DISLOCATIONS AND LIGAMENTOUS INJURIES OF THE DIGITS
III – THE HAND > Trauma > CHAPTER 39 – DISLOCATIONS AND
LIGAMENTOUS INJURIES OF THE DIGITS
and mobility, the hand allows us to manipulate our environment. The
thumb’s mobile carpometacarpal joint and stable metacarpophalangeal
(MP) and interphalangeal (IP) joints allow both precision pinch and
power movements, including grasp. The stable carpometacarpal joints of
the index and long fingers provide for stability along the central
longitudinal axis of the hand, whereas the relatively mobile ring and
little carpometacarpal joints provide mobility to allow cupping or
flattening of the hand. The hingelike MP and especially the IP joints
allow the ability to grasp objects of varying size.
forces, dislocations and ligamentous injuries of the digital joints are
quite common (396,397). Proximal interphalangeal (PIP) joint injuries are probably the most common joint injuries in the hand (68,128).
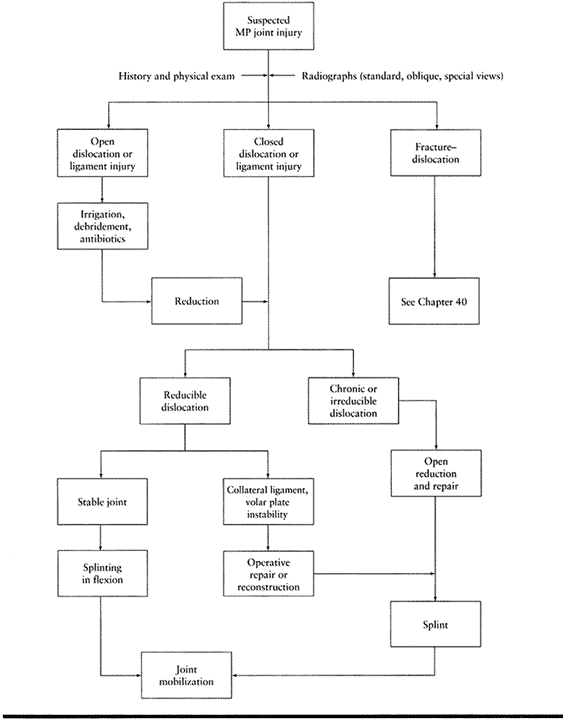
Fortunately, in the acute phase, most digital dislocations and ligament
injuries can be treated by closed or nonoperative means. This chapter
discusses these topics by joint. The fingers are covered as one, except
where a specific injury to a specific joint in a specific finger
requires individual attention. The joints of the thumb are addressed
separately. A general treatment algorithm is provided at the beginning
of each section.
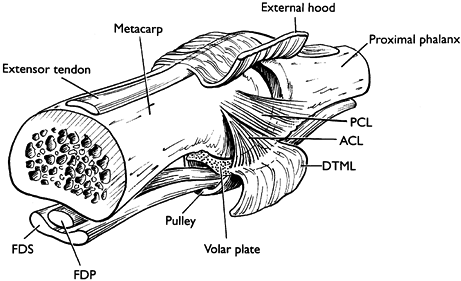
similar in that their stability is provided by a series of ligaments.
The major stabilizers of these joints include the volar plate and the
collateral ligaments. The volar plate is a fibrocartilaginous structure
firmly attached to bone distally, with a filmy proximal recess. On the
sides of each joint are the collateral ligaments, which blend palmarly
with the accessory collateral ligaments. The shape of these collateral
ligaments varies from a slightly fanlike shape at the proximal IP level
to very fan-shaped at the MP joint.
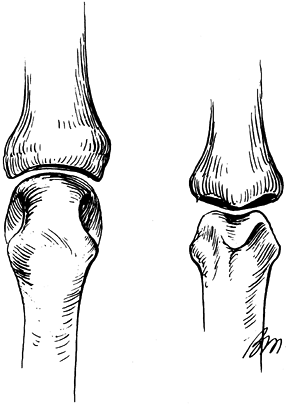
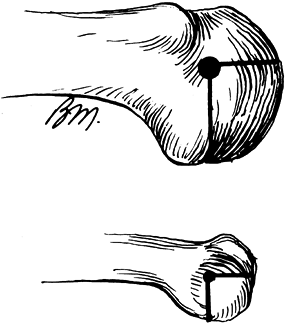
similar in configuration. The PIP joint is a hinge or ginglymus joint,
consisting of a convex bicondylar proximal phalangeal head articulating
with the biconcave middle phalangeal base. It allows approximately 100°
to 110° of flexion. A centrally located proximal phalangeal notch
articulates with a corresponding middle phalangeal median ridge (Fig. 39.1).
Dorsally, the central slip attaches to a tubercle on the base of the
middle phalanx. Palmarly, the volar plate forms the floor of the joint.
The volar plate has a thickened distal fibrocartilagenous portion that
is thicker along its lateral edges. The volar plate attaches along the
volar base of the middle phalanx, blending with the volar periosteum of
the middle phalanx centrally and the collateral ligaments laterally (Fig. 39.2) (12,14,15,20,28,38,76,77,82,95,137). The proximal portion of the volar plate tapers along its lateral edges to form two check-rein ligaments (Fig. 39.3) (12,14,15,82).
Laterally, the collateral ligaments consist of a thicker dorsal
cordlike collateral ligament proper, and a thinner volar accessory
component (76,91,137).
The collateral ligaments arise from a concavity along the lateral
aspect of the proximal phalangeal head. The ligaments pass obliquely
and palmarly to attach distally into a volar lateral tubercle on the
base of the middle phalanx and along the distal lateral margin of the
volar plate. The volar plate provides resistance to hyperextension
injuries of the PIP joint. Resistance to lateral stresses are provided
mostly by the collateral ligaments and secondarily, if at all, by the
volar plate (68,114). Some stability is also afforded by the surrounding tendon and retinacular system (15,82,124).
Disruption of at least two portions of the volar plate and two
collateral ligaments must occur for displacement of the PIP joint (30).
 |
|
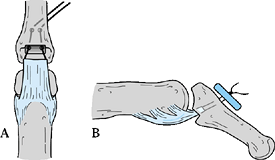
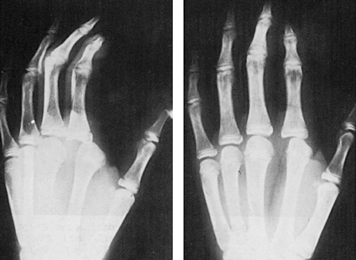
Figure 39.1. The fit of the articular surfaces of the metacarpophalangeal joint (left) and proximal interphalangeal joint (right). (From Green DP, Butler TE. Fractures and Dislocations in the Hand. In: Rockwood CA, Green DP, Bucholz RW, Heckman JD, eds. Fractures in Adults, 4th ed. Philadelphia: Lippincott-Raven, 1996:677, with permission.)
|
 |
|
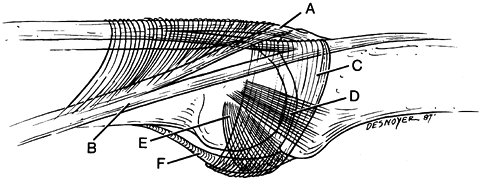
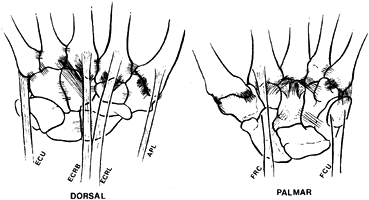
Figure 39.2.
Basic anatomy of the proximal interphalangeal joint. A, central extensor slip; B, intrinsic lateral band; C, transverse retinacular ligament; D, dorsal cord portion collateral ligament; E, accessory collateral ligament; F, volar plate. (From Vicar AJ. Proximal Interphalangeal Joint Dislocations without a Fracture. Hand Clin 1988;4:5, with permission.) |
 |
|
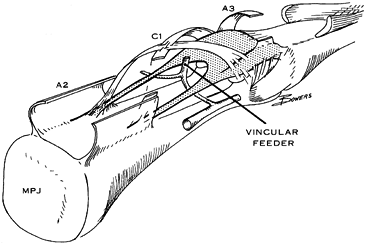
Figure 39.3. The proximal portion of the volar plate tapers along its lateral edges to form two check-rein ligaments. (From Bowers WH, ed. The Interphalangeal Joints. Edinburgh: Churchill Livingstone, 1987, with permission.)
|
the stability provided by the collateral ligaments and volar plate, has
some dynamic stability provided by the insertions of the flexor
digitorum profundus and the terminal
tendon of the extensor mechanism on the base of the distal phalanx.
consisting of a relatively ovoid metacarpal head articulating with an
elliptical cavity at the base of the proximal phalanx. The metacarpal
head is narrower dorsally than palmarly in the sagittal plane, and it
has a proportionately larger anteroposterior diameter than that of the
phalangeal head (Fig. 39.4). Joint motion is
primarily in the sagittal (flexion–extension) plane, but both coronal
(abduction–adduction) plane and small circumduction movements also
occur (217).
 |
|
Figure 39.4. Comparison of the metacarpal head (top),
which is narrower dorsally than volarly in the sagittal plane and has a proportionately larger AP diameter than that of the phalangeal head (bottom). (From Green DP, Butler TE. Fractures and Dislocations in the Hand. In: Rockwood CA, Green DP, Bucholz RW, Heckman JD, eds. Fractures in Adults, 4th ed. Philadelphia: Lippincott-Raven, 1996:677, with permission.) |
the base of the proximal phalanx. Volarly, the joint capsule blends
with the volar plate, which consists of a thick fibrocartilagenous
distal portion and a thin membranous proximal portion. The volar plate
is more securely attached to the proximal phalanx than to the
metacarpal neck. The volar plate is also continuous medially and
laterally with the deep transverse metacarpal ligament (Fig. 39.5) (162,167,172,173,192,217).
Dorsally, the MP joint capsule is thin, and it is reinforced by a loose
insertion of the common extensor tendon. The collateral ligaments
extend from the metacarpal head to the base of the proximal phalanx,
and they also insert into the volar plate. In addition, the metacarpal
origin of the collateral ligament is more dorsal than its counterpart
at the PIP joint (207). These factors dictate that the collateral ligaments of the MP joint are at their longest or most taut in full flexion (Fig. 39.6),
while those of the PIP are most taut at only a few degrees of flexion.
It is important to remember this when testing for collateral ligament
stability or when determining
the
tension appropriate for a repaired ligament, both during the repair and
after surgery. Additionally, the sagittal bands and intrinsic muscle
tendons provide secondary support to the MP joints (124).
 |
|
Figure 39.5.
Basic anatomy of the proximal interphalangeal joint. A, central extensor slip; B, intrinsic lateral band; C, transverse retinacular ligament; D, dorsal cord portion collateral ligament; E, accessory collateral ligament; F, volar plate. (From Vicar AJ. Proximal Interphalangeal Joint Dislocations without a Fracture. Hand Clin 1988;4:5, with permission.) |
 |
|
Figure 39.6.
The collateral ligaments of the metacarpophalangeal joint are taut with the joint in flexion and lax with the joint in extension. |
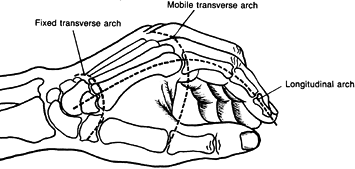
a fixed, stable central unit that comprises the index and long CMC
joints and the relatively mobile radial (thumb) and ulnar units (ring
and little). Together they form the fixed transverse metacarpal arch of
the hand (Fig. 39.7). The index and long finger
metacarpals articulate with the trapezoid and capitate with strong CMC
ligaments, providing relatively little motion (242,244,263,271).
Stability of these joints is provided by tight joint articulations,
thick dorsal capsular ligaments, volar ligaments, interosseous
ligaments, and by some support of the transverse carpal ligament.
Additionally, insertions of the flexor carpi radialis and extensor
carpi radialis longus into the base of the index metacarpal, and of the
extensor carpi radialis brevis into the base of the long metacarpal
provide some dynamic stability to the these joints (Fig. 39.8).
 |
|
Figure 39.7. The carpometacarpal joints of the index through little fingers form the fixed transverse arch of the hand.
|
 |
|
Figure 39.8. The carpometacarpal joints with supporting ligaments and tendon insertions. (From Gunther SF. The Carpometacarpal Joints. Orthop Clin North Am 1984;15:25, with permission.)
|
relatively mobile, providing approximately 10° to 30° of flexion and
extension, respectively, as well as a few degrees of supination (212,244).
They articulate with two separate hamate facets. A slightly convex
fifth metacarpal base articulates with a slightly concave ulnar hamate
facet, whereas a somewhat flatter fourth metacarpal articulates with
the radial hamate facet. Stability to these joints is provided by the
carpometacarpal and interosseous ligaments. Additionally, the
hypothenar muscles and insertions of the extensor carpi ulnaris and
flexor carpi ulnaris via the pisometacarpal ligament (a continuation of
the
flexor carpi ulnaris insertion) provide some dynamic stability to these joints.
of external forces. These forces can be direct (crush, burns,
lacerations) and/or indirect forces (rotational, bending, axial
loading). With indirect forces, the direction of the deforming force
determines the type of joint injury, while the amount of force dictates
whether the injury is a subluxation or a dislocation. For instance,
dorsal PIP joint dislocations are often accompanied by a longitudinal
compressive force; the magnitude of compression affects the complexity
of the injury. When greater longitudinal compressive forces are
combined with a hyperextension deforming force, dorsal PIP
fracture–dislocations are produced. The mechanism of injury for a
particular joint disorder is further discussed with each specific
injury.
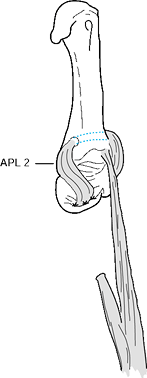
frequently accentuate the deformity. For instance, insertion of the
abductor pollicis longus on the base of the thumb metacarpal, and of
the adductor pollicis on the metacarpal shaft, will accentuate a thumb
CMC joint dislocation or fracture–dislocation.
direct forces or excessive indirect forces, can produce open wounds or
neurovascular injuries. These injuries will ultimately affect the
course of treatment. The treatment of an open dislocation with
neurovascular compromise is different from that of a simple closed
injury.
ligament injuries is to restore functional, pain-free, and stable joint
motion. To accomplish this goal requires an early, accurate evaluation
and diagnosis of the injury and adequate treatment. The goal of
treatment for injuries seen late is usually to provide pain relief.
extension, flexion, lateral deviation force) and timing of the injury
(acute versus chronic). Examine for active joint range of motion,
neurovascular status, flexor and extensor tendon function, areas of
localized tenderness, and, finally, passive joint stability.
and simple can be treated by nonoperative means. Digital block or nerve
block anesthesia can be helpful in evaluating joint stability or
reducing dislocations, but this is often unnecessary. Determine and
record the neurologic status prior to an anesthetic or treatment of the
injury.
examination, but good radiographs in at least two orthogonal planes
(perpendicular to one another) are necessary. With a digital injury,
radiographs of the digit (not of the hand) before and after treatment
are needed to accurately assess any associated fractures, as well as
the efficacy of treatment.
If used, anesthesia (usually a digital block or intraarticular
injection) is helpful to reap the maximum benefit from a stress view.
Similarly, stress views of the injured joint under fluoroscopy, when
compared to the uninjured joint in the opposite hand, can be helpful in
detecting ligament injuries (Fig. 39.9B).
 |
|
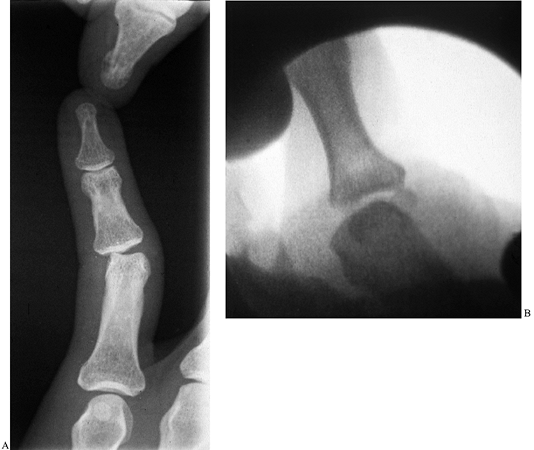
Figure 39.9. A:
AP radiograph with lateral stress applied to the proximal interphalangeal joint. Lateral deviation of more than 20° is indicative of a complete collateral ligament injury. B: Fluoroscopic stress view of the thumb MP joint showing lateral subluxation of the proximal phalanx. |
evaluating particular joint injuries. An oblique view (Brewerton view)
of the metacarpal heads may be helpful in detecting small metacarpal
head fractures (171,185,189,206).
The Brewerton view is taken as an anteroposterior (AP) view of the hand
with MP joints of the hand flexed approximately 65° and the x-ray beam
tilted 15° from an ulnar to radial direction (185). Evaluation of the thumb CMC joint requires a true AP view and a lateral view of the joint (Robert view) (403).
The AP radiograph is taken with the hand fully pronated and with the
dorsum of the thumb lying flat on the x-ray plate. The x-ray beam is
then centered over the thumb CMC joint. The lateral radiograph of the
joint is taken with the radial side of the thumb lying on the x-ray
plate (thumbnail lying perpendicular to the plate) and the x-ray beam
centered over the joint. Evaluation of the finger CMC joints will
frequently require oblique views of the hand. Occasionally, due to the
difficulty in evaluating these joints, tomography or computed
tomography (CT) may be needed.
stability (full active range of motion) and passive stability
(passively applied medial–lateral and anterior–posterior stress). If
the injury is amenable to closed treatment, use
a
cast dressing that immobilizes the hand and wrist as well as all the
fingers and, if necessary, the thumb. Take care when using a digital
splint, as an acutely injured digit can be further harmed by
immediately taping it to a digital splint. After surgical intervention,
a similar cast dressing is applied.
changed within 5 days. Begin an appropriate active motion program,
modifying for the specific injury. The same is recommended for many
postoperative cases. The goal is to provide joint stability and
adequate protection against reinjury or disruption of the repair while
gaining maximal motion to prevent tendon adherence or joint stiffness.
interphalangeal, metacarpophalangeal, and carpometacarpal joints can be
classified similarly. Classification can be based on the status of the
skin (closed versus open), the duration of injury (acute versus
chronic), the degree of joint displacement (subluxation versus
dislocation), the status of the joint surface (dislocation versus
fracture–dislocation), and the ability to reduce the joint dislocation
(simple versus complex).
joint soft tissue supporting structures, but some contact remains
between the articular surfaces. With dislocations, there is a loss of
contact between the joint surfaces. Joint dislocations and subluxations
can be further subclassified based on the direction of displacement of
the distal portion of the injured digit relative to the proximal
portion, that is, dorsal, lateral, or palmar (volar) dislocations.
open injuries are common (Table 39.1).
Assess these structures and obtain true AP and lateral radiographs of
the digit and particularly of the DIP joint. Open dislocations require
adequate debridement and antibiotics.
 |
|
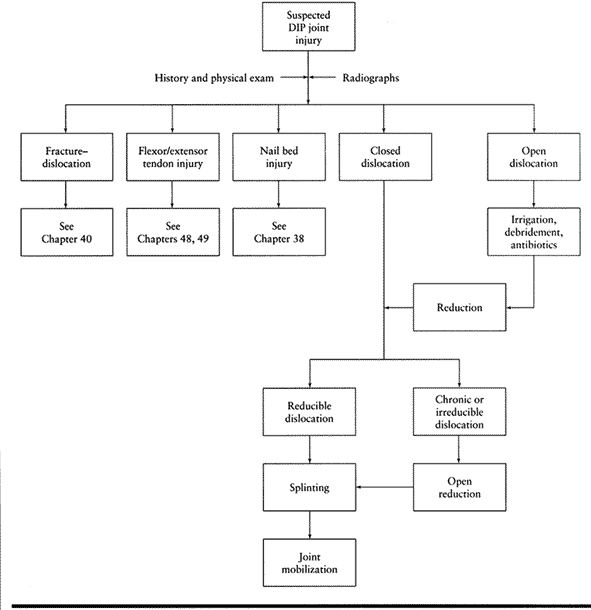
Table 39.1. Algorithm for Assessment of Distal Interphalangeal (DIP) Joint Injuries
|
The more common injuries occur secondary to a hyperextension force
(dorsal dislocation, dorsal lip fracture or fracture–dislocation),
forced extension against resistance (flexor profundus tendon avulsion
injury), flexion injury (extensor tendon avulsion injury), hyperflexion
force
(palmar dislocation), and lateral deviation force (collateral ligament
injury). The addition of a longitudinal compression force usually adds
some form of an intraarticular fracture.
These injuries are usually produced by a longitudinal compression and
hyperextension of the joint. Occasionally, a lateral, and even less
commonly a palmar, dislocation can occur. Look for flexor (jersey
finger) (Chapter 48) or extensor tendon (mallet finger) (Chapter 49)
avulsion injuries, which are common. Simultaneous dislocation of the
distal and proximal interphalangeal joints has been described and
should be detectable by careful clinical examination and adequate
radiographs of the injured digit (5,6,9,32,45,47,50,52,54,57,73,75,99,117,139,142).
-
Perform a closed reduction, with or without digital block anesthesia, using longitudinal traction on the distal phalanx.
-
Place direct pressure on the dorsal base of the distal phalanx, displacing it distally and palmarly.
-
Postreduction radiographs should confirm congruous reduction of the joint.
-
After joint reduction, assess joint
stability and flexor and extensor tendon function. If joint instability
is present after joint reduction, splint the joint for 2 to 3 weeks in
10° to 20° of flexion (for dorsal dislocations). -
With a palmar dislocation, dorsal lip
fracture–dislocation, or terminal extensor tendon avulsion (mallet
finger) injury, avoid splinting the DIP joint in hyperextension. This
prevents dorsal skin wound problems. Splint, generally, for 6 weeks or
more to promote healing (see Chapter 49). Fracture–dislocations of the joint can occur (46,51). -
If the flexor digitorum profundus is avulsed with the volar fragment, reattach the tendon.
-
Open dislocations of the DIP joint are
frequent and require irrigation, debridement, and antibiotics. Repair
any associated nail bed injuries or nail plate avulsions. -
When the dislocation is chronic (greater
than 3 weeks) or irreducible, perform an open reduction. Irreducible
DIP joint dislocations may be secondary to interposed volar plate,
flexor tendon, fracture fragment, or a sesamoid bone (32,44,53,58,67,70,98,103,107,108,112,118,122,123,130,133,150). Remove the interposed structure to reduce the joint.
-
Make a straight dorsal midline,
transverse, or H-shaped incision and split the extensor tendon
longitudinally in the midline. Alternatively, divide the tendon
transversely and repair it at the time of closure. -
If the volar plate is interposed between the joint surfaces, incise as much of it as necessary to displace it palmarly.
-
Release the collateral ligaments
subperiosteally at their insertion into the middle phalanx and continue
the dissection until the joint can be reduced. Test the joint for
stability. -
If the joint is grossly unstable,
transfix the joint with smooth 0.035–0.045 Kirschner (K-) wire(s) for 3
weeks. If the joint is fairly stable, immobilize it in a splint for a
few days for comfort. -
Then apply a dorsal-block splint and allow active flexion. Remove the splint after 3 weeks.
-
If the joint surface damage is extensive, perform a primary arthrodesis (see Chapter 72).
will usually occur from a failure in diagnosis, from a delay in
treatment, or from undertreatment. Failure to recognize a concomitant
injury to soft tissues (e.g., flexor or extensor tendons) will result
in a deformity (e.g., jersey finger or mallet finger) (186).
Unrecognized dislocations generally require an open reduction and pin
fixation, instead of a closed reduction. Delayed reduction of the joint
may also result in significant articular damage, necessitating an
arthrodesis. Redislocation of a dorsal DIP joint dislocation can occur
if hyperextension is not prevented for at least 3 weeks.
injuries of the DIP joint are partial tears or sprains at the DIP joint
level and thus can be treated nonoperatively. Temporary splinting for a
few days for comfort should be followed by an early, vigorous active
motion program.
subluxations are frequently associated with an injury to the volar
plate, collateral ligament, extensor tendon (central slip), and joint
articular surface (Table 39.2). Assess these
structures and take true AP and lateral radiographs of the digit,
particularly of the PIP joint. Stress views to assess collateral
ligament injuries may be helpful. Open dislocations require adequate
debridement and antibiotics.
 |
|
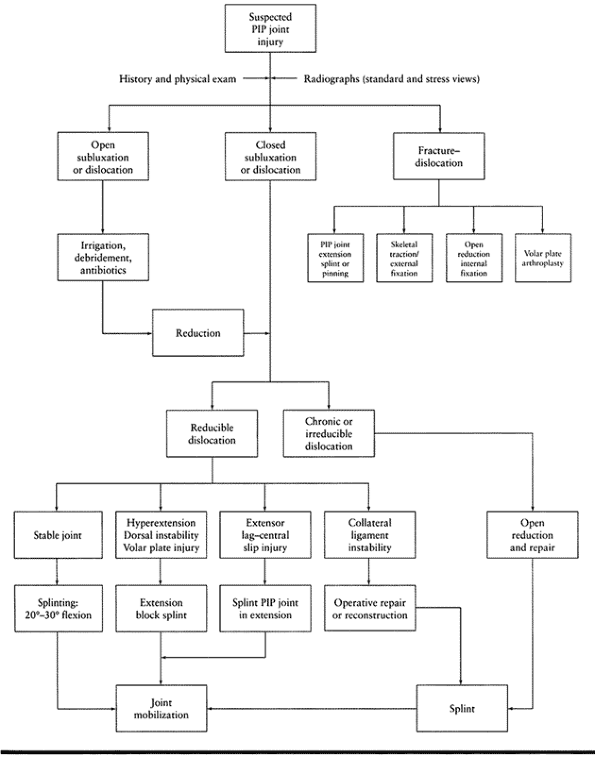
Table 39.2. Algorithm for Assessment of Proximal Interphalangeal (PIP) Joint Injuries
|
ranging from a simple hyperextension injury, as seen in sporting
injuries, to a severely comminuted fracture. The more common injuries
occur secondary to a hyperextension force (dorsal subluxation or
dislocation,
volar
plate rupture), longitudinal compression and hyperextension force
(dorsal fracture–dislocation), lateral deviation force (collateral
ligament injuries), and combined rotatory and longitudinal compression
force (rotatory dislocations).
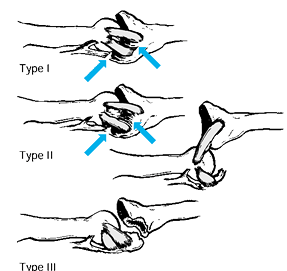
However, generally three types can be categorized depending on the
degree of hyperextension force applied to the joint and any associated
fractures (28,38).
-
Type I is a hyperextension injury to the joint with subluxation but not dislocation.
-
Type II is a dorsal dislocation.
-
Type III is a shear fracture of the volar base of the middle phalanx, producing a fracture–dislocation (Fig. 39.10).
Type I injuries are associated with avulsion of the volar plate, and a
partial horizontal split occurs between the volar and dorsal portions
of the collateral ligaments. Type II injuries are associated with a
complete avulsion injury of the volar plate and a greater longitudinal
tear of the collateral ligaments (12,18,28,38).![]() Figure 39.10. Three types of dorsal PIP joint hyperextension injury (see text for description of injuries).
Figure 39.10. Three types of dorsal PIP joint hyperextension injury (see text for description of injuries).
reduced by closed means. A digital block is often unnecessary. The
volar plate, by necessity, is ruptured, usually from the middle
phalanx, but the collateral ligaments rarely are ruptured completely
from their attachments (10,12).
Perform reduction with longitudinal traction and direct pressure on the
dorsal base of the middle phalanx, displacing it distally and palmarly.
Confirm congruous reduction of the joint with postreduction
radiographs. Assess both active and passive stability of the joint
after reduction. With type I and II dorsal dislocations, the joint is
usually stable after reduction (56,126).
Type III injuries are discussed in the following section. Use a resting
splint with the finger flexed to 20° to 30° for 7–10 days. Do not
splint the digit in flexion for an extended period of time, and begin
early active motion with protection against hyperextension.
Alternatively, use an orthoplast figure-eight splint, preventing joint
hyperextension (79). Protect the injured digit,
especially during sporting activities, by taping it to the adjacent
uninjured digit. Reassure the patient that persistent swelling and slow
resolution of stiffness is to be expected.
and require open reduction. An attempt at gentle closed reduction under
adequate anesthesia is permissible but is best done in the operating
room; if it is unsuccessful, the joint then can be approached
surgically.
-
Make a straight or slightly curvilinear dorsal longitudinal incision.
-
Divide the central slip of the extensor
mechanism in the midline but do not dissect distal to the base of the
middle phalanx, as the attachments of the central slip to the middle
phalanx and triangular ligament must remain intact. -
If the volar plate is interposed, split
the interval between it and each accessory collateral ligament.
Mobilize the volar plate and perform a trial reduction of the joint. -
If this fails, release the origins of the
collateral ligaments from the proximal phalanx by sharp subperiosteal
dissection. This should allow reduction if the joint is hyperextended
and the volar plate is pushed palmarward. -
After reduction, test the joint for
instability. If instability is present, transfix the joint with smooth
0.035–0.045 K-wire for 3 weeks. -
If the joint is fairly stable, close the
extensor split and the skin separately with nonabsorbable sutures. Take
postreduction radiographs to confirm congruous reduction of the joint. -
Immobilize the hand in a cast dressing
with the PIP joints flexed no more than 10°. After 5–7 days, begin
active flexion for an additional 2–4 weeks, using a dorsal
extension-block splint to prevent hyperextension of the joint.
the volar plate (also referred to as a pseudoboutonnieére deformity) (90,91).
A significant contracture can be treated with dynamic splinting, serial
casting, or, eventually, surgical release of the contracture (25,38,80,88,140).
joint hyperextension is not prevented for at least 3 weeks, either
redislocation of the joint or a chronic swan-neck deformity may occur (104).
A true lateral radiograph will help guard against persistent
subluxation. With a chronic swan-neck deformity, painful snapping of
the lateral bands over the phalangeal heads or inability to initiate
joint flexion may occur. Treatment includes primary reattachment of the
volar plate or sublimis tenodesis (see the section below on volar plate ruptures) (1,7,12,22,38,72,78,91,109,110,132,136,144,195).
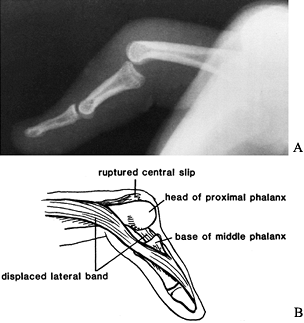
The injury results in volar displacement of the middle phalanx relative
to the proximal phalanx. There is a disruption of the extensor
mechanism (central slip), creating a boutonnieére injury. One proximal
phalangeal condyle may herniate between the central slip and the
lateral band, producing a rotatory or irreducible PIP joint dislocation
(see Rotatory Dislocations). There may be an injury to a collateral
ligament and the volar plate (Fig. 39.11) (33,37).
 |
|
Figure 39.11. A: Lateral radiograph of volar proximal interphalangeal dislocation. B: Diagram showing how the boutonnieére develops as the head of the proximal phalanx herniates through the extensor mechanism.
|
-
Reduce a palmar PIP joint dislocation with gentle traction on the middle phalanx with the MP and PIP joints flexed (134,146).
Wrist extension may relax the extensor mechanism. In general, full
passive extension of the joint is obtainable and postreduction
radiographs should confirm congruous reduction of the joint. -
After reduction, test active PIP joint
extension to determine the status of the central slip. With disruption
of the central slip, the PIP joint should be splinted in extension for
4–6 weeks, either with smooth K-wire transfixing the joint or simply
with an external splint. -
The DIP and MP joints should be permitted
to move so that the extensor mechanism is less likely to become
adherent. If the dislocation is irreducible or chronic (34,106,110,111), surgery is necessary.
-
Make a straight dorsal or slightly curvilinear incision.
-
Mobilize the lateral bands so that the head of the proximal phalanx is no longer caught between them.
-
Reduce the joint, and transfix it in extension with smooth 0.035–0.045 K-wire.
-
Reattach the central slip to the base of
the middle phalanx with nonabsorbable sutures to remaining periosteum,
through bone holes, or with miniature suture anchors. Repair the
interval between each lateral band and the central slip with
nonabsorbable sutures. Postreduction radiographs should confirm
congruous reduction of the joint. -
Remove the pin after 6 weeks, having allowed active motion at the MP and DIP joints during that time.
joint dislocation tend to be poor, emphasizing the need for early
recognition of the injury (28,34,38,41,106,110,146).
If any or too early PIP flexion is allowed during the immobilization
period, a boutonnieére deformity will result. Treatment of the
boutonnieére deformity varies depending on the duration of the
deformity (35,89).
complex volar-lateral dislocation, is an uncommon injury in which the
middle phalanx is displaced laterally and palmarly (8,21,24,30,36,39,59,61,63,65,69,93,98,100,102,106,110,111,122,127,135,143). The injury occurs secondary to a combined rotatory and compressive force applied to
the PIP joint. Clinically, the PIP joint is swollen and tender. The
digit may be deviated and flexed. In contrast to the palmar PIP joint
dislocation, for which passive extension is possible after reduction,
there is resistance to active and passive flexion and especially to
passive extension.
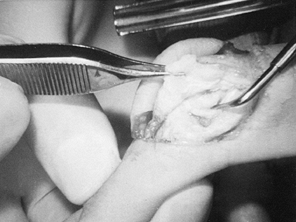
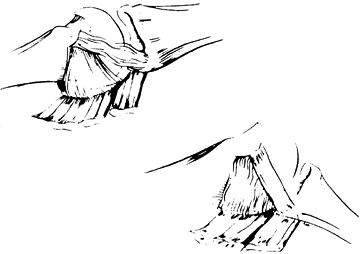
ligament is ruptured and the condyle of the proximal phalanx usually
penetrates through a longitudinal rent between the lateral band and the
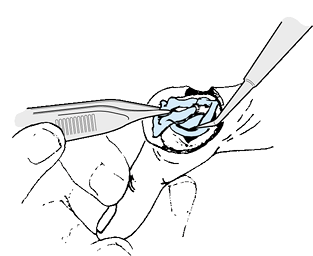
central slip (Fig. 39.12). The lateral band is looped through the joint around the condyle, preventing reduction.
 |
|
Figure 39.12. A longitudinal rent in the extensor mechanism produced by the condyle of the proximal phalanx (above probe) splits the central slip (held by forceps) from the lateral band (below probe). The band then loops around the condyle and through the joint, preventing reduction.
|
be improved by closed reduction, but there will be a persistent
subluxation and widening of the joint space on the side of injury (Fig. 39.13).
Due to the rotatory nature of the injury, on a true lateral radiograph
of the digit, one phalanx may appear slightly rotated relative to the
other. This persistent subluxation of the joint usually must be treated
surgically. Attempt closed reduction following digital block
anesthesia, with gentle longitudinal traction and finger rotation (20,28,38,134).
Flex the MP and PIP joints to relax the lateral bands, and extend the
wrist to relax the extensor mechanism. Confirm congruous reduction with
radiographs and test for active motion and active and passive
stability. With incomplete active PIP joint extension, splint the joint
in full extension for 3–6 weeks.
 |
|
Figure 39.13. AP radiograph showing persistent subluxation or widening on one side of the PIP joint.
|
-
Make a mid-axial or dorsal curvilinear
incision angled toward the injured side of the PIP joint. The condyle
protruding between the central slip and the lateral band will be seen
at once (Fig. 39.14).![]() Figure 39.14. Clinical photograph corresponding to Figure 39.12.
Figure 39.14. Clinical photograph corresponding to Figure 39.12. -
Remove the lateral band from the joint with a blunt instrument. The joint will promptly reduce.
-
Repair the collateral ligament if
disruption of the collateral ligament results in persistent joint
instability or subluxation. If the lateral band is not badly damaged,
repair the longitudinal rent in the interval between the lateral band
and the central slip. If the lateral band is severely damaged, excise
it. -
The remaining intact central slip and lateral band are sufficient to provide full extension of the finger (100). Intraoperative postreduction radiographs should confirm congruous reduction of the joint.
-
After 5–7 days of immobilization in a
cast dressing, start active motion, with the finger strapped to the
adjacent finger to protect against reinjury. Protect the finger for 4–6
weeks.
dislocations are usually due to failure to diagnose the dislocation,
causing a delay in treatment that results in a fixed flexion deformity (146).
Incomplete joint reduction results from incomplete removal of the
lateral band. Joint instability results from inadequate collateral
ligament repair. Failure to adequately reduce the joint will result in
a fixed flexion deformity. Late treatment consists of volar plate and
collateral ligament release, excision of the lateral band, and
reduction of the joint (106).
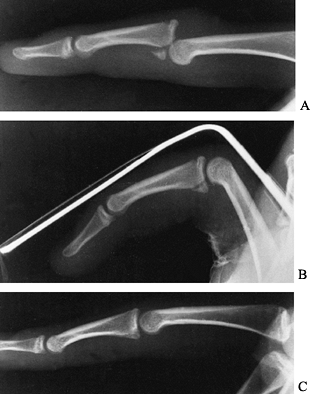
most difficult fracture–dislocation to treat in the hand. As the middle
phalanx displaces proximally and dorsally, the head of the proximal
phalanx is driven into the palmar lip of the base of the middle
phalanx. A comminuted depressed fracture usually results and can
involve 70% or more of the articular surface. These injuries can be
divided into stable and unstable fracture–dislocations (28,38).
In stable fracture–dislocations, the volar lip fracture usually
involves less than 40% of the articular surface. The dorsal portions of
the collateral ligaments remain attached to the middle phalanx. With
unstable fracture–dislocations the volar lip fracture involves more
than 40% of the articular surface. The collateral ligaments usually
remain attached to the volar lip fracture. Dorsal joint subluxation,
which is difficult to reduce and to maintain by closed means, tends to
occur with PIP joint extension.
Dorsal subluxation associated with volar lip middle phalangeal
fractures can occasionally be reduced with PIP joint flexion. Always
try this technique first, since it yields the best results if
applicable (Fig. 39.15). The key to its
usefulness is restoration of the joint alignment, not reduction of the
fracture. If the fracture reduces also, this is a bonus.
 |
|
Figure 39.15. Fracture–dislocation of the PIP joint. B:
Joint reduced by flexion of the finger to 60° or more. The fracture reduction (anatomic here) is a bonus but is not necessary for a good result. C: Healed fracture–dislocation with good joint congruity. |
-
Use a padded hand-based aluminum splint
or combine an aluminum splint with a short arm cast. With the latter
technique, a padded aluminum splint loop is taped to a short arm cast
over the top of the finger being tested (Fig. 39.16).![]() Figure 39.16. Extension-block splint.
Figure 39.16. Extension-block splint. -
Fashion the splint so that the PIP joint
is flexed approximately 10° to 15° short of the unstable, dorsally
subluxed position, which is generally between 30° to 40° of PIP joint
flexion. -
A true lateral radiograph of the digit will confirm that the joint subluxation is corrected.
-
Adjust the splint weekly by reducing the
degree of PIP joint flexion by 25%, or approximately 10°. Take
radiographs weekly to ensure that dorsal joint subluxation has not
recurred. -
If joint alignment cannot be restored by
closed means, extension-block splinting should be abandoned and an
alternative procedure used. These measures include extension-block
pinning (135,138), skeletal tractionor dynamic skeletal traction (2,3,17,22,55,97,105,115,119,121), dynamic hinged external fixation (48,49,66,74), open reduction and internal fixation (33,40,60,61,81,86,91,128,141,144,147,148 and 149), and vo-lar plate arthroplasty (11,29,31,60,61,87).
-
Place a smooth K-wire in the proximal
phalangeal head and shaft from a distal to proximal direction at an
angle, with the PIP joint partially flexed, which places it dorsal to
the middle phalanx, and with the dorsal fracture–subluxation reduced. -
The wire prevents dorsal subluxation of the middle phalanx as seen on a lateral radiograph.
-
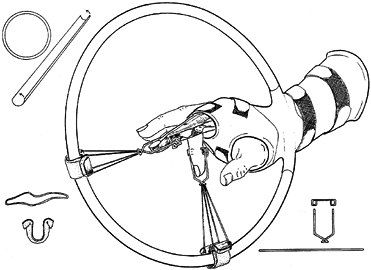
Use a small needle to identify the joint line (Fig. 39.17A).
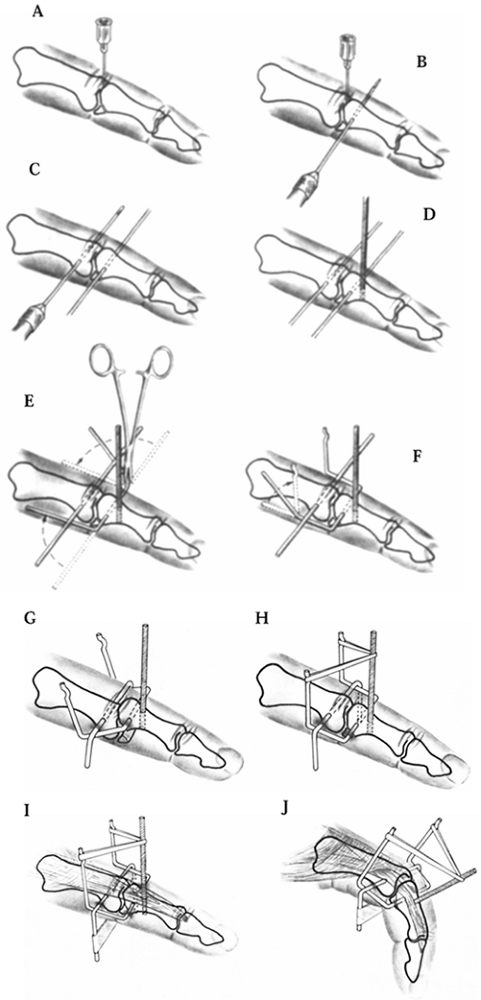 Figure 39.17.
Figure 39.17.
Force-couple splint. See text for a description of each step in the
technique. Agee JM. Unstable Fracture Dislocation of the Proximal
Interphalangeal Joint: Treatment with the Force Couple Splint. Clin Orthop 1987;214:101. -
Insert smooth K-wires transversely into the middle phalangeal base (Fig. 39.17B) and into the center of the proximal phalangeal head (Fig. 39.17C), parallel to the PIP joint articular surface.
-
Place a threaded K-wire in a dorsal to volar direction in the proximal half of the middle phalanx (Fig. 39.17D) and through the dorsal and volar cortices, being careful not to penetrate the flexor tendon.
-
On both sides of the finger, bend the distal K-wire proximally at 90° and pass it proximal and palmar to the proximal wire (Fig. 39.17E).
Make a second 90° bend in the distal wire, 5–10 mm proximal to the
proximal wire, and direct the wire dorsally or vertically (Fig. 39.17F). Bend a hook into the ends of the K-wire to retain a rubber band. -
On both sides of the finger, bend the proximal K-wire at 90° in a palmar direction (Fig. 39.17G). Bend the proximal wire outside of the distal wire.
-
Connect the vertically oriented, threaded
K-wire and the vertical arms of the distal K-wire with a rubber band,
producing linkage, or a force couple (Fig. 39.17H). -
Place adhesive tape around the ends of the proximal K-wire to prevent the two ends of the wire from spreading apart (Fig. 39.17I).
-
The force couple allows joint range of
motion and is used to palmarly displace the middle phalanx and dorsally
displace the proximal phalanx and thereby reduce dorsal subluxation of
the PIP joint fracture–dislocation (2,3) (Fig. 39.17J).
-
Place a transosseous wire horizontally
into the distal head of the middle phalanx and bend the wire distally
on both sides of the finger at 90° angles. -
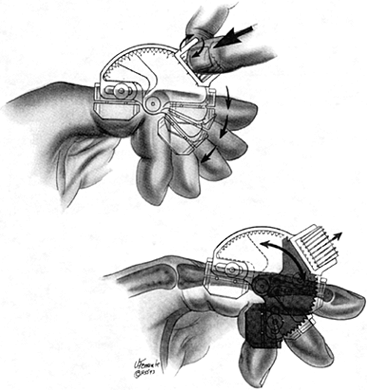
Place a loop into the ends of the wire
and connect with rubber bands, the ends of the wire to a sliding
U-shaped thermoplastic component. -
The U-shaped component is looped over a circular 3- or 6-inch-diameter hand/forearm outrigger hoop splint.
-
The rubber band provides traction across the PIP joint. Use of the outrigger splint allows active finger flexion and extension (119,121) (Fig. 39.18).
![]() Figure 39.18.
Figure 39.18.
Outrigger splint. From Schenk RR. The Dynamic Traction Method.
Combining Movement and Traction for Intra-Articular Fractures of the
Phalanges. Hand Clinic 1994;10:187.
-
Under fluoroscopic guidance or open
visualization, place a K-wire horizontally into the proximal phalangeal
head center axis of rotation. -
Place the centering hole of a hinged
external fixator [e.g., the Compass PIP Hinge (Smith and Nephew
Richards, Memphis, TN)] over the central axis pin (Fig. 39.19).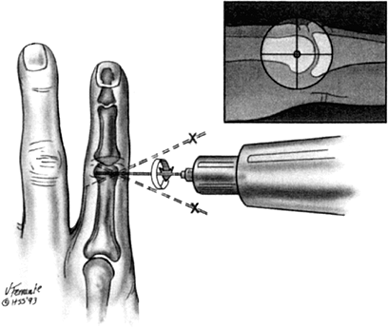 Figure 39.19. Placement of the hinged external fixator. From Jones BF, Stern PJ. Interphalangeal Joint Arthrodesis. Hand Clinic 1994;10:267.
Figure 39.19. Placement of the hinged external fixator. From Jones BF, Stern PJ. Interphalangeal Joint Arthrodesis. Hand Clinic 1994;10:267. -
Place smooth K-wires initially through
the proximal and then through the distal pin blocks in the mid-axial
line of the digit. Hold the middle phalanx reduced during K-wire
placement in the distal pin block. -
Apply joint distraction or passive joint motion, as needed, using a built-in distraction screw or worm gear mechanism (Fig. 39.20).
![]() Figure 39.20. Application of joint distraction. From Jones BF, Stern PJ. Interphalangeal Joint Arthrodesis. Hand Clinic 1994;10:267.
Figure 39.20. Application of joint distraction. From Jones BF, Stern PJ. Interphalangeal Joint Arthrodesis. Hand Clinic 1994;10:267.
of the palmar lip fracture is a demanding and often frustrating
technique. If the fragment is sufficiently large and the fracture
fairly fresh, however, internal fixation may provide reasonably good
joint motion. Methods of fixation include K-wires, screw fixation, and
intraosseous wiring.
is an alternative that can be used for acute as well as chronic
injuries. Advancement of the volar plate attempts to restore the
impacted volar articular surface.
-
Make a palmar zigzag incision over the PIP joint.
-
Elevate the flexor sheath from the distal edge of the A2 to the proximal edge of the A4 pulley, protecting the digital arteries and nerves at all times.
-
Retract the flexor tendons without damaging the vincula.
-
Mobilize the volar plate and accessory
collateral ligaments with the attached palmar lip fragment from the
middle phalanx, leaving it attached proximally. -
Excise the remaining collateral ligaments
connecting the proximal and middle phalanges (especially in chronic
cases), and then open the joint by hyperextending it (like a shotgun) (Fig. 39.21). Figure 39.21. PIP joint exposed by opening like a shotgun. From the bottom:
Figure 39.21. PIP joint exposed by opening like a shotgun. From the bottom:
Fracture fragment with attached volar plate, head of proximal phalanx,
base of middle phalanx with defect from compression fracture. -
Debride small or loose fragments. If the
fragment attached to the volar plate is large, fix it with fine smooth
K-wire(s), screws, or an interosseous wire to the middle phalanx, being
careful to establish a smooth articular surface and a congruous joint
reduction. -
Confirm congruous reduction of the joint with postreduction radiographs.
-
More commonly, the volar plate fragment
cannot be used. Dissect it free subperiosteally from the volar plate,
retaining all possible length of the plate. Mobilize the volar plate as
much as possible, leaving its proximal attachment intact, by freeing
any restraining bands in the recess. -
Create a transverse trough in the middle
phalangeal defect at the dorsalmost part of the cancellous defect, near
the palmar margin of the remaining dorsal articular cartilage. The
trough must be perpendicular to the long axis of the middle phalanx.
Place drill holes at the lateral margins of the trough. -
Reduce the PIP joint, and pull the volar plate into the trough with the joint flexed no more than 30° (Fig. 39.22). Tie the suture over a protected button dorsally.
![]() Figure 39.22. A:
Figure 39.22. A:
View from palmar side of volar plate arthroplasty as sutures lead the
distal edge of the volar plate into the trough at the base of the
middle phalanx. B: Lateral view of volar plate arthroplasty, secured with the joint flexed. -
Confirm congruous reduction of the joint
with intraoperative postreduction radiographs. Suture any remaining
collateral ligament to the lateral margin of the volar plate. -
Transfix the joint with a smooth 0.035–0.045 K-wire with the joint in 20° to 30° of flexion.
-
Immobilize the hand in a cast dressing.
Remove the wire at 2 weeks, and encourage active flexion with use of an
extension-block splint. Begin active extension at 4 weeks and extension
splinting at 5 weeks if full extension is lacking. Motion may continue
to improve for several months.
usually due to failure to treat the initial injury adequately or
secondary to loss of reduction of the joint. Persistent joint
dislocation can occur with closed treatment when the joint hinges
instead of reducing congruously, or redislocation occurs with too rapid
mobilization of the joint into extension. Redislocation can also result
from inadequate reduction at surgery, or from failure of the pullout
suture or of internal fixation. Angulation of the joint can occur
secondary to asymmetrical impaction of the volar lip fragment or with
oblique placement of the volar plate bone trough. Flexion contracture
occurs with prolonged immobilization. Posttraumatic arthritis results
from articular damage.
release, repeat open reduction and internal fixation, opening-wedge
osteotomy and bone grafting, volar plate arthroplasty, and joint
arthrodesis (27,28,31,38,64,140,146,149).
Clinically, tenderness occurs over the site of injury, and joint laxity
to lateral stress may be present. Most PIP joint collateral ligament
injuries are incomplete and need only to be protected by strapping to
an adjacent digit for 3–6 weeks (41,96).
However, lateral dislocations of the PIP joint can result in complete,
but uncommon, rupture of a collateral ligament and at least a portion
of the volar plate (28,38). Angulation greater than 20° with lateral stress testing indicates a complete collateral ligament injury (34,68,95) (Fig. 39.9A).
controversial. After closed reduction, assess stability of the joint by
active motion and confirm joint congruency on radiographs. Acutely, use
a temporary splint for comfort, followed by strapping to an adjacent
digit for 3–4 weeks, encouraging full active motion. Repair of the
collateral ligament has been described (4,13,16,41,60,61 and 62,91,94,113,116),
but joint stiffness is a problem. The index radial collateral ligament
is probably the only ligament that needs early surgery (41,62,94).
-
Make a radial mid-axial incision.
-
Divide the transverse retinacular ligament, reflect it, and retract the radial lateral band dorsally.
-
Identify and repair the torn collateral
ligament. The stump usually is still attached at the middle phalanx and
is repaired with nonabsorbable sutures. -
If no residual stump is present, roughen
the bone and drill parallel holes obliquely across the phalanx. Pass a
nonabsorbable suture, using a modified Bunnell suture technique,
through the torn edge of the ligament. Pass the two suture ends through
the holes in the bone and out through the skin. Tie the suture over a
protected button with the joint reduced and the ligament pulled taut.
Miniature suture anchors can be used instead of a transosseous pullout
suture technique (Fig. 39.23). Figure 39.23. Miniature suture anchors can be used instead of a pullout suture technique to repair the collateral ligament.
Figure 39.23. Miniature suture anchors can be used instead of a pullout suture technique to repair the collateral ligament. -
Repair the accompanying partial tear of the volar plate as well.
-
Repair the retinacular ligament, close the skin, and confirm congruous reduction of the joint with radiographs.
-
Splint the digit in no more than 20° of
PIP joint flexion for 5–7 days and then start active motion with
adjacent finger-strapping for an additional 2–3 weeks.
sufficiently symptomatic to require reconstruction. Often, there are
degenerative changes in the joint, and ligament reconstruction cannot
be expected to alleviate symptoms due to arthritis. Once again, if
reconstruction of a chronic PIP collateral ligament rupture is
necessary, it is on the radial side of the index finger.
shortening or imbricating the remaining ligament or by augmenting the
repair, usually with a slip of the superficialis (78,91,104,113).
-
Make a surgical approach similar to that made for the acute collateral ligament injury.
-
Identify the ligament and dissect it
free. Imbricate it in its midportion, or shorten it and suture it with
a nonabsorbable suture at the proper length. -
If further reinforcement is needed,
separate the radial slip of the superficialis, leaving it attached
distally detaching it proximally. Pass the tendon through a drill hole
in the head of the proximal phalanx with a pullout suture and tie the
suture over a protected button on the ulnar side of the proximal
phalanx. -
Alternately, pass the superficialis
through two holes drilled on the radial aspect of the proximal
phalangeal head and suture the tendon to itself. Spread out the tendon
dorsally and suture its radial (now dorsal) edge to the remaining
fibers of the collateral ligament. -
Close the wound as previously described.
After 10 days of immobilization in no more than 20° of flexion,
encourage the patient to actively exercise with strapping to the
adjacent long finger for an additional 4–5 weeks.
dislocations usually occur from inadequate initial treatment, and they
are frequently an expected outcome of the injury, even with adequate
treatment. Pain, instability, loss of motion, and arthrosis can occur
from incomplete joint reduction, lateral translocation, or uneven
forces within the joint secondary to excessive scarring (146).
perfectly stable joint. Potential problems of ligament reconstruction
include joint stiffness or persistent laxity.
dorsal PIP joint dislocation or hyperextension injury (type 1 dorsal
PIP joint dislocation). The volar plate usually detaches distally from
the middle phalanx, with or without a piece of bone. If the volar plate
ruptures distally with a small fragment of bone (as seen on the lateral
radiograph), the joint is inevitably congruous. This injury must be
differentiated from the serious PIP joint fracture–dislocation. Treat
the minor volar plate fracture as any other volar plate injury, with
protection against hyperextension by either a temporary dorsal-block
digital splint or by strapping to an adjacent finger for 3 weeks.
Encourage full flexion.
deformity with dorsal subluxation of the lateral bands. Painful flexion
of the PIP joint can occur as the lateral bands sublux palmarly over
the proximal phalangeal condyles. Distinguish this swan-neck deformity
from the type of swan-neck deformity secondary to an extensor terminal
tendon disruption (mallet finger). With volar plate insufficiency, the
patient will be able to actively extend the DIP
joint
with the PIP joint held in full extension. Nonoperative treatment
includes use of a orthoplast or silver (double-ring) splint to help
prevent PIP joint hyperextension (Fig. 39.24). Symptomatic volar plate ruptures (Fig. 39.25)
can be helped by surgical correction. Options include late reattachment
or shortening of the volar plate, with or without some form of volar
reinforcement (1,7,12,22,72,78,91,104,109,132,136,144).
 |
|
Figure 39.24.
Silver ring (or double-ring) splint used for swan-neck deformity to prevent hyperextension at the PIP joint. The splint can be padded if it irritates the dorsum of the digit. |
 |
|
Figure 39.25. Chronic volar plate rupture in a basketball player; it subluxated each time he caught the ball.
|
-
Make a palmar zigzag incision and release the flexor sheath between the A2 and 4 pulleys.
-
Protect the digital vessels and nerves
while retracting the flexor tendons to expose the volar plate. If it
has been ruptured in midsubstance and repair is possible, suture the
edges directly. -
More often, it will be detached distally (Fig. 39.26A).
In that case, roughen the base of the middle phalanx and create a
transverse trough. Place a nonabsorbable suture in the distal end of
the volar plate with a modified Bunnell suture technique. Place drill
holes at the lateral margins of the trough in a distal but somewhat
lateral direction so that the extensor mechanism will not be injured or
trapped by the passing of the pullout suture. Pass the ends of the
suture from the volar plate through the drill holes, and tie them over
a protected button. To prevent tethering of the distal extensor
mechanism, flex the DIP joint 30° when passing the sutures dorsally. As
the suture is tied, flex the PIP joint. Apply gentle traction on the
suture so the distal end of the volar plate is pulled snugly into the
trough (Fig. 39.26B).![]() Figure 39.26. A: Volar plate rupture usually occurs distal from the base of the middle phalanx. B:
Figure 39.26. A: Volar plate rupture usually occurs distal from the base of the middle phalanx. B:
The distal margin of the volar plate is pulled snugly into a trough in
the middle phalanx and secured through drill holes in the bone. -
If there is not enough of the volar plate
left to advance or repair, a volar reinforcement procedure can be used.
With this technique, isolate either slip of the superficialis. Leave it
attached distally and detach it proximally under the A2 pulley. -
Place a drill hole transversely in the
neck of the proximal phalanx. Draw the proximal end of the detached
superficialis slip into the hole, using a pullout nonabsorbable suture,
and tie it over a protected button (Fig. 39.27).
P.1284
Take care to ensure that the superficialis slip is taut when the PIP joint is in 10° to 15° of flexion. Figure 39.27. One superficialis slip is fixed to the proximal phalanx, creating a tenodesis of the PIP joint.
Figure 39.27. One superficialis slip is fixed to the proximal phalanx, creating a tenodesis of the PIP joint. -
Temporarily fix the joint with a
0.035–0.045 smooth K-wire for 3 weeks, and then protect it with a
dorsal-block splint for an additional 4 weeks.
ruptures are the same as for dorsal PIP joint dislocations. Operative
repair for chronic volar plate ruptures, as for any ligament repairs or
reconstructions, can lead to some loss of motion and chronic
thickening. A flexion deformity is common.
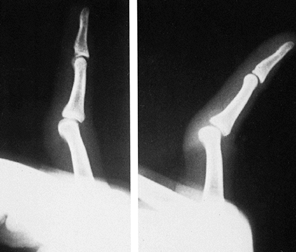
associated with an injury to the volar plate, collateral ligament, and
joint articular surface, which require adequate assessment and AP,
lateral, and oblique radiographs of the hand (Table 39.3).
A Brewerton view or oblique view of the metacarpal heads may be helpful
to identify small fractures (see the section above on General Principles of Treatment) (171,185,189,206). Open dislocations require adequate debridement and antibiotics.
 |
|
Table 39.3. Algorithm for Assessment of Metacarpophalangeal (MP) Joint Injuries
|
joints are uncommon. Most of these occur with the fingers in some
extension when the collateral ligaments are more lax. This provides
some margin for protection so that complete ligament rupture is
unusual. The most common mechanism of injury is hyperextension or ulnar
deviation of the joint. The most commonly involved joint is the index
finger, followed by the thumb and little finger. Central digit
dislocations are usually associated with dislocation of either the
adjacent index or little finger (42,151,153,154,156,170,177,180,182,187,188,195,200,202,211,212,216).
dislocations or collateral ligament injuries. The dislocations are
based on the direction of the dislocation (dorsal versus volar) and
whether they are easily reducible (simple) or irreducible without
surgical intervention (complex).
membranous portion of the volar plate usually ruptures off the
metacarpal neck. Dorsal MP dislocations can be classified as simple
(subluxation) or complex dislocations (165,172,174).
Simple MP joint dislocations are easily treated by closed reduction.
Take care not to converta simple dislocation into a complex dislocation
(165,172,176,190,383).
With simple MP joint dislocations, the proximal phalanx is
hyperextended on the metacarpal head, but some contact remains between
the MP joint articular surfaces. The proximal edge of the volar plate
lies palmarward over the metacarpal head. Therefore, the base of the
proximal phalanx should be pushed distally and palmarly. If
hyperextension with traction is mistakenly used, the volar plate can
slip dorsally over the metacarpal head and prevent reduction.
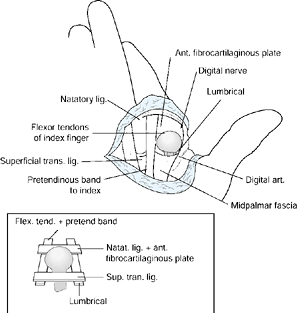
head and the base of the proximal phalanx makes this complex
dislocation irreducible (183). The lumbrical
medially and the flexor tendon laterally around the metacarpal neck
prevent reduction of the dislocation by longitudinal traction only (Fig. 39.28) (175).
With a complex dislocation of the little finger, the structures
preventing reduction include the abductor and flexor digiti minimi
ulnarly and the lumbrical and flexor tendon radially (154).
 |
|
Figure 39.28.
The factors producing a complex dorsal MP joint dislocation (see text for details). (From Kaplan EB. Dorsal Dislocation of the Metacarpophalangeal Joint of the Index Finger. J Bone Joint Surg 1957;39A:1081, with permission.) |
the phalanx appearing parallel to the metacarpal with a tendency for
the digit to overlap its neighbor (Fig. 39.29).
On the palmar surface, the skin is puckered or dimpled.
Radiographically, the joint space is widened, the joint surfaces are
offset, and the sesamoid appears to lie within the joint (Fig. 39.30) (163,175,201,208).
 |
|
Figure 39.29. Complex MP dislocation with the finger parallel to the metacarpal.
|
 |
|
Figure 39.30. The phalanx is offset at the MP joint, lying parallel to the metacarpal in a complex dislocation.
|
-
Attempt a single effort at a closed
reduction under a good anesthetic in the operating room with the wrist
flexed to relax the flexor tendons. -
Apply pressure dorsally and distally to
the base of the proximal phalanx while attempting to slide the proximal
phalanx over the metacarpal head. -
Confirm reduction clinically and
radiographically. Assess active and passive joint stability, splint the
hand with the MP joints flexed for a few days for comfort, and start
early active motion with an extension-block splint. If a closed joint
reduction fails, perform an open reduction.
-
Make a straight or slightly curvilinear dorsal incision over the joint.
-
Longitudinally release the extensor
tendon or the sagittal band (usually on the ulnar side) and perform a
dorsal midline capsulotomy. -
Identify and carefully incise
longitudinally the volar plate in the midline; avoid damaging the
metacarpal head articular surface. Flex the wrist to relax the flexor
tendon and reduce the joint. -
If needed, push the separate halves of the volar plate over and around the metacarpal head.
-
After the joint is reduced, separately
repair the capsule, the extensor tendon or sagittal band, and the skin.
Intraoperative postreduction radiographs should confirm congruous
reduction of the joint. -
As with a closed reduction, splint the
hand with the MP joints flexed for a few days and then begin active
motion with an extension-block splint.
-
Make an incision that connects the
mid-axial line with the transverse mid-palmar crease. Take great care
to avoid injury of the digital artery and nerve (especially the
radial), which are pressed against the deep surface of the skin by the
metacarpal head. Retract the nerves and arteries gently. -
Incise the A1 pulley and retract the flexor tendons and lumbrical. The metacarpal head now dominates the field (Fig. 39.31A).
![]() Figure 39.31. A:
Figure 39.31. A:
When the skin is opened before reduction, the metacarpal head dominates
the field. The flexor tendons lie ulnarly, the lumbrical and digital
nerve radially, and the volar plate dorsally, blocking reduction. B: The volar plate (held by the forceps) has been extricated and the joint reduced. -
Carefully make a longitudinal incision
between the sides of the volar plate and the deep transverse metacarpal
ligament. Insert a sturdy but narrow-angled dental probe or skin hook
around the volar plate to extricate it from between the phalangeal base
and the metacarpal head. The joint will snap into the reduced position (Fig. 39.31B). -
Because the volar plate is still attached to the phalanx, no repair is needed.
-
Repair the skin incision and splint the
hand with the MP joints flexed for a few days. Then start active
motion, preventing MP joint hyperextension with a dorsal-block splint
for 3–4 weeks.
may result either from a delay in treatment or from overly aggressive
treatment. Damage to the articular surfaces can occur with repeated
attempts at a closed reduction or secondary to a forceful open
reduction. Traction and hyperextension of the digit can possibly
convert a simple MP joint dislocation into a complex dislocation.
occur with delayed reduction. A combined volar and dorsal approach and
collateral ligament release may be needed to openly reduce a
longstanding dislocation (165,173,174,178,186,198,213).
Injury to the neurovascular bundles can occur in the palmar approach
with an inappropriate skin incision. Redislocation can occur if
hyperextension is not prevented, and loss of joint motion can occur
with prolonged immobilization.
from the metacarpal proximally or the volar plate from the proximal phalanx, or collateral ligament avulsion, can occur (159,197,203,215).
Interposition of these structures between the metacarpal head and
proximal phalanx can occur, producing a complex dislocation (174). If an attempt at a closed reduction under adequate anesthesia is unsuccessful, an open reduction is warranted.
missed. Since the collateral ligaments of the MP joint are at their
longest or most taut in full flexion, testing for collateral ligament
stability must be performed with the joint flexed maximally. The
mechanism of injury usually consists of forced ulnar deviation of the
digits. The injury seems to occur mostly in the ulnar three fingers and
to the radial side (166,172).
Clinically, tenderness is present over the injured ligament, and stress
testing (passive radial/ulnar deviation) with the MP joint flexed
produces pain. Obtain radiographs, including oblique and Brewerton
views (171,185,189,206,213), to identify avulsion fractures. Stress views with the MP joint in full flexion may help confirm a ligament tear (213). Arthrography has been used to identify the location of the collateral ligament injury (164,181). The collateral ligament is avulsed off the metacarpal head most commonly but can also be torn distally or in midsubstance (195,196,213).
with the MP joints flexed 30° to 50° for 3 weeks, followed by taping
the finger to the adjacent digit for an additional 3 weeks (167,172,174). Surgery is advocated for gross instability of the joint (60,61,164,181,205,217),
an associated displaced avulsion fracture (displaced 2 or 3 mm), or a
displaced or rotated avulsion fracture involving 20% or more of the
articular surface (174). With persistent joint instability, late reconstruction has been advocated (164,166,178).
-
Make a longitudinal incision in the dorsum of the web space on the affected side of the digit.
-
Incise and retract the transverse fibers
of the extensor hood. Incise the joint capsule dorsal to the collateral
ligament parallel to its dorsal margin. Dissect and mobilize the
ligament. -
If there is an attached avulsion fracture
of adequate size attached to the ligament, reduce and fix the bone
fragment with one or two smooth 0.035 K-wires (Fig. 39.32). Figure 39.32. A: A displaced articular fracture usually is attached to the collateral ligament. B: K-wire fixation of the displaced fracture often must be done by placing the wire in the phalanx first.
Figure 39.32. A: A displaced articular fracture usually is attached to the collateral ligament. B: K-wire fixation of the displaced fracture often must be done by placing the wire in the phalanx first. -
Close the transverse fibers of the hood
and skin in layers and check for congruous reduction of the joint and
adequate alignment of the fracture fragment with radiographs. -
Immobilize the hand with the MP joints
flexed to 45° for 3 weeks and protected by taping the finger to the
adjacent digit for another 3 weeks.
minimally symptomatic. If they prove disabling, surgical treatment can
be difficult. The same approach as previously described is used.
Carefully tease out the collateral ligament, and mobilize it to its
maximum length. Repair the ligament to the phalanx by the pullout
suture technique. Perform closure as previously described.
ruptures are usually due to undertreatment of the injury. They include
residual pain, joint swelling, instability (index finger with pinch),
and deviated digit (abducted little finger) (166,179,186,213).
tightly (i.e., collateral ligament repair with the joint held in
extension) will result in a loss of joint motion.
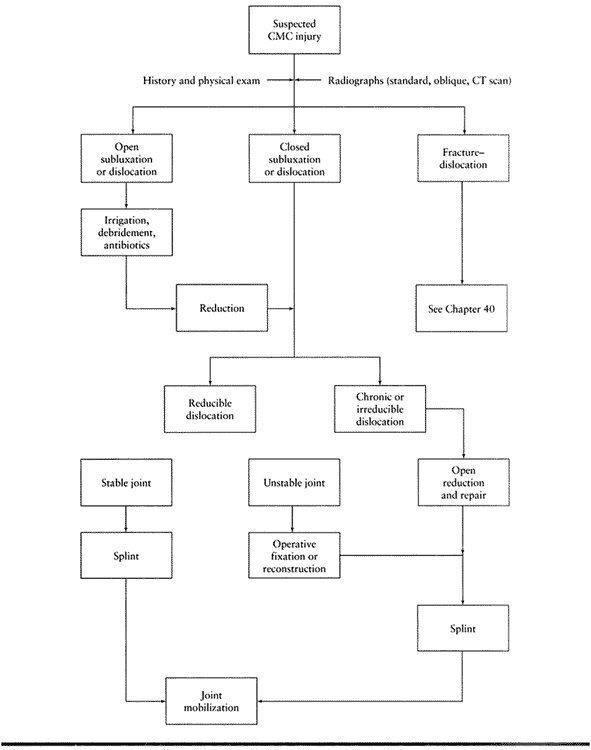
associated with intraarticular fractures, so adequate assessment of the
articular surfaces is needed with true AP, lateral, and oblique
pronated radiographs of the hand (Table 39.4).
Occasionally, tomography or a CT scan may be helpful to identify small
fractures. Open dislocations require adequate debridement and
antibiotics.
 |
|
Table 39.4. Algorithm for Assessment of Carpometacarpal (CMC) Joint Injuries
|
are virtually synonymous and will be considered together. Due to the
inherent stability of the CMC joints, which are further strengthened by
strong surrounding ligaments, pure CMC joint dislocations are uncommon;
fracture–dislocations of the CMC joints are much more common.
Isolated dorsal CMC dislocations or fracture–dislocations generally
occur when a longitudinal compressive force is applied to the dorsal
aspect of the metacarpal head. This force produces a longitudinal
compressive and flexion moment to the metacarpal. Occasionally, volar
CMC dislocations can occur (218,224,228,257,265,267,277).
Multiple CMC dislocations or dislocations of the index and long CMC
joints generally occur when larger forces produce the injury. These
injuries are frequently associated with metacarpal shaft fractures and
soft-tissue injuries (219,222,227,230,231,235,237,238,242 and 243,245,246,247,248 and 249,251,252 and 253,254,257,264,268,269,273,274,275 and 276,278,279 and 280).
A 30° pronated lateral view, which places the fourth and fifth CMC
joints in profile, will help in diagnosing dislocations or
fracture–dislocations of these joints (221,232,233,250). Tomography or CT scan can be used to further delineate the injury or help diagnose occult fractures (250).
include a closed reduction, closed reduction and percutaneous K-wire
fixation, and open reduction internal fixation of the dislocation (229,236,239,244). Closed reduction is usually possible.
-
With adequate analgesia, apply
longitudinal traction to the involved digit(s). Apply pressure over the
dorsal base of the dislocated metacarpal in a distal and volar
direction, then extend the metacarpal to help reduce the dislocated
joint. Occasionally, closed reduction will fail because of interposed
soft tissues or chondral fragments. -
If the reduction is successful,
immobilize the hand with the wrist extended, the MP joints flexed, and
the IP joints extended for 3–4 weeks. -
The CMC joint(s) must be frequently
evaluated for redislocation. Because of the possibility of
redislocation, closed reduction with percutaneous pinning is preferable
(227,228 and 229,235,236,238,247,259,271). -
Transfix the metacarpal to the
appropriate carpal or an adjacent stable metacarpal. Small associated
fractures with some articular incongruity are unimportant (270).
substantial intraarticular fracture is present and remains
significantly displaced after a closed reduction, do an open reduction.
Chronic dislocations usually require open reduction and internal
fixation. Extensive dissection with excision of scar tissue may be
necessary to achieve reduction. If symptomatic posttraumatic arthrosis
is present, a resection or resection–interposition arthroplasty is
useful, and an arthrodesis remains an option (220,221,223,225,226,229,234,236,241,245,246,254,255,258,260).
-
Make a dorsal longitudinal or oblique incision over the affected joint. Protect the dorsal sensory nerve branches and veins.
-
Retract the extensor tendons and
visualize the injured joint. Retract the ruptured ligaments and debride
any small loose fragments about the joint. Gently reduce the joint. -
Reduce any intraarticular fractures and
transfix them with one or two smooth 0.035–0.045 K-wires. If no
fracture is present, reduce the dislocation and secure it with a
0.035–0.045 smooth wire placed obliquely from the metacarpal across the
joint into the appropriate carpal bone or to an adjacent stable
metacarpal. -
Ligament repair is unnecessary, although capsular closure can be performed. Confirm reduction of the joint with radiographs.
-
Close the skin and splint the hand for
3–4 weeks, allowing full finger motion after the first few days. Remove
the pins at 6 weeks.
-
Use the same approach as described for an open reduction of an acute dislocation.
-
Incise and reflect the scarred ligaments
by subperiosteal dissection. Perform an open reduction of the joint if
the joint surfaces are preserved. Confirm proper position with
radiographs. -
If arthrosis is present, resect the
proximal 1 cm of the base of the metacarpal. A tendon anchovy or a
portion of the joint capsule may be interposed in the area of the
resected metacarpal. Repair the dorsal ligaments and close the skin.
Use K-wire fixation if the joint is unstable. Splint the hand for 3–4
weeks, but permit early finger motion.
take care to preserve the transverse metacarpal arch by fusing the
fourth and fifth metacarpals in some flexion.
Undertreatment may result in a redislocation of the CMC joint following
closed reduction alone or secondary to premature removal of fixation
wires.
protecting them is imperative. Improper pinning of metacarpals to
adjacent metacarpals can lead to a “pancake” hand from flattening of
the transverse metacarpal arch. Posttraumatic arthritis can occur with
poor surgical alignment of the carpometacarpal or intermetacarpal
joints.
different from that of the other digits. Like the finger MP joint, the
thumb MP joint is a condyloid joint allowing for flexion–extension and
abduction–adduction. The amount of thumb MP joint flexion varies
widely, ranging from 5° to 115° (356). Variable amounts of MP joint hyperextension can also occur, ranging up to 45° (average 8°) (285). The amount of MP joint abduction–adduction is less in the thumb than in the fingers (0° to 20°, average 10°) (296).
A slight difference in the shape between the proximal phalangeal
condyles produces a slight amount of pronation of the thumb with MP
flexion (285,308,373).
supported by strong collateral and accessory collateral ligaments as
well as a volar plate. The adductor pollicis inserts into the ulnar
sesamoid located within the volar plate, as well as the proximal
phalanx. The abductor pollicis brevis and flexor pollicis brevis insert
into the radial sesamoid, also located within the volar plate.
Additionally, the adductor and abductor pollicis brevis tendons have an
insertion or expansion into the extensor aponeurosis (328,370,371,376).
Further support to the MP joint is provided by extensor pollicis longus
and brevis tendons associated with the dorsal MP joint capsule and the
flexor pollicis longus tendon, overlying the volar plate and sesamoids,
volarly. Stability is therefore provided by both static and dynamic
restraints.
The longitudinal axes of each joint surface are oriented perpendicular
to one another, allowing flexion–extension, abduction–adduction, and
some pronation–supination (389,390,395).
An elongated volar lip of the thumb metacarpal provides an attachment
site for the volar metacarpal ligament to the tubercle of the
trapezium. Although it has a relatively loose capsular support,
thickenings in the joint capsule help provide joint stability. Four
ligaments have been frequently cited as the main stabilizers of the CMC
joint: the volar or anterior oblique (palmar trapeziometacarpal)
ligament, the dorsal (posterior) oblique ligament, the dorsoradial
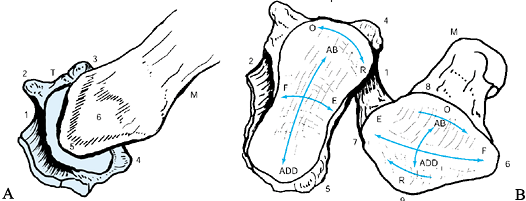
ligament, and the intermetacarpal ligament (386,387,389,392,399,402,404,406,408,409,411). Tubercles on both the metacarpal and trapezium serve as attachment sites for these ligaments (Fig. 39.33).
 |
|
Figure 39.33. A: Trapeziometacarpal joint seen from the volar side. T, trapezium; M, base of first metacarpal; 1, FCR tunnel; 2, radiovolar tubercle and ridge; 3, dorsoradial tubercle; 4, dorsoulnar tubercle; 5, volar metacarpal beak; 6, volar tubercle. B: Articular facets of the trapezium (T) and first metacarpal (M). 1, dorsal ligament; 2, FCR tunnel; 3, volar radial tubercle; 4, dorsoradial tubercle; 5, dorsoulnar tubercle; 6, volar metacarpal beak; 7, dorsal beak; 8, radial or lateral tubercle; 8, ulnar or medial tubercle. (From Zancolli EA, Cozzi EP. Atlas of Surgical Anatomy of the Hand. New York: Churchill-Livingstone, 1992, with permission.)
|
to those of the MP joint of the fingers. Thumb MP joint injuries are
frequently associated with collateral ligament and volar plate
injuries, as well as an occasional intraarticular fracture.
ligament injuries, and volar plate ruptures. The dislocations are based
on the direction of dislocation of the phalanx (dorsal versus volar)
and whether they are easily reducible (simple versus complex).
The dislocation results in a complete tear of the volar plate
proximally and usually of a portion of the collateral ligaments (377). Dorsal subluxation of the MP joint can occur with less severe hyperextension injuries (324). Volar MP dislocations are not as common (313,322,344,348,349,383).
Clinically and radiographically, hyperextension of the MP joint is
noted. Widening of the joint space is suggestive of soft-tissue
interposition. Interposition of the sesamoids between the metacarpal
head and the base of the proximal phalanx is highly suggestive of a
complex MP joint dislocation.
-
Perform closed reduction of the
dislocated joint under adequate analgesia with the wrist and IP joint
flexed to relax the flexor tendon. -
Avoid longitudinal traction and
hyperextension of the thumb MP joint, and push the base of the proximal
phalanx distally and palmarly. -
Confirm congruous reduction of the joint
on radiographs and test for active and passive joint stability. Test
for collateral ligament stability and treat accordingly (see sections
below on collateral ligament ruptures). -
Occasionally, dorsal dislocations may
prove to be irreducible because of interposition of the volar plate or
other structures (e.g., sesamoid, flexor pollicis longus) between the
base of the proximal phalanx and the head of the metacarpal (296,301,310,312,323,329,341,343,354). When this situation is present, do an open reduction. Volar (323,341), dorsal (160,301), and lateral (354) approaches to the MP joint have been advocated.
-
Make a chevron-shaped incision on the
radial aspect of the joint, bringing the apex of the incision somewhat
palmarly. Take care to not injure the digital nerves, especially the
radial. -
Partially release the proximal flexor tendon pulley and retract the flexor pollicis longus.
-
Make a longitudinal incision between the
radial collateral ligament and the edge of the volar plate. Place a
stiff-angled probe or a skin hook behind the volar plate, extricate it
from the joint, and allow the joint to reduce. -
Repair the ligament, if needed, either directly or using pullout suture technique.
-
Close the skin. Confirm congruous
reduction of the joint with radiographs. After initial immobilization
for comfort for a few days, begin motion using an extension-block
splint for 3–4 weeks.
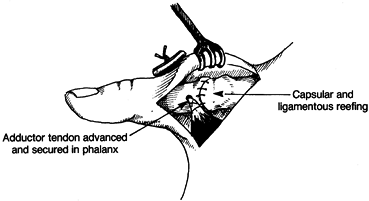
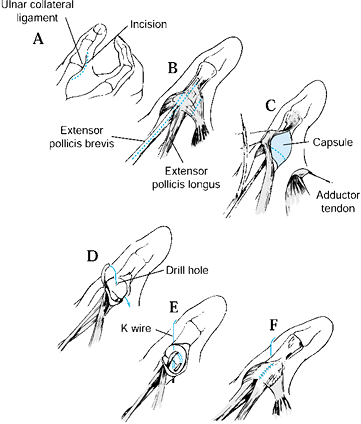
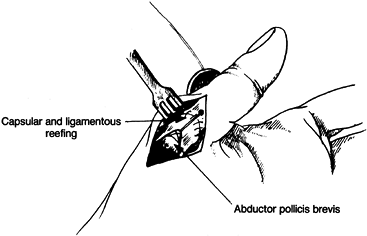
referred to as gamekeeper’s thumb and skier’s thumb, are common
injuries (289,295,296,304,305,325,343,345,346,351,368,371,385).
The mechanism of injury includes forceful abduction or radial deviation
of the thumb proximal phalanx. Other injured structures may include the
volar plate, the dorsal MP joint capsule, and the adductor aponeurosis,
or there may be an avulsion fracture of the proximal phalanx (289,293,296,297,304,305 and 306,322,327,329,333,340,343,347,357,362,371,376,378,379).
when there is interposition of the adductor aponeurosis between a
completely avulsed ulnar collateral ligament (avulsed from the proximal
phalanx) and the proximal phalanx ligament insertion site, or between
two ends of a midsubstance ligament tear (Fig. 39.34).
Interposition of the adductor aponeurosis interferes with healing of
the ulnar collateral ligament. Complete ligament avulsion is needed to
produce a Stener lesion; therefore, differentiating the complete from
partial ligament avulsion injury is necessary to diagnose a Stener
lesion. The reported incidence of a Stener lesion occurring with an
acute ulnar collateral ligament rupture varies with different series,
but it ranges from 14% to 83% (311).
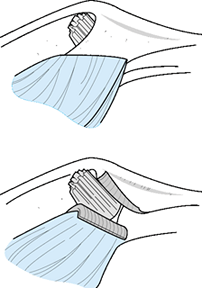 |
|
Figure 39.34.
The ulnar aspect of the metacarpophalangeal joint of the right thumb. After distal rupture, the ulnar collateral ligament has been folded right over. The torn end sticks out proximal to the adductor aponeurosis (shown divided in the lower picture). (From Stener B. Displacement of the Ruptured Ulnar Collateral Ligament of the Metacarpophalangeal Joint of the Thumb. A Clinical and Anatomic Study. J Bone Joint Surg 1962;44B:869, with permission.) |
tenderness over the region of the ulnar collateral ligament, with
instability when gently applying radial stress to the thumb MP joint (289,295,296,304,311,356,371,376). If there is no end point of resistance and angular deformation is more than 30° compared to the uninjured thumb (Fig. 39.35), a complete ulnar collateral ligament rupture is likely (289,304,318,355,356,372).
Perform the test with the MP joint in full extension and at 30° of
flexion. Palpation of the end of the ruptured collateral ligament is
difficult, but it confirms a complete ligament rupture (282).
Local or nerve-block anesthesia may be helpful in testing the
collateral ligament if there is significantpain or muscle spasm (289,304,311,329,340,347,356,357,368).
 |
|
Figure 39.35.
Complete instability to radial stress of the MP joint of the thumb. (From Neviaser RJ, Wilson JN, Lievano A. Rupture of the Ulnar Collateral Ligament of the Thumb—Correction by Dynamic Repair. J Bone Joint Surg 1971;53A:1357, with permission.) |
These tests should not be done in the presence of a significant
articular fracture but can be of value with a small avulsion fracture.
The fracture is not always attached to the ligament (Fig. 39.37), so the position of the fracture fragment does not always identify the location of the ruptured ligament end (320,338).
 |
|
Figure 39.36. Comparative stress radiographs showing instability of the left thumb.
|
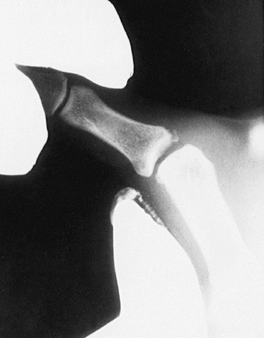 |
|
Figure 39.37. Stress radiograph in which “avulsion” fracture follows phalanx, suggesting it is not attached to the ligament.
|
repair provides the greatest security that a stable joint will result.
Theoretically, a complete ligament rupture without a Stener lesion can
be treated nonoperatively (296,360,376).
Because this lesion frequently cannot be determined by physical
examination, stress or plain radiographs, or arthrography, surgical
repair is usually recommended (30,60,61,296,304,306,310,322,329,337,340,343,344 and 345,349,352,355,371,376,379,382).
The ulnar collateral ligament can be directly repaired (midsubstance
tears) or reattached to bone by pullout suture technique, mini-suture
anchor, or absorbable tack, and by K-wires or tension-band wiring for
small avulsion fractures (286,288,308,326,332,363,366,381).
-
Make a chevron-shaped or curvilinear
incision on the ulnar side of the MP joint. Take care not to extend the
incision across the web space, which produces a contracting scar.
Carefully elevate the skin flaps, protecting the branches of the dorsal
radial sensory nerve. The torn ligament is usually seen at the proximal
edge of the adductor aponeurosis. -
Divide the adductor pollicis aponeurosis
just ulnar to its insertion into the extensor tendon and reflect it for
later repair. Remove loose bone fragments from the MP joint. -
Note the level of injury to the ulnar
collateral ligament. The ligament is typically avulsed distally from
its insertion into the proximal phalanx. A midsubstance ligament tear
may be directly repaired. Usually, the ulnar collateral ligament needs
to be mobilized. Place a 4-0 nonabsorbable suture in its distal end
using a modified Bunnell suture technique. -
Roughen the base of the proximal phalanx where the ligament is to be attached. Place one or two drill holes
P.1295
obliquely and through the opposite cortex. Place the ends of the
sutures through the drill hole(s) and through the skin. Reduce the MP
joint and tie the suture over a protected button. Alternatively, repair
the ligament using miniature suture anchors placed within the bone
trough (Fig. 39.23). -
Repair any rent in the dorsal capsule.
Place a suture in the volar ulnar corner of the volar plate–collateral
ligament complex to repair any tears in this region. -
If a small avulsed bone fragment is
present, excise the fragment and repair the ligament; or, if the
fragment is sufficiently large, repair it using K-wires or pullout
suture technique. -
Repair the adductor aponeurosis to the extensor mechanism and close the skin.
-
A K-wire can be used to transfix the MP joint, but it is usually not needed.
-
Immobilize the thumb in a spica cast for
4 weeks and then begin protected motion in a removable custom splint
for another 2–3 weeks. IP joint motion can be started earlier. Avoid
forceful stressing of the ligament repair for 3 months.
Treatment options include reefing or imbrication of the scarred
collateral ligament or reattaching a remnant of scarred tissue to the
proximal phalanx (60,61,346,348,357,379), dynamic tendon transfers (283,310,311,327,340,351,367,368), static tendon transfers (305,334,357,379), free tendon grafting (284,290,305,308,309,339,344,355,369,371,379), or MP fusion (304,333,337,343,352,357,371). Joint arthrodesis is generally recommended if posttraumatic arthritis is present (296,304,314,317,345,352) (see Chapter 72).
If the joint is not arthritic, the following reconstructive procedures
are valuable. There are, however, many other techniques using tendon
grafts (284,308,335,339,350,371,379).
-
Use the approach for the acute collateral ligament injury. Protect the digital nerves dorsally and palmarly (Fig. 39.38).
![]() Figure 39.38.
Figure 39.38.
Adductor pollicis advancement technique for chronic thumb ulnar
collateral ligament injury. Capsuloligamentous complex is reefed, and
the tendon of the adductor pollicis is advanced and inserted into a
drill hole in the mid-axial region of the proximal phalanx. -
Isolate and detach the major tendon of
insertion of the adductor pollicis. Leave enough tendinous tissue to
accept a pullout suture. -
Mobilize a broad, proximally based,
U-shaped flap on the metacarpal. Drill a bicortical hole in the ulnar
mid-axial line of the proximal phalanx, 10–12 mm distal to the joint.
Enlarge the opening on the ulnar side of the proximal phalanx to accept
the adductor tendon. -
With the joint reduced, imbricate or
advance the flap of scarred collateral ligament and suture it to the
residual soft tissue at the phalangeal base with a nonabsorbable suture. -
Place a nonabsorbable modified Bunnell
suture in the adductor tendon and pass it through the proximal phalanx
to exit percutaneously on the radial side. With the thumb adducted, tie
the suture over a protected button, making sure the adductor tendon is
pulled well into the ulnar hole of the phalanx. -
Repair the aponeurosis and skin
separately and immobilize the thumb in a spica cast for 4 weeks. Then
begin protected motion in a removable custom splint for another 2–3
weeks. Remove the button and pullout suture at 5–6 weeks. Avoid
forceful stressing of the ligament reconstruction for 3 months (351).
-
Use the approach for the acute collateral ligament injury (Fig. 39.39).
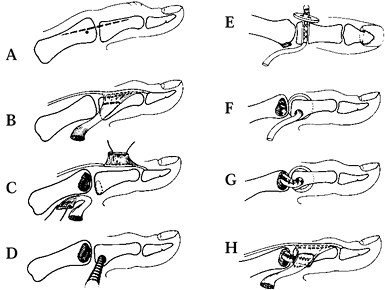 Figure 39.39.
Figure 39.39.
Free tendon graft technique for chronic thumb ulnar collateral ligament
injury. See text for details. (From Smith RJ. Posttraumatic Instability
of the Metacarpophalangeal Joint of the Thumb. J Bone Joint Surg 1977;59A:14, with permission.) -
Drill a hole transversely, in a radial to
ulnar direction, along the base of the proximal phalanx just distal to
the articular surface. -
Place the hole volar to the axis of joint
motion. Place a suture in the end of the free tendon graft and pass it
through the proximal phalanx to exit percutaneously on the radial side,
pulling the tendon through the ulnar hole. Tie the suture over a
protected button. -
Pull the remaining portion of the free
tendon graft to the metacarpal head. Make parallel longitudinal
incisions in the remnant of the collateral ligament. Secure the tendon
graft, with nonabsorbable sutures, to the metacarpal head by weaving
the graft through the ligament. -
Alternatively, place two holes in the
ulnar side of the metacarpal head, one dorsal and one volar. Pass the
tendon graft between the two holes and through an intramedullary
tunnel. Pass the remaining portion of the tendon graft distally back on
itself, parallel and volar to the other limb of the tendon graft.
Suture the two limbs of the tendon graft to one another. Repair and
imbricate, if needed, the adductor aponeurosis to the extensor
mechanism and then close the skin (371).
-
Use the approach for the acute collateral ligament injury (Fig. 39.40).
![]() Figure 39.40.
Figure 39.40.
Extensor pollicis brevis tendon transfer technique for chronic thumb
ulnar collateral ligament injury. See text for details. (From
Sakellarides HT, DeWeese JW. Instability of the Metacarpophalangeal
Joint of the Thumb. Reconstruction of the Collateral Ligament Using the
Extensor Pollicis Brevis. J Bone Joint Surg 1976;58A:106, with permission.) -
Transversely incise the scarred collateral ligament and create proximal and distal flaps.
-
Dissect and mobilize the extensor
pollicis brevis. Detach either half or all of the tendon distal to the
MP joint, leaving it proximally based. -
Drill two holes, one dorsally and one
medially, in the base of the proximal phalanx. Place a nonabsorbable
modified Bunnell suture in the extensor pollicis brevis tendon and pass
it through the dorsal hole, exiting medially. Suture the end of the
tendon to the remaining proximal stump of collateral ligament. If no
proximal metacarpal ligament stump is available, use a pullout suture
technique. Repair and imbricate any remaining portion of the collateral
ligament. -
Repair the adductor aponeurosis to the extensor mechanism and close the skin. Stabilize the MP joint with a K-wire, if needed (368).
ulnar collateral ligament injuries can result in chronic MP joint
instability with pain, loss of pinch strength, and, with time,
arthrosis (335,382).
injury and web space contractures can occur. A loose ligament repair
may leave a lax joint. Loss of joint motion is common following
ligament repair or reconstruction. Residual pain can persist from
unappreciated joint arthritis.
and is usually caused by forceful adduction, ulnar deviation, or
torsion of the thumb proximal phalanx. The radial collateral ligament
can be avulsed from either the base of the proximal phalanx or the
metacarpal head, or it can be attenuated in its midportion (294,300,371).
The dorsal joint capsule may also be torn. The thumb often lies in
ulnar deviation and slight pronation, a finding confirmed by
radiographs (Fig. 39.41). Without a radial
collateral ligament to provide stability, the proximal phalanx is
deviated ulnarly by the strong pull of the adductor pollicis. The
patient will have localized tenderness over the area of injury. The
metacarpal head may be prominent dorsoradially. Check with passive
ulnar stress of the MP joint with the joint in extension and at 30° of
flexion. Instability of greater than 30° as compared to the opposite
thumb, without a firm end point, is indicative of a complete tear of
the radial collateral ligament. Stress views of the MP joint may also
be helpful to determine the integrity of the ligament.
 |
|
Figure 39.41. Radial collateral ligament rupture leaves the phalanx subluxated ulnarly by the strong pull of the adductor pollicis.
|
until found in the chronic state. As with the ulnar collateral
ligament, treatment options include direct ligament repair (304,343,371),
reefing or imbrication of the scarred collateral ligament or
reattaching a remnant of scarred tissue to the proximal phalanx (294,310), dynamic tendon transfers (294,310,350,351), free tendon grafting (291,307,371),
or MP fusion. If there is posttraumatic arthritis, do an arthrodesis.
If the joint is not arthritic, use the following reconstruction (350,351).
-
Make a chevron incision on the radial side of the MP joint, protecting the dorsal radial sensory nerve.
-
Divide the abductor pollicis brevis
aponeurosis just radial to its insertion into the extensor tendon, and
reflect it for later repair. Repair the ligament either in midsubstance
or to either the proximal phalanx or metacarpal head, depending on the
area of injury. If the ends of the torn ligament are identifiable,
divide the capsule and ligament transversely and imbricate them. Repair
any capsular and extensor mechanism tears. -
Close the skin separately. Stabilize the
joint with a K-wire fixation if there is residual joint instability.
Postoperative treatment is similar to that for ulnar collateral
ligament tears.
-
Use the approach for the acute collateral
ligament injury. Detach the tendon of the abductor pollicis brevis with
sufficient length to hold a suture. -
Create a proximally based, U-shaped flap of scarred radial collateral ligament mass.
-
Drill a bicortical hole about 10–12 mm distal to the joint. Enlarge the radial hole with a curet.
-
Imbricate or reef the ligament flap with
the joint reduced. Pass a nonabsorbable suture through the abductor
pollicis brevis tendon using a modified Bunnell suture technique. Pass
both ends of the suture through the drill hole in the proximal phalanx
and out through the skin on the ulnar side. Tie the suture over a
protected button, making sure the tendon fits snugly in the radial hole
(Fig. 39.42).![]() Figure 39.42.
Figure 39.42.
Capsuloligamentous complex is reefed, and the tendon of the abductor
pollicis brevis is advanced to a drill hole on the radial side of the
phalanx in the mid-axial plane. -
Close the skin. Immobilize the thumb in a
spica cast for 4 weeks and then begin protected motion in a removable
custom splint for another 2–3 weeks. Remove the button and pullout
suture at 5–6 weeks. Avoid forceful stress on the ligament repair for 3
months.
collateral ligament injuries are the same as those listed under ulnar
collateral ligament tears described earlier.
common and can be diagnosed by eliciting tenderness over the volar
plate and detecting hyperextensibility of this joint (with the IP joint
flexed) compared to the opposite thumb (311,377).
Unlike the finger PIP joints, the volar plate detachment occurs
proximally from the metacarpal. Treat with dorsal-block splinting
(restricting the last 20° of extension) for 4 weeks.
For patients failing nonoperative measures, the operative options for
chronic MP joint instability include a volar plate capsulodesis (343,384), tenodesis (302,330), dynamic tendon transfer (361), or arthrodesis if arthritic changes are present.
-
Make a palmar zigzag incision and retract the digital arteries and nerves.
-
Incise the A1 pulley in its
proximal portion and retract the flexor pollicis longus. Incise the
intervals between the sides of the volar plate and the accessory
collateral ligaments. Release the distally based volar plate proximally
and excise the sesamoids subperiosteally. -
Using an osteotome or a dental chisel,
create a transverse trough in the metacarpal neck. Drill a hole through
each edge of the trough obliquely through the metacarpal. Perform a
trial reduction of the proximal edge of the volar plate into the
trough. When the plate is properly seated, passive extension of the MP
joint should be limited to 15° of flexion. If less flexion is evident,
trim a portion of the free edge of the volar plate and recheck the
position of the MP joint. -
Weave a nonabsorbable suture through the
free proximal edge of the plate, using a modified Bunnell technique.
Pass the suture ends through the drill holes and the skin and tie over
a protected button, thereby drawing the volar plate securely into the
trough. -
An alternative, but more difficult,
method includes creating a synostosis between the sesamoids and
metacarpal neck to produce a 15° to 20° flexion deformity of the MP
joint. Transfix the joint with a smooth K-wire to maintain the joint
position. -
Suture the accessory collateral ligaments to the edges of the volar plate with 5-0 nonabsorbable suture and close the skin.
-
Use a plaster thumb spica splint for 4
weeks, allowing IP joint flexion at 1 week. Remove the splint and pin
at 4 weeks. Begin exercises with an extension-block splint for 2 more
weeks, followed by removal of the button, suture, and splint.
Chronic instability can occur if hyperextension is not prevented for a
sufficient amount of time. Degenerative arthritis can occur after
chronic instability has developed (314).
permanent flexion contracture is common. Recurrent hyperextensibility
is the result of a loose capsulodesis, insecure fixation of the volar
plate to the proximal phalanx, or insufficient immobilization.
Sesamoid excision is performed through a volar approach to the MP joint
volar plate, with enucleation of the sesamoid through a longitudinal
incision in the volar plate (380).
with intraarticular fractures. To assess, take true AP and lateral
radiographs of the thumb CMC joint (Robert view) (403).
Dorsoradial subluxation of the CMC joint may indicate ligament injury.
Stress radiographs may be helpful in diagnosing instability of the
joint (392,393,395).
fracture are rare. Most dislocations occur dorsally. The mechanism of
injury is thought to be axial compression with a load on the metacarpal
in flexion (405,411). Disruption of the dorsal ligaments probably occurs to allow the joint to dislocate (398,410,411), but the volar ligament is intact and is subperiosteally stripped off the base of the metacarpal (388,413).
Clinically, a prominence is noted dorsoradially at the base of the
thumb metacarpal with the thumb held is an adducted position, similar
to that seen with a fracture–dislocation at the CMC joint.
reduction, with or without K-wire fixation, and thumb spica cast
immobilization (252,400,401,410,412).
-
Perform a closed reduction under adequate
analgesia using longitudinal traction, abduction, and extension of the
thumb. Place direct pressure on the base of the thumb metacarpal base,
displacing it distally, volarly, and ulnarly. -
Postreduction radiographs should confirm congruous reduction of the joint.
-
Immobilize in a thumb spica cast with the
thumb held in abduction and extension and pressure placed on the
dorsoradial aspect of the metacarpal base. With joint instability or
radiographic signs of persistent subluxation, add percutaneous
transarticular K-wire pinning. Remove the wires and cast at 6 weeks and
begin exercises.
the thumb CMC joint, instability and redislocation are common, and
early ligament reconstruction may be necessary. It is important to
monitor the patient radiographically after K-wire removal at frequent
intervals until it is certain that stability has been achieved.
with posttraumatic arthritis, arthroplasty or arthrodesis is preferred
(see Chapter 71, Chapter 72).
If there is no significant arthritic change, do a ligamentous
reconstruction. The most widely accepted technique uses the flexor
carpi radialis as described by Eaton (390,392,395).
-
Make an incision along the dorsoradial
margin of the thumb metacarpal and curve it palmarward as it approaches
the wrist flexor crease, ending over the flexor carpi radialis. Take
care to protect the sensory nerves (Fig. 39.43 and Fig. 39.44).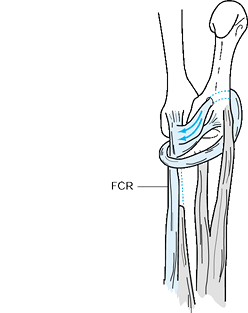 Figure 39.43. Stabilization of the trapeziometacarpal joint by half of the flexor carpi radialis (FCR).
Figure 39.43. Stabilization of the trapeziometacarpal joint by half of the flexor carpi radialis (FCR).![]() Figure 39.44. Using the accessory slip of the abductor pollicis longus (APL) to stabilize the trapeziometacarpal joint.
Figure 39.44. Using the accessory slip of the abductor pollicis longus (APL) to stabilize the trapeziometacarpal joint. -
Extraperiosteally elevate the thenar
muscle origin from the trapezium and metacarpal and retract it
distally. Incise the roof of the flexor carpi radialis tunnel and any
remaining volar radial CMC joint capsule. -
Longitudinally split half of the flexor
carpi radialis for 6 cm, leaving it distally based. Expose the proximal
portion of the tendon through transverse incisions over the tendon. -
Pass the tendon through the bone trough,
in a volar to dorsal direction, using a suture or wire to guide the
tendon through the trough. Reduce and pin the joint with a smooth
K-wire, avoiding the tendon slip. -
Pull the tendon slip taut and suture it to the dorsal periosteum of the metacarpal.
-
Redirect the tendon slip beneath the
extensor pollicis brevis and abductor pollicis longus proximally across
the joint and back under the remaining intact portion of the flexor
carpi radialis. Turn the tendon slip back to the palmar periosteum of
the metacarpal, and suture it there. Place additional sutures wherever
the tendon slip changes direction. -
Close the skin and immobilize the thumb
in a thumb spica cast for 4 weeks. Remove the K-wire and protect the
thumb for an additional 2 weeks with a removable thumb spica splint.
Start active exercises, but do not expect maximal return of motion for
up to 4–6 months. -
An alternative to using the flexor carpi
radialis tendon is to use one of the slips of the abductor pollicis
longus. The most common insertion for the commonly present second slip
is into the trapezium (407). This natural anchor can be used to advantage. -
Make a longitudinal incision starting
along the dorsal ulnar side of the proximal third of the first
metacarpal, curve it palmarward over the trapezium, and continue it
along the anterior border of the first dorsal compartment. -
Dissect free an 8 cm distally based slip of the abductor pollicis longus attached to the trapezium.
-
Use a drill or gouge to make a
dorsal-to-palmar hole in the metacarpal parallel but distal to the
trapeziometacarpal joint. Pass the slip of abductor pollicis longus
tendon through the hole using a suture attached to the end of the
tendon slip. -
Reduce the joint and tighten the tendon. Loop the tendon back on itself and suture to its trapezial insertion.
-
Reinforce the new “ligament” by spreading
it out and suturing it to the capsule on each side of the tendon
wherever it crosses the joint. -
Pin the joint with a smooth K-wire if
necessary. Immobilize the thumb in a thumb spica splint or cast for 6
weeks. When the cast and pin are removed, begin exercises (392).
dislocations are usually the result of failing to identify the injury.
Failing to immobilize an incomplete ligament injury can lead to
persistent joint instability, requiring ligament reconstruction (391,392). Failingto recognize a complete dislocation will require an open reduction and ligament reconstruction (391,392,414). Persistent instability may lead to symptomatic joint arthritis requiring arthrodesis or arthroplasty (see Chapter 71, Chapter 72). Persistent subluxation can result if the new ligament is not tightened sufficiently with the joint reduced.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
JM. Unstable Fracture Dislocations of the Proximal Interphalangeal
Joints of the Fingers: A Preliminary Report of a New Treatment
Technique.J Hand Surg 1978;3:386.
JM, Linscheid RL. Simultaneous Dorsal Dislocation of the
Interphalangeal Joints in a Finger. Case Report and Review of the
Literature. Orthopedics 1988;11:1079.
MB, Johannsen H. Double Dislocation of the Interphalangeal Joints in
the Finger. Case Report and Review of Publications. Scand J Plast Reconstr Hand Surg 1993;27:233.
ZJ, Vender MI, Bonavolonta M, Knutson K. Fracture Subluxation of
Proximal Interphalangeal Joint Treated by Palmar Plate Advancement. J Hand Surg 1994;19A:189.
WH, Wolf JW Jr, Nehil J, Bittinger S. The Proximal Interphalangeal
Joint Volar Plate. I. An Anatomical and Biomechanical Study.J Hand Surg 1980;5:79.
JC, Conners JJ, Franco RS. Irreducible Palmar Dislocation of the
Proximal Interphalangeal Joint with Bilateral Avulsion Fractures.J Hand Surg 1990;15A:460.
RY, Hurst LC, Leppard J, Dick HM. Complex Dislocations of the Proximal
Interphalangeal Joint. A Pathoanatomic Classification of the Injury. Orthop Rev 1984;13:21.
A, Smith J, Redding M, Akelman E. Acute Open Reduction and Rigid
Internal Fixation of Proximal Interphalangeal Joint Fracture
Dislocation. J Hand Surg 1992;17A:512.
DW, Quinton DN. Dorsal Fracture Subluxation of the Distal
Interphalangeal Joint of the Finger and the Interphalangeal Joint of
the Thumb Treated by Extension Block Splintage.J Hand Surg 1992;17B:591.
TB. Long Flexor Tendon Entrapment Causing Open Irreducible Dorsoradial
Dislocation of the Distal Interphalangeal Joint of the Finger.Orthop Rev 1982;11:117.
H, Ninomiya S, Okutsu I, et al. Dynamic External Finger Fixator for
Fracture Dislocation of the Proximal Interphalangeal Joint. J Hand Surg 1993;18A:160.
FG, Greene MH. Another Cause of Irreducible Dislocation of the Proximal
Interphalangeal Joint of a Finger: A Case Report. J Bone Joint Surg 1966;48A:542.
NF, Jupiter JB. Irreducible Palmar Dislocation of the Proximal
Interphalangeal Joint Associated with an Epiphyseal Fracture of the
Middle Phalanx.J Hand Surg 1985;10A:261.
JM, Berrettoni BA, Seitz WH Jr, et al. The Figure-of-Eight Splint for
Proximal Interphalangeal Joint Volar Plate Injuries. Orthop Rev 1992;21:457.
EC, Dobyns JH, O’Brien ET. Management of Fracture-Dislocation of the
Proximal Interphalangeal Joints by Extension-Block Splinting.J Bone Joint Surg 1972;54A:1705.
JP, Gordon DA, King MS, et al. Dynamic Digital Traction for Unstable
Communited Intra-articular Fracture-Dislocations of the Proximal
Interphalangeal Joint. J Hand Surg 1995;20A:565.
RJ, Wilson JN. Interposition of the Extensor Tendon Resulting in
Persistent Subluxation of the Proximal Interphalangeal Joint of the
Finger. Clin Orthop 1972;83:118.
MA, Wilenski M. Irreducible Volar Dislocation of the Proximal
Interphalangeal Joint of a Finger Caused by Interposition of an Intact
Central Slip.J Bone Joint Surg 1978;60A:133.
I, Williams JT. Rupture of a Collateral Ligament of the Proximal
Interphalangeal Joint of the Finger: Analysis of 18 Cases.J Bone Joint Surg 1967;49A:322.
MB, Greenfield GQ. Irreducible Dorsal Dislocation of the Small Finger
Distal Interphalangeal Joint: The Importance of Roentgenograms—Case
Report.J Trauma 1991;31:1450.
M, Choi BY. Anterior Dislocation of the Proximal Interphalangeal Joint:
A Cause of Rupture of the Central Slip of the Extensor Mechanism. J Bone Joint Surg 1970;52A:1329.
WD. Displaced Intra-articular Osteochondral Fracture—Cause for
Irreducible Dislocation of the Distal Interphalangeal Joint. J Hand Surg 1982;7:77.
RS, David HG. The Doorstop Procedure. A Technique for Treating Unstable
Fracture Dislocations of the Proximal Interphalangeal Joint. J Hand Surg 1993;18B:714.
SF. Extension Block Pinning for Proximal Interphalangeal Joint Fracture
Dislocations: Preliminary Report of a New Technique. J Hand Surg 1992;17A:6.
MS, Barenfield PA, Eisenstein AL. Simultaneous Dorsal Dislocation of
Both Interphalangeal Joints in a Finger. A Case Report. J Bone Joint Surg 1978;60A:1142.
JN, Rowland SA. Fracture-dislocation of the Proximal Interphalangeal
Joint of the Finger: Treatment by Open Reduction and Internal Fixation.
J Bone Joint Surg 1966;48A:493.
NP, Stark HH, Ashworth CR, Boyes JH. Chronic Fracture Dislocations of
the Proximal Interphalangeal Joint—Treated by Osteotomy and Bone Graft.J Hand Surg 1981;6:447.
GA, Light TR. Simultaneous Complex Dislocation of the
Metacarpophalangeal Joints of the Long and Index Fingers: A Case
Report. J Bone Joint Surg 1981;63A:1007.
LW, Miller DL, Lockhart D, Evans EB. Metacarpophalangeal Joint
Dislocations of the Fingers. A Comparison of the Pathological Anatomy
of the Index and Little Finger. J Bone Joint Surg 1967;49A:1587.
PA, Wesley MS. Dorsal Dislocation of the Metacarpophalangeal Joint of
the Index Finger Treated by Late Open Reduction. J Bone Joint Surg 1972;54A:1311.
K, McGee H, Curtin J. Complex Dislocation of the Metacarpophalangeal
Joint of the Index Finger. A Comparison of the Surgical Approaches. J Hand Surg 1988;13B:466.
JL, Christian JD Jr, Goodwin HN, Jackson JG. A Simplified Technique for
Treating the Complex Dislocation of the Index Metacarpophalangeal Joint.J Bone Joint Surg 1975;57A:698.
RR, Browne EZ, Perry GB, Resnick EJ. The Complex Volar
Metacarpophalangeal Joint Dislocation. A Case Report and Review of the
Literature. J Bone Joint Surg 1982;64A:1374.
PG, Gelberman RH, Vandell RF, Salamon PB. Complex Dislocations of the
Metacarpophalangeal Joint: Operative Reduction by Farabeuf’s Dorsal
Incision. Clin Orthop 1982;164:208.
JR, Atkinson RE. Rupture of the Radial Collateral Ligament of the
Metacarpo-phalangeal Joint of the Index Finger: A Report of Three Cases.J Hand Surg 1989;14B:248.
G, Millender LH, Nalebuff EA. Rupture of the Radial Collateral Ligament
of a Metacarpophalangeal Joint to One of the Ulnar Three Fingers.J Hand Surg 1979;4:346.
TC, Pho RWH. Avulsion-Fracture at the Proximal Attachment of the Radial
Collateral Ligament of the Fifth Metacarpophalangeal Joint—A Case
Report.J Hand Surg 1982;7:526.
RE Jr, Gleason TF, Kasa RF. Simultaneous Closed Dislocations of the
Metacarpophalangeal Joints of the Index, Long, and Ring Fingers: A Case
Report. J Hand Surg 1985;10A:81.
JC, Watts HB, Glasgow JD. Dorsal Dislocation of the Metacarpophalangeal
Joint of the Index Finger with Particular Reference to Open
Dislocation. J Bone Joint Surg 1967;49A:1572.
JW Jr, Rohrich RJ, Sheppard JS. Closed Complex Dorsal Dislocation of
the Middle Finger Metacarpophalangeal Joint: Anatomic Dissection
Considerations and Treatment. Plast Reconstr Surg 1988;82:690.
R, Sadler AH. An Isolated, Closed, Complex Dislocation of the
Metacarpophalangeal Joint of the Long Finger: A Unique Case.J Hand Surg 1986;11A:558.
Ruiz G, Combolia Alue A, Valer Tito A, et al. Simultaneous Subluxation
of the Metacarpophalangeal Joints of all Four Fingers: A Case Report. J Hand Surg 1985;10A:78.
SF, Heare TC, Calhoun JH. Complex Fracture Dislocation of a Fifth
Metacarpophalangeal Joint: Case Report and Literature Review.J Trauma 1989;29:521.
JS Jr, Kamionek S, Weiss AC, Akelman E. The Surgical Approach in
Non-Border Digit Complex Dislocations of the Metacarpophalangeal Joint.
Orthop Rev 1994;23:601.
EE, Murphy DF. Ulnopalmar Dislocation of the Fifth Carpometacarpal
Joint—Successful Closed Reduction: Review of the Literature and
Anatomic Reevaluation. J Hand Surg 1986;11A:521.
BJ, Stark HH, Ashworth CR, et al. Tendon Interposition Arthroplasty of
the Fifth Carpometacarpal Joint for Treatment of Posttraumatic
Arthritis.J Hand Surg 1991;16A:520.
WB, Grantham SA. Multiple Volar Carpometacarpal Joint Dislocations.
Case Report of Traumatic Volar Dislocation of the Medial Four
Carpometacarpal Joints in a Child and Review of the Literature. J Hand Surg 1978;3:377.
RM, Seitz WH Jr. Post-traumatic Arthrosis of the Index Carpometacarpal
Joint. A Rationale for Treatment and Report of Two Cases. Orthopedics 1987;10:1429.
PJ, Quinlin W. Fracture Dislocation of the Fifth Metacarpal Resulting
in Compression of the Deep Branch of the Ulnar Nerve. J Hand Surg 1993;18B:190.
MV, Stark HH. Dorsal Dislocation of the Fourth and Fifth
Carpometacarpal Joints and Simultaneous Dislocation of the
Metacarpophalangeal Joint of the Small Finger: A Case Report.J Hand Surg 1984;9A:714.
RL, Yancey AG. Carpometacarpal Dislocations, With Particular Reference
to Simultaneous Dislocation of the Bases of the Fourth and Fifth
Metacarpals. J Bone Joint Surg 1948;30A:397.
AJ, Lister GD, Villarreal-Rios A. Volar Fracture Dislocations of the
Second and Third Carpometacarpal Joints Associated with Acute Carpal
Tunnel Syndrome.J Trauma 1976;16:672.
S-O, Sollerman C, Lundborg C, et al. Diagnosis of Displaced Ulnar
Collateral Ligament of the Metacarpophalangeal Joint of the Thumb.J Hand Surg 1990;15:457.
JC, Tan AM, Van Thiel TPH, Daantje CRE. Free Tendon Grafting to Repair
the Metacarpophalangeal Joint of the Thumb. Surgical Techniques and a
Review of 70 Patients. J Bone Joint Surg 1989;71B:383.
AJ, Koniuch MP, van Holsbeeck M. Ultrasonographic Detection of Thumb
Ulnar Collateral Ligament Injuries: A Cadaveric Study. J Hand Surg 1994;19A:304.
RW, Goldner JL. A Study of the Pathological Findings and Treatment in
Soft-Tissue Injury of the Thumb Metacarpophalangeal Joint. J Bone Joint Surg 1968;50A:439.
EF Jr, Curtis DJ. Patient-Induced Stress Test of the First
Metacarpophalangeal Joint: A Radiographic Assessment of Collateral
Ligament Injuries. Radiology 1986;158:679.
J, Ganel A, Ditzian R, Militeanu J. Arthrography as a Method of
Diagnosing Tear of the Ulnar Collateral Ligament of the
Metacarpophalangeal Joint of the Thumb (“Gamekeeper’s Thumb”). J Trauma 1979;19:106.
G, Johansson O. Surgical Repair of Rupture of the Ulnar Collateral
Ligament of the Metacarpophalangeal Joint of the Thumb. Acta Chir Scand 1956;112:58.
C, Senn E, Matter P. Skier’s Thumb. Surgical Treatment of Recent
Injuries to the Ulnar Collateral Ligament of the Thumb’s
Metacarpophalangeal Joint. Am J Sports Med 1981;9:171.
SZ, Malerich M, Pearce SM, Littler JW. Ligament Replacement for Chronic
Instability of the Ulnar Collateral Ligament of the Metacarpophalangeal
Joint of the Thumb.J Hand Surg 1993;18A:930.
K, Mittler C, Oser W. Ulnar Collateral Ligament: Differentiation of
Displaced and Nondisplaced Tears with US and MR Imaging. Radiology 1995;194:65.
P, Gelberman RH, Duncan K, Hipp JA. Injuries of the Ulnar Collateral
Ligament of the Thumb Metacarpophalangeal Joint—Biomechanical and
Prospective Clinical Studies on the Usefulness of Valgus Stress
Testing. Clin Orthop 1993;292:165.
DH, Erickson SJ, Chamoy L, Timins ME. Ulnar Collateral Ligament of the
Thumb: MR Findings in Cadavers, Volunteers, and Patients with
Ligamentous Injury (Gamekeeper’s Thumb). AJR Am J Roentgenol 1994;163:1431.
EB. The Pathology and Treatment of Radial Subluxation of the Thumb with
Ulnar Displacement of the Head of the First Metacarpal. J Bone Joint Surg 1961;43A:541.
DS, Huebner JJ Jr, Hankin FM. Rupture and Displacement of the Ulnar
Collateral Ligament of the Metacarpophalangeal Joint of the Thumb:
Preoperative Diagnosis.J Bone Joint Surg 1986;68A:1320.
IM, Dinkhauser LM, Orthner E, et al. Ulnar Collateral Ligament:
Differentiation of Displaced and Nondisplaced Tears with US. Radiology 1995;194:61.
MA, Langa V, Ambrose L. Intrinsic Muscle Advancement to Treat Chronic
Palmar Instability of the Metacarpophalangeal Joint of the Thumb. J Hand Surg 1988;13A:110.
JP, Phair IC, Quinton DN. Ulnar Collateral Ligament Repair of the
Metacarpophalangeal Joint of the Thumb: A Study Comparing Two Methods
of Repair. J Hand Surg 1992;17B:160.
HT. The Surgical Treatment of Old Injuries of the Collateral Ligaments
of the MP Joint of the Thumb Using the Extensor Pollicis Brevis Tendon
(A Long Term Follow-up of 100 Cases). Bull Hosp Joint Dis Orthop Inst 1984;44:449.
HT, DeWeese JW. Instability of the Metacarpophalangeal Joint of the
Thumb. Reconstruction of the Collateral Ligament Using the Extensor
Pollicis Brevis. J Bone Joint Surg 1976;58A:106.
C, Abrahamsson S, Lundborg G, Adalbert K. Functional Splinting Versus
Plaster Cast for Ruptures of the Ulnar Collateral Ligament of the
Thumb. A Prospective Randomized Study of 63 Cases. Acta Orthop Scand 1993;62:524.
HJ, Abrams RA, Bock GW, et al. Gamekeeper Thumb: Differentiation of
Nondisplaced and Displaced Tears of the Ulnar Collateral Ligament with
MR Imaging. Radiology 1993;188:553.
B. Displacement of the Ruptured Ulnar Collateral Ligament of the
Metacarpophalangeal Joint of the Thumb. A Clinical and Anatomic Study. J Bone Joint Surg 1962;44B:869.
B. Hyperextension Injuries to the Metacarpophalangeal Joint of the
Thumb—Rupture of Ligaments, Fracture of Sesamoid Bones, Rupture of the
Flexor Pollicis Brevis. An Anatomical and Clinical Study. Acta Chir Scand 1963;125:275.
B. Skeletal Injuries Associated with Rupture of the Ulnar Collateral
Ligament of the Metacarpophalangeal Joint of the Thumb. A Clinical and
Anatomic Study. Acta Chir Scand 1963;125:583.
G. Total Rupture of the Ulnar Collateral Ligament of the
Metacarpophalangeal Joint of the Thumb. Result of Surgery in 35 Cases. Acta Chir Scand 1959;118:72.
K, Juutilainen T, Patiala H, et al. Reinsertion of the Ruptured Ulnar
Collateral Ligament of the Metacarpophalangeal Joint With an Absorbable
Self-Reinforced Polylactide Tack. J Hand Surg 1993;18B:200.
RG, Lane LB, Littler JW, et al. Ligament Reconstruction for the Painful
Thumb Carpometacarpal Joint: A Long Term Assessment. J Hand Surg 1984;9A:692.
RJ, Behrman MJ, Rossenwasser MP. Acute Dislocation of the
Carpometacarpal Joint of the Thumb: An Anatomic and Cadaver Study. J Hand Surg 1994;19A:93.
JT, Chandra D, Satku K. Simultaneous Dislocations of the
Interphalangeal and Carpometacarpal Joints of the Thumb: A Case Report.
J Hand Surg 1988;13B:224.