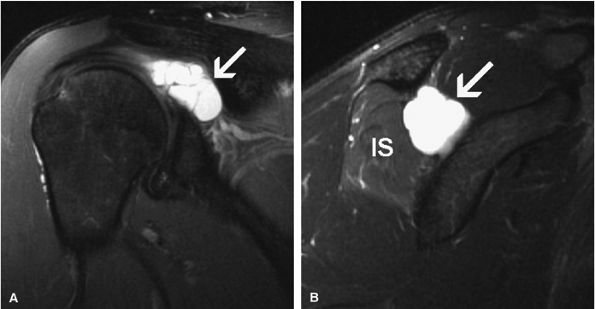
The Parsonage-Turner syndrome is primarily associated with suprascapular nerve disease, although the axillary, radial, or phrenic nerves or the entire brachial plexus may be affected.
the glenoid rim.17 Using statistical analysis, these investigators showed that the axillary nerve travels at a fixed distance of approximately 2.5 mm from the inferior glenohumeral ligament throughout its course. An articular branch of the axillary nerve supplies the shoulder joint capsule.
 |
|
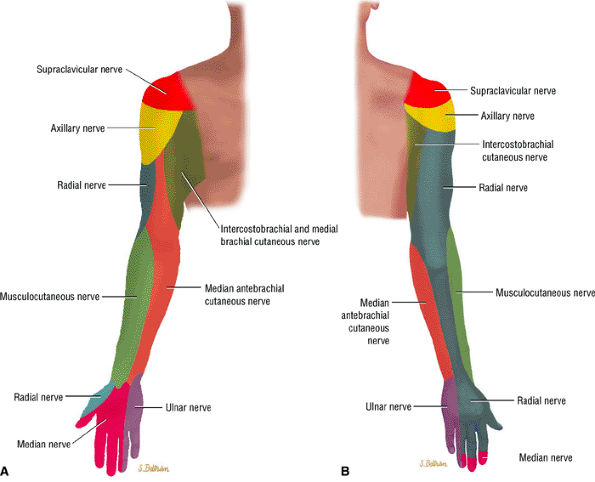
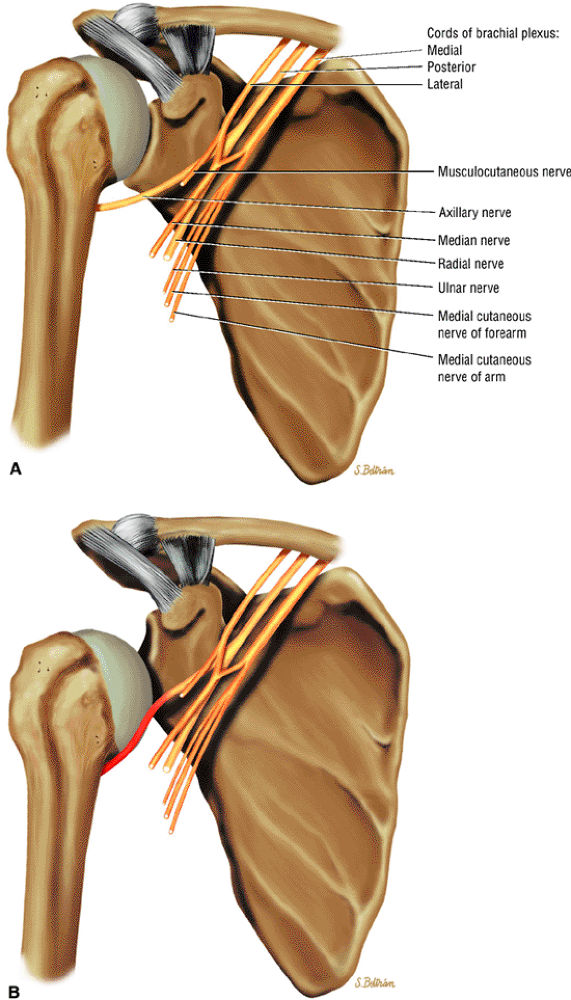
FIGURE 12.2 ● The suprascapular nerve in the shoulder.
|
 |
|
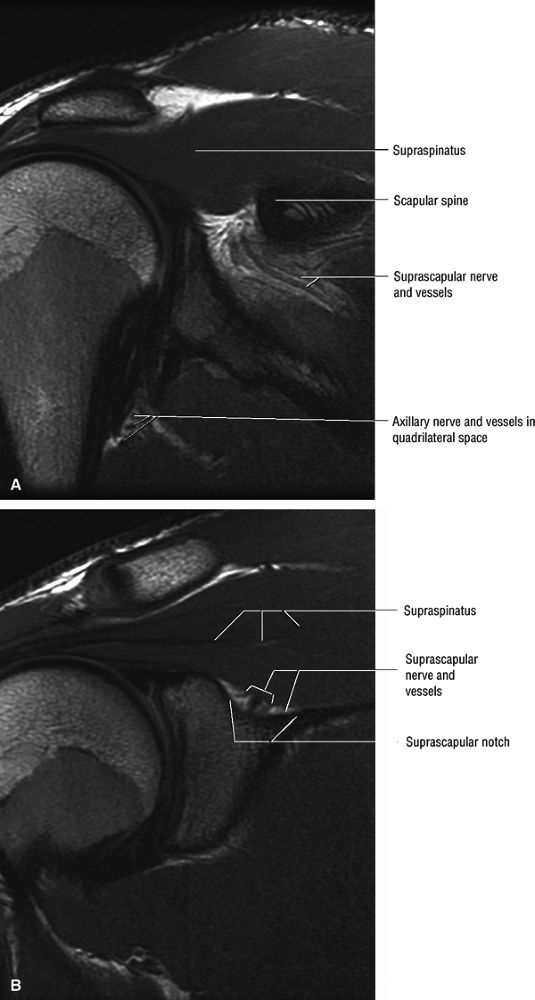
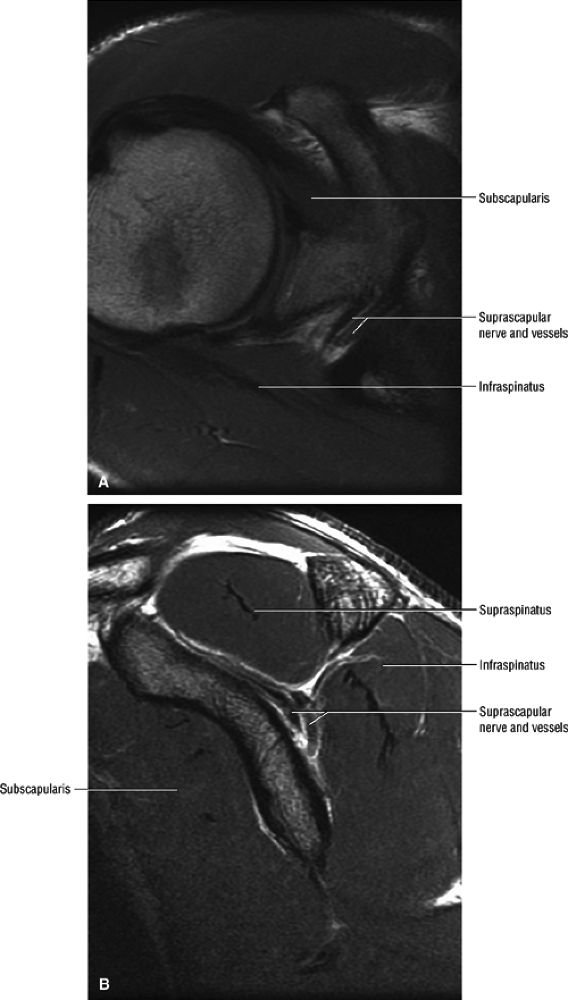
FIGURE 12.3 ● Normal MR anatomy of the suprascapular nerve. (A) Coronal PD-weighed image demonstrates suprascapular nerve and vessels outlined by fat within the spinoglenoid notch. The axillary nerve and vessels within the quadrilateral space are noted. (B) A more anterior coronal PD-weighed image demonstrates the suprascapular nerve and vessels outlined by fat within the suprascapular notch (or incisura).
|
 |
|
FIGURE 12.4 ● Normal MR anatomy of the suprascapular nerve. (A) Axial PD-weighted image demonstrates the supra-scapular nerve as a linear, intermediate-signal structure at the level of the suprascapular incisura. (B) Sagittal PD-weighed image at the level of the spinoglenoid notch demonstrates the supra-scapular nerve and vessels.
|
 |
|
FIGURE 12.5 ● Normal MR anatomy of the axillary nerve. Oblique sagittal PD-weighted image shows the axillary neurovascular bundle traveling between the teres minor muscle and the teres major muscle just medial to the humeral diaphysis in the quadrilateral space.
|
-
Suprascapular ligament stretching from repetitive scapular motion
-
Scapular fractures or other direct trauma
-
Posttraumatic calcification of the suprascapular ligament
-
Adduction and internal rotation caused stretching of the suprascapular nerve underneath the spinoglenoid ligament14
-
Overhead activities (e.g., painters, electricians, volleyball and tennis players), which may result in chronic mechanical stretching and irritation of the suprascapular nerve
-
Rotator cuff injury (Vad et al.,19 using electrodiagnostic testing, studied patients with full-thickness tears of the rotator cuff presenting with shoulder muscle atrophy. They found a relatively high prevalence (28%) of peripheral nerve injury, including suprascapular neuropathy, axillary neuropathy, and cervical radiculopathy.)
-
Iatrogenic injury to the suprascapular nerve during rotator cuff repair
-
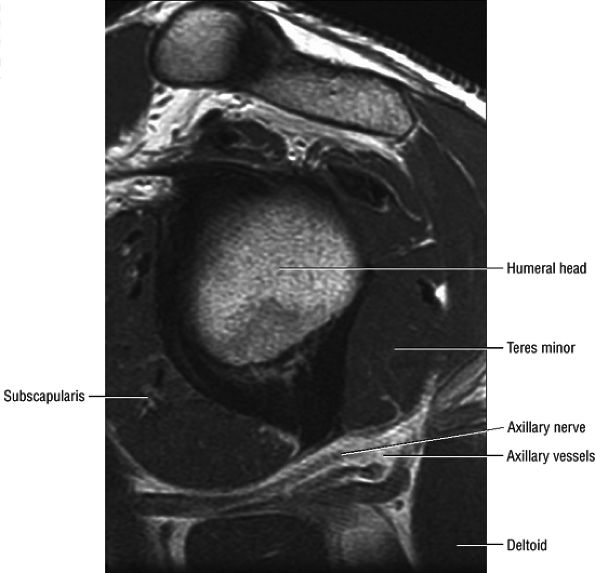
Soft-tissue masses, osseous tumors, and vascular malformations, which can also compress the nerve along its course (Fig. 12.6)
-
Ganglion cysts at the scapular incisura, typically associated with superior and posterior labral tears (Fig. 12.7)
 |
|
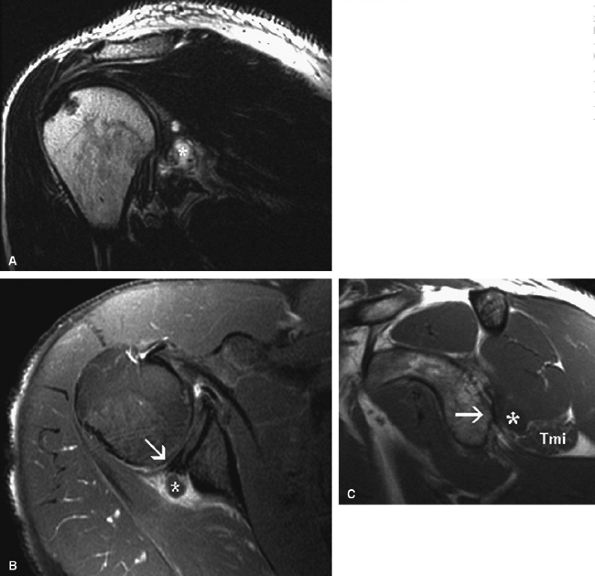
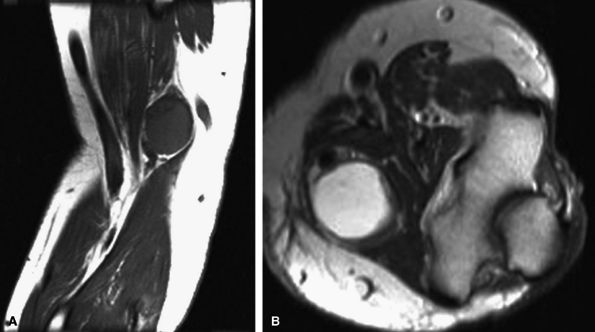
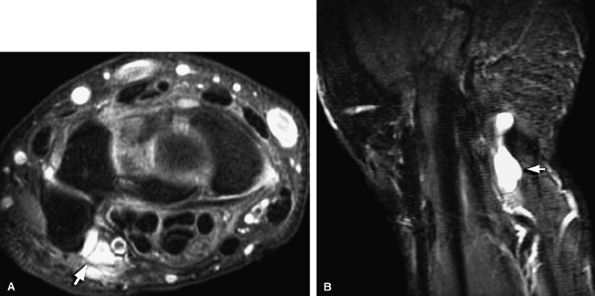
FIGURE 12.6 ● Suprascapular nerve syndrome secondary to a suprascapular varix. Oblique coronal fat-suppressed T2-weighted (A) and axial PD-weighed (B) images demonstrate prominent suprascapular veins (arrow) within the suprascapular incisura and denervation edema of the infraspinatus (IS) muscle.
|
 |
|
FIGURE 12.7 ● Suprascapular nerve syndrome secondary to a ganglion. Oblique coronal (A) and sagittal (B) fat-suppressed T2-weighted images demonstrate a large cystic lesion occupying the suprascapular incisura and spinoglenoid notch in keeping with a ganglion (arrow). Abnormal T2 hyperintensity consistent with denervation edema involving the infraspinatus muscle (IS) is noted.
|
-
Using muscular denervation edema, sensitivity and specificity were shown to be 94.5% and 100%, respectively.
-
Using fatty changes and muscle atrophy (decreased muscle bulk, best seen on sagittal oblique spin-echo T1-weighted images), sensitivity and specificity were 81% and 80%, respectively.
-
Using fatty infiltration of the supraspinatus and/or infraspinatus muscles, sensitivity and specificity were 25% and 96%, respectively.
-
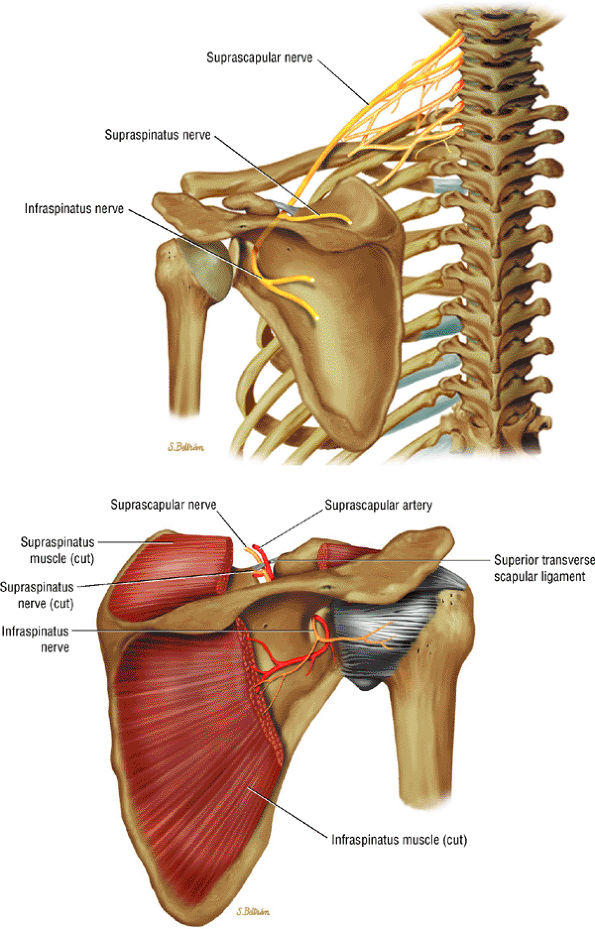
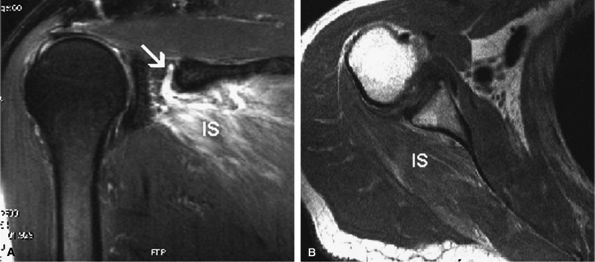
In anterior shoulder dislocation, axillary nerve injury results from traction and compression of the nerve and the subscapularis muscle by the dislocated humeral head (Fig. 12.8). The shoulder is the most common joint dislocation seen in the emergency department and has an overall incidence of 1.7% in the population.28 Nerve injury complicates shoulder dislocation in up to 45% of cases,29 and the axillary nerve is the most commonly involved because of its relatively tethered course through the quadrilateral space.
-
The risk for axillary nerve and brachial plexus injury is greater if the shoulder is not reduced within 12 hours. Although neurologic injury is well known to orthopaedists who treat shoulder dislocation, few reports in the radiologic literature stress the association of teres minor atrophy with prior shoulder dislocation.30,31,32 Axillary nerve injury may develop after manipulative reduction in which traction with rotation or abduction is simultaneously applied.33
-
Posttraumatic injury to the axillary nerve can also be secondary to proximal humeral fractures34 and rarely as a result of a direct blow to the deltoid muscle.
prolongation can be appreciated within 15 days of the injury.36 The following MR findings are helpful in evaluating axillary neuropathy:
-
Denervation muscle edema, not observed as often as fatty infiltration and atrophy
-
Teres minor fatty infiltration and decreased muscle bulk with or without involvement of portions of the deltoid.36 The incidence of atrophy or abnormal signal in the teres minor muscle has been reported to be as low as 0.8%.36
-
Associated abnormal MR findings such as labral tear, rotator cuff tear, subacromial subdeltoid bursitis, and acromioclavicular joint degenerative osteoarthritis
-
The identification of teres minor atrophy in the absence of quadrilateral space lesions should prompt careful evaluation for signs of posttraumatic glenohumeral instability and prior dislocation.30,31
 |
|
FIGURE 12.8 ● The axillary nerve. (A) The axillary nerve is seen coursing within the quadrilateral space in close relationship to the inferior glenoid rim. (B) Traction on the axillary nerve by a dislocated humeral head.
|
 |
|
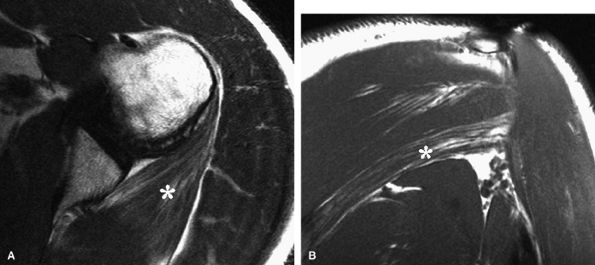
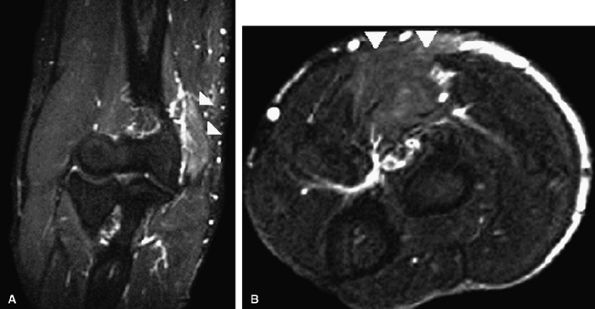
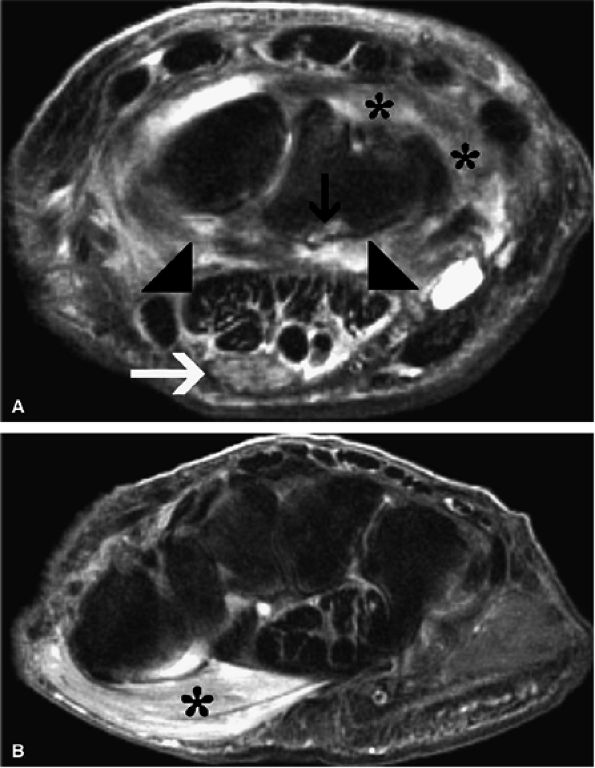
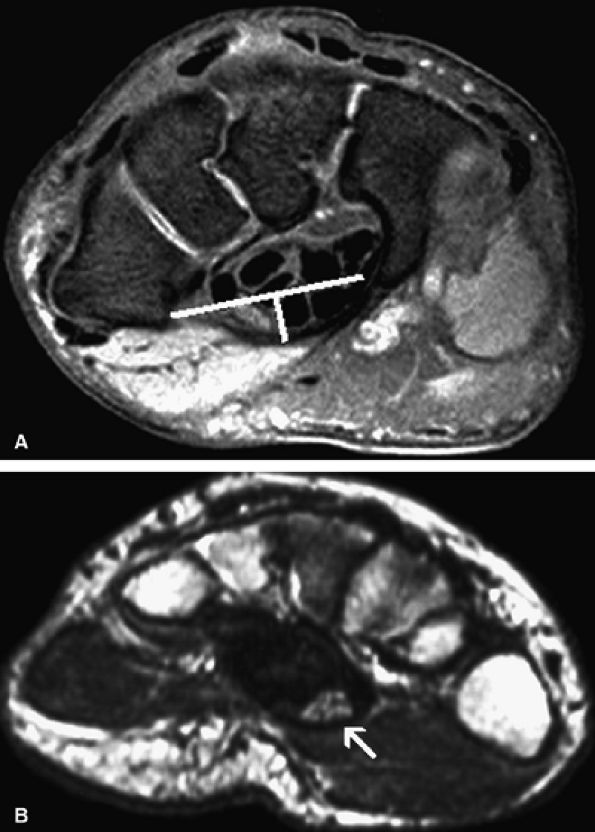
FIGURE 12.9 ● Quadrilateral space syndrome. Axial (A) and oblique coronal (B) PD-weighted images demonstrate selective atrophy and fatty infiltration of the teres minor muscle (asterisk).
|
may be helpful in pain relief and in preventing stretching of the affected muscles. Once the pain subsides, physical therapy is recommended. The overall prognosis is good, with almost 75% of patients experiencing complete recovery within 2 years. However, the period of time for complete recovery is variable, ranging from 6 months to 5 years.
 |
|
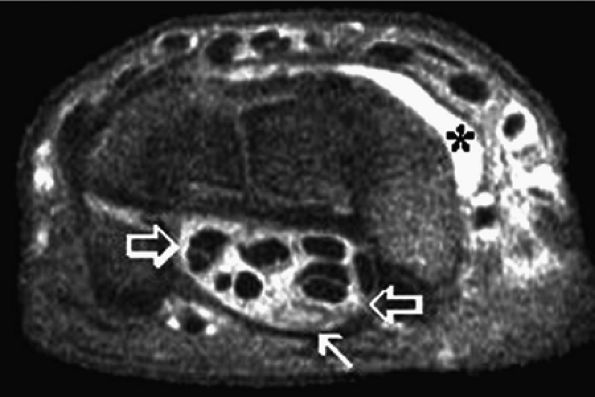
FIGURE 12.10 ● Posttraumatic axillary neuropathy secondary to a paralabral cyst. Oblique coronal fast spin-echo T2-weighted (A) and axial fat-suppressed post-gadolinium T1-weighted (B) images demonstrate a large multiloculated paralabral cyst (asterisk) in association with posterior labral tearing (arrow). (C) Oblique sagittal T1-weighted image shows selective fatty infiltration and atrophy of the teres minor muscle (Tmi) associated with remodeling of the posterior glenoid rim (arrow) and posteroinferior paralabral cyst (asterisk).
|
 |
|
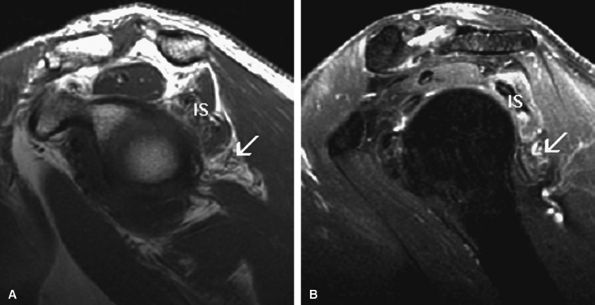
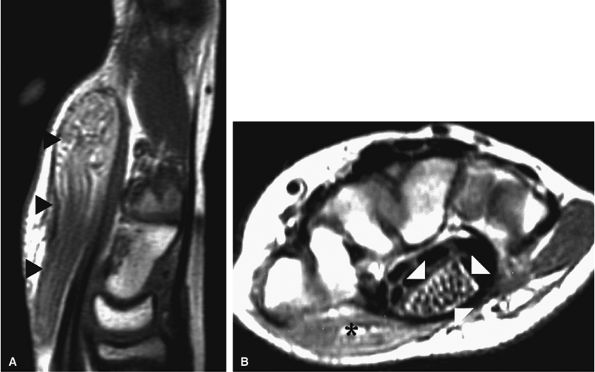
FIGURE 12.11 ● Parsonage-Turner syndrome. Oblique sagittal T1-weighted (A) and fat-suppressed T2-weighted (B) images show denervation edema and atrophy of the infraspinatus (IS) and teres minor (arrow) muscles.
|
-
The cubital tunnel is the most common site of ulnar neuropathy.
-
Ulnar neuropathy also occurs at the arcade of Struthers, the edge of the medial intermuscular septum, the ligament of Struthers, the arcuate ligament, and the deep flexor pronator aponeurosis.
-
The pronator syndrome is the most common cause of median nerve entrapment. It is characterized by numbness in the median nerve distribution occurring with repetitive forearm pronation/supination.
-
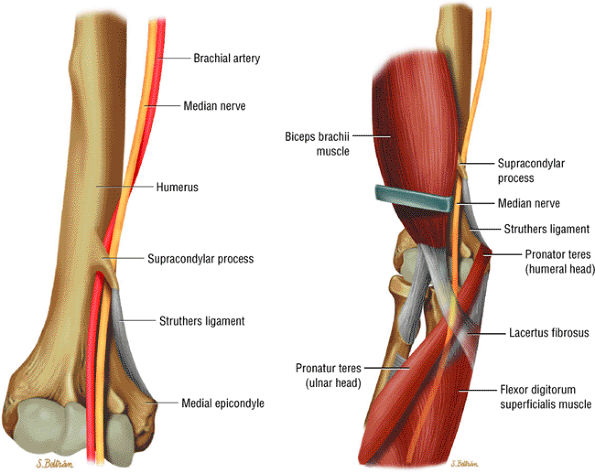
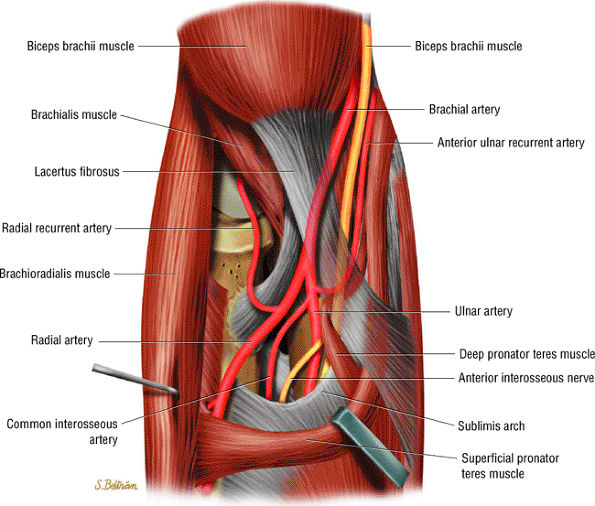
Potential sites of compression in the pronator syndrome include the supracondylar process/ligament of Struthers, the lacertus fibrosus, the pronator teres muscle, and the proximal arch of the flexor digitorum superficialis muscle.
-
The anterior interosseous syndrome affects only the motor branch of the median nerve and is less common than the pronator syndrome.
-
The radial tunnel syndrome involves compression of the posterior interosseous nerve without motor deficit.
-
The posterior interosseous nerve syndrome is a motor neuropathy with the same potential sites of compression as in the radial tunnel syndrome.
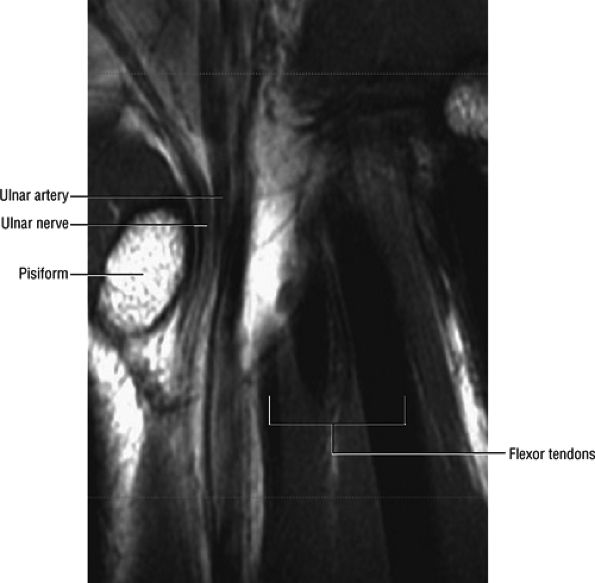
and the flexor digitorum profundus muscles in the forearm. It splits into superficial and deep branches at the wrist.
 |
|
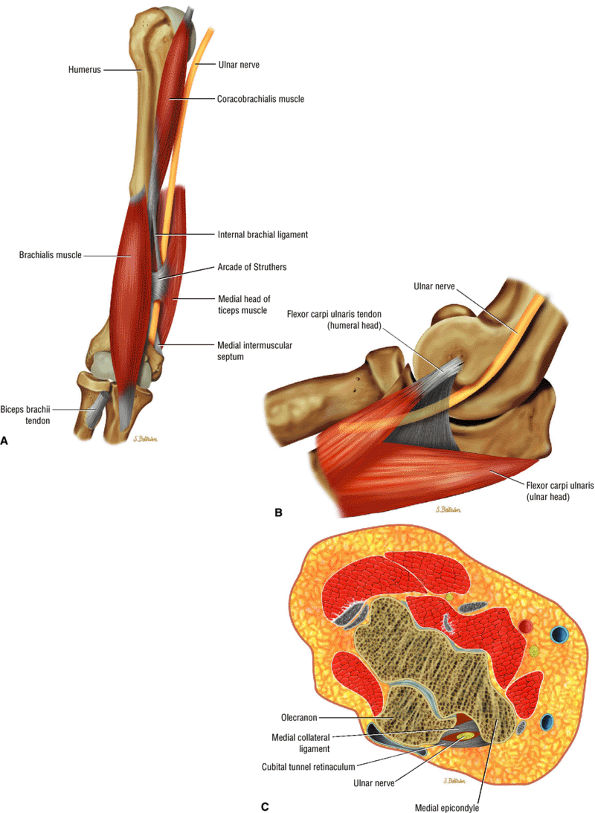
FIGURE 12.12 ● The ulnar nerve: anterior (A), medial (B), and axial (C) views. In the distal arm the ulnar nerve descends within the arcade of Struthers, then runs posterior to the medial epicondyle and deep to the cubital tunnel retinaculum and arcuate ligament within the cubital tunnel before entering the forearm between the two heads of the flexor carpi ulnaris muscle.
|
 |
|
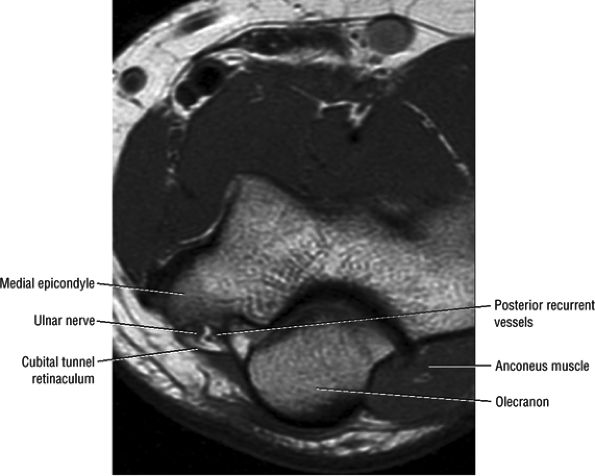
FIGURE 12.13 ● Normal MR anatomy of the ulnar nerve. Axial PD-weighted image demonstrates the ulnar nerve posterior to the medial epicondyle and medial to the posterior recurrent vessels.
|
 |
|
FIGURE 12.14 ● Normal MR anatomy of the ulnar nerve. Axial PD-weighted image depicts the ulnar nerve surrounded by fat as it courses between the ulnar and humeral heads of the flexor carpi ulnaris muscle.
|
-
The elbow joint
-
The flexor carpi ulnaris muscle and the ulnar half of the flexor digitorum profundus to the fourth and fifth fingers
-
The palmaris brevis (the superficial motor branch of the ulnar nerve)
-
The hypothenar muscles, the third and fourth lumbricals, all interossei, the adductor pollicis, the deep head of the flexor pollicis brevis, the flexor digiti minimi, the abductor digiti minimi, and the opponens digiti minimi (the deep motor branch of the ulnar nerve)
-
The medial palm
-
The palmar and distal dorsal skin of the fifth finger
-
The medial half of the fourth finger
(lacertus fibrosus) and the brachialis muscle, traveling deep to the pronator teres as it courses into the forearm (Fig. 12.16). In the elbow region, the median nerve supplies all the superficial muscles of the ventral forearm (the pronator teres, the flexor carpi radialis, the palmaris longus, and the flexor digitorum superficialis) except the flexor carpi ulnaris muscle.
 |
|
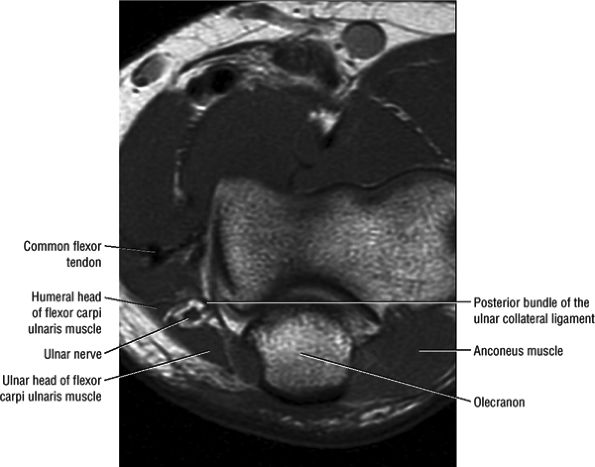
FIGURE 12.15 ● The median nerve. The four potential sites of compression are the supracondylar process and ligament of Struthers; the ulnar and humeral heads of the pronator teres; the lacertus fibrosus; and the fibrous edge of the flexor digitorum superficialis.
|
 |
|
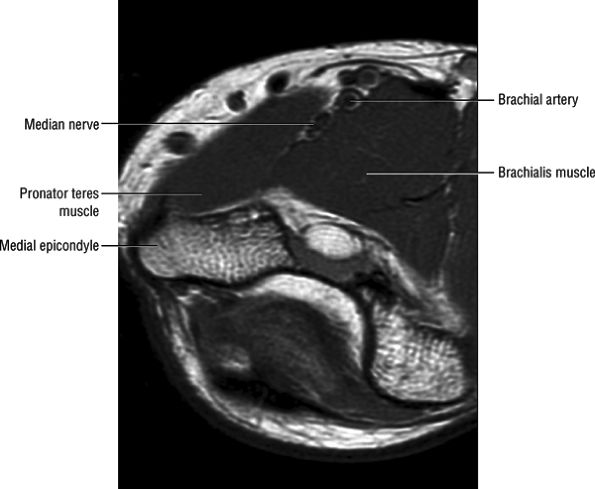
FIGURE 12.16 ● Normal MR anatomy of the median nerve. Axial PD-weighted image demonstrates the median nerve between the pronator and the brachialis muscles.
|
-
A motor branch from the median nerve in the proximal forearm to the ulnar nerve in the middle to distal third of the forearm
-
A motor branch from the anterior interosseous nerve to the ulnar nerve
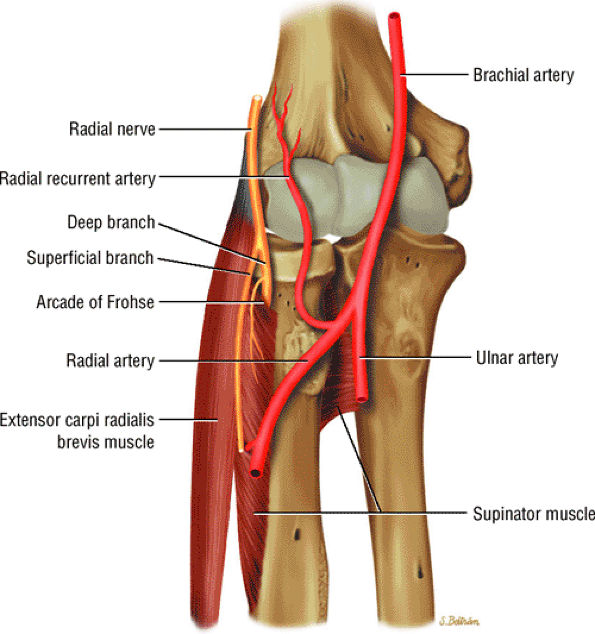
muscles form the anterolateral margin of the tunnel, whereas the brachialis muscle bounds the tunnel medially. In the region of the radiocapitellar joint, the radial nerve divides into the motor branch, the posterior interosseous nerve, and the superficial sensory branch. The superficial sensory branch passes into the forearm deep to the brachioradialis. The posterior interosseous nerve passes into the posterior compartment between the superficial and deep heads of the supinator muscle to supply nine muscles on the extensor aspect of the forearm. The nerve then passes under the arcade of Frohse, the proximal edge of the superficial head of the supinator muscle. Fibrous or tendinous thickening of the arcade has been described in 32% to 65% of the population. The posterior interosseous nerve innervates the supinator, the extensor carpi ulnaris, the extensor digitorum communis, the extensor digiti quinti, the abductor pollicis longus, the extensor indicis proprius, and the extensor pollicis longus and brevis muscles.
 |
|
FIGURE 12.17 ● The radial nerve. The radial nerve splits into the superficial radial nerve and the posterior interosseous nerve at the radiocapitellar joint. The posterior interosseous branch courses between the deep and superficial heads of the supinator muscle.
|
 |
|
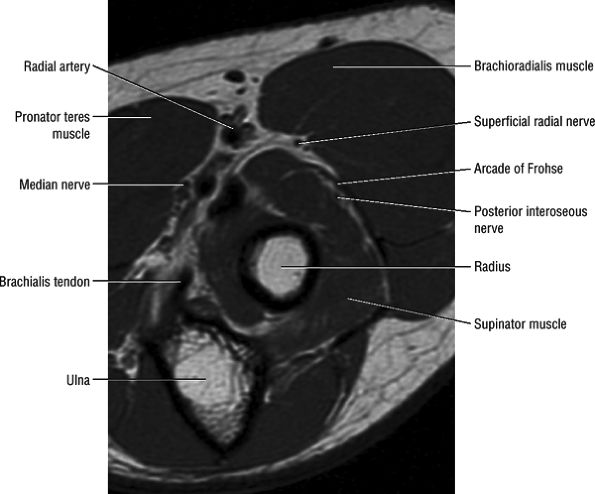
FIGURE 12.18 ● Normal MR anatomy of the radial nerve. Axial PD-weighted image of the proximal forearm shows the posterior interosseous nerve between the arcade of Frohse and the deep head of the supinator muscle.
|
-
The arcade of Struthers
-
The edge of the medial intermuscular septum
-
The ligament of Struthers
-
The thickened arcuate ligament
-
The deep flexor pronator aponeurosis (4 cm distal to the medial epicondyle)
-
Physiologic cubital tunnel syndrome occurs secondary to the normal loss in volume and increase in pressure within the tunnel during elbow flexion. This is the mechanism seen in sleep palsy, when the arm is held in flexion for a prolonged period of time.
-
Acute external compression syndrome typically follows a single episode of blunt trauma to the cubital tunnel. The sensory fibers of the ulnar nerve are located superficially under the arcuate ligament, making them most vulnerable to external compressive forces.
-
Subacute compression syndrome has been described in bed-ridden or wheelchair-bound patients and following surgery. Avoidance of prolonged pronation and flexion of the arm should decrease the risk of cubital tunnel external compression syndrome.
-
Chronic cubital tunnel syndrome may be caused by masses such as tumors, distended bursae, ganglions, hematoma, inflammatory pannus, gouty tophi, loose bodies, osteophytes, and scarring (Figs. 12.19 and 12.20)
-
Callus formation from distal humeral and supracondylar fractures
-
Elbow dislocation
-
Avulsion of the medial epicondylar apophysis (Fig. 12.22)
accentuated by elbow flexion. Congenital absence (Fig. 12.25), laxity or tear of the arcuate ligament, trochlear hypoplasia, and posttraumatic cubitus valgus deformity are all postulated etiologic factors of ulnar nerve instability. Snapping triceps syndrome, dislocation of the medial head of the triceps muscle over the medial epicondyle, has been implicated as an additional cause of ulnar nerve dislocation (Fig. 12.26).59,60
 |
|
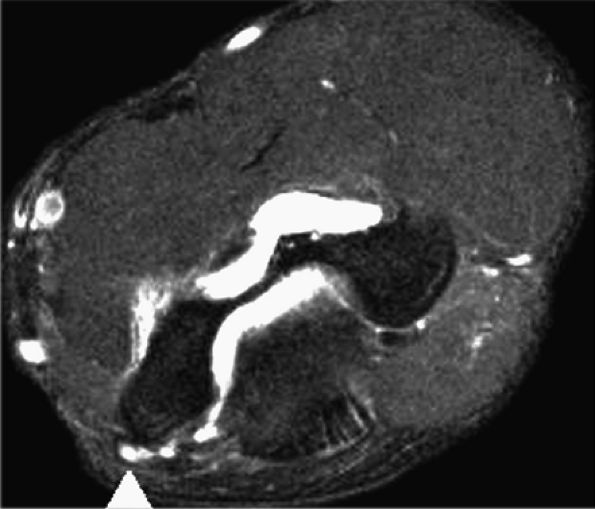
FIGURE 12.19 ● Ulnar neuropathy secondary to compression by hemangioma. An axial post-gadolinium fat-suppressed T1-weighted image shows an avidly enhancing soft-tissue mass encasing (arrowhead) the ulnar nerve (solid arrow) in the medial aspect of the distal arm, consistent with a hemangioma (asterisk). Note invasion of the medial humerus by the mass (open arrow).
|
 |
|
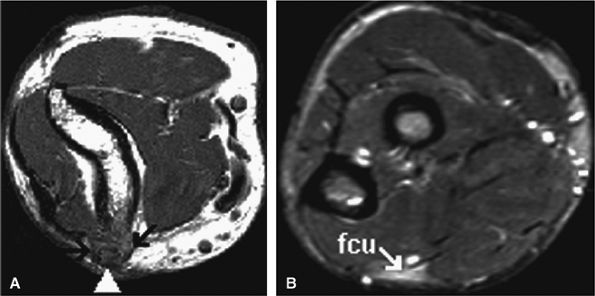
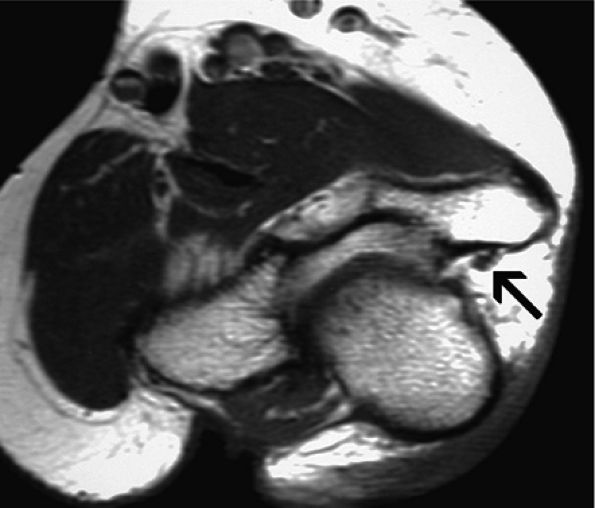
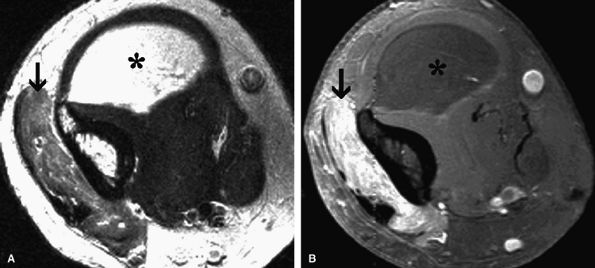
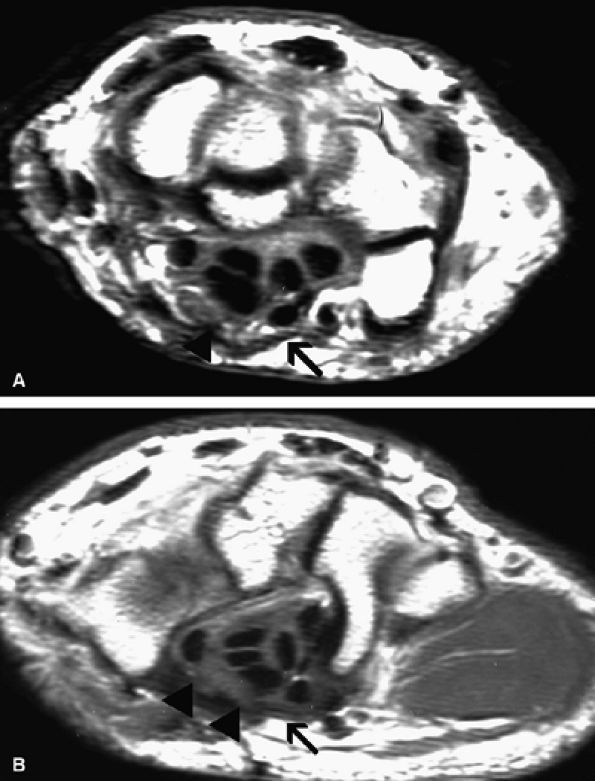
FIGURE 12.20 ● Ulnar neurop-athy secondary to scar. Axial T1-weighted (A) and fat-suppressed T2-weighted (B) images demonstrate encasement of the ulnar nerve (arrowhead) by scar tissue (arrows). Selective denervation edema of the flexor carpi ulnaris (fcu) muscle in the proximal forearm is noted.
|
 |
|
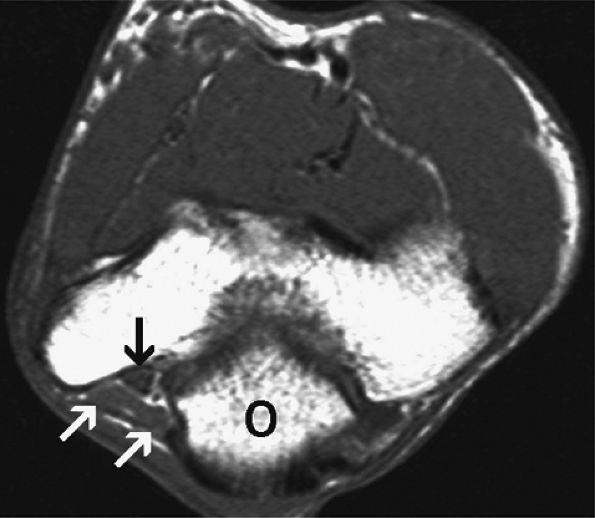
FIGURE 12.21 ● Anconeus epitrochlearis muscle. Axial T1-weighted image demonstrates the accessory muscle (white arrows) effacing the fat within the cubital tunnel. The ulnar nerve (black arrow) is normal. O, olecranon.
|
 |
|
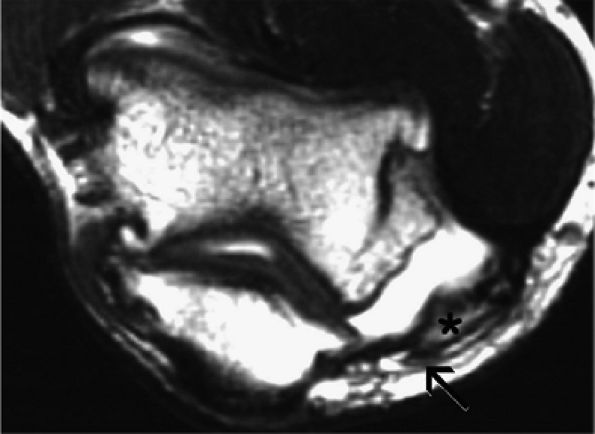
FIGURE 12.22 ● Compressive ulnar neuropathy caused by a displaced fracture fragment. Axial fast spin-echo T2-weighted image shows an old, displaced, non-united avulsion fragment (asterisk) of the medial humeral epicondyle resulting in mass effect and secondary subluxation of the ulnar nerve (arrow).
|
is warranted. For chronic neuropathy associated with muscle weakness, or for neuropathy that does not respond to conservative measures, surgery, including medial epicondylectomy and anterior ulnar nerve transposition, is usually necessary.61
 |
|
FIGURE 12.23 ● Ulnar neuritis. Axial fat-suppressed T2-weighted image shows thickening and increased signal within the ulnar nerve (arrowhead). Note associated edema and partial tear of the common flexor tendon (arrow).
|
 |
|
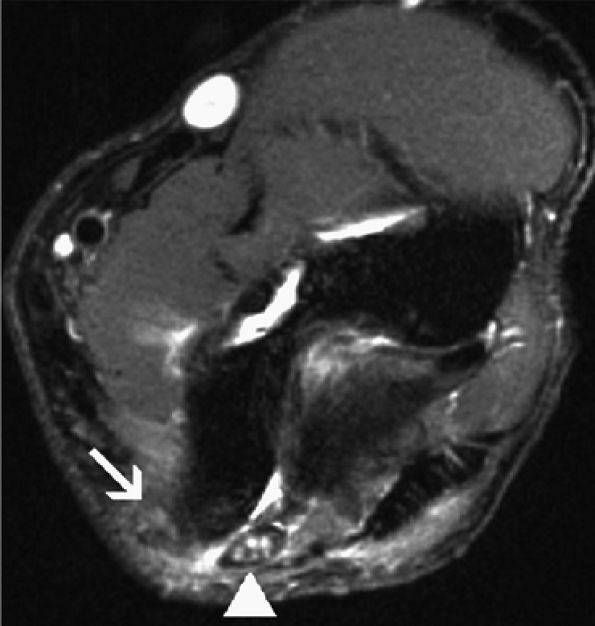
FIGURE 12.24 ● Ulnar nerve subluxation. Axial fat-suppressed T2-weighted image shows an anteriorly subluxed, thickened, and edematous ulnar nerve (arrowhead). The arcuate ligament is absent.
|
 |
|
FIGURE 12.25 ● Absent arcuate ligament. Axial T1-weighted image demonstrates absence of the arcuate ligament incidentally noted in this asymptomatic patient. The ulnar nerve is normal (arrow).
|
 |
|
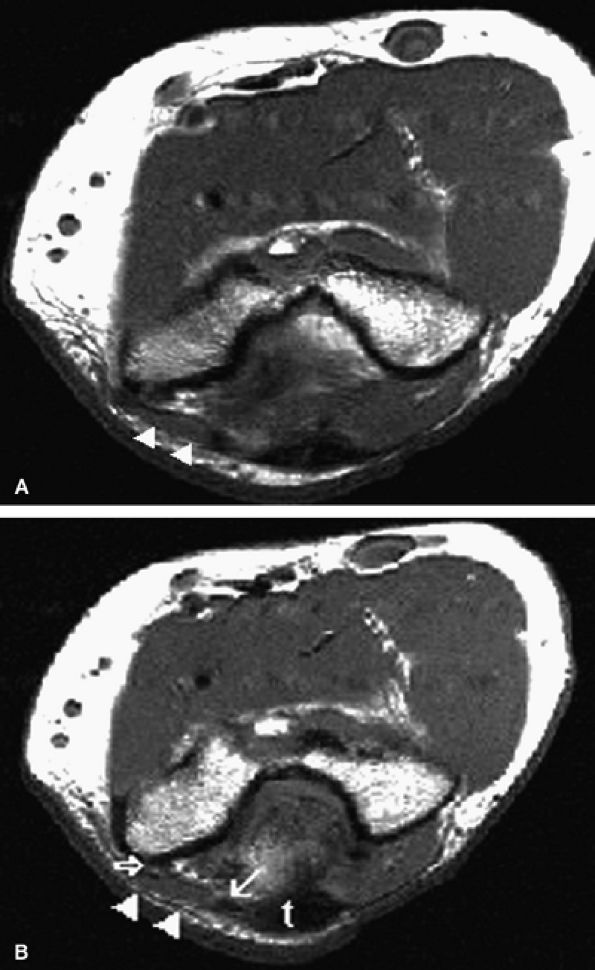
FIGURE 12.26 ● Medial head of triceps. Axial T1-weighed images depict a prominent medial head of triceps muscle (arrowheads) and tendon (arrow) at the level of the cubital tunnel (open arrow). Note blending of the medial head tendon with the main triceps tendon (t) on a more distal image, a feature distinguishing it from the anconeus epitrochlearis muscle.
|
-
Ganglion cysts, soft-tissue tumors (see Fig. 12.19), degenerative spurs, and anomalous muscles such as the anconeus epitrochlearis (see Fig. 12.21) may be responsible for compressive ulnar neuropathy and can be easily depicted on MR images.
-
Selective denervation edema and atrophy of the flexor carpi ulnaris and flexor digitorum profundus muscles, best appreciated on axial forearm images, are additional contributory features in the MR diagnosis of ulnar neuropathy (see Fig. 12.20).62
-
The arcuate ligament should always be evaluated for thickening, tearing, or congenital absence.
-
Subluxation of the ulnar nerve may be seen on standard axial MR images performed with full extension of the elbow (see Fig. 12.24). However, when a history of ulnar nerve subluxation is available, MR imaging in elbow flexion is preferable for eliciting the subluxation.63 MR diagnosis of snapping triceps syndrome also can be enhanced by imaging in elbow flexion.64
-
On MR examinations obtained after anterior ulnar nerve transposition, T2 hyperintensity equalize within the ulnar nerve may persist long after the surgery (Fig. 12.27). Intense increased signal, however, is more likely to reflect persistent neuritis. Ulnar nerve thickening can be seen in the first postoperative year in up to 50% of patients following transposition.65 Tethering of the nerve and engulfing scar can also be identified. Other causes
P.1957
for persistent pain after anterior ulnar nerve transposition include extensive scarring or retearing at the resection site of the pronator–flexor muscle group.
 |
|
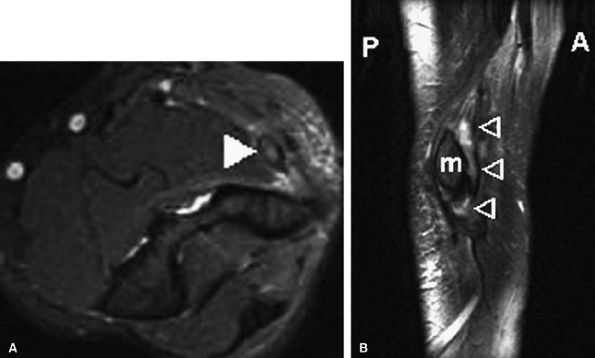
FIGURE 12.27 ● Failed anterior ulnar nerve transposition. Axial post-contrast fat-suppressed T1-weighted image (A) and oblique sagittal fat-suppressed T2-weighted image (B) demonstrate increased signal and thickening of the transferred ulnar nerve (arrowheads). m, medial epicondyle.
|
-
Elbow fractures and dislocations66
-
Accessory muscles such as the Gantzer muscle (the accessory head of the flexor pollicis longus muscle)
-
Soft-tissue masses (Fig. 12.28)
-
Dynamic forces at the elbow
-
Prolonged pressure on the forearm (honeymooner's paralysis refers to median neuropathy secondary to pressure from a lover's head against a partner's forearm)
-
The supracondylar process/ligament of Struthers
-
The lacertus fibrosus
-
The pronator teres muscle
-
The proximal arch of the flexor digitorum superficialis muscle
with supracondylar process syndrome. An unusual musculo-aponeurotic band that originates as the ligament of Struthers but terminates as the brachiofascialis muscle of Wood, resulting in high median nerve entrapment, has recently been described.69
 |
|
FIGURE 12.28 ● Cystic schwannoma of the median nerve. (A) Coronal T1-weighted image demonstrates ovoid mass arising from the median nerve. A comet sign is noted proximally (arrow). (B) Axial fast spin-echo T2-weighted image shows marked homogeneous hyperintensity in keeping with a cystic variant of schwannoma.
|
 |
|
FIGURE 12.29 ● Supracondylar process. Lateral radiograph of the elbow depicts osseous excrescence arising from the anterior aspect of the distal humerus and pointing toward the elbow joint.
|
-
When the ligament of Struthers is the culprit for median nerve compression, a linear low-signal-intensity structure emanating from the supracondylar process can be seen.73
-
The pronator syndrome may lead to signal abnormalities or atrophy in the pronator–flexor muscle group, including the pronator teres, the flexor carpi radialis, the palmaris longus, and the flexor digitorum superficialis muscles (Fig. 12.31).
-
Fatty replacement with atrophy indicates irreversible loss of muscle fibers and is seen with chronic denervation over the course of several months.
-
MR imaging to assess median nerve entrapment may be indicated in patients following posterior elbow dislocation who present with difficulty in reduction, median nerve symptoms, pain more severe than usual, and an increase in medial joint space on radiographs. In a patient with median nerve entrapment secondary to elbow dislocation, areas of normal muscle signal within the pronator–flexor group may be correlated with electromyographic findings of re-innervation after nerve release.66
-
MR imaging can depict displacement or engulfment of the median nerve by space-occupying lesions, ganglions, or a distended bicipitoradial bursa.60
 |
|
FIGURE 12.30 ● Median nerve in supination and pronation of the elbow. The nerve may become trapped between the two heads of the pronator teres in forearm pronation. This is the most common compression site in pronator syndrome. (Adapted from
Pecina MM, Drmpotic-Nemanic J, Markiewitz AD. Tunnel syndromes in the upper extremities. In: Pecina MM, Krmpotic-Nemanic J, Markiewicz AD, ed. Tunnel syndromes. New York: CRC Press, 1991:29-53
, with permission.) |
 |
|
FIGURE 12.31 ● Pronator syndrome. Oblique coronal (A) and axial (B) fat-suppressed T2-weighted images show diffuse denervation edema of the pronator teres muscle (arrowheads).
|
-
Trauma, such as supracondylar fractures
-
Posttraumatic thrombosis of the ulnar artery
-
An aberrant or thrombosed radial artery in the mid-forearm
-
A fascial band at the origin of the flexor digitorum superficialis
-
A tendinous origin of the ulnar head of the pronator teres
-
Anomalous muscles such as Gantzer's muscle or the palmaris profundus muscle
-
An enlarged bicipital bursa
-
Displaced humeral shaft fracture77
-
Inappropriate use of axillary crutches
-
Proximal prolonged tourniquet application
-
Lateral or posterior arm intramuscular injection
 |
|
FIGURE 12.32 ● High radial nerve entrapment secondary to intramuscular lipoma. (A) Axial T2-weighted and (B) post-contrast fat-suppressed T1-weighted images at the level of the distal arm demonstrate a large intramuscular lipoma (asterisk) obliterating the fat planes in the location of the radial nerve. Triceps muscle denervation edema is noted (arrow).
|
-
Fibrous bands extending from the radiocapitellar joint
-
The tendinous edge of the extensor carpi radialis brevis muscle
-
The radial recurrent artery and branches (leash of Henry)
-
The arcade of Frohse at the proximal edge of the supinator muscle80
-
A fibrous band at the distal end of the supinator muscle81
bursa may also result in compressive neuropathy of the radial nerve at the tunnel (Fig. 12.34).88
 |
|
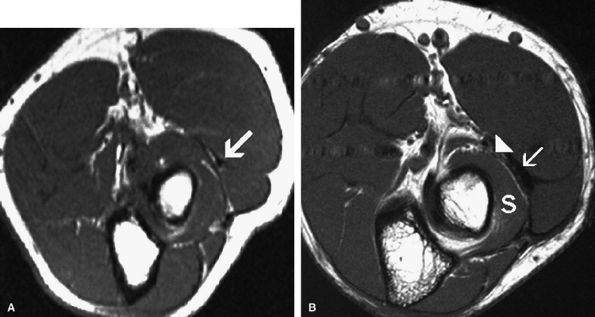
FIGURE 12.33 ● Free edge of the thickened extensor carpi radialis brevis. (A) Axial T1-weighted image depicts a low-signal free edge of the extensor carpi radialis brevis in an asymptomatic individual. (B) The thickened free edge (arrow) is shown in close proximity to the posterior interosseous nerve (arrowhead) in a patient with radial tunnel syndrome. Associated mild fatty infiltration of the supinator muscle (S) is noted.
|
 |
|
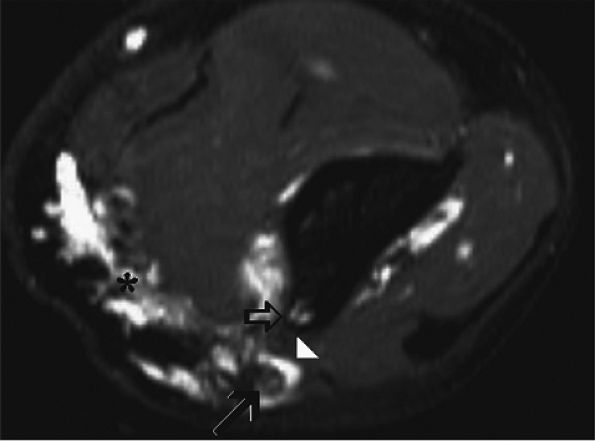
FIGURE 12.34 ● Posterior interosseous nerve syndrome secondary to bicipitoradial bursitis. (A) Axial PD-weighted image shows a markedly distended bicipital radial bursa (arrows) adjacent to the posterior interosseous nerve (arrowhead). (B) Axial fat-suppressed T2-weighted image demonstrates denervation edema and mild atrophy of the supinator (s), extensor carpi ulnaris (ecu), and extensor digitorum communis (edc) muscles in the proximal forearm.
|
 |
|
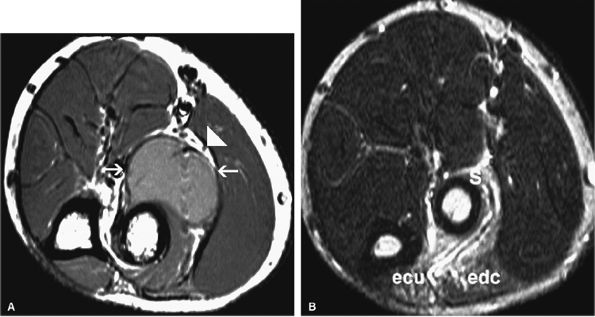
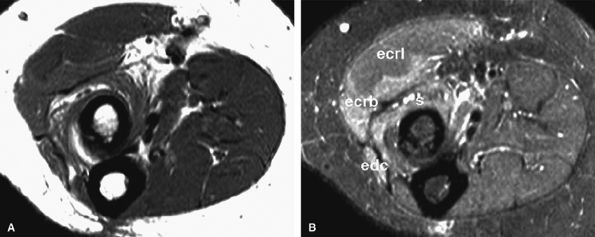
FIGURE 12.35 ● Posterior interosseous nerve syndrome. Axial T1-weighted (A) and fat-suppressed T2-weighted (B) images at the proximal forearm show atrophy and edema of the supinator and extensor musculature. The extensor carpi radialis longus, which is not innervated by the posterior interosseous nerve, is not involved. s, supinator; edc, extensor digitorum communis; ecrb, extensor carpi radialis brevis; ecrl, extensor carpi radialis longus.
|
-
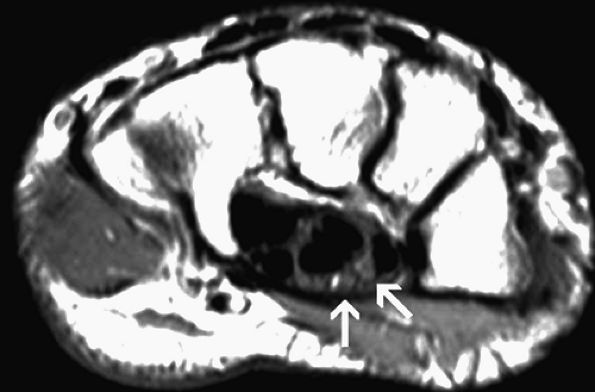
The carpal tunnel syndrome with compression of the median nerve occurs at the proximal aspect of the transverse carpal ligament or at the level of the hook of the hamate.
-
In the ulnar tunnel syndrome, sensation to the dorsal ulnar hand is spared. In contrast, ulnar compressive neuropathy proximal to the wrist is associated with loss of sensation in this area.
-
The superficial radial nerve syndrome involves entrapment of the sensory branch of the radial nerve in the distal forearm.
-
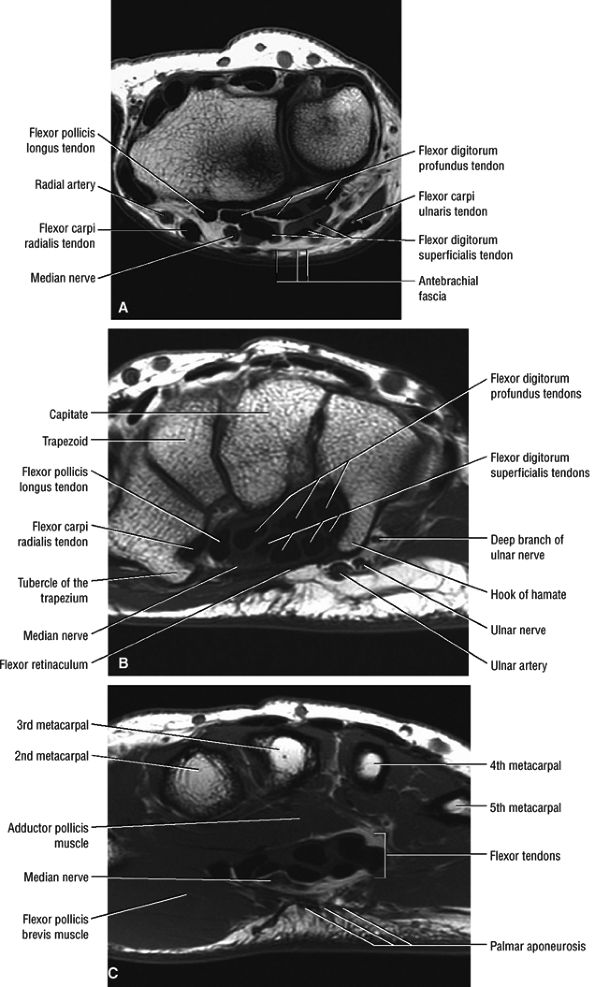
The antebrachial fascia proximal to the wrist (Fig. 12.37A)
-
The transverse carpal ligament proper (Fig. 12.37B)
-
The palmar aponeurosis between the thenar and hypothenar muscles (Fig. 12.37C)
palmar and distal dorsal aspects of the radial three-and-a-half fingers.
 |
|
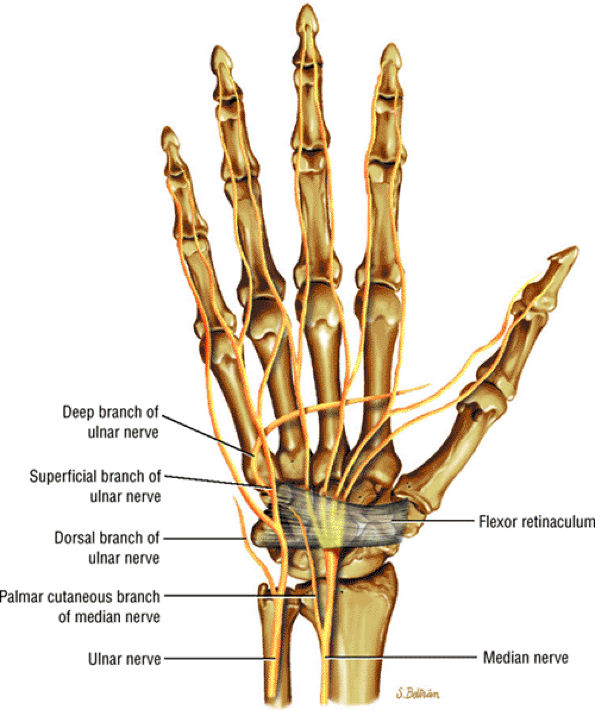
FIGURE 12.36 ● The median and ulnar nerves in the wrist and hand.
|
 |
|
FIGURE 12.37 ● Normal MR anatomy of the median nerve. (A) Axial T1-weighted image at the level of the distal radioulnar joint demonstrates the antebrachial fascia overlying the median nerve. (B) Axial T1-weighted image at the level of the distal carpal tunnel shows the flexor retinaculum extending between the hook of the hamate and the tubercle of the trapezium. (C) Axial T1-weighted image at the level of the proximal metacarpals shows the palmar aponeurosis and the proximal digital branches of the median nerve.
|
 |
|
FIGURE 12.38 ● Guyon's canal. This coronal PD image demonstrates the ulnar nerve as it travels within Guyon's canal.
|
-
Variations in the course of the thenar branch
-
Accessory branches at the distal carpal tunnel
-
A bifid median nerve or high division of the distal median nerve (Fig. 12.39)
-
Accessory branches proximal to the carpal tunnel
 |
|
FIGURE 12.39 ● Bifid median nerve. Axial fat-suppressed T2-weighted image shows high bifurcation of the median nerve (arrows) at the level of the carpal tunnel.
|
 |
|
FIGURE 12.40 ● Accessory flexor digitorum superficialis muscle. Axial T1-weighted image shows anomalous muscle (asterisk) deep to the lateral flexor tendons at the level of the metacarpals.
|
-
It has been hypothesized that median nerve compression most likely occurs during wrist flexion at the proximal edge of the transverse carpal ligament.56
-
Alternatively, the median nerve can be compressed where the carpal tunnel is narrowest, at the level of the hook of the hamate, by either synovial hypertrophy or a mass lesion.
-
In asymptomatic individuals, dynamic MR imaging has demonstrated that in wrist flexion the median nerve moves radially and posteriorly and becomes interposed between the flexor tendons.94 In patients with carpal tunnel syndrome, the median nerve is more likely to remain adjacent to the flexor retinaculum during wrist flexion, perhaps predisposing it to compression and subsequent carpal tunnel syndrome.
-
Increased pressure within the carpal tunnel has also been noted following repeated flexion and extension movements.
Complications of carpal tunnel release include incomplete release, injury to the median or ulnar nerves, and injury to the digital nerves, the ulnar artery, or the superficial palmar arch.114
 |
|
FIGURE 12.41 ● Carpal tunnel syndrome and rheumatoid arthritis. (A) Axial fat-suppressed T2-weighted image at the level of the proximal carpal row shows swelling and edema of the median nerve (white arrow) associated with flexor tendinosis (arrowheads), erosive changes (black arrow), and extensive inflammatory pannus (asterisks). (B) Axial fat-suppressed T2-weighted image at the level of the hook of the hamate demonstrates denervation edema of the thenar muscles (asterisk).
|
 |
|
FIGURE 12.42 ● Carpal tunnel syndrome and flexor tenosynovitis. Axial fat-suppressed T2-weighted image demonstrates marked peritendinous inflammatory edema of the flexor tendons within the carpal tunnel consistent with tenosynovitis (open arrows). Note flattening and edema of the median nerve (arrow) and associated synovitis in this patient with rheumatoid arthritis (asterisk).
|
 |
|
FIGURE 12.43 ● Fibrolipomatous hamartoma of the median nerve. (A) Sagittal T1-weighted image shows a fat-containing fusiform mass with typical spaghetti-like appearance (arrowheads). (B) Axial PD-weighted image demonstrates pathognomonic coaxial-cable–like appearance of the nerve (arrowheads) at the level of the carpal tunnel. Denervation edema of the thenar musculature (asterisk) is noted.
|
 |
|
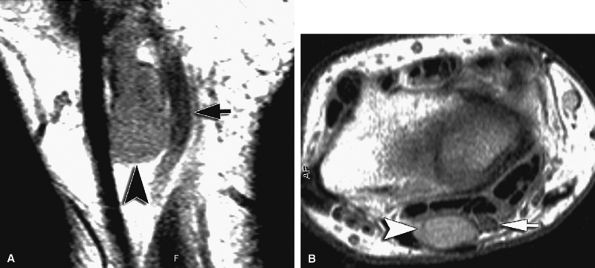
FIGURE 12.44 ● Ganglion cyst. Coronal (A) and axial (B) PD-weighted images show a volar ganglion cyst (arrowheads) displacing the median nerve (arrows).
|
-
Size of the nerve. The cross-sectional area of the median nerve is significantly larger in patients with carpal tunnel syndrome than in asymptomatic individuals.116 However, the cutoff size of the cross-sectional area between a normal and a pathologic median nerve is unclear. To evaluate proximal enlargement of the median nerve on axial MR images, comparison of the cross-sectional area of the nerve at the level of the radioulnar joint and at the level of the pisiform bone should be obtained. In patients with carpal tunnel syndrome, the median nerve at the level of the pisiform may be twice or three times as large as at the level of the radioulnar joint.117
-
Nerve flattening. Flattening of the nerve can be evaluated using flattening ratios, defined as the ratio between the major and minor axes of the nerve both at the level of the distal radioulnar joint and at the level of the hook of the hamate.117 A flattening ratio greater than 3 at the level of the hook of the hamate may indicate median nerve pathology.
-
Flexor retinaculum bowing. Bowing of the flexor retinaculum likely reflects increased pressure or volume within the carpal tunnel. In normal individuals, the flexor retinaculum at the level of the hook of the hamate should be flat or slightly convex. The degree of bowing is determined by dividing the distance of palmar displacement of the retinaculum by the distance between the hook of the hamate and the tubercle of the trapezium. In normal patients, the ratio varies from 0 to 0.15 (mean 0.05). In carpal tunnel syndrome, however, the ratio varies from 0.14 to 0.26 (mean 0.18).117
 |
|
FIGURE 12.45 ● Carpal tunnel syndrome. (A) Axial fat-suppressed T2-weighted image through the distal carpal tunnel demonstrates enlargement of the median nerve with bowing of the flexor retinaculum. The bowing ratio of the flexor retinaculum, determined by dividing its palmar displacement by the distance between the hook of the hamate to the tubercle of the trapezium, was 0.18 (normal ratio, 0 to 0.15). (B) Axial T2-weighted image through the proximal metacarpal region shows a swollen and hyperintense median nerve (arrow).
|
-
Zone 1 extends from the proximal edge of the palmar carpal ligament to the bifurcation of the ulnar nerve into the deep motor and superficial sensory branches.
-
Zone 2 extends from the bifurcation of the ulnar nerve just distal to the fibrous arch of the hypothenar muscles and contains the deep motor branch of the ulnar nerve.
-
Zone 3, which is parallel to zone 2, extends to the distal end of Guyon's canal and contains the superficial sensory branch of the ulnar nerve.
 |
|
FIGURE 12.46 ● Failed surgical release of the flexor retinaculum. Resection of the flexor retinaculum (arrow) with palmar displacement of the median nerve and flexor tendons is seen at the proximal (A) and distal (B) carpal tunnel. Note the surgical scar effacing the median nerve (arrowheads).
|
 |
|
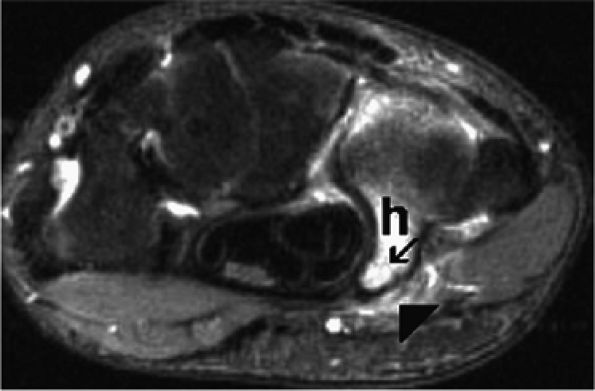
FIGURE 12.47 ● Ulnar neuropathy secondary to fracture of the hook of the hamate. Axial fat-suppressed T2-weighted image demonstrates a non-displaced fracture (arrow) of the hook of the hamate (h) associated with edema within Guyon's canal (arrowhead).
|
-
Zone 1 lesions present as combined motor and sensory deficits.
-
Zone 2 lesions are characterized by pure motor deficits.
-
Zone 3 lesions present with isolated sensory deficits.
-
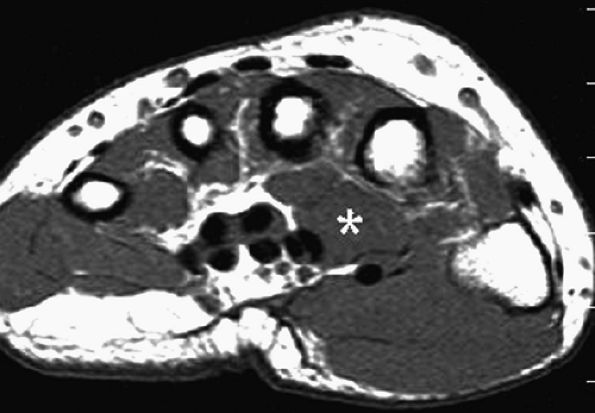
Accessory muscles such as an anomalous abductor digiti minimi, an anomalous flexor digiti minimi brevis, or a reversed palmaris longus124,125,126
-
Ulnar nerve schwannoma
-
Ganglion cyst127
-
Lipoma96
 |
|
FIGURE 12.48 ● Ulnar nerve schwannoma. Axial fast spin-echo T2-weighted image demonstrates a high-signal fusiform mass arising from the superficial branch of the ulnar nerve (arrow).
|
 |
|
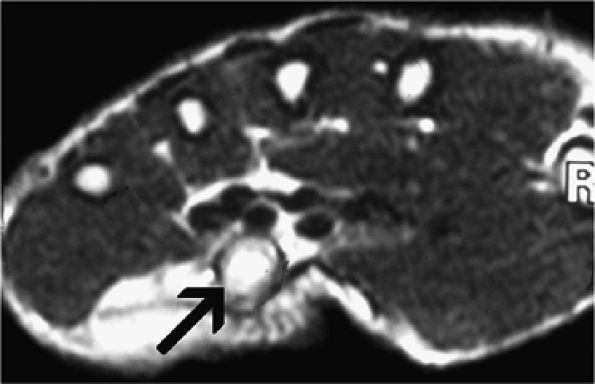
FIGURE 12.49 ● Ganglion cyst compressing the ulnar nerve. Axial (A) and oblique coronal (B) fat-suppressed T2-weighted images demonstrate a ganglion cyst (arrows) within Guyon's canal.
|
 |
|
FIGURE 12.50 ● Ganglion cyst compressing the superficial radial nerve. Axial fast spin-echo T2-weighted image (A) and coronal T1-weighted image (B) show a bilobed ganglion cyst (arrows) compressing the superficial radial nerve and radial artery (arrowheads).
|
-
Fascial bands in the subcutaneous plane at the nerve's exit point
-
The tendon of the brachioradialis
-
The tendon of the extensor carpi ulnaris longus
-
Ganglion cysts arising from the radiocarpal joint